FEDERAL COURT OF AUSTRALIA
Al Muderis v Nine Network Australia Pty Limited (Trial Judgment) [2025] FCA 909
File number(s): | NSD 917 of 2022 |
Judgment of: | ABRAHAM J |
Date of judgment: | 8 August 2025 |
Catchwords: | DEFAMATION – where the applicant is a well-known orthopaedic surgeon – where applicant sues in defamation over a 60 Minutes program broadcast by Nine Network – where publications televised, published online and in print – where 75 defamatory imputations alleged DEFAMATION – defences – substantial truth – justification defence – s 25 of the Defamation Act 2005 (NSW) – where imputations conveyed may be summarised into 9 stings – imputations involving improper sales tactic, misleading osseointegration patients, poor patient selection, negligent post-operative care, illegal procedures in the United States, prioritising money, fame, reputation and numbers, mistreating staff, lying to journalists, unethical conduct case DEFAMATION – defences – contextual truth – s 26 of the Defamation Act 2005 (NSW) – some imputations established as substantially true – whether imputations not substantially true or where there is no truth defence do not further harm the applicant’s reputation – contextual truth considers the facts, matters and circumstances relied upon to support the substantial truth of the contextual imputations rather than the terms of the imputation – defence established
DEFAMATION – defences – public interest – s 29A of the Defamation Act 2005 (NSW) – consideration of legislative construction – whether the respondents reasonably believed the matters published was in the public interest – flaws in a matter will not necessarily preclude the defence – inform prospective patients about a cohort of the applicant’s patients who had negative experiences – defence established EVIDENCE – observation as to fact-finding, onus and standards of proof – inferences in relation to the failure of a party to call a particular witness: Jones v Dunkel [1959] HCA 8; (1959) 101 CLR 298 – principles in Browne v Dunn (1893) 6 R 67 (HL) – consideration of contemporaneous documents – consideration of standard practice and inferences that may be drawn – consideration of the impact of mental health issues and trauma on the reliability of evidence |
Legislation: | Competition and Consumer Act 2010 (Cth), Sch 2, Australian Consumer Law, ss 18, 21(4), 33, 54 Evidence Act 1995 (Cth) ss 63, 64, 79, 126K, 140, 164(1), 174 Defamation Act 2005 (NSW) ss 3(b), 4, 8, 25, 26, 29A, 30(4), 31 Defamation Act 1974 (NSW) (repealed) s 16 Defamation Act 2013 (UK) s 1, 4 Fla Stat § 456.065 Ky Rev Stat Ann § 311.560 (2017) La Rev Stat Ann § 37:1271 (2018) Medical Practice Act of 1987, 225 Ill Comp Stat 60/3, 60/3.5, 60/50, 60/59 (2017) NY Education Law §§ 6512, 6520-6521 (2018) NY Public Health Law (2018) Federal Court Rules 2011 (Cth) r 23.13 Explanatory Note, Defamation Amendment Bill 2020 (NSW) |
Cases cited: | Allen v Tobias [1958] HCA 13; (1958) 98 CLR 367 Allianz Australia Insurance Limited v Delor Vue Apartments CTS 39788 [2021] FCAFC 121; (2021) 287 FCR 388 Allied Pastoral Holdings Pty Ltd v Federal Commissioner of Taxation [1983] 1 NSWLR 1; (1983) 44 ALR 607 Al Muderis v Nine Network Australia Pty Limited [2023] FCA 1623 Al Muderis v Nine Network Australia Pty Limited (No 2) [2024] FCA 136 Ange v Fairfax Media Publications Pty Ltd & Ors [2010] NSWSC 645 Australian Broadcasting Corporation v Chau Chak Wing [2019] FCAFC 125; (2019) 271 FCR 632 Australian Competition and Consumer Commission v Delta Automation Pty Ltd [2023] FCA 880 Axent Holdings Pty Ltd t/a Axent Global v Compusign Australia Pty Ltd [2020] FCA 1373 Banks v Cadwalladr [2019] EWHC 3451 (QB) Banks v Cadwalladr [2022] EWHC 1417 (QB); [2022] 1 WLR 5236 Banks v Cadwalladr [2023] EWCA Civ 219; [2023] 3 WLR 167 Banque Commerciale S.A., En Liquidation v Akhil Holdings Ltd [1990] HCA 11; (1990) 169 CLR 279 Bathurst Regional Council v Local Government Financial Services Pty Ltd (No 5) [2012] FCA 1200 Besser v Kermode [2011] NSWCA 174; (2011) 81 NSWLR 157 Betfair Pty Limited v Racing New South Wales [2010] FCAFC 133; (2010) 189 FCR 356 Boyd v Mirror Newspapers Ltd [1980] 2 NSWLR 449 Bridges v Pelly [2001] NSWCA 31 Briginshaw v Briginshaw [1938] HCA 34; (1938) 60 CLR 336 Browne v Dunn (1893) 6 R 67 Capic v Ford Motor Company of Australia Pty Ltd [2021] FCA 715 CCL Secure Pty Ltd v Berry [2019] FCAFC 81 Chakravarti v Advertiser Newspapers Ltd [1998] HCA 37; (1998) 193 CLR 519 Channel Seven Sydney Pty Ltd v Mahommed [2010] NSWCA 335; (2010) 278 ALR 232 Chau v Australian Broadcasting Corporation (No 3) [2021] FCA 44; (2021) 386 ALR 36 Chau v Fairfax Media Publications Pty Ltd [2019] FCA 185 Commercial Union Assurance Company of Australia Ltd v Ferrcom Pty Ltd (1991) 22 NSWLR 389 Connor v Blacktown District Hospital [1971] 1 NSWLR 713 Cubillo v Commonwealth (No 2) [2000] FCA 1084; (2000) 103 FCR 1 Dasreef Pty Ltd v Hawchar [2011] HCA 21; (2011) 243 CLR 588 Deeming v Pesutto (No 3) [2024] FCA 1430 Deputy Commissioner of Taxation v Shi [2021] HCA 22; (2021) 273 CLR 235 Drummoyne Municipal Council v Australian Broadcasting Corporation (1990) 21 NSWLR 135 Duma v Fairfax Media Publications Pty Ltd (No 3) [2023] FCA 47 Edwards v Nine Network Australia Pty Ltd (No 5) [2024] FCA 422 Elliott v The Queen [2007] HCA 51; (2007) 234 CLR 38 ET-China.com International Holdings Ltd v Cheung [2021] NSWCA 24 Fairfax Digital Australia & New Zealand Pty Ltd v Kazal [2018] NSWCA 77; (2018) 97 NSWLR 547 Fairfax Media Publications Pty Ltd v Gayle [2019] NSWCA 172; (2019) 100 NSWLR 155 Farquhar v Bottom [1980] 2 NSWLR 380 Favell v Queensland Newspapers Pty Ltd [2005] HCA 52; (2005) 219 CLR 165 Flood v Times Newspapers Ltd [2010] EWCA Civ 804; [2011] 1 WLR 153 Fonterra Brands (Australia) Pty Ltd v Viropoulos (No 3) [2015] FCA 1050 Ford v Narrabri Shire Council [2022] NSWPIC 119 Fox v Percy [2003] HCA 22; (2003) 214 CLR 118 GLJ v The Trustees of the Roman Catholic Church for the Diocese of Lismore [2023] HCA 32; (2023) 97 ALJR 857 Greek Herald Pty Ltd v Nikolopoulos & Ors [2002] NSWCA 41; (2002) 54 NSWLR 165 Griffiths v TUI (UK) Ltd [2023] UKSC 48; (2023) 3 WLR 1204 Habib v Nationwide News Pty Ltd [2010] NSWCA 34; (2010) 76 NSWLR 299 Haddon v Forsyth [2011] NSWSC 123 Hanson v Burston [2023] FCAFC 124; (2023) 413 ALR 299 Harvey v John Fairfax Pty Ltd [2005] NSWCA 255 Herron v HarperCollins Publishers Australia Pty Ltd [2022] FCAFC 68; (2022) 292 FCR 336 Hockey v Fairfax Media Publications Pty Limited [2015] FCA 652; (2015) 237 FCR 33 House v King [1936] HCA 40; (1936) 55 CLR 499 Hughes v St Barbara Mines Ltd (No 4) [2010] WASC 160 John Fairfax Publications Pty Ltd v Blake [2001] NSWCA 434; (2001) 53 NSWLR 541 Jones v Dunkel [1959] HCA 9; (1959) 101 CLR 298 Katsilis v Broken Hill Pty Co Ltd (1977) 18 ALR 181 Kazal v Thunder Studios Inc (California) [2023] FCAFC 174 Lehrmann v Network Ten Pty Ltd (Trial Judgment) [2024] FCA 369 Lewis v Daily Telegraph Ltd [1964] AC 234 M v The Queen [1994] HCA 63; (1994) 181 CLR 487 Maisel v Financial Times Limited (1915) 112 LT 953; 84 LJKB 2145 Masterton Homes Pty Ltd v Palm Assets Pty Ltd [2009] NSWCA 234; (2009) 261 ALR 382 Mirror Newspapers Ltd v World Hosts Pty Ltd [1979] HCA 3; (1979) 141 CLR 632 Morsman (by his next friend Bampton) v State of Victoria (Department of Education and Training) [2020] FCA 763 Murdoch v Private Media Pty Ltd [2022] FCA 1275 Nassif v Seven Network (Operations) Ltd [2021] FCA 1286 Nationwide News Pty Ltd v Rush [2020] FCAFC 115; (2020) 380 ALR 432 Nationwide News Pty Ltd v Weatherup [2017] QCA 70; [2018] 1 Qd R 19 Neat Holdings Pty Ltd v Karajan Holdings Pty Ltd [1992] HCA 66; (1992) 110 ALR 449 O’Brien v Australian Broadcasting Corporation [2017] NSWCA 338; (2017) 97 NSWLR 1 Oneflare Pty Ltd v Chernih [2017] NSWCA 195 Palios Meegan & Nicholson Holdings Pty Ltd v Shore [2010] SASCFC 21; (2010) 108 SASR 31 Palmer v McGowen [2021] FCA 430 Palmer v McGowan (No 5) [2022] FCA 893 Palram Australia Pty Ltd v Rees [2013] FCA 649 Phelan v Melbourne Health [2019] VSCA 205 Project Blue Sky v Australian Broadcasting Authority [1998] HCA 28; (1998) 194 CLR 355 Radio 2UE Sydney Pty Ltd v Chesterton [2009] HCA 16; (2009) 238 CLR 460 Reynolds v Times Newspapers Ltd [2001] 2 AC 127 Reifek v McElroy [1965] HCA 46; (1965) 112 CLR 517 Roberts-Smith v Fairfax Media Publications Pty Ltd (No 41) [2023] FCA 555; (2023) 417 ALR 267 Roberts-Smith v Fairfax Media Publications Pty Ltd [2025] FCAFC 67 Rofe v Smith’s Newspapers Ltd (1924) 25 SR (NSW) 4 Rush v Nationwide News Pty Ltd [2018] FCA 357 Rush v Nationwide News Pty Ltd (No 7) [2019] FCA 496 Russell v Australian Broadcasting Corporation (No 3) [2023] FCA 1223 Sampson in his Capacity as Trustee for the Bankrupt Estate of Tannous v Tannous [2022] FCA 1427 Schellenberg v Tunnel Holdings Pty Ltd [2000] HCA 18; (2000) 200 CLR 121 Schiff v Nine Network News Pty Ltd (No 2) [2022] FCA 1120 Seven Network (Operations) Limited v Greiss [2024] FCAFC 162 Seymour v Australian Broadcasting Commission (1977) 19 NSWLR 219 Slim v Daily Telegraph Ltd [1968] 2 QB 157 State of New South Wales v Wraydeh [2019] NSWCA 192 Sutherland v Stopes [1925] AC 47 SZTAL v Minister for Immigration and Border Protection [2017] HCA 34; (2017) 262 CLR 362 The Ophelia [1916] 2 AC 206 Thomson v STX Pan Ocean Co Ltd [2012] FCAFC 15 Trkulja v Google Inc LLC [2010] VSC 226 Trkulja v Google LLC [2018] HCA 25; (2018) 263 CLR 149 Unique International College Pty Ltd v Australian Competition and Consumer Commission [2018] FCAFC 155; (2018) 266 FCR 631 V’landys v Australian Broadcasting Corporation (No 3) [2021] FCA 500 V’landys v Australian Broadcasting Corporation [2023] FCAFC 80 Volonakis v Erceg [2019] NSWSC 1875 Wong v National Australia Bank Ltd [2022] FCAFC 155 |
Division: | General Division |
Registry: | New South Wales |
National Practice Area: | Other Federal Jurisdiction |
Number of paragraphs: | 2958 |
Date of last submission/s: | 21 June 2024 |
Date of hearing: | 4–5, 8, 11–13, 19–22, 25–29 September 2023, 3–6, 9–13 October 2023, 4–8, 11–15, 18–22, 25–28 March 2024, 2–5, 8–11 April 2024, 7–10, 13–16, 23 May 2024, 3–6, 13 June 2024 |
Counsel for the Applicant: | Ms S Chrysanthou SC, Mr N Olson and Mr T Smartt |
Solicitor for the Applicant: | HWL Ebsworth Lawyers |
Counsel for the Respondents: | Dr M Collins AM KC, Mr D Roche SC, Ms M Marcus, Mr M Mukerjea and Ms C Roberts |
Solicitor for the Respondents: | Thomson Geer Lawyers |
ORDERS
NSD 917 of 2022 | ||
| ||
BETWEEN: | MUNJED AL MUDERIS Applicant | |
AND: | NINE NETWORK AUSTRALIA PTY LIMITED First Respondent FAIRFAX MEDIA PUBLICATIONS PTY LIMITED Second Respondent THE AGE COMPANY PTY LIMITED (and others named in the Schedule) Third Respondent | |
order made by: | ABRAHAM J |
DATE OF ORDER: | 8 August 2025 |
THE COURT ORDERS THAT:
1. The application is dismissed.
Note: Entry of orders is dealt with in Rule 39.32 of the Federal Court Rules 2011.
[1] | |
[1] | |
[11] | |
[10] | |
[22] | |
[31] | |
[31] | |
[32] | |
[33] | |
[34] | |
[34] | |
[35] | |
[35] | |
[36] | |
[42] | |
[48] | |
[59] | |
[78] | |
[83] | |
[90] | |
[100] | |
Section 4 — Meaning of “negligence” and “unethical” in the imputations | [101] |
[101] | |
[108] | |
[110] | |
[110] | |
[122] | |
[134] | |
[153] | |
[165] | |
[179] | |
[184] | |
[184] | |
[187] | |
[213] | |
[213] | |
[220] | |
[234] | |
[242] | |
[251] | |
[263] | |
[265] | |
[293] | |
[305] | |
[307] | |
[323] | |
[329] | |
[332] | |
[332] | |
[334] | |
[336] | |
[339] | |
[341] | |
[347] | |
[348] | |
[348] | |
[351] | |
[355] | |
[368] | |
[374] | |
[377] | |
[383] | |
[383] | |
[410] | |
[447] | |
[494] | |
[494] | |
[494] | |
[537] | |
[597] | |
[615] | |
[634] | |
[656] | |
[671] | |
[671] | |
[700] | |
[745] | |
[745] | |
[767] | |
[827] | |
[827] | |
[898] | |
[968] | |
[1071] | |
[1106] | |
[1135] | |
[1148] | |
[1245] | |
[1304] | |
[1342] | |
[1342] | |
[1418] | |
[1508] | |
[1508] | |
[1596] | |
[1693] | |
[1748] | |
[1841] | |
[1887] | |
[1909] | |
[1922] | |
[1922] | |
[2040] | |
[2064] | |
[2106] | |
[2141] | |
[2141] | |
[2151] | |
[2166] | |
[2177] | |
[2187] | |
[2197] | |
[2199] | |
[2210] | |
[2210] | |
[2220] | |
Sting 2 — Misleading osseointegration patients (false promises, downplaying risks and complications) | [2251] |
[2278] | |
[2294] | |
[2348] | |
[2384] | |
[2428] | |
[2434] | |
[2438] | |
[2447] | |
[2453] | |
[2470] | |
[2473] | |
[2476] | |
[2479] | |
[2480] | |
[2482] | |
[2489] | |
[2498] | |
[2506] | |
Section 3 — The parties responsible for the defamatory matters | [2511] |
[2529] | |
[2534] | |
[2546] | |
[2552] | |
[2555] | |
[2562] | |
[2564] | |
[2566] | |
[2569] | |
[2588] | |
[2605] | |
[2606] | |
[2613] | |
[2615] | |
[2619] | |
[2643] | |
[2651] | |
[2699] | |
[2714] | |
[2719] | |
[2724] | |
[2735] | |
[2758] | |
[2767] | |
[2775] | |
[2791] | |
[2813] | |
[2821] | |
[2825] | |
[2870] | |
[2877] | |
[2879] | |
[2880] | |
[2886] | |
[2904] | |
[2905] | |
[2916] | |
[2956] | |
REASONS FOR JUDGMENT
ABRAHAM J:
PART 1 — INTRODUCTION
Section 1 — Introductory remarks
1 The applicant, Dr Munjed Al Muderis, an orthopaedic surgeon, is suing Nine Network Australia Pty Limited (Nine Network), Fairfax Media Publications Pty Limited (Fairfax), The Age Company Pty Limited (The Age Company) and journalists, Ms Charlotte Grieve, Mr Tom Steinfort and Ms Natalie Clancy (together, the respondents), for defamation in relation to television, video and newspaper (print and online) publications published in September 2022.
2 It is not disputed that at the time of publication, Dr Al Muderis had a high profile. He had featured on the television programs 60 Minutes (a separate episode to that the subject of these proceedings), Foreign Correspondent, Inside Story and Anh’s Brush with Fame. On his own account he was one of the busiest orthopaedic surgeons in Sydney. He held several clinical, consultant, academic and other professional appointments. He is a prolific author, accomplished public speaker (including at significant forums), the recipient of many awards for his medical and humanitarian achievements and was the 2020 NSW Australian of the Year. His fame was also because of his backstory; from escaping Iraq as a refugee, to holding the various positions and obtaining the achievements described (expanded upon below). The respondents described his reputation as “glittering”.
3 The matters published stemmed from a joint investigation conducted from May 2022 until the date of publication, between 60 Minutes, The Age and the Sydney Morning Herald, into information that had been obtained that portrayed a different picture of Dr Al Muderis. Although the respondents accepted Dr Al Muderis is, to many, an Australian hero who has devoted much of his life’s work to helping amputees walk again, they contended their investigation revealed that there was a significant cohort of unhappy patients. The journalists gave evidence that they found that some of the patients’ experiences with Dr Al Muderis were inconsistent with that portrayed in the media, including experiences where patients were vulnerable and susceptible to pressure tactics, where some patients had not had the risks of the surgery properly explained to them and where some patients said they had not received proper aftercare. After the investigation, a decision was made to publish the impugned matters. The journalists’ evidence is that they believed it was in the public interest to do so. The matters covered topics including allegations that Dr Al Muderis engaged in improper sales tactics, misled patients and downplayed the risks of osseointegration surgery, did not provide proper aftercare, and prioritised money over patient care.
4 There are seven matters sued on:
(1) a promotion for the then upcoming episode of 60 Minutes entitled “Sneak Peek: Cut to the Point”, published on 8 September 2022, and on the 60 Minutes Australia YouTube page from about 14 September 2022 (Sneak Peek) (see transcript at Annexure A);
(2) an episode of 60 Minutes entitled “Cut to the Point”, broadcasted on 18 September 2022 (Broadcast) (see transcript at Annexure B);
(3) a print article in the Sydney Morning Herald newspaper entitled “Surgeon ‘botched amputee aftercare’”, published on 19 September 2022 (SMH Article) (see Annexure C);
(4) an article on the Sydney Morning Herald’s website entitled “Oozing and maggots: The stories one of Australia’s most celebrated surgeons doesn’t want you to hear”, published on 18 September 2022 (SMH Online Article) (see Annexure D);
(5) a print article in The Age newspaper entitled “Celebrity Surgeon ‘left patients in pain, to rot’”, published on 19 September 2022 (Age Article) (see Annexure E);
(6) an article on The Age’s website entitled “Oozing and maggots: The stories one of Australia’s most celebrated surgeons doesn’t want you to hear”, published on 18 September 2022 (Age Online Article) (see Annexure F); and
(7) a video on The Age’s website entitled “Oozing and maggots: The stories one of Australia’s most celebrated surgeons doesn’t want you to hear”, published on 18 September 2022 (Grieve Video) (see transcript at Annexure G),
(the Publications).
5 The applicant alleges those matters convey 75 defamatory imputations (see a list of the pleaded imputations at Annexure H), some of which are admitted by the respondents to be conveyed to the ordinary reasonable reader or viewer (others are disputed). The respondents rely on the defences of justification (substantial truth) to most of the imputations, contextual truth, public interest and honest opinion, relying on ss 25, 26, 29A and 31 of the Defamation Act 2005 (NSW), respectively.
6 The issues which arise for the Court’s consideration are:
(1) whether the defamatory imputations pleaded at [13.24] and [16.1] (in the SMH Article, the SMH Online Article, and the Age Online Article) of the Statement of Claim (SOC) (together, the Denied Imputations) were conveyed;
(2) whether the defamatory imputations pleaded at [10.1], [10.2], [10.3], [10.4], [10.5], [10.6], [13.2], [13.6], [13.20], [16.4], [16.8], [16.13], [16.15], [16.20], [16.23], [16.27], [16.29] and [16.30] of the SOC (the Disputed Imputations), are confined to the applicant’s performance ‘in the operating theatre’, and if so, whether they were conveyed;
(3) whether the pleaded defamatory imputations in the SOC which are conveyed (save for [13.24], [16.9], [16.28] and [28.6]) are substantially true: defence of justification, s 25 of the Defamation Act. The respondents in oral closing submissions characterised their case as one of contextual truth, not a justification case;
(4) whether some or all the imputations on which the respondents rely as contextual imputations are substantially true and whether, in light of their substantial truth, any residual defamatory imputations do not further harm Dr Al Muderis’ reputation: defence of contextual truth, s 26 of the Defamation Act;
(5) whether the respondents reasonably believed that the Publications were in the public interest: defence of public interest, s 29A of the Defamation Act;
(6) whether the Publications were expressions of opinion on matters of public interest based on proper material: defence of honest opinion, s 31 of the Defamation Act; and
(7) various findings of fact which Dr Al Muderis invites the Court to make in relation to his alleged entitlement to damages and aggravated damages.
7 It is appropriate to observe at the outset that this is not a medical negligence case. The relevant issues are determined based on the principles applicable in defamation proceedings.
8 For the reasons below:
(1) Imputations [13.24] and [16.1] (in respect of the SMH Article, the SMH Online Article and the Age Online Article), are not conveyed by the Publications. The Disputed Imputations, being [10.1]-[10.6] (Sneak Peek), [13.2], [13.6], [13.20] (Broadcast), [16.4], [16.8], [16.13], [16.15], [16.20], [16.23], [16.27], [16.29] and [16.30] (Articles) are not conveyed. The remaining imputations are conveyed;
(2) it follows that in relation to the Sneak Peek, it has not been established that any of the pleaded imputations have been conveyed. The Broadcast, Articles, and the Grieve Video each conveys defamatory imputations;
(3) the respondents have established the defence of contextual truth under s 26 of the Defamation Act in relation to the Publications in which imputations are conveyed;
(4) the respondents have established the defence of public interest under s 29A of the Defamation Act in relation to the Publications in which imputations are conveyed; and
(5) given the above, it is unnecessary to determine the respondents’ claim to the defence of honest opinion.
9 Accordingly, the application is dismissed.
Section 2 — Overview
Dr Munjed Al Muderis
10 Dr Al Muderis was born in Baghdad, Iraq in 1972. He completed his medical studies at the University of Baghdad, graduated in 1996 with the degrees of Bachelor of Medicine and Bachelor of Surgery and was licensed to practice medicine in Iraq shortly afterwards. He came to Australia by boat in November 1999 and was detained at Curtin Detention Centre in Western Australia, where he spent nearly a year before his asylum claim was accepted. He was granted an Australian visa in 2000.
11 From shortly thereafter he has held positions in various hospitals. In 2002, Dr Al Muderis passed the Australian Medical Council’s examinations to earn recognition in Australia of his Iraqi medical qualifications. In 2008, he passed the examinations which qualified him as an orthopaedic surgeon.
12 Dr Al Muderis is a Fellow of the Royal Australian College of Surgeons and the Australian Orthopaedic Association, a Clinical Professor at the Macquarie University Faculty of Medicine and Health Sciences, and an Adjunct Clinical Professor at the University of Notre Dame Australia School of Medicine. He is also an Honorary Associate in the School of Aerospace, Mechanical and Mechatronic Engineering in the Faculty of Engineering and IT at the University of Sydney.
13 He has held consultant positions as an orthopaedic visiting medical officer at Norwest Private Hospital since 2010, Macquarie University Hospital since 2010, Hurstville Private Hospital since 2016 and East Sydney Private Hospital since 2020. He has also held and currently holds numerous leadership and executive positions, including: Member of the MQ Health Clinical Leadership Council since 2019; Member of the Medical Advisory Committee at Macquarie University Hospital since 2021; Member of the MQ Health Clinical Executive Committee since 2021; Head of the Lower Limb Orthopaedics and Sports Medicine Discipline at MQ Health since 2022; and Member of the SydOrth Board Committee since 2022.
14 He has been involved in clinical education and supervision, including as the Chief Supervisor for three fellowship training programs accredited by the Australian Orthopaedic Association, and as Director of Registrar Training at MQ Health since 2019. He is an ambassador for a number of charitable and humanitarian organisations including the Red Cross and Amnesty International Australia; is or has been a patron of a number of other organisations including the Multicultural Disability Advocacy Association of NSW, Asylum Seekers Centre and Amputees NSW; is represented by Saxton Speakers and has been regularly engaged to speak on topics including human rights issues and charitable causes.
15 He has published extensively in the field of orthopaedics generally, and osseointegration in particular, by co-authoring 40 original publications in international peer-reviewed journals (including four on the topic of osseointegration in 2022) and authoring or co-authoring ten textbook chapters on orthopaedics (including seven on the topic of osseointegration in 2022). Dr Al Muderis has also presented academic papers at many medical conferences, in Australia and overseas and has been awarded research grants with a cumulative value of over $7,000,000 over the last decade.
16 In 2022, Dr Al Muderis was awarded the degree of Doctor of Medical Science by the School of Medicine at the University of Notre Dame for his thesis “Osseointegration for Amputees: Past, Present and Future: Basic Science, Innovations in Surgical Technique, Implant Design and Rehabilitation Strategies”.
17 Dr Al Muderis is the inventor of several patents for prosthetic devices, which are held either by him personally or through his company, Osseointegration International Pty Ltd (Osseointegration International). These include patents for an osseointegratable device and other orthopaedic and deformity correction devices. He has also contributed to the design and development of other systems, including an osseointegrated prosthetic limb system.
18 He has been involved in charity and humanitarian work, providing consultations and medical procedures to amputees and other patients (including orthopaedic and osseointegration procedures) in countries including India, Poland, Cambodia, Lebanon, the Palestinian territories in Ramallah and the West Bank, Iraq, Israel and Ukraine.
19 He has been the recipient of numerous awards including the Asia Game Changers Award for humanitarian work in 2018, the GQ Man of the Year Social Force Award in Abu Dhabi for surgical and humanitarian work in 2019 and NSW Australian of the Year for surgical innovations and humanitarian works in 2020.
20 Dr Al Muderis estimated he has performed more than 9,000 orthopaedic procedures since 2012, and over 800 osseointegration procedures.
21 Generally, Dr Al Muderis conducts his consultations at the Limb Reconstruction Centre (LRC) in Macquarie University Hospital (which was formerly at Norwest Private Hospital). He is the Chairperson and Founder of the Osseointegration Group of Australia. His company, Osseointegration International, was incorporated on 20 February 2015.
Osseointegration
22 The Publications featured the experiences of ten of Dr Al Muderis’ osseointegration patients. It is helpful at this stage to briefly address the nature of this surgery.
23 Traditionally, amputees used socket-mounted prostheses to mobilise and regain use of their affected amputated limb. The socket attaches to the amputation stump via suction, meaning that such prostheses do not require invasive surgical procedures. When used for the lower limb, an artificial knee joint and lower leg prosthesis attach to the socket.
24 Osseointegration, is a term that describes the in-growth and integration of living bone onto the surface of an artificial implant, without an intermediate layer of soft tissue. In the 1960s, the concept of osseointegrated reconstruction originated in the dental implant field. In the 1990s, Dr Rickard Brånemark pioneered the use of a screw-fixation implant under the name OPRA (Osseointegrated Prosthesis for the Rehabilitation of Amputees), following which, transdermal osseointegrated implants for attachment of prosthetic limbs were first used. As a procedure, extremity osseointegration is a relatively new major elective and invasive orthopaedic surgery which allows for direct attachment of an external prosthesis to the skeleton through the surgical implantation of an intramedullary device (a device inserted into the medullary cavity of the femur or tibia, i.e. into the central cavity of the bone). The three basic elements of osseointegration are: the residual bone, the metal implant and the transdermal surface. The metal device is implanted into the end of the residual bone of the amputated limb, then exits the soft tissue and skin through a surgically created transdermal opening in the body, known as a stoma, to attach and interface with an external prosthesis. Osseointegrated devices are typically made of titanium, which is a particularly biocompatible material. Bone grows onto and integrates with the surface of the implant, and osseointegration occurs. Over time, this creates a stable and solid connection between implant and bone.
25 Until about 2014, most osseointegration procedures worldwide were performed in two stages: the first stage to insert the intramedullary implant; and the second stage, to create the stoma, allowing for transcutaneous abutment attachment and prosthesis fitting. There were two main approaches for osseointegration procedures: the OPRA system and EndoExo system. Osseointegration using the OPRA system screws the implant into the bone in the first stage with a six to nine-month interval between stages. Implantation of the OPRA system occurs in two stages because the implant is not initially stable and time needs to be given to allow strong osseointegration to occur before load is placed on the implant, otherwise it may fail. By contrast, the EndoExo system inserts a press-fit implant made of cobalt chrome alloy, driven into the medullary cavity with a mallet (instead of being screwed in, per the OPRA system) and requires a four to eight-week interval between stages. A more recent version of the implant is called the Integral Leg Prosthesis (ILP).
26 Dr Al Muderis’ evidence was that he began his practice using the two-stage EndoExo system. In 2013, he designed modifications to the system in collaboration with Permedica S.p.A in Milan and renamed it to Osseointegrated Prosthetic Limb (OPL) system. The OPL system retains the EndoExo press-fit concept, and according to Dr Al Muderis’ description, has several advantageous features.
27 The image below depicts the main components of the OPL system used by Dr Al Muderis. 
28 The dual cone adaptor connects the intramedullary implant to the external prosthesis and is secured by the internal locking screw. Dr Al Muderis’ evidence is that the dual cone adaptor has a highly polished surface to minimise soft tissue friction, and is coated with Titanium Niobium, which has antibacterial properties. The OPL system includes a “fail-safe” connector, which includes a taper sleeve component that connects on the distal end of the dual cone. The bushing component has two fail-safe pins that slot into matching holes on the taper sleeve. These pins are designed to break away if they are exposed to excessive rotational force, such as in the event of a fall, so that the excessive load can pass through and avoid damage to the implant or patient. The distal locking screw secures both the bushing and the taper sleeve on the dual cone. These three components form an abutment that can be inserted into the connector, which enables the quick attachment of the external prosthetic limb into the osseointegrated implant via the operation of a grub screw. The connector is then distally attached onto compatible commercially available prosthetic limbs via an industry standard four-hole base profile.
29 Since about April 2014, Dr Al Muderis has been performing a single-stage surgery with the OPL system, a modified surgical technique under the Osseointegration Group of Australia Accelerated Protocol-2 and a structured post-operative loading protocol. According to Dr Al Muderis, single-stage implantation is possible with the OPL system because of its design: the fluted proximal section of the OPL implant is both axially and rotationally stable after implantation. Dr Al Muderis owns personally, or through his company (Osseointegration International), the patent for his osseointegration device used in the surgery. His company manufactures the implants.
30 Dr Al Muderis, and various of the expert witnesses gave evidence which addressed the advantages and disadvantages of the different systems for osseointegration surgery. However, it is important to remember that this is not a case about the merits of osseointegration. Nor is it about which is the better system.
The journalists
Ms Charlotte Grieve
31 Ms Grieve is an investigative journalist in The Age’s Investigations Team. In June 2022, she was appointed as a secondee in that team. It was in that context that she conducted the investigation into Dr Al Muderis’ practice. Ms Grieve’s affidavit details her experience including the work undertaken in the roles she has held, the stories she has been involved in, and awards and commendations she has received. She began working in the media in various positions while studying for her Masters of Journalism in 2016 to 2017. She explained she also acted as a freelance journalist during this period, with articles published in The Guardian, The Age, SBS and the Sydney Morning Herald. In October 2018, she commenced as a trainee journalist at The Age. From around December 2019, she worked as a business journalist with the newspaper. She was awarded the 2021 and 2022 Citi award for young business journalist of the year.
Mr Tom Steinfort
32 At the time of the Publications, Mr Steinfort was a journalist with 60 Minutes. He first joined the 60 Minutes team in 2018. Mr Steinfort has been a journalist for nearly 20 years. He has extensive experience in both news and investigative journalism, having worked for various programs, including Today, A Current Affair, Inside Story, 60 Minutes and Nine News. In February 2022, as a senior journalist, he assisted judging the 66th Walkley Awards for excellence in journalism. In August 2022, he won the Kennedy Award for Outstanding Foreign Correspondent for his reporting of the Ukrainian war and was also announced as a finalist in the Outstanding Finance Reporting category. In November 2022, he was part of a group nominated as finalists for the radio/audio feature of “Liar Liar: Melissa Caddick and the Missing Millions” as part of the 67th Walkley Awards for Excellence in Journalism.
Ms Natalie Clancy
33 Ms Clancy joined 60 Minutes in October 2019 as an Associate Producer. In January 2022, she became a Producer of the program. By September 2022, she had been a journalist and a producer in television news and current affairs programs for approximately six years. Ms Clancy detailed in her affidavit the significant stories and investigations in which she had been involved. She was a finalist in the 2018 Walkley awards and the 2018 Kennedy awards, for her reporting in relation to Dr Emil Gayed. In 2021, she won the Paul Lockyer Kennedy award for Outstanding Regional Broadcast Journalism with Gareth Harvey and Liz Hayes for her investigation into healthcare in regional and rural NSW.
Section 3 — The present proceedings
The parties sued
34 It is helpful to set out which respondents are sued in relation to each Publication:
(1) Nine Network is sued in respect of the Sneak Peek and the Broadcast;
(2) Fairfax is sued in respect of the SMH Article and the SMH Online Article;
(3) The Age Company is sued in respect of the Age Article, the Age Online Article and the Grieve Video;
(4) Ms Grieve is sued in respect of all the Publications except the Sneak Peek, that is, she is sued in respect of the Broadcast, the SMH Article, the SMH Online Article, the Age Article, the Age Online Article (together, the Articles) and the Grieve Video;
(5) Mr Steinfort is sued in respect of the Broadcast and the Articles; and
(6) Ms Clancy is sued in respect of the Broadcast and the Articles.
PART 2 — THE DEFAMATORY IMPUTATIONS
Section 1 — The pleaded imputations
35 As mentioned above, the applicant pleaded 75 defamatory imputations in his SOC. I do not propose to recite them here. Rather, they have been annexed to this judgment as Annexure H. There is an issue as to the meaning of certain imputations, and whether they are conveyed (with the conclusions below also being identified in Annexure I).
Section 2 — Legal principles
36 The principles in relation to meaning are well established, and not in dispute between the parties: Favell v Queensland Newspapers Pty Ltd [2005] HCA 52; (2005) 219 CLR 165 at [6]-[12], [17]; Trkulja v Google LLC [2018] HCA 25; (2018) 263 CLR 149 (Trkulja) at [30]-[32]. For application, see, for example, Rush v Nationwide News Pty Ltd (No 7) [2019] FCA 496 (Rush) at [70]-[85] (with there being no suggestion of any error in this collection of principles on appeal to the Full Court); Nationwide News Pty Ltd v Rush [2020] FCAFC 115; (2020) 380 ALR 432; Hockey v Fairfax Media Publications Pty Limited [2015] FCA 652; (2015) 237 FCR 33 (Hockey) at [63]-[73]; Chau v Fairfax Media Publications Pty Ltd [2019] FCA 185 at [14]-[27]; Australian Broadcasting Corporation v Chau Chak Wing [2019] FCAFC 125; (2019) 271 FCR 632 (Wing); V’landys v Australian Broadcasting Corporation (No 3) [2021] FCA 500 (V’landys) at [41]-[55]; Hanson v Burston [2023] FCAFC 124; (2023) 413 ALR 299 at [43]-[48]; Kazal v Thunder Studios Inc (California) [2023] FCAFC 174 (Kazal) at [336]-[337].
37 An applicant bears the onus of establishing on the balance of probabilities that an ordinary reasonable reader, viewer or listener would understand that the publication sued upon bears the alleged defamatory meanings or imputations as pleaded and particularised.
38 The relevant question is whether the publication would have conveyed the alleged meanings to an ordinary reasonable person. It is to be objectively determined. The hypothetical individual is a person with various characteristics, including: they are of fair to average intelligence, experience, and education; are fair-minded and neither perverse, morbid, suspicious of mind, nor “avid for scandal”; and that they do not examine the publication overzealously. While they do not search for hidden meanings or adopt strained or forced interpretations, they nevertheless draw implications, especially derogatory implications, more freely than a lawyer would: Rush at [75]-[77]; Kazal at [336]-[337]. The ordinary reasonable person is also taken to have read the entire publication, considered the context as a whole, and taken into account emphasis that may be given by conspicuous headlines or captions: see Rush at [77]; Trkulja at [32]; and the summary in V’landys at [41]-[55]. They are more likely to consider a publication cautiously and carefully, and less likely to jump to conclusions or engage in loose thinking, where the publications purport to be serious investigative journalism concerning matters of importance (a topic to which I return below). For transient publications such as television broadcasts (even where those publications are available to be viewed or re-viewed via the internet), ordinary viewers are likely to have watched the publication only once, without pausing or going back over it: Chau v Australian Broadcasting Corporation (No 3) [2021] FCA 44; (2021) 386 ALR 36 (Chau) at [35]; V’landys at [73].
39 However, it does not follow that each part of the publication must be given equal significance, as striking words or images may stay with the reader, viewer or listener and give them a predisposition or impression that influences all that follows: V’landys at [51]. A pleaded imputation, and whether it has been proven to be substantially true, requires attention to context, as provided by the balance of the publication and any wider context within which it is to be understood. The natural and ordinary meaning of words is not limited to their literal meaning. The ordinary reasonable person is not a lawyer or be taken to have a detailed understanding of the law: Trkulja at [32]. The imputations are considered by reference to the ordinary meaning, not their legal meanings, because that is the way the terms would be understood by ordinary reasonable people. Words do not necessarily have a fixed meaning that applies in all circumstances; even benign words may convey a worse, or better, impression when regard is had to how and when they are deployed: see, for example, Greek Herald Pty Ltd v Nikolopoulos & Ors [2002] NSWCA 41; (2002) 54 NSWLR 165 at [21]-[27]; Lewis v Daily Telegraph Ltd [1964] AC 234 at 258. The meaning that an individual would attribute to a publication, or the impression that the reader forms, may be influenced by the overall tone or tenor of the article in question: Rush at [80].
40 Given that the meaning is to be determined objectively, the audience is taken to have a uniform view of that meaning. The publisher’s intended meaning and that understood by individual readers of the matter complained of, are irrelevant: Rush at [84]-[85]. The determination of the natural and ordinary meaning of words involves the application of the “single meaning” rule. Although different people might in fact have understood the meanings conveyed by a matter in different ways, the Court must arrive at a single objective meaning: Slim v Daily Telegraph Ltd [1968] 2 QB 157 at 171-175; Hockey at [73]; Wing at [32]. The issue is the single meaning that an objective audience composed of ordinary reasonable persons should have collectively understood the matter to bear: Wing at [32].
41 A matter is defamatory if it carries a meaning about the applicant which is calculated to: expose him or her to hatred, contempt, or ridicule; lower him or her in the estimation of ordinary right-thinking members of society; or cause others to shun and avoid him or her: Boyd v Mirror Newspapers Ltd [1980] 2 NSWLR 449 at 452-453; Mirror Newspapers Ltd v World Hosts Pty Ltd [1979] HCA 3; (1979) 141 CLR 632 at 638-639; Radio 2UE Sydney Pty Ltd v Chesterton [2009] HCA 16; (2009) 238 CLR 460 at [5].
Section 3 — Consideration
42 In this case, there are two imputations which the respondents deny are carried: Imputations [13.24] and [16.1] (in relation to the SMH Article, the SMH Online Article and the Age Online Article) (the Denied Imputations). There are a further 18 imputations where the meaning is disputed. If the applicant’s meaning is accepted, the imputations are denied. If the respondents’ meaning is accepted, they admit that meaning is carried, relating to Imputations: [10.1]-[10.6], [13.2], [13.6], [13.20], [16.4], [16.8], [16.13], [16.15], [16.20], [16.23], [16.27], [16.29] and [16.30] (the Disputed Imputations). The remaining imputations are those which the respondents admit are carried, those being imputations [13.1], [13.3]-[13.5], [13.7]-[13.19], [13.21]-[13.23], [13.25]-[13.30], [16.1] (only in relation to the Age Article), [16.2], [16.3], [16.5]-[16.7], [16.9]-[16.12], [16.14], [16.16]-[16.19], [16.21], [16.22], [16.24]-[16.26], [16.28] and [28.1]-[28.9].
43 I accept the respondents’ submission that in assessing the meaning of these imputations that:
Ordinary reasonable viewers and readers of the Publications will have understood that 60 Minutes, the Sydney Morning Herald and The Age are reputable sources of serious news and current affairs. They will have known that these publishers employ reputable and experienced journalists who are not prone to exaggeration and sensationalism. They will have immediately understood that the Publications concerned serious matters of public importance in connection with the provision of medical care to vulnerable members of society. Such persons are not unusually suspicious or avid for scandal and do not search for sinister meanings. They will have approached serious, long-form journalism of this kind with caution and care, and been reluctant to leap to conclusions or engage in loose thinking.
44 That submission was not disputed.
45 In support of the submission, the respondents referred, inter alia, to the observations of Wigney J in V’landys at [72]-[73] (a passage upheld on appeal in V’landys v Australian Broadcasting Corporation [2023] FCAFC 80 at [75], [79] and [82]):
[72] The first general observation is that the report was broadcast as part of an episode of one of the ABC’s flagship news and current affairs programs. That program, 7.30, is a half-hour long program which the ordinary reasonable viewer would understand generally includes well-researched reports by experienced journalists and social and political commentators concerning serious issues of public interest or concern. It should be noted, in this context, that, somewhat unusually for the 7.30 program, the report in question was almost 50 minutes long and occupied the entire episode of 7.30 on 17 October 2019.
[73] Returning to the nature of the program generally, while views may of course differ, the ordinary reasonable viewer of 7.30 would most likely understand that the program was a respected current affairs program which was generally not prone to sensationalism, or loose or imprecise journalism or reporting. The ordinary reasonable viewer of 7.30 would be a person interested in watching a program containing serious and well researched reporting about important issues. Such a viewer would generally be more likely to view the program carefully and be less likely to engage in loose thinking and speculation than viewers of more sensationalist and less informative programs aimed more at entertainment than serious journalism.
46 The Full Court rejected the appellant’s ground that there was no basis for that observation: see [75]. At [81]-[84], Rares J (with whom Katzmann and O’Callaghan JJ agreed) concluded:
[81] The ordinary reasonable reader, listener or viewer is a person whose understanding of what the matter complained of in a defamation action conveys necessarily must be representative of the class of ordinary reasonable members of the community who read, listened or viewed the publication. Different classes of readers, listeners or viewers will have different appreciations of what a publication is saying. Thus, the readers of a technical scientific journal that allegedly conveys a defamatory meaning, and those readers’ characteristics or approach, are not likely to be the same as those of ordinary reasonable persons who read a tabloid newspaper or a weekly gossip magazine.
…
[83] Depending on the nature of the program that the viewer has selected to watch, his or her focus may be to learn from what is broadcast or to be informed, amused, distracted or entertained by it. It is a feature of everyday life that people change their approach to absorbing or comprehending communications that they read, hear or see depending on the context of the publication and the person’s purpose in reading, listening to or viewing it. …
[84] But in every case where the question is whether a video or television publication conveys a defamatory imputation, the hypothetical viewer is an ordinary reasonable member of the type of audience who watches a program of the kind in issue in the way in which such a person ordinarily does. This required his Honour to take into account, in assessing how the viewer would understand the report and whether it conveyed the imputations, the degree to which such a program’s viewers had a proneness to loose thinking.
47 I accept the observations of Wigney J are apt to describe the Articles in The Age and the Sydney Morning Herald, as well as the Broadcast by 60 Minutes, which is a public affairs program. This was investigative, long-form journalism on a serious topic of the standard of medical care provided by Dr Al Muderis. The applicant admitted that the Publications were in the public interest. These were not entertainment stories but raised serious concerns and allegations about a serious subject matter of public interest: see Chau at [39].
The Denied Imputations
Imputation [13.24]: Dr Al Muderis improperly profits from his patients by charging them twice for the parts and procedure.
48 This imputation is said to arise from the following statement spoken by Mr Steinfort, in the Broadcast:
Dr Munjed Al Muderis’ business model is ingenious because not only does he carry out the surgery, but he also designs his own implants, so effectively he profits twice by charging for the parts and the procedure.
49 The applicant submitted that while Mr Steinfort did not expressly allege that this arrangement is “improper”, the notion of impropriety was conveyed by: the proximate context of the line to references in the Broadcast of Mr Bruha (one of his patients) saying he felt Dr Al Muderis was “a bit of a cowboy”; Mr Steinfort describing Mr Bruha as feeling like “just another number in a moneymaking machine” and stating that this feeling got worse with “another shocking development”, namely that when one of Mr Bruha’s parts broke, he was charged for the replacement; and Mr Bruha saying that this added “insult to injury”. The applicant also referred to the broader context of the Broadcast, which stated it is “all about the numbers” and referenced Dr Al Muderis going from “rags to riches”, with his expensive penthouse and car. He submitted that the Broadcast’s central theme was that the profits Dr Al Muderis supposedly makes from the components are exploitative, audacious and scandalous. It was submitted that when Mr Steinfort described Dr Al Muderis’ “business model” as “ingenious”, it was not a compliment, rather, the ordinary reasonable viewer would understand “ingenious” in this context to mean “devious” or “crafty”.
50 The respondents submitted that the imputation relates to a short part of the Broadcast lasting seconds and consisting of two sentences (which includes the next sentence being “[i]n fact, court documents from the US reveal that on average his business makes a profit of 110,000 Australian dollars for every American patient”). They submitted there is nothing in Mr Steinfort’s tone, nor the substance of his words, that would have conveyed to ordinary reasonable viewers that there was anything “improper” in the mere practice of Dr Al Muderis profiting from both the performance of osseointegration surgery and the supply of parts for that surgery. Their submission was that ordinary viewers, not avid for scandal, not searching for hidden or sinister meanings, and approaching the Broadcast cautiously with regard to the whole of its contents, will have understood that: (a) osseointegration surgery is “ground-breaking” and “cutting edge surgery”; (b) the surgery is radical, in that it involves implanting a metal rod into an amputee’s residual bone and connecting it to a robotic limb, making them “half-human, half-machine” in order to enable them to walk again; (c) surgery of this kind involves specialist skill and sophisticated hardware, both of which are expensive; (d) Dr Al Muderis is one of the leading exponents of the surgery in the world and has been feted for his performance of the surgery; (e) in the circumstances, Dr Al Muderis would be expected to profit handsomely; and (f) there is nothing inherently improper about that.
51 The respondents submitted the real sting of the Broadcast in so far as it concerns Dr Al Muderis’ business practices was not whether there is anything improper in Dr Al Muderis profiting from both his performance of surgery and his supply of parts but, rather, his practice of allegedly driving up patient numbers, prioritising the growth of his practice over patient care and treating patients like numbers (with the respondents pointing to other aspects of the Broadcast they submitted emphasised this). The respondents also referred to what Dr Anstee said in the Broadcast, where he expressed his opinion as to the propriety of Dr Al Muderis’ marketing practices but cast no judgment on the fact that Dr Al Muderis profits from both the parts and surgery, a matter the respondents argued would not have been lost on ordinary viewers.
52 I accept the respondents’ submission that the imputation as pleaded is not conveyed. An ordinary reasonable viewer would consider this statement in its broader context, considering the whole of the Broadcast. As the respondents submitted, the sting of the Broadcast in respect to Dr Al Muderis’ business practices relates to driving up patient numbers, treating patients as numbers, and prioritising growth of the business over patient care. At best, as the respondents submitted, it might support a finding that the Broadcast imputed that Dr Al Muderis engaged in commercially shrewd or opportunistic conduct in relation to the mechanisms by which he profits from osseointegration surgery. The statement conveys profiteering, but in context, not improperly so.
53 Imputation [13.24] is not carried.
Imputation [16.1]: Dr Al Muderis is a callous surgeon who routinely left patients in pain to rot after their surgeries
54 This imputation is disputed in so far as it is said to be carried by each of the SMH Article, the SMH Online Article, and the Age Online Article. The respondents no longer dispute the imputation is carried in relation to the Age Article.
55 The applicant submitted that it is conveyed explicitly by the front-page headline of the Age Article, “Celebrity surgeon ‘left patients in pain, to rot’”. He submitted that the ordinary reasonable reader would consider this to be callous behaviour by a surgeon towards his patients. The headline conveys that this is routine behaviour because it is expressed in absolute terms: Dr Al Muderis “left patients in pain, to rot”, not just “some patients”. The ordinary reasonable reader would understand that this occurred on more than a few occasions. It was submitted that with the exception of the Age Article headline, the text of the Articles is relevantly the same, and that the Articles presented numerous examples of patients who presented to Dr Al Muderis with complaints of pain or infection but were either ignored or brushed off (with the applicant providing examples thereof). The applicant submitted from the statements identified, that the ordinary reasonable reader would consider that what is described are the actions of a surgeon who is callous towards patients who are in pain and literally “rotting” because of infections. The applicant also submitted that the notion that Dr Al Muderis “routinely” ignores these patients arises in two ways: first, it is suggested that some of the patients profiled in the Articles raised concerns with him on multiple occasions and that he consistently ignored them; and, second, the notion that this kind of treatment is a routine occurrence across Dr Al Muderis’ practice as a whole is conveyed by the accumulation of examples.
56 The respondents accepted that the imputation is conveyed in the Age Article, but contended it is not conveyed in the SMH Article, the SMH Online Article and the Age Online Article. They submitted that each of those publications made no reference to Dr Al Muderis leaving patients to “rot after their surgeries”. The Articles did refer to some of Dr Al Muderis’ patients who had suffered ongoing and severe pain following osseointegration surgery but submitted that none suggested that Dr Al Muderis had left them to “rot” after surgery. They submitted that ordinary readers could only have arrived at such a meaning as a result of applying their own beliefs and prejudices in a search for a hidden or sinister meaning.
57 The SMH Article, the SMH Online Article and the Age Online Article do not contain a reference to “rot”. It is to be recalled that from the passages in the Articles relied on by the applicant in support of his submission, he contended that the ordinary reasonable reader would consider that the patients were “literally ‘rotting’ because of infections”. Considering those passages in the context of the whole of the Articles, I am not persuaded that is what is conveyed.
58 Imputation [16.1] is not carried in the SMH Article, the SMH Online Article and the Age Online Article.
The Disputed Imputations
59 It will be recalled that the Disputed Imputations are [10.1]-[10.6] (Sneak Peek), [13.2], [13.6], [13.20] (Broadcast), [16.4], [16.8], [16.13], [16.15], [16.20], [16.23], [16.27], [16.29] and [16.30] (Articles, noting [16.27], [16.29] and [16.30] are not pleaded in relation to the SMH Online Article and the Age Online Article (together, the Online Articles)). Each of these imputations incorporates words or phrases such as “operated”, “surgical abilities”, “conducted surgery” and “performed surgery”, or slight variations thereof.
60 There is an issue as to the meaning of those terms. As explained below, the applicant proceeded to conduct his case on the basis that those words or phrases mean what occurs in the operating theatre. That is, the conduct of the surgery itself, which they submitted must involve taking a scalpel to a patient. The respondents do not admit the imputations with that meaning. Rather, in their Amended Defence, their admission was only on the basis that ordinary reasonable viewers and readers would have understood them as impugning his surgical practice more generally, including “pre-operative and post-operative consultations, considerations and care” (being the broader meaning). The respondents submitted that the Disputed Imputations are not conveyed if understood in the narrower sense as advanced by the applicant, that is, only concerning Dr Al Muderis’ conduct of surgery in the operating theatre. The respondents submitted that if that is accepted, the applicant’s case in respect of those imputations must fail, because it has not been established that they are conveyed. They submitted that nonetheless, in that circumstance, they rely on the imputations with the broader meaning as contextual imputations. I note that the respondents also submitted that in any event, the evidence adduced at trial supports a finding that Imputations [10.1], [10.2], [10.4], [16.4] and [16.30] are true even in the narrower sense posited by the applicant.
61 In his written closing submissions, the applicant took issue with the respondents’ approach, contending that rather than addressing the issue of which imputations are carried by the matters, the contention about the meaning of “surgery” appears to be directed more to the extent to which certain particulars of justification, even if made good, are relevant to establishing the substantial truth of the imputations of which Dr Al Muderis complains. He submitted that the respondents seek to expand the meaning of “surgery” to broaden the matters which may be relevant to justifying those imputations. During oral submissions, the applicant contended it is for the Court to determine the meaning of “surgery” by reference to what the ordinary reasonable reader or viewer thinks it means. He submitted that as the respondents have admitted the broader interpretation is conveyed, the Court should conclude that meaning, as a minimum, applies and conclude, per the respondents’ case, that those imputations are carried.
62 I do not accept that that is the approach taken by the respondents. Rather, the respondents have addressed as the first step, the question of the meaning of the imputations, contending that the imputations are not conveyed if understood as the applicant contended. The respondents submitted that if that is correct, they are then able to otherwise rely on the Disputed Imputations with the broader meaning (as contextual imputations) for the purposes of their defence of contextual truth. The applicant repeatedly criticised the form of the respondents’ pleading but brought no application challenging its sufficiency or appropriateness, prior to the hearing.
63 An initial issue arises as to what the applicant pleaded in relation to the Disputed Imputations. In the applicant’s oral closing submissions (which I note for context were heard after his written closing submissions were filed), the applicant submitted that he was taken by surprise by the respondents’ approach to this issue, because at no point did he seek to define the meaning of “operation” or “surgical” or “surgery”, and it was not the applicant’s job to do so.
64 As the applicant submitted from the outset, it is his prerogative to choose the battleground by choosing the imputations on which he relies. That choice is a matter for the plaintiff: Wing at [16]-[17].
65 An imputation should identify the act or condition the plaintiff claims was attributed to him, as they would be understood by the ordinary reasonable reader, viewer or listener. The meaning would usually be distilled or inferred from the words used in the publication: Harvey v John Fairfax Pty Ltd [2005] NSWCA 255 at [118]-[132]; Drummoyne Municipal Council v Australian Broadcasting Corporation (1990) 21 NSWLR 135 (Drummoyne) at 137. If the publication gives rise to one or more possible meanings of a particular condition attributed to an applicant, the applicant is obliged to specify how and in what respects that condition is conveyed in the imputation: Trkulja v Google Inc LLC [2010] VSC 226 at [19]-[20], citing Gleeson CJ in Drummoyne.
66 As explained above, an applicant bears the onus of establishing that an ordinary reasonable reader, viewer or listener would understand the publication sued upon bears the alleged defamatory meanings or imputations as pleaded and particularised, which is seen to extend to any meanings that are not substantially different from or more serious than those pleaded meanings (often described as a mere shade or nuance of the pleaded meaning, or a permissible variant): Wing at [17]-[18]; Chakravarti v Advertiser Newspapers Ltd [1998] HCA 37; (1998) 193 CLR 519 at [21]-[23], [60], [139]; Nassif v Seven Network (Operations) Ltd [2021] FCA 1286 (Nassif) at [80].
67 The respondents submitted that at least from the case management hearing held on 24 August 2023, the meaning identified by the applicant and relied upon as conveyed is “surgery” and “operation” in the narrow sense, that is, confined to what occurred in the operating theatre. I accept that the position of the parties was apparent from at least that case management hearing (after the pleadings and evidence had been filed, but before the trial).
68 So much was made clear by the applicant in his written opening submissions. He submitted:
Whatever else might be comprehended within those expressions [“operated on”, “conducted surgery”, “performed surgery” and “performed osseointegration surgery”], the natural and ordinary meaning of them, as any ordinary reasonable person would understand them, must involve taking a scalpel to the patient. If the respondents are not in a position to justify the imputations in that sense, particulars about other aspects of medical practice which might form part of an extended notion of “performing surgery”, such as preoperative consultations and informed consent procedures, will not assist them because they will have failed to justify what is obviously a material part of the imputations as pleaded, namely the performance of surgery stricto sensu.
69 The applicant’s oral opening submission was consistent with that. The applicant’s written closing submissions are in the exact same terms. This approach is also reflected in those written submissions that concern whether the justification defence has been established in relation to the imputations in issue. The reasons given in the annexure to the applicant’s submissions addressing why he contended justification is not established in relation to these imputations, refer to the imputations as involving negligent surgery, negligently conducting surgery, or conducting the actual operation. The broader imputation is not addressed.
70 It is in that context that the applicant’s oral closing submission, referred to above, was made. That is, at no point did he seek to define the meaning of “operation” or “surgical” or “surgery”, and it was not his job to do so. He submitted that the meaning of “operation” or “surgery” only becomes relevant for the truth case if there is a dispute about meaning. However, the first issue is whether the applicant has established that the imputation has been carried. If it has not, the occasion for a defence does not arise.
71 The applicant’s oral closing submission was ultimately, that at a minimum, the Court should find that the imputations are carried, even if I accept that the respondents’ view of surgery is correct. He submitted that the respondents have admitted the imputations are carried. He submitted his position as to the meaning of surgery is “not black and white” on every imputation, because of the context in which it occurred. However, in respect to the Disputed Imputations that is not how his case was conducted. For example, the applicant submitted the Sneak Peek, is only talking about surgery in the narrow sense. To illustrate, the applicant accepted that his position in relation to Mr Smith is that surgery meant the operation itself:
That his surgery, as a surgeon, caused Brennan Smith to cut his flesh off, caused him excruciating pain like being electrocuted, caused maggots in a surgical wound, surgery, negligent performance of surgery.
72 That is, Dr Al Muderis negligently conducted the operation which caused Mr Smith to cut off his own skin. His submission on the other imputations is consistent with that; that these imputations all relate to surgery in the narrow sense, and that they could not mean anything else. The applicant’s submission also does not sit with the manner he opened his case wherein he submitted the respondents need to establish the justification defence for these imputations in respect to surgery in the strict sense, without which the justification defence fails.
73 The applicant’s closing submission proceeded on the basis that the respondents admitted the Disputed Imputations are conveyed, but as explained above, the respondents did not admit these imputations were carried by the Publications if the meaning of the terms was construed in the narrow sense, being the operation or performance of the surgery itself.
74 The respondents submitted:
The ordinary reasonable person understands what surgery entails. They know that the surgeon’s role involves much more than the time spent in an operating theatre. They will appreciate that surgical practice involves assessing whether surgery is necessary, what type of surgery, whether the patient is a suitable candidate for that surgery, the disclosure of information about the surgery, the preparation of the patient for surgery, the performance of the surgery itself, and all aspects of ongoing post-surgical care, treatment and rehabilitation. When a person says in common parlance that they are “having surgery”, ordinary reasonable members of the community understand that this is not simply a reference to the process of laying on an operating table to undergo a surgical procedure. It is a reference to an entire process.
75 I accept that submission. As the respondents submitted, the narrow interpretation of the terms also does not reflect either the words or substance of the Publications, which do not contain any express allegation concerning Dr Al Muderis’ performance of surgery “in the operating theatre”. As explained below, in my view, the Publications convey acts which would be understood by the ordinary reader, as within the broader concept of what is involved in having surgery (not confined to what occurred in the operating theatre). Where the word surgery is used (which is limited), in context, would be understood by the ordinary reasonable reader to be referring to surgery of this type, not this operation. Where the word operation is used, it is a reference to the fact of the operation.
76 I accept the respondents’ submission that the applicant conducted his case on the basis of the meaning of the terms in the Disputed Imputations as surgery in the narrow sense (i.e. what occurred in the operating theatre which must involve taking a scalpel to a patient). That is the meaning of the imputations he intended to convey by his pleading, and on which he chose to rely.
77 The issue then becomes whether those imputations (on the meaning pleaded by the applicant, bearing in mind permissible variants) are carried. The relevant question is whether the Publications would have conveyed the alleged meanings to an ordinary reasonable person.
The Sneak Peek
78 The applicant pleaded six imputations in relation to the Sneak Peek, all of which he contended would be understood as having conveyed that Dr Al Muderis negligently operated or conducted surgery on a patient, specifically in the operating theatre. To use the applicant’s language, this “must involve taking a scalpel to the patient”.
79 I do not accept that the ordinary reasonable viewer would have understood this publication to impugn Dr Al Muderis’ conduct of surgery in the operating theatre. That is not what is conveyed by the Sneak Peek. This is a very brief advertisement, promoting and directing attention to an upcoming program “on 60 Minutes”, that is, the Broadcast. The publication directs attention to the substantive broadcast. Given that context, as the respondents submitted, it does not descend to any level of detail as to the type of conduct attributed to Dr Al Muderis. The terms pleaded (being negligent surgery, negligently conducting surgery, or negligence in performing surgery) are not used in that publication, save for one reference to surgery, but not in the sense relied on by the applicant. That sole reference in the Sneak Peek to surgery pertains to the question posed by Mr Steinfort to Mr Smith: “What sort of surgery leaves you having to cut your own flesh off?” As evident from the use of the phrase “sort of surgery”, in context, it conveys a type of surgery as opposed to the conduct or performance of a particular operation. There is no reference to “conducted surgery”, “performing surgery”, “operated on”, or “surgical abilities”, being the terms used in the pleaded imputations. Rather, the publication conveys false promises, broken promises, patients turning against Dr Al Muderis, and complications arising after surgery (e.g. smells akin to a dead body, excruciating pain or needing to cut off flesh).
80 Contrary to the applicant’s submission, the Sneak Peek does not convey that Dr Al Muderis was negligent in the operating theatre during the operation such that it caused Mr Smith to cut his own flesh off and experience excruciating pain likened to being electrocuted.
81 The applicant submitted that as an imputation contains all variant meanings, even if a broad view of surgery is accepted, his case does not fail.
82 That raises the issue of whether, what is conveyed, is a permissible variant. I am not persuaded that surgery in the broad sense is a mere variant or nuance of surgery in the narrow sense. The focus in the latter interpretation is on a confined aspect of conduct (Dr Al Muderis’ conduct in performing the operation) whereas, the Publications had as their focus, the broader concept.
The Broadcast
83 In relation to the Broadcast, the imputations in issue, [13.2], [13.6] and [13.20], all relate to Mr Urquhart, and include the allegation that Dr Al Muderis negligently performed surgery on him.
84 I do not accept that the ordinary reasonable viewer would have understood the Broadcast to impugn Dr Al Muderis’ conduct towards Mr Urquhart in performing the surgery in the operating theatre. The nature of the complaints that supposedly have patients turning against Dr Al Muderis is identified at the outset:
Now a number of the surgeon’s patients are turning against him, accusing him of not taking proper care of them. And when you see the evidence you’ll understand why they’re so angry.
85 That is the framing of the Broadcast. As the respondents submitted, the reference to “care” was sufficiently broad to have been understood as extending to all aspects of Dr Al Muderis’ care for patients.
86 There are several other instances in the Broadcast which support the respondents’ submission. For example (any emphasis is added):
(1) shortly after the above statement, there is a clip of Mr Urquhart with Mr Steinfort referencing out-of-control infections and maggots in a voiceover;
(2) the Broadcast then turns to Mr Smith with Mr Steinfort’s voiceover describing him as “a patient feeling so abandoned he had to take to his own leg with a kitchen knife” over a video to this effect, followed by Mr Smith’s interview where he describes the excruciating pain he experienced;
(3) Mr Steinfort remarks that “[t]hese patients are left feeling like they’re just a number”;
(4) the Broadcast returns to Mr Urquhart with Mr Steinfort referring to the fact that within three months of rehabilitation he was able to walk, but there were “horrible complications” including pain, infections, repulsive odour, what is known as the “Febreze incident” (discussed further below) and maggots;
(5) the Broadcast also returns to Mr Smith, with Mr Steinfort referring to his hypergranulation, with Mr Smith saying “if you take on a job you take it on and start to finish to its entirety, and you got a responsibility and duty of care”, to which Mr Steinfort responds: “Care’s the important word there isn’t it?”;
(6) the Broadcast shows Ms Grieve and Mr Steinfort discussing their joint investigation, and Ms Grieve saying “[s]o we’ve got traumas, infections” followed by Mr Steinfort describing in a voiceover that Ms Grieve interviewed overseas patients “who felt neglected after Dr Al Muderis operated on them”, such that Ms Grieve described a theme of Dr Al Muderis abandoning patients, over-promising and viewing patients as numbers;
(7) following Ms Stewart’s interview, Mr Steinfort remarks that “Shona says once operated on, rehabilitation care for patients was inconsistent”;
(8) in his interview with Dr Anstee, Mr Steinfort notes “[c]omplications will arise. I guess the issue is how well you manage those complications”, to which Dr Anstee responds: “Yeah. And how well you plan to avoid the complications. But if you do have a complication, you’ve got to wear it. That’s your problem until you die or the patient dies.” Mr Steinfort further asks “[i]s there any excuse for a surgeon to – to palm that off to someone else?” and Dr Anstee replies “… you’ve got to look after the patient”;
(9) Mr Steinfort’s voiceover: “While some question how well Dr Al Muderis looks after his patients …”;
(10) the Broadcast later turns to Mr Bruha, and Mr Steinfort’s voiceover remarks “… like a number of other patients, his wound became infected”, Mr Bruha stating in his interview that “[t]hey sent me home with an infection in my leg and an open wound”, and Mr Steinfort’s later voiceover that “Chris Bruha has ongoing issues with pain”;
(11) regarding Ms Cindy Asch-Martin, the Broadcast states “even Cindy admits she did suffer major complications and was sent back to America afterwards with a dangerous infection”; and
(12) in the course of his interview with Mr Steinfort, Dr Al Muderis was asked about abandoning Mr Urquhart, maggots as a complication, downplaying infection and odour by recommending the use of Febreze, performing procedures and hosting medical clinics in the United States potentially in breach of United States laws, high-pressure sales tactics, encouraging staff to teach patients how to fundraise for the surgery, being motivated by money, paying people to recruit patients and mobilising patients to protect his reputation.
87 As the respondents submitted:
Conspicuously absent from all of this was any suggestion, complaint, allegation or accusation that Dr Al Muderis had at any stage acted negligently when performing surgical procedures “in the operating theatre”.
88 I agree with that description. I accept the respondents’ submission that ordinary reasonable viewers would have understood the Broadcast as conveying that Dr Al Muderis has engaged in negligence or other discreditable conduct in his practice as a surgeon generally and specifically in relation to Mr Urquhart, including the disclosure of risks and post-operative care. Again, it is difficult to accept this is simply a mere variant or nuance of the pleaded imputations.
89 I am not satisfied that Imputations [13.2], [13.6] and [13.20] are conveyed.
The Articles
90 In relation to the SMH Article and the Age Article, the Disputed Imputations are [16.4], [16.8], [16.13], [16.15], [16.20], [16.23], [16.27], [16.29] and [16.30].
91 As the respondents submitted, the headline for each article (which for reference are “Surgeon ‘botched amputee aftercare’” and “Celebrity surgeon ‘left patients in pain, to rot’”) are plainly directed to the quality of Dr Al Muderis’ post-operative care. Thereafter, the Articles are virtually the same. The focus on aftercare is reinforced at the commencement of the article:
[Dr Al Muderis] has been accused by patients and former staff of failing to provide adequate care following surgeries, leaving some people mutilated, wheelchair-bound or reliant on heavy pain medication.
92 There are several other examples in the body of these articles which support the respondents’ submission. Given these articles are virtually indistinguishable, the following examples are taken from the contents of the Age Article, which will apply mutatis mutandis to the SMH Article (any emphasis is added).
93 In the introductory portion of the article:
(1) the statement “[b]ut now more than 25 patients, 15 surgeons and a dozen of Al Muderis’ current and former business associates have told the Herald and 60 Minutes of concerns about the surgeon’s approach to patient selection and aftercare” and similarly “[i]nterviews with more than 25 patients, 15 surgeons and a dozen of Al Muderis’ current and former business associates have raised questions about the professor’s approach to patient selection and care”;
(2) the statement “[h]e has also been accused of using high-pressure sales tactics to boost patient numbers”;
(3) the statement “veterans Mark Urquhart and Brennan Smith claim they were not properly warned of the risks and were left in agonising pain”;
(4) the statement “Urquhart, a former paratrooper, claims to have been ignored when he found maggots in his leg after his bone was left exposed for years”; and
(5) the statement “Al Muderis denied using high-pressure sales tactics and apologised to patients who felt abandoned but said these were a disgruntled minority”.
94 In the remainder of the article:
(1) the article turns to the individual experiences of a number of Dr Al Muderis’ patients. One of these stories is that of Mr Urquhart and includes the statement that “the procedure left the veteran with a chronic infection and the worst pain he had ever experienced”. This is later followed by a description of the “Febreze incident” (discussed elsewhere in the judgment), being a matter that arose during post-operative care;
(2) the statement “[s]ome [patients] say risks were minimised when their operations were explained, complications ignored and patients left wheelchair-bound or mutilated”;
(3) the statement “Al Muderis acknowledged in an interview that mistakes had been made, and he apologised to patients who felt abandoned or hurt”. Later in the article, Dr Al Muderis’ comment includes “I acknowledge that people have the feeling that we did not do our duty of care. This is not the aim. We try our best to give every patient the care they deserve”;
(4) after returning to Mr Urquhart again, the statement “[f]or years, [Mr Urquhart] says he was told the smell of rotting flesh, redness, oozing pus and blood were normal and part of the healing process. Even when Urquhart’s wound was infested by maggots, he was told there was nothing to worry about”. The article also later describes “Al Muderis went ahead [with the surgery] nonetheless. A year later Urquhart was in unbearable pain”;
(5) following mention of Ms Stewart’s role with Dr Al Muderis’ clinic, the statement that she “quit in 2017 after she became uncomfortable with the clinic’s approach to patient selection and aftercare”;
(6) following mention of patients getting in touch after Dr Al Muderis became aware of the investigation, the statement “[s]upporters sent a large number of emails detailing the benefits of osseointegration and praising Al Muderis’ personal care”; and
(7) following mention of Dr Anstee, his comment directed to the management of complications that “[c]omplications will arise” and “if you do have a complication, you’ve got to wear it. You’re the surgeon. It’s your problem. You fix it”.
95 In the article’s break-out section:
(1) for Ms Todd, that she “has chronic pain after osseointegration” and her statement “I was standing in my laundry, and about half a litre of blood and pus came out of my leg. I’ve been dealing with infections ever since”;
(2) for Ms Ulrich, that after surgery she developed a blood clot which medical staff failed to detect, nearly costing her life;
(3) for Mr Smith, that he “was in so much pain from his osseointegration he began cutting his own skin off”, and his statement “[t]he after-care was non-existent”;
(4) for Mr Warland, that he “lost his house, relationship and job after pain related to osseointegration” and his statement that his experience since osseointegration has been “a rollercoaster”;
(5) for Mr Bruha, that Dr Al Muderis failed to treat a post-surgical infection, was difficult to contact and then downplayed the infection;
(6) for Ms Koolhoven, her complaint that after returning to California she “started running into problems and didn’t get answers”, followed by a summary of her experience of replacing her implant after falling post-surgery; and
(7) regarding an anonymous patient, the statement “he treated me like a cash cow”.
96 The respondents submitted, with reference to some of these examples, that ordinary reasonable readers of those articles are likely to have understood them as raising significant allegations and concerns about several aspects of Dr Al Muderis’ surgical practice, including disclosure of risks, patient selection, management of complications, adequacy of post-operative care, abandoning patients and questionable marketing and sales tactics, but not his competence in the operating theatre. The respondents noted for example, that conspicuously absent from the introductory section of the articles was any suggestion of negligence in the operating theatre. I agree that is what would have been conveyed to the ordinary reader.
97 The SMH Online Article and the Age Online Article, are materially the same as their printed counterparts, save for what is at [38], [51], [91], [97]-[98] of those matters, attached to this judgment as Annexures D and F. Those passages relate to pre- and post-surgical events. The Disputed Imputations regarding these articles are [16.4], [16.8], [16.13], [16.15], [16.20] and [16.23]. Of the additional passages [38], [51] and [91] are directed to post-surgery, while [97]-[98] are about patient selection.
98 Again, ordinary readers of those publications would have understood those articles to convey meanings that Dr Al Muderis has engaged in negligence (as the term is explained below) or other discreditable conduct in his practice as a surgeon generally (and particularly in relation to disclosure of risks, patient selection and post-operative care).
99 I am not satisfied that the Disputed Imputations in the Articles are conveyed.
Conclusion
100 It follows that I am not satisfied the Disputed Imputations, being [10.1]-[10.6] (Sneak Peek), [13.2], [13.6], [13.20] (Broadcast), [16.4], [16.8], [16.13], [16.15], [16.20], [16.23], [16.27], [16.29] and [16.30] (Articles) are carried. I am satisfied that the respondents can rely on those imputations containing the broader understanding of having surgery, as contextual imputations for the purpose of their contextual truth defence. I am also not satisfied that the Denied Imputations, being [13.24] (Broadcast) and [16.1] (in respect of the SMH Article, the SMH Online Article and the Age Online Article) are carried.
Section 4 — Meaning of “negligence” and “unethical” in the imputations
Negligence
101 An issue arose during closing about the meaning of negligence. The respondents submitted the pleaded imputations fall to be considered by reference to the ordinary meaning of terms, not their legal meanings, because it is the way the terms would be understood by ordinary reasonable people, not lawyers, and not taken to have a detailed knowledge of the law, citing inter alia, Trkulja at [32] and Herron v HarperCollins Publishers Australia Pty Ltd [2022] FCAFC 68; (2022) 292 FCR 336 (Herron) at [30], [73]. They submitted that therefore, for the purposes of the Publications and the pleaded imputations, “negligence” should not be equated with a failure to meet a particular legal or professional standard of competence. The respondents submitted that it would not, for example, have been understood by ordinary reasonable viewers and readers as requiring the existence of a tortious duty of care having regard to a complex reconciliation of “salient features” such as proximity, foreseeability, knowledge, control, vulnerability, reliance and public policy considerations. Nor, they contended, would it have been understood as connoting a failure by Dr Al Muderis to discharge such a duty by exercising the standard of care and skill expected of a specialist orthopaedic surgeon in his position (having regard to the consensus of medical opinion in that field) in order to guard against a reasonably foreseeable risk of injury, loss or damage. Such concepts are alien to ordinary reasonable viewers and readers. It was submitted that rather, in so far as the Publications conveyed meanings that Dr Al Muderis had acted “negligently”, they would have been understood by ordinary reasonable viewers and readers as amounting to an allegation that Dr Al Muderis had acted with neglect, by failing to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected. This might include acts of carelessness. They submitted that although dictionary definitions ought not be overemphasised, the respondents’ posited construction has the advantage of being broadly consistent with dictionary meanings of “negligence”.
102 The applicant’s written closing submissions accepted that one considers the natural and ordinary meaning of the word but contended that it corresponds with its legal meaning, such that legislation may ultimately feed into that meaning (and outlined the features that were contained within that meaning with reference to medical negligence case law). He submitted that an ordinary and reasonable person would understand that “negligence, medical negligence against a doctor, is a legal concept, and it is a legal term”. The applicant submitted that therefore:
[t]o prove an imputation that a doctor has been guilty of negligence requires proof not merely of an adverse outcome, nor even an error which a reasonably competent professional person acting with ordinary care might commit, but of [an] act or omission showing a lack of reasonable care or skill causing harm.
103 The applicant relied in aid of his submission on: Haddon v Forsyth [2011] NSWSC 123 (Haddon) at [241]; Lehrmann v Network Ten Pty Ltd (Trial Judgment) [2024] FCA 369 (Lehrmann) at [568]; and Edwards v Nine Network Australia Pty Ltd (No 5) [2024] FCA 422 (Edwards) at [161]. However, those cases reflect that it is the natural and ordinary meaning of terms, not their legal meanings, that apply. Although the legal meaning may provide some guidance (or may in some circumstances coincide with or closely resemble the natural and ordinary meaning), it is the ordinary and natural meaning of the words in the context in which they appear that is pertinent to the consideration: e.g. Haddon at [241] and Edwards at [161]. However, those cases do not reason that an ordinary and reasonable viewer would understand the word in issue to have a technical meaning, and therefore, the technical meaning is what would be conveyed.
104 I do not accept the applicant’s submission. The characteristics of the ordinary reasonable viewer or reader are described above (see Consideration in Part 2, Section 3).
105 The word “negligence” (or any deviation thereof) does not appear in the Publications, but is a term relied on by the pleader (see e.g. of the Imputations carried: [13.22], [16.2], [16.3], [16.6], [16.7], [16.12], [16.25], [16.26] and [28.4]). I agree with the respondents’ submission that, given that fact, ordinary and reasonable viewers and readers would not have understood the Publications to convey the legal concept of negligence. Properly considered, the ordinary reasonable viewers and readers of the Publications would consider that they were alleging in this regard that Dr Al Muderis had acted with neglect, by failing to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected. I do not consider that the natural and ordinary meaning of the word, in context, corresponds with its legal meaning.
106 The applicant’s submission is artificial. As the respondents correctly observed, the fallacy of the applicant’s submission is reflected by the features he said legal concepts encompassed, because the ordinary and reasonable viewer is not likely to have understood, let alone invoked, the concepts he identified.
107 In oral closing submissions, the applicant submitted that as the Amended Defence in relation to the respondents’ justification claim refers to negligence, it must be taken to mean the concept in its legal sense. However, the problem with that contention is that the Amended Defence (and evidence) is directed to responding to the imputations pleaded, and to justifying those imputations. The respondents’ reference to the word “negligence” for this purpose does not mean they accept the applicant’s contended meaning of it. As explained above, the ordinary reasonable viewer and reader would not have understood that negligence in the legal sense is what was conveyed. The pleaded imputations are relied on by the respondents to establish the justification defences. The respondents pleaded the Amended Defence in terms that corresponded to the SOC. They are not required to establish the substantial truth of something not conveyed by the Publications. The respondents are only required to establish what is conveyed is substantially true.
Unethical
108 The term unethical appears in Imputations [16.10], [28.8] and [28.9]. The meaning of unethical is also that which will have been understood by ordinary reasonable viewers and readers in its ordinary sense. It follows that in respect to the justification defence, which is a defence to the meanings published, the issue whether the words employed were true in substance and in fact is to be determined by reference to the same standard as to whether the defamatory meaning was conveyed. The respondents submitted that “unethical”, in the context of the Publications, meant conduct that fell short of the standards of honesty, integrity, candour, morality or propriety that ordinary persons in the position of Dr Al Muderis’ patients would have expected, citing, inter alia, the Australian Concise Oxford Dictionary 5th Edition as follows:
not ethical, esp. unscrupulous in business in professional conduct; see also the definition of ‘ethical’: 1 relating to morals, esp. as concerning human conduct; 2 morally correct; honourable.
109 I accept that is how the concept of unethical would have been understood.
PART 3 — FACT FINDING
Section 1 — Onus and standard of proof
110 As already referred to, the applicant bears the onus of proof in relation to whether the imputations are conveyed in the Publications. The respondents carry the onus of proof with respect to their defences.
111 As to the standard of proof, the Evidence Act 1995 (Cth) applies to these proceedings and s 140 of that Act is in the following terms:
(1) In a civil proceeding, the court must find the case of a party proved if it is satisfied that the case has been proved on the balance of probabilities.
(2) Without limiting the matters that the court may take into account in deciding whether it is so satisfied, it is to take into account:
(a) the nature of the cause of action or defence; and
(b) the nature of the subject-matter of the proceeding; and
(c) the gravity of the matters alleged.
112 The matters set out in subsection (2)(a), (b) and (c) are mandatory but not exhaustive considerations: see e.g. Roberts-Smith v Fairfax Media Publications Pty Ltd (No 41) [2023] FCA 555; (2023) 417 ALR 267 (Roberts-Smith) at [96]-[97].
113 The principles as to the approach to the application of s 140 are well established and have been discussed recently by this Court in, inter alia, Roberts-Smith at [96]-[110], and in the judgment of the Full Court, Roberts-Smith v Fairfax Media Publications Pty Ltd [2025] FCAFC 67 (Roberts-Smith (Appeal)) at [15]-[21]. They are not in dispute between the parties.
114 Nonetheless, it is appropriate to refer briefly to the discussion in Roberts-Smith (Appeal). There, the Court observed that “[t]he difference between the criminal and civil standards of proof is ‘not a mere matter of words’ but one of ‘critical substance’; in a civil case, ‘no matter how grave the fact which is to be found … the mind has only to be reasonably satisfied’”, quoting Reifek v McElroy [1965] HCA 46; (1965) 112 CLR 517: Roberts-Smith (Appeal) at [16]. The Full Court recited with approval the passage from Bromwich J in Australian Competition and Consumer Commission v Delta Automation Pty Ltd [2023] FCA 880 at [56]-[57]. The Court also quoted from the oft cited passage from Briginshaw v Briginshaw [1938] HCA 34; (1938) 60 CLR 336 at 362:
But reasonable satisfaction is not a state of mind that is attained or established independently of the nature and consequence of the fact or facts to be proved. The seriousness of an allegation made, the inherent unlikelihood of an occurrence of a given description, or the gravity of the consequences flowing from a particular finding are considerations which must affect the answer to the question whether the issue has been proved to the reasonable satisfaction of the tribunal. In such matters “reasonable satisfaction” should not be produced by inexact proofs, indefinite testimony, or indirect inferences …
115 The Full Court also referred to Neat Holdings Pty Ltd v Karajan Holdings Pty Ltd [1992] HCA 66; (1992) 110 ALR 449 at 450, before observing that these principles have effectively been codified in s 140 of the Evidence Act.
116 As recently explained by the High Court in GLJ v The Trustees of the Roman Catholic Church for the Diocese of Lismore [2023] HCA 32; (2023) 97 ALJR 857 at [57] per Kiefel CJ, Gageler and Jagot JJ:
Section 140(2)(c) of the Evidence Act reflects the position of the common law that the gravity of the fact sought to be proved is relevant to “the degree of persuasion of the mind according to the balance of probabilities”. By this approach, the common law, in accepting but one standard of proof in civil cases (the balance of probabilities), ensures that “the degree of satisfaction for which the civil standard of proof calls may vary according to the gravity of the fact to be proved”.
117 As those and other cases outline, cogent evidence commensurate with the seriousness of the allegations is required. I have approached the standard of proof in accordance with these principles.
118 The respondents accepted that the gravity of the conduct alleged against Dr Al Muderis is serious and that a high degree of moral opprobrium attaches to conduct of the kind alleged.
119 The respondents also submitted that the approach to fact-finding necessitated by s 140(2) is equally applicable to: (a) each of the factual findings that Dr Al Muderis seeks against the respondents in support of his alleged entitlement to aggravated damages; and (b) each of the factual findings that Dr Al Muderis invites the Court to make in defeasance of the respondents’ honest opinion defences. The respondents submitted that Dr Al Muderis seeks serious adverse findings in relation to the respondents’ honesty (wherein the applicant asserted, inter alia, that the respondents engaged in a campaign to denigrate him and conspired with former patients to concoct complaints) tantamount to allegations of dishonesty or fraud.
120 I accept that s 140(2) also applies to the allegations made by the applicant.
121 I have applied s 140(2), and the principles relating thereto, to my assessment of the evidence and factual findings.
Section 2 — Browne v Dunn
122 The applicant criticised the respondents for failing to cross-examine his expert witnesses and put certain propositions to them, including by allegedly failing to cross-examine them about alleged “standard practices”. The applicant also submitted the respondents failed to cross-examine medical professionals present at the consultations. The applicant alleged this conduct breached Browne v Dunn (1893) 6 R 67.
123 The respondents submitted, referring to authority as to the import of Browne v Dunn, that there were no such breaches. The respondents submitted that they were required to go into evidence by affidavit (including expert evidence) on matters in respect of which they bore the burden of proof before the applicant. The applicant also had the benefit of the detailed particulars of justification in the respondents’ Amended Defence. By the time the respondents had served all their evidence and expert reports, the applicant was properly on notice of the case being advanced and the case he would have to meet at trial. This included the patients’ recollections of what they were told or not told during consultations.
124 As to the complaint about the cross-examination of others present at the consultations, the respondents correctly observed that, overwhelmingly, the evidence adduced by Dr Al Muderis from persons who were present at consultations was silent as to what they saw, observed, and said in those consultations. The respondents submitted that they were not required to cross-examine to “plug [the] holes” in the applicant’s evidence. The evidence had been challenged in the manner described (i.e. the respondents had already put on their evidence addressing the issues).
125 The respondents submitted that, in those circumstances, they had discharged their obligations pursuant to the rule in Browne v Dunn, citing Seymour v Australian Broadcasting Commission (1977) 19 NSWLR 219 at 224; Allied Pastoral Holdings Pty Ltd v Federal Commissioner of Taxation [1983] 1 NSWLR 1; (1983) 44 ALR 607 (Allied Pastoral Holdings) at 16; Masterton Homes Pty Ltd v Palm Assets Pty Ltd [2009] NSWCA 234; (2009) 261 ALR 382 (Masterton) at [105]; Oneflare Pty Ltd v Chernih [2017] NSWCA 195 at [40], [42]; Fairfax Media Publications Pty Ltd v Gayle [2019] NSWCA 172; (2019) 100 NSWLR 155 at [123]-[128].
126 Of these authorities, the respondents expressly referred to Masterton in their oral submissions, reciting the passage at [105]:
While the evidence was not cross-examined on, that does not necessarily mean that the judge was obliged to accept it. A judge can reject evidence that has not been cross-examined on if, for example, it was inconsistent with other evidence that he accepted, or if it was inherently incredible: Sullman v Sullman [2002] DFC ¶95-248; [2002] NSWSC 169 at [304]-[306]; Caldwell v J A Neilson Investments Pty Ltd (2007) 69 NSWLR 120; [2007] NSWCA 3 at [96]; Ellis v Wallsend District Hospital (1989) 17 NSWLR 553 at 586-8. Nor did the rule in Browne v Dunn (1893) 6 R 67 (Browne) prevent the judge from rejecting the evidence. That is because Ms Maude had given her evidence on affidavit in advance of the trial … and Mr Miles had replied to that affidavit in advance of the trial … Exchange prior to trial of affidavits that disclose the position of the respective parties concerning a particular evidentiary matter can prevent a Browne point being successfully raised: West v Mead (2003) 13 BPR 24,431; [2003] NSWSC 161 at [95]-[99]. Thus, I do not accept that the absence of cross-examination required the judge to accept [the witness’] evidence.
127 The other authorities referred to above are to the same effect.
128 The applicant did not address these submissions, or Masterton, in his written reply filed after the oral hearing, but rather chose simply to repeat the criticism he made earlier.
129 Rather, in his reply, the applicant relied on Griffiths v TUI (UK) Ltd [2023] UKSC 48; (2023) 3 WLR 1204 (Griffiths) to contend that the consequence of the failure to challenge the plaintiff’s expert in that case was that the Supreme Court accepted that unchallenged evidence, allowing the appeal accordingly (at [78]). That submission is misplaced. Leaving aside the question of whether there was a failure to cross-examine in this case, Griffiths does not support a conclusion that the failure of the respondents to challenge the applicant’s experts’ evidence in cross-examination in this case meant the evidence should not be permitted to be challenged in address. To the contrary, at [69] of Griffiths, Lord Hodge DPSC (with whom the Supreme Court agreed) referred to Browne v Dunn as a rule of fairness, and not an inflexible one, with its application varying depending on the circumstances of the case. I do not accept the applicant’s submission. Further, Griffiths is a case factually far removed from this one. In that case, no affidavit or report was ultimately relied on by the cross-examiner in advance, meaning that the expert evidence was uncontroverted as it was not in conflict with any other evidence led at the trial.
130 This case is to be considered in the context of the authorities referred to above at [125]-[126]. The applicant was on notice of the respondents’ case. In respect to the expert evidence, the applicant chose to lead rather limited evidence from his experts in his case. As discussed elsewhere, there is an issue with the independence of these witnesses. If the applicant chose not to address certain topics in his experts’ evidence, the respondents are not required to cross-examine them.
131 As to the cross-examination in relation to the consultations, the applicant was on notice of the respondents’ case on this topic. I note that in limited circumstances, the applicant’s witnesses who were present at Dr Al Muderis’ consultations did address in their affidavit evidence a particular consultation with a patient (for example, Mr Grieve and Mr Urquhart), which reflects the obvious, that he was on notice of the respondents’ case. That the applicant chose not to have his witnesses address other consultations in their affidavits, was a forensic decision he made. I accept the respondents’ submission, that they were not required to plug holes in the applicant’s evidence.
132 The applicant’s submissions fail to appreciate the premise of Browne v Dunn, it being a rule of practice underpinned by procedural fairness. It applies where the other party is not on notice of the cross-examiner’s intention to rely on a particular matter, to give the witness an opportunity to respond to it: see e.g. Allied Pastoral Holdings at 16. That is not this case.
133 I am not satisfied that there has been any breach of Browne v Dunn in relation to the topics referred to above.
Section 3 — Jones v Dunkel
134 The applicant relies on what he says is the respondents’ failure to call witnesses: Jones v Dunkel [1959] HCA 9; (1959) 101 CLR 298; the failure to ask witnesses who are called (by either side) about material matters: Commercial Union Assurance Company of Australia Ltd v Ferrcom Pty Ltd (1991) 22 NSWLR 389 (Ferrcom); the failure to tender relevant documents: Jones v Dunkel at 320-321; and the act of destroying relevant documents: Allen v Tobias [1958] HCA 13; (1958) 98 CLR 367 (Allen v Tobias) at 375-376, submitting that these are all matters which the Court ought to take into account in deciding whether the respondents have discharged their various burdens of proof.
135 During oral closing submissions, the applicant identified persons he said should have been called such that the failure to do so engages Jones v Dunkel. Before addressing those submissions, it is necessary to consider the principles discussed in Jones v Dunkel because, generally, the way in which those submissions were advanced, failed to grapple with such principles.
136 The rule is that the unexplained failure of a party to give evidence may, in appropriate circumstances, lead to an inference that the uncalled evidence would not have assisted that party’s case, so entitling a court to more readily draw an inference against that party: Jones v Dunkel at 308, 312, 320-321; Cubillo v Commonwealth (No 2) [2000] FCA 1084; (2000) 103 FCR 1 (Cubillo) at [353]. The rule only applies where a party is “required to explain or contradict” something. No inference can be drawn unless evidence is given of facts “requiring an answer”: see Jones v Dunkel at 319, 321-322; Cubillo at [355]; Schellenberg v Tunnel Holdings Pty Ltd [2000] HCA 18; (2000) 200 CLR 121 at [51]; Fonterra Brands (Australia) Pty Ltd v Viropoulos (No 3) [2015] FCA 1050 at [103]. The rule is not to be used to complete gaps in the evidence or to convert conjecture into inference. As explained in Cubillo at [353], while it is possible to state the rule in general terms, its application must be considered in relation to each situation in which a witness is alleged to be absent.
137 I will address the submissions in respect to the nominated witnesses when considering evidence on the topic.
138 However, there are three matters appropriate to address at this stage.
139 First, the applicant submitted that an inference should be drawn from the respondents’ failure to call its confidential sources. The applicant accepted during closing submissions, that was a rational decision because if they were called to give evidence, they could have been asked questions about whether they were a confidential source, therefore rendering it rational for the respondents to protect them by not calling them. In relation to the s 29A public interest defence, he submitted the witnesses ought to have been called because there is a dispute with Ms Grieve’s affidavit being “wholly inconsistent with her notes in serious respects” in circumstances where Ms Grieve destroyed documents. The sources were also said to be relevant to the truth defence, where the applicant asserted that Drs Phil Huang, Sean Nicklin, and Andrew Wines, as well as Mr Steven Gray are confidential sources who had direct interactions with various patients. The applicant submitted that the respondents “tactically elect[ed] to not call key witnesses. Every inference can be drawn against them for that”. When pressed that there was an accepted rational basis for the respondents’ decision not to call the sources, he submitted the failure should be “held against them” arguing it was a “reasonable journalistic decision, not a litigation decision”. When pressed on what the inferences were, the applicant submitted that:
The inference is that, for Mr Mortimer, the evidence of Mr Gray could not have assisted them. For Mr Urquhart, the evidence of Dr Huang could not have assisted them. … I can’t say that there’s – they positively would have said things. All I can say is that they couldn’t have assisted the respondents’ case.
140 Reciting the summary of the submissions reflects the generality in which they were advanced.
141 The submission falls at the first hurdle. Jones v Dunkel is only triggered when the failure of a party to call a witness is unexplained. As the respondents submitted, in relation to the confidential sources, the obvious and reasonable explanation for the respondents’ failure to call any of them as witnesses is the existence of the respondents’ confidentiality obligations, which were upheld by the Court: Al Muderis v Nine Network Australia Pty Ltd [2023] FCA 1623. Indeed, as mentioned above, the applicant accepted that the decision not to call them is a rational one. The distinction drawn by the applicant between a journalistic and a litigation decision for the purposes of Jones v Dunkel, is artificial. It has no support in Jones v Dunkel. Not surprisingly, explanations for a failure to call a witness often include matters personal to the witness (e.g. ill-health). The question is whether the failure to call the witness is unexplained. On the applicant’s own submission, this failure is explained, and as the applicant accepted, the decision is plainly a rational one.
142 The applicant’s submission that there was evidence the respondents had made an agreement with their confidential sources not to call them, has no foundation. The applicant does not point to any such evidence, but rather simply makes the bald assertion.
143 In any event, the applicant did not and could not articulate the inference sought to be drawn. The submission that “every adverse inference” ought to be drawn against the respondents for failure to call their confidential sources is meaningless, without identification of the inferences and the basis for them. To submit simply that the witness would not assist the respondents’ case of a particular patient is plainly insufficient. So too, is a generalised assertion about inconsistencies in relation to Ms Grieve’s affidavit in circumstances where the applicant pointed to no specific inconsistency. The applicant must, inter alia, identify the inference sought in each case and the existing ground in the evidence that would warrant the drawing of that inference: see Jones v Dunkel at 309-310. Nor has the applicant identified what is required to be explained, contradicted, or answered.
144 I am not prepared to draw any Jones v Dunkel inference in relation to the confidential sources.
145 Second, as the respondents submitted, there is no obligation on a party to adduce evidence that is merely corroborative of, or cumulative upon, other evidence. The rule does not compel time to be wasted by calling unnecessary witnesses: Cubillo at [360]; s 164(1) Evidence Act.
146 The submissions in respect to lay witnesses also generally suffered from the same failures. To take one example. In respect to Mr Billy Wynne III, the applicant submitted that his wife, Ms Wynne, was a witness to many of the events described in his affidavit, and although she sat in the courtroom during his evidence, she was not called as a witness, such that a Jones v Dunkel inference should be drawn accordingly. That was the extent of the submission, with no identification of the inferences the applicant was asking the Court to draw or the basis of them. As the respondents submitted, her evidence was “unneeded”.
147 I am not prepared to draw an adverse inference from the failure to call Ms Wynne.
148 Third, the applicant placed reliance on the respondents’ failure to call Dr Solon Rosenblatt, (Dr Al Muderis’ former representative in the United States), to give evidence. The respondents submitted the evidence was equivocal as to which party’s ‘camp’ he resided. Although the respondents accepted that Dr Rosenblatt was one of the respondents’ sources – in that he spoke to Ms Grieve – they pointed to the evidence in Dr Al Muderis’ cross-examination, that he was also in regular communication with Dr Rosenblatt concerning Ms Lisa Çalan, including during, or very shortly before, the commencement of the trial. It was submitted in those circumstances that although there may have been some falling out, there was some evidence to suggest that position did not persist given Dr Al Muderis’ evidence as at 22 September 2023, which indicated he was receiving recent updates from Dr Rosenblatt.
149 The respondents submitted that no inference should be drawn, rather it is a neutral point, because Dr Rosenblatt cannot be said to be in the respondents’ camp.
150 I accept the position of Dr Rosenblatt is unclear, and therefore in that circumstance, I am not prepared to draw any Jones v Dunkel inference.
151 On the other topics raised by the applicant, I note the submission about the failure to tender relevant documents is based on Jones v Dunkel at 320-321 and involves the same reasoning process as described above. A similar process is involved in reasoning in respect to the failure to ask witnesses who are called about material matters, which is described as a Ferrcom inference. These matters are addressed when they arise in considering the evidence.
152 In relation to the final matter – the act of destroying relevant documents – I return to address Allen v Tobias in detail below in considering the s 29A defence in Part 9.
Section 4 — Contemporaneous documents
153 In summary, the applicant submitted that the Court should proceed on the basis of the contemporaneous documents and the evidence of Dr Al Muderis’ standard practice, where there is a conflict between such evidence and the evidence of a patient.
154 The applicant submitted that fact-finding should be based, as much as possible, on “contemporary materials, objectively established facts and the apparent logic of events”: Fox v Percy [2003] HCA 22; (2003) 214 CLR 118 at [31]. Contemporary documents are usually the most reliable source of evidence as to what occurred and are usually a good reference point for assessing the reliability of witness testimony: ET-China.com International Holdings Ltd v Cheung [2021] NSWCA 24 at [25]. While the evidence of witnesses should not be disregarded, greater weight is usually accorded to contemporaneous documentary evidence, citing Bathurst Regional Council v Local Government Financial Services Pty Ltd (No 5) [2012] FCA 1200 (Bathurst) at [1247]-[1248]; Hughes v St Barbara Mines Ltd (No 4) [2010] WASC 160 at [157]; Volonakis v Erceg [2019] NSWSC 1875 (Volonakis) at [150]; Sampson in his Capacity as Trustee for the Bankrupt Estate of Tannous v Tannous [2022] FCA 1427 (Sampson v Tannous) at [61].
155 The applicant pointed to three factors which he submitted support the proposition that his documents can be expected to be a reliable record of what occurred: (1) Dr Al Muderis’ documents were created contemporaneously, and with a small handful of exceptions, before there was any reason to believe that there would be a controversy in relation to the patient’s care; (2) in many cases, the document is not Dr Al Muderis’ document alone. Many of the documentary exhibits were created partly or wholly by nurses or fellows or formed part of hospital records. The notion that those documents are inaccurate, incomplete or unreliable implies that other professionals were also negligent or complicit in misconduct; and (3) in many cases, Dr Al Muderis’ consultation reports were provided to the patient him or herself at the relevant time. If the reports misrepresented what occurred at the consultation, one might expect the patient to have taken issue with this.
156 The applicant submitted that where so many of the facts in issue concern medical advice, which may be complex and nuanced, or diagnosis, which may depend on precise details, witness evidence alone (particularly lay witness evidence) is generally an unreliable basis on which to make findings. He submitted that is not to say that the witnesses were necessarily subjectively dishonest, citing M v The Queen [1994] HCA 63; (1994) 181 CLR 487 at 534 and Wong v National Australia Bank Ltd [2022] FCAFC 155 at [129], although the applicant contended that in some cases they were.
157 The applicant pointed to several reasons why the recollections of witnesses may be unreliable, even when the witness is adamant about the quality of their memory. He also submitted that, in addition to specific credibility issues regarding each witness, which I address when considering that witness, there were some general reasons why less reliance could be placed on the witness testimony in this case, especially in so far as it is inconsistent with documentary evidence.
158 The applicant submitted that this included: (1) the complexity of the medical issues is such that witnesses (especially lay witnesses) are unlikely to be able to recall the relevant facts with the level of specificity or precision necessary to reliably support findings on key questions, such as whether a patient had an infection at a particular time; (2) although it might sometimes be thought that a patient is more likely to have an accurate memory of a medical consultation or procedure, because it is a major event in their life, that reasoning is less plausible in this case because most of these patients have complex medical histories and have had many procedures and consultations with a number of different specialists; (3) there are examples of patients talking to each other about their experiences with Dr Al Muderis and about this proceeding. The patient’s perception of their experience with Dr Al Muderis and their evidence may have been influenced by information or opinions shared by others; and (4) in the majority of cases, the patients did not come forward with any complaints about the care they had received from Dr Al Muderis until after the publication of the matters. The patients’ perception of their experience with Dr Al Muderis may have been influenced by the way he was represented in the matters. The applicant submitted that as the lay witnesses gave their evidence-in-chief by way of affidavits, contemporaneous documentary evidence is of greater importance, referring to Lehrmann at [763]-[764]. He also submitted the oral evidence of a witness carries greater significance than affidavits curated by lawyers. The applicant referred to Lehrmann at [763]-[764], where Lee J said, in the circumstances of that case, that affidavit material would be accepted if it was persuasive “in the sense that it [did] not jar with candid contemporaneous representations”.
159 The premise underlying the reliance on contemporaneous documents is uncontroversial: Sampson v Tannous at [62]. Where there are disputed facts from events occurring many years ago, contemporaneous documents, where available, “are invaluable and often more revealing of the true position than flawed attempts at recollection by those with an interest in the outcome of the litigation”: Bathurst at [1247]. That is not to suggest that evidence of witnesses should be disregarded. Rather, it is said that greater weight is usually accorded to contemporaneous documentary evidence.
160 As the respondents correctly submitted, this is not to be elevated to an inflexible rule. The authorities make clear that these are questions of fact that turn on the quality of the evidence in each case, bearing in mind the issues for determination: Volonakis at [150]; Sampson v Tannous at [62].
161 That said, I am mindful of the frailties of human recollection and the difficulties which affidavits can present. I am also mindful of the effect of the passage of time on human memory and the processes of memory being overlaid by perceptions or self-interest as well as conscious considerations of what should have been or could have been said. I must also bear in mind the possible effect of rumours and discussions and the capacity of the human mind for ex post facto rationalisation of events and the phenomenon of false memories: see discussion in Roberts-Smith at [163]-[166]. I take these matters into account in assessing the evidence. The respondents submitted that the patients’ evidence was compelling, consistent on key issues and corroborated by contemporaneous records. I address this when considering the case studies.
162 I consider the documentary evidence below, in application to the evidence and issues in this case. Suffice to say at this stage, the application of the principles is not as straightforward as the applicant suggests. For example, the applicant’s submissions as to his documents and their reliability treats them all the same. As explained below, I accept that in relation to documents generated by him, or on his behalf, there are issues as to their reliability (for some). As the respondents submitted, many of Dr Al Muderis’ documents and record-keeping appeared to be formulaic and riddled with errors, and as described elsewhere, no contemporaneous consultation reports appear to exist in relation to some consultations. I note also that although the applicant submitted his documents are to be relied on, in some instances he claims a meaning to them, or a qualification on their contents which is contrary to the plain reading. It is to be borne in mind also that although the applicant’s submission is referring to medical records, the contemporaneous records in this case are broader.
163 I assess each witness below. In assessing the credit of a witness and their reliability, it is necessary to have regard to the whole of the witness’ evidence while at the same time recognising that the witness may be correct as to one matter and mistaken as to another, or truthful as to one matter and dishonest as to another. It is uncontroversial that the rejection of a witness’ evidence on one topic does not necessarily mean they are not to be accepted on others: CCL Secure Pty Ltd v Berry [2019] FCAFC 81 at [94]. It has long been recognised that it is for the Court, having seen and heard the witness, to decide whether the evidence is worthy of acceptance, which may involve accepting or rejecting the whole of the evidence, or accepting some and rejecting the rest: Cubillo at [118]-[123]. As will be apparent from the discussion in relation to the patient case studies, for the most part, the evidence I have relied on is supported by other evidence. Although the supporting evidence may be in the form of contemporaneous documentation, it is not necessarily confined to that. It may also, depending on the circumstances, be in the form of evidence from other witnesses, including other patients and the applicant himself.
164 This simply illustrates at this stage, as explained in the authorities, that the application of the principles is to be considered on the evidence.
Section 5 — Standard practice
165 The applicant referred to many authorities as to the relevance of Dr Al Muderis’ standard practice. This included Elliott v The Queen [2007] HCA 51; (2007) 234 CLR 38 at [28], where the High Court succinctly described as a “basic proposition” that:
To prove an act has been done, it is admissible to prove any general course of business or office, whether public or private, according to which it would ordinarily have been done, there being a probability that the general course will be followed in the particular case.
See also Connor v Blacktown District Hospital [1971] 1 NSWLR 713 at 721.
166 The applicant submitted that if a professional person habitually follows an established practice or procedure in certain situations, it is reasonable to infer that it is more likely than not that he or she would have followed the same practice on the relevant occasion.
167 The applicant referred to two cases where he said this principle has been applied to make findings about the content of advice given by professionals such as lawyers and doctors to illustrate his point: Palios Meegan & Nicholson Holdings Pty Ltd v Shore [2010] SASCFC 21; (2010) 108 SASR 31 (Palios); and Phelan v Melbourne Health [2019] VSCA 205 (Phelan) respectively.
168 The respondents took issue with the applicant’s description that Phelan bears a factual resemblance to this case. Briefly summarised, the issue in Phelan was whether certain medical advice had been given, in circumstances where the patient purported to have a specific recollection that it was not, and where the doctors had no specific recollection of that patient but said the advice in question “would have been given” because it was their standard practice to give that advice in such cases. The respondents pointed out that Phelan concerned only one patient, whereas this case involves a “significant cohort of patients giving strikingly similar evidence”. In reply, the applicant submitted it makes no difference that there is more than one patient, as each individual case must be analysed on its own merits. Both approaches are rather simplistic. There are several factual differences between this case and those relied on by the applicant, and the reasoning in Phelan depended in part on the evidence particular to that case and on the credit findings in respect to the relevant witnesses. That said, the fact that there is more than one patient who gives evidence on a topic, depending on the evidence, may be relevant. The applicant’s submission fails to recognise that while individual cases are to be analysed, depending on the evidence, they are not to be done so in isolation.
169 The applicant submitted that the respondents do not grapple with the significance of the evidence of Dr Al Muderis’ standard practices.
170 However, properly read, Phelan (and Palios) illustrate no more than each case is fact specific. As the Court observed in Phelan at [84]:
Plainly, the weight to be given to the evidence of usual practice, and the question whether that evidence is to be preferred, must depend upon the specific nature and quality of the evidence that is given in the particular case.
171 The applicant’s closing written submissions devoted a section to this topic entitled “standard processes and procedures in Dr Al Muderis’ practice”, which addressed the following: the booking process and arrival at Dr Al Muderis’ rooms; the assessment by Dr Al Muderis and other specialists; the discussion of risks and complications; consultation reports; post-consultation procedures; procedures on the day of the surgery; and rehabilitation and post-operative procedures. Some of these topics are more contentious than others. For some, while the fact of an event occurring may not be contentious, the content of it may be.
172 Where relevant, I address these topics below. However, several issues arise as to the content of what is said to be Dr Al Muderis’ standard practice. To take four examples.
173 First, in so far as consultation reports are addressed by the applicant under this section, it is difficult to understand what is said to be the relevant standard practice except that either Dr Al Muderis or a fellow would dictate the consultation report. For example, if the purpose of these reports is said to be part of the standard practice, the evidence in the applicant’s case as to this, is inconsistent. If it is the content of the reports that is said to be part of the standard practice, there are issues as to the accuracy and reliability of some of the reports. No consultation reports appear to exist in relation to some consultations.
174 Those and other issues with the consultation reports are addressed separately below (see Part 6, Section 1).
175 Second, in so far as the affidavit evidence of Dr Al Muderis and the other doctors from his clinic who gave evidence refers to a standard practice – including in respect to conducting group consultations and what is said about risks and complications at such consultations – that practice is stated in absolute terms. However, the practice described did not apply to the American (or other international) patients who were called in this case. Indeed, what occurred in relation to those patients, as reflected in the consideration of those patients below, does not accord with the practices referred to in the applicant’s affidavit evidence (or that of his witnesses).
176 Third, on some of the occasions in cross-examination where the applicant referred to what he did as part of his standard practice, it is only his evidence of that practice being standard (particularly, in relation to some of the American patients). For example, his evidence in cross-examination was that he routinely tells international patients that their surgery booking is only “tentative” and therefore not confirmed. This is addressed below but suffice to say that his evidence of that purported standard practice is inconsistent with all the relevant documentation sent to those patients from his office.
177 Fourth, I will address the issues in relation to risks and complications below. Suffice to say, although the witnesses for the applicant gave evidence of what they say was a standard practice regarding what the patients are told, there are inconsistencies between them. For example, Dr Al Muderis asserted that he told all patients that “infection is a matter of when, not if” and that “there is a 100% chance that [they] will develop an infection at some stage”. Although Dr Kevin Tetsworth also gave evidence that every patient is told there is a 100% chance of getting an infection, Drs Tim O’Carrigan and Chris Basten and Ms Claudia Roberts referred only to this being regularly said, and Dr Karan Doshi did not recall it being said at all (and agreed that if it was said, it was important to be recorded in the consultation report). I note for completeness that Ms Shona Stewart (a former nurse called by the respondents) said some patients may have been told that but did not remember it being “part of every conversation”. It was put to only some patients in cross-examination, and even fewer said they were told that information. As explained below, only one of the consultation reports in evidence recorded that was said. In relation to the other reports concerning the patients’ first consultations, those tendered generally recorded that there was a “low”, or “relatively low risk” of infection: see Consultation reports, Part 6, Section 1 below.
178 Those examples serve to illustrate that, as described in Phelan, the question of whether standard practice evidence is to be preferred, depends upon the specific nature and quality of the evidence that is given in a particular case. It also depends on the issues to be determined in the case. It is unnecessary to make findings about matters not relevant to determining the issues in the proceedings. Therefore, it is neither necessary nor appropriate to determine Dr Al Muderis’ standard practice on a topic (if there be one) in a vacuum. I return to this topic below.
PART 4 — DEFENCES: INTRODUCTORY REMARKS
179 The respondents rely on three defences: contextual truth, honest opinion and public interest. Although justification is pleaded, it is only a complete defence where all imputations are substantially true, and the respondents did not plead that in respect to four imputations (being, [13.24], [16.9], [16.28] and [28.6]). As the respondents submitted in closing, on truth, this is a case of contextual truth. That said, it is necessary for that purpose to consider the concept of substantial truth.
180 The respondents submitted in closing that I could commence by considering the public interest defence, and if that was found to be established, it would be unnecessary to consider the remaining defences. However, given the time devoted to the justification defences, I consider it appropriate to commence with that issue. I then turn to consider the public interest defence.
181 Given my conclusions in respect of those two defences, I do not consider it necessary to consider the honest opinion defence. It would unnecessarily delay delivering what is already a very lengthy judgment.
182 It is appropriate to recall, as observed at the outset, that this is not a medical negligence case. The relevant issues are determined based on the principles applicable in defamation proceedings.
183 As a preliminary note to the reader, this judgment includes many extracted quotes from evidence including, inter alia, transcripts, messages, emails, medical reports and other documentary evidence. This has been done to accurately capture the evidence before the Court and the experiences of the witnesses in their own words. In most cases, I have extracted the quotes verbatim such that any typos or grammatical errors that were originally contained within the source document have been reproduced. Where necessary to understand the meaning of a quote in context, I have replaced certain aspects as delineated by square brackets.
PART 5 — SECTIONS 25 AND 26
Overview
184 The respondents presented their case on this defence by calling patients to give evidence of their experiences with Dr Al Muderis. The respondents called 29 patient witnesses, with the hearing involving 33 patient case studies (two patients were deceased, Mr Ford and Mrs Gollan; one patient was not available to testify, Ms Young; and one patient had an affidavit from her filed by the applicant, but she was not called, Patient X). This included not only those named in the Publications, but a broader range of patients. Mr Urquhart, Mr Smith, Mr Bruha, Ms Ulrich, Ms Todd, Ms Koolhoven (formerly Ortiz), and Mr Warland, were patients referred to in the Publications and have a case study. Mr Mortimer was a confidential source of Ms Grieve who later agreed to give evidence.
185 There were both osseointegration and orthopaedic patients. Those patients were presented, in effect, as case studies, with additional evidence being led from other witnesses (e.g. medical and expert witnesses) and documents tendered (e.g. medical records and correspondence) in relation to each case study. These reasons will address each of the case studies individually, which will involve a consideration of the evidence relied on by the respondents and the applicant for each patient. It is after considering each of the case studies that the defamatory stings to the Publications (discussed below) will be addressed.
186 It is helpful to outline the structure of this section. After some preliminary observations in respect to the pleadings, the relevant legal principles will be referred to.
Preliminary observation
187 There is a dispute between the parties as to the adequacy of the pleadings in respect to this aspect of the proceedings.
188 The principal bases for the applicant’s complaint were that various aspects of the respondents’ evidence have not been particularised in the defence; in defamation cases the matters and circumstances supporting a defence of justification or contextual truth must be particularised with detail and specificity; and anything outside of the particulars in the defence is not relevant. The applicant contended that he should not be required to defend every aspect of his treatment of the 33 patients pleaded in the defence without notice. It was submitted that it was necessary to plead which aspects of the treatment were alleged to have been improper.
189 This complaint as to the pleadings was not raised prior to the hearing and nor was there any application to strike out aspects of the defence.
190 To the contrary, the matter proceeded to hearing by the filing of affidavits by each party in respect to the applicant’s primary case and the respondents’ defences, including justification. There was no suggestion that the applicant was unable to prepare evidence in response to affidavits filed by the respondents in relation to the patients (and any medical evidence). The premise underpinning the applicant’s submission – that he was not on notice of various matters referred to in the respondents’ affidavits (filed in advance of the applicant’s evidence) – was generally not accepted during the hearing. The rulings I made on each objection on this basis are evident from the transcript, and it is not necessary or appropriate to refer to each occasion. Below are some additional observations.
191 The pleading is to be assessed against the purpose it is to serve. It is important in that context to remember, as Dawson J said in Banque Commerciale S.A., En Liquidation v Akhil Holdings Ltd [1990] HCA 11; (1990) 169 CLR 279 at 293, “[p]leadings are but a means to an end and not an end in themselves”.
192 In Thomson v STX Pan Ocean Co Ltd [2012] FCAFC 15 at [13], the Court observed that:
It is well-established that the main purposes of pleadings are to give notice to the other party of the case it has to meet, to avoid surprise to that party, to define the issues at trial, to thereby allow only relevant evidence to be admitted at trial and for the trial to be conducted efficiently within permissible bounds: see, eg Dare v Pulham [1982] HCA 70; (1982) 148 CLR 658 (at 664–665). However, it is also well-established that pleadings are not an end in themselves, instead they are a means to the ultimate attainment of justice between the parties to litigation: see Banque Commerciale S.A. (in liq) v Akhil Holdings Ltd [1990] HCA 11; (1990) 169 CLR 279 (at 293) per Dawson J who cites Isaacs and Rich JJ in Gould and Birbeck and Bacon v Mount Oxide Mines Ltd (in liq) [1916] HCA 81; (1916) 22 CLR 490 (at 517). For these reasons, the courts do not, at least in the current era, take an unduly technical or restrictive approach to pleadings such that, among other things, a party is strictly bound to the literal meaning of the case it has pleaded. The introduction of case management has, in part, been responsible for this change in approach: see the observations of Martin CJ in Barclay Mowlem Construction Limited v Dampier Port Authority [2006] WASC 281; (2006) 33 WAR 82 (at [4]–[8]). Even before the widespread use of case management, the High Court reflected this approach in decisions such as Leotta v Public Transport Commission (NSW) (1976) 50 ALJR 666 (at 668–669) per Stephen, Mason and Jacobs JJ and Water Board v Maustakas [1988] HCA 12; (1988) 180 CLR 491 (at 497) per Mason CJ and Wilson, Brennan and Dawson JJ.
193 This was recently cited with approval in Allianz Australia Insurance Limited v Delor Vue Apartments CTS 39788 [2021] FCAFC 121; (2021) 287 FCR 388 at [152].
194 Although this case alleges defamation, these principles apply with equal force.
195 In Herron, a ground of appeal related to the admissibility of evidence in relation to patients who were not particularised in the defence. At [404] of Herron, the factual basis of the ground was described by Lee J as follows:
Dr Gill submitted the primary judge erred in admitting and relying on evidence in respect of patients treated at Chelmsford who were not particularised in the publishers’ defence. It is said that the publishers relied upon evidence (both medical records and hearsay notices) that went well beyond the patients identified in their defence as “case studies” who suffered adverse outcomes during their treatment and other patients who are said to have not consented (or provided informed consent) to the treatment they received at Chelmsford.
196 The argument was ventilated during cross-examination of the witnesses on the eighth day of the hearing (though it had been raised on the fourth day and was deferred). At [415] of Herron, Lee J recites the primary judge’s ruling:
On the eighth day of the trial, when the issue was again ventilated, submissions were made on the issue and her Honour made the following ruling (which, although directed to the issue of the fraud allegation, both parties accepted also relates more broadly to the allegation as to a lack of particularisation of patients):
HER HONOUR: … In my view, there is sufficient particularisation of the allegation of fraud in the sense that it is a straightforward allegation that between two periods of time, Dr Herron, as he was, was charging patients for an anaesthetic treatment accompanying ECT when no anaesthetic was administered. What’s missing from the particulars is identification of the patients who were charged, and while it can be said, with the benefit of hindsight, that the pleading is inadequate in this respect, it was always clear from the correspondence from the respondents that the respondents did not consider that they had to provide the names of patients in this regard, and no application was made by the applicant to strike out the pleading.
Rather, the applicants … have waited until the hearing … to allege that documentary evidence in support of the particular cannot be relied upon because of the inadequacy of the particular. It seems to me that it was incumbent upon the applicants to move to either obtain an order for further particularisation or to strike out the particular on the basis of the inadequacy at a much earlier time.
(emphasis in original)
197 On appeal, it was necessary for the appellants to establish an error of the kind identified in House v King [1936] HCA 40; (1936) 55 CLR 499. Lee J accepted that any error of the primary judge cannot be identified by some failure to apply the strictures of the rules relating to pleadings and particulars. That was said to be “because her Honour’s ruling … is caveated with the acceptance that ‘it can be said, with the benefit of hindsight, that the pleading is inadequate’”: Herron at [418]. This ground of appeal was dismissed. Wigney J at [262] of Herron agreed with Lee J, and his Honour’s reasoning. Rares J did not consider it necessary to address the ground given his conclusion on other grounds.
198 Lee J found no error for three reasons. First, it was open to find that the publishers were not sitting on the evidence of Mr Green (a patient who had not been particularised in the publishers’ defence) and purposefully did not inform Mr Herron and Dr Gill (the appellants) that he may be the subject of questioning. Second, there was no reason to doubt that it was open for her Honour to conclude that in the circumstances no “real prejudice to the applicants arising from the admission” of the materials was established by Mr Herron and Dr Gill. Third, “and more importantly, the primary judge was right to point out that, given the parties remained in contest as to the adequacy of the pleadings, more was needed than, in effect, relying on objections being taken at trial as to the scope of the case”: Herron at [419].
199 As to the third point, his Honour observed at [420]:
This Court runs a docket system. One advantage of such a system is that the judge case managing the case will usually be the trial judge, and there is every opportunity of raising matters relevant to the conduct of the trial with the presiding judge promptly, and in advance of the final hearing. If a dispute arises as to the ambit of the case and there is an apparent asymmetry of understanding between the parties, the days have long passed where it is appropriate (if it ever was) to simply put a stake in the ground and say objection will be taken at trial. An issue as to the ambit of the case requires resolution and for symmetry to be restored, perhaps by requiring the provision of further particulars or an amendment to pleadings, or for such a resolution to be refused and it being made plain, in advance of trial, that foreshadowed evidence will not be admissible as it falls outside the permissible ambit of the case. The present dispute was identified and joined in advance of trial and, consistently with the dictates of Pt VB of the Federal Court of Australia Act 1976 (Cth), Mr Herron and Dr Gill should have pressed to bring these matters to a head before the docket judge and have them resolved. Modern case management imperatives mean it was insufficient for Mr Herron and Dr Gill to sit tight and simply assume that their characterisation of the pleading and the scope of the case, which was being put in contest, would find favour at the hearing.
200 Those observations are equally apt in this case.
201 The issue first arose during cross-examination of Ms Roberts, an early witness in the applicant’s case (and called before the applicant himself). Objection was taken to some questions on the basis that a matter had not been pleaded in the defence. I did not agree with many of the submissions that the relevant matter was not pleaded. The applicant also conflated pleadings with evidence, which does not need to be pleaded. There is a well-established distinction between particulars and evidence, a pleading contains the former, not the evidence to be relied on to prove the case: Palram Australia Pty Ltd v Rees [2013] FCA 649 at [31]. The evidence adduced at trial will inevitably be more detailed: Rush v Nationwide News Pty Ltd [2018] FCA 357 at [49].
202 In any event, the applicant was on notice of these matters complained of. In that context, I allowed the questions to be asked if it was relevant to the issues in the proceedings. That said, on occasions when the applicant submitted that he was taken by surprise by the questioning (although not accepted) and needed time to address the evidence, he was given that time and afforded an opportunity to consider his position in relation to the evidence. He was allowed time to address the evidence. This approach was apparent from very early in the applicant’s case. The conduct of his case thereafter is in that context.
203 The conduct of the case at the time the objection was raised, and thereafter, does not support the applicant’s contention that he is prejudiced by any of the evidence objected to. Rather, it bespeaks the opposite.
204 The applicant was aware of the evidence of the patient witnesses, and (with limited exception which only became apparent during the hearing) any medical evidence in support. The 33 patient case studies related to patients who were all, at one time, the applicant’s patients. The applicant has the records in relation to them. Indeed, the applicant had filed affidavit and documentary evidence in response, which detailed his dealings with the patients, in chronological order. The applicant also filed expert reports. In opening, the applicant addressed some of the patients, and was prepared to specifically allege, inter alia, that they were lying, giving false evidence or that the particulars pleaded in relation to them were incorrect or “lies”.
205 The applicant did not bring any pre-trial application in respect to the pleadings. That the applicant wished the matter to proceed to trial as expeditiously as possible (which he submitted was his reason for not bringing a pre-hearing motion), was a forensic decision made by him. As Jagot J observed on ruling the evidence admissible at first instance in Herron, “it was incumbent upon the applicants to move to either obtain an order for further particularisation or to strike out the particular on the basis of the inadequacy at a much earlier time”: Herron at [415]. As Lee J correctly observed in Herron, Jagot J was right to point out that, given the parties remained in contest as to the adequacy of the pleadings, more was needed than, in effect, relying on objections being taken at trial as to the scope of the case.
206 Further, this issue arises in circumstances where this matter, at the applicant’s request, was listed for hearing expeditiously. Any imperfections in pleadings (where I accepted during the hearing there were some) must be considered in that context. The context also includes that the applicant, in his affidavits, addressed the history of his interactions with the patient witnesses, not confined to those matters pleaded. It was said by the applicant that that was done as a matter of chronology. However, the applicant’s approach, evident from the filing of his evidence and reflected in cross-examination and closing submissions, was that it is necessary to consider each of the patients with a full chronology of what happened with each patient, starting from how they came to be in Dr Al Muderis’ care, and then what relevantly occurred thereafter. It was submitted that was the only approach the Court could properly adopt. On the applicant’s approach, he could give evidence of such matters, but any evidence from the relevant patient which addressed those matters could not be led unless it was in the pleadings (although the applicant was on notice about it as it was referred to in the affidavits filed by the respondents before the hearing). That approach is artificial, and not conducive to determining the issues justly.
207 It should also be observed that during the hearing the applicant accepted that, generally, an objection that evidence was not relevant was made only on the basis that it was not referred to in the pleadings. That is, it was accepted that such evidence was relevant to the issues for determination, with the only basis of objection being a failure to plead the allegations (or evidence).
208 The applicant submitted in closing that they held the respondents to their pleading. Such a submission misstates a party’s capacity to direct the course of the proceedings. The course of proceedings is in the control of the Court. That control is to be exercised for the attainment of a just outcome: Betfair Pty Limited v Racing New South Wales [2010] FCAFC 133; (2010) 189 FCR 356 at [55].
209 Despite the applicant continuing to contend in closing submissions that he has been prejudiced, no prejudice has been identified, and there is no evidence in support. The mere assertion in submissions is insufficient, particularly in circumstances where some of the applicant’s speculation proffered in submissions during the trial, was not carried through. I will refer to just one example of alleged prejudice which concerns the topic of why payment from overseas patients was required in advance of their arrival to Australia. Early in the hearing, the applicant objected to cross-examination on this topic on the basis this matter was not pleaded, and he was prejudiced because he could have led evidence from certain people to address this topic. I allowed the cross-examination, as the topic was relevant (as will be apparent from the discussion of the evidence below). Leaving aside the correctness of the underlying premise, the applicant chose not to lead any such evidence. The applicant was given an opportunity to address this topic during his own case, but did not do so. Rather, the only evidence he chose to lead on the topic was documents from a government website concerning the government requirements for obtaining a medical visa (which were led in reply). In his case in reply, the applicant submitted that an email tendered during the respondents’ case explained why the practice of prepayment was employed, being for a medical visa. Again, leaving aside the correctness of that assessment of the evidence, it was on that basis that the applicant tendered the government regulations in reply. That the applicant chose only to rely on that evidence was a forensic choice.
210 The applicant had ample opportunity to address the evidence led by the respondents. As a general proposition, I observe that one cannot choose, for forensic reasons, not to address evidence if an opportunity is given, simply to preserve a pleadings appeal point.
211 In this context it is also appropriate to record that during submissions which occurred on day 15 of the hearing (during the applicant’s evidence), the applicant advanced a case which went further than what was presented in opening (which included, amongst other things, a submission that patients and others were lying about the complaints), by alleging there was a concoction between various persons (some named by the applicant) to falsely disparage the applicant. It was alleged that the complaints were concocted, it appears, as a part of a plan or scheme. Although the patients were not named, it is plain from the submission that this was said to include patients. This case was not pleaded. When this was raised by the respondents, the applicant submitted it was unnecessary for him to plead this allegation. I do not agree. It is an allegation that these persons were acting dishonestly and were involved in fraudulent conduct. Such allegations should have been pleaded and should not have emerged on day 15. That said, the applicant was not prevented, based on a lack of pleading, from advancing his case in that regard. It has never been withdrawn, although the applicant did not advance a submission to that effect in closing submissions.
212 Finally, before leaving this topic, it appropriate to refer to my rulings in relation to the applicant’s case in reply, as that also was considered in the context of the orders made for the conduct of the hearing as described above. The respondents accepted that some topics had arisen during the hearing and as such were properly the subject of reply; but objected to some of the evidence, primarily on the basis it was an attempt by the applicant to adduce further evidence in chief many months after he had closed his case. That is, the applicant was on notice of these matters at the time of the respondents filing their evidence in chief, and there is no proper basis for him now seeking to rely on the evidence in reply. The applicant again relied on the failure of the respondents to plead matters. Again, my rulings and the bases thereof are evident from the transcript and unnecessary to repeat. I simply note three matters. First, when the topic of reply evidence was raised, the applicant identified possible witnesses because of “new evidence” of certain witnesses in the hearing. Those referred to relate to topics that arose during the hearing. The evidence the applicant ultimately sought to lead was broader. Generally, evidence can only be led in reply if it arises from matters that arose in the respondents’ case, and what arose was not reasonably foreseeable (although that rule is applied less strictly in civil cases). That is to be considered in the context of the case management orders made for the conduct of this hearing, as referred to above. In those circumstances, a party cannot hold back evidence to simply lead it in reply. Second, this was not a situation where in relation to expert evidence, the applicant was seeking to recall expert witnesses who had already given evidence as part of the applicant’s case in relation to a patient. I note that because in respect to one witness, Dr Qurashi, the expert report sought to be relied on in reply appeared to be based on a 2014 report he had prepared and addressed topics that were or could have been addressed by the expert witness called by the applicant for that patient. Reply is not simply an opportunity to lead further evidence from a different witness. That said, I did allow those witnesses to be called to give evidence on certain topics. Third, I did not generally permit evidence to be led in reply when the applicant was on notice of it. There was material that did arise after the close of the applicant’s case in respect to the case studies of Ms Mooney, Ms Heffernan, Mrs Gollan and Ms Ulrich. I permitted evidence to be called in reply which related to or was associated with that new material. In relation to Mrs Gollan, the circumstances were such that (including relating to the pleadings), I considered it appropriate the applicant be able to call evidence in reply (although the applicant was on notice of the evidence). The reply evidence is referred to when considering those patient case studies in Part 6.
Section 1 — Legal principles
Substantial truth
213 The respondents have pleaded the defence of justification or substantial truth under s 25 of the Defamation Act. Section 25 states that “[i]t is a defence to the publication of defamatory matter if the defendant proves that the defamatory imputations carried by the matter of which the plaintiff complains are substantially true”. Section 4 of the Defamation Act defines “substantially true” as “true in substance or not materially different from the truth”.
214 The respondents must establish that every material part of an imputation is true, with the defence of substantial truth being concerned with meeting the sting of the defamation: Channel Seven Sydney Pty Ltd v Mahommed [2010] NSWCA 335; (2010) 278 ALR 232 at [138]. A “material part” is any detail which alters or aggravates the character of the imputations: Rofe v Smith’s Newspapers Ltd (1924) 25 SR (NSW) 4 at 22.
215 Although this is a contextual truth case, the approach to assessing whether it has been established that an imputation is substantially true, applies.
216 To determine whether an allegation has been established to be substantially true, the allegation is considered in a non-technical, non-legal sense; in the way it would be understood by the ordinary reasonable viewer or reader. As discussed above, the ordinary reasonable viewer or reader is not a lawyer and is not taken to have detailed knowledge of the law: Farquhar v Bottom [1980] 2 NSWLR 380 at 386; Trkulja at [32]. Therefore, where the natural and ordinary meaning of a publication is relied on, the meanings will fall to be considered by reference to the ordinary meaning of terms, not their legal meanings, because it is the way the terms would be understood by ordinary reasonable people, not lawyers, that is important: see e.g. Haddon at [34]; Lehrmann at [568].
217 In Sutherland v Stopes [1925] AC 47 at 78-79, Lord Shaw of Dunfermline explained:
It remains to be considered what are the conditions and breadth of a plea of justification on the ground of truth. The plea must not be considered in a meticulous sense. It is that the words employed were true in substance and in fact. I view with great satisfaction the charge of the Lord Chief Justice when he made this point perfectly clear to the jury, that all that was required to affirm that plea was that the jury should be satisfied that the sting of the libel or, if there were more than one, the stings of the libel should be made out. To which I may add that there may be mistakes here and there in what has been said which would make no substantial difference to the quality of the alleged libel or in the justification pleaded for it.
218 The focus is on the sting of the libel.
219 Where an applicant pleads that the respondent published an imputation alleging a general charge is conveyed, the respondent is entitled to give particulars demonstrating why that was true by reference to a wide variety of matters which are not confined to the facts in the article: Maisel v Financial Times Limited (1915) 112 LT 953 at 955; 84 LJKB 2145 at 2147; and see e.g. Ange v Fairfax Media Publications Pty Ltd & Ors [2010] NSWSC 645 at [38]-[41]; Habib v Nationwide News Pty Ltd [2010] NSWCA 34; (2010) 76 NSWLR 299 at [314]. This is orthodox and unexceptional. The respondents seek to justify many of the imputations by reference to facts beyond those included in the Publications. I accept that a number of the applicant’s pleaded imputations involve general charges that are capable of being justified by reference to facts not stated in the Publications: e.g. Imputations [10.1] (“negligently operated on his patients”), [10.2] (“deliberately misled his patients about his surgical abilities”), [13.1] (“falsely portrays himself as a devoted doctor”), [13.4] (“prioritises money over his patients’ care”), [13.14] (“runs his surgical practice as a numbers game”), [13.18] (“exploited vulnerable patients”), [16.1] (“is a callous surgeon who routinely left patients to rot”), [16.2] (“routinely negligently failed to provide after surgery care”), [16.5] (“uses improper sales tactics”), [16.10] (“glittering reputation and praise for his work as a surgeon is undeserved”), [16.25] (“negligent in his selection of patients”) and [16.26] (“habitually failed to explain risks and complications”).
Contextual truth
220 Section 26(1) of the Defamation Act prescribes a defence to the publication of defamatory matter if the respondent establishes that:
(1) the matter carried one or more imputations that are substantially true (contextual imputations); and
(2) any defamatory imputations of which the applicant complains that are not contextual imputations and are also carried by the matter do not further harm the reputation of the applicant because of the substantial truth of the contextual imputations.
221 The contextual imputations on which the respondent may rely to establish the defence include imputations of which the applicant complains: s 26(2) of the Defamation Act.
222 A defence of contextual truth “must defeat the whole defamatory matter (cause of action) of which the plaintiff complains, that is to say all of the plaintiff’s stings”: Besser v Kermode [2011] NSWCA 174; (2011) 81 NSWLR 157 at [78].
223 Prior to 1 July 2021, s 26 was in different terms. In particular, the amendment introduced s 26(2). That provision is significant in this case, as it is no longer necessary that a respondent’s contextual imputations be different in substance from an applicant’s pleaded imputations. As plain from the text of the provision, a respondent may now rely on any imputations carried by a publication, whether the same as, permissible variants of, carrying a common sting with, or entirely different in substance from, the imputations of which the applicant complains, as contextual imputations.
224 As mentioned, the respondents submitted that this case is really one of contextual truth. The respondents’ position was clearly articulated in their written submissions as follows. They rely on all the imputations to which they have pleaded a justification defence, including the Disputed Imputations, as contextual imputations. The respondents contended that ordinary reasonable readers and viewers of the Publications will not have understood them to convey imputations that Dr Al Muderis was negligent in his performance of surgery “in the operating theatre” but will rather have understood the references to “surgery” and like terms as extending to all aspects of Dr Al Muderis’ surgical practice. I resolved that dispute above. The respondents submitted the Publications conveyed the Disputed Imputations in the sense for which the respondents contended: that is, imputations to the effect that Dr Al Muderis was negligent in those aspects of his surgical practice relating to pre-operative considerations and consultations and post-operative care, including patient selection, disclosure of risks, misleading patients, making false promises, abandoning patients and negligent post-surgery care. They submitted that so long as they were conveyed, the respondents are permitted to rely on them as contextual imputations for the purposes of s 26. It was submitted that the Disputed Imputations in this broader sense, together with the other imputations which are the subject of the contextual truth defence of the Amended Defence, are substantially true and that, taken together, the substantial truth of the contextual imputations swamps the defamatory effect of any residual imputations which the Court may find have not been proven to be true, such that any imputations which are not true do not further harm Dr Al Muderis’ reputation.
225 There is one aspect of this defence, being the approach to the assessment of further harm, which is the subject of dispute between the parties.
226 That is, the approach to assessing whether the defamatory imputation carried by the matter does not further harm the reputation of the applicant because of the substantial truth of the contextual imputations. The respondents submitted that the Court weighs the particulars, and the evidence relied upon in support of the substantial truth of the contextual imputations, and considers whether, in light of that evidence, the applicant’s reputation was not further harmed by the residual imputations of which the applicant complains, citing, inter alia, John Fairfax Publications Pty Ltd v Blake [2001] NSWCA 434; (2001) 53 NSWLR 541 (Blake) at [61] and Roberts-Smith at [2602].
227 On the other hand, the applicant submitted that the further harm requirement of s 26 should be understood as involving an assessment of whether the plaintiff’s imputations (taken together) harm the plaintiff’s reputation in light of the defamatory impact (truth of) the defendant’s contextual imputations. This was said to be because of an alleged difference in the language used in s 26 of the current Defamation Act and its predecessor, being s 16 of the Defamation Act 1974 (NSW), such that the task instead is to engage in a weighing of imputations, rather than a weighing of the evidence supporting the substantial truth of the imputations. He submitted that subsequent authority, which stems from the reasoning in Blake, does not apply, does not specifically address the distinction, or is plainly wrong.
228 The Full Court in Seven Network (Operations) Limited v Greiss [2024] FCAFC 162 (Greiss), has since addressed this issue. One of the issues before the Court was whether the primary judge erred by relying upon decisions concerning the Defamation Act 1974 (NSW) and applying them to the application of s 26 of the Defamation Act. There it was submitted that the primary judge erred in holding that the Court’s focus in determining the question of further harm must be on the facts, matters and circumstances establishing the substantial truth of the contextual imputation, rather than the terms of the contextual imputation. The Full Court (Lee J, with whom Cheeseman and Jackman JJ agreed), held that no error in that regard was established, and concluded that the primary judge was correct to reason as she did, which was consistent with Blake: see Greiss at [59]. The Court also noted the application of the principle in this Court: see Nassif at [125] and Palmer v McGowan (No 5) [2022] FCA 893 at [321].
229 In Blake, Spigelman CJ (with whom Rolfe AJA agreed), in relation to s 16 of the Defamation Act 1974 (NSW), observed at [5]:
Section 16(2)(c) does not focus attention on a contextual imputation as such but on the proposition that such an imputation is a “matter of substantial truth”. It is “by reason” of such “substantial truth” that a defence to an imputation pleaded by a plaintiff can be made out on the basis that the plaintiff's imputation does not “further injure the reputation of the plaintiff”. For purposes of determining whether the s 16 defence is capable of being made out, the Court must focus on the facts, matters and circumstances said to establish the truth of the contextual imputation, rather than on the terms of the contextual imputation itself.
(emphasis in original)
230 In Greiss, Lee J also pointed out at [60] that importantly, the primary judge also referred to Nationwide News Pty Ltd v Weatherup [2017] QCA 70; [2018] 1 Qd R 19, where at [46] Applegarth J (Fraser JA and Douglas J agreeing) noted (emphasis added in Greiss):
The requirement to prove no further harm to the plaintiff’s reputation focuses on the facts, matters and circumstances which establish the substantial truth of the contextual imputations. This reflects the language of the section. The alternative approach of weighing the imputations about which the plaintiff complains, and the contextual imputations which are proven to be substantially true, may be a convenient shorthand or lead to no different outcome in practice.
231 In Greiss, Lee J concluded at [64]:
… there is no demonstrated “compelling reason” for this intermediate appellate court to depart from the decisions of other intermediate appellate courts on the operation of this statutory defence contained in uniform legislation.
232 Although in Greiss the former iteration of s 26 was considered, s 26(b) (the further harm requirement) is relevantly in the same terms. The mischief to which the amendments to s 26 were directed was only concerning the unintended uncertainty about whether a defendant can plead back a plaintiff’s imputations. It is that uncertainty that was rectified (which is permitted under the current version of s 26). There is nothing in the text of the new provision which would result in a conclusion that Greiss does not apply to the current provision. Indeed, as explained above, the premise of the submission was based on Blake being inapplicable or incorrect. The applicant did not draw any relevant distinction in this argument between the terms of s 26 as applied in Greiss, and its current form. I consider myself bound by Greiss. That said, in my view, the reasoning in Blake and later authorities is consistent with the text of s 26.
233 Therefore, in undertaking the assessment of whether the defamatory imputations do not further harm to the reputation of an applicant, the Court considers the facts, matters and circumstances relied upon to support the substantial truth of the contextual imputations rather than the terms of the imputations itself.
Section 2 — Defamatory stings
234 The applicant pleaded that the Publications carried 75 defamatory imputations. The respondents did not plead a truth defence with respect to four of those imputations (being Imputations [13.24], [16.9], [16.28] and [28.6]). They pleaded that the remaining 71 imputations were substantially true within the meaning of s 25 of the Defamation Act. The imputations are generally pitched by the applicant at the most serious level. That is a forensic choice he made but has the consequence that if it is not established, the imputation is not carried. That is what occurred in relation to the Sneak Peek, with six imputations being pleaded (from 24 lines of transcript) each alleging imputations confined to surgery (in the operating theatre). As stated above, I have not found those imputations to be carried.
235 The respondents submitted that the “scattergun pleading” of imputations is a “distraction”. Regardless, the volume of imputations (and their overlapping and repetitive nature) necessarily makes the resolution of the issues in these proceedings more time-consuming.
236 In that context, the respondents submitted that the Court is free to determine the meaning or meanings the Publications would be understood to convey to ordinary readers and viewers, applying the authorities in relation to the determination of meaning, subject to the caveat that an applicant cannot succeed on an imputation which is substantially different from or more serious than a pleaded imputation, citing inter alia, Wing at [22]. The respondents submitted that at a high level, the Publications would have been understood by ordinary viewers and readers to carry ten distinct defamatory stings covering conduct in relation to various aspects of Dr Al Muderis’ practice. In closing submissions, the respondents addressed what they contended is the evidence establishing the truth of those stings. In doing so, the respondents identified the imputations which they said fell within each sting, and the evidence relied on (in submissions and one of the aide memoires provided, being Aide Memoire 4). The respondents also identified which patients’ evidence is relevant to the proof of each of the imputations which is alleged to be substantially true (in Aide Memorie 6).
237 The applicant submitted that approach is in error because it is necessary to address each of the pleaded imputations and that can only be done by looking at each patient’s interaction with Dr Al Muderis and medical issues chronologically (as opposed to considering the patients per sting). As to the first aspect, contrary to the applicant’s submission, I do not take the respondents to be suggesting that the imputations as pleaded not be considered. As to the second aspect, although all the evidence must be considered, some of the imputations relate to discrete matters which are not necessarily impacted by the whole chronology of events relating to a patient. Similarly, to address the issues in this hearing, it is unnecessary to address the entire chronology for each patient in these reasons. The extent of my discussion in relation to each patient is necessarily impacted by the relevant matters (and issues) to be resolved. Moreover, the approach adopted by the applicant in his submission considers each patient in isolation. The applicant’s submission is that each individual case must be analysed on its own merits. As explained elsewhere, that fails to recognise that considering an individual case does not mean considering the evidence in isolation. There is no proper basis to do so, where the evidence of others (or other documents) may be relevant. Again, whether that is so depends on the issue being resolved. As apparent from my consideration of the evidence, I do address the patients, but only in respect to relevant issues. That has been considered in the context of all relevant evidence and submissions. They are not considered in isolation.
238 Nonetheless, considering the evidence in the context of the stings as they arise from the Publications (given the number and nature of the imputations), is appropriate. That said, as foreshadowed earlier, the respondents submitted that each of the pleaded imputations fits within one or more of ten stings. They identified them as follows:
(1) misleading patients / false promises / failing to disclose risks;
(2) poor patient selection;
(3) improper sales tactics;
(4) negligence in the operating theatre (but only if the applicant’s construction of the Disputed Imputations is accepted);
(5) performing procedures illegally in the United States;
(6) negligence in post-operative care;
(7) abandoning patients;
(8) prioritising money / fame / reputation / numbers;
(9) poor treatment of staff; and
(10) lying to 60 Minutes.
As can be seen, one of those stings (being, sting (4), negligence in the operating theatre) was only said to arise if I was against them in relation to the meaning of the Disputed Imputations, discussed above in Part 2, Section 3. Given my conclusion in relation to the Disputed Imputations above, the fourth sting is not carried. The respondents appeared to have derived the ten stings from some aggregation of the Publications. The proceedings concern seven discrete matters (i.e. the Publications), and any defamatory meaning is to be inferred with respect to each matter, not some aggregation thereof. As explained above, the respondents did identify which imputations, they said, are encompassed in each sting.
239 Each publication, assessed individually, would nonetheless have been understood by ordinary viewers or readers to carry fewer distinct defamatory imputations than the applicant suggested in his pleadings. According to the respondents’ categorisation, the Publications share certain stings which are, as a matter of practicality, the same; that is, certain stings are carried in more than one Publication. Generally, I agree with the respondents’ formulation of the stings. However, in my view there is no real distinction between the respondents’ stings (6) and (7) (noting also that they were addressed under the same rubric). Some imputations also carry more than one of the stings. It is also worth noting that three imputations (being Imputations [16.10], [28.8] and [28.9]) do not appear to be addressed by a sting number. In submissions they were grouped to encompass unethical conduct which is more properly categorised as a separate sting. Compiling the stings from the Publications, there are nine main stings. Although this reformulation may be in a different order, and use slightly different language, in general terms they accord with the respondents’ stings and convey Dr Al Muderis:
(1) using improper sales tactics which pressures patients into having osseointegration surgery with him;
(2) misleading osseointegration patients (e.g. false promises, downplaying the risks and complications of osseointegration surgery to patients);
(3) engaging in poor patient selection for osseointegration surgery (including that assessments are inadequate);
(4) providing negligent post-operative care;
(5) performing surgery illegally in the United States;
(6) prioritising money, fame, reputation and numbers over his patients;
(7) mistreating his staff;
(8) lied to the journalists investigating his practice; and
(9) engaging in conduct that is unethical.
240 The reference to “negligent” and “unethical” in those stings each bear the meaning as described above: see Part 2, Section 4.
241 I return to these stings below. It is necessary at this stage to consider the evidence relevant to this defence.
Section 3 — Temporal limitation
242 In his written closing submissions, the applicant contended that where reliance is placed on events long before publication and there has been a substantial change of circumstances since that time, the evidence may have little probative force, referring to State of New South Wales v Wraydeh [2019] NSWCA 192 (Wraydeh) at [39]. The applicant submitted that in this case, for example, evidence of Dr Al Muderis’ surgical skill at or near the start of his surgical career proves little or nothing about his surgical skills during his surgical career years later. He submitted that evidence about practices five years or more before publication are not proof of current practices for the purposes of proving a present state of affairs (giving as examples, Imputations [13.1], [13.4], [13.13], [13.14], [13.16], [13.26], [13.30], [16.1], [16.4], [16.5], [16.10], [28.1], [28.5], [28.6], [28.7], [28.8] and [28.9], being imputations framed in the present tense). He submitted that there are no particulars in the Amended Defence of current practice to prove the substantial truth of any of these imputations.
243 The respondents correctly submitted this submission as to a temporal limitation to some of the applicant’s pleaded imputations (in particular, Imputations [13.26] and [16.1]) was raised for the first time in closing submissions. They submitted that none of the Publications purported to be directed only to a time that was temporally proximate to the date of publication and none of the pleaded imputations are so limited in their terms. They submitted that evidence that Dr Al Muderis was negligent in relation to a significant cohort of his patients is relevant to justify the pleaded imputations irrespective of when the negligence occurred. They also submitted that if Dr Al Muderis’ case was that his imputations were temporally limited, then he ought to have amended his SOC to make this clear or applied to strike out the Amended Defence as being unresponsive to the pleaded imputations. He did neither. The respondents contended it is not now open to the applicant to seek to restrict his case in this way at the end of a 65-day trial. I agree that it would be expected that if the imputations were temporally limited in the way the applicant contended, it would have been raised before closing submissions. There was no objection during the hearing to any of the evidence led based on a temporal limitation.
244 It is appropriate to briefly consider Wraydeh. This was an appeal from an interlocutory decision of the primary judge which allowed Mr Wraydeh, as the driver involved in a fatal car crash and who was referred to as a “criminal” in a press statement, to amend his statement of claim to adopt two contextual truth imputations. The State, in its defence, had pleaded contextual truth relying on two imputations, including an imputation of the general attribute “that the plaintiff is a criminal” which it sought to prove by evidence that Mr Wraydeh had prior criminal convictions unrelated to the events of the fatal crash. Mr Wraydeh thereafter sought leave to amend his pleading to adopt the two contextual imputations. At that time, the effect of such an amendment was that the imputation in question could no longer be a “contextual imputation” within the meaning of s 26 of the Defamation Act, even if proved to be substantially true (citing Fairfax Digital Australia & New Zealand Pty Ltd v Kazal [2018] NSWCA 77; (2018) 97 NSWLR 547).
245 One of the allegations on appeal was that the application to amend the pleading was an abuse of process. Part of that ground of appeal included an assertion that the primary judge erred in finding that the evidence of prior convictions was insufficient to constitute proof of an imputation that “the plaintiff is a criminal”. In addressing that ground, McCallum JA observed that the question raised was whether the “criminal” imputation must be known by the plaintiff to be true, in which case it ought to have been concluded the application to amend was an abuse of process in seeking vindication of reputation in respect of an imputation the truth of which cannot properly be controverted: at [34]. Her Honour observed that the submissions implicitly contended that, because the plaintiff had prior convictions, the imputation he is a criminal must be true to his knowledge. However, as held by the primary judge, that is contestable. It is in that context that the passage relied on by the applicant in those proceedings at [39] arose. Her Honour there observed (with whom Emmett AJA agreed):
That is not the position in the present case [that the imputation the truth of which is incontrovertible]. The question whether a person is to be characterised in the present tense as “a criminal” is not answered determinatively by establishing that he or she has committed a criminal offence in the past. In the first instance, as noted by the primary judge, that ignores the possibility of change and rehabilitation. Further, not every prior conviction would be regarded as necessarily warranting that label.
246 The applicant also relied on Simpson AJA at [58]:
Underlying the series of propositions is the unstated premise that a person who has a criminal record is, therefore, necessarily to be categorised as “a criminal”. The State relied (simplistically) on a dictionary definition of “criminal” as “a person guilty of or convicted of crime” (Macquarie Dictionary, 2nd ed). The premise, as McCallum JA says, is contestable. Whether a criminal history necessarily constitutes its owner a criminal will, in some cases, involve questions of fact and degree. Is a person convicted of shoplifting at age 18 forever to be branded “a criminal”? Is a person convicted of motor traffic offences (which are criminal in nature) to be branded “a criminal”? These questions do not arise in the present case. But they illustrate that the State’s propositions would involve this Court embarking on questions the determination of which properly lies within the province of a jury. It would only be in a very unusual case that the Court would, at an interlocutory stage, embark on the determination of the truth of a pleaded imputation. Yet that is what the State invited the primary judge, and this Court, to do.
247 As can be seen, the applicant’s submission puts a gloss on the observations relied on. The passages reflect that whether the evidence relied on in proving substantial truth establishes a proposition depends on the circumstances of the case. It does not create some principle that the evidence is of light weight, but rather the weight will necessarily depend on the evidence.
248 Moreover, the applicant’s submission is also based on a substantial change of circumstances and uses his surgical skill as an example. Acknowledging that the respondents have the onus to establish the defences, nonetheless, the applicant did not give evidence that what had occurred earlier had anything to do with his surgical skills – his evidence is he has done nothing wrong in respect to any of the patient witnesses. Further, as previously discussed, the stings from the Publications relate to surgery in the broad sense, not confined to the operating theatre. There is no evidence to suggest that the evidence of impugned practices has changed, but rather it was that the events as described did not occur (or are not to be interpreted in that manner).
249 Wraydeh does not support the applicant’s submission that practices five years or more before the Publications are not proof of current practices. The term of five years appears to be arbitrary. I note that elsewhere in his submissions the applicant submitted that a patient witness needed to be a “recent patient”, which he defined as persons who became a patient within two years of the Publications. Again, an arbitrary temporal limitation. The flaws of that approach are addressed at [261].
250 There is no proper basis to impose any temporal limitation on the evidence. Rather, whether the substantial truth of any imputation has been established will be assessed by considering the evidence relevant to that imputation.
Section 4 — Generalisation
251 The applicant submitted that the negative experiences of the patient witnesses are not generalisable in this case, in that general inferences about Dr Al Muderis’ practice cannot properly be drawn from the experiences of the individual patient witnesses selected by the respondents. He submitted the respondents needed to demonstrate that the methodology they employed to find these witnesses resulted in representative or random selection, referring to Unique International College Pty Ltd v Australian Competition and Consumer Commission [2018] FCAFC 155; (2018) 266 FCR 631 (Unique). In that case, the Full Court allowed an appeal against the judgment of the primary judge because, inter alia, his Honour had inferred a “system of conduct or pattern of behaviour” under s 21(4) of the Australian Consumer Law (ACL) in connection with the supply of online vocational education courses to consumers, based on the evidence of conduct in relation to four sites out of 428 and about six students out of 3,600, in the absence of any evidence as to how those sites or students were selected or whether they were representative or random: Unique at [162] and [208]. The applicant also referred to: Capic v Ford Motor Company of Australia Pty Ltd [2021] FCA 715 (Capic) (a representative action for damages on the basis that Ford engaged in misleading and deceptive conduct under ss 18 and 33 of the ACL, and that vehicles were not of acceptable quality when supplied to consumers, under s 54 of the ACL); and Morsman (by his next friend Bampton) v State of Victoria (Department of Education and Training) [2020] FCA 763 (Morsman) (which involved violations of the Disability Discrimination Act 1992 (Cth), where the Court at [48] cited Unique to demonstrate “the difficulty of asserting from a series of unique instances that a system exists”).
252 From that, the applicant submitted that the respondents’ attempts to generalise the experience of the unhappy patient witnesses in this case cannot be accepted as there is no evidence that these patients are representative of or randomly selected from the thousands of patients that Dr Al Muderis has treated over the years. He submitted that the evidence establishes:
many of the respondents’ patient witnesses were patients that Mr Hernandez chose to refer to Ms Grieve, or patients who reported negative experiences to the respondents after the respondents grossly defamed Dr Al Muderis in their publications.
253 It was submitted that the respondents cannot logically use the anecdotal experiences of their patient witnesses to support proof of the general imputations. Proof of the general imputations required a far more rigorous methodology than was employed by the respondents in this case. The applicant also contended the patients had interacted with Ms Grieve and Ms Stewart before providing their affidavits or had approached the respondents after the Publications were published, and therefore were not representative of Dr Al Muderis’ patients. He also submitted that none of the respondents’ witnesses were “recent patients” and so none of them gave evidence to the current experience of prospective patients.
254 In addition, the applicant submitted that the respondents’ justification and contextual truth defences necessarily require them to prove a pattern of behaviour, referring to Imputations [13.1], [13.4], [13.13], [13.14], [13.19], [13.26], [16.26], [28.1], [28.8] and [28.9], which involve generalisations about Dr Al Muderis’ habitual practice. Although, as I note below, there is a dispute as to whether these imputations fall within the category of generalisations, the respondents admitted that each of those imputations are carried and purported to justify them. The applicant also pointed to certain words and phrases used in the Publications which he said supported the proposition that the matters allege a system or pattern by Dr Al Muderis. The applicant further submitted the substantial truth of Imputation [16.26], that he “is a negligent surgeon in that he has habitually failed to explain risks and complications to patients before performing osseointegration surgery”, cannot be established:
by the personal experiences of the relatively tiny and non-representative cohort selectively called as witnesses by the respondents, even if it were true that the experience of those witnesses was that risks and complications were not explained to them.
255 The applicant submitted that the matters were only newsworthy because they alleged a pattern or system of behaviour in Dr Al Muderis’ practice. He submitted that the proposition that a surgeon, even a high profile one, had some patients with complications or failed to provide sufficient aftercare in individual instances would hardly warrant a “special edition of 60 Minutes” or a “special investigation” on the front page of two major national newspapers. The public interest in the story is dependent on the allegations representing fundamental and systemic issues in his practice.
256 The respondents contended that this is not a case where the respondents rely on the experiences of a small sample of patients and invite the Court to draw inferences or make findings about Dr Al Muderis’ standard practices with his patients taken as a whole. They do not seek or need to establish a “pattern” or “system” of conduct based on extrapolation from a sample set. Rather, the respondents rely on evidence relating to a significant cohort of patients and assert that the similar experiences of that cohort are sufficient to justify imputations that Dr Al Muderis negligently operated on patients (Imputation [10.1]), deliberately misled his patients about his surgical abilities ([10.2]), does not take adequate care of his patients ([13.1]), behaved inexcusably towards his patients ([13.21]), misleads patients by downplaying risks ([13.30]), routinely failed to provide after surgery care ([16.2]) and negligently performs surgery on unsuitable patients ([16.4]). The respondents submitted that to justify imputations of this kind, they do not need to prove that Dr Al Muderis engages in the relevant conduct in relation to all his patients, or the majority, nor that he does so invariably. They contended that it is sufficient for the respondents to establish that he has done so in relation to a significant cohort of patients or that the conduct has occurred with sufficient frequency as to be more than just a coincidence or anomaly. They submitted the statements in Unique and Capic are not relevant.
257 This argument is directed only towards the generalised imputations, and there appears from the submissions to be a dispute about which fall within this category.
258 That said, as a general proposition, this case as presented does not have the character of the allegations in Unique, where the Court considered a claim of unconscionable conduct under s 21(4) of the ACL, which was based on allegations of a “system of conduct or pattern of behaviour” as those terms are used in s 21(4) of the ACL. Capic and Morsman are similar, in that the nature of the allegations required proof of a system. That is, what was necessary in those cases was proof of a system, pattern or representative conduct, which generally would not be satisfied by reference to individual examples. The Publications properly considered, do not bear that feature. In this case, the Publications do not allege that there is a system or practice by Dr Al Muderis, but that for a cohort of patients, he similarly did or failed to do things (e.g. failed to explain risks or complications, failed to provide post-operative care). That is, the picture portrayed by Dr Al Muderis about his services, is not the only one. In other words, there was another side to the story.
259 The passages of the Publications relied on by the applicant said to demonstrate his position, must be viewed in their proper context. This includes that it is readily apparent from the Publications the number of sources spoken to, and that would have been evident to the reader or viewer. For example, it is plain from the Broadcast that many patients have had positive experiences with Dr Al Muderis, and that some people regard him as “their God in a sense”. The Broadcast refers to another cohort of patients who feel like they have been abandoned so to show people have had polarising experiences. That does not bespeak of and would not have been understood by the viewer as referring to a system of conduct, in the manner considered in Unique. The example given by the applicant in the SMH Article is the reference to “concerns about the surgeon’s approach to patient selection and aftercare”, which is used to suggest – by relying on the word “approach” – that there were general problems with Dr Al Muderis’ practice. However, this is in the context of that article proximately referring to patients describing experiences “ranging from life-changing to life-destroying”. That is not referring to a system in the Unique sense, but that there is a cohort of patients negatively impacted by Dr Al Muderis’ services, and these patients are not, as the respondents described, outliers, or anomalies. An event can be frequent without it being systemic. I accept the respondents’ submission.
260 Given that, the applicant’s submissions directed to what he says are the flaws in choosing these patients, as noted above, do not have the significance on this issue as he contended.
261 That said, it is helpful to address one of those issues, being the applicant’s submission that the respondents did not call any “recent patients”, as it contains factual flaws. As noted earlier, the applicant defined such individuals as those who became a patient in the year or two preceding the Publications, which it is to be recalled were published in September 2022. It is difficult to understand why that approach is limited to patients seeing Dr Al Muderis for the first time within that time frame, when his imputations include the adequacy of Dr Al Muderis’ aftercare which, as he accepted for some earlier patients, he was still providing during that time. The submission fails to grapple with the import of the Publications. It is artificial and based on the premise of the case being a representative one, which as explained above, it is not. In any event, there is no suggestion in the evidence that there had been any relevant change to his practice, but rather the applicant’s case was these events did not occur, or there was no basis for complaint. The experiences of these patients are, if accepted, no less significant simply because they did not occur in that last one to two years before the Publications. Moreover, contrary to his submission, there were two case studies in relation to patients who first saw Dr Al Muderis in the two years before the Publications: Mr Ford (who is deceased); and Patient X (who was to be a witness for the applicant but was ultimately not called): see Part 6, Section 3 below. Further, there was evidence from Dr Al Muderis’ websites, obtained during the respondents’ investigation, including information sheets and brochures, which were material accessible by prospective patients as at the time of the Publications.
262 Suffice to say, I do not accept the applicant’s submission regarding what he described as “recent patients”.
Section 5 — The applicant’s witnesses
263 Although I refer to the applicant’s witnesses first, it is important to recall the respondents bear the onus of establishing this defence. In referring to the applicant’s witnesses, at this stage, I am addressing issues as to their assessment as witnesses. Although the content of their evidence is referred to later in these reasons, including in considering the patient case studies, I have taken it into account in assessing the witnesses.
264 In this section I only refer to the principal witnesses called by the applicant, with others being addressed when considering the issues to which their evidence is directed.
Dr Al Muderis
265 Three affidavits of Dr Al Muderis were read (subject to objections) and two expert reports tendered.
266 In summary, the respondents submitted that Dr Al Muderis was an extremely unsatisfactory witness. They submitted that he was evasive, inconsistent and in some instances untruthful. He gave answers in the fashion he thought would most assist his case. The respondents submitted that at times, Dr Al Muderis was an all-purpose medical expert able to opine on any subject that assisted him, and at other times, resisted answering questions on the basis that it was outside his expertise. He claimed to have no memory of certain events, and a very clear recollection of others, in circumstances where neither could be believed. It was submitted that Dr Al Muderis did not make appropriate concessions in his evidence, was incapable of admitting error, was combative, invented evidence, and changed his evidence to suit his case. It was submitted that Dr Al Muderis’ documentary evidence was unreliable, and extraordinary propositions were put to witnesses (it can be inferred on his instructions). The respondents provided detailed submissions said to illustrate each proposition. As a result, the respondents submitted that generally, the Court should find that: (a) where Dr Al Muderis’ evidence was at odds with contemporaneous records (subject to (c) below), the records should be preferred; (b) where Dr Al Muderis’ evidence was at odds with the credible recollection of a patient as to an interaction (or he had no recollection), the patient’s evidence should be accepted; and (c) Dr Al Muderis’ documentary records should be treated with a high degree of caution unless uncontroversial or corroborated.
267 In closing submissions in chief, Dr Al Muderis submitted he should be accepted as an honest witness, who was doing his best to answer the questions posed to him. The applicant also submitted that his memory of the complications and complaints patients had was impressive, even though he could not recall the dates that each such incident occurred. The applicant submitted in reply that it is not uncommon for very intelligent people and lawyers to make somewhat unsatisfactory witnesses, for example, because they tend to overthink questions, seek to anticipate the direction of the cross-examination, or advocate for themselves instead of simply taking the questions as they come. It was submitted that it is easy to describe this kind of conduct by a witness as unresponsiveness, but it does not necessarily follow that the witness is unreliable, let alone that the witness is not credible or is dishonest. Pausing there, even accepting that is so, that does not explain or account for the issues that arose in the applicant’s evidence.
268 The applicant submitted that he endured an uncommonly difficult cross-examination, because of its length and the complexity of its subject matter, in circumstances where he was required to explain the medical treatment of dozens of different patients out of thousands he has treated during his career and English is not his first language. I am conscious of, and have considered, the circumstances in which each of the witnesses were cross-examined. As the applicant conceded, Dr Al Muderis speaks English fluently. There was nothing about his evidence, nor any submissions made, which suggest any lack of understanding. That said, I accept that caution should be exercised before proceeding from any impression that he was not a good witness to a finding that he was also an unreliable or dishonest one.
269 I accept that Dr Al Muderis’ evidence generally bore the features described by the respondents. I have considered the various explanations proffered by the applicant, the length and circumstances of the cross-examination, and the criticisms he makes of the respondents’ manner of cross-examination.
270 In assessing Dr Al Muderis as a witness, I considered the applicant’s submissions. I am unable to accept the submission he was an honest witness, as he was not always honest in the answers he gave.
271 Dr Al Muderis was cross-examined for nearly ten days. A good deal of his evidence involved issues of fact. I gained the very strong impression that he answered questions based on what he considered would assist his case. This resulted in his evidence, at times, being inconsistent. I agree with the respondents that such inconsistencies included making up evidence to provide what he considered was a suitable answer. He was argumentative at times. He gave the very strong impression that he considered his answers and opinions were unchallengeable. Frequently, he did not accept the plain meaning of words in a text or email if they were, on their face, critical of him. Conversely, he embraced such matters when he saw it as favourable to him and wanted to rely on them. The same could be said of his recall of events. On many occasions in cross-examination when Dr Al Muderis was asked about what he had done in response to various acts or events, although claiming no recall, he proffered without any evidence in support, that he may have done something, for example had a phone call (even where it did not sit with the surrounding documentary evidence, e.g. messages). He frequently avoided or did not answer the question and rather volunteered answers which were not responsive but justified his position. He did not make appropriate concessions. These features are evident from the discussion of his evidence in the patient case studies below.
272 Dr Al Muderis also gave speeches justifying the importance of what he did and stressing the importance of his experience (including, by contrast with others), in what appeared to be an attempt to bolster his evidence. To give but one example: in the middle of an answer to a question on infection in cross-examination, Dr Al Muderis volunteered that his opinion is as “the person that has done the largest number of osseointegration surgeries in the world”. This was a statement made to suggest his opinion carried more weight and should be accepted above others. He sometimes made similar broad assertions to counter any criticism of himself.
273 As referred to above, two expert reports by Dr Al Muderis were tendered. The respondents submitted that although they did not press for the exclusion of Dr Al Muderis’ expert reports, the Court should find that, in relation to any issue of controversy, save where it is against his interests, the reports are to be approached with “sceptical caution”.
274 In each report he ascribed to the Harmonised Expert Witness Code of Conduct (Expert Code of Conduct), which includes that:
An expert witness is not an advocate for a party and has a paramount duty, overriding any duty to the party to the proceedings or other person retaining the expert witness, to assist the Court impartially on matters relevant to the area of expertise of the witness.
275 It is difficult to understand how an applicant to any proceedings could ascribe to being impartial in giving evidence. An applicant gives evidence to advance the case brought by them, with a self-evident interest in its outcome. Here, Dr Al Muderis is not, and could not be, an impartial independent expert. As the respondents submitted, this is his case, he has an obvious vested interest in its outcome. It is a case where he asserts his reputation was harmed. Regardless of how it came to be that the evidence was provided by reports, that he affirmed in reports that he considered himself to be impartially assisting the Court, reflects adversely on him. Instead of giving the evidence contained in the reports in affidavit form, as he would have been entitled to do. Rather, he chose to present himself as an expert witness in this case, it appears, to have his opinions carry greater weight. It does not on that account.
276 Indeed, the lack of partiality is patent on the face of the reports. The content in part is taken from his thesis, and he promotes his method of surgery over others. I agree with the respondents that at times the reports read as a submission. For example, he refers to one study he undertook, in the following way:
Its uniqueness lies in the experience I have gained from my extensive patient cohort, rendering it an unparalleled resource for comprehensive and informative insights into infection management and treatment outcomes.
277 That in closing submissions the applicant now accepts that as a party, Dr Al Muderis’ opinion cannot be treated as independent, and that this has some relevance to the Court’s assessment of the weight to be given to his opinion evidence, does not alter the fact he was prepared to ascribe to the Expert Code of Conduct, with what that entails.
278 Examples of the features of Dr Al Muderis’ evidence I have described above, are evident in the consideration of the respondents’ case below. At this stage, I provide three examples to illustrate.
279 First, his understanding of various terms. The respondents made submissions regarding Dr Al Muderis’ cross-examination on the terms of “clinics” and “representative” in relation to the evidence of his United States practice, as examples of his failure to make appropriate concessions. To that, the applicant submitted that several of the matters relied on by the respondents as demonstrating Dr Al Muderis’ lack of credit owe to the imprecise or vague way in which he was cross-examined. I do not accept the applicant’s submission.
280 On the meaning of “clinic” in particular, this was a topic that Dr Al Muderis was alert to, given he was aware that Dr Rosenblatt (his United States representative) had warned him that he should not refer to the patient meetings in the United States as “clinics”, as he was not licensed to practice medicine in the United States. To give just one example, in an email dated 14 May 2018, from Dr Rosenblatt to Ms Roberts, copying in Dr Al Muderis, he states:
Please do NOT call the gathering in New York a clinic. Munjed will get into trouble for holding a medical clinic without a medical license. That is a grave offence and could mean serious fines and also revoking of his visa.
281 This topic also arose in his interview with Mr Steinfort. This is evident in the complete transcript of the unedited 60 Minutes interview with Mr Steinfort. There, he had the following interaction, which did not ultimately make it into the final publication of the Broadcast:
Mr Steinfort: Have you ever performed medical consultations or procedures in the United States?
Dr Al Muderis: No. No.
Mr Steinfort: We we’re aware of discussions among your colleagues about the wording they needed to use about patient gatherings, advising their own staff, not to call them clinics because they didn't want you to get in trouble for breaching your visa.
Dr Al Muderis: Look, the FDA and the medical boards in the United States have certain regulations. We have to respect that we have to be abide by it. We do attend conferences. … I give lectures. I give advice and I give general talks to amputees. This is general knowledge, and that’s not dissimilar to all the clinicians that come from Germany, from Holland, from Sweden. And they do the same. We meet altogether. And by the same token surgeons coming from New York, if they go to California, they’re not allowed to see, to speak to patients or consult with patients because their medical board is different. So this applies to everybody. So we have to be careful when we give advice to patients and we can speak in general terms, we can give an educational advice, but you can’t do a particular consultation on a patient in the United States or any other country if you are not registered.
…
As I mentioned to you, we when we go to conferences, when we go to places where we see patient gatherings, I give lectures, I give educations and there will be people there. There will be patients there. And basically the forum is in an open forum in conference rooms. And we give general information to patients.
282 It was in that context that Dr Al Muderis was asked about the clinics in cross-examination. He insisted that he did not understand the term and that he did not know what the word “clinic” meant. He was slow to accept that he held “clinics” in Australia, at first saying “I don’t know what you mean by clinic”, before then describing these as an “osseointegration service”. He continued:
I don’t understand the definition of a clinic … I don’t understand what a clinic means … I don’t understand what’s wrong with calling anything a clinic … there are clinics in the United States. There are – I mean a clinic could be a place. A clinic could be a setting. Like, for example, there is a Mayo Clinic, which is a location.
283 I note that at one point, he accepted that he used the word “clinic”, and that it was his word, but purported not to understand what it meant. Then, after insisting that there had been a “gathering” rather than a “clinic” in the United States, he could not articulate a difference: “It’s – people – I don’t understand what a clinic means … As I said, there is a Cleveland clinic, there is the Mayo Clinic, and they are buildings”.
284 The respondents submitted that Dr Al Muderis denied what was obvious – that he sought to avoid the word “clinic” and instead used a word conveying a social rather than clinical interaction, because he knew that he was not entitled to provide medical services in the United States.
285 That Dr Al Muderis well understood the meaning of clinic was evident in his later evidence in cross-examination when asked about an email sent arranging a clinic in New Orleans. Dr Al Muderis gave evidence that Ms Roberts should not have described it as a clinic, because it is “not a clinic”. His evidence was that Ms Roberts’ use of the word “clinic” was wrong. It is difficult to accept that one can claim they have no understanding of a certain word, while also stating that its use in a particular context was incorrect.
286 Finally, as the respondents submitted, during his evidence, Dr Al Muderis referred to “clinics” run by the Red Cross in Cambodia and to patients attending a “clinic” in Australia but was evasive in his answers when asked about this word in the context of the United States (as noted above).
287 There did not appear to be any vagueness in the applicant’s cross-examination, and no genuine confusion on the part of the applicant. It was evident from the content of the evidence, and from seeing and hearing this cross-examination, that Dr Al Muderis was being evasive and disingenuous in his purported failure to understand the questions, or the meaning of certain words. The applicant’s submission as to the point that Dr Al Muderis was said to be making in cross-examination (that is the term “clinic” does not have a consistent meaning), ignores the context of the cross-examination. The nature of the clinics is evident in evidence discussed below. I accept the respondents’ submission that Dr Al Muderis’ evidence of a lack of understanding of the term was disingenuous. The applicant knew he was not authorised to provide medical services in the United States, and his concern about that was the basis for his answers.
288 The same observations can be made of Dr Al Muderis’ evidence of his understanding of the word “representative”. Dr Al Muderis gave evidence that Dr Rosenblatt was “not [his] American representative”. Later, when then asked to confirm that his evidence was that Dr Rosenblatt had not at any time been his representative in the United States, he responded: “No, I did not say that”. Dr Al Muderis then purported not to understand the meaning of the word “representative” when put to him in cross-examination: “I don’t – I don’t understand that word representative means”. He refused to accept the proposition that Dr Rosenblatt was his representative where it was plain (from documentary evidence) that he was. When Dr Al Muderis was shown an email from Ms Roberts in cross-examination which referred to Mr Hernandez and Dr Rosenblatt as his representatives, he initially agreed it was “correct” and that he had instructed Ms Roberts to send the correspondence in those terms. However, when pressed and reminded of his previous answers which appeared to be inconsistent with the email, he maintained he was not a representative: “He’s a colleague. He represent[s] osteointegration. He is – he represents his own practice. I mean, we’re playing with words here”. This response is not indicative of confusion on Dr Al Muderis’ part, but rather an attempt at evasion. Emails sent from Dr Al Muderis’ practice refer to Dr Rosenblatt and Mr Hernandez as “our representatives” and Ms Roberts accepted that to be the position.
289 Second, as the respondents submitted, Dr Al Muderis on occasions used a technique in cross-examination to avoid answering questions which included asserting at various times that he was “not a pain specialist”, “not a prosthetist”, “not a psychologist”, “not a radiologist”, “not a lawyer”, not a qualified person to understand a contract, “not a physician”, “not a pathologist”, and “not a statistician”. This was acutely illustrated in cross-examination about the terms of a contract with Mr Hernandez (discussed in Part 5, Section 6) where Dr Al Muderis said, on several occasions, he did not understand the contract, and that “I’m not a qualified person to put a contract or make a contract or understand the contract”. I do not accept that evidence or that Dr Al Muderis regarded himself in that position, but rather it was entirely disingenuous to suggest that he could not understand the contract, with the answers given to avoid admitting his understanding of its plain terms. As explained below, Dr Al Muderis’ evidence in cross-examination in relation to the contract was not just evasive, it was false.
290 Third, to provide an example of a different nature. As will be apparent when considering the case study in relation to Ms Mooney (a non-osseointegration patient), Dr Al Muderis gave an answer in cross-examination, conceding an issue which he had repeatedly denied: see Part 6, Section 8. A critical aspect in respect to Ms Mooney’s case was whether Dr Al Muderis observed a malalignment in her leg at the time of surgery. His case as deposed to in his affidavit and repeated in cross-examination was that at the time of surgery, there was no malalignment and because of swelling he could not tell if there was any malalignment. Despite that evidence, Dr Al Muderis ultimately conceded in cross-examination that he observed a deformity during Ms Mooney’s surgery:
… that could not be rectified at the time of that particular surgery, considering that the surgery took more than five hours, and the decision had to be made to conclude the surgery without compromising the patient leg.
291 That answer is inconsistent with the case he advanced. It is a topic on which there can be no misunderstanding.
292 Other examples of these features of Dr Al Muderis’ evidence discussed elsewhere include: evidence of his explanations when questioned on whether he had responded to messages from patients for help; his failure to accept the obvious meaning of messages sent to him by patients who were complaining about the position they were in (e.g. Ms Çalan and Mr Urquhart); and his failure to accept what was obvious in x-rays (e.g. Mr Mortimer).
Ms Claudia Roberts
293 Ms Roberts has been the Accounts Manager at the LRC since about July 2021. She also worked for Dr Al Muderis as the Clinical Coordinator and Rehabilitation Manager at his practice, Norwest Advanced Orthopaedics, from July 2017 to October 2020 before going on maternity leave. She is a physiotherapist by training. She is the applicant’s life partner.
294 Ms Roberts was cross-examined over a period of a day and a half. It appeared at times that Ms Roberts had a prepared statement to make on some topics. Her answers sounded prepared and at times were not responsive to the questions being asked but rather were defensive of the actions taken by her or the applicant. It was apparent that in relation to some topics, she was acutely aware of what not to say. It was also plain that Ms Roberts was aware of how she was to respond to certain lines of questioning, even in the face of clear contemporaneous evidence (including from her) to the contrary.
295 To take as an example her evidence about the “clinics” conducted in the United States (also referred to above in considering Dr Al Muderis’ evidence). On Dr Al Muderis’ trips to the United States, Ms Roberts organised the “clinics” for him to see existing and prospective patients and often travelled with him to do so. An email in evidence from Ms Roberts sent to 96 existing or prospective patients in the United States, dated 9 May 2018, states:
Hello again from Claudia in Sydney!
I am delighted to [tell] you that Munjed will be running an Osseointegration clinic in New York on 9th of June and has allocated time to meet and examine you in person. We will have some of our older patients attending who have already had Osseointegration who you will be able to talk to as well and find out more information first-hand. In our experience after nearly 500 cases, this type of clinic is the most valuable.
If you can meet him in New York please let me know, alternatively we will be in Tucson around 12-14th of July if this would suit you better.
Please let me know.
(emphasis in original)
296 On 6 June 2018, Ms Roberts sent a follow up email to the recipients with details of the “OI clinic”, requesting they bring recent x-rays with them. I note that in both emails, Ms Roberts’ title in her email signature is “Clinical Coordinator and Rehabilitation Manager”.
297 Those emails and her evidence makes clear that Ms Roberts, at the direction of Dr Al Muderis, had organised a clinic in New York with the objective of Dr Al Muderis reviewing patients including a physical examination and an examination of their x-rays, to advise whether or not they were suitable for osseointegration surgery. In relation to the arrangements for that clinic in New York, an email from Ms Roberts liaising with Mr Hernandez, explains that she had spoken to Dr Al Muderis and the suggestion was to book an additional hotel room where “Munjed said the patients can be met in the foyer and be brought up to the hotel room for a consultation”: see e.g. Mr Wynne and Ms Schaeffer patient case studies in Part 6, Section 4, whose evidence is consistent with that (relating to other occasions).
298 Ms Roberts, in cross-examination, gave evidence that before these trips, including to New York, she would email patients (both who had osseointegration or were interested in it) to inform them that Dr Al Muderis was travelling to the United States, and to offer them a timeslot to see him. Ms Roberts was shown in cross-examination the email extracted above. She accepted that the purpose of those meetings was to meet and examine patients in person, as well as to conduct follow-up assessments. She also accepted that one of her jobs during those meetings was to display on her laptop things like x-rays of the patients’ hips and legs to give to Dr Al Muderis. She gave evidence that shortly after those meetings, upon returning to Sydney, she would provide patients who had met with Dr Al Muderis, information about booking osseointegration surgery (including fee estimates).
299 Despite this evidence, Ms Roberts claimed in cross-examination that there was a distinction between consultation and meeting, contending that what was organised was the latter:
Well, I would like to explain that a consultation – when a patient comes to a clinic, they come to see a medical practitioner with the view of getting an assessment. So the medical practitioner will make a judgment on their current situation and either seek advice or treatment, and none of which Munjed did in America. He did examine patients, meaning inquire into, to gather information, to give education, but it was only once Professor Al Muderis was back in Australia he would then make the – the assessment.
300 Ms Roberts then denied knowing, or having been told, that it was an offence to provide medical services in the United States without a licence, and that it would be a grave offence for Dr Al Muderis to do so. However, after having been shown the email from Dr Rosenblatt (referred to above at [280]), she accepted that this was the case. Ms Roberts eventually conceded that she had been told it was unethical and illegal for Dr Al Muderis to provide any form of medical service to patients in the United States.
301 Ms Roberts said in cross-examination that she stopped calling it a “clinic” because she was told she used the wrong term. In cross-examination, she initially referred to them as meetings (and accepted use of the word “gathering”). However, over time Ms Roberts did not maintain this pretence in the face of the evidence, and then reluctantly accepted the obvious, that what was being organised was a clinic and consultations.
302 Internal emails sent within Dr Al Muderis’ team in the lead up to the organised events supports those descriptions. She also accepted that she intended to promote the clinics or consultations on social media, but had been told not to, so that regulators did not find out that Dr Al Muderis was seeing patients in circumstances where he had no entitlement to do so. Ms Roberts accepted that she and Dr Al Muderis agreed not to do so, because she appreciated from what Mr Hernandez had said to her in an email dated 15 May 2018, that widely promoting it on social media would bring it to the attention of the wrong people, that is, the regulators.
303 The language initially used by Ms Roberts in cross-examination in relation to the consultations (e.g. as a “meeting”) was carefully chosen to avoid any suggestion of advice being given, because she was acutely aware that it was illegal for Dr Al Muderis to provide medical advice, as he was not licenced to do so. Her answers on this topic were deliberate, and prepared. Her evidence is inconsistent with the evidence of patients discussed below who attended these clinics, and documentary evidence including emails sent by her for that purpose: see Part 6, Section 4.
304 The clinic was organised, patients were advised in advance, an appointment time was provided to the patient to meet Dr Al Muderis and for him to examine them (e.g. by considering their x-rays in the process), advice was given, and patients then acted on that advice. Although Dr Al Muderis denied examining patients, he ultimately said:
I did look at the patient, I looked at the X-rays, I did hear their stories, and I did tell them that they may be suitable for [osseointegration] surgery pending the consult.
I do not accept that such meetings were merely a patient gathering, to “give education”. I do not accept Ms Roberts’ evidence on that topic (noting her evidence changed during cross-examination). Calling it a meeting or gathering, as Ms Roberts (and Dr Al Muderis) repeatedly attempted to do, does not alter what occurred. They did so because describing it as a clinic brings with it certain connotations. The description of “clinic” was used in correspondence by Ms Roberts because that is what she organised. Referring to it as a clinic in the circumstances creates an expectation among the patients as to what would occur when they attended, which was no doubt reinforced by the patients being asked to bring their x-rays and being told they would be examined. What occurred on the patients’ evidence was a consultation, examination and assessment, albeit brief. That there were obvious deficiencies (e.g. no notes were taken, patients were not advised of the risks and complications) does not alter that. On the strength of what Dr Al Muderis advised the patient as to their suitability, many of them made the decision to undergo the surgery. For all intents and purposes, and as a matter of common sense, such meetings operated as a clinic: see Part 6, Section 4 on the international patients.
Expert witnesses
305 The applicant relied on expert reports of Dr Tetsworth and Dr Stoita. He also relied on an expert report from Dr Rozbruch (from the United States) which was tendered, with him not being required for cross-examination.
306 The applicant also called doctors (and prosthetists) who are involved in his practice (or with whom he works closely) to give evidence, inter alia, of what is said to be his standard practice. Some of these witnesses are discussed below under the heading “other witnesses”.
Dr Kevin Tetsworth
307 There were three affidavits of Dr Tetsworth read as evidence, and four expert reports tendered.
308 Dr Tetsworth is an orthopaedic surgeon, specialising in limb reconstruction surgery and osseointegration. He has been clinically active in orthopaedics for over 35 years. He is a consultant staff surgeon in the Orthopaedic Trauma and Limb Reconstruction department at the Royal Brisbane and Women’s Hospital (RBWH) but also travels to Sydney every two weeks to see patients and perform surgeries at Dr Al Muderis’ clinic at Macquarie University Hospital. He has worked with Dr Al Muderis since 2015. He has held several positions as a professor at the University of Queensland. He has published extensively in his area.
309 Dr Tetsworth did not disclose in any of his affidavits or expert reports that he is a director alongside Dr Al Muderis of several companies, including the Limb Reconstruction Centre Pty Ltd, the Academy of Musculoskeletal Reconstruction and Osseointegration Surgery Pty Ltd, and PedCAT Imaging Pty Ltd. He accepted in cross-examination that he is also a shareholder in these companies.
310 In addition, Dr Tetsworth considers himself to be a long-standing friend of Dr Al Muderis. There is a text message exchange that occurred between Dr Tetsworth and Dr Al Muderis shortly after the airing of the Broadcast and the publication of the Articles. For example, in those messages, Dr Tetsworth offered his support by asking Dr Al Muderis to “let [him] know what if anything [he] can do” and stating, “Always got your back – just let me know”. Both of them also referred to the other as their “mentor”.
311 In that context, Dr Tetsworth provided three reports relating to three different patients in these proceedings. One of those patients, Mrs Gollan, is a patient he had seen in a clinical context and had operated on. In his affidavits, he refers to his involvement with four patients who gave evidence. However, it appears Dr Tetsworth may have also been clinically involved with Dr Al Muderis in relation to a further 11 patients called by the respondents. To put it another way, Dr Tetsworth appears to have had active involvement with these patients, who have now given evidence in these proceedings of issues they have experienced. These matters were not disclosed by Dr Tetsworth in any of his affidavits or reports. The expert report in relation to Mrs Gollan does not refer to his clinical involvement with her.
312 Dr Tetsworth has ascribed to the Expert Code of Conduct which, inter alia, refers to an expert being impartial in the expression of their opinion. It is readily apparent that the matters referred to above are all relevant to the question of the independence or impartiality of Dr Tetsworth. His answers in cross-examination on this topic were unsatisfactory.
313 For example, in relation to his business associations with Dr Al Muderis, he said the information was of “such limited consequence and importance to the proceedings that [he] did not find them relevant”. As to the text messages relating to his offer to testify in support of Dr Al Muderis, when asked what the difference was between that and giving an expert opinion, he said:
I’m generally supportive of Munjed and able to testify as to the quality of his care and the passion that he brings to the care of his patients and the dedication and the time and effort he puts into it, and the other is expert opinion as to the nature and quality and benefit to patients for – of osseointegration itself.
He considered these matters that had not been disclosed “immaterial” to the Court’s ability to assess his independence and integrity. When subsequently asked about whether he therefore considered the Court’s knowledge that he “said to Dr Al Muderis … [he] would testify in support and do whatever it takes” to be immaterial in its assessment of his independence and integrity, he replied: “I think it’s – it’s evidence that I was able to successfully differentiate between the two – the personal relationship and the expert opinion”. It is difficult to understand how, as Dr Tetsworth said, it was evidence that he was able to “differentiate”. It is not an answer to the question. As to the fact he had seen one of the patients about whom he later purported to give an impartial expert report, his failure to refer to his previous contact with her was said to be because he was only asked to address specific questions.
314 Dr Tetsworth has a strong view about Dr Al Muderis’ ability as a doctor, the manner he treated his patients, the quality of his care and the passion he brings to that. He denied that his knowledge and respect for Dr Al Muderis would have influenced his ability to be an expert witness. However, I note Dr Tetsworth approached his expert reports on the assumption that Dr Al Muderis would not have been negligent, and that in his opinion he is a responsible surgeon (as clear from his evidence about Ms Mooney).
315 Dr Tetsworth’s failure to recognise the potential significance that the matters referred to above may have had on his independence as an expert, or that it is for the Court to decide whether that is so, also impacts the assessment of his evidence.
316 Dr Tetsworth presented as a witness confident in the correctness of everything he said and gave the strong impression that what he viewed could not be questioned. That is evident, for example, in his responses in cross-examination on his relationship with Dr Al Muderis (as noted above), with the effect of Dr Tetsworth’s evidence being that these are immaterial considerations because he has told the Court he complied with the Expert Code of Conduct. Dr Tetsworth’s failure to grasp the potential significance of this is troubling.
317 I refer to two further examples relevant to considering Dr Tetsworth’s independence in giving evidence.
318 First, he wrote a report written in support of an application for Mr Ford as part of his workers compensation claim to receive funds to undergo osseointegration surgery (Mr Ford’s case study is addressed below in Part 6, Section 3). The report expressed the view that Mr Ford was a suitable candidate for osseointegration, as did a separate letter by Dr Al Muderis. The terms of the report make plain it was written to support the opinion of Dr Al Muderis. Leaving the merit of any opinion expressed aside, Dr Tetsworth’s report criticised the experience of other doctors who had expressed views to the contrary. He was prepared to make such comments when holding himself out as an expert in circumstances where he said in the report that he had not read their reports, rather emphasising to the reader that he was far more qualified to express an opinion, and that Dr Al Muderis is one of the global leaders in the field. This was the basis for his view that Dr Al Muderis’ report should be accepted. His preparedness to express his opinion in that way, and willingness to do so without even considering what other doctors opined, reflects adversely on him.
319 Second, Dr Tetsworth gave evidence in these proceedings in circumstances where his conduct in relation to Mr Urquhart, a patient referred to in the Publications, is the subject of a complaint by the patient. Namely, that Dr Tetsworth suggested to Mr Urquhart during a consultation that he spray Febreze, a carpet deodoriser, on his stump to deal with the odour emanating from his stoma that he had been complaining about (see Part 6, Section 7). Dr Tetsworth in cross-examination expressed the view that “Febreze is the single most effective odour fighting agent available”. He said he has discussed this with patients many times. However, he accepted that he had not sought to investigate the use of Febreze in a clinical setting, including whether it is appropriate for such use. He does not know if it is clinically approved for such use. Rather, on his evidence, the extent of his knowledge on Febreze is from reading its Wikipedia entry on one occasion. I accept the respondents’ submission that this reflects poorly on his practice.
320 The applicant in closing submissions accepted Dr Tetsworth has a professional relationship with Dr Al Muderis, and that this must bear on the Court’s assessment of the weight to be given to his opinion evidence. The applicant nonetheless submitted that:
[r]egardless of Dr Al Muderis’ interest as a party and Dr Tetsworth’s relationship with him, the difference between them and the respondents’ experts in expertise on osseointegration – as measured by both clinical experience and academic research – and in the quality of their reports is so large that the Court would accord their opinions on disputed issues in relation to osseointegration substantially more weight than that of the respondents’ experts.
321 I note that out of the three patients on which Dr Tetsworth gave an expert opinion, being Mrs Gollan, Ms Mooney and Mr Mortimer, only the latter is an osseointegration patient. That said, he did give evidence in relation to other osseointegration patients he was clinically involved with.
322 The applicant’s submissions directed to the matters of non-disclosure by Dr Tetsworth were limited. The description in the submission above about him having a “professional relationship” with Dr Al Muderis understates the matters relied upon by the respondents noted above, which include, inter alia, the business relationship and the nature of the text messages.
Dr Razvan Stoita
323 There were three affidavits of Dr Stoita read as evidence, and six expert reports tendered.
324 I note that Dr Stoita’s affidavit refers to him having had clinical involvement with three patients (or prospective patients) involved in these proceedings. However, it appears from the evidence that he may have had some clinical involvement with a further four patients involved in the proceedings.
325 Dr Stoita has worked with Dr Al Muderis at the clinic since about 2016 or 2017 (and says he has known the applicant for around six years). He is partners with Dr Al Muderis, being a director and shareholder of Limb Reconstruction Centre Pty Ltd. He therefore has a financial interest in the success of the LRC. In addition to that, Dr Stoita and Dr Al Muderis are common shareholders in the new hospital that has been built at Macquarie University Hospital with other doctors, Medibank and the hospital itself. They are also partners in radiology equipment they purchased to provide services to patients, as Macquarie University Hospital lacked the funds to provide that equipment.
326 He regards himself as a friend, colleague and supporter of Dr Al Muderis. He holds the view that Dr Al Muderis is a good surgeon, noting he “otherwise wouldn’t be in practice with him if he wasn’t”. He encouraged Dr Al Muderis to sue for defamation and believes the reporting is unfair. This is reflected in text messages exchanged between them at the time of the Publications, which also reflect the support Dr Stoita was providing – and intended to continue providing – to the applicant in the future. A text exchange included Dr Stoita texting “you’ve got all of us ready to go in to bat for you. Just let us know” and Dr Al Muderis texting to him at a later date, “we need to be solid on this”. His affidavit evidence in respect of the applicant’s reputation refers to him as “one of the most skilled surgeons [he has] ever met and … treats every patient with the utmost care and regard for their health”. His position is clear regarding his view of the applicant. He gave evidence that most of his discussions with the applicant about the case have been to offer support (although he also said Dr Al Muderis mentioned to him about being asked questions in cross-examination about an overseas patient).
327 The expert reports provided by Dr Stoita do not disclose any of the financial matters connected to the applicant. His failure to disclose such matters reflects adversely on him, in a context where he asserts in the reports, by ascribing to the Expert Code of Conduct, that he is an independent and impartial expert. Dr Stoita appears to regard himself as capable of giving independent evidence on the basis that all his reports “are backed by the literature” and have “nothing to do with … Dr Al Muderis”. That statement is rather disingenuous given the evidence related to Dr Al Muderis’ practice as a surgeon. I note for example, that Dr Stoita accepted in cross-examination that his evidence on a particular topic (in relation to Mr Marlborough) was based on an assumption as to what Dr Al Muderis did, rather than on what was recorded in the consultation report. Dr Stoita also accepted that he had discussed Ms Heffernan’s case with Dr Al Muderis (being one of the patients he provided an expert report on), although he said he could not recall whether the discussion took place before or after he had completed his report. When asked whether he should have disclosed the discussion in the report if it occurred beforehand, Dr Stoita said: “Possibly. Now, I don’t really – I’ve still made the report based on the evidence that was presented in the notes … [s]o not from the discussion that I had with Dr Al Muderis”. Regardless of Dr Stoita’s view, he still discussed the patient with the applicant in a context where he was going to give expert evidence on her. Dr Stoita accepted that some of the financial matters may be relevant in addressing the strength of his evidence but not the reliability. Dr Stoita’s lack of appreciation of the potential significance of these matters to the assessment of any opinion he expresses is troubling.
328 I note that the applicant did not address the evidence of Dr Stoita, as an expert in these proceedings, in his closing submissions (i.e. he referred only to himself, Dr Tetsworth and Dr Rozbruch as experts in osseointegration). As such, the applicant did not make any submissions in respect of the issues, including Dr Stoita’s non-disclosure, that arise in his evidence.
Dr S. Robert Rozbruch
329 Dr Rozbruch is an orthopaedic surgeon from New York and has practiced for 28 years with experience in trauma and amputation surgery. He is the chief of the Limb Lengthening and Complex Reconstruction Service, and the director and founder of the Osseointegration Limb Replacement Centre at Hospital for Special Surgery in New York. He first became engaged in osseointegration in 2015 and has since performed about 150 osseointegration surgeries.
330 Although the respondents noted his close relationship with Dr Al Muderis, they did not require him for cross-examination. I note a couple of the publications referred to in the curriculum vitae attached to his expert report are co-authored with Dr Al Muderis (one of these being in 2020 and also has Dr Tetsworth as a co-author).
331 Dr Rozbruch’s report does not address specific patients but rather expresses opinions in his answers to questions posed relating to osseointegration generally (some of which respond to statements from the respondents’ witnesses’ expert reports). The respondents did not challenge that the opinions expressed in his report are genuinely held. The respondents submitted that some of his views are at odds with those expressed by Dr Al Muderis, giving two examples. First, Dr Rozbruch opines that in relation to infection sometimes the diagnosis can “be made with simply observation”. Second, in relation to the use of a plastic surgeon for osseointegration, Dr Rozbruch uses one at his discretion, where he explained that the soft tissue contouring, stoma creation and nerve reconstruction require a surgeon skilled in that area, which may be an orthopaedic and/or a plastic surgeon. I proceed on the basis Dr Rozbruch genuinely held the views he expressed in his report.
Other witnesses
Dr Tim O’Carrigan
332 Dr O’Carrigan is an orthopaedic surgeon and a current member of Dr Al Muderis’ team at the LRC, having started in around April 2018. He has known the applicant since this time and is one of four orthopaedic surgeons who were part of the development of the LRC (along with the applicant, Dr Tetsworth and Dr Stoita). He gave evidence that he would usually attend the LRC on a weekly basis, on Wednesdays to operate, and on Thursdays to consult (but every second week he would see his own patients, not connected to the applicant). His affidavit evidence on Dr Al Muderis’ reputation makes it clear he has a positive view of the applicant. For example, his affidavit refers to the applicant having a reputation of being, inter alia, a “competent surgeon”, “trustworthy, wanting the best for his patients” and “an innovator”.
333 At times, Dr O’Carrigan gave evidence in a very defensive manner. Although he accepted certain propositions in cross-examination as to the conduct of Dr Al Muderis or that expected of a surgeon, at times, he was reluctant to do so. On occasions he attempted to avoid answering questions in relation to conduct he perceived would ultimately reflect badly on the applicant, only to eventually, and sometimes begrudgingly, do so. This relates to propositions accepted by other medical witnesses regarding the proper conduct of a surgeon as to the care of a patient (or prospective patient) who undergoes osseointegration surgery. Dr O’Carrigan also said in response to some questions, that he did not know, or was not aware of aspects of Dr Al Muderis’ practice, or certain issues that were said to have arisen in respect of patients. Given his role and involvement at the clinic for several years, this is difficult to accept in all instances.
Dr Mustafa Alttahir
334 Dr Alttahir is an orthopaedic surgeon who is part of Dr Al Muderis’ team at the LRC. He first met Dr Al Muderis in 2009. Dr Alttahir commenced working with the applicant during his fellowship at Macquarie University Hospital between August 2019 and January 2020. He then returned to become part of the LRC in 2020. Dr Alttahir regards himself as “good friends [with the applicant] outside work”. He gave evidence Dr Al Muderis had a reputation for having “an impressive work ethic, being a leader, and being innovative and brilliant as a surgeon”.
335 At times he gave evidence in cross-examination in a defensive manner, as well as volunteering explanations or justifying his position rather than answering the question. He was reluctant to accept propositions put to him which were accepted by other witnesses (including those in his team at the clinic). He appeared conscious of the consequences of an answer to the applicant’s case. He also referred to a matter from the applicant’s opening, reflecting he was aware of at least part of the case presented and was acting accordingly. He did not present as impartial, but rather as a witness who had an interest in the outcome of the case.
Dr Abdul Haidary
336 Dr Haidary is a rehabilitation specialist at Sydney Adventist Hospital, The Hills Private Hospital (The Hills) and the LRC at Macquarie University Hospital. He started working as a rehabilitation consultant for Dr Al Muderis in around 2015, and since then has looked after Dr Al Muderis’ patients in the provision of pre-operative care and rehabilitation.
337 His evidence on Dr Al Muderis’ reputation makes it clear Dr Haidary has a positive view of him. In his affidavit, he refers to Dr Al Muderis being a “highly skilled surgeon and an innovator”, where he “cannot recall having ever heard a complaint about [his] conduct or his patient’s outcomes”.
338 Dr Haidary gave evidence confidently, at times defensive, and was dismissive of any suggestions put to him contrary to his evidence. From the outset, when answering questions (including in examination-in-chief), Dr Haidary did not do so, but rather volunteered statements he perceived to be advantageous to the applicant’s case. His evidence, on occasions, was also not based on what he recalled from being present at a consultation, but what he expected to be the case. For example, in relation to Mr Smith, Dr Haidary was prepared to say in his affidavit evidence that it was a “ridiculous” suggestion by Mr Smith to say he was not informed of the rehabilitation process, asserting it was explained to every patient. Yet he gave evidence in cross-examination that he does not recall being present at the pre-operative consultation (noting there was no consultation report produced). It is not an answer for Dr Haidary to say he knows the process from having been “to all of the clinic[s]”, meaning “it’s impossible somebody will not” have the rehabilitation process explained to them. I note that despite Dr Haidary’s description as to the pre-operative process, he is not listed in any of the initial pre-operative consultation reports in evidence as having been present (and most reports did not record any rehabilitation consultant as present). On the other hand, he also omitted to refer in his affidavit to the fact that the nursing notes of Mr Smith at The Hills reflected that Mr Smith had notified the nurse that his stump was bleeding when he was sitting down on the toilet, identifying “+++” as to the quantity of blood. This is consistent with Mr Smith’s evidence. Dr Haidary’s explanation for omitting this incident in his evidence varied and was unsatisfactory (including that it was hard to tell how much of the blood referred to was Mr Smith’s “imagination” or ooze).
Dr Karan Doshi
339 Dr Doshi is an orthopaedic surgeon, qualified in India. He worked with Dr Al Muderis as his fellow and under his supervision from April 2019 to January 2023 at East Sydney Private Hospital, Macquarie Hospital and Norwest Private Hospital. During that period, he gave evidence he worked with Dr Al Muderis daily. He considered his job with Dr Al Muderis to be “fantastic”.
340 Dr Doshi appeared more willing to make appropriate concessions than other doctors referred to above. He typically accepted propositions put to him in cross-examination about the conduct expected of a surgeon. However, when he was asked questions directed to Dr Al Muderis’ conduct or his practice, in many cases, he either did not recall, or was unaware of certain practices or patients.
Mr Stefan Laux
341 Mr Laux is a clinical prosthetist and manager at APC Prosthetics in Sydney. He first started working with Dr Al Muderis in 2011.
342 Mr Laux was generally an honest witness but appeared to be conscious of saying anything which might be seen as critical of Dr Al Muderis. He appeared to be very uncomfortable giving evidence and was hesitant at times.
343 I note that Mr Laux gave evidence that he has referred patients or prospective patients who were interested in osseointegration to other doctors, including Dr Huang, whom he held in high regard. In relation to Mr Urquhart, Mr Laux also said that when Mr Urquhart mentioned his troubles to him regarding his implant and wanting a second opinion, Mr Laux recommended Dr Huang (amongst a couple other surgeons).
344 After the completion of the evidence in the hearing, the applicant attempted to tender a statement apparently signed by Mr Laux dated 29 August 2022 (shortly before the Publications) about his interactions with Ms Grieve as at that date. The argument about admissibility occurred on 23 May 2024, at which time, I did not admit the document but gave the applicant leave to put on further submissions. He did so in his closing submissions, contending that the document is admissible under s 64(3) of the Evidence Act, and that the applicant could not have tendered it before the conclusion of the examination-in-chief of Mr Laux because of s 64(4).
345 That submission is misconceived. Mr Laux gave evidence for the applicant. The applicant was aware of this document and what he says is the status of Mr Laux before he gave evidence. The applicant asserts that he is one of the confidential sources. The applicant could have, but did not, lead evidence from Mr Laux of any of his dealings with Ms Grieve. The document (and any dealings with Ms Grieve) was not referred to in his affidavit, nor was it sought to be lead orally. That was a choice the applicant made. Section 64(4) did not prevent that from occurring. This is also in a context where prior to the commencement of the hearing, the applicant had been attempting, through various applications, to obtain information about the identity of confidential sources. In that context, the applicant cannot, at the end of the hearing, seek to tender a document containing a previous representation of a witness who gave evidence in the proceedings (for the truth of the content) on a topic they say is of relevance, but chose not to lead in his case. The applicant ignores the premise of s 64, which is that the person who made the previous representation is available to give evidence about that representation. The obvious reason for s 64(4), that the representation must not be tendered before the end of examination-in-chief without leave of the Court, is that the witness would no doubt give evidence about, or authenticate, the document before it is tendered. Leave was not sought by the applicant to tender it. The further submissions do not alter my view that the document is not admitted.
346 I note, despite the applicant’s assertion, Mr Laux did not identify he was a confidential source. He has never released Ms Grieve from the promise of confidentiality.
Section 6 — The respondents’ witnesses
347 Before addressing the case studies, it is appropriate to refer to the expert witnesses called by the respondents. An assessment of the principal witnesses is addressed below, with others referred to in the patient case study in relation to which they gave evidence. It is also appropriate to consider the evidence of witnesses who worked with Dr Al Muderis, being Ms Stewart, Mr Grant and Mr Hernandez. The evidence of some patients (addressed later in these reasons) is relevant to the assessment of these witnesses, and it is important to bear that in mind when considering their evidence.
Expert witnesses
Dr Stephen Ruff
348 Dr Ruff is an orthopaedic surgeon and has been a staff member of the Royal North Shore Hospital (RNSH) and Dubbo Hospital for 40 years and 25 years, respectively. He was a member of the Court of Examiners for the Royal Australasian College of Surgeons for eight years. He is also the recipient of three awards from the Royal Australasian College of Surgeons including the NSW State Branch Merit Award (2006), the award for Outstanding Service to the Fellowship (2009) and the award for Outstanding Services to Surgery (2014). Over the years, he has been a member or chairman of various medical committees. His interests are trauma, spine, hip and knee surgery, and he has performed thousands of hip and knee arthroplasties.
349 There was one affidavit of Dr Ruff read as evidence, and two expert reports tendered. His evidence largely relates to non-osseointegration patients, or a surgeon’s conduct generally. Despite not having experience in performing osseointegration, I accept that Dr Ruff also has some knowledge of the procedure (noting he did the Brånemark’s course at San Francisco General Hospital). He was an impressive witness, who gave evidence carefully, in a considered manner, and was trying to assist the Court. He was an honest and reliable witness. He made appropriate concessions. He explained his opinions clearly and provided the foundation for them. His evidence was measured.
350 The applicant accepted that Dr Ruff was impressive and forthright in his oral evidence and had clearly attended to assist the Court. However, in relation to Ms Mooney, he submitted that Dr Ruff’s written report was in many respects unfairly critical of Dr Al Muderis. I address this submission below. Suffice to say at this stage, that I do not accept that submission in relation to his evidence concerning Ms Mooney.
Dr Michael Leung
351 Dr Leung has more than 35 years of experience as a plastic surgeon. He was employed at The Alfred Hospital (The Alfred) as a plastic surgeon from 1989 to 2017 and was the Director of the Plastic Surgery Unit at Alfred Health from 2002 to 2016. In 2009, he was appointed as an Associate Professor at Monash University.
352 In his report, Dr Leung identifies his qualifications, noting that Alfred Health runs a major Trauma Centre in Victoria, and the Plastic Surgery Unit runs an osseointegration unit involving craniofacial osseointegration, hand osseointegration, and upper and lower limb osseointegration. In those circumstances, he says he has experience in dealing with major trauma, including major limb amputations, as well as referrals regarding chronic stump problems in amputees. His report also details his education and post-graduate training. He has received direct teaching from Professor Per-Ingvar Brånemark regarding the techniques of osseointegration and craniofacial osseointegration. Dr Leung is a Member of the Order of Australia for significant service to medicine and the international community.
353 Similar to Dr Anstee (as discussed below), the applicant submitted Dr Leung had limited experience in osseointegration and his evidence was of limited relevance.
354 As Dr Leung’s evidence in cross-examination progressed, it became more apparent that he is obviously qualified to express opinions on the topics he has. The tenor of his cross-examination was at times belittling if he did not accept the propositions put to him. His honesty was questioned by the applicant. I accept he was an honest witness. I accept that Dr Leung is qualified to give the opinions he did about osseointegration surgery.
Dr Paul Stalley
355 Dr Stalley is an orthopaedic surgeon with over 39 years of experience, practicing at the Royal Prince Alfred Hospital. He is a Member of the Order of Australia for “significant service to medicine, particularly the treatment of bone and soft tissue cancers”. He has served as the Program Director of Surgery of Sydney Local Health District and either chaired or served on multiple government committees. He has held multiple administrative and clinical leadership roles. He has published many medical and academic papers and regularly presented at conferences. He is also a Clinical Associate Professor. There were four expert reports of Dr Stalley tendered in these proceedings. His reports discussed osseointegration generally, as well as a large number of the patient case studies.
356 As the respondents submitted, in his first report, he described his relevant experience including in relation to amputations and the management of large-embedded prostheses. In cross-examination, he explained that although osseointegration was not a procedure he performed, it was a simple one well within his skill set. His evidence was that he “declined to carry out those procedures because [he] feel[s] that there are vastly better options available”, and that osseointegration itself is a “very simple, straightforward operation, which [he] would leave to a fellow to do”.
357 Pausing there. The applicant criticised that evidence of Dr Stalley as “an arrogant and ignorant response which speaks poorly of his credibility”. He submitted that it demonstrates Dr Stalley approached this matter “with the preconception that osseointegration itself is a procedure which should not be caried out”. However, Dr Ruff also explained that the actual orthopaedic component of osseointegration “is terribly simple; it’s not much different from putting a cement-free component down a–a hip replacement, intramedullary nailing a femur”. He said it is the soft-tissue component “where it rises and falls” on the stoma that causes difficulties. Dr Anstee described it as follows:
The postoperative-care needs of osseointegration patients are high; it’s a complex system; troubles occur; there’s all sorts of rehabilitation needed. Just the osseointegration itself is a small part of the deal.
358 Dr Doshi, called by the applicant, also opined that the surgery itself is not complex, it is the management of potential complications that is complicated. Given that evidence, the applicant’s submission cannot be sustained. Besides, the import of Dr Stalley’s evidence was not a generalised opinion of osseointegration, but rather an explanation as to why he personally had not carried out the procedure before.
359 Dr Stalley proactively disclosed material in relation to his previous dealings with Dr Al Muderis in his report. It was appropriate to do so.
360 The applicant’s submissions were rather scathing of Dr Stalley, alleging he was dishonest in his evidence. He also submitted that Dr Stalley was “wholly unimpressive as an expert witness”, and that no weight should be placed on his opinions. He submitted that “he has no expertise at all in relation to osseointegration and is unqualified to opine on it”. It was submitted Dr Stalley’s opinion should therefore be treated as irrelevant and be disregarded when he purports to opine on osseointegration issues.
361 I do not accept that Dr Stalley was dishonest, or that he was an unimpressive witness. His evidence was clear and he explained the bases of his opinions (which covered many topics). Dr Stalley was put in a difficult position given the number of patients he was asked to give expert evidence about. The questions in cross-examination were rather acrimonious at times.
362 As the respondents pointed out, Dr Stalley was not wholly critical of Dr Al Muderis. For example, he volunteered that Dr Al Muderis “was a good clinical, dexterous surgeon”:
Ms Chrysanthou: You have never in relation to any of these patients, have you, criticised my client’s surgical skills?
Dr Stalley: No. His decision-making, soundly. Surgical skills, no.
363 I accept Dr Stalley may not view Dr Al Muderis in high regard. In disclosing his previous dealings with Dr Al Muderis, Dr Stalley also referred to there being:
several events which were unimpressive to me in terms of patient management and l was significantly unimpressed by his performance on an ethical basis and also on a personal basis.
364 Notwithstanding that, his evidence was reasoned and forthright.
365 The applicant was dismissive of Dr Stalley, and when asked about an opinion he expressed, Dr Al Muderis responded:
Dr Stalley had never done a single osseointegration surgery, so he doesn’t, to my knowledge, know anything about osseointegration surgery, what it involves. So it’s – it’s very arbitrary to make such a comment about surgery that he’s not familiar with.
366 That is more than disagreeing with the opinion expressed, but a criticism of the witness for expressing it. It was gratuitous.
367 Even if Dr Stalley has not performed the osseointegration procedure before, I do not agree with the applicant’s submission that he is not qualified to opine in relation to it given his experience. What weight is to be given to any opinion expressed will depend on the issue being considered.
Dr John Anstee
368 Dr Anstee is a plastic and reconstruction surgeon, who has served as a Senior Plastic Surgeon at The Alfred since 1987. Since 1990, he has been a part of the osseointegration unit at The Alfred. He has been involved in performing approximately 50 osseointegration surgeries. He is still part of The Alfred’s osseointegration services but stopped operating in about 2013. The Alfred is both the biggest trauma centre and the only adult burns unit in Victoria. Dr Anstee had previously observed and consulted some of Dr Al Muderis’ patients, including having had a consultation with Ms Todd.
369 He is one of Ms Grieve’s sources and appears in the Broadcast. He is also mentioned in each of the other Publications. Dr Anstee appropriately disclosed his involvement with Ms Grieve and 60 Minutes. He was forthright in his evidence on this topic.
370 The applicant submitted that as Dr Anstee is a plastic surgeon and not an orthopaedic surgeon, he is only qualified to opine on the management of soft tissue. I disagree. The evidence of Dr Anstee’s qualifications and experience renders him qualified to opine on osseointegration. In cross-examination, he explained how his plastic surgery training relates to the performance of osseointegration surgery. He was previously the leader of the osseointegration team at The Alfred (a role he was succeeded in by Dr Leung). As such, during that time, the ultimate decision as to who would receive osseointegration at that institution lay with him. I note that some topics on which Dr Anstee gave evidence were not confined to osseointegration but also addressed broader issues of surgical practice.
371 Dr Anstee gave evidence in a manner which displayed his expertise, and he clearly explained the bases for his evidence. He made appropriate concessions in doing so.
372 I note that the applicant’s submission with respect to Dr Anstee and Dr Leung, that they are not qualified to opine on osseointegration because they are plastic surgeons, is somewhat consistent with aspects of Dr Al Muderis’ evidence during the hearing discussed below in relation to his multidisciplinary approach (see Part 6, Section 1). That is, persons who are not orthopaedic surgeons cannot opine on whether a patient is suitable for surgery (which Dr Al Muderis has said is an orthopaedic decision).
373 That said, I note that the applicant accepted that Dr Anstee and Dr Leung both had experience with osseointegration but submitted that the extent of their experience was limited to the OPRA system, noting they had no experience with the OPL system. Notwithstanding the differences between the systems, the weight to be given to any opinion expressed by Drs Anstee and Leung will depend on the issue being considered.
Dr Saul Geffen
374 Dr Geffen is a rehabilitation physician. His qualifications and field of expertise are different to the other expert witnesses called by the respondents (who are all surgeons), yet the questions posed of him on which to provide an expert opinion were, in effect, the same. This included whether certain patients were suitable candidates for osseointegration surgery. As he conceded in cross-examination, he has “only ever referred four patients for consideration of an osteointegration system”. His opinion is therefore derived from the role which he performs in practice of deciding whether someone should be referred to a doctor to investigate undergoing osseointegration. That is not the question posed to him in his brief. Although Dr Geffen has experience in the types of conditions which may be relevant to an assessment of suitability, less experience with the surgery is required to fulfil the role he performs, compared to assessing a patient as suitable for osseointegration. That said, Dr Geffen acknowledged in his report, at times, the need to defer to the opinion of an independent osseointegration surgeon when he opined on orthopaedic and surgical issues. On his own evidence, he therefore limits the weight that could be attached to it on certain issues. He gave evidence that he has looked after amputees and people who have undergone osseointegration surgery, including from the pre-operative to post-operative stage. He is qualified to opine on general matters relating to the conduct of medical practice, and on matters such as aftercare and rehabilitation.
375 However, in relation to the question of suitability and other questions, at times, in his written report Dr Geffen provided gratuitous opinions on matters not related to the question. That, considered in combination with his qualifications and experience, reflects a lack of understanding of the remit of his brief as an expert witness in this matter.
376 Accordingly, with very limited exceptions, I do not rely on the evidence of Dr Geffen in resolution of these issues. Where his evidence is referred to, it relates to matters of a general nature.
Observations in relation to expert witnesses
377 I addressed the expertise of the respondents’ witnesses above. The applicant takes issue with the manner the respondents’ witnesses were instructed (i.e. on occasions their brief included a patient’s affidavit as opposed to assumptions as to facts). It is trite that the underlying facts on which the opinion is based must be established. I am acutely aware of that when referring to any expert opinions below. Where opinions are relied on, I am satisfied the factual foundation has been established.
378 In a comparison of the expert witnesses, the applicant submitted that their witnesses, Dr Al Muderis, Dr Tetsworth and Dr Rozbruch, are globally pre-eminent in the field of osseointegration, having done thousands of cases between them and published dozens of peer-reviewed articles, book chapters, and conference papers (I note that Dr Stoita was not included in this submission). As referred to above, he submitted that regardless of Dr Al Muderis’ opinion not being able to be treated as independent and Dr Tetsworth’s professional relationship with him:
the difference between them and the respondents’ experts in expertise on osseointegration … and in the quality of their reports is so large that the Court would accord their opinions on disputed issues in relation to osseointegration substantially more weight than that of the respondents’ experts.
379 I do not accept that as a global submission, but rather I am of the view that each issue that arises must be considered in light of the relevant evidence. The interests of the witnesses (i.e. arising from any association or past interaction with Dr Al Muderis) may not be so easily dismissed.
380 In his case in chief the applicant chose to only rely on expert reports in relation to the patient case studies that were prepared by doctors with whom he works and, as described below, has very close associations (Dr Tetsworth and Dr Stoita), even in relation to the non-osseointegration patients. Dr Rozbruch, whose expert report addressed more general questions about osseointegration, also has a close association with Dr Al Muderis. It was not until the applicant’s case in reply that he called another expert witness, Dr Sol Qurashi (but in respect to the orthopaedic patients).
381 Further, I note that the applicant submitted that Drs Leung, Anstee, Stalley and Geffen were no more disinterested or impartial than Dr Al Muderis or Dr Tetsworth, primarily because Drs Leung, Anstee and Geffen had dealings with Ms Grieve, and Dr Stalley held animus towards him. I do not agree with that as a general proposition. Although all relevant in assessing their evidence, the interest or lack of partiality of Dr Al Muderis and Dr Tetsworth, is of a different nature, and not comparable as framed by the applicant.
382 That said, I observe that many of the issues in dispute in the patient case studies involve matters of the credibility and reliability of the witness (considered in the context of the relevant evidence), and not ones of expertise.
Other witnesses
Mr Mitch Grant
383 Mr Grant was a patient of Dr Al Muderis and a patient advocate for his practice. Mr Grant was a credible and reliable witness.
384 The applicant withdrew his attack on Mr Grant’s credibility in closing submissions. It was plain from the applicant’s submissions during the trial that he was contending, inter alia, that Mr Grant had a commercial conflict of interest because of his business (which supplies osseointegration parts), which affected his credibility. Further, at several points in the hearing, the applicant alleged that Mr Grant was part of a concoction allegation, contending that it was “wholly beyond coincidence” that some patients had concocted complaints about Dr Al Muderis after contact with Mr Grant (among others), but this was subsequently withdrawn in relation to Mr Grant.
385 The applicant now accepts that Mr Grant is a credible witness other than what he described as “some small things that he misremembered”. However, the differences between Mr Grant’s account and that of Dr Al Muderis, can hardly be described as relating to “small things” or misremembering. Further, although the applicant referred to and relied on aspects of Mr Grant’s evidence, the recitation of it is not complete and in a manner that tended to distort his evidence on those topics.
386 In 2009, Mr Grant had his left leg amputated above the knee because of a motorcycle accident. In September 2011, Mr Grant underwent osseointegration surgery with Dr Al Muderis, using the EndoExo system, with the surgery conducted in two stages. He was Dr Al Muderis’ third patient to undergo the procedure. Mr Grant spoke of his good fortune in having the surgery and had a very positive experience. He has had little problems.
387 Mr Grant started working with Dr Al Muderis as a patient advocate in about 2012 and remained so for about four to five years. The patient advocate role lasted until 2017, although there was a hiatus of about six months in 2015 due to his frustrations with Dr Al Muderis in negotiating a consultancy agreement. I discuss this further below. Mr Grant returned to the role when Dr Rosenblatt became involved in the practice on the basis that he would deal with him (instead of Dr Al Muderis).
388 Against that brief background there are several points to be addressed.
389 First, I accept Mr Grant’s evidence that he became a patient advocate following an approach by Dr Al Muderis, who told him he was doing “really well”, and asked if he would “go and speak to these patients who are interested”. Mr Grant agreed because he was “happy to do so” as he thought the operation really worked and wanted to be able to help other people. He explained that because it was a new procedure, prospective patients benefitted from meeting patients like him who had had the operation.
390 As part of his role, Mr Grant routinely met with people who were considering the surgery to share his experience. He said he was passionate about his work. His role developed over time and got busier. Initially, he dropped by the hospital if he was asked to attend, and later, when Dr Al Muderis launched his clinics, he was asked to, and did, spend the whole day at the clinics. Beyond the clinic, Mr Grant did other things in his patient advocate role at least once a week. According to Mr Grant, there was no set schedule. He would speak to patients or prospective patients at Dr Al Muderis’ rooms, at the hospital or over the phone. Dr Al Muderis would also send patients to Mr Grant’s gym, and Mr Grant would speak with them there. Mr Grant’s evidence was that sometimes he was asked to help entertain someone at dinner.
391 He travelled around Australia with Dr Al Muderis, speaking together at conferences, clinics and groups of interested persons. Eventually, he was travelling overseas with the Osseointegration Group of Australia associated with Dr Al Muderis’ practice eight to ten times a year. On two to three occasions when Dr Al Muderis did not attend (for example, due to a missed flight), Mr Grant was required to present Dr Al Muderis’ part of the presentation, even though he had no medical background, which he felt uncomfortable about. Although that was denied by Dr Al Muderis, I accept Mr Grant’s account. Mr Grant’s travels included trips to the United States, at least until Mr Hernandez was employed, at which point it became his responsibility.
392 In cross-examination, Dr Al Muderis distanced himself from Mr Grant and downplayed his role. He denied that he requested Mr Grant: be a patient advocate; to speak to people; or to attend the clinics. He said it was Mr Grant who requested the title of “patient advocate” and he just voluntarily attended clinics in his free time, without being asked to do so. He also said that the number of trips Mr Grant attended with him was exaggerated, and he travelled in accordance with an arrangement between Mr Grant and the company EndoExo ExoFix Pty Ltd (EndoExo Company), Mr Mark Whelan’s company. He said he had no details about that arrangement, and he never spoke to Mr Grant about his financial circumstances. His evidence was that Mr Grant shared his experience as a patient and was “not talking him up”. Dr Al Muderis said that as a patient advocate, Mr Grant was to share his experiences – “the good, the bad, the ugly” – and that Mr Grant had had several complications. However, that does not accord with Mr Grant’s evidence, who said he had few issues.
393 As to the nature of his role and the circumstances in which it arose, I accept the evidence of Mr Grant. His evidence on this and other topics, in respects, is supported by others. Dr Al Muderis’ evidence is implausible. As foreshadowed earlier, Mr Grant’s evidence concerning his role, and the basis on which he undertook that role, are not “small things that he misremembered”.
394 Second, although Mr Grant gave evidence that Dr Al Muderis never told him what to say to a patient, he had been chosen for the role because of his positive experience. He was asked to share his experience with prospective patients. He said the goal was to get people to do the surgery. He promoted the surgery, with Dr Al Muderis as his surgeon. To suggest otherwise, in the circumstances in which this was done, as the applicant did, is implausible. The promotion of the surgery was to prospective patients of Dr Al Muderis.
395 Third, Mr Grant had Dr Al Muderis’ mobile number; he contacted him whenever he wanted to ask him something; and he responded. Mr Grant explained Dr Al Muderis responded quickly in the early days of his practice but became slower over time. Although Mr Grant confirmed Dr Al Muderis responded eventually, Mr Grant explained others in his team also responded. I note that is in the context of his relationship with Dr Al Muderis, where he was part of Dr Al Muderis’ team.
396 Fourth, Mr Grant was not paid anything in his role as a patient advocate for approximately the first two years, but as the demand grew, he approached Mr Whelan (who provided the implants used by Dr Al Muderis, before he used his own implant) in about February 2014 about a consultancy arrangement with the Osseointegration Group of Australia. They discussed Mr Grant being paid a commission for implants where patients whom he had spoken to had gone ahead with the osseointegration surgery. Those discussions of Mr Grant’s role evolved. While travelling with Mr Whelan and Dr Al Muderis, they would discuss the fact that the manufacturing implants business was growing. He said he would sit next to Dr Al Muderis on flights who would say things to him such as “this is going to be really big” and “we want you to be a part of this”, and “we can pay you a commission and you can have an interest in the business”. At this time in 2014, there was a draft consultancy agreement between Mr Grant and the EndoExo Company which contemplated paying Mr Grant a commission of $2,500 per implant for each patient who went ahead, but it was never signed. He was adamant in evidence that he spoke to Dr Al Muderis about these arrangements, that there were “a lot” of discussions with him, and it was clear to him that it was Dr Al Muderis who was the ultimate decision-maker. From his perspective, during his time, Dr Al Muderis was the “boss of the Osseointegration Group [of Australia]”.
397 Mr Grant said he became frustrated as the negotiations dragged on. Eventually, there was an agreement to pay him $500 each time he attended a clinic. He said he was told that by Mr Nick Birbas, who he understood was Dr Al Muderis’ lawyer. Mr Grant said Dr Al Muderis told him that he covered the cost of his implant in exchange for being a patient advocate. Mr Grant considered that misleading because although Dr Al Muderis did not charge him any out-of-pocket costs, his insurer still paid Dr Al Muderis for his surgery. He elaborated:
He goes around saying that he does the surgery for free, but we’re in a country where the private health pays for it. So he gets seventy-something thousand dollars from HCF or Medibank or whoever. Maybe he might not charge his surgery fees over – over the two or three grand or whatever it is, but he still gets paid. More – with mine, it was maybe a little bit different, because, as you said, you know, it was – he – I don’t know who owned the implant back then, but HCF, from what I’m aware, paid someone for something.
398 I accept Mr Grant’s evidence of his interactions with Dr Al Muderis in relation to attempts to negotiate a financial arrangement, and the reasons why he pursued it with Dr Al Muderis. I note also that, as discussed elsewhere, there was a commission paid to Mr Hernandez, of which Dr Al Muderis was aware.
399 Fifth, Mr Grant said that in the early days, Dr Al Muderis assessed fewer patients as being suitable for osseointegration. However, by the end of his time with Dr Al Muderis in about 2017, Mr Grant’s impression was that Dr Al Muderis would say that almost anyone was suitable for the operation. He said he could see the pool of prospective patients Dr Al Muderis was advising included smokers, diabetics, elderly patients and severely overweight patients, when previously that had not been the case. He accepted that for overweight patients they were told they should lose weight, but even if they did not, the surgery still went ahead. (I note Dr Al Muderis’ evidence is that he would advise a patient to lose weight, but he cannot “dictate to the patient what to do”, with the implication being the surgery goes ahead nonetheless.) Mr Grant’s experience is based on what he saw as a patient advocate, the types of patients in the waiting rooms, and in the Osseointegration Facebook group. A consideration of the patients in the case studies supports this. In addition to Mr Grant, there is also evidence from other witnesses that Dr Al Muderis’ selection criteria broadened over time, from Dr Al Muderis himself, Dr Doshi, Dr O’Carrigan, and Dr Tetsworth.
400 Mr Grant also maintained hearing Dr Al Muderis say to patients “you’ll be back, you have no other option, you have nowhere else to go”, particularly to the American patients. Mr Grant gave evidence that Dr Al Muderis gave patients a lot of hope that their surgery would be successful. He said Dr Al Muderis said things like “we’ll make you walk” or “you’ll be up in no time”. Mr Grant saw him say to patients at international conferences words to the effect that it was a “no brainer” that they needed this surgery. He denied that evidence was incorrect, and although he accepted in cross-examination that he could not recall the name of a particular patient whom Dr Al Muderis had said this to, he was clear that Dr Al Muderis said it quite often. Again, there is other evidence which is consistent with this both as to Dr Al Muderis saying to a patient that they would be back (e.g. Ms McIntyre), and the positive statements he says to prospective patients that he will make them walk (see [2264] and discussion in sting 2, Part 7).
401 Sixth, Mr Grant said he observed Dr Al Muderis treat his staff terribly and explained that this was the norm, not the exception. He witnessed Dr Al Muderis’ bad treatment of staff from the very beginning and reiterated this in cross-examination. His evidence was that Dr Al Muderis was never polite to his staff and would not talk to them like he would talk to other people. He said he witnessed many instances where Dr Al Muderis yelled and abused staff, particularly female staff. Mr Grant rejected the suggestion that Dr Al Muderis did not particularly target female staff, explaining that he saw Ms Belinda Bosley (who previously worked as Dr Al Muderis’ clinical and research coordinator and business manager, as well as his pre-operative nurse surgical assistant) and other staff cry on multiple occasions. Mr Grant confirmed Ms Bosley would also yell at Dr Al Muderis, describing their behaviour as “very unprofessional, the pair of them … It was always about the work context, like, something she was doing wrong or something”. He detailed examples of the conduct. Mr Grant said Dr Al Muderis’ behaviour exacerbated over time. Dr Al Muderis denied this conduct in relation to his staff. I will return to this below, suffice to say at this stage, I accept Mr Grant’s evidence. It is supported by other evidence.
402 Seventh, as referred to above, Mr Grant stopped working with the Osseointegration Group of Australia in 2017. He deposed that one reason for this was because of the issue about payment. Mr Grant explained:
… ultimately, we couldn’t come to an agreement, … I felt used. I felt let down, because … I did think of him as a friend first and foremost. Yes, [Dr Al Muderis] was a surgeon but – but also a friend, and they promised me all this stuff … I’m happy to do things for free, but then there has got to become a time … the contract … that never came from me. That came from them. I didn’t stipulate three per cent or – or – or a dollar figure. I didn’t stipulate nothing. They did all that. So they led me to believe there was going to be a great future in this with them, and … I felt like I was just getting dragged along. … it wasn’t all about the money. It was about helping the patients … There was many factors. … but that was a big part of it – was because we couldn’t come to an agreement.
403 He also said he thought the team was run poorly. He felt that Dr Al Muderis had grown a huge ego, which became worse over time as he became wealthier and more famous. When challenged in cross-examination, he explained:
it was definitely not what it was in the first couple of years … as he grew as a personality, things started changing, and the culture changed. It wasn’t a type of environment, obviously, I wanted to work along, but, like I said, when Solon come along and I was told that I don’t have to … deal with anybody other than Solon, that’s when I was excited, because like I said, I felt Munjed … was going the wrong way… and then that sort of all unfolded again …
404 He described it as being like the “Munjed show”, with the surgery coming second. Based on his observations of patients, he did not like the way Dr Al Muderis was pressuring patients, referring particularly to those from the United States.
405 Mr Grant said he believes Dr Al Muderis is giving osseointegration a bad name because he does not deliver the great experience that osseointegration is capable of bringing patients. When challenged, Mr Grant conceded that was “not 100% of the time”, but he thinks it is a true statement. He explained:
… there’s a lot of surgeons that won’t work with him, so it makes it difficult for us as a whole [and] me personally to grow the brand of osteointegration, to be able to reach patients. My goal is not to give everyone an implant that needs it, or make money. My goal is to … have it … available in the public system, which we did, and be able to have people in Australia who may be able to have access to great medical benefits that they can’t afford …
406 Mr Grant’s evidence included the difficulties that he said have arisen in relation to Dr Al Muderis’ patients using his connectors and adapters (instead of those used by Dr Al Muderis). Mr Grant understood that Dr Al Muderis told patients not to use the parts he was selling as it voided their warranty. This is supported by other evidence, for example, Facebook messages from patients of Dr Al Muderis. His evidence is that a number of health professionals and patients will not use his product, for fear of going against Dr Al Muderis. I note that this is the connector that was used by Mr Smith which caused the issue with Dr Al Muderis, described by him in his case study: see Part 6, Section 7.
407 Eighth, Mr Grant gave evidence of his perception of the conflict of interest which occurs when a doctor owns the implant he is promoting and using in surgery. As he described:
if I own the product and I’m also inputting the product in – morally, you’re not supposed to … a surgeon shouldn’t own a product that they’re putting in because at the – the end of the day they could potentially not do what’s best for the patient, [but] do best what’s for their bottom dollar.
408 This is in the context where Mr Grant said that during the discussions of his position, Dr Al Muderis told him that he himself could not own an interest in an implant or a company as a surgeon, which Mr Grant said he believed.
409 It is permissible for Dr Al Muderis to own the part (the implant), provided it is declared to patients. However, as noted elsewhere, ownership of rights in the implant has the capacity to compromise the integrity of a patient’s decision about whether to have osseointegration surgery. Owning the product may also act as a disincentive to inform patients of alternatives to the surgeon’s proprietary implant.
Mr Fred Hernandez
410 Mr Hernandez lives in the United States and was an osseointegration patient of Dr Al Muderis. He underwent the surgery in April 2013. Following his surgery, Mr Hernandez became a promoter of Dr Al Muderis’ services in the United States, however, the capacity in which he did so was an issue of dispute in the trial.
411 His affidavit was read in the proceedings, however, the applicant did not require Mr Hernandez for cross-examination, having reached an agreement with the respondents that, in such circumstances, they would not take a Browne v Dunn point, on the applicant’s failure to do so. This occurred in a context where an application was made by the respondents for him (and certain other persons) to give evidence by AVL. The applicant submitted that the Court cannot be satisfied that any of Mr Hernandez’s evidence is a genuine attempt at recollecting events that actually happened. He also contended that Mr Hernandez’s evidence is a fiction devised to advance his commercial and emotional goals, such that no weight should be placed on his evidence unless it is an admission against interest or corroborated by reliable evidence. Not cross-examining Mr Hernandez was a forensic choice the applicant made. However, the Court is left to assess his evidence. That Mr Hernandez has not been given an opportunity to address the allegations that the applicant makes, is relevant to assessing his evidence.
412 In the Broadcast, Mr Steinfort asked Dr Al Muderis about Mr Hernandez and whether he had paid people to recruit patients for him – to which Dr Al Muderis responded: “No. That’s not the case” and “I don’t have to do that, Tom”. This led to the following interaction in the Broadcast:
Mr Steinfort: What about Fred Hernandez? Was he paid to try and recruit patients for you?
Dr Al Muderis: No. That’s not true.
Mr Steinfort: It’s not true?
Dr Al Muderis: Definitely not true. I mean – look, honestly, this is not true. I mean Fred is just a piece of work. Anyway – Tom, why would I do that? Why would I do that? I have patients – like, we’re choked with patients. We can’t even – we can’t even do our day to day work and – in – in a sensible way. We try to provide safe practice and I don’t have enough hours in the day to function.
413 The above extract relates to Imputation [13.29] which alleges that Dr Al Muderis lied to 60 Minutes about paying people to recruit patients for him (and Imputation [16.19] which alleges Dr Al Muderis lied about paying commissions to Mr Hernandez).
414 Further on this topic, during the interview (as part of the raw footage transcript but was not included the Broadcast), Dr Al Muderis also denied that Mr Hernandez received any financial incentive for referring patients to him, saying his job was merely to provide parts and distribute components to patients in the United States stating, inter alia, that Mr Hernandez “had no links to [him] as a surgeon”. Dr Al Muderis said Mr Hernandez worked for Osseointegration International, the manufacturing company.
415 As will be addressed further below, Dr Al Muderis’ evidence on the topic of his agreement and involvement with Mr Hernandez was inconsistent.
416 The applicant’s closing submission was scathing of Mr Hernandez, as were Dr Al Muderis’ comments in his interview with Mr Steinfort, where Dr Al Muderis referred to Mr Hernandez as “a piece of work”. He submitted that:
Mr Hernandez has waged a campaign of denigration against Dr Al Muderis, initially borne out of a breakdown in their business relationship and later exacerbated by Dr [Al] Muderis’ successful lawsuit against Mr Hernandez …
…
Mr Hernandez has influenced a number of witnesses in these proceedings to give adverse evidence about Dr Al Muderis.
417 It is appropriate at this stage to look at other aspects of his evidence, although the allegations in relation to Mr Hernandez are further addressed below in considering the patient case studies.
Background
418 Mr Hernandez had osseointegration surgery with Dr Al Muderis in 2013. It is unnecessary to refer to all of Mr Hernandez’s evidence as to how this came about. In short, he explained he was interested in having osseointegration surgery but could not afford it. He said as a result he sent a proposal to various surgeons in February 2012, including Dr Al Muderis, to the effect that he would actively promote osseointegration technology at a grassroots level on a full-time basis in the United States in exchange for complimentary osseointegration surgery. Mr Hernandez also said he emailed a link to his website to Dr Al Muderis’ email address. He said he was subsequently contacted by Ms Bosley, followed by a call from Dr Al Muderis, saying he would be in San Francisco for a conference, that he liked Mr Hernandez’s website and that he had described Dr Al Muderis on the website as a “pioneer of osteointegration”. In late February 2012, Mr Hernandez sent a proposal letter to Dr Al Muderis. In the letter, Mr Hernandez wrote:
My objective is to not only obtain the implant but to engage in a partnership with Osseointegration Group of Australia to bring awareness to their Endo-Exo technology here in America. I believe there is an opportunity for the company to engage in a grassroots campaign here in the states. By doing so, it will not only ensure brand recognition once FDA approval occurs but will increase sales of their product by bringing awareness to the amputee and general public. I am more than prepared to actively promote this technology full time.
…
I propose Osseointegration Group of Australia sponsor my implant surgery and engage in a partnership to bring awareness to the general public in America; by participating in large media events and engaging the public sector on a personal level. This level of awareness can be achieved by simple but effective means by profiling the technology and more importantly the company’s product at major events. …
…
This type of grassroots campaign would not only bring awareness to osseointegration technology but more specifically allow Osseointegration Group of Australia’s product to be the first name that comes to mind when Americans hear about implant technology. …
…
Garnering interest in America will bring an increase in sales by motivating amputees to obtain the surgery. Osseointegration technology is a life changer and once amputees see the implant for themselves, they will do whatever it takes to obtain it.
419 In around early January 2013, Mr Whelan telephoned Mr Hernandez in response to the proposal letter and said words to the effect of:
… last year we weren’t ready, but now we are and we want you to put on a couple talks in Los Angeles, one oriented at patients and one oriented at medical professionals, we want to meet you in Los Angeles.
420 In or around early January 2013, Mr Hernandez met Mr Whelan in Los Angeles at a hotel, who at the meeting said words to the effect of: “We want you to give these talks” and:
we want you to market for us and promote us on social media and blog about your journey through osseointegration surgery to raise Dr Al Muderis’s profile and the profile of the Osseointegration Group of Australia (OGA) in North America primarily.
According to Mr Hernandez, there were discussions about what the work with them would entail. Mr Hernandez’s evidence was that in liaison with Mr Whelan, he assisted with the organisation of a conference in Los Angeles in February 2013. At the conference he also met and spoke to Dr Al Muderis, Ms Bosley and Mr Grant. He said that when they were all out socially having drinks at the bar, Dr Al Muderis verbally agreed to provide osseointegration surgery to him, saying words to the effect of: “Come to Australia and I will do the surgery for you”. Also at the bar, Mr Whelan said words to the effect of: “We will pay for your surgery and accommodation in Australia for your promotion of OGA [Osseointegration Group of Australia] and Dr Al Muderis”. Following this, Mr Hernandez emailed back and forth with Mr Whelan and Ms Bosley about plans to come to Australia. In or around March 2013, Mr Hernandez flew out to Australia for osseointegration surgery with Dr Al Muderis.
Arrangements with Dr Al Muderis
421 The applicant’s case is that Dr Al Muderis had nothing to do with the arrangements in relation to Mr Hernandez’s surgery, and the circumstances in which he began working for them. He said all the arrangements (including what occurred after surgery) were organised with Mr Whelan, and later Osseointegration International. The applicant submitted he was not involved in any way, and did not know of or approve the arrangements. He contended that the suggestion of being party to the arrangements is implausible and made up by Mr Hernandez to hurt Dr Al Muderis.
422 I do not accept that submission. The evidence establishes that in practical terms, Dr Al Muderis was involved. As with Mr Grant, Mr Hernandez understood that it was Dr Al Muderis making the decisions. That is hardly surprising as what was being promoted by each, was osseointegration surgery to be performed by Dr Al Muderis. There is also email evidence which makes Dr Al Muderis’ involvement clear( e.g. an email dated 6 June 2013 from Mr Hernandez which states that Mr Hernandez had discussed with Dr Al Muderis plans for the United States).
423 Mr Hernandez’s evidence was that Dr Al Muderis and Mr Whelan were working together on this enterprise, with Mr Whelan undertaking the business side. He said that in the period that followed his surgery, he received a monthly pay and a commission for each patient that he referred to Dr Al Muderis to have surgery. In 2015, he was told by Mr Whelan that a new company would be taking over the payments to Mr Hernandez. In April 2015, Dr Al Muderis’ lawyer and CEO of Osseointegration Group of Australia and Osseointegration International, Mr Birbas, became involved and arranged a written contract. An email from Mr Birbas to Mr Hernandez dated 7 April 2015 included the following:
I will be speaking to Munjed over the next few days and I am aware that you are an important part of our team so I will be suggesting we formalise a contract for your services. Can you please advise of your rates you are currently charging, the description of the work you will be performing and I can then discuss it with Munjed and include in the contract. I can then get a draft contract over to you during the course of next week.
424 Dr Al Muderis was copied into this email (as were Ms Bosley and Mr Whelan). Mr Hernandez was also told in this email to send his invoices to Mr Birbas and that those invoices should be made out to Osseointegration International. In a later email exchange dated 8 April 2015, Mr Whelan, Mr Birbas and Mr Hernandez emailed back and forth about invoices and payment owed to Mr Hernandez. Dr Al Muderis was copied in this email chain. There is documentary evidence which supports Mr Hernandez’s evidence, including a contract (discussed below), invoices and emails. I also note in relation to an email sent by Mr Whelan on 19 March 2015 where he tells Mr Hernandez “[t]he new company is taking over the payments to consultants”, the applicant submitted that there was nothing in that email to suggest that the payments were commissions. Given the circumstances in which the payments were made, the compelling inference given the evidence, is that they were commissions. That description is apt.
425 Although much of the written documentation is with Mr Whelan and then Mr Birbas, I am satisfied that Dr Al Muderis was aware of, and involved in, the arrangements (and knew the basis for it). Mr Birbas was Dr Al Muderis’ lawyer, and to state the obvious, would have been working under his instructions and with his approval.
426 At the time of the breakdown of the relationship in August 2018, in email exchanges between Mr Hernandez, Mr Birbas and Dr Al Muderis, Mr Hernandez made his position clear. One email in this exchange, which was addressed specifically to Dr Al Muderis, included:
Moving forward, I am happy to continue to work for OGA but only under a specific contract that details what my duties are and under clear guidelines. … As there are a lot of unhappy patients out there and I hear from them all on a regular basis. Your reputation in the U.S. is not getting any better and I am finding it more and more difficult making excuses for your behavior and lack of patient follow up. I don’t think you have any idea of how many people are unhappy with the level of service coming out of Sydney; other than the nursing staff and physio team.
…
Look, anyone can show up at a booth and say, hey look at my implant but not everyone can do what I do and have done in this industry. Personally I feel confident that I have done an excellent job for you over the last five years. I know you probably feel differently but no one in the U.S. really knew who you were before I started creating and building up this persona and hitting the marketing aspect hard. Before me, you couldn’t find the subject of Osseointegration in the social media world; let alone any information on you and the OGA team.
427 This was Mr Hernandez’s state of mind at the time. Irrespective of whether his position was correct, Dr Al Muderis was put on notice that this is what Mr Hernandez perceived the position to be in relation to his patients who had returned to the United States after surgery. It is a contemporaneous statement which reflects his view of the role of Dr Al Muderis, and the nature of his relationship with him. This was in reply to an email from Dr Al Muderis which included the statement: “I thought we had an agreement in Tuscon which appeared in my view to be working well – I need to know what has changed?” Again, this reflects Dr Al Muderis’ relationship with Mr Hernandez, which is consistent with Mr Hernandez’s understanding, that is, that there was an agreement as to their dealings (which Dr Al Muderis was aware of). Nonetheless, the email written by Mr Hernandez was on the basis that he still wished to do business with Dr Al Muderis. Mr Hernandez’s agreement was terminated, according to an email from Mr Birbas (in the same email chain, with Dr Al Muderis copied), on the basis that he had reached out to a competitor which was in “direct conflict to [Mr Hernandez’s] obligations under our agreement”. That is, it was said he breached the exclusivity clause which was part of his agreement with Dr Al Muderis and Osseointegration International.
428 The applicant’s submission is that Mr Hernandez was working for Mr Whelan and the EndoExo Company (i.e. the implant company, not Dr Al Muderis). However, when Dr Al Muderis set up Osseointegration International, Mr Hernandez, as an “important part of [Dr Al Muderis’] team”, went with him. That is, Mr Hernandez continued to perform his role, but through Osseointegration International. That is because his role related to Dr Al Muderis. Mr Hernandez continued his role, even though the implant being promoted at that stage was not that used in his own surgery, but Dr Al Muderis’ design. Further, as to Mr Hernandez’s role, he was referred to by Ms Roberts and others in written communications as their “representative” (including in the August 2018 email to patients at the time of the breakdown of Mr Hernandez and Dr Al Muderis’ relationship). As at that time, Mr Hernandez’s email signature referred to himself as the “US Operations Manager, Osseointegration International”. As discussed elsewhere, his role included: the promotion of Dr Al Muderis’ surgery on social media and at meetings/conferences; preparing and distributing promotional brochures and flyers (including for Dr Al Muderis’ upcoming conferences); organising booths at conferences; and meeting and liaising with (prospective) patients. His evidence on these activities is supported by other evidence, for example, the email exchange referred to above in Ms Roberts’ section in Part 5, Section 5, in relation to the organisation of a clinic in New York.
429 As evident from the discussion above, Mr Hernandez’s evidence is supported by documentary evidence (e.g. the invoices sent by Mr Hernandez, the draft contract and emails).
The terms of the arrangement
430 It will be recalled that Mr Birbas wrote to Mr Hernandez about formalising a contract: see [423] above.
431 Dr Al Muderis had an ongoing and mutually beneficial financial relationship with Mr Hernandez from around April 2013. As Mr Hernandez described, there was a written contractual relationship from May 2015. Although the contract in evidence is signed only by Mr Hernandez, as illustrated above, it is clear there was an agreement to that effect between the parties.
432 The contract was stipulated to be between Osseointegration International (The Practice) and Mr Hernandez (Contractor). Osseointegration International, albeit a subsidiary to a chain of companies in a corporate structure, is Dr Al Muderis’ company. His partner, Ms Roberts, is the current director and secretary, and he is the sole shareholder. At the time the contract was entered into with Mr Hernandez, Dr Al Muderis was one of two directors of Osseointegration International, the other being his lawyer, Mr Birbas.
433 The terms of the contract are clear: Mr Hernandez, as an independent contractor, was entitled to and paid a service fee of US$3,500 per month, and a commission of US$1,000 for every patient he refers that purchases an implant by “the Surgeon”. “Surgeon” is defined as Dr Al Muderis. It was an agreement that exclusively benefited Dr Al Muderis given only Dr Al Muderis was identified and defined as “the Surgeon”. The recitals to the contract stated that the “Contractor agreed to provide services to the Practice and the Surgeon” in return for payment. The agreement stipulated that Mr Hernandez was to provide his services to assist Osseointegration International and Dr Al Muderis (as the named surgeon). Among other clauses, the agreement included that its terms were to be kept confidential (cl 15.3) and Mr Hernandez was not permitted to disclose the business interests of Osseointegration International or Dr Al Muderis (cl 15.6). A plain reading of the clauses reiterates that it prevented Mr Hernandez from disclosing to patients that he was receiving a commission on the sale of implants he was promoting to them. That is, the prospective patients who contacted Mr Hernandez for assistance, information or advice, under the terms of the agreement could not be told that he would receive a commission if they agreed to undergo the surgery. In effect, Mr Hernandez could not tell them he was paid to promote the surgery, and Dr Al Muderis.
434 In around July or August 2016, Mr Hernandez renegotiated the base salary for the service fee to US$5,000 per month, plus the commission. His evidence is this negotiation was with Dr Al Muderis in person. In these proceedings, Mr Hernandez produced invoices he issued to Osseointegration International from June 2015 to May 2017, which reflect: the fee terms of the agreement; the increase to US$5,000 as “approved by Munjed” (as recorded on the invoice of 1 July 2016); and the patients he obtained commission for after they had surgery with Dr Al Muderis, including Ms Schaeffer, Ms Koolhoven and Ms Ulrich (each a witness in these proceedings). They were three of the many patients referred to in the invoices for which Mr Hernandez received a commission.
Dr Al Muderis’ evidence in relation to Mr Hernandez
435 Dr Al Muderis was cross-examined on the terms of the contract between Osseointegration International and Mr Hernandez. His answers were unsatisfactory. Dr Al Muderis said the “contract [with Mr Hernandez] came to [his] knowledge in the 60 Minutes” program. He said he had not read the contract before then. As alluded to earlier, on several occasions in cross-examination, Dr Al Muderis said he did not understand the contract, and that “I’m not a qualified person to put a contract or make a contract or understand the contract”. I do not accept that evidence or that he regarded himself in that position, but rather it was entirely disingenuous to suggest that he could not understand the contract. This was an answer given to avoid admitting his understanding of the meaning of the plain terms of the contract. Dr Al Muderis’ cross-examination in relation to the contract was not just evasive, it was false.
436 Dr Al Muderis’ answers after being taken through the contract in cross-examination are telling of his disingenuous attempts to distance himself from the arrangement:
Dr Collins: That was your understanding of the nature of the agreement?
Dr Al Muderis: Yes. But that doesn’t specify – it’s contract to provide services for – it could be many surgeons.
Dr Collins: Well, you see it’s:
…to assist the practice and the surgeon.
You see that?
Dr Al Muderis: Yes. But he was – my understanding, that he was paid for – commission to any surgeon. So if he sell in America, he get a commission for that. He sell in Canada, he get commission for that. If it’s in the UK, he gets commission for that. So it’s not specific to one particular surgeon.
Dr Collins: Yes. You see, Doctor, you know that’s not true, don’t you, because you know that the term “the surgeon” in this agreement is defined to mean you and you alone?
Dr Al Muderis: That’s not true.
Dr Collins: All right. Can we go to the next page, please? You see the definition of surgeon under [cl 1.1(n)] ... surgeon means you?
Dr Al Muderis: Yes. But I – okay. I can see that.
Dr Collins: Yes. Well, that was – this was an agreement to provide services to Osseointegration International and to you personally, wasn’t it?
Dr Al Muderis: Well, I don’t – I don’t understand that but that’s what I can read here now.
437 As evident from the discussion above of the work that Mr Hernandez undertook, it was consistent with the terms of the contract. He was promoting the surgery and Dr Al Muderis as a surgeon.
438 Dr Al Muderis denied the obvious in evidence to maintain the position he stated to Mr Steinfort, that he had no links to Mr Hernandez and did not pay people to recruit patients for him. Given the evidence, it is apparent he denied it in the interview because it reflected adversely on him. The statement to Mr Steinfort that Mr Hernandez “had no links to [him] as a surgeon” was false. The evidence shows that Dr Al Muderis had an ongoing and mutually beneficial financial relationship with Mr Hernandez from around April 2013 until 2018 (when the relationship broke down). I also do not accept Dr Al Muderis’ answers in cross-examination that only Mr Birbas was aware of and negotiated the contract with Mr Hernandez. This was another attempt to distance himself from Mr Hernandez.
439 When the relationship broke down, Dr Al Muderis said he spoke to Mr Hernandez complaining he was selling products other than those produced by Osseointegration International to others, which was in breach of the exclusive nature of the contract. Dr Al Muderis gave evidence that by doing so, Mr Hernandez was contravening the agreement to represent Osseointegration International. It follows, that Dr Al Muderis must have been aware of the terms of the contract as at the date of the confrontation with Mr Hernandez in 2018. It is timely to recall that Dr Al Muderis later said in cross-examination that he had not read the contract before the Broadcast on 6 September 2022.
440 Dr Al Muderis’ evidence that Mr Hernandez was paid a commission on the sale of the implant, rather than to recruit patients for him, is artificial. It is an artifice set up likely to distance himself. It does not reflect the nature and reality of Mr Hernandez’s role (as supported by the evidence discussed above). Mr Hernandez liaised with patients and promoted Dr Al Muderis – not to sell them an implant – but to have them undertake the surgery. As his invoices reflect, after they had surgery, he was paid a commission. Dr Al Muderis denied that he paid people to recruit patients for him. That was the arrangement Mr Hernandez had with Dr Al Muderis since 2013 until it was terminated in 2018. Dr Al Muderis’ evidence was plainly false.
441 Although I addresses to the stings below, I am satisfied that Imputations [13.29] and [16.19] are substantially true – that Dr Al Muderis lied to 60 Minutes about paying people to recruit patients for him and about paying commissions to Mr Hernandez.
Other evidence
442 There are some further observations to be made about Mr Hernandez’s evidence.
443 First, Mr Hernandez’s evidence is not to be considered in isolation. Dr Al Muderis also sought to distance himself from Mr Grant and Ms Stewart on the basis it was not him but Mr Whelan who made any arrangements with them as to their respective roles with Dr Al Muderis. As discussed there, I do not accept the submission for either of them.
444 Second, there are some similarities with the evidence in respect to Mr Hernandez and Mr Grant. Mr Grant gave evidence of undertaking a role as a patient advocate predominantly in Australia and for some time internationally, and of his interactions with Dr Al Muderis (including in relation to discussions concerning a financial agreement). As explained elsewhere, Dr Al Muderis said that Mr Grant travelled by an arrangement with the EndoExo Company, Mr Whelan’s company. Dr Al Muderis said he had no details about that arrangement, and he never spoke to Mr Grant about his financial circumstances. However, I have found that: Mr Grant spoke to Dr Al Muderis about these proposed financial arrangements; there were “a lot” of discussions with him; and it was clear to him that it was Dr Al Muderis who was the ultimate decision-maker. Mr Grant’s evidence was that by talking to prospective patients about his experience, his goal was to get them to have the surgery with Dr Al Muderis. Mr Grant was eventually paid $500 for each clinic he attended. Dr Al Muderis told him that he had covered the cost of Mr Grant’s implant in exchange for him being a patient advocate, as the basis for not remunerating Mr Grant for his role.
445 Third, both Mr Grant and Mr Hernandez were submitted to be part of the concoction allegation. As explained elsewhere, the applicant initially alleged this about Mr Grant, only to withdraw it at the end of oral submissions, following a question from the Court. It had been suggested that a cohort of patients changed their evidence after they had dealings with Mr Grant. Nonetheless, this reflects the preparedness of the applicant to make such serious allegations blaming others, where it appears there is no basis. Although, the same submission was made about Mr Hernandez, he has not had an opportunity to respond, because of the applicant’s decision not to cross-examine him. It is said that the description of Mr Hernandez’s conduct is apparent from his electronic communications with various people. It can readily be accepted that Mr Hernandez strongly dislikes the applicant and the basis for that is obvious (after the relationship was terminated, Dr Al Muderis sued Mr Hernandez for allegedly making false and misleading statements concerning Dr Al Muderis, Osseointegration Group of Australia and Osseointegration International, where Dr Al Muderis then obtained summary judgment against him for US$2,610,000). However, the communications do not support the applicant’s submission. That he may have given names of patients to Ms Grieve to assist her investigation does not support the submission. To the contrary, asking witnesses to come forward and speak of their experiences is not inappropriate, and does not support a submission that their evidence is fabricated. It is also in a context where shortly prior to the termination of his agreement in 2018, Mr Hernandez said to Dr Al Muderis that many people were unhappy with his care. The patient witnesses alleged to have been part of the cohort that concocted complaints about Dr Al Muderis (e.g. Ms Schaeffer, Mr Bruha and Mr Ladouceur) denied the assertion.
446 Finally, the submission that Mr Hernandez influenced a number of witnesses in these proceedings to give adverse evidence about Dr Al Muderis is addressed below. Suffice to say, as just observed, it may be accepted that Mr Hernandez holds strong views against Dr Al Muderis. It may also be readily accepted the language Mr Hernandez used in private exchanges with others (e.g. Ms Schaeffer and Mr Grant) while watching these livestreamed proceedings on YouTube was unpleasant. However, the evidence of his communications with others does not support the applicant’s assertion. There is no suggestion in any of the material before the Court that he influenced anyone to give false evidence. Rather, in his messages with Mr Grant in September 2023, Mr Hernandez speculated about what he might be asked about in cross-examination and said “[i]t’s all truth anyway”, to which Mr Grant replied “[i]f you just say the truth you got nothing to hide”. I return to this topic below.
Ms Shona Stewart (formerly Wilmot)
447 Ms Stewart is a former employee of Dr Al Muderis. She featured in the Publications, where she alleged unethical practices by Dr Al Muderis including high-pressure sales tactics, inadequate patient selection and aftercare, and an abusive workplace culture.
448 Ms Stewart was a generally honest witness, albeit aspects of her evidence were rather unsatisfactory. I do not accept the applicant’s submission that her evidence was fabricated. Her evidence on some significant topics is supported by other evidence.
449 Ms Stewart’s evidence was that she met Dr Al Muderis in 2013 and by 2014, had worked with him as a nurse employed at Macquarie University Hospital. She commenced working for him in about January 2015 as an “Osseointegration Coordinator”. She explained that she was “effectively a nurse” in that position as well as a “patient liaison”:
I helped patients in their journey from when they first approached the clinic, through their initial consultations with Dr Al Muderis, through surgery, and then in their aftercare.
450 She resigned on 20 March 2017.
451 Ms Stewart’s evidence was that she was in a relationship with Dr Al Muderis from around December 2013 until late 2015 or early 2016. She said it ended amicably. The applicant submitted that there was only a one-off sexual encounter with Ms Stewart, in 2013. He submitted that she was initially employed by Mr Whelan in a non-clinical role, and it was not until mid-2016 that Dr Al Muderis employed her to work in the clinic as a nurse. He submitted that Ms Stewart resigned in March 2017 to work closer to home. Apart from being directed to Ms Stewart’s credit, I assume this submission is to limit the time Ms Stewart was said to be exposed to Dr Al Muderis.
452 The documentary evidence establishes that Ms Stewart was offered the Osseointegration Coordinator position on 16 January 2015, which she agreed to commence in February 2015. Although the covering email is from Mr Whelan, it copies Dr Al Muderis, and it is apparent from the face of the email that the discussion and agreement as to salary was a separate conversation between the three of them. She was to be working with the “OI team”. Ms Stewart said that she was initially paid by the EndoExo Company but was under the direction of Dr Al Muderis. That she was under his direction is supported by the terms of the agreement that she “attend all OI clinics and attend the office of A/P Al Muderis 4 days a week and a work from home arrangement as agreed upon with A/P Al Muderis prior to commencement”, as well as the job description:
… [The employee] [i]nteracts with patients … with regard to patient-related issues as directed by A/P AL Muderis … [and] [m]akes decisions … with instructions from A/P Al Muderis.
453 I note that Mr Grant also gave evidence that he understood the relationship between Mr Whelan and Dr Al Muderis was such that Dr Al Muderis was the decision-maker. This also accords with the evidence of Mr Hernandez.
454 I note also that, as apparent from the email described below at [574], in February 2016, at a time before Dr Al Muderis said he employed Ms Stewart, Dr Al Muderis was giving her directions and had been for some time. There are documents which demonstrate that in 2015 and early 2016, she was liaising with and obtaining information from prospective patients who had made inquiries, on behalf of Dr Al Muderis. The applicant’s evidence that Ms Stewart only worked with Dr Al Muderis for around seven months is not supported by the evidence.
455 Ms Stewart said that when Dr Al Muderis discovered she had begun a new relationship in May 2016, he sent her to work at new locations, including where she had no direct contact with him, patients or other members of the team.
456 Ms Stewart’s resignation in March 2017 is also not as simple as the applicant contended. In her letter of resignation, she states:
Over the last few months I feel that my role within the team has not been meeting my professional expectations nor your’s.
457 This is consistent with her evidence of what occurred while working for Dr Al Muderis.
458 Other aspects of Ms Stewart’s evidence, which are challenged by the applicant, are supported by other evidence. To provide several examples.
459 First, Ms Stewart gave evidence that “a big part of her role [with Dr Al Muderis] was sales”. She described being given a spreadsheet on her first day, with a list of prospective patients. Her goal, she was told, was to contact them “to get them to come to the clinic and have surgery”. She explained the spreadsheet had details from online forms completed by prospective patients from all over the world. I note the position description for Ms Stewart’s role included “to assist the business module of the OI team”.
460 As discussed in more detail below, there is other evidence that Dr Al Muderis promoted his business and that he wanted people to undergo osseointegration surgery with him (see e.g. discussion under stings 1 and 6 in Part 7, Section 1). His practice in the United States is an obvious example. Further, Ms McIntrye (a prospective patient) gave evidence that after she had an initial consultation with Dr Al Muderis about osseointegration surgery, she told him she wanted to consider her position. Dr Al Muderis was aware that she was also considering surgery with another surgeon in South Australia. About a week after the consultation, Ms Roberts attempted to contact Ms McIntrye by phone and then by email. Ms McIntyre did not respond. Dr Al Muderis’ evidence was the email was “a standard follow-up for patients who come to the clinic”. I note Ms Stewart’s evidence was that:
Dr Al Muderis said to me on a number of occasions words to the effect “Your job is to get [patients] to come and have surgery.” … If I called a patient and they didn’t answer, Dr Al Muderis made me follow up with an email and a text message to their mobile number.
461 The compelling inference is that Ms McIntrye was contacted as part of the practice’s business model, with the objective of wanting her to agree to having surgery with Dr Al Muderis: see Part 6, Section 2.
462 Second, Ms Stewart gave evidence that Dr Al Muderis and Ms Bosley told her to advise patients to fundraise (i.e. to raise money to pay for the cost of the surgery). She observed that practice occurring and participated in it herself. In evidence is a 2016 email from Dr Melton, a United States-based practitioner. She wrote to Dr Al Muderis of a patient who “may be interested in OI in the future, though funding will be a problem”. Dr Al Muderis replied, “[the patient] is suitable for osseointegration from the X Ray point of view … We may need to start a discussion with the patient to teach him how to do fund raising for his surgery”.
463 Further, as explained below, Ms Ulrich, Mr Bruha and Ms McIntyre each gave evidence that Dr Al Muderis raised fundraising with them. This topic is discussed further below: see Fundraising in Part 6, Section 1.
464 Third, Ms Stewart gave evidence that on Dr Al Muderis’ instructions, she was required to write consultation reports. There is an email in evidence supporting her evidence, which is discussed immediately below.
465 Fourth, Ms Stewart gave evidence that she was poorly treated, bullied and belittled by Dr Al Muderis, and she observed him do that to others (including Ms Bosley).
466 There is evidence of an email in February 2016 from Dr Al Muderis reflecting that behaviour: see email at [574] below. Dr Al Muderis described his comment in the email as a “heated moment”. However, that response is problematic. The email related to a patient’s incomplete initial letter, in a context where Dr Al Muderis’ evidence was that he dictates the letters during or after the consultation. Ms Stewart merely expressed the view in the email chain, an understandable one, that she could not complete the letter (which apparently related to a report of a consultation) because she had not attended the consultation. Dr Al Muderis’ response (“Shona should have done this”) presupposes Ms Stewart should have completed the letter, and her questioning of it drew the abuse that he is “sick of these stupid responses”. That response reflects that he perceives Ms Stewart to regularly give “stupid responses”. It is consistent with her evidence that “[it] was very common for Dr Al Muderis to call me stupid or mock me in front of my colleagues whenever I asked a question”.
467 The email contained gratuitous abuse. It reflects a very low tolerance on his part. It speaks of his attitude towards Ms Stewart. With considerable reluctance, Dr Al Muderis ultimately accepted that the comment was inappropriate.
468 Her evidence as to her treatment is also supported by the evidence of Mr Grant, Mr Hernandez and Ms Schaeffer.
469 Ms Schaeffer deposed that she saw Dr Al Muderis say to Ms Stewart words to the effect of: “are you that stupid?”, “this shouldn’t happen” or “you should have known better”. She said that Ms Stewart “looked miserable”. She felt as though Dr Al Muderis “was being flippant and that he pretended as if he was making a joke but really, he was just being mean towards her”.
470 As already discussed, Mr Grant’s evidence was that Dr Al Muderis treated his staff poorly. He further deposed that Dr Al Muderis yelled and abused staff, and “particularly targeted female staff in this regard”. He explained that Dr Al Muderis treated Ms Bosley especially poorly, and “witnessed physical, mental and emotional abuse between” the two. He gave an example of the two “arguing and throwing food at each other” on a business class flight. As previously discussed, Mr Grant is accepted by the applicant to be a witness of credit, whose evidence I accept.
471 Mr Hernandez’s evidence is to the same effect. He deposed that in Australia and in the United States, he “regularly saw Dr Al Muderis scream at [Ms Bosley] and have her in tears”. He would call Ms Bosley “dumb dumb” and disparage her in public. He would also talk down to Ms Stewart. Mr Hernandez described a culture of fear of standing up to Dr Al Muderis, because he “wielded so much power over our income”. Indeed, the asymmetries are self-evident.
472 Dr Al Muderis’ evidence, addressing their evidence in relation to Ms Bosley, is telling. As previously described, Mr Grant said that he witnessed Dr Al Muderis abusing Ms Bosley physically, mentally and emotionally. He said the disputes were always about work, for example, including things he understood her to be doing wrong. Mr Hernandez’s evidence was to a similar effect.
473 In cross-examination, Dr Al Muderis denied he reduced Ms Bosley to tears on several occasions. At one point, he replied “I have a lot of respect to Belinda Bosley and I never belittled her. Actually, we used to banter all the time”. When put to him that there was an occasion where he and Ms Bosley had a fight on a plane which concluded with a loud argument and throwing food, he replied:
We used to banter, we used to have heated discussions. She used to shout at me. I shout at her back. It’s no dissimilar to what happened on the side of the bar table. We are passionate about what we do, and we witness … heated discussions. That’s not belittling. That’s just because we’re passionate about what we do.
474 What Mr Grant described in evidence is not “banter”, and nor is it what occurs in a courtroom. If Dr Al Muderis considers it as such, he fails to appreciate the nature of his conduct. The applicant’s submission that Mr Grant’s evidence “about the alleged food throwing on the plane demonstrates that the incident was frankly trivial” does not properly characterise Mr Grant’s evidence. Dr Al Muderis plainly had the upper hand in the relationship, as he reduced Ms Bosley (and others) to tears. I accept Mr Grant’s evidence. Ms Stewart’s evidence is to the same effect.
475 The applicant referred to several witnesses whom he called who said they had not observed any bullying (including of Ms Stewart or Ms Bosley), and that the work environment was collegiate. Those witnesses work with Dr Al Muderis in different capacities One of the witnesses is Ms Roberts, who, as I found earlier, gave evidence of what she understood she was to say to assist the applicant’s case (e.g. about whether consultations were conducted in the United States). Other witnesses had little or no overlap with Ms Stewart’s employment. I prefer the evidence of Mr Grant and Ms Stewart (which is supported by the email from February 2016 referred to above) as to Dr Al Muderis’ conduct. It is supported by other evidence.
476 The applicant submitted that Ms Stewart is dishonest as to what occurred because she communicated with Dr Al Muderis between 2019 and June 2022 which shows that she thought highly of him (e.g. congratulating him on receiving the 2020 NSW Australian of the Year award). The submission fails to appreciate the complexities of relationships, noting this relationship traversed professional and personal contexts. One may outwardly admire or care for another while hiding resentment or sadness towards them. I do not regard the matters the applicant relies on as undermining her evidence. In comparing her evidence with the communications the applicant relies on, it is apparent she is grappling with the conflicting emotions borne by her experiences. In any event, there is other evidence supporting her evidence.
477 Fifth, Ms Stewart gave evidence that Dr Al Muderis’ patient selection changed over time to include patients who he had previously excluded. This is supported by the evidence of Dr Al Muderis, Dr Doshi, Dr O’Carrigan, Dr Tetsworth and Mr Grant.
478 Dr Al Muderis’ evidence that studies over time “demonstrate” that outcomes for osseointegration patients with certain conditions are not materially different from patients without those conditions is circular and unfounded. He refers to two published peer-reviewed papers (concerning patients with peripheral vascular disease and, separately, a history of smoking) and one unpublished paper (concerning diabetes).
479 The study relating to peripheral vascular disease involving five transtibial osseointegration patients (after 12 months), published on 20 September 2017, is a study he co-authored. Its conclusion expressly limits its findings (citing, inter alia, the small sample size):
… this study showed that osseointegrated implants can be an effective treatment for transtibial amputees with peripheral vascular … Additional evidence is required to confirm the feasibility of implementing osseointegration surgery as standard care for amputees with peripheral vascular disease.
(emphasis added)
480 A plain reading of that conclusion could not be said to “demonstrate” that outcomes for patients with peripheral vascular disease are not materially different than outcomes for patients without the condition. The unpublished study on diabetic patients similarly concludes “17 patients is not large enough to provide definitive understanding”.
481 I note Dr Al Muderis said Ms Ulrich was a good candidate for transtibial osseointegration in March 2016, despite her having disclosed that she has peripheral vascular disease. He performed the surgery in March 2017.
482 As explained elsewhere, it is difficult to see how some criteria could properly change (see e.g. the Patient X and Mr Ford case studies in Part 6, Section 3).
483 Sixth, Ms Stewart gave evidence that Dr Al Muderis would instruct her to ensure Mr Grant would attend clinics on certain days to speak to patients to share his positive experiences. Mr Grant also gave evidence that Dr Al Muderis asked him to attend certain clinics.
484 Seventh, Ms Stewart gave evidence that Dr Al Muderis wanted his clinic to look busy, because it suggests the surgeon is more successful – or at least gives that impression. She said, to that end, Dr Al Muderis wanted to double-book patients, which she maintained in cross-examination when it was put to her that was false.
485 There are two emails in evidence, each authored by Ms Annie Livingstone (Dr Al Muderis’ practice manager) and sent a few days in advance of clinics to be held on 7 July 2016 and 14 March 2017 to the persons who were to conduct those clinics. The emails detailed the list of patient attendees and identified whether they were new patients or review patients. In the case of the former, appointment times were specified. The documents reflect there were multiple double bookings, and in one case a triple booking. For example, for the 7 July 2016 clinic, there were three new patients listed at 8.00 am, two more at 9.00 am, and another two at 9.45 am. The email reflects there were a total of seven new patients, with a possibility of another new patient (awaiting confirmation) and nine review patients (without appointment times).
486 For the 14 March 2017 clinic, there were 12 new patients listed from 8.00 am to 1.00 pm, with two appointment times being double-booked. There were a further 15 review patients listed to attend for review that day (with no appointment time). Mr Warland (a witness in these proceedings) was one of the new patients double-booked for the 11.00 am appointment. Ms Ulrich also saw Dr Al Muderis that day although she is not listed. This evidence is consistent with Ms Stewart’s evidence, and it is proximate to when she worked with Dr Al Muderis. As expanded upon later in these reasons, the scheduling of appointments as demonstrated in those emails (and on Dr Al Muderis’ estimations (as well as his witnesses’ estimations) of the typical number of appointments he would have during those clinic days), means that there is support for the patients’ evidence as to the brevity of some consultations.
487 Against the above context, it is appropriate to address Ms Stewart’s evidence that on occasions she was directed by Dr Al Muderis to forge prescriptions for pain medication for patients. She explained patients would call Dr Al Muderis, and he would ask Ms Stewart (and others) to write a script and fax it to the pharmacists. She said she would do it under his direction.
488 The applicant’s approach to this topic is inconsistent. As the respondents submitted, it was, on the one hand, put to Ms Stewart that she “broke the law” by forging prescriptions but on the other hand, put to her that it was a “complete lie” that he told her to do so. Ms Stewart, when asked if she knew the forgery was illegal at the time, said “I had a feeling that it wasn’t correct, but I was under the direction of Dr Al Muderis, and I was told that it was okay to do it because that’s what he wanted”.
489 The applicant’s closing submission proceeded on the basis that Ms Stewart did forge the prescriptions, as she gave evidence of doing so. The applicant submitted on that basis, and because she betrayed the confidence of her patients by sending Ms Grieve their private medical records without their consent, that “Ms Stewart is a thoroughly dishonest and untrustworthy person and not a witness of credit”. The submission also relied on the fact that Ms Stewart did not disclose this conduct in her application for admission as a solicitor. Ms Stewart’s cross-examination was conducted in a very aggressive manner.
490 Her evidence about the prescription is a statement against her interest, particularly given she is now admitted as a solicitor. She described the circumstances in which this occurred. I accept that evidence. No basis has been advanced for why she would fabricate the evidence. This evidence does not render her a witness who has no credit. As I referred to above, aspects of her evidence were unsatisfactory, but as evident from the discussion above, significant aspects of her evidence are supported by other evidence.
491 The respondents submitted that this evidence about the prescriptions “was an appalling example of Dr Al Muderis pressuring Ms Stewart in the workplace”. I accept that submission.
492 There is no motive advanced by the applicant for Ms Stewart to provide what they allege is fabricated evidence. None is apparent on the evidence.
493 Although in cross-examination the applicant put to Ms Stewart that she spoke up about Dr Al Muderis because she was “excited at the prospect of marshalling a class action to take part in as part of [her] new career as a lawyer”, she denied it, and pointed out she was a criminal defence lawyer, not a class actions lawyer. However, the applicant does not refer to this assertion in his submission, and did not pursue the allegation. In any event, Ms Stewart’s evidence was she admitted to sending emails to about ten patients about a class action when she was a paralegal but stated that she was in no position to rally a class action because she had no relevant experience. She explained that she simply assisted a handful of patients to speak to a class actions lawyer to enable them to get legal advice. She said from the limited inquiries there were issues, and so she abandoned it. It appears the patients’ claims became actions in negligence. In any event, it involves circular reasoning because it presupposes there is evidence to bring a case (i.e. a legal case is only contemplated if there is evidence).
PART 6 — PATIENT CASE STUDIES
Section 1 — General observations
The patients
494 As earlier explained, I am mindful of the frailties of human recollection and the difficulties which affidavits can present. Although it is necessary to consider the evidence of each case study individually, some general observations can be made. Many of these observations are underpinned by the evidence discussed and factual findings I make below in relation to the patient case studies.
495 First, it can readily be accepted that many people have benefited from osseointegration. That said, it is elective surgery. It involves technology which Dr Al Muderis described in cross-examination as in its infancy, which he said confuses a lot of clinicians. The evidence establishes that not everyone is suitable for the procedure. It comes with risks and complications which can be serious and ongoing, as well as severely affecting a person’s health, adversely impacting on the quality of their life.
496 Generally, the patient witnesses had undergone hardship and were vulnerable at the time they consulted Dr Al Muderis. Most had traumatic experiences associated with their injuries, especially the osseointegration patients, with many suffering from related issues, (such as post-traumatic stress disorder (PTSD), other mental health issues, and pain related issues). Dr Al Muderis in his interview with Mr Steinfort recognised as much, describing patients as “severely traumatised, mentally, physically and psychologically”, and that he sees them at a low point in their life. The surgery is therefore often contemplated in circumstances where the potential patient has other health conditions (sometimes very significant ones).
497 For the osseointegration patients, the offer of surgery that would enable them to walk (or with more ease) would be very compelling. Some of the patients gave evidence which reflected their experiences had dramatically influenced their perception of risk. For example, Ms Mattiske described being “desperate to walk again” and “having ‘tunnel vision’ about the operation”. Mr Urquhart had said, “give me just one per cent chance of getting up and walking my daughter … down the aisle when she gets married, I would take that chance 10 times a day.” As referenced earlier at [418], Mr Hernandez recognised the interest and desire that such technology would have on amputees, stating in his proposal letter to Dr Al Muderis that “once amputees see the implant for themselves, they will do whatever it takes to obtain it”. The need for such patients to be properly warned of, and fully appreciate, the risks and complications of the procedure, is especially important. A patient should be put in a position to and given time to properly, and in an informed manner, consider their options. Osseointegration is elective surgery. There is no immediate urgency. The orthopaedic patients were also vulnerable and faced their own challenges, looking for solutions for injuries they had. Many were older persons.
498 In that context, patients were also vulnerable at the time they gave evidence. It was apparent some were suffering physically and emotionally during their time in the witness box.
499 Second, generally the patients have endured many medical appointments, procedures, and surgeries during their lives. The witness’ affidavits in this case were often prepared without the benefit of medical records (the respondents submitted, and the applicant did not challenge that although they had subpoenaed these records, the applicant resisted this process). Cross-examination of the patients is to be considered in that light. A witnesses’ evidence is not necessarily unreliable simply because they are incorrect as to when something occurred or was said. It also does not necessarily follow that because the timing of an event is incorrect, the evidence as to what occurred at the event is unreliable. On the other hand, the patients’ circumstances reflect that they are experienced patients, exposed to many medical professionals, and who may be more aware about medical aspects of their lives than others. In that context, it may readily be accepted that certain aspects of certain interactions with medical professionals could stand out to some patients because of their nature and impact. Many witnesses described events as shocking such that it stuck in their memory. Mr Wynne, for example, defended his recall of an interaction with Dr Al Muderis on the basis that “it was so profoundly shocking … I could see it right now”: see his case study in Part 6, Section 4.
500 All that said, I am very conscious that a patient may be a poor historian on aspects of their history, and care needs to be taken to consider what impact that has on their credibility and the reliability of their evidence, considered in the context of all the evidence. Amongst other things, I have looked to whether there is other evidence and considered how a patient’s evidence stands with other evidence. In doing so I am mindful of the standard of proof, as discussed above in Part 3, Section 1. That said, as will be apparent from my discussion in the patient case studies, much of their evidence is supported by other evidence.
501 Third, also in that context, the cross-examination of the patients generally took events in chronological order, as to each interaction with Dr Al Muderis and others. Often, propositions that certain events occurred were put to a witness without the witness being told their bases. As illustrated below, patients may well have assumed that the basis for the propositions (or questions) were medical notes. The manner of the cross-examination was generally to assert that the event occurred. The nature of the question presupposed the correctness of the propositions contained therein.
502 It was plain that, on occasions, witnesses were only ostensibly accepting propositions put to them. I raised with counsel, on at least one occasion, that it should not be assumed that the witnesses were assenting to the propositions. For example, during Mr Mortimer’s cross-examination I said that:
… some of the answers that have been given in the last while, I do not know whether [Mr Mortimer is] agreeing. He appears not to be agreeing, even though he said the word “right” on various occasions because of the way you’re putting propositions.
503 Similarly, during the cross-examination of Mr Warland, it became apparent as a result of the Court raising the issue, that Mr Warland was saying “yes” to propositions in the sense he was merely “tak[ing] [counsel’s] word for it” (see also Ms Schaeffer below in Part 6, Section 4).
504 Care must be taken in assessing the answers. For those witnesses, the applicant made submissions based on the answers reflecting the witnesses agreed with the propositions put.
505 Fourth, with few exceptions, the patients, their treating doctors and expert witnesses who gave evidence adverse to the applicant were variously accused in cross-examination of lying, giving false evidence, fabricating evidence or dishonesty. Their cross-examination was, at times, in an aggressive manner. Generally, no motive for that alleged conduct was put to witnesses.
506 The applicant, in oral closing submissions, took issue with the respondents’ submission that he had conducted his case in that manner. The respondents’ submission is correct. So much was evident during the hearing in this case.
507 That the applicant may have pulled back in closing submissions from some of the assertions put during the hearing does not alter that. Being accused in cross-examination of such conduct may have impacted on the witnesses giving evidence. It was plain several of the witnesses found it confronting and appeared offended by the allegation. Some medical witnesses were obviously surprised that such an accusation was being made. The applicant’s change of position in relation to some witnesses raises an issue as to the basis of some of the assertions that had been made (although it is unnecessary to address). One assumes it was on instructions.
508 Fifth, related to that was the “concoction” theory the applicant outlined as his case, which is referred to above at [211]. In their written reply the respondents submitted:
When asked by the Court during the course of oral closing submissions to explain Dr Al Muderis’ “concoction” theory, Dr Al Muderis’ senior counsel: (a) limited the submission to an alleged concoction of complaints by Ms Schaeffer, Mr Bruha, Mr Ladouceur, Mr Hernandez, Ms Ulrich, Ms Mattiske, Mr Smith, Mr Wynne, Mrs Todd, Mr Mortimer and Mr Urquhart; (b) withdrew the suggestion that the “concoction” of complaints was part of a conspiracy or scheme between these witnesses; (c) withdrew any attack on the credit of Mr Grant; and (d) could offer no motive on the part of the respondents to participate in a conspiracy to concoct false complaints.
509 Although the applicant made varying allegations of conspiracy and concoction during the hearing and conducted much of his cross-examination accordingly, he did not raise those matters in his written or oral closing submissions. When pressed by the Court as to the nature of the concoction and its participants, the applicant explained that his case was that the patients concocted complaints after their contact with one or more of Mr Hernandez, Ms Stewart, Ms Grieve, the team at The Alfred (being those involved with osseointegration), or Dr Huang. He denied he had advanced a conspiracy theory. He said his case for those witnesses was that their evidence of complaints is a recent invention.
510 In the respondents’ closing submission in chief, they submitted:
It was first suggested that the respondents had assisted patients in concocting messages – a claim that was subsequently withdrawn. It was then suggested that the patients had been turned against Dr Al Muderis and motivated to discredit him – either before or after the matters complained of (different propositions were put at different times), and by a variety of individuals including Mr Hernandez, Dr Huang, Dr Wines, Mr Gray, and the team at The Alfred in Victoria, among various others. None of this found the remotest support in the evidence, and it was not even pursued in cross-examination of Ms Grieve, Mr Steinfort or Ms Clancy.
511 That accurately describes the position put by the applicant during the hearing.
512 The applicant’s final position as articulated before closing submissions was that:
I should have said “concocted complaints” [rather than “concocted messages”] …We allege that the complaints are concocted from … about May 2022 onwards. And that all the complaints that came through from May 2022 were part of a concocted scheme.
(emphasis added)
513 Despite the applicant’s denial in closing submissions of having advanced an allegation of a conspiracy, his submission of the existence of a scheme of which he alleged the respondents were part, plainly fits that description.
514 Notwithstanding the respondents’ submission to the contrary, the applicant has not withdrawn the scheme submission. Rather, the applicant seeks to recast his case in the manner described above.
515 Further, although the applicant put (directly or indirectly) to Ms Ulrich, Mr Bruha, and Mr Ladoucer that they had spoken with Ms Grieve to help Mr Hernandez, it was not explicitly put to them they made up what they said to her (and their evidence) to help him. In relation to other witnesses, it was not suggested to them that they made up their evidence because of any dealings with certain persons. It was not put to any of the respondents that they were party to any scheme. No motive has been suggested for these, or any of the other patient witnesses (except the three above), as to why they would give false evidence. Again, this raises an issue as to the basis of such assertions being made (although it is unnecessary to address).
516 I note that in relation to many of the patients, there appears to be no relevant connection between them. That said, simply because patients may have known, or been friends with others, is not of itself a basis to make the accusations. The applicant mistakes a motive to speak publicly about the experiences that they say have occurred for a motive to lie.
517 As discussed elsewhere, some witnesses have had their osseointegration implant removed (e.g. Mr Urquhart, Mr Mortimer, Mr Haskett, Ms Mattiske and Mr Bruha) and some, before the Publications, sought second opinions (e.g. Mr Urquhart, Ms Todd, Mr Smith, Mr Mortimer, Ms Mooney and Ms Heffernan), complained to Dr Al Muderis directly (e.g. Mr Mortimer, Ms Todd, Mr Haskett, Mr Urquhart and Ms Çalan) and complained to the Health Care Complaints Commission (HCCC) (e.g. Ms Mooney and Ms Heffernan). Two patients had also brought negligence proceedings against him (receiving substantial settlements) (Ms Mooney and Mrs Gollan).
518 The applicant’s submission that the majority of patients did not come forward with any complaints about Dr Al Muderis until after the Publications, also fails to grapple with the fact that although some of the patients may not have formally complained before the Publications, it does not necessarily follow they did not have a complaint (or a basis for one).
519 I will address the witnesses separately, but as a general proposition, as the respondents submitted, the patients are a diverse group of people, coming from diverse locations, being patients (or prospective patients) over many years. All had suffered significant forms of personal hardship. Some were clearly reluctant to appear before the Court at all. They had no reason to come to give evidence other than to tell their stories. No other motive was put to them (apart from the three in relation to Mr Hernandez). They stood to gain nothing by giving evidence, other than saying what had happened to them.
520 Sixth, the applicant’s approach in cross-examination and closing submissions with respect to the patient witnesses’ evidence was, in many respects, simplistic. For example:
(1) it was put to some patients that they were mobile after Dr Al Muderis’ surgery where they had previously struggled to mobilise or were immobile, to then submit that therefore there was no basis for a patient’s complaint;
(2) it was put to many patients that they had been on holiday at some time since their surgery with Dr Al Muderis or there were photographs on social media with them smiling (or enjoying themselves) after surgery, such that their evidence of complaints, complications or pain cannot be accepted;
(3) it was put to some that they had said positive things on social media about Dr Al Muderis to support a submission that therefore any later complaint cannot be accepted; and
(4) if a patient is happy that they had osseointegration (or have more mobility), it was said they could not have any complaints, and the complaints made are not true. In that context, the applicant repeatedly made submissions that osseointegration surgery for various patients was “wholly successful”, and therefore there is no basis for any complaint (see e.g. Dr Al Muderis’ description of Ms Todd’s surgery being successful at [1832]). I note that it is apparent that Dr Al Muderis regarded the surgery as successful if, for any time, the patient was able to mobilise regardless of any complications they suffered. In his recorded interview with Mr Steinfort, he says:
if you have a patient that has an infection or pus coming out of their stoma, but they are playing soccer and running around with their children and fully active, fully employed and performing their day to day activity, would you call that a complication? I wouldn’t because these patients have their quality of life.
521 These propositions were said to demonstrate the falsity of various patients’ evidence as to their complaints, or criticisms they had as to their dealings with Dr Al Muderis. As a general proposition the reasoning underpinning those submissions is flawed. That said, it is necessary to consider the evidence in relation to each patient witness to assess what, if any, significance or weight attaches to the submission.
522 Other examples include that Dr Al Muderis is at times generous (e.g. by offering patients discounts for surgeries or doing humanitarian work) is not inconsistent with him prioritising his own interests (e.g. money and fame). Similarly, the proposition that he has a busy waiting room is not inconsistent with Dr Al Muderis actively seeking out new patients by promoting his business. These propositions are not mutually exclusive.
523 Seventh, the osseointegration patients’ evidence and interactions with Dr Al Muderis are in a context where he promoted to them that if a person has the procedure with him, they have a connection for life. As explained below, several witnesses gave evidence that Dr Al Muderis said to patients, in effect, that they will be family, and that he would be there for them. Dr Al Muderis took patients out to dinner and socialised with them. Some described him as a friend in a manner that was more than a doctor-patient relationship (which puts the terms of some emails and social media posts in context). Patients put their trust in him. He used patients to promote the surgery to others. When he was in the United States at conferences, patients would be used in promoting his implants and osseointegration in Australia. Patients were dependent on him because of what he had said to them, and as the implants were proprietary (once he began using his implants), this affected the extent they needed him for any issues that arose or parts to be replaced. International patients were especially vulnerable. For example, Ms Ulrich described in re-examination:
I was scared to sever this relationship, because if something went wrong with this, who was going to help me, since USA doctors and surgeons were scared to even touch my leg with this implant in it.
524 Mr Wynne similarly described:
… when I had this [osseointegration] done, I was essentially married to Munjed … he’s the only person I could go to if I needed anything done. There’s no other [doctor] in the world, that I knew of … where I could go to for help. I was, in a sense, stuck with him. … it’s a messed-up situation. Even though … I felt that he was very reckless, I was also stuck with him. … I didn’t get any sort of follow-up with Munjed. … it did feel like that relationship was dangling by a string, that if I wanted to keep the relationship going, I had to try hard … just to be able to ensure that I would get care for this part because without Munjed, I’m stuck. …
… I did feel like I had to keep this relationship going to ensure I still had a doctor to take care of me because, especially when I left Australia, there was no connecting me with a doctor for wound care in America. There was no connection [for] care for my osseo part once I returned to America, and I felt like it was completely all on me to keep this relationship happy and alive …
It was a scary spot to be in.
525 I accept that evidence. These matters can impact a patient’s behaviour towards Dr Al Muderis and their interactions with him. It alters the doctor-patient relationship.
526 Eighth, aligned with that, a patient may accept certain complications of a surgery for a period, particularly where they have confidence in their surgeon and if they are mobile. Being told by your surgeon that what they are experiencing is normal, and everything will be fine may be seen as acceptable, at least for a time. They may regard certain events as normal or usual. Red flags might not be questioned. However, patients’ views of their doctor (or circumstances) may change over time. They may eventually question what is happening. A patient may be worn down by what they have had to deal with from the surgery, continuing over time. Frustration may set in, particularly if they perceive that their problems are not being listened to or addressed. With the benefit of hindsight, events that occurred earlier in the relationship may later be seen in a different light. If something adverse had occurred, that no complaint may have been made about it at the time, does not alter the nature of the event. Assessing whether conduct is negligent is not dependent on there being a complaint about it at the time.
527 Ninth, it can be accepted that a patient may be unhappy about the outcome of a medical procedure and blame the doctor in circumstances where they were not at fault. I am conscious of that in assessing the evidence. However, an unhappy outcome may also have been because of (or contributed to by) the conduct of the surgeon. Conversely, it does not follow that simply because a patient is happy with the fact of having had the surgery, that they can have no complaints about their doctor and the services provided (both before and after surgery).
528 Similarly, the issue is not as simple as the applicant portrays when he repeatedly submitted that because a condition or consequence (e.g. an infection or implant removal) is said to be a known complication, no blame can be attributed to him. As a general proposition it is too broad sweeping and is devoid of context. In addition, the applicant’s submission fails to grapple with the nature of the allegations made in the different cases. Dr Ruff did not agree that simply because something is a known complication (which after all only means an event which has been known to occur) does not mean it is not negligent. I accept that evidence. Each case turns on its own facts.
529 Tenth, although the patients need to be considered individually, that does not mean that their evidence must be viewed in isolation. To the contrary, a witness’ evidence of an experience in one case, depending on its content and reliability, may be relevant to the probability of that experience occurring in other cases. Moreover, although a patient’s evidence needs to be considered (as with all the evidence in relation to their case study), evidence of their entire medical experience (although considered) need not be referred to in these reasons, let alone in a chronological manner. Not all disputes are relevant to the issues to be determined (or otherwise impact on the evidence). I have considered all the evidence and submissions advanced. As referred to above, I have considered whether there is other evidence, and how a witness’ evidence fits with any other relevant evidence. I have considered the impact of the evidence in the assessment of a witness’ credibility and reliability. It must also be remembered that ultimately what needs to be proved is the defence, that is, whether the imputations (or contextual imputations) are substantially true. That relies on a combination of the evidence. It is the probative force of that combined evidence which is to be assessed. The evidence is not to be considered in a piecemeal fashion. Proof of some facts may be affected by the Court’s assessment of other facts. As already referred to, the standard of proof I have applied is in accordance with the principles discussed above.
530 Having made those general observations, I address the patient case studies.
531 The patient case studies are categorised in the following manner. First, prospective patients who consulted Dr Al Muderis but did not proceed with the osseointegration surgery (Ms McIntyre and Mr Grieve): see Section 2. Second, Mr Ford and Patient X, who consulted Dr Al Muderis in 2021, that is, shortly before the Publications: see Section 3. Third, the international patients (the patients from the United States, being Mr Wynne, Ms Ulrich, Mr Bruha, Ms Schaeffer, Ms Koolhoven and Mr Ladouceur (who also did not proceed with the surgery) and from Turkey, Ms Çalan): see Section 4. Fourth, the Cambodian patients (Ms Eang and Mr Pril): see Section 5. Fifth, the domestic patients, upper limb osseointegration (Mr Mortimer and Mr Haskett): see Section 6; and lower limb osseointegration (Mr Urquhart, Mr Smith, Ms Mattiske, Ms Todd, Mr Warland, Mr Mailler, and Ms Rochford): see Section 7. Finally, other domestic orthopaedic patients (Ms Mooney, Mrs Gollan, Ms Heffernan, Ms Young, Ms Brandon, Ms Hutton, Mr Wright, Ms Slater, Ms Jones-Baldwin, Mr Rahiman and Mr Marlborough): see Section 8.
532 As will be apparent, I commence with a consideration of patient case studies that, with limited exception, were not referred to in the Publications. This, in large part involves patients (where they were called) who were not ultimately challenged in the same manner as those who were the subject of the Publications.
533 Having considered the case studies, I return to consider the stings from the Publications (see Part 7), which will bring together the evidence discussed in these patient case studies.
534 I note at the outset that there are four main case studies addressed in respect to the orthopaedic patients (Ms Mooney, Mrs Gollan, Ms Heffernan and Ms Young). Some other patient case studies in relation to the orthopaedic patients are dealt with in less detail as the issues in their cases are more confined. In those instances, their cases would be insufficient by themselves to establish the substantial truth of the stings, without being satisfied in respect to at least some of the osseointegration cases. These cases do not relate to any persons who are the subject of the Publications.
535 I note that in their Amended Defence the respondents, after referring to a patient, in most instances (but not all), alleged negligence by Dr Al Muderis because of matters, inter alia, his failure to adequately assess the patient, the patient was not a suitable candidate for surgery, his failure to adequately advise of the risks and complications associated with the surgery, and his failure to provide post operative care. I generally address what I have been satisfied of in respect to such allegations at the conclusion of my consideration of each patient, if I had not already done so during my analysis in the case study.
536 Before addressing those named patients individually, it is appropriate to first refer to some general topics and observations which are relevant to the consideration of the evidence in respect to the patient case studies.
Consultation reports
537 Given the applicant’s reliance on medical records, it is appropriate at this stage to address aspects of those documents. The primary focus was on the reports of consultations Dr Al Muderis had with patients. An issue arose as to the reliability of those produced by his practice.
538 Any discussion as to the contents of the consultation reports is in a context where witnesses from LRC said it has a practice of forwarding the reports to both the referring doctor and the patient or prospective patient. Dr O’Carrigan and Dr Alttahir gave evidence that this practice occurred despite there being no industry standard to provide the patient with the reports. However, once it is accepted that providing the reports to prospective patients is a standard practice at the clinic, but not an industry standard, this does not assist the applicant or overcome any deficiencies in the reports. To the contrary, that the reports were prepared in that context is the backdrop against which the reports are to be assessed. That is so, irrespective of whether they were sent to the patients on each occasion.
539 Dr O’Carrigan explained that the consultation report:
is an executive summary of … the consultation. … You have a complex amount of information that needs to be assimilated and crystallised for the patient’s benefit, as well as the surgeon’s benefit, as well as the referring doctor’s benefit, so that you have a clear understanding of what the clinical problem is and the treatment that can be possibly … provided to the patient.
540 Dr O’Carrigan accepted that consultation reports: allow patients to reflect on what had been said during the appointment; inform a patient’s referring doctor of what was discussed, such that they can offer the patient assistance in understanding their options, the risks, and any available alternatives; and ensure that the clinic has a record of what occurred. Dr Doshi gave evidence to a similar effect. Both doctors accepted that it is part of a surgeon’s duty to ensure that consultation reports are comprehensive and accurate.
541 It was generally accepted that it would be significant if a consultation report had omitted or misstated something material. Dr O’Carrigan explained a consultation report is “a legal document”, and therefore it is “very important to make it as accurate as possible”. It was also generally accepted that it was important that the report reflect the discussion of the risks with the patient.
542 Aspects of Dr Al Muderis’ and Dr Alttahir’s evidence on the consultation reports differed significantly from their peers. I return to their evidence below. The evidence of Dr Al Muderis is particularly problematic on this topic, and it conflicts with the evidence of others in his team (and the content of the reports themselves).
543 The applicant described propositions accepted by Dr Doshi and Dr O’Carrigan in cross-examination as to the degree of detail expected in consultation reports as “absurd”. He highlighted Dr Alttahir’s evidence that what mattered was that the consultation was comprehensive, not the report. He submitted that Dr Alttahir’s description of the purpose of the report as a summary of the pertinent points of the consultation, not a transcript inclusive of every detail, was more realistic. However, Dr Doshi and Dr O’Carrigan did not suggest that a report should be as detailed as a transcript.
544 The applicant, relying on the evidence of Dr Alttahir, and in contrast to the evidence of Dr Doshi and Dr O’Carrigan, submitted that the primary purpose of the report is to remind the doctor of pertinent points of the consultation, so they remember next time they see the patient. It was submitted that Dr Alttahir’s evidence is borne out by consultation reports prepared by other doctors, citing Dr Matthew Lyons’ and Dr Richard Carey-Smith’s reports as examples. He submitted that it would be otiose for a surgeon to record standard advice or standard procedures mechanically in every report and unnecessary for such standard processes to be written in the report in order for the surgeon to be able to remember it. That description of the purpose of consultation reports is unduly narrow.
545 It may readily be accepted that the content of consultation reports and the degree of detail varies between doctors, within reasonable bounds. Yet, in this case, the reports are sent to patients (or prospective patients) and their referring doctors. Critically, the reports’ contents (particularly in relation to the first consultation) are also directed to the patient and, given the reports’ terms, are designed to promote osseointegration surgery to the patient: see below. Relying on the contents of reports prepared by other doctors in other circumstances does not assist the applicant.
546 It may also be accepted that consultation reports benefit the doctor by recording what occurred at the consultation. However, the applicant’s submission that these reports are not for the patient’s benefit cannot be accepted, given the context in which these reports were prepared and used. The evidence of Dr O’Carrigan and Dr Doshi is that the consultation reports are also for the patient’s benefit. Dr Alttahir also accepts that as a purpose. Again, one only need to look at the contents of the reports in evidence in relation to the initial consultations (as noted below) to see that the applicant’s submission is not correct. Moreover, even if the report is for the doctor, and its primary purpose is as the applicant describes, that does not preclude the consequences of sending it to their patient and referring doctor. A consultation report should not be sent to those parties recommending highly invasive elective surgery be undertaken if that report is inaccurate or misleading. Even Dr Alttahir gave evidence it should contain “the pertinent points of the consultation”. Even if only a summary, it should be accurate.
547 That the reports are also sent to the patient’s referring doctors, often their GP, adds to the importance of accuracy. The referring doctor is not present at the clinic consultations. As Dr O’Carrigan accepted, the reports inform a patient’s referring doctor of what was discussed, such that they can offer the patient assistance in understanding their options, the risks, and any available alternatives. The applicant’s case is that the reports do not need to be comprehensive, and that it is acceptable that he and his team omit details from the reports which the patients are told orally. For example, although many reports record that the patient’s risk of infection is low (or relatively low), the patient is (on Dr Al Muderis’ evidence) warned orally that infection is inevitable. If that occurs, that practice is apt to mislead a referring doctor and the patient in turn. In discussing the surgery with their GP, it cannot be expected that a patient will supplement the report with what was said orally at the clinic, particularly in so far as what was discussed and what is recorded in the report are ostensibly inconsistent. A patient is entitled to accurate medical records.
548 Although I will address Dr Al Muderis’ consultation reports in the case studies as they relate to each patient, there are some common features which appear in many of the reports. Most of the reports of the initial consultations in relation to osseointegration appear to have a format, with some pro forma content.
549 Against that background, at the outset, it is appropriate to make several observations which impact on the reliance that can be placed on the reports.
550 First, of the reports of patients’ initial consultations in evidence, nearly all are formulaic. Some of the initial consultation reports in evidence, include the statement:
The team and I interviewed and discussed thoroughly with [the patient] the advantages and disadvantages of [the procedure] and explained the process of the operation including its complications like:
1. Death
2. Septicemia
3. Loss of rest of [limb]
4. Need for Revision of implant
5. Conversion back to socket prosthesis
6. Need for Multiple debridements
7. Need for Parentral antibiotics
8. Need for Oral antibiotics
(e.g. Ms Koolhoven, Mr Wynne, Mr Warland, Mr Haskett, Ms Ulrich, Ms McIntyre, Ms Schaeffer and Ms Mattiske).
551 However, the list is typically followed by:
So far we have performed over [X] osseointegration cases and it has been shown clearly that functional capacity of all our cases has increased dramatically with a high statistical significance, furthermore complication rate has been extremely low and last but not least cost effectiveness has been high especially considering that a significant number of our patients have returned to the workforce after being unemployed for several years.
552 The stated number of osseointegration cases performed increases over time in the reports.
553 The reports then frequently state:
[The patient] does understand the risk of infection associated with this surgery, however we regard [the patient] as relatively low risk. [The patient’s] procedure would be very standard.
554 They typically conclude with the statement:
Due to the increasing challenges [the patient is experiencing], it is my [Dr Al Muderis’] opinion and I do believe that it is necessary for this procedure and would expect to see an improvement in [the patient’s] mobility. Given that osseointegration surgery is acceptable worldwide, it is reasonable to offer [the patient] this option to improve [their] quality of life.
555 Even if a list of risks is included in the report (including a possible need for parenteral or oral antibiotics), it is followed by statements emphasising the success of the surgery, that the complication rate has been “extremely low” and infection is a “relatively low risk” for the patient.
556 I note that some consultation reports simply include the pro forma statement regarding the “relatively low risk” of infection (recited above), but otherwise refer to no other risks (e.g. Ms Todd, Mr Mailler and Mr Mortimer (with the exception of Mr Mortimer, who, as an upper-limb patient, is also advised he faces a lower risk of infection than lower-limb patients)). Ms Çalan’s report contains no reference to risks.
557 The terms of these reports differ considerably from what Dr Al Muderis deposes as to what he tells each patient. His evidence is:
I … specifically discuss risk and potential complications [with patients]. The first thing I tell them about risk is “you could die”. I then tell them that:
(a)“infection is a matter of when, not if”, and that there is a 100% chance that the patient will develop an infection at some stage - I tell patients “you may get it while you are in hospital, or in a month, a year, ten years or 100 years”;
(b) they could be left in a vegetative state from severe infection;
(c) they could lose the rest of their leg;
(d) they could have an infection so severe that they need intravenous antibiotics for a prolonged period;
(e) they could have an infection that may require oral antibiotics for the rest of their life;
(f) the wound may require debridement or washing out;
(g) revisional surgery might be required;
(h) multiple hospital admissions or visits may be necessary;
(i) the patient might develop hypergranulation which needs to be treated with the application of silver nitrate or surgery … ;
(j) the patient will be left with a permanent stoma, which will be ugly … ;
(k) there will be some amount of drainage from the stoma and it might smell.
I explain to patients that “This is not a pain-relieving procedure. This procedure is about mobility”.
558 I note that this is disputed by many of the patient witnesses, which is addressed elsewhere.
559 There is one report in evidence, which relates to Mr Bruha, in which the risks and complications are described in greater detail, and also varies from what is included in the formulaic reports, particularly in relation to infection:
I advised Chris that the infection risk is extremely high. It is 100% in every patient but whether he will get it immediately after the surgery or he would get it a year or two after the surgery is the question. He may get it ten years after the surgery. The risk of infection in the literature is between 34-55%, however in my opinion whenever I advise a patient regarding osseointegration, I inform them that the risk of infection is 100% for them considering that there is a piece of metal sticking out of the skin. Infection risk is dramatic with osseointegration surgery and he may lose his leg above the knee as a result of that. He may need multiple debridements, he may need removal of the implant and he may need to have IV antibiotics or oral antibiotics for a prolonged period. My advice is that self-care and hygiene is paramount. There is a risk of granulation tissue, especially activity related. If he does a high level of activity then granulation tissue will be higher. We have not had any transtibial osseointegration that has fractures but periprosthetic fracture can happen and it is more often with transfemoral osseointegration. Other risks associated with this surgery are clots in the leg, clots in the lung and other complications with general anaesthesia including death, neurovascular risk, strokes, heart attacks and others.
560 There is no evidence explaining difference between this report, and each of the others referred to above. As addressed further below, the applicant’s submission on this topic does not provide a satisfactory reason in the context of the evidence: see Mr Bruha’s case study in Part 6 Section 4.
561 Indeed, the formulaic reports generally reflect a very positive outlook for the patient. They downplay the risks and promote the benefits of the surgery, encouraging the prospective patient to agree to the surgery. That the reports generally portray this picture affects their reliability, including as an accurate summary of what occurred at each consultation. Many of the first consultation reports in evidence state, inter alia:
(1) Dr Al Muderis has performed many osseointegration surgeries, such that he is very experienced;
(2) in all of his cases, the functional capacity of the patient has increased;
(3) the complication rate has been extremely low;
(4) cost effectiveness has been high;
(5) patients have returned to the workforce after several years of unemployment;
(6) the surgery has world-wide acceptance; and
(7) the particular patient:
(a) understands the risk of infection, but is at a relatively low risk;
(b) would have a very standard procedure;
(c) is experiencing challenges which are increasing;
(d) would expect to see an improvement in their mobility and quality of life; and
(e) the surgery is necessary.
562 Pausing there. As can be seen from the passage recited typically included in the reports at [554], the applicant generally referred to the surgery as being “necessary” for the patient. This is an elective surgery. As Dr Doshi accepted in cross-examination, it would be wrong to tell a patient that it is necessary to have osseointegration surgery. Dr O’Carrigan also accepted as much.
563 Second, the formulaic reports’ description of infection discords with what Dr Al Muderis purports to tell patients orally. Although those reports generally describe infection as “relatively low risk” and the complication rate of surgery as “extremely low”, the applicant’s evidence was that he would tell prospective patients orally that “infection is a matter of when, not if”, with there being a “100% chance” that the patient will develop an infection at some stage. I note that, at times, the evidence is that Dr Al Muderis tells patients that the “risk of infection is 100%”. Read in context, when he describes infection as having a “100% chance” or a “100% risk” in his discussions with patients, he uses the terms synonymously to convey that infection is inevitable.
564 That discord is problematic. On the one hand, if he orally warns prospective patients that infection is inevitable, an issue arises as to why the reports generally omit so much but otherwise describe infection as “relatively low risk” and complication rates as “extremely low”, particularly given that they are provided to the referring doctor and patient. The import of those descriptions (and the omission) is that developing an infection is not inevitable. As Dr O’Carrigan accepted, if a surgeon had told a patient that there was a 100% risk of infection but wrote in the consultation report that the patient was regarded as having a relatively low risk of infection, that report would be inaccurate. So much is self-evident.
565 On the other hand, if Dr Al Muderis only told the prospective patients there was a “low risk” of infection, as is generally reflected by the reports in evidence, an issue arises as to why that is so if he is of the view that infection is inevitable. Much of the patients’ evidence reflects that Dr Al Muderis did not orally convey that infection was inevitable. Many patients gave evidence that he downplayed the risk of infection, including that they were told there was a low risk of infection which could be dealt with by antibiotics. That the reports describe infection as low risk is consistent with that evidence.
566 The applicant’s closing submissions on this topic were unsatisfactory and cannot be accepted.
567 The reports per se do not explain what is meant by a “low risk” (or “relatively low risk”) of infection. The applicant submitted that the reference to low risk of infection relates to serious infection. He also submitted that as the report is only a summary of pertinent points, there is no reason to presuppose, because a report says that “we regard the patient as relatively low risk”, that represents the totality of what the patient was told. He pointed to Ms Stewart’s evidence:
Dr Al Muderis would explain to patients that there [were] three levels of infection risk – “mild”, “moderate” and “severe”. He explained that “Mild” involved superficial skin infection which would have symptoms such as redness, pain and oozing. He told patients that would usually be treated with antibiotics. He explained that “moderate” would be more serious and might require IV antibiotics and hospitalisation. He explained that “severe” related to an infection in the bone that could in very rare circumstances result in the implant removed and the patient going back to socket prosthesis.
568 However, a plain reading of the reports does not support the submission that “low risk” refers to “low risk of serious infection”. Leaving aside the issue as to what patients were told (which in respect to some patients is in dispute), the submission that the patient would have understood it that way because they were told of different types of infection in the consultation cannot overcome the plain terms of the report. Given it was intended to be sent to patients and their referring doctors, such a proposition would have been expected to be clearly stated.
569 In that context, nor can the applicant’s submission be accepted that, given the primary purpose of the report was to remind the doctor of what happened, it did not need to include the doctors’ standard speech (i.e. “it’s not if, but when, a patient would have an infection”).
570 In his written submissions in reply, the applicant’s position changed, contending that the phrase “relatively low risk” is to be interpreted as a reference to the patient’s position relative to other patients. That also does not assist, as it does not address what is meant by “low risk”, which is not addressed in the report. Further, on the applicant’s evidence, infection is inevitable.
571 Either way the reports’ description of infection reflects adversely on the applicant. If a patient is told infection is inevitable, but the statement that there is a “relatively low risk” of infection is recorded in the report, the compelling inference is that it is to downplay the risks of the procedure and therefore encourage patients to agree to undertake the surgery. On the other hand, if the applicant did not say infection was inevitable, but rather said there was a relatively low risk, he is knowingly giving incorrect information (which also downplays the risks of the surgery given his evidence). As reflected in Mr Bruha’s letter, he believes “the risk of infection is 100%” and that the “[i]nfection risk” of osseointegration surgery is “dramatic”, citing potential consequences including further amputation and loss of implant. This also raises issues with the credibility and reliability of his and his witnesses’ evidence as to their interactions with the patients (or prospective patients).
572 Third, there is a standard template used in relation to osseointegration reports, with some aspects of the reports being cut and pasted. So much was accepted by Dr Al Muderis when questioned about Mrs Gollan’s report. Dr Al Muderis gave evidence he dictated reports, which leaves open the question if the report is not seen by Dr Al Muderis before it is sent out (which typically is stated on the reports), and there is cut and paste, who checks that it accurately reflects what occurred? There is no evidence as to what is in the template. Dr Al Muderis said he dictated a report while seeing a patient or immediately after, but some he did at the end of the day or later. This is in a context where he was typically seeing 30 or more patients on a clinic day.
573 I note that, although Dr Al Muderis generally produced reports for consultations, there are no reports for some consultations despite him giving evidence of the consultation occurring, or the documentary evidence otherwise establishing that they occurred (e.g. Mr Urquhart’s first consultation, Mr Smith’s first and second consultations, and a pre-operative consultation of Mr Haskett). That is, out of the 20 osseointegration case studies (not including the Cambodian patients), pre-operative consultation reports were not produced for three patients. It is difficult to understand how such reports could be missing for this number of patients if, as he gave evidence, he dictated the reports as a matter of practice, proximate to the consultation. In the circumstances, the obvious inference is that there are no reports for these meetings.
574 Fourth, as already discussed, Ms Stewart gave evidence that she often wrote consultation reports for Dr Al Muderis. An email exchange discussing the drafting of a consultation letter for a patient in the UK is informative. It commences with an email from Dr Al Muderis’ practice manager, Ms Livingstone:
Ms Livingstone: Hey, The initial letter in [the patient’s] file isn’t complete, that needs to be done before I print everything
Ms Stewart: Munjed did the consult in the UK. It needs to be completed by him
Ms Livingston: Hey Munjed, Need to print [the patient’s] entire file for tomorrow as its his last appointment, are you able to dictate an initial letter before he leaves? …
Dr Al Muderis: Shona should have done this
Ms Stewart: I wasn’t present with his initial appointment
Dr Al Muderis: Shona Since when it matters if you were there or not. You did the COR I am sick of these stupid responses
Ms Stewart: The letter in draft form in [the patient’s] file that is not in the clinic letter format I normally do. I do not know what you would add or confirm in it from the uk clinic
575 The terms of the exchange support Ms Stewart’s evidence. Ms Livingstone’s request that Dr Al Muderis “dictate an initial letter” evinces that it is not yet drafted. Dr Al Muderis’ reply that “Shona should have done this” reflects an expectation that she would draft the letter, and that he would not. Ms Stewart’s reply (“I wasn’t present …”) reflects her understanding of that expectation, at least when present at the consultations (I note Ms Stewart’s evidence is that the COR (a database in which diagnostic measurements for patients is maintained) “never goes in the letter”). In that context, that Dr Al Muderis writes that she “should have done this” irrespective of whether she was “there or not”, and that Ms Stewart writes that the letter “is not in the … format I normally do”, suggests Ms Stewart is habitually involved in drafting the reports.
576 That is consistent with Ms Stewart’s evidence. The following exchange occurred in Ms Stewart’s cross-examination:
Ms Chrysanthou: You - - -?
Ms Stewart: I was – I was asked to write the reports after osteointegration clinic days.
Ms Chrysanthou: Dr Al Muderis, or one of the other doctors or fellows, dictated the reports?
Ms Stewart: No, I also dictated the reports, and there would be – there would be emails to the – the lady that did the – that did the reports up from the Dictaphone.
Ms Chrysanthou: And you weren’t asked to write up reports and interpret x-rays, were you?
Ms Stewart: Yes, I was. That was part of the template of – of the report. I struggled with this so much, because I didn’t have the qualifications or the knowledge to be able to provide in these reports.
Ms Chrysanthou: That’s true?
Ms Stewart: And I would ask for assistance to be able to do this, and I was met with so much resistance.
Ms Chrysanthou: You didn’t have the qualifications to do it; you agree?
Ms Stewart: No, that’s right. And I – I had to get a lot of help. And the lady that did the reports struggled with them, because the – the reports were late because I had to basically get so much help with them to be able to provide what was accurate and true in the report.
Ms Chrysanthou: You weren’t asked to write the reports?
Ms Stewart: I was asked to write the reports.
Ms Chrysanthou: And you didn’t regularly write them?
Ms Stewart: I did regularly write them.
577 I note that several of the consultation reports in evidence record Ms Stewart as present at the consultation (e.g. Mr Warland, Ms Mattiske, Mr Urquhart, Ms Ulrich and Ms Schaeffer).
578 The suggestion in cross-examination that she was not being asked to complete the consultation report (which she rejected), is not borne out by the email exchange.
579 I note that, if Dr Al Muderis is in fact delegating the drafting of some the reports, this email raises a question as to why he is doing so to staff who are not present at the appointments.
580 Fifth, some of the pro forma elements of the initial consultation reports in this case, are questionable. As recited above, the reports generally refer to the number of osseointegration surgeries Dr Al Muderis has performed, which is used to explain that “it has been shown clearly that functional capacity of all our cases has increased dramatically” (emphasis added). Yet many (if not all) the reports in evidence are provided in circumstances where patients’ functional capacity had not “increased dramatically” (e.g. Ms Todd) or where some patients have had their implant removed (e.g. Mr Mortimer). In that context it is difficult to understand how that statement could be accurate.
581 In the pro forma reports, the procedure is also referred to as “standard” which, given the patients’ individual circumstances and surgeries, could not properly describe each patient’s situation. For example, the upper-limb surgeries of Mr Mortimer and Mr Haskett were not surgeries Dr Al Muderis commonly performed. Mr Mortimer must have been one of Dr Al Muderis’ first upper-limb patients, which hardly makes it a standard procedure. As explained below, the same could be said for Ms Mattiske’s surgery (see her case study in Part 6, Section 7 below).
582 Further, the reports refer to a worldwide acceptance of the procedure, in circumstances where it was not approved by the United States Food and Drug Administration (FDA) at the time of these reports.
583 In Mr Wynne’s case, his initial report refers to a “thorough discussion amongst the team”, despite the only persons present at that consultation being Dr Al Muderis and Ms Roberts, and they accepted they were the “team” referred to.
584 Many of the reports state:
[The patient] individually met with other patients who are at various stages post-operatively as well as patients who are contemplating the procedure, all of who were able to share their experience and discuss the pros and cons of such a procedure. This is a vital part of the osseointegration clinic protocol due to the complexity of the process.
585 In cross-examination, when pressed as to the accuracy of that occurring in each case, Dr Al Muderis said that he knew it was correct in relation to “every single patient” because “I go out to the waiting room all the time and I speak to patients and I introduce patient to each other”. Moreover, that passage appeared in relation to Mrs Gollan’s consultation, a non-osseointegration patient. Her letter also stated she had met with members of the Osseointegration Group of Australia, when she did not. On 13 July 2017, Mrs Gollan was sent a letter for a follow-up consultation at the osseointegration clinic, with all the details for her attendance at the clinic, including that she will meet with other osseointegration patients. Again, this is incorrect. A similar letter was sent to her on 1 November 2017. This was obviously a cut and paste from a pro forma template, which plainly did not reflect what occurred. The error was perpetuated on many occasions. There are other pro forma statements in reports which could not be correct. For example, Mr Mortimer doing the six-minute walk test when he was an upper-arm patient.
586 Ms McIntyre’s report is illustrative of the unreliability of consultation reports. Her report contains the standard template contents recited in the first observation above. Ms McIntyre’s evidence (concerning a different risk to infection) is also illustrative of how telling patients one thing orally, but another in the report (recalling it is sent to them), can mislead the patient:
I don’t understand why Al Muderis said [in the consultation report] the complication rate had been “extremely low” when he told me [orally] there was a one in ten chance the surgery wouldn’t be successful. That seemed contradictory to me.
587 Ms McIntyre also gave evidence that Dr Al Muderis told her that there was a higher risk of infection in her case because of her work environment and lifestyle. She pointed out in evidence that in the consultation report she and her doctor received, the risk of infection associated with surgery in her case is described as relatively low risk. As explained below in her case study (see Part 6, Section 2), I accept her evidence of the events.
588 Sixth, in the above context, some patients also took issue with the content of the reports accurately reflecting what they discussed with Dr Al Muderis. For example, Mr Mortimer’s report records that he “has expressed that his functional level has declined”. When it was put to him in cross-examination that he said that, he replied, “… that’s so strange. No, it was never declining. … I wanted to improve and do more but it was not declining, no. So I don’t know why they said that.” Mr Grieve’s evidence was that the report was not an accurate reflection of his consultation with Dr Al Muderis: see his case study below in Part 6, Section 2. Ms McIntyre also highlighted several errors in her report: see case study below.
589 The applicant submitted that there were passages of cross-examination of various patients where the substance of a report was put to the patient and the patient agreed or disagreed with it. He submitted these references show that the substance of the reports was regularly corroborated by, or consistent with, other evidence or not disputed by the patients when it was put to them. I will address this when considering the patients. Suffice to say at this stage, on occasions where there is a submission that the substance of a report is put and agreed to by the patient, the submission generally is not borne out by the evidence. I will mention two patients briefly. The submission in relation to Mr Mortimer’s answers in cross-examination being an acceptance of the substance of the consultation report of 25 February 2017, is not supported by the evidence: see [1387]. Similarly, the submission in relation to Mr Bruha that “[i]n cross-examination, when the substance of Dr Al Muderis’s consultation report was put to him, he agreed with effectively all of it, and the Court would therefore accept that the report is an accurate summary of the consultation”, is not supported. Much of the substance was not put to him: see [1020].
590 Moreover, the whole premise of the applicant’s submission about the reports is that they are only a summary and do not reflect the totality of what was said. Further, care needs to be taken with the applicant’s submission that a patient in cross-examination (e.g. Mr Bruha) agreed with the substance of a consultation report (and therefore what occurred at the consultation). To take an example. It was put that Mr Mortimer agreed that in the February 2017 consultation, he was told by Dr Al Muderis that his issues with mobility were caused by rubbing due to tissue shrinkage. However, it does not necessarily follow that that was the cause of his condition. In relation to Mr Mortimer, Dr Al Muderis later opined in a consultation report dated 31 October 2017 that “[f]or Shane we feel as though he is actually doing quite well with his implant”, a statement which, for the reasons given below, was not correct: see his case study in Part 6, Section 6).
591 Seventh, it is appropriate at this juncture to refer to the letter Dr Al Muderis wrote to Ms Mooney’s referring doctor reporting his treatment of her. Ms Mooney had two surgeries with Dr Al Muderis, the second being revision surgery. In the letter dated 21 April 2011 to her GP, Dr Louisa Ahmed, Dr Al Muderis said in the first paragraph:
[Ms Mooney] was seen by one of our experienced orthopaedic surgeons, Dr Ali Gursel, who then referred her to me due to the complexity of her injury to manage her tibial plateau and tibial shaft fracture. I attended to her with multiple surgeries. The first stage was to stabilize the fracture by plate and screws and then the second stage was to permanently fix the fracture with an intramedullary nail and bone grafting to the tibial plateau.
592 As explained further elsewhere, this statement is incorrect. During closing submissions, the applicant accepted that this statement was a mistake. It is, considered in context, not simply a case of not being “well drafted”, as suggested by the applicant.
593 This impression of what occurred is perpetuated further in a letter to Dr Ahmed dated 14 July 2011:
Her injury was so extensive that I performed two surgeries the first being to stabilise her fracture of the tibial plateau and shaft with a plate and screws and second surgery to remove Leah’s plate and screws before inserting an intramedullary nail.
594 This is misleading, and deliberately so. It creates the impression that it was preplanned to have two surgeries, as opposed to the second surgery being a revision surgery. Although Ms Mooney may have informed Dr Ahmed otherwise, that would have been inconsistent with the written document before Dr Ahmed.
595 I note also in relation to Ms Mooney, that the drill bit broke off in her knee. There is no reference to the drill bit being left in Ms Mooney’s leg in the operation report. This is discussed in considering Ms Mooney’s case study: see Part 6, Section 8.
596 Contrary to the applicant’s contention, I am not satisfied that the consultation reports constitute a reliable body of evidence. The above provides some examples reflecting why that is so (others are evident in consideration of the patient case studies below). The reports in evidence span many years. Moreover, although inaccuracies in a report or document may exist and may be unknowing, the description of the reports being a reliable body of evidence cannot be applied to many of the examples given above. The reports appear to favour a result that the prospective patient is suitable for the surgery or that it is necessary (or otherwise favourably portray the patient’s situation). It may be accepted that some of the inaccuracies may be a result of oversight. Given the nature of the inaccuracies, it may be only that Dr Al Muderis was not listening or paying attention to what the patient was saying. Some appear to be a matter of a conscious choice (e.g. promoting the surgery in a positive manner, portraying the surgery as necessary, or to explain favourably why surgeries had occurred, (e.g. Ms Mooney)). Regardless of the reasons for the inaccuracies or misleading statements, the consequence is that it necessarily affects the reliability of the reports and generally impedes the ability to simply accept them at face value. Their assessment may be impacted by considerations including the topic on which they are relied, how it fits with other evidence in the case study, and whether it is controversial or corroborated. That said, the individual case studies must be considered in the context of all the evidence. The relevant reports are considered in addressing each of the patient case studies.
Standard practice – application
597 I have addressed the principles in relation to relying on evidence of standard practice above. As explained there, the question of whether standard practice evidence is to be preferred, depends upon the specific nature and quality of the evidence that is given in a particular case. That is, attention must first be directed to what the standard practice relied on is said to be, and its content (e.g. there could be a standard practice that something is done, but not how it is done).
598 As earlier referred to, the applicant devoted one section of his written closing submissions to the topic of his standard practice. I note that the submission addresses evidence on the topics of the booking processes and arrival at Dr Al Muderis’ rooms, assessments by Dr Al Muderis and other specialists, discussion of risks and potential complications, consultation reports, post consultation procedures, procedures on the day of surgery and hospital care, and rehabilitation and post-operative care. Some care needs to be taken in considering the submission. Although it may be accepted that there were some standard practices, what they were, what they entailed, and the frequency with which they were applied, is in issue. The applicant’s submission contains many generalised statements, and some of the evidence relied on is insufficient to support the propositions put. To provide just two examples, in relation to aftercare. First, for interstate patients, the submission as to the practice is that they follow the same regime as local patients. Mr Mortimer’s evidence described below in Part 6, Section 6, does not accord with that (e.g. his experience after being released from hospital post-surgery and returning interstate). Second, as to the international patients, the submission is that when they return to their home countries the patients are referred to local specialists for any immediate treatment concerns. The evidence relied on in support of the submission is primarily Ms Roberts’ affidavit evidence, and an aspect of Dr Al Muderis’ evidence in chief. The evidence is inconsistent, as at the passage of Dr Al Muderis’ evidence relied on, he said the standard protocol was that once the patient returned home, he would consult with them on a regular basis, and if they needed any help, he would refer them to a local clinician in the area (this evidence being given in respect to Ms Çalan). As will be apparent from the patient case studies, neither what is said by Ms Roberts to be the practice for post-operative care, nor what Dr Al Muderis described in relation to Ms Çalan, occurred in relation to the international patients who gave evidence: see Part 6, Section 4.
599 The applicant emphasised that the evidence of standard practices included Dr Al Muderis himself, and “came from no fewer than 15 sources, covering a spectrum of roles within the practice”, referring to Drs Tetsworth, O’Carrigan, Stoita, Alttahir, Doshi, Al-Jawazneh, Basten, Haidary and others, being Mr Laux, Ms Geada, Ms Dean, Ms Moti, Ms Roberts, and Ms Harris. Those witnesses did give evidence as to standard practices on varying topics, at various times and to varying degrees. Some of the affidavits are sparse and can only cover a limited time (e.g. reflecting their period of working with Dr Al Muderis). I have considered their evidence.
600 The aspect that received the most focus, was what was said to be a standard practice for discussing the risks and complications of osseointegration surgery with patients.
601 To illustrate the caution needed, and the need to focus on the evidence, it is sufficient to refer to the applicant’s submission (made at the outset on this topic) that “[t]hroughout the relevant period, the website [being Dr Al Muderis’ website to which patients were directed to] contained information about Dr Al Muderis, the procedure, and the risks” The reference to support that submission is the affidavit of Ms Roberts, which itself refers to exhibits.
602 However, a consideration of that evidence, and the exhibits referred to reflects that any risks referred to were only acknowledged in a limited way, and the websites form part of the basis of the respondents’ claim that they contained misleading information (which I accept as established). As referred to elsewhere, the websites as at 2023 still stated that the risk of infection is “very low”. I note also that, in the context of directing patients to preliminary information, no reference is made in this submission to the brochures, which as I find elsewhere, suffer from the same defects: see the Brochures – misleading statements in Part 6, Section 1 below.
603 The applicant submitted that while in the waiting room for their consultation, the patient also “had the opportunity … to read written information about the surgery, such as the Patient Guide to osseointegration”. The document referred to from the evidence of Ms Roberts is the document titled “Osseointegration Surgery A Guide for Patients” dated 1 May 2018 (with Ms Roberts’ evidence being it was still in circulation after that time). That document does list some associated risks, but states that these complications are “rare”, that the list is “to inform, not alarm you” and “serious complications are uncommon”. It states the most common complication is infection and refers to this as a risk of “minor” infection, and claims this risk has “dramatically reduced with the introduction of the single-stage surgery and refinement in surgery techniques”. It states that most of the time, a course of oral antibiotics is sufficient, in rare cases intravenous antibiotics or surgical debridement may be required, and in extreme cases a second operation may be needed to remove the implant, followed by a third operation to re-insert it. Many of the risks and complications that were experienced by the patients who gave evidence are not referred to (e.g. odour, hypergranulation and maggots). I note also that on the first page of the Guide, it refers to the implant being directly attached to the skeleton, which “allows for freedom of movement, greater control of the limb and reduced overall pain” (emphasis added).
604 Dr Al Muderis’ evidence as to what he told patients in relation to the risks and complications of surgery is set out in the discussion above in relation to consultation reports. The applicant submitted:
The witnesses did not describe the risks and complications discussed with patients in exactly the same terms, because they did so in their own words, but considering the evidence as a whole, a consistent picture emerges as to the nature and content of the discussion. The Court would be satisfied that Dr Al Muderis’s usual practice included discussion of the following risks and complications:
(a) Death. Dr Al Muderis, Ms Roberts and Ms Harris deposed that the first thing he would say during the discussion of risks was always “You could die”. This is an alarming and attention-grabbing way to begin the discussion which would serve to make the patient take notice and take the discussion seriously.
(b) General risks of surgery. Apart from death, those discussed included heart attack, stroke, deep vein thrombosis, pulmonary embolism, pain and complex regional pain syndrome, and delayed recovery.
(c) Likelihood of infection. Many witnesses deposed that Dr Al Muderis regularly uses phrases such as “infection is a matter of when, not if” and “there is a 100% chance you will get an infection”. Patients were told they might get recurrent infections, particularly above-knee amputees, those who were overweight, and those with more fleshy tissue.
(d) Severity of infection. The distinction between a superficial infection localised to the skin or the stoma, on the other hand, and a deep infection around the bone, on the other hand, was explained to patients. They were told that less serious infections could be resolved with oral antibiotics, but that deeper or more serious infections might need intravenous antibiotics, surgical debridement and washing out, or removal of the implant.
(e) Failure of the implant. It was explained that the implant might become loose, either due to infective or non-infective loosening, and need to be removed.
(f) Re-amputation and bone loss. Patients were told that, due to infection or other complications, it might become necessary to amputate more of their leg, and that they could lose the rest of the leg. Dr Tetsworth deposed that patients are told “There is a possibility we could make you much worse”. They were told that they might end up back in a socket prosthesis or be left wheelchair-bound.
(g) Pain. Numerous witnesses deposed that Dr Al Muderis habitually says “This is not a pain-relieving procedure. This procedure is about mobility”. Patients were told that the level of pain post-surgery was highly variable and difficult to predict. They were told that they were likely to suffer from nerve pain, because amputation involves severing nerves, which causes neuroma formation. They were told that TMR [Targeted Muscle Reinnervation] could be performed to address this issue, but that a portion of patients still suffer ongoing neuropathic pain. It was explained to them that osseointegration in itself would not improve neuropathic pain.
Patients consulted a specialist pain physician as part of the consultation process.
(h) Wound healing complications. Apart from infection and implant loosening, these included fractures, malunion, and non-union of the bone.
(i) Revisional procedures. Patients were told that revisional surgery such as stump refashioning or nerve surgery may be necessary, usually around one year post-surgery, and that stump refashioning was more likely for above-knee amputees, women, and those with a higher body mass index.
(j) Drainage and odour. It was explained that there would be discharge from the stoma, the amount of which could vary from significant to minimal. Patients with a larger body mass index and transfemoral amputees tend to have more discharge. Odour associated with the discharge from the stoma was often discussed, but not always because it is not consistently a problem for patients.
(k) Stoma hygiene. Patients were educated about what it meant to have a stoma and the steps they would need to take to maintain the hygiene of the stoma.
(emphasis in original)
605 The applicant identified that this list had been compiled from the affidavit evidence of Drs Al Muderis, Tetsworth, Stoita, O’Carrigan, Alttahir, Basten, Doshi and Al-Jawazneh, as well as Mr Laux, Ms Roberts and Ms Harris.
606 The applicant sought a finding that Dr Al Muderis’ standard practice regarding the advice he gives to patients of the risks and complications of osseointegration included those matters. I note at the outset there is no reference to any time frame at which it is said these matters are to be regarded as part of Dr Al Muderis’ standard practice (given the timing of the events described by the patients). The applicant’s witnesses’ evidence appears to be based on their presence at, for example, the group consultations. However, no witness gave evidence that all those matters were discussed with patients. Rather, the list is a combination of aspects of each of the witnesses’ evidence. For some of those topics, only one or two doctors deposed to the matters (e.g. recurrent infections at [604] above, is only mentioned in the evidence of Drs O’Carrigan and Tetsworth, while the evidence of more discharge in certain circumstances is only mentioned in the evidence of Dr Stoita). As described earlier, there are inconsistencies in the evidence in relation to whether Dr Al Muderis told patients that “infection is a matter of when, not if” and that “there is a 100% chance that [they] will develop an infection at some stage”, with Dr Doshi’s evidence being that he did not recall it being said at all (and agreed if it was said, it was important to be recorded in the consultation report). The submission above that odour is not always discussed because it is not consistently an issue for patients refers to Dr Tetsworth’s evidence that they do not discuss it with every single patient, but that it comes up “quite often”. On the other hand, Dr Stoita’s evidence was that they tell the patients that “all develop an odour associated with their stoma at some point”. Of the 11 witnesses relied on for the purposes of this submission, only Drs Al Muderis, Tetsworth, Stoita, O’Carrigan and Ms Roberts deposed to the patients being told that the surgery is not a pain-relieving operation, but about mobility. Further, only Dr O’Carrigan stated that they tell patients of the risk of maggot infestation. This is in a context where Dr Al Muderis said in cross-examination that maggots were not discussed until after the Broadcast:
… the maggots are not a complication of the surgery, so it’s not a standard – it was not a standard discussion. It is now after the episodes of 60 Minutes … We chose to inform patients about maggots now since the episode of the 60 Minutes.
I note also that only Dr Al Muderis referred to a patient being told about granulation or hypergranulation, what it is, or how it is treated (although I note this is not included in the aforementioned list of risks in his submissions at [604] above). These provide only some examples of the issues that arise.
607 Given the context that the witnesses said these risks were referred to in consultations, the fact that some topics were not referred to by many of those witnesses is telling. It is difficult to understand how something can be regarded as a standard practice when those who the applicant relies on to establish the practice do not refer to it. This is particularly so where, even on the evidence relied on by the applicant, a topic of risk (e.g. odour) is not always discussed. Dr Tetsworth’s explanation justifying the approach in respect to odour because it is “less consistently an issue” reflects a misunderstanding and is troubling. That this issue may arise for a patient having had the surgery is known. That is the basis in which a patient should be told about a risk.
608 I am not persuaded that it has been established that all the risks and complications identified above were discussed or communicated to patients as a matter of standard practice by Dr Al Muderis in the group consultations. Although risks and complications as a topic was raised with patients, the applicant’s evidence does not establish the standard practice in relation to the extent of the content provided. Further, evidence of a standard practice does not address how a witness is told the information. For example, a doctor might recite the risks and complications but downplay the seriousness of them. This evidence is also to be considered together with other evidence, including, amongst other things, the consultation reports.
609 I note also, as evident from other discussions, the international patients, and some interstate patients did not have a group consultation in the manner that typically occurred at the LRC (e.g. for international patients, Mr Bruha’s and Ms Çalan’s consultation reports do not list anyone else as having been present, while Mr Wynne’s report only lists Ms Roberts; for an interstate patient, Mr Haskett’s report only refers to his prosthetist, a researcher and Ms Roberts being present).
610 The applicant submitted that the proposition that a surgeon “as senior and experienced” as he routinely tells patients nothing or almost nothing about material risks of major surgery is inherently very implausible. He submitted it “presupposes a breach of medical professionalism to an extraordinary degree” and “is even more implausible and extraordinary when one considers that he was accompanied during osseointegration consultations by other numerous medical professionals, including other orthopaedic surgeons”. I am conscious of this submission in assessing the evidence. However, it is not as simple as the applicant contends. As reflected from the discussion above, there are limitations in the evidence. As apparent from the paragraph immediately above, the contention that other orthopaedic surgeons were present at group consultations does not apply to some of the circumstances in this case.
611 Before leaving this topic, I will address the applicant’s submission in relation to the first risk identified above, being death, which is said to be “an alarming and attention-grabbing way to begin the discussion which would serve to make the patient take notice and take the discussion seriously”. That death is a risk of all surgery is well known and patients seeking osseointegration are likely to be experienced patients. In this case, many patients gave evidence of having had numerous surgeries prior to meeting with Dr Al Muderis in relation to osseointegration. In that context, telling the patient about the risk of death is hardly likely to be either alarming or attention-grabbing. It was not suggested to any witness that that was the effect of what was being told. To the contrary, it was apparent that the witnesses were generally familiar with the standard risks of surgery; the issue is whether they were informed about the specific risks associated with osseointegration.
612 The applicant submitted that the Court should not conclude that Dr Al Muderis’ practice is any different in general orthopaedic consultations, as compared to osseointegration consultations. He relied on the evidence of Ms Moti (a nurse who mainly dealt with patients having joint replacements and arthroscopies and did not have much involvement with osseointegration patients), which is said to be similar to the evidence given in relation to osseointegration cases. She deposed that she “observed that [Dr Al Muderis] takes time to explain the risks of surgery to patients during his consultation”, and that “no surgery has a guarantee of a successful outcome”. The basis of Ms Moti’s evidence is unclear as her affidavit said she generally saw the patients straight after their consultation with Dr Al Muderis. Although she said she “observed” Dr Al Muderis, there was no evidence that she was at the consultations. In any event, that is the extent of the evidence. Furthermore, some of the consultation reports in evidence concerning orthopaedic patients do not refer to any risks and complications being explained, but rather with him having provided them with the Australian Orthopaedic Association information pamphlet and asking them to read it for the purposes of informing the patient about the risks and complications of the procedure (e.g. Ms Hutton, Mrs Gollan, Ms Slater, and Mr Rahiman).
613 As referred to elsewhere, Dr Ruff said that the provision of the brochure and other documents was insufficient to explain the treatment options, benefits and risks, and is only an adjunct to the process of informed consent.
614 The evidence in relation to standard practices is considered in the context of all other relevant evidence, in assessing the issues in the patient cases studies.
Multidisciplinary approach
615 The applicant repeatedly promoted that his clinic adopted a multidisciplinary approach. For example, Dr Al Muderis’ affidavit states:
[50] When I consult new patients who are considering whether to have osseointegration surgery at the Limb Reconstruction Centre, I do so in a clinic with a number of other medical professionals. Typically, this will include other orthopaedic surgeons – including my colleagues Dr Kevin Tetsworth, Dr Razvan Stoita, Dr Tim O’Carrigan and Dr Mustafa Alttahir – as well as fellows, nurses, and prosthetists. The patient is also consulted by a psychologist and a pain physician as part of my clinic. The psychologist and the pain physician sometimes join in on the group consultation with me and the other orthopaedic surgeons.
[51] During the group consultations, all the consultants present are invited to express their opinion on the patient. We also consider the radiology and reports prepared by the pain physician and the psychologist. We then discuss the case as a group and endeavour to reach a consensus as to the patient’s suitability for the surgery.
616 This is also evident in the complete transcript of the unedited 60 Minutes interview with Mr Steinfort, where Dr Al Muderis said the following (none of which was included in the final publication of the Broadcast):
We work in a very large multidisciplinary team. Every single member of our team has equal vote equal right of refusal.
…
I work in a very large multidisciplinary team. We are five surgeons at the moment. Every single individual is equal and we all work independently and collectively with each other, we [work] in a team where there is a rehabilitation physician. There is a physiotherapist, there is a [prosthetist], there is a psychologist, there is a pain specialist. There is an infectious disease consultant. They’re all individuals, they [are] all independent.
…
Every single person that I work with has equal influence and equal decision making and equal importance in the outcome of every single patient.
617 To repeat the observation above, despite those assertions, the evidence reflects that such multidisciplinary clinics did not apply to international patients (and some interstate patients).
618 Imputation [16.17] is that Dr Al Muderis overrode the protocol of a specialist assessment team deciding the suitability of patients to have surgery, by going ahead irrespective of the team’s decision. The respondents alleged in their defence that Dr Al Muderis’ practice changed such that even if everyone else in his multidisciplinary team came to an opinion that a patient was not a suitable candidate for surgery, but Dr Al Muderis considered they were, his opinion prevailed.
619 There are several points to address.
620 First, the applicant referred to the evidence of Dr Al Muderis’ colleagues, Drs Stoita, O’Carrigan, Alttahir and Basten, submitting that their evidence that Dr Al Muderis did not disregard or override the opinions of others should be accepted. The applicant submitted that the evidence reflects that a patient is referred to a particular surgeon, and that surgeon has ultimate decision-making responsibility for the patient. When there are divided opinions, somebody needs to make an executive decision, and if Dr Al Muderis is the surgeon with the referral, that responsibility falls to him.
621 It is appropriate to consider the terms of the evidence. Dr O’Carrigan’s evidence was as follows:
[6] I understand it is alleged that Dr Al Muderis dominates the group and imposes his view on the rest of us, if he deems the patient suitable for osseointegration. This is not the case. Dr Al Muderis is not an indecisive surgeon, and in my view he has good instincts and good clinical judgment, but he is also not inflexible and there have certainly been cases where another member of the group has changed his mind about the proper diagnosis or treatment.
[7] Ultimately, however, someone has to take responsibility for making a decision, and that is the surgeon holding the referral. If the patient was originally referred to Dr Al Muderis, the patient is his responsibility and it is up to him to make a call.
622 Consistent with that evidence, Dr O’Carrigan accepted in cross-examination that if the patient had been referred to Dr Al Muderis, he would ultimately be responsible for the patient. Dr Tetsworth described that Dr Al Muderis typically acted as the leader of the decision-making process. Further, Dr Stoita described:
I understand it is alleged that Dr Al Muderis will overrule the rest of us, if he thinks the patient is suitable for osseointegration and we do not. This is not true. He does not overrule others, but if the patient was referred to him, he is ultimately responsible for the patient and he is the one who must make the decision.
623 Dr Alttahir’s evidence was to a similar effect:
I understand that it is alleged that Dr Al Muderis “overrides” the surgical team regarding a patient’s suitability for surgery. This is not the case. There is a collective decision-making process between the surgeons. A consensus between the surgeons often determines the final decision, in conjunction with the patient’s preference for treatment options. The referring surgeon ultimately takes medical responsibility for the decision-making process, and hence they make the call on the surgical plan.
624 It follows then, that regardless of the opinion of others, if it is Dr Al Muderis’ patient, he ultimately makes the decision. That decision may be contrary to the opinions of others. That is not described by these witnesses as him overruling other opinions, but rather, as fulfilling his responsibility. That is rather a matter of semantics. It is a distinction without a difference. Moreover, on Dr Alttahir’s evidence, it is the views of the surgeons (as opposed to the broader multidisciplinary team) that are necessarily involved in the decision-making process. So much was also apparent from Dr Al Muderis’ evidence (addressed immediately below).
625 Second, the evidence reflects that from Dr Al Muderis’ perspective, the question as to whether a person is suitable for surgery is determined from an orthopaedic perspective. That was clear from Dr Al Muderis’ approach to Patient X, where he conceded in cross-examination that his focus was on an orthopaedic outcome (on mobility): see [784] below. This is also exemplified in Dr Al Muderis’ evidence in relation to the opinions expressed by Dr Basten (a clinical psychologist) in relation to Mr Ford (see [760] below), where he stated:
… he knows his limitation and his jurisdiction. He can comment on the psychological aspect of the patient, not on the rehabilitation aspect or the physical aspect of the patient.
626 As discussed below at [759]-[762], given Dr Basten’s report and the opinions expressed therein, it is difficult to understand how he is said to have exceeded his jurisdiction. It is also difficult to understand this in circumstances where Dr Al Muderis stated in his affidavit that:
I always listen to the opinions of my colleagues, and there have been times when I have changed my own opinion because one of my colleagues has persuaded me. If the psychologist considers that the patient is not mentally fit for the surgery, then his view always prevails.
627 Dr Al Muderis made similar comments in respect to Dr Andrew Paterson’s opinions about Mr Urquhart, where he referred to him in evidence as a pain specialist, and stated his advice is about pain management (implying, in the circumstances in which that was said, that it did not concern suitability of a patient for surgery): see [1523] below. Further, in response to a question about Dr Ho’s report which summarised Mr Warland’s issues with pain, Dr Al Muderis said:
Dr Ho is a pain specialist and he is – his – his assessment for Mr Warland is how to manage the pain. His assessment is not to tell me what to do with regards to the mechanical part of the surgery. Each individual clinicians that we have in the multidisciplinary team have their own job and we respect each other’s job and that is – there is a clear demarcation between – I don’t interfere with Dr Ho’s job about prescribing what medications for the patient and he doesn’t interfere with my job, telling me whether this patient is suitable for surgery or not because that – that designation is separate and each individual clinician has their own designation of how to treat the patient in accordance with their clinical ability, knowledge and skills.
It is difficult to understand how this attitude sits with his response to Mr Steinfort, that every person he works with “has equal influence and equal decision-making power”.
628 This evidence also reflects his attitude towards the opinions expressed by others in his team.
629 Third, the respondents submitted that repeatedly at trial Dr Al Muderis’ evidence oscillated. In some instances, for example, he sought to disclaim any responsibility for clinical decisions concerning his patients by saying they were matters for others, but in other cases (referring to Mr Ford), he denigrated the competence of other professionals or overrode their recommendations, despite their obvious cogency. I accept that his evidence did change, and seemingly did so when he provided answers which he considered best suited his case (at that time). As explained elsewhere, the applicant repeatedly gave evidence that, for example, he was not a pain specialist, psychologist or prosthetist, in answer to questions as to why there were no responses to requested help. At times, in cross-examination he answered that a particular observation (which tended to be contrary to his own) was merely proffered by a nurse, GP, plastic surgeon or other health professional, in response to not acting on information (or accepting information) from said individuals (e.g. nurse discharge summary in relation to Ms Çalan; opinions of Dr Frank Bruscino-Raiola in relation to Mr Mortimer as he is only a plastic surgeon; concerns about Patient X’s compliance recorded in a physiotherapist note as it was merely the physiotherapist’s view: see Part 6, Sections 3, 4, and 6), but on other occasions he relied on the views of others (e.g. radiologist reports in relation to Mrs Gollan and Ms Young: see Part 6, Section 8) If Dr Al Muderis considered a person suitable for surgery despite concerns expressed by other professionals, his view prevailed. He did override them.
630 I also refer to the discussion below in relation to Patient X: see Part 6, Section 3. In her case, the consultation report of 28 October 2021 sent to her GP records that bilateral osseointegration surgery was to be undertaken (given this was the consensus reached by the team). When pressed in cross-examination about Patient X’s concerns of bilateral surgery, Dr Al Muderis said that he “always” intended to only do surgery on the right leg. As discussed below, I do not accept his evidence as to intention. Regardless of the veracity of Dr Al Muderis’ evidence of intent, his evidence reflects that his attitude is that it was his decision, regardless of the opinion of others. That is, the team’s decision had no practical bearing on the surgery he would ultimately perform. On his evidence, the consultation report was “the conclusion of the team”, explaining “it’s a team decision, and the team wanted to do that”, but what mattered was his intention. On his evidence, that report does not accurately record, or inform the GP of the surgery to be undertaken.
631 Fourth, as discussed elsewhere, the patients from the United States and Turkey who gave evidence, generally did not have a multidisciplinary consultation, or if they were seen by other doctors, it was after they had fully paid for their surgery.
632 Finally, I note that Dr Paterson was not called to give evidence. Dr Paterson’s reports feature in several of the case studies, most prominently in relation to Mr Urquhart, although issues also arose in relation to other patients.
633 When it was put to Dr Al Muderis in cross-examination that Dr Paterson resigned from his team in November 2016, he gave evidence that although he resigned for a time, “he returned back and he has been working with us for many years now”. If he is working with Dr Al Muderis, then his absence as a witness stands in stark contrast to other members of his team who were called. Dr Paterson could give evidence on topics directly in issue in these proceedings (e.g. his report on Mr Urquhart). Some of the applicant’s witnesses gave evidence on the topic directly said to arise in relation to Dr Paterson, namely whether Dr Al Muderis overrides the opinions of others (being, inter alia, Dr Paterson’s opinion in relation to Mr Urquhart expressed in his consultation reports). The applicant submitted that the respondents could have issued a subpoena for Dr Paterson to give evidence, and without that Dr Al Muderis’ evidence in relation to Mr Urquhart’s consultation should be accepted. However, in circumstances where Dr Paterson is working with Dr Al Muderis, it would be expected if he were to be called, it would be by the applicant. I return to this topic when discussing Mr Urquhart’s case study.
Brochures – misleading statements
634 The brochure “Osseointegration: The Australian Experience”, published by Osseointegration International on about 30 August 2016 is a promotional brochure of 28 pages, with a large photograph of Dr Al Muderis on the cover. It features four case studies of successful osseointegration patients, including Mr Hernandez and Mr Grant. The brochure contains statements including:
(1) “perfect fit every time”;
(2) “Why settle for anything less than complete comfort for your mobility?” (under a photograph of a person with osseointegration walking along a beach);
(3) “There will be a small amount of discharge from the stoma. This amount varies from patient to patient and some have none at all”;
(4) “With normal daily hygiene the risk of infection is very low. Washing once a day in the shower, paying attention to the stump and stoma is all that is needed”; and
(5) “there is no permanent medication required”.
635 Those, amongst other statements, are alleged by the respondents to be misleading.
636 The respondents also alleged that this promotional brochure contains a number of misleading omissions, including that:
(1) osseointegration may fail;
(2) osseointegration may result in a patient’s stump becoming shorter, making it more difficult to use a traditional socket;
(3) osseointegration may result in serious infection, including osteomyelitis;
(4) osseointegration may increase the pain experienced by a patient;
(5) osseointegration may result in constant oozing and bleeding from the stoma for many years;
(6) the stoma may become infested with maggots; and
(7) osseointegration may result in hypergranulation, requiring painful treatment with silver nitrate.
637 Dr Al Muderis gave evidence that the brochure was written for use at conferences of the Amputee Coalition of America and its purpose was to showcase the technology of osseointegration. He said it was not written or used to advise patients about the suitability of osseointegration surgery for their personal circumstances. He said there was a clear disclaimer at the end of the brochure which makes it plain, amongst other matters, that the brochure is not for the purpose of providing medical advice. The applicant also disagreed with the respondents’ allegation that certain statements in the brochure were misleading.
638 It suffices to refer to three of the statements identified by the respondents as misleading in the Amended Defence (as set out at [634] above).
639 First, is the statement that: “[t]here will be a small amount of discharge from the stoma. This amount varies from patient to patient, and some have none at all”. Dr Al Muderis said it is true the amount of discharge from a stoma varies from person to person, and that patients do not always experience discharge. However, that evidence does not address the context of the statement itself, which commences by stating there “will be a small amount of discharge” (emphasis added). The next sentence must be read in this light.
640 Second, is the statement that: “With normal daily hygiene the risk of infection is very low. Washing once a day in the shower, paying attention to the stump and stoma is all that is needed”. Dr Al Muderis said it is true that the risk of infection is low with normal daily hygiene. However, this does not sit with his evidence that he told every patient when discussing the risks and complications of osseointegration surgery that “infection is a matter of when, not if”.
641 Third, is the statement: “Why settle for anything less than complete comfort for your mobility?” On page three of the brochure it also states: “Osseointegration surgery provides amputees with greater mobility, range of motion, comfort and quality of life”. The respondents submitted these statements convey to the ordinary reader that osseointegration is a pain-relieving procedure. Dr Al Muderis disagreed, noting the statements themselves do not say that. The applicant submitted that Dr Al Muderis’ view is plainly correct based on the ordinary use of the English language. The applicant submitted this is particularly so, in the context that the brochure only spoke about pain in connection with “socket related pain”. I disagree. The brochure read holistically (including patient cases referred to therein) implies to the ordinary reader that the procedure relieves pain. This is inconsistent with Dr Al Muderis’ evidence that osseointegration is not a pain-relieving procedure and a person cannot expect a pain-free experience. Rather, he said that osseointegration gives pain-free mobility, and improves mobility as compared to using a socket.
642 In relation to the alleged misleading omissions, Dr Al Muderis gave evidence that those matters are generally things about which a patient who is “actually considering osseointegration surgery” ought to be advised. He said such information did not need to be included in the brochure, since the brochure is not intended as medical advice or to advise patients of their suitability for surgery. However, the websites or brochures are designed to attract the attention of prospective patients. The brochure paints a positive picture of osseointegration, and as explained below, is used as a marketing tool. On the applicant’s evidence, it is only after the patient has taken the next step of considering surgery and having started the consultation process with Dr Al Muderis, that they then need to be told about other risks and complications. In a context where the brochure otherwise refers to risks, specifically the very low risk of infection with normal daily hygiene, or minimal discharge, the failure to refer to other risks associated with osseointegration is misleading.
643 The respondents also referred to material used in the United States to promote lectures at which Dr Al Muderis was to speak to patients and families. The flyer for a lecture held on 3 April 2015 in New York stated:
Dr. Al Muderis will discuss this ground breaking medical procedure, through which a stem made of a solid titanium core is implanted directly into the bone. The OPL connects directly to an external prosthetic device modeled on the anatomy of the human body, which promotes a more natural and pain-free experience.
644 A leaflet for a lecture in Texas on 4 November 2015, said:
The direct skeletal attachment promotes a more natural and pain free experience by utilizing the latest in implant technology, the Osseointegration Prosthetic Limb.
645 Again, I am satisfied from the passages in these promotional materials, that it would be understood by the ordinary reader that osseointegration provides an amputee with a pain-free experience. Those statements would not likely be understood as being confined to socket pain. As that is not so, the flyers are misleading.
646 The brochure “Osseo Integration: Direct Skeletal Prosthesis” (undated) published by Osseointegration Group of Australia, is said, on the respondents’ case, to downplay the risk of infection and implant failure. This has similarities with the brochure “Osseointegration: The Australian Experience” referred to above. This promotional brochure is 28 pages of the same ilk. It features six successful case studies.
647 In relation to the downplaying of risks, the respondents pointed to the responses in the “frequently asked questions” section of the brochure on page 26. This includes the response to the question “[w]hat are the risks of infection?”, where the respondents alleged Dr Al Muderis misrepresented the risk of infection by stating:
(1) “As with any surgical or invasive procedure, there is always the risk of infection, however, long term antibiotic therapy is not required for patients receiving the OGAAP-OPL”;
(2) “The patient may develop a minor infection at the skin-implant interface at approximately six weeks post-surgery. In the case of a suspected infection, the patient is advised to visit a general practitioner and obtain a culture swab of the wound. The general practitioner will then prescribe the appropriate antibiotic treatment for the patient”; and
(3) “Most minor infections can easily be managed with oral antibiotics, and patients are advised to consult the general practitioner whenever required.”
648 As to the question “[h]ave there been any failures?”, the brochure states in response:
To date, there has been no single case that resulted in the loss of the rest of the limb or bone of any patient. If the surgery does not work for some reason, the patient can always return to a socket prosthesis.
649 On the evidence, I am satisfied that the brochure downplays the risks of infection and implant failure.
650 The respondents also submitted that as at 2023 (as reflected in screenshots of websites), Dr Al Muderis’ two websites, www.almuderis.com.au and www.osseointegration.org, continued to claim that discharge will be a “small amount” and many patients will “have none at all”, and that the risk of infection is “very low”. That is so for the www.almuderis.com.au website. On the www.osseointegration website, printed on 8 July 2023, but as it appeared as at 31 March 2023, this description is slightly expanded upon, but still only stated under the frequently asked questions section that:
There is a risk of bone fracture during implantation, [this] happens in approximately 10% of cases in Sydney. A fracture MAY slow your rehab down by a few weeks however in the long term outcomes are comparable. There are risks of infection, in fact you are more than likely to have a soft tissue superficial infection in the first few weeks after surgery which is routinely treated with antibiotics.
651 To the question of whether there will be a “need to be on long term antibiotics”, the response is “[n]o, it is not needed routinely”. I note that the website also contained on this page a statement that “[n]o case is too challenging”. I am satisfied that the websites at that time downplayed the risks of osseointegration surgery.
652 These brochures, flyers and websites comprise public-facing material, that provide a very positive image of osseointegration surgery and Dr Al Muderis’ practice. As the respondents submitted, their content and tenor, portray happy patients with the surgery being successful, enjoying mobility, and a significant improvement to their quality of life. This is, in part, because the risks are downplayed. Where there is a reference to risks it is very limited. This is material designed to promote the procedure and encourage its use. It is directed at prospective patients. Mr Steinfort gave evidence that Dr Al Muderis’ promotional material painted a “rosy” picture, which is an apt description. It is to get people to book in a consultation. That is the image of the procedure a prospective patient has been presented at the time of organising a consultation. It can be inferred that this is a deliberate approach.
653 The evidence of the patients as to what they said they were told about the risks and complications of the surgery is against that background which, inter alia, reflects a preparedness to downplay the risks and complications.
654 The respondents’ case is that the applicant did not inform or properly inform his patients of the risks and complications of surgery. That is, if risks and complications were explained, they were downplayed. For the osseointegration patients, as discussed elsewhere, the consultation reports (with limited exception) refer to the risk of infection being low or relatively low. Patients said they were told the low risk of infection could be dealt with by antibiotics and presented it in a manner that made it seem like it was not an issue. A positive picture was portrayed.
655 The public-facing material referred to, including the websites and brochures, promoted the positives of the procedures. To do so, the material contains misleading statements and omissions.
Fundraising
656 It is appropriate to return to a topic referred to briefly when considering the evidence of Ms Stewart, that is, that patients were advised to fundraise in order to pay for surgery with Dr Al Muderis: see [462]-[463]. Although relevant because the applicant pleads a specific imputation is conveyed in the Broadcast which alleges that Dr Al Muderis lied to 60 Minutes about encouraging staff to teach patients how to fundraise for surgeries (Imputation [13.28]), it is has a broader import. It relates, amongst other things, to the context for some of his patients and reflects on Dr Al Muderis’ practice.
657 The applicant submitted that: he does not dispute that fundraising may have been discussed with patients sometimes; that “it is unclear why it matters if he did”; and that there is nothing unethical about a surgeon in private practice charging patients for surgery as they are entitled to be compensated. Given he alleges a specific imputation about fundraising, it is difficult to understand the suggestion that he does not know why it matters. It is patently obvious.
658 The applicant referred to the evidence of Ms Harris (his practice manager since 2020), that she never witnessed him suggest to patients how they might personally finance surgery, and to the evidence of Mr Laux, Ms Dean and Dr Alttahir, to the same effect. He submitted that the evidence of Ms Roberts was that she did not recall any conversations about fundraising, loans, mortgages, or otherwise in relation to Dr Al Muderis’ osseointegration patients. Dr Al Muderis also had no specific recollection of these matters, saying that patients may have used their superannuation or taken out loans, and that some people fundraise, but that the financing aspect was not something he generally involved himself in.
659 As referred to above, Ms Stewart gave evidence that she was told by Dr Al Muderis and Ms Bosley to tell overseas patients how to fundraise if they were concerned about money. She maintained this when challenged in cross-examination. As explained above, Ms Stewart’s evidence is supported by other evidence, including evidence of two emails.
660 First, is in an email by Ms Bosley to a prospective patient from the United States, dated 8 January 2016, where she noted that they did not offer payment plans for international patients, but stated that “the other possibility is looking at fundraising or taking a loan in the US to cover the cost of your surgery”. Given Ms Bosley’s position (who it is to be recalled previously worked as Dr Al Muderis’ clinical and research coordinator and business manager) and in light of the context of other evidence of the patients referred to below, the compelling inference is that such suggestions were made with the applicant’s knowledge.
661 Second, is in an email exchange in September 2016 between Dr Al Muderis and another doctor in the United States, where that doctor informed Dr Al Muderis of a prospective patient interested in osseointegration but noted that funding would be a problem. Dr Al Muderis responded, copying Ms Bosley, stating inter alia, “[w]e may need to start a discussion with the patient to teach him how to do fund raising for his surgery”.
662 The applicant submitted this email was not shown to him during the hearing, and he has not been given an opportunity to address the issue, and therefore the allegations about fundraising should not be entertained. I do not accept that submission. The email is in evidence.
663 It is necessary to put that submission in context. In the Broadcast, Dr Al Muderis was asked by Mr Steinfort whether he had encouraged his staff to teach patients how to fundraise, to which he responded: “No. That’s never happened. That – I’m actually – as a matter of fact I’m very strongly against that. GoFundMe and these things we don’t allow it”. Dr Al Muderis went on to emphasise that he never has, and “never will” do this:
[d]efinitely never encouraged any of the staff or any person. This is not my practice. This is not what I would do. This never happened in – in the past, would never happen in the future.
664 At one stage, as part of the above passage of questions, the transcript of the raw footage of Dr Al Muderis’ 60 Minutes interview records that he also said “as a matter of fact, I’m philosophically oppositional to anyone raising money or go and GoFundMe to pay for their surgery”. Although this statement was not included in the Broadcast, the SMH and The Age Online Articles refer to it. The Broadcast then explained that there were leaked documents:
leaked documents tell a different story with an email from the surgeon himself suggesting his staff teach a patient how to do fundraising for his surgery. Another email shows an employee proposing a different patient look at fundraising or taking a loan so they could afford osseointegration.
665 It is plain from the Broadcast there were two leaked emails, one of which was an email from Dr Al Muderis. These are the two emails referred to above. The content of Dr Al Muderis’ emails was published in some of the Publications complained of, being the SMH and The Age Online Articles. Dr Al Muderis was plainly on notice of the existence of the emails – they are from his business. Despite that, he chose to plead the imputation he did in relation to the Broadcast. These two emails are in evidence, to which there was no objection. Although the September 2016 email does not appear to have been put to him in cross-examination, it can hardly be said that the applicant was not on notice about its existence, nor that he was unaware of its contents. The submission that he has not been given an opportunity to comment on it, given the circumstances, cannot be accepted. He could have commented but chose not to.
666 Pausing there. Dr Al Muderis’ statement to Mr Steinfort that he is “philosophically oppositional to anyone raising money or go and GoFundMe to pay for their surgery”, although not published in the Broadcast, was made by him for publication. It is in the other Publications. When Dr Al Muderis made the statement, he was not to know it would not be part of the Broadcast. It was a gratuitous statement, it can be inferred, said to lend sincerity and veracity to his denials, reflecting he was morally opposed to fundraising as a means of paying for surgery. He embellished his denials, to make them sound more convincing. This was said in a manner which also sought to achieve that. His denials about not advising about fundraising (and getting Ms Stewart and others to advise) are untrue. His preparedness to not only lie to the public about fundraising, but to embellish that lie in the manner he did tells generally against his credit.
667 His knowledge and involvement in suggesting fundraising is also supported by the evidence of patients. Ms McIntyre, Ms Ulrich and Mr Bruha each gave evidence that Dr Al Muderis said to them that one way to raise money to pay for the surgery was to fundraise.
668 Although the applicant submitted that he did not dispute fundraising may have been discussed, he denied for example, in his affidavit that he discussed fundraising with Ms McIntyre as alleged, but did not otherwise elaborate further. In cross-examination, he purported to have no recollection of conversations to that effect with Mr Bruha, Ms Ulrich or Ms McIntyre. He said that he did not recall: telling Mr Bruha that “fundraising is one of the ways patients have paid for their surgery”; telling Ms Ulrich that “some people fundraise, some people put their house up and take a mortgage”; or telling Ms McIntyre that a lot of patients choose different ways to raise the money whereby “[s]ome patients have private means. Some patients take out personal loans and some fundraise”. Dr Al Muderis’ evidence in cross-examination was that he does not go into details with patients about how to raise funds. I note that shortly after that first meeting between Ms Ulrich and Dr Al Muderis, Ms Ulrich started a “GoFundMe” online fundraiser and raised around US$20,000 from contributors. Mr Bruha also undertook fundraising to finance his surgery. I accept the evidence of each of those witnesses, that Dr Al Muderis raised fundraising with them.
669 I am satisfied that Dr Al Muderis, and others on his instruction, raised fundraising with some prospective patients as a means of obtaining the funds to pay him for surgery.
670 I am satisfied that the respondents have established that Imputation [13.28] – that he lied to 60 Minutes about encouraging staff to teach patients how to fundraise for surgeries – is substantially true.
Section 2 — Ms Megan McIntyre and Mr Donald Grieve
Ms Megan McIntyre
671 Ms McIntyre was an honest, credible, and reliable witness. I accept her evidence.
672 Ms McIntyre owns a business as a horse trainer. She lives on and tends to a rural property in South Australia, which requires physical labour. She lives a very active lifestyle. As a result of an accident in 2016, she has a right below-knee amputation.
673 She attended the consultation with Dr Al Muderis to discuss osseointegration on 24 May 2018. She was seeking a second opinion, having spoken to a surgeon in Adelaide, Dr Tom Savvoulidis. She gave evidence that Dr Savvoulidis told her that one concern with having the surgery was that, as a horse trainer, her working environment exposed her to a higher risk of infection. Dr Al Muderis opined in the consultation report that she was suitable for surgery, and it was “reasonable and necessary” that she be offered it. Ms McIntyre chose not to undertake the surgery.
674 On arriving at Dr Al Muderis’ clinic, Ms McIntyre was directed where to sit, which was between two women who had positive outcomes from the surgery. One was a fellow horse rider.
675 Aspects of the events thereafter are in dispute and are significant.
676 First, her consultation involved Dr Al Muderis and Ms Roberts, and although she accepted there were others in the room, her evidence was that they were not participants in the consultation. I note that nonetheless the consultation report lists other participants who purportedly consulted with Ms McIntyre, which does not accurately reflect what occurred. In cross-examination, Dr Al Muderis did not recall Ms McIntyre, and his evidence that there were seven people involved in the consultation is evidently based on the information contained in the consultation report. I have addressed the question of reliability of these reports above.
677 Second, and more concerningly, Ms McIntyre gave evidence that there was a discussion about the risk of infection with Dr Al Muderis, including him telling her that there was a higher risk of infection in her case because of her work environment and lifestyle. Despite that, as Ms McIntyre pointed out, the consultation report she and her doctor received described the risk of infection associated with her surgery as relatively low (in the same pro forma way as discussed previously, as with many of the consultation reports in this case generated by Dr Al Muderis). That was one of three errors Ms McIntrye identified on reading the report (which included incorrectly recording her date of birth). Dr Al Muderis’ evidence was that the words he said to Ms McIntyre relating to risk were those captured in the report: “we regard Megan as relatively low risk. Her procedure would be very standard”. Given that the context for her consultation included that one of her concerns was that she may be a higher infection risk, it is likely that she would accurately recall the advice given to her.
678 Ms McIntyre also gave evidence that Dr Al Muderis told her if she followed his protocol she would have “little to no complications” following the procedure. That is to downplay the risks and complications. The consultation report similarly stated the “complication rate for the procedure has been extremely low”.
679 Third, Ms McIntyre gave evidence that the reference in the report to the “phantom sensation” being “troublesome for [her]” is inaccurate. Although, in a pre-surgery questionnaire she answered “yes” when asked if she experienced phantom pain, she did so because there was no category to describe her distinct feeling. Dr Al Muderis deposed, citing the pre-surgery questionnaire, that Ms McIntyre answered that she did experience phantom limb pain, had experienced it several times in the last week, and that on average each episode lasted several hours.
680 However, Ms McIntyre’s evidence was that she subsequently told Dr Al Muderis during the consultation that she did not experience phantom pain, but more a sensation like pins and needles. Moreover, Ms McIntyre’s evidence was that she never implied that the sensation was “a large enough issue to require additional [TMR] surgery” and that it was odd to her that a surgeon would suggest TMR surgery in that context.
681 The applicant submitted that Ms McIntyre, in giving evidence that the report was inaccurate in recording that “phantom sensation is … troublesome for Megan”, misread the report. He asserted that she agreed, in cross-examination, that “phantom sensation” was discussed as set out in the report. That is a strained reading of the evidence. At no point did Ms McIntyre agree her experience with pins and needles was a “phantom sensation”, nor did she ever describe it in those terms. That said, although the report is not correct, I accept that it may have been a result of a misunderstanding in the circumstances.
682 Fourth, Ms McIntyre’s evidence was that during the consultation, Dr Al Muderis implied that his implants were superior to those used by other surgeons. He told her that the implant that would be used was designed by him and was the best available. He said words to the effect of: “I am the most experienced surgeon at performing this surgery in Australia and we have the most experienced team.” When she told him she had seen Dr Savvoulidis, he said words to the effect of: “I believe he’s not very experienced”.
683 Ms Roberts gave evidence that Dr Al Muderis did not make that comment about Dr Savvoulidis. Dr Al Muderis denied discouraging her from seeing any other surgeon and suggesting to her that Dr Savvoulidis was not very experienced.
684 Fifth, Ms McIntyre’s evidence was that during the consultation she asked about the price of the procedure. Either Dr Al Muderis or Ms Roberts suggested that the procedure would be somewhere in the region of $40,000 to $50,000 out of pocket. Dr Al Muderis said it might be more if something went wrong with the surgery. He said words to the effect of:
A lot of patients choose different ways to raise that money. Some people decide to re-mortgage their homes. Some patients have the private means available. Some patients take out personal loans. And some fundraise.
685 Ms McIntyre told him she did not own her home and was not in a position to get a personal loan for that sort of money, so she would have to go the fundraising route. Ms McIntyre’s evidence in cross-examination was that she then turned to her friend Rachel, also present at the consultation, and mentioned they could do chocolate fundraisers like they do in primary schools. Dr Al Muderis laughed and said words to the effect of: “that’s a lot of Freddo Frogs”.
686 The applicant submitted that Ms McIntyre’s oral evidence that she was the first to raise the notion of chocolate fundraisers “wholly undermines her allegation”. Whether she or Dr Al Muderis was the first to do so is immaterial. Ms McIntyre’s evidence otherwise demonstrates that Dr Al Muderis was the first to raise the topic of fundraising more broadly.
687 Ms Roberts’ notes from the consultation on 24 May 2018 do not reflect that fees were discussed. In their affidavits, Dr Al Muderis denied discussing fundraising with Ms McIntyre, and Ms Roberts did not recall whether any discussion of fees occurred. In cross-examination both Ms Roberts and Dr Al Muderis accepted they could not recall whether conversations about fundraising had occurred. I note Dr Al Muderis does not dispute that fundraising may have been discussed with patients sometimes. Ms McIntyre’s evidence that he raised fundraising is consistent with the evidence of some other patients (e.g. Ms Ulrich). I do not accept Dr Al Muderis’ evidence that he did not discuss fundraising with Ms McIntyre.
688 Sixth, Ms McIntyre’s evidence was that she felt rushed. She said she felt pressured by Dr Al Muderis to have osseointegration surgery. Dr Al Muderis told Ms McIntyre that if she did not proceed with the operation quickly, her bone density would decrease because she was not weightbearing. Dr Stalley expressed the view that this advice had been misguided and there was no urgency on that basis for having the procedure. Ms McIntyre thought Dr Al Muderis was trying to convince her that the sooner she had the procedure the more likely it would succeed. He told her that she would never be comfortable in a traditional socket and suggested that she would always have skin breakdowns. Ms McIntyre felt that the consultation report, which she read at a later stage, put more pressure on her to get the surgery. She identified parts of the report in her evidence.
689 That feeling is logical given the terms of the report and its recommendation. A plain reading of it is that it was designed to promote the surgery being done in a timely manner.
690 The applicant submitted Dr Al Muderis’ warning about the risk of worsening muscle atrophy and osteoporosis (in the report) was not to put pressure on Ms McIntyre, but a statement of medical fact. That submission ignores that that medical fact, if true, would pressure Ms McIntyre to proceed with the surgery in circumstances where Dr Al Muderis has utilised it in his report. The inference is there is an urgency. In circumstances where Dr Al Muderis was applying other pressures (e.g. to raise funds), that Ms McIntyre felt pressured to proceed with surgery because of a purported urgency, is readily understandable irrespective of whether the surgery was in fact urgent.
691 Ms McIntyre also gave evidence that she told Dr Al Muderis she intended to consult with other practitioners for their opinion on her best treatment options. He said words to the effect of: “That’s entirely up to you, but I feel that once you’ve done your research, you’ll be back”. I note that this is consistent with other evidence as to comments made to patients that they would be back (e.g. Mr Grant).
692 Despite obviously wanting time to consider her position, which was entirely appropriate, only four days later, on 28 May 2018, Ms Roberts rang Ms McIntyre to follow up on the initial consultation and left a voicemail. It can be inferred Ms McIntyre did not respond. On 6 June 2018, Ms McIntyre received a further follow up email from Ms Roberts. By this stage, Ms McIntyre had decided not to proceed with the surgery with Dr Al Muderis. She does not recall responding to the correspondence.
693 As explained above, Ms McIntyre has never had the procedure. She continues to use a socket prosthesis, having recently changed her prosthesis and obtained an improved prosthetic foot which has been effective.
694 Where there is a dispute in the evidence as to what occurred, I prefer the evidence of Ms McIntyre. Ms McIntyre did not undergo the surgery and there is no obvious reason for her to be involved in this matter, except that she feels compelled to speak of her treatment. Her evidence is supported by other evidence.
695 I accept her evidence that Dr Al Muderis told her that there was a higher risk of infection given her circumstances. This is a topic which Dr Savvoulidis raised with her and given the circumstances, it can be inferred that it was a topic of interest to her. In my view the consultation report does not accurately reflect what occurred in the consultation.
696 I accept that the conversation concerning fees and fundraising occurred as she describes, with Dr Al Muderis first raising the issue of fundraising. As Ms McIntyre’s evidence reflects, she was concerned about the cost of the surgery. This was in circumstances where she did not have private health insurance. Again, that she would raise the topic that would lead to a discussion concerning fees and fundraising is credible. Other patients gave evidence that Dr Al Muderis discussed the cost of surgery when meeting with him (e.g. Mr Wynne, Mr Bruha and Mr Smith), and others gave evidence that he raised fundraising (e.g. Mr Bruha, Ms Ulrich, and see Fundraising in Part 6, Section 1 above).
697 I also accept that Dr Al Muderis said Dr Savvoulidis was not very experienced while bolstering or promoting his own experience. That Dr Al Muderis stated in his consultation report that he was “more than happy” for Ms McIntyre to pursue osseointegration under the care of Dr Savvoulidis should she prefer, does not detract from the reliability of Ms McIntyres’ evidence on this topic. This is also consistent with his general approach when referring to other doctors (e.g. questioning Dr Huang’s experience in relation to Mr Urquhart, and the evidence of Ms Mattiske that he “verbally denigrates, knocks other surgeons”, noting also that was his approach in conducting this hearing). I note also that in the circumstances, the unsolicited follow up with Ms McIntyre shortly after her consultation gives rise to an inference that Dr Al Muderis was courting her business.
698 I accept that Ms McIntyre felt pressured into undergoing the surgery. As previously described, the consultation reports are written in a manner that would lead the reader to consider that, as Dr Al Muderis writes in the report, it is necessary to undergo the procedure, and in a timely manner (or otherwise her bone density would deteriorate). The report downplayed the risks, using what appears to be pro forma language (despite having told Ms McIntyre during the consultation that she had a higher risk of infection). It also described her condition in such a way to suggest it was necessary, while at the same time saying how experienced Dr Al Muderis is, that the functional capacity in all the cases increased dramatically, and the complication rate has been “extremely low”. For example, it states:
… her activity level has declined in an accelerated fashion.
…
Unfortunately, Megan is not performing optimally with a socket, it is likely her condition will continue to deteriorate with muscle atrophy and osteoporosis which will be irreversible without intervention.
I believe that it is reasonable and necessary that Megan be offered this surgery.
…
Due to the increasing challenges Megan is experiencing, it is my opinion and I do believe that it is necessary that she be offered this procedure and would expect to see an improvement in Megan’s quality of life.
He promoted his experience. Having told Dr Al Muderis that she wanted to consider her position and to do more research, she was quickly and repeatedly followed up by the LRC in the manner described.
699 Ms McIntyre described that upon leaving the consultation she was hopeful that she could have the surgery, but from her perspective, when she returned home and discussed her experience with her partner, she realised that she had ignored some red flags.
Mr Donald Grieve
700 Mr Grieve is Ms Grieve’s father. Mr Grieve is a left below-knee amputee. Since February 1963 he has been ambulatory with the aid of a socket prosthesis. Mr Grieve consulted with Dr Al Muderis for advice on osseointegration on 25 October 2018 at the Complex Reconstructive Clinic at Hurstville Private Hospital. He was 74 years old at the time.
701 He gave evidence he was concerned about phantom pain. That was the only reason he was interested in osseointegration. He gave evidence that he had heard Dr Al Muderis speak about his life at a meeting at the Australian Club and he took the opportunity to ask him whether osseointegration helped with phantom pain, which Dr Al Muderis confirmed at the time. On being told it does, he decided to obtain a referral to Dr Al Muderis and book in a consultation. He also gave evidence that before the consultation he had read Dr Al Muderis’ book in relation to his life and enjoyed it. He had regard for Dr Al Muderis from the talk he attended and was impressed by his book. He had researched osseointegration.
702 Before the consultation, Mr Grieve completed various paperwork, had his legs x-rayed and undertook a bone density test.
703 What occurred at the consultation is in dispute. Mr Grieve’s evidence was that Dr Al Muderis told him words to the effect that he was ideally suited to undergo osseointegration. Dr Al Muderis said words to the effect that “[y]ou are now in your mid-70s and I expect that if you do not undergo [osseointegration surgery] you will be wheelchair-bound by the time you turn 80”. He said he would lose mobility and be wheelchair-bound within five years. He was told he could be immobile within a year.
704 As Dr Al Muderis said this, he drew a graph on the back of Mr Grieve’s x-ray envelope to model what he said was, and would be, Mr Grieve’s mobility over time, including the prospective impact of having osseointegration. Mr Grieve produced the x-ray envelope.
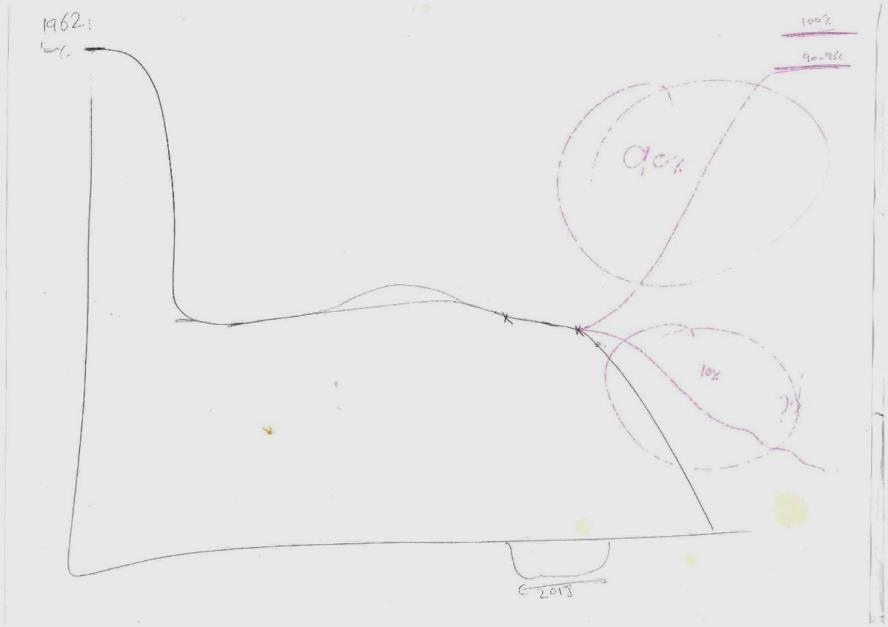
705 Mr Grieve said that only Dr Al Muderis spoke during the consultation, and the questions he asked were ignored. He said the consultation took, at most, about ten minutes. On leaving the consultation, he saw Mr Laux, who he knew. Mr Laux advised against having the procedure given the risk involved. Mr Grieve did not undertake the surgery, and his mobility continues to be as it was in the years before October 2018. He plays 18 holes of golf twice a week, walking the first ten.
706 Dr Al Muderis’ evidence was that himself, Dr Stoita, Dr O’Carrigan, Dr Basten, Mr Laux and “others” were in attendance during the consultation. He also gave evidence that he and nine other medical practitioners reviewed Mr Grieve. Dr Al Muderis denied that he told Mr Grieve he would be in a wheelchair within five years unless he underwent the surgery. Dr Al Muderis said Mr Grieve told him that his mobility had started to decline slightly in 2018. Following the consultation, Dr Al Muderis sent a consultation report to Mr Grieve’s GP, Dr Bruce Greig. The report is undated (only noting the date of the consultation) but his medical file records it was sent on 9 November 2018. The report, which is in evidence, suggests it was copied to Mr Grieve’s email address.
707 Mr Grieve gave evidence that although he recently discovered his GP had received a copy of the report, he had never received a copy or discussed it with his GP, and that the report was not an accurate reflection of the consultation. Dr Al Muderis relied on this consultation report in giving evidence.
708 Dr O’Carrigan gave evidence that the advice given at the consultation was that, as Mr Grieve had good mobility and function with his socket prosthesis, osseointegration was of no advantage to him. He had no recollection of the graph being drawn but did not dispute it. He accepted in cross-examination that Dr Al Muderis “could have” told Mr Grieve that if he had osseointegration surgery he could expect his mobility to improve to 90-95% of what it had been prior to the accident.
709 Ms Roberts also gave evidence of persons (besides herself and Dr Al Muderis) who were at the consultation. However, her evidence did not entirely accord with the consultation report as she said Dr Tetsworth was present, which is not recorded. She said that the consultation lasted about an hour. She did not observe Dr Al Muderis drawing a graph on the x-ray envelope. She said she did not deny it was drawn, but that she is often writing notes and therefore is not aware what is occurring around her. She accepted her memory of what occurred at the consultation was incomplete.
710 Mr Laux also gave brief evidence of the consultation. He said he probably was not in the room for the whole consultation, but rather in and out of the room “quite a few times because … we consult and treat patients at the same time”. He did not see Dr Al Muderis draw the graph. He did not know whether he was in the room at the end of the consultation. Mr Laux gave evidence that he does not believe that Dr Al Muderis was pressuring Mr Grieve into the surgery. That evidence must be viewed in light of his concession that he was in and out of the room and did not see Dr Al Muderis draw the graph. He also gave evidence that Dr Al Muderis advised Mr Grieve there is no need for osseointegration if he is able to walk without issue and is mobile, which I note is not inconsistent with Mr Grieve’s account.
711 Dr Stoita conceded during cross-examination that his evidence of the consultation is based entirely on the consultation report, and he has no independent recollection of the events.
712 In summary, none of the applicant’s witnesses gave evidence of or recalled that a graph was drawn by Dr Al Muderis, although Dr Al Muderis himself accepted as much. Mr Grieve’s evidence of the drawing of the graph during his conversation with Dr Al Muderis is in the context of the lack of evidence from those witnesses. The applicant’s witnesses’ evidence was generally reliant on the consultation report, which Mr Grieve said is inaccurate.
713 Although Mr Grieve was somewhat curmudgeonly at times when giving evidence, his evidence was given in a direct and straightforward manner. He had a good recollection of events. My clear impression is that Mr Grieve was honest, credible and reliable. I accept his evidence.
714 This was Mr Grieve’s only consultation with Dr Al Muderis, and he had organised it for a purpose. He has cause to remember the events. This is to be contrasted to the other persons who were present, where this was one of very many consultations attended over the years. For them, there is no particular reason to remember this one consultation. Dr Stoita’s evidence in this respect is illustrative: “I see about 100 patients a month or so, even more. So it would be impossible to remember [this consultation with Mr Grieve]”.
715 On the other hand, Mr Grieve, whose mobility had been largely stable since his accident, had been told that was to rapidly change. His evidence was that he was extremely concerned about what he had been told and as a result consulted his prosthetist. He did not have the procedure and his mobility, as noted above, has continued to be as it was in the years before October 2018.
716 The graph Dr Al Muderis drew during the consultation which Mr Grieve kept, supports key aspects of Mr Grieve’s evidence of what occurred.
717 The diagram depicts a black line, which Dr Al Muderis and Mr Grieve agree demonstrates what happened to Mr Grieve’s mobility in the period after his accident, including a stable but lower level of mobility in the 50 years following. Dr Al Muderis gave evidence that he drew the line dropping around the period marked “2018” because Mr Grieve conveyed to him that his mobility was on the decline in the period leading into and including 2018. Mr Grieve did not directly address this point in his evidence (although he explained that “the section on the y-axis to the right of [the] notation [“2018”] was intended to be in the order of one year”).
718 Although the meaning of the graph in the period following 2018 is mostly in dispute, Dr Al Muderis and Mr Grieve agree that the black line, which declines sharply, depicts a very quick drop off in mobility down to nothing (i.e. to being wheelchair-bound). They also agree that the upper most line (with the entry 90%), in pink, shows an increase in Mr Grieve’s mobility back to 90-95% of his 1962 level, which he would eventually enjoy if he underwent osseointegration.
719 A second downward line (with the entry 10%) is less sharp and is also in pink. It appears to depict a scenario in which Mr Grieve’s mobility as at 2018 will suffer over time, but does not diminish to zero. Mr Grieve, in cross-examination, did not understand the meaning of this third line and did not recall what was said to him about it. Dr Al Muderis’ evidence was that the line represented a “realistic expectation” for Mr Grieve if he continued with his socket prosthesis. I return to the possible meaning of the third line below.
720 The obvious reading of the graph reflects that it was drawn to create the impression that without osseointegration, his mobility, which had been stable for about 50 years, would rapidly decline, but if he undertook the operation, he would regain 90-95% of his pre-amputation mobility. The compelling inference from the diagram is that it was drawn to convey to Mr Grieve that unless he underwent osseointegration, his mobility would be in serious decline in the short term. Although Dr Al Muderis gave evidence that the black line represented a decline in mobility per “the statistics from the literature”, as opposed to Mr Grieve specifically, Dr Al Muderis (nor his counsel) pointed to any such literature. That this line is drawn in black (and not pink), as is consistent with the line mapping his progress to 2018, also suggests it is the scenario that will eventuate if Mr Grieve’s circumstances (being his use of a socket prosthesis) continue.
721 No other credible basis for the diagram was ventured. The suggestion that the diagram was not drawn to scale does not alter that. The year 2018 is marked, being the time of the consultation. Mr Grieve was then 74 years old. If Mr Grieve’s mobility was stable and had been for 50 years, there was no need to draw a diagram to illustrate that to him.
722 As to the third line, several circumstances give colour to its possible meaning. First, the figure “10%” accompanies this line; accompanying the upward sloping line is the figure “90%”. Second, both lines are drawn in pink. Third, Mr Grieve gave evidence that, in asking Dr Al Muderis of the downside risk in this procedure, Dr Al Muderis said words to the effect of:
The risk of failure is no more than 10%. But if the procedure is not successful I would simply proceed to amputate your leg above the knee and to insert titanium rod in your residual femur.
723 I note counsel for the applicant agreed Mr Grieve was told of the 10% failure rate for transtibial osseointegration.
724 It can be inferred, therefore, that the two pink lines represent the scenarios Mr Grieve would face if he underwent the procedure, wherein there is a 90% chance of his mobility being restored to 90-95% of its pre-amputation level or, alternatively, a 10% chance of failure, further amputation, and concomitant decline or uncertainty in his mobility. The two question marks on the y-axis (measuring mobility), as well as the waves toward the end of the downward-sloping line, suggest Mr Grieve’s expected mobility, on this scenario, was uncertain but likely to decline. Indeed, the pink lines reflect the scenarios Mr Grieve faces if he undergoes osseointegration; the black line reflects his fate if he continues to use a socket prosthesis.
725 Although this interpretation of the third line provides additional support to Mr Grieve’s overall account of the graph, it is inessential to conclude whether that is so. I note there is no fourth line predicting continued stability in Mr Grieve’s mobility, a scenario which has eventuated.
726 Mr Grieve’s evidence is also supported by a letter he sent to Dr Al Muderis via email the morning after the consultation, in which he thanked Dr Al Muderis for his “valuable, if rather gloomy, advice as to what lies ahead for me.” That the advice he received had been “gloomy” supports Mr Grieve’s recollection of events. Further, Mr Grieve gave evidence that following the consultation he sought advice from his prosthetist, Mr David Howells, because he was concerned about Dr Al Muderis’ expectation that he would become wheelchair-bound unless he underwent the procedure. The fact of seeking further advice is also consistent with his evidence as to what occurred at the consultation. He gave evidence he acted on the further advice and did not have the surgery.
727 Mr Grieve’s 9 June 2022 email to his daughter is also consistent with his version of events. It was sent in the early stages of Ms Grieve’s investigation, and prior to the commencement of these proceedings:
When I saw Al Muderis, [Stefan Laux] was there and I had a brief discussion with him, the upshot of which is that he agreed with my assessment that the risk of failure was far too great and that my preference to continue using a socket prosthesis was probably sound. One thing that I do recall from the consultation (with Al Muderis) was that he (very aggressively) forecast that if I did not undergo osseointegration I would probably be wheelchair-bound by [the] time I was in my early 80s. I passed that forecast on to David Howells who said that it was ridiculous … his patients included several amputees in their 90s who were continuing to cope very satisfactorily with socket prostheses.
728 I accept Mr Grieve’s evidence as to what was said and done by Dr Al Muderis when drawing the graph. The impression it created was clear. The applicant’s submission in closing that it was done to emphasise why Mr Grieve does not need surgery is inconsistent with the graph and unpersuasive.
729 The applicant submitted that Mr Grieve’s account should be rejected in circumstances where it is contradicted by other witnesses’ evidence and contemporaneous documents, particularly the consultation report. He also submitted that Mr Grieve cannot be regarded as an independent or disinterested witness and that he came for the purpose of supporting his daughter and assisting her defence.
730 I have addressed the reliability of Dr Al Muderis’ medical records elsewhere. Suffice to say that Mr Grieve disagreed with several aspects of this report, particularly its recommendation, on which the applicant’s submission partly relies:
Donald would be a very good candidate for osseointegration however he is functionally well enough that he can continue to perform well with the socket prosthesis. I have advised Donald to avoid osseointegration for the time being until he goes downhill. Donald will consider his options and he will see us if needs to. We have advised Donald to stay with the socket for the time being.
(emphasis added)
731 The recommendation’s terms, as emphasised, are curious. Mr Grieve denied that words to that effect were said to him. At first blush, the terms sit uncomfortably with Mr Grieve’s account. Strictly speaking, however, they are not inconsistent with Mr Grieve’s evidence about what was said. That Mr Grieve “can continue” to perform well with his socket prosthesis and is advised to “avoid osseointegration for the time being until he goes downhill” does not preclude that he was given advice that he should undergo the procedure as a matter of some urgency. The graph also depicts that when he starts to deteriorate, the rate will be rapid. I note that this is in a context where Mr Grieve had informed Dr Al Muderis that he could not undergo any surgery for at least a year due to medication he was taking for a cardiovascular condition.
732 In any event, it is apparent that the report, given the force of Mr Grieve’s evidence (as outlined), distorts the advice Dr Al Muderis gave during the consultation. In omitting details of the conversation (which is supported by the graph), which infers an apparent urgency of Mr Grieve’s case, the report is misleading. It follows that the applicant’s witnesses’ evidence about the consultation is tainted to the extent it relies on this report, which is generally the case.
733 I note that Mr Grieve is only one of several witnesses who gave evidence that the consultation reports or documents did not accurately record the events.
734 In closing submissions, the applicant made several allegations about Mr Grieve’s candour. Although some were later withdrawn, and the applicant submitted it was not necessary to make a finding of dishonesty, but rather unreliability, that is not the way in which Mr Grieve’s cross-examination was conducted on some topics. The applicant’s case is not that his evidence was unreliable, but that it was false. Ultimately, the applicant submitted that he confined his case on dishonesty to what was asserted in cross-examination.
735 In cross-examination, it was put to Mr Grieve that his evidence of the content of the Australian Club conversation with Dr Al Muderis was false. I do not accept that submission.
736 The conversation occurred on 5 June 2018. Mr Grieve said he had asked Dr Al Muderis whether osseointegration relieved phantom pain, and he said “certainly”.
737 The applicant made several related submissions challenging the veracity of Mr Grieve’s evidence on this point. First, that Mr Grieve’s evidence that phantom pain was the only factor of interest to him in seeking to consult Dr Al Muderis should be rejected. He pointed to an email dated 11 June 2018 that Mr Grieve sent to Dr Al Muderis following up on their initial conversation. He asserted Mr Grieve’s evidence was inconsistent with that email because it says nothing about phantom pain. Second, that it is unlikely that Mr Grieve asked about phantom pain during the one- or two-minute conversation given that phantom pain was, in Mr Grieve’s words in 2018, an “exceptionally irregular” occurrence. Third, the applicant submitted that Mr Grieve’s evidence, being that it was incorrect to say he had very little phantom pain in 2018, should be rejected. In this regard the applicant relied on a range of documentary evidence, including:
(1) Mr Grieve’s referral letter to Dr Al Muderis from his GP, which discloses nothing about phantom pain or ongoing pain medication;
(2) an online patient information form for Dr Al Muderis, in which Mr Grieve stated he experiences phantom pains “quite irregularly and not, in any [sense], chronically”;
(3) Dr Basten’s pain and psychological questionnaires, in which Mr Grieve seemed to report low levels of phantom pain, phantom pain episodes lasting 30-45 seconds (noting none occurred in the week prior), and that phantom pain had not interfered with his normal lifestyle in the week prior (but see Dr Basten’s summary of Mr Grieve’s experience with pain, below); and
(4) an email from Mr Grieve to Ms Roberts, in which he reported a “minimal incidence of pain” and that phantom pain was “exceptionally irregular”.
738 In so far as the applicant relies on the 11 June 2018 email and referral letter to challenge Mr Grieve’s evidence, it does not follow that he did not experience phantom pain because it is not mentioned in those documents. Mr Grieve himself recognised as much during cross-examination.
739 In so far as the applicant relies on evidence that Mr Grieve’s pain was “irregular”, of “minimal incidence” and “not … chronic”, his submissions seem to emphasise Mr Grieve’s rate of pain while ignoring its severity. Yet both frequency and severity are relevant considerations, as is reflected in Dr Basten’s pain questionnaire (and Mr Grieve’s responses).
740 Mr Grieve has experienced phantom pain of varying severity (despite aspects of his answers to the pain questionnaire suggesting otherwise). In a pre-consultation form, he explained he is “not pain-free and would like to know more about the osseointegration process as a possible alternative” to his socket system. Dr Basten’s report on Mr Grieve, which apparently accounts for Mr Grieve’s responses in the pain questionnaire, also supports as much. His report disaggregates Mr Grieve’s rate and severity of pain:
He is interested in OI because he gets some chaffing on the lateral side of the tibia and in the hope that the surgery might alter his moderately severe occasional phantom limb pain.
(emphasis added)
741 Mr Grieve’s evidence in cross-examination was that he experiences “phantom pains from time to time, of varying severity, but generally speaking they’re not an overriding problem”. He has, on one occasion, required painkillers for “abnormally prolonged phantom pains”.
742 Although the applicant submitted Mr Grieve made up his evidence to assist his daughter (given that one of the allegations in the proceedings is that Dr Al Muderis promises pain relief), the evidence he relies on does not support that. The occurrence of the conversation in the Australian Club is plausible (the evidence supports he suffers such pain), and that Dr Al Muderis gave a positive response. It is unclear how this is said to assist his daughter. It will also be recalled from the discussion above, that “Osseointegration Surgery A Guide for Patients” dated 1 May 2018 (being a document available for patients to read in the waiting room), states that the implant being directly attached to the skeleton, “reduced overall pain”. The Guide also states that it is “likely that phantom limb pain will reduce after osseointegration”.
743 The applicant also submitted that Mr Grieve, at times, refused to make obvious concessions during cross-examination. The applicant relied primarily on some cross-examination in relation to an email between Mr Grieve and his daughter on 8 June 2022 about the investigation. Properly read, I do not consider that this has the effect the applicant contended for. Even if it did, I am not persuaded that it affects his credit generally.
744 There was no clinical basis for the opinion Dr Al Muderis expressed: that Mr Grieve was likely to end up wheelchair-bound in the short term if he did not have the procedure. I am persuaded in that circumstance, by doing so, Dr Al Muderis inappropriately endeavoured to pressure Mr Grieve to have osseointegration surgery with the message conveyed that there was an urgency to it. There is no other proper basis on which the graph would have been drawn by Dr Al Muderis as it is. That was the message taken by Mr Grieve from the consultation. He acted accordingly, by consulting his prosthetist because of his concerns in relation to the prognosis given to him.
Section 3 — Mr Kerry Ford and Patient X
Mr Kerry Ford
745 Mr Ford passed away prior to the trial and no evidence from him was led at trial. Dr Al Muderis did not substantively address Mr Ford’s case in his affidavit but answered questions relating to Mr Ford during cross-examination.
746 Mr Ford suffered a penetrating injury to his left foot after stepping on a pine stake in 1993. He suffered multiple infections over the following 15-year period, ultimately requiring the amputation of two toes in 2019. Mr Ford also sustained a non-healing ulcer on his right foot after walking for an extended period during 1998 and eventually underwent a right below-knee amputation at the same time as the left foot toe amputation in 2019. Between 2019 and 2021, Mr Ford was wheelchair-bound and did not make any use of a socket prosthesis.
747 Mr Ford and his carer attended a consultation with Dr Al Muderis on 27 May 2021. Mr Ford was 71 years old at the time and lived at an aged care facility. Mr Ford’s insurance had agreed to fund the group assessment with Dr Al Muderis and his team.
748 I note a letter sent to Mr Ford on 4 May 2021 confirming his upcoming consultation suggested Drs Al Muderis, O’Carrigan, Stoita, Tetsworth and Alttahir and Ms Roberts would be in attendance. It appears from Dr Basten’s letter of 11 June 2021, that he sat in on the consultation too.
749 The consultation report was sent to Dr Andrew Whittaker (the referring doctor) on Dr Al Muderis’ behalf on 27 May 2021. The report said, inter alia:
We will be admitting Kerry into the hospital for IV antibiotics to treat the cellulitis as well as the non-healing ulcers in both bilateral limbs. Dr Mohabbat will address the vascular occlusion early next week.
We have advised him from an orthopaedic point of view we would like to aim towards a right transtibial osseointegration and a left below knee amputation and transtibial osseointegration as well. This would not only improve his mobility but also resolve the issues of the foot deformity on the left side and phantom pain. We would recommend a TMR to be done at the same time as the osseointegration. This is not only reasonable but necessary to improve his overall quality of life and is his only shot at ever walking again. If the right transtibial osseointegration does not work then we might need to proceed to an above knee amputation with transfemoral osseointegration though this is not the preferred option that would give him the best outcome at this stage.
Thank you for your ongoing care of Kerry and we seek speedy approval for his surgeries as well as vascular reperfusion with Dr Mohabbat.
(emphasis added)
750 It may be accepted that a letter sent from Dr Doshi to the insurer on 28 May 2021 refers to the further surgeries being dependent on Mr Ford’s current symptoms. However, as apparent below, the reports thereafter from Dr Al Muderis, Dr Tetsworth, and Dr Haidary, are not so qualified.
751 At the time of his consultation with Dr Al Muderis, Mr Ford suffered from very significant co-morbidities including, according to a letter dictated by Dr Al Muderis and sent to Mr Ford’s insurer on 11 June 2021, type 2 diabetes (accepted by Dr Al Muderis to be poorly controlled insulin-dependent type 2 diabetes), non-healing ulcers, history of heart failure, chronic kidney disease, vascular dementia, significant right knee arthritis, and significant obesity. The applicant’s submission that there “was no evidence of [vascular dementia] being a confirmed diagnosis” is not borne out by the evidence. The reports written on behalf of and by Dr Al Muderis referred to Mr Ford suffering from that condition and the diagnosis appeared to form a basis of opinions expressed by Dr Al Muderis. That Mr Ford had vascular dementia was also accepted by Dr Tetsworth in his report of 10 September 2021.
752 Notwithstanding these co-morbidities, Dr Al Muderis recommended osseointegration and opined in the 11 June 2021 letter to Mr Ford’s insurers, that Mr Ford was a terrible candidate for the use of a conventional socket prosthesis. He stated that Mr Ford’s chance of mortality in the coming year was greater than 50% unless he was granted the opportunity to resume weight bearing and mobilisation activities “as quickly as possible”, which would be achievable using osseointegration. Dr Al Muderis said:
within 12 weeks we would expect him to be able to ambulate independently and within a period of several weeks he should be able to resume rehabilitation and early ambulation partial weight bearing using a frame or crutches.
Dr Al Muderis opined that it would be “indefensible” if “he were to god forbid pass away during the next several months while he is waiting to even trial a socket mounted prosthesis”. The letter continued, “I do not believe I am overstating the case or exaggerating unnecessarily and I am simply stating my opinion based on documented facts and the benefits that we know will accrue to him if he has osseointegration” (emphasis added). Dr Al Muderis opined that the “core and fundamental component of his rehabilitation should begin with osseointegration”, describing it as “the absolute most critical aspect of his rehabilitation”, and “the starting point for his rehabilitation planning”. As the respondents correctly submitted, this is a “clear recommendation on Dr Al Muderis’ part that Mr Ford undergo urgent osseointegration surgery”.
753 The applicant submitted that the purpose of the letter was only to answer specific questions posed by the insurer, and that Dr Al Muderis was not giving general advice or making recommendations. That submission is not borne out by the terms of the letter, or the context in which it was sent. For the same reasons, the applicant’s submission that Dr Al Muderis was essentially asked to compare socket prostheses and osseointegration and to explain the recommendation for TMR surgery, is not an accurate reflection of the letter. Moreover, as apparent from the face of Dr Al Muderis’ letter, the questions posed by the insurer are directed to “the proposed OI [osseointegration] and TMR procedure for Mr Ford’s right leg”. I note the letter posing the questions is not in evidence.
754 To suggest, as the applicant does, that he did not provide an opinion in relation to Mr Ford’s insurance application, is disingenuous. He was providing a report to the insurance company in relation to the claim. It is difficult to accept, given the terms of his letter, that Dr Al Muderis thought the letter would be considered in a way other than as being in support of the surgery being approved. The letter is advocating a position, and in strong terms. The applicant’s submission that he was not cross-examined on the report before the member of the personal injury commission (who was ultimately deciding Mr Ford’s claim) as somehow lessening the significance of or affecting the nature of the contents of the letter, cannot be accepted. Additionally, I observe that despite the purpose of the letter, Dr Al Muderis does not refer to, or address in the letter any of the risks that would accompany osseointegration, or the impact of Mr Ford’s very many comorbidities and conditions on those risks. It is no answer to submit that Dr Al Muderis was simply answering questions, because the letter went far further.
755 As referred to above, Dr Tetsworth also provided a report in relation to Mr Ford, advocating for osseointegration surgery. The report was relied on by Mr Ford in his application for workers’ compensation to fund the surgery. This is the report in which Dr Tetsworth lists euthanasia as an option for Mr Ford. Dr Tetsworth’s attitude as to the suitability of Mr Ford for osseointegration surgery, and the opinion of others who expressed an opinion to the contrary, is referred to above (when considering Dr Tetsworth as a witness in Part 5 Section 5) and is unnecessary to repeat.
756 The tenor of Dr Tetsworth’s report is that he supported the opinion of Dr Al Muderis. Despite Dr Al Muderis’ denial that he had formed an opinion about the suitability of Mr Ford for osseointegration, the report from Dr Tetsworth reflects his understanding of Dr Al Muderis’ position: “I agree wholeheartedly with the opinion of Professor Al Muderis in that this is Mr Ford’s best option, far and away” and “[t]hose surgeons who are most knowledgeable in this area [being osseointegration], including myself and Professor Al Muderis, both emphatically agree that this is in the very best interest of Mr Ford”. In expressing his opinion in his report, Dr Tetsworth understood at the time that Dr Huang and Dr Wines had also written reports expressing a contrary opinion, although he had not read them. However, Dr Tetsworth conceded in cross-examination that Mr Ford had a terrible prognosis generally, that there was a material risk that Mr Ford would not survive the surgery recommended, that Mr Ford had been non-compliant with medical directions in the past, and that if he survived surgery, he would struggle with rehabilitation.
757 In addition, I note that Dr Haidary, a rehabilitation physician who works with Dr Al Muderis, also said in a very brief report that Mr Ford was a suitable candidate for osseointegration but would benefit from pre-operative physiotherapy.
758 Though these reports advocate for Mr Ford’s suitability for osseointegration surgery, it can readily be accepted that there were red flags in relation to Mr Ford. Some of those red flags plainly go to issues such as whether Mr Ford could give informed consent. Although Dr Al Muderis accepted that he would not want to perform osseointegration surgery on a patient who had not had a comprehensive assessment of their cognition, he rejected that a consultation report written by Dr Basten raised any red flags.
759 Dr Basten prepared a consultation report on 11 June 2021, having seen Mr Ford on the ward the day prior. He noted that Mr Ford was under a guardianship order or power of attorney. Although Dr Basten did not conduct a neuropsychological assessment, he thought “it was clear enough that there was impairment sufficient for us to act with caution”. He explained there were signs of disinhibition, poor self-monitoring and self-regulation of behaviour, with Mr Ford being completely dismissive of those problems, which demonstrated a lack of insight. Dr Basten accepted that these characteristics are red flags for surgery because they go to matters such as the likelihood that the patient would be compliant with medical and other directions. Dr Basten was of the view that there were further steps that would need to be undertaken before he could be satisfied that Mr Ford was psychologically suitable for osseointegration. From his letter of 11 June 2021, and Dr Basten’s evidence, it is apparent that at that stage, Dr Basten was not prepared to recommend Mr Ford as being psychologically suitable for the surgery.
760 Dr Al Muderis disagreed that disinhibition, poor self-monitoring and poor self-regulation of behaviour are necessarily red flags for osseointegration surgery, that Dr Basten was implying that Mr Ford could not give informed consent, and that Dr Basten was clearly conveying that he did not consider that Mr Ford was psychologically suitable for osseointegration surgery. It was put to Dr Al Muderis that Dr Basten’s opinion would have suggested that he should not have stated in the 11 June 2021 letter to the insurer that the “core and fundamental component of [Mr Ford’s] rehabilitation should begin with osseointegration”. As foreshadowed in the multidisciplinary section above, tellingly, Dr Al Muderis answered:
That is not what Dr Basten said. Dr Basten is a very experienced clinical psychologist, and he knows his limitation and his jurisdiction. He can comment on the psychological aspect of the patient, not on the rehabilitation aspect or the physical aspect of the patient. So I disagree with the statement.
761 Shortly thereafter, in answer to a question in cross-examination that Mr Ford exhibited limited insight into his own care (obviously based on Dr Basten’s report), Dr Al Muderis said he could not comment on that because he had not made his own informed decision.
762 Dr Al Muderis’ failure to accept in cross-examination that there were red flags, or that the conditions described gave rise to concerns in relation to performing osseointegration surgery, reflects adversely on him. The evidence also reflects his attitude towards the opinions expressed by others in his team (which has been discussed above). As the respondents submitted, the fact of a multidisciplinary approach being adopted in his practice was repeatedly highlighted by the applicant, as there was input from different experts. In that context, as noted in the multidisciplinary section above (see Part 6, Section 1), it is difficult to understand how Dr Basten would have exceeded his jurisdiction by advising against osseointegration as a means to rehabilitate Mr Ford. These answers in cross-examination showed a lack of respect for the expertise of others. They reflect that, from Dr Al Muderis’ perspective, the decisions were ultimately his to make (regardless of the opinions of others in his team to the contrary).
763 On the evidence, I am satisfied that Dr Al Muderis had recommended that Mr Ford was a suitable candidate for the osseointegration procedure. That further tests may have been conducted before the surgery occurred does not detract from the fact that a recommendation was made.
764 As Dr Stalley opined, given Mr Ford’s comorbidities (which Dr Al Muderis accepted existed), a recommendation to have osseointegration was a “terrible thing to do”. The premise underpinning Dr Stalley’s opinion is established. He opined the risks were just too great. I accept his evidence.
765 On the evidence, I am persuaded that Mr Ford was not a suitable candidate for osseointegration surgery.
766 Mr Ford ultimately did not undergo osseointegration. The osseointegration surgery proposed by Dr Al Muderis was rejected by the personal injury commission as being a not reasonably necessary treatment: Ford v Narrabri Shire Council [2022] NSWPIC 119 (Ford). That is a fact which explains why the surgery did not proceed. I do not rely on the conclusion for any purpose of truth defence, but I note the judgment is relevant to the s 29A defence.
Patient X
767 This patient was referred to as Patient X in these proceedings. She had a left transtibial amputation in May 2020. She underwent right below-knee amputation and transtibial osseointegration with Dr Al Muderis on 11 December 2021. On 10 August 2022, she underwent left transtibial osseointegration with Dr Al Muderis’ colleague, Dr Alttahir.
768 Patient X was 34 years old when she first consulted Dr Al Muderis and his team in September 2021. She has an extensive list of comorbidities including severe anorexia nervosa, starting when she was 15 years old, and a history of excessive exercise and non-compliance with medical guidance. The extent of the issue is apparent from the fact that she was, at some point, placed under a community treatment order.
769 Although the respondents ultimately relied on this case study as being relevant to proof of the truth of several imputations, the crux of the issue in her case study was her suitability for surgery.
770 Moreover, Patient X was not called to give evidence, despite the applicant filing an affidavit in her name. That necessarily limits the scope of the consideration of her case and its relevance to broader imputations.
771 Patient X’s September 2021 consultation with Dr Al Muderis was four months after Mr Ford’s first consultation. The respondents rely on these cases as “the two paradigm examples” of Dr Al Muderis recommending (and in Patient X’s case, performing) osseointegration surgery for patients who were said not to be suitable. As with Mr Ford’s case (see above), there were other medical professionals who raised concerns as to Patient X’s suitability for surgery.
772 I note these cases occurred not long before the Publications, in a context where the evidence was that Dr Al Muderis’ practice expanded over time to include patients that he would not have previously accepted as being suitable to undergo osseointegration surgery.
773 Dr Ross Hawthorne was involved in Patient X’s care in 2020. He is a Rehabilitation Medicine Practitioner who has been employed by the Sydney Local Health District and its previous entities for over 33 years. He has been the Head of Department of Rehabilitation Medicine at Concord Repatriation General Hospital since 1999. He has conducted a prosthetic clinic at the Royal Prince Alfred Hospital for around 25 years. It was in that latter context that he met Patient X, whom he consulted on 13 August 2020, approximately three months after her left below-knee amputation.
774 During cross-examination, Dr Hawthorne described Patient X as an:
exceedingly difficult patient, an extraordinary patient, a unique patient that had suffered an amputation, was looking at bilateral amputations at such a young age with … essentially anorexia nervosa as the cause of those amputations.
775 Ms Geada is a clinical prosthetist at APC Prosthetics, who was also involved in the care of Patient X. She started in her current role at APC Prosthetics in September 2017 and met Dr Al Muderis shortly thereafter. She had worked on Dr Al Muderis’ cases with him from time to time. Although the applicant relied on her evidence as to his standard practice, it is very brief on that topic. Her evidence in cross-examination principally related to her involvement with Patient X and Dr Hawthorne.
776 Given the issue in this case study, it is necessary to consider the events leading up to the surgery, in part at least, in chronological order.
777 On 30 September 2021, Patient X attended her first consultation with Dr Al Muderis and his team. Her medical history, including an extensive list of comorbidities, are summarised in a letter sent to her GP on behalf of Dr Al Muderis that day. This letter concludes, “[w]e can offer her an osseointegration implant on the left side to deal with her soft tissue problems. For the right leg we think we need to do a staged procedure”. It also recorded that Patient X “is mobilising indoors with a wheeled frame”, and that “[o]n examination she has a limping gait”. This is inconsistent with Dr Al Muderis’ evidence that Patient X was “wheelchair bound” when he first consulted with her.
778 Patient X’s medical history and conditions are also detailed in Dr Basten’s report of the same date, which Dr Al Muderis accepted was reported to him. The report describes, inter alia, that:
The eating disorder remains severe. … [Patient X] still exercises a minimum of three hours a day (e.g. three hours on her indoor training bike and will often cycle outdoors as well). [She] would find it extremely hard (probably impossible) to comply with instructions to exercise less or eat more if that were required for medical reasons.
779 Dr Basten opined that Patient X “needs more information to make an informed decision”.
780 In evidence is an email chain commencing 7 October 2021 involving Patient X, Mr Ward of Innovo Prosthetics (Patient X’s prosthetist at the time), and Ms Geada. An email Mr Ward sent to Patient X and Ms Geada that day reflects his concerns about her undergoing osseointegration, given her medical history. He recommended that she “have the OI team consult with your rehab consultant Ross Hawthorne”. In response, Patient X said she has not met Dr Hawthorne, and will have Dr Sanjeev Gupta (who, she explained, “has done all my previous surgeries for both legs”) consult with Dr Al Muderis and Dr O’Carrigan. Mr Cameron Ward urged her to “discuss all options with Dr Gupta before proceeding with any surgery”.
781 In a later email of 8 October 2021, Patient X wrote to Ms Geada, removing Mr Ward from the chain:
I spoke with Tim O’Carrigan yesterday regarding the future outcome of potential ankle reconstruction and he has advised that after looking at my CT scans the likelihood of surgery being successful and healing etc would be very poor and together agree that going forward we will firstly perform osseointegration on my left leg and straighten my right knee and then once healed will also have osseointegration on my right leg / ankle.
If [Mr Ward] feels uncomfortable remaining my prosthetist with this decision I would appreciate your help and support finding one that will?
782 Patient X was obviously aware of concerns Mr Ward held about her proceeding with the surgery.
783 On 28 October 2021, Dr Al Muderis attended a discussion about Patient X. Patient X attended the clinic that day. The report to her GP records:
We had a discussion with the Limb Reconstruction Team including Professor Munjed Al Muderis, Dr Razvan [Stoita], Dr Mustafa Alttahir and our Psychologist Dr Chris Basten to see if we can go ahead with the operation. The consensus of the group is that there are no good reconstruction options for her foot. The patient prefers osseointegration in both legs. The psychologist support team thinks that she is good to go through surgery.
We will plan her for a right below knee amputation, high tibial osteotomy and bilateral tibial osseointegration in one operation. We will address her shoulder problems at a later stage.
784 Dr Al Muderis accepted the focus of the discussion about whether Patient X should proceed with the surgery was on mobility. The applicant submitted the group concluded that the consensus was that there were no good reconstruction options for her right foot, and that it was reasonable for her to have a right below-knee amputation and bilateral transtibial osseointegration. I return to that submission below.
785 Dr Basten wrote a report to Dr Al Muderis dated 3 November 2021, describing a meeting with him and Patient X the week prior (the report’s terms suggest the meeting occurred on 28 October 2021). Dr Basten wrote:
[Patient X’s] drive to restrict food and to exercise ritualistically is likely to be present as soon as she is physically able to exercise and this could compromise her post-operative rehabilitation.
On seeing her again last week, I noted a deterioration in her foot such that she can no longer walk at all and cannot even use her exercise bike. I think that this shifts the appraisal of risks. The dangers of compromised post-operative care are still present. However, they are predictable and manageable. On the other hand, there is a 100% chance of impaired quality of life to leave both legs as they are without operating. Thus, it seems reasonable and wise to tolerate and manage the risks posed by her chronic eating disorder. I suggest that the team obtains a written contract from [her] that she will only exercise as prescribed by her physiotherapist and surgeon.
786 There were several communications between Patient X and the LRC shortly after 28 October 2021, which the respondents submitted raised red flags.
787 On 31 October 2021, Patient X emailed Dr Al Muderis:
Thankyou for allowing me the chance to meet you and your team and not simply write me off as having too many medical red flags like many have done before. I connected with your personal experience with trauma and discrimination and how you have overcome it all to pioneer life changing medical technology. I too would like to leave a legacy that benefits the greater good and so wish to volunteer for any future osseointegration techniques that you are currently working on? I am happy to sign any waivers necessary and hope that my complex medical morbidities will be useful despite the risks involved?
I am especially keen to try a faster loading process for my bilateral surgery and understand my bones might fracture as a result? Either way if there is any way I can help I would love to volunteer?
788 On 1 November 2021, Patient X received an email from Ms Connie Gambra, a nurse with the LRC, confirming her surgery was booked for 11 December 2021 and that a pre-surgery consultation was scheduled for 30 November 2021. I note Ms Gambra requested certain forms be read, signed and returned to the LRC, including a “copy of the risks of osseointegration”. Patient X responded the next day, with the email (according to its contents) attaching signed copies of the estimate of fees form and risk of osseointegration form. Neither document is in evidence. Nonetheless it is obvious that she signed and returned the risks form in circumstances where no surgeon (or medical professional) assessed her understanding of the form, or its contents. The LRC nevertheless received a signed copy of the document wherein, one may infer, Patient X claims to understand the risks of surgery.
789 On 3 November 2021, Patient X sent an email to Ms Gambra as part of this chain:
Is there anyway I can possibly meet with Munjed before my surgery as I’m worried that I am being selfish and rushing into major surgery when I’ve only been an amputee for a little over months. I’ve been told by many others that I should be patient with my knee socket despite the ongoing pressure sores and wait for many more years before getting OI and whilst I don’t necessarily agree I am concerned that Munjed also agrees that I don’t really need OI compared to most others?
Now please don’t think I’m being ungrateful as I understand how valuable Munjeds time is but I did honestly feel that the decision to do OI on both legs at the same time was rushed and the significance of the trauma I will experience especially trying to cope once home alone without legs for 6 weeks wasn’t discussed? I know that Munjed cares greatly about his patients but I never really got a chance to speak with him one to one and fear that he doesn’t really know my particular circumstance and struggles I will face (as I don’t have any family support and solely rely on NDIS providers)?
I’m sorry if this sounds selfish and if it’s not possible to see Munjed before surgery I still wish to proceed and will simply stop complaining and trust he knows my personal circumstance.
I also just need to check if the estimated fees for surgery include Munjeds personal fees as in my initial meeting after seeing the extensive damage to my body he said he personally would not charge me? However if he has since changed his mind I totally understand and am in the process of accessing the money my mother left for me so should hopefully be able to pay in a couple of days time?
Again please don’t think I am ungrateful as I feel honoured to have met Munjed and still wish to proceed with surgery but have a few more questions to ask beforehand so I can best plan for support after?
790 Later that day, Patient X had a telephone call with Ms Gambra. Ms Gambra’s note of the call recorded booking an appointment with Dr Al Muderis for 18 November 2018, “as [Patient X] feels she is rushing into surgery and [didn’t] get a 1 on 1 with [Dr Al Muderis] to go through the surgery.” Ms Gambra also recorded informing Patient X that although there would be no out-of-pocket expenses for the procedure, the external componentry is not covered by insurance, and that “she will need 2 of these” as she is undergoing bilateral surgery.
791 I accept the respondents’ submission that there were red flags. They were plainly evident, particularly given what was known about the state of Patient X’s mental health. As the respondents submitted, Patient X was effectively offering herself to Dr Al Muderis as a form of a human guinea pig in her 31 October 2021 email, whatever the personal costs, and then, three days later, indicated grave hesitation and reluctance to have the surgery. She felt she was “rushing into major surgery when” she only recently became an amputee, and “that the decision to do OI on both legs at the same time was rushed”. That sentiment is not surprising. Her first consultation with Dr Al Muderis was on 30 September 2021, the decision for single-stage bilateral surgery was made on 28 October 2021, and her surgery was confirmed four days later for 11 December 2021. Patient X, uncertain as to where she would recover from the surgery, said there was no discussion as to how she would manage at home in circumstances where she lived alone and lacked family support.
792 There are several further points to be made about these emails. First, Patient X declared a personal connection with Dr Al Muderis given his history, and that she was inspired by him to offer herself in the way she described. She talked of being honoured to have met him. Second, she was aware that she had a complex history such that Dr Al Muderis was offering her treatment that other doctors would not. Third, despite her concerns, she did not want to trouble Dr Al Muderis. She trusted him to the extent that she was prepared to proceed with surgery even if she could not see him beforehand to discuss those concerns. Fourth, it is obvious that others were warning her about undergoing the surgery. For example, she wrote, “I’ve been told by many others that I should be patient with my knee socket despite the ongoing pressure sores and wait for many more years before getting OI”. There is evidence that she was receiving such warnings, as explained below.
793 I agree with the respondents’ submission that Patient X’s correspondence during this period should have raised concerns with Dr Al Muderis as to her capacity to give informed consent. The applicant’s submissions are entirely silent on these communications and Dr Al Muderis’ evidence about the 3 November 2021 email. There is no evidence of anything having been done to address the issues as to consent that arose. I note also that it is apparent from this correspondence that although a surgery date had been set, and consent asked for and obtained, Patient X had not been provided with information about rehabilitation. It is difficult to understand how informed consent can be obtained without a patient being aware of such relevant information.
794 Patient X attended the appointment scheduled for 18 November 2021. Dr Al Muderis’ report describes a decision to proceed with surgery on her right side only (being amputation and osseointegration), with a view to osseointegration on her left leg “maybe six months after the first operation”. Continuing with the right side only was said to be wise because Christmas was approaching and her housing issues were unresolved. Dr Al Muderis performed right below-knee amputation with osseointegration on 11 December 2021.
795 Dr Al Muderis’ evidence in relation to the email of 3 November 2021 and the circumstances of the change of plan was unsatisfactory.
796 In cross-examination, when pressed about Patient X’s concerns of the scheduled bilateral surgery, Dr Al Muderis gave evidence that he had no intention to perform bilateral surgery, and that Patient X was mistaken. Yet the documentation supports that that was the plan as of 28 October 2021. It was the surgery which had been booked.
797 The applicant submitted that on 28 October 2021, Drs Al Muderis, Stoita, Alttahir and Basten reached a consensus that it was reasonable for Patient X to have bilateral surgery. Concerningly, when Dr Al Muderis was pressed in cross-examination on his intentions for surgery, his response was that he “always” intended to only do surgery on the right leg, and that the report of 28 October 2021 was “the conclusion of the team”, explaining “it’s a team decision, and the team wanted to do that”. That answer only raises more questions. If that was his intention as the surgeon responsible, the group consultation was meaningless. That is, the team’s decision had no practical bearing on the surgery he would ultimately perform. It also means the terms of the consultation report which was sent to Patient X’s GP that record “we [the Limb Reconstruction team] will plan her for a right below knee amputation, high tibial osteotomy and bilateral tibial osseointegration in one operation”, is inaccurate. Moreover, his evidence was that he “always wanted to do the right leg. I didn’t want to do the left leg … that was my intention. I thought the left leg can be left alone” (emphasis added). That evidence sits uncomfortably with his first consultation report of 30 September 2021, in which he advised “[w]e think it will be wise to start with the osseointegration on the left side”.
798 I consider it more likely that Dr Al Muderis’ intention on 28 October 2021 was to perform surgery on both legs. Patient X expressed concerns of undergoing bilateral surgery to Dr Al Muderis’ clinic in her 3 November 2021 email and, it can be inferred, with Dr Al Muderis directly on 18 November 2021. The plan to perform bilateral surgery was abandoned that day. Dr Al Muderis’ evidence that he never intended to perform bilateral surgery was to overcome questions put to him in cross-examination, that were critical of his conduct. Patient X had no misunderstanding. I do not accept Dr Al Muderis’ evidence.
799 As is clear from Patient X’s email of 3 November 2021, she had been receiving advice from third parties. One such person was her doctor, Dr Gupta.
800 On 18 October 2021, Dr Gupta wrote a letter to Patient X’s GP, having reviewed her “a few times over the last two weeks”. He expressed his concern about her undergoing osseointegration, giving several reasons. He recorded that she was considering getting a second opinion (he suggested Dr Huang and Dr Wines) and advised that she discuss the matter further with Mr Ward and Dr Hawthorne.
801 Dr Mark Horsley, an orthopaedic surgeon and a recipient of Dr Gupta’s letter, sent a letter in reply on 3 November 2021. Noting he had reviewed Patient X at least twice, he raised serious concerns about the surgery proceeding and recommended she obtain a second opinion.
802 On 18 November 2021, Ms Geada saw Patient X, as she was referred to her ahead of the surgery, now planned for her right side. She sent an email to Dr Hawthorne and others the following day, explaining that Patient X was scheduled for surgery and wrote, “I believe I share a few of your concerns and I don’t even know the whole story”. Dr Hawthorne responded that day:
This is dreadful news as we discussed. I believe that this is an appalling decision. I think we should do anything we reasonably can to stop it. I will try and contact Munjed next week when I get my thoughts more organised.
803 On 21 November 2021, Dr Hawthorne, feeling he was in an ethical dilemma, sought advice from the then medical director of the NSW Medical Council. His evidence was he was told there was little the Council could do, especially as the surgery was imminent, but that he should consider making a complaint to the Australian Health Practitioner Regulation Agency (AHPRA), which he did the following day.
804 On 2 December 2021, Dr Hawthorne wrote to Dr Al Muderis setting out his concerns about the proposed surgery (and posted the letter). He opined that Patient X was an inappropriate candidate for the surgery and that it should not proceed. His evidence was that the dual purposes of the letter were to resolve (what he felt was) an ethical obligation, and to inform Dr Al Muderis “that at least one doctor out there was of the opinion that this was absolutely the wrong thing to do”.
805 As the respondents submitted, following the surgery, those treating Patient X started to experience the very issues with her rehabilitation that had been discussed before the surgery. Issues with over-exercising arose repeatedly. Ms Bridget Dean, a physiotherapist, left a note in Patient X’s hospital file on 20 January 2022, “NOT TO TAKE FOOT HOME”. On 25 January 2022, she recorded, “NOT TO TAKE FOOT HOME OR STRONGLY ENCOURAGE NOT TO USE LEG, over doing it is how she lost her legs”.
806 It was put to Dr Al Muderis that the 25 January 2022 note was consistent with the concern that Patient X was prone to over-exercising. Instead of accepting the obvious, he was dismissive of the suggestion, suggesting instead that the note was merely the physiotherapist’s view.
807 That Ms Dean repeatedly left notes of that nature in subsequent consultations, culminating in a note on 8 February 2022, “[l]eg has been left at physio to prevent use at home”, reflects ongoing issues with Patient X’s compliance. Ms Geada gave evidence she was concerned during this period that Patient X was not following instructions in respect to how often she should use her prosthetic leg.
808 I note that Dr Al Muderis’ consultation report of 3 February 2022 recognised that Patient X was “doing a bit too much loading”, and advised, “based on the advice of” Ms Dean and Ms Geada, that her leg be taken from her. The respondents submitted this was an admission by Dr Al Muderis that the physiotherapists’ concerns were very real and valid, despite his resistance to such a proposition during cross-examination. I agree.
809 By February 2022, Patient X had experienced issues with infections, swelling and non-compliance. When these issues were put to Dr Al Muderis in cross-examination, he was argumentative, asserting many patients experience infection and all experience swelling. He denied that Patient X had been non-compliant to the point that her leg had been taken away from her on his advice. He said Patient X was “extremely happy with her right side of osseointegration” and she proceeded with surgery for her left leg in turn. He repeatedly volunteered, Patient X was wheelchair-bound “when she came to” him and “is now fully active”. As referred to above, his evidence of her being wheelchair-bound at that time is inconsistent with the consultation report. I note she required further surgery on her right leg in April 2022 (which included treatment for infection), such that Dr Al Muderis deferred the surgery to her left leg. She continued treatment for infection in May 2022.
810 The left leg surgery was performed by Dr Alttahir on 10 August 2022. Despite Dr Basten advising on 23 June 2022 that there are no psychological problems that the team would need to consider ahead of surgery, a hospital note dated 14 August 2022 flagged Patient X “for review of Dr Basten before discharge due to suicidal ideation and feeling depressed”. Ms Geada gave evidence that in November 2022 and February 2023, Patient X was not complying with rehabilitation instructions.
811 On 14 April 2023, Dr Rishi Narasimhan of the LRC sent a letter to Dr Tillman Boesel, a rehabilitation specialist, writing, inter alia:
[Patient X] is an extremely high risk candidate for any upper limb surgery given her physiological status and her poor wound healing capacity and general poor nutrition. I do not think [she] would be suitable for a reconstruction procedure including a reverse shoulder replacement at this stage.
812 That same day, Patient X emailed Dr Al Muderis’ office saying she was “keen to start running again” and asking for clearance from Dr Al Muderis, which he subsequently gave.
813 The respondents submitted that Dr Stalley was candid that an assessment of Patient X’s suitability for surgery would require an assessment of information beyond that briefed to him, including psychiatric, functional, skin and infection assessments. Dr Stalley was only briefed with Dr Hawthorne’s affidavit. That said, his evidence was that he shared Dr Hawthorne’s anxieties and noted there were red flags in Patient X’s presentation. He opined:
Patient X … was, according to Dr Hawthorne’s description, a keen runner but suffering from longstanding anorexia nervosa. This leads to poor bone quality, multiple fractures, poor wound healing and often, non-compliance with medical advice. All of these things would be red flags for someone recommending osseointegration. I accept that evidence.
814 Although the respondents also relied on the evidence of Dr Geffen, it does not assist on this topic.
815 The applicant was highly critical of Dr Hawthorne’s conduct, suggesting to him in cross-examination that his complaint to AHPRA was to denigrate Dr Al Muderis. That was despite Dr Hawthorne having already explained his ethical dilemma, and that he felt he had a legal obligation to make the complaint.
816 As noted earlier, Dr Hawthorne sought advice from the medical director of the Medical Council of NSW, who advised that there was little they could do, and suggested he might submit a complaint to AHPRA. Dr Hawthorne agreed he did not email his letter (dated 2 December 2021) to Dr Al Muderis or send it to his clinic and ask them to give it to him urgently. It was put to him that if he really wanted Dr Al Muderis to be aware of his concerns, prior to proceeding with the surgery, he would have communicated with him in a more urgent fashion. Dr Hawthorne said that Dr Al Muderis was already aware of all the concerns that he put in the letter and was going ahead anyway. He was also criticised for breaching Patient X’s confidence.
817 I accept Dr Hawthorne’s evidence as to why he did not call Dr Al Muderis. Apart from being daunted by the prospect of calling Dr Al Muderis and having been cautioned about him being extremely litigious, he considered it futile to do so.
818 Dr Al Muderis was aware, given what Patient X raised in her 31 October 2021 email, that other clinicians had declined to perform surgery on her, and she understood that he was prepared to do what they were not. There appears to be no evidence that Dr Al Muderis sought to speak to any of her previous treating team (and the applicant does not suggest otherwise). As the respondents correctly submitted, Dr Al Muderis was dismissive of those clinicians’ underlying concerns, giving evidence that: the problem with Patient X was that “she has been mismanaged” and “severely neglected”; “she may have been misled to believe that she’s too complicated, but she was not too complicated”; and that other clinicians who had been unwilling to treat her were under-skilled.
819 Dr Hawthorne was an honest, credible and reliable witness. I accept he felt he was in a dilemma as to a legal obligation to report. He was not the only person who had concerns about performing osseointegration on Patient X. Dr Gupta, Ms Geada and Dr Horsley also held those concerns. The concerns each of those parties expressed as to Dr Al Muderis’ decision to proceed with the surgery are entirely reasonable.
820 Ms Geada gave evidence that she held the view Dr Hawthorne and Mr Ward should be kept informed as to what was occurring with Patient X in relation to any medical procedures being considered or discussed. This was apparent in her email exchange (noted above) with Dr Hawthorne (amongst others) both expressing concerns about Patient X undergoing osseointegration, and informing them about what was occurring. Ms Geada gave evidence that she decided to contact Dr Hawthorne about Patient X because he had initially referred Patient X to them (as her rehabilitation consultant) when she first became an amputee. Therefore, he was to be kept informed of what was happening, as he was Patient X’s consultant for her whole life, regardless of whether she had osseointegration or otherwise. Ms Geada’s evidence reflects she respected Dr Hawthorne and his advice. Her evidence reflects that after both the first surgery and second surgery there were repeated concerns about Patient X’s non-compliance with her instructions in relation to rehabilitation. That is, Patient X was not complying by doing more than the protocol permitted (e.g. over-exercising and not using her crutches when she was required) which had consequences for her (as mentioned above).
821 I note an osseointegration brochure in evidence, “Osseointegration: The Australian Experience” (discussed above in relation to the brochures in Part 6, Section 1), lists non-compliance and mental instability as exclusion criteria. Accepting that this was published circa-2016, it is difficult to see how the non-compliance and mental instability criterion could change over time. The underlying reason for excluding patients with a history of non-compliance is obvious, with such patients facing serious ramifications if they have the surgery. Dr Al Muderis was warned of Patient X’s history of non-compliance. Dr Basten’s 30 September 2021 report included that Patient X’s “anorexia nervosa was severe enough and her ability to accept treatment so poor, that [she] was placed under a community treatment order several years ago.”
822 The applicant submitted that the potential issues Dr Hawthorne identified with Patient X’s suitability for surgery in his affidavit were specifically considered by Dr Al Muderis and his team in their assessment. He further submitted that there is no evidence to conclude that the assessments were inadequate or improper in any way, or that the group’s conclusion – that her issues were able to be successfully managed – was wrong. There is a circularity to that submission. It implies because the assessment was done, it was adequately or appropriately done.
823 Further, as the respondents submitted, there is no evidence of any careful consideration at the 28 October 2021 meeting of Patient X’s ability to manage post-operative instructions, or mechanisms that could be put in place pre-operatively to increase her prospects of a satisfactory outcome. Nor is there any reference in any of the LRC’s consultation reports prior to her first operation to steps to mitigate the risk of issues likely to arise given her history, or to address those issues should they arise (which would be expected, if the matters had been properly considered). As is apparent from Patient X’s 3 November 2021 email, by which time she had been assessed as suitable for bilateral osseointegration and her surgery had been booked, Patient X was uninformed of the rehabilitation process and whether she would be at home alone for that process. I accept the respondents’ submission as to these matters, and that a reasonable practitioner, given the circumstances, ought to have had them front of mind.
824 As the respondents submitted, Dr Al Muderis’ single focus appears to have been on mobility, in circumstances where a much more holistic analysis was called for. It bears similarities to Mr Ford’s case. Dr Al Muderis’ assessment of her suitability was lacking. I am satisfied that, in the circumstances, it was inadequate.
825 There were obvious red flags and contra-indications to surgery. Her precarious psychological state, as apparent from the emails recited above, was obvious. There is no evidence this was properly addressed (and having her undergo surgery on one leg, does not do so). She felt rushed, and given the speed with which this happened, that is not surprising. There was no urgency. That expressed concerns of others came to fruition after the surgery is similarly unsurprising, and Dr Al Muderis’ attempts to diminish those issues do not assist him. In April 2023, Patient X’s issues (which appear to be long standing, being her physiological status and her poor wound healing capacity and general poor nutrition) meant that she was not suitable for surgery on her shoulder. I also note the problem with Patient X’s wound healing issues that could lead to deep infection all being related to her nutritional problems was an issue raised by Dr O’Carrigan in his report of 7 October 2021.
826 The respondents submitted that Patient X was a witness in Dr Al Muderis’ camp, and in circumstances where he had filed an affidavit on her behalf but did not call her, the Court ought to infer that Patient X’s evidence would not have assisted Dr Al Muderis’ case. There may be reasons why Patient X was not called and exposed to cross-examination (particularly given her conditions). None have been proffered by the applicant. Although I accept that Patient X is in Dr Al Muderis’ camp, nonetheless, in these circumstances I am not prepared to draw the inference sought by the respondents. Her contemporaneous records speak for themselves (and they do not assist the applicant’s case). That said, Dr Al Muderis’ evidence of his view as to her current state, or her state of happiness at any time with the procedures, absent the witness being called, is of little, if any weight. Dr Al Muderis’ evidence as to his assessment of the successfulness of the surgery, or a patients’ happiness, as reflected in other case studies below, is generally inconsistent with the evidence (and is confined to mobility). In any event, as I have observed elsewhere, a patient’s contentment with the procedure does not address the issues for determination. It does not address the issues raised in this case study.
Section 4 — International patients
Mr Billy Wynne III
827 Mr Wynne lives in the United States. He had osseointegration surgery with Dr Al Muderis on 6 June 2018.
828 The applicant submitted that although Mr Wynne answered questions clearly and directly and purported to have strong recall of the events, he was not credible as a witness. He submitted that his account is “constantly contradicted” by the contemporaneous records and the inherent logic of the events to which he deposes. He submitted that Mr Wynne’s evidence should not be accepted unless it is an admission against interest or corroborated by reliable evidence. The applicant also submitted that it was clear “from the numerous corrections made to the section of Mr Wynne’s affidavit from [75] to [87], Mr Wynne has misremembered the chronology in serious ways, with numerous events being confusedly spliced together”. In addition, the applicant submitted that Mr Wynne’s last communication with him was positive. From that, it was submitted that Mr Wynne had concocted his complaints about Dr Al Muderis to support Mr Hernandez in his case against Dr Al Muderis.
829 I have considered the matters relied on by the applicant, and I do not accept the submission that Mr Wynne’s account is illogical or constantly contradicted by records. Mr Wynne was honest, credible, and his evidence was generally reliable. He was an impressive witness. His evidence, in many respects, is supported by other evidence. That at the outset of his evidence he corrected the order of some paragraphs in his affidavit does not alter that. There is nothing to suggest those events did not occur, rather there is evidence supporting that they did.
830 There is no evidence to support the submission that Mr Wynne concocted his evidence. I address elsewhere the fallacy that patients do not have complaints because their communications with Dr Al Muderis are otherwise positive: see The patients in Part 6, Section 1.
831 Mr Wynne lives in Oklahoma. While working as a flight paramedic in the United States in February 2013, his left leg was amputated below the knee following a helicopter accident. It was further amputated above the knee around one month later. He was in hospital for around six months following the accident and underwent approximately 20 surgeries. He was fitted with a traditional socket prosthesis after being discharged from hospital but experienced difficulties using it. He ceased work after the accident. Following a lawsuit against the helicopter company, he receives a monthly annuity.
832 Mr Wynne came across the Osseointegration Group of Australia online in late 2017. On 22 November 2017, he completed a contact form on their website expressing interest in osseointegration. Later that day, Ms Roberts responded and requested an x-ray of his femur so that Dr Al Muderis could assess how complex his procedure would be.
833 Mr Wynne’s evidence was that in early December 2017, he received a call from Mr Hernandez, who he understood to be the United States’ representative of Osseointegration Group of Australia. Mr Hernandez gave him general information about osseointegration with Dr Al Muderis. He began texting with Mr Hernandez after they first spoke, and he began to feel like a friend. Mr Wynne gave evidence that he did not know that Mr Hernandez might be getting a commission if he got surgery with Dr Al Muderis until after he had the surgery.
834 Mr Wynne sent x-rays to Ms Roberts on 5 December 2017. Ms Roberts replied that same day thanking him for his x-rays and saying, “I have spoken to Munjed and he agrees your procedure would be very do-able in a single stage operation”. Dr Al Muderis gave evidence that by that time he had formed the view Mr Wynne’s surgery “could be done in one stage”.
835 From 30 January 2018 to 5 February 2018, Mr Wynne and Ms Roberts corresponded to arrange for Mr Wynne to see Dr Al Muderis in New Orleans on 16 or 17 February 2018. In their emails, Ms Roberts noted that she had “included Fred Hernandez on this email stream who is coordinating this clinic with me” (emphasis added). Ms Roberts accepted that it was part of her role to arrange for Dr Al Muderis to see potential osseointegration patients in the United States and what she arranged was a clinic. I discussed earlier Ms Roberts’ and Dr Al Muderis’ evidence as to this topic: see Part 5 Section 5.
836 On 16 February 2018, Mr Wynne met with Dr Al Muderis in New Orleans. He gave evidence that Dr Al Muderis was holding appointments in a hotel room. He was unnerved because the room “appeared cheap” and there were other patients in the room when he arrived. He said Dr Al Muderis examined him there in front of the other patients. Dr Al Muderis asked him to remove his pants while the other patients remained in the room and could see. He said that Dr Al Muderis’ examination of him lasted no longer than one minute. During the examination he touched his leg. Dr Al Muderis told him that he had looked at his x-rays. He advised he could proceed with the surgery, saying words to the effect of: “You’re good, no problem. You got any questions?”. Mr Wynne told Dr Al Muderis that he was very concerned that the scar tissue on his leg would be an issue, and that any cutting on his leg does not heal and that made him scared. He said Dr Al Muderis told him that it was not a problem and that he could proceed with the surgery. Mr Wynne asked Dr Al Muderis about the cost wherein Dr Al Muderis showed him a price sheet for someone else, with a total price of AU$110,000. Dr Al Muderis told him that his costs would be “really close” to this, and asked him not to show the sheet to others. Mr Wynne took a photograph of the price sheet.
837 Mr Wynne gave evidence that there was no discussion of risks of the procedure. His evidence was that he “noticed this because there were always risks discussed before the 20+ surgeries I had previously undergone”. Mr Wynne explained that, had Dr Al Muderis been an American doctor, he would have declined to proceed; “there were red flags everywhere”. He said that he told himself that Dr Al Muderis is from Australia, where things might be done differently. He thought that the procedure looked amazing and so tried to rationalise the conduct.
838 Dr Al Muderis accepted it was possible the meeting took place in a hotel room, and that there were other patients there when Mr Wynne arrived. He denied that he had: asked Mr Wynne to remove his pants; examined his leg (but conceded he may have looked at it); said to Mr Wynne “you’re good”; and shown Mr Wynne a price sheet. He could not recall whether Mr Wynne had raised concerns about his extensive scar tissue and the ability of any wound on his leg to heal, or whether there was any discussion about risks and complications.
839 The applicant’s submission that Mr Wynne’s account of the events at the hotel should be rejected appears to be based, for a significant part, on Dr Al Muderis denying the events. The applicant gave additional reasons for rejecting Mr Wynne’s evidence, including:
(1) it does not make sense that Dr Al Muderis requested Mr Wynne to strip to his underwear in front of other patients because: Dr Al Muderis had already reviewed the x-rays and found Mr Wynne to be suitable for single-stage osseointegration (subject to the usual checks in Australia) and so there was no need for him to examine Mr Wynne at that time; it is inherently unlikely that any doctor would do that, and there is nothing to suggest otherwise in the evidence that Dr Al Muderis would do it; and that it wholly lacks corroboration;
(2) it does not make sense that Mr Wynne would agree to such a request. He is an adult male who presented as being assertive and mentally sound. There are few men of that description who would agree to strip to their underwear in a hotel room in front of people they had never met;
(3) although Mr Wynne gave evidence that he saw “red flags everywhere” but nevertheless tried “to make it work in [his] brain”, he did not convey so much when he described the meeting to Ms Roberts in a 27 March 2018 email; and
(4) that Mr Wynne said that he called and texted Mr Hernandez after he left the hotel room to share that he was a candidate for osseointegration does not make sense, as he had already been told that months earlier by email.
840 Pausing there. I accept Mr Wynne’s evidence of what occurred in the hotel room in New Orleans. His evidence is supported by other evidence. This includes the email from Ms Roberts arranging his attendance at the clinic (see [835] above), and documentary evidence in relation to other clinics she organised which were held in the United States in the same circumstances (and see Dr Al Muderis’ letter to Mr Bruha’s insurer in his case study below): see also Ms Roberts evidence discussed in Part 5, Section 5.
841 In the circumstances in which this clinic was conducted and given its purpose, I do not consider it illogical or improbable that Dr Al Muderis asked Mr Wynne to remove his pants to enable him to examine his leg. Nor is it illogical or improbable he complied with the request. I accept that Mr Wynne was given medical advice, being told he could proceed with the surgery.
842 After Mr Wynne left the hotel, he spoke to Mr Hernandez. As he was staying in New Orleans until the next day, he asked what Mr Hernandez was doing that night and whether he could come along. Mr Hernandez then invited him to join him and other osseointegration patients for dinner. Mr Wynne said he was sold on osseointegration with Dr Al Muderis after the dinner, having seen how well those patients walked compared to him.
843 Mr Wynne contacting Mr Hernandez after leaving the clinic, in the circumstances he describes, is not unusual or improbable. This was the first time he had seen Dr Al Muderis. There is no evidence of any direct contact with him before this time. Dr Al Muderis had told him he was able to have the surgery. To share that with the person who he considered a friend, is logical. His evidence that he asked and was told about the costs, and that it should be kept confidential, is consistent with the evidence of other witnesses (e.g. Mr Smith). As noted above, he photographed the price sheet he was shown by Dr Al Muderis (which is in evidence).
844 However, Dr Al Muderis did not arrange for Mr Wynne to be at the dinner with the other patients, rather Mr Wynne had asked Mr Hernandez what he was doing that night. Mr Hernandez’s invitation to dinner was in the context of his role with Dr Al Muderis. The result was that Mr Wynne socialised with Dr Al Muderis and some of his patients. As discussed elsewhere, that he socialised with Dr Al Muderis in attending the dinner disturbs the balance of the doctor-patient relationship.
845 On 27 March 2018, Mr Wynne sent Ms Roberts an email explaining, inter alia, that he would like to proceed with the surgery. Ms Roberts replied on 10 April 2018, confirming availability for surgery on 6 June 2018. She described the estimate of fees for the procedure, which align with the figures in the “price sheet” Dr Al Muderis had shown Mr Wynne in New Orleans.
846 In the 27 March 2018 email, Mr Wynne also requested a discount on the implant, explaining he will otherwise have to delay surgery by a year. Ms Roberts replied:
I discussed it with Munjed who is compassionate and does not want finances to delay surgery so he is willing to help by the following: (taking into consideration that the only fee that Munjed can control is his own surgical fees)
- Prior to the surgery you transfer $84,000 AUD (to pay for anaesthetics, hospital fees, implant, tool kit, pain specialist, general physician, psychologist, physiotherapist, prosthetist, accom[m]odation and medical-related transport)
- I have attached a breakdown in the Estimate of Fees, as you can see the surgical fee (Munjed and team) is $26,000 AUD. He has kindly offered for you to pay off this remaining amount ($26,000AUD) in installments over a year after the surgery
- The reason being - because the implant company is not as compassionate and cannot lower the cost of the implant price.
(emphasis in original)
847 I note that the estimates of fees provided to some of the domestic patients disclose that Dr Al Muderis is the sole shareholder of the companies which owns the rights to and distributes the OPL implants, and that he may receive a financial benefit from their sale. It is from his company that Mr Wynne received an OPL implant.
848 When Ms Roberts saw the 27 March 2018 email, she was in no doubt that Mr Wynne understood he was clear to proceed with the surgery.
849 On 22 April 2018, Ms Roberts sent Mr Wynne pre-admission paperwork and a pain survey, including a letter headed “Hospital Admissions Information” confirming surgery for 6 June 2018.
850 On 29 April 2018, Ms Zamani (Dr Al Muderis’ accounts manager) emailed Mr Wynne saying that she was “pleased to confirm that your surgery is scheduled for the 6th June 2018”, and attached an invoice that accorded with the payment plan Ms Roberts had detailed in the 27 March 2018 email above. In a 2 May 2018 email, Ms Zamani explained payment will need to be cleared before arriving in Australia, and to allow seven to ten working days for the transfer to complete. On 19 May 2018, Mr Wynne sent through a credit card authorisation for partial payment of the surgical fees. His emails with Ms Zamani indicate he wired the balance of the fees in early May. In other words, Mr Wynne’s surgery had been booked, confirmed, and paid for, before he had undergone any proper assessment. This all occurred before there was any discussion of the risks and complications of the surgery which, on Dr Al Muderis’ evidence, occurred in the consultation on 5 June 2018, the day before the surgery.
851 On 30 May 2018, Mr Wynne flew to Sydney with his family.
In Australia
852 On 4 and 5 June 2018, Mr Wynne had pre-operative tests and assessments, and a consultation with Dr Al Muderis. This was the first time he had seen Dr Al Muderis since New Orleans. Mr Wynne checked in with Ms Roberts and she walked him to Dr Al Muderis’ office. Dr Al Muderis introduced himself saying words to the effect of: “I’m Munjed Al Muderis. OK, you’re Billy Wynne and you’re here about osseointegration”. Mr Wynne gave evidence that Dr Al Muderis continued talking about osseointegration for about a minute and “everything he’s done in it”, before saying words to the effect of: “Is it something you would be interested in?”
853 Mr Wynne’s evidence was that he said to Dr Al Muderis he was there for surgery and his surgery was booked for the following day. He told Dr Al Muderis he had paid and that he had flown his family to Australia. Dr Al Muderis started looking through his papers and, as Ms Roberts passed by, he asked her who he was. She replied: “This is Billy, the one you met in New Orleans”. Dr Al Muderis said words to the effect of: “Oh, of course I know who you are”. Dr Al Muderis did not recall whether he had initially forgotten that he had met Mr Wynne. Mr Wynne gave evidence that this consultation was very brief. Mr Wynne, when challenged as to whether that exchange occurred, gave evidence that the interaction with Dr Al Muderis “was so profoundly shocking … I could see it right now”. Given the circumstances, Mr Wynne’s evidence of that exchange is plausible.
854 Dr Al Muderis’ evidence of the consultation relied on the consultation report. The applicant submitted the amount of detail in the consultation report shows that it must have lasted more than two minutes.
855 This consultation report, like others in evidence in these proceedings, includes many pro forma statements. I have addressed the issue of reliability of the reports elsewhere: see Part 6, Section 1.
856 Simply because something is described in the report as occurring, particularly if it is in pro forma language, does not necessarily mean that it did. I note there are errors in Mr Wynne’s report. For example, it states that Mr Wynne will be transferred to an inpatient facility for two weeks after leaving the hospital. The report also describes “a thorough discussion among the team” and a thorough interview and discussion between “the team and I” and Mr Wynne. Yet the team consisted only of Dr Al Muderis and Ms Roberts. These reflect the insertion of pro forma paragraphs as to what occurred.
857 Further, contrary to the applicant’s submission, that the consultation report refers to and describes x-rays does not necessarily mean Dr Al Muderis examined them in Mr Wynne’s presence. That said, I accept that the imaging documents in evidence say that they were ordered by Dr Al Muderis on 5 June 2018 and collected before the consultation that day. One of the topics of Mr Wynne’s cross-examination was whether Dr Al Muderis looked at his x-rays during this consultation. Mr Wynne said that could not have occurred because he did not have it done until after the consultation. Mr Wynne is mistaken about the timing of the x-rays.
858 I note that the consultation report suggests Mr Wynne had yet to pass a psychological assessment. Yet Dr Basten sent Dr Al Muderis his assessment of Mr Wynne on 18 May 2018, reporting “no major concerns that the team needs to be aware of”. On 19 May 2018, Dr Basten also emailed Dr Al Muderis, noting that Mr Wynne “seems fine” following their interview. Dr Al Muderis therefore appears not to have been aware that Mr Wynne had spoken to Dr Basten at the time of the consultation. Importantly, Dr Basten’s report said Mr Wynne “needs and deserves a little more information and reassurance than usual after a bad past experience with poor anaesthesia” (guidance which the respondents submitted Dr Al Muderis did not take into account). Dr Basten provided a similar warning in his 19 May 2018 email to Ms Roberts (which Dr Al Muderis was also sent).
859 Mr Wynne’s evidence was that Dr Al Muderis did not explain any risks during the pre-operative appointment. He gave evidence that Dr Al Muderis said he would not have an infection, but if he did, antibiotics were available. He said when he raised his concerns with Dr Al Muderis about the scar tissue on his leg, Dr Al Muderis said words to the effect of: “There’s absolutely nothing to worry about. You’re fine”. Dr Al Muderis showed him a picture of a patient he had operated on that had a burnt limb. He considered that Dr Al Muderis was dismissive of his concerns.
860 Dr Al Muderis initially said in cross-examination that Mr Wynne may have mentioned something about the scar and the healing but then appeared to have a recall that they then had a thorough discussion about that. He said that because Mr Wynne had “significant scarring on his leg and … significant burns”, he spent “significant time” talking to Mr Wynne about the healing scar. He said he remembered showing him a photo of another patient who had a “very lengthy healing scar … that had taken over a year to heal”. Dr Al Muderis said burn patients take a very long time to heal.
861 There is no reference in the consultation report to the scar tissue, the extent of it, or that he is likely to take a long time to heal as a result, something which was a pertinent matter if discussed. A matter which would be expected to be referred to in the report if the discussion occurred in the manner described by Dr Al Muderis. Rather, the report has the pro forma statement: “Billy does understand the risk of infection associated with this surgery however we regard Billy as relatively low risk. His procedure would be very standard”. Although Dr Al Muderis and Mr Wynne appear to agree that at some point Dr Al Muderis showed him a photograph of another patient who had a burnt limb, Mr Wynne suggested in cross-examination it may not have been during the 5 June consultation.
862 My Wynne’s evidence was that his biggest concern was his scar tissue healing, if cut, as this had previously been a significant issue for him. I accept that evidence. In that light, I accept that he raised this concern with Dr Al Muderis in the hotel in New Orleans and in the consultation in Australia. As a matter of importance to him, he is likely to remember Dr Al Muderis’ responses to his queries and his attitude towards it. I accept that it is probable that when he raised this, Dr Al Muderis told him that it was not an issue.
863 Mr Wynne gave evidence that for such a major surgery, he thought the pre-operative appointment should be more thorough. He had had approximately 20 operations in the United States where surgeons had been careful to explain risks to him on every occasion. According to Mr Wynne, this was the shortest pre-operative appointment he had ever had. He was concerned that Dr Al Muderis did not recognise him, and thought he was joking as he had flown half-way around the world, paid 80-90% of the costs of the procedure, and had a surgery date booked for the following day.
864 Mr Wynne, in response to the applicant’s suggestion that he had misremembered the entire interaction with Dr Al Muderis on 5 June 2018, replied, “it was so profoundly shocking … I could see it right now”.
865 Mr Wynne underwent osseointegration surgery on 6 June 2018. While Dr Al Muderis met with him immediately before the surgery, the interaction was brief: “If anything was explained, it was just reiterating ‘We’re doing osseointegration, above-knee, left side.’” Mr Wynne denied that Dr Al Muderis explained the risk of death, the risk of cardiac failure, or the risk of vascular problems. When asked in cross-examination if Dr Al Muderis explained to him the risk of pain after surgery, Mr Wynne replied “at that moment, no”, but supposed that they discussed it at some point. Mr Wynne denied that, in relation to the TMR procedure, Dr Al Muderis explained to him that the pain would get worse before it got better: “there was no conversation at all”. Mr Wynne said that he was asked for the first time at that meeting by Dr Al Muderis whether he experienced phantom pains in his legs, and Dr Al Muderis told him he could do a surgery for that but did not describe what the surgery was (Mr Wynne gave evidence that he assumed it was TMR surgery). I note TMR surgery is not referred to in the consultation report of 5 June 2018.
866 The operation report of 6 June 2018 contained the pro forma statement:
Patient was fully informed and has given consent for surgery. Patient is aware of all risks and complications of surgery such as general concern of anaesthetics including developing deep venous thrombosis and death. Patient is aware of specific complications of surgery such as nerve damage, vascular injury, wound infection, cardiac complications and pulmonary complication.
Post-surgery
867 Mr Wynne’s evidence was that on 8 June 2018, Dr Al Muderis removed his bandages. Text messages between Mr Wynne, Dr Al Muderis and Ms Roberts dated 8 June show that that afternoon, Mr Wynne reached out for help because his stump was swollen and hot, and he was experiencing nerve pain. Ms Roberts replied that it was not uncommon and organised for Dr Al-Jawazneh to see him in hospital. Dr Al Muderis also replied, advising Mr Wynne to elevate his leg above the level of his heart. Mr Wynne deposed that on or around 9 June 2018, he raised his concerns about infection again with Dr Al Muderis and Ms Roberts via text message; his evidence appears to be in relation to these 8 June messages. He separately deposed that by 9 June 2018, the end of his leg was getting red blood blisters and black skin was appearing. He believes this is where the tissue was dying because of the swelling. In evidence is a photo of his leg he sent Dr Al Muderis and Ms Roberts on the morning of 9 June, which appears to match that description. Dr Al Muderis responded, “[n]othing need to be done except monitoring”.
868 Mr Wynne was discharged on 11 June 2018 and experienced problems thereafter.
869 On 12 June 2018, Dr Al Muderis and Mr Wynne had a consultation, with the consultation report stating that his wounds “appear healthy. There is mild bruising and haematoma around the central portion of his wound without signs of infection”. However, the clinical consultation notes by Ms Dean that same day recorded that he “has been having trouble with nerve pain”, had “moderate swelling – burnt and skin graft makes hard to determine” and that he had a “[s]uperior abutment blood blister present approx. 6 cm long 1 cm width – need to monitor (pt advised of same)”.
870 Mr Wynne gave evidence that he returned to his hotel room that day, where he experienced severe pain that became unbearable. He texted and called Ms Roberts and Dr Al Muderis saying that he needed to go to the hospital and that he was about to call an ambulance. Ms Roberts told him not to go to the hospital and instead sent Dr Ho to his hotel room to take care of him. At that time the pain was so extreme Mr Wynne felt like he was dying. Dr Ho gave him a single injection into the spine for the pain (misdescribed originally as a spinal block). The metadata of a time-stamped photograph of Dr Ho during this visit states 12 June 2018, 6.37pm.
871 Mr Wynne’s evidence was the injection did nothing to help the pain in his leg and shortly thereafter, he called Dr Al Muderis and Ms Roberts again to let them know he had to go to the hospital. Dr Al Muderis called back and said words to the effect of: “I’ve got you a room at Macquarie University Hospital. You figure out your own way there”. He caught an Uber to the hospital. He said his leg was bleeding everywhere. Mr Wynne was admitted to hospital and stayed overnight. He was given a ketamine infusion, which he accepted was effective for his pain for a few days.
872 On 16 June 2018, he messaged Dr Al Muderis and Ms Roberts attaching a photograph of his stoma, asking whether he needed antibiotics because he was concerned it was infected. Dr Al Muderis responded that he should monitor it and that antibiotics were not the best option unless it was definitely infected. When shown the photograph during cross-examination, Dr Al Muderis said that it is “just bruising” from or after the surgery, “so it doesn’t look infected. No.”
873 On 19 June 2018, Mr Wynne was seen in Dr Al Muderis’ rooms, with Dr Al-Jawazneh preparing a report on behalf of Dr Al Muderis. It recorded that: “On examination his wounds look clean. There is mild oozing from his stoma and the stoma looked good and there is no signs of infection”. Mr Wynne’s evidence was he disagreed with Dr Al Muderis’ opinion on the possibility of infection. Mr Wynne recalled that Dr Al Muderis had said that there was “nothing to worry about”. Mr Wynne said Dr Al Muderis was against giving him antibiotics and assured him the redness and swelling would go down. Dr Al Muderis told him to soak his leg in Epsom salts and water every day.
874 Mr Wynne explained that because of his work as a paramedic for five to six years until his accident, “he developed something of an expertise” in responding to infections because many of his patients suffered from infections. Accepting this evidence, it follows that Mr Wynne is at least aware of and sensitive to symptoms of infections. His evidence that he believed he suffered from infections in the immediate aftermath of his osseointegration surgery with Dr Al Muderis, and that he disagreed with Dr Al Muderis’ assessment is in that context. He said Dr Al Muderis failed to diagnose those infections and, in that context, declined to administer antibiotics.
875 On 20 June 2018, Mr Wynne’s wife posted on Facebook that his “leg has been very swollen for the last few days, and [is] causing him a lot [of] pain”.
876 On 22 June 2018, Mr Wynne texted Dr Al Muderis and Ms Roberts, explaining his leg was swollen, sending a photo and asking for help. Five hours later, Ms Roberts replied, telling him to come to see Dr Al Muderis at the hospital. When shown these messages in cross-examination, Dr Al Muderis agreed that Mr Wynne was worried that his stump was swollen and therefore required attention.
877 Mr Wynne gave evidence he first saw Ms Roberts at the hospital, who told him his leg was not infected. He said he was concerned because Ms Roberts was not a doctor and had not looked at his leg.
878 The consultation report by Dr Al Muderis recorded that there were no clinical signs of infection, that Dr Al Muderis performed a wound clean, and that there were no concerning features. The report said that his stoma will take considerable time to heal due to previous damaged tissue which was burnt in the accident and required extensive grafting. Mr Wynne’s evidence of the consultation was that Dr Al Muderis scraped away the dead tissue off the wound, told him to keep soaking his leg, and that it would be fine. Mr Wynne gave evidence that he had previously had wounds smaller than this one that had taken over a year to heal and he felt like it was a big deal, although Dr Al Muderis did not act as if it was.
879 On 22 June 2018, Mr Wynne’s wife posted what the respondents described as “a sad and telling post to Facebook” detailing Mr Wynne’s pain and suffering and that they were continually being told he did not have an infection. That is an accurate description of the post. The post is entirely consistent with the evidence Mr Wynne gave as to his condition.
880 On 23 June 2018, Mr Wynne messaged Dr Al Muderis, saying his pain had been non-stop “since yesterday afternoon” and asking for help. Dr Al Muderis promptly arranged to see him that day at his clinic, recording in the consultation report that:
Billy contacted me regarding new onset pain yesterday evening which he was concerned about. I arranged for an urgent review in the clinic promptly between surgeries. I noted a clean stoma with normal bleeding, no signs of infection and no evidence of periprosthetic complications. I irrigated the stoma and am happy with the progress of Billy’s healing. I reiterated to Billy that his stoma will take considerable time to heal given his scarring.
881 On 24 June 2018, Mr Wynne and Ms Roberts exchanged messages about a boat trip. Mr Wynne advised that he could not attend because he had made other plans. Mr Wynne accepted in cross-examination that he did a “few touristy things” with his family around Sydney that day and that he was able to “get out and about”. To the suggestion in cross-examination that he felt better after his 23 June treatment from Dr Al Muderis, Mr Wynne said, “no. It was pretty touch and go … it [was] just manageable”, with some parts of the day being slightly better than others, but that “for the rest of the time in Australia it was pretty horrible”.
882 On 26 June 2018, Dr Al Muderis consulted with Mr Wynne. The report recorded, “he is progressing well and he is doing much better now and he is happy with the results”. He records “the wound is clean. I did some debridement today but nothing much, not like before”. Although Mr Wynne accepted that his wife’s Facebook post that day – in which she said he “has been feeling a little better the last couple of days. The doctors have gotten his pain under control” – was true, he pointed out that he remained in pain despite it being manageable. Dr Al Muderis continued to tell him his wound was not infected, but Mr Wynne did not believe him.
883 Dr Al Muderis consulted Mr Wynne again on 3 July 2018. The report recorded, “[o]n examination the wound is clean. We did some debridement about one week ago and now the wound does not look bad”.
884 Mr Wynne’s evidence was that he was furious during his last consultation with Dr Al Muderis and showed him how big the wound in his leg was. Mr Wynne accepted he probably did not express fury towards Dr Al Muderis, explaining that he was “completely depleted inside”. Mr Wynne said he told Dr Al Muderis that he knew the wound would take months or years to heal. Mr Wynne’s evidence was Dr Al Muderis disagreed and told him he was wrong and that it would heal in days or weeks, “absolutely not” months. Dr Al Muderis, in evidence, denied telling Mr Wynne his wound would take days or weeks to heal.
885 Either at that conversation or earlier, Dr Al Muderis showed Mr Wynne photos of another patient whose wound completely healed from a worse state than his. He showed him a photo of the wound post-surgery and a second photo of it healed. Mr Wynne recalled Dr Al Muderis saying the photos were taken two or three weeks apart. Dr Al Muderis’ evidence was that the photos were taken ten months apart.
886 To the suggestion that Dr Al Muderis said to him that he might need a skin graft, Mr Wynne explained:
I had been saying … since right after they took the bandages off that I believe that needed to be grafted, [and Dr Al Muderis replied,] “no. you don’t”, and there was the very last meeting, and he said, “… you may benefit from a skin graft.” And that was the first time he had ever mentioned it, and I remember sitting there thinking, “I’ve been saying this this whole time.” And he said, “But … it really will heal on its own.”
887 Mr Wynne gave evidence that Dr Al Muderis did not ask his doctors in the United States to coordinate his ongoing treatment. His evidence was that he thought there should have been a continuation of care plan and Dr Al Muderis should have coordinated with a plastic surgeon and wound care doctor in the United States to see the wound through its healing stages. Mr Wynne explained that by the time of the final consultation, he was convinced that Dr Al Muderis was “completely reckless” and he was ready to go home.
888 Mr Wynne returned to the United States on 11 July 2018. On 21 July 2018, he texted Dr Al Muderis and Ms Roberts with an update on his progress:
… Wound is clean, and continuing to close up nicely. The muscles in my leg are getting stronger, and my gait is improving daily. However, the greatest improvement, (that nobody can see), is the phantom/nerve pain I USE TO HAVE in that leg! It was a daily 12+ hours a day / 7 days a week! Ranging from 1/10 & what felt like rubbing a hair brush on the lateral side of my left phantom foot, to 10/10 & having the sensation of what felt like lightning bolts of electricity firing out of my phantom toes. Other than the few bad episodes of phantom/nerve pain on those first few days out of the hospital, it has COMPLETELY gone away! … Thank you again for everything!!
889 On 8 November 2018, Ms Roberts texted Mr Wynne, “... How is everything?” He replied on 9 November 2018, “... Good to hear from you! I’m doing well, the wound around the stoma continues to heal nicely!” He explained his wound had seen “quite an improvement”, sending a photo of it “from a few weeks ago” and a second “from the beginning” to demonstrate as much. He sent a further message:
Walking is incredible, so much easier now. And for the first time in over 5 years, I’m able to ride my bike with our kiddos! (something I tried over and over with the socket, but never able to do). I really hope Munjeds procedure takes off around the world, because this has truly been life changing!! Do you guys have any plans to be back in the USA any time soon? If so, let me know, I would love to meet up with you guys, to show you the progress. I hope you guys are doing well. Take care!
890 When put to Mr Wynne in cross-examination that the positive sentiment in his 9 November 2018 text messages to Dr Al Muderis was genuine, Mr Wynne explained:
… The procedure itself … is truly life-changing. … It has been the best thing that has ever happened to me. … there’s no question about that. … I really did truly hope osseointegration did take off around the world. …
Just to give a bigger picture, when I had this done, I was essentially married to Munjed … he’s the only person I could go to if I needed anything done. There’s no other [doctor] in the world, that I knew of … where I could go to for help. I was, in a sense, stuck with him. … it’s a messed-up situation. Even though … I felt that he was very reckless, I was also stuck with him. There’s that message I got from Claudia checking in. I didn’t get any sort of follow-up with Munjed. That was the only follow-up I got with Claudia. … it did feel like that relationship was dangling by a string, that if I wanted to keep the relationship going, I had to try hard … just to be able to ensure that I would get care for this part because without Munjed, I’m stuck. …
… I understand the way it looks like, and at the time I was on cloud nine about it. I was getting around better than I ever have. … I was truly happy, to an extent. There was still a good amount of pain, but walking around … was truly amazing. It was and is. …
… I did feel like I had to keep this relationship going to ensure I still had a doctor to take care of me because, especially when I left Australia, there was no connecting me with a doctor for wound care in America. There was no connection [for] care for my osseo part once I returned to America, and I felt like it was completely all on me to keep this relationship happy and alive …
It was a scary spot to be in.
891 I note that his sentiments are consistent with the evidence of other patients who are discussed below (see e.g. Ms Ulrich at [961], Ms Schaeffer at [1101] and Ms Koolhoven at [1119]). Mr Wynne separately deposed, “[w]hile osseointegration has been the best thing I had since my crash, I would not recommend my worst enemy to Dr Al Muderis”.
892 Mr Wynne gave evidence that he experienced ongoing issues with his leg upon his return to the United States. He has since suffered ongoing nerve pain. By August 2018, his primary physician had given him antibiotics on at least three occasions, and he said he was twice admitted to the emergency room to receive intravenous antibiotics for his leg. He said that each time he was put on antibiotics, it was due to the same symptoms he was experiencing in Sydney, namely redness, swelling and extreme pain in his stump. I note for completeness that after he had osseointegration surgery in 2021 on his right leg with Dr Stoneback, a United States-based surgeon, and he said was hospitalised for a serious infection.
893 Mr Wynne agreed that when he was given Dr Al Muderis’ and Mr Roberts’ contact details, he was told that he could contact them at any time, where he contacted them when he needed them, and they always responded to him.
894 In December 2018, August 2019, and September 2019, components of Mr Wynne’s osseointegration prosthetic limb broke. He reached out to Ms Roberts seeking assistance, and parts were promptly sent to him on at least the first two occasions.
895 The applicant submitted that Mr Wynne’s evidence as to ongoing issues with his leg after returning to the United States should be rejected. He submitted that evidence was inconsistent with the positive terms Mr Wynne used in his correspondence with Dr Al Muderis, his office and Ms Roberts after his return home. I disagree. I accept Mr Wynne’s explanation as to his feelings towards Dr Al Muderis and the position he considered himself to be in which, given the circumstances he found himself in, is entirely understandable. Mr Wynne, and other patients, were vulnerable and dependent on Dr Al Muderis. I note that these messages were sent in 2018. Further, there is no basis to equate those messages with there being no ongoing issues after he returned to the United States. He gave direct evidence that he was given antibiotics on multiple occasions, including intravenously when hospitalised, which he understood was administered because he was experiencing the same symptoms that he experienced in Sydney.
896 I am satisfied, amongst other things, that Dr Al Muderis failed to adequately advise of the risks and complications. When he met the applicant in the United States, no advice was given. I accept Mr Wynne’s evidence as to his pre-operative consultation with Dr Al Muderis. The consultation report shows only Dr Al Muderis and Ms Roberts were present. Any explanation of risks and complications was inadequate. The reference to infection downplayed its potential, particularly through the statement that if he developed an infection, antibiotics would be available. He did not address Mr Wynne’s legitimate concerns about the scar tissue on his leg, but rather downplayed it. The inadequacy as to the advice and the timing of it, as explained elsewhere, impacts the consent given by the patient.
897 I am also satisfied that Dr Al Muderis failed in his provision of aftercare to Mr Wynne. The set-up for his aftercare while he was still in Australia, being partly based in a hotel, leads to obvious problems. There were no arrangements in place for his aftercare after he returned to the United States. As the respondents submitted, whether Mr Wynne would have been better off had Dr Al Muderis put him on antibiotics is now not possible to test, but in any case, the post-operative treatment he received left him feeling unheard and poorly cared for. Again, this is in a context where Mr Wynne had raised concerns as to his scar tissue which were not acknowledged until after the surgery. I am satisfied in the circumstances that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Ms Rachael Ulrich
898 Ms Ulrich is also an American patient. She lives in Texas. She underwent osseointegration surgery with Dr Al Muderis in Sydney on 15 March 2017.
899 Ms Ulrich was an honest, open, credible and generally reliable witness. I accept her evidence. As explained below, aspects are supported by other evidence.
900 In closing written submissions, the applicant accepted that the Court should have no concerns about Ms Ulrich’s credit. He described her as forthright, direct and responsive. However, he submitted that her recollection of events in Australia was far from perfect and was unreliable, and the contemporaneous documentary evidence and evidence of other witnesses should be preferred.
901 Despite the above submission, in oral closing submissions he contended that Ms Ulrich had concocted evidence. An allegation of concoction is an allegation that a witness gave false evidence deliberately. In Ms Ulrich’s case, it was said to assist Mr Hernandez, an allegation also made by Dr Al Muderis himself during cross-examination. The problem for the applicant, as he recognised, is that Ms Ulrich was a credible witness, even if (on his case) a poor historian at times. Although she was mistaken about the dates and duration of some events, her evidence has support in the documentary evidence. I do not accept the submissions relating to concoction. I have addressed this issue elsewhere.
902 Dr Stephen Flecknoe-Brown and Dr Ruff were called by the respondents and gave expert evidence on Ms Ulrich’s case. I have addressed elsewhere my assessment of Dr Ruff as a witness. I accept his evidence in relation to Ms Ulrich. Dr Flecknoe-Brown is a consultant physician and clinical pathologist. He has served on health department advisory committees in both NSW and Queensland in relation to the development of guidelines for the management of anticoagulant medications and for prevention of venous thromboembolic disease in hospitalised patients. He is obviously qualified to express the opinions he did (which are referred to below). I accept his evidence as it relates to Ms Ulrich.
Background to surgery with Dr Al Muderis
903 Ms Ulrich was born with a vascular malfunction called venous arterial vascular malformation in her right leg and pelvis. She explained this means she is more prone to experiencing blood clots. Ms Ulrich’s foot had become extremely malformed because of her condition. In 2012 she had reconstructive foot surgery, from which she suffered infections.
904 Those infections, together with her vascular issues, caused a series of complications culminating in surgeries to amputate parts of her right foot in 2013 and 2014, and ultimately her entire right foot and ankle in 2015. Ms Ulrich said she also experienced a blood clot in 2009 and again in 2014. She also gave evidence of the care she received from her vascular surgeon, Dr Dennis Gable, in the context of her 2015 surgery, including that he was so concerned about her clotting risk that he instituted an anti-clotting protocol (which she described). As explained below, her evidence of what occurred in her previous surgeries (and her understanding of why) is relevant to her actions in relation to informing Dr Al Muderis of medical condition.
905 Ms Ulrich’s condition meant that it was difficult to use a socket prosthesis. She walked on one leg with crutches. While searching for a solution, she came across Dr Al Muderis’ website. She contacted his practice on 22 January 2016, completing an osseointegration health questionnaire via telephone with Ms Stewart. This form listed the cause of Ms Ulrich’s amputation as “[s]urgical amputation due to vascular malformations – Congenital”. In evidence is a generic “proposal for treatment and care” for Ms Ulrich dated 23 January 2016, and a fee estimate generated for her on 22 February 2016. It quotes US$78,000/AU$109,000 for her procedure.
906 Ms Ulrich’s evidence was Mr Hernandez, who contacted her as a result of her inquiry, informed her that Dr Al Muderis would be in Orlando, Florida in March 2016 at an orthopaedic conference. She then made plans to attend the conference with her then-boyfriend. In Orlando, she arranged to meet with Mr Hernandez and Dr Al Muderis in a hotel lobby. She said that Dr Al Muderis was sitting at a table with a woman named Shona (whom one can infer is Ms Stewart) and a woman who had osseointegration. There were other amputees nearby. She had not attended the conference, or the presentation Dr Al Muderis had given.
907 Ms Ulrich gave evidence that she and her boyfriend sat down at the table with Dr Al Muderis, and she explained her medical history to him. She said she told him of her vascular malformation issues, the dozens of surgeries she had, her history of amputations, blood clots and pain, and the difficulties she was having walking. She reiterated in cross-examination that she told him at this time she “had one clot, or a couple of clots”. She accepted she spoke briefly with Dr Al Muderis of her medical history.
908 She gave evidence that Dr Al Muderis did not ask her any questions about her medical history, did not write down anything that she said, and had a quick look at her leg (she was wearing shorts) without closely inspecting or touching it. Dr Al Muderis then said that she looked like a good candidate, and that he had plenty of patients who had vascular anomalies who had successfully had the surgery. Ms Ulrich’s evidence was Dr Al Muderis said surgery would entail an ongoing medical relationship with him, “a connection for life”, and that she would need him if anything were to go wrong, because the parts he used were patented and nobody else could “do what he does”.
909 Ms Ulrich’s evidence was that she then told Dr Al Muderis she wanted to proceed with the surgery, and that he and Shona provided her a quote for US$78,000 on the spot. She explained this was a shock to her and her boyfriend; she did not have that kind of money and had been unemployed for some time due to her medical issues. She gave evidence that Dr Al Muderis said that most people fundraise, and some put their house up and take a mortgage. According to Ms Ulrich, the entire conversation took 10 to 15 minutes. Dr Al Muderis did not provide her with any information about the risks of the surgery during this conversation.
910 Dr Al Muderis’ evidence was that he may have met Ms Ulrich in Florida but did not recall doing so. Nor, when put to him, did he recall any of the specific matters Ms Ulrich recounted in her evidence. Although he did not recall saying to her “if you have surgery with me, we will have a connection for life”, he agreed that it is the kind of thing he would say.
911 Ms Ulrich’s evidence was that she subsequently spent nearly a year fundraising and working for the operation and travel expenses, which she estimated would cost US$100,000. She created a GoFundMe on 12 March 2016. By February 2017, she had raised enough money.
912 Ms Ulrich gave evidence that she informed Mr Hernandez in February 2017 that she had raised the money and wanted to proceed with osseointegration. On 3 February 2017, a further estimate of fees was generated, honouring the US$78,000 quote she received in Florida in 2016. The AUD total was “discounted” by several thousand dollars to reflect the relatively favourable exchange rate as at 3 February 2017.
913 Hospital admissions paperwork addressed to Ms Ulrich and dated 28 February 2017 confirmed her surgery was booked for 15 March 2017. She had paid nearly all of her fees by 14 March 2017. She completed a Macquarie University Hospital pre-admission form on 3 March 2017.
914 Ms Ulrich arrived in Australia around 10 March 2017. She attended several pre-operative appointments, including a consultation with Dr Al Muderis on 14 March 2017. There is a dispute as to what occurred during this consultation, which I address below. She underwent surgery the following day.
915 Ms Ulrich developed blood clots while in hospital recovering from osseointegration surgery. A CT pulmonary angiogram dated 19 March 2017 demonstrated large bilateral pulmonary embolisms. A focus of this case study is whether Ms Ulrich disclosed her clotting history to Dr Al Muderis or his team, and Dr Al Muderis’ responsibilities as Ms Ulrich’s surgeon.
916 Venous thromboembolism (VTE) involves the formation of a blood clot within the deep veins, most commonly of the legs or pelvis (namely, deep venous thrombosis or DVT). These blood clots may become dislodged and then obstruct the pulmonary artery or one of its branches (being a pulmonary embolism or PE). Dr Ruff’s evidence was the pulmonary embolisms Ms Ulrich suffered, left untreated, may have resulted in long term respiratory compromise, pulmonary hypertension, or death. Dr Al Muderis accepted VTE can result in death.
Proof of Ms Ulrich’s history
917 The applicant submitted that there are no documents confirming Ms Ulrich’s evidence that she had previously experienced blood clots. In closing, he suggested that the Court act on the basis that there were no previous clots, or that Ms Ulrich misunderstood what she had been told. There is no basis in the evidence for why that would be so. Ms Ulrich gave direct evidence of specific actions she and her medical practitioners took on these previous occasions and, significantly, the precautionary steps her vascular surgeon took at the time of her amputation, including the rationale he gave her for those steps.
918 In any event, the submission misses the point. The issue is not whether the previous clots in fact occurred but rather, given Ms Ulrich believed they had occurred in the circumstances she described, whether Ms Ulrich disclosed a clotting history to Dr Al Muderis (or his team), and whether he acted on that information.
919 In the pre-operative stages, patients are asked various questions about their medical conditions, and on the applicant’s case, the medical team rely on their answers. A patient is asked about a previous history of DVT because it is expected that the medical team would be told if there was one and would act accordingly. Dr Ruff explained that a surgeon who is presented with a patient with a history of DVT must ensure the patient is anticoagulated at the time of surgery and for some period thereafter.
920 The applicant also submitted that the evidence of Dr Flecknoe-Brown proceeds on the assumption that Ms Ulrich had previously suffered DVT, and without proof of that, there is no foundation for his opinions. Given the nature of Dr Flecknoe-Brown’s opinions I refer to below, I disagree. As detailed below, Ms Ulrich informed Dr Al Muderis and others in his medical team of her previous blood clotting events, including Dr Gregory Bennett, a physician. Similarly, Dr Ruff’s expert evidence expressly refers to the evidence that Ms Ulrich had disclosed her previous blood clot to Dr Bennett, evidence which I accept.
Disclosure in Orlando
921 Ms Ulrich said that she told Dr Al Muderis in Orlando of her clotting history. The respondents submitted he was on actual notice of Ms Ulrich’s clotting history and was negligent in failing to take this into account both pre- and post-operatively.
922 I accept Ms Ulrich’s evidence that when she met Dr Al Muderis in Orlando, she gave him a brief medical history which included her history of blood clots. I do not accept the applicant’s submission that that is unlikely because the meeting was brief. I also accept that, having heard her history and having had a brief look at her leg, Dr Al Muderis told her she was a good candidate for the surgery (and that the conversation was generally in the terms she described).
923 The applicant submitted that even if Ms Ulrich had told Dr Al Muderis about blood clots in the meeting in Orlando, this was a “casual conversation” and not something Dr Al Muderis would be expected to remember a year later. They highlighted there were no notes of the meeting. He further submitted that, in any event, Ms Ulrich was not Dr Al Muderis’ patient.
924 The applicant’s submission illustrates a broader problem. The evidence which I accept reflects that Dr Al Muderis discussed medical matters with Ms Ulrich as a prospective patient and expressed opinions and gave medical advice without notes being taken. As previously discussed, that the applicant calls these meetings informal, or a mere chat, does not alter their true nature. Ms Ulrich acted on what Dr Al Muderis told her in Orlando. I note that Ms Ulrich’s disclosure of her blood clot history to Dr Al Muderis in Orlando is consistent with her doing the same with other medical practitioners after arriving in Australia: see below.
925 The applicant’s submission also minimises Dr Al Muderis’ responsibilities as Ms Ulrich’s surgeon. Ms Ulrich’s evidence is that, while in Australia, he did not speak to her about her history of blood clots before surgery. There is no evidence that Dr Al Muderis considered her history of blood clots. Being told of this in Orlando put him on notice and required him to take it into account in caring for her.
926 I note also Dr Flecknoe-Brown opined that although Ms Ulrich had raised the issue in Orlando, “the subject should have been raised [by Dr Al Muderis] closer to the time of surgery, in view of the rather informal way in which the initial interview was conducted in Florida in 2016”.
Disclosure in Sydney
927 Ms Ulrich gave evidence that in Australia she shared her history of blood clots with healthcare professionals who Dr Al Muderis organised for her to see. Her evidence is supported by documentary evidence from two pre-operative consultations.
928 On 13 March 2017, Ms Ulrich met with a physiotherapist. Although she was scheduled to meet Ms Sarah Benson, she may have consulted someone else. In any event, the handwritten notes of that consultation record, inter alia, “blood clot issues” (emphasis in original), and “vascular [unintelligible]” (emphasis in original). Dr Al Muderis did not recall being told that Ms Ulrich’s history of blood clot issues had been raised with a physiotherapist but accepted that “if a patient had disclosed to [Ms Ulrich’s physiotherapist] blood clot issues, that’s a matter [he] would expect be passed on to [him] as her surgeon”.
929 On 15 March 2017, the day of the surgery, Ms Ulrich had a consultation with Dr Bennett. She gave evidence that she was concerned because Dr Bennett appeared to have no familiarity with her medical history. She explained she took him through her medical history in detail, including that she had been born with vascular malformation which previously required surgery. She told him of her history of blood clots and the anti-clotting protocol that her Dr Gable placed her on when she had her leg amputated. She said she asked him whether she would be put on a blood thinner when she awoke from surgery, noting that is what occurred following her amputation surgery; he told her it would not be necessary. When she asked if he was sure given her history of blood clots and the protocol in place with her amputation, he replied that they did not want to do that because she could bleed too much during surgery.
930 A form that Ms Ulrich had completed for Dr Bennett, titled “Pre-Operative Assessment –Medical Questionnaire”, recorded that she had a superficial blood clot removed in 2008. She had also ticked “Yes” in answer to the question, “Have you or any of your blood relatives suffered a thrombosis, DVT, lung clots or clots elsewhere?”, leaving a comment, “superficial in right calf”.
931 A pre-operative consultation form Dr Bennett completed also recorded “superficial blood on the blood clot – right leg”. Dr Al Muderis accepted that Dr Bennett generally reports his pre-operative assessment to him but denied Dr Bennett told him that Ms Ulrich had disclosed any prior blood clot, DVT, or thrombosis. He accepted that if that had been disclosed to Dr Bennett, it would have been an important matter to pass on to him.
932 The applicant did not make any substantial written submissions directed to the pre-operative consultations with the physiotherapist or Dr Bennett and the notes regarding clots. In oral submissions, he downplayed the evidence. He submitted that the notes of Ms Ulrich’s consultation with Dr Bennett, in merely referring to a “superficial” blood clot, did not amount to a DVT disclosure, and Dr Bennett accordingly decided against following a clotting protocol.
933 That submission fails to grapple with Ms Ulrich’s evidence that she asked Dr Bennett about anti-coagulants and thereby put him on notice that they were considered necessary in her prior surgery. Dr Flecknoe-Brown explained that “a course of injections around the time of an operation … is the way of preventing … postoperative deep vein thrombosis”. I note that Dr Flecknoe-Brown inferred that, because of Ms Ulrich’s evidence that she had an ultrasound and injections following her 2009 and 2014 blood clots, she experienced DVT on those occasions.
934 Ms Ulrich was not required to prove to her treating doctors in Australia that she had suffered from blood clots before being listened to. That said, she did list Dr Gable as a vascular doctor on her health questionnaire and gave permission for Dr Al Muderis’ practice to contact him. There is no evidence that Dr Al Muderis or any person working with him ever sought to contact Dr Gable in connection with Ms Ulrich’s care.
935 The evidence establishes the applicant intended to file an affidavit of Dr Bennett and call him as a witness but chose not to. The respondents submitted that the Court ought to infer that Dr Bennett’s evidence would not have assisted Dr Al Muderis’ case. The respondents also point out the applicant opened his case asserting there was no medical record that they had seen suggesting Ms Ulrich disclosed blood clots to Dr Bennett. That plainly cannot be sustained on the evidence now before the Court. I accept Ms Ulrich’s evidence of her interactions with Dr Bennett. They are supported by documentary evidence. That conclusion can be more comfortably reached in the absence of Dr Bennett giving evidence.
Dr Al Muderis’ responsibilities
936 The respondents submitted Dr Al Muderis would have been negligent even if he was not in fact aware of Ms Ulrich’s clotting history, because he had a responsibility as her treating surgeon to ensure he had obtained a comprehensive picture of her clinical background that covered significant risks, including of clotting.
937 The applicant submitted that in the osseointegration health questionnaire Ms Ulrich completed with Ms Stewart on 22 January 2016 (see above), Ms Ulrich did not disclose any history of blood clots and that, in answer to a question about peripheral vascular disease, the response recorded is “Right side – Knee downward – some to hip (No anticoagulation medications required)”. I note that Dr Al Muderis accepted in cross-examination that he did not expect a patient to identify every medication they had ever taken where the form asks patients to list their medications, only the current medications they are on.
938 In the pre-admission form for Macquarie University Hospital which Ms Ulrich completed on 3 March 2017, she recorded, “No” to “Blood disorders / bleeding problems / bruise easily / clotting disorders”, and “No” to whether she had taken blood thinning medication in the past 12 months. Asked in cross-examination why she said “No” to the former question, she explained she does not have a clotting or blood disorder.
939 Dr Flecknoe-Brown observed the 22 January 2016 “questionnaire does not seek any information about previous episodes of DVT in the patient or family history of venous thromboembolic disease (VTE)”. As the respondents correctly highlighted, various patients in these proceedings completed patient intake forms, both before and after Ms Ulrich’s visit, that specifically asked about their history of DVT, but that question was not asked of her. Dr Flecknoe-Brown similarly opined that the 3 March 2017 form had not asked “the key question”, namely: “have you had thrombosis in association with surgery in the past or is there a family history of thrombosis”.
940 His evidence was, prior to the type of surgery Ms Ulrich underwent, Dr Al Muderis should have specifically asked whether she had a previous history of VTE or a family history of VTE. He opined that a form asking whether a patient has a history of blood clots is not adequate for the purpose of being satisfied that a patient does not have a previous history of venous thrombosis: “I don’t think a tick box like that is quite enough”.
941 He explained that adducing a history of thrombosis:
is an active process … it’s not just for …the patient to volunteer; it is also … for the doctor who is responsible for the question to ask the right question and go back and make sure that the patient understood the question and gave an answer upon which that doctor can rely. … the primary responsibility for obtaining a history of thrombosis preoperatively in an orthopaedic surgical patient is the orthopaedic surgeon’s responsibility.
942 He noted that Dr Al Muderis has formal training on hip and knee arthroplasty including primary and complex revision hip and knee replacement, and explained:
DVT and pulmonary embolism are high risk complications of orthopaedic surgery on the lower limbs, particularly hip and knee replacement. Thus, it would be expected that Prof Al Muderis would be aware of this issue and would assess his patients’ VTE risk pre-operatively and take appropriate precautions. Specifically, the patient should be asked about whether they have a past or family history of venous thrombosis.
943 Dr Flecknoe-Brown also gave evidence in cross-examination that neither hospitals nor anaesthetists can be relied upon to double check the patient’s DVT history. He explained in his report that “[o]rthopaedic surgeons should all be aware of the risk of VTE and ensure their patients are properly assessed for and protected from this risk” (emphasis added).
944 Dr Flecknoe-Brown was asked about Macquarie University Hospital’s use of the VTE risk assessment, which the hospital used to assess Ms Ulrich before and after her surgery. He was asked, if Ms Ulrich had disclosed any blood clotting or DVT history as part of that assessment, whether he would expect it to be listed in her clinical notes as an issue identified. He said no, he would not assume that it would be highlighted in that entry.
945 Dr Ajay Kumar, Ms Ulrich’s anaesthetist, deposed (in reply) that he held a pre-anaesthetic consultation with her the day of surgery, where he undertook a physical examination and took a pre-operative history. Thereafter, his evidence merely described his general practice. On that basis, he said he would have recorded Ms Ulrich’s history of clotting if she had disclosed it during their consultation.
946 The applicant’s submission that Dr Kumar asked Ms Ulrich about her blood clot history given his general practice places his evidence too highly. As the respondents correctly submitted, there is no evidence that he did this for Ms Ulrich. The pre-admission questionnaire he relies on does not ask the key question Dr Flecknoe-Brown described. I note Ms Ulrich also raised her history of blood clots with Dr Bennett that day. Given Ms Ulrich disclosed that history to him (and a physiotherapist on 13 March 2017), and given her concerns, it is unlikely that she would not have done the same with Dr Kumar if he had asked her the right questions.
947 I note also Dr Flecknoe-Brown’s evidence was that the medical records demonstrate that, by the time of the consultation, Dr Kumar had already planned an epidural for Ms Ulrich. He explained that because administering an epidural and Clexane (an anticoagulant) simultaneously can produce “devasting effects, including permanent paralysis below the waist”, the decision that Ms Ulrich would not be given post-operative Clexane would have already been made if an epidural was planned. The corollary for Dr Flecknoe-Brown was that he would not assume that Dr Kumar would ask questions that had already been expected to have been asked, that is, questions pertaining to previous blood clots. It is timely to recall Ms Ulrich’s evidence that Dr Bennett did not think it was necessary, and did not want to put her on a blood thinner post-surgery, and that they had discussed Ms Ulrich’s history of blood clots: see [929]. Dr Flecknoe-Brown separately explained “it’s not very common” for anaesthetists to ask about any previous DVT during a pre-operative assessment, and that it was not part of the routine pre-anaesthetic checklist.
948 It was Dr Al Muderis’ responsibility to ensure Ms Ulrich was anticoagulated (or otherwise provide appropriate care given her history) given what she disclosed to him and his team. He failed to do so. Even if Dr Al Muderis was not told of Ms Ulrich’s history, he bore the ultimate responsibility over whether she needed to be anticoagulated, as both Dr Flecknoe-Brown and Dr Ruff described. Against that background it cannot be accepted that Dr Al Muderis was not responsible for ensuring so much, because her care was shared amongst a multidisciplinary team. That he failed to obtain Ms Ulrich’s history of blood clots and act accordingly is sufficient to conclude that he was negligent in caring for Ms Ulrich. It needed to have been taken into account by Dr Al Muderis pre- and post-operatively.
949 Ms Ulrich experienced blood clots after her surgery, exposing her to the attendant risks. After the treatment of her pulmonary emboli began, her issues resolved. However, the condition untreated can be life threatening. Dr Ruff opined Ms Ulrich may have died in the immediate post-operative period.
950 To take it a step further, Dr Flecknoe-Brown and Dr Ruff were critical of Dr Al Muderis’ failure to put Ms Ulrich on a post-operative anticoagulation protocol, which they suggest was called for given she had disclosed a history of blood clots. Dr Ruff considered that anticoagulation at the time of, and following, surgery was a necessary step for Ms Ulrich. I accept that evidence.
951 I note that, although the applicant submitted that the hospital notes reflect that some steps were in place to manage Ms Ulrich’s VTE risk post-operatively, he relied on Dr Flecknoe-Brown’s evidence that those steps were appropriate. Dr Flecknoe-Brown’s evidence, however, was that the steps in place amounted to “good management, but [was] not enough” because Ms Ulrich should have had Clexane. He regarded post-operative Clexane as standard for a high-risk patient having a high-risk surgery.
Further issues
952 Below I address six further issues relating to Ms Ulrich.
953 First, Dr Al Muderis’ office generated a fee estimate for Ms Ulrich on 22 February 2016. Regardless of whether Ms Ulrich received this, or her recalling it, the fact that it was generated is significant. Dr Al Muderis gave evidence that he must have had a conversation with someone in his rooms to give them the information necessary to provide that estimate. His evidence was that a fee estimate is based on his assessment. At that time, the only information that Dr Al Muderis had of Ms Ulrich was her responses to the osseointegration health questionnaire she completed via telephone, and Ms Stewart’s notes of that call. Dr Al Muderis took issue with the suggestion his assessment was based only on health questionnaire information. However, it is plain from the documents that was the approach. Dr Al Muderis gave evidence that an assessment for a fee estimate needed to be made on clinical evidence, and not just a questionnaire. As it became apparent during cross-examination that there was no such evidence before the Court, Dr Al Muderis suggested he could have had a telephone conversation or Zoom consultation with Ms Ulrich before the estimate was generated. There is no record or other evidence of such a consultation as would be expected in a medical practice. Nor was it put to Ms Ulrich that she had spoken to him over the phone before meeting him in Orlando. His evidence was speculative and given to explain a fee estimate which had been generated in circumstances which the evidence establishes were neither appropriate nor acceptable. I note that Ms Schaeffer was similarly provided a fee estimate after submitting an online inquiry, but before any assessment by Dr Al Muderis was conducted: see case study below.
954 Second, Ms Ulrich said that she asked about the cost of the surgery in Orlando and was shocked by the amount. Although the fee estimate had been generated by that time, there is no evidence it was sent to her or that she received it. In any event, I accept there was a conversation about cost and financing in Orlando. It is plain the cost of the surgery was a significant issue for her, and it is probable she raised it in those circumstances. Her evidence of the discussion about how people raise money is consistent with that of other witnesses from the United States and Australia (see above in Fundraising in Part 6 Section 1). Shortly after the hotel meeting, Ms Ulrich set up a GoFundMe page to fund the surgery in Australia.
955 Third, Ms Ulrich’s surgery was booked and substantially paid for before she arrived in Australia; that is, before any discussion of the risks and complications of surgery. Prior to her consultation with Dr Al Muderis in Australia the day before her surgery, her only meeting with him was in the hotel in Orlando.
956 Fourth, contrary to the consultation report and the applicant’s case, Ms Ulrich denies attending a consultation where a large group of medical practitioners were present on 14 March 2017 (or at any time). I have considered the difference in Ms Ulrich’s description of her consultation with Dr Al Muderis in Australia from that of Dr Al Muderis, who relies on the 14 March 2017 consultation report.
957 The applicant submitted that the likelihood is that the consultation report is correct given that she had her consultation the same day as Mr Warland (discussed below in Section 7), whose consultation report contains a similar list of participants and who agreed that his consultation was with a group of people. However, an email circulated on 7 March 2017 listing new patients for Dr Al Muderis’ 14 March clinic lists Mr Warland as a patient but not Ms Ulrich. Ms Ulrich’s 14 March consultation report is also afflicted by pro forma or cut and paste statements. I note also that, typically, the American patients who gave evidence did not have a group consultation of the nature described in Ms Ulrich’s report. Despite the consultation report and, given the different context of the consultations for the American patients compared to the Australian patients, I consider it unlikely a large consultation occurred. Ms Ulrich gave evidence she had separate appointments with other members of Dr Al Muderis’ team in the days leading up to the consultation (rather than meeting them together). That is also consistent with documents in evidence.
958 Fifth, I have considered Ms Ulrich’s evidence of her final consultation in Australia with Dr Al Muderis, in which she recounted the anger her father expressed to Dr Al Muderis and Dr Al Muderis’ attitude in that context. Ms Ulrich’s father, on her evidence, was displeased with Dr Al Muderis’ failure to acknowledge what occurred with the blood clots or apologise. He had travelled to Australia earlier than he had planned to because of her medical condition. Ms Ulrich’s evidence was that Dr Al Muderis was blasé about what had occurred.
959 The discussion as described by Ms Ulrich is entirely plausible. The applicant’s submission that it is unlikely to have occurred given that Ms Ulrich had already lodged a complaint about the hospital and its staff, but not Dr Al Muderis, does not undermine that. That complaint was about the failure to pick up the DVT. It will be recalled that Ms Ulrich described that, in Orlando, she had a conversation with Dr Al Muderis in which he explained she would need him in the future if any complications arose. Her evidence was that this conversation “played on [her] mind” such that she was reluctant to complain when things went wrong because she believed he was the only person who could help her.
960 Sixth, the applicant submitted that Ms Ulrich was happy with Dr Al Muderis until his dispute with Mr Hernandez and, in that context, she concocted evidence in these proceedings to assist Mr Hernandez. Ms Ulrich accepted in cross-examination she saw Dr Al Muderis in September 2017 at a conference. She explained Mr Hernandez had asked her to come to the conference to model the implants and that she was at a booth for that purpose. In cross-examination of Ms Ulrich, the applicant displayed a series of upbeat WhatsApp messages between Ms Ulrich and Dr Al Muderis throughout 2017 and 2018. The messages ceased in late 2018, by which time Dr Al Muderis and Mr Hernandez’s dispute was underway. It was put to her that, in that dispute, she chose Mr Hernandez’s side.
961 Ms Ulrich acknowledged her messages with Dr Al Muderis do not reflect a problem with him, but she explained she had her “own reasons for not trusting” Dr Al Muderis. Sometime after returning to the United States, she met him at a convention and pointed out to him that a screw from her implant was digging into her leg, causing a tunnel wound. She said he told her she would need to pay $5,000 for a new piece of hardware and that he did not seem to care or want to help her. At that point, she explained, she “was done with him in my head”, but remained:
friendly with him because he had … drilled it into my head that he was the only surgeon in the world who could fix something with his patented implant in my body if something went wrong with it.
962 The applicant put to her that there was no tunnel wound and no such interaction with Dr Al Muderis, which she denied. She explained she had surgery to fix the tunnel wound. That is plausible, and I accept her evidence.
963 Ms Ulrich explained her lack of trust in Dr Al Muderis started in Australia with:
No accountability when … I ended up in the CCU [coronary care unit]. No admittance of that his team had been negligent, and not listened to me, and had dismissed my complaints for about 24 hours with all of my symptoms [when] I kept saying, “I’m pretty sure I have a blood clot.”
964 Ms Ulrich accepted she reached out to Dr Al Muderis when she needed a certificate in 2019 from him saying it was safe for her to have an MRI with the hardware in her. It is not surprising that he was the person to provide such a certificate. Ms Ulrich described in this context being:
scared to sever this relationship, because if something went wrong with this, who was going to help me, since USA doctors and surgeons were scared to even touch my leg with this implant in it.
965 Dr Ruff’s evidence on their relationship is perceptive:
It was disturbing to see Ms Ulrich’s reaction to Dr Al Muderis telling her, in Orlando Florida that because of the patents on the components of his implants she would be his for the rest of her life. She admitted that this played on her mind and skewed her attitude towards questioning Dr Al Muderis both before and after her surgery. It seems to be unreasonable control to exert over a patient who is vulnerable enough to start with and in addition making the patient less likely to question it allows the surgeon to be more dismissive. This made the patient unreasonably dependent upon the surgeon and disturbs the balance of the doctor/patient relationship in favour of the doctor. The surgery has dramatically changed Ms Ulrich’s life in the short term, it may also have ended it in the immediate post operative period.
966 Ms Ulrich’s explanation for the sentiments she expressed to Dr Al Muderis are common amongst the patient witnesses. It is something, by his conduct, he fosters.
967 I am satisfied that Ms Ulrich was not adequately assessed, given her history of blot clots, and there was a failure in her aftercare. In the circumstances, Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Mr Chris Bruha
968 Mr Bruha lives in the United States. On around 5 May 2016, he lost the use of his legs after a paragliding accident in Honolulu, Hawaii. On 12 July 2017, he underwent bilateral below the knee amputation and osseointegration surgery with Dr Al Muderis.
969 The applicant submitted that Mr Bruha is not a good historian, his evidence is unreliable, and that he is a person of no credit. It was submitted that he was “fundamentally dishonest”, and that the Court should not accept any of his evidence, except to the extent that it was against his interest or corroborated by contemporaneous documents. The basis for the submission is addressed below, and it is best understood in light of the issues that arise in this case study. Suffice to say at this stage, I disagree with that description of him, although I accept that care should be taken with his evidence. Aspects of his evidence are supported by other evidence.
Background
970 Mr Bruha gave evidence that he broke his back and crushed his ankles in the paragliding accident. He explained his back injury caused nerve damage which extended down his right leg, causing a lot of pain and weakness. He explained that for around a year after the accident, his doctors tried to operate on his ankles to save them. Mr Bruha agreed there is a lot of hardware in his body as a result of many surgeries, including hardware in the bottom half of both his legs, more so on the left than the right. He agreed that walking caused him extreme pain, explaining he was “pretty much” wheelchair-bound.
971 Mr Bruha’s evidence was that he saw a doctor in Idaho some time in February 2017 who diagnosed him with a bone infection in his left ankle. He was told there was a risk the infection would spread up the bone if left untreated.
972 He explained that he conducted research online “to try to find ways to get back on my feet”. He came across osseointegration and Dr Al Muderis when he saw a YouTube video of a below-knee amputee with osseointegration mountain biking. He contacted the amputee on Facebook, and she gave him Mr Hernandez’s number, who she said represented Dr Al Muderis in the United States. Mr Bruha telephoned Mr Hernandez, who informed him that Dr Al Muderis was going to be at a conference in Chicago.
Chicago
973 Mr Bruha attended the conference in Chicago with his mother on 5 March 2017. His evidence was that Dr Al Muderis was also meeting with about 30 to 50 amputees and others looking into undergoing osseointegration. After a lecture given by Dr Al Muderis, Mr Bruha and some of the other attendees waited to see Dr Al Muderis at the back of the conference room.
974 Mr Bruha said Dr Al Muderis conducted an individual assessment of him. This was a sit-down meeting. Dr Al Muderis examined his legs (although Mr Bruha did not say he touched them) and told him words to the effect of: “I have no concerns with your surgery and I think you are a good candidate for osseointegration”. Mr Bruha’s evidence was he had brought his x-rays with him, and Dr Al Muderis held them up to the lights so he could “take a look and see” what they showed. Mr Bruha agreed in cross-examination that Dr Al Muderis told him he would need to have tests in Sydney, and that he understood he would have to travel there “to be fully medically assessed before [it] could be confirm[ed] that [he] could have the surgery”.
975 Mr Bruha gave evidence Dr Al Muderis (without specifying the currency) quoted $75,000 per leg during the assessment. He told Dr Al Muderis that Mr Hernandez had led him to believe that the procedure would be at least half that cost. Dr Al Muderis said words to the effect of: “We have expenses we had not anticipated and are not able to cover at the lower price we were previously charging for the procedure, and so we had [to] put the price up”. Mr Bruha said that Dr Al Muderis looked over to Ms Roberts to ask how much they were charging. He felt they were making it up as they went. Dr Al Muderis said words to the effect of: “Fundraising is one of the ways patients have paid for their surgery”. Mr Bruha felt sick when he received the quote from Dr Al Muderis. He explained he wanted to get osseointegration as soon as possible but did not know how he would be able to afford it.
976 Mr Bruha’s evidence was that Dr Al Muderis did not seem concerned that he had previously been diagnosed with bone infection or that he was on very serious painkillers just to get around. Dr Al Muderis accepted that Mr Bruha may have told him of these concerns. Mr Bruha recalled that Dr Al Muderis said words to the effect of: “You will be able to walk pain free after surgery with me.”
977 Mr Bruha gave evidence that, because of the risk of his bone infection spreading up his ankle, he had limited time to make several important decisions. He explained he was “super vulnerable at the time”, and that he was “on massive doses of oxycontin while trying to make these decisions”.
978 Mr Bruha found ways to come up with extra money to fund the procedure. He said he fundraised about US$17,000, received US$25,000 from friends and took out a loan against his house to cover the balance. As explained further below, Dr Al Muderis’ office sent Mr Bruha an email attaching an invoice for the surgery (and related costs) totalling AU$176,400, requiring him to pay in full before arriving in Australia.
979 In cross-examination, it was put to Mr Bruha that he had said to Mr Steinfort that “he [Dr Al Muderis] did not” provide him with medical advice in the United States. Mr Bruha responded, “I don’t know why I would say that. I met with him for those reasons in Chicago at that point”. I note there is no suggestion that Mr Bruha did not tell Mr Steinfort what occurred when he met with Dr Al Muderis in Chicago. I note the applicant, in putting that to Mr Bruha, did not disclose that Mr Bruha subsequently said to Mr Steinfort “And if he did [provide medical advice], I don’t recall.” However, Mr Bruha characterises the statements made by Dr Al Muderis during the assessment as being of little weight, where the evidence otherwise reflects that, in substance, Dr Al Muderis provided him with medical advice in Chicago. Dr Al Muderis initially denied he had evaluated or assessed Mr Bruha at the conference or gave him advice about his suitability for osseointegration. His evidence was that they had a general discussion about the surgery and told him he would need to come to Sydney for a formal medical examination. However, he later gave evidence in cross-examination that he told Mr Bruha that he “may be suitable for osseointegration”. He later said from “the physical point of view … he was probably suitable”. This is in a context where he had considered the x-rays which Mr Bruha was asked to bring.
980 In evidence is a letter to Mr Bruha’s insurance company dated 18 May 2017. It is on Dr Al Muderis’ letterhead and bears his signature.
981 Given the terms of the letter, it was written by Dr Al Muderis on behalf of Mr Bruha for the purposes of seeking to persuade the insurance company to fund Mr Bruha’s osseointegration surgery (Dr Al Muderis agreed in cross-examination that purpose “makes sense”). The letter makes clear that the procedure is available in only a few European countries and Sydney, but not the United States. The letter recounts aspects of Mr Bruha’s conversation with Dr Al Muderis in Chicago. It refers to information which was “recorded” at the time Mr Bruha was “evaluated by Dr Al Muderis”. It also included the following:
… Dr. Al Muderis examined Chris as well as his x-rays and spent considerable time discussing the various surgical versus non-surgical options available to Chris.
Dr. Al Muderis offered Chris to come to Sydney, Australia to undergo bilateral below the knee amputations and then immediately proceed to a single stage Osseointegration procedure for both lower extremities. Dr. Al Muderis recommended that Chris have the procedure performed at the Osseointegration Center of Australia where we have performed over 300 osseointegrated procedures as of this date and more than any other center in the world. As of the date of this letter, we have performed 79 below the knee Osseointegration procedures of which 16 have been bilateral.
…
As of the date of this letter, 64 patients from the United States have chosen to undergo Osseointegration procedures at the Osseointeg[r]ation Centre of Australia. We pride ourselves in the close follow up we establish with each and every one of our patients. …
982 The letter concludes, “I am strongly requesting that you consider Chris’ appeal”, that is, that the insurance company consider Mr Bruha’s (and Dr Al Muderis’) appeal for assistance with this surgery.
983 That letter is consistent with the events that Mr Bruha described occurring at the consultation in Chicago, including that he brought his x-rays, and there was an examination and recommendation made. Its terms are unequivocal. It supports his evidence, and also that of Ms Ulrich and Mr Wynne as to the nature of the consultation in the United States. I note that the letter states that at that time 64 patients from the United States had undergone osseointegration surgery at the Osseointegration Centre in Australia.
984 Dr Al Muderis accepted he was responsible for the letter’s contents, although at the same time, distancing himself from it.
985 He disputed the accuracy of the letter’s contents. For example, he denied offering Mr Bruha to come to Sydney to undergo bilateral below-knee amputations and immediately proceed to a single-stage osseointegration procedure.
986 The applicant submitted that the letter was clearly written by Dr Rosenblatt based on information Mr Bruha provided to him in a telephone call. The applicant relies on an email chain dated 16 May 2017 involving Mr Bruha, Dr Rosenblatt, Mr Whelan and Mr Hernandez. Those emails do not support the submission.
987 The chain commences with Mr Hernandez asking Mr Whelan if someone can contact Mr Bruha, explaining that Mr Bruha had contacted Mr Hernandez seeking information before proceeding with booking his surgery. In the next email, Mr Whelan explains to Mr Hernandez “the information required is medical … Solon [Rosenblatt] will call Chris tomorrow”. The next email is from Dr Rosenblatt to Mr Bruha:
… I understand you met Munjed recently and you have some questions regarding the osseointegration procedure? I am one of the surgeons that works with Munjed and would be happy to answer any questions you might have. I understand you live in Montana? What is a good time for me to call you? …
988 Mr Bruha then proposes a call for that day.
989 It is plain from the correspondence that Dr Rosenblatt was not at the consultation in Chicago, and the purpose of the call was for Dr Rosenblatt to field Mr Bruha’s questions about osseointegration. There is no suggestion in the correspondence that Dr Rosenblatt needed or intended to ask medical questions of Mr Bruha to procure any of the detail underlying the letter. Conceivably, Mr Bruha may have raised the need for an appeal to his insurer and some discussion ensued, but there is no evidence to that effect, let alone any to support the applicant’s submission Dr Rosenblatt wrote the letter (or any part of it). Nor is there anything in the evidence to suggest that this letter was written based on anything Mr Bruha said to him.
990 The only other evidence relied on by the applicant in support of his submission is that although the letter is on Dr Al Muderis’ letterhead, it also has what is said to be Dr Rosenblatt’s logo on it.
991 Mr Bruha’s evidence on the topic does not assist as he is unclear as to who he talked to about the letter, and when or how any conversation occurred. As to the email exchange, he deposed that his telephone conversation with Dr Rosenblatt was about administrative matters for when he arrived in Australia and the procedure generally.
992 The applicant’s submission presupposes that Mr Bruha told Dr Rosenblatt what occurred at the consultation in Chicago and that Dr Rosenblatt blithely put it in the letter on that basis. That premise has no foundation. It also presupposes Dr Rosenblatt then sent the letter in Dr Al Muderis’ name, without checking with Dr Al Muderis whether its contents as to what occurred at the consultation and the advice given to Mr Bruha as recorded in it were correct. That is inherently implausible. There is no explanation as to why that would have occurred. The letter, as apparent from what is recited above, includes information which is said to have been recorded at the time of the Chicago consultation. Dr Rosenblatt was not at that consultation. It contains details, such as the fact and content of the recorded information referred to which would not be known by Mr Bruha. If the letter was written by Dr Rosenblatt on his own volition, there is no reason why he would not have signed it. It bears Dr Al Muderis’ signature. I do not accept the applicant’s submission. In any event, regardless of who wrote the letter, I do not accept that Mr Bruha provided the information for its contents.
993 The applicant submitted that the proposition that Mr Bruha was confirmed as suitable for osseointegration in Chicago is inconsistent with contemporaneous documents. I note Mr Bruha’s evidence was that Dr Al Muderis said he was a good candidate for osseointegration. He does not use the word confirmed. In any event, the primary contemporaneous document referred to is the email chain dated 16 May 2017 described above. The applicant submitted that well after the Chicago conference, Mr Bruha contacted Mr Hernandez to say (according to Mr Hernandez’s email) that he was “looking to book in July but needs some information before he can proceed”. That correspondence is not inconsistent with Mr Bruha’s evidence. The applicant conflates two different concepts; one being what Dr Al Muderis told Mr Bruha as to his suitability for surgery, the other being Mr Bruha’s decision to undergo the surgery.
994 As to the assessments which were to occur in Australia, the fee estimate, emailed to Mr Bruha on 21 May 2017 (the estimate itself is dated 18 May 2017), states, inter alia, that “[w]e require patients to arrive 5 days pre-surgery to complete all necessary pre-operative assessments”, and:
[t]his time frame will also allow you to settle in as well as undergo some routine investigations i.e., pathology collection, gait analysis prior to the surgery, and further investigations to examine energy expenditure etc.
995 It states that “[a]fter confirmation of a surgical date, patients will receive an invoice reflecting” the estimate provided. As discussed elsewhere, Dr Al Muderis’ office required Mr Bruha to make payment in full before arriving in Australia. The description of undergoing pre-operative assessments is consistent with the surgery date being confirmed.
996 The applicant placed emphasis on a passage in the covering email from Dr Al Muderis’ office:
We appreciate your assistance in answering all the questions for our medical screening. This along with x-rays and pictures assists us in our assessments and if you have not yet been able to send x-rays or pictures we would very much like them to be sent to us in the very near future. …
We have attached some information for you to read as well as a cost estimate so that you can be informed about your choices.
997 That a patient is providing information and completing forms before arriving in Australia is not inconsistent with Mr Bruha’s evidence as to the nature of the meeting in Chicago or what he said Dr Al Muderis told him. The invoice for AU$176,400 was sent to Mr Bruha on 7 June 2017, which noted surgery was for 12 July 2017. A separate document establishes that the surgery date was confirmed by 24 May 2017, with the document also recording that the pre-admission papers and pain forms had been received from Mr Bruha.
998 The applicant relied on the passage from the covering email recited at [996] to submit:
The communications summarised above are consistent with Dr Al Muderis and his team continuing to collect medical information about Mr Bruha as of May 2017, the assessment process being ongoing, and no final decision to proceed with surgery having been made as of that time. The Court would accept Dr Al Muderis’s evidence that he did not conduct a full examination of Mr Bruha and did not definitively advise that he was suitable for osseointegration, during the meeting in Chicago.
999 The limited information collected by this time is that referred to above. The respondents did not submit that Dr Al Muderis conducted a “full examination” of Mr Bruha in Chicago, only that he conducted an examination. Indeed, part of the complaint is the scant nature of the examination, and the limited information provided to patients. Further, advising a patient that they are suitable for osseointegration in the manner described by Mr Bruha does not necessarily equate with advising a final decision to proceed. The applicant appears to be setting up a strawman. That these assessments are occurring in Australia is not inconsistent with and does not undermine Mr Bruha’s evidence.
1000 The applicant criticised the respondents’ cross-examination of Dr Al Muderis on the basis that he had no communication with Mr Bruha between the meeting in Chicago and Mr Bruha’s arrival in Sydney. The applicant submitted that although Dr Al Muderis did not recall specifically doing so, he explained that it was highly unlikely that there were no communications, because in every case there are phone consultations with the team. It is plain from the terms of the cross-examination that it was directed to Dr Al Muderis’ contact with Mr Bruha, not others. Dr Al Muderis answered that although he did not know, it was “very unlikely” that he had no other communication with Mr Bruha during this intervening period. There is no evidence of any other communication between him and Mr Bruha. Nor is there any documentary evidence of a further consultation. It was not put to Mr Bruha that he spoke to Dr Al Muderis during this period. Mr Bruha did not give evidence of any communication. No evidence supports Dr Al Muderis speaking with Mr Bruha again until their consultation on 11 July 2017, the day before his surgery. There is nothing improper about the respondents’ questioning. I do not accept there was any other consultation or communication by Dr Al Muderis with Mr Bruha in the intervening period.
1001 What is really at issue is that Mr Bruha, (and the other American patients who had met him in the United States), based their decision to pay for surgery and subsequently travel to Australia on Dr Al Muderis’ advice. That is so even if they were also getting information about the process from others in Dr Al Muderis’ team. They were expecting surgery to occur. The terms in which the fee estimates are couched are consistent with the conduct which Mr Bruha described occurred in Chicago.
Misleading information
1002 Two aspects of information given to Mr Bruha in Chicago are said by the respondents to be misleading: being told he would be pain free and the infection rates.
1003 As to the first, it will be recalled that Mr Bruha gave evidence he was told that he would be able to walk pain free after the surgery. Dr Al Muderis could not recall saying this. The respondents submitted that the Court ought to be satisfied that the statement was said, consistent with Mr Smith’s evidence, and that it too constituted a serious failure to warn of the risks and complications of the proposed surgery. This statement is akin to that which Mr Smith said he was told by Dr Al Muderis: see case study below in Part 6, Section 7. As already explained, there is also promotional material from which a reasonable person would understand osseointegration surgery was a pain free experience (see Brochures – misleading statements in Part 6, Section 1). In that context, I consider it likely that the statement was made to Mr Bruha.
1004 As to the second, the infection rates, the respondents submitted Dr Al Muderis’ slide show and presentation in Chicago (which Mr Bruha and other prospective patients attended) presented a positive, and totally misleading, picture about low rates of infection related to osseointegration surgery. They submitted that Mr Bruha’s evidence about what was said as the slides were shown is entirely consistent with the ordinary reading of those slides. The slides of the presentation are in evidence.
1005 Dr Al Muderis’ evidence was that the slides related to a study. The purpose of the study, he said, was to introduce a classification system for infection and complication rates and was not to convey the results of complication rates. He rejected the suggestion that he was presenting a representative study, explaining the presentation “was presenting results of a particular paper on a particular cohort of patient[s] in a particular period of time … [t]hat does not reflect the overall complication rate”.
1006 The study was conducted between 2009 and 2013 on a cohort of 86 osseointegration patients. Mr Bruha deposed that during Dr Al Muderis’ presentation he said words to the effect of: “The rates of infection in my patients are really low and where infection does occur, it can be dealt with very easily”. He explained Dr Al Muderis made it sound like it was a rarity that his patients ever had their osseointegration surgeries reversed. Dr Al Muderis rejected Mr Bruha’s evidence.
1007 The slides showed that 30% of patients in the cohort experienced grade 1 infections (the least serious), 5% experienced grade 2 infections, and no patients experienced grade 3 or grade 4 infections (being “deep infection” and “implant failure”, respectively). Dr Al Muderis accepted in cross-examination that at the time of this presentation some of his own patients had experienced grade 3 and 4 infections (but said those matters were not captured by the particular paper he was presenting).
1008 There is no express disclosure in the slides that the cohort was not representative. To the contrary, aspects of the slides convey that the cohort was representative. One slide includes an excerpt of the paper that originally published the study: “We report on the safety of press-fit osseointegrated implants currently used in Australia and the Netherlands”. The presentation otherwise holds the paper out as “The Safety Paper”. Absent an express disclaimer, it was open to the audience to infer that the basis for a safety report is a representative sample of patients.
1009 In any event, there is no evidence that Dr Al Muderis identified any limits on those figures for the audience. Significantly, nor is there evidence that Dr Al Muderis spoke of the patients outside of the study’s cohort who had in fact experienced the serious symptoms reflected in grades 3 and 4 infections.
1010 The problem with the presentation is the audience included prospective patients in addition to clinicians. Although Dr Al Muderis may have been presenting non-representative figures, that does not answer the claim that the presentation was misleading. The figures show a very positive result, which could readily be understood by a lay person to have broader application, as in the case of Mr Bruha. In that context, Mr Bruha’s evidence of Dr Al Muderis’ statements about infection (see e.g. [1006] above) is plausible. Mr Bruha, who was particularly concerned about infection, given what he was advised was his condition, would have been alert to any information on the topic.
1011 As will be apparent from a consideration of the case studies, other patients gave evidence of being told by Dr Al Muderis in their consultations, in effect, that infections rates were low and not a matter of concern and, as discussed elsewhere, the consultation reports generally downplayed the risks of infection.
1012 I am satisfied the presentation was misleading to lay persons. The slide show conveyed that the risk of serious infection for osseointegration patients was remote or non-existent.
Risks and complications
1013 It is appropriate at this stage to refer to the broader evidence in relation to what Mr Bruha was told about the risks and complications of the surgery.
1014 Mr Bruha deposed Dr Al Muderis did not explain any of the risks of the surgery to him during the Chicago meeting (or on any other occasion), other than a risk of mild infection. As the applicant submitted, the slide show presentation at the conference did refer to complications other than infections, including fractures, over-granulation (i.e. hypergranulation), skin redundancy, implant failure and loosening, as well as red flags during rehabilitation. These complications (but not the rehabilitation red flags) appear to be results of “The Safety Paper”.
1015 Mr Bruha accepted that the presentation ran for about 45 minutes and that Dr Al Muderis explained the surgery, talked about the upsides and downsides of osseointegration and the risks of the surgery. Of the risks put to him in cross-examination that were discussed, he particularly remembered infection and stress fractures (from the implantation of the prosthesis). Mr Bruha said he was concentrating on his phone as he was recording parts of the presentation; he explained that the most important part to him was meeting Dr Al Muderis after the presentation, and that “the slide show was something I was just going to look at on my phone afterward”. Mr Bruha did capture parts of the presentation on is smartphone which are in evidence.
1016 Irrespective of what was said in a presentation at a conference, that Mr Bruha attended the presentation does not alleviate a doctor’s responsibility to explain the risks and complications to patients. As Dr Ruff explained:
The use of brochures or other documents explaining treatment options, benefits and risks that are prepared by the surgeon or a professional association is only an adjunct to the process of informed consent. They do not replace a discussion with the patient …
1017 I am satisfied that at the time Mr Bruha paid for his surgery, before arriving in Australia, Dr Al Muderis had not explained to him the risks and complications of the procedure (nor how they would pertain to him).
1018 Mr Bruha next saw Dr Al Muderis in Australia on 11 July 2017. In this regard the applicant relied on the consultation report dated 11 July 2017, being the consultation the day before Mr Bruha’s surgery. This report is discussed above: see Consultation reports in Part 6, Section 1.
1019 This report is far more detailed than that of other patient witnesses. It is unsigned and has no addressee. There is no evidence of Mr Bruha seeing this report. Mr Bruha agreed in cross-examination that he and Dr Al Muderis had talked about risks and complications generally. As to whether Dr Al Muderis said there was a high risk of infection, Mr Bruha said that he had no recollection of it being said but agreed it may have been.
1020 The applicant submitted that, when the substance of Dr Al Muderis’ consultation report was put to Mr Bruha in cross-examination, he agreed with effectively all of it, and the Court should therefore accept that the report is an accurate summary of the consultation. Although some of the report’s substance was put to Mr Bruha, other key details were not (e.g. that the infection risk is “100%”; that he may lose his leg above the knee as a result of the “dramatic” infection risk; that he might need intravenous antibiotics; that he may need to take antibiotics “for a prolonged period”; that he may need multiple debridements; that the implant may need to be removed; that self-care and hygiene is paramount; granulation risk, “especially activity related”; risk of periprosthetic fracture; clots in leg/lung; general anaesthesia risks (death etc)).
1021 The applicant’s submission that the discussion of risks was recorded in more detail than usual in this report because of Dr Basten’s warning that Mr Bruha was particularly anxious about infection and required special reassurance is rather curious (he did not do this for other patients who were anxious about infection (e.g. Mr Wynne) who Dr Basten advised needed extra reassurance). That was not Dr Al Muderis’ evidence. His evidence was that he “went into great detail informing Mr Bruha about the risk of infection in light of Dr Basten’s advice that he was anxious about infection” (emphasis added). The implication from that answer is that he told Mr Bruha more than he ordinarily would, not that he recorded more in his report. In any event, it will be recalled that on the applicant’s case, the report is not for the patients’ benefit: see Consultation reports in Part 6, Section 1.
1022 It follows that, on the applicant’s case, the discussion he had with Mr Bruha about the risks and complications of the procedure occurred on the day before the surgery was scheduled to occur. The implications of this have been explained elsewhere.
The surgery
1023 I address two issues.
1024 First, during Mr Bruha’s surgery, Dr Al Muderis amputated his left leg higher than his right leg because there was more proximal hardware in the left leg than the right. Although the consultation report explains the “amputation will be at a clear level away from the hardware to avoid any contamination”, there is nothing in the report that supports the proposition that his legs would be uneven. That is also consistent with Mr Bruha’s evidence. Mr Bruha deposed, and largely reiterated in cross-examination, that after the surgery Dr Al Muderis told him words to the effect of:
I had a hard decision to make to make it uneven. You will just have to live with it. I made the decision because you had metal in your left leg and I had to get above that on the leg.
1025 Dr Al Muderis’ evidence in re-examination was that he remembered discussing with Mr Bruha pre-operatively “that he had the hardware at different levels. And I explained to him on the screen how and where his leg would be amputated to have a clear margin” and “that was a difference in the … legs”.
1026 As the respondents pointed out, this discussion was not put to Mr Bruha, which would have been expected. Nor is the discussion relied on in the applicant’s submissions. I note also that the applicant’s evidence does not explain why the legs are uneven. That it was necessary to be clear of the hardware does not explain that.
1027 Second, shortly before the surgery, Mr Bruha drew on his own legs with a Sharpie, pointing to where the amputations were to occur. He gave evidence that this was because the paperwork in relation to the operation incorrectly described that the amputations were to occur above the knee. Photographs taken at the time show that there were markings above his knees, being the words “no femur”, with arrows pointing down to his feet, Mr Bruha described he did that to emphasise that the amputation was not to be done at his femur. The hospital record also mistakenly states the operation performed was at the femur level, while also later stating it was a below the knee amputation.
1028 There is also a photo with Mr Bruha’s initial markings mostly scrubbed off, with fresh markings extending to his lower legs, with lines across each of his shins. The lines appear even on each leg. Mr Bruha’s evidence was that Dr Al Muderis was upset at him for using a Sharpie, citing a risk of infection, and he then cleaned Mr Bruha’s legs and made the fresh markings. Although there might have been an issue as to which of the pre-operative rooms this occurred in, it can be accepted such an incident occurred.
1029 Mr Bruha’s concern about the paperwork correctly reflecting the procedure is not unreasonable given it involved amputating his legs.
Post surgery
1030 Mr Bruha gave evidence that he had a hole in his right shin following surgery. Photographs taken before and after the surgery demonstrate as much. He said he observed the hole as soon as his dressings were changed for the first time following his surgery. Mr Bruha deposed that the wound in his right leg looked like a gunshot wound, which was “about the size of a US quarter”.
1031 Mr Bruha’s description of it being a hole appears apt on the photographs. What is less clear is when the hole was evident, and the cause of it. Mr Bruha deposed that Dr Al Muderis did not give a straight answer as to what the hole was, although in cross-examination he accepted that Dr Al Muderis was not dismissive of his concerns in relation to the hole. He said no one would take responsibility for it. Mr Bruha opined in his affidavit that the cause of the hole was an incision, but that is speculation.
1032 Nonetheless, Dr Al Muderis does not address the hole in his affidavit. Mr Bruha deposed that Dr Al Muderis blamed him for the hole and told him: “The infection probably occurred because you were a mountain biker and had scratches on your leg from before the surgery.” Mr Bruha maintained in cross-examination that when Dr Al Muderis first saw the hole he blamed him, saying, “What did you do here”, and that “he thought it came from the mountain bike wreck”. In cross-examination, Dr Al Muderis denied that it was a surgical incision, explaining that it was a fracture blister that occurred after the surgery.
1033 Dr Al Muderis in cross-examination said that on 7 August 2017, the date of his last consultation with Mr Bruha, he wrote a prescription for antibiotics because Mr Bruha had a fracture blister, which increases the risk of infection. I note that there is no reference to that fact, or to what is said to be a fracture blister, in the consultation report for that day or any other day. Mr Bruha said he had not heard of the hole being a fracture blister until his cross-examination.
1034 Dr Al Muderis’ evidence in cross-examination as to the reason he prescribed antibiotics is inconsistent with his affidavit evidence. He deposed:
I did not observe any signs of infection when I saw him on 7 August 2017, just as there had been no evidence of infection throughout the post-operative period. I wrote him a script for antibiotics to take home, but I routinely do that with international patients in case they develop an infection whilst in transit.
1035 None of the other American patients who were called gave evidence supporting that practice (indeed, Mr Wynne explained that Dr Al Muderis refused to prescribe him antibiotics before returning home: see [872]-[873]). Given the applicant addressed in his affidavit the purpose of prescribing antibiotics on 7 August 2017, that he failed to initially cite the fracture blister as a basis for the prescription is noteworthy.
1036 I note although Dr Al Muderis said that there was no evidence of Mr Bruha having an infection after surgery while he was in Australia, there is no evidence that Mr Bruha had any infection tests conducted post-operatively. This is to be contrasted with the evidence of pre-operative tests. Dr Flecknoe-Brown expressed the view that if something is done, a doctor should record it (“not documented, not done”). Although Dr Stoita opined that, based on Mr Bruha’s symptoms, clinical examination and investigations, there is no evidence that he had an active bone infection at the time of the consultation on 11 July 2017, Dr Stoita does not (and was not asked to) express an opinion about an infection suffered by Mr Bruha at any other time.
1037 There is no sufficient evidential basis to make a finding as to the cause of the hole in Mr Bruha’s leg. The photographs by themselves are insufficient, as is Mr Bruha’s speculation. I recognise that there appears to have been no explanation proffered to Mr Bruha, which is curious. It is unclear why, if it was a fracture blister, he was not told that. There is no documentary record in support of that. Of course, absence of evidence does not amount to evidence of the opposite. In any event, for present purposes, the cause of the hole is not as significant as what was said to stem from it.
1038 Mr Bruha’s evidence was that he had an infection after surgery and was given three rounds of antibiotics in Sydney, which held it at bay. Dr Al Muderis’ evidence is that Mr Bruha’s concern about having a potential infection during this period “was not rational” noting he was “seen regularly by physicians and nursing staff at Macquarie University Hospital who did not identify signs of infection”. Mr Bruha had post-operative consultations on 18 July 2017, 31 July 2017 and 7 August 2017. The 31 July 2017 consultation report recorded that Dr Al Muderis prescribed him Keflex (an antibiotic) on that day. Mr Bruha said he knew he had an infection and that there were photos of his right leg inflamed. He described that his leg was painful and hot. He said that one of those photos showed that there was redness around the sutures and to the right of the leg, but the left leg was healing nicely by comparison. He disagreed that Dr Al Muderis said to him he saw no signs of infection: “the discussion I recall was that I had an infection”. Mr Bruha was not challenged on his evidence as to the courses of antibiotics he had in Australia. Being prescribed antibiotics is consistent with Mr Bruha’s evidence, particularly given Dr Al Muderis’ inconsistent explanations for the last prescription (referred to above).
1039 The applicant submitted that Mr Bruha’s claims that he has suffered “ongoing infection issues”, that he has been on and off antibiotics “for the entire time” after the osseointegration, and that doctors at a wound clinic were concerned about a possible bone infection in his legs, are unsupported by any medical records.
1040 Mr Bruha accepted in cross-examination that he was told by the hospital staff it was better to leave the dressing off the hole so that it could breathe.
1041 He explained that a month after returning to the United States the wound still had not healed, and so he attended a specialty wound clinic. He had tried to take care of it himself at home, but to no avail. His evidence was he visited the wound clinic for two to three weeks. Mr Bruha said the clinic advised he leave the dressing on and keep the wound moist, and that it then healed within approximately three weeks. He said that the doctors were concerned about how long the wound had been open, and of a possible bone infection in that leg and the left leg. Mr Bruha was put on intravenous antibiotics in Bozeman, Montana, before moving to a hospital closer to his town.
1042 Mr Bruha’s evidence that he went to a wound clinic to treat the hole in his shin is supported by an email he sent to Dr Rosenblatt on 6 October 2017. Mr Bruha wrote to Dr Rosenblatt:
I am going to a wound clinic for that open spot on my [right] shin. They are worried because it has been open this long that the bone may be infected. They would like to [do] a CT scan but are worried the metal may heat up, They are wondering how you would deal with this issue? …
1043 This is a contemporaneous record of what he said he was doing and why.
1044 Mr Bruha gave direct evidence of attending the clinic, the period of doing so, that he was given drugs intravenously, and that the wound appeared to have healed. Mr Bruha can give evidence of what he said are the symptoms he experienced at various times, and that he was given drugs that he believed were antibiotics.
1045 Jumping ahead. In early 2020, Mr Bruha said he received advice from a doctor in Montana that he would need to have the implants removed because the infection would not go away and he would otherwise be on antibiotics the rest of his life. He explained he acted on this advice and had his implants removed by Dr Stoneback, an orthopaedic trauma surgeon at the University of Colorado Anschutz Medical Campus.
1046 Dr Stoneback’s evidence was that he examined Mr Bruha on 23 October 2019. Mr Bruha’s case was then presented to a multidisciplinary team. The team’s consensus was Mr Bruha’s chronic pain and drainage symptoms were most likely due to chronic osteomyelitis of his bilaterial tibias, his left side worse than the right. An intravenous antibiotic therapy course was discussed with Mr Bruha, including the possibility of implant removal if his pain subsequently returned. Mr Bruha underwent the course, which resolved his pain within days.
1047 Dr Stoneback’s evidence was that on 21 December 2019, Mr Bruha elected to come off antibiotics and have his implants removed, given his multiple recurrences of infection. Dr Stoneback conducted the surgery on 6 January 2020. He also conducted deep bone biopsies which tested positive for chronic osteomyelitis and infection. Mr Bruha now uses socket prostheses.
1048 Mr Bruha described that he had spikes inserted into his bones in both legs where the implant had been which fed antibiotics directly into the infected bones (Dr Stoneback describes the process as intramedullary antibiotic nail treatment). Mr Bruha went to the hospital every day to have the intravenous antibiotics administered into the spikes, before they were removed six weeks later. Mr Bruha and Dr Stoneback each gave evidence that the infection was gone after the spikes were removed.
1049 The applicant’s submission that removal of the implant is a known complication of the surgery misses the point. It fails to address how that complication materialised, given Mr Bruha’s evidence of ongoing symptoms of infection and being given drugs for it.
1050 The applicant referred to three matters which are said to be inconsistent with Mr Bruha’s evidence about infections: (1) Mr Bruha participating in a 50-mile trek in Sydney with other osseointegration patients (“Amp Trek”) in May 2018; (2) him attending a conference for amputees in Tucson, Arizona in July 2018; and (3) him appearing in a video, made by College Park (a prosthetics company), shortly after that conference in which he is hiking.
1051 Those activities are not inconsistent with his descriptions of infection. Bearing in mind that Mr Bruha gave evidence that he misses the lifestyle he had when he had the osseointegration implants.
1052 Mr Bruha accepted: he saw Dr Al Muderis while in Sydney for Amp Trek; that Dr Al Muderis got him to have an x-ray; and that he went to the clinic to do some walking tests.
1053 Mr Bruha gave evidence that he saw Dr Al Muderis at a conference for amputees in Tucson, Arizona in 2018, and told him he “still had infections”. Mr Bruha explained Dr Al Muderis got down on his knees, pulled up his pants and said words to the effect of: “It looks fine, you’ll be okay”. Mr Bruha said Dr Al Muderis wanted him to wear shorts so that people could see his osseointegration prostheses at the conference. Mr Bruha explained that he was wearing long pants to conceal his legs because, at that time, he had an infection, and his legs were oozing and in pain. He explained that he changed into shorts because Dr Al Muderis insisted that he do so, asking him repeatedly. Mr Bruha maintained that he wore pants when he first arrived because his stomas were not healthy. The applicant put to Mr Bruha that this was a concoction. This seems to be based on a video that shows him wearing shorts at the conference. That video is not inconsistent with Mr Bruha’s evidence.
1054 The video made by College Park promoted the prostheses Mr Bruha was using. When the applicant suggested to him there was nothing oozing out of his stomas, Mr Bruha asked to watch the video again. He pointed out that in one frame one can see a stoma was red at the bottom and that there was ooze coming out. The redness is seen on the video. The respondents submitted that “[t]he purpose” of showing Mr Bruha the video “was to allege that [he] was lying about being infected as he was wearing shorts”.
1055 None of those matters relied on by the applicant are inconsistent with Mr Bruha’s evidence of infections.
Assessment as a witness
1056 Returning to explain the basis of the applicant’s submission, it is contended that Mr Bruha is not a good historian, unreliable, a person of no credit, and “fundamentally dishonest”.
1057 The applicant relies heavily on a text Mr Bruha sent to Dr Al Muderis on 24 February 2023 to submit that he should not be considered an honest and reliable witness. The applicant recited part of it:
This is Chris Bruha, I have a suggestion to see if you have any interest in making a deal.
I have a loan amount of Around 223k to have you do my surgery.
I am asking that you pay me back so I will not be 60 minutes main wittiness’s. …
However if you decide not to pay me back what I feel you took from me I will do whatever it takes.
… I will sign off with you and your attorney’s not become a bigger financial burden if we can agree on an amount between us. …
1058 The applicant submitted that the text message is a “naked attempt at blackmail”, and Mr Bruha’s warning that he would “do whatever it takes” if Dr Al Muderis did not comply is indicative of a willingness to say anything for the sake of damaging him, regardless of whether it is true.
1059 The respondents submitted that the submission misrepresented what Mr Bruha said, explaining that it was clear from Mr Bruha’s evidence that while the amount of money he sought repayment of was higher than what he had paid Dr Al Muderis, the additional amount covered matters associated with his procedure (including loans and other expenditure). They submitted that it was not an extortion attempt. Mr Bruha was doing no more than holding out to Dr Al Muderis that he would cease to cooperate with the respondents if Dr Al Muderis acted honourably by reimbursing him for his losses by reason of his failed surgery.
1060 Sending such a text can properly be criticised. However, the text and its implications are not quite as simple as the applicant portrays. As set out below, the terms of the text considered in full (only part of which the applicant recites) are premised on problems that Dr Al Muderis faces arising because of his lack of patient care being true:
Your poor Pt care is going to ruin you. If I ever failed like you have I would have to repay my customer. I guess you do not play by those rules. …You are a sad idea of a surgeon for sending me home with an open wound that took specialists to heal and almost three years of IV antibiotics. Karma will take care of you in the end I guess.
1061 He is not suggesting that he would concoct evidence, but rather he would not give what he said was evidence of his experience. He was holding out that he would cease to cooperate with the respondents if Dr Al Muderis reimbursed him. It was submitted that Mr Bruha was seeking to make a profit, because the amount sought was more than he spent on the surgery. The amount sought, which is oddly specific, was described as a loan amount, and Mr Bruha gave evidence he took out a loan. As Mr Bruha accepted, the amount was more than he paid for the surgery, but there were other expenses (repaying loans, paying for the removal of the implants). In all the circumstances, I do not agree with the description of making a profit.
1062 I note that another of Dr Al Muderis’ former patients, Mr Mortimer, asked to be repaid for the money he had expended, in a letter dated 12 November 2019, detailing his issues with Dr Al Muderis: see Part 6, Section 6. There was no response.
1063 It is plain that particular care must be taken in assessing Mr Bruha’s credibility and the reliability of his evidence. It appears that the submission in relation to him being a poor historian is, in large part, based on the fact his evidence is disputed by the applicant or is said by Dr Al Muderis to be inconsistent with his conduct (examples are addressed elsewhere).
1064 That said, as apparent from the discussion above, there is support for parts of Mr Bruha’s evidence, including from the applicant. There is also support from evidence in some of the other case studies. Moreover, there is also support for his concern that he had infections, and that he left Australia with an open wound. It is to be recalled also that on medical advice his implants were ultimately removed.
1065 The applicant also alleged that Mr Bruha concocted evidence because of Mr Hernandez. The submission was that Mr Bruha was “wholly happy” with Dr Al Muderis a year after surgery. The applicant cited as examples: Mr Bruha’s trip to Australia for Amp Trek, his last interaction with Dr Al Muderis being positive (when Dr Al Muderis and Ms Roberts expeditiously replaced his dual cone: see below), and his last pre-publication public statement about Dr Al Muderis being “a very grateful social media post”. It was submitted that attitude changed because of dealings with Mr Hernandez, suggesting Mr Bruha rewrote history to help him. I do not accept that submission about him, or similar submissions made about other American patients.
1066 The applicant submitted Mr Bruha (and other patients) had full contact with Dr Al Muderis until his dispute with Mr Hernandez. He explained the absence of messages to Dr Al Muderis after the initial period above was “probably because” Mr Bruha did not need him, as there were doctors in the United States who could assist.
1067 Given how Mr Bruha described Dr Al Muderis’ responses when he raised concerns about infection, it is hardly surprising that he did not request his assistance. It does not follow that the issues did not occur, bearing in mind his implants were removed (which is well before the Publications). It also does not follow he was “wholly happy”. His need to go to the medical clinic because of the condition of the open wound shortly after his return to the United States (which is supported by contemporaneous evidence) suggests otherwise.
1068 There was a later occasion when Mr Bruha contacted Dr Al Muderis for assistance. This occurred when he snapped his dual cone on his left leg in around July 2019, needing a replacement. He agreed that Ms Roberts and Dr Al Muderis organised to have the parts sent to him but said that Dr Rosenblatt helped him after that. He agreed he received his dual cones within a few days. An email from him to Ms Roberts establishes he was grateful for the speed with which his issue was taken care of. Given that they are Dr Al Muderis’ implants, that he contacted them and there was a quick response should be expected. By this time, Dr Rosenblatt and Mr Hernandez were no longer working with Dr Al Muderis, and Ms Roberts told him (and others) that his first port of call was to Dr Al Muderis and herself. I note Mr Bruha was initially charged for the replacement dual cone, which was later waived.
1069 The text and Facebook messages between Mr Hernandez and Mr Bruha provide no support for the submission that Mr Bruha has concocted his evidence to support him. To the contrary, the exchanges reflect an interest in speaking the truth about their experiences. It is also readily apparent that they are aware they may be excluded or removed from osseointegration support groups, and that they will be criticised for sharing their experiences with the media. That there may be offensive language used by the participants in those messages at times does not alter that.
1070 As explained above, I am satisfied that Mr Bruha was not advised by Dr Al Muderis of the risks and complications of surgery before arriving in Australia, and nor was he adequately advised of them while in Australia, in circumstances where his consultation was only the day before surgery. He was provided misleading information. That all impacts on Mr Bruha’s consent. Further, Mr Bruha left Australia on antibiotics (although Dr Al Muderis denied he had an infection). He was treated for those symptoms at a medical clinic shortly after arriving in the United States (and on later occasions). He sought the advice of other doctors. On medical advice, he had chronic osteomyelitis and infections such that his implants were ultimately removed. I am also satisfied in the circumstances that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Ms Lisa Schaeffer
1071 Ms Schaeffer is a right below-knee amputee who lives in the state of Georgia in the United States. She first learnt about osseointegration in detail at the Amputee Coalition National Conference in Arizona in mid-July 2015, where she spoke with Mr Hernandez. She subsequently emailed Dr Al Muderis’ rooms expressing her interest and completed an online form. Dr Al Muderis personally responded to the email. She underwent osseointegration surgery on 7 October 2015.
1072 Ms Schaeffer was a forthright and impressive witness who provided considered answers. The applicant submitted that Ms Schaeffer told the truth during most of her evidence except for isolated occasions when she concocted evidence because “it is clear that her post-event malice has caused her to veer away from the truth”. I do not accept the evidence relied on by the applicant supports that assertion. I return to discuss this below.
1073 Given the issues in relation to Ms Schaeffer, it is necessary to address the following topics.
1074 First, the steps involved in coming to Australia to undergo her osseointegration procedure on 7 October 2015. The events themselves are not in issue. Ms Schaeffer was required to pay and did pay for her surgery (US$78,067) before she arrived in Australia, and before she had a consultation with Dr Al Muderis. This was before the risks and complications of the surgery were explained. On the applicant’s case, the risks and complications were explained during the consultation with Dr Al Muderis, which occurred on the day before her surgery.
1075 In summary, the online inquiry was submitted by Ms Schaeffer on 25 July 2015, to which Dr Al Muderis responded in a positive manner, informing her a member of his staff would contact her. By 31 July 2015, a proposal for treatment had been sent to Ms Schaeffer. On 5 August 2015, Ms Stewart emailed Ms Schaeffer telling her that she had shown Dr Al Muderis the photos received, to which he said that “surgery would be an option for [her]”. An estimate of between US$50,000 and US$70,000 was provided. The email also requested x-rays and pre-operative medical questionnaires to complete the eligibility process. Ms Schaeffer responded on 6 August 2015, informing Ms Stewart she had an appointment to obtain x-rays on 11 August 2015. On 7 August 2015, a quote for US$78,067 was generated. Ms Schaeffer said that after she sent the documents requested to Dr Al Muderis’ rooms, Ms Stewart called her to say they could proceed with the surgery and said words to the effect of: “Everything looks good, we can go ahead and schedule surgery”. As mentioned above, payment was required before arriving in Australia. Ms Schaeffer completed a pre-admission form for Macquarie University Hospital on 14 August 2015. On 28 August 2015, a letter was sent to Ms Schaeffer confirming her surgery was booked for 7 October 2015. I note Ms Schaeffer’s blog of 21 August 2015 records she had been approved for surgery and had been provided possible dates. She recorded she chose 7 October 2015. Following this, Ms Schaeffer attended a pre-operative consultation locally in Kentucky on 31 August 2015 to obtain surgical clearance from a cardiovascular standpoint. On 8 September 2015 (i.e. after she had been approved for surgery, a date had been booked and she had been invoiced), Dr Basten sent an email to Dr Al Muderis confirming he had completed a psychological assessment of Ms Schaeffer on Skype and noted that she had many positive prognostic factors. Ms Schaeffer did not have any appointments with Dr Al Muderis or any communication with him before travelling to Australia, other than an email exchange about infection as suggested by her orthopaedist (which is not before the Court, with there being no detail as to its contents).
1076 By 11 September 2015, Ms Schaeffer had paid the US$78,067 in full, as required. Ms Schaeffer explained that to do this, she and her husband had to move around some of their investments, take out a loan and borrow money from their son to make the operation possible.
1077 I have addressed the impact of requiring prepayment elsewhere. Explaining the risks and complications of the surgery after payment, and on the day before surgery, impacts on whether any consent is informed in the required sense.
1078 Second, five days before her scheduled surgery, Ms Schaeffer attended a dinner in Sydney on 2 October 2015 (which she posted about the following day) with other amputees and Dr Al Muderis, which he had organised. This social function occurred before Ms Schaeffer had a consultation with Dr Al Muderis. The issues that arise from such events are discussed elsewhere: see e.g. The patients in Part 6, Section 1.
1079 Third, the pre-operative consultation with Dr Al Muderis on 6 October 2015. There is a dispute as to what is said to have occurred at this consultation, with Ms Schaeffer describing it as only a brief interaction of “about 10 minutes – 15 minutes tops”. There was no group consultation as described as Dr Al Muderis’ standard practice. Rather, only Ms Stewart, Ms Bosley, and a Fellow were recorded as persons present at the pre-operative consultation.
1080 Ms Schaeffer’s evidence was that Dr Al Muderis called her fat during the initial consultation and said that she would eventually need a knee replacement because of her weight, which Dr Al Muderis denied. Ms Schaeffer was adamant in cross-examination that the comment about her weight was made, because she said she recalled being offended and insulted by it in front of her husband. Ms Schaeffer also gave evidence that during the consultation, Dr Al Muderis said words to the effect of: “I will always be there as we’re going to be family now”. This is a common theme from the evidence (see e.g. Ms Ulrich’s case study as to his statement that they would have a connection for life) and is a statement of the nature Dr Al Muderis accepted he makes.
1081 Ms Schaeffer was cross-examined about some blog entries she posted, including on the day of this consultation. The applicant submitted that the blog recounted her appointments (including with Dr Al Muderis) and said that the people in the Australian healthcare system were “polite, thorough and professional”. He submitted that Ms Schaeffer’s evidence about a comment on her weight should be rejected because her description sits uncomfortably with the allegation she made for the first time in these proceedings – that Dr Al Muderis insulted her weight at the consultation. I note that Ms Schaeffer’s comment in her blog post was not particular to Dr Al Muderis’ consultation, rather, it appears at the end of the process for that day where Ms Schaeffer met others (e.g. after having her blood drawn). Further, given the personal nature of the comment, it is unlikely that Ms Schaeffer would have referred to any comment made about her weight. I note that it is also apparent from her blog that Ms Schaeffer was late to the appointment as there was a mix up as to the location of the consultation. Ms Schaeffer recorded that on arriving, she and her husband had to wait, and she had several other appointments booked later for other processes. In that context, that the consultation was brief, as she described, is plausible.
1082 Various propositions were put to Ms Schaeffer in cross-examination based on the content of the consultation report. That the report was said to be the source of the question was the clear impression created by the questions asked. It was apparent from her responses, that although she did not have any recollection of various statements, she generally approached the questions on the basis that if the proposition or statement was in the report, it must have occurred, and therefore she agreed. In other words, Ms Schaeffer presupposed the accuracy of the report. For example, although Ms Schaeffer could not recall the discussion of risks beyond infection, after a series of questions addressing whether she was told about a particular risk, she said, “they’re all right there, yes”, meaning that they appeared to be in the consultation report. It is also apparent that Ms Schaeffer assumed that the general risks of surgery would have been discussed.
1083 The risk she remembers and deposes to Dr Al Muderis referring to is infection and him telling her it is:
not a matter of if, it’s a matter of when, you will get an infection. It’s not as if everything is flesh eating. As long as you catch it, you can take antibiotics and you will be fine.
In cross-examination, Ms Schaeffer used those same terms in her recollection of this discussion. That description is not an accurate or complete one but rather downplays the risk. That the risk is “not if, but when”, is not recorded in the consultation report. The report recorded that Ms Schaeffer is a “relatively low risk” patient (a pro forma term frequently used in the consultation reports in evidence). The significance of such a risk being omitted in the consultation report is discussed elsewhere. Ms Schaeffer also did not recall doing a six-minute walking test or timed up and go test. In any event, doing such a test when Ms Schaeffer was not wearing her prosthesis but was using a walking aid (a crutch) seems unlikely, as it would not be a realistic assessment of her position. The artificiality of the report is apparent from such statements as “I am more than happy to organize surgery for her as soon as she wishes”, in circumstances where Ms Schaeffer was already booked for surgery the next day and had been informed of such since 28 August 2015.
1084 Although Ms Schaeffer was advised of some risks and complications, the severity of the risks and complications were downplayed, as the evidence in relation to the risk of infection reflects. In any event, even if the severity of risks and complications were discussed as Dr Al Muderis described in the report, the circumstances he created, including the prepayment, the travel from overseas, and the booking of surgery having already been made for the next day, undermine the consent given.
1085 I accept Ms Schaeffer’s evidence that the consultation on 6 October 2015 was brief. This accords with the evidence provided by other patients. For the overseas patients, everything was already in place, with the surgery booked prior to their arrival in Australia. It can be inferred, in practical terms, that the consultation was a formality given the late stage it occurred. The patient having already made the decision to proceed with the surgery. That is not to suggest that something might not arise in the tests that altered the plans, but subject to that, the surgery was expected to proceed.
1086 The length of the consultation cannot be judged by the consultation report. I accept the respondents’ submission that there was no way that all the matters listed could be discussed in such a short timeframe. That said, if the matters listed were all spoken of, given the number, they could not have been properly discussed by Dr Al Muderis to constitute adequate consent in circumstances where the consultation likely lasted 15 minutes at most. That is a matter of common sense. In any event, this is also the opinion expressed by Dr Stalley.
1087 Fourth, Ms Schaeffer underwent her surgery on 7 October 2015, and it is unnecessary to detail that or the events that occurred while she was still in Australia. She accepted that at that time, she considered Dr Al Muderis to be her hero and she felt fortunate to have had osseointegration.
1088 Fifth, after returning to the United States, Ms Schaeffer attended the Amputee Coalition National Conference, the same conference where Ms Schaeffer had initially learnt about osseointegration and Dr Al Muderis’ work. In June 2016, this was held in North Carolina. She explained that she, and other patients of Dr Al Muderis were asked to wear t-shirts which identified them as part of the osseointegration Australia team, to promote him and his company. They were to be part of the booth promoting the surgery, wherein people could look at their legs (as they were wearing shorts). Mr Hernandez had been asked to organise this for the group. When it was suggested to her in cross-examination that she had been happy to support Dr Al Muderis at the conference, Ms Schaeffer clarified that she attended because she paid to attend the conference just like any other amputee, paid for her hotel, and she is a member of the Amputee Coalition. During that conference, Ms Schaeffer attended a party celebrating Dr Al Muderis, his staff and all his patients that attended the conference. During the hearing, a video was shown of the party. The extent of socialising with former patients impacts their relationship with Dr Al Muderis, particularly in a context where there is a level of dependency on him.
1089 Ms Schaeffer also attended conferences in 2017 and 2018 in Louisville and New Orleans, respectively, to meet with Dr Al Muderis.
1090 In July 2017, the inner screw in Ms Schaeffer’s prosthesis cracked and then broke in half. She reached out to Dr Al Muderis, who said he could fix it when he was in the United States for a conference in Kentucky. In August 2017, she attended a hotel room which she described as appearing to have been set up as a room for treating patients during the convention. She gave evidence that she spent time in what she described as the waiting room before going into the main room, where Dr Al Muderis replaced the inner screw on her implant while she sat on the bed. Mr Lui (who was helping with parts) and Ms Roberts were present. Ms Schaeffer described being sent an invoice for the new screw, but after she sent paperwork indicating the implant was under warranty, Dr Al Muderis’ office did not chase the payment further.
1091 In February 2018, there was a second occasion when an issue arose with her prosthesis. In a similar fashion and again at a conference, this time in a hotel room in New Orleans, Dr Al Muderis looked at her leg and performed an adjustment on her prosthesis.
1092 Sixth, Ms Schaeffer accepted that after she returned to the United States, she messaged Dr Al Muderis at various times seeking help, and she described him responding (although she qualified that as “eventually”), to which I return below. However, the messages became very infrequent over time. After 2019, there appears to be no messages until the last communication in early June 2022. That said, I note that in May 2021, Ms Schaeffer did repost an earlier photograph of her and Dr Al Muderis. Ms Schaeffer accepted in cross-examination that she posted positive messages about Dr Al Muderis.
1093 The applicant submitted that until June 2022, Ms Schaeffer was “happily in contact” with Dr Al Muderis and a “beamingly happy patient”. It was submitted that she had “never ever said a negative word” against him until her dealings with Ms Grieve. As referred to above, the applicant submitted that she concocted allegations to help Mr Hernandez, and that Ms Schaeffer told the truth during most of her evidence except for isolated occasions where she concocted allegations about Dr Al Muderis’ conduct.
1094 The applicant submitted that “[t]he foundation for evaluating Ms Schaeffer’s credit is that her osseointegration has been wholly successful”. This starkly reflects a flaw in the applicant’s approach; simply because surgery is successful, or that a person is happy with the outcome, does not mean they cannot have any complaints or issues with Dr Al Muderis or the process.
1095 As the respondents submitted, Ms Schaeffer had raised some issues with Dr Al Muderis over the years.
1096 Ms Schaeffer gave evidence that after her return to the United States, she felt as if Dr Al Muderis “ghosted” her. She said she would message and sometimes phone him and that although Dr Al Muderis would eventually respond to her, it would take hours or a couple of days.
1097 Ms Schaeffer also gave evidence that she raised some concerns about her prosthesis and stoma with Dr Al Muderis in January, February and May of 2016. Her evidence was that she felt he was not taking her concerns seriously and not really engaging with the issues she was having. This is reflected in some of her Facebook messages in evidence.
1098 On 13 August 2018, Ms Schaeffer reported to Dr Al Muderis and others in his team about a rusting problem in her taper sleeve which could not easily be removed, and which resulted in the cancellation of an MRI she was scheduled to have. She described her recent issue as giving her “some, what could have been really bad, complications”. The email noted that she had not been informed about a protocol requiring the parts be removed and cleaned and referred to speaking to other former patients about this issue. That email included the following:
The last thing we were told was we are family now. But honestly, I kinda feel like the red headed stepchild when it comes to getting help in general.
I understand it is a unique position to be on the front end of technology and it is ever evolving, but not being updated as far as protocols, maintenance, and recall of parts is not very good follow through or after care for your patients (Our OI family).
I get updates from my Vet for my pets and from my auto dealership regularly for any necessary appts. There should be the same type of registry and follow up with your patients. Especially in the event of emergencies.
My OI has gone relatively smoothly with very little issue and I have sung it’s praises to anyone who would listen, many of which have themselves gone on to get the procedure because it is so awesome.
I just feel there are still unaddressed issues when it comes to keeping track of who we are, what we have had done and the inventory of the parts we have in our bodies because clearly issues such as what I recently encountered will come up and quite frankly it’s a scary thing to feel so vulnerable.
1099 I note that although Ms Schaeffer is singing its praises, such praises are directed to the surgery, not the surgeon. Again, this is plainly a complaint. It expresses Ms Schaeffer’s genuinely held concerns. The terms of the email reflect that her concerns were not confined to the issue she raised but had broader import. The statements were made well before the Publications, and certainly well before speaking with Ms Grieve. That email alone demonstrates the applicant’s submission is incorrect.
1100 On 9 August 2019, Dr Al Muderis sent a Facebook message to Ms Schaeffer requesting she post a positive message about him on Facebook:
Dr Al Muderis: Can you please mention on Facebook that I got back to you. Some people are trying to make me look bad and they posted on Facebook that I am not communicating with my patients which is not true. It is not [sic] disheartening to see some people using innocent components like your [sic] to damage my relationship with the osseointegration family.
I would really appreciate it Lisa.
Ms Schaeffer: No problem:)
Dr Al Muderis: Thanks
Ms Schaeffer: Done
Dr Al Muderis: Thank you
1101 It is apparent from the face of the message exchange that Dr Al Muderis was aware at that time, that some patients had posted comments on Facebook regarding his failure to communicate with them. Taking issue with this, his response was to request Ms Schaeffer to counter these posts with a positive post of her own. Although Ms Schaeffer posted something (however I note that she clarified this was a comment on someone else’s post, rather than her own post), the circumstances in which it occurred were solicited, undermining its authenticity as a genuinely held opinion. This is clear in Ms Schaeffer’s affidavit: “I wrote the brief comment because I did not want to cause any issues with Dr Al Muderis”. The request also reflects the importance to Dr Al Muderis of positive comments being made in relation to him. By then, complaints about not responding had been communicated to him (e.g. by Ms Çalan, Ms Todd and Mr Hernandez, etc).
1102 There appears to have been no further communication between Dr Al Muderis and Ms Schaeffer for some considerable time.
1103 Ms Schaeffer gave evidence that how she was treated changed over time. When it was put to her that she continued to obtain his assistance years after her surgery, she responded “[b]ecause we were family”, being a reference to Dr Al Muderis’ description of the relationship he said they would have, mentioned several times above. For example, on 6 September 2019, Ms Schaeffer messaged Dr Al Muderis asking on behalf of her surgeon (she was having an arthroscopy on her left hip) about the implant, and if she needed to take pre-emptive antibiotics. She then sent him some follow-up messages informing him her surgeon had attempted to contact him and asking him to respond. Similarly, Ms Schaeffer described contacting Dr Al Muderis either in relation to an MRI or colonoscopy she had (she could not recall which) “because nobody in the US knew anything about osseointegration or what my implant entailed. So I had to ask the source of it if I could get those procedures done”. As noted above, that sentiment is unsurprising and demonstrates an obvious level of dependency arising from the fact that Dr Al Muderis conducted this surgery (which he described as in its infancy), and the implant was proprietorial. Ms Schaeffer said, she asked him as he was “the authority” on the topic.
Assessment
1104 Returning to the assessment of Ms Schaeffer as a witness. The messages between Ms Schaeffer and Mr Hernandez which the applicant relied on to support his concoction allegation in relation to Ms Schaeffer, properly read, do not do so. Again, some of the messages may appear unpleasant. As Ms Schaeffer described, this was private messaging between friends. Properly read, there is no suggestion in the messages that anything false was said by Ms Schaeffer in giving evidence. To the contrary, the messages proceed on the basis of the truth of the assertions that were coming out. Some comments disagreed with the accuracy of Dr Al Muderis’ evidence. It was put to Ms Schaeffer that she was a “malicious hater” of Dr Al Muderis, on the basis that her experience was wholly positive, it changed her life, and she was (and should be) forever grateful. However, as discussed elsewhere, that conflates several issues. It is also difficult to understand what is said to have occurred as a result of the alleged concoction. It was put to Ms Schaeffer that any complaint she had made in her affidavit or in evidence is a recent invention, which Ms Schaeffer denied. However, with limited exception, no issue is taken by the applicant with the content of Ms Schaeffer’s evidence. Although Dr Al Muderis claimed to have no memory of events, he, at times, said they may have happened: for example, that he may have helped her with her prosthetic component in the United States in August 2017. In part, the applicant’s criticism is that she is giving evidence of her experience when, being grateful for her osseointegration, she should not.
1105 As apparent from the discussion above I am satisfied there was no information given as to the risks and complications of the surgery before it was booked, and payment made. There had been no assessment of her by Dr Al Muderis as to her suitability. The consultation in Australia shortly before the surgery was brief, and any risks then referred to were downplayed. This impacts on whether her consent was informed. Ms Schaeffer had made complaints to Dr Al Muderis after returning to the United States (e.g. as plain from the email recited above). She was used by Dr Al Muderis to promote his surgery to others at a conference and to counter negative posts made about his aftercare online. She had consultations with him in the United States to fix issues with her implant. I am also satisfied in the circumstances that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Ms Michelle Koolhoven (née Ortiz)
1106 Ms Koolhoven is a patient from the Unites States. She has been a left above-knee amputee since 22 June 2013 and previously mobilised using a socket prosthesis. Ms Koolhoven found out about osseointegration through Mr Hernandez’s posts about Dr Al Muderis in an amputee Facebook group. After reaching out to Mr Hernandez, she subsequently completed an online enquiry form through Dr Al Muderis’ website on 18 August 2015, expressing her interest in osseointegration. Ms Stewart replied to Ms Koolhoven’s enquiry by email on 19 August 2015. On 5 November 2015, several events occurred: Ms Koolhoven submitted her responses to a health questionnaire; Ms Bosley sent Ms Koolhoven a quote for osseointegration surgery, totalling US$78,000 but discounted to US$58,000; and Ms Koolhoven was sent a proposal for treatment and care. Dr Al Muderis agreed in cross-examination that he provided the instructions as to the amount of the estimate. On 10 November 2015, Ms Stewart sent Ms Koolhoven a letter confirming she was booked for surgery on 13 January 2016, but subsequent correspondence indicated the surgery was rescheduled to 10 February 2016. On 27 November 2015, the invoice for US$58,000 was issued to Ms Koolhoven. On 7 December 2015, Dr Basten completed his psychological assessment of Ms Koolhoven. Her pre-admission form was completed on 20 December 2015. Ms Koolhoven paid the invoice on around 27 January 2016. She arrived in Australia on about 4 February 2016, met Dr Al Muderis for the first time on 8 February 2016, and underwent osseointegration surgery on 10 February 2016.
1107 Ms Koolhoven presented as a credible and reliable witness. The applicant accepted that she was a responsive and “wholly honest” witness whose evidence could generally be accepted, but there are some aspects which should not be accepted as she is mistaken (for example, the shortening of her leg), which are addressed below.
1108 There are several points to be addressed.
1109 First, at the time when the fee estimate was provided on the instructions of Dr Al Muderis, he only had the online questionnaire (which Ms Koolhoven completed on the same day). Dr Al Muderis agreed in cross-examination that as at the date of the fee estimate, he had neither met nor examined Ms Koolhoven. His evidence was unsatisfactory on this topic, suggesting he may have had a telephone call with her. As referred to in relation to Ms Ulrich, Dr Al Muderis had previously said that he would not provide a fee estimate without a clinical assessment and an online health questionnaire was insufficient for these purposes. His answers to this line of questioning strengthened from not recalling speaking to her, to suggesting he “may have” spoken to her, to he “would have” spoken to her, despite having no recollection and there being no evidence to support this occurring. There is no record of any conversation. If there had been a conversation sufficient to enable a clinical assessment so as to send a fee estimate (and ultimately an invoice), one would expect it to be recorded. I do not accept his evidence. Ms Koolhoven does not give evidence of any such conversation, and it was not suggested to her that there was one. Rather, her evidence was she did not speak to Dr Al Muderis before her arrival in Australia.
1110 Second, Ms Koolhoven paid the invoice, as she was required to, before travelling to Australia. At that time, Ms Koolhoven had not met Dr Al Muderis and he had not told her of the risks and complications of surgery. Nothing in the documentation sent to her before then covered such topics, and in any event, that would not have been sufficient or appropriate. Dr Al Muderis described in his affidavit that he provided Ms Koolhoven with “a detailed information sheet about post-operative care”. The document exhibit for that proposition does not contain such information. Rather, the document referred to is a generic document not tailored to Ms Koolhoven’s situation. The proposal document Ms Koolhoven was sent is referred to at [1106] above, and as Dr Al Muderis conceded, contained no information about the risks and complications of osseointegration surgery. There is also nothing in the proposal, or hospital admission information pack dated 10 November 2015 about who will be responsible for post-operative management for overseas patients like her. The impact of prepayment on informed consent is addressed elsewhere and there is no need to repeat that discussion: see e.g. Observations about the international patients, below.
1111 Third, there is a dispute in the evidence about whether Dr Al Muderis told Ms Koolhoven that he would need to shorten her leg to complete the osseointegration. Ms Koolhoven denied this, stating that Dr Al Muderis told her that the leg would be stronger and better in terms of mobility if they kept the length the same. This is in a context where Ms Koolhoven’s evidence is that she was concerned from the outset about the length of her leg, was already having problems with her socket because of it and as a result, raised the issue with Dr Al Muderis.
1112 The respondents submitted that at the very least, the issues with Ms Koolhoven’s leg length should have been carefully considered and documented prior to and at the time of surgery. There is no evidence of any measurement being taken or any planning done for how her amputated limb would interact with her new prosthesis in the lead up to the surgery, other than a cursory reference to it in the consultation report dated 8 February 2016 that to:
achieve equal knee height, her femoral stump will need to be shortened to allow a clearance of 150mm. This will allow sufficient clearance of the prosthetic limb in walking and will give her a more natural gait.
Ms Koolhoven disputed this was said at the consultation and gave evidence that she had never seen the letter. I note that the operation report makes no reference to the amputation length.
1113 The applicant submitted that as this relates to a medical issue, it is more likely that Dr Al Muderis and the consultation report are correct. Ms Koolhoven was adamant that Dr Al Muderis did not tell her that her leg needed to be shortened and posed the question in cross-examination of why it was not ultimately done, if Dr Al Muderis had discussed it with her. Regardless, following surgery, Ms Koolhoven remained of the view that the length of her leg was too long, because when she sat down with her prosthetic leg attached to her implant, the knee joint component extended way beyond the length of her right knee.
1114 I note that on repeated occasions after the surgery, Ms Koolhoven raised with others the length of her leg, and the problems it was causing. There is documentary evidence supporting her concerns. For example, there were a series of communications in July 2017, after Ms Koolhoven had an x-ray taken which she sent to Dr Rosenblatt, asking whether there was a problem. Ms Koolhoven’s evidence was that she requested a shorter dual cone because of problems with her knee heights. Upon receiving the x-ray, Dr Rosenblatt wrote to Mr Laux, a clinical prosthetist working with Dr Al Muderis, saying: “I thought she looked like her left knee joint is lower than the non amputee side”. Mr Laux responded in an email of 12 July 2017: “a normal and textbook position of a prosthetic knee joint axis is 15mm more proximal than the contralateral sound side”. I note this accords with Dr Stalley’s evidence that absolute equalisation of leg length is ill-advised because the prosthesis may catch on the ground and therefore, he aims for a 1 cm difference (with anything above 2 cm being ill-advised). Mr Laux explained in that email:
if we made them both the same height in full extension it would result in a shorter shank/longer femoral section of the prosthetic knee in full flexion, which is disadvantageous when sitting.
He said Ms Koolhoven’s dual cone should be shorter to improve structural stability, to allow a closer approximation of the anatomical knee joint height and also provide her with maximum strength of the component.
1115 It appears that before that email exchange between Dr Rosenblatt and Mr Laux, Ms Koolhoven received an email from Dr Rosenblatt on 11 July 2017 stating, “I reviewed your x-rays with [Dr Al Muderis] and [Mr Laux] and everyone agrees they look great! Perfect alignment and good length!” Despite this response, it is clear Ms Koolhoven’s concerns about her leg length were not alleviated as she asked about changing her dual cone and enquired about a “connector with extremely short build height”. Dr Rosenblatt replied he would not change the dual cone because of the difficulties in removing it, with which he said Dr Al Muderis agreed. I note that Ms Koolhoven continued to enquire about solutions for her leg length, as evidenced by a Facebook message to Dr Al Muderis on 15 June 2019:
Hi I am wondering if you make a connector that has low build height we are having do much problems as I don’t have enough room for prosthetics and my knee center is always too long it would help if we can get connector with minimal build height? Thank you
1116 And again in September 2019:
Hi Munjed … can we take up my leg anymore so we can put a shorter dual cone in to give me more room as it’s a problem cause I’m so long
…
I hear you have a new dual cone out too that is stronger I would like to see that I get that as well and hopefully the shorter one but I feel we may need to take my leg up some more refashioned.
1117 As is clear from the evidence, whatever was said during the consultation about the length of her leg, its length still caused ongoing issues for her, long after her surgery.
1118 Fourth, the applicant submitted that Ms Koolhoven was a “wholly happy patient” and “overwhelmingly positive” about him, until she was told that she was given a defective part, after which she became very agitated when she sought to find out what part she had been given. The applicant submitted that Ms Koolhoven was concerned that she had been given the Type B dual cone that Mr Hernandez had said was recalled.
1119 That submission is not supported by the evidence. Ms Koolhoven accepted that she posted positive messages on social media about Dr Al Muderis. She explained that she is “not one to be negative”. When asked why she had posted positive messages after she experienced the problems she described in evidence, she explained:
… the ones that I was posting that were positive in 2017, I hadn’t started infections yet and I was – I guess I was finally convinced that I was just going to have to deal with having this rotation problem and hope kind of for the best. And also at that time I had no other person that I could actually get help with osseointegration. So I mean, it’s a good idea to keep that person kind of close to you in a way.
1120 That accords with the evidence of other osseointegration patients, from the United States and Australia (e.g. Mr Wynne, Ms Ulrich and Ms Schaeffer).
1121 The problems Ms Koolhoven experienced after her surgery as she described in her evidence, including, amongst other things, the lack of prosthetists with any training enabling them to treat her, her fall and safety concerns of her implant, the infections, and the unequal leg lengths, are all referred to in documentation at the relevant contemporaneous times.
1122 To illustrate, after her return to the United States, Ms Koolhoven experienced difficulties with finding a prosthetist capable and willing to attend to her prosthetic needs. In November 2016, she contacted Mr Laux explaining this issue. It is evident from the evidence that Mr Laux well understood that there were insufficiently trained prosthetists in the United States capable of working with Dr Al Muderis’ osseointegration implants. To that end, he described that there had been discussions with the Osseointegration International team about the need to train or accredit prosthetists in the United States. Nothing eventuated. Mr Laux described that as at November 2016, he had been discussing this with Dr Al Muderis for a few years. The suggested training never eventuated. The response from Mr Birbas of Osseointegration International (Dr Al Muderis’ company) to Ms Koolhoven’s request for help in 2017 (being after she had her fall) was that it would take time to educate others. He also suggested to Ms Koolhoven that she could either see a prosthetist “familiar with OI in Orange County, Phoenix” or sign a legal waiver in respect to the work done by her local prosthetist.
1123 In relation to her fall, which occurred about seven months after returning to the United States, Ms Koolhoven’s evidence was that the internal screw inside her implant broke. She said that this affected the alignment of her dual cone, and her walking ability and she was concerned about the safety of her implant as a result. On 19 February 2017, she reached out to Dr Al Muderis’ office by email, asking for documentation explaining that the temporary solution proposed (by fixing the dual cone adapter, rather than replacing it, as was ultimately required) would be safe for her. Ms Stewart responded, referring to a discussion with her the previous week, that Ms Koolhoven needed to get the dual cone tightened by the internal screw, and that she should see a prosthetist to get it properly aligned. She was told to contact Mr Hernandez for his prosthetist’s details. I note that his prosthetist was in Arizona, and Ms Koolhoven lived in California, a three-hour drive away. The next day, 20 February 2017, Ms Koolhoven emailed again requesting a response and explanation from Dr Al Muderis as to whether the proposed solution would keep her safe and whether she would have the same safety as before. Having received no response, about five weeks later, on 24 March 2017, Ms Koolhoven chased up the office for a response. She was told by Ms Stewart that as her concerns pertained to a safety issue for the designer of the implant and surgeon responsible for her care, it was suggested that she contact Dr Al Muderis directly, which she did. In his response on 26 March 2017, Dr Al Muderis said there were two safety mechanisms, which minimised but did not eliminate risks of fracture. There was approximately a five-week delay before Ms Koolhoven’s questions as to the safety of her implant were responded to. In so far as Dr Al Muderis appeared to suggest in cross-examination that there were “extensive” communications happening at that time with her, that is inconsistent with the terms of the emails and Ms Koolhoven’s follow-up requests. Contrary to what Dr Al Muderis said, it is not supported by any other evidence (such as texts or Facebook messages), rather his answer was provided as an explanation only when he was questioned about the delay in responding to Ms Koolhoven’s concerns. Had Ms Koolhoven been satisfied with the responses that she received (if any), she would not have needed to resort, as she did, to sending follow-up emails.
1124 After Ms Koolhoven’s fall, the temporary measure suggested by Dr Al Muderis of tightening the screw, left her without the full safety mechanisms in the implant and constantly scared of falling.
1125 I note that between about March and June 2018, it appears that Ms Koolhoven saw Dr Rosenblatt several times, which included him replacing her dual cone for the newer Type B dual cone in March 2018. Ms Koolhoven had issues with the result, including increased drainage from the stoma. On 18 June 2018, Ms Koolhoven underwent a further exchange procedure putting in a new Bres Medical dual cone. A consultation report dated 19 June 2018, dictated by Dr Rosenblatt on behalf of Dr Al Muderis contains this information. It appears from the consultation report that the Type B dual cone used in March 2018 did not have an anti-bacterial coating and was thought by Dr Rosenblatt to account for the increased drainage Ms Koolhoven experienced.
1126 Thereafter, Ms Koolhoven’s evidence was that she had constant infections, oozing and pain. Given the circumstances, Ms Koolhoven naturally sought Dr Al Muderis’ assistance. Dr Al Muderis said that they exchanged regular messages during this period. While there are text messages between Ms Koolhoven and Dr Al Muderis in the three months from August 2018, the respondents described the messages as reflecting the fact that Ms Koolhoven was in a “terrible” situation and was begging for assistance. That is an apt description of those exchanges. Although Dr Al Muderis responded, at least generally, it could well be said that little was given by way of answers. To illustrate just a few of the message exchanges:
24 August 2018
Ms Koolhoven: Hi Munjed I just started Bactrim today but I just wanted to tell u something is not right my leg has never done this or hurt.. maybe this dual cone is causing it but something isn’t right thanks
Dr Al Muderis: Let me know how it feel in two days
28 August 2018
Ms Koolhoven: Munjed things don’t seem To be getting any better please let me know what to do
30 August 2018
Ms Koolhoven: Munjed checking in wanting to know the game plan please
31 August 2018
Ms Koolhoven: Ok can you please get in touch with me hoping we have a plan
…
7 September 2018
Ms Koolhoven: Munjed can you call me please
Munjed I have these MRI Contrast results and stuff did I do something wrong I’m scared and feeling really alone
Munjed are you free to talk
I’m in extreme pain I’ve taken all antibiotics I’ve been so patient.. I am being persistent because I’m telling you something is wrong.. from what it sounds like I’m going to a consultation? I will be traveling alone but this is getting progressively worse.. please get in touch with me. … I mean I’m not a science project .. Munjed I don’t believe I’m over reacting please I don’t know what I would do if I loose my implant I just don’t think I could take it
It’s hard to keep it together I will try and do my best but maybe I’m a little confused about what exactly Robert [Rozbruch] In (NY) knows about my situation (Is he apart of Osseo group looking after me for you) I just need to know that if I whisk off to New York he will take care of me “As if I were in Sydney”. … I will have to book the flight cause I just can’t put this off.. As far as I knew and was assured you have approved everything all along. I’m sorry I’m so upset but this is not my fault and it’s very scary and upsetting because this is already affecting my house with just my Son and I. So if you can kindly try to rest assure me that I will be taken care in NY I probably would feel a hell of a lot better with a small sense of relief and security
What exact type X-Ray angle or view should they be
Dr Al Muderis: Just a femur x Ray AP and Lateral
…
8 September 2018
Ms Koolhoven: So do you think we should replace the dual cone immediately with one that’s not been tampered
Dr Al Muderis: Yes once we find out what is going on.
Ms Koolhoven: Ok so what do you need me to do to find out. I am being persistent as I felt something was wrong so I spent the whole day at the hospital to get answers
…
Ok I still need the know what we are going to do? I have this other connector too but no prosthetist has ever been able to fit me with it cause there is no room .. it’s not that I don’t want to use it .. do u need it back ? I just feel we’re not on the same page I need to know you have my back are we together
Dr Al Muderis: Can your u send me a photo of it
Ms Koolhoven: Yes it’s currently in the closet I’ve never got to use .. tired of things not going my way,. .. that’s your only response to what I said
…
3 October 2018
Ms Koolhoven: I wished this little conversation would of been a little more reassuring kinda rubbed me the wrong way
1127 This appears to suggest that Ms Koolhoven on many occasions communicated her fears and chased Dr Al Muderis for an answer and information to alleviate her concerns. As to those exchanges, in cross-examination Ms Koolhoven described:
Well, I mean, he was kind of responding to me. But the fact that I knew that I was having an infection and I knew I was getting, you know, sicker by the moment and it was – I was just getting pushed back and nobody had an answer. And so … I had to kind of advocate for myself … to let him know there’s something wrong with me and I am sick and I need some help. And I just – you know, when some – you have an infection going, who knows what can happen? And so [I] felt I wasn’t getting addressed in time.
1128 As the applicant put to Ms Koolhoven, Dr Al Muderis did organise for her to see Dr Rozbruch to address the issue with her dual cone, but as she said, it was at her own “costly expense”. Dr Rozbruch operated in New York. Further, it took three months from when she first contacted Dr Al Muderis about the infections arising from her dual cone in August 2018 for Ms Koolhoven to have an appointment to see Dr Rozbruch in October 2018. I note that Ms Koolhoven was sent back to California following this appointment. It was only after this initial consultation with Dr Rozbruch that a plan was put in place for Ms Koolhoven to have surgery and debride her leg, which occurred after Ms Koolhoven travelled to New York on a second occasion in late October 2018. This delay was despite Ms Koolhoven telling Dr Al Muderis that because of the pain she was experiencing, she couldn’t wait that long for a solution. When questioned on this in cross-examination, Dr Al Muderis’ evidence was:
That plea was her feeling about her condition. I consulted with her. I consulted with Dr Rozbruch, and there was no clinical need – Dr Rozbruch obviously didn’t feel that there was a clinical need for him to see her earlier than that. I could not make any other changes. I don’t have control on Dr Rozbruch’s appointments, and if she was in a serious emergency situation, there is a close hospital that she can go to and she would be attended to.
1129 Indeed, in the intervening period, Ms Koolhoven saw her local GP and made two trips to the emergency room. However, she explained the difficulties with doctors not being familiar with the surgery, or the implant, which resulted in her being sent home. Dr Al Muderis’ evidence above attempts to downplay his involvement in Ms Koolhoven’s situation. For example, Dr Al Muderis asserted in his affidavit that he is “not able to provide post-operative care to a patient in the United States”. As the respondents submitted, that is disingenuous. I agree. He accepted he was responsible for Ms Koolhoven as her surgeon. That responsibility did not end when she returned to the United States. It also directly contradicts assurances he gave to other patients from the United States, such as that given to Ms Ulrich that, “if you have surgery with me, we will have a connection for life” and “you’ll need me if anything goes wrong” (and see e.g. Ms Schaeffer’s evidence above that he said “I will always be there as we’re going to be family now”).
1130 The messages exchanged during this time also reflect that Dr Al Muderis told Ms Koolhoven that he disagreed with Dr Rosenblatt’s approach to handling her issues. Further, Ms Koolhoven was having difficulties obtaining her medical records from Dr Rosenblatt and raised this with Dr Al Muderis, to which she received no response. On 20 September 2018, Ms Koolhoven asked Dr Al Muderis why he could not attend to her when he was in the United States, to which he replied that Dr Rosenblatt would “report [him] to the medical board if [he sees] any patient”, and that “he is threatening us”. I note that Dr Al Muderis did not explain he is not licensed to practice medicine in the United States. It will be recalled that Dr Rosenblatt treated her, according to the consultation letter, on behalf of Dr Al Muderis, but by this time, there had been a falling out between Dr Rosenblatt and Dr Al Muderis. Ms Koolhoven, as a patient, was caught in the middle of this, a matter Dr Al Muderis refused to accept.
1131 In 2019, there was intermittent contact between Ms Koolhoven and Dr Al Muderis, primarily about problems with the components of her implants. The text messages again reflect that it was Ms Koolhoven who (to use an earlier term she referred to) was advocating for herself and chasing up inquiries made with Dr Al Muderis, as she was looking for a solution. This is the problem she described she had since her fall in 2016. After persistent enquiries by Ms Koolhoven, Dr Al Muderis eventually said he had a “great plan” to fix it with Dr Rozbruch, but the surgery was cancelled, with her being informed that it was Dr Al Muderis who had done so. Ms Koolhoven did not accept Dr Al Muderis’ denials of doing so, given, as she described, it was his plan. Ms Koolhoven gave evidence that the alignment problem still existed at the time of her giving evidence. She said it was a design problem, and that “you would think the designer of the implant would want to fix the problem”. Ms Koolhoven also gave evidence that she still has problems with infections and her leg is always oozing.
1132 In 2019/2020, Ms Koolhoven consulted Dr Stoneback, who advised her that given her unequal leg lengths, history of infection and redundant soft tissue envelope, she should have the implant removed, with treatment for infection followed by a higher revision to address the uneven leg lengths. This did not occur at that time due to insurance issues.
1133 Both Dr Stoneback and Ms Koolhoven’s evidence is that repeated requests by them for information about what the dual cone (which was used in her leg) is made of, have not been answered.
1134 As apparent from the reasons above I am satisfied that there was an inadequate disclosure of the risks and complications (given the circumstances), which impacts on Ms Koolhoven’s informed consent, and there was inadequate aftercare. Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Mr Jeff Ladouceur
1135 Mr Ladouceur was involved in a hit and run in 2012 following a motorcycle accident, which caused him to suffer multiple injuries, including a broken hip and crushed femur. He underwent an amputation of his right leg below the knee in 2012. In around 2014, after several unsuccessful surgeries he was advised to get an amputation above the knee, which he did.
1136 Mr Ladouceur gave evidence that in around 2017, due to issues he was having with his socket prosthetic and skin grafts, his prosthetist recommended Mr Ladouceur attend a conference in Las Vegas to get more information about osseointegration, which he did. Mr Hernandez was one of the speakers at the conference. In cross-examination, Mr Ladouceur accepted that Dr Al Muderis was also at the conference. Mr Ladouceur said he spoke to Mr Hernandez and got the impression that he worked with Dr Al Muderis. Mr Ladouceur was adamant that Mr Hernandez told him about a conference in New York which he and Dr Al Muderis would be attending, where the latter could assess Mr Ladouceur’s candidacy for osseointegration. I note from the outset that Mr Ladouceur did not ultimately proceed to have osseointegration surgery with Dr Al Muderis (but rather with another surgeon).
1137 The circumstances in which Mr Ladouceur travelled to New York to see Dr Al Muderis should be uncontroversial. He received an email from Ms Roberts dated 9 May 2018, advertising a clinic to occur on 9 June 2018. In a further email from Ms Roberts dated 6 June 2018, Mr Ladouceur was requested to bring recent x-rays with him to the clinic, which Mr Ladouceur understood were required for Dr Al Muderis to assess his suitability for osseointegration. Ms Roberts accepted in cross-examination that she was coordinating a clinic in the United States and the purpose of the clinic was to meet and examine patients. She also accepted that Dr Al Muderis asked her to make sure the patients who came to the clinic had recent x-rays with them.
1138 Mr Ladouceur said his consultation occurred on a couch in a corner of the public conference room and lasted around 15 minutes. He recalled Ms Roberts had a laptop and pulled up images of his hip and leg. Ms Roberts accepted in cross-examination that although she did not recall the interaction with Mr Ladouceur, this was a practice she would have done at the clinic. Dr Al Muderis also accepted in cross-examination that when he saw patients at the hotel, he would look at their legs and their x-rays. Mr Ladouceur said Dr Al Muderis told him he had seen the images, meaning the x-rays. This is consistent with Ms Roberts’ evidence in cross-examination where she said Dr Al Muderis would typically say something along the lines of, “I can see your x-rays”. Mr Ladouceur said Dr Al Muderis asked him to remove his prosthesis so he could see the stump, then proceeded to look at the stump, and felt around it briefly. Mr Ladouceur gave evidence that soon into the consultation, Dr Al Muderis said that he could help him and told him he was a candidate for osseointegration. He said Dr Al Muderis expressed no reservations about the surgery and did not discuss any of Mr Ladouceur’s medical issues, including the titanium mesh in Mr Ladouceur’s hip. Mr Ladouceur also said that during the consultation, there was no mention of any risks, physical therapy follow-up or the care required to look after the stoma. Mr Ladouceur said he raised the issue of cost because of his financial concerns, following which, Dr Al Muderis quoted him a discounted price of US$50,000 (from US$80,000). Mr Ladouceur recalled being taken aback by the amount, but considered it kind of him to make the offer.
1139 I accept there are some unsatisfactory aspects of Mr Ladouceur’s evidence, of which I have taken into consideration and addressed below. But his evidence as to what occurred at the consultation and the circumstances in which he attended it, is supported by other evidence.
1140 I accept that prior to attending the New York clinic in June 2018, Mr Ladouceur had sent earlier communications to Dr Rosenblatt on 13 December 2017 in which he provided his email address, and also to Ms Roberts on 9 February 2018, stating that he was unable to “afford this surgery”. However, I do not accept the applicant’s submission that Mr Ladouceur would not have attended the clinic and was not examined as he says, because Mr Ladouceur had already been assessed by Dr Rosenblatt as suitable, and Dr Rozbruch could have performed the surgery as a local alternative.
1141 Dr Rosenblatt had not assessed Mr Ladouceur as suitable for surgery. Rather, the emails and consultation report in evidence reflect that although he had seen Mr Ladouceur’s x-rays, Mr Ladouceur wanted to consider his options after talking to Dr Al Muderis. Notwithstanding the fact that an email was sent thereafter to Mr Ladouceur by Ms Roberts on 8 February 2018 stating that Dr Al Muderis had looked at his scans and wanted to discuss them with him, there is no evidence that this occurred. Rather, the invitation to attend the clinic in New York months later was issued with a subsequent request to Mr Ladouceur to bring his recent x-rays. Within that time, there is no evidence any in-person consultation had occurred, nor is there any evidence Mr Ladouceur had spoken to Dr Al Muderis, let alone met him. Mr Ladouceur travelled, it appears from Las Vegas, to attend the clinic where Dr Al Muderis was “to meet and examine” him in person, according to the invitation from Ms Roberts. Similarly, I do not accept the submission that it is unlikely that Dr Al Muderis looked at his x-rays while talking to Mr Ladouceur at the clinic as prior emails reflect they had been reviewed at an earlier point in time. Even if Dr Al Muderis had previously reviewed Mr Ladouceur’s x-rays, it does not follow that he did not review them again at the clinic, particularly because this was the first occasion that Dr Al Muderis had met Mr Ladouceur in person (noting the invitation also asked patients to bring their recent x-rays). Given that Mr Ladouceur was being assessed, it is probable (and would be expected) that Dr Al Muderis reviewed the x-rays in his presence. Mr Ladouceur’s evidence as to the circumstances in which he travelled to New York for the clinic is supported by the documentary evidence.
1142 It was put to Mr Ladouceur in cross-examination that he went to New York, not to be assessed, but to discuss where he should have the procedure and who should perform it. He denied this, stating that he went to be assessed and explained that this was the reason he brought his x-rays and was examined in the conference room. No details of a purported discussion regarding the procedure were suggested to him or provided by Dr Al Muderis. I find that Mr Ladouceur went there to be assessed and was assessed, which is supported by Ms Roberts’ evidence in cross-examination and the email which Dr Al Muderis had instructed Ms Roberts to send (informing patients of the clinic). Mr Ladouceur’s evidence as to the clinic and the nature of the examination is also supported by other American patients who received a similar invitation or otherwise saw Dr Al Muderis while he was in the United States. This is seen, for example, in the case of Mr Wynne, who was asked to remove his pants, obviously to enable Dr Al Muderis to look at his stump. It is also supported by the description of what occurred in relation to Mr Bruha, described in the letter to his insurer, referred to above.
1143 It is also entirely plausible that Mr Ladouceur raised the issue of costs at the time of meeting Dr Al Muderis, given his financial circumstances. It is a natural question. This is so, even though Mr Ladouceur had previously understood that the surgery would be US$80,000. It is unclear where this understanding came from. In any event, there had been no discussion with Dr Al Muderis about costs before New York. There is evidence of other patients in the same circumstances, discussing the cost of surgery during initial consultations with Dr Al Muderis (e.g. Ms Ulrich, Mr Bruha and Ms McIntyre). There is also evidence of Dr Al Muderis telling patients he would give them a discount, and a deposit was needed to secure their place in the operation schedule (e.g. Mr Smith).
1144 It is also entirely plausible that Dr Al Muderis and Ms Roberts gave the impression they were very busy. Such an impression was clearly understood by Mr Ladouceur as early as 9 February 2018, in an email he sent to Ms Roberts stating, “I know your a busy clinic and I did not intend to waste your time”, which was also foreshadowed by the email Ms Roberts sent to patients on 6 June 2018 (referred to above) ahead of the osseointegration clinic, anticipating that “[i]t will be a busy day with lots of people attending”.
1145 However, I have concerns with Mr Ladouceur’s evidence, particularly that he felt at the time, that his dealings with Dr Al Muderis were unpleasant, and that they pressed him for a decision the next day, given the amiable email which appears to be from his email address and in his name, dated 18 June 2018. His explanation for this email was unsatisfactory. That said, given the evidentiary support for what happened at the time of the examination in New York, I do not consider that impacts on his reliability on that aspect. The email in which he thanked Ms Roberts and Dr Al Muderis for the compassion they showed in New York, is not inconsistent with an offer to discount a fee to enable him to have the surgery. Rather, that is consistent with what some other patients have described (e.g. Mr Smith). The email dated 18 June 2018 can be interpreted in one sense with a note of finality as a polite way of declining any offer made, or to discontinue any interactions with Dr Al Muderis’ team, particularly given there is no evidence of any further communication between Mr Ladouceur and Dr Al Muderis, Ms Roberts or Dr Rosenblatt after this email.
1146 The applicant’s submission that only Mr Ladouceur’s evidence describes what happened at the clinic in New York, is not correct. The terms of the invitation to attend the clinic which described what was to occur, with the follow-up email to bring recent x-rays, speak for themselves. Further, the evidence concerning accounts of what happened at other clinics that Dr Al Muderis conducted in the United States, is also relevant and it supports the plain meaning of the invitation to attend the clinic.
1147 I am satisfied that the consultation occurred as described by Mr Ladouceur, and that he raised the question of cost, and was offered a discount.
Ms Lisa Çalan
1148 Ms Çalan lives in Turkey. She is a filmmaker. On 5 June 2015, while attending a pro-Kurdish Peoples’ Democratic Party rally in Turkey, she became an above-knee double amputee after the Islamic State detonated a bomb in the crowd. She subsequently underwent many surgeries. She mobilised using a wheelchair at that time, although she was told she would be able to walk with a socket insertion.
1149 Ms Çalan gave evidence by video link from Turkey. Her evidence was given through an interpreter. She was an honest, credible, and generally reliable witness.
1150 The applicant submitted that Ms Çalan generally presented as direct and responsive, but her evidence about her medical condition was at odds with her own contemporaneous photographs and video which presented a different picture. He submitted that the Court should prefer the contemporaneous evidence where it conflicts with her evidence, and her oral evidence over her affidavit. As apparent from the discussion below, I do not accept that submission as to inconsistency. The applicant’s submission in respect to the photographs is advanced on a misconceived basis.
1151 Ms Çalan gave evidence that she came across information about osseointegration and Dr Al Muderis in early 2017. On 11 October 2017, she underwent bilateral transfemoral single-stage osseointegration.
Risks and complications
1152 In enquiring about osseointegration and, later, preparing for surgery in Australia, Ms Çalan corresponded with Dr Rosenblatt and other members of Dr Al Muderis’ team via email. Ms Çalan, who speaks Turkish, required an interpreter or translator to communicate in English. She relied on English-speaking friends to translate what doctors said to her in person, in writing and over the phone.
1153 On 6 March 2017, Ms Çalan’s case was presented to the Musculoskeletal Reconstruction and Osseointegration Clinic. At the clinic, the team, who included Dr Al Muderis, Dr Rosenblatt and Dr Tetsworth, discussed Ms Çalan’s situation. Ms Çalan did not attend. There appears to be no record of this consultation apart from a consultation report dated 16 August 2017, which was emailed to her. At this stage, Dr Al Muderis had not spoken to Ms Çalan and there is no evidence that she had been assessed for her suitability for the procedure by a pain specialist or a psychologist. Rather that report records the conclusion was based on x-rays, as well as her medical history. She had not undergone a physical examination. Despite this, Dr Al Muderis and the team concluded that she “would be an excellent candidate to undergo bilateral, transfemoral single-stage osseointegration procedures”.
1154 The consultation report is brief. It contains no reference to potential risks or complications of the surgery. According to Dr Al Muderis, it was not translated. Dr Al Muderis was aware that Ms Çalan did not read or speak English. The report concluded by inviting “Ms Çalan to Australia to undergo bilateral transfemoral osseointegration procedures as soon as possible”.
1155 Dr Al Muderis was cross-examined about the report’s lack of reference to risks and complications. His answers were unsatisfactory. After accepting that the report did not contain references to those matters, he qualified his answer by saying that the four research papers referred to at the bottom of the report “would” discuss risks of surgery or would “very likely” represent risks and complications. As the respondents submitted, he gave those answers to overcome the failure of the report to address any risks or complications of the surgery. That being so, the reasoning proceeds on the basis that Ms Çalan could have downloaded the scientific papers and read for herself what risks or complications she might face (bearing in mind that she lives in Turkey and does not speak or read English).
1156 On 16 July 2017, Dr Rosenblatt provided Ms Çalan with an estimate of fees totalling AU$113,100. In his covering email, he explained the estimate reflected a discount of more than AU$50,000. As referred to above, on 16 August 2017, the report was sent to Ms Çalan. On 20 August 2017, she completed a pain survey, which disclosed that she was routinely suffering from excruciating pain and provided details (including that it interfered with her life “quite a bit”). Ms Çalan also completed other forms required, for example, hospital admission.
1157 By 12 September 2017, Ms Çalan was booked in for double osseointegration surgery, confirmed for 11 October 2017. By 4 October 2017, she had paid for the surgery, being AU$108,151.47 (a further discount of AU$4,848.53 had been given). Her evidence was her colleagues helped fundraise for the surgery.
1158 It was readily apparent that Ms Çalan was a very vulnerable patient. Like other patients, she was determined to walk again, having experienced an incredibly traumatic and life-changing incident. Dr Al Muderis gave evidence that he was aware Ms Çalan had severe PTSD, suffered panic attacks, had a significant pain issue, and was dependent on opioids. He was aware pain was a significant concern to her.
1159 In that context, Ms Çalan had paid for her surgery and travelled to Australia without Dr Al Muderis having explained the risks and complications of the surgery to her. There is also no evidence that Dr Al Muderis told her that her pain may be worse after the surgery. The respondents submitted that in circumstances where Ms Çalan completed a pain survey, disclosing that she suffered routinely from excruciating pain, and where Dr Al Muderis otherwise knew pain was a significant concern to her, Dr Al Muderis ought to have ensured that she was fully aware that she could end up in more pain after the operation than before. They submitted the evidence showed he failed to do so.
1160 The applicant referred to two aspects of the evidence to support a submission that Ms Çalan was aware of the risks and complications of the surgery before she paid for the surgery.
1161 First, he relied on Ms Çalan’s evidence of a conversation with Dr Rosenblatt. She described him as telling her there was an infection risk, but that it could be controlled. She also said she did her own research and understood there was an infection risk.
1162 Plainly, this does not satisfy any obligation on Dr Al Muderis’ part to ensure that a patient is fully informed of the risks and complications.
1163 The applicant also submitted that Ms Çalan sent “a list of about 20 questions concerning risks and complications to Dr Rosenblatt” and the Court should infer he would have answered them. However, Ms Çalan’s evidence was that the questions “included” questions about risks and complications, not that all twenty questions were of that kind. There is no evidence of a written reply to her questions. Ms Çalan’s evidence was that she raised the issue of infection with Dr Rosenblatt, and he said there was such a risk, but that that would be dealt with without it being a problem. Beyond being told she would be left with an open wound following surgery, Ms Çalan does not refer to any other matters being raised. She was specifically asked in cross-examination about being told the operation might not work, which she denied, explaining that she was told the operation would be good for her. She was not cross-examined to suggest Dr Rosenblatt or Dr Al Muderis explained other specific risks and complications to her on this occasion. Dr Al Muderis’ obligations are not satisfied in those circumstances. There is no evidence to suggest he was aware of what Dr Rosenblatt said on this topic.
1164 Second, the applicant referred to his evidence that he had a telephone call with Ms Çalan. It is unclear when this is said to have occurred. Ms Çalan was clear that she only ever spoke to Dr Rosenblatt before coming to Australia. The applicant submitted that his and her accounts are not irreconcilable, as Ms Çalan might not have realised that Dr Al Muderis was also on the phone during a call with Dr Rosenblatt. However, Dr Al Muderis did not suggest in evidence that the calls he was referring to were those where Dr Rosenblatt spoke with Ms Çalan, rather his evidence was that he personally made calls to Ms Çalan. Nor is it suggested (and there is no evidence) that he discussed risks and complications on such a call. There is no documentary evidence supporting the applicant’s evidence. Given the circumstances, if there had been such a conversation, it would be expected to have been documented. I also accept the respondents’ submission that the evidence failed to show Dr Al Muderis ensured that Ms Çalan was fully aware that she could end up in more pain after the operation than before.
1165 As referred to above, the 16 August 2017 consultation report (relating to the presentation of Ms Çalan’s case to Dr Al Muderis’ team) also does not contain any references to the risks and complications of surgery. The applicant’s evidence about the report was disingenuous and was said to overcome what is an obvious omission from the report.
In Australia
1166 Ms Çalan arrived in Australia on 4 October 2017 and met with Dr Al Muderis on 5 October 2017. Dr Al Muderis accepted that the first consultation with her in person was very important. He accepted he needed to satisfy himself that Ms Çalan understood the risks and complications of the surgery and that she gave informed consent for the surgery. He had not organised for a certified interpreter to be present and instead relied on a friend of Ms Çalan’s to translate.
1167 The 5 October 2017 consultation report has scant detail. There is no reference to any risks or complications, or even any discussion on this topic. I have referred elsewhere to the applicant’s evidence as to consultation reports being a summary for his use (see Consultation reports, Part 6, Section 1). I note Ms Çalan was the first patient Dr Al Muderis was cross-examined on. Of the consultation reports in evidence relating to first consultations, the content in this report is remarkably brief. The report does not refer to anyone else being present. The report does not provide any recommendation or advice regarding Ms Çalan’s suitability for surgery but rather proceeds on the basis that the surgery will occur. That reflected the reality of the surgery having been booked and paid for before she arrived in Australia.
1168 Ms Çalan’s evidence was that the consultation was short. She explained that while Dr Al Muderis mentioned the risk of infection and bleeding, he said words to the effect that these were things that could be kept under control. Dr Al Muderis accepted these are words he might have said. Ms Çalan assumed, without recalling, that he explained the procedure to her.
1169 This consultation was held before Dr Basten’s assessment of Ms Çalan on 6 October 2017, from which his report provided recommendations regarding communicating with Ms Çalan, including in relation to her concern about pain. There is no evidence of what, if anything, was done with these recommendations.
1170 Ms Çalan also gave evidence that Dr Al Muderis did not tell her that he designed the implants and that they could degrade. He denied not telling her that the implants were his proprietary implants. I note the financial disclosure form is in English and there is no evidence it was translated for her. The applicant’s reliance on her signing this form does not assist.
1171 On 11 October 2017, Ms Çalan underwent bilateral transfemoral single-stage osseointegration.
1172 The operation report does contain a pro forma statement of consent. This is a discussion that occurs in the anaesthetic bay. Dr Al Muderis said this report is normally completed by a fellow. He said that some of the risks referred to are general, and some are specific to the actual part of the body that is to be operated on. He explained that the matters in the consent paragraph of the report are a summary of the important, material points covered, although it extends beyond that.
1173 This operation report refers to general risks of surgery, with no mention of any risks specific to osseointegration, for example, recurrent infections, a need for further surgery, or that pain after surgery may be worse than before. One would have expected that if specific risks were discussed, they would be material and recorded. In any event, that this discussion occurred immediately prior to surgery renders reference to any of those specific matters insufficient. As discussed elsewhere, by this time, patients – particularly overseas patients – have committed to the surgery.
1174 As previously explained, Ms Çalan relied on her friends to translate what doctors said to her in person. Dr Al Muderis did not organise for a certified translator to be present in the consultations, including, significantly, those consultations conducted before surgery where obtaining informed consent was required. Dr Geffen gave evidence that he “would have expected an independent certified translator to be present for all consultations and in particular for consent”, and that he did not consider assistance from Ms Çalan’s friend to be adequate. Given the importance of informed consent, Dr Geffen’s evidence of the use of a certified translator should hardly be controversial.
1175 As evident from the discussion above, the applicant’s submission that the Court should reject any suggestion that Dr Al Muderis did not adequately explain the risks and complications, is in part based on the acts of others. For example, it relies on Ms Çalan accepting in evidence that she understood before surgery that the procedure was risky. However, that evidence was not based on anything Dr Al Muderis said to her; she explained she came to understand so much through her own research. Further, her evidence of her understanding of the specific risks was limited to infection.
1176 I am satisfied that Dr Al Muderis did not adequately explain to Ms Çalan the risks and complications of this surgery before she had paid for it, or before the surgery occurred. It follows that Dr Al Muderis could not have obtained her informed consent.
Post surgery
1177 After surgery Ms Çalan had ongoing issues, including with pain, infection, and granulation tissue. On 17 October 2017, she was discharged from Macquarie University Hospital to the Meriton. On 29 October 2017, she was transferred to The Hills for rehabilitation, where she stayed until 26 November 2017.
1178 Her progress at The Hills was slow, and complicated by a stump infection. On one occasion, she was admitted to Norwest Private Hospital under the surgical team for management of her stump infection, which was treated with intravenous antibiotics (as described in her medical discharge from The Hills dated 25 November 2017). Her nursing discharge summary from The Hills dated 26 November 2017 states, inter alia, that she was on antibiotics at that date due to infection, and that she had a high temperature.
1179 The date of her admission to Norwest Private Hospital is unclear. A consultation report dated 13 November 2017, dictated by Dr Rosenblatt on Dr Al Muderis’ behalf, notes that Ms Çalan was on antibiotics at that time, although it records that they should be discontinued due to the absence of any evidence of infection. I note the report also states that Dr Al Muderis will be “coming by the Hills” on 16 November 2017, “to inspect the stomas at that time”. This is rather unusual given his explanations in evidence as to why he had not visited other patients of his at The Hills: see [1636]. This consultation appears to be before her admission to Norwest Private Hospital. It can be inferred that the antibiotics that Ms Çalan was taking had been prescribed by a doctor at The Hills and that it was considered necessary.
1180 It was put to Ms Çalan in cross-examination that she was mistaken about the reason for her going to Norwest Private Hospital from The Hills being because of infection or fever, which she denied. As she said, she was given antibiotics. This continued when she went back to The Hills. Her evidence is supported by contemporaneous records.
1181 Despite documents from The Hills recording her medical position at the time of discharge, and during her stay (including her condition at the time of her admission to Norwest Private Hospital), in cross-examination Dr Al Muderis was reluctant to accept that Ms Çalan was suffering from an infection at that time, because he had not seen the temperature chart and he had not made the diagnosis. This reflects a general inconsistency in the applicant’s approach (as reflected in his evidence), where he submitted that contemporaneous records should be relied on but nevertheless challenges the veracity or accuracy of the content of such records where they do not assist him.
1182 A further consultation report dated 21 November 2017 (again dictated by Dr Rosenblatt on Dr Al Muderis’ behalf) notes that Ms Çalan “is still complaining of a considerable amount of pain in both stumps” and had a significant amount of granulation tissue. This appears to be after her admission to Norwest Private Hospital. It recorded:
the patient recently was admitted to the Emergency Department with acute exacerbation of her pain, elevated blood pressure and elevated temperature all of which appeared to be due to a very hyper anxiety state … [t]he patient was started on Cefazolin [an antibiotic] at that time … and then she returned to The Hills Rebab Centre.
1183 The report concluded that Dr Al Muderis considered that:
a considerable amount of her pain and discomfort is psychological and that she simply needs to get out of The Hills as often as possible and to get out and about and see some of Australia.
1184 Dr Al Muderis placed Ms Çalan on antibiotics before she returned to The Hills. Again, this is consistent with Ms Çalan’s evidence.
1185 The respondents submitted the conclusion in the report that her pain and discomfort is psychological sits uneasily with the repeated insistence by Dr Al Muderis during cross-examination that he deals only with orthopaedic issues and is not qualified to deal with pain or psychological issues. He usually gave such an explanation when challenged in cross-examination for failing to act in response to an issue of that nature being raised by a patient.
1186 There is no evidence of any psychologist at this consultation, or being consulted before this conclusion was expressed and plan implemented. There is no evidence that Dr Al Muderis took any steps for a psychologist to be involved. As referred to above, Dr Basten had opined before her surgery (but after Dr Al Muderis’ pre-operative consultation), that Ms Çalan had concerns about pain. There is no evidence that this was addressed in the manner he suggested.
1187 On 26 November 2017, Ms Çalan was discharged from The Hills. She gave evidence of a conversation with Dr Rosenblatt expressing her desire to stay in Australia longer to continue treatment because she was experiencing ongoing pain and other symptoms. She also had a conversation of a similar nature with Dr Al Muderis. Dr Al Muderis said no, she needed to “get back to [her] normal life” and that he would monitor her in Turkey, saying “I’ll arrange a doctor in Turkey and make sure they look after you while you’re in Turkey.” Ms Çalan told Dr Al Muderis there were no implant doctors in Turkey. When she told him she wanted to stay to seek proper medical treatment, he said he feared she would seek asylum and that that would have negative implications for him.
1188 Dr Al Muderis gave evidence that he told her she needed to go back home and that he did not know how he could help her stay in Australia. He did not recall saying to Ms Çalan that he would arrange a doctor in Turkey to look after her, or her saying that the reason she didn’t want to go back was because there were no implant doctors in Turkey. He denied saying to her that he was worried she would seek asylum, which would have negative implications for him.
1189 Dr Al Muderis confirmed in evidence that he told her he would liaise with doctors in Turkey if need be, stating:
she was given the … standard post-operative protocol rehabilitation, and she was recommended to go back to Turkey, and … if she need any help … we would refer her to a local surgeon or local clinician in her area, wherever she is around the world.
1190 Ms Çalan’s evidence was that Dr Al Muderis did not tell her who that doctor would be. He said she was fine to fly. She received a little case with spare parts. She was not referred to a prosthetist in Turkey. That evidence was not challenged.
Return to Turkey
1191 In late December 2017, Ms Çalan returned to Turkey having undergone highly invasive surgery and experiencing ongoing post-operative issues. That Ms Çalan did so without Dr Al Muderis making any arrangements with a local doctor to treat her, and without any information about or names of doctors who had the knowledge and ability to do so, is uncontentious. Dr Al Muderis did not know of any doctor in Turkey who could treat Ms Çalan. There were no post-operative care plans in place.
1192 For Dr Al Muderis to perform the surgery in those circumstances, without satisfying himself that she could be appropriately cared for when she returned to her home country, is self-evidently inappropriate and does not constitute appropriate care. To send Ms Çalan home to face those circumstances is a failure of the same kind.
1193 As the respondents submitted, this was certainly not “best practice” post-operative care envisaged by Dr Al Muderis’ own witness, Spanish orthopaedic surgeon, Dr Pablo Corona. Dr Corona agreed that if a patient travels from another country for surgery, the surgeon should not perform the surgery unless satisfied there are medical practitioners in the patient’s home country who can look after the patient when they return home.
1194 Ms Çalan gave evidence that after her return to Turkey, she continued to experience problems and that Dr Al Muderis was largely unresponsive to her requests for help. Her evidence was that she has suffered ongoing issues with her implants in Turkey and has repeatedly sought medical assistance in relation to her implants, both in and outside of Turkey.
1195 The applicant submitted that after Ms Çalan returned to Turkey, she was under the care of her local treating surgeons, and that there is no cogent evidence that she had any serious health problems which required Dr Al Muderis’ personal attention. As a starting point, this submission ignores that on his evidence there was no doctor in Turkey (as far as he knew) with any experience with osseointegration patients who could treat her.
1196 The applicant submitted that an important issue in Ms Çalan’s case is what the Court should make of the many social media posts in evidence in which she frequently documented herself being active, mobilising on her prosthetic legs, and appearing happy. He focused much of his evidence and submissions in relation to Ms Çalan on social media posts which he says “permits the inference that … even if she was not always doing well, she was regularly and consistently doing well” and that the evidence “also gains cogency from the degree to which it is at odds with the very negative way in which Ms Çalan described her condition in her evidence in chief”. The applicant relied on the volume of the photographs and videos depicting her life. He submitted that:
[c]onsidering her contemporaneous social media publications as a whole, it is impossible not to conclude that Ms Calan was able to lead a normal and fulfilling life to a significant extent, even if she may also have had some problems along the way.
1197 I return to address this below.
1198 The applicant submitted that the Court should reject the allegation that Dr Al Muderis was unresponsive to Ms Çalan’s messages and requests in circumstances where it is said Ms Çalan’s own evidence corroborated Dr Al Muderis’ evidence that he discussed her care with her friend Amy by phone on multiple occasions. It was submitted that, given that evidence, there is no reason not to accept Dr Al Muderis’ and Ms Roberts’s evidence that messages were responded to. The evidence establishes that there were phone calls between Amy and Dr Al Muderis (or Ms Roberts). However, it cannot be extrapolated from that, as the applicant has done, that the applicant was always responsive to the messages, or that his evidence that he rang must be accepted. Ms Çalan’s answers in cross-examination, read in context, do not support that proposition. The submission proceeds on a misunderstanding of her evidence. Moreover, the submission also equates responding or speaking to Amy with being responsive to the request.
1199 Ms Çalan also gave evidence of not receiving responses, and of receiving responses considerably later than the request to Dr Al Muderis for help (including on occasions where his responses were so late that, in the meantime, Ms Çalan had the surgery that was the subject of the query). Although Amy and Dr Al Muderis may have had many conversations, Ms Çalan wanted Dr Al Muderis to talk to her doctors, and her evidence was that “there was no … proper discussion with the actual doctor”. Ms Çalan’s evidence is supported by the contemporaneous documentation.
1200 It is readily apparent from the content of some of the messages Ms Çalan sent, or were sent on her behalf, to Dr Al Muderis and Ms Roberts, that they were not responded to (or not for a considerable time in circumstances where the request on its face, had a degree of urgency). There were intermittent responses to some messages. Dr Al Muderis’ evidence that he would have called Amy on those occasions is often inconsistent with the content of those messages.
1201 Further, there are some emails Ms Çalan wrote (apparently with the assistance of a translator or translation software) which reflect on her state of mind at the time of writing. That Dr Al Muderis did not accept they did so is irreconcilable with their content.
1202 Take one such email, sent in April 2018:
Dear Dr. Solon and Dr. Munjid,
As you know, I have been in Turkey for over three months. From the minute I left Australia, I have caught an infection two times, and have been undergoing treatment at the hospital, often having to stay as an inpatient, for a long time. Since my pain is quite severe, I have been using narcotic painkillers, and my wounds have not yet closed. Before my return, I was fairly concerned about continuing my treatment in Turkey because no one here is familiar with this kind of treatment. However, you assured me by saying that you would always remain in contact with my doctor and the situation would be under your control. And believing you, I returned.
Unfortunately, you have not provided this contact, and have left me alone without recommending medication, talking to my doctor, or informing us whether this level of pain is normal or not. Moreover, even though we have informed Dr. Munjid that in case of the infection passing to the bone the prosthesis will be taken out, he has still not made contact with us! I’m very saddened by this situation. I have spoken to my other friends who have undergone the surgery and they said they have had no problems in communicating with Dr. Munjid. So I wonder why in my case, you are not staying in contact? Despite having informed Dr. Mujid of my infection and my pain level, why has he still not replied? I am not asking for too much; I only want, as a patient, to receive information and recommendations from my doctor. I have had, and am still having, many problems! The main ones are:
1. For my pain, and for the situation in general, Dr. Sinan Adiyaman needs to talk to you.
2. Since it was an Ottobock leg implant, they do not adjust the prosthesis; they say this treatment is not approved, and will not even tighten a screw. Since my knee joints have not been adjusted, I cannot walk or comfortably move around. I tried to talk with Stevan but could not get ahold of him either. Can you please speak with Ottobock in order for them to adjust my prosthesis? If these adjustments aren’t done, I will not be able to use my prosthesis.
I wish you a good day. Please do not leave me alone anymore.
Sincerely,
Lisa Calan
1203 This reflects Ms Çalan’s state of mind at the time, and her understanding of her circumstances. It also includes descriptions of her direct experiences of what had occurred (e.g. hospitalisations, experiences with pain etc). It is also a relevantly contemporaneous document consistent with her evidence as to the concerns she held before leaving Australia that she expressed to Dr Al Muderis. It is consistent with evidence of her understanding of what was to occur on her return to Turkey if assistance was needed. She plainly felt abandoned at that time. It can readily be accepted that she faced difficulties, which are not surprising given the circumstances of her return to Turkey.
1204 The applicant’s evidence in cross-examination on this email was evasive and argumentative. The questions asked were clear and direct. In relation to the inquiry about pain and whether he responded, the applicant said:
I clearly explained to her on several occasions … that I am not a pain specialist. I’m here to look after her osseointegration surgery. I repeatedly mentioned it to her that I don’t manage pain. We have a pain specialist that managed pain. I repeatedly mentioned it to Lisa herself, to Amy, that I’m not a pain specialist … I continue to say it and I say it to every patient, “I’m not a pain specialist. I am just a carpenter. I do surgery. I don’t understand pain management. I don’t prescribe pain medications.”
1205 There is no documentary evidence of any advice given in relation to pain. There is no evidence that Dr Al Muderis responded to this plea, including by informing her of the fact he is not a pain specialist. In response to the proposition that he did not ever tell Ms Çalan whether the level of pain she was experiencing was normal, Dr Al Muderis said that “I don’t comment on pain unless it’s related to an injury that occurs or a complication of osseointegration surgery.” He said he triages the messages he receives from patients, and if the pain that they suffer from is related to a mechanical problem in relation to osseointegration that can be reversed by a surgical intervention or a surgical advice, he responds immediately.
1206 That he said he is not a pain specialist is not a basis for a failure to respond to this plea for help.
1207 That answer also does not address that the email complains about the failure to respond in relation to her infections. In his cross-examination, Dr Al Muderis said that Ms Çalan’s reference to infections in her messages was “her feeling”. He also gave evidence that he does not accept a patient telling him they have been diagnosed with an infection at face value. Rather, he said that “if a clinician make[s] the assessment about infection and conveyed it to me and I respond to them immediately”. However, the email also refers to the frustration towards Dr Al Muderis for not talking to her doctors, with Ms Çalan emphasising her doctor, “needs” to speak with them about her pain and situation in general.
1208 The other issue Ms Çalan identified in the email was Ottobock’s refusal to adjust the prosthesis, which is a practical problem. Again, there appears to be no response from Dr Al Muderis. I note that there is no evidence that, having given a patient his telephone number, he told them that he will triage the message sent, or that he will only respond if he considers it appropriate. The plain expectation is that a message (particularly a request for help) would be responded to.
1209 The applicant’s submission in relation to this email is that Dr Rosenblatt replied to it the following day, pointing out that Ms Çalan had failed to follow-up on his recommendations for qualified surgeons in Turkey she could speak to, and that Dr Rosenblatt’s email also attached written information about stoma hygiene and routine daily care. I note that Dr Rosenblatt’s reply does not state that he, or Dr Al Muderis, are not pain specialists, and therefore cannot answer her request. Rather, Dr Rosenblatt said he had tried to explain that the surgery may or may not get rid of neuropathic pain. That is not an answer to her question. Nor did Dr Rosenblatt respond to her request that her doctor needed to speak to them.
1210 Dr Rosenblatt did provide names of four doctors in Ankara who are “familiar with osseointegration” in response to Ms Çalan’s April 2018 email. Those four doctors were included in a list of eight doctors Dr Rosenblatt provided to her in December 2017, who he explained had “expressed an interest in osseointegration”. I note that in cross-examination Dr Al Muderis said he did not know anyone on the list of the eight doctors.
1211 In a 23 January 2018 email, Dr Rosenblatt had also provided the names of the four doctors, but said he knew nothing about them. In that email, he suggested Ms Çalan could travel to see surgeons in Jordan or Israel. On 25 January 2018, Ms Çalan replied, outlining the issues she was having:
As I [tried] to inform you before, when I arrived [in] Istanbul, the first reactions of doctors to my request for medical treatment of open wounds were, unfortunately, unclear and dismissive. Their main argument is that they haven’t experienced such a surgery before so they can not take the risk of intervening in my healing process.
1212 Ms Çalan also explained in the email that she did not have financial resources to travel to another country for treatment. The email concluded, “Dear Solon, I am begging you to not leave me alone at this point since I truly fear of [losing] my prosthesis because of false treatments and unnecessary surgeons.” The reaction she described of doctors in Istanbul is consistent with Dr Al Muderis’ evidence as to the technology being in its infancy. It is unsurprising.
1213 Ms Çalan’s evidence was she started to see the doctors on Dr Rosenblatt’s list, but they could not even prescribe medication because they knew nothing about the procedure. Properly considered, the evidence does not support the applicant’s submission that Ms Çalan only tried to contact one doctor.
1214 In this context, it is appropriate to refer to later occasions where Ms Çalan responded to requests from Dr Al Muderis’ office.
1215 The first was in July 2018, when Ms Michelle Nairne reached out to Ms Çalan. She explained that Dr Al Muderis’ ghostwriter wanted to mention her in his upcoming book, attaching a draft of a section featuring Ms Çalan. Ms Çalan responded in November 2018:
A few months ago you sent me an email requesting to include me in an upcoming book. Owing to Dr. Munjed’s ongoing refusal to engage with me or my doctors in a serious manner after my osseointegration surgery, I wanted to inform you that I do not give permission for my name or my story to appear in his book.
1216 On a separate occasion in August 2019, Dr Al Muderis’ office requested Ms Çalan complete a survey. She responded:
My experience with you was awful. I still have not been able to recover, because every time I had complications your team either ignored my messages, or dismissed my concerns. After several months of trying (and failing) to get your team to take my concerns seriously, I had to go to Germany for another surgery. This surgery did not go as well as it could have. It would have been much better if the doctor on your team who did the original surgery (Dr. Munjed) had been available to treat me in Australia, which was my first preference. I still deal with a lot of pain every day.
Considering all the trouble I have had with your team, I am not going to take time out of my day to fill out this survey. However, I will say that I would never recommend your team to anyone seeking osseointegration surgery.
1217 In March 2021, Ms Çalan received a request to complete another survey, to which she responded:
First of all, I want to thank you for performing the surgery which has enabled me to walk again, which has been a wonderful thing. However, after the surgery was completed, I did not receive adequate aftercare, nor communication from the team of doctors. Because of this, I experienced several complications which made the last three years very difficult! My friends and I sent countless emails and messages to Dr. Munjed, and even spoke with him on the phone, but on the rare occasions when we were able to get in touch with him, he did not take the complications I was experiencing seriously. I needed surgery to resolve those complications but since Dr. Munjed ignored my requests for help, I had to go from country to country seeking care. First I went to the Netherlands, then Germany, where I finally underwent surgery in Hanover. However, I still have problems with my legs and have not been able to solve them. Every doctor I have seen has told me that the original doctors who did my surgery need to fix it. I feel hopeless, and this hopelessness has greatly affected my mental health, despite being able to walk again. All around the world, if a doctor performs surgery on you, they are your doctor for the rest of your life, but unfortunately in my case, the necessary level of communication was not maintained. What I have gone through has led me to question medicine, doctors, and the hippocratic oath. One of the worst aspects of this situation is that with no one to turn to, I don’t even know what I will do if one of my implants is damaged. So that’s your answer - fill out the form yourself.
1218 To this email Ms Çalan attached earlier emails she had sent, as examples of the pleas for help she had made over the years. Those emails were consistent with the content of this email.
1219 These more recent emails also reflect Ms Çalan’s state of mind at the time of writing. A consistent picture is portrayed from the time she left Australia. The emails cohere with her evidence of her contact with Dr Al Muderis in that period. They are also written well before the publications and are contemporaneous with the events.
1220 The applicant does not refer to these emails in his closing submissions. They are inconsistent with the applicant’s submissions as to Ms Çalan’s life.
1221 The fact that Dr Al Muderis was not always responsive is also supported by the fact that he proffered several explanations for failing to respond to the messages for help. Regardless of whether these explanations are accepted, it is the fact of the explanations that recognises there were no responses on those occasions. One example, referred to above, is Dr Al Muderis’ evidence that he triages messages from patients, so that he only responded when he considered it was appropriate for him to do so. He explained that, in accordance with this system, he did not respond to a message relating to Ms Çalan’s pain because he was not a pain specialist. However, as noted above, after giving his telephone number to patients, there is no evidence that he told them he may not respond if contacted. As previously noted, the message he gives to his patients, and the impression they were plainly under, was that he would respond in any event.
1222 At other times, Dr Al Muderis would point to his limited expertise to explain a failure to respond to correspondence. For example, on 7 June 2018, Amy asked Dr Al Muderis via WhatsApp, “would you be able to send ottobock an email confirming it is safe for them to adjust Lisa’s prothesis?” When asked in cross-examination whether he did that, Dr Al Muderis responded that he is “not a prosthetist”. There was no apparent response to Amy’s message. That explanation given also suggests so much.
1223 The applicant also submitted as an explanation that not all the questions or requests Ms Çalan made, or were made on her behalf, were reasonable. In relation to several of Ms Çalan’s messages to Dr Al Muderis in May 2018 requesting that he contact her doctor, and which were prima facie not responded to, Dr Al Muderis said Ms Çalan “was in hospital. It’s inappropriate for me to intervene with her care when she’s under the care of a different clinician”. He said he had “a duty of care toward the patient and I have a duty of care toward colleagues”.
1224 If that was the position, it would have been expected to have been explained to Ms Çalan. There is no evidence that was explained to her. Nor is there any apparent reason one colleague could not talk to another, particularly in circumstances where it is evident that the surgery that Ms Çalan had undergone was not well known (and on his evidence, in its infancy which confuses a lot of clinicians). Dr Al Muderis instead opted not respond to Ms Çalan’s pleas for help. Again, the message he gave to Ms Çalan before leaving Australia was that he would contact her doctors.
1225 In any event, it is also evident on the face of the messages between Amy and Dr Al Muderis between May and June 2018 in evidence, that Amy had understood that Ms Çalan’s doctor, Dr Adiyaman, had sent emails to Dr Al Muderis trying to communicate with him. What can readily be inferred from the face of those messages is that Dr Al Muderis had not spoken to Dr Adiyaman during that time. Dr Al Muderis’ evidence that he had spoken to him is inconsistent with those messages.
1226 It is unnecessary to recite all the messages sent. Having considered all the evidence and accepting that although Dr Al Muderis did respond to some messages and did speak to Amy, there were many occasions where the response was delayed or non-existent. I accept that Ms Çalan was unhappy with the lack of response, and that given what I accept she was told by Dr Al Muderis before she left Australia, there was a basis for that unhappiness.
1227 Returning to the topic of Ms Çalan’s social media. The applicant relies on social media posts, photographs and videos, and on trips she has taken over the years (some documented on social media) to submit that this is inconsistent with her messages for help and the stated medical issues. This submission was that “Ms Çalan was able to lead a normal and fulfilling life to a significant extent, even if she may also have had some problems along the way”.
1228 I have considered this evidence along with all the other relevant evidence. I do not accept that submission as to inconsistency. I have addressed elsewhere the simplistic nature of this submission. The submission does not account for Ms Çalan’s evidence of what occurred, and the repeated messages she sent, and those sent on her behalf, to Dr Al Muderis and Ms Roberts seeking help. The social media relied on is not inconsistent with the contemporaneous messages which detail the help she was seeking and the reason for it. Further, simply because Ms Çalan is out and about and being active when she otherwise claims to be experiencing post-operative complications does not lead to the inference that at that time, she was not suffering in the way described in those messages. The evidence of her apparent wellbeing is not inconsistent with her evidence as to pain. When asked about a video of her dancing, Ms Çalan explained:
I like to dance, and when I feel okay, I try to take advantage of that feeling and do things that make me enjoy things. … I’ve spent … so much time in hospitals, and what you’re focusing on is … what’s posted in social media.
1229 Further, Ms Çalan’s evidence of looking for doctors to help her, to being in hospital often, to being concerned about the treatment she was getting, to reaching out to Dr Al Muderis for help, can hardly be described as a normal life. Yet Ms Çalan described doing those things, and her evidence is supported by contemporaneous messages (some of which are referred to below). I accept her evidence.
1230 Moreover, in this case, this submission also fails to address the matter relevant to the resolution of the issues before this Court. The question is not whether Ms Çalan is mobile, or whether she can go about her life, or undertake activities. Nor is the question whether Ms Çalan can undertake activities now which she could not do before the surgery. Rather, in this instance, it is whether it has been established that Dr Al Muderis failed to provide after care with the level of care, skill and attention that an ordinary person in the position of his patients would have expected. The applicant nevertheless appears to address the matter indirectly: if it is demonstrated that Ms Çalan’s post-operative health was sufficiently good, such that she did not require post-operative care to the extent asserted, then Dr Al Muderis’ obligations would not extend so far (and there would be no concomitant failure). The premise of that approach, however, is unfounded.
1231 It is appropriate to address aspects of the applicant’s submission through several examples.
1232 For example, the applicant refers to several social media posts between June and August 2018 and submitted they are inconsistent with her assertions as to her medical condition. He submitted these show that she is active and being social. However, the evidence also contains messages from May 2018 with images of her stump, its condition and that she had stiches in it, with repeated requests for help. In large part, there is no reply to the messages. Those events are referred to above. Although the applicant complains there are no clinical records from the hospital, the inference from the messages and photographs is that she is in hospital, and what is described is consistent with the photographs.
1233 In August 2018, there is another series of messages where, after a request for help was made, Ms Roberts asked Ms Çalan to send scans, which she did. This occurred on 21 August 2018, and thereafter there were repeated pleas for a response to the scans, including from Amy:
21 August 2018
Amy: Hi Claudia, I hope this message finds you well. Lisa’s doctors say that the reason she has so much pain/swelling is due to an abcess in her leg and recommended surgery. Lisa was planning on coming to Australia for treatment via a friend’s invitation, however, they were unable to do so. She would like to know if Dr. Munjid can issue her a one month medical visa? We tried messaging him but haven’t heard back.
Ms Roberts: Hi Amy
Munjed would like to see Lisa’s scans to confirm that there is an abscess. Can you please send them to us?
Amy: Yes, I will have Lisa send them ASAP. Thanks for getting back to me so quickly.
24 August 2018
Amy: Hi Claudia, I have sent the scans to Dr. Munjed’s email address. Please let me know if there are any problems viewing them. Thanks.
27 August 2018
Amy: Hi Claudia, Did you receive the email with the scans?
29 August 2018
Amy: Hi Claudia, Lisa just wanted to know if there are any updates regarding the scans. Her pain is getting worse and the doctors here are unable to treat her.
1234 Ms Çalan similarly pleaded for a response via email on 29 August 2018:
Hi Dr. Munjed, Claudia
Did you get a chance to look at the scans we sent last week? If so, do you think I can come to Australia for treatment? My pain has become intolerable, and I am unable to have any semblance of a normal life. If anything, my situation is worse than before the surgery. The doctors here say that they do not have enough resources or experience to help me. I will be returning to Diyarbakir soon, as there is no reason for me to stay in Ankara without treatment. However, there are no treatment options in Diyarbakir either, as I’m sure you are aware. For these reasons, I would like to know if you would be able to assist me in getting a visa for Australia to continue my treatment there. I would greatly appreciate if you could inform me of your decision as soon as possible, regardless of whether it is positive or negative, so that I can at least know what my options are.
Best wishes
Lisa
1235 And again later that day: “Very very pain please help me”. Dr Al Muderis did not recall responding to this email, and there is no evidence of any response.
1236 I note that, as the respondents submitted, Dr Al Muderis disagreed that Ms Çalan writing “[v]ery very pain please help me” was a cry for help. He explained that was so “because she knows I’m not the pain specialist”. He disagreed that “the proper human response on receiving a message like that is to respond to it in a sensitive and timely manner”. The respondents submitted this was callous. That is an apt description. It also illustrates his approach in giving evidence where he would not admit anything he perceived might reflect adversely on him (and justifying his position).
1237 Another example relates to the submission as to events in 2019, a time after Ms Çalan saw Dr Oscar van Waes.
1238 Ms Çalan was asked about seeing Dr van Waes in the Netherlands. She consulted him on 7 January 2019. It is correct, as the applicant submitted, that after seeing Dr van Waes, he emailed Dr Al Muderis for his advice as to what to do:
She complaints of pain of both left and right stoma. Left is stuck on implant; no signs of infection. Told her to leave it / treat expectant. Right had a surplus which is painful; is it an option to excise stoma; and take old scar to remove excess subcutaneous fat?
1239 It appears Dr van Waes attached several images to his email. Dr Al Muderis replied, “[y]ou could remove the excess tissue but my fear is that this will not improve her symptoms as they were significantly disproportionate to the physical finding.” I note he also told Dr van Waes that Ms Çalan: “[t]ook [a] very long time to mobilise and continue[s] to struggle with her condition”; he “failed to find a physical problem to address”; she had had “multiple falls but to date no fracture”; “[s]he has been led to belief that she has chronic infection from n [sic] the bone from what I was told”; she “[h]as seen few surgeons in Turkey who kept giving her antibiotics despite my objections”; and those surgeons “[a]lso offered her removal of implants”. It appears that Dr Al Muderis had been provided with some information about Ms Çalan. It also reflects that he was aware that there were issues with her treatment in Turkey, as she (via Amy) had been complaining about it.
1240 Dr van Waes responded that he concurred with Dr Al Muderis’ opinion, and explained that there were no signs of infection, and that he would advise Ms Çalan to wait and see, as she can always email him if “something alters for the worse”. In his initial email, he noted that she complained of pain in both the left and right stoma. The report he wrote thereafter, dated 8 February 2019, is consistent with that advice of Dr Al Muderis.
1241 This is the only documentary evidence of Dr Al Muderis communicating with a doctor (outside of his team) who consulted with Ms Çalan.
1242 The applicant’s submission that Dr van Waes’ report wholly contradicts Ms Çalan’s evidence of her problems is not correct. The report reflects that there was no sign of infection at that time. In Dr van Waes’ email, he was considering an excision and the removal of excess tissue. It cannot be said that there were no issues. Further, the history recorded by Dr van Waes accords with Ms Çalan’s description, and Dr Al Muderis advised Dr van Waes (it is unclear on what basis) that her issues are disproportionate to the physical findings. I note that Ms Çalan gave evidence she did see doctors in the Netherlands, who said Dr Al Muderis had got in touch with them and told them he had everything under control, and that they did not need to worry. She said she felt that Dr Al Muderis was trying to dismiss her, and that she had difficulty trying to convince the doctors to help her.
1243 Again, the applicant submitted that consistent with the advice given by Dr van Waes as to her medical condition, Ms Çalan’s contemporaneous social media posts spanning 8 March to 7 August 2019 continued to depict her regularly being active and socialising. I have considered these, and later images referred to by the applicant. In my view they are not inconsistent with Ms Çalan’s evidence of her condition and the email sent to Dr Al Muderis’ clinic in August 2019 refusing to participate in the survey, referred to above at [1216].
1244 I am satisfied that Dr Al Muderis failed to adequately assess Ms Çalan before informing her that she was a suitable candidate for osseointegration surgery and failed to adequately advise her of the risks and complications (and certainly not before the surgery was booked and paid for). In that context, any consent given was not properly informed. Further, he sent Ms Çalan back to Turkey without having post-operative care in place and the aftercare he provided was inadequate. He failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Observations about the international patients
1245 Before considering further the domestic patients, it is appropriate to make some general observations that arise from the evidence of the international patients. These patients are relied on by the respondents (together with other evidence) in relation to proving the substantial truth of various imputations, including those relating to, inter alia, the prioritisation of money, fame, reputation and numbers, the downplaying of the risks and complications, and aftercare. This evidence is also relevant to other factual issues, for example, Dr Al Muderis’ evidence (and his witnesses’ evidence) of his standard practice. The evidence is revealing.
1246 In relation to the American patients, the evidence reflects that business was an imperative for Dr Al Muderis’ practice. He travelled to the United States not only to speak at conferences and lectures, but to promote himself and his osseointegration system to prospective patients. That is, to attract patients to Australia to undergo osseointegration surgery with him. As Ms Roberts accepted in cross-examination, Dr Al Muderis would travel to the United States for conferences and meet with potential (and existing) osseointegration patients. He would meet those patients in a hotel room, hotel conference room or hotel lobby. Patients were invited to attend his presentations.
1247 He had representatives in the United States, including Dr Rosenblatt and Mr Hernandez until at least mid-2018 (and, more recently, Ms Nikki Grace-Strader). As explained above, Mr Hernandez had an agreement with Dr Al Muderis (through his company, Osseointegration International) to promote him and his company. In practical terms, he was paid a commission for each patient he recruited to have surgery with Dr Al Muderis (as they would purchase Dr Al Muderis’ implant for that purpose). Significantly, as discussed elsewhere, the commission was to be kept confidential pursuant to the terms of their agreement. This prevented Mr Hernandez from disclosing to patients that he was receiving a commission. The invoices submitted by Mr Hernandez to Osseointegration International included bills for referrals of Ms Schaeffer, Ms Koolhoven and Ms Ulrich. The business model, in other words, was designed to conceal that fact from patients. Dr Al Muderis’ financial benefit was revealed in the financial disclosure form, which patients typically signed (with other papers) after they had arrived in Australia (where the surgeries were scheduled imminently and already paid for).
1248 As already discussed, when Dr Al Muderis attended conferences in the United States, his office organised clinics for him to see prospective and existing patients. Mr Hernandez was involved in organising these clinics, as evident from the emails in evidence. His work at the conferences generally included organising a booth for Dr Al Muderis (so he had a physical presence), arranging for him to present on osseointegration, and preparing and distributing promotional brochures. Dr Al Muderis sought to see as many patients as possible. Emails organising these clinics support that was the approach taken.
1249 The evidence from these former patients, as well as photos and videos, reflected that there was typically a booth advertising Dr Al Muderis’ osseointegration services (e.g. Ms Ulrich, Ms Schaeffer and Mr Bruha). Patients would staff the booth, wearing T-shirts advertising and promoting Osseointegration International. These patients typically wore shorts to display their osseointegration protheses. Mr Bruha gave evidence that Dr Al Muderis insisted he do so after he saw him wearing trousers, despite the fact Mr Bruha did not want to because of the condition of his stomas.
1250 It was agreed in these proceedings that Dr Al Muderis made US$75,000 in profit per American patient in 2018 and 2019.
Common features
1251 The experiences of all the international patients who gave evidence, including Ms Çalan, share several features. As will have been apparent from the earlier discussion, the evidence as to this aspect of Dr Al Muderis’ practice is supported by the documentary evidence and other evidence.
1252 First, although Dr Al Muderis deposes to a procedure (which is said to be his standard procedure) for evaluating prospective patients, that procedure did not occur or apply in relation to the international patients. Any pre-operative assessments generally did not occur until the patient arrived in Australia by which time they had a confirmed surgery date (according to the documentation they received). Patients had also already paid for the surgery but had not yet been warned of the risks and complications of surgery (as discussed below).
1253 Second, of the patients who had contact with Dr Al Muderis before arriving in Australia, their meetings abroad are properly described as consultations. Mr Bruha, Ms Ulrich, Mr Wynne and Mr Ladouceur saw Dr Al Muderis in hotel or conference rooms in the United States and did not see him again until arriving in Australia (except for Mr Ladouceur, who did not proceed with the surgery).
1254 These patients each gave evidence that during these meetings in the United States, they were assessed or examined by Dr Al Muderis, were told (or led to believe) that they were suitable for osseointegration surgery and discussed the cost of the procedure with him. The applicant denied those details of the meetings, alleging the witnesses had concocted their evidence. Their evidence of the consultations is consistent with the description of the clinics in the correspondence of Ms Roberts, correspondence providing patients a confirmed date for surgery before arriving in Australia, and quotes/invoices issued with the price of the surgery (generally consistent with the price quoted to patients during the meetings). It will also be recalled that the letter to Mr Bruha’s insurance company dated 18 May 2017, referred to above at [980]-[983] supports the patients’ evidence of the nature and content of the meetings. As apparent from the consideration of their evidence, I accept the evidence of each of those patients as to the meetings.
1255 Third, Ms Schaeffer, Ms Koolhoven and Ms Çalan gave evidence that they did not have a consultation with Dr Al Muderis until they arrived in Australia shortly before their surgery. That is, they had not met him before arriving in Australia. Although during cross-examination Dr Al Muderis suggested he would have spoken to those patients before they arrived, there is no evidence of this (i.e. no documentary evidence, or evidence from these patients). This was not put in cross-examination to the patient witnesses from the United States. Ms Çalan was clear she only spoke to Dr Rosenblatt before coming to Australia.
1256 Fourth, despite the international patients having limited or no contact with Dr Al Muderis before arriving in Australia, their pre-operative consultations with him in Australia occurred within days of the surgery (sometimes on the day before surgery).
1257 Fifth, all these patients were required to pay for the surgery (and associated expenses) before arriving in Australia, the purpose and significance of which is canvassed below.
1258 Sixth, the first consultations in Australia with Dr Al Muderis generally did not involve any other doctor, in contrast to the domestic osseointegration patients. This is reflected in most of the consultation reports. Certainly, they were not the kind of multidisciplinary consultation meetings Dr Al Muderis described in his evidence. That reflects the relative level of care these international patients received, including the time they were afforded to consider the risks and complications of the procedure. The purpose of the domestic patients’ consultations was to assess their suitability for surgery, such that they had not yet made any meaningful commitment to proceed. As discussed below, the circumstances surrounding these international patients’ consultations were very different and impacts on the issue of whether they gave informed consent.
1259 Seventh, whereas the Australian patients generally underwent rehabilitation in dedicated facilities, the international patients typically underwent rehabilitation as outpatients staying in a nearby Meriton apartment. This meant, for example, in relation to Mr Wynne, his post-operative care when an issue arose, depended on successfully contacting Dr Al Muderis or his team. As discussed elsewhere, generally this dependency continued upon their return overseas.
1260 Eighth, Dr Al Muderis was not proactive in liaising with the patients’ existing doctors or any other local medical professionals. The pre-operative consultation reports (for those consultations held in Australia the day or days before surgery) are not addressed to any doctor. There is no evidence that Dr Al Muderis provided the consultation reports to any local doctor to assist with the patients’ post-operative care. There is also no evidence that Dr Al Muderis liaised with any of the patients’ local doctors prior to surgery or satisfied himself that their doctors were informed on how to provide post-operative care. Nor is there any evidence of Dr Al Muderis giving patients the names of local doctors or prosthetists familiar with the surgery or his system. Rather, the evidence was that the patients were provided with their medical records to give to their doctors on their return. As apparent from the evidence, these patients had difficulties finding qualified persons to provide post-operative care upon their return.
1261 Ninth, and in that context, Dr Al Muderis created a relationship of dependency with the international patients. I discuss this issue with respect to the patients generally in greater detail elsewhere highlighting how the dependency was acute for international patients: see sting 4 in Part 7, Section 1. Dr Al Muderis told these patients to contact him if any issues arose after leaving Australia, giving them his mobile phone number. He told them that once they underwent surgery, they were family. Each of these patients said they attempted to contact Dr Al Muderis when issues arose. That this was the approach to be taken by the patients was emphasised by Ms Roberts in an email to Dr Al Muderis’ American patients on 15 August 2018, after his relationship with Dr Rosenblatt and Mr Hernandez was terminated. It informed them:
I wish to advise the recent organisational changes within the Osseointegration Group of Australia. Until now, Dr Solon Rosenblatt and Fred Hernandez were our representatives across Northern America however I need to inform you they are no longer part of our team. I strongly encourage all clinical enquires to be forwarded directly to Munjed or myself and all service/componenry queries be sent to Philip Hall.
We will endeavour to provide you with the best service and can be contacted as follows:
[Dr Al Muderis’ and Ms Roberts’ mobile phone numbers]
1262 Relatedly, Dr Al Muderis socialised with prospective and existing patients. Although the applicant considers this to be a positive occurrence, his approach fails to grapple with how those circumstances might impact a patient’s decision to proceed with the surgery: see The patients in Part 6, Section 1.
1263 Tenth, the patients were typically in Australia for one month before being sent back overseas. Some patients were sent home despite being concerned about their medical condition. The prepayment would appear to cover expenses for that month (including, inter alia, hospital fees, implant, accommodation, physician expenses and surgical fee).
Prepayment
1264 Dr Al Muderis required the international patients to pay for their surgery and have the money cleared before their arrival in Australia. As evident from the evidence, this policy applied irrespective of whether they first saw Dr Al Muderis before or after arriving in Australia. At the time payment was made, the patients who gave evidence had been provided with documentation containing a confirmed date for their surgery. Payment was required before Dr Al Muderis had adequately assessed the patients (if they were assessed at all). In neither scenario (even on the applicant’s case) had Dr Al Muderis explained the risks and complications of the surgery to them before they paid. The implication of this for the patient, nonetheless, was that they were suitable for surgery.
1265 I elaborate on the significance of these circumstances below.
1266 Dr Al Muderis gave evidence that the patients only paid for a “tentative” surgery. That is, payment by the patient was not indictive of surgery having been confirmed. Yet none of the documents from Dr Al Muderis’ office sent to these patients describe the surgery as tentative but rather convey that their surgery was to proceed. Some documents record, for example, “This is to confirm that you have been booked in to have your Osseointegrated Prosthetic Limb”. In Mr Bruha’s case, he was provided a document which was titled “CONFIRMED INTERNATIONAL OI SURGERY” for a procedure date of 12 July 2017. Further, the cover letter with his fee estimate stated that: “After confirmation of a surgical date, patients will receive an invoice reflecting” the amount in the fee estimate. The latter documents were sent on 7 June 2017, for a procedure on 12 July 2017.
1267 The high point of the applicant’s case on this issue is his reliance on Ms Ulrich’s evidence. He submitted that she initially said she was always under the impression that her surgery was going ahead, because it was scheduled, but she later conceded that she had to be assessed as physically safe to have the surgery, and that the point of all the pre-operative tests was to confirm that it was safe for the surgery to proceed. The applicant referred to Ms Ulrich’s statement in cross-examination where she agreed that “I guess if there was something found wrong that prohibited me from having surgery due to safety, yes, I would think they would not do surgery” and submitted that this was the case for every American patient. Ms Ulrich accepted the reason for doing the tests was to ensure that it was safe for the surgery to proceed. I note that the applicant also relied on Mr Bruha’s evidence where he accepted that he needed to be medically assessed in Sydney before it was confirmed that he could undergo his osseointegration surgery.
1268 However, that does not make the surgery “tentative” or “pending”, as Dr Al Muderis repeatedly suggested in his cross-examination. When asked in cross-examination, he could not point to anything in the standard form arrival schedule or pre-operative assessment documents suggesting that the surgery was tentative. Rather, as noted earlier, the documentation refers to a confirmed surgery date. His evidence was that several members of his staff told the patients the booking was tentative. However, when pressed in relation to particular patients (such as Mr Bruha and Mr Wynne), he said he did not know who had told them. He also proffered that he himself tells the patients this, despite saying he could not recall when he had done so. There was no evidence which supported his assertion. Indeed, none of the patients gave evidence that they were told it was a “tentative” booking. Rather, the date for surgery had already been confirmed, but as both Ms Ulrich and Mr Bruha accepted, that date was subject to whether something made it medically unsuitable for them to proceed. This does nothing to alter the patient’s expectations.
1269 It can be accepted that the patients knew at some stage they had to undergo tests on arriving in Australia. However, it does not follow that they regarded their surgery booking as anything other than a confirmed date. That is so, even if it was understood that a test result may alter that.
1270 Although it may be accepted some communications were to confirm the date of surgery, rather than to confirm a patient’s suitability, the circumstances are such that a patient would readily infer that they are suitable for the surgery.
1271 The bottom line is that the patients were required to pay for their surgery before they arrived in Australia. At that time, they had not been told the risks and complications of the surgery. Such consultations only occurred shortly before the surgery, and in four instances, the day before the scheduled surgery (this being Mr Bruha, Ms Schaeffer, Ms Ulrich and Mr Wynne). I return to this below.
1272 The applicant’s case is inconsistent as to why prepayment was required. Initially, when cross-examined on this topic, he said he did not know that there was a standard practice for payment by international patients, and how or when the fees were paid. He also denied that all the American patients had to pay the fee estimate before they arrived. Later, he gave evidence that being required to pay in advance of their arrival to Australia was an oversight because the patients are required to prepay “before undergoing the surgery” and hospitals do not allow patients to be admitted otherwise. Shortly thereafter in cross-examination, Dr Al Muderis explained prepayment was required because of the risk of non-payment for international patients. Dr Al Muderis described that it was not fair otherwise, because there is no way for him to chase up a patient from overseas if they fail to pay following surgery. By this stage of the cross-examination, he accepted that he had a detailed understanding of how the prepayment process works and said that he had known the system since international patients started travelling to Australia for surgery with him.
1273 He gave evidence that:
… the purpose of it is before getting admitted to the hospital. They pay for the service – so, for example, … when they arrive to Australia, upon arrival at the airport, there is a taxi driver waiting for them that incur fees. So instead of inconveniencing the patient and getting the patient to pay for that, it’s paid upfront in – in trust, and from that trust, that fee gets paid to that person. Then, when they go and check in at the Meriton Apartment or whichever hotel … the hotel will ask them for payment, … this process is done to facilitate that for the patients. That doesn’t mean that it’s an obligation for the patient – that the money is gone and it’s not refundable … I had a British patient who arrived to Australia and was not found suitable for the surgery … and then … the patient went back … then whatever money is there … was refunded to them, so it is a refundable amount to the patient, if they don’t go ahead with the surgery. I understand it’s inconveniencing the patient that they travel all around the world to come to Australia and then they find out that they are not suitable, but there is no other way of doing it.
1274 I note there is no explanation in any of the documentation in evidence, including in any of the documentation sent to these patients requiring prepayment which explains that position, or that the money they paid is being held for them similar to a trust fund.
1275 Significantly, Dr Al Muderis’ explanation is not the explanation put by the applicant in cross-examination of the respondents’ witnesses. Rather, it was put to some patients in cross-examination that prepayment was a requirement to obtain an Australian visa. The applicant in reply tendered printouts of various policies and regulations relating to medical visas. Nothing in the documentation provided to the patients in evidence stated that the basis of prepayment was to obtain a medical visa. I note Ms Schaeffer, Ms Ulrich and Ms Koolhoven were provided a letter titled “Hospital Admissions Information”, which simply stated:
VISA REQUIREMENTS: Visitors to Australia do require a visa. This is dependant upon your Nationality and Country of origin. Please check the following website to check your visa requirements - www.immi.gov.au/Pages/Welcome.aspx
1276 Suffice to say, the information pack letters do not mention that proof of prepayment was required to obtain a visa. Nor do they instruct patients that they would need to request a letter from the clinic proving such payment.
1277 It is plain that Dr Al Muderis’ office required that the amount be paid and cleared into his account before their arrival in Australia (not just prior to surgery). An email sent to Mr Bruha from Ms Zamani, Dr Al Muderis’ accounts manager, states, “the invoice must be paid in full before your arrival to Australia”. Similarly, an email to Mr Wynne from Ms Zamani states, “[i]n order for surgery to go ahead prepayment is required in full” and again in a later email, “[p]ayment will need to be cleared before you arrive in Australia”.
1278 The applicant put to Mr Wynne in cross-examination that he needed to submit paperwork, including proof of payment, to obtain a medical visa, to which he replied he could not recall. However, text messages between himself and Mr Hernandez demonstrate that Mr Wynne asked him about a visa before arriving in Australia. Mr Hernandez advised him to get a tourist visa, which Mr Wynne confirmed he did in re-examination. Further, an email from Mr Wynne to Ms Zamani prior to his arrival stated the steps he had undertaken at that point, which included obtaining tourist visas. Given the evidence, it is difficult to understand the basis on which it was put to Mr Wynne that he obtained a medical visa. The same proposition was put to Mr Bruha, that he applied for a medical visa and was required to submit payment records to do so, which he similarly said he could not recall. There is no evidence that he applied for a medical visa. Given that was not Dr Al Muderis’ evidence of the purpose of the prepayment, again, it is unclear what the basis of the question was.
1279 Ms Stewart also gave evidence that staff (on Ms Bosley’s direction) recommended patients obtain a tourist visa to avoid the documentation and the more tedious process associated with obtaining a medical visa. An email from Dr Rosenblatt to Ms Çalan dated 16 July 2017 supports this, where his response to a visa-related question was as follows:
Most people simply request a tourist / visitor visa as the Visa for health reasons is very complicated and are often refused. If you simply request a tourist visa for 1 month that will satisfy all of the authorities.
1280 The applicant submitted that Ms Bosley provided an explanation for the charging procedures in an email to Ms Stewart. After Ms Bosley was forwarded a medical visa application from a patient, she wrote:
I don’t think these people are applying properly for their visas.
To get a medical visa they have to have a letter from us and show payment of their account in full prior to coming.
This hasn’t been done to my knowledge.
1281 However, that email does not support the submission that the prepayment policy was implemented because of any medical visa requirement. That was not Dr Al Muderis’, or anyone else’s, evidence. There is no evidence of any letters of the type Ms Bosley refers to.
1282 Ms Roberts also gave evidence that the American patients were required to make payments that cleared before they arrived in Australia. She described the practice as “standard”. She did not suggest or refer to this being a medical visa requirement. As Ms Stewart said in evidence, consistent with the evidence of the patients and Mr Hernandez, patients generally travelled on a tourist visa.
1283 In any event, it is difficult to see on the regulations tendered how the timing of the payment the applicant requires (that is, in time to clear into the applicant’s account before arriving in Australia) would be sufficient to enable a medical visa to be obtained.
1284 As the respondents submitted, Dr Al Muderis’ evidence was that prepayment was a billing practice he imposed to avoid bad debts. An email from Ms Bosley to a potential patient on 8 January 2016, referring to the need for payment and stating “we do not offer payment plans to international patients as the possibility of having a bad debt is just too high” supports that. I do not accept that the requirement for prepayment was limited to third party providers (such as the hospital and hotels), as Dr Al Muderis’ description of the rationale described above suggests. Nor do I accept that it is put in place for the patients’ benefit.
1285 That a particular patient may have required or applied for a medical visa (which may be a better option than a tourist visa for some foreign nationals) does not provide any basis to infer that, in the circumstances of this case, that was the rationale for the policy. There is no evidence to establishing (or even supporting) that proposition. It does not counter the compelling inference on the evidence that the purpose of the policy was to avoid bad debts. It was a business decision for Dr Al Muderis’ financial benefit. Although the applicant bears no onus, if the evidence otherwise existed, it would have been easily led (particularly in circumstances where the applicant chose to lead evidence to address this topic, being the tender of governmental policies of medical visa requirements). I do not accept that the requirement for prepayment of the surgery imposed by Dr Al Muderis is based on any need to obtain a medical visa.
1286 Dr Al Muderis’ evidence in cross-examination on this topic, and its inconsistencies, reflects adversely on him.
1287 The applicant also submitted that the issue of prepayment was not pleaded, does not address any imputation, and that there is no evidence adduced that there are any ethical constraints on surgeons about charging patients prior to surgery. Given this, and given that no amendment application had been made, it was submitted that the Court should not entertain this allegation. I have addressed the pleadings complaints elsewhere. Suffice to say, the applicant was on notice and given an opportunity to address it. So much is apparent by the fact that he led evidence on the topic in reply.
1288 There are several important aspects to this evidence. It is relevant to the assessment of the patients’ evidence as to their understanding of their position before travelling to Australia. That is, whether they understood that their surgery was confirmed. It is part of the context in which they came for surgery, having paid at a time, on their evidence, when they had not been warned abouts the risks and complications. It is also the context in which the consultations in Australia occurred. Contrary to the applicant’s submission, it is evidence in support of several of the imputations The evidence relates, inter alia, to proof in relation to pressure on patients, sales tactics, risks and complications, patient consent, prioritising money, unethical conduct, and his practice being a numbers game.
Further observations
1289 It is appropriate to make two further observations, which are particularly relevant to the international patients who gave evidence. That said, it is important to recall that this evidence is not to be considered in isolation.
1290 First, the circumstances in which Dr Al Muderis discusses the risks and complications with the internationals patients denies them a genuine opportunity to rationally assess their commitment to the surgery, bringing into doubt whether they gave informed consent.
1291 By the time the risks and complications were said to be discussed, the patients had incurred considerable pecuniary and non-pecuniary costs. Those costs already paid generally included the surgical and hospital fees for the procedure, which were substantial (in addition to other costs including travel from the United States and living expenses). For several of these patients, this involved fundraising or going into debt to afford the surgery and the associated costs. The costs of travelling to and staying in Sydney were significant. Australia was an objectively faraway destination for each of these patients. Several patients travelled with their family or friends for support. The patients generally expected to stay in Australia for a month. By the time the patient had arrived in Australia for their pre-operative consultations, they expected to benefit from a life-changing operation. It was conveyed to the patients that they were suitable for the surgery, with their surgical dates confirmed. Any emotional or psychological commitment would have been significant.
1292 Yet, despite those circumstances, Dr Al Muderis – on his case – only discussed the risks and complications of the surgery with these patients a day or days before surgery. Indeed, these patients’ pre-operative consultations were inadequate, having been conducted in circumstances where they either had a consultation in the United States that was itself inadequate, or no consultation at all prior to arriving in Australia.
1293 The respondents pointed to the evidence of Dr Geffen that:
… I do not believe, after a substantial deposit is paid, that an objective and rational view of the risks and complications possible in this surgery, are assessable by a reasonable person. In simpler terms, their judgement is clouded as they already have made a substantial commitment to proceed.
1294 That is a logical, common-sense assessment, and one that applies equally to non-pecuniary costs. Once such an investment has been made, the ability to rationally assess what is being said is likely impacted.
1295 I note that the applicant claimed in his proceedings against Mr Hernandez that he made US$75,000 in profit per American patient for each surgery in the years 2018 and 2019. That amount of profit at that time was ultimately agreed by the applicant during this hearing. There is a clear financial advantage to Dr Al Muderis in charging such fees.
1296 Requiring prepayment of such significant fees places pressure on the patient, which the international witnesses experienced, to proceed with the surgery. The occasions where Dr Al Muderis said he would or did provide a discount, provide a reduced rate, or permit the delay in some of the payment to enable them to have the surgery, exacerbates that. A patient would be grateful for the favour, as if they were being treated specially, further impacting their ability to rationally assess their commitment to the surgery. The pressure the patients face would be compounded by any non-pecuniary costs incurred.
1297 The applicant’s submission that there is no evidence adduced concerning whether there are any ethical constraints on surgeons charging patients prior to surgery misses the point. The implication being, there is nothing wrong with the practice. However, the issue that arises here is not payment before surgery, but payment before any consultation (or any proper consultation) has occurred, or requisite discussion of the risks and complications.
1298 The respondents referred to the evidence of Dr Doshi who accepted that it would be unethical to require a patient to pay for surgery before they had been assessed as being suitable for it. They also referred to the fact that Dr O’Carrigan accepted that a patient should never be booked in for osseointegration surgery to occur until they have been assessed as suitable for the surgery. Dr O’Carrigan also stated that it would be “unusual” for a patient to pay for osseointegration surgery before their suitability had been assessed. When asked whether he thought that to ask a patient to do so would be unethical, Dr O’Carrigan reluctantly said, “I guess so”. Dr Geffen also similarly described the circumstances in his report and concluded that the resultant pressure on patients would be unethical.
1299 It will be recalled that one of the stings conveyed is that his conduct was unethical. Suffice to say at this stage, given the meaning of unethical described above, this practice is unethical. However, this should not be considered in isolation.
1300 Second, Dr Al Muderis provided inadequate post-operative care to several of the international patients despite having created a relationship of dependency with them. The shortcomings share similarities with several of the domestic osseointegration patients. However, they are more acute in many respects, including because, on Dr Al Muderis’ evidence, he lacks the ability to provide post-operative care to patients in the United States. As he accepted, he does not have a licence to practice medicine in the United States.
1301 The implant system is proprietary. Osseointegration was not approved by the FDA in the United States at the relevant times.
1302 The procedure is, on Dr Al Muderis’ evidence, “an innovative technology that is … still in its infancy.” He stressed that was a reason for following up with patients. He explained later in his cross-examination, when discussing infection:
Patients with osseointegration surgery … it’s a technology in its infancy. It confuses a lot of clinicians when they see it. … when GPs see a piece of metal sticking out of the leg with serious discharge coming out … the first thing come to their mind is that, “Is this infected or not?” And that’s a natural occurrence and that’s … what we face with osseointegration technology, as osseointegration surgeons, and it will take decades to educate the population of clinicians about what is infected, what’s not infected.
1303 Dr Corona, a witness for the applicant, agreed that if a patient travels from another country for surgery, the surgeon should not perform the surgery unless they have satisfied themselves that there are medical practitioners in the patient’s home country who can look after them upon returning home. It was incumbent on Dr Al Muderis to ensure that these patients would receive adequate post-operative care after leaving Australia, especially given the nature of the procedure.
Section 5 — Ms Eang Srey Da and Mr Pril Sina
1304 Two witnesses were called who underwent osseointegration surgery with Dr Al Muderis during a humanitarian trip to Cambodia in 2015: Ms Eang Srey Da and Mr Pril Sina. The trip to Cambodia was filmed, and an episode of Inside Story about Dr Al Muderis featured, amongst other things, aspects of that footage. The program producer, Ms Karen Willing, gave evidence for Dr Al Muderis. While reliance is placed on the footage, particularly by the applicant, some care should be taken as it was known it was being recorded. People may act differently in that context. Further, there are only short snippets relating to the Cambodia trip contained in the program.
1305 Ms Eang became a left above-knee amputee in 2009 after an unhealed ankle fracture from a fall later became infected. On 9 September 2015, Ms Eang had osseointegration surgery with Dr Al Muderis. Prior to this, Ms Eang had been ambulating with an artificial leg, which fastened with a belt around her waist.
1306 Mr Pril had been in a traffic accident in early 2015 and broke his left leg, which was later amputated above the knee. He too received and relied upon a conventional artificial leg, which was strapped on with a belt around his waist. He was contacted by the Kien Khleang National Rehabilitation Centre for Persons with Disabilities and asked if he would be interested in osseointegration. On 7 September 2015, Mr Pril had osseointegration surgery with Dr Al Muderis.
1307 In addition to Ms Eang and Mr Pril, Dr Al Muderis also completed two other osseointegration surgeries while in Cambodia, thus operating on a total of four osseointegration patients during that trip. Those two other patients were not witnesses in this case but are noted for context.
1308 The surgeries took place in the Children’s Surgical Centre (the Centre) in Phnom Penh, Cambodia, a hospital located at the Kien Khleang Centre which provides care for children and adults without financial means to afford care in government hospitals.
1309 The evidence in Ms Eang’s affidavit, which is in her native language, as to the effect of the surgery on her, and her desire to have the implant removed, was not challenged. Although the applicant suggested to the interpreter of their affidavits, that several aspects of Ms Eang’s translation were not quite correct, these did not relate to matters of any particular significance. They did not relate to her evidence that she “had pus and fluid come out of [her] leg every day”, or that she said it still happens. Nor was her evidence challenged that sometimes her leg is “red and hot”, that it is sore, she is in pain every day and that she attempted to obtain help, but her attempts were futile. Given her symptoms, Ms Eang did not accept what she was repeatedly told by doctors – that her leg was fine or normal. Nor was it challenged that she asked Dr Jim Gollogly, an American orthopaedic surgeon who headed the Centre, to remove her implant, which he said he could not do. According to her evidence, she still wants the implant removed.
1310 The circumstances in which these surgeries occurred are that the patients could not afford the surgery. There is no evidence of any assessment undertaken as to whether the patients were in a position (because of their personal circumstances, including financial position) to return to the hospital for any help after the surgery. This is in a context where Dr Al Muderis described the surgery as being in its infancy, and where the patients were exposed to the risks and complications that could occur from the surgery (as illustrated by the evidence of other patient witnesses). According to the evidence before the Court, Ms Eang lived in a village about 60 km from the hospital. Mr Pril lived about an hour away from the Centre. As mentioned earlier, both Ms Eang and Mr Pril were previously able to walk using a socket device.
1311 A record of Ms Eang’s patient details does not include clinical information, but only basic background data. The same can be said of Mr Pril. Further, Ms Eang’s name had not appeared on an earlier list of possible patients, but had been added (as in, registered in the Centre’s system) closer to the surgery on the same day as the group consultation on 7 September 2015 (discussed below).
1312 The respondents submitted that Ms Eang and Mr Pril were not adequately warned of the risks and complications of the surgery.
1313 There was one group consultation in Cambodia which was that featured (albeit not in its entirety) in the footage of the Inside Story episode. Dr Al Muderis is seen in the footage responding to a question from a patient about risks with “there are risks with this operation”. Dr Gollogly then added: “Munjed, this is not Australia, right. Everybody will walk out”. The implication was that the patients would leave, if scared off by the risks. The respondents submitted that there is no proper or adequate response shown in the footage to this question. Dr Al Muderis gave evidence that, after Dr Gollogly’s interjection, he said “I need to tell them exactly the risks associated with the surgery. It’s their life ultimately. We’re here to serve them”. There is no evidence from him as to what, if anything, he then said to those at the consultation about the risks. What Dr Al Muderis said occurred does not appear in the recording shown on the program and neither Ms Eang nor Mr Pril gave evidence that supported this.
1314 The recording also showed Mr Pril saying that the implant looked “so big”, and Dr Al Muderis responded “yeah – yours will be smaller”, before continuing to describe how it would be inserted into his leg. Mr Pril asked (through a translator) whether the operation could “make him die”. Dr Al Muderis’ response was “yes, infection may make you die. It’s not likely but it may. It’s like the amputation. This could have made you die. Same risk”. Again, the respondents submitted that the responses were not adequate. His responses about the size of the implant and the possibility of death were brief and, as the respondents submitted, unsatisfactory.
1315 I note that Ms Eang does not appear in the footage.
1316 Ms Willing gave evidence of filming this session, describing that Dr Al Muderis, through the translations of a local doctor, explained to the other doctors and patients the osseointegration surgery, the risks and the upsides and downsides. He explained what a stoma was and what it would mean for the patients to have a stoma and how they would need to look after it. She also gave evidence that he spoke to each patient before surgery and examined each patient separately. Her evidence was that he spoke to them about risks and complications and emphasised to them that the surgery could not be guaranteed. She said he even told the patients that they could die.
1317 On the evidence, the explanations of the risks and complications do not appear to encompass the detail which Dr Al Muderis said in his affidavit is given to his patients, detail which he says is necessary.
1318 Any conversation Dr Al Muderis had with the patients was through a translator. These patients were vulnerable. There is no evidence of any steps taken by Dr Al Muderis to verify or ensure their understanding of the surgery they were agreeing to undertake, or of the risks and complications that can arise. Given the language barrier, there should have been a heightened awareness of the need to do so. Without a proper understanding, informed consent by the patients cannot be provided.
1319 There are no signed consent forms in evidence in relation to either Ms Eang’s or Mr Pril’s surgeries. On 5 September 2015, Ms Eang signed a form consenting to participate in a University of Notre Dame Australia research study, titled “Management of Complex Lower Limb Amputations, Using a Transcutaneous Bone Anchoring Device – Early Results of a Novel Treatment”. That form is unrelated to her consent to surgery.
1320 The evidence of Ms Eang and Mr Pril reflects a lack of understanding of the risks associated with the surgery.
1321 In cross-examination and re-examination, Ms Eang could not recall what specific risks from the procedure were discussed. Ms Eang’s evidence was that all she knew was that she needed to look after her wound, she could get an infection if she did not look after it properly, and that it would heal. She said if she was “told about the risks, what’s going to happen severely, [she] wouldn’t have had the surgery, but [she] wasn’t aware of any risk besides that”. That, according to her re-examination, is the extent of what she was told by Dr Al Muderis. In cross-examination, propositions were put to Ms Eang (over several pages of transcript), to which she simply replied “yes”. This included an exchange where Ms Eang answered “yes” to the question whether she remembered “the lady” (referring to Ms Bosley) speaking to her about things that could go wrong after the surgery. However, when asked in re-examination about these same matters, it was apparent that she was not sure about things or could not recall (for example, what the “foreign lady” said could go wrong with the surgery). Care needs to be taken to the evidence elicited in that manner. As observed above, Ms Eang does not appear in the TV program. It was put to Ms Eang in cross-examination that she told the crew that she did not want to be filmed, to which she responded “yes”. Again, this is in the context of a series of mere “yes” answers through an interpreter. The respondents submitted that it was “far from clear” that she understood what was being asked (i.e. gratuitous concurrence). That is an apt observation. I note that Dr Al Muderis suggested that she may not have wanted to be filmed, but Ms Willing does not recall anyone requesting that.
1322 In any event, it is clear from her evidence that Ms Eang did not understand that there would be fluid coming from her leg on an ongoing basis. She was not informed or properly informed of that prior to agreeing to the surgery. Rather, her evidence was that she was told she had two options: to have the surgery or not have it. Ms Eang said she was shown pictures of people with the implant, and she thought it looked “beautiful”, so she went ahead with the surgery.
1323 In relation to Mr Pril, he said Dr Al Muderis showed him a video, and was asked by him “‘Is it okay? Are you accept the surgery?’, and I said yes”. Mr Pril recalled a lady telling him that if he had serious issues, he should come back to the doctor. He recalled being told to keep his leg clean every day and if he did not keep it clean, he could get an infection. He did not recall being shown how to clean it. It will be recalled that it is Mr Pril who appears in the footage.
1324 The applicant referred to a photograph of Ms Bosley before a whiteboard as evidence that a discussion with the patients on wound care, long-term stoma care, infection and cleanliness occurred before the surgery proceeded. However, there is limited information on the board, it is about post-operative care, and to state the obvious, it is in English.
1325 It is apparent from contemporaneous correspondence (to which Dr Al Muderis and Ms Bosley were copied), that there were issues raised by the patients from very shortly after the surgery. For example, documentation records that very shortly after her surgery, Ms Eang wanted the metal implant removed because it was not what she had understood to be her implant, given the images she had been shown before the procedure. This reflects not only that Ms Eang was misled about the implant she thought she would receive, but she also did not appreciate the nature and impact of the surgery. It is plain she did not understand the procedure she agreed to undergo. One could infer in these circumstances that informed consent was not obtained.
1326 Indeed, the documents record that each of the four patients who underwent the surgery complained that the legs provided to them were not those shown in the video presentations by Dr Al Muderis, and those which the patients understood they were being provided. All four patients expected that they would be fitted with an Ottobock titanium limb as they had been shown in a video and were disappointed and dissatisfied with discovering after the surgery that they had been fitted with the International Committee of the Red Cross (ICRC) plastic prosthesis they had already been using. The document described that once they became aware that it was their ICRC limb they had used before, “their motivation and satisfaction for fitting the limb [was] very low”. There were also issues raised by a person who was associated with their care. For example, the correspondence also reflects that there were practical, biomechanical issues when using the implants with the ICRC component that needed to be addressed, which were over and above what was described as “very poor cosmesis”.
1327 That shows the level at which the information appears to have been provided and communicated to these patients. It can be inferred from the correspondence that despite the videos being shown to entice them to undertake the procedure, the patients were not informed (or properly informed) they were not getting the leg shown in the video. It is an obvious and natural inference to draw from being shown the video that this was what they were to be given (particularly when there was also a language barrier). Ms Eang and Mr Pril both had that expectation, which was entirely reasonable. Mr Pril expressly said in his affidavit that he agreed to have the operation so that he “could have a leg like they showed [him] in the videos” and was “disappointed” when the part he had was “not the same as the leg [he] saw in the videos”. They therefore agreed to the surgery on a false premise. The compelling inference was that the patients were not happy at the time. In cross-examination, Dr Al Muderis would not accept that proposition, and his answers on this topic, and to issues raised in emails by Dr Gollogly, were unsatisfactory. It is no answer to suggest that he did not promise them Ottobock limbs, if the videos or pictures they were shown of the result of the surgery had persons with such implants (or implants of a like-kind). There is no evidence of any explanation given to the patients that they would not be getting the legs shown on the persons in the video but rather would be using the ones they already had from the ICRC.
1328 The applicant does not refer to this issue, or this aspect of Ms Eang and Mr Pril’s complaints in his closing submissions. The contemporaneous correspondence supports the evidence of Ms Eang and Mr Pril, as to their understanding at the time, the basis for it, and their reactions post-operation.
1329 It is apparent from contemporaneous correspondence that there were other issues raised by those caring for the patients, apart from the type of leg provided. Dr Gollogly, in responding, looked to Dr Al Muderis for advice. There are other instances of that type of request from him. This reflects that although the applicant took offence to the suggestion that the local staff at the hospital might not be in a position to properly care for the patients after he returned to Australia, Dr Gollogly sought help, as did others. One email records that the prosthetists in Cambodia were uncomfortable with the new concept of osseointegration and did not want to get involved and so were looking forward to Dr Al Muderis’ next visit to await advice for prosthetic adjustments. That is unsurprising given, as noted above, the applicant’s own evidence of the technology being in its infancy (recalling also that this surgery occurred in 2015).
1330 The absence of paperwork for these surgeries was explained by Dr Al Muderis, in part on the basis that it was a humanitarian mission, and he assumed that documentation would have been kept by others. As to there being no signed consent forms, he said he did not know the process over there and did not get involved in administration. Dr Al Muderis gave conflicting evidence of his role. He said in respect to Mr Pril, that he completed an examination and formed his own assessment before surgery that he was suitable. Shortly thereafter, in relation to Ms Eang he said the opposite: “The patients get prepared for us by the team and we just get told what – what to do based on the – the assessment at the time”. It is apparent at least that Dr Al Muderis does not appear to have kept any records of what he did. He has no record of consent being given.
1331 It is apt to describe the surgeries in Cambodia as humanitarian work, but that does not distract from the rights of these patients, that they needed to understand what they were agreeing to undergo and the position they were left in following Dr Al Muderis’ departure. As Dr Corona said in evidence, surgeons performing surgery in a developing country have the same responsibilities and obligations to patients with respect to obtaining informed consent, as in their home country.
Patient follow-up
1332 As to patient follow-up, the applicant gave evidence it was “in a similar manner” to those scheduled in Australia. That is not the case. It appears from Dr Al Muderis’ records in evidence that he sought updates from the Centre regarding the patients’ progression on about four occasions over the eight-year period following the surgeries in 2015. Dr Gollogly’s reply to a request for an update by Ms Roberts on 5 November 2017, forwarded an email showing Ms Eang had not returned since her last follow-up on 27 March 2017, and stated:
We presume, rightly or wrongly, that they’ll come back if they have a problem, but we don’t go looking for them unless we know there’s a problem and they can’t come for some reason ... tell Munjed that’s the best we can do at the moment.
1333 Although Dr Al Muderis accepted, in light of that email, that the position differed from what patients in Australia received, he did not accept that it fell below the standard that would be expected in the circumstances, even by comparison to Australia.
1334 In relation to Ms Eang, I accept the respondents’ submission that her post-operative care was limited and intermittent. The records in evidence reflect that Ms Eang was not seen regularly after surgery, as would have occurred for domestic patients. I also accept the respondents’ submission that the limited records raise various concerns. The emails support her evidence of her concerns about discharge, among other issues, which she described in her affidavit. For example, on 5 October 2015, an email to Ms Bosley from Yong-June Kim reports Ms Eang failed to attend an appointment, that Ms Eang was worried about the serous discharge, and raised the issue that local prosthetists were reluctant to perform adjustments as they lacked expertise. This was responded to by Ms Bosley, but provided little assistance, writing only that:
It is quite normal for females to have higher serous discharge than the men, it is quite normal and usually settles in time. Please reassure the young girl that it will settle in time.
1335 On 27 March 2017, an email update to Dr Al Muderis and his practice manager, Ms Livingstone, records that Ms Eang had bigger complaints than the other three patients who underwent osseointegration. She detailed the repeated breaks of the thread inside the part for the front locking screw and the issue of an infection on the stump site. An email dated 18 July 2017 refers to Ms Eang as having returned to the clinic “many times” and describes her breaking the thread three times. The email raises Ms Eang’s misunderstanding as to the attachment of the leg. It also notes Ms Eang’s attendance at a follow-up on 27 March 2017, following her involvement in a motor vehicle accident the previous day. An email by Ms Roberts on 5 November 2017 requesting an update essentially involves much of the same information provided in the July 2017 email being repeated while noting that Ms Eang never returned for a follow-up. This information is reflected in a consultation record dated 7 November 2017. There is then no further update until 18 October 2022, which appears to have been sought proximate to the Publications. It is apparent from the email, that the patients were trying to be located for follow-up at that time.
1336 In relation to Mr Pril, updates were sought or provided at the same time. Again, they were very intermittent. There are records on 2 December 2015 (recording a follow-up on 18 November 2015), 27 March 2017 (which records Mr Pril’s last follow-up on 7 June 2016, and as at that time was not contactable), 7 November 2017 and then not until after the Publications, on 18 October 2022. I note that in the 27 March 2017 email update, it reports the other two male patients had not been seen since January 2016 and were not contactable. That remained the position in the 7 November 2017 update. While Mr Pril was seen at the time of the October 2022 update, the two other male patients could again not be contacted or located. The email reflects that one of the male patient’s last follow-ups was in June 2019, the other male patient was seen incidentally in June 2022 after attending the Centre for his children and Ms Eang’s last follow-up at the Centre was in September 2022.
1337 Again, the emails reflect patients did not attend appointments. Both witnesses gave evidence as to this. Mr Pril said that he could not afford to go to the Centre hospital and in any event, they just gave him supplies such as alcohol swabs and bandages, and otherwise did not help with his issues. He also gave evidence of the expenses required for him to maintain his leg which are significant given his financial position. Ms Eang’s evidence was to a similar effect. As referred to above, her evidence was of the difficulty in obtaining help, and that her attempts were futile.
1338 I note that September 2015 was the only time Dr Al Muderis operated in Cambodia, and he has not seen the patients since his visit but rather relies on the patients returning to the Centre if there are any issues. As I observed earlier, the follow-up for both these patients was intermittent, and in any case, what little updates were communicated to Dr Al Muderis and his team were rarely responded to by Dr Al Muderis.
1339 The applicant submitted, in addressing these patients, that:
The notion that patients in developing countries should not be given the same opportunities as others when it comes to medical attention and life changing surgeries is surprising. It is patronising (and somewhat racist) to suggest that local doctors are incapable of addressing complications, at least to the extent that they are able to seek opinions and advice from Dr Al Muderis should it be necessary. Irrespective of the (imagined and unproved) conditions, whatever the country, trained doctors are involved.
1340 However, the premise underlying that passage does not reflect the respondents’ submission. Rather, the respondents acknowledged that “the offering of surgical assistance to patients in developing countries on a humanitarian basis is admirable” but submitted that “it comes with concomitant responsibility”. The respondents then referred to the evidence of Dr Corona, who said in re-examination that when he goes to developing countries to operate, he first trains the local practitioners in post-operative care. He described that normally this involves them going to Barcelona (where he is based) to be trained in post-operative care. Dr Corona then performs the first surgical cases in the country and maintains a very close connection with the local doctors “to guarantee the best practice”, noting they have a “lot of options to be connected 24/7”. It is in that context, the respondents submitted that Dr Al Muderis needed to ensure that patients in countries such as Cambodia have access to medical providers experienced in osseointegration surgery who can provide satisfactory postsurgical care that the patients can take advantage of. That submission is not patronising or racist. This is also in the context of the applicant’s description that the technology was in its infancy.
1341 As evident from the above I am satisfied that the circumstances in which the risks and complications were conveyed Ms Eang and Mr Pril were inadequate to ensure a proper understanding of what they were agreeing to. There is no evidence to suggest that steps were taken by the applicant to ensure appropriate post-operative care given the nature of the surgery, and the risks and complications associated with it, as well as it being in its infancy (noting this was in 2015). There appears to have been no system put in place to ensure that the patients were monitored, and that aftercare was adequately provided.
Section 6 — Domestic patients: upper limb osseointegration
Mr Shane Mortimer
1342 Mr Mortimer who lives in Western Australia, became an upper-left humerus amputee when he was 13 years old, after being in an accident. He had surgery performed by Dr Al Muderis on 28 October 2015.
1343 Mr Mortimer presented as an honest, credible and generally reliable witness. The applicant accepted he was an honest witness.
1344 The applicant submitted that Mr Mortimer’s affidavit contained a lot of material that was directly inconsistent to what he agreed, during his cross-examination, had occurred. It was submitted that in those instances where his oral evidence is inconsistent with his affidavit, Mr Mortimer’s oral evidence should be preferred. The respondents submitted that the applicant’s submission that Mr Mortimer agreed with a lot of propositions put to him during cross-examination, ought to be treated with caution. The respondents submitted that questions were put to Mr Mortimer in a rapid fashion and so the Court cannot be confident he was in fact agreeing to matters that were inconsistent with his affidavit evidence in circumstances where those inconsistencies were not tested in cross-examination.
1345 I agree that caution is required. This is an example of the cross-examination I referred to earlier where I raised with counsel the manner of the questions asked, and that the answers given should not be assumed to be an acceptance of the proposition put (even if the answer was in the affirmative). This was apparent from watching the witness. Further, putting propositions as a fact, and implying (or stating) that the witness was being told what happened, can be problematic. This concern about his answers was raised by the respondents during Mr Mortimer’s cross-examination.
1346 In that context, the applicant did not challenge Mr Mortimer’s affidavit on the topics now said to be inconsistent with his oral evidence. There is no suggestion from Mr Mortimer that those matters are incorrect. Indeed, on the few occasions where aspects of his affidavit were challenged in cross-examination, Mr Mortimer maintained that they were correct.
Background
1347 Mr Mortimer, who resides 720 km from Perth in Western Australia, was introduced to the concept of osseointegration by his prosthetist, Andrew Vearing.
1348 His evidence was that prior to the operation with Dr Al Muderis, he was quite active and enjoyed fishing, kayaking and target rifle shooting. He also said he has a black belt in jiu jitsu. Mr Mortimer explained that he previously enjoyed full movement in his left arm and did not experience any pain, other than mild phantom pain which only occurred when he thought about it. He used a body-powered arm with a socket, harness, and mechanical locking elbow for 31 years. For much of this time, the arm had a cosmetic hand. He said that he got a myoelectric arm in about 2000 but stopped using it in about 2012.
Pre-surgery
1349 Mr Mortimer gave evidence that he attended Dr Al Muderis’ clinic in Perth on or around 15 November 2014 but did not want surgery straight away and wanted to think about it. From his perspective, the first consultation was finding out what it was about.
1350 Mr Mortimer said that during the clinic Dr Al Muderis explained the osseointegration procedure. He said he was told that he would have a custom-made implant inserted into his arm, that screws would be put in, but they would be removed after a period of time. He agreed that Dr Al Muderis explained the advantages and disadvantages of osseointegration as well as some of the general risks and complications of the procedure, being that he might get an infection, that the implant might have to be taken out and that there was a risk of death. Mr Mortimer said he was also emailed a document from Dr Al Muderis after the clinic, which explained the risks of the procedure.
1351 After the clinic, a consultation report dated 15 November 2014, and then an amended report was sent to Mr Mortimer’s GP. On Mr Mortimer’s evidence, the reports (which is in the standard form referred to in Consultation reports in Part 6, Section 1 above) are incorrect. They state that Mr Mortimer told Dr Al Muderis that his function level was declining. He was clear in evidence that he did not say that. Rather, he gave evidence that he attended the consultation with Dr Al Muderis because he wanted to improve and do more, not because his function was declining. I accept his evidence. I do not accept the applicant’s submission that Mr Mortimer’s evidence on this topic is inconsistent with his other evidence (for example, about the difficulties he was having with his socket prosthesis).
1352 Further, although the consultation report followed the general pro forma approach, this procedure related to Mr Mortimer’s upper-left arm. Despite that, the report, as was typical of the other reports, referred to the number of lower limb surgeries that had been performed and that in all cases, there was an increase in functionality:
[t]he functional benefits associated with the lower limb osseointegration in our opinion can be applied to the upper limb with increased effectiveness and safety as infection risk is lower. We expected that osseointegration will enable Shane to optimize his prosthetic use.
1353 Even if this was not the first upper limb procedure, it must have been one of the first. In that context, there was no proper basis to describe the procedure as “standard”. I note also that the report refers to Mr Mortimer having a relatively low risk of infection.
1354 It was many months after the first clinic before Mr Mortimer decided to have the surgery. He attended a couple of other clinics during that time, and tests were conducted. At the clinics, Mr Mortimer met patients with both positive and negative stories, although he said generally the patients he heard from were very happy following their operation. He was told the cost would be $30,000 but received a 5% discount for prepaying.
Surgery
1355 The surgery was performed on 28 October 2015.
1356 Mr Mortimer gave evidence that while he was in the prep room waiting to go into the theatre, Dr Al Muderis, or a member of his team, said that Dr Al Muderis would have to split his humerus to get the implant in. Mr Mortimer was confused because he had understood that the implant would be custom-made. He did not see the implant prior to the surgery. He gave evidence that if he had seen how big it was, he would not have proceeded with the surgery.
Post-operative
1357 Mr Mortimer’s evidence was that he felt immense pain in his arm following the operation. He said the pain became worse and worse and he remembered having pain the whole time in the immediate post-operative period. This is evident in text messages sent from Mr Mortimer to Dr Al Muderis in mid-November 2015 conveying the pain he was experiencing and discussing his pain management medication. It was put to him that the pain he experienced was at the distal end of his stump, with which he agreed.
1358 Mr Mortimer rejected the applicant’s suggestion put in cross-examination that he had not had horrific pain following the operation. He explained that the pain became worse with the metal sticking into him, but that he would have been in pain the whole time. I note, to state the obvious, that any purported pain measurements said to be recorded shortly after surgery or while still in hospital were taken at a time when the patient was being managed with medication.
1359 Apart from the pain, two issues in the immediate post-operative period should be mentioned. First, Mr Mortimer gave evidence that two physiotherapists came to see him in hospital on about 29 October 2015 and wanted to hang weights off his arm, to load the prosthesis. Mr Mortimer would not let them do so. Following this, Dr Al Muderis was spoken to, and Mr Mortimer was told there should not be any loading on the prosthesis and that he was to rest and go home. The loading procedure, which was to be followed by the physiotherapists, related to lower limbs. Second, Mr Mortimer gave evidence that he had expected to go to Mt Lawley Rehabilitation Centre after being in hospital (based on an email he had received from Ms Stewart), but it was apparent nobody had organised this. He had nowhere to go and could not drive 720 km from Perth to his home given the medication he was on. After staying in Sydney by himself for three days, Mr Mortimer gave evidence that he had to organise to stay with a friend in Perth and looked after himself.
1360 Mr Mortimer’s evidence understandably reflects that he struggled on his return to Perth, where he was looking after himself and attending to his own dressings. He got an infection. Mr Mortimer disagreed that the only infection he had was on this occasion in November 2015, explaining that he went to the emergency department, and was on and off antibiotics. Dr Al Muderis accepted that he knew Mr Mortimer had been on and off antibiotics over the two years following his surgery. This is consistent with what Mr Mortimer reported to The Alfred in Melbourne in 2017 as part of his history, as reflected in a letter from them to his GP (which is discussed below). Mr Mortimer said discharge would come out of the wound when he moved his arm.
1361 Mr Mortimer also gave evidence which makes it clear that he struggled with pain after his release from the hospital following surgery. He said that the pain he experienced when he was first released was an eight out of ten, and that losing his arm was less painful than the procedure. He went back to the hospital within two to three days because of the pain. When the pain from the operation had stopped, he still had (sharp) pain from the implant. He rejected the applicant’s suggestion that the pain first arose in June 2016, saying it was an ongoing problem.
The Alfred
1362 It is appropriate at this stage to jump ahead to October 2017 when Mr Mortimer first consulted with the osseointegration team at The Alfred. That is because it provides a context against which the events leading up to this point in time can be addressed.
1363 The results of tests conducted by The Alfred in October 2017 were consistent with findings of chronic osteomyelitis with associated soft tissue infection. A letter from The Alfred team to Mr Mortimer’s GP, signed by Dr Bruscino-Raiola, also records that the CT scan they undertook showed that Mr Mortimer’s implant had breached the head of the humerus, into the shoulder joint, causing his pain and decreased range of movement. The Alfred advised Mr Mortimer to return to see Dr Al Muderis as a matter of urgency, as it was his unique system which was implanted and Dr Al Muderis’ team was in the best position to deal with the problem.
1364 Mr Mortimer returned to see Dr Al Muderis. In the consultation report dated 31 October 2017, Dr Al Muderis stated, amongst other things, that “[f]or Shane we feel as though he is actually doing quite well with his implant”. The report went on to state that “[w]e do not feel as though he has a deep infection however we cannot fully rule this out” and advised that they wanted to take a bone sample for testing, which they did on 1 November 2017. Mr Mortimer gave evidence that following this procedure, he was told by Dr Miriam Paul, a microbiologist, that he had “osteomyelitis and a couple of other infections, and [he would] need to have the implant removed within the year”. The hospital clinical notes record that Dr Paul saw Mr Mortimer, and although osteomyelitis was not recorded in the notes, it states that Mr Mortimer “was informed about the infection and the possibility of removing the implant”, and that he was upset. Mr Mortimer gave evidence that he told Dr Al Muderis of the osteomyelitis and that Dr Al Muderis questioned who had told him that. Mr Mortimer said that the following day, Dr Al Muderis acknowledged that he had osteomyelitis, and that the implant would need to be removed (although I note that Dr Al Muderis denied in evidence that Mr Mortimer had chronic osteomyelitis as at 8 November 2017). Mr Mortimer decided to have his implant removed at that stage. The implant was removed on 8 November 2017. I note the operation report states in its operative findings that there were “no obvious signs of osteomyelitis”. Antibiotics were then administered to Mr Mortimer through a peripherally inserted central catheter (PICC) line for about four weeks, followed by oral antibiotics for about another two months.
1365 Mr Mortimer gave evidence that following the removal of his implant, his arm felt much better, and the pain was gone. However, as Mr Mortimer explained, his stump is now much shorter than before the original operation. There is a dispute in the evidence as to how much shorter. Dr Al Muderis’ evidence was that it was approximately 2.5 cm shorter. However, Dr Stalley opined that Dr Al Muderis’ measurement was incorrect, because it failed to have regard to the different points of measurement in the CT scans. Dr Stalley said the correct calculation is that the stump is over 6 cm shorter. I prefer the evidence of Dr Stalley, and his explanation for the difference in measurements. Although Mr Mortimer referred to the loss as between 8 and 10 cm, Dr Stalley’s evidence accords with his evidence that the stump is significantly shorter.
1366 Mr Mortimer described that a few weeks later, Dr Al Muderis called him and asked him to have scans done to explore having another osseointegration surgery, saying: “If you have the operation, I will treat you like you are my only patient”. Mr Mortimer gave evidence that he considered it a strange thing to say because he expected Dr Al Muderis would have treated him like that the first time. He declined to explore another surgery with Dr Al Muderis.
1367 On 12 November 2019, Mr Mortimer wrote to Dr Al Muderis requesting a refund. The complaints made by him in that letter are consistent with his evidence.
1368 I will return to the request for a refund below, as well as the issue of whether the implant breached the head of the humerus.
Events following Mr Mortimer’s initial surgery
1369 As the respondents alleged that, inter alia, Dr Al Muderis was negligent in the performance of Mr Mortimer’s surgery and that he ignored complications, it is necessary to consider the events following Mr Mortimer’s initial surgery in more detail.
1370 Dr Al Muderis denied that he ignored Mr Mortimer’s post-operative complications. The applicant submitted that Mr Mortimer was followed up at regular intervals after his initial surgery and that his complaints were attended to promptly. He submitted that in cross-examination, Mr Mortimer repeatedly described Dr Al Muderis’ team as “good” and responsive. It was submitted that the evidence suggests (and because Mr Mortimer did not say otherwise in cross-examination) that until Mr Mortimer consulted the team at The Alfred, he was happy with his experience.
1371 It can readily be inferred that Mr Mortimer attended The Alfred because he was frustrated with what had occurred up until that point of time. This can be inferred from the fact of attending The Alfred in the circumstances Mr Mortimer describes. It is also confirmed by the information Mr Mortimer provided to The Alfred. At that time, he told The Alfred he had just finished his course of antibiotics. He described the pain being very distressing, and that the skin was shedding like a bad sunburn. He described:
The pain has been about 7/10 at times, but is fine if I don’t move my arm, and the ooze was literally running out on the Monday the 16 October, yellow with blood in it.
1372 Dr Al Muderis’ evidence – that he did not agree that Mr Mortimer going to obtain a second opinion at the Alfred meant dissatisfaction with his services, but that “the pure reason for a second opinion is to give an opinion” – fails to address Mr Mortimer’s evidence of why he attended there, as reflected in the contemporaneous reports.
1373 It may be accepted that after his surgery there was some contact between Mr Mortimer and Dr Al Muderis or his staff, and that Mr Mortimer kept them updated. However, the fact of contact does not, by itself, necessarily address the issue of proper aftercare. Although it may be accepted that communications from Mr Mortimer had generally been responded to, they were not responsive in addressing his ongoing issues.
1374 I have already referred generally to the position of Mr Mortimer after his initial release from hospital post-surgery. There are other aspects that are appropriate to refer to.
1375 There was a consultation with Dr Al Muderis on 11 March 2016, with the report stating that Mr Mortimer’s wound had healed nicely, that he had no infection, and that a new x-ray showed good alignment and healing. It stated that Mr Mortimer had no pain and was functioning reasonably well. In cross-examination Mr Mortimer said he thought he had mentioned the pain from the implant rubbing against him, and that he had no pain from the operation. I do not agree with the applicant’s submission that Mr Mortimer agreed with the substance of the report. As to the accuracy of the report, I note that immediately after the passage referred to, the report states that Mr Mortimer was able to complete the six-minute walk test with pleasing results, a test which appears to have no apparent relevance to upper limb patients. In this same passage, the report states that Mr Mortimer completed the “QTFA” questionnaire, an initialism short for Questionnaire for persons with a Transfemoral Amputation, which again is relevant to lower limb patients which has no apparent relevance to Mr Mortimer as an upper-left humerus amputee. It will be recalled that the reliability of Dr Al Muderis’ consultation reports has been addressed above: see Part 6, Section 1.
1376 Mr Mortimer said that in the years following the operation, he told Dr Al Muderis several times that there was a sharp bit in his arm which he wanted fixed.
1377 Mr Mortimer gave evidence that on 28 June 2016, he attended a Skype meeting with Dr Al Muderis and Ms Bosley. This was arranged after Mr Mortimer had been complaining about a sharp and rough edge cutting into him. These complaints are evident in text messages sent to Dr Al Muderis (and Ms Bosley) on 18 May 2016, referring to a lot of pain (including on the skin) and blood coming out, and again on 21 June 2016, referring to the sharp and rough edge, burning pain, and blood. They are also evident from his written communications with Mr Vearing which support Mr Mortimer’s evidence of his concerns. It had been an ongoing, persistent problem, and he was experiencing pain, described sometimes as a ten out of ten. As he wrote to Mr Vearing, “the pain I have been in has been unbearable”. Mr Mortimer gave evidence, supported by written communications, that he had tried various things to ease the pain, including putting cotton wool on the rim and spending “many a night and day with [his] arm in [a] cold bucket of water”.
1378 In the meeting on 28 June 2016, Mr Mortimer said that Dr Al Muderis told him that he could not resort to any surgical intervention within the first 12 months of having the implant in. His evidence was that Dr Al Muderis did not listen to his concerns, in the sense that he did not believe him. This is illustrated by what Mr Mortimer said Dr Al Muderis told him: “the pain is from the surgery, not the implant. Leave it a year and we will see where we go from there”. Following the meeting, Mr Mortimer suggested in an email to Ms Bosley about using an O-ring, that is, a rubber ring to go over the sharp edge complained of, but when he tried and failed to make one himself, he ended up continuing to pack the rim with cotton wool instead. Shortly after the meeting that night, Mr Mortimer sent an email with a summary of the meeting to Dr Al Muderis (and Ms Bosley) and forwarded a copy to Mr Vearing.
1379 The email to Dr Al Muderis and Ms Bosley states:
Thanks for your time tonight. I will try the vasoline cream as recommended by Professor Munjed al Munderis as it might help slightly, but it not just chaffing me but cutting me. After our talk without that padding it started cutting into my arm already.
This seems like the wrong implant, with that rim cutting into me seems that it should have been a smooth cone, or as if it came out 15mm more as discussed.
Waiting a few months I would say will be impossible, as the pain is not good.
I hope you can come up with a solution, if you do I will fly over. grinding to a cone or the edges right back is the only solution I can see.
1380 I accept the respondents’ submission that the email reflects that Mr Mortimer knew: that Vaseline was not a solution; that at the time of their call, the implant was already cutting into his arm; that it seemed to him that Dr Al Muderis had inserted the wrong implant; and that he could not manage another few months because of the pain. The urgency of Mr Mortimer’s circumstances is evident in the fact that he said he would fly over to Sydney as soon as Dr Al Muderis came up with a solution. Dr Al Muderis’ evidence in cross-examination was that he did not recall seeing the email, and claimed aspects of it were not factual. I accept the evidence of Mr Mortimer which is supported by contemporaneous documents.
1381 In forwarding this email to Mr Vearing, Mr Mortimer wrote:
Hi Andrew, here is an email of after my appointment of what we discussed, to keep you informed.
The outcome.
The implant has a sharpish concave rim. Is not removable but part of the implant. (why did they put that part is doing in my arm? )
The implant is made of titanium (google, hardest metal known to man)
Munjred will think of an solution. ‘grinding may damage my implant’. (It will not be able to be grind that I know of)
Munjred does not want to touch my arm until 12 months. It is now 8 months
I have been thinking of putting an o’ring to get rid of the edge.
1382 Several months after the Skype call, on 15 and 17 November 2016, Mr Mortimer emailed Mr Vearing about ongoing issues he had in relation to pain, noting his arm was “too sore to do anything” and a “sharp edge cutting” him. On 23 November 2016, Mr Mortimer sent a text message to Dr Al Muderis complaining about the sharp rim and rough shaft, requesting for it to be ground down as it had been 13 months since he had the implant. On 25 November 2016, Mr Mortimer left a message with Dr Al Muderis’ office attempting to contact him as he was having issues with “sharp bits and pain” which was causing him grief in his arm. After the message was passed on, Dr Al Muderis confirmed in a reply email that he had spoken to Mr Mortimer. On 12 January 2017, Mr Mortimer texted Dr Al Muderis that something had to be done about the pain. When Mr Mortimer failed to receive a reply, he sent a follow-up email to Ms Stewart on 20 January 2017, stating that the sharp edges in his implant caused him a lot of pain for a period of nearly 15 months, urging Dr Al Muderis’ office to contact him. Throughout this time, Mr Mortimer had oozing and discharge from his stoma as well as regression of his skin.
1383 I accept the respondents’ submission that the evidence establishes Dr Al Muderis was aware no later than by mid-June 2016 that Mr Mortimer was experiencing persistent problems with the implant, significant pain in his arm and thought there was a sharp protrusion or rough edges causing the pain. No solution was forthcoming from Dr Al Muderis. Mr Mortimer was left to cope and come up with his own solutions to ease the pain. Despite repeatedly reaching out for help and a solution, the only one proffered was Vaseline which, given the complaint, would never have been sufficient.
1384 Dr Al Muderis’ original affidavit evidence that he did not know about Mr Mortimer’s concerns until 25 November 2016 is, as Dr Al Muderis eventually conceded in cross-examination, plainly incorrect. Where there is any difference with Dr Al Muderis’ account of the dates regarding when Mr Mortimer first raised the complaints of pain, Mr Mortimer’s account is to be preferred. It is supported by contemporaneous documentary evidence.
1385 Dr Al Muderis saw Mr Mortimer on 25 February 2017. The consultation report noted that Mr Mortimer was struggling with his mobility in the shoulder. It said this was because the scarring was rubbing against the implant, that the tissue had shrunk dramatically over the time since the surgery such that the edge of the implant was rubbing against the inner side of his armpit, and he had lost some of his shoulder movement. The report also stated that there was some discharge, it did not appear to be an infection, but there was tenderness around the anterior and medial aspect of Mr Mortimer’s arm. The experiences relating to the rubbing of the implant and loss of movement were long standing complaints raised by Mr Mortimer, which had not been addressed. The report highlighted matters Mr Mortimer had been complaining about for months.
1386 Before this consultation, on 23 February 2017, a CT scan was undertaken, although this is not referred to at all in the consultation report. This is the scan which is said to show the breached humerus head, to which I will return.
1387 Mr Mortimer gave evidence that in one of his consultations in Perth (which appears to be the 25 February 2017 consultation) with Dr Al Muderis (in which Mr Vearing, Ms Bosley and other patients were present), he asked why he could no longer lift his arm up. His evidence was that Dr Al Muderis said “I am not a shoulder expert”. This was denied by Dr Al Muderis. Although Dr Al Muderis accepted in cross-examination that during the 25 February 2017 consultation, Mr Mortimer asked why he could not lift his arm, he said he had explained to him that it was due to the tethering of the distal end of the implant by Mr Mortimer’s soft tissue, which had scarred significantly. When Mr Mortimer was challenged in cross-examination, he was adamant this interaction occurred and explained that at the time there was an x-ray on the wall which obviously indicated that his implant had punctured through his shoulder, but nobody said anything. Mr Mortimer said that he and Mr Vearing talk about the incident often.
1388 I accept that Mr Mortimer’s question about being unable to raise his arm was asked because he could not do so, he did not know why and wanted an explanation. Mr Mortimer’s evidence – that Dr Al Muderis replied that he was not a “shoulder expert” – has a ring of truth. As explained earlier, statements to the same effect were repeatedly made by Dr Al Muderis during his cross-examination in a context where he was questioned as to why he had not done certain things. As described above, he used this technique to avoid answering questions: see [289] above (e.g. “not a pain specialist”, “not a prosthetist”, “not a psychologist”, “not a radiologist”, “not a lawyer”, “not a physician” etc). I accept Mr Mortimer’s evidence on this topic. Although Dr Al Muderis may have said at some stage during a consultation that tethering inhibited Mr Mortimer’s shoulder movement, this does not mean this statement was not said.
1389 Mr Mortimer did not agree that tethering was the problem in relation to lifting his arm. He rejected the cross-examiner’s assertion that it was the pain from the stump that was inhibiting his range of movement. Mr Mortimer said that after the operation, there were certain spots in which he could not lift his arm more than 45 degrees (but others he could). His evidence was that following his first and second operations with Dr Al Muderis, his shoulder movement had decreased. Mr Mortimer demonstrated the limitation to his shoulder movement in Court and in re-examination he identified a photo which shows the movement or limitation he described. Mr Mortimer gave evidence that this photo reflected his movement at the time he was corresponding with Dr Al Muderis in June 2016. There is no evidence as to when the photograph was taken. The photo also shows the packing Mr Mortimer had placed around the stoma, and what he described as the purulent “pussy stuff”, which looked “disgusting”.
1390 Dr Al Muderis accepted that in the February 2017 consultation, Mr Mortimer was complaining of pain and that there was discharge from the stoma. However, Dr Al Muderis said he did not test for infection in Mr Mortimer’s arm because Mr Mortimer did not complain of symptoms of infections. Dr Al Muderis disagreed with the proposition put to him in cross-examination that he did not investigate whether an infection was present, although when asked what actions he took, he could not recall, but stated he conducted a clinical examination and there were no signs of infection. I note that discharge and oozing from the stoma may be indicative of infection.
1391 Following Dr Al Muderis’ recommendation, Mr Mortimer said that he had his second procedure on 13 March 2017, to refashion the stoma and change the dual cone to a shorter one. His evidence was that Dr Al Muderis did not address the sharp edges sticking into the flesh of his arm during this procedure and that it continued to feel like serrated edges were rubbing against the inside of his stump. Mr Mortimer said that his pain had reduced significantly, immediately following this procedure.
1392 Mr Mortimer gave evidence that within a couple of months after the March 2017 operation, the stoma shrank over the gold plating and the pain returned. Mr Mortimer also gave evidence at that time that there was flesh hanging off his stump, there was almost always a lot of fluid coming out of the stump and the smell was putrid. During cross-examination, Mr Mortimer said all the tissue (not just the skin) had pulled back.
1393 Mr Mortimer’s evidence was that on 10 June 2017, he attended a clinic in Perth to consult with Dr Al Muderis. Mr Mortimer agreed Dr Al Muderis looked at his stump and said that his skin had regressed. The regression is also noted in the consultation report. Mr Mortimer said that he told Dr Al Muderis again that he had pain from the sharp edges of the implant rubbing inside his arm. He recalled saying he wanted all the sharpness to be ground off. He agreed Dr Al Muderis responded that he would not cut the end off because it would weaken the strength of the implant. He gave evidence that Dr Al Muderis said, “I can take the big implant out and put a little one in”. Mr Mortimer said he replied with words to the effect of: “I thought that was what I was getting to start with!” but explained that this was not a heated conversation. He also explained he did not want to take the implant out “after all the dramas”. He said he told Dr Al Muderis he would try to manage his symptoms with oregano oil and colloidal silver. Those interactions about the offer to remove the implant to replace it with a shorter one, and the reasons he declined, are reflected in the consultation report.
1394 The referral letter to The Alfred from Mr Mortimer’s GP, dated 10 October 2017, inter alia, expresses the referring doctor’s concern about osteomyelitis developing. The Alfred report is summarised above and is unnecessary to repeat.
1395 In the above context, where Mr Mortimer had been suffering pain, discharge, loss of movement, retraction of skin and had sought an opinion from The Alfred where the doctors expressed opinions that were dire (see [1363] above), it is difficult to understand how the statement (referred to above) recorded in Dr Al Muderis’ consultation report dated 31 October 2017 – “[f]or Shane we feel as though he is actually doing quite well with his implant” – could have genuinely been believed to be correct. This reflects an unwillingness by Dr Al Muderis to recognise the obvious.
1396 I have already referred to the consultation on 31 October 2017 above. There is one further aspect to address. At this consultation, Dr Al Muderis recommended more surgery, including using “a burr to smooth the distal aspect of the implant so as to make it more tolerable for the soft tissues surrounding it”, which was undertaken on 1 November 2017 (a week before the implant was removed). The respondents submitted that the consent form signed by Mr Mortimer for this procedure did not reflect what was done, a matter denied by Dr Al Muderis. That submission is correct. Mr Mortimer’s evidence was that when the edge was smoothed, it felt as it always should have, and that the pain he was experiencing was gone. That was what Mr Mortimer had been asking for since 28 June 2016. Notwithstanding the fact that Dr Al Muderis said he could not resort to a surgical solution within the first 12 months of inserting Mr Mortimer’s implant, there is no evidence from Dr Al Muderis as to why such a solution could not have been done at a much earlier time after the 12 months had passed in November 2016. In any event, I note that there is no evidence from Dr Al Muderis as to why a non-surgical solution (other than Vaseline) could not have been suggested earlier, as opposed to leaving Mr Mortimer to suffer, and to proffer his own.
1397 As previously discussed, the implant was removed shortly thereafter, on 8 November 2017.
1398 It was suggested to Mr Mortimer in cross-examination that after he left hospital from these operations in November 2017, that he was feeling good. Mr Mortimer’s response is telling: “apart from not being able to use an arm, yes”.
Two further matters
1399 It is necessary to return to two matters.
1400 First, the issue of whether the implant inserted by Dr Al Muderis breached the head of the humerus. According to Dr Stalley, the CT scan images unequivocally show that the intramedullary nail had penetrated through the sub-chondral bone and into the shoulder joint. As Dr Stalley explained what, in his opinion, should have occurred:
Because of the severe pain that this man had at the time immediately post-operatively and with a plain x-ray showing the nail very close to the sub-chondral bone of the humeral head, it would have mandated in my practice a detailed three dimensional CT Scan to make sure the nail had not in fact penetrated through the sub-chondral bone and into the shoulder joint.
1401 As he further opined in evidence:
The subsequent fracture generated will release blood and blood products into the shoulder joint, producing what is called a hemarthrosis or a joint full of blood. That is the cause of this man’s acute pain in the post-operative period. The nail that has been placed up his humeral stump is too long for the amount of bone there and it has permeated through the humeral head and just entered the shoulder joint.
1402 Dr Tetsworth, who gave evidence in the applicant’s case, when shown the CT images from 23 February 2017 in cross-examination, conceded that the images showed the implant breached Mr Mortimer’s humeral head, albeit very reluctantly. In answering this, Dr Tetsworth conceded the implant “appears to” have pierced the subchondral surface, “[t]here may be that one edge of it on the far left there” and “possibly, one corner of it may have penetrated”. Then when asked whether he conceded that the images showed the implant penetrating through the subchondral bone and into the shoulder, Dr Tetsworth stated: “On one small portion of it. On that left side, it does”.
1403 Dr Al Muderis’ evidence when it was put to him that he missed the diagnosis of a breach of the humeral head, and shown the scan of 23 February 2017, replied:
I say, no, that this is not – it’s not clinically relevant. The patient did not have any issues with his shoulder. The patient has restriction of range of movement of the shoulder because of the tethering of the tissue at the distal end of the stump. When we treat a patient with a humerus fracture, one of the methods of treatment is inserting an intramedullary nail. The intramedullary nail is inserted through the shoulder joint, and usually, the intramedullary nail have to breach the shoulder joint. That is a standard treatment. Hypothetically, even if this shoulder joint is breached, it’s no – any different to a treatment of an intramedullary nail that is inserted for the treatment of a humerus fracture. So it’s a standard treatment. Then an intramedullary nail for treatment of – for a humerus fracture, which should not be allowed if that would be having any clinical consequences, so I disagree with your argument…It’s a standard of care that a humeral nail can be sitting where this nail is sitting, even if you suggest that there is a breach of the subchondral surface, but I disagree with that.
1404 I note, as explained above, Mr Mortimer does not agree that the issue was tethering of the tissue, and he explained why (see [1389] above).
1405 Dr Al Muderis disagreed with Dr Bruscino-Raiola’s statement reporting the conclusions from The Alfred that there is a breach of the humeral head, adding that Dr Bruscino-Raiola is a plastic surgeon, not an orthopaedic surgeon, and he cannot comment on an implant in a humerus. Dr Al Muderis described Dr Bruscino-Raiola’s conclusion as an “inappropriate statement”. I note that The Alfred’s report is written in a manner as being a report from the team who did the assessments.
1406 The Alfred team also performed a gallium SPECT/CT scan. The findings were:
… compatible with active inflammation in the soft tissues posterior to the distal aspect of the humerus, likely infection. Gallium activity tracking up the humerus is suggestive of further inflammation/infection and the overall bone gallium scan findings suggest impartially treated/chronic osteomyelitis with associated soft tissue infection.
1407 Dr Al Muderis also rejected the conclusion that the bone scan showed a pattern consistent with infection, stating that a bone scan was a blunt tool.
1408 The respondents submitted that the Court should conclude that, in his evidence about The Alfred’s report, Dr Al Muderis was seriously dishonest and again denigrating of a medical professional without any proper basis. This was generally the approach taken by him in evidence when he disagreed with another doctor. It is one thing to disagree with an opinion expressed in a report, and quite another to assert a conclusion as inappropriate. There appeared no proper basis to do so.
1409 The applicant submitted that the radiologists’ reports for the scan of 23 February 2017 did not refer to any fracture and therefore there was no reasonable basis for him to have known there was an issue. However, as Dr Ruff explained (in relation to another patient), surgeons should look at the x-rays as they are a lot better at looking at them than a radiologist, and a radiologist will not necessarily identify an issue unless given the right information about what they are looking for.
1410 As referred to above, Dr Al Muderis was aware that Mr Mortimer could not raise his arm in certain angles, to certain degrees and this fact called for particular attention to be directed to determining the cause. The applicant’s submission that numerous radiologists did not report a breach of the humeral head does not relieve Dr Al Muderis of his responsibility to examine the scans, particularly given he knew of an issue with Mr Mortimer lifting his arm. Unlike the radiologists, he knew the issue. Dr Stalley gave evidence that Mr Mortimer’s inability to move his arm “was the classic presentation of an acute hemarthrosis in the shoulder joint”.
1411 As mentioned above, the scan of 23 February 2017 is not referred to in the consultation report for the consultation on 25 February 2017. Dr Al Muderis disagreed that if he reviewed it before seeing Mr Mortimer, he would have been gravely concerned. His evidence in cross-examination about the scan is referred to above at [1403]. Even if the matters he refers to were to be accepted, none of those answers address the issue that Mr Mortimer could not lift his arm. Further, I do not accept the submission that Mr Mortimer’s evidence conveyed that his pain was only ever at the distal end.
1412 I am satisfied that the implant did breach the humeral head, and that Dr Al Muderis would have seen this if he examined the scan he ordered (as he ought to have). The breach is apparent from the scan of 23 February 2017, as even Dr Tetsworth conceded. Dr Al Muderis’ unwillingness to acknowledge that in cross-examination, and minimising its significance, tells adversely against him.
1413 Second, as referred to above, in a letter to Dr Al Muderis dated 12 November 2019, Mr Mortimer sought a refund for the expenses he incurred. The letter is as follows:
Dear Dr Munjed Al Munderis,
In October 2015 I purchased your osseointegration titanium implant and dual cone products which I paid into your account $28,000.00. The wrong size implant and wrong size dual cone was inserted at Macquarie hospital 28 October 2015.
The product was supposed to be custom made to fit my undeveloped humorous as per your letters and consultations. Which is what I based my commitment to buy your product and go ahead with the procedure. I took two years to go ahead with all the risks that was advised. So, I am not sure why all the precautions were not taken and for the correct size products and aftercare treatment as was promised.
Outside the door of the theatre you told me my Humorous was to be split, under pre op medication.
I was shocked but put my faith in you and a large implant was inserted. In punching a hole through into my shoulder, which was quite clear to see in the x rays. The part of the implant that was supposed to be in my Humorous was far too long protruded into my flesh causing ulceration and severe pain for two years. The dual cone was too long, and a prosthesis cannot be fitted. I had to have a male thread adaptor made from a friend who is a fitter and turner so it could be fitted. I also had one made for Shek.
In February 2016 I asked for you to hone down the rough edges, also mention in an email 28/06/2016.
In March 2017 you refashioned my stoma, I was horrified when you took the dressing off. You also inserted a shorter dual cone.
My arm retracted back in months to hardly anything left, contacting you several times.
I had a second opinion who told me to get over there as quick as possible. After one week of scans and test said it was diagnosed as osteomyelitis and the implant needed to be removed.
The following week It was eventually confirmed of osteomyelitis in Sydney by Dr Paul and the prosthesis had to be remove.
Dr Paul changed my antibiotic. I had another operation to remove the implant and dual cone, which I have not seen again.
Pick line was inserted on 10/11/2017, for about a month and 5 tablets a day for another 2 months.
All up I have spent over $50,000.00 on scans flying to Sydney, accommodation, Medicare and HBF gaps, medication and anthesis and had four operations.
This is a request for a refund of the oversized implant that that really has destroyed my life, for the sum of $28,000.00 and if possible, the $50,000.00 of oval of my costs.
All chance of further osteointegration is lost, due to the 80mm loss (most) of my Humorous. And any chance of lengthening procedure with the humorous is too badly damaged.
I have most of my shoulder movement use back but not all.
I think you are decent person and on a business and medical aspects you agree on the above, as you have mentioned before in previous discussions.
I look forward to your response and think you will find this is a fair and not unreasonable request.
Regards Shane.
Shane Mortimer
1414 There was no response from Dr Al Muderis.
1415 As already explained, after the implant was removed, Mr Mortimer’s stump was significantly shorter than it had been before he had osseointegration. He said that this outcome has significantly impacted his life. As he explained, and as Dr Stalley reiterated, the longer the stump the more leverage he has. Although Mr Mortimer still wears a prosthesis, it is difficult to use. He cannot do activities he enjoyed before, including kayaking, fishing and target rifle shooting. As Mr Mortimer cannot hold the rifle up with his prosthesis, he has started F-class shooting, where he can shoot while his rifle is placed on a stand. Before the operation, he was a good runner and played soccer but now it is very difficult for him to run because his prosthesis will not stay on while he runs, and running with only one arm is too hard.
1416 The applicant took issue with the reported consequences of the operations on Mr Mortimer’s life, and the respondents’ submission about their impact on him. Dr Al Muderis, in effect, said that Mr Mortimer did not need to be in that position, because he had not been given the opportunity to complete a revision surgery (as he had done with other patients, for example, Mr Mailler). He submitted that a loss of the implant is a known complication and therefore not his fault. Financial considerations aside, it is entirely understandable that Mr Mortimer may not want another surgery. Holding this opinion does not lessen the impact the osseointegration clearly had on him. The applicant’s submission fails to acknowledge the conduct (or lack of care) that Mr Mortimer endured and reflects a lack of understanding of the impact these medical events had on him. I accept that it reflects a rather callous approach to the position Mr Mortimer finds himself in.
1417 As apparent from the above I am satisfied that Dr Al Muderis breached Mr Mortimer’s humeral head in inserting the implant, and that his aftercare was inadequate. I am satisfied in the circumstances that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Mr Shannon Haskett
1418 Mr Haskett suffered a motorcycle accident in Darwin on 26 May 2004, resulting in the amputation of both of his left limbs. His leg was amputated above the knee and the stump of his left arm was approximately 15 cm long. He underwent osseointegration surgery in relation to his left arm with Dr Al Muderis in September 2018.
1419 Mr Haskett was an honest, credible and generally reliable witness. By the end of cross-examination, as he said, he was getting flustered by dates being put to him. That was apparent from the manner he responded and was reflective of the subject matter of the cross-examination at the time. In my view this does not affect the general reliability of his evidence.
1420 The applicant submitted that it became clear during cross-examination that Mr Haskett’s recollection of events was limited, which casts doubt as to the reliability of his evidence-in-chief. That was not the import of his evidence, considered as a whole. While any assessment of Mr Haskett’s credit is necessarily in the context of his cross-examination, it does not follow from his evidence in cross-examination, that his recollection in chief of events is in doubt. That said, as always, care should be exercised when assessing his evidence as its reliability may vary.
Background
1421 In January and April 2013, Mr Haskett successfully underwent two-stage osseointegration surgery in his left leg with Dr Richard Beaver in Perth. In June 2017, he experienced a mechanical issue with his leg prosthesis that Dr Beaver and his prosthetist, Mr Brendan Cahill, were unable to fix. At that time, Dr Beaver and Mr Cahill told Mr Haskett that Dr Al Muderis was visiting Perth and holding a clinic at their rooms and that he may be able to help. On 10 June 2017, Mr Haskett met Dr Al Muderis. Dr Al Muderis used an electric tool to grind the seized part of Mr Haskett’s prosthesis to resolve the issue.
1422 Mr Haskett’s evidence was that Dr Al Muderis subsequently asked him why he did not have a prosthetic arm, and he explained the difficulties he was having with a suction prosthetic. Mr Haskett said Dr Al Muderis asked whether the Department of Veterans’ Affairs was covering his medical expenses, and he explained they were covered by an insurer. Mr Haskett said Dr Al Muderis then recommended that he undergo osseointegration on his arm and said words to the effect of: “I could have a robotic prothesis fitted which would connect with and be controlled by your nerves. You would have far greater functionality with an osseointegrated solution”. Dr Al Muderis showed him a video of young men with robotic arms. He told him he was “one of only three surgeons in the world who has done an osseointegration to the humerus and the only one in Australia”.
1423 There is a dispute about aspects of this conversation, much of which Dr Al Muderis could not recall in cross-examination. He denied that he recommended to Mr Haskett that he undergo osseointegration surgery on his arm but said they may have had a conversation about the topic. Mr Haskett’s version of the conversation has a ring of truth. It contains elements of things said and done by Dr Al Muderis consistent with his approach in relation to other patients.
1424 Mr Haskett gave evidence he approached Dr Al Muderis’ offices a few weeks later, and a consultation occurred on 14 April 2018. The report states:
Unfortunately due to challenges with his traditional socket prosthesis, Shannon has limited function of his left upper limb since his accident. In my opinion, he is underperforming for a young man his age and clinical condition. I believe it is reasonable and may become necessary that Shannon be offered surgical intervention as traditional methods have proven ineffective.
…
I believe that it is reasonable and may become necessary that Shannon be offered this surgery to improve his quality of life. Using this technology will benefit Shannon greatly and will negate the difficulties which he was experiencing using the socket prosthesis. Target muscle reinnervation will help power a myoelectric arm and maximise utilisation whilst osseointegration will be the closest option to reproduce the natural biomechanics of the arm through direct skeletal attachment.
1425 There was a further consultation on 28 July 2018, for which there is no consultation report in evidence.
1426 Dr Al Muderis performed TMR surgery on Mr Haskett on 31 August 2018, and osseointegration surgery on 7 September 2018.
1427 Mr Haskett was never provided with a suitable prosthesis for his arm. On 11 November 2021, his implant was removed.
1428 Mr Haskett said he told Dr Al Muderis that his hope was to have some functionality with an arm if osseointegration was possible, saying “that was the whole reason of getting it done”.
The risks and complications
1429 The consultation report for 14 April 2018 contains many pro forma statements including a list of risks. That is immediately followed by a reference to nearly 500 osseointegration cases his team has performed, claiming that functional capacity in all cases has increased dramatically. The issues with the accuracy of this are addressed elsewhere. Added to that I note that it does not address whether those cases are lower limb, or upper limb. Significantly, given Mr Haskett is an upper limb patient, the reference to nearly 500 cases all having dramatically increased functionality is in the face of Mr Mortimer’s case where he plainly did not. Mr Mortimer’s implant was removed in November 2017, before Mr Haskett’s first consultation.
1430 The report also states that, in that context, the complication rate has been extremely low. Infection is the only risk the report elaborates on, albeit in the usual pro forma manner: “Shannon does understand the risk of infection associated with this surgery, however we regard Shannon as relatively low risk. His procedure would be very standard”.
1431 Mr Haskett gave evidence he was not told about various risks and complications, including that:
there was a risk that I would suffer a severe infection with a putrid smell emanating from my arm that would be offensive for me to live with and which would make me reluctant to go out in public or to socialise with others.
1432 He rejected the suggestion that he remembered Dr Al Muderis explaining there were different types of infection or infections of varying severity. There is no suggestion that Dr Al Muderis ever spoke of the smell, which was an issue for several patients in these proceedings.
1433 Mr Haskett said that Dr Al Muderis “explained that there could be a risk of infection, but because of my age and my fitness, that it was a very, very, very slim chance of that actually occurring”.
1434 Mr Haskett gave evidence that Dr Al Muderis said words to the effect of: “These are some of the things that could go wrong, they haven’t gone wrong before. You’re a young, healthy guy, I don’t see it happening for you.” Asked if he remembered Dr Al Muderis talking to him about some of the risks of operations, Mr Haskett said:
he just gave me a quick glance over it, like, sort of, tell me there was risks but with my health being in my age and how fit I was and my health at the time, that those risks wouldn’t really impact me.
1435 Dr Al Muderis asserted he discussed with him beforehand that “he could die from the surgery. He could have severe infection … septicaemia … all sorts of serious adverse outcomes”. He otherwise accepted in cross-examination that the message that he left with Mr Haskett was that he was a relatively low risk patient, and the procedure he was to undergo was standard.
1436 Whatever risks he identified, statements of this nature downplay the risks involved, which was what was conveyed to Mr Haskett.
1437 I note also that this was not a group consultation as the report only identified Mr Vearing, Dr William Lu (a researcher) and Ms Roberts as present.
1438 There is no report for the consultation with Mr Haskett on 28 July 2018, which, given its proximity to the surgery, is an important consultation. Mr Haskett described this consultation as “short and abrupt”. Dr Al Muderis told him he had spoken to Mr Haskett’s insurer, and everything was ready to go.
1439 Mr Haskett gave evidence that he felt anxious about having the surgery, where it felt rushed. His experience in the lead up to having surgery in relation to his arm was different to what he had experienced prior to his surgery on his leg. In response to the proposition put in cross-examination that he knew he could ask questions before the surgery, he said that was “not – not how [he] felt at the time”. He said he:
remember[ed] thinking I couldn’t really back out of it now because my insurance company had paid – paid for everything. I had been flown over. I was in Sydney by myself in – in hospital, and I was, sort of, committed to getting it done.
The lack of a connector
1440 When Dr Al Muderis performed osseointegration surgery on Mr Haskett, he used a custom implant. Dr Al Muderis explained there was no standard implant that could fit Mr Haskett’s humerus at that time.
1441 The evidence reflects that Mr Haskett faced two issues in receiving the custom implant.
1442 First, the immediate problem for him after surgery was that there was no connector to connect any myoelectric arm to the custom implant, meaning he did not have a working arm following surgery. He was not told before surgery that he would be without a working arm following surgery.
1443 Second, as reflected in Dr Al Muderis’ explanation in examination-in-chief, the custom implant was equipped to connect to a new generation of myoelectric arm which was not yet available:
… the advantage [of the custom implant] … was – number 1, it was titanium, so it’s a newer generation [of] implant that’s more biocompatible and, the second, has perforations in the implant – holes in the implant – that is designed for an upper limb where it can allow … the possibility of transmitting the implantable electrodes for transmitting the signals into a myoelectric prosthesis. … I explored … that particular technology [with Mr Haskett], which was not available yet to us and still is not. But that … would be available for him if … that technology become available to us. But it’s not available to this day.
1444 The applicant submitted that this was a non-issue, as there were other myoelectric arms available for Mr Haskett.
1445 At times, witnesses and counsel appeared to conflate or confound these two issues such that, for example, one might mistakenly refer to the missing connector as a missing prosthesis. In any event, the essential point is that Dr Al Muderis had no prosthesis ready to attach to Mr Haskett’s implant following surgery: the new generation of prosthesis was unavailable, and no connector was available for his current prosthesis. Dr Al Muderis failed to tell Mr Haskett before he had surgery that there was no prosthesis ready to attach to his implant.
No prosthesis
1446 Mr Haskett only became aware of there being any issue with having a functioning arm when he spoke to Dr Al Muderis during rehabilitation at The Hills. On being informed by Dr Al Muderis that he would not be able to use a prosthetic arm in the manner Dr Al Muderis had described, Mr Haskett became upset and raised his voice at him. He described the conversation as “heated”. A nurse intervened to stop the conversation.
1447 Mr Haskett described the circumstances in which Dr Al Muderis visited him at The Hills. He explained that a nurse arranged for Dr Al Muderis to see her before she brought him to meet a gathering of patients that included Mr Haskett. Mr Haskett thought Dr Al Muderis appeared surprised to see the patients. He said that Dr Al Muderis talked to the group for about an hour, and the conversation he had with him was in the hallway after this gathering had finished. In so far as Mr Haskett’s evidence referred to conversations with other people, that evidence was limited to the circumstances in which he said the meeting with Dr Al Muderis occurred, and not to the truth of those other conversations. Dr Al Muderis denied the conversation with Mr Haskett at the Hills occurred.
1448 Mr Haskett’s mother, Ms Haskett, gave evidence of an occasion when he telephoned her from rehabilitation a few weeks following surgery in a distressed state, relaying that, after meeting with Dr Al Muderis, he learnt there was no connector to support a functioning arm. I accept that Ms Haskett was a credible and honest witness. Although there are some issues with the reliability of her evidence as it relates to the order of some other events, that does not, in my view, impinge on the reliability of her evidence on this topic. Her evidence supports Mr Haskett’s evidence of the fact of the conversation occurring in the manner he described. It is evidence of him referring to the conversation in a manner consistent with his evidence, contemporaneous with the event.
1449 Given the import of the conversation, and the impact on Mr Haskett, I accept his account of what occurred. This was a shocking event for him. Given the circumstances, a conversation on this topic would have been expected to have occurred. Mr Haskett rightly expected to have a functioning arm which, as he explained, “was the whole reason of” the procedure. He was defiant at any suggestion that the conversation did not occur.
1450 The consultation report of 14 April 2018, referred to above, does not refer to there being any delay between the surgery and access to a prosthesis. Indeed, the last sentence in the passage from the report recited at [1424] above, clearly implies the contrary.
1451 Nor was there any indication in Dr Al Muderis’ correspondence with others about Mr Haskett, that there would be some delay in him using the prosthetic arm as envisaged.
1452 As referred to above, Mr Haskett’s medical costs are covered by an insurer, and approval from the insurer was required for the procedure before it could be undertaken. To that end, Dr Al Muderis prepared a report to the insurer dated 13 June 2018 answering questions it had raised.
1453 In response to the expected timeframe for rehabilitation, Dr Al Muderis’ report stated:
Shannon will commence his rehabilitation day one following surgery; initially he will start his loading and distraction phase which will gradually prepare him over a number of weeks to be fitted with his prosthetic limb. I would anticipate that Shannon can be fitted as soon as four weeks post surgery. In terms of TMR rehabilitation, Shannon will complete intensive rehabilitation with a occupational therapist and his prosthetist and is expected to see signs of early signals four months following surgery and mature signals by 12 months.
(emphasis added)
1454 Dr Al Muderis gave evidence that the emphasised text referred to Mr Haskett using a loading prosthesis rather than a prosthetic limb. He denied the response conveyed to Mr Haskett that a prosthesis would be ready for him to use within four weeks following surgery. I agree with the respondents’ submission that Dr Al Muderis’ suggestion that he was referring to a “loading prosthesis” in the letter is implausible. There is nothing in the letter to suggest that it is to be read as he suggests.
1455 The applicant points to Dr Al Muderis’ evidence that he explained to Mr Haskett that “with upper limb, because it’s not a loading part, the rehabilitation can take much longer” and that “patients could not be fitted with the prosthesis for the first three months at a minimum, but that there were still patients who were being trialled and fitted for their prosthesis two years after surgery”. His evidence is inconsistent with his letter to the insurer.
1456 In the 13 June 2018 report, Dr Al Muderis also responded to questions from the insurer as to when Mr Haskett could return to work:
Depending on the type of work, Shannon can return to light office duties part time as soon as his wounds heal and staples are removed, I would anticipate 4-6 weeks post surgery.
1457 And in what capacity:
Office-work or study. He should commence with a graded return to work timeline, commencing light duties from 4-6 weeks. We will be following his progress post operative x-rays frequently to monitor the integration of his implant. I anticipate Shannon will be back to full work duties by six months following surgery.
1458 Six months following surgery, on 18 March 2019, Dr Al Muderis updated Mr Haskett’s insurer on his current capacity for any work and prognosis:
He would be suited to training for a desk job when his sites have reached maturity (I will review 12 months post surgery to determine). … I anticipate Shannon will develop the capacity to utilize a prosthetic limb and will achieve maximal functional capacity after two years from his surgery date.
1459 The difference between the correspondence as to what the expected progress is, is self-evident.
Infection
1460 An issue intersecting with the lack of prosthesis is infection.
1461 Mr Haskett gave evidence that between 2018 and 2020, he suffered repeated infections in his arm. He said he was alert to the risk of infection because it was dangerous for him. He recalled occasions where he went to his GP when he experienced symptoms. His GP would diagnose an infection, citing redness and a putrid smell, before giving him (what he was told were) antibiotics. He recalled going to his GP “quite a lot of times” in those circumstances. He deposed his stoma would also weep ooze, pus and fluid during this period. Mr Haskett described when he took the antibiotics his symptoms would improve but would flare up again when he stopped.
1462 The applicant complains that there is no objective evidence before the Court, in the form of contemporaneous medical records from any doctor, that Mr Haskett was ever diagnosed with an infection in his arm during this period.
1463 In the consultation report of 1 March 2019, Dr Al Muderis records that Mr Haskett:
mentioned to me that he had a couple of infections in the arm which was not painful but he felt gunky discharge coming out and it seems that it is natural secretions. I advised him to avoid antibiotics unless there is redness and pain and swelling as antibiotics may suppress his natural flora.
1464 In December 2019, Mr Cahill, Mr Haskett’s prosthetist, wrote to Dr Al Muderis, attaching photos of Mr Haskett’s stump:
Hi Munjed,
We are contacting you about concerns regarding fitting trans-humeral clients due to the lack of specific OI connector. The threaded end left can be used to attach a prosthesis using rudimentary prosthetic components however there are no safe guards built in to such a prosthesis to protect an implant in the case of an impact, and most importantly a torque impact. Without an appropriately designed and tested connector [we] are not willing to fit a [prosthesis]. We are very concerned with the risk of potential spiral fracture or shoulder injury in the case of a fall or when the amputee is anchored via the prosthesis such as riding a bike or where the prosthetic hand may be attached to a door handle.
Are there any plans in place to provide a Transhumeral connector in the near future?
…
Shannon getting frustrated with constant infections in arm, which end up with gunky bodily fluid blocking the ports in the abutment on his arm.
He has been regularly needing to take AB’s which clear the infection, however this comes back when he stops the AB treatment.
Shannon not understanding any advantage with this abutment and he would prefer a simpler setup without a reservoir for infected bodily fluid.
1465 There was no reply to that email. Mr Cahill followed up on 7 February 2020, resending the above email and adding:
Hi Munjed,
Just following up on the below email sent to you in December. We’d love your thoughts on this matter as Shannon is very keen to move ahead with having a prosthesis fitted but we are unable to do so without an appropriate connector[.]
1466 Again, there was no response.
1467 The effect of Dr Al Muderis’ evidence was that he did not recall receiving or having the emails brought to his attention. When the content of the email relating to the connector was put to him, he repeatedly asserted that it would have been sent to the manufacturing company as it was a componentry issue and not a medical matter. He insisted that was the case although the email’s contents were addressed to him. However, as reflected in further cross-examination, the email also raised medical matters. Although he accepted that he would want to know information relating to Mr Haskett’s infections, he also said he could not recall if he would want to know about Mr Haskett’s concerns regarding the abutment acting as a reservoir for infected bodily fluid. Dr Al Muderis’ responses were entirely unsatisfactory.
1468 On 3 March 2020, Mr Merlo, Mr Haskett’s stepfather, emailed Ms Roberts:
Dr. Munjed Al Muderis
I have been asked by Shannon Haskett who is my stepson to help with his ongoing medical condition.
It is my understanding that you have been advised of Shannon’s condition with images by way of two emails from Brendan Cahill.
We have yet to receive a response and are very concerned.
Shannon has ongoing continual infections and these infections are increasing exponentially in duration and severity.
We are concerned that if these infections are left to continued unabated then there is a real risk that the implant will need to be removed.
This will cause an increased disability to what Shannon had prior to the trans-humeral osseointegration due to the reduced stump length.
This will not be an outcome that we will accept.
We also have been informed that you will not allow a third party to replace the connector which in Brendan Cahill’s opinion is not suitable (and I have been advised is the cause of the infection via the perforations. We need clarity on this).
Can you please respond as to what is the best course of action as I believe the situation is now critical.
Regards
Aldo Merlo
1469 That email is entirely consistent with Mr Haskett’s evidence of what he said he was enduring at the time and his concerns. The applicant did not make any submissions about these emails or address his failure to respond to these email communications.
1470 Pausing there. Mr Haskett’s evidence was that he had made several calls to Dr Al Muderis between 2018 and 2020 but only spoke to him once and otherwise if he spoke to anyone it was Ms Roberts. That said, his evidence was that at one stage during this period he sent photos to Dr Al Muderis’ staff of his stump and was reassured that everything looked fine. Ms Haskett also gave evidence that on occasions she observed her son attempting to contact Dr Al Muderis or his office for help, with no response. That Dr Al Muderis did not respond on occasions can be accepted. By the time these emails were sent, Mr Haskett described being depressed and having difficulty leaving his couch.
1471 A response to the emails only occurred after the email of 3 March 2020 from Mr Haskett’s stepfather, with Ms Roberts contacting Mr Haskett and his mother. Mr Haskett then attended an appointment with Dr Al Muderis in Sydney on 19 March 2020 with his mother and stepfather. This was at a time when the state borders were about to close because of the onset of the Covid-19 pandemic. The level of concern Mr Haskett held about his condition is reflected by the fact that he and his family travelled in these circumstances.
1472 The consultation report of 19 March 2020, written on behalf of Dr Al Muderis, records that Mr Haskett:
complains of ongoing ooze and skin erythema which has been managed by his GP as periodic infections, and he gets monthly antibiotics for flares of this infection. There is no pain, however he does complain about the smell and discharge at these times.
1473 The report also records there is no evidence of acute infection at that time. Mr Haskett recalled white ooze and pus were seeping out of his arm and said that he and his parents raised their concerns about infection with Dr Al Muderis. He said Dr Al Muderis told him that he could not see any evidence of infection. Despite the circumstances surrounding his visit to Dr Al Muderis and his expressed concerns, Dr Al Muderis neither touched him, nor swabbed his stoma or ordered any blood tests during the consultation. Nevertheless, he told him there was no active infection.
1474 Mr Haskett deposed that when he asked Dr Al Muderis when his prosthesis would be ready, he said words to the effect of: “I am not an engineer, I have done my part with the two procedures. I will get you to see my engineer, he will tell you.” Dr Al Muderis did not recall this conversation. However, the phrase, “I am not an engineer”, is a statement of the same nature as the evidence Dr Al Muderis gave on occasions when challenged in cross-examination about why he had not done something. This evidence has a ring of truth in that context.
1475 Ms Haskett’s evidence as to her son’s state at the time of this consultation – that there was white ooze and pus, and he was sweating profusely – is consistent with Mr Haskett’s evidence. She described him as quite sick at the time, and that there was a putrid stench coming from his arm, so he would not go out in public. Ms Haskett also gave evidence that Dr Al Muderis said that “I am not an engineer”.
1476 While in Sydney, Dr Al Muderis sent Mr Haskett to see Mr Lu (a clinical researcher who works with Dr Al Muderis) about his prosthesis. However, Mr Lu had no designs to show Mr Haskett. Mr Lu sent an email the next day introducing the team who would “help Shannon get his upper limb prosthesis up and running.” The email referred to “the connector being manufactured here in Sydney and is estimated to be ready by next week”. Mr Haskett gave evidence that blueprints for a connector were eventually sent to his prosthetist, but they were not viable. No connector was ever supplied.
1477 Dr Al Muderis gave evidence that at the 19 March 2020 consultation he also offered that Mr Haskett see his prosthetist, which Mr Haskett adamantly denies. He said that was never discussed with him.
1478 Mr Haskett returned to Perth with no connector or solution.
Applicant’s submissions on no prosthesis and infection
1479 It is appropriate at this stage to address two of the applicant’s submissions.
1480 First, as referred to above, the applicant submitted that there is no objective evidence Mr Haskett was ever diagnosed with an infection in his arm starting in the six months following surgery, and otherwise no cogent evidence before the Court to enable it to find that he had any infection in his arm during this period.
1481 Given Mr Haskett’s evidence of the symptoms he suffered, that he attended his GP, and he was repeatedly prescribed what he understood to be antibiotics, it can be inferred that he suffered from what a doctor determined was an infection. The symptoms he described are consistent with an infection. It can also be inferred that Mr Haskett’s GP prescribed antibiotics on the basis he considered they were warranted, and that Dr Al Muderis was aware that antibiotics were being prescribed (Mr Haskett told him so). Mr Haskett gave evidence that when he took the drugs his symptoms settled, and when he stopped, they flared. There is no evidence of Dr Al Muderis taking his concerns seriously or responding to the emails where the depths of his fears of the potential consequences of continual infections were expressed.
1482 Second, the applicant submitted that there is no basis for the Court to conclude that Mr Haskett was unable to be fitted with a prosthesis at the time of Mr Cahill’s emails, rather his prosthetists simply refused to do so because of their own conceptions about the safety mechanism. He submitted that the evidence is that it was Dr Al Muderis’ expectation and understanding that Mr Haskett could be fitted with the prosthesis, and that it was safe to fit one, because the implant had an internal safety mechanism. The applicant’s submission relies on his evidence that the implant had an internal safety mechanism and therefore did not need an external safety mechanism.
1483 I do not accept that submission.
1484 As referred to above, the design specification for Mr Haskett’s custom implant is in evidence. It is accompanied by a letter addressed to Dr Al Muderis which lists several points to consider in proceeding with the use of the supplied components, including:
The proposed design has no safety mechanism associated with the connector system. This is considered acceptable given the assurances provided by yourself with respect to the safety mechanism incorporated into the external connectors available to you …
1485 This is the opposite of Dr Al Muderis’ evidence. It is consistent with the concerns Mr Cahill expressed in his emails.
1486 Dr Al Muderis’ signature on the design specification and accompanying letter approved the construction of the implant in that form, which he then used in Mr Haskett’s surgery. I accept that evidence. The concerns Mr Cahill expressed in his emails to Dr Al Muderis have a real and proper basis. It is not, as the applicant submitted, that the prosthetist merely declined to fit Mr Haskett with a prosthesis.
1487 The applicant submitted orally that Mr Mortimer had a myoelectric arm and therefore there were arms available. He submitted that the electrodes on that arm are external, and his plan was that eventually patients would be able to have internal electrodes, and he wanted to give Mr Haskett an implant that would be able to use those electrodes for when they were available.
1488 However, as the respondents submitted, Mr Haskett had a newer, custom-made implant, with perforations designed specifically for transmitting implantable electrodes for a myoelectric prosthesis. The implant is not the same as Mr Mortimer’s. As explained above, Mr Haskett’s implant did not have an internal safety mechanism. I note that on the letter sent to Dr Al Muderis, the designer (and manufacturer) made clear that he only considered that acceptable because of Dr Al Muderis’ assurances as to the safety mechanism in the external connector.
1489 As explained above, the March 2020 email from Mr Lu after seeing Mr Haskett in Sydney reflects there was no connector available at that time.
1490 Dr Al Muderis was informed before Mr Haskett’s surgery that this custom designed implant had no internal safety mechanism. There is no evidence that Dr Al Muderis did anything to ensure there was a connector with a safety mechanism ready for Mr Haskett to use with this implant after surgery. Rather, he claimed not to have responsibility as it was a componentry issue. I do not agree. To advise that a patient undergo surgery, and book them in for surgery, it must be incumbent on a surgeon to ensure that the componentry required to meet the objective of the surgery is available. This was a novel procedure, as is apparent from Dr Al Muderis’ explanation above. That is why Dr Al Muderis commissioned a custom-made implant. It can be inferred he knew what else was required for a prosthetic arm to be attached to the implant, as the design was signed off on. Separately, he was required to inform Mr Haskett that the technology for the use of the myoelectric arm as described to him did not yet exist.
1491 Dr Al Muderis was recommending this surgery. A patient who consents to surgery based on their surgeon’s advice is entitled to expect that the necessary components for the surgery to be of any use are available. If not, the patient would be expected to be told. There was no point in doing the surgery unless the componentry existed.
1492 Dr Al Muderis performed osseointegration surgery (and, to that end, TMR) on Mr Haskett in circumstances where the connector necessary to enable his implant to connect to a myoelectric arm did not exist. As the respondents submitted, he performed surgery in circumstances where he never bothered to explain to Mr Haskett that the prospect of that occurring was entirely hypothetical and might occur at some unstated future date; he then washed his hands of all responsibility.
Return to Western Australia
1493 On 19 March 2020, Dr Al Muderis referred Mr Haskett to Dr Richard Carey-Smith to care for him in Perth. Dr Beaver (his surgeon who conducted his leg osseointegration) had retired and, because of the expected pandemic restrictions, Mr Haskett wanted a local doctor. As at that time, there is no evidence to suggest that there was any issue with his osseointegration implant in his femur. To the contrary, it appears from the evidence that Mr Haskett functioned well with that implant.
1494 The applicant submitted that the initial reports of Dr Carey-Smith focus on Mr Haskett’s leg and contradict Mr Haskett’s evidence that he was complaining about his arm. Mr Haskett denies that. It appears highly unlikely given the circumstances that preceded Dr Carey-Smith’s involvement that Mr Haskett would not have said anything about the issues in relation to his arm. His evidence was those circumstances remained. The submission creates a false dichotomy, as Mr Haskett explained:
We were also discussing the arm in the meetings that I would see him. But because I wasn’t using the arm implant at the time – well, at all, ever – and I was using the leg every day … we were just focusing and concentrating on the leg.
1495 On 3 May 2021, Dr Carey-Smith reported to Mr Haskett’s GP, copying Dr Al Muderis, that his leg implant would be removed because of an infected osseointegration stem with increasing pain. On 29 October 2021, Dr Carey-Smith recorded it was apparent Mr Haskett’s humeral osseointegration stem was infected, with an offensive odour, and it was to be removed.
1496 Dr Al Muderis gave evidence that he understood that Mr Haskett had his humeral implant removed as a result of a deterioration in Mr Haskett’s psychological state. That ignores the fact of the infection. Dr Casey-Smith, in his 29 October 2021 report to Mr Haskett’s GP, states that Mr Haskett “has never used his humeral osseointegration stem and is increasingly troubled by this and would like the stem removed.” That is, three years after he underwent Dr Al Muderis’ surgery, he still did not have the connector to use his arm. That impacted on his psychological wellbeing.
1497 The respondents submitted that the Court should accept the opinions of Dr Leung and Dr Stalley, that an infection in Mr Haskett’s arm was most likely the cause of the failure of the previously successful left above-knee osseointegration procedure, resulting in the removal of that implant. However, the evidence is not so clearcut.
1498 One of the assumptions the respondents provided to Professor Leung in relation to Mr Haskett was that the infections from his arm “gradually spread throughout his system and eventually his leg stoma also became infected”. Asked in cross-examination whether he assumed that proposition, Professor Leung replied:
I would say [it] is not an unreasonable assumption, [it] is one of those things you can never prove. … [it] is just timing and coincidence. I think one lead to another is an assumption, is not definitive.
1499 He subsequently explained the infection in Mr Haskett’s leg could be a secondary one from his arm.
1500 Dr Al Muderis’ evidence was this it was a “ridiculous” suggestion that an infection in his arm could spread to his legs and cause complications for his leg implant. In that context, he accepted that he did not warn Mr Haskett of such a complication.
1501 Dr Stalley’s opinion is more qualified than the respondents suggest. He expressly stated he does not have the bacteriology to prove whether a delay in the diagnosis in the infection of the arm led to a haematological spread of infection to the stump.
1502 Although I do not accept that the proposition is a ridiculous suggestion, it does not follow that the respondents have proved the conclusion they contended for. It is understandable why Mr Haskett and his family have the belief that the events are connected, given that there was no issue with his leg, but his arm was being treated for infections. However, proof of the connection is necessary to establish the respondents’ submission. It could be the cause, but there is insufficient evidence to establish that, on balance, that occurred. The opinions do not rise to the level the respondents submitted.
1503 That said, when Mr Haskett made the decision to have the implant removed from his arm, his arm was infected, and the symptoms he described existed. At that time, he had undergone surgery three years earlier for no purpose, as no suitable connector was ever provided. During those three years, Mr Haskett suffered in the manner described in his evidence. His evidence, and the impact it had on him, is supported by contemporaneous evidence, including documentary evidence.
1504 Mr Haskett gave evidence that following the humeral osseointegration with Dr Al Muderis and its subsequent reversal and stump revision, his arm stump is now significantly shorter.
1505 His arm stump had previously given him enough length to undertake some day-to-day tasks and recreational activities, such as cooking and pistol shooting. The shortening has reduced his functionality. Mr Haskett said Dr Al Muderis did not explain to him pre-operatively that his stump could be left shorter if the implant was removed.
1506 Dr Al Muderis gave evidence he did say that he could end up with a shorter stump if the implant had to be removed, but agreed he did not say that would result in reduced functionality and quality of life. He said he did not do so because Mr Haskett “did not have functionality of his arm”. However, Mr Haskett did have some functionality which was reduced.
1507 I am satisfied that Mr Haskett agreed to surgery in circumstances where, unbeknown to him, there was no suitable connector available to enable him to use a myoelectric arm, where the technology which he agreed to have implanted had not yet become (and is still not) available. Further, the risks and complications were downplayed. Accordingly, his consent was not an informed one. The problems that arose after surgery including the infections, smell, and lack of connector, significantly impacted Mr Haskett’s life. There was no connector, and limited (if any) assistance provided to address his problem (in circumstances where the documentation in relation to the custom-made implant made clear it had no safety mechanism). Most of his pleas for help were not responded to, and where they were, no real solution was proffered. His concerns were dismissed. I am also satisfied that, in the circumstances, Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Section 7 — Domestic patients: lower limb osseointegration
Mr Mark Urquhart
1508 Mr Urquhart suffered catastrophic injuries in 1992 and 1993 while working as a paratrooper in the Australian army. He had multiple operations to his knees, ankles, hips, legs, shoulders and back between 1993 and 1999 to address these injuries. He was also diagnosed with PTSD. In 1999, Mr Urquhart was provided with an implantable morphine pump that delivered pain relief straight to his spinal column. As a result of the operation to remove the pump in 2008, he became a T7 incomplete paraplegic, confined to using a wheelchair. Subsequently, he became an elite, highly accomplished disabled athlete. On 23 July 2016, Dr Al Muderis simultaneously performed bilateral above-knee amputations and single-stage transfemoral osseointegration surgery on Mr Urquhart. On 17 December 2020, Mr Urquhart terminated his relationship with Dr Al Muderis.
1509 The applicant submitted that Mr Urquhart was not a reliable witness, that his version of events is demonstrably wrong by reference to contemporaneous documentary evidence (stating that in some instances his chronology was wrong by as much as a year), he was a poor historian, and the Court should place little weight on his evidence, except in so far as it is corroborated. The contemporaneous documents referred to include statements in emails and texts, in the media and on social media. The import of the applicant’s submission was that Mr Urquhart was happy with Dr Al Muderis, until Covid-19 when he was stuck in Victoria and became increasingly depressed. It was only then that he went to another doctor and had complaints about Dr Al Muderis. The applicant also relied on the allegedly violent incident in 2023 between Mr Urquhart and Mr Smith, submitting Mr Urquhart’s version of those events is likely untrue, and therefore undermined his credit. As discussed elsewhere, I do not consider that incident to impact on the evidence of either witness.
1510 Mr Urquhart presented as a genuine, honest and credible witness. Although there are some issues with his evidence, particularly as to when certain events happened and reliability as to timing, he presented as a positive person who did not complain.
1511 His cross-examination was lengthy, at times in an aggressive manner, during which it was repeatedly put to him that he was lying. It was put to him that his quality of life only deteriorated after he stopped being Dr Al Muderis’ patient, and it was a result of his actions and those of Dr Huang. Mr Urquhart remained polite and respectful throughout, but the impact on him was evident. He appeared at times worn down. The respondents described Mr Urquhart as someone clearly suffering from PTSD, who just wanted to be out of the witness box and was prepared to not accede, but just say, “yes, ma’am; no, ma’am,” to question after question in the hope that it would end. That appears to be an apt description. He appeared to be stressed and described himself as such on multiple occasions:
Sorry, I’m just stressed and a bit – okay, and I’m trying to get my words right.
…
I’m so stressed sitting up here, ma’am. I don’t know, ma’am. I don’t know what to do because I was just here telling my story, that’s all, in amongst a whole bunch of other people, ma’am. I have nothing to do with this.
1512 These matters all factor into my assessment of his evidence. Although, as apparent from the discussion below, I regard Mr Urquhart mistaken at times as to certain events and their timing, I do not accept the applicant’s assertions that he gave knowingly false evidence.
1513 I have addressed elsewhere, the applicant’s reliance on the media and social media, to suggest that a witness’ evidence is not consistent with that conduct (see e.g. Ms Çalan’s case study above, and The patients in Part 6, Section 1). The applicant submitted Mr Urquhart’s explanations of painting a positive picture in the media and elsewhere is self-serving and untrue. Contrary to the applicant’s contention, it is entirely plausible that a person in Mr Urquhart’s position would present to the world the results of what he had chosen to do in the most positive light. He was walking, in circumstances where he was desperate to do so. He was obviously proud of his achievement. He saw himself as a success story. He proved he could walk, and in his words “the impossible”. That is, a positive picture can be painted despite, for example, suffering from pain or other issues. The two are not mutually exclusive. I accept his explanation for that. As a general concept, contrary to the applicant’s submission, I also accept that positive statements indicating Mr Urquhart’s support in texts and emails to Dr Al Muderis are not necessarily inconsistent with his evidence of what occurred. I will return to this below. Suffice to say at this stage, Mr Urquhart regarded Dr Al Muderis as a friend, to whom he was grateful. However, because of the circumstances he was experiencing, and had been for some considerable time, a stage was reached where he considered he needed a second opinion.
Pre-operative interaction with Dr Al Muderis
1514 Mr Urquhart, as revealed when first presenting to Dr Al Muderis, was an incomplete paraplegic who was wheelchair bound, with a history of depression and PTSD, back and joint pain, arthritis, chronic pain, and was on a cocktail of painkillers.
1515 There were three pre-operative consultations held on 1 October 2015, 2 June 2016 and 7 July 2016. There is no consultation report for 1 October 2015 in evidence, and no evidence of there being a consultation report for that occasion, despite Dr Al Muderis accepting in cross-examination that he had conducted an examination of Mr Urquhart at that first consultation. Unlike most other consultations where Dr Al Muderis relied on his reports to give evidence, he claimed that he remembered this consultation and the details of it, even though it extended (on his evidence) over two hours.
1516 As observed above, Mr Urquhart underwent simultaneous amputation and osseointegration surgery on 23 July 2016. That procedure was inconsistent with the statement on his own website, osseointegration.com.au, which stated regarding when osseointegration surgery can be performed after an amputation: “[t]he earliest has been 1 year after amputation”.
1517 There are several topics in the lead up to the surgery to be addressed.
1518 First, at the initial consultation on 1 October 2015, it was concluded that further testing needed to be undertaken. A decision was made to reassess Mr Urquhart in six to 12 months.
1519 Mr Urquhart also had a consultation with Dr Paterson on 1 October 2015, where he concluded that he was not a suitable candidate for osseointegration surgery. He opined that:
At the time of writing I do not believe he is a suitable candidate for the osseointegration procedure, and if he were to be considered he would need to be reviewed at length by rehabilitation specialists, ideally with experience in treating spinal cord injury, who felt that there was either signs of increasing hip flexor extensor strength and core strength in order to support his ability to walk. …
1520 He detailed the reasons behind that opinion, being: the unpredictable nature of a patient’s pain after such a procedure, particularly where there is a distinct possibility that surgical insult, especially in the context of Mr Urquhart’s hip flexor spasm, could make his pain worse; his previous issues with medication over-use; his history of PTSD and in the context of previous medical mishaps, the risk of anxiety attacks; his fervent beliefs as to a timeline to be standing; and his significant history of impulsivity related to his PTSD or high levels of function with his sporting activities, which may give rise to issues with pacing during the rehabilitation process if he were to be operated on, and potentially cause self-injury. The applicant relied on Mr Urquhart’s answers in cross-examination – that he did not recall Dr Paterson telling him each of those things – and submitted that should be taken as evidence of his unreliability. However, there is nothing in Dr Paterson’s report (which is addressed to Dr Al Muderis and copies in his team) to suggest he provided this information (or the substance of it) to Mr Urquhart. This is to be contrasted with the later report of Dr Paterson of 2 June 2016, which states there had been a detailed discussion with Mr Urquhart about various matters. The report was not provided to him at the time but was again addressed to Dr Al Muderis.
1521 Given that there is no record of Dr Al Muderis’ first consultation, it is unclear what was discussed about Dr Paterson’s report, if anything. On the evidence, it is also unclear whether Dr Paterson’s consultation preceded or followed Dr Al Muderis’.
1522 The report by Dr Al Muderis for the 2 June 2016 consultation, records that “Dr Andrew Paterson’s report was reviewed today” (presumably referring to the one dated 1 October 2015) and that there was a request by Dr Al Muderis for Mr Urquhart to be assessed that day by Dr Paterson “as to his current pain management issues”. I note that the issues raised by Dr Paterson in his original report addressed broader concerns. The other concerns are not referred to in this consultation report.
1523 In any event, as alluded to above, Dr Paterson further reviewed Mr Urquhart on 2 June 2016. Although Dr Paterson appears to have softened his view, it is apparent from the terms of the report that he still had significant reservations about Mr Urquhart undergoing osseointegration surgery. The report reflects that Dr Paterson was waiting for further reports and results. The report is also couched in terms of “if we were to proceed” and “if we were to consider surgery”. In that context, the report recommends, inter alia, that “consideration should be given to the role for a prehabilitative process pending his attending for the procedure namely, hip flexor, extension and gluteal strength”. I note that Dr Al Muderis’ evidence in cross-examination was that Dr Paterson’s report is “not a report saying that [Mr Urquhart] was not suitable”. As referred to earlier, when challenged, Dr Al Muderis said that Dr Paterson is a pain specialist, and his advice was about pain management, the implication being that his advice was not about patient suitability. He ultimately agreed the report expresses reservations, which on a plain reading of it, it does.
1524 The recommendation by Dr Paterson on 2 June 2016 is consistent with what he opined in the first consultation in the passage recited above at [1519] that “if he were to be considered he would need to be reviewed at length by rehabilitation specialists, ideally with experience in treating spinal cord injury”. Dr Al Muderis in cross-examination initially said he had no recollection of any such review having occurred, nor any recollection of having followed up to see if it had been done. There is no evidence before the Court that this was done. However, later when asked, he said that “Dr Pugh is the referring specialist and that is the rehabilitation specialist that – who has extensive rehabilitation with spine injury”. The only evidence in relation to Dr Kathryn Pugh is her referral letter to Dr Al Muderis of 22 September 2015, which does describe her as a rehabilitation physician. However, on 2 June 2016, Dr Paterson was still of the view that there should be consideration of the role of prehabilitation, from which it can be inferred, he did not consider it had been, or was being, undertaken. Dr Al Muderis’ answer recited above did not suggest that Dr Pugh had undertaken a review. The applicant submitted that it would be unsafe to conclude that Mr Urquhart was not reviewed by a rehabilitation physician in this period, especially when Mr Urquhart did not say otherwise in his evidence-in-chief and could not recall in cross-examination. However, there is no reference in any consultation report to having received (or reviewed) any report from a rehabilitation specialist, or that any request had been made to one, including Dr Pugh.
1525 Dr Al Muderis gave evidence that the view of the group at Mr Urquhart’s third consultation on 7 July 2016 was unanimous as to the procedure being offered to him. I note that is to be considered in the context of the discussion above about the approach taken in a multidisciplinary consultation by his clinic. Dr Paterson’s second report does not advise Mr Urquhart is a suitable candidate. On Dr Al Muderis’ evidence, Dr Paterson does not address patient suitability as he is giving pain management advice as a pain specialist. The problems with that approach have been addressed above: see Multidisciplinary approach in Part 6, Section 1.
1526 The applicant submitted in closing that having given evidence that the advice to Mr Urquhart was unanimous, the respondents could have issued a subpoena to Dr Paterson. This had not been done. As such, he submitted the Court would conclude that any concerns Dr Paterson had were resolved to his satisfaction before the decision to operate on Mr Urquhart was made. However, as previously explained, it would be expected in the circumstances that if Dr Paterson was to be called, it would be by the applicant. In the circumstances, I am not prepared to draw the inference sought. The concerns Dr Paterson raised are not referred to in Dr Al Muderis’ consultation reports.
1527 In any event, there is no evidence from Dr Al Muderis as to how the concerns expressed, and the steps Dr Paterson said should be undertaken were addressed (if at all).
1528 Second, the 2 June 2016 consultation report records Mr Urquhart’s goals from osseointegration as including to run at the Invictus Games. The report records that “[w]e have discussed with him that it is unknown as to whether or not by providing him with bilateral amputations that he would be able to run”. Nonetheless, to that end, as the respondents submitted, the report records two options which are both assessed by reference to which was most likely to enable Mr Urquhart to run. The first option of bilateral through-knee amputations was identified as problematic given it would “reduce his control in running”, while the second option of bilateral above-knee amputations with osseointegration was said to “allow for a lower centre of gravity, more control and the opportunity possibly to run with suitably made prosthesis”. Dr Al Muderis claimed that he had no memory of Mr Urquhart’s ambition to run and said that “it’s not feasible for a bilateral above knee amputee with osseointegration to run … [i]t’s not physically possible”. However, the reports reflect, at least at that time, it had been an expressed ambition, and the options provided were assessed and accommodated in the context of achieving that ambition. When questioned about the options in cross-examination, Dr Al Muderis did not accept this and ultimately said he did not recall. The report for the third consultation, on 7 July 2016, again presents the two options, despite curiously recording that:
Mark has expressed that he has had an opportunity to consider the ramifications of above knee amputation and has vocalized his understanding that he will not be able to run with osseointegration. He has said that he will restrict his sporting activities to seated sports.
1529 By the time Mr Urquhart had surgery, he accepted he knew he could not run. There is no basis to conclude that by that time, he had been misled as to the prospect of him running. That said, it is unclear why the option was being actively considered, as reflected in the consultation reports, given Mr Urquhart’s circumstances.
1530 Third, there is an issue as to the adequacy of any discussion with Mr Urquhart of the risks and complications of the surgery.
1531 Mr Urquhart deposed that during the third consultation, the discussion about risks was limited to “a risk of minor infections” that “would clear up with antibiotics”, the “worst case scenario” was that Mr Urquhart might not be able to walk but would still be better off than he was before surgery by effectively standing on his stumps, and that “there would be a bit of oozing at first but then that would clear up as it healed”. He maintained that in cross-examination. Mr Urquhart accepted that he had been told of the general risks of surgery, including death, blood clots and infection and that he needed to look after his stoma if he had osseointegration.
1532 In cross-examination, Dr Al Muderis, in response to being asked whether he told Mr Urquhart each of the following – that there was a risk his stomas would become flyblown and infested with maggots; that there was a risk the stoma would have a horrible smell; that there was a risk that the stomas would weep with fluid and pus constantly; that he would have bare bone poking out of his leg; that he might need painful skin grafts in order to deal with complications from the surgery; that there was a risk he would be left in excruciating pain; that there was a risk that he would be left with nerve issues after the surgery; and that there was a risk osseointegration would ruin his sporting career and his ability to engage in recreational sport – said that he did not recall saying that. In response to the question as to whether he told Mr Urquhart there was a risk that the stomas would weep fluid and pus constantly, Dr Al Muderis said he did recall saying that the risk of infection and oozing would be definite, and fluid would be discharging from the stoma. He also said he did recall telling him there was a risk that he might suffer infections so severe the implants might need to be removed, that he might find himself back in a wheelchair and that he might also need hip placement surgery which could interact with his osseointegration.
1533 Those responses are to be contrasted with Dr Al Muderis’ affidavit, where he deposed that he had a “vivid memory” of advising Mr Urquhart of the risks and complications because of the extensive nature of the consultation process, compared to other patients.
1534 The applicant submitted that Mr Urquhart’s evidence is contradicted by his contemporaneous statements and admissions, which are consistent with him having an understanding that the procedure carried significant risks and that the outcome was uncertain. Various messages were pointed to in support.
1535 Dr Al Muderis deposed that Mr Urquhart, on numerous subsequent occasions, acknowledged that he was aware of the risks of the procedure, the uncertainty of the outcome, the risk of complications and the possibility of further procedures. He identified various Facebook messages and emails in support. It can readily be accepted that Mr Urquhart understood that the outcome was uncertain, and that there may be issues along the way. However, those messages and emails are not consistent with him being told specific risks and complications of the surgery. Knowing that it might not succeed is not the same as knowing the specific risks and complications. Similarly, knowing there are risks, particularly significant risks, is one thing, but knowing what they are is another. I observe there are some matters which Mr Urquhart says he was not told, which it appears on Dr Al Muderis’ evidence is not in issue (including the maggots and protruding bone). Although Dr Al Muderis deposed that he told him there was likely to be some smell, there is no suggestion that he was told that there would be an ongoing foul stench (for which Dr Al Muderis had no solution). These are notable omissions which one might expect a patient who is contemplating undergoing this surgery would want – and expect – to be warned about.
1536 I observe that although there are consultation reports for 2 June 2016 and 7 July 2016, the first does not refer to risks, and the latter only records, as noted below at [1540] in the recited passage, the risk of infection resulting in loss of femur as “a very low risk”. Other risks are not referred to, with there being a bald assertion that the risks and complications had been “thoroughly discussed”. Those reports were intended to be provided to Mr Urquhart (they are copied to him). In circumstances where Mr Urquhart was considering his position after those consultations, one might wonder why such limited information was provided as to risks and complications if they had been discussed. The respondents commend the evidence of Dr Stalley where he notes, in an experimental procedure setting (as was the case here), failure to document significant risks and poor outcomes is inadequate. That is logical and can readily be accepted.
1537 As the applicant pointed out, Dr Paterson’s report on 2 June 2016 records he had a long discussion which included the “unpredictable nature of nerve innervation and pain in the wake of a partial spinal cord injury and potentially that this may yet serve to increase his pain” which “may be difficult to control post-operatively”. As noted earlier, this report was not provided to Mr Urquhart at the time.
1538 Fourth, it was put to Mr Urquhart during cross-examination that he had to convince Dr Al Muderis to do the osseointegration surgery. He disagreed:
I don’t convince anyone of anything … I can’t convince a doctor to do that kind of surgery on me … I didn’t convince a doctor of doing anything … just because I believe something doesn’t mean I can convince a doctor to do that.
1539 He accepted that there were many discussions about “what could happen and what might happen”, and that nobody could predict the outcome. However, his evidence was that:
Munjed actually had the convincing of me that he was such a good doctor that his ability to do what he does, I would have the ability to do what I wanted to do.
He continued:
[What] I’m saying is our discussion was that even though we didn’t know the outcome, that he believed in himself so much and I believed in myself so much, that if the two were to meet, in perfection, then I would have gotten what I wanted to do.
…
[T]he discussions between Munjed, myself and the other doctors was that Munjed was such a good doctor that he has done a lot of these surgeries. He has had minimal amount of bad things happen … I did go into that with the one per cent chance that it could work, because I believed in Munjed, because Munjed believed in himself.
1540 The suggestion by the applicant that, somehow, Mr Urquhart was the only person who considered it might succeed cannot be accepted. The cross-examination does not sit with what appears in the consultation report of 7 July 2016:
After thorough discussion with the team today, we feel that Mark’s quality of life has diminished in the past 12 months and may progressively continue to do so. Upon examination of the investigations and findings, the team is confident that Mark will be able to walk unaided with above knee amputation and osseointegration. This will alleviate the complications which arise from being wheelchair bound as well as providing Mark with more mobility and function. The risks and complications of this procedure have been thoroughly discussed with Mark and he does understand that this surgery does not come without risk. Mark has been found to be competent and capable of making such decisions and understands that there is risk of infection in association with osseointegration which may result in loss of his femur. This is a very low risk however has been discussed.
1541 That is not to suggest that Mr Urquhart thought there was any guarantee it would succeed, but rather to put in context the applicant’s suggestion in cross-examination, where Dr Al Muderis had distanced himself from any expectations of success. Dr Al Muderis was obviously presenting a positive picture to Mr Urquhart in circumstances where Mr Urquhart had a great desire to walk again. As described above, Mr Urquhart said Dr Al Muderis believed in himself, as did Mr Urquhart. Any discussion about risks and complications is to be understood in that context.
Post-operation
1542 Mr Urquhart’s surgery took place on 23 July 2016. There is no complaint about what occurred during the operation. For completeness, I note that Mr Urquhart had a stroke after his operation while in recovery because of a hole in his heart. That is not relevant to this case, except to provide some medical context.
1543 The complaints relate to the aftercare provided by Dr Al Muderis. As noted above, Mr Urquhart terminated his relationship with Dr Al Muderis on 17 December 2020 via Facebook to Dr Al Muderis, followed by an email to Ms Roberts. The communications respectively informing them of this are recited below at [1575]-[1576].
1544 The issues that Mr Urquhart raised there – the protruding bone (the exposed femur), foul stench, continuous bleeding and leaking of fluid, infections, severe pain and the maggots – all occurred while he was Dr Al Muderis’ patient. Other issues, such as granulation tissue, while not expressly raised in Mr Urquhart’s terminating message, were raised in previous messages. As explained below, these are matters which had been raised (some repeatedly so) with Dr Al Muderis and were a matter of concern at the time Mr Urquhart looked for a second opinion.
1545 It is appropriate to address these complaints.
Granulation
1546 In relation to granulation, Mr Urquhart gave evidence that hypergranulation was an issue for him from the outset. He gave evidence of the discomfort it caused and sent photos of his stumps to Dr Al Muderis. This is supported by other evidence, including a series of Facebook messages to Dr Al Muderis on 12 and 15 October 2016, 15 November 2016, 27 January 2017, 21 February 2017, 11 and 25 July 2017 as well as the consultation reports dated 3 November 2016, 2 February 2017 and 27 July 2017. The latter report records that Mr Urquhart had “significant granulation tissue on both legs”, that was affecting his mobility and ability to utilise the legs, and surgery was recommended. A surgical debridement of the wound to remove the significant amount of granulation on both stumps, and a refashioning of the stumps was undertaken on 10 August 2017. This was his second surgery with Dr Al Muderis. Dr Al Muderis in cross-examination accepted that hypergranulation was a persistent problem for Mr Urquhart after the surgery. It was a repeated complaint. Further debridements were undertaken, for example on 5 March 2018 and 4 July 2018.
1547 Mr Urquhart deposed that he often applied silver nitrate on the hypergranulation to burn the excess skin off. His evidence was that initially a home nurse assisted him with this process, but he eventually removed the skin himself. The reports record that he was advised to use silver nitrate to treat his hypergranulation. He deposed that he would then “hack” the skin off his leg, with a high-pressure shower head, his fingernail or an Allen key, which he regularly used to scrape the hypergranulation down. He maintained that in cross-examination, in the face of being accused of giving false evidence. The applicant suggested to Mr Urquhart that he made up the evidence of self-debriding his granulation tissue with silver nitrate after seeing the Broadcast (in respect to Mr Smith, who is discussed below). However, as the respondents submitted, Ms Mattiske also undertook this process. Given the ongoing issue faced by Mr Urquhart, his evidence on this is plausible.
Infection
1548 In relation to infection, Mr Urquhart gave evidence that he developed an infection in his right leg in early 2017 and was in hospital for an extended time. Although Mr Urquhart may be mistaken about the dates or time frame, the import of his evidence was that he had an ongoing infection in 2017. Leaving aside the dates, the evidence establishes that after the surgery on 10 August 2017 (referred to above), Mr Urquhart did suffer from an ongoing infection.
1549 A letter to Dr Tetsworth dated 25 August 2017 from Dr Steele in Hurstville Private Hospital indicated that Mr Urquhart was diagnosed with Pseudomonas aeruginosa and Streptococcus milleri (from swabs taken on 20 August 2017) and was administered antibiotics via a PICC line. A Facebook message from Mr Urquhart to Dr Al Muderis on 19 August 2017 supports this, where he stated, “Well I’m in a spot of bother here old chap … Left leg infected. Doc just saw me and said it needs to be debridaled to get bug out”. The letter to Dr Tetsworth further explained that, due to a family issue, Mr Urquhart was discharged from Hurstville Private Hospital, was reluctant to be treated as an inpatient, and returned to Brisbane where he subsequently presented, as advised, to the emergency department at the RBWH. He was then advised to present to Redland Hospital, where he was treated by Dr Runnegar. On 20 September 2017, Dr Runnegar wrote to Dr Al Muderis about the infection. Separately, but on the same day, Mr Urquhart also sent Dr Al Muderis photos of his infected leg via Facebook. It is apparent from Dr Runnegar’s letter that she spoke to Dr Al Muderis that day. The letter states that Mr Urquhart had completed a course of intravenous antibiotics, which was followed by one month of oral antibiotics to treat his previously diagnosed left stump infection. A photo of two boxes of the oral antibiotics Mr Urquhart was taking was sent to Dr Al Muderis on Facebook on 28 September 2017. Dr Runnegar also newly diagnosed an infection in the right stump (noting there had been ongoing ooze from the wound for two weeks). She reported that “mycobacterial infections generally require surgical debridement with antibiotics” and so no treatment had started. She wrote that she suspected the organism had been present for many weeks. She described concerns about the bacteria becoming drug resistant, and the need for him to be closely supervised. She informed Dr Al Muderis that Mr Urquhart was going to Melbourne, and advised what she considered ought to be done in the lead up to what appears to have been a scheduled visit for Mr Urquhart with Dr Al Muderis on 28 September 2017.
1550 Dr Al Muderis, in cross-examination, disagreed with much of the content of the letter. While he was prepared to accept that Mr Urquhart was suffering from an infection and had been for some time, he disagreed that he was suffering from a serious infection. Dr Al Muderis accepted, albeit somewhat reluctantly, that it was his responsibility to closely monitor his patient, until the infections resolved. There is no evidence this occurred. Rather, according to Dr Al Muderis’ affidavit, he said he understood from Dr Runnegar’s note that Mr Urquhart’s infection was being appropriately managed by the team at Redland Hospital. That is inconsistent with the terms of the note of the call outlined in her letter, for although the infections were being managed, Dr Runnegar informed him (as Mr Urquhart’s surgeon) that Mr Urquhart was leaving Brisbane and was handing on her notes for Dr Al Muderis’ (or his infectious diseases physician’s) continued care. Therefore, leaving aside the dates in 2017, Mr Urquhart’s evidence, that he had an ongoing infection in 2017, is supported by other evidence.
1551 I also observe that during this time in 2017, the failsafe mechanism in Mr Urquhart’s implant was replaced many times, which he physically did himself.
Protruding bone
1552 In relation to the protruding bone, Mr Urquhart gave evidence that the issue arose after his first surgery where he noticed bone poking out of his right stump. He regarded it as a major concern which Mr Urquhart repeatedly asked Dr Al Muderis to fix. On Mr Urquhart’s evidence of the responses given to him, Dr Al Muderis diminished his concerns. An email from Mr Urquhart to Ms Roberts dated 28 December 2020 (11 days after Mr Urquhart terminated his relationship with Dr Al Muderis) supports his concerns, where it states:
… The problem is that I have had exposed femur for so long and having asked and asked to have it fixed and always being brushed off like its nothing. I have asked for over two years now that I have an issue with this and in fact I have said it right from the beginning three and a half years ago… I was never happy of having exposed bone and that is what I think caused that really bad infection in 2017 …
…
… I have repeatedly asked for the right stoma and exposed bone to be attended to simply because of the wretched smell I smell, all day everyday its my own dying flesh I am smelling …
…
… I am pretty upset at having to start from scratch again and put the onis and blame on Munjed for me having to start again because of the exposed femur that I have spoken of so many times.
1553 Dr Al Muderis deposed that the first time the presence of necrotic bone was identified was at a consultation on 1 February 2018. This is referred to in the consultation report of that date. However, he accepted in cross-examination that he was aware of that problem before that date, and he may have been told about it “soon after” the surgery. At the consultation on 1 February 2018, Mr Urquhart presented in a wheelchair, had ongoing pain, and as explained above, there was also granulation tissue. The recommendation recorded in the report was for surgical bilateral split skin grafting around his femoral stomas and a right femoral osteotomy. He accepted that the refashioning and skin graft would cover the bone, reduce the amount of discharge and reduce the smell. It is plain by this time the foul smell and discharge from his stoma were complaints made to Dr Al Muderis by Mr Urquhart. This surgery took place on 21 February 2018. This was the third surgery that Mr Urquhart underwent. The skin grafts were unsuccessful (it partially failed). Contrary to the applicant’s submission that the operation report shows Dr Al Muderis addressed the issue of exposed bone when it was raised, an operation report dated 4 July 2018 (discussed further below), states that among other issues, a “bone protrusion through the [right] stump” was an indication for surgery on that occasion. This suggests that the protruding bone had clearly been an ongoing issue, despite Mr Urquhart’s third surgery. I note that Mr Urquhart continued to have concerns about the exposed bone, as indicated in a message to Dr Al Muderis on 19 November 2019:
… One thing though still An issue for me is the back of the right stoma with the exposed bone.
I know you have said use deodorant but that doesn’t work. I smell it all the time as do people around me. Is there a way for you to think of a wAy to fix that issue or a plastic surgeon ?
Just with warm weather it is starting to smell worse no matter what I do.
1554 I also note that in response to Mr Urquhart’s 28 December 2020 email (being part of an email chain following the termination of his relationship with Dr Al Muderis), Ms Roberts said on 1 January 2021:
With regards to the exposed bone, I spoke to Munjed about it, and he admitted he did not appreciate how bothersome it was for you and he is happy to rectify this.
1555 Dr Al Muderis accepted in cross-examination that he assisted Ms Roberts in preparing that response. The applicant’s submission that Dr Al Muderis “addressed [the] issue”, and along with Dr Al Muderis’ response in cross-examination that the exposed bone was “addressed, and it was covered, and it was no longer an issue because the bone was covered”, is not consistent with his offer to “rectify” the problem referred to in Ms Roberts email. It is also inconsistent with the ongoing complaints as described above. I note that when pressed in cross-examination about Mr Urquhart’s complaint that he continued to suffer from an exposed femur by December 2020, Dr Al Muderis accepted he had a small piece of exposed necrotic bone but claimed it “didn’t have any clinical significance”. I note that in re-examination, Dr Ellis who was called by the respondents, was shown a photo that Mr Urquhart sent on 24 October 2018. He described that it showed bone protruding by more than 15 mm. I return to explain Dr Ellis’ involvement below.
Maggots
1556 In relation to the maggots, after Mr Urquhart discovered maggots in the stoma on his right leg, on 26 April 2018, he sent a Facebook message to Dr Al Muderis on that date. He referred to the maggots “attached to the dead smelly part” of his right leg. He described having his 13-year-old son help him get the maggots out. Although the timing of Mr Urquhart’s evidence in his affidavit is incorrect, he stated that he felt “traumatised” in asking for his son’s assistance. His experiences and feelings in that regard withstand inaccuracies as to timing. Dr Al Muderis was overseas at the time, but responded promptly in the early hours of 27 April 2018 that he would arrange for Ms Roberts to send information about how to get rid of the maggots, and said it was “common” during the season. Mr Urquhart replied with a thumbs up and referred to the bone being “smelly and necrotic”, and the fact he had an appointment “on the 3rd”, meaning 3 May 2018. No information was sent to Mr Urquhart thereafter until the date of his appointment (being eight days after his request for help). I note that Dr Anstee described maggots as a “social and psychological emergency for the patient, the relatives, the nursing staff, anybody involved”. This is an understandable description.
1557 The applicant’s submission that it can be inferred that the information was not ultimately sent because Mr Urquhart volunteered that he was booked for an appointment on 3 May 2018 “anyway”, cannot be accepted. First, Mr Urquhart did not use the word “anyway” in his correspondence. His message cannot reasonably be construed as declining Dr Al Muderis’ offer for information on getting rid of maggots in lieu of an appointment a week later, particularly in circumstances where maggots were not an advised risk of osseointegration. Second, there was no request by Mr Urquhart to delay being provided with the information. On the contrary, Mr Urquhart’s thumbs up in response to Dr Al Muderis’ message – which suggested Ms Roberts would send information about maggots – could only be understood as approving the proposed course of action (being that he would be sent information about maggots). Third, there is no evidence that Dr Al Muderis requested this information be provided to him. Fourth, although Mr Urquhart had an appointment booked, he reached out to Dr Al Muderis immediately for help. Despite that request, no information was provided until the consultation. I note also that although there was a consultation on 3 May 2018, again, there is no consultation report. When pressed in cross-examination, Dr Al Muderis conceded that to leave a patient in such circumstances for a week without access to information was unacceptable. In the face of that answer, Dr Al Muderis volunteered that he may have called Mr Urquhart in that intervening period between 27 April 2018 and 3 May 2018. However, Dr Al Muderis then said he was not able to recall whether he called him or not, and in any case, there is no evidence to support this claim. The evidence is speculative. I have discussed elsewhere how that is an answer given by Dr Al Muderis on other occasions in evidence where the propriety of his conduct might be otherwise questioned (see Dr Al Muderis in Part 5, Section 5). In any event, it appears the maggot protocol was provided to Mr Urquhart at the consultation on 3 May 2018.
1558 Pausing there. In relation to Mr Urquhart’s maggot infestation in April 2018, the applicant’s submission is that it was not symptomatic of an ongoing problem, but it was caused by a lack of hygiene, relying upon the evidence of Dr Gill. I agree with the respondents’ submission that Dr Gill’s evidence, properly read, does not support that submission. Although Dr Gill was of the view that where there is a wound that is not being managed appropriately it is possible it could become colonised with larvae, this related to healing of normal wounds. As the respondents submitted, Dr Al Muderis was at pains throughout the trial to differentiate between a surgical wound and a surgically-created stoma. Dr Gill said that a surgically-created stoma has different characteristics from a post-surgical wound. He said he had never seen maggots as a complication of an elective orthopaedic procedure. Further, the applicant’s submission, that it is not a recurring problem, belies the evidence of repeated infestations, particularly in circumstances where Ms Roberts confirmed in cross-examination that she knew Mr Urquhart to be the patient who found maggots in his stoma on several occasions.
1559 Mr Urquhart continued to suffer maggot infestations. For example, Mr Urquhart sent Ms Roberts videos on 2 December 2020, showing one such occasion. It appears from the metadata in evidence the video was recorded on 26 October 2020. (I note that Mr Urquhart’s affidavit refers to an incident of maggots in around late 2019). I accept the timing of the events by Mr Urquhart is incorrect. I note also that Mr Urquhart did not recall the April 2018 infestation. That said, as I address below, the import of his evidence is supported by contemporaneous evidence and the videos and messages establish that this was an ongoing issue.
Ongoing complaints
1560 It was only two months after Mr Urquhart’s first maggot infestation, on 3 July 2018, that Mr Urquhart again saw Dr Al Muderis, complaining of significant neuroma pain, a foul odour, and failure of the skin graft (which was undertaken in February 2018). Dr Al Muderis accepted that Mr Urquhart “complained from foul odour constantly”. The consultation report recorded that the neuromas were causing Mr Urquhart “significant grief”, were “affecting his mobility”, and he was in “severe pain”. Dr Al Muderis recommended another skin graft and debridement. On 4 July 2018, Dr Al Muderis performed a sciatic and femoral nerve neurectomy, TMR and debridement of granulation tissue on the left side, and an osteotomy and skin graft on the right side. This was Mr Urquhart’s fourth surgery. Mr Urquhart’s evidence was that he was in extreme pain after the surgery and that it did nothing to reduce the pain he had been experiencing in his leg. This is supported by his terminating email and message recited below.
1561 Over September and October 2018, Mr Urquhart sent photos of his stomas to Ms Roberts requesting they be shown to Dr Al Muderis. He refers to several complaints, including pain, the exposed bone, oozing and continual bleeding.
1562 In a consultation in April 2019, Mr Urquhart was recorded complaining of pain in his left hip. The same complaint was recorded as having been made in another consultation in June 2019, where the report stated that a radiographic examination showed “significant osteoarthrosis” in his left hip. Dr Al Muderis performed a hip replacement on 7 August 2019. This was Mr Urquhart’s fifth surgery.
November 2019 onwards
1563 The next consultation on 21 November 2019 was also attended by Dr Tetsworth, Dr O’Carrigan, and Dr Stoita. Like the February 2018 consultation described above, the report recorded that Mr Urquhart presented in a wheelchair. The brief consultation report hardly reflects what occurred at that meeting. It records Mr Urquhart’s complaints of the odour from the stoma on his right-hand side and mild left hip pain. The report also records that he “has been doing very well”, and the solution proffered in it for the odour from his right stump is “deodorant”. Mr Urquhart disagreed with that description. He also disagreed that they were the only issues. In any case, as apparent from the events recorded above, the complaint about the smell was long-standing. It was in this consultation that Dr Tetsworth recommended that he use Febreze on his stump, and others laughed. I have addressed this elsewhere when considering Dr Tetsworth: see [319] above. Suffice to say, Mr Urquhart was deeply offended and left the room. In a message to Dr Al Muderis that night, Mr Urquhart said:
Tell me to use FEBREEZE on my leg was a disgrace. I cannot believe a so called medical professional tells me to use a product that is a carpet and furniture deodorant to cover up the odour of my leg stoma. To then be laughed at by your team I was not very fucking happy. How would one of them feel having their limbs cut off and for the first couple of years have problems and surgeries to fix them. Continual recoveries are difficult to get over but I have never complained to you about anything ever. I suck it up and do my best … I feel the exposed femur somehow needs to trimmed off and around stoma fixed. Sorry mate but I am extremely upset and my PTSD very nearly got the better of me and that, trust me is not a good thing for those immature boys that are supposed specialist. Fucking disgraceful. And if that ever happens again I will no longer attend your clinics.
Dr Al Muderis disagreed that Mr Urquhart was dissatisfied with the degree of care he received from him. It is apparent from this message that the protruding bone was still an issue. It is one he likely would have raised at the consultation. So too, the issue with maggots, given his experiences with them were ongoing. In response, Dr Al Muderis apologised, acknowledged how bad the smell was, told him he “look[ed] very good”, and suggested he use betadine liquid antiseptic as “[t]his may work”. In reply, Mr Urquhart then said:
Remember when my legs were even worse than this I never really complained and it has taken since 23/07/16 to get to this point over 3 years now I keep mentioning not even really highly complaining and the solution to exposed femur is FEBREEZE or Deodorant well now I am complains about that bullshit I was basically ridiculed and laughed at by them all like a big joke. I was extremely embarrassed and to the point of I had to walk out before I yelled and said something I would regret.
1564 Mr Urquhart also wrote a lengthy email to Dr Al Muderis on 24 November 2019, apologising to him for his outrage, accepting it was not Dr Al Muderis who was responsible for the comment and explaining his reaction. His distress at the incident and his complete dissatisfaction were evident. I note that Dr Al Muderis’ responses to both the Facebook messages and email included repeated statements that he regarded him as a friend.
1565 In 2020, Mr Urquhart was in Melbourne and Covid-19 border restrictions meant he was unable to see Dr Al Muderis. He suffered because he could neither exercise, nor swim. He described the impact this had on him and his health, including his mental health. It is evident in an email dated 13 July 2020, attaching a referral to the Inner West Pain Centre, that he was suffering from significant pain. He described, inter alia:
I have pain from the rib cage down the back is extremely painful but then my hip is just as painful, that is the hip replacement, then the stumps are always burning pain.
1566 On 2 December 2020, he sent two videos of his stoma to Ms Roberts, (one of which is referred to above) and said:
Claudia, can munjed recommend a plastic surgeon to fix this I’m a little sick of the constant bleeding and then fly’s getting at it and I end up cleaning maggots out of me. Smells and embarrassing as people smell it.
I keep clean I’m either swimming in a chlorine pool or I’m showering 2-3 times a day. Which being on tank water is costly for me anyways.
Either munjed can fix it or I need a plastic surgeon.
…
I am just getting tired my hip operation hurts but I put that maybe down to weight but was hurting before anyways.
It will have to be looked at after Christmas but it has to be fixed either by munjed or plastic surgeon I reckon.
1567 As already mentioned, it appears that one of the videos was taken on 26 October 2020. By this time, Mr Urquhart was back in Queensland. He asked that the videos be shown to Dr Al Muderis. Ms Roberts replied she would. Mr Urquhart responded that he did not want it touched until after he had Christmas with his children, and expressed his frustrations that he would “get well then crash get well then crash”.
1568 There was no response to this message. The applicant’s submission in respect to that was “Ms Roberts said that she would show the messages to Dr Al Muderis, but Mr Urquhart said that he did not want anything done to it until after Christmas”. That is not an accurate reading of the exchange. It was plain that Mr Urquhart wanted Ms Roberts to show it to Dr Al Muderis, as that was the purpose of sending the request. As is evident from Mr Urquhart’s Facebook message to Dr Al Muderis on 17 December 2020, which stated that he “sent the video to [Ms Roberts] to show [Dr Al Muderis] but, yep no response from [him] or anyone in the team to give [Mr Urquhart] any other ideas”, it is clear that he wanted a response before Christmas. It was just that he did not want “it touched” that is, the fix (being any surgery on his leg), to occur until after Christmas. It is not an explanation for no response being sent.
1569 The complaints raised by Mr Urquhart in that message were those he had been raising for some years.
1570 Mr Urquhart sought a second opinion. It appears that a recommendation to see Dr Huang came from Mr Laux. Mr Laux recalled speaking with Mr Urquhart about his desire to see different surgeons for a second opinion. Mr Laux gave evidence that he suggested to Mr Urquhart that Dr Huang may be able to provide an opinion and that he knew Dr Huang to be someone with an interest in osseointegration.
1571 Mr Urquhart saw Dr Huang in mid-December 2020.
1572 Dr Al Muderis suggested in cross-examination that it is significant that Mr Urquhart continued to communicate positively with him for another year after the Febreze incident, until he terminated the relationship on 17 December 2020 and sought an opinion from another surgeon. The applicant submitted that those communications, and what Mr Urquhart said thereafter are “inconsistent with, and contradicted by, things he had said or written throughout the preceding years”. The applicant pointed to occasions when Mr Urquhart was mobilising, active and saying he was healthy. He relied on photos or messages, principally in earlier times, expressing satisfaction with his service. For example, the applicant pointed to a questionnaire in January 2019, where Mr Urquhart ticked, “definitely true” or “mostly true” to a question as to whether his health was excellent. I note that Mr Urquhart also responded in that questionnaire to pain in the last four weeks, as “moderate” to “severe”. However, the applicant’s submission misses the point. As Dr Al Muderis conceded in cross-examination (although the concessions were pulled back at times), Mr Urquhart had had constant problems since the original surgery and complained constantly about his legs. Further, it is apparent from the discussion above, that some of the applicant’s submissions and evidence of what he had done, or why certain matters were not done, are inconsistent with the evidence itself (i.e. Mr Urquhart’s messages asking for help). Notwithstanding any explanation proffered, Dr Al Muderis’ evidence dismissed Mr Urquhart’s concerns, consistent with Mr Urquhart’s evidence of Dr Al Muderis’ approach at the time.
1573 From Dr Al Muderis’ perspective, as he volunteered in answer to a question about satisfaction with his services, Mr Urquhart had achieved his goal from the surgery, as he was walking.
1574 Given the circumstances in which Mr Urquhart was seeking a second opinion, it can be inferred he did so because he was unhappy with the care he was receiving. He said so expressly in the emails he sent to Ms Roberts terminating the doctor-patient relationship. The communications reflect an obvious frustration with the issues he has faced since his osseointegration surgery, and the fact that they still exist.
1575 There are two communications of relevance that should be extracted. The first is the email to from Mr Urquhart to Ms Roberts on 17 December 2020, terminating the doctor-patient relationship (as referred to above):
Claudia,
I would like to ask for either the original or a copy of my files please.
I am no longer a patient of Munjeds.
I have asked for to long to have my stomas attended to. I’ve already had the one bad infection back sometime ago. I have basically felt ignored by Munjed so I have searched out another surgeon who does Osseo the Swiss version.
My legs as you have seen by photos and video I have sent you ages ago are a disgrace, I’ve asked about the smell and the exposed femur being a source of infection. I am basically ignored and told nahhhh it is fine wah it and cover in Vaseline which wears off and then legs for the 4th or 5th time I’ve had maggots appear on my stumps and it’s because the blood dries on the exposed femur. I cannot continue to live this way.
The nerve pain I had slightly when just a plain para but not this bad it’s tripled in its intensity. Nothing that has been tried has worked to fix the nerve problem that TMR surgery that was 9 months of hell and it didn’t do a darn thing to fix the pain
I have met with another surgeon but for my own files I would like to have a complete copy of my files. I am keeping copies of every
I am rolling away from munjed and the team especially Tetsworth I cannot be in a room with that Man ever again or I’ll knock his block off.
My legs continually bleed and are hypersensitive.
I can deal with a lot of pain but I’m done.
I don’t regret having this procedure done but I did not expect to have problem after problem, year after year it has worn me down.
I have ruined clothes and furniture because of the leaking body fluid and the continual bleeding. I’m sorry I have to do this. In actual fact It was pretty over the last time I was in the office when Tetsworth made that stupid remark about FEBREEZE.
I’m not arguing with him, I am just walking away and having the Swiss technology done on my legs, which will seal all the leaking problems, bleed continually yesterday I sat on the toilet and as I sat a spurt of blood pfff all over the floor and even spited out far enough to get the back of toilet door.
Like I have said to Munjed the very first meeting I didn’t do this off a whim and I didn’t expect to have a pain free life I just want to be comfortable that’s all. I don’t need to speak with Munjed about anything I’ve asked and asked about my femurs.
So I am hereby terminating any contract and contact with Munjed as my doctor and formally asking and requesting a complete copy of my medical files. …
1576 The second is a Facebook message sent to Dr Al Muderis earlier on the same day, also expressing the same frustrations:
So I have a serious question Munjed. On the osseo page (i know your not the admin) but my questions get ignored. I have serious issues and I am ignored. For the fourth time already this year i have had maggots in my stoma. The right leg. I shower three times a day i use vaseline like you suggested my stomas kill me with nerve pain seems like nerve endind are right at the very surface of the stomas. Anything that touches them is super painful even the wind blowing the hair and I dont even feel to touch my body from the chest down. as you well know. I am tired of dealing with maggots on the exposed femur that is there that i have asked many times to have fixed. I have never recieved an apology from tetsworth for his stupid remark about using the carcinogenic FEBREEZE on my open wounds. My stumps contin ually bleed and leak body fluid over all my clothes and furniture. I never had this done thinking i was going to be pain free I had it done to walk but what i did not exp;ect is that the p;ain would multiply immensely. I have sent video and photos to Claudia to show you again the next lot of maggots. M y questions are not posted or if they are they are removed. I thought the whole idea of the page was so that everyone could support each other. Well gotta say all of a sudden I am left out in the dark so who ever is admin is clearly not allowing my question to be posted. I am unsure why as it has not abused anyone I am always polite I am just trying to find out if others have similar issues and if they do could they share with me any ideas that could help me. But clearly showing my stomas is offensive to the admin for whatever reasons they may be Maybe they don’t like the sight of maggots squirming all over, in and out of the stoma and the open femur which i keep saying is a dangerous source of possible infection and they would get infected if i didnt keep myself as clean and healthy as i do. I am so over the nerve pain which that TMR most painful operation I have had out of the many many i have had. I have always sup;ported you, sprouted about how grerat you are and how grateful i am, to you for helping me walk again. Now I am just like the military just a number. I am beginning to feel like I am a pest for asking to have stomas that don’t bleed, leak, stink to high heaven and continually get maggots not matter what i do. My GP is horrified at my stumps as am I. I feel like I am a rotting corpse walking around and hear comments like “omg what is that smell when I am in a room with people of course they immediately look at me. In fact i am feeling so embarressed in front of people i just dont leave home again. I sent that video to Claudia to show you but, yep no response from you or anyone in the team to give me any other ideas. I have used about every smelly natural creams I can find. So i am fairly pissed off at the admin for not allowing my posts to go up so other people on the page can give me other ideas that i may not have thought of.
…
it is bloody disgusting and makes even me now want to throw up at the smell and continual leakage
Normally blood and guts nor the smell of dead bodies bother me but this is getting to me physically and mentally.
So here is the thing it affects me so much I have gone to find someone for a second opinion. Well that orthopaedic surgeon couldn’t believe their eyes at my stomas and especially the exposed femur of which i have always said is a huge issue for me. So to be 110% open and honest with you I am extremely disappointed because I have shouted your name from the rooftops as my hero for helping me walk again. I have always been positive about you but it is becoming increasingly difficult for me to do that. I just feel totally ignored by you; now I am no longer in Invictus Games and close contact with Prince Harry. So I am afraid to say, I am so very upset about my health problems with these stumps that I am of the opinion there is no other choice for me, except to part ways with you and your team. I will be taking up this other orthopaedic surgeons offer to completely remove all of the hardware you put in me and start again which for me as a sportsman takes me out of action again for an extended period and which is kicking my PTSD into next gear. So from here on; I am no longer a patient of yours I leave this group in absolute disbelief I have to do this but you have left me no choice. Not just disbelief but upset you haven’t fixed the exposed femur you just brush it off like its nothing. I fly down to sydney to see you along with a myriad of other people I wait patiently then I get 5 or 10 minutes in the room with you and leave very disappointed with you, then fly home. One ten minute appointment with you takes two days out of my life. I can no longer stand and sing your praises unfortunately especially once this other doctor saw this work and all they could say is they were sad and sorry I have had to go through not just serving my country with distinction; but to suffer even more from a surgery that should have been done correctly in the first place and or every other time. So with a sad heart from here on in I am no longer a patient of yours and I will inform the Department of Veteran Affairs of the same thing that I no longer attend your practice. I had such high hopes but i roll away with a sad heart and a very painful pair of stumps. Seems also by looking at the osseo page that there are a crapload of men and women with serious pain issues and other issues the same such as hypersensitivity, soreness, redness, continual leaking and continual extreme pain; all the people seeking remedies from each other to find out what others have tried to assist them to heal at least some of the pain. We all know we will never be completely pain free but all anyone that you have operated on wants is to be somewhat comfortable without having to rely on excessive pain medication. Good Luck in the future and I sincerely hope you figure out a way to help people live comfortable lives without having to go through the pain a lot of us do. One last note I will not be singing your praises from the rooftops anymore. I honestly do not think I could nor will I recommend you, which does sadden me. Mark.
1577 Photos attached to the message reflect that the description he gave of the condition of his legs appears apt.
1578 Dr Al Muderis disagreed with much of the content of the communications. For example, he said that he had dealt with the protruding bone (which as explained above, was not fixed). He disputed he was aware there was a problem with bleeding, but there is evidence to the contrary in messages and photos sent to him. Dr Al Muderis said that he had various correspondence with Mr Urquhart which indicated that he was performing well, and that while there may have been concerns, there was no serious complaint raised prior to his email to Ms Roberts. That does not sit with the issues raised by Mr Urquhart (as reflected above) and is consistent with Mr Urquhart’s evidence that Dr Al Muderis was dismissive of his concerns.
1579 The applicant conflates seeing or communicating with a patient as synonymous with proper aftercare, regardless of the content of it. It may be accepted that there is a system in place for follow-up consultations (e.g. at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months), but it does not follow that the attention given is of the quality required. This is particularly so if complaints are not attended to, brushed off, or the patient is not listened to. Similarly, and contrary to the applicant’s submission, providing his mobile telephone number does not, by itself, suggest aftercare over and above that required.
1580 He also disputed the complaint raised about short consultations. From the message extracted above, Mr Urquhart’s complaint was that he would travel from interstate to see Dr Al Muderis, wait around, and then only see him for five to ten minutes. Although this was denied, the cross-examination of Dr Al Muderis reflected that simple math based on his consultation numbers supports Mr Urquhart’s evidence. Dr Al Muderis accepted that he typically sees about 30 patients on a clinic day, and that the new patients (being on average between zero to four patients) take up to an hour or more each. That leaves little time for the remaining 25 to 30 patients. The duration of Dr Al Muderis’ consultation is also supported by the evidence from other patients, which I have addressed elsewhere. I return to this topic below when addressing the imputations: see sting 4 in Part 7, Section 1.
1581 Mr Urquhart requested his files from Ms Roberts. As mentioned above, the responses to his emails by Ms Roberts had input from Dr Al Muderis. The first request was on 17 December 2020, the day the relationship was terminated. Ms Roberts responded on 18 December 2020, where she attempted to persuade him to speak to Dr Al Muderis, raised concerns about the experience of his new surgeon, Dr Huang, and indicated that she had asked their staff to start preparing a copy of his medical records. Ms Roberts’ other response on 1 January 2021 within the chain of correspondence was in the same terms but made no mention of his medical records. A further request was made on 6 January 2021, and again on 19 April 2021, with the documents being provided on 26 April 2021. It took more than four months for the request to be complied with. It was a reasonable request, wherein Mr Urquhart explained that he wanted his new surgeon to readily access his medical history. There is no explanation for the delay.
1582 On 11 February 2021, Mr Urquhart’s case was presented by Dr Huang at a “Bone Breakfast” meeting, a forum discussing complex patients, at the Royal North Shore Hospital Department of Orthopaedics and Traumatic Surgery. Those who attended Dr Huang’s meeting included a number of senior orthopaedic surgeons, a Professor of Orthopaedics from the University of Sydney, other medical staff, Dr Ellis as the head of the hospital’s Department of Orthopaedics and Mr Urquhart.
1583 Pausing there. Dr Ellis gave evidence in these proceedings about his involvement with Mr Urquhart. Dr Ellis has worked as a specialist orthopaedic surgeon for nearly 30 years with 25 years’ experience as a trauma surgeon, where he has been involved in the care of patients requiring complex surgeries. He has also served nine years on the Board of the Australian Orthopaedic Association (ending as its President in 2019/2020). His elective practice is focused on lower limb reconstructive surgery, principally through hip and knee replacement. The applicant submitted in closing that Dr Ellis was a “wholly credible witness” and that the Court should accept his evidence. I note that he was one of Ms Grieve’s confidential sources.
1584 Dr Ellis gave evidence that Dr Huang sought further advice from the group about Mr Urquhart’s case, given its complexity. The meeting was on whether the course of action about to be advised was a reasonable one. He said Dr Huang informed the attendees that he had recommended that Mr Urquhart’s right osseointegrated implant be removed to produce some healing and that the exposed bone be removed. The concern was primarily regarding the right femur, where there were signs of infection and discharge. Dr Ellis was challenged on his evidence that there was a discussion about infection, or any concern about osteomyelitis, because there was no reference to that in the PowerPoint shown at the meeting. Although he accepted it was not referred to in the PowerPoint, he explained why that might come about, as it was prepared by a junior registrar. He also accepted that it was not mentioned in his affidavit and said that was an oversight. He denied the suggestion there was no discussion. He agreed in cross-examination that the recommendation was the implant be taken out to produce some healing and that exposed bone be removed but also explained that was because it was “not likely to heal with chronic infection at the end”. He said that when:
bone is prominent through the skin for a period of time and there is leakage … in excess of normal leakage – and from time to time the patient is on antibiotics and different things … the reality of there being some degree of colonisation and infection at the end of that exposed bone is high.
1585 Dr Ellis said that the exposed bone was evident in the image on the final slide shown at the meeting. His evidence was that the attendees at the meeting discussed the issues and options for Mr Urquhart and a consensus was reached amongst the attendees in support of Dr Huang’s recommendation for Mr Urquhart. They were aware Mr Urquhart wanted a wound which was healed, and which did not smell or discharge anymore.
1586 In February 2021, Mr Urquhart had his right implant removed and in December 2022, his left implant was cut and the stoma was closed over. He now has no stomas and is wheelchair-bound.
1587 In cross-examination, Dr Al Muderis gave evidence that he had, and still has, serious concerns about Dr Huang’s capacity to treat complex osseointegration patients and believed Mr Urquhart had been given the wrong advice by him. Dr Huang, it appears, took a responsible approach by presenting the case at the “Bone Breakfast”, attended by very senior and experienced practitioners, to obtain advice.
1588 The applicant cross-examined Mr Urquhart on the basis that removal of his implant was his choice, and that he had been told by Dr Huang that he would get new implants, being the other type of osseointegration implant, OPRA. That is, it was suggested the removal was to replace the system, not because there was any medical need for removal. Mr Urquhart denied the proposition. Although he denied that the plan was to receive a new implant, the possibility of getting another system later does not mean that removal was not for a medical purpose. I do not accept the applicant’s submission. It is not supported by evidence. The “Bone Breakfast” meeting attended by Dr Ellis, as explained in his evidence, does not support that proposition. On the applicant’s submission, Dr Huang must have misled the meeting, because the basis on which he sought advice was a medical one. There is no basis for such an assertion. As discussed elsewhere, the applicant’s submission – that there should be an inference drawn from the respondents’ failure to call Dr Huang, suggesting that his evidence in respect to Mr Urquhart would not assist their case – cannot be accepted.
Conclusion
1589 As referred to above, I accept that Mr Urquhart may be a poor historian in some respects. He accepted he was not good with dates. He may be mistaken about the timing of events (e.g. the timing of the infection in 2017 or when he saw Dr Huang) and could not recall some events (e.g. the maggots in April 2018), nonetheless, the summary is not solely dependent on Mr Urquhart’s evidence.
1590 The recitation of the events above, which is supported by contemporaneous records, the opinions of others, and concessions made, collectively establish that during this time, Mr Urquhart had experienced, inter alia, the protruding bone, the foul odour, infection, bleeding and oozing, severe pain, hypergranulation and maggots. He had undergone multiple surgeries, with no solution to matters of significance to him. These issues still existed when he went to obtain a second opinion. That there were positive messages of gratitude or that he referred in various communications to the activities he was able to undertake at times does not diminish that. Mr Urquhart was entitled to consider that enough was enough.
1591 Mr Urquhart said, he could deal with a lot of pain and had for many years. He had problems since the first surgery and had more surgeries to fix them, as well as continued recoveries, but he did not complain. In his words, he just “suck[ed] it up and [did his] best”. But, as he said, on what he was told as to the risks and complications, he never understood that he would continually have the issues he did, with their obvious consequences.
1592 The applicant in cross-examination dismissed the foul smell and maggots as not serious. He also said that the exposed bone was “not a serious problem”. They were all said to be not uncommon occurrences, yet they are not matters that patients were warned about. Mr Urquhart was not warned of these matters, and nor was a solution found. As explained above, a patient is entitled to expect to have been warned of these matters. This impinges on the issue of informed consent. It can be readily accepted that both can be distressing, and the constancy of them impact significantly on the quality of a person’s life.
1593 The proposition put to Mr Urquhart in cross-examination by the applicant that his quality of life only deteriorated after he stopped being Dr Al Muderis’ patient, is inconsistent with the evidence.
1594 The osseointegration surgery was conducted despite the concerns expressed by Dr Paterson in his reports. It can properly be described as experimental. As explained above, although his second report is tempered, those concerns remained. There appears to be no evidence that the steps he said ought to be undertaken if surgery was to occur were undertaken or actioned. The concerns he raised, given Mr Urquhart’s circumstances, were real and obvious ones. Despite that, Mr Urquhart was nonetheless regarded as suitable for surgery with Dr Al Muderis recording in the consultation report the team is “confident that [Mr Urquhart] will be able to walk unaided with above knee amputation and osseointegration”. Mr Urquhart’s other health issues (e.g. relating to his pain and mental health, as raised by Dr Paterson), and how the surgery may impact on them needed to be addressed before the decision about his suitability was made.
1595 I am satisfied that Mr Urquhart was assessed as suitable for this surgery where there is no evidence Dr Paterson’s concerns had been addressed, where he was also not adequately warned about the risks and complications of the surgery. I am also satisfied in respect to aspects of his aftercare that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Mr Brennan Smith
1596 Brennan Smith is a veteran, having previously served in the Australian Army and the Air Force. He was discharged from service in 2007. In April 2017, he injured his left leg in a motorcycle accident and underwent treatment at the RBWH. While in hospital he developed an infection. Complications meant that in about May or June 2017, Dr Tetsworth amputated Mr Smith’s left foot. He ultimately required an above-knee amputation to stop the infection spreading. Mr Smith’s evidence was that following that surgery, he could not walk more than ten metres without excruciating pain while using sockets and needed to use either a wheelchair or crutches.
1597 Mr Smith had osseointegration surgery with Dr Al Muderis on 4 July 2018. His evidence was that he has had ongoing issues arising from the surgery, including debilitating granulation and pain, and repeated infections. He has also had repeated problems with the prosthesis coming loose, which Dr Al Muderis designed and (via his company) supplied upon surgery. Mr Smith later used a different attachment to his implant because he considered it unsafe (until, he says, Dr Al Muderis changed the attachment back without his consent): see discussion below.
1598 The applicant submitted that Mr Smith was a poor historian, and that his evidence should only be relied on to the extent it is corroborated. The applicant submitted some of his evidence was absurd. Mr Smith is one of the witnesses the applicant alleged has concocted evidence after contact with Ms Grieve.
1599 The applicant referred to evidence that there was an altercation of some kind between Mr Urquhart and Mr Smith in February 2023. Mr Urquhart and Mr Smith told conflicting narratives of the incident. Although the applicant submitted that it is unnecessary for the Court to resolve what happened between them, he nevertheless submitted one of them was not telling the truth about the incident, and that would cause the Court to have reservations about the credit of both men. This is an incident which occurred in February 2023, in relation to something which prima facie has nothing to do with what either witness said occurred to them in relation to their interactions with and treatment by Dr Al Muderis. There appears to be alcohol involved and the altercation occurred in circumstances where they both suffer from PTSD. Also, given the circumstances, it is not necessarily the situation that one is deliberately misrepresenting events. In any event, it is not necessary to resolve. It does not have any bearing on the evidence given in relation to the issues in this hearing.
1600 The respondents submitted Mr Smith’s evidence is reliable, and that he has been clear and consistent on matters of significance.
1601 There are aspects of the evidence of which Mr Smith does not recall (for example, scheduling, but not attending, an appointment with Dr Al Muderis in 2017, and the June 2018 consultation at Leading Edge, a prosthetics company in Queensland). It does not necessarily follow that his recall on other matters is lacking or unreliable. There are some aspects which are supported by other evidence, such as his experience with granulation. I accept that in relation to significant matters he has been consistent, and as apparent from the discussion below, his evidence is supported by other evidence (including contemporaneous documents).
Background to surgery
1602 Mr Smith met with Dr Al Muderis twice before the day of his surgery: in February 2018 and in June 2018.
1603 Mr Smith was referred to Dr Al Muderis by Dr Thomas Crookes on 4 July 2017. Mr Smith then submitted an enquiry through Dr Al Muderis’ website before exchanging emails with Ms Roberts. Although Mr Smith accepted that he made that inquiry, he had no specific recollection of it.
1604 Ultimately, on 23 February 2018, Mr Smith met Dr Al Muderis while he was in Brisbane to present at a conference. Although they planned to meet at the RBWH, they met instead in a hotel lobby. What occurred at this meeting is in dispute. There is no contemporaneous record or consultation report. Mr Smith’s evidence was that it lasted about 35 to 40 minutes, and that Dr Al Muderis, Ms Roberts, and another amputee and his wife were present. Dr Al Muderis did not explain why the other amputee (or his wife) was there.
1605 Mr Smith gave evidence that Dr Al Muderis looked at his leg (Mr Smith took the sock off his stump to enable that to happen) and said words to the effect of: “That’s not good”. Dr Al Muderis did not otherwise conduct a physical examination, nor did he discuss what Mr Smith hoped to achieve from the surgery. He said Mr Smith would be pain free and have a new lease on life. Dr Al Muderis told him he would be an excellent candidate for osseointegration, that he would be able to swim and run, and that it was a simple procedure that he had done hundreds of times.
1606 Although Mr Smith accepted that although there had been some discussion of risks before he had the surgery, he explained not all risks and complications were discussed.
1607 That said, he explained that at the hotel meeting there was no discussion with Dr Al Muderis about risks or complications, including infection and granulation. Mr Smith said after meeting Dr Al Muderis, he and Ms Roberts discussed oozing, infection, and granulation, but there was never any discussion about constant infections or excessive granulation. Properly read, his evidence is that this discussion occurred at the hotel lobby meeting.
1608 Mr Smith gave evidence that, during this meeting, Ms Roberts showed him photos of an amputee running, another swimming, a third walking, and a fourth on a dirt bike. On 25 February 2018, he emailed Ms Roberts asking for those photos and enquired whether one can run on the implant. In response to Mr Smith’s enquiry about running, Ms Roberts wrote:
We advise strongly against running for the first 12 months, to give the implant time to integrate. However after that we do not encourage it as we do not know what might happen- there is no research in this area. However we do have a few of our patients who do run, we just don’t advocate for it.
(emphasis in original)
1609 That email is not inconsistent with Mr Smith’s evidence that he was told he could run. As Mr Smith said, the advice is to leave it to the patient to decide whether they can run, not that a person cannot or should not run. I note that, on the FAQ section of the Osseointegration Group of Australia website (as of 31 March 2023), it advises patients against high impact activities for the 12 months following osseointegration surgery, and it is then up to them to decide whether to take the risk.
1610 The applicant submitted that the fact that Mr Smith asked whether running was possible in his 25 February email demonstrates that he was not told during the meeting that he could run. Mr Smith rejected that explanation in cross-examination, explaining that he asked the question because he sought confirmation. Mr Smith’s explanation may be accepted in circumstances where the content of the email demonstrates he sought certainty, in writing, on a topic on which his understanding was incomplete, having been shown by Ms Roberts (according to his email) photos of osseointegration patients undertaking outdoor activities.
1611 Mr Smith’s evidence is also supported by the slide pack Dr Al Muderis presented at the conference that day. Ms Roberts had access to those slides (with the photos). It contains photographs which fit the description of the images Ms Roberts showed Mr Smith. Dr Al Muderis’ evidence was that he showed Mr Smith those slides in the hotel lobby. As explained below, Mr Smith denies that. Nonetheless, the slides contain photos of osseointegration recipients running (captioned “RUNNING”), swimming (captioned “SWIMMING”), and doing other physical activities. Mr Smith gave evidence that one photo Ms Roberts showed him was of “a guy on … a dirt bike in mud”; one slide contains a photo of a man on a quad bike in mud (captioned “NO LIMITS”).
1612 Ms Roberts’ advice that Dr Al Muderis does not encourage or advocate for running is inconsistent with promotional material of osseointegration users running which, on the applicant’s case, is shown to prospective patients, including Mr Smith.
1613 Dr Al Muderis had only a vague recollection of the 23 February meeting. He accepted he may have looked at Mr Smith’s leg but said he did not conduct a physical examination because that was not the purpose of the meeting, which was to provide general information. Dr Al Muderis said they discussed his case, his complaints, and he showed Mr Smith his presentation. I note from that, the applicant has extrapolated in his submissions that it was the entire presentation (or at least dozens of its slides) and that those slides include information on risks and complications. The presentation contains 211 slides. Mr Smith denied that he was shown slides. Given this meeting was in a hotel lobby and was not, according to Dr Al Muderis, a consultation, it seems unlikely that the whole presentation had been shown to Mr Smith in those circumstances. It is far more plausible that he was shown the limited slides containing photographs of people undertaking physical activities, as Mr Smith described.
1614 Dr Al Muderis denied saying to Mr Smith that he would be pain free or that he would be able to run on the basis that that is not what is part of his standard discussions with prospective patients. Given Mr Smith’s email to Ms Roberts following the February meeting and his recall of what was discussed – that Dr Al Muderis had recently presented a slide deck advertising photos of patients running, and that he had shown Mr Smith those photos (via Ms Roberts) – Dr Al Muderis’ evidence that he did not tell Mr Smith at the meeting that he would be able to run is implausible.
1615 Mr Smith also gave evidence that in the February meeting Dr Al Muderis said he would need to transfer him $10,000 to secure his place for surgery and to keep it secret. He felt a sense of urgency; Dr Al Muderis and Ms Roberts kept telling him they were very busy and that if he did not act quickly, he might miss out.
1616 Although Dr Al Muderis did not recall saying to Mr Smith that he needed to transfer $10,000 into his account to secure his place in the operation schedule, he denied saying the amount must be kept secret. Mr Smith’s evidence is supported by later correspondence from Ms Roberts. On 17 May 2018, in response to an email from Mr Smith (who had yet to decide whether to undertake the surgery), Ms Roberts asked him whether he would consider using his private health insurance and said that, as Mr Smith was a veteran, Dr Al Muderis “would honour his discounted rate at $10,000” out of pocket. Ms Roberts wrote “[t]his needs to remain confidential please”. This was only part of the payment, with Mr Smith believing that outstanding costs were covered by Bupa. That Mr Smith paid so quickly after he had decided to proceed, after he received the fee estimate and before he was formally assessed by Dr Al Muderis as described below, is consistent with a belief in an urgency to pay.
1617 Mr Smith gave evidence that the February meeting was like a sales pitch. He described that Dr Al Muderis would say something, and then Ms Roberts or the other amputee in attendance would chime in. Ms Roberts said words to the effect of: “We have done many, many patients, we have positive outcomes, it will change your life, you won’t know yourself”.
1618 In an 18 May 2018 email, Mr Smith told Ms Roberts he was “[definitely] considering this procedure”. On 28 May 2018, a further consultation was booked with Dr Al Muderis for 16 June 2018. Mr Smith was sent a fee estimate for the surgery, $35,000 discounted to $10,000, dated 30 May 2018. Mr Smith made payment on 13 June 2018, three days before the consultation. On 30 May 2018, Ms Roberts sent him a Surgery Information Pack, confirming surgery for 4 July 2018 and including the hospital admission form. That admissions form was signed on 8 June 2018.
1619 It follows that Mr Smith’s surgery was booked and paid for before the 16 June 2018 consultation. Contact with Dr Al Muderis himself (as opposed to his office) was confined to the hotel lobby meeting in February 2018. Mr Smith said he had been told he was an excellent candidate for the surgery. He had been told limited information and there had not been any detailed assessment. Even accepting the applicant’s version of the February meeting, which was that its purpose was for Mr Smith to have the opportunity to meet Dr Al Muderis and be given general information about the surgery (with which Mr Smith agreed in cross-examination), there was no assessment before his surgery was booked and paid for. I note that, in cross-examination, Ms Roberts said the hotel meeting was not an assessment of Mr Smith’s suitability for surgery. The payment of the $10,000 is consistent with Mr Smith having been told he was an excellent candidate for the surgery, and that he needed to pay the money to secure his place.
1620 The applicant submitted the payment was not a deposit to secure Mr Smith’s place, but a discounted veteran rate constituting the full amount Mr Smith had to pay. The respondents submitted the practice was an unethical sales tactic amounting to pressuring a patient into making a life-changing decision there and then.
1621 The applicant’s submission not only creates a false dichotomy, but also ignores that key aspects of the payment – that it was a prepayment; that he was told it was to secure his place and that he might miss out; and that it was specially and confidentially discounted for him – coalesce to create the impression of an alluring offer to be attended to urgently.
1622 Those circumstances raise a further issue relating to informed consent. As Dr Geffen explained, a substantial deposit of the kind Mr Smith paid may affect a patient’s judgment in assessing the risks and complications of surgery, given the patient will, upon payment, have made a substantial commitment to proceed. These issues have been discussed above in relation to the international patients: see Part 6, Section 4.
1623 I note that the $10,000 may well be the “full amount” Mr Smith had to pay, but that was in relation to his out-of-pocket expenses, which ignores the insurance money Dr Al Muderis would receive if Mr Smith underwent the procedure.
1624 The consultation occurred on 16 June 2018 at Leading Edge in Queensland. There is no consultation report in evidence. Dr Al Muderis gave evidence that his standard practice was to dictate a report after a consultation; he would have done it on this occasion but said it could not be found. Dr Al Muderis demonstrated no recollection of what occurred at the consultation, other than saying he would have followed his standard practice. As referred to earlier, this is not the only occasion when a consultation report is missing (or as explained earlier I infer does not exist) in relation to a patient witness.
1625 A document dated 28 May 2018 and addressed to Mr Smith confirms details of the upcoming consultation, including the team members he would meet. The persons intended to be present were Dr Al Muderis, Ms Roberts, Mr Stuart Crampton (a prosthetist) and Mr Lu (a researcher). There is no evidence that a pain specialist, or that an infectious diseases specialist (given the history which led to his amputation), were consulted before surgery.
1626 Mr Smith does not recall the consultation. Although it can be inferred that Dr Al Muderis concluded that Mr Smith was suitable for the surgery. The applicant’s submission in respect to this consultation referred to Dr Al Muderis conducting a physical examination and discussing the risks and potential complications of the procedure with Mr Smith, citing his affidavit evidence. He submitted that during the consultation, he gave Mr Smith a copy of a brochure published by the Osseointegration Group of Australia titled “Osseointegration Surgery A Guide for Patients”, which they discussed. The applicant does not provide any evidence to support that submission. It is not referred to in his affidavit nor is there any other evidence in support. The applicant detailed what he said was in the document. There is no evidence that this was his standard practice (there is no evidence it occurred on other occasions). This document is described above at [603]. In any event as mentioned, there are issues with the content of that Guide (including no reference to hypergranulation, odour, maggots, but there is reference to reduced overall pain).
1627 Mr Smith’s interview with Dr Basten, via telephone, occurred on 19 June 2018. This is in a context where he was diagnosed with PTSD after his military service. He told Dr Basten that he continued to see a psychiatrist and a psychologist for this. He developed depression after his amputation. In his report Dr Basten opined that “[h]e is distressed by his pain and his questionnaire responses suggest that he focuses on the pain anxiously”. This is obviously after his consultation with Dr Al Muderis, and there is no evidence of this being addressed by him.
1628 On 4 July 2018, the applicant performed a single-stage left transfemoral osseointegration on Mr Smith at Macquarie University Hospital.
1629 As referred to above, although Mr Smith accepted that there had been some discussion of risks and complication before surgery, there was no discussion about constant infections or excessive granulation, which he later experienced.
Post surgery
1630 On 11 July 2018, Mr Smith was discharged from Macquarie University Hospital to The Hills for rehabilitation. Mr Smith gave evidence that Dr Al Muderis did not provide documentation in relation to what was expected in rehabilitation. Mr Smith said that while at The Hills he asked for a copy of the rehabilitation program many times but was not given anything. He alleged that a rehabilitation plan was not prepared for him. Dr Al Muderis denied this, stating that he was placed on his standard protocol and that a copy of this protocol was provided to the team at The Hills. He also gave evidence that Mr Smith was provided with routine daily instructions. Dr Al Muderis produced those instructions with his affidavit. However, the document he produced is the operation report. Dr Al Muderis says the last three lines of the document contain the plan and instructions; those lines only refer to the patient being on the standard loading protocol. As an operation report, it was not given to Mr Smith.
1631 That document’s brief reference to the standard loading protocol could not properly be described as a rehabilitation plan or daily care instructions. Yet that was the evidence relied on by the applicant.
1632 On one occasion at The Hills, Mr Smith was on the toilet and noticed that his stump was bleeding badly. He was in excruciating pain. The nursing notes confirmed there was bleeding in the circumstances described by Mr Smith. The nursing notes describe that the left stump bled about 50 ml of fresh blood. As noted above, this incident was not referred to in Dr Haidary’s affidavit evidence, and his explanation in cross-examination for this omission was rather unsatisfactory.
1633 Mr Smith was cross-examined about a message he sent to Dr Al Muderis while in The Hills, showing him walking two weeks after the operation. To similar effect was a video he sent to Leading Edge. Mr Smith was effusive in both messages towards Dr Al Muderis and osseointegration. He accepted that he told Dr Al Muderis he was very happy during a consultation during this time, explaining that he was “stoked” and happy because he could move.
1634 The applicant submitted that the discharge summary records that Mr Smith’s post-operative recovery was unremarkable. The discharge summary notes that he developed a wound infection, which was effectively treated, and had pain mostly due to muscle tightness. By the time he was discharged, he was independent with activities of daily living and could mobilise independently with crutches.
1635 The applicant referred to Dr Haidary’s evidence that the rehabilitation process was explained to Mr Smith, that Mr Smith improved steadily during rehabilitation and achieved his goals, and that he was discharged normally and walked out of the rehabilitation hospital.
1636 In the circumstances it is unnecessary to resolve submissions relating to Mr Smith’s care at The Hills. I note that complaints were made by several patients in relation to their stay at The Hills. Although I have considered the evidence in each instance, as it may affect other issues, generally it was not necessary to resolve any disputes on this topic. Dr Haidary was responsible for The Hills, not Dr Al Muderis. As mentioned earlier, Dr Haidary’s evidence was unsatisfactory in some respects. That said, a frequent complaint appears to be that Dr Al Muderis did not visit his patients. Dr Al Muderis’ evidence was that he did not have visiting rights at The Hills so he could not visit patients and give care. If that is so, it appears rather unusual given that it is the facility he sends his patients to post-surgery.
1637 After returning home, Mr Smith’s leg experienced oozing which subsided after several months. He gave evidence that he suffered greater pain than he had before the surgery, ongoing nerve pain, and persistent hypergranulation that became more aggressive in 2019. The hypergranulation has required regular debridement and treatment with silver nitrate.
1638 Ms Roberts was aware that Mr Smith suffered persistent hypergranulation following his surgery and that he was in touch with Dr Al Muderis’ rooms on many occasions about it.
1639 On 29 August 2018, Mr Smith texted Ms Roberts, “I’ve had another infection that has been treated with the same meds Mu[n]jed had me on in hospital”. He mentioned his stoma has a “lot of leaking fluid”. There appears to be no response.
1640 In a text message to Ms Roberts on 8 September 2018, Mr Smith sent a photo of his stoma with a message: “Is this normal??? I need some direction as this is starting to stink. No one up here seems to have an idea. Who do I contact? I don’t want another infection.” Ms Roberts replied: “Wash with Epsom salts bath. [The] [s]mell is normal body bacteria, you can use deodorant on it after a shower”. Mr Smith responded: “Ok thanks. Riding up to 5klm every second day and walking 1.6klm the other days. Awesome. Sockets are so yesterday.” I note that in submissions the applicant only referred to Mr Smith’s reply in the text exchange that day, and not the remainder of the messages relating to his request for help.
1641 On 11 September 2018, Mr Smith sent further photos to Ms Roberts, asking whether Dr Tetsworth can get rid of the granulation or whether a GP could do it. On 12 September 2018, she informed him “your GP can treat the granulation with silver nitrate, it may need a few treatments to resolve it”. On 13 September 2018, he asked if there is any other product that has the same function as silver nitrate, to which she says “[n]o, best to go to your GP”. Mr Smith then explained his GP was having trouble sourcing it. The next relevant text in the chain is 12 May 2019, which I return to below.
1642 In an email to Mr Smith on 25 September 2018, Ms Roberts writes: “Keep going with the silver nitrate, it may take a few treatments. Otherwise try soaking in epsom salt baths.” The email appears to be further to their text message conversation from 13 September 2018, as described above.
1643 On 2 November 2018, Mr Smith emailed Ms Roberts, complaining:
Gday Mate
Just a quick one to ask a few questions.
Firstly; I am continually having excess tissue growth out of the stoma and [I’]ve had it burnt off twice with silver nitrate stick, which hurts and burn[s] for two days. I am looking at another session next week as the exces[si]ve tissue growth presses against the internal stoma wall and creates a lot of pain when I walk. Is this normal, is [t]here some way to stop this from happening?
Secondly; I have heard that some surgeon in Melbourne has been able t[o] attach skin onto the rod in the femur thus closing out the stoma opening [f]ully. have you heard anything about this or has Munjed got this on his pot[e]ntial scope? …
1644 Ms Roberts did not remember this email and when asked if she responded, she said she did not remember. There is no evidence of a response.
1645 There is no evidence of any written communication between the time this request was made and 12 May 2019. On 12 May 2019, Mr Smith sent a text to Ms Roberts which she accepted in evidence was a plea for help. He wrote:
… I’m still having problems with excessive growth around and under the stoma. [I] have used silver nitrate for the tenth time and the pain and burning is intense.
I spoke with you last year and you said I couldn’t get operated on for a year. I’m wondering if I can get sooner than later get the laser surgery that you do around the stoma. …
1646 There is no evidence of any response. I note also that the next text message in the chain is 12 October 2020.
1647 The plain reading of the communications is that Mr Smith had an ongoing problem with hypergranulation. Some of the communications, although calling for a response, appear not to have been responded to.
1648 Mr Smith’s evidence was that he called Dr Al Muderis’ offices multiple times about the hypergranulation issue over several months. He got through to Ms Roberts on two or three occasions, who told him there was nothing they could do and that he should go to the RBWH. She said words to the effect of: “Use silver nitrate there is no other way”. Given the responses that Ms Roberts had given to Mr Smith via email and text message, and the apparent hiatus in those communications, there is a ring of truth to his evidence as to when he was able to speak to Ms Roberts and that, when he did, he was simply told to use silver nitrate.
1649 Mr Smith explained that he eventually gave up on contacting them because he would be given the same response, that is, to use silver nitrate. Silver nitrate, for the reasons Mr Smith gave in the written communications (and explained in his evidence), was practically ineffective (as the granulation would return).
1650 Mr Smith’s primary communication with Dr Al Muderis was via Ms Roberts, in significant part by text message and email. Given the contents of the communications, it can be inferred this was based on his expectation that Dr Al Muderis would be involved in any solution. On the evidence, the only advice he ever received was from Ms Roberts, who was not qualified to give medical advice.
1651 Dr Al Muderis accepted in cross-examination that he understood hypergranulation was a matter of persistent concern to Mr Smith.
1652 Mr Smith’s evidence was that he was ultimately driven to cut off his granulation tissue with a knife. One of the videos he had taken of doing so was part of the Broadcast. The metadata of the video in evidence establishes that it was recorded on 11 April 2022.
1653 Mr Smith’s evidence was that he had no other choice than to do the silver nitrate burning himself. He would sterilise his leg and remove the new excess growth with a kitchen knife in his bathroom. He did this many times, sometimes up to two to three times a week. Mr Smith explained he could not continually see his GP for assistance because he was working full time. He explained that he had to do the burning himself “because the amount of time it took to get there, get it done, then travel back to my work, I was going to lose my job”.
1654 Before returning to consider that evidence, it is appropriate first to address several other events for context.
1655 On 12 August 2019, Mr Smith was invited for a check-up with Dr Al Muderis at Leading Edge. He said Dr Al Muderis arrived with Ms Roberts many hours late. After some time, he spoke to Ms Roberts before Dr Al Muderis came into the room. Mr Smith told Ms Roberts that his mobility was fair, but the nerve pain was bad. He asked when the oozing/discharge would stop, her answer was soon and that it was a process. He also asked about the granulation. She told him that there was nothing he could do apart from silver nitrate.
1656 Mr Smith said that when Dr Al Muderis came into the room, he saw that he did not have his (Dr Al Muderis’) connector on his implant. Dr Al Muderis aggressively berated Mr Crampton for changing the connector which Dr Al Muderis said was not safety tested; he also criticised Mr Smith.
1657 Mr Smith gave evidence that Dr Al Muderis did not examine him. He denied telling Dr Al Muderis that he had no complaint about nerve pain. He denied that he did not have any discharge at that point. Mr Smith’s evidence was that he was experiencing both.
1658 Dr Al Muderis’ evidence was that although he noticed the connector, he denied becoming angry or aggressive. He counselled Mr Smith and Mr Crampton that the connector had not been safety tested for compatibility with his system and warned them of the risks. He said Mr Smith said that he was happy with the connector and did not want to change it. Dr Al Muderis’ evidence was that he observed that his stoma looked healthy, he was walking very well, and that Mr Smith expressed that he was very happy with his results.
1659 The consultation report from that check-up sent to Mr Smith’s GP states, in its entirety:
Progress review:
Brennan is one year down the track post-osseointegration. I am so glad that he is back at work and he is now Gold Card veteran and the wound looks very good. I don’t have a new x-ray but he is walking very well and his life has changed dramatically. He is very happy with the results and I am very happy with the results.
Plan of management:
I will see him again in another year and I will keep you posted.
(emphasis in original)
1660 Dr Al Muderis’ evidence as to what occurred appears to have been based on the brief consultation report. Yet that description appears to bear no meaningful correlation with what Mr Smith had been experiencing since his surgery, as reflected in the repeated messages referred to above and what he communicated to Ms Roberts at Leading Edge. It discords with what Mr Smith said occurred at the consultation and what his condition was at the time. It is improbable that, given the texts and emails, that Mr Smith would not have raised his issues with granulation and oozing. Rather, the report presents an entirely positive picture of his progress in circumstances where Mr Smith had repeatedly raised issues related to his surgery.
1661 This is also in a context where Mr Smith sought a second opinion from The Alfred which appears to have occurred in October 2019 (there is no documentation in evidence). His evidence was that he sought assistance with neuromas and granulation. He gave evidence that The Alfred conducted scans which confirmed an infection had not gone into the bone. Mr Smith asked if they could operate to stop the nerve pain, remove the neuromas or perform TMR. He was told the staff first had to discuss it. He later received a phone call from The Alfred saying they could not help him. When he pressed for an explanation, he said Mr Steven Gray, an employee of The Alfred, said words to the effect of: “We can’t operate on patients Munjed has operated on” (I note Mr Smith’s evidence relates to the fact that was said to him, not the truth of what was said).
1662 On 10 October 2020, Mr Smith’s dual cone snapped while walking in a cross-fit challenge. Mr Crampton reached out to Dr Al Muderis asking him to help and he responded promptly. Mr Smith travelled to Sydney for Dr Al Muderis to replace the dual cone.
1663 Mr Smith gave evidence that Dr Al Muderis said to him words to the effect of: “I could do it in the ward, but it has to be done in the theatre, due to regulations” and “I’ve even changed people’s snapped rods in car parks and airport toilets”. Mr Smith gave evidence that, while under general anaesthetic for changing the dual cone, Dr Al Muderis changed his connector without his consent. This is in the context where, as described above, Mr Smith said that Dr Al Muderis had previously made it clear he was unhappy that he was not using his connector.
1664 On 20 October 2020, Mr Smith emailed Ms Roberts:
… Thanks for getting me in on a quick turnaround for the operation, I really appreciate it. Secondly all the best for the birth of your child. Hope all goes well and you have a great happy future together. …
1665 Mr Smith gave evidence that in April 2022, another amputee recommended he see Dr Wines. Mr Smith and Dr Wines initially conversed via telephone and email. A report dated 3 May 2022 stated Mr Smith required hospital admission for thorough debridement of his excessive granulation tissue and intravenous antibiotics. On 12 May 2022 he attended a consultation with Dr Wines. Mr Smith’s GP apparently referred him to Dr Wines in the intervening period. The report from Dr Wines describes abundant granulation tissue around his prosthesis with haemosiderous ooze. Dr Wines texted Dr Al Muderis that day:
… Just letting u know I’m taking BJ Smith to theatre today as he has been struggling with excessive granulation tissue and purulent discharge. Please let me know if u have any advice. …
1666 Dr Al Muderis responded asking for photos, and one was sent by Dr Wines. Dr Al Muderis texted: “Looks [a] bit angry I agree he would need debridement” and asked to be kept posted.
1667 On 20 September 2022 (two days after the Broadcast), Mr Smith saw Dr Tetsworth. It was put to Mr Smith that he telephoned the hospital for an appointment in July 2022. He said he could not remember doing that. There is no documentary evidence of when the appointment was made. Mr Smith explained it was difficult to get an appointment with Dr Tetsworth, and Dr Tetsworth’s evidence was that an appointment of this nature would have been scheduled several weeks prior.
1668 The examination on 20 September 2022 confirms the state of Mr Smith over four years after surgery. Dr Tetsworth describes in his report:
… he has what I consider a persistent localised infection of the distal end of his femur and even more problematic is his continuing pain. He did undergo targeted muscle reinnervation by myself at the Royal Brisbane in November 2020 but still has significant complaints of pain both anteromedial and posteromedial on the distal end of the residual limb. He does not complain of much phantom limb or phantom pain, but it is instead well localised to the distal end of the stump as noted. …
Plain radiographs were quite revealing in that the distal end of the implant near the stoma exhibited substantial periosteal thickening of the femoral shaft, as well as an expansion of the bone to essentially a trumpet shape that was no longer in contact with the implant. In three dimensions this results in a protected micro-environment where bacterial colonisation can sometimes proliferate, resulting in a persistent low-grade infection. This is certainly consistent with his history of hypergranulation and continued drainage with episodic local inflammation that responds to short courses of oral antibiotics. He manages the hypergranulation with self-administered silver nitrate topically PRN as well as occasionally performing limited debridements of hypergranulation tissue himself, using a “kitchen knife”.
1669 The report also states that, having discussed his findings with Mr Smith, “… we agreed that given the significant pain as well as the recurrent localised infections and hypergranulation that this was not an ideal situation”. The respondents aptly describe that conclusion as an understatement.
Specific submissions
1670 Turning to some specific submissions.
1671 First, the applicant submitted that the evidence does not establish that the granulation Mr Smith suffered was as severe as he now claims. The applicant referred to photographs which he said the respondents put forward as evidence of the granulation tissue. He submitted that when these photographs were shown to Dr Al Muderis in cross-examination, he explained that some showed epithelialised tissue rather than granulation, others showed only some granulation tissue, and he described the appearance of the stoma in many of the images as “beautiful”.
1672 Dr Al Muderis took issue with the photos showing anything other than “very minor” granulation, although he accepted Mr Smith required regular treatment with silver nitrate. Dr Al Muderis said the treatment is not normally painful. He understood that Mr Smith was concerned about granulation tissue and that he raised that issue several times with Dr Al Muderis and, on a few occasions, other clinicians.
1673 Mr Smith gave evidence that he considered he had no choice but to use a knife to remove granulation tissue himself, recording a video of him doing so on 11 April 2022. Dr Al Muderis described what he saw in the video as a “very tiny area of granulation tissue that is less than one centimetre that could have been treated with silver nitrate”. Yet by 12 May 2022, Dr Wines’ report stated that surgery was required to remove what he described as abundant tissue. Dr Al Muderis agreed debridement was needed. On 20 November 2022, Dr Tetsworth’s examination found Mr Smith was experiencing significant pain, recurrent infections and aggressive hypergranulation, which is consistent with Mr Smith’s descriptions.
1674 The applicant’s submission does not address the text and email messages referred to above (see [1643]-[1645]), where Mr Smith was plainly seeking assistance. He wrote contemporaneously of his complaints. As explained, Ms Roberts accepted that Mr Smith was experiencing persistent problems with hypergranulation and that one message was a plea for help. The submission also does not address the evidence of Mr Smith’s consultations with Dr Wines and Dr Tetsworth.
1675 The applicant’s submissions – that Mr Smith had never complained to him, that there was never any complaint until after he became a subject of Ms Grieve’s investigation, and that his last communication with him was positive – suffer from the same flaw.
1676 Mr Smith sought opinions from The Alfred in 2019 and Dr Wines in April 2022. It can be inferred that Mr Smith was unhappy with Dr Al Muderis’ care. He had stopped contacting his office for help with the problems he was experiencing. Messages went unanswered, and if he had a response, it was from Ms Roberts, who told him the same thing: use silver nitrate. His pleas for assistance, as he said, were ignored. That in 2020 Dr Al Muderis attended to Mr Smith’s broken dual cone (as his surgeon), does not alter that. His post-surgery complications were ongoing and unaddressed.
1677 Mr Smith’s evidence as to his experience with granulation is supported by other evidence. I accept his evidence. This was an ongoing serious issue for Mr Smith. I do not accept the applicant’s submission which suggests that Mr Smith is concocting its severity. The submission of a recent invention or concoction cannot be sustained. The contemporary records, and his actions, establish otherwise.
1678 Second, the applicant submitted that if Mr Smith developed significant granulation tissue, a contributing factor is likely to have been the fact that he led an active lifestyle. That submission relies on Dr Al Muderis’ evidence that Mr Smith’s active lifestyle is likely to have promoted the growth of granulation tissue. I note Dr Al Muderis separately deposed that higher levels of activity can provoke the development of granulation tissue.
1679 That submission, which was used to imply that Mr Smith is to blame if he did have hypergranulation, cannot be accepted. Osseointegration is promoted on the basis that a person can walk and be active. The photographs of osseointegration patients used in presentations and brochures (some of which Ms Roberts showed to Mr Smith) makes that plain. In any event, that Mr Smith is active does not alleviate that this is a matter adversely affecting him, which the applicant did not address.
1680 In circumstances where Dr Al Muderis deposed that higher levels of activity can promote granulation tissue, where he promoted osseointegration as a means of supporting an active lifestyle (to Mr Smith and others), and where Mr Smith expressed interest in osseointegration partly because he wanted to pursue such a lifestyle, there is an issue as to whether Dr Al Muderis warned Mr Smith of the risk of activity-related granulation. Mr Smith denied being told that his increased activity would increase his granulation tissue. There is no evidence to the contrary. I accept he was not warned of this.
1681 I note that Dr Tetsworth, in his 20 November 2022 report, commented that Mr Smith’s history of hypergranulation was consistent with his stump hosting “a protected micro-environment where bacterial colonisation can sometimes proliferate, resulting in a persistent low-grade infection”. Dr Anstee opined that there was too much mobility of the skin around the implant which invites infection and encourages the growth of granulation tissue. Dr Al Muderis refused to accept that mobility invites infection and the growth of granulation tissue, although he conceded that mobilisation may encourage the growth of granulation tissue.
1682 Third, the applicant submitted the suggestion that Mr Smith had no choice but to do the silver nitrate burning himself was “absurd”. He submitted he could have gone to other doctors, including Dr Tetsworth and the doctors at the RBWH, which he frequently did. Therefore, the applicant submitted, it was Mr Smith’s decision to burn the granulation tissue off with silver nitrate at home and use the knife.
1683 Leaving aside that Mr Smith’s evidence was that he could never get through to Dr Tetsworth and that he could not contact him directly (noting that Dr Tetsworth himself described the appointment that Mr Smith sought in September 2022 as one that must be booked weeks ahead), the applicant’s submission misses the point. Mr Smith had concerns he would lose his job if he did not treat the hypergranulation himself, given the frequency with which this issue arose and the time needed to attend appointments. As he explained, the only way he could get to a doctor for silver nitrate treatment was to take time out from work and travel some distance, putting his employment at risk. This was four years after the surgery. There was no sign of the problem dissipating. Mr Smith gave evidence of the frustration that led him to doing what he did. I accept that he genuinely felt that way.
1684 Similarly, the applicant’s submission that Dr Wines’ reports fail to corroborate that Mr Smith needed to cut his skin fails to grapple with the evidence of the circumstances in which he came to take matters into his own hands. Dr Wines’ report supports Mr Smith’s evidence as to his condition.
1685 The applicant’s submissions fail to grapple with the consequences of complications on a patient, and the impact physically, mentally, and financially, they can have.
1686 Fourth, the applicant submitted that there was no failure to provide post-operative care for Mr Smith, including in relation to granulation, where he was under the care of local practitioners in Queensland. The applicant pointed to his cross-examination (in answer to a question about his involvement in Mr Smith’s rehabilitation program), where he explained “medical practice in Australia doesn’t work that way”, because systems exist to ensure continuity of care without one practitioner having to be personally responsible for everything to do with the patient.
1687 That may be so: Dr Anstee gave evidence that, if a patient moves interstate (or overseas), it is reasonable to refer management of their care to a qualified person in that other location.
1688 Yet Dr Al Muderis’ office, in continuing to provide medical advice and administrative support to Mr Smith after he had left for Brisbane (via Ms Roberts), evidently created an expectation in Mr Smith’s mind that Dr Al Muderis was his primary surgeon. There is no evidence Dr Al Muderis’ office referred Mr Smith to a local surgeon in Brisbane. Mr Smith’s evidence was that, while in Brisbane, “because Munjed did the surgery … I would contact Claudia if I needed something”. That Mr Smith found it difficult to contact Dr Tetsworth seemed to solidify that expectation; he preferred to contact Dr Al Muderis’ office rather than Dr Tetsworth. As noted above, Dr Al Muderis organised a check-up with him on 12 August 2019 in Queensland. He also flew to Dr Al Muderis in Sydney when he needed his broken dual cone replaced in 2020.
1689 Dr Al Muderis conducted Mr Smith’s osseointegration surgery, and while interstate, Dr Al Muderis sustained an expectation that he was Mr Smith’s primary caregiver (relating to osseointegration). Dr Anstee’s evidence on the scope of a surgeon’s responsibilities is instructive:
… as surgeon, if you take on a patient and operate on them, then you are stuck with that patient …
Complications happen. However, when they happen it is the job of the surgeon to manage the complication, even if it is not the surgeon’s fault.
1690 Fifth, the applicant put to Mr Smith that the continuing pain he experienced well after osseointegration surgery was no worse than his pain before the procedure. It is unclear the basis on which this question could be put. In any event, Mr Smith disagreed. I accept Mr Smith’s evidence. I note some other patients also gave evidence that the pain they experienced was worse after having had the surgery (e.g Ms Mattiske and Mr Warland).
1691 Sixth, Mr Smith accepted he was informed of some risks and complications, but not to the extent that he has experienced. To submit that Mr Smith was aware of granulation, is not to the point. Mr Smith’s evidence is he was not warned about granulation to the extent he has experienced it, that is, with an ongoing need for treatment, which must be done frequently and is painful. Indeed, the applicant has not pointed to any evidence to the contrary. A significant part of the applicant’s submission about advice given on risks and complications relies on what he was told elsewhere, or what was in brochures he was said to have received. Leaving aside the question of whether Mr Smith received the brochures, as none were put to him, they do not address the point. More importantly, that is not a substitute for advice on risks and complications for such an intrusive, and life changing elective surgery. It is not a sufficient basis to obtain informed consent. As referred to elsewhere, Dr Ruff explained a brochure is no substitute for a doctor ensuring the patient is told and understands the risks and complications of the surgery. There is no evidence Mr Smith was warned about his pain being worse than before the operation and potentially persisting for years, including, amongst other things, recurrent infections and hypergranulation.
1692 I am satisfied that Dr Al Muderis failed in those circumstances to adequately inform Mr Smith of the risks associated with the surgery. I note that Mr Smith had a confirmed surgery date and had prepaid for the procedure before Dr Al Muderis had a consultation with him (excluding the hotel lobby meeting). Mr Smith agreed to the surgery not having been properly informed of the risks, and as such, his consent was not informed. As evident from the discussion above, his aftercare was lacking (in particular in relation to his hypergranulation). In the circumstances, I am satisfied that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Ms Rowena Mattiske
1693 In May 2004, Ms Mattiske sustained a serious injury to her ankle when she slipped off a footpath and broke her talus bone. Between then and 2014, she underwent about 20 major operations attempting to return her foot to its pre-injury condition. Ms Mattiske’s evidence was that during this time in 2010, she was diagnosed with PTSD and an adjustment disorder and had ongoing psychiatric and psychological treatment for these conditions. In September 2014, Ms Mattiske elected to undergo a below-knee amputation of her right leg due to ongoing issues, which resulted in escalating pain levels from her injury and a removal of about a third of her leg. Approximately one year later, she started to experience nerve pain in her right knee and stump, which prohibited the use of a socket limb. She gave evidence that her pain escalated and required frequent ketamine treatments. Ms Mattiske heard about Dr Al Muderis in around October 2015, through her rehabilitation doctor at the time. In 2016, Ms Mattiske underwent two-stage surgery with Dr Al Muderis: the first stage being a total right knee replacement in June 2016 and the second stage inserting the implant in September 2016. In May 2023, the implant was removed by Dr Wines, Dr Huang and Dr Tim Wang. She was about 62 years old at this time.
1694 The applicant’s closing submission is that Ms Mattiske concocted parts of her evidence after contact with Ms Stewart and Ms Grieve. I note, however, that Dr Al Muderis, in evidence, asserted that Ms Mattiske’s change in attitude was a result of Mr Grant and Dr Wines. In any event, during the applicant’s cross-examination, he accused Ms Mattiske of giving false evidence or lying (including asserting one aspect was a “shameless lie”). In written closing submissions, the applicant submitted she was a poor witness, an unreliable historian and that her version of events was repeatedly contradicted by contemporaneous documents, including her own contemporaneous statements. He submitted that: Ms Mattiske’s answers were often drawn out with irrelevant, unresponsive details; there was substantial exaggeration and dramatisation of events; Ms Mattiske discussed her evidence with Ms Stewart, and even asked Ms Stewart to “coach” her; and the messages between Ms Mattiske and Ms Stewart went beyond discussion of the process of giving evidence and were replete with Ms Mattiske asking Ms Stewart to remind her of details about her interactions with Dr Al Muderis.
1695 The respondents submitted that Ms Mattiske was reliable and credible, her evidence ought to be accepted, and that there was no reason for her to lie.
1696 Ms Mattiske has no reason to make up evidence. She has nothing to gain from these proceedings. Rather, by giving evidence she had to endure lengthy cross-examination, while in pain, in which she was accused of lying. The submission that Ms Stewart somehow “coached her” by telling her what to say, is not supported by the evidence referred to by the applicant. I accept Ms Mattiske’s evidence of what she meant by the text sent to Ms Stewart on that topic. As to the submission that her evidence is inconsistent with her contemporaneous documents, that proceeds in large part on an interpretation of those documents (emails, texts etc) that one cannot be active and participate in life, yet also be suffering. As I discuss below, this is also in a context where Ms Mattiske was aware, from her first consultation with Dr Al Muderis, that he was concerned about the prospect of her complaining which, given the conversation, would caution her against doing so (as discussed below there is evidence supporting a conversation to that effect). I note the applicant relies on Ms Mattiske’s evidence when the answer is perceived to be favourable to him, but when it is not, her reliability is challenged. I regard Ms Mattiske as an honest witness. That said, I accept that Ms Mattiske is a poor historian in relation to some matters. I have focused on the documentary evidence, which also includes contemporaneous messages from Ms Mattiske to Dr Al Muderis detailing her symptoms at various times.
1697 Turning to some of the specific issues raised in her case study.
Risks and complications
1698 The respondents alleged that Ms Mattiske was not properly warned of the risks and complications of surgery. They contended that Ms Mattiske was misled, because Dr Al Muderis did not inform her that osseointegration was not a pain-relieving procedure, in circumstances where pain reduction was expressly said to be a significant issue for her. The respondents submitted, relying on the consultation notes of Dr Basten, and the pre-operative report of Dr Paterson, that Dr Al Muderis was aware that Ms Mattiske had significant pain issues and that one of her key goals from surgery was pain relief.
1699 To elaborate, on 11 November 2015, Dr Basten had a consultation with Ms Mattiske, with his report recording her issues with pain. As the respondents correctly described, the focus of the report was Ms Mattiske’s significant issues with pain. Dr Basten recorded that her main goal for the surgery was pain reduction. He detailed her history of pain since her injury, the recent extent of that pain, and the treatments undertaken, including through medication and a pain psychologist. He concluded:
… there are a few issues that the team should be cautious of and investigate before proceeding with therapy. Firstly, her pain is an issue from a number of perspectives. She is somewhat sensitised to pain now and she is resting her hopes optimistically on surgery reducing or removing her pain. If she continues to have pain, Rowena would be disappointed and may get more depressed.
1700 Dr Basten’s conclusion about Ms Mattiske seeking a reduction in pain more generally was consistent with Dr Paterson’s report to Dr Al Muderis on 12 November 2015, which listed Ms Mattiske’s objectives from the surgery as follows:
Rowena hopes to look at ways to both reduce her pain but also to reduce her requirement on medications as well as possibly improving her mobility, which at the time of writing is limited due to her inability to wear a prosthesis.
1701 At that time, Ms Mattiske had two pain specialists.
1702 Dr Paterson similarly framed his conclusion in terms of Ms Mattiske’s pain:
… given the issues with her pain sensitisation I believe that some time between surgical procedures should be considered and optimisation of non-interventional pain management ie trialling mirror box therapy, mindfulness techniques and graded exposure is also to get Rowena better reconditioned.
I feel that we should review Rowena in 3-6 months after a period of conservative management at which juncture we can reconsider the potential role for the osseointegration procedure.
1703 Ms Mattiske attended her consultation with Dr Al Muderis on 12 November 2015. The consultation report records Dr Basten and Dr Paterson were present. The consultation report states that “[c]urrently Rowena’s main concerns are related to the disabling pain caused by wearing the socket and the prevention of mobility”. That does not accord with the descriptions as to the sources of pain recorded in Drs Basten’s and Paterson’s reports. Those consultations, which were contemporaneous, describe much broader, significant pain issues. These included, inter alia, residual limb pain, phantom limb pain, spasmodic pain surges, stump pain with neuropathic descriptors and significant pain sensitisation secondary to multiple procedures. The references elsewhere in the report to her reporting chronic pain, are not confined to socket pain. The inaccuracy in Dr Al Muderis’ report as to her issues of pain, given both his colleagues raised the issues of her pain, is concerning.
1704 There are other issues that arise from the contents of the report. For example, Dr Al Muderis’ report contains the pro forma list of risks that appear in some other reports but then states that Ms Mattiske “does understand the risks associated with this surgery”, that she is regarded as “relatively low risk” and that her “procedure would be very standard”. In the report, he also notes that Ms Mattiske is overweight and categorised as obese, (which I note can be issue for undergoing osseointegration surgery). Dr Al Muderis said in cross-examination that Ms Mattiske was a “complex patient from the physical point of view”. It is difficult to understand how the description of being a “relatively low risk” and “very standard” procedure could apply to a case with such complexities. As the respondents submitted, that report understates Ms Mattiske’s medical position, as apparent from the reports of Drs Basten and Paterson.
1705 Further, the description of it being a “very standard” procedure, which Dr Al Muderis maintained in cross-examination, is inconsistent with his recommendation to complete the two-stage procedure described above, “comparatively to the OGAAP single stage protocol” and the observation “she may be required to spend more than usual time in the hospital/rehabilitation facility”. Osseointegration incorporating a knee replacement, from Ms Mattiske’s understanding, was very new. She said that there was little to no publicly available information about the procedure and so she relied on Dr Al Muderis. Dr Stalley referred to the procedure as not being well documented, within the “experimental range” and a “most unusual surgery”. He remarked that because the osseointegration component communicates with the knee joint, if there is contamination of the osseointegration component, there would be an “extraordinarily high likelihood of developing secondary infection in the knee”. Dr Leung similarly described it as “unusual”, also noting that if the knee joint prosthesis was incorporated in the osseointegration implant, it would imply that the knee joint was in “direct communication to the stoma and external environment, which would increase the chance of knee joint prosthesis infection”.
1706 The applicant referred to Ms Mattiske’s evidence, where she agreed in cross-examination that she told Dr Al Muderis during the consultation that her aim of osseointegration was to improve her mobility. The applicant also referred to Ms Mattiske’s affidavit, where she deposed that she was “desperate to walk again”, pointing out that it does not refer to her having any expectation about pain relief. However, as the applicant repeatedly submitted, reliance should be on contemporaneous documentary evidence. At that point in time, Ms Mattiske also expressed desires about pain relief (evident in the reports of Drs Basten and Paterson). There is no reason to suggest that was not also a genuinely held desire at that time. The two are not mutually exclusive, because as Ms Mattiske explained, her pain was “all-consuming”.
1707 The applicant also referred to a Facebook post published on 31 January 2016, in which Ms Mattiske said she met with Dr Al Muderis and his team and commented, “[m]aking me walk again he said would not be a problem but reducing my pain that he couldn’t do … But of course would try his best”. The applicant submitted it could be inferred from this post that Dr Al Muderis had an explicit discussion with Ms Mattiske at the consultation about the fact that osseointegration would restore her mobility but would not reduce her pain. The respondents submitted it was evident that Ms Mattiske was talking about her existing pain. I accept the applicant’s submission that the Facebook post does give rise to the inference that there was some discussion about pain, which Dr Al Muderis said he could not reduce. I note that it appears from the Facebook post that he also said in that context that he “would try his best”, which somewhat undercuts the message to her that he could not reduce her pain. The respondents also submitted that Ms Mattiske’s evidence was that she never understood that her pain would get any worse or more intense than what it was. I accept that evidence. It is consistent with the evidence of other patients (e.g. Mr Smith and Ms Çalan). There also is no evidence that Dr Al Muderis warned Ms Mattiske that might occur, being a risk, which in her circumstances, would have been particularly concerning.
1708 Given the terms of the Facebook post, and contrary to the respondents’ submission, it has not been established that Dr Al Muderis did not advise her it would not reduce her pain. As to walking again, the Facebook post reflects the confidence with which Dr Al Muderis spoke to her about the surgery being successful in achieving that.
1709 That said, there were real concerns raised in the reports of Dr Paterson and Dr Basten about the significant pain issues experienced by Ms Mattiske. Her issues with pain were significant, and necessarily a factor in considering surgery. In that circumstance, any advice given to her as to the risks of the surgery, would need to address the impact of the proposed surgery on that pain. Ms Mattiske ought to have been fully informed that osseointegration surgery may result in a higher level of pain. She was not. As she said in evidence, she was not told that might happen, and it is not what she signed up for. I accept Ms Mattiske’s evidence that after the osseointegration surgery and over time, her pain became worse than it had been before the surgery. As explained below, her distress at the level of pain she experienced is supported by contemporaneous evidence.
1710 A final matter in relation to the consultation. Ms Mattiske did not recall a discussion about the risks and complications, except to a limited extent. At this consultation she was provided with a handout about osseointegration, but it was generic and did not deal with any risks or complications of the surgery. Her evidence was that at some stage, although it is unclear when, she was warned about infection, as she said that she was to look for signs of infection, pain, ooze and redness. In the consultation report there is only the pro forma list of risks. The consultation report then merely states that Ms Mattiske “does understand the risks associated with this surgery, however we regard [her] as a relatively low risk”.
1711 In his affidavit, Dr Al Muderis does not refer to any discussion of risks in this consultation but rather referred to Ms Mattiske having signed a consent form for the osseointegration surgery which “outlined a number of risks and explained that the procedure may not give the expected result”. The consent form exhibited to his affidavit does not outline the risks of osseointegration. As to the pro forma list of risks set out in the consultation report, although the applicant conceded that risk of infection is not specifically referred to, he submitted that the list included matters that are all consequences and treatments for infection, and so “it follows from the fact that these were discussed that infections, both minor and serious, must have also been discussed”. However, in cross-examination, it was put to Ms Mattiske that it was Ms Bosely who explained to her the risks and complications. Ms Mattiske had no recollection of such a discussion. The applicant’s closing submission that Ms Mattiske was advised of the potential risks of osseointegration is based on her being told about the risks and complications by Dr Al Muderis, his colleagues or staff and the provision of handouts. I note that after that first consultation with Dr Al Muderis on 12 November 2015 when she was told she was suitable for the procedure, Ms Mattiske was taken to speak to Ms Bosley, and on that day she signed the consent form for surgery and estimate of fees and was booked into surgery. On the applicant’s case, whatever Ms Mattiske was told about risks and complications, it occurred on the same day she agreed to this surgery. Given the significance of the surgery and the complexities of her case, that allows no time for proper consideration. Ms Mattiske’s take away from the consultation is expressed in the Facebook message referred to above, “[m]aking me walk again [Dr Al Muderis] said would not be a problem”.
1712 In terms of chronology, I note also, as referred to above, that Dr Paterson’s report of 12 November 2015 expressed the opinion that Ms Mattiske ought to be reviewed in three to six months after a period of conservative treatment before reconsidering osseointegration. However, in his consultation report with Ms Mattiske which occurred that same day, Dr Al Muderis expressed the opinion, inter alia, that he believed the procedure was “necessary”. That report does not refer to Dr Paterson’s opinion, or address any of the concerns he had expressed in his consultation report. Nor does he refer to the issues raised by Dr Basten in his report of 11 November 2015 which led him to opine that the team should be cautious and investigate before proceeding with therapy. Further, in circumstances where the surgery was not urgent, there is no evidence any more conservative treatment options were to be considered. Rather, Ms Mattiske went from Dr Al Muderis’ consultation to meet with Ms Bosley, at which stage she signed consent forms for the surgery.
Post-surgery
1713 The applicant submitted that Ms Mattiske: had pre-existing pain before she met Dr Al Muderis; was not previously walking and had little prospect of walking again without osseointegration; underwent osseointegration because she wanted to walk; was told by Dr Al Muderis that it was not a pain-relieving procedure and she had no expectation of pain relief from the surgery; after osseointegration, and “notwithstanding bumps along the way”, was able to walk for six years, which enabled her to lead a fulfilling life, returning to the outdoor activities she enjoyed and making two major overseas trips to Europe and Canada; was a seemingly happy patient right up until May 2022 when she had a stump refashioning with Dr Al Muderis, and weeks before she was first contacted by Ms Grieve and reconnected with Ms Stewart; did not raise any complaint with Dr Al Muderis until after the defamatory Broadcast; and had the implant taken out, can no longer walk, and is still in pain (which has increased since the implant was removed).
1714 There is a simplicity in those submissions. It brushes aside and downplays the very many issues referred to above, which she endured, as mere “bumps” along the way.
1715 It is plain Ms Mattiske has suffered much over the years since she first had surgery with Dr Al Muderis: multiple further surgeries, repeated infections requiring antibiotics, significant pain, several trips to the emergency ward, a further amputation, hypergranulation as well as multiple TMR surgeries and aspirations, many of which required weeks of rehabilitation and recovery in hospital. This began shortly after the surgery. By about November 2016, Ms Mattiske had started to develop deep chronic pain in her right leg, was admitted to the RBWH on 13 December 2016 and was discharged three days later. She was again admitted to the same hospital on 27 December 2016 with pain, reduced range of movement, an infection and septic arthritis in her knee joint and was put on intravenous and oral antibiotics for six weeks. Dr Tetsworth performed an aspiration on 28 December 2016 as well as a washout, revision and debridement of her right knee prosthesis on 29 December 2016. I note that although the applicant challenged Ms Mattiske’s evidence as to her pain being worse after she underwent osseointegration surgery, a consultation report of Dr Al Muderis dated 2 February 2017, states:
Irrigation debridement of her right knee was performed six weeks ago. She was doing better but is now having pain and stinging in the knee. She is taking a lot of narcotics. She states she cannot walk from the pain and weakness. She is currently in a wheelchair.
1716 In any case, leaving aside the issue of pain, that she experienced those post-operative events cannot be in contention, as they do not depend on Ms Mattiske’s evidence. Moreover, that in some periods thereafter, particularly in the earlier period of 2017 and 2018 (and before the further amputation), Ms Mattiske was active and walking, does not alter or undermine her evidence of the suffering that she endured. In Ms Mattiske’s own words: “just because I live[d] an active life doesn’t mean to say that I was not without pain”.
1717 Jumping ahead, in November 2022, there were text exchanges between Ms Mattiske and Dr Al Muderis. This occurred after the Publications in circumstances where Dr Al Muderis was aware, in October 2022, that Ms Mattiske had sought a second opinion from Dr Wines (who had contacted Dr Al Muderis). It appears from the text messages exchanged on 17 October 2022 that Dr Al Muderis had tried to call Ms Mattiske, but she responded by text, confirming that she was seeing Dr Wines for a second opinion. In this series of messages, Ms Mattiske wrote on 6 November 2022:
Munjed Thankyou for the letter very detailed n thorough … I really appreciate the information.
Munjed the truth is I’m actually not mobile. I live in my chair all day everyday. I only put the leg on to walk down the stairs if I absolutely have to, stand to hang washing n get in n out of pool. When standing the femur bone aches … n the weight of the leg on while sitting in the chair makes my pain go crazy …
Also over the past 6 yrs Munjed I have had 12 surgeries! 8 by you n 4 by KT [Dr Tetsworth] … n since the above knee amputation I’ve hardly walked at all n the pain continues to intensify … despite intervention. Of course I want to walk but right now I don’t care anymore … Munjed I expressed that to u that I wanted the rod out when I was down in April/May … you laughed at me n said ‘You wouldn’t do that!’ Munjed I don’t complain unless it’s really bad l told you that from the very 1st consult when we 1st met. But when you, my surgeon whom I’ve placed my trust n whole life into his hands laughs at you it wounds very deep. Munjed if Claudia had the lack of life like I have and her surgeon laughed at her you would be furious!!! It gets so bad Munjed I have days where I can’t do it anymore n want to die in my sleep…. You know I’m a fighter n I have battled for 18 1/2 yrs now but I’m truly exhausted …. I hope that explains my story a little more
Ro
1718 In one of Dr Al Muderis’ responses, he apologised if Ms Mattiske “felt” that he laughed and acknowledged there was an occasion when he saw Ms Mattiske in the corridor of the hospital where she said she was in pain. Regarding this occasion, he wrote that he said (at that time) he would not want to remove the implant. He concluded the text with a statement that he would love to help her to be pain-free and to be able to walk again. In response, Ms Mattiske texted, inter alia, that she wanted to share with him “what it’s like on the other side of the fence and give [him] suggestions”, that she knows he cares, but “sometimes life [and] busyness just get in the way”. He agreed that being busy can get in the way.
1719 At a practical level, care needs to be taken with these messages. Dr Al Muderis’ responses are in a context of him having instituted these proceedings. His responses are remarkably prompt and deploy language designed to have her regard him highly. They are even flattering of her at times.
1720 There are four matters to note from the messages: first, Ms Mattiske said at the first consultation, she told Dr Al Muderis that she would not complain, which is addressed further below; second, his acknowledgement that there was a reference or some discussion as to her implant being removed, which is also addressed further below; third, his acknowledgment of the effect of being busy, despite his claims that being busy did not affect his ability to care for his patients; and fourth, his attempts to have Ms Mattiske return to his care, including he “would love to help [her] be pain-free and being able to walk again” (emphasis added) in circumstances where he repeatedly said in evidence that he is not a pain specialist and osseointegration surgery does not reduce pain.
1721 Turning first to the fact that in the message extracted above, Ms Mattiske reminded Dr Al Muderis that in her first consultation, she told him she does not complain. She gave evidence that during that consultation, Dr Al Muderis said that as her case was complicated, he was concerned that she might complain about things such as pain, as another patient had done. Dr Al Muderis denied this. It is timely to recall the applicant’s closing submission that Ms Mattiske concocted complaints after contact with Ms Stewart and Ms Grieve, because she had not previously raised complaints with Dr Al Muderis before that time. However, this discussion supports that the issue of complaining was pre-emptively raised. The penultimate sentence in the last paragraph of the message extracted below at [1728] also suggests that a conversation with Dr Al Muderis against complaining rings true.
1722 Turning then to the conversation about the implant being removed. As evident in one of his text responses to Ms Mattiske’s message extracted above, Dr Al Muderis accepted that there was an occasion Ms Mattiske referred to, where reference was made to her implant being removed. Ms Mattiske refers to it as having occurred in April or May 2022. The last occasion Ms Mattiske had been in hospital in Sydney with Dr Al Muderis before she sought a second opinion, was in May 2022. As at that time, Ms Mattiske’s position was so dire from her perspective, that she wished for the implant to be removed. Notably, this occurred before she had any contact with Ms Stewart, Ms Grieve, Dr Wines or Mr Grant. Ms Mattiske was, to say the least, very unhappy about the position she was in.
1723 That is not surprising given that (further to what is described above) since early 2019, Ms Mattiske had undergone many surgeries and procedures: on 27 February 2019, Dr Al Muderis operated in Sydney to realign her right kneecap, and a month later on 26 March 2019, Dr Tetsworth performed an aspiration of her right leg in Queensland; on 21 August 2019, Dr Al Muderis performed TMR surgery in Sydney in relation to painful neuromas in her right leg; on 4 October 2019, Dr Al Muderis performed realignment surgery in Sydney on her left knee, following which she had another aspiration in Brisbane on 18 October 2019; on 28 February 2020, Dr Al Muderis aspirated a large haematoma on her right knee in Sydney (in a consultation room); on 17 March 2020, she underwent another aspiration at the RBWH; on 31 March 2020, Ms Mattiske developed cellulitis in her left leg, which was treated in hospital on the Sunshine Coast; on 13 July 2020, Dr Tetsworth revised her right knee replacement (which had been mechanically dislodged from the tibial tray, which Dr Al Muderis described as a “catastrophic failure”) and identified mobile metallosis throughout the knee replacement; on 12 August 2020, Dr Al Muderis performed a right above-knee amputation and transfemoral osseointegration in Sydney; on 25 September 2020, Dr Al Muderis performed a stump refashioning and debridement; on around 28 January 2021, a procedure was undertaken to burn off hypergranulation with silver nitrate; and on 18 May 2022, Dr Al Muderis performed a right stump refashioning and sciatic nerve and saphenous TMR at Macquarie University Hospital.
1724 The mere recitation of those events, which is supported by contemporaneous records, reflects the serious state of her situation. I note that for many of these procedures, Ms Mattiske was required to rehabilitate for various periods ranging from days to weeks post-procedure, as well as travel interstate to see Dr Al Muderis, which according to her evidence required her to fly to Sydney, find and pay for her accommodation and arrange and pay for transport to his clinic.
1725 In addition, throughout this period, there were ongoing infections. It may be accepted that on some occasions when blood tests were performed, the results were normal. However, the symptoms she was experiencing were such that tests were undertaken. I note for example, as the respondents submitted, Dr Al Muderis resisted suggestions of infection when shown a photo texted by Ms Mattiske on 31 August 2020 of her leg, which was swollen, sore and had smelly “muck” coming out of it (as described by her in a contemporaneous text message). However, in response to that message, Dr Al Muderis had asked her if she had started on intravenous antibiotics, as that should settle it, and alternatively suggested a PICC line. He accepted that he thought it was appropriate for Ms Mattiske to be on intravenous antibiotics, but said it was inappropriate for him to prescribe antibiotics because she was under the care of another physician at The Hills.
1726 Ms Mattiske’s evidence was that when she was taking antibiotics, she felt fine, but as soon as she stopped taking them, she became very sick again. This evidence, both as to the infections and the effect of the antibiotics, is addressed in the 16 March 2021 report of Dr Sarah Kirkham, her GP, to the emergency department at the Sunshine Coast University Hospital. The report requests her admittance to the hospital, stating:
I am very concerned this patient has an ongoing focus of infection around her new amputation site/interossesous integration. She has had multiple presentations with pus from the stoma site, pain and cellulitis since her operation. She gets better with IV abs [antibiotics], last had some in Nambour last week. She was sent home on oral clindamycin which finishes today and has already been getting worse again for 2 days.
1727 This is consistent with Ms Mattiske’s evidence.
1728 In Ms Mattiske’s text messages sent to Dr Al Muderis and Ms Roberts from early 2019, she detailed her symptoms. I accept that they, amongst other things, reflect that at times, Ms Mattiske was in excruciating pain, and it was increasing. They include pleas for help. The messages also reflect the symptoms as she describes them that led to the procedures above, and the consequences of those procedures. For example, Ms Mattiske sent the following message on 26 April 2019 to Ms Roberts (and it appears to Dr Al Muderis as well):
Hi lovely Claudia
Not sure if you guys are back yet from O/S but just sent this to Munjed
…
Hi Munjed Just checking in to clarify with you that at 8 wks post surgery my knee should still be swollen n extremely painful to walk on with 2 crutches having bone pain down into phantom leg... knee still very warm to touch... pain so sharp at times it takes my breath away n am resorting to wheelchair... am still 90 % of day on bed resting only way to find some type of relief but hardly ever pain free...though doing exercises from physio on bed most of day intermittently... just checking this level of pain is normal as it has moved from muscular to bone pain with still some nerve pain ... if to be expected that’s fine I will continue as I am but if not I will make a dr appoint n get an X-ray n blood tests done.... I thought by now it might have settled somewhat... which I felt it dead beginning to do but then it seems to have flared up again but maybe that is me tiring of the journey or my anxiety ...
Thankyou Munjed... am finding this recovery most difficult, the worst of all my 27 surgeries thus far n trust me that’s saying something... I’m not complaining just being honest with you n real. I appreciate your input very much.
Thankyou again
Rowena
1729 The events over those years cannot simply be described as mere “bumps”. They significantly impacted her life. As she described in her affidavit, the operations and related complications thereafter have, understandably, had a huge mental toll on her.
1730 The text exchanges with Ms Roberts and Dr Al Muderis are, in many respects, as described by the respondents, fawning. Nonetheless, these messages are also a contemporaneous account of the symptoms she was experiencing and the pain she was enduring. There was a period, particularly in 2017 and 2018, in which there were less issues. Ms Mattiske did travel during that time, before she had her above-knee amputation, and gave evidence that she was generally able to return to living an active life. The applicant’s submission referred to above – that Ms Mattiske was able to walk for six years, lead a fulfilling life, return to the outdoor activities she enjoyed and travel on two major overseas trips – ignores that one can be active whilst in pain, and selectively focuses on one period of time while disregarding the other occasions and periods of her life she described in evidence. Even during that period, it fails to reflect as Ms Mattiske explained that while she travelled overseas, she said she “spent a lot of that time resting, sitting and enjoying what [she] could see while [her] husband did the adventurous-type things”. Those other times not referred to, for example, that she missed celebrating Christmas on two occasions in 2019 and 2021 because of her pain, are credible.
1731 In that context, her evidence that she said to Dr Al Muderis in May 2022 that she wanted her implant removed, reflects the state she was in at that time.
1732 I note also in this context that it was put to Ms Mattiske on several occasions that Dr Al Muderis saw her in ward rounds two to three times each week in the hospital. Ms Mattiske said that was “totally incorrect”. Her evidence was that she saw Dr Al Muderis once a week at most when she would run into him in the corridors. Dr Al Muderis himself said the conversation about removing her implant occurred in the corridor.
1733 As I mentioned earlier, all these events occurred prior to the Publications, and any contact with any relevant persons, being Ms Stewart, Ms Grieve, Dr Wines or Mr Grant. Ms Mattiske’s described series of events occurring before October 2022. Although Ms Mattiske might not have expressly said she was complaining, it is plain she was unhappy about her medical condition. The above is not dependent on the evidence of Ms Mattiske but is also based on and supported by the documentary evidence.
1734 The applicant relied heavily on Ms Mattiske’s messages being inconsistent with the state of mind she is now expressing she had at the time. I have addressed the general nature or tone of her messages above, but it is appropriate to return to that submission.
1735 I will refer to two passages of evidence where Ms Mattiske described why she wrote the messages she did, in the way that she did.
1736 First, in evidence, Ms Mattiske described an occasion where she (just a few weeks after the second stage of her osseointegration surgery) and three other patients rehabilitating at The Hills were invited by Dr Al Muderis to go on his yacht around Sydney Harbour. She accepted the patients had approved day leave from rehabilitation. Ms Mattiske described how they travelled by bus and train to get to Darling Harbour. She described that it was apparent that Dr Al Muderis only realised there was a problem in terms of the patients’ accessibility once they arrived, because the wheelchairs could not be used to board the boat. Her evidence was that to get on the boat, this involved the patients:
… getting out of [their] chair, bum walking to the edge of the wharf, throwing [their] good leg into the boat and someone on the other side pulling [them] over and into the boat.
1737 Ms Mattiske agreed that she had a lovely day, but that she was in excruciating pain by the end. This was challenged in cross-examination, but as I have addressed above, the mere fact that Ms Mattiske was active or enjoying herself does not negate any experience of pain. The applicant cross-examined Ms Mattiske, suggesting that her evidence that there was an issue with their medical care while on the boat was false. Ms Mattiske said she chose to be positive; “it was an amazing day”, “it was wonderful to be out”, and “he was generous”. She said however, that “there was a flipside to that, and it was negligence of care”.
1738 Ms Mattiske, in reply to a question that if she truly felt Dr Al Muderis had been negligent in his care on that occasion, she would not have written the positive message, said:
That is totally incorrect. You do not know me. I often – that’s part of my personality. And I will be honest and say that my psychologist is working with me on being too nice. So I did mean those words that I said … when you are under someone’s care and the surgeon indirectly – and his associates – say that “He is the best surgeon”, and he verbally denigrates, knocks other surgeons and says “He’s the best”, you are not about to say to him “What about our care?” I wasn’t strong enough at that point, emotionally, to be able to confront him on those things, and I am not going to do that because he’s my only lifeline, my line of oxygen that I am breathing on, and I am longing to walk. So I am not going to upset that in any state or form.
1739 That latter aspect is consistent with the evidence of other patients and highlights the innate dependency such patients have on Dr Al Muderis.
1740 I have addressed elsewhere the appropriateness of such social occasions, and the impact that has on the doctor-patient relationship.
1741 Second, Ms Mattiske gave evidence that she did not know why she continued to go back to Dr Al Muderis. She said she was desperate to walk and had “tunnel vision” about him and osseointegration. Ms Mattiske elaborated during cross-examination that when she came to Dr Al Muderis, she expected that she would only have at most three surgeries (being the initial two surgeries for her osseointegration, and potentially an additional surgery later) but in fact had very many more while under his care. It was put to Ms Mattiske that, given her experience with multiple surgeries prior to her contact with Dr Al Muderis, she did not think that having osseointegration would mean all of her medical conditions would disappear. Ms Mattiske said:
They weren’t medical conditions. They were things that – yes, they were, I suppose, but they weren’t existing – pre-existing conditions. They – they resulted from each surgery that I had had, and when I went to Dr Al Muderis, he was painted as the pinup boy, the expert in the world and – and Australia, and naively, on my behalf, I had absolute faith and trust in him. I handed my life to him, in his hands, because this is what he promised, “I can make you walk again, Rowena”. There was no mention of lots of surgeries.
1742 It can readily be accepted that a person can put their trust in someone and later realise that what occurred was not acceptable. One can be blind to what is occurring, but that does not mean it did not happen. I note that he would have promised her he can make her walk again is consistent with other evidence: see sting 2 in Part 7, Section 1.
1743 The applicant also relied on Ms Mattiske’s evidence where she accepted that her pain was currently worse. However, Ms Mattiske’s evidence in relation to that is not to be considered in isolation. Her evidence is that her pain increased after her osseointegration surgery. As earlier explained, the applicant challenged that evidence, although the basis of the challenge is unclear. The applicant wants this Court to accept Ms Mattiske’s evidence of her level of pain after the removal of the implant at the time of the hearing, but not her evidence on the level of her pain after the osseointegration surgery. This is in a context where Dr Al Muderis stated that Ms Mattiske “had pain all the way, unfortunately”. I accept Ms Mattiske’s evidence as to her pain after her osseointegration surgery, and after the removal of her implant (although her pain has increased over time).
1744 Ms Mattiske gave evidence that after seeing Dr Wines in October 2022 in Sydney and returning to Queensland, she later attended the emergency department in Nambour Hospital with a high temperature and chronic pain, before being transferred to the RBWH. Ms Mattiske explained Dr Wines had asked that she discontinue antibiotics for eight weeks so that the infection could be detected on tests and the correct antibiotics could be prescribed. Dr Tetsworth referred her to Dr Wines (as he was going overseas). On 7 December 2022, Dr Wines performed a debridement of her knee stump and sent samples to microbiology. Ms Mattiske was diagnosed with a chronic infection in her right femoral osseointegration, and on 24 May 2023, Dr Wines, Dr Huang and Dr Wang removed the osseointegration implant.
1745 Ms Mattiske explained her decision to have the implant removed as follows:
At this time, I had decided that I no longer wanted to have the implant inserted into my leg. I had kept the implant inserted, despite ongoing infections, for many years in the hope and belief that I would one day be able to walk again with the assistance of osseointegration. However, I was exhausted from all the infections and complications I had experienced. For example, when I had the implant, I would keep towels around the house so that I could use them to wipe away the gunk and oozing from the implant site. I would also keep towels in the car and would sleep on towels, the oozing was so bad. I was exhausted from having to travel for ongoing medical treatment, particularly for the persistent infections I had experienced. I was also frustrated because I felt I was not believed by Dr Al Muderis when I raised concerns about my health and wellbeing. Due to the complications from my osseointegration surgery, I had lost my love for life. My life had become joyless. I was moody and withdrawn because of the pain.
I decided my quality of life was not intrinsically tied to my ability to walk. I just wanted to be healthy and happy again. I was content in the knowledge that, by removing the osteointegration implant, I may live the rest of my life in a wheelchair. I was willing to take that risk if it would restore my quality of life.
1746 I am satisfied that the concerns of Drs Basten and Paterson were real, and there is no evidence they were addressed before the decision as to suitability was made (noting also the context where this surgery is described as “most unusual”, and the potential risks that flow from its nature): see [1705] above. Ms Mattiske was inadequately warned about the risks, including there was no warning that her pain may be worse after she has the surgery. This was particularly important given her issues with pain at the time and that her expressed desire was that she was looking for pain reduction. I am satisfied the message conveyed to her was a positive one, where her circumstances were complex. Because of that, and Dr Al Muderis’ failure to properly warn of the risks, and the potential consequences thereof, Ms Mattiske had no understanding that what she endured over the years after having the surgery was part of the risks of the surgery. Her consent was not an informed one. I am also satisfied that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
1747 Based on the evidence before me I am not persuaded the allegation of inadequate aftercare has been established. It does not diminish Ms Mattiske’s experiences during that time, and the complications she endured. That said, Dr Al Muderis’ conduct (e.g. laughing when she told him she wanted the implant removed), was rather cruel and reflects an approach towards her which diminished her concerns, and the position she was in. This is also reflected in the manner the case has been presented by the applicant, referring to the very many issues, as “bumps” in her life. Her evidence was she trusted Dr Al Muderis and went along with what he said. It can also be accepted that the osseointegration surgery (and what ensued) significantly reduced the quality of Ms Mattiske’s life.
Ms Carol Todd
1748 Ms Todd underwent a procedure to amputate her left leg below the knee when she was six weeks old. She used a prosthetic limb until she was in her late 50s. In 2014 she underwent osseointegration surgery with Dr Al Muderis.
1749 Ms Todd gave evidence in an honest and genuine manner. She was a credible witness. It was apparent that at times she was confused as to dates, and that tended to fluster her. She, not surprisingly, lacked memories of some specific interactions with doctors. Her evidence on some events may not have been reliable (or could not be accepted on balance). That said, I do not accept that she was deliberately giving untruthful evidence. Rather, I accept that she believed what she recalled had occurred. The applicant in his written submissions accepted that Ms Todd largely presented as credible, but that her oral evidence should be preferred to her affidavit evidence, and contemporaneous documents should be preferred to her evidence. There is one topic of her evidence that was highlighted by the applicant as adverse to her credibility, relating to the removal of some silicone (see [1763]-[1766] below). Despite the applicant’s written submissions, in oral submissions the applicant alleged that Ms Todd concocted her evidence, as her complaints only arose after her communications with The Alfred team and Dr Huang. As explained below, Ms Todd sought a second opinion within 18 months of her surgery. The applicant cannot point to any basis for that submission. I do not accept that Ms Todd has concocted her evidence.
Background
1750 Ms Todd was born in 1951 with a medical condition called infant methemoglobinemia, a condition in which there is not enough oxygen in the blood. About one month after birth, she developed a blood clot during a medical procedure which later became infected. As a result, when she was six weeks old, she underwent a procedure to amputate her left leg below the knee. When she was about two years old, she was fitted for her first prosthetic leg. She continued to use prosthetic limbs until her late 50s.
1751 Ms Todd underwent osseointegration in two stages. The first stage took place on 15 January 2014, and the second on 19 March 2014.
1752 Ms Todd’s first consultation with Dr Al Muderis was on 4 July 2013. She presented as highly functional and in general good health, able to perform all daily activities, including long distance walking, but she also experienced skin irritation and lower back pain from her socket prosthesis.
1753 As the carer for her husband Mr Todd, who suffered from Parkinson’s disease, a key outcome for Ms Todd from osseointegration was the ability to better assist her husband, including as his condition progressed. Dr Al Muderis was aware of that fact. Given that circumstance, the risk of the surgery exacerbating her health would have a significant impact on her and her family.
1754 The 4 July 2013 consultation report records that Ms Todd was found suitable for surgery. It further records that she understood the risk of infection associated with the surgery but was regarded “as relatively low risk”. It concludes that Ms Todd “suffered significant reduction in her quality of life due to her amputation”, and Dr Al Muderis believed that she “would greatly benefit” from the procedure. There is no reference in the report or evidence that any alternative conservative options or prosthetics were proposed or discussed by Dr Al Muderis to Ms Todd.
1755 Ms Todd gave evidence of what may be described as a high-level discussion of risks. She deposed that she raised the issue of infections, and Dr Al Muderis responded that “[t]here could be infections, but that is normal and if that happens it can be addressed with antibiotics which will clear it up.” She gave evidence to the same effect in cross-examination. I note the only particular risk referred to in the consultation report, referred to above, is infection; a “relatively low risk” for her. This accords with Ms Todd’s evidence. This is to be contrasted with Dr Al Muderis’ evidence that infection is inevitable.
1756 Further, Dr Stoita agreed that, given Ms Todd’s desire to be able to better assist her husband, the risk of losing mobility as a result of having the surgery would likely be a highly relevant consideration in deciding whether surgery was appropriate or not. There is no evidence that this consideration was appropriately addressed. Rather, the risks were downplayed.
1757 It may be accepted, as the applicant submitted, that prior to their first consultation, Ms Todd and her husband had been to a presentation by Dr Al Muderis held in Queensland and had done their own research. She accepted that she understood from the research there was a risk of infection, and that the procedure may not work. Mr Todd was a prosthetist, having retired in 2013.
1758 The presentation made an impression on Ms Todd. She gave evidence that Dr Al Muderis said words to the effect that he was the best at what he does, and he was the only one who did osseointegration. He had invited a person who had undergone the procedure to present, prompting Ms Todd to think: “Wow. This is a new way of life for me”. Ms Todd described that Dr Al Muderis “sold it so well” at the meeting.
1759 However, that and any research Ms and Mr Todd conducted does not alleviate Dr Al Muderis of his responsibility to explain, properly and realistically, the risks and complications involved in osseointegration. Not surprisingly, the position of the surgeon carries weight in relation to the advice provided.
1760 That said, the 4 July 2013 consultation occurred in a context where Ms Todd had already formed a positive view about the applicant.
1761 Ms Todd gave evidence that her bones were very small. She explained Dr Al Muderis confirmed so much with her during a consultation and informed her she would need to wait about six months to undergo the procedure while a smaller rod was made. As it turns out, although a smaller prosthesis was made, a standard one was used instead.
Post surgery
1762 The operation report of 15 January 2014 noted a “split in the femur which was fixed using 3 Dal Mile Cables”. Ms Todd’s evidence was that her nurses told her of this. Dr Al Muderis gave evidence that the split was inconsequential, as the bone readily heals. However, Ms Todd’s clear evidence is that Dr Al Muderis did not tell her of the split, or the use of cables.
1763 Ms Todd gave evidence that on 3 April 2014, while in hospital recovering from her second surgery, there was an incident where Dr Al Muderis forcibly removed some silicone from her leg causing her considerable pain and to cry. Dr Al Muderis denied the incident. The applicant submitted that the incident as described was physically impossible, ridiculous and bizarre.
1764 Documentary evidence supports there was an issue with the silicone cover on Ms Todd’s leg. Her diaries record that, on or around 1 April 2014, her physiotherapist told her that “the silicone cover had been put on the wrong way”. She wrote it was “like that since my [operation on] 19th March” and that it was painful, complaining that “I have been telling them it was sticking inwards for nearly 2 week[s]”. She also gave evidence that having the silicone on the wrong way was painful. The diary records that the physiotherapist and Mr Lye came by to attend to it. The diaries, while referring to those individuals, do not refer to Dr Al Muderis being present that day.
1765 Ms Todd’s diary entry of 3 April 2014 records that:
Doctor came in today told him about silicon [being] back to front it had been like that for 12 day[s] + physio + Bob turn it around for me + did not say anything about it. Look at wound + said it look good + you are right to go to Rehab. Was not in more than 3 mins at the most.
1766 The respondents submitted it was obvious that Dr Al Muderis removed something from Ms Todd’s leg despite it causing her significant pain and upsetting her enormously and that, as she said, she had no reason to lie. There is evidence that supports her evidence the silicone was back to front for days, which begs the question of how that could have been allowed to have occurred if she was being properly attended to. That said, although I accept something may well have happened, I cannot be satisfied to the required standard that it occurred as Ms Todd describes. However, I do not accept this adversely effects her credibility.
1767 Upon Ms Todd’s return to Queensland, she experienced ongoing issues with pain, and pus and blood in her wound.
1768 On 21 May 2014, Ms Todd contacted Dr Al Muderis and had a conversation via telephone with him in which she reported that she was having significant discharge and some pain, and that she had had a fever.
1769 Dr Al Muderis’ report to Ms Todd’s GP of the same date relevantly records:
I had a conversation with Carol today and she is having significant discharge and some pain and yesterday she had a fever. I advised her to change her antibiotic to Clindamycin, three times a day, to see if this has any effect. She started the antibiotic yesterday and it seems today that her temperature has settled. She does still have discharge how ever not as significant.
I advised her to continue observing her symptoms and the discharge very carefully. If at any stage she shows any signs of sepsis then I need to see her straight away by either her coming to Sydney or she could go to the nearest hospital to her home. I discussed thoroughly with Carol that we will monitor her discharge over the coming week and if there are no signs of improvement then we might need to perform surgical debridement for the wound which I will organise for her next week if need be. If she responds to the antibiotic and everything settles then we will continue with the antibiotic until the infection clears. Obviously she does have signs of infection however we will keep monitoring this closely.
1770 Three matters to note.
1771 First, Dr Al Muderis did not arrange for any tests despite being concerned that she had an infection and the risk of sepsis. Rather, he arranged for a change in antibiotics and “advised her to continue observing her symptoms and the discharge very carefully”. As the respondents observed, this:
… was unusual advice from a doctor who spent the entirety of the trial arguing that infection could not be detected without clinical diagnosis and objecting to evidence from any patient who alleged they had an infection based upon their own observations.
1772 At the very least, the approach stands in contrast to his evidence in some of his explanations in cross-examination as to why he had not responded to requests for help from a patient in relation to infection (e.g. he would only act if he had been sent results from a doctor raising serious concerns about infection, a swab sample does not mean there is an infection, or that a patient’s evidence of having an infection based on their observations of the symptoms could not be accepted: see e.g. in relation to Mr Warland, Ms Çalan and Mr Bruha).
1773 Second, there is no satisfactory evidence of any contact between Dr Al Muderis and Ms Todd following her discharge from hospital until she reached out to him on 21 May 2014. It was put to Ms Todd that she saw Dr Al Muderis at Mr Barry Leech’s office on 10 May 2014, to which she responded that is “probably right”. However, there is no evidence of such a meeting, with the applicant relying only on Ms Todd’s response in cross-examination. Dr Al Muderis does not give evidence of a meeting, there is no report of any consultation on that day, and there is no evidence as to what occurred at this supposed meeting.
1774 Third, there is no evidence of any follow-up thereafter by Dr Al Muderis. The next contact appears to be Ms Todd again reaching out to Dr Al Muderis on 28 May 2014.
1775 On 4 June 2014, Ms Todd texted Dr Al Muderis explaining she was experiencing significant pain and that her stoma did not look good. He responded by text, advising her to stop using Keflex (an antibiotic) for 24 hours and then to go to the GP to get a swab, writing that the GP should start her on Keflex again. He asked to be kept updated.
1776 On 18 June 2014, Ms Todd sent Dr Al Muderis two text messages seeking guidance and asking him to call her. In the messages she describes experiencing pain and oozing. There is no evidence of any response.
1777 Ms Todd’s evidence was that while at home on 22 June 2014, there was pus around her wound and, whilst she was walking, blood dripping out of her stoma onto the floor. Blood clots and pus then started coming out of her wound, which alarmed her. She was in a lot of pain. She sent text messages and photos to Dr Al Muderis describing what occurred and asking he call her urgently. Because she had received no response after several hours, she messaged Dr Aditya Khemka, Dr Al Muderis’ registrar, also attaching photos. Dr Khemka responded that “[t]here seems to be some infection” and said he would ring her shortly.
1778 On 23 June 2014, Ms Todd travelled to Sydney and was admitted to Norwest Private Hospital for treatment.
1779 Dr Al Muderis performed three procedures for Ms Todd to treat the infection. First, on 30 June 2014, he irrigated her stump with saline, explored the wound and observed pus near one of the three cables which had been used to secure the split in her femur. He removed the three cables, revised the stoma, and applied a vacuum dressing to the stoma. The cables were contaminated with infection. Dr Al Muderis denied the cables were the source of the infection. He explained that he removed the cables because they had “done their job”. He added that “if they can be contributing to any source or any problem of irritation that may lead to an infection, then they can be removed”. Second, on 7 July 2014, Dr Al Muderis changed the vacuum dressing, partially closed the wound, and applied a new vacuum dressing. Third, that same day, Dr Al Muderis removed the vacuum dressing, and samples were taken.
1780 The applicant took issue with the description of the three procedures, saying it was a single-staged procedure. Regardless, each were surgical procedures performed under general anaesthetic.
1781 During the July 2014 procedures, Ms Todd had a PICC line inserted into her neck to deliver intravenous antibiotics.
1782 She returned to Queensland following discharge. Although the applicant submitted that to facilitate this Dr Al Muderis referred her to Dr Craig Dancer (the infectious diseases doctor at Ipswich Private Hospital at that time) for care, that submission is not supported by evidence. To the contrary, Ms Todd gave evidence that Dr Al Muderis promised her she would go to Ipswich Private Hospital.
1783 Ms Todd gave evidence that Ipswich Private Hospital did not know what to do with her when she arrived: “I had no letter, no nothing”. They nevertheless admitted her after she explained her position. Her evidence was that it appeared that the hospital did not know what treatment she required; she called Dr Al Muderis’ rooms and requested they speak to the head nurse to give instructions (the first aspect of this evidence is subject to a s 136 Evidence Act limitation, the latter is describing her actions).
1784 Ms Todd’s evidence was she had a new PICC line inserted while at Ipswich Private Hospital and she spent a further three weeks there recovering from the infection. After leaving the hospital, she returned every day to have antibiotics administered. When at home, she had a bottle around her neck which administered antibiotics via the PICC line. She was on antibiotics for about six months.
1785 Ms Todd accepted, having been shown her diary entries dated 18, 25 and 28 July 2014, that Dr Al Muderis had contacted her on a few occasions that month. Ms Todd gave evidence that she was the one who always initiated the calls given her ongoing issues.
1786 Ms Todd saw Dr Dancer regularly. In his report dated 31 July 2014, he stated that Ms Todd had completed “six weeks of intravenous meropenem for the Morganella infection of her intraosseous implant”. The applicant emphasised that the report stated that there was only a small amount of discharge from the leg, and it otherwise looked “quite good”. However, the report recorded that there was an intention to give Ms Todd six months of antibiotic treatment, and expressed concern as to a cure, because the implant was “extending out into the open”.
1787 Following her appointment, Ms Todd recorded in her diary that “Munjed rang at 8:00pm tonight to say I heard you walk[ed] + said I have been through a lot + not to give up + they will be there for me they won’t give up on me”. The applicant submitted that the fact that Dr Al Muderis made this call and knew that Ms Todd was walking again indicates that he must have been in contact with Dr Dancer about Ms Todd’s condition, because it is not apparent how else he could have known this on the same day that Ms Todd saw Dr Dancer. Regardless of how that call came about, from the diary entry it is apparent Dr Muderis is saying he would be there for her in a way that reinforces an expectation.
1788 On 3 August 2014, Ms Todd recorded that Dr Al Muderis rang again to see how she was going.
1789 Dr Al Muderis saw Ms Todd on 9 August 2014 for a regular follow-up consultation. The applicant submitted that, based on the consultation report, Dr Al Muderis observed that she was doing well and that her wound was clean and healthy. He submitted that these observations are consistent with those Dr Dancer made on 31 July 2014, and that Ms Todd did not dispute them in cross-examination. He submitted the Court should accept that the consultation report is a substantially accurate summary of what occurred.
1790 The consultation report of 9 August 2014 is scant and inaccurate. It records “Carol is one month post 2nd stage osseointegration and change of vac dressing and she is doing extremely well and the wound is looking clean and healthy” (emphasis added). That is the extent of the brief report, the remainder being formulaic. The emphasised portion of that sentence, not referred to in the applicant’s submission, is plainly inaccurate. Ms Todd had the second surgery in March 2014. As at the time of the report, she had just completed a six-week course of intravenous antibiotics and had commenced a six-month course of oral antibiotics in circumstances where Dr Dancer held concerns about an eventual cure. The report contains no reference to those matters, nor the pain, infections, or the lengthy hospital stay. In those circumstances, it is difficult to accept that Ms Todd could properly be described as doing “extremely well”. The scant nature of the report and its terms underplay the seriousness of her situation. This provides a further example of inaccuracies in Dr Al Muderis’ consultation reports, which have been discussed above: see Part 6, Section 1.
1791 An email to Dr Al Muderis from Mr Leech, Ms Todd’s prosthetist, dated 30 January 2015, records that he had reviewed her the previous day and that, inter alia, she had been suffering pain for some time, had a constant fluid draining and buildup of a mucus, and the distal portion of the stump was soft and somewhat baggy. He records that Ms Todd was fearful of further infection and opined that “this is some of her issues appearing larger than they are” (sic). It is apparent from the email that Dr Al Muderis was aware of the aspects of Ms Todd’s condition that Mr Leech describes. He accepted he received the email from Mr Leech.
1792 Ms Todd sent Dr Al Muderis some text messages and photos on 20 and 24 January 2015. On 21 January 2015, Dr Dancer had sent a report to Dr Al Muderis, which recorded that Ms Todd had increasing pain in her left leg and ooze. Although she had been on six months of antibiotic therapy by this time, Dr Dancer decided to continue her on antibiotics. The report concludes that he “look[s] forward to [Dr Al Muderis’] opinion”. There is no evidence of any response to the letter. It is hardly surprising that Ms Todd was concerned about further infection given the consequences for her and her family if a sufficiently harmful infection materialised. Dr Dancer also obviously had concerns.
1793 In this context I note that Ms Todd gave evidence that “the infectious disease doctor [told] me that I had Morganella and that I would be on antibiotics for the rest of my life … the only way you can get rid of the bug is to take the rod out”. As explained above, Dr Dancer expressed concern about the infection ever being cured in his 31 July 2014 report.
1794 Although Ms Todd gave evidence of a debridement procedure with Dr Al Muderis on about 9 January 2015, she appears to be mistaken about that.
1795 She underwent further procedures in early February 2015. On 7 February 2015, Dr Al Muderis performed a stump refashioning procedure. Two tests were undertaken before the procedure. On 3 February 2015, she had a CT and x-ray of her left femur. On 4 February 2015, she had a bone scan, which revealed “[n]o specific features of osteomyelitis”, and suggested a “progress study with gallium could be performed if there are ongoing clinical findings”.
1796 The applicant submitted that he did act on concerns that Dr Dancer reported, for example, when he admitted her to hospital in February 2015 for investigation of the symptoms reported in a 21 January 2015 letter from Dr Dancer. However, that correlation is unfounded. Dr Al Muderis did not give evidence of responding to Dr Dancer, and the submission he made does not suggest he did. Rather, it attempts to equate that act (being the investigations in February 2015) with Dr Dancer’s concerns. As evident above, the tests were done about two weeks after Dr Dancer’s report. Also, after that report, Ms Todd attended to Mr Leech for review. The basis for doing so is unclear. Only after that was Ms Todd admitted to hospital. I note that in her diary entry of 5 January 2015, Ms Todd records that she was told she did not have an infection, and they can go ahead with the reconstruction of the stump.
1797 Ms Todd and Dr Al Muderis exchanged text messages in February and March 2015. On 2 February 2015, in response to photographs she sent him, he said she had an infection and to call him. This was the day before the tests referred to above were undertaken. On 6 March 2015, Dr Al Muderis requested she have a swab taken, and to take a particular antibiotic, flucloxacillin. On 7 April 2015, she sent further photos, and he replied saying that if the pain is under control, it should be fine. Ms Todd had described blood, oozing lots, and a smell.
1798 On 10 July 2015, Ms Todd sent an email to Dr Al Muderis, informing him that she experienced another infection “a couple months ago”, and that Dr Dancer had sent him a letter to which he had not responded. She disclosed she was still taking antibiotics. She also informed Dr Al Muderis, inter alia, of ongoing pain she had been experiencing “for over a few months”, which was increasing. She explained that she had not told him of the pain because she thought it would go away, and that she had “written this letter because you are so busy and I don’t know” when to call. Dr Al Muderis replied offering to see her, and the two scheduled an appointment in Brisbane for 24 July 2015.
1799 On 30 July 2015, Dr Dancer sent a report to Dr Al Muderis recording that Ms Todd “is doing well at the moment”, her inflammatory markers have settled, she is tolerating the ciprofloxacin (an antibiotic), and the ooze had settled. He said he would continue the ciprofloxacin “for at least a further 6 months given the difficulty a relapse of infection would cause”. He sent Dr Al Muderis a further report with identical terms on 10 September 2015. The applicant’s submissions about the reports fail to refer to the fact that antibiotics were to continue, and Dr Dancer’s concern should there be a relapse.
1800 On 11 September 2015, Ms Todd attended a clinic and consultation with Dr Al Muderis and Dr Tetsworth. The consultation report records that the stoma looked dry, clean and free of infection, that she remained on clinidmycin (an antibiotic), and that she would attend the:
RBWH orthopaedic clinic in 2 weeks’ time with a follow up bone scan/SPECT scan for the consideration of a stress fracture surrounding the prosthesis which may be the cause of her ongoing anterior thigh pain.
1801 It is unclear the basis on which it is recorded in that report that she remained on clinidmycin, as Dr Dancer’s report of the previous day refers to him continuing to prescribe ciprofloxacin.
1802 On 26 September 2015, Ms Todd received a text from Dr Al Muderis saying he could see her that day at the Sofitel in Brisbane, and to bring x-rays. Ms Todd’s evidence was they met in the lobby briefly, he looked at her x-rays and said, “they look good”. I note that Dr Al Muderis did not give evidence of this consultation and nor is there any record of it.
1803 At this time Ms Todd continued to take antibiotics.
Second opinion
1804 Pausing there. In October 2015, Ms Todd sought a second opinion. Her GP referred her to doctors at The Alfred. Dr Edwards, an orthopaedic, trauma and reconstructive surgeon at The Alfred, interviewed and examined Ms Todd on 19 October 2015. He reviewed her x-rays and opined that there had been very significant bone loss of the left femur, associated with ongoing infection which had caused her prolonged hospitalisation following surgery in March 2014. He maintained that view in cross-examination.
1805 Dr Al Muderis disagreed with that opinion. He deposed that:
the significant osteoporosis suffered by her is likely to be the result of stress-shielding … The Endo-Exo implant used on Ms Todd is made of a chrome cobalt alloy which has a high tensile strength, taking much of the load off the bone. This would have resulted in osteoporosis over time …
1806 There is no evidence that Ms Todd was told of stress-shielding when she was deciding whether to undergo the procedure.
1807 Dr Edwards disagreed that stress-shielding caused Ms Todd’s bone loss. In evidence he gave several reasons. First, in Ms Todd’s x-rays he observed osteolysis (complete loss of bone), not osteoporosis (thinning of the bone). Osteolysis is usually caused by infection. Second, the pattern of the alteration of the bone structure was inconsistent with stress shielding. Third, not enough time had passed for Ms Todd to develop stress shielding. Stress shielding is caused by loading. In his experience, it develops over two to five years. Only 18 months had passed in Ms Todd’s case, during which she had been hospitalised for extended periods, leaving him to assume she was not loading her implant for more than six months of that period. To develop stress shielding of this magnitude in less than 12 months was not a realistic possibility.
1808 Dr Edwards said he was not sure whether Ms Todd was experiencing an ongoing infection at the time as she had been on antibiotics for 18 months, so the infection would have been suppressed. He agreed that he did not recommend any orthopaedic intervention at that time, but that it would be discussed with a plastic surgeon, something which did not occur. He said the plan was for him to give an opinion, it “was never really to treat her”.
1809 The applicant does not address Dr Edwards’ evidence in his written submissions. In oral submissions he accepted that Dr Edwards was a wholly credible witness, who I should accept. I do accept Dr Edwards’ evidence, which includes his assessment of whether stress-shielding caused Ms Todd’s bone loss.
1810 Given the circumstances as to what Ms Todd had endured up until her seeking a second opinion, it can be inferred that Ms Todd was unhappy or dissatisfied with the care given by Dr Al Muderis.
1811 On 3 November 2015 Ms Todd wrote a letter sent by Mr Todd in an email to Dr Al Muderis, which included the following:
I was waiting for you or Belinda to contact me while you we’re in Brisbane … seeing you was very important to me to finally get some answers.
…
The reason I have not been calling you any more is because I find our conversations unsatisfactory and I find I get no response to my questions when I call you. The truth is, I don’t feel you are taking my problem seriously.
I have been in constant pain since I have had this procedure[.] Having this done was to prevent me from being in a wheel[chair]. It was to change my life, well it sure has I now have no life at all. It’s good not having to wear a socket but it has brought much disappointment to me. I cannot do the things I used to do because I am in pain no matter what I do.
…
Where the stoma is situated, this area is painful all of the time. The pain seams to go right into the rod, [it’s] horrible. It is painful all of the time when I put my leg on, walk or sit. I am walking with my walking stick and when home I try not to use the walking stick. Where does it all end? I am not happy any more.
…
I have a husband to worry about with Parkinson’s and my grandson who requires special care[.] How can I give them the care and attention they require if I am continually trying to push through my pain.
…
It has been two years of pain since the operation and I have been away from my family. I cannot not take it any more. I HAVE HAD ENOUGH.
1812 Dr Al Muderis gave evidence he does not recall receiving this email. He rejected the accuracy of the complaints.
1813 It was suggested to Ms Todd that she was put up to sending the email by others, including Mr Gray of The Alfred, and that it exaggerated claims. She denied that it was exaggerated. She gave evidence that her family encouraged her to write it, explaining “they [were] the ones that were upset, because I was sick all the time”. I accept her evidence as to her motive for sending the email, and that the email accurately reflects her feelings at the time as to Dr Al Muderis’ care.
1814 On 10 November 2015, Dr Dancer sent another report to Dr Al Muderis. In the report, he wrote:
The bone appears intact on x-ray but there is a very thin rim of bone around the implant and due to concerns about cure of the infection with the implant in place, at this point I have continued her on ciprofloxacin which she has been tolerating without major incident and inflammatory markers have remained suppressed.
1815 That reflects Dr Dancer’s concern about curing the infection, in a manner consistent with Ms Todd’s evidence that “the only way you can get rid of the bug is to take the rod out”.
2016
1816 On 29 July 2016, Ms Todd’s GP, Dr Baker, wrote to Dr Al Muderis seeking his assistance. The letter advised that Ms Todd was experiencing episodes of bleeding and thick yellow discharge and that she was continuing to experience neuropathic pain. She observed that Ms Todd was “getting more depressed with the intensity of the pain she is in”. Dr Al Muderis had no recollection of responding to this letter, nor is there evidence of a response.
1817 On 31 August 2016, Ms Todd went to see Dr Baker. When Dr Baker examined her stoma, she noticed something white sticking out of it. She observed Ms Todd pull it out and saw that it was a 1cm x 1cm piece of jagged bone.
1818 On 8 September 2016, Dr Baker wrote to Dr Al Muderis seeking urgent advice. She was worried because the tests on the bone suggested osteomyelitis, despite the regular preventive antibiotics Ms Todd had been prescribed. The following day, Dr Baker followed up with an email to Ms Bosley, who she understood worked with Dr Al Muderis. Ms Bosley telephoned her. There was then some email exchange with, it appears, Ms Bosley. In any event, Dr Baker was told to contact Dr Jen Kok, a local infectious diseases physician, directly.
1819 I note that Dr Al Muderis’ cross-examination on this topic was unsatisfactory. He suggested he, as opposed to Ms Bosley, may have spoken to Dr Baker at this time. There is no evidence to support that. He questioned the veracity of the test results and minimised Dr Baker’s concerns. Dr Baker, quite appropriately concerned about her patient, sought assistance.
1820 The applicant suggested that Ms Todd stopped seeing Dr Al Muderis because she did not want to continue travelling to Sydney for follow-ups, and her post-operative care was therefore transferred to Dr Tetsworth at the RBWH in September 2015. As evident from the description above, she did at times see Dr Al Muderis thereafter, or he was contacted for her care. Dr Al Muderis said he saw Ms Todd in mid-2018, and there is a letter confirming an appointment for 16 June 2018.
1821 I note that by 2018, Dr Baker had referred Ms Todd to The Alfred. In August 2018, she sent a consultation report to Mr Gray, explaining that Ms Todd:
… has come to the point of not being able to cope with the level of pain she experiences & is very clear that she does not want to have further surgery with [Dr Al Muderis].
1822 This at least implies that Dr Al Muderis was regarded as her surgeon, and that she did not want to see him. It can also be inferred that Ms Todd was unhappy with her care by Dr Al Muderis.
1823 The applicant submitted that the allegation Dr Al Muderis failed to provide reasonable post-operative care to Ms Todd should only go up until September 2015. He submitted that given that, in September 2015, Ms Todd’s regular post-operative care was transferred to Dr Tetsworth and the team at the RBWH, what happened after this point is not relevant to considering whether it is true that Dr Al Muderis failed to provide reasonable post-operative care to her. I do not accept that proposition. The consultation report of 11 September 2015 still refers to Dr Al Muderis wanting to see Ms Todd at Dr Tetsworth’s recommendation or again in 12 months’ time. Further, as apparent from the events described above, Dr Al Muderis continued to be involved in her care after that time. The letter written by Ms Todd sent by Mr Todd via email to Dr Al Muderis on 3 November 2015 does not reflect that intention. In response to that letter, Dr Al Muderis, inter alia, provided his mobile number and told them to contact him any time. Further, Dr Al Muderis was being sent the medical reports from other experts, for example, Dr Dancer, regarding their treatment of Ms Todd.
1824 Ms Todd deposed that she has had numerous admissions to hospital for intravenous drug treatment and would return home with antibiotics. She believed that they were infections; she is aware of the symptoms. In any event, there is documentary evidence supporting her evidence from the years immediately following surgery and more recently. Dr Baker’s medical report of 21 February 2019 describes that Ms Todd was recently admitted to St Andrews Ipswich Emergency for intravenous antibiotics and that she has been on long term antibiotics. Dr Tetsworth’s report of 29 November 2022 records that Ms Todd had recently been admitted to Gold Coast Hospital for a course of intravenous antibiotics. In January 2023, Ms Todd emailed Dr Huang from hospital, informing him that she has been admitted again and is having intravenous antibiotics.
1825 At the time of the hearing, Ms Todd walks with the implant but said she is in immense pain all the time. She uses a wheelchair around the house/complex in which she lives. She described that, at one point in about 2021 she was walking well and was hopeful that she may be able to undertake more physical activities. She has not been able to achieve these goals.
1826 Ms Todd gave evidence that around early 2022, Dr Huang (who she had consulted) told her that the only solution to remove the bacterial infection would be a complete amputation to her left leg, a procedure which she understood would eliminate any possibility of her returning to walk with a prosthetic leg. She said that, at that time, she chose not to have her implant removed, as her leg was not too bad, and she was able to tolerate the pain.
1827 On 29 November 2022, Ms Todd saw Dr Tetsworth in Brisbane. Dr Tetsworth gave evidence that he understood that the nature of Ms Todd’s complaint as at late 2022 was bleeding and discharge, ongoing pain in the left leg, recurrent infections, and increasing irritation, meaning reduction of her mobility.
1828 The respondents submitted that Dr Tetsworth’s report of the consultation has to be treated with caution, as he prepared it knowing Ms Todd had featured in some of the Publications. Dr Tetsworth’s evidence of what he knew about that was somewhat unsatisfactory. It is plain Dr Al Muderis had instituted proceedings by that time. Although not apparent from his report, a separate report from Dr Al Muderis on that date implies he and Dr Tetsworth discussed Ms Todd while she was at the clinic with Dr Tetsworth. I note that report from Dr Al Muderis records that Dr Tetsworth sought advice from him as to Ms Todd’s management. There is an artificiality to this situation, and the report written of his communication with Dr Tetsworth.
1829 Dr Tetsworth was aware of the advice Ms Todd had received to remove the implant, and that that was a reason she consulted him.
1830 Dr Tetsworth’s report goes beyond addressing Ms Todd’s condition and states that he disagreed with the advice about removal of the implant. In particular, he emphasises that Dr Huang had no experience regarding the management of osseointegrated implants, and that other surgeons Ms Todd had dealt with were far less experienced in osseointegration than Dr Al Muderis. I note that Dr Tetsworth also disparaged Dr Huang (and another surgeon) in a report he wrote in relation to Mr Ford.
1831 Ms Todd’s evidence was that, since undergoing osseointegration surgery, she has regularly and consistently experienced: persistent oozing and pus located on and around the surgical site; regular episodes of unprovoked bleeding from the surgical site; excess fatty tissue at the surgical site; pain and discomfort at the surgical site when applying and removing the prosthetic limb; constant pain requiring ongoing and permanent administration of pain relief; depressive episodes of significant severity, including occasions of suicidal ideation; loss of energy; and significant reduction in her enjoyment of life. Even from the brief reference to the evidence above, there is evidence which supports her description of each of those experiences.
1832 Dr Al Muderis described that Ms Todd had successful osseointegration surgery. When questioned as to what that meant, he explained:
The patient underwent a procedure that was performed by inserting the implant … in her leg, and she managed to walk with that … to this day. So from the functional point of view, which is what this surgery is designed to provide, that was successful.
Current state
1833 In closing submissions, the applicant stressed that Ms Todd entered the Court in a wheelchair but got out of it to walk around into the witness box. He also stressed that Ms Todd was walking at the consultation with Dr Tetsworth in November 2022.
1834 Ms Todd has not suggested she cannot walk. It fails to recognise that when Ms Todd initially presented to Dr Al Muderis, she was a highly functional woman, walking and generally in good health. From the time she returned to Queensland after osseointegration surgery she has experienced issues. Although she can walk (using a wheelchair when necessary), she is, on her evidence, in a worse position following surgery. Given what she has experienced since then, as is borne out by the documentary evidence, it is not surprising that she sought a second opinion in October 2015. The view she expressed to Dr Al Muderis in the email of 3 November 2015 is entirely understandable. Ms Todd was in a serious condition.
1835 The applicant submitted that Dr Al Muderis was regularly in contact with Ms Todd and gave examples of him responding promptly to her concerns. Typically, Ms Todd reached out to Dr Al Muderis. That he responded to her concerns with varying degrees of promptness is not a response. He did not follow-up with her. She expressed the view in the 3 November 2015 email that she did not get answers to her questions when she spoke to him, and she did not consider he took her problems seriously. Dr Al Muderis’ evidence, the documentation and submissions are consistent with that. They accentuate any positive aspect and fail to grapple with the negative.
1836 They do so to the extent they do not accurately reflect the situation Ms Todd was experiencing. For example, she said that Dr Al Muderis would tell her to be more active. So much is also borne out in Mr Leech’s 30 January 2015 email – advice that Mr Leech was also giving. Mr Leech’s view appears to be that her fears of infection were unjustified. I do not agree. Ms Todd said she was active, but that was limited by the pain and other symptoms that she was suffering. In those circumstances, it was unhelpful for her to repeatedly be told to do things she either was already doing, or at times, could not do. Her complaints or concerns were not listened to. I note there are other examples of patients being told to be active, such as Ms Mooney and Mrs Gollan (discussed in Part 6, Section 8), when they had medical issues not being addressed by Dr Al Muderis.
1837 Ms Todd deposed:
If I had been warned that I may be left in significant pain or that the procedure might fail and I would lose my quality of life I would not have gone ahead with the procedure. I had coped in my daily life and had lived with my existing stump for 63 years.
1838 As the respondents submitted:
… one of her goals was to remain mobile, so that she could assist her husband, who had been recently diagnosed with Parkinson’s disease. The worst possible outcome for her is what ended up happening, the surgery failing and her being essentially now wheelchair bound.
1839 I accept the respondents’ submission that Dr Al Muderis promised Ms Todd that she would greatly benefit from osseointegration and that it would negate the difficulties she was experiencing using her socket prosthesis (being, essentially, pain), which proved to be completely wrong.
1840 As explained above, I am satisfied that the risks and complications of the surgery were downplayed. There were significant consequences for her and her family (as she was her husband’s carer) if any of the complications eventuated. That circumstance impinged on her assessment of whether she considered herself suitable for the surgery, and whether she would undertake it. This was accepted by Dr Stoita to be a highly relevant consideration for her. As explained above, there is no evidence that this was discussed. In that context, the consequences of downplaying the risks are even more acute. The infections, debilitating pain and loss of mobility have put Ms Todd in a worse off position. Ms Todd’s views as to her aftercare are described in her letter to Dr Al Muderis in November 2015 and reflected in her seeking an opinion from others on multiple occasions because of her concerns. As explained, there was correspondence from other doctors to Dr Al Muderis about Ms Todd which, it is apparent he did not respond to. I am satisfied in the circumstances that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Mr Blythe Warland
1841 Mr Warland became a left below-knee amputee following a motorbike accident in 1987. He used a socket prosthetist for about 30 years. On 22 November 2017, he underwent single-stage left transtibial osseointegration surgery with Dr Al Muderis.
1842 Mr Warland was open, honest and credible. Although, in respect to the order of certain events, he accepted he was confused.
1843 The applicant submitted that save for the last part of Mr Warland’s affidavit, his evidence was generally honest except for some confusion about the timing or order of events and certain details of events. He submitted that his cross-examination should be preferred in favour of his affidavit. I take have taken that into account in considering the evidence below.
Initial consultation
1844 In completing a health questionnaire for Dr Al Muderis’ office on 9 May 2016, he disclosed that he had: current issues with neuromas, pressure sores, ulcers and skin folds; a prior diagnosis of PTSD; chronic pain; depression; back pain; shoulder pain; arthritis; and a range of previous surgeries. Dr Al Muderis accepted in cross-examination that he knew that neuromas and pain were matters of concern to Mr Warland before surgery.
1845 On 14 March 2017, Mr Warland attended a consultation with Dr Al Muderis and other medical professionals, including Dr Ho, a pain specialist. Prior to the consultation, he filled out a standard patient details form, in which he disclosed experiencing “chronic” regional pain syndrome (i.e. complex regional pain syndrome, or CRPS), depression, PTSD, and back pain from limping. Mr Warland gave evidence that he ticked the box for CRPS as he mistakenly read it as “chronic pain”. He said he had not been diagnosed with CRPS at that time. I note a referral letter to a psychologist dated 18 April 2016 refers to Mr Warland suffering chronic pain and makes no reference to CRPS. Nor does the 9 May 2016 questionnaire or Dr Philip Davidson’s referral letter to Dr Al Muderis of 8 March 2017 refer to him suffering from CRPS.
1846 Dr Ho’s consultation report of 14 March 2017, addressed to Dr Al Muderis, included that Mr Warland’s goals for osseointegration included to reduce pain medication and to be able to return to work at better capacity. That those two goals were related is apparent from Mr Warland’s evidence. He explained how his reliance on medication affected his cognitive skills and, in that context, his teaching and related duties.
1847 Dr Al Muderis’ consultation report contained matters typically seen in his first consultation reports for other patients that are in evidence (see Consultation reports in Part 6, Section 1). It contained the standard claim as to how many cases had been performed (“over 291” at that time), that functional capacity in all previous patients had increased dramatically, and the complication rate was extremely low. The pro forma list of risks and complications said to have been given is included in the consultation report. It also includes the standard reference that Mr Warland “does understand the risk of infection associated with this surgery, however we regard Blythe as relatively low risk.” It says that in Dr Al Muderis’ opinion the surgery is “necessary”. There is no reference to Mr Warland’s goals. Although his goals included reduction in pain medication, the report does not reflect that that could not be achieved given osseointegration is not a pain-relieving procedure. Nor is there any reference in the report or any evidence that Mr Warland was warned that his pain might increase after the surgery. As explained in more detail below, I accept that the evidence establishes he did suffer from infections, and his pain increased since undergoing the surgery.
1848 It may be recalled that in the earlier discussion about the multidisciplinary team (see Part 6, Section 1), reference was made to Dr Al Muderis’ evidence in relation to Dr Ho. That evidence was given in respect to his cross-examination on Dr Ho’s report on Mr Warland of 14 March. When aspects of the report were put to him, he purported not to understand what was meant by Dr Ho in the report, but accepted he never sought to clarify that with Dr Ho. Given Dr Al Muderis failure to address the issue of Mr Warland’s pain in his own consultation report, it is appropriate to recall that evidence. Dr Al Muderis said that each member of the multidisciplinary team has their own jobs and “there is a clear demarcation”; he does not “interfere with Dr Ho’s job about prescribing what medications for the patient and [Dr Ho] doesn’t interfere with my job, telling me whether this patient is suitable for surgery or not”.
1849 Two aspects of the consultation on 14 March are worth emphasising.
1850 First, Mr Warland gave evidence of an event that occurred in the waiting room beforehand. He described it was in the context where the psychologist had said he was concerned about Mr Warland’s laissez-faire approach to life and to the proposed procedure. The clinic manager brought an above-knee amputee who was previously a below-knee amputee into the consultation to speak with him. Mr Warland said the patient told him that he was now an above-knee amputee as he had not followed Dr A1 Muderis’ advice.
1851 This may have given Mr Warland some insight to the fact of complications. However, the purpose appears to be to ensure Mr Warland appreciates that, if he proceeds with osseointegration, complications occur in circumstances where patients fail to adhere to Dr Al Muderis’ advice. It is also in a context where it appears that despite the complication (which the patient said was his fault), the surgery succeeded.
1852 Second, as the applicant correctly points out, Mr Warland summarised his evidence in relation to risks and complications as follows: “… he was quite thorough … thorough enough that … I was comfortable that everything had been explained to me, that I was prepared to sign … on the dotted line.” He said he felt comfortable asking questions at the first consultation which, as far as he remembered, were answered.
1853 Mr Warland’s evidence, however, can only be taken so far. Although Mr Warland may have felt Dr Al Muderis thoroughly discussed the risks and complications with him, his assessment of Dr Al Muderis’ duties is necessarily limited. That is, Mr Warland, a layperson, does not know what he does not know. The risks and complications referred to in the consultation report were pro forma. I note that in relation to the risk of infection, the report contained the standard statement that Mr Warland was “relatively low risk”, which Dr Al Muderis accepted was said. Again, that does not sit with the applicant’s evidence that there was a 100% chance of infection. Mr Warland’s evidence was that Dr Al Muderis mentioned a general risk of infection and said words to the effect of: “If it happens, we’ll deal with it”. That was his takeaway from the consultation, which is consistent with the emphasis in the consultation report and the evidence of other patients. I note that there are no references in the report to the risks including chronic and increased pain (particularly when Dr Al Muderis knew pain was a matter of concern for Mr Warland before surgery).
Post-operative complications and events
1854 It is unnecessary to refer to all aspects of Mr Warland’s history. I focus on infections and pain as issues he identified. It can be accepted that Mr Warland did not recall some of the consultations and was confused with the sequence of some events. Consequently, attention is given to any supporting evidence.
Infection
1855 Mr Warland gave evidence of having an infection while in The Hills for rehabilitation after surgery. His evidence was that Dr Al Muderis did not visit him while he was in rehabilitation at The Hills and that he could not get questions answered, including in relation to an infection in his leg. Although Dr Al Muderis initially denied that Mr Warland had an infection at that time, in cross-examination he did not recall it coming to his attention that he had an infection and was otherwise “not sure if he had an infection”. In so far as his initial denial is based on the consultation reports of December 2017, his evidence was that Mr Warland’s stoma and wound were healing well and showed no signs of infection on this occasion.
1856 Mr Warland gave evidence of suffering serious and long-lasting infections in the years following surgery, including an infection that lasted five months. He explained he experienced an infection about every six months. When he suspected an infection – that is, when his stoma skin felt tight and warm exudate started to ooze out, and smelt – he would go to his GP. Although Dr Al Muderis disputes that Mr Warland suffered multiple infections, there is evidence which supports what Mr Warland says. This falls into two categories: records from Mr Warland’s GP; and emails Mr Warland wrote to Dr Al Muderis’ offices, contemporaneously with his infection lasting five months. Neither is to be considered in isolation.
1857 A proper consideration of the GP records supports Mr Warland’s evidence that he suffered repeated infections, with him being prescribed antibiotics. They reflect, inter alia, the description of symptoms he says occur before he goes to the GP with a concern of an infection. The applicant attempts to minimise the evidence of infections in his submissions.
1858 Relevantly, on 22 May 2020, Mr Warland emailed Ms Roberts saying he had had an infection since February, and that it “gets close to gone but isn’t clearing up completely”. He detailed the medication his doctor had him on, included a printout of some test results, and wrote, “Thought I should let you guys know, can you please get back to me to let me know if this is ok?”.
1859 Ms Roberts acknowledged in cross-examination, not surprisingly given the content of the message, that this message deserved a prompt response. She acknowledged he was informing her of a serious matter. Ms Roberts could not remember if she had responded to the message. That said, Mr Roberts in cross-examination suggested that there may have been some response, stating “there’s a lot of different means by which we respond, not just necessarily over email”, mentioning phone calls, text messages, and Facebook. Dr Al Muderis also accepted in cross-examination that the email required a response from him and “it would have been responded to accordingly”. He did not purport to remember doing so.
1860 On 9 June 2020, Mr Warland sent Ms Roberts another email, attaching an updated printout of test results:
Hi Claudia
I have had no reply to my last email, I still have this infection for over 5 months now. I am going to see a infectious disease specialist and getting X-rays of my stump as they are talking about sending me to an orthopaedic surgeon
This is serious and it would be nice to get some guidance from you guys
Cheers
1861 The compelling inference is that Dr Al Muderis’ office had not responded to Mr Warland’s request for assistance.
1862 Dr Al Muderis was pressed in cross-examination about responding to the 22 May 2020 email. He said:
This is a standard swab [referring to the printout of test results in the email], which doesn’t mean that he developed an infection. That’s his interpretation, or his GP’s interpretation. So if it was serious enough, he would have symptoms of an infection and he would have contacted us.
… The patient has mentioned that he has been having issues with his leg for three months. So that has been a chronic problem … that he has. And it could be nerve pain, it could be neuropathic pain. And adding a swab sample doesn’t add any significance, because that it is not necessarily a diagnosis of infection. So it would have been responded to. And he has access to myself, he has access to Claudia, he has access to many people. But it would have been responded to at the time.
1863 To state the obvious, Mr Warland had reached out to them for help to no avail.
1864 On being shown the 9 June 2020 email, Dr Al Muderis disagreed that no response for 18 days was an unacceptable delay in the circumstances:
I disagree with this statement, because there is no correspondence from the GP, and if there was a correspondence from a GP raising serious concern about infection, … that would be responded to, and a swab sample does not mean that there is an infection.
…
… if the patient had signs of infection, that would be addressed immediately. So a swab does not mean an infection and … a swab will grow bugs. If you take a sample from your nostrils or your ears or your mouth, they will grow bugs. That doesn’t mean an infection. Mr Warland had chronic pain in his leg, and that was the most likely diagnosis for his symptoms. Taking a swab doesn’t add any clinical evidence, unless he has clinical features of an infection. Now, if he had clinical features of an infection, he could have gone to emergency, gone to his GP, and the GP would have contacted us. That’s the normal path of communication. … [The] normal path of communication is between clinicians, not a patient diagnosing himself based on a swab.
1865 Those answers were given to justify the failure to respond to Mr Warland. They do not sit with the applicant’s evidence he repeatedly gave and relied on in his submissions; that he gives his contact details to patients which, at the very least, implies that he can be contacted and would respond. His explanation of what is the “normal path” of communication is disingenuous in that context. Only a few answers earlier he said Mr Warland had access to himself and Ms Roberts: see [1862]. There is nothing in the email to suggest, as Dr Al Muderis asserted, that Mr Warland had not been to his GP or that he was self-diagnosing. The 22 May 2020 email included the drugs his GP had prescribed. Rather than acknowledge a shortcoming, the justification for the failure appears to be that Mr Warland’s GP, not Mr Warland, should have contacted him. I note in this context, the document “Osseointegration Surgery A Guide for Patients” (referred to by Mr Roberts and relied on as part of the applicant’s standard practice where patients can access this Guide while in the waiting room: see, Part 6, Section 1 above), includes the following passage:
If you suspect that you have an infection (pain, redness, fever or unusual discharge), please contact the team immediately. Describe your condition in as much detail as possible and send photos to the team to assist with the diagnosis.
1866 That also does not sit with the Dr Al Muderis’ evidence of the “normal path of communication”. I note that these emails, and the cross-examination are not referred to in the applicant’s closing submissions.
1867 The emails confirm Mr Warland understood he had an infection in May or June (the printouts of the test results attached as an image in the email describe infection) and his GP had been prescribing antibiotics, which he was taking.
1868 I note that Mr Warland had a consultation with Dr Al Muderis on 25 June 2020. Dr Al Muderis’ report records that Mr Warland:
… reports that he has significant nerve pain and neuroma pain which is causing him grief and significantly affecting his life. … He has no clinical or radiological sign of infection and we would recommend that the antibiotics are stopped for him. Swabbing the stoma will grow colonised organisms and not indicative of infection [sic].
1869 Dr Al Muderis accepted that he conducted no investigation to confirm whether there was an infection. He explained that was so because Mr Warland had no signs of infection. He elaborated:
[Osseointegration is] a technology in its infancy. It confuses a lot of clinicians when they see it. … when GPs see a piece of metal sticking out of the leg with serious [serous] discharge … the first thing come to their mind is that, “Is this infected or not?” And that’s a natural occurrence and that’s what … we face with osseointegration technology, as osseointegration surgeons, and it will take decades to educate the population of clinicians about what is infected, what’s not infected. So my clinical diagnosis about [Mr Warland’s case], as the person that has done the largest number of osseointegration surgeries in the world – [is] that this was not infected, and his symptoms were clearly neuropathic symptoms.
1870 That answer is problematic. If correct, it only serves to highlight the importance of responding to requests for help from patients. It also highlights the importance of ensuring, in respect to the overseas and interstate patients, that arrangements are in place before they return home connecting them with doctors qualified to address any medical issues that arise.
1871 Mr Warland was clearly of the view that what was occurring was not normal, and was sufficiently concerned to attend a GP, who diagnosed an infection and prescribed antibiotics. As explained above, Mr Warland explained that the symptoms he had when he considered he had an infection, including discharge, were different to what he normally experienced, hence his concern of infection.
Pain
1872 As noted above, on 25 June 2020 Mr Warland reported that he was experiencing such nerve and neuroma pain that it was causing him grief and significantly affecting his life. Mr Warland’s evidence was that the pain he suffers today has been severe, horrendous, and of a kind that had never occurred before the osseointegration procedure. When put to Mr Warland that the pain he described existed pre-operatively, he disagreed. He explained Dr Ho said the different pain he was experiencing may be due to CRPS. Dr Ho’s reports of 11 February 2021 and 7 June 2021 refer, inter alia, to probable CRPS. Dr Anstee accepted that the diagnosis of CRPS is largely clinical and one of exclusion, and there is no specific diagnostic test that can be carried out to confirm its presence.
1873 I note that when Dr Wines saw Mr Warland on 8 August 2022, his consultation report states that there was generalised tenderness to palpation though no obvious signs of CRPS.
1874 Dr Al Muderis records Mr Warland suffering from pain in his consultation reports of 24 May 2018, 30 August 2018, and 5 December 2019 (the last of which describes significant nerve pain causing him grief, and that and he is struggling with the pain). Dr Al Muderis had referred him to Dr Ho. Mr Warland consulted Dr Al Muderis on 14 June 2022, with the report recording, “Mr Warland had quite significant stubbing [sic], burning, and nerve pain on the anterior side of the stoma”. This evidence is consistent with Mr Warland’s evidence of suffering ongoing pain.
1875 It was put to Mr Warland in cross-examination that the chronic pain he had experienced for many years before he had osseointegration was no different in its extremity to the pain he has experienced since the surgery. Mr Warland disagreed with that assertion, explaining only the pain relating to the neuromas was unchanged. It is unclear the basis on which that question was put. As the respondents correctly submitted, Dr Al Muderis has no way of knowing that and is in no position to compare the pain Mr Warland experienced before surgery to the pain he experiences today. Despite that this proposition was put to several of the patients (e.g. Mr Smith).
1876 I accept Mr Warland’s evidence of the level of pain he now suffers, and that he suffers in ways he did not before the surgery. That conclusion does not rest on any concept of CRPS, but rather, Mr Warland’s description of his pain relative to his experience before the surgery.
1877 I note that in November 2020, Dr Al Muderis certified that Mr Warland was totally and permanently disabled. His diagnosis included an amputation with osseointegration, nerve and neuroma pain in his left stump, and left shoulder and back pain.
Complaint and second opinion
1878 Mr Warland has had several issues with connectors on his implant. On two occasions in 2021, he fell because the connector snapped. Following the second fall, he went to see Dr Al Muderis. His evidence was that when he spoke to him about the connector, Dr Al Muderis said words to the effect of: “Do you want me to remove the implant?” Mr Warland said words to the effect of: “No, I want you to fix me.” Mr Warland deposed that it “was the real beginning of the end” and that Dr Al Muderis did not acknowledge his concerns.
1879 He gave evidence of an appointment with Dr Al Muderis following the second fall:
[Dr Al Muderis] said they didn’t break … it was rapid disassemblement, but when you fall on your stump, it doesn’t matter where it breaks or is rapid disassemblement. The outcome is the same. So I went down. … and I actually got to see Munjed. That was one of the only times that I can recall getting him by himself. I explained everything to him. I explained how – that they had broken. … And when I had finished speaking, Munjed turned and looked at the nurse and said, “Book him in debridement,” and just said … words to the effect of, “We will see you for the debridement.” Totally and utterly ignored the fact that – and I’m now on S8 painkillers. … Two of the components fell apart. The first time, I went leg up, stark naked in the wet shower, as I was stepping out, and that hurt. The second time, fortunately, my trailer was – it fell apart right beside the trailer, so I was able to break my fall and landed on gravel, and it hurt … The problem was, I went down to see him specifically about the componentry failure, and he absolutely ignored me. Even if he had of just said, “We will look into it,” I would have been happy with that. But there was nothing, no comment whatsoever, except … “book him in for debridement.”
1880 Mr Warland gave evidence that in seeking a second opinion with Dr Wines, he was told a debridement was not necessary and appears to have declined the procedure as a result. I note there is no reference to debridement in Dr Wines’ consultation reports. This caused Mr Warland concern that Dr Al Muderis simply recommended this treatment unnecessarily without listening to him. That is relevant to Mr Warland’s state of mind.
1881 Mr Warland’s outward attitude to Dr Al Muderis fluctuated over time. He spoke very highly of Dr Al Muderis and the benefits of osseointegration in public (e.g. in 2019, he was interviewed for an article in The Australian). Yet at times he also thought he was not being listened to, he had repeated infections and doses of antibiotics, and he was in more pain. His concern in relation to the connector was dismissed. Mr Warland’s evidence was that he is constantly on pain medication. One of the reasons he had osseointegration was to get off painkillers, but now he takes more of them.
1882 Mr Warland explained that, in some ways, he thinks osseointegration is fantastic, but his experience with osseointegration has taken a strong toll on his life.
1883 The applicant submitted that Mr Warland was a happy patient, and a wholly successful one. Even the brief rehearsal of aspects of Mr Warland’s circumstances above reflects that is incorrect.
1884 The applicant’s suggestion that Mr Warland’s only complaint was an engineering one is incorrect. Again, that a patient did not complain about Dr Al Muderis’ conduct, or lack thereof, does not equate to there being no basis for complaint. The component was more than an engineering issue. Given it was Dr Al Muderis’ implant that was in Mr Warland and that Mr Warland had made relevant inquiries elsewhere about the connector, does not excuse Dr Al Muderis’ conduct in dismissing his concerns. Moreover, Dr Al Muderis’ suggestion was for him to undergo another procedure (a debridement) which did not address the concerns he raised. The falls (particularly the second) occurred because of the connectors and aggravated his injury and pain.
1885 Although the applicant’s oral submission was that Mr Warland’s complaints coincide with his contact with Ms Grieve, it is not ultimately suggested that he concocted his evidence. Certainly, his ongoing infections and Dr Al Muderis’ failure to respond to his emails was before time. That being so, and given he is accepted by the applicant to be an honest witness, it is unclear what that submission is directed to.
1886 I am satisfied that Mr Warland was inadequately advised about the risks and complications of the surgery, and the risks were downplayed. This impinges on his consent for the surgery. There is no evidence Mr Warland was told his pain may increase after undergoing surgery, this was also in a circumstance when pain reduction was an aim of his in having the surgery. There is no evidence Dr Al Muderis addressed that issue in assessing his suitability for surgery. The aftercare of Mr Warland was, at times, also inadequate. Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Mr Peter Mailler
1887 Mr Mailler has had a complex medical history from a young age, which included radiation therapy on his right leg that caused massive scarring affecting soft tissues and bone. Mr Mailler described that the radiation therapy damaged his nerves and compromised circulation in his leg. He experienced infections at the time and subsequently had a higher risk of infection. His right leg was amputated through the knee when he was 15 years old. Mr Mailler had single-stage osseointegration surgery with Dr Al Muderis on 7 July 2014. He was one of the early single-stage patients (as Dr Al Muderis only commenced performing single-stage operations in 2014). At the time, Mr Mailler was 43 years old.
1888 Mr Mailler was a straightforward and honest witness. As the applicant submitted, he gave direct, considered and thoughtful answers to the questions asked of him. That said, he also gave the impression of being stoic, a person who did not complain, but rather blamed himself for some events that transpired (e.g. that he should have advocated for himself better). This is also reflected in his evidence that he thinks “patients need to accept responsibility for their own decisions”.
1889 Although Mr Mailler was regarded as a positive witness for Dr Al Muderis, despite being called by the respondents, his evidence must be seen in its proper context. For example, Mr Mailler’s evidence was that in hindsight, he did not ask about the possible impact of the radiation on the surgery at his consultation with Dr Al Muderis, probably as forcefully as he should have. He said that he did not advocate as strongly for himself as he perhaps needed. His evidence was also that Dr Al Muderis’ failure to quickly escalate the investigation of the issues he raised meant things became worse for him. He said that Dr Al Muderis would have and should have known his issues. From Mr Mailler’s perspective, for a long time, it was obvious that there was something wrong with him. He said that Dr Al Muderis took too long to identify and treat his chronic infection. In his affidavit, he described there is “a natural process of confirmation bias in people looking for solutions to chronic problems that will bias their judgment”, and that Dr Al Muderis needed to be more careful and responsive when dealing with vulnerable people who are in pain and suffering to ensure closer alignment of expectations. I take that to be his opinion based on his experiences.
1890 Given the issues in relation to Mr Mailler, there are two topics I propose to address.
1891 First, in around April 2014, Mr Mailler attended an information seminar presented by Dr Al Muderis about osseointegration, following which Mr Mailler had an individual consultation with him. I note that presenting at the seminar was Mr Brendan Burkett, a patient of Dr Al Muderis, who had undergone the surgery and was a strong advocate for osseointegration and Dr Al Muderis. Mr Mailler described that Mr Burkett’s confidence in osseointegration gave him confidence, although he accepted in cross-examination that Mr Burkett did not present a rose-coloured picture. In any event, following the seminar, he had a consultation with Dr Al Muderis that same day, with his prosthetist present (it being his prosthetist who had arranged the seminar). There was a discussion between Dr Al Muderis and Mr Mailler about the impact of Mr Mailler’s radiotherapy (and his associated medical issues) on osseointegration. Mr Mailler had been the one to raise the issue. Mr Mailler’s evidence was that Dr Al Muderis said words to the effect of: “This is a good stump to work with, there’s no excess tissue”. In cross-examination, Dr Al Muderis recalled stating that, but did not recall Mr Mailler responding: “It has all been irradiated. There’s no excess tissue because it’s all scar tissue”. He accepted that he reassured Mr Mailler about his concern that he had undergone radiotherapy by saying: “There is healthy tissue at the end which is pink, which means there is blood getting to that”. Mr Mailler’s evidence was that he thought the bone higher up was likely to be healthier. He asked Dr Al Muderis about amputating higher to do the osseointegration, to which Dr Al Muderis said words to the effect of: “The shorter you go, the less mobile you’ll be. You lose a lot of control of your leg. You’re better off keeping as much length as you can”. In cross-examination, Dr Al Muderis said that he had a thorough discussion with Mr Mailler and his prosthetist about the amputation point and said it was agreed that there was viable tissue, and the decision was made not to shorten the leg. Mr Mailler agreed that if it was possible to keep the full length of the stump, it would be better for his long-term mobility.
1892 On 27 May 2014, Mr Mailler attended a consultation with Dr Al Muderis. The consultation report states Mr Mailler had x-ray images taken that day (with the report recording they show “[t]he bone quality is poor compared to the non affected femur”). The report also recorded that “[o]verall the skin of the stump is not healthy looking comparatively to the non affected side”. Mr Mailler was assessed that day as suitable for osseointegration and was offered the surgery with Dr Al Muderis describing it in the report as being, in his opinion, “necessary”.
1893 As the respondents submitted, that decision was made without obtaining any input from a radiation oncologist or plastic surgeon who could have informed the assessment. This is despite Dr Al Muderis’ knowledge that Mr Mailler had undergone radiotherapy.
1894 The consultation report contains no reference to the risks of osseointegration surgery (apart from infection) or Mr Mailler’s complicated medical history (including the aggressive radiation therapy and complications following his amputation). These are matters highly relevant to the assessment of Mr Mailler’s suitability for the surgery. Rather the report records that Mr Mailler “does understand the risk of infection associated with this surgery”, he is regarded as “relatively low risk” for infection, the procedure would be “very standard”, and he “would be a perfect candidate for single stage surgery” (emphasis added).
1895 Those descriptors of Mr Mailler, including as “a perfect candidate” are difficult to accept in circumstances where, inter alia, having undergone radiation treatment, which was a contraindication for osseointegration surgery.
1896 Dr Al Muderis’ own affidavit states that “[w]hen [he] first started performing osseointegration surgery, [he] excluded patients who: … (d) had received radiation therapy to the affected limb; (e) had active infections”. Mr Mailler, as noted earlier, was: (1) one of Dr Al Muderis’ early single-stage osseointegration patients; (2) had received radiation on his osseointegrated leg; and (3) had a history of recurring infections. Further, a document titled “Osseointegration Surgery A Guide for Patients” with Dr Al Muderis’ letterhead (produced in mid-2018), records that contraindications for osseointegration surgery include “[r]adiation to the affected bone”. Dr Doshi conceded in cross-examination that prior exposure to radiation was a contraindication. Dr O’Carrigan also accepted that radiotherapy on the limb subject to osseointegration, was a red flag, explaining the patient would need to be told that there is a higher risk of poor healing of the bone onto the implant, loosening and implant failure.
1897 Given this evidence, and Mr Mailler’s medical circumstances and history of complications, it is difficult to understand how Dr Al Muderis could have described Mr Mailler as being a “perfect candidate” with his infection risk being “relatively low” or that the procedure would be “very standard”.
1898 Not surprisingly given that context, Dr Stalley said he regarded Mr Mailler as being of “dubious suitability” for osseointegration due to his history of radiation. He said that the explanation he would have given to Mr Mailler would be as follows:
(1), You have very dubious poor skin; (2) Osseointegration has a very significant incidence of infection at the introitus; (3), The likelihood of you getting an infection at the introitus of a radiotherapy-affected stump is, in my experience – would be 100 per cent. So if you want to go ahead with an operation, you have to go ahead with it in the knowledge that you’ve got a 100 per cent chance of infection …
1899 Similarly, Dr Leung also opined that “[i]n the presence of severe radiotherapy changes in the skin, osseointegration is relatively contraindicated. At the least, plastic surgery opinion should be sought prior to any further operation”. As Dr Geffen outlined in his report: “I would have thought it prudent to seek the opinion of a radiation oncologist prior to his procedure”. The applicant submitted that the opinions should be given limited weight primarily on the basis that they have no expertise in osseointegration. I have already addressed that proposition in assessing those witness: see Part 5, Section 6. Suffice to say as a general proposition, I do not accept that basis. That is particularly so here, given that even Dr Al Muderis’ evidence (and the evidence in relation to osseointegration generally) recognises that radiotherapy to the affected limb was a contraindicator. The opinions expressed do no more than recognise the obvious risks and steps that they opined ought to have been taken to ensure that a fully informed decision was made.
1900 Despite that, the consideration given by Dr Al Muderis to the assessment of Mr Mailler’s suitability did not extend to consulting persons with other relevant expertise, notably oncology and plastic surgery.
1901 Indeed, Dr Al Muderis did not refer Mr Mailler to an oncologist for their assistance until 18 May 2015. The referral to Dr Annie Ho, an oncologist, was made on the basis that he “had constant discomfort” since his surgery. Dr Al Muderis accepted that at that time, he was aware that Mr Mailler was increasingly concerned about the results of his osseointegration and was struggling mentally. By that time, Mr Mailler was in a bad way. Dr Al Muderis’ practice notes for Mr Mailler record that on 22 April 2015, Dr Al Muderis spoke with Mr Mailler’s wife and it was reported that he “continues to have ongoing pain”. Dr Al Muderis’ possible findings were listed as “infection, aseptic loosening or septic loosening” and surgical intervention may be required. As explained above, Mr Mailler was aware of the impact of the radiation on his leg, and that it made him more prone to infection. This was also communicated by Mr Mailler’s GP in her referral letter to Dr Al Muderis, dated 26 May 2014, which stated that Mr Mailler had “the usual host of complications with intermittent [stump] infections” and he “has had a stump infection most years”. In that circumstance, Dr Al Muderis should have been alert to the risk of infections. He would have been aware of this if he had sought advice from a radiation oncologist before he performed surgery.
1902 Second, as apparent from what has already been said, Mr Mailler had ongoing issues with his osseointegration from the time of his surgery, including infections and pain. This started when he was at The Hills for rehabilitation. On 23 August 2014, Mr Mailler emailed Dr Al Muderis stating that, among other things, he had a “[s]econd minor wound infection” and his GP had put him on antibiotics. A report from a nuclear medicine physician, dated 16 October 2014, indicates that Mr Mailler was referred by his GP to undergo a Leukoscan (a bone scan) for “further evaluation of possible infection in the right leg”. The findings of the report, which were sent to Mr Mailler’s GP and copied in Dr Al Muderis, supported an infection being present. Mr Mailler said he was in excruciating pain, there was a lot of pus coming from his wound and he was perpetually on antibiotics, which as identified elsewhere, are markers of infection. At the three-month post-surgery consultation on 25 November 2014, the consultation report recorded that Mr Mailler continued to have pain, “around 7/10 in severity”, and discharge. It also recorded that the CT scan appeared to show no evidence of infection, but the other tests Dr Al Muderis chose to undertake (including a blood test and bone scan) did not exclude the possibility that he had an infection. There were other tests, for example a gallium scan, which could have been, but were not undertaken to detect whether there was infection. In cross-examination, Dr Al Muderis accepted he could have performed a gallium scan but stated that one needs to be careful with prescribing it haphazardly because of its harmful effects, and he did not consider it necessary to administer at the time. Rather, as the report recorded, he was “erring towards the presence of a neuroma in the sciatic nerve that would be causing this pain”. As such, Dr Al Muderis recommended that he perform a neurectomy, which he did on 3 December 2014. It did not resolve Mr Mailler’s issues.
1903 Mr Mailler said that at Christmas time in 2014 he was in excruciating pain. He deposed that at that time he could squeeze his bone and make pus come out of the stoma. He said that at some point in 2015 he went for another bone scan which was also negative for infection. He was increasingly concerned about his circumstances and was struggling mentally with the pressure of running his farm while so unwell and with no notion of how to resolve it. He spoke to a friend who is a radiologist, Dr Carolyn Keith, and asked whether bone scans can produce false negatives. He was told that they can, with Dr Keith suggesting that a gallium scan could confirm this. It is clear Mr Mailler’s concerns prompted him to seek Dr Keith’s opinion. Mr Mailler’s condition is referred to above. Pausing there, given that the correspondence referred to earlier of 23 August 2014 and 16 October 2024 (being the report from the nuclear medicine physician) raised concerns about infection with Dr Al Muderis before the three-month consultation, I do not accept that a gallium scan was unnecessary at the time.
1904 In May 2015, Mr Mailler travelled to Sydney to see Dr Al Muderis personally, which he did on 22 May 2015. In the consultation report for that occasion, Dr Al Muderis recorded that Mr Mailler was still complaining of pain in his stump and discharge. He recorded “Peter feels unwell”. Despite that, Dr Al Muderis denied in cross-examination that Mr Mailler was unwell at the time, stating: “No … he had discomfort and he was struggling with his mobility, but not being unwell”. He plainly was unwell, yet Dr Al Muderis chose to deny the obvious when he gave evidence. Dr Al Muderis recommended immediate hospitalisation, but Mr Mailler explained he could not do so as he needed to return to his farm to finish planting crops, failing which, his business would not survive. As such, Dr Al Muderis prescribed him stronger antibiotics and Mr Mailler returned to his farm. Besides stating that Dr Al Muderis advised Mr Mailler to be reviewed by their infectious diseases consultant, the consultation report made no further reference to infection.
1905 Mr Mailler returned to Sydney thereafter, where he attended Norwest Private Hospital on 1 June 2015 to undergo a stump wound swab. On 4 June 2015, a gallium scan confirmed the results were consistent with peri-prosthetic right femoral osteomyelitis. On 6 June 2015, a consultation report recorded that Dr Al Muderis concluded that the infection was so serious that the implant had to be removed entirely in a two-stage revision procedure. I note that there is no reference to (or it appears, adherence to) Dr Ho’s handwritten letter to Dr Al Muderis of 22 May 2015, which stated that:
My recommendation would be for Peter to undergo hyperbaric oxygen treatment prior to revision/redo of osseointegration if he is keen to have re-op. That might help with post-op healing.
1906 On 8 June 2015, Dr Al Muderis removed the implant from the infected leg, amputated Mr Mailler’s leg higher up at a level of healthy tissue and bone, and about four weeks later, the further implantation at a different osseointegration stem occurred. Between the two procedures, Mr Mailler gave evidence that he was put on a PICC line and his antibiotic treatment was changed dramatically.
1907 The applicant submitted that once the infection was identified it was dealt with promptly. That is so, but if the gallium scan had been performed earlier, it is likely that the infection would have been detected. As explained above, Dr Al Muderis should have been alert to infection given the effect of the radiation treatment on Mr Mailler and his history of infections prior to osseointegration. Given Mr Mailler’s condition at the time of the three-month consultation, Dr Al Muderis should have conducted the appropriate tests to determine if infection was present (noting also this was in the context of the correspondence he had received before then). The neuroma surgery on 3 December 2014 did not resolve his issues, and Dr Al Muderis was aware that by Christmas 2014 Mr Mailler was suffering excruciating pain.
1908 I am satisfied that Dr Al Muderis failed to adequately assess Mr Mailler, at least by not consulting an oncologist before surgery. Dr Al Muderis’ post-operative care in the manner described above was inadequate. He failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Ms Anna Rochford
1909 Ms Rochford was eight years old when her right leg was amputated, after having been diagnosed with an aggressive bone cancer. Ms Rochford could not use a socket prosthesis as her stump was too short. She said she intermittently used a prosthetic leg but had not done so since 2010. On 4 September 2014, she first reached out to Dr Al Muderis’ clinic for advice about the extreme phantom pain she had been experiencing. She said, at that time, “the pain was excruciating all day and night”. She first attended a consultation with Dr Al Muderis on 15 September 2014. There is no consultation report in evidence. On 7 November 2014, Ms Rochford had a neurectomy for right sciatic nerve neuroma performed by Dr Al Muderis. I note that Ms Rochford accessed her superannuation fund to pay for the balance of her surgery. When she first woke up after the surgery Ms Rochford said she “didn’t have a lot of pain” and was “given more pain relief in recovery”. However, the next day she started experiencing extreme pain and spent about ten days in the ICU. Although Dr Al Muderis discussed osseointegration with her, she never underwent the surgery.
1910 Ms Rochford’s evidence was that she has suffered significantly since her surgery with Dr Al Muderis.
1911 Ms Rochford gave evidence by AVL. The applicant submitted that Ms Rochford’s evidence should be approached with caution, and her evidence was often much more dramatic and condemnatory of Dr Al Muderis than contemporaneous records. He also submitted it was inconsistent with contemporaneous records or the inherent logic of situations she described. As a general proposition, I do not accept the description of her evidence as advanced by the applicant. I consider Ms Rochford an honest witness. That said, I accept that care needs to be taken with the reliability of aspects of her evidence. I address the issue to the extent it is relevant below.
1912 I only propose to address certain issues.
1913 First, there is no evidence that Dr Al Muderis referred Ms Rochford to Dr Paterson or any other pain specialist before she underwent the neuroma surgery. It was only after surgery that Dr Al Muderis referred her to Dr Paterson. This is in a context where on her evidence, Ms Rochford told Dr Al Muderis during her consultation that she had fibromyalgia and that her pain tolerance was not very good. This reflected a concern she had as to coping with the surgery. Dr Al Muderis’ evidence was that he did not recall referring her to a pain specialist albeit noting that the “the natural thing to do is for her to see a pain specialist”. He recalled she had a pain specialist locally, being Dr Prickett, who she had seen for many years. It is no answer to suggest that Ms Rochford had a pain specialist she had already been seeing. This is particularly so when Ms Bosley had emailed Dr Al Muderis on 23 September 2014 (being after their first consultation), asking whether he “want[ed] Andrew Paterson involved”. Instead of referring her to a pain specialist, Ms Rochford’s evidence was that in response to concerns she raised during their first consultation about managing her pain, Dr Al Muderis said words to the effect of: “We’ll look after you, we’ll take care of you”. There is otherwise no evidence of Dr Al Muderis consulting a pain specialist prior to Ms Rochford’s surgery. Given Ms Rochford’s circumstances, he should have done so. I note that Dr Paterson opined in his consultation report of 8 October 2015 that the neurectomy performed by Dr Al Muderis and previous attempts to treat her headache, being radiofrequency ablations, had “served if anything, to make her pain worse”.
1914 Second, whatever details of the risks of neurectomy were told to Ms Rochford, her evidence was that Dr Al Muderis said the operation was a simple procedure, likely requiring two to three days in hospital and a couple of weeks at home on pain medication. That was not the case. Dr Al Muderis agreed he “may have” told her this.
1915 Third, there was a discussion during this consultation about osseointegration. Ms Rochford’s evidence was that she brought up the topic of osseointegration because she had discovered during her online research that Dr Al Muderis performed the surgery for amputees. She asked, due to the level of her amputation, whether it would be possible for her to have osseointegration. Dr Al Muderis told her that he had performed osseointegration on another woman on the Central Coast who had their leg amputated as high up as she had, which had been successful. He suggested she would likely need a hip replacement first as her hip had deteriorated since her amputation. He told her that when he was operating on the neuroma, he would look around at the bone and see whether it would be possible to perform osseointegration. Ms Rochford thought osseointegration sounded hopeful, and the discussion indicated to her “[a]n extremely strong possibility” that it could be done in the future. However, Ms Rochford knew the first step was removal of the neuroma. She would then have to wait at least six months to then look at having osseointegration.
1916 Dr Al Muderis denied this conversation as recounted by Ms Rochford (and set out above), giving evidence that he could not have performed osseointegration on Ms Rochford as the height at which her right leg had been amputated meant that she was not a suitable candidate. Specifically, he explained that: he did not have the skills, experience, or technology to perform osseointegration on a short femur at that time; and he did not reassure Ms Rochford that osseointegration would be possible. I note that contrary to the applicant’s submission, Dr Al Muderis’ evidence was not that it was unlikely he told Ms Rochford that it was possible to perform osseointegration on her, but that he dismissed the possibility of being able to do so at that time.
1917 I note that Ms Rochford was sent a letter to attend the osseointegration clinic, dated 2 December 2014 (this was after her neuroma surgery). Dr Al Muderis disputes the meaning of that letter. Leaving that to one side, Dr Al Muderis was cross-examined about the paragraph in the letter that refers to “the opportunity to speak with other Osseointegration patients” at the clinic:
Well, why would it be relevant for Ms Rochford to speak with other osseointegration patients if she was not coming to see you, following up on an inquiry about osseointegration services? -- That is not necessarily the case. It is – for patients who are coming to seek advice and this is the right of every patient, to come. She – Ms Rochford, okay – would be a suitable – potentially suitable – candidate for osseointegration at this particular moment, because she is still wheelchair-bound. As a matter of fact, she can be helped at the moment. She would be, very likely, a suitable candidate for osseointegration surgery at this particular day because we have the technology to help her.
That letter is consistent with Ms Rochford’s evidence that there was a conversation about osseointegration. Further, I note that despite Ms Rochford’s medical circumstances at the time of the hearing, Dr Al Muderis volunteered that she was, at the time he gave evidence, very likely to be a suitable candidate for osseointegration. He volunteered that “she can be helped at the moment”. His preparedness to make such statements without any assessment having been made is consistent with his approach of promoting the surgery. It is also consistent with his focus being only on mobility.
1918 I accept that there was a discussion during the consultation about osseointegration generally of the tenor described by Ms Rochford. Given her circumstances, osseointegration would have been something that she was interested in, and she was hopeful about. The applicant’s submission that the difference in the version of events between himself and Ms Rochford in relation to the osseointegration conversation is immaterial, cannot be accepted.
1919 In the context of that conversation, I also accept Ms Rochford’s evidence that in a subsequent appointment on 27 February 2015, there was a conversation where Dr Al Muderis dismissed the possibility of osseointegration. Ms Rochford had seen Dr Paterson after receiving the letter referred to above. Her evidence was that Dr Al Muderis said words to the effect of: “Paterson says he doesn’t hold up much hope for your future”; and it was “no longer an option to have osseointegration because of how [her] body had reacted”. Dr Al Muderis said he did not recall making either statement. The applicant put to her that that conversation did not occur, which she denied. Regardless of the precise words spoken, given the context above, it is natural and likely, that the topic was discussed.
1920 Fourth, the respondents submitted that on 14 December 2014, Ms Rochford emailed Dr Al Muderis’ office about her ongoing pain and distress, and that it required an urgent response, which did not occur. On the other hand, the applicant, in his submissions, merely described the content of this email, stating that she “said that her condition was ‘much improved’ from hospital discharge”. That does not accurately depict the tenor of the email. Although the email does contain that phrase, the applicant takes it out of context. Ms Rochford stated in her email: “I’m just concerned that, even though things are much improved from hospital discharge, I am still having a great deal of pain”. She then detailed the amount of pain and the consequences of it. She said she was still taking the dosage of medication prescribed when she left the ICU and was struggling to control the pain. I also note the subject line of the email is “Painful – post operative – residual limb after removal large Neuroma”. She does ask for help. When first asked about the email, Dr Al Muderis said he thought an appointment was made for her to come see him at the clinic. Dr Al Muderis then said he could not recall whether he had addressed it in any way and speculated that maybe Ms Bosley took care of it. Ms Bosley forwarded the email to Dr Al Muderis and Dr Khemka the day after receiving it. There is no record of any response. Dr Al Muderis did not meet with Ms Rochford for more than two months after she sent that email, on 27 March 2015, where Dr Al Muderis noted she was “experiencing significant pain in the stump”. The email required a response, and a prompt one. I am satisfied this was an inadequate approach to her aftercare.
1921 I am satisfied that Al Muderis assessed Ms Rochford for the surgery without consulting a pain specialist, downplayed the risks of surgery, and in the events described immediately above, he failed to provide appropriate aftercare.
Section 8 — Domestic patients: other orthopaedic patients
Ms Leah Mooney
1922 Ms Mooney suffered a traumatic injury to her left leg while skiing in Canada on 24 January 2011. She was 59 years old at the time. She came under Dr Al Muderis’ care upon her return to Australia.
1923 Before addressing the issues in detail, it is helpful to give a brief overview of the patient’s history, assess the witnesses’ credit, and resolve several conflicts in the evidence.
Overview
1924 Following Ms Mooney’s accident, she was treated non-operatively in British Columbia, before returning to Sydney for surgical treatment on 30 January 2011. She was taken to Sydney Adventist Hospital by ambulance on arrival.
1925 On 31 January 2011, Dr Al Muderis consulted Ms Mooney after receiving a referral from Dr Ali Gursel. He gave evidence that, on 1 February 2011, he performed an arthroscopic assisted minimally invasive open reduction and internal fixation of the tibial plateau and tibial shaft fractures (first surgery). Ms Mooney gave evidence that after surgery, she complained her left leg pointed in one direction.
1926 On 23 February 2011, due to valgus malalignment of Ms Mooney’s leg, Dr Al Muderis performed revision surgery at Macquarie University Hospital (second surgery). There, she received post-operative treatment and was later transferred to Lady Davidson Hospital, where she was discharged on 25 March 2011.
1927 After discharge, Ms Mooney raised concerns about her leg with others (including to her GP, Dr Louisa Ahmed), which culminated in an appointment with Dr Stuart Watson on 19 April 2011. He provisionally diagnosed osteomyelitis of the tibia and informed Dr Al Muderis. Ms Mooney had a consultation with Dr Al Muderis on 21 April 2011, but he dismissed any suggestion that she had an infection.
1928 On 20 July 2011, Ms Mooney fell causing a femoral fracture. The next day, Dr Robert Sew Hoy performed remedial surgery at Mona Vale Hospital. While in rehabilitation, Dr Bernie Hudson, an infectious diseases specialist and microbiologist, became concerned about her leg and the possibility of infection. Ms Mooney was discharged on or about 20 August 2011, with the discharge notes recording she was taking flucloxacillin and clindamycin for osteomyelitis. On 29 August 2011, she was seen by Drs Ed Marel, David Dickison and Chris Roberts, who reported to her GP “that it is more likely that infection is destroying this knee rather than reflex sympathetic dystrophy”, which led to her seeing Dr Andrew Ong for x-rays and a CT scan. Dr Ong opined the results were consistent with established osteomyelitis.
1929 On 31 August 2011, Ms Mooney rang Dr Hudson and told him she was in severe pain. He advised her to go to the emergency department at Royal North Shore Hospital (RNSH). The following day, she attended the RNSH emergency department. Dr Papadimitriou examined her and concluded, based upon his review of the x-rays and CT scans, that:
… she had osteomyelitis and septic arthritis of the knee and that any prospect of joint salvage, we had missed the boat for. … the joint was already destroyed. Major erosions of the bone in the femur, kneecap, patella and tibia, and the joint … had almost no motion … the infection had already pretty much done its worst locally, but it was still causing her symptoms in the sense of pain.
1930 On 9 September 2011, Dr Papadimitriou operated on her knee. His report records performing “a left knee arthrotomy, debridement and biopsy, removal of left tibial nail and associated screws, and left tibial debridement and removal of broken drill bit”. Dr Papadimitriou gave evidence that Ms Mooney’s infection was “very extensive”, and the degree of bone destruction indicated it had been there for some time.
1931 In 2012 Ms Mooney made a complaint to the HCCC about Dr Al Muderis. In 2013, Ms Mooney commenced legal action against Dr Al Muderis alleging negligence. In 2016, orders were entered by consent in the Supreme Court of New South Wales allowing the proceedings and awarding $1,750,000 to Ms Mooney, inclusive of costs. Ms Mooney’s complaints were made prior to the Publications.
1932 Ms Mooney was not a subject of the Publications. In that context, the applicant submitted in closing that Ms Mooney’s case was over a decade before the Publications, that she underwent emergency surgery, that Dr Al Muderis was obliged to operate, that he was a junior surgeon at the time, and the surgery was in relation to the worse type of break that can occur to a tibia. It was contended therefore that the events are not “even remotely relevant” to the Publications. Although it can be accepted that aspects of Ms Mooney’s case are unique in these proceedings, the relevance of this case study is to be assessed in light of the imputations carried.
1933 However, I note that part of the applicant’s submission is premised on the fact that he was a junior surgeon at the time. It is unclear what reliance he has placed on this fact, given his case in relation to Ms Mooney is that he did nothing wrong. His evidence was:
Ms Mooney’s incidents have changed my life, and … it did affect me deeply, and to this day, every day I wake up, I think what would I have done different, and to this day, I think that I’ve done everything that I could do to help this woman.
1934 Although I address the applicant’s credit above, it has particular difficulties as it relates to Ms Mooney.
1935 Dr Al Muderis’ preparedness to make the assertion on oath that he thinks of Ms Mooney every day, attempting to embellish his evidence, tells against his credit. Even if the assertion is hyperbole, it is made (when not true) to emphasise his concern for the position Ms Mooney was in. Similarly telling, is his evidence that he cannot conceive that more could have been done in her case, even with the benefit of hindsight. Among other things, revision surgery was required and he erroneously dismissed Dr Watson when he raised the possibility of osteomyelitis (discussed below) in circumstances where he should have suspected Ms Mooney had an infection. Moreover, despite the 2013 proceedings resolving in favour of Ms Mooney, the applicant in these proceedings chose to challenge any assertion critical of his conduct. In doing so, he made allegations that Dr Papadimitriou, Ms Mooney and Mr Tim Mooney lied in evidence. As I explain below, I do not accept those allegations. This is also in a context where, as explained below, the applicant’s case significantly changed in relation to this witness, with his concession in cross-examination about having observed a deformity during the first surgery, being a concession which was only recognised by the applicant in his written submissions in reply.
Witnesses
Ms Mooney and Mr Mooney
1936 The applicant submitted that the Court could not rely on the evidence of either Ms or Mr Mooney. In addition to the allegations of dishonesty, among other things, he alleged that Ms Mooney’s recollections are skewed to focus on the issues she put forward in the 2013 proceedings. He further alleged that her and Mr Mooney’s recollections contradict each other, offering examples.
1937 Ms Mooney was an honest and forthcoming witness. Her reliability as a historian was affected by her recall, which, at times, was lacking. That is readily understood given the passage of time. However, on significant matters her recall was clear and supported by contemporaneous (or near contemporaneous) records. I accept her evidence to that extent.
1938 Mr Mooney was also an honest witness. He had a clearer recall of events. He was generally a reliable witness. Similarly, in respect to significant matters, his evidence is supported by other evidence.
Dr Papadimitriou
1939 Dr Papadimitriou is an orthopaedic surgeon based in Sydney. His chief practice is at RNSH and North Shore Private Hospital. He has also worked at Ryde Hospital, Sydney Adventist Hospital, and Dubbo Private Hospital. He has specialisations in trauma management and joint replacement.
1940 Dr Papadimitriou was an honest and reliable witness. He had a good memory of events and had reviewed the records before giving evidence. He was clearly experienced in his field and qualified to speak on the topics he did. I accept his evidence of Ms Mooney’s condition, the basis of it, what he did to treat her and why it was necessary to do so.
1941 Dr Papadimitriou’s cross-examination was conducted in a combative manner, with him being accused of making up evidence. I reject the submission that Dr Papadimitriou was giving false evidence. His evidence is supported by the material available to him at the time. The questions asked of him to that effect in cross-examination appear to be without evidential foundation, as do the submissions advanced in closing. It is to be borne in mind that Dr Ruff’s evidence in relation to Ms Mooney supports that of Dr Papadimitriou.
1942 The applicant submitted that Dr Papadimitriou was not called as an expert witness, such that “any opinion that he proffers that falls outside his direct observations in 2011 is inadmissible”. Given the submission, it is appropriate to address the sequence of Dr Papadimitriou’s evidence.
1943 Dr Papadimitriou was led viva-voce, there being only an outline of evidence. The applicant’s complaint during the hearing was based on the absence of an expert report, being primarily the failure to give notice of the evidence to be given. He was a treating doctor not being called as an independent expert. The admissibility of evidence of Dr Papadimitriou’s opinions requires s 79 of the Evidence Act to be satisfied. To be admissible under s 79(1), the evidence must satisfy two criteria: first, the witness “has specialised knowledge based on the person’s training, study or experience”; second, the opinion expressed by the witness “is wholly or substantially based on that knowledge”: Dasreef Pty Ltd v Hawchar [2011] HCA 21; (2011) 243 CLR 588 at [32]. In any event, non-compliance with r 23.13 of the Federal Court Rules 2011 (Cth) or the Expert Code of Conduct could not have affected the admissibility of the evidence but only goes to weight: Axent Holdings Pty Ltd t/a Axent Global v Compusign Australia Pty Ltd [2020] FCA 1373 at [809].
1944 I gave the applicant the opportunity for the witness’ evidence to be adjourned before cross-examination permitting him time for further preparation if that was considered necessary, but he chose to cross-examine on what he could at that time. Dr Papadimitriou referred to several documents (scans, inter alia) that he had access to before Ms Mooney’s surgery. On completion of the cross-examination, the respondents sought the production of those documents referred to by Dr Papadimitriou before re-examination. The witness was stood down. This was at the conclusion of the first tranche of evidence in October 2023.
1945 The second tranche of evidence in the hearing commenced in March 2024. In the meantime, two affidavits from Dr Papadimitriou were produced which, inter alia, listed and produced the material he had access to when treating Ms Mooney. Only two paragraphs in one of the affidavits were objected to, which commented on three of those documents. The material in the affidavit could have been the subject of re-examination without any requirement for further affidavits. On that basis I admitted the two paragraphs. The affidavits provided the applicant with notice of what would have been in re-examination and entitled the applicant to cross-examine on it. It is to be recalled the primary objection originally was the absence of notice. The applicant ultimately cross-examined on this material before there was any re-examination.
1946 Although Dr Papadimitriou did not give evidence as an independent expert, he was entitled to express opinions based on his expertise. Any such opinions fell within s 79 of the Evidence Act. The applicant did not suggest otherwise. To take a simple example: the applicant cross-examined Dr Papadimitrou on several topics on which he was qualified to express opinions, such as osteomyelitis. He did so, and the opinions are admissible because of s 79. In that circumstance, there is an artificiality to the applicant’s submission that his evidence is confined to what he directly observed. The applicant had a full opportunity to cross-examine the witness. He identifies no prejudice.
1947 The applicant also submitted that Dr Papadimitriou was unreliable, said to be demonstrated by the fact he could not now distinguish between what he knew in September 2011 and what he has subsequently discovered or deduced since then. It was submitted that the Court could not conclude that his evidence is his actual recollection of what he was told at the time. As a “good example” the applicant referred to Dr Papadimitriou’s description during his evidence-in-chief of Ms Mooney’s medical history the first time he saw her. The applicant submitted that it was “incomprehensible that Ms Mooney gave a history to that effect”. However, I note his consultation report for 1 September 2011, the day on which he first saw Ms Mooney, provides a detailed history consistent with his evidence-in-chief.
Dr Ruff
1948 Dr Ruff’s credit is addressed elsewhere. Suffice to recall that Dr Ruff is eminently qualified to give evidence on the subjects to which he spoke. His evidence was clear and considered. He made concessions where appropriate. His evidence supports that of Dr Papadimitriou.
1949 Although the applicant accepted that Dr Ruff was impressive and forthright in his oral evidence and had clearly attended to assist the Court, he submitted that, in relation to Ms Mooney, Dr Ruff’s written report was in many respects unfairly critical of Dr Al Muderis. I readily accept the former proposition, and I return to address the latter below. Suffice to say I do not accept it.
1950 The applicant criticised both doctors and submitted that Dr Papadimitriou and Dr Ruff recommended that Ms Mooney sue Dr Al Muderis, which Ms and Mr Mooney denied. Dr Papadimitriou and Dr Ruff each denied recommending that Ms and Mr Mooney litigate. The evidence referred to by the applicant does not support his submission. The high point for the applicant is the note of the conversation he had with Ms and Mr Mooney on 20 November 2011 (recited below), where Mr Mooney recorded that he had told Dr Al Muderis many doctors had told them to take legal action. Despite all the evidence, the applicant nonetheless advanced the submission, claiming in relation to Dr Papadimitriou, that he “plainly did so”. I do not accept that submission. Even if I did, it does not affect my assessment of his evidence. The applicant does not advance how this has impacted Dr Papadimitriou’s evidence, particularly given what matters are now actually in dispute. The applicant’s submissions as to Dr Ruff do not suggest that he is not an expert witness honestly, credibly, and reliably giving evidence to assist the Court.
1951 The applicant’s criticisms, at times, seem to be made for the sake of it. For example, the applicant submitted it is remarkable that Dr Papadimitriou made no enquiries at all of any of the doctors that treated Ms Mooney from February to July 2011, and he did not review the x-rays from Mona Vale Hospital taken in July and August 2011, even though they were available to him. He submitted that Dr Papadimitriou’s explanation for these omissions was unconvincing and evidenced his bias against the applicant. Dr Papadimitriou gave evidence of the reports, scans, and x-rays he had in making the diagnosis in relation to Ms Mooney’s knee. I do not then understand how the failure to directly contact these doctors evidenced bias.
1952 As explained below, there is now no challenge to Dr Papadimitriou’s evidence that Ms Mooney suffered from chronic osteomyelitis at the time he operated on her. Nor is Dr Ruff’s evidence as to the timing of the chronic infection challenged. No alternative timing was put to Dr Ruff.
Dr Qurashi
1953 I note the applicant chose to call Dr Tetsworth as his expert witness in relation to Ms Mooney in his case in chief. However, in closing, the applicant only relied on Dr Qurashi who was called in reply. His reply evidence was limited to evidence relating to, or associated with, the scans produced by either Dr Ruff or Dr Papadimitriou in the hearing during the respondents’ case. That is because the other evidence in Dr Qurashi’s report sought to be relied on in reply related to matters on which the applicant was on notice and had been (or could have been) addressed by Dr Tetsworth in his expert report, or his evidence.
1954 In relation to Ms Mooney, Dr Qurashi said there was no evidence of any deformity at the end of the 1 February 2011 surgery but accepted in cross-examination that if Dr Al Muderis gave evidence that he had seen a deformity intraoperatively (information with which he had not been provided), his report would be incorrect. Dr Al Muderis, as explained below, did give that evidence. The applicant’s submission that Dr Qurashi was not deterred from his opinions in cross-examination does not reflect a proper reading of his evidence. The concession he made in relation to Dr Al Muderis’ evidence on the deformity, is one example.
1955 I accept Dr Ruff’s evidence including to the extent it conflicts with Dr Qurashi’s evidence.
Conflicts in the evidence
1956 There are several direct conflicts in the evidence that impact the conclusions in this case study and shed further light on the witnesses’ credit.
1957 First, there are competing descriptions of Ms Mooney’s two surgeries with Dr Al Muderis. As explained above (in the section addressing consultation reports in Part 6, Section 1) in a 21 April 2011 letter dated to Dr Ahmed, Dr Al Muderis said in the first paragraph:
[Ms Mooney] was seen by one of our experienced orthopaedic surgeons, Dr Ali Gursel, who then referred her to me due to the complexity of her injury to manage her tibial plateau and tibial shaft fracture. I attended to her with multiple surgeries. The first stage was to stabilize the fracture by plate and screws and then the second stage was to permanently fix the fracture with an intramedullary nail and bone grafting to the tibial plateau.
1958 That summary of events in the letter, which creates the impression that a two-stage process was intended, is incorrect. Although the applicant submitted this was a mistake, it is difficult to understand, given the content, how that could be so. It is designed to recast the events in a more favourable light, to disguise that the second surgery was required because of his conduct in the first. That Dr Ahmed may have, by other means, become aware of the fact it was revision surgery does not alter that.
1959 Dr Al Muderis maintained and embellished this in his 14 July 2011 report to Dr Ahmed:
Her injury was so extensive that I performed two surgeries the first being to stabilise her fracture of the tibial plateau and shaft with a plate and screws and second surgery to remove Leah’s plate and screws before inserting an intramedullary nail.
1960 In these proceedings, Dr Al Muderis accepted the second surgery was not planned.
1961 Second, Ms Mooney gave evidence that shortly after the first surgery, her son pointed out to Dr Al Muderis in their presence that Ms Mooney’s leg was crooked, and Dr Al Muderis replied: “No, that should be okay”. Mr Mooney also described that after the first surgery, Ms Mooney’s “leg went off at an angle”. I accept that occurred. Similarly, I accept Ms Mooney’s evidence (and Mr Mooney’s evidence to a similar effect) that Dr Al Muderis said before the second surgery: “I won’t get it wrong again, my reputation depends on it. The plate was manufactured incorrectly, it’s the third time this has happened. I will change my suppliers”.
1962 Ms Mooney made statements to the same effect that were contemporaneous with these events. Dr Papadimitriou gave evidence that Ms Mooney, in giving her medical history to him in 2011, said that she and Mr Mooney had pointed out the crooked leg to Dr Al Muderis, who (on his recall) “told her there was a problem with the plate that had caused it and he had had similar problems with the plate in the past and that he would stop using that plate”. I accept Dr Papadimitriou’s evidence of that. I note that the timeline attached by Ms Mooney to her complaint to the HCCC has entries that record, and are consistent with, these two conversations with Dr Al Muderis.
1963 I prefer the evidence of Ms and Mr Mooney on this topic. This conversation also reflects that Dr Al Muderis was prepared to blame what had occurred on the equipment. There is no basis for doing so, and Dr Al Muderis does not suggest there is. I note also that Ms and Mr Mooney’s evidence – that they saw a deformity after the surgery – is also supported by Dr Ruff’s evidence, that the deformity was immediately apparent. I return to this topic below.
1964 Dr Ruff explained that medical professionals have an “overarching responsibility … to be honest” with their patients:
With respect to the first operation complicated by the failure of reduction and fixation of the fracture, Dr Al Muderis’ correspondences to Dr [Ahmed] … suggesting the fracture was managed in a staged manner to first correct the joint surface and the second to correct the mechanical axis is at best disingenuous. His discussion with the Mooneys immediately prior to the corrective surgery where he informed Mr Mooney the deformity was due to the plate and that he was having trouble with his manufacturer because he had 3 plates with the same problem is at best disingenuous and probably dishonest.
1965 Third, the timing and content of a file note made by Mr Mooney recording a telephone call from Dr Al Muderis to Ms Mooney is in dispute. It is not ultimately in dispute that the telephone call itself occurred in November 2011, or that Ms Mooney initially spoke to Dr Al Muderis before handing the telephone to Mr Mooney.
1966 The note, which Mr Mooney transcribed, is in evidence.
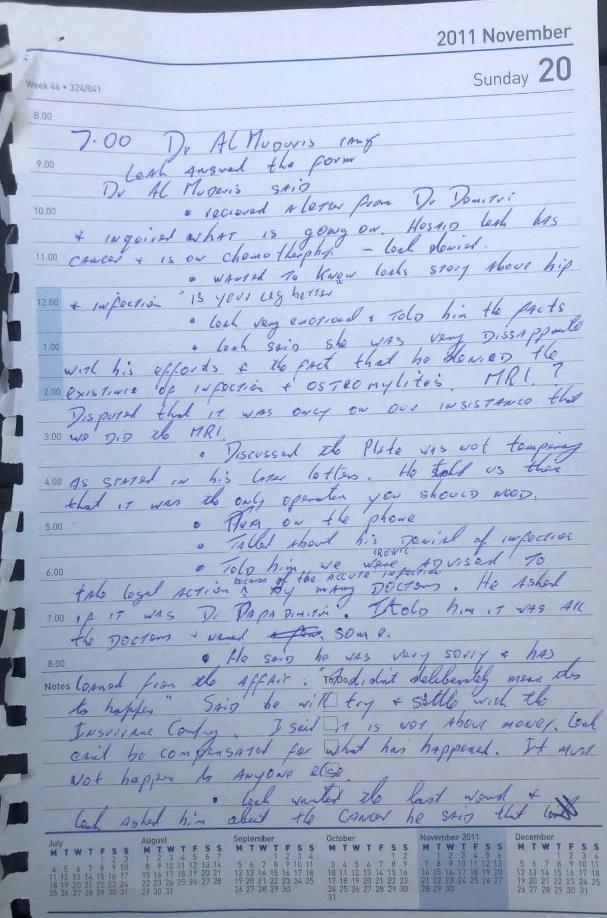
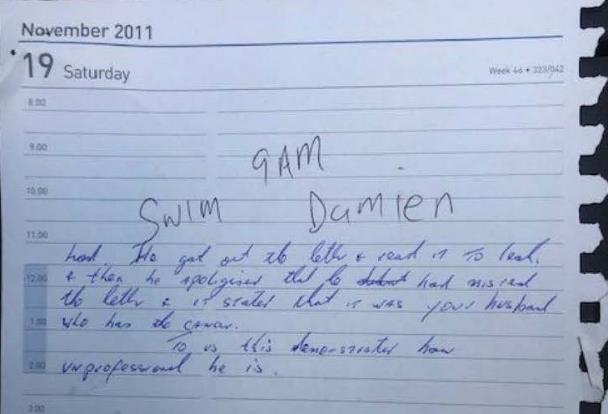
1967 Ms and Mr Mooney gave evidence the call occurred on 20 November 2011. The applicant submitted that the “so-called ‘file note’ of the conversation” is a significant point of credit in respect to Ms and Mr Mooney. He alleged some of the note’s contents were inaccurate, and that Ms and Mr Mooney lied in saying it was made contemporaneously, submitting it was not made until 2014. Mr Mooney’s evidence was that he made the note within five minutes of the conversation occurring.
1968 Given the note is written on a page with the date pre-printed, the applicant insinuates that in 2014, Ms and Mr Mooney retrieved a diary from 2011 to fabricate the note and aspects of its contents.
1969 I do not accept the applicant’s submissions as to the note’s timing. In written submissions, the fabrication allegation is said to be based on a comment Mr Mooney made in cross-examination:
[Dr Al Muderis] wrote letters to Dr Ahmed saying, “I intended to do this over two operations,” and all our experts said that was absolute lie, because it was obvious what he did in the first operation was to fix it properly with the plate.
(emphasis added)
1970 The applicant submitted the file note was not contemporaneous because it includes advice given by experts in the 2013 proceedings. However, the note does not contain any reference to such advice. It records, “the plate was not temporary as stated in his later letters. [Dr Al Muderis] told us then that it was the only operation you should need.” Mr Mooney identified in cross-examination that he had received the letters sent to Dr Ahmed by Dr Al Muderis, recited above at [1957] and [1959], which was the basis of the issue he raised with Dr Al Muderis in the November conversation about the number of operations they were told Ms Mooney needed. Given his and Ms Mooney’s experience with what occurred, it was plain that the statement in Dr Al Muderis’ letter to Dr Ahmed dated 14 July 2011 was incorrect. Mr Mooney had that letter at the relevant time – a matter not addressed in the applicant’s submission.
1971 I note also that the applicant submitted in closing that his allegation as to the timing of the file note’s creation was made in response to Mr Mooney’s evidence. However, that cannot be correct as that allegation was also put to Ms Mooney, who gave evidence before her husband.
1972 The applicant submitted that Ms Mooney telling Ms Grieve that the conversation was about 12 months before the settlement, which he says occurred in early 2016, is consistent with the note being prepared in mid-2014. However, a statement of that nature made in 2022 to Ms Grieve (which relates to the conversation, not the note) does not undermine Ms Mooney’s evidence as to the contemporaneous nature of the note, or the timing of the call. There is only one call. Dr Al Muderis gave evidence of the call being in November 2011, and the applicant conceded so much in oral submissions. The timing of the call is consistent with its contents and the purpose for making it.
1973 As to the note’s contents, the applicant submitted the note does not accurately record the conversation. It records that Dr Al Muderis “was very sorry”, that he “has learned from the affair”, that the outcome was not deliberate, and that he will “try [and] settle with the insurance company”.
1974 Although Dr Al Muderis accepted that he said he was sorry for Ms Mooney’s suffering, he denied saying: “I didn’t mean it to happen. I’m sorry it happened. I’ll take a step back and let the legal people handle it. You’ll get a big payment”, or that he would learn from this. His evidence was also that it was Mr Mooney who said that “it’s all about money” and that the “insurance companies will settle it”. Although Dr Al Muderis said in cross-examination that Mr Mooney’s “words … remained in my head forever” and that he was “absolutely shocked”, he makes no reference in his affidavit to what Mr Mooney purportedly said. When it was put to him that Mr Mooney had said, “this is not about money, but Leah has to be compensated for what happened and this can’t happen to anyone else”, he disagreed and asserted it was he, not Mr Mooney, who said those words.
1975 I note that in Ms Mooney’s 13 July 2012 complaint to the HCCC, she records that Dr Al Muderis was “very apologetic and sorry this has happened[.] [He] [d]idn’t mean it to happen to me”. That was made relatively proximate to the event. That is consistent with Ms and Mr Mooney’s evidence of the timing of the call, and Mr Mooney’s note of its content.
1976 I do not accept the applicant’s evidence on this topic.
1977 I accept the evidence of Ms and Mr Mooney as to the timing of the conversation, the timing of the note, and its content. That evidence accords with the events that were occurring at about that time (e.g. having received a letter from Dr Papadimitriou, and Mr Mooney dealing with cancer). I accept their evidence that Dr Al Muderis apologised, and said he did not mean it to happen, and that it was he who raised the matter of insurance. I do not accept the applicant’s submissions.
Medical issues
1978 Turning to the medical issues. There are three issues to address: the malalignment (management of the tibial plateau fracture), the failure to remove the broken drill bit, and post-operative care.
Management of tibial plateau fracture
1979 Dr Al Muderis ultimately conceded in cross-examination that he observed a deformity during Ms Mooney’s first surgery despite initially denying that any malalignment was obvious. He explained:
… there was a residual deformity that could not be rectified at the time of that particular surgery, considering that the surgery took more than five hours, and the decision had to be made to conclude the surgery without compromising the patient leg …
1980 The applicant’s submission simply ignored that evidence until his written reply (after the oral closing submissions). Significantly, when this evidence was referred to in reply, he did not address that it was contrary to the case he had been advancing. His concession is inconsistent with his repeated evidence (beginning in his affidavit) and submissions that, at the time of surgery, there was no malalignment and that because of the swelling he could not tell if there was any malalignment. If he observed a deformity, the fact he denied it repeatedly, on oath, tells against his credibility.
1981 Dr Ruff’s evidence was that the intraoperative images show a significant and “very obvious” valgus deformity (of at least 15 degrees). He said it should have been seen intraoperatively and corrected at the time. To the suggestion that Dr Al Muderis may not have been able to see the valgus deformity at the end of the surgery because of the severity of the swelling, Dr Ruff replied, “It would have been obvious”.
1982 The second surgery should not have been necessary. Dr Ruff was clear that Dr Al Muderis could have rectified the malalignment at the time of the first surgery, explaining that even when the plate is on, a surgeon can take it off and redo it. He explained the best time to have fixed it was there and then. I accept that evidence. Dr Papadimitriou’s evidence was consistent with that evidence.
1983 The applicant submitted that Dr Ruff’s criticism of the 1 February 2011 surgery was based on five intraoperative images, when the full set comprised of 39 images. That submission, advanced to minimise the criticism’s significance, does not assist. Although all 39 intraoperative images were before the Court, the applicant does not explain how the balance of the images might affect Dr Ruff’s opinion. I note Dr Ruff’s opinion was unchanged when he was re-examined on an image not included in the limited set, being the last point-in-time image.
1984 The applicant’s submission referring to Dr Ruff’s concessions is selective. For example, in submitting that Dr Ruff conceded that a valgus deformity can occur after the procedure from collapse of the fracture, the applicant omits his evidence that with the Less Invasive Stabilisation System (LISS) and locking screws, it is highly unlikely to occur as the system is designed to stop that from happening. Dr Ruff went on to explain that the deformity is visible on the intraoperative images and had not changed since the plate was put on. Dr Ruff’s evidence was that when Dr Al Muderis saw a deformity intraoperatively he either did not recognise or did not want to recognise the deformity. A further example is the reference to Dr Ruff’s concession that an 18 February 2011 x-ray shows a valgus deformity of 15 degrees. Although that is correct, his evidence relevantly was that “[t]he deformity should have been evident to Dr Al Muderis assessing the alignment intra-operatively with the image intensifier screening” during the first surgery. He also gave evidence that the images show that the plate is too long, and inappropriately fixed, which contributes to further valgus. The applicant’s submissions also fail to grapple with Dr Al Muderis’ concession that there was malalignment observed by him in the first operation.
1985 Dr Ruff’s evidence is consistent with the evidence of Ms and Mr Mooney that the deformity was immediately apparent.
1986 In so far as the applicant relies on his operation notes at the time, an issue arises as to the confidence one can have in those notes. The notes’ recording that “[p]osition of fracture is then re checked with II showing acceptable alignment from the limited views” is relied upon by the applicant to demonstrate that there was no malalignment. However, that submission is inconsistent with Dr Al Muderis’ evidence in cross-examination that he observed a deformity at the time of surgery, different to what was advanced in his written submission in closing, before his case changed in reply, where the applicant then acknowledged that evidence.
1987 I note also the applicant’s submissions at times erroneously approached the issues as if the respondents must establish propositions beyond reasonable doubt (e.g. by making the submission it is “possible that the fracture collapsed slightly to cause” the significant deformity while Ms Mooney was at Lady Davison Hospital).
1988 I am satisfied that Dr Al Muderis’ performance of the 1 February 2011 surgery did not accord with the usual management of a tibial plateau fracture.
Failure to retrieve drill bit
1989 It is uncontentious that a drill bit broke off during the first surgery and was left in Ms Mooney. Dr Al Muderis’ evidence was that this is a relatively common occurrence, and it is often more harmful to remove the drill bit than to leave it in. He did not consider it clinically appropriate or in Ms Mooney’s best interests to retrieve it.
1990 Although Dr Papadimitriou accepted that a failure to remove a broken bit is not always a problem, he explained it can become one if an infection occurs, if it obstructs future surgery, or if it migrates. He explained that the drill bit is left inside the bone.
1991 He explained that in Ms Mooney’s case, the drill bit could have been removed, and he would have removed it at the time of surgery:
… what a surgeon would normally do is make an assessment – the harm that comes out of taking it out versus the good that comes from taking it out. We don’t lightly leave drill bits in. … it’s an awkward conversation with a patient to tell them that they’ve got a broken drill bit in their tibia. … it brings in a process where, essentially, there’s an incident form put in in the hospital. You have to record it in the notes … the other thing is, for the patient is it’s a lot easier to remove it before the fracture is healed … because you still have fracture gaps.
1992 His evidence that it is an event which is required to be recorded in the hospital notes can readily be accepted. It is an incident that occurred during surgery which may have future ramifications.
1993 Dr Al Muderis’ evidence was that the decision not to retrieve the drill bit is not necessarily something that needs to be noted in the operation report because it is inconsequential to the patient and was obvious in a post-operative x-ray. I find it difficult to accept that leaving a drill bit in a patient is not a matter which a surgeon is required to record in an operation report. By it not being referred to in the reports, the fact it occurred is not obvious. That it might be obvious on looking at the x-rays is not a response, as identifying the relevant information would require looking beyond the operation report to see what occurred.
1994 Dr Ruff gave evidence that the intraoperative images show that the drill bit broke before the plate was secured and it could easily have been removed. He explained it follows that Dr Al Muderis’ observation that its removal would pose greater problems than its retention is untrue. Dr Papadimitriou also gave evidence that, from reviewing x-rays taken during the 1 February 2011 procedure, it was apparent to him this had occurred at that stage of the surgery. Regardless of whether the drill bit ought to have been removed, I prefer their evidence to Dr Al Muderis’ evidence that the drill broke off as the final screws were being inserted (i.e. after the plate was secured).
1995 Dr Al Muderis said he mentioned the drill bit to Ms Mooney. She and Mr Mooney gave evidence that they did not know that Dr Al Muderis left a drill bit in Ms Mooney until Dr Papadimitriou told her in September 2011, when it was apparent on scans that had been taken in relation to her admission to the RNSH. Dr Papadimitriou discussed the drill bit with her because:
… part of what we had to do was to remove the implants and part of the implant was the drill bit … there was the potential that we would need to increase access to the bone. Do a thing called a bone window … And that can have some implications in the future … there’s more opportunity for the bone to break.
1996 He gave evidence that Ms Mooney did not know there was a drill bit and was upset to find that out. That is consistent with her and Mr Mooney’s evidence. This discussion was proximate to the events in question. Given the nature of the information, it would have been expected that if Ms Mooney had been told about the drill bit at the time by Dr Al Muderis, she would remember it.
1997 Although Dr Al Muderis’ intra- and post-operative conduct was rather unsatisfactory on this topic, I am not persuaded that the failure to remove the drill bit per se, leads to the conclusion sought by the respondents that the surgery was negligent.
Post-operative care
1998 Ms Mooney suffered osteomyelitis in her tibia causing irreversible damage to her joint. The infection went undiagnosed and untreated for several months. In these circumstances, the respondents alleged Dr Al Muderis’ post-operative care was negligent.
1999 Dr Ruff’s evidence was that the likely cause of Ms Mooney’s osteomyelitis was “[d]eep infection complicating the second operation on 23rd February, 2011”. Dr Papadimitriou’s evidence was that the infection developed from at least the date of her second surgery. I accept their evidence. I do not accept the applicant’s submission that the respondents have not established Ms Mooney had a bone infection in March or April 2011.
2000 There is no dispute that when Dr Papadimitriou operated on Ms Mooney on 9 September 2011, she was suffering from chronic osteomyelitis. His evidence was that by this stage, there was no prospect of joint salvage. He said it was apparent during this procedure that:
It was a very extensive infection. It’s rare to see a septic arthritis that has reached that stage because normally we treat it so much earlier … it was unusual and it was quite striking in how severely damaged the knee was, but it did correlate what the CT scan had suggested. And it has also suggested chronicity. In other words, this was not something that happened in the last couple of weeks. It’s a months-long process that had evolved to allow sufficient bone destructions to have occurred to that extent. And that matched with the pathology which came back which suggested chronic osteomyelitis.
2001 Dr Ruff’s opinion accords with that evidence. The applicant did not advance any submission challenging Dr Papadimitriou’s evidence as to the state of Ms Mooney’s knee at the time he treated her.
2002 It is helpful to describe some key events prior to September 2011 before making further observations.
2003 On 16 March 2011, when Dr Al Muderis consulted with Ms Mooney, she told him that she was struggling with her range of movement, which he accepted. He advised her to increase her physiotherapy. Her evidence was that her leg was not going well when she was discharged from Lady Davidson Hospital on 25 March 2011, although I note that the applicant relies on the discharge summary to suggest otherwise. Ms Mooney’s evidence was that she raised concerns about her leg with Dr Ahmed on or about 12 April 2011, who subsequently conducted blood tests. That her doctor conducted tests and sought a second opinion shortly after her discharge, gives rise to the inference that Ms Mooney’s concerns existed, they had not been addressed, and she wanted the advice of someone other than Dr Al Muderis.
2004 On 19 April 2011, Ms Mooney saw Dr Watson for a second opinion. Dr Watson is a sports and exercise physician. He is the medical director of the Narrabeen Sports and Exercise Medicine Centre. He explained his practice mainly relates to musculoskeletal injuries, especially knees.
2005 Dr Watson explained Ms Mooney was referred to him because Dr Ahmed was concerned that she was not rehabilitating well following surgery, and that she may have an infection. That day, Dr Watson wrote to Dr Ahmed and Dr Al Muderis saying that he had provisionally diagnosed Ms Mooney with ongoing osteomyelitis of the tibia, citing, inter alia, Dr Ahmed’s “blood tests which showed a CRP of 68.9 consistent with ongoing infection possibly in the deeper tissues of the leg”. The letter also records that Ms Mooney had “noticed increased pain, increased swelling and some serous ooze from the puncture wounds in the lower leg over the last seven days”.
2006 Dr Al Muderis accepted that it had come to his attention that Ms Mooney was complaining of increased pain, swelling and ooze from the puncture wounds. During cross-examination, he gave evidence that Dr Watson is not a qualified infectious diseases consultant, and that raised C-reactive protein (CRP) can mean anything and does not necessarily indicate osteomyelitis. His evidence was that he told Dr Watson when Dr Watson had telephoned him, that osteomyelitis is not a term he would use or would be used lightly. He agreed that he said to Dr Watson that Ms Mooney needed urgent reassessment.
2007 On 21 April 2011, Dr Al Muderis consulted with Ms Mooney. He concluded that she did not have an infection. In cross-examination, he explained that he noticed Ms Mooney’s leg was swollen but that the oozing had stopped. He said that he was aware she was in pain.
2008 That day, Dr Al Muderis wrote to Dr Ahmed, copying Dr Watson:
I examined [Ms Mooney] today and she does not have any fever or pain. She does not have any discharge from her leg. She does have a significant problem with her leg though which is completely different to what she came to me with. She has significant stiffness in her knee and significant fixed flexion deformity which makes me feel very unhappy about the results of the rehabilitation that she has been undergoing so far. I repeated the X-Ray which showed no evidence of osteomyelitis, and the wound seems to have healed very nicely. She does have significant swelling in her leg which is expected to last for around a year due to the severity of her injury. Unfortunately, Mrs Mooney and her family are preoccupied with the fear of infection and that may have an adverse outcome of their motivation to get her range of movement back, which is the main aim. I have tried my best to reassure Mrs Mooney that she does not have infection because she’s neurologically intact and she doesn’t have diabetes so she does not have any evidence of neuropathy or any condition that might obliterate the pain sensation that you would get with infection. She feels well and she doesn’t have pain, as I mentioned before, so the likelihood of her having infection is extremely low. I again reassured Mrs Mooney and reinforced my initial drive for her to get her range of movement and walking back because she needs to start getting back to normal and the thoughts of infection may delay that significantly.
2009 His evidence was that he ordered an urgent full tibia MRI scan to determine if there was any evidence or collection of osteomyelitis to put her mind to rest.
2010 On 20 May 2011, Dr Watson saw Ms Mooney again. His report to Dr Ahmed of the consultation reflects his acceptance of Dr Al Muderis’ opinion. Dr Watson’s evidence was that he was surprised with the content of Dr Al Muderis’ report because he expected he would have identified infection, but he accepted it at face value. He explained he was happy at the time to rely on Dr Al Muderis’ interpretation of the x-ray and said he was reassured by the fact that, even though the x-ray was inconclusive in terms of showing obvious signs of osteomyelitis, the investigations could be repeated if Ms Mooney did not improve. He expected that Dr Al Muderis would be able to investigate and manage Ms Mooney’s symptoms appropriately.
2011 As discussed above, Ms Mooney fell at home and required surgery on her hip in July 2011. In hospital, both Dr Sew Hoy and Dr Hudson expressed concern about possible infection in her leg. A bone scan was undertaken on 17 August 2011, which recorded “possible infection in the left tibial shaft plus probable atrophic non-union of the tibia.” A gallium scan was performed on 19 August 2011, which recorded, “[v]iewed in conjunction with the recent bone scan, this scan suggests the presence of infection in the mid shaft of the left tibia.” A discharge referral report dated 19 August 2011 recorded “[o]steomyelitis left tibial shaft” as an active secondary diagnosis.
2012 On 29 August 2011, orthopaedic surgeons Dr Marel, Dr Dickison and Dr Roberts examined Ms Mooney. Dr Marel authored the consultation report, recording that “we all agree that it is more likely that infection is destroying this knee rather than reflex sympathetic dystrophy”. The report concludes, “[l]ong term this knee appears to be so destroyed that only knee replacement will be an option”. On 30 August 2011, Dr Marel received the results of an x-ray and CT scan he had ordered, which reported results “consistent with established osteomyelitis”.
2013 As described above, Ms Mooney came under Dr Papadimitriou’s care on 1 September 2011, his report recording that Ms Mooney appears to have “chronic osteomyelitis and septic arthritis”. Dr Al Muderis was copied into this correspondence.
2014 In that context, I make these further observations.
2015 First, Dr Ruff’s evidence was that a surgeon conducting a revision procedure in Ms Mooney’s circumstances should have taken swabs intraoperatively so that any infection could be identified. There is no evidence that Dr Al Muderis took a swab during the second procedure. Dr Ruff explained there is “a distinct probability [the infection] was there after the first operation, not identified at the second operation and the treatment that was instituted was late.” He explained that “if [a swab] had been taken and if it had identified an organism, such as the one that was causing the subsequent infection, you’re going to be miles ahead in treating it”, such that the situation could have likely been salvaged.
2016 Second, Dr Ruff did not agree that Dr Al Muderis was not being presented with any suspicion of infection on 21 April 2011. He opined that following the revision surgery, Dr Al Muderis “failed to correctly interpret symptoms and signs” of infection. He ultimately “failed to diagnose deep sepsis at the internal fixation site which subsequently allowed destruction of the knee joint requiring knee fusion”.
2017 Dr Ruff gave evidence that:
[Dr Watson] was very concerned. … [Ms Mooney] had a progressively swollen, red, painful leg and it just got worse … the natural history of injury is it gets better, not worse. … there’s red flags all the way along that something is going – two big operations. The one thing that should be going on in your mind is is this infected[?]
2018 Third, Dr Al Muderis in 2011 attributed several of Ms Mooney’s symptoms to reflex sympathetic dystrophy (also known as complex regional pain syndrome, or CRPS), and a tooth abscess.
2019 Dr Al Muderis had referred Ms Mooney to Mr Albert Coleiro, a physiotherapist. In a 1 June 2011 letter to Dr Al Muderis, he stated that he felt Ms Mooney was exhibiting signs of CRPS, and that could explain the stiffness, swelling and increased pain levels. The next day, Dr Al Muderis reported on a consultation he had with Ms Mooney, recording that she has “developed what looks like” CRPS. Dr Al Muderis in evidence said he did not make that diagnosis, and that it was made by her physiotherapist. The consultation report also stated that the “suspicion of osteomyelitis” by a rehabilitation doctor had been a setback, and that “we discovered the inflammation had been from her tooth which had an abscess” (Ms Mooney gave evidence that, on 12 May 2011, her dentist discovered an abscess in her back upper molar). It was written in a critical manner, further asserting the fear of osteomyelitis “did great damage by delaying physiotherapy until it was ruled out”.
2020 On Dr Al Muderis’ evidence, Ms Mooney mentioned the tooth abscess, and “that may have given the false finding of raised CRP.” However, he denied that his view was that the pain she was reporting, the swelling and the lack of mobility might not have been related to the surgery. Dr Ruff’s evidence was CRPS is “extraordinarily uncommon from [Ms Mooney’s] sort of injury”. He also rejected Dr Al Muderis’ opinion that the inflammation was coming from a tooth abscess. The prospect of infection, which Dr Ruff explained should have been front of mind, plainly was not.
2021 Fourth, Dr Ruff’s evidence is that Dr Al Muderis failed to carry out the appropriate diagnostic tests on 21 April 2011. He explained Dr Al Muderis was wrong to order an MRI, and that he ought to have undertaken a bone scan coupled with a gallium scan or obtained a deep swab. He explained: “I can’t imagine anyone ordering an investigation such as [an MRI] with an intramedullary nail to exclude an infection. … it has got serious limitations”. He highlighted comments from the radiologist’s 21 April 2011 letter to Dr Al Muderis, who introduced his findings on the MRI as follows:
There was substantial magnetic susceptibility artefact resulting from the intramedullary nail and the hardware from the lateral tibial plateau ORIF. This limited the diagnostic utility of the study. Within this constraint, no obvious phlegmon or collection or osteolytic process was demonstrated.
(emphasis added)
2022 It follows that Dr Al Muderis was on notice of the limitations of an MRI in Ms Mooney’s case. The evidence is that despite that Dr Al Muderis nevertheless rang Ms and Mr Mooney that evening to inform them that the MRI showed no infection. They accepted Dr Al Muderis’ advice.
2023 Fifth, and in that context, Dr Al Muderis displayed an aversion or reluctance to investigating infection. Ms and Mr Mooney’s evidence is that the MRI was done at their insistence. Mr Mooney describes the 21 April 2011 consultation with Dr Al Muderis in his affidavit:
On 21 April 2011, I accompanied Leah to a consultation with Dr Al Muderis. We talked about whether Leah had an infection and said that we were very concerned. Dr Al Muderis got cranky and rose his voice. He said “She in no way has an infection”. He asked “Leah are you in SEVERE pain?” Leah hesitated and said “no”. Dr Al Muderis said he could send her for an MRI, but it was not necessary. I insisted on an MRI and Dr Al Muderis provided a referral.
At this meeting, Dr Al Muderis referred to the fact that Dr Watson had raised that Leah might have an infection. Dr Al Muderis said about Dr Watson words to the effect “He’s only a sport medicine doctor, I am an orthopaedic surgeon. What would he know?”
(emphasis in original)
2024 The applicant denies describing Dr Watson in that way. That the applicant is alleged to have minimised Dr Watson’s expertise by comparison to his, has a ring of truth. I note that there is other evidence of statements to the same effect being made by Dr Al Muderis about other doctors: see [2311].
2025 I note also that in relation to the phone call with Dr Al Muderis in November 2011, referred to above, the note records that Ms and Mr Mooney insisted on an MRI. This is also consistent with the complaint to the HCCC, which recorded that they insisted on an MRI after Dr Al Muderis “said we could have an MRI to check if we insisted”.
2026 Mr Mooney also gave evidence about that consultation on 21 April 2011 in cross-examination:
I will never forget that day. It was monumental. He said … there was no sign of infection. There was no way that your leg was infected and we argued that, you know, … you know, Dr Watson’s words and … Dr Al Muderis got very heated and even – he said things like, “Leah” – yelling at her. “Do you say you have severe pain?” ... you’ve met Leah. She’s meek and mild and she just went, “No. No.” But she did. She was in terrible pain, you know.
2027 When challenged as to his recollection, Mr Mooney replied: “I am definite about my recollection of that. There’s nothing more frozen in my mind”.
2028 Mr Mooney took Ms Mooney for an MRI after the appointment. He said they were not given the MRI report until the 2013 proceedings.
2029 I note that Dr Watson gave evidence of his telephone call with Dr Al Muderis on about 19 April 2011 which included that:
… the tone of the conversation … was not friendly.… I got the impression … that I was almost insulting Dr Al Muderis by suggesting that [Ms Mooney had] an infection. … I felt that I was being talked down to. And I do admit to being a little bit intimidated by that.
2030 Dr Al Muderis recalled telling Dr Watson during that call that “osteomyelitis is not a term I would use lightly.” In his report to Dr Ahmed of the 21 April 2011 consultation, Dr Al Muderis wrote “even the suspicion of osteomyelitis which is a diagnosis that we don’t like to use in orthopaedic surgery [sic]”.
2031 Ms Mooney’s evidence conflicted with aspects of the consultation report of 21 April 2011, including as to her current condition. However, the consultation report does not sit with the basis of referral by Dr Ahmed to Dr Watson, which it will be recalled, is recorded by Dr Watson in his report of 19 April 2011 as Ms Mooney having over the last seven days experienced increased pain, increased swelling and some serous ooze from the puncture wounds in the lower legs. It was of concern to her to get a second opinion. Yet Dr Al Muderis records in his consultation report to Dr Ahmed two days later, inter alia, that she “feels well and she doesn’t have pain … so the likelihood of her having an infection is extremely low”.
2032 Sixth, there is a further issue as to whether Ms Mooney was experiencing a weeping sinus while under Dr Al Muderis’ care, such that he should have suspected infection. Dr Papadimitriou’s evidence was that, in Ms Mooney’s case, a draining sinus from a post-surgical wound demonstrates a 99% or 100% chance of infection. In that context the applicant submitted no draining sinus was present when Ms Mooney consulted Dr Al Muderis on 18 February, 16 March, 21 April, 2 June and 14 July 2011, as recorded in his consultation reports. Even accepting that was so on those occasions, Dr Papadimitriou’s evidence was that a sinus may drain “on and off”, with infection being present all the while. Dr Ruff also accepts that Ms Mooney could have had a draining sinus episodically. I accept that evidence.
2033 Dr Watson’s 19 April 2011 report, copied to Dr Al Muderis, records that Ms Mooney “noticed … some serous ooze from the puncture wounds in the lower leg over the last seven days …”. Dr Al Muderis accepted that, having received that report, it had come to his attention that she was complaining of serous ooze from the puncture wounds. His evidence was that “by [the] time” of the 21 April 2011 consultation, “the ooze … had stopped”. I note that Dr Al Muderis did not deny being told by Dr Ahmed on about 12 April 2011 that Ms Mooney was experiencing ooze from her wound.
2034 Dr Al Muderis’ failure to conduct proper investigations in April 2011 is therefore also in a context where he was aware Ms Mooney had reported recently experiencing serous ooze. That is so even if Ms Mooney exhibited no draining sinus at the time of the consultation with Dr Al Muderis, given that such drainage may occur on and off.
2035 I note that Ms Mooney’s 19 August 2011 discharge summary from Mona Vale Hospital records Ms Mooney experiencing a discharging sinus, and that Dr Papadimitriou gave evidence that when he first saw Ms Mooney in September 2011, Ms Mooney had a discharging sinus that had scabbed over. As he described, the scab was “crusted over” and explained it had to have been discharging recently “because they had done a swab in the last few weeks”.
2036 I am satisfied Dr Al Muderis failed to provide post-operative care to Ms Mooney in failing to diagnose and treat her osteomyelitis. So much is readily established given his failure to correctly interpret and investigate the symptoms and signs of infection on 21 April 2011 or subsequently where, as Dr Ruff explained, the possibility of infection should have been front of mind. I am fortified in that conclusion given that I accept: Dr Ruff’s evidence that a surgeon conducting a revision procedure in Ms Mooney’s circumstances should have taken swabs intraoperatively to identify any infection; Dr Ruff’s evidence that Dr Al Muderis failed to carry out the appropriate diagnostic tests on 21 April 2011; that Dr Al Muderis was on notice of the limitations of an MRI to exclude an infection in Ms Mooney’s circumstances on 21 April 2011; that Dr Al Muderis displayed an aversion to investigating infection; and, that Dr Al Muderis failed to carry out further investigations in April 2011 when he was aware Ms Mooney had reported recently experiencing serous ooze.
2037 I am satisfied in the circumstances that Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Jones v Dunkel
2038 The applicant complains about the respondents’ failure to call Dr Ahmed and Dr Hudson, such that a Jones v Dunkel inference should be drawn. I disagree. Dr Ahmed’s correspondence with others and her actions, speak volumes as to her concerns. Dr Hudson’s records also clearly set out his findings at various stages of his interactions with Ms Mooney. There is no necessity to call these persons as witnesses. In the circumstances, there is no proper basis to draw any adverse inference for failure to having done so.
2039 I note that the submission also fails to consider the basis of Dr Ruff’s evidence. That is, given what had occurred, and the condition in which Ms Mooney was presenting, the concern about infection should have been at the forefront of Dr Al Muderis’ mind. It also ignores the evidence that the applicant failed to undertake the correct test, evidence which I accept. If a test is to be done, it should be the correct one.
Mrs Kim Gollan
2040 Mrs Kim Gollan passed away on 10 June 2022 when she was 58 years old. Her daughter Ms Temperance Gollan gave evidence.
2041 Mrs Gollan was admitted to Macquarie University Hospital where she underwent a bilateral total knee replacement with Dr Al Muderis on 10 August 2016. He had been consulting with her since about July 2015.
2042 Ms Gollan gave evidence of the difficulties she observed her mother experiencing after the operation. On 19 December 2016, Dr Al Muderis performed remedial surgery to fix a fracture of her left leg, inserting an intramedullary nail. On 4 April 2017, Mrs Gollan was readmitted to Norwest Private Hospital suffering from an infection in her tibia. Dr Al Muderis performed surgery on 7 April 2017, removing the nail and putting an antibiotic rod into the bone. Mrs Gollan was subsequently diagnosed with left leg osteomyelitis associated with the intermedullary nail Dr Al Muderis inserted on 19 December 2016. Mrs Gollan underwent further surgeries in 2017, and continued antibiotics treatment until December 2018. Mrs Gollan’s physical and mental condition continued to deteriorate.
2043 Mrs Gollan sued Dr Al Muderis for medical negligence. The proceeding was settled in 2020 on confidential terms (and without an admission of liability) with Dr Al Muderis (by his insurer) and a radiologist, agreeing to pay Mrs Gollan $1.2 million. Two statements made by Mrs Gollan for the purposes of those proceedings (dated 12 July 2018 and 9 February 2020), were before this Court and admitted pursuant to s 63 of the Evidence Act. The applicant submitted that as she was not available to be cross-examined, her evidence should be approached with considerable caution as it has not been tested: Herron at [522]. The applicant also submitted that aspects of Mrs Gollan’s second statement were “concocted” and “deliberately dishonest” to bolster her negligence claim. I do not accept that submission. In relation to Ms Gollan, the applicant submitted that to the extent her evidence is contradicted by medical records, her mother’s evidence, or that of Dr Al Muderis, it should not be accepted. As a general proposition, I do not accept the applicant’s submission. I address the issue where relevant below. I note that Dr Al Muderis does not have a specific recollection about many matters relevant to Mrs Gollan’s case.
2044 An issue arises as to the placement of the navigation pins during Mrs Gollan’s knee replacement surgery on 10 August 2016. The applicant submitted that this was not pleaded in the Amended Defence. So much may be accepted. It was, however, addressed in the expert report of Dr Ruff dated 28 June 2023, which was served on the applicant prior to the hearing. As such, the applicant was on notice of the evidence and, in any event, granted leave to call evidence in reply, being Dr Qurashi. No prejudice has been identified. I have addressed the applicant’s pleading submissions more generally above, and it is not necessary to repeat here. It is plain from the evidence in Dr Ruff’s report, that this evidence is relevant as it informs the assessment of Mrs Gollan’s aftercare, and the allegation that Dr Al Muderis failed to diagnose and treat her fractures, matters which were pleaded.
2045 In his report, Dr Ruff opined:
… in the process of placing navigation pins to hold the tibial trackers on the left tibia below the left … surgical site the distal of the two tracking pins was transcortical instead of bicortical, thus passing across one cortex rather than through it.
2046 He opined that this weakened the bone and allowed a fracture. Dr Ruff’s view is that fracture in the tibia is a recognised complication of using navigation pins for total knee replacements, and the risk of fracture is enhanced by inappropriate transcortical placement of the pin. He gave evidence that if a patient has:
… a painful tibia after a total knee replacement, [the] first thing we ask is have they had navigation pins put in. If they have, they’ve got a fracture. If there was ever going to be a fracture, this was one that was going to fracture. She repeatedly came back saying she was tender and sore there, and they didn’t seem to even think that there was a fracture.
2047 That is, where a pin is identified as transcortical (instead of bicortical), a doctor should be on the lookout for pain or tenderness at the pin site, because of the weakened bone. In his report, Dr Qurashi opined that there “is some weak evidence that the risk of fracture is higher through a transcortical pin placement compared with the other two positions” (being bicortical and unicortical). Dr Qurashi was cross-examined about the literature he refers to in his report, and he accepted that it supports the proposition that transcortical pin placement is associated with complications such as fractures. He accepted transcortical pin placement is undesirable. If there is any difference, I prefer the evidence of Dr Ruff. This is relevant to the issue of whether Dr Al Muderis should have investigated the possibility of a fracture earlier than December 2016. Dr Ruff’s opinion was that the circumstances were such that he should have done so. He opined that Dr Al Muderis should have arranged a CT scan for Mrs Gollan “the first day she turned up” complaining of tenderness and soreness around the left pin site.
2048 On 22 September 2016, Dr Orville Samuels, one of Dr Al Muderis’ fellows, saw Mrs Gollan on his behalf for her six-week post-operative appointment. Dr Samuels records in his consultation letter that:
… [s]he had a small area of tenderness to her left pin sites but no current discharge and for precaution I have put her [on] one week of flucloxacillin just to make sure no skin infection develops in that area.
2049 Mrs Gollan’s statement said she told Dr Samuels that she was “struggling to walk and move due to [the] pain” and that she had a lot of pain in her left leg at the top of her shin and could not put weight on her left leg. Dr Tetsworth accepted that if a patient is complaining of a small area of tenderness to her left pin sites, that is a matter which requires further investigation, and it is not possible to fully assess matters such as implant alignment on short radiographs such as x-rays. He accepted that a plain x-ray had not been done on Mrs Gollan. Dr Ruff’s opinion was that a CT scan should have been performed that day. The applicant submitted that Dr Al Muderis was not present during the consultation implying, given the context of the submission, that he did not know of the left pin site pain, which impacts on the issue of whether he should have investigated. However, as the respondents submitted, the consultation report is signed “for and on behalf of” Dr Al Muderis. As Dr Samuels was attending to Mrs Gollan on Dr Al Muderis’ behalf, one would expect Dr Al Muderis to have had the information available to him to act accordingly. None of those investigations occurred.
2050 On 11 October 2016, Mrs Gollan felt an odd snapping sensation in the lower part of her left leg while moving a bin onto the porch at her daughter’s home. Following continuing deterioration and pain, on 15 October 2016, Mrs Gollan was admitted to the emergency department at Norwest Private Hospital. Mrs Gollan’s statements say that she was standing at the kitchen sink of her home and found herself unable to move. An ambulance was called. Ms Gollan gave evidence that her mother was complaining at that time of pain so bad in her leg that she thought she had broken it. Mrs Gollan’s statements are consistent with that. She said that is what she told the ambulance officers transporting her to hospital. Mrs Gollan was then admitted to the orthopaedic ward at Norwest Private Hospital, where she remained until 25 October 2016. Ms Gollan’s evidence was that Dr Al Muderis diagnosed her mother with a left leg deep vein thrombosis (DVT) and prescribed her with warfarin. Mrs Gollan said in her statement that when Dr Al Muderis visited her at the hospital, he said words to the effect of: “I am unsure as to why you are in so much pain”. Mrs Gollan said that a few days later, Dr Al Muderis told her she needed to be walking. In cross-examination Dr Al Muderis said he did not recall saying that, and the treatment for DVT is elevation, rest and ice. He said that he was consulted about Mrs Gollan and visited her when she was an inpatient for DVT. Dr Al Muderis accepted that Mrs Gollan was noted to have increased left leg pain which was DVT, as well as decreased mobility. Ms Gollan accepted in cross-examination that her mother did physiotherapy during her admission (consistent with her being told to walk by Dr Al Muderis), but said that her mother’s mobility did not improve, and she was crying from the pain.
2051 X-rays were taken of Mrs Gollan’s leg on 13 October 2016 (before she was admitted to hospital). The x-rays appear to have been ordered by Mrs Gollan’s GP, as a result of her consulting him after 11 October 2016 because of her condition at the time (as described above). When shown to Dr Al Muderis in cross-examination, he said he had not seen the x-rays before this trial and could not see a fracture. He repeated that evidence in re-examination. Dr Ruff gave evidence that he could see a fracture in the x-rays, albeit accepting he knew there was one there because he had read Mrs Gollan’s file. That said, conscious of having that knowledge, as the respondents submitted, Dr Ruff asked other medical practitioners if they could see anything on the x-rays. Dr Ruff gave evidence they saw the fracture too (evidence adduced without objection). During cross-examination Dr Ruff identified the fracture on the x-ray. I accept Dr Ruff’s evidence that he could see a fracture in the October 2016 x-ray. Where there is a conflict between his evidence and Dr Al Muderis’, I prefer the evidence of Dr Ruff.
2052 I note that the applicant relied on a radiologist report relating to the x-rays dated 13 October 2016 that did not identify a fracture. The applicant criticised Dr Ruff for giving evidence that he characterises as critical of radiologists. However, all that Dr Ruff explained when giving evidence was that radiologists are only as good as the information they are given, and here the report does not reflect that the radiologist had all of the relevant information (being that Mrs Gollan had “[n]avigated knee replacement, inferior pin inappropriately cutting the cortex, pain at that sight, feels that she has got a fracture”). When it was put to him that other doctors were also attending to Mrs Gollan during her October hospital stay, Dr Ruff answered:
… she’s in hospital for some days complaining of leg pain, with a drill hole cutting the tibia in two almost, complaining of leg pain. It needs to be looked at properly. If you can’t look at the X-ray and see the fracture, you get a CAT scan or a bone scan. And it should have been done. That standard of care, it is standard of care. It doesn’t matter who else is seeing her, the only person that’s supposed to diagnose this is Dr Al Muderis.
2053 As Dr Ruff explained, Dr Al Muderis should have been “vigilant that something is going to happen”. Dr Ruff said he assumed that Dr Al Muderis had seen the x-ray, but irrespective of this, he should have been aware of it and should have investigated.
2054 I find it surprising that Dr Al Muderis would not have seen the x-rays of October 2016 at the time (even if Dr Al Muderis himself did not order them), given he was her surgeon. That said, given the circumstances, I am satisfied in any case that Dr Al Muderis should have investigated Mrs Gollan’s symptoms further which would have revealed the fracture. I do not accept Dr Al Muderis’ evidence that there is no fracture shown on the x-rays.
2055 I note also that although the consultation report of 22 September 2016 records tenderness at the left pin sites, this does not appear to have been considered by Dr Al Muderis during Mrs Gollan’s hospital admission in October 2016.
2056 Ms Gollan’s evidence was that after her mother was discharged from hospital in October 2016, her mother was not able to work or properly weight bear. She witnessed her mother “shuffling on her bottom around the house to avoid the pain of walking” and “her legs were still swollen and a deep purple-red colour and would sometimes leak and ooze from the swelling”. Mrs Gollan had a bump on her skin and her legs were swollen and disfigured. Ms Gollan went with her mother to a GP appointment at the Hills Family Practice on 14 December 2016. Her mother was advised to attend hospital that day. Mrs Gollan’s doctor, Dr Yu, wrote to Dr Al Muderis that day, detailing her condition (she was at risk of osteomyelitis and infection, struggling with DVT and unable to independently mobilise with pain, swelling and weakness).
2057 Mrs Gollan was admitted to hospital that day under the care of Dr Al Muderis. He arranged for x-rays to be taken. The x-ray showed that Mrs Gollan had a fracture in her left lower leg. On or about 19 December 2016, Mrs Gollan underwent open reduction and internal fixation surgery. Ms Gollan gave evidence that prior to the operation, Dr Al Muderis made jokes about her mother’s condition, saying to her mother words to the effect of: “You’re lucky you’re getting two operations for the price of one!”. Ms Gollan said she visited her mother in hospital after the operation. She described one occasion where Dr Al Muderis came into the room crying, saying words to the effect of: “This is all my fault, the break happened during the initial surgery. It was a hairline fracture that no one had caught”. It was put to Ms Gollan that Dr Al Muderis said that the break was not caught while her mother was in hospital in October (not that the break was not caught in the initial surgery), which she denied.
2058 Dr Ruff opined that the December 2016 x-ray showed a fracture that was both deformed and healing, meaning it had been there for weeks.
2059 On 15 December 2016, Dr Al Muderis admitted in correspondence to Mrs Gollan’s GP that:
We were startled that Kim had a fracture that was missed from her last admission five weeks ago and it is likely that the fracture occurred several weeks ago while she was admitted to Norwest Private Hospital by ambulance because she was having pain in the leg. When I saw her there the leg was straight and she had a haematoma which we were under the impression was due to the anticoagulation for the treatment of the DVT she developed. Obviously there was misleading diagnosis that complicated the final diagnosis which is very clear now to me.
…
It is very unfortunate that this happened to her and I sincerely apologised to Kim about missing this fracture.
2060 The applicant attempted in cross-examination to minimise the effect of this letter, saying that it was “speculation” as to what had happened. That report also stated that Mrs Gollan had been “unfortunately continuing physiotherapy and trialling to walk”.
2061 I accept that investigations should have been undertaken prior to December 2016, given the circumstances of the navigation pins, and the complaints of pain and tenderness at the pin sites by Mrs Gollan six weeks post-operation. Mrs Gollan had been experiencing pain and had difficulty walking immediately following her surgery and thereafter. The transcortical placement of the pins being associated with a fracture of the tibia is a recognised complication, which as Dr Ruff said, a surgeon should be alert to. Dr Al Muderis attempted to justify his failure to detect the fracture. There were red flags that called for investigation. He failed to do so. As her surgeon, he was the person responsible. The respondents submitted that had Mrs Gollan’s fracture been detected in October 2016, the December 2016 surgery would not have been necessary. If the fracture had been detected earlier, as it should have been, there is little doubt that Mrs Gollan would have been treated differently, with non-weight bearing crutches or a frame. It is to be recalled that Mrs Gollan’s evidence is that in October 2016 Dr Al Muderis told her to walk. I accept the respondents’ submission.
2062 It is unnecessary to detail what occurred after this incident.
2063 I am satisfied that in relation to Mrs Gollan’s aftercare, Dr Al Muderis failed to conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Ms Mary Heffernan
2064 On 23 October 2020, Ms Heffernan underwent a total left knee replacement, performed by Dr Al Muderis. She was 76 years old at the time of the surgery.
2065 The applicant submitted that although Ms Heffernan was not dishonest, she was a poor historian and her recollection is unreliable. The respondents submitted she was an accurate historian. I accept Ms Heffernan was an honest, credible and generally reliable witness.
2066 I note at the outset that on 28 July 2021, Ms Heffernan met with another orthopaedic surgeon to obtain a second opinion because of the pain she was still suffering, which led to revision surgery. Further, Ms Heffernan submitted a complaint about Dr Al Muderis to the NSW HCCC on 13 January 2022, which was well before the Publications, and proximate to the events.
2067 There are three topics to address: aftercare; the Zimmer Biomet ROSA Knee System (or otherwise known as, Robotic Stereotactic Assistance or ROSA) data; and risks and complications.
Aftercare
2068 I accept Ms Heffernan’s evidence that when she attended her post-operative follow-up consultations with Dr Al Muderis, she told him she was in significant pain and her knee was red, clicking and swollen. It affected her walking.
2069 Although Ms Heffernan’s evidence is consistent with several contemporaneous records, it is important to recall that the significance of Ms Heffernan’s evidence is that it is directed at what she told Dr Al Muderis as to the symptoms she said she was suffering from at the time (and that she was suffering those symptoms).
2070 For example, on 1 December 2020, a physiotherapist at Hunters Hill Private Hospital wrote a letter to Dr Al Muderis describing Ms Heffernan’s main issue as “quite sharp pain”, and that occasionally she experienced a “loud clicking” in her knee which (as Dr Al Muderis deciphered for counsel in cross-examination) prevented her from walking with her legs as well as the physiotherapist would like.
2071 As a result of the letter, on 3 December 2020, Dr Al Muderis saw Ms Heffernan and wrote in his consultation report that:
Mary is doing very well with her knee seven weeks down the track post left knee replacement. She feels very bad. She feels that it is clicking and she feels very straight, as she was very valgus, and now it is all stretched out. The first few weeks were horrible for her but now it seems she is improving and has turned a corner.
At that time, the report said he would see her again in six weeks. The applicant submitted that Ms Heffernan agreed with the substance of the report in cross-examination and therefore I should accept it as accurate. He submitted that it was inconsistent with Ms Heffernan’s affidavit evidence. However, that submission, as in other instances, was directed to what Dr Al Muderis did and said as recorded in the report, not on what Ms Heffernan described her condition was at the time. Contrary to the applicant’s submission, the consultation report is not inconsistent with Ms Heffernan’s evidence.
2072 The applicant relied on a physiotherapy discharge summary report dated 8 December 2020, which states, inter alia, that Ms Heffernan “walks well, depending on pain”. Although it records Ms Heffernan as having “nil” mobility aids, it also records, that she required a walking stick “as needed” (the meaning of the remainder of the entry is unclear). Ms Heffernan recalled doing a 10-minute walk test at rehab, but although she could not recall she said she was sure she completed it with her walking stick (not without any aids). It also records that Ms Heffernan “continues to experience intermittent sharp pain” and will “continue here doing hydro only as this is better tolerated and beneficial for her”. Ms Heffernan’s evidence was that she used her walking stick all the time. However, a consultation report dated 17 December 2020, dictated by Dr Ali Moaaz (on behalf of Dr Al Muderis) records:
[During the last consultation] Mary was extremely teary and in a lot of pain from the left knee. She felt there was some clicking on the anterior aspect of the knee, which was causing her a lot of grief.
On today’s examination Mary reiterates that the symptoms have persisted and have actually become worse over the last two weeks with a very palpable and audible click on the anterior part of the knee just medial to the incision and also pain at the back of the knee.
It is difficult to reconcile that description of Ms Heffernan as she appeared at the last consultation, with what is recorded in the consultation report for her consultation with Dr Al Muderis on 3 December 2020.
2073 According to Ms Heffernan, the pain and inflammation was so severe that on 19 December 2020 she presented at the emergency department at Ryde Hospital, before being transferred to Macquarie University Hospital the following day. She described her symptoms as including, inter alia, a swollen knee, extensive pain such that it was difficult to walk, hearing clicking noises when she walked, and the feeling that her knee was slipping. On Ms Heffernan’s evidence, she had repeatedly complained to Dr Al Muderis (until she obtained a second opinion in July 2021) that there was something wrong with her knee. She told him she felt her knee slipping. The repeated response from Dr Al Muderis was that there was nothing wrong with her knee, everything was fine, and it just took time to heal. That evidence that Dr Al Muderis repeatedly told her everything was fine is reflected in the consultation reports which state, among other things, “I reassured her that everything is going the right way”, “the wound has healed very nicely”, “[she] is doing very well”, “x-rays are fine with stable position”, “we are pleased with her progress and continued improvement”. Those statements are from reports where Ms Heffernan is suffering significant pain (e.g. the report of 3 December 2020, which we know from the passage recited above that she was in a lot of pain, and the report of 17 December 2020 where she reported the pain had become worse).
2074 A CT scan which was performed on 21 December 2020 identified a small bone fragment at the medial aspect of the knee. The scan report concluded that “further assessment with ultrasound maybe helpful”. Dr Al Muderis deposed that it was outside the knee joint and so unlikely to explain her pain and did not justify surgical exploration of the knee.
2075 On 7 January 2021, Ms Heffernan had a further consultation with Dr Al Muderis, during which he aspirated her knee to exclude infection, with the aspirated fluid containing blood in it. The consultation report records that Ms Heffernan complained that the pain had worsened, it was global in the left knee, and it was present during weight-bearing as well as with range of motion. It records she said that “she feels that it is a stabbing pain and partly burning as well, deep seated in the knee”. The report records that there is “no significant demonstrable collateral instability”, and that there does not seem to be a mechanical cause that would explain her pain. I return to this consultation below.
2076 Pausing there. Dr Ruff’s evidence was that Ms Heffernan’s knee should not have been aspirated in Dr Al Muderis’ rooms. He said that doing so is not the standard of care, “not satisfactory for an arthroplasty” and should have been done in a sterile environment, such as a hospital operating theatre.
2077 Ms Heffernan did not accept the propositions that she told Dr Al Muderis on 28 January 2021 or 25 March 2021 that her pain was subsiding and continued to decrease, noting that is recorded in both of those consultation reports. As to the earlier of those two consultations, this seems very unlikely where just two weeks prior on 7 January 2021, Ms Heffernan had complained of worsening pain in her left knee which led to the aspiration. Although (as recorded in the consultation report of 28 January 2021) no infection was found in the aspirated fluid, no further tests were undertaken in respect to the cause of the symptoms she had complained of. Further, although Ms Heffernan was not to see Dr Al Muderis for another three months after 28 January 2021, she made an appointment for 25 March 2021 because her knee was still painful with a grating sensation. Her evidence was that he told her there was nothing wrong with her knee and that it takes time to heal. He recorded in the consultation report of 25 March 2021 that Ms Heffernan felt her knee was now stable, and that she reported “a clicking sensation and she feels uncomfortable”. However, Ms Heffernan said that when she told Dr Al Muderis something was grating on the underside of her left kneecap, he said that it was nerve pain and referred her to the pain clinic for pain management. She said that she explained to him that she knew her “own body and [she] had that feeling that something was amiss”. None of this appears in the consultation report of 25 March, including the referral to the pain clinic. The applicant does not refer to the referral in evidence, and it is unclear whether the fact of it is in issue. In any event, I accept that there was referral. Ms Heffernan provided detailed evidence of what occurred which, in the circumstances is entirely plausible (bearing in mind that she made an appointment to see Dr Al Muderis at this time because of her pain). On Ms Heffernan’s evidence, she attended the pain clinic and was prescribed lignocaine pain patches, however the medication had adverse side effects on her, was only a temporary fix, and the pain came back very quickly. The referral, and this evidence of what occurred at the clinic is logical and plausible. Again, the circumstances of this consultation and the referral to the pain clinic makes it unlikely that she told Dr Al Muderis that her pain had “continued to subside” and that “she feels minimal pain, tenderness or soreness” (as recorded in the consultation report). The consultation in March 2021 was her last with Dr Al Muderis. Thereafter, she sought a second opinion from Dr Lyons.
2078 Dr Al Muderis accepted that the number of follow-up appointments with Ms Heffernan (which was more than what was his usual practice after such a surgery around this time) reflected that she had concerns. He also accepted that he had concerns, giving evidence that the successive appointments reflect he was taking care of her. The applicant submitted that such a sequence of events evidences he had not failed in his post-operative care of her. However, the mere fact of seeing a patient does not necessarily equate with providing appropriate care for that patient. As Dr Ruff opined, certain steps in treating Ms Heffernan should have been taken by Dr Al Muderis, which were not. I return to this below.
2079 Ms Heffernan’s evidence, which I accept, was that she was still in pain and she had told Dr Al Muderis that.
2080 Although the precise time Ms Heffernan first contacted Dr Lyons is unclear, after initially liaising with Dr Lyons’ rooms, she waited to see him (on their advice), undertaking physiotherapy in the meantime, until her first appointment on 28 July 2021. Her evidence was that she was still in pain at this time. It can be inferred that she sought a second opinion because she was dissatisfied with her care by Dr Al Muderis. Indeed, if her knee was as Dr Al Muderis described in the March consultation (as opposed to what Ms Heffernan described as to her condition), it is difficult to understand the need for any second opinion. Everything was, on Dr Al Muderis’ account, going well.
2081 Dr Lyons’ evidence of what he was told by Ms Heffernan of her condition during their consultation on 28 July 2021, and the purpose of seeking a second opinion, is consistent with the evidence she has given to this Court. Given she told Dr Lyons of, inter alia, the pain and the sensation of her knee giving way (slipping), I find it difficult to accept that she never informed Dr Al Muderis of that, as he contended.
2082 Dr Lyons gave evidence that upon examination of Ms Heffernan’s knee, he formed the view that the knee was unstable but exclusion of other potential causes for an “unhappy knee replacement” was required. He referred her for several tests and Ms Heffernan returned for a further consultation on 10 August 2021.
2083 On 11 November 2021, Dr Lyons performed exploratory and revision surgery, during which he removed and replaced Ms Heffernan’s prosthesis. Dr Lyons explained he did that because during the surgery it was apparent the knee joint was unstable in the sagittal, axial and coronal planes due to implant orientation. The global imbalance could not be addressed by an exchange of polyethylene and a revision of all components was required to achieve appropriate knee stability. That her knee was unstable in all three planes is reflected in his correspondence with Ms Heffernan’s GP. Ms Heffernan said that after her operation, Dr Lyons told her that the prosthesis was loose. I accept Dr Lyons’ evidence of what he observed during the surgery.
2084 The applicant put to Dr Lyons that Ms Heffernan’s symptoms were not consistent with what he said he found, being instability in all three planes. His response was that “they absolutely do, and they are the cardinal features of instability in a total knee replacement”. Dr Lyons said that Ms Heffernan’s knee was globally unstable, which accorded with the symptoms she had described to him, including pain, swelling, and inability to rise from a chair and descend stairs. He described that:
They are signs and symptoms of instability, and that would be reflected mostly as soon as the knee starts to – to flex and underload. In extension, she was able to stand, so she would mobilise but any kind of knee flexion under load, then she would become unstable.
2085 Dr Ruff’s evidence was to the same effect. Dr Ruff opined that Ms Heffernan’s instability was not going to stop her from walking around, but it was going to make life difficult for her when getting out of chairs and the like. As he said, that was where she felt the instability.
2086 Dr Al Muderis’ evidence was that the implant could not have been found to be loose during the revision surgery, stating that:
If the implant was as loose as it is alleged to have been, this would have shown up on the x-rays, CT scans and bone scans ordered by both myself and by Dr Lyons, but it did not.
2087 Dr Lyons disagreed with that, explaining why that is so. The effect of Dr Lyons’ evidence is that while his pre-operative investigations excluded causes such as infection, fracture, and insufficiency of osteolysis, his “working diagnosis” was always that the knee was unstable, hence the need for exploratory surgery.
2088 Dr Ruff’s evidence is that Dr Al Muderis “failed to diagnose instability which he either knew to be present or should have considered from the symptoms and signs on physical examination”. His evidence is that Dr Al Muderis should have examined the knee and detected instability under anaesthetic. Dr Ruff also said that undertaking the aspiration during the 7 January 2021 consultation and identifying blood in it should have raised suspicions that the knee was unstable (even though he accepted that blood in the aspirate could be due to a burst blood vessel). He said a doctor does not have to undertake the aspiration “three or four times and get blood in it to say it is unstable”. Rather, he said that having found blood in the aspirated fluid, and noting Ms Heffernan’s complaints, the next step was to examine the knee properly under anaesthetic; and if it was found to be unstable, to “act on it immediately”.
2089 The applicant submitted that he could not have factored a sensation of slipping in his clinical decision-making, because Ms Heffernan’s evidence was that she did not report it at the time following her surgery. Ms Heffernan described that sometime between 24 and 28 October 2020, during her admission in hospital, she got up with the assistance of a high walker to attempt to walk for the first time following the operation. She said that when doing so, she felt her left knee slipped sideways and did not feel stable. She gave evidence that she thought it did not feel right but that she told herself not to worry and did not report it to the medical staff on that occasion as she did not know what a total knee replacement surgery should feel like. However, Ms Heffernan also gave evidence that she told Dr Al Muderis at some stage before her admission into hospital in December 2020 (presumably during the second post-operative consultation), that there was a clicking noise, it felt like her knee was slipping, and she was in a lot of pain. Dr Al Muderis did not recall her saying that her knee slipped when she walked, said he did not understand what the word “slip” means, but then suggested that was not a term a patient would use, because the knee does not slip (it is to be recalled, as earlier described in Part 5, Section 5, there are other examples of Dr Al Muderis denying knowing the meaning of a word in cross-examination). I accept she told him about the slipping. Given she told Dr Lyons about her sensation of instability, there is no reason for her not to tell Dr Al Muderis in circumstances where she gave evidence of having that sensation. It was a concern which, among other things, led to her getting a second opinion.
2090 I accept that Dr Al Muderis was on notice that her complaints included that she felt her knee was slipping. In any event, Dr Ruff opined as follows in response to a question in cross-examination:
Ms Chrysanthou: I want to suggest to you that there was no – assuming she didn’t tell anyone about that first instance of her feeling in the hospital when she stood up for a moment, other than that, I want to suggest to you that there were no signs or symptoms that were presented to Dr Al Muderis over the period of time that he was assessing her postoperatively which made it – or, should have made it obvious to him that she had a diagnosis of instability?
Dr Ruff: No, I don’t agree with that. Most of his correspondences suggest that he’s looking for it. I don’t deny that he’s looking for it. He’s looking –at one stage he aspirated it to see if it was infected and there was blood in the aspirate; that’s a feature of an unstable knee as well. [Hemarthrosis] or blood-stained effusion or recurrent infusions. I think that he was thinking that there was instability and he wasn’t able to prove it for his own … I know that it frequently said “stable in extension”. Well, we know it’s stable in extension. We know it’s stable in extension from the ROSA data. And the symptoms of instability are really when the knee is bent. And he repeatedly looked for it, so he was actually thinking of it.
2091 It was suggested to Dr Ruff that it was not unreasonable for Dr Al Muderis to continue with his conservative advice, noting it was less than six months after surgery. He disagreed. I accept Dr Ruff’s evidence that there were steps that Dr Al Muderis ought to have taken to investigate, which he did not do (or did not recognise the significance of the result or information before him, e.g. blood in the aspiration being a feature of instability). Dr Ruff opined that her knee was “not right”, and Dr Al Muderis should have looked at it straight away. I accept that evidence. As the respondents submitted, if that had occurred, the problem of the knee’s instability would have been found and addressed.
2092 I note that the applicant asked a general question as to whether instability could have occurred after the surgery, to which Dr Ruff said that was highly unlikely, and very uncommon. That evidence is not to be considered in isolation, but with other evidence (including Ms Heffernan’s evidence as to the feeling of slipping at the outset, and the symptoms she suffered thereafter as discussed above).
ROSA data
2093 Dr Al Muderis used a ROSA system during Ms Heffernan’s surgery to facilitate navigation, realignment and implantation of a Zimmer Biomet Persona Total Knee. The system allows for real-time tracking. Significant time during the hearing was taken with evidence in relation to a spreadsheet recording data obtained by the ROSA system of Ms Heffernan’s knee during her initial surgery (Spreadsheet). However, this data was not obtained until after Dr Lyons’ and Dr Ruff’s evidence as to their opinions had first been provided. A supplementary affidavit and report by Dr Lyons and Dr Ruff, respectively, were read/tendered thereafter. The data did not alter the opinions that Dr Lyons and Dr Ruff had previously expressed, it was relied on as being consistent with those opinions.
2094 The evidence of the state of Ms Heffernan’s knee, and the opinions referred to thus far in this judgment are not based on the ROSA data. I prefer the evidence of Dr Lyons and Dr Ruff to that of Dr Al Muderis and Dr Stoita (who was relied on by the applicant as an expert in his case in chief).
2095 There was much dispute as to whether the data recorded the end point, or final knee state, that is, the final position of Ms Heffernan’s knee at the conclusion of the initial surgery. It is common ground between the parties that if the data in the Spreadsheet recorded the final knee state and is accurate, then it records gross instability in Ms Heffernan’s knee. It would then follow, in that scenario, that the data supports what Dr Lyons said he observed. Dr Ruff accepted that the data is possibly not the final data, although he suspected it was. It would be expected that a competent surgeon would record the final knee state, and if the data does not include that, it raises the issue of why it was not recorded. On Dr Al Muderis’ case, he failed to do so for Ms Heffernan. Therefore, if the final knee state is not recorded in this data, it does not assist the applicant. Dr Ruff opined that either way, whether it recorded the final knee state or not, Ms Heffernan had an unstable knee afterwards and it needed to be revised. Dr Stoita conceded in cross-examination that it is important to record the test that was used to assess whether the knee was stable in flexion before concluding the surgery – so that adjustments can be made before the final implantation, and so that it can be demonstrated later that the implant was installed correctly. He also acknowledged that this was not done in Ms Heffernan’s case, even on Dr Al Muderis’ evidence.
2096 Dr Richard Verheul, who is an orthopaedic surgeon, gave evidence in reply, directed to the conclusions in the supplementary reports of Dr Lyons and Dr Ruff concerning the ROSA data. (The evidence in reply was confined to those topics because the other opinions sought to be led related to material on which the applicant was on notice, and Dr Stoita which were (or could have been) addressed by Dr Stoita in his report of 5 August 2023, the expert witness relied on in chief. Given the orders made for the conduct of this hearing, it was not evidence in reply).
2097 However, the evidence having been admitted, it appears from the evidence of Mr Ben Edwards, Managing Director of One Surgical (an exclusive sale agent for Zimmer Biomet, which developed the robotic surgical assistant), also called by the applicant in reply, that the Spreadsheet is not a diagnostic tool and may not have recorded accurate data, given the version of the system used in the surgery. That being so, it also follows that there is nothing in the data that is inconsistent with the observations Dr Lyons made intraoperatively.
2098 Given that, and the possible limitation of the data, I put the ROSA data aside. At its highest, it is consistent with the evidence of Dr Lyons (including as to his observations during the revision surgery) and Dr Ruff. At the very least, it is not inconsistent with their opinions. I have decided the issues based on the remaining evidence.
2099 The applicant submitted that Dr Lyons was a poor witness, and his evidence was unreliable. He submitted he was dishonest in giving evidence, a proposition put to him in cross-examination. The applicant’s submission was based entirely on Dr Lyons’ evidence as to his experience with and interpretation of the ROSA data, describing it as the “centrepiece” of his evidence and alleging that his evidence was designed to mislead the Court. I do not accept that submission. I accept Dr Lyons’ evidence as to his consultations with Ms Heffernan, the investigations he conducted and his observations during the surgery. The ROSA data was not the centrepiece of his evidence. Dr Lyons operated on Ms Heffernan and observed the state of her knee. He was the doctor who observed the knee in the revision surgery. He is plainly well qualified, and experienced.
2100 In addition, I note that Dr Ruff opined in his report that concluding the operation without detecting instability fell below the reasonably acceptable standard (again an opinion expressed by him without consideration of the ROSA Data). As noted above, Ms Heffernen’s evidence (which I accept) is that she felt her knee slipping from the outset post-operatively. I accept Dr Ruff’s evidence.
2101 I am satisfied that Dr Al Muderis failed to diagnose the instability in her knee and failed to provide adequate post-operative care. His conduct did not have the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Risks and complications
2102 The respondents submitted that the risks and complications associated with a total knee replacement were not adequately explained to Ms Heffernan. Ms Heffernan’s evidence was that when she attended her initial consultation with Dr Al Muderis on 13 August 2020, she was given the impression that the fix for her knee would be relatively easy, with Dr Al Muderis saying words to the effect of: “Oh, I can fix that!”. Although Dr Al Muderis denied using that phrase, he accepted in cross-examination that he may have said he could fix the problem. She described it as a very quick consultation, only 15 or 20 minutes, following which she was whisked down to the nurse and filled out the pre-admission and consent forms. Ms Heffernan accepted that at that initial consultation, she met with a nurse and signed the consent form but denied that a nurse sat down with her and talked to her about the risks and complications of the surgery. The consent form is a one-page document, and although it refers to an acknowledgement that she understands that complications may occur, the document does not list or otherwise provide such information. I note that the consent form Ms Heffernan signed for her knee replacement procedure is near identical to that signed by (among others) Ms Ulrich and Ms Mattiske, who, it is to be recalled, undertook entirely different procedures as osseointegration patients. This illustrates the consent form could in no way be a substitute for a detailed discussion of the specific risks and complications associated with a knee replacement surgery.
2103 Ms Heffernan remembered being given a booklet on pain management, but not a brochure on the knee replacement procedure. I note if a pamphlet was given to her the day of her initial consultation, it either would have been provided shortly before she signed the consent form, or after she had consented to the surgery, for her to take home. On either alternative, it is difficult to see how Ms Heffernan would have had adequate opportunity to consider the information contained therein before making a decision to proceed with the surgery. For consent to be informed, the information must be provided before a decision is made. Further, as referred to elsewhere, Dr Ruff’s evidence is that such a brochure does not take the place of a surgeon providing the information and is only an adjunct to the process of informed consent.
2104 By contrast, Dr Al Muderis deposed in his affidavit that he “fully informed her of the relevant risks and potential complications”, despite accepting that he had no independent (or a vague) recollection of the first consultation
2105 Suffice to say, amongst other things, I am satisfied that Ms Heffernan was not adequately advised of the risks and complications of the surgery, which impacts on the consent she provided.
Ms Fay Young
2106 On 10 July 2017, Dr Al Muderis operated on Ms Young, performing a right total hip replacement. She was 77 years of age at the time. Dr Brian Owler, Ms Young’s neurosurgeon, had provided the referral on 15 June 2017 on the basis that he thought she had right hip pathology given she was experiencing right buttock and groin symptoms, radiating down into the thigh. Ms Young had her first consultation with Dr Al Muderis on 26 June 2017. I note that she signed the consent form for the total hip replacement surgery that same day.
2107 Mr Wright (who is also a patient of Dr Al Muderis, with his case study considered below), is Ms Young’s son. At the time he gave evidence in his affidavit, she was 83, had dementia, and so did not give evidence. The applicant took issue with Ms Young being unavailable to testify, submitting that according to Dr Sullivan in his affidavit, she was competent to give him consent to draft his affidavit. However, given Mr Wright’s evidence as to his mother’s medical condition and age, I do not consider there is anything untoward about her not being called. Mr Wright gave some brief evidence of his observations about his mother and her surgery. I note his evidence was that he was unaware that Dr Al Muderis was her surgeon until after her hip operation.
2108 Dr Ruff provided an expert report, in which his evidence in relation to Ms Young was that:
Dr Al Muderis failed to diagnose a periprosthetic fracture around the acetabular component of Ms Young’s right total hip replacement that left her walking on a fracture, untreated, for seven months.
2109 This observation of Dr Ruff was the main issue in contention concerning Ms Young. Dr Ruff opined:
Dr Al Muderis ordered an x-ray of the pelvis in October, 2017 when she repeatedly vented inability to walk because of pelvic pain. That x-ray performed on 18th October showed an acetabular fracture consistent with her presentation. The images are clearly different from the images obtained [in] September [and] should have raised the suspicion of a fracture against the background of her age and the surgery that had been performed and her persisting disability. They also suggest the acetabular component is loose. The presence of this fracture was again confirmed by radionucleotide imaging performed on 14th December, 2017 and requested by Dr Owler which showed a healing fracture around the acetabular component of the hip replacement. A copy of the correspondence from Dr Owler was sent to Dr Al Muderis with the report only [stating] that she had a sacral insufficiency fracture. That is part of the pelvis and Ms Young had pelvic pain after a hip arthroplasty that should have prompted a review of the bone scan. This did not occur.
2110 And:
… The fracture indeed became obvious on 17th October, 2017. Even if not convinced of a fracture he should have following comparison with the x-rays performed on 1st September investigated further with computerised axial tomography. Again, it was present on radionucleotide imaging in December. That there was a fracture of the pelvis obvious on this mode of imaging communicated to Dr Al Muderis didn’t stimulate him to review the images himself. Radiologist’s report of normality in an x-ray of specialist interest should not stimulate the specialist in the field to neglect to look at the studies himself. These oversights occasioned a 10 month delay of Ms Young’s treatment.
2111 Dr Al Muderis denied that there is a fracture evident on the x-ray dated 18 October 2017. When it was put to him that the difference between that x-ray and those obtained in September 2017 should have raised suspicion of a fracture given Ms Young’s age, the symptoms with which she presented and the surgery he performed, he said that was not true. He disagreed: the x-ray showed the acetabular component was loose; with Dr Ruff’s opinion as to what the x-ray showed; and, that further investigation was required. He submitted that even if the x-rays of October 2017 do show a fracture, there is insufficient evidence that failing to detect it was negligent.
2112 The applicant also submitted that as Ms Young did not provide an affidavit, she had not given express consent for the use of her medical information in these proceedings. As such, Dr Al Muderis considered himself legally and ethically precluded from giving evidence-in-chief about his treatment of Ms Young and submitted that allowing any evidence outside of the pleading in the circumstances causes prejudice to the applicant. However, no prejudice was identified. There was nothing to prevent Dr Al Muderis from preparing to be asked questions about Ms Young’s case, which he obviously fully understood (and was expecting) as he simply asked for a direction from the Court that he answer, to enable him to do so. That direction was given. As apparent from the passages recited above, Dr Ruff’s evidence was provided in his expert report, which was served prior to trial. Dr Al Muderis was plainly on notice of the respondents’ case. He was cross-examined in detail and was invited to respond to Dr Ruff’s accusation that he failed to detect the fracture, which he did (as apparent from the analysis below). I note, unlike with some other patients, the applicant chose not to adduce any evidence in reply. The failure to do so was a forensic decision.
2113 I accept Dr Ruff’s evidence.
2114 The respondents summarised Dr Ruff’s evidence in their closing submissions as follows (omitting evidence references):
Dr Ruff’s evidence about Mrs Young was very clear: (a) she was an elderly lady whose bone quality made her more prone to fracture; (b) the nature of the operation (a cement free socket through an anterior approach) required Dr Al Muderis to hit the implant with some force in order to make the implant fit; (c) an expected complication from that type of surgery in an elderly woman would be a fracture of the acetabulum: “And for six weeks afterwards she can’t walk. You should only be thinking that you’ve fractured the acetabulum. You should be looking for it”; (d) 90% of patients with severe arthritis of the hip are in less pain after surgery than they were the night before; the fact that she was in pain was a warning sign and should have been investigated; (e) the presence of a sacral insufficiency fracture (as described in Dr Owler’s report sent to Dr Al Muderis on 15 December 2017) was a “red flag” which tended to suggest that Mrs Young was excessively weight bearing on the opposite side of the fracture; (f) a CT scan should have been performed immediately when she presented with pain in October 2017; it was “almost mandatory”; (g) Dr Al Muderis failed to investigate the obvious clinical symptoms and repeated imaging available to him, and as a result, he failed to diagnose the fracture, which was a failure in his standard of care; (h) it was incumbent on Dr Al Muderis to review the x-rays himself, rather than relying on radiological reports because orthopaedic surgeons were the most qualified to do so, knowing the nature of the surgery the patient had undergone, and being vigilant for fractures; and (i) Dr Al Muderis encouraged Mrs Young to walk on the fractured hip causing her pain, and aggravation of her symptoms, including stress fractures across the sacrum which were part of the same propagation of fracture.
2115 That summary is accurate.
2116 It highlights the obvious: that it is necessary to consider each aspect of the evidence (including Dr Al Muderis’ evidence) in its proper context.
2117 First, as Dr Ruff said, Ms Young’s older age made her more prone to fracture. This is in a context where the surgery undertaken required Dr Al Muderis to hit the implant with force to make the implant fit. Dr Ruff said that a known complication of that type of surgery in an elderly woman is a fracture of the acetabulum. Although Dr Al Muderis does not address these issues, they could not seriously be in issue. They form part of the relevant context for assessing what occurred thereafter.
2118 Second, Ms Young was in pain and had difficulty walking after her hip operation with Dr Al Muderis. This is evident in the consultation report dated 1 September 2017 (seven weeks post-operation), which recorded that she was “still using a walker when walking” and “complaining of what appears to be some start up pain in the interior right thigh”. Dr Al Muderis recorded in that same report that “start up pain in the right thigh … is a very common occurrence following a press fit total hip surgery” and that:
I explained to the patient that the more she walks the quicker the ingrowth into the implant will occur and that it is really in her best interests to try to walk as much as possible in order to improve the bone remodeling around the implant.
2119 Dr Ruff’s evidence was that given 90% of patients with severe arthritis of the hip are in less pain after surgery than they were the night before, that Ms Young was in pain after the surgery was a warning sign and should have been investigated. As the respondents submitted, her pain and difficulty walking were red flags that should have prompted Dr Al Muderis to immediately obtain a CT scan to rule out a fracture. Dr Al Muderis did not do so (he only ordered x-rays on 1 September 2017). I note that although the plan of management recorded in the 1 September 2017 report was to see Ms Young in three months, Ms Young attended Dr Al Muderis’ clinic again five days later on 6 September 2017, complaining from increasing fluid in her right anterior thigh and pain in the anterior groin region. She underwent an aspiration on that occasion and was admitted to hospital overnight for further testing. Dr Ruff’s opinion was that given Ms Young had fluid aspirated from the surgical field, a cement-free arthroplasty and pain, a CT scan would not have been difficult to obtain and was “almost mandatory”. Contrary to the applicant’s submission, Ms Young was exhibiting symptoms of a fracture. Indeed, the 6 September 2017 consultation report recorded that Dr Al Muderis’ plan of management following the aspiration was to, inter alia:
… get new x-rays of the right hip, a standing AP of the pelvis to include both hips as well as a frog leg lateral of the right hip to rule out a possible fracture that could be causing the increasing bleeding in the area.
However, when Ms Young returned to the clinic on 11 September 2017 following her aspiration, Dr Al Muderis recorded in the consultation report that she was feeling better, but did not otherwise order new scans to rule out fracture: “[n]o x-rays were obtained today”. Dr Al Muderis said that this was unnecessary “because she had an x-ray just a week before”. X-rays were not obtained again until the October 2017 consultation.
2120 Third, as apparent from the summary of Dr Ruff’s evidence, his opinion was that the x-rays of 18 October 2017 showed an acetabular fracture consistent with her presentation. He also said that in any event, there was obviously a clear difference between those images, and the ones taken in September 2017, which should have raised the suspicion of a fracture in her circumstances (as described above). Dr Ruff said, in answer to questions in cross-examination, that one would not necessarily expect to see the fracture in the earlier x-rays, but rather that a CT scan would have been required given her progress at that time reached the six-week mark.
2121 The applicant submitted that there was no evidence of any consultation on 18 October 2017. It is unclear how that assists the applicant. It is plain from the evidence, namely the radiologist’s report, that it was Dr Al Muderis who ordered the x-ray on 18 October 2017 and that he was the referring doctor. One assumes that was ordered for a reason. Records from the clinic’s SMS communications with Ms Young reflect that she did have an appointment at around the time the x-ray was taken. In summary: on 16 October 2017, the clinic texted Ms Young about her next appointment with Dr Al Muderis on 20 October 2017; the x-ray was taken on 18 October 2017, as ordered by Dr Al Muderis; and on 19 October 2017, following another text reminding her about the appointment the following day, Ms Young replied ‘Y’ to confirm (as requested). Although there is no evidence that the consultation took place, there is similarly no evidence that it was cancelled or that Ms Young did not turn up. Dr Al Muderis did not recall whether it took place. There is also no record that Dr Al Muderis reviewed the x-ray of 18 October 2017 or compared it with the September 2017 x-ray.
2122 The applicant’s submission relies on his evidence of standard practice, that he would usually compare x-rays with previous x-rays. However, given the circumstances of the 18 October 2017 x-ray, the issue the applicant raises of whether there was a consultation, and the lack of any records, as described above, it is difficult to accept the applicant’s submission that it is likely he followed his standard practice. Moreover, if the consultation occurred, there is no consultation report, which is also contrary to his standard practice (although there is evidence of other instances of that in this case, e.g. Mr Haskett, Mr Smith, Mr Urquhart). As such, he cannot describe her symptoms that day or suggest they were not consistent with the fracture. It was apparent that Dr Al Muderis had no memory of the events and was dependent on his records. The problem is there is no record. As he has no memory of this critical consultation, there is no basis for his evidence or submission that he believed Ms Young’s problems had resolved. This is in a context where the existence of an October 2017 consultation is consistent with the plan of management outlined in preceding consultation reports from September. It was three months post-surgery, and when last seen by Dr Al Muderis on 11 September 2017, the plan recorded in the report was to see Ms Young in one month. Those reports recorded that Ms Young was still using a walker.
2123 The applicant also submitted that Dr Ruff’s evidence regarding the October 2017 x-ray should not be accepted because the radiologist supports Dr Al Muderis’ opinion, given he stated in his report that there were “[n]o complications seen” of the right hip. It is to be recalled that the applicant similarly relied on a radiologist report which did not identify a fracture in the case of Mrs Gollan. Dr Ruff’s opinion was that:
[Radiologists] look at multiple different x-rays all day, and they’re as good as the information that’s given to them … we’re doing things that they wouldn’t dream of looking for … we [orthopaedic surgeons] know what happens to people after we’ve put things in them. Fractures occur, and we’re vigilant for it.
Consequently, as referenced above, Dr Ruff was of the opinion that “[r]adiologist’s report of normality in an x-ray of special interest should not stimulate the specialist in the field to neglect to look at the studies himself”. Dr Al Muderis’ evidence on that topic was unsatisfactory. Initially he disagreed with the proposition put to him in cross-examination – that the diagnosis of a fracture is a matter of reading the imaging, rather than relying on what might be written in a report. He continued, saying that a radiologist’s job is “to diagnose fractures and diagnose pathologies and … they are the most qualified people in diagnosing a pathology on an x-ray”, before eventually accepting (albeit reluctantly) that as the specialist, he is to form his own view. However, the problem for the applicant’s case is that there is no evidence that he did that here or that he compared it to the earlier x-ray obtained in September. Given that lack of evidence, to state the obvious, Dr Al Muderis’ opinion is expressed in evidence in this hearing occurring in 2023 to 2024, not in October 2017.
2124 The applicant raised that Dr Ruff may have used hindsight reasoning in his analysis. However, Dr Ruff was conscious of avoiding that (i.e. looking for issues) and explained how he satisfied himself that it had not formed the basis of his view in this case.
2125 Fourth, there was further imaging obtained on 22 November 2017 and 30 November 2017 which were “scout images”. Dr Al Muderis said in respect to the 22 November 2017 image that it was “inappropriate for any clinician to make comments about this image with regard to any abnormality”. Although Dr Ruff conceded that he had no basis to assume these scout images were sent to Dr Al Muderis, his evidence was that the referring doctor would have access to them. Dr Ruff obtained them himself through his own practice in preparing his report in these proceedings. Although he accepted that scout images are generally not used for any diagnostic purpose in so far as they are not a clinical tool used to assess fractures. In response to the proposition put to him in cross-examination – that scout images ought not be used to diagnose a problem – he said:
No, I wouldn’t agree with that at all. I would agree that if you suspect a fracture and you can’t see it on a scout image, it may still be there, but I wouldn’t agree that if you can see a fracture on a scout image that it’s probably not there. The scout image is better than that. The scout image is being performed so that you can find out exactly where you are in the skeleton. It’s of sufficient quality to be able to identify – if a fracture is obvious, scout image is perfectly satisfactory … So, yes, they can be used to diagnose a fracture. They can’t be used to say a fracture is not there; they’re not of sufficient quality. But if a fracture is obvious enough, clearly they can be used, and that’s the case here.
2126 Although the 30 November 2017 images were also scout images, Dr Al Muderis accepted (first without any prompt upon being shown the image) that “[it was] a clear image” stating “I can see a fracture very clearly … Yes, there is a fracture here. I can see there is disruption, correct”. This was also Dr Ruff’s evidence, that is, that the image showed the fracture. The evidence is silent on the purpose of any activity on 22 and 30 November 2017, which resulted in the scout images being taken.
2127 Fifth, on 5 December 2017, Ms Young attended a further consultation with Dr Al Muderis. The consultation report, dictated by Dr Shakeeb Jawazneh on behalf of Dr Al Muderis, records that Ms Young was “progressing slowly” from her hip replacement and that she was “satisfied with the [right] hip and does not report any issues with her hip”. However, she was:
… complaining from left hip pain and she said that the pain is very, very severe and affects her quality of life and she does use a stick to help her ambulate.
It also records that she ambulated using a wheelchair at the consultation. There is no reference in the report to the x-rays of 18 October 2017, or any of the preceding events (and the issues that arose for her). There is also no reference to the events that led to the scout images taken in November 2017. As referred to above, there is no evidence as to the purpose of the activity that resulted in those scans, although they were obviously taken for a reason.
2128 The content of the consultation report must be considered in a context where Ms Young did, in fact, have a fracture in her right hip, as Dr Al Muderis accepted was clearly shown on the scout image dated 30 November 2017.
2129 Jumping ahead, it was not until July 2018 when Ms Young’s fracture was first diagnosed by Dr Al Muderis. Ms Young had contacted his practice with a complaint as to her condition, namely that she “was in a significant amount of pain for the past several months” and was subsequently seen “on an urgent basis”. On attending, the consultation report for 31 July 2018 records that she “has been struggling to mobilise [ever] since her surgery”. That is consistent with what is recorded as to her state in the reports that exist for consultations in 2017. It is consistent with there being a fracture, as Dr Ruff explained was in the 18 October 2017 x-ray, and accepted by Dr Al Muderis was apparent in the 30 November 2017 scout image.
2130 Sixth, on 14 December 2017, Dr Tung Vu conducted a whole-body bone scan and sent a letter to Dr Owler (as the referring doctor), in which he records a conclusion that there was a “[p]robable non-acute right acetabular fracture”. Dr Al Muderis said he was not sure whether he had seen the letter before, but that he “may have”. Ms Young was examined by Dr Owler at a consultation on 15 December 2017, who reported that she had attended the appointment in a wheelchair, had severe pain over the sacral region (mainly on the left side) and that as demonstrated in the bone scan, she had “sacral insufficiency fractures, being much worse on the left than the right side”. This letter was copied to Dr Al Muderis. It is unclear on the evidence whether the underlying imaging or report from Dr Vu was sent to Dr Al Muderis with the correspondence from Dr Owler. Regardless, and contrary to the applicant’s submission, Dr Ruff’s opinion is not dependent on that occurring. The applicant also submitted that Dr Owler’s letter reported “sacral insufficiency fractures”, which are “wholly unconnected to the hip replacement” given the right hip replacement was not in the sacrum (at the back of the body) but in the acetabulum (at the front). He submitted that there was nothing in Dr Owler’s letter to indicate that the imaging showed a fracture in the acetabulum. Dr Ruff’s evidence was that:
A copy of the correspondence from Dr Owler was sent to Dr Al Muderis with the report only that she had a sacral insufficiency fracture. That is part of the pelvis and Ms Young had pelvic pain after a hip arthroplasty that should have prompted a review of the bone scan. This did not occur.
As Dr Ruff explained in cross-examination:
… [Dr Owler] has told [Dr Al Muderis] he [identified] a stress fracture of the sacrum … And that’s connected to the acetabulum. Really, you put a cement free arthroplasty in an elderly lady, and she can’t walk, you’ve got to actually ask yourself why.
Further, he was asked:
Ms Chrysanthou: In relation to what you said about the sacral insufficiency, those fractures were in fact on the other side, not on the same side as the hip replacement. Do you agree if that’s all that Dr Al Muderis was told and was not given the bone scan.
Dr Ruff: No, I don’t. He should have been aware of it. So why – why has she developed – let’s – let’s assume that it’s not related in a direct continuity with the fracture which turned out to be a double column fracture. So it goes right round into that posterior. That has only occurred because she – she has got it worse on the opposite side because she has been weight bearing on that side because she can’t take any weight on the other side. They’re all red flags.
2131 If the scans had been considered (as they should have been), the right acetabular fracture would have been clear.
2132 Dr Al Muderis suggested he may not have seen or read the letter from Dr Owler as it is not practical to do so for all the reports copied to him. However, this relates to a patient who he had recently operated on (just five months prior) and who had ongoing issues with pain and mobility as at the time he last saw her (just ten days prior on 5 December 2017). That consultation report recorded that he wanted to see her again in three weeks. As mentioned above, it also recorded she had made slow progress, had reported severe pain, used a walking stick to ambulate and was still presenting in a wheelchair. It is difficult to understand, given the circumstances, why Dr Al Muderis did not have a responsibility as her surgeon to consider this correspondence and its implications given her ongoing symptoms and his intention to assess her progress at the next consultation. She was his current patient. He was the orthopaedic surgeon, not Dr Owler (who was a neurosurgeon).
2133 I note that there are no further documents between December 2017 and July 2018 in evidence. The consultation report on behalf of Dr Al Muderis dated 31 July 2018, recorded “[s]he was last seen … on 5 December 2017 and has not followed up since”. There is no evidence of Dr Al Muderis’ office following up with Ms Young during this time despite the management plan in the December 2017 report referring to Dr Al Muderis saying he “would like to see her again in three weeks time for further clinical review”. As noted above, Ms Young had prompted the communication with Dr Al Muderis in July 2018.
2134 On 25 July 2018, Dr Owler ordered further x-rays. The x-ray report dated 28 July 2018 compared the scans to those obtained on 18 October 2017 and recorded findings as follows: “There is a periprosthetic fracture through the pelvis at the acetabulum. There is mild displacement. There is increasing subluxation at the pubic symphysis”. Although ordered by Dr Owler, the report stated, “This report is for: A/Prof M. AL MUDERIS” and “Copies: A/Prof M. AL MUDERIS”. Dr Al Muderis accepted in cross-examination that the report was brought to his attention.
2135 On 31 July 2018, Ms Young called his office, the consultation notes record that she was “very angry” at her condition, that she refused to come in to see Dr Al Muderis and that she “just wanted [him] to check her scans”. After Dr Al Muderis called her himself, Ms Young agreed to attend a consultation with him that same day (as referred to above). Dr Al Muderis ordered a CT scan at that consultation, with the report of that scan confirming that there was an “[a]cute periprosthetic fracture adjacent to the right acetabulum, in association with bilateral sacral fractures and displacement of the pubic symphysis”. The consultation report records evidence “suggestive of the chronicity of the injury”. That day, Dr Al Muderis booked Ms Young in for corrective surgery scheduled for 22 August 2018, but that booking was later cancelled by her husband on 7 August 2018. On 9 August 2018, Ms Young had a consultation with another orthopaedic surgeon, Dr James Sullivan (having been referred to him by her GP), who performed revision hip arthroplasty surgery on 17 October 2018.
2136 I accept Dr Ruff’s evidence that in the circumstances, Dr Al Muderis should have investigated the possibility of a fracture, and he did not. I accept that a fracture is evident on the October 2017 x-rays. I also accept Dr Ruff’s evidence that if Dr Al Muderis had considered the October 2017 x-rays (at that time), he should have seen the fracture, or at the very least, a comparison with the September 2017 x-rays would have showed differences such that it should have led to further investigations. That would have revealed the fracture. Other red flags were missed thereafter (e.g. the letter from Dr Owler) which occasioned a delay in Ms Young’s treatment.
2137 Mr Wright gave evidence that his mother:
… required the assistance of a wheelchair to mobilise, she can barely walk these days. Since the surgery with Dr Al Muderis, she has been wheelchair bound for 90 percent of the time. She wasn’t in a wheelchair before her surgery with Dr Al Muderis.
2138 I note that the applicant submitted that there is no medical evidence linking these alleged conditions to Dr Al Muderis’ surgery. However, Mr Wright’s evidence is a direct observation of Ms Young from the time of her surgery. And, as explained above, the evidence establishes, she did have a fracture which went undiagnosed by Dr Al Muderis for many months. That Ms Young obtained a second opinion from Dr Sullivan, in the circumstances of this case, gives rise to the inference that Ms Young was unhappy with the care that Dr Al Muderis had provided. As referred to, on 31 July 2018, Ms Young called his office. The consultation notes record that she was “very angry”. On 4 November 2020, Ms Young telephoned Dr Al Muderis’ rooms to “communicate to Munjed ‘what he has done to [her]’”, with that complaint recorded in the clinic records. This was well before the Publications.
2139 Finally, I note that the applicant submitted that the Ms Young was “wholly happy” with her hip replacement after her surgery. That does not accord with the observations of her son, that Ms Young was angry when she rang in July 2018, or that she did not proceed with her scheduled surgery with Dr Al Muderis in 2018. The applicant submitted that it is unknown when the facture occurred and that whether Ms Young experienced a fall. However, I accept that the x-rays of October 2017, ordered by Dr Al Muderis, showed a fracture. Even leaving that aside, Dr Al Muderis admitted that the 30 November 2017 scout image showed “a fracture very clearly”. Dr Al Muderis saw Ms Young after that time, in December 2017 (with the consultation report making no refence to the October 2017 x-rays).
2140 I am satisfied that Dr Al Muderis failed to provide post-operative care with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
Further patients
Ms Deborah Brandon
2141 Ms Brandon joined the Royal Australian Air Force (RAAF) in February 2012. Dr Al Muderis performed a left knee arthroscopy with lateral release on 5 May 2014 and a left patellofemoral joint replacement on 2 February 2015.
2142 Although it appeared Ms Brandon was visibly distressed in giving evidence, she was an honest, credible and generally reliable witness. Ms Brandon had an unrelated medical incident before her contact with Dr Al Muderis which impacted her.
2143 When Ms Brandon joined the RAAF, she was 39 years old, an achievement which she worked hard to attain at a more mature age and was very proud of. Having a deployable role in the RAAF was extremely important to her. In summary, after Ms Brandon began experiencing problems with her knees while she was a rookie in 2012, she was referred by the RAAF doctor to an orthopaedic surgeon who recommended she undergo bilateral knee arthroscopies, which he subsequently performed in April 2013. Following the surgery, she continued to experience pain in her left knee and on 28 April 2014, she was then referred to Dr Al Muderis. As mentioned above, Dr Al Muderis performed a left knee arthroscopy with lateral release on 5 May 2014 and a left patellofemoral joint replacement on 2 February 2015 (also known as a partial knee replacement). Neither procedure resulted in any improvement and Ms Brandon continued to experience significant pain, struggled with her mobility and was on heavy painkillers. Ms Brandon was subsequently medically downgraded and classified as non-deployable (and was never deployed) on 9 April 2015 and was medically discharged from the RAAF on 7 April 2016. In late 2020, she obtained a second opinion and subsequently underwent a total knee replacement with another orthopaedic surgeon.
2144 In cross-examination, Dr Al Muderis was questioned on his opinion in a consultation report dated 20 January 2015, that Ms Brandon was not suitable for a knee replacement at the time. Dr Al Muderis’ evidence was that a total knee replacement would have affected Ms Brandon’s ability to be deployed to a certain extent. He said that, rather, a patellofemoral joint replacement would be “the happy medium” to give her pain relief and, at the same time, keep her employed and deployable. He said that this was a relatively intermediate solution for Ms Brandon to continue with her career.
2145 The applicant submitted that Dr Al Muderis’ advice was conservative given her age at the time. The applicant also relied on the evidence of Dr Stoita as to the suitability of this option. He expressed the view that Ms Brandon was a suitable candidate for either a patellofemoral joint replacement or a total knee joint replacement and the decision making needed to be shared between the patient and the surgeon.
2146 Dr Ruff, who gave evidence that he was a Lieutenant Colonel in the Australian Army and had been an orthopaedic advisor to Eastern Land Command, opined that “[n]o one with a patellofemoral joint [replacement] is going to have the fitness that … they require for deployment”. Dr Ruff’s evidence was that Ms Brandon should have been advised of that prior to any surgery. He said she should have been told to reduce her activity instead, which could have avoided the patellofemoral joint replacement. Dr Ruff said such replacements are rarely performed in Australia because they are so hard to get right (he discussed that in the year Ms Brandon underwent her procedure, 600 patellofemoral joint replacements were performed in Australia, compared to 55,000 knee replacements). Dr Stoita similarly conceded that such procedures are performed infrequently. Dr Ruff’s evidence was that Ms Brandon should also have been told the failure rate for patellofemoral arthroplasty in Ms Brandon’s age group, and if it fails, that knee replacement is the only option. Dr Stoia’s evidence appears to be to the same effect. I note that the applicant gave evidence that Dr Ruff had misinterpreted the figures and was referring to those for men and not women. On either scenario (i.e. regardless of the precise figures), it is an operation rarely or infrequently performed. Dr Ruff took issue with the opinion expressed by Dr Stoita as to Ms Brandon’s suitability for patellofemoral joint replacement and explained the basis for his contention. I prefer the evidence of Dr Ruff that given Ms Brandon’s objective, she should have been told that she would not be deployable as well as the failure rate of the procedure (accepting that there is some dispute in the evidence as to what that rate is), before she made the decision to have the surgery.
2147 Dr Ruff was asked in cross-examination if he agreed with the proposition that, if Ms Brandon had several reasons why she would never be deployable and that aim could not be achieved with any orthopaedic remedy, would she be a suitable candidate for the surgery, to which he replied, “yes … if she understood what her limitations are to that surgery”. The question misses the point. As does the applicant’s hindsight submission that Ms Brandon was never deployable. Indeed, as referred to above, on the applicant’s evidence, this surgery would keep her deployable. Deployment was Ms Brandon’s objective, which I accept she told Dr Al Muderis. I note that Dr Paterson’s letter to Dr Al Muderis dated 21 May 2015, reports on her progress and records that Ms Brandon’s objective was deployment, and so she apparently told others. Given this objective, Ms Brandon should have been provided with the relevant information that would have allowed her to make a fully informed decision. There is no reference in any of Dr Al Muderis’ consultation reports to Ms Brandon’s objective, or that the limitations of the surgery were discussed, despite Dr Al Muderis conceding that he knew her employment was very important to her. Dr Stoita also conceded that this should have been discussed and there would need to be a careful discussion which encompassed both the risks of the surgery and Ms Brandon’s expectations.
2148 I accept that Ms Brandon was not informed that she would not be deployable after having this surgery. Given that this was her objective, she should have been provided with this information before making the decision as to whether to undergo the patellofemoral joint replacement procedure. It impacts on the consent she gave. It was not informed.
2149 Finally, I simply note that Ms Brandon took issue with the accuracy of Dr Al Muderis’ consultation reports after her patellofemoral joint replacement surgery. For example, Ms Brandon said that the consultation reports dated 10 February 2015 and 11 August 2015 that record her being “satisfied” with her results are wrong. She denied saying that she was happy with her results so far, said there was no satisfaction and that she was still in a lot of pain. Further, she said the consultation reports dated 24 March 2015 and 5 May 2015 misstated the level of pain she was experiencing and that it was higher in actuality. When it was put to Ms Brandon that on 5 May 2015, she told Dr Al Muderis that she felt she was improving (as it was recorded in the consultation report), she responded that that was a lie. She said that her pain never improved, and although Dr Al Muderis recorded in that report that she had a very good range of motion, she disagreed, saying her knee was too swollen and sore. That said, I note that Dr Paterson’s report of 23 July 2015 recorded that:
On the whole [Ms Brandon] says that her left knee pain is gradually getting better and has seen a slow improvement in her pain which has been of benefit given she was somewhat catastrophic about her slow progress.
2150 These are some examples in her evidence. I have addressed the inaccuracies of consultation reports as compared to patient evidence elsewhere. It is unnecessary to resolve the all the disputes as to the accuracy of the reports. That said, given her circumstances, and evidence as to her post-surgical experience, it is unlikely that she would have said she was satisfied with the results, at the time those statements are attributed to her in Dr Al Muderis’ consultation reports.
Ms Kathryn Hutton
2151 In or around 2013, Ms Hutton was diagnosed with osteoarthritis in her right knee and gave evidence that over time the condition worsened. Ms Hutton underwent her right total knee replacement with Dr Al Muderis on 30 July 2018.
2152 Ms Hutton gave evidence in an honest, clear, and direct manner. She was a credible witness. The applicant did not contend otherwise, although he raised issues as to her reliability.
2153 Dr Al Muderis consulted with Ms Hutton on 2 January 2018 after she was referred by her GP in relation to constant pain in both of her knees. At that consultation, Dr Al Muderis recorded in his report that the MRI scans showed arthritic changes, that Ms Hutton had exhausted all conservative measures, and that she would benefit from a total knee replacement. He stated that he would replace one knee at a time, starting with the right knee. She decided to proceed with the right total knee replacement surgery and signed the consent form that day.
2154 Ms Hutton gave evidence that the initial consultation lasted about five minutes (or if longer, not by much), and that Dr Al Muderis did not explain the procedure, the risks involved, or what preparation would be required. Dr Al Muderis disagreed but accepted he had no memory of what occurred at that consultation. I note that the consultation report for that date does not refer to any such matters being discussed, but rather records that Dr Al Muderis provided her with an information pack from the Australian Orthopaedic Association in relation to total knee replacement, which provides information on the procedure, rehabilitation and informs the patient about the benefits, risks, complications, and red flags. The consultation report also records that he would like Ms Hutton to peruse the information pack and that he would be happy to answer any further questions. Ms Hutton recalled being provided with this information pack. The presence of this passage in the report (which appears pro forma), in context, supports Ms Hutton’s evidence as to what occurred (or rather, what did not occur). Indeed, Dr Al Muderis accepted in cross-examination that to the best of his recollection this was “the extent of what occurred on that occasion”.
2155 As referred to elsewhere, Dr Ruff said that the provision of brochures or other documents is insufficient to explain the potential risks, consequences and complications of surgery. Further, as I discussed above in relation to Ms Heffernan, I note that as the brochure was provided to Ms Hutton on the day of her initial consultation (on the applicant’s case), it would have been provided to her shortly before she signed the consent form that day, or after she consented to the surgery, for her to then take home. On either alternative, Ms Hutton did not have an adequate opportunity to consider the information before being asked to consent to the surgery.
2156 Separately, in his affidavit, Dr Al Muderis referred to providing Ms Hutton with a hospital admissions information sheet to contend that she had been informed about the preparation required ahead of her surgery. I note that this is a very high level and general one-page document that does not include any mention of risks or complications. Dr Al Muderis also relied on Ms Hutton’s signed consent form as evidence that she was informed of the risks and understood the nature of the procedure. However, I note the language used in the consent form is similarly very general, as it acknowledges that the doctor has told the patient that the operation “carries some risks and complications” (I have discussed the use of a generic consent form for other patients elsewhere, e.g. Ms Heffernan). That is in the context where Dr Al Muderis accepted the extent of what occurred in Ms Hutton’s first consultation was the provision of the information book. Those general documents are not sufficient. As the respondents submitted, this general paperwork does not obviate the need for a detailed discussion between Ms Hutton and her treating surgeon.
2157 I turn then to the consideration of Ms Hutton’s assessment for knee replacement surgery. Ms Hutton’s evidence was that she weighed around 130 kg at the time of her first consultation. Her BMI was 41. In cross-examination, Dr Al Muderis accepted in respect of another patient (Mrs Gollan), that a BMI of 41 is, in clinical terms, in the category of morbidly obese. According to Dr Ruff, the American College of Knee Arthroplasty Surgeons recommends against performing knee arthroplasty in patients with a BMI over 40. The only reference to her weight in the consultation report is that she was “unable to lose weight because she is unable to exercise because of the pain in her knees”. Ms Hutton gave evidence that Dr Al Muderis did not warn her that her weight would affect her recovery. Dr Ruff’s evidence was that although the report dismisses Ms Hutton’s chances of reducing her weight through exercise, there ought to have been a discussion at this stage about changes to Ms Hutton’s diet that may have reduced her weight (noting that weight reduction is 80% diet).
2158 As Dr Ruff pointed out, there is no record in any consultation report of any physical examination of Ms Hutton’s hip in the lead up to her knee replacement surgery. Ms Hutton was not asked about an examination of her hip. She said she had no memory of any physical examination when asked about her knee.
2159 As stated earlier, Dr Al Muderis did not recall the consultation. Nonetheless, he gave evidence that he conducted a physical examination of Ms Hutton, which included her knee, hip, foot and ankle, as well as a neurovascular examination and an assessment of her gait. That, he said, is his standard practice. His evidence was that he examines the hip, and if there is a positive finding, that would be recorded (i.e. if a clinically significant symptom is identified). That is problematic given the purpose of medical records. On this approach, another doctor looking at Ms Hutton’s medical records would be unaware of whether an adequate hip examination had been undertaken, in circumstances where an examination is required (as noted by Dr Ruff below).
2160 Dr Ruff noted that in his pre-operative assessments, Dr Al Muderis:
… failed to record symptoms or signs associated with the ipsilateral hip which is essential in all cases of arthritis of the knee because of the prevalence of hip pathology presenting with knee pain. There is no record of an assessment of the arterial supply to the leg or the neurological function in the lower limbs.
2161 He said that an examination was “essential” to exclude the possibility of Ms Hutton’s pain being due to hip arthritis. Dr Ruff opined, in a context where there is no evidence Dr Al Muderis conducted any adequate physical examination of Ms Hutton at the 2 January 2018 consultation (despite some examination of her knee being recorded), that Ms Hutton may have had a knee replacement when she in fact had arthritis of the hip.
2162 He observed that this is in a context where, just 14 months after her right knee operation, Ms Hutton was experiencing pain from arthritis in her hip on the same side, and Dr Al Muderis advised on 10 September 2019 that she had hip arthritis which could be fixed with a total hip replacement.
2163 This is also in a context where Dr Al Muderis recommended a knee replacement on the basis of severe lateral compartment arthritis of the knee, which was not visible on an x-ray and only visible on “more recent scans” of her knee (as referred to in his consultation reports dated 2 January 2018 and 8 May 2018), which have never been produced. In cross-examination, Dr Al Muderis was asked where those “more recent scans” were, to which he said “I wouldn’t have a clue. I’m not sure”. He said the MRI scans would be accessible via a computer, and he would look for them. They were not produced.
2164 The respondents submitted that as there is no satisfactory explanation for the failure to produce the “more recent scans”, the Court should infer the “more recent scans” do not exist, or alternatively, that they do not support the conclusion that Ms Hutton required knee surgery. They contended it is open to the Court to conclude, as did Dr Ruff, that Ms Hutton likely received a knee replacement from Dr Al Muderis when in fact she needed a hip replacement. At best, she received a knee replacement where the justification for doing so was speculative. The applicant does not address this issue. Rather, the applicant’s submissions omit any reference to the recent scans, stating only that Dr Al Muderis “reviewed MRI scans from 2015 which showed arthritic changes”.
2165 I am satisfied that Dr Al Muderis failed to adequately advise Ms Hutton of the risks associated with the surgery (including a failure to warn Ms Hutton of the impact of her weight on her recovery). This impacted on her consent being informed. I accept Dr Ruff’s opinion, given Ms Hutton’s weight, that steps ought to have been taken to attempt to reduce this before surgery. The absence of the most recent scans despite the request from the respondents, which according to the consultation reports, was the basis for Dr Al Muderis’ conclusion as to severe lateral compartment arthritis of the knee, is most concerning. It is without explanation. Rather, the applicant chose not to address the issue in closing (including in reply). This is in a context where the scans would have addressed the issue raised by Dr Ruff that this surgery might not have been necessary. This is also in the context where Dr Al Muderis’ evidence he performed a hip examination at the consultation consistent with his standard practice is unsupported, given his failure to record an examination. That is, there is no medical record in evidence reflecting that an adequate assessment for Ms Hutton’s suitability for the surgery was undertaken. Given that and the failure to produce the scan, I am not prepared to accept Dr Al Muderis’ evidence that he examined her hip based on what he said was his standard practice.
Mr Adam Wright
2166 After experiencing pain in his left knee, Mr Wright was referred to Dr Al Muderis on 21 February 2014 by Dr Emad Hanna, who sought Dr Al Muderis’ opinion regarding a possible meniscal tear. He was 48 years old at the time. Mr Wright consulted with Dr Al Muderis on 25 February 2014. Dr Al Muderis agreed with Dr Hanna that Mr Wright may have injured his medial meniscus and that, if confirmed on an MRI, he would be “more than happy” to operate on him. Dr Al Muderis recommended that Mr Wright undergo keyhole surgery (knee arthroscopy) to clean up the meniscus. Mr Wright said that during his half-hour consultation, Dr Al Muderis “went through some of the risks, but indicated it was a minor surgery that needed to be done, and he was quite confident in the outcome”. I return to the discussion of risks below.
2167 The MRI was undertaken on 28 February 2014, with the report stating:
COMMENT: Torn medial meniscus and medial compartment chondral wear and arthrosis. Small joint effusion and pes anserinus bursitis. No loose bodies of note.
2168 On 31 March 2014, Dr Al Muderis performed an arthroscopic and medial femoral condylar chondroplasty on Mr Wright.
2169 Mr Wright was an honest, credible and reliable witness. The applicant accepted that he gave clear, direct and responsive answers in cross-examination and that except for a few issues, his evidence could be accepted.
2170 There is a discrete matter in issue concerning the conclusions to be drawn from the MRI. Dr Al Muderis’ evidence was that the results confirmed that Mr Wright had an injured medial meniscus.
2171 Dr Ruff opined that it was clear from the MRI that there was “medial compartment chondral wear and arthritis. Arthrosis means arthritis”. It showed “chondral wear at the edge of the tibial plateau and femoral chondral with subchondral bone change” and that is “osteoarthritis of the knee”. He opined that:
In the setting of osteoarthritis of the knee, meniscal pathology observed on an MRI scan may be part of the arthritic process and not an acute injury in which case arthroscopic debridement of the meniscus may make arthritis progress rapidly. The probability of this is of the order of 10%. Forty percent of patients will see no improvement and 50% may find improvement that is temporary. It doesn’t appear Mr Wright was aware of this. Dr Al Muderis’ correspondence doesn’t include an explanation of this in the lead up to the arthroscopy.
2172 Mr Wright was not warned of the risk that an arthroscopy may potentiate the setting of osteoarthritis of the knee. As Dr Ruff noted, in Dr Al Muderis’ operation report, under the heading of “consent”, it refers to the patient being aware of all the risks and complications, despite there being “no mention that the surgery may make knee pain worse in the setting of arthritis”.
2173 Dr Al Muderis disagreed with Dr Ruff’s opinion above but conceded that an arthroscopy to debride articular cartilage “may lead to progression of arthritis”. Even on Dr Al Muderis’ evidence, the risk should have been disclosed to obtain informed consent. That said, I prefer the evidence of Dr Ruff. In cross-examination, Dr Ruff gave evidence that advising Mr Wright of the risk is part of the standard of care. I accept that Dr Al Muderis did not warn Mr Wright that the arthroplasty may make arthritis progress more rapidly. I accept that his failure to do so resulted in the risks and complications not being adequately explained prior to surgery.
2174 Mr Wright did experience complications after surgery including swelling, pain and stiffness in his knee. This is supported by Dr Al Muderis’ consultation reports dated 22 May 2014 and 11 November 2014. Post-surgery, the very risk that had not been disclosed became a reality: diagnostic imaging and MRI results taken on 21 January 2015 confirmed the progression of arthritis in Mr Wright’s knee.
2175 I note for completeness that Mr Wright gave evidence of obtaining a second opinion from Dr Roberta Chow as early as December 2014, and a sports and exercise medicine physician, Dr Corey Cunningham, on 9 June 2021. When Mr Wright was contacted by Dr Al Muderis’ receptionist about one year after his operation, advising him to attend a 12-month post-operative consultation with Dr Al Muderis, he informed them he had sought a second opinion and did not need a follow-up. Mr Wright’s evidence was that shortly after this, Dr Al Muderis called him personally and asked why he had sought a second opinion, as well as who he had sought that second opinion from. He said that Dr Al Muderis’ tone was aggressive, and that he “was sort of grilling [him] a little bit as to why [he] got a second opinion”. Dr Al Muderis denied the conversation occurred, saying that he did not recall calling him, and that he would not have been angry or aggressive that Mr Wright sought a second opinion. Mr Wright’s evidence has a ring of truth. I accept that this conversation between Mr Wright and Dr Al Muderis occurred in the way Mr Wright described.
2176 Finally, I observe that Mr Wright’s evidence of his experience was that Dr Al Muderis’ demeanour changed post-operation, describing that Dr Al Muderis was “dismissive” of him and “abrupt”. He explained that “prior to [the] operation [Dr Al Muderis] was quite open and friendly towards [him], and then post-op … he just seemed to be quite dismissive or wanting to rush [him] through”, and that he did not seem “caring”. He said that the approach Dr Al Muderis took was: “It will be – it will be fine. Do what I tell you to do and – you know, do the physiotherapy, your knee will be fine”. Dr Al Muderis disagreed that he was dismissive, stating that he cared about Mr Wright’s reported issues. Dr Al Muderis did suggest an MRI during the 11 November 2014 consultation, which I note was prompted by Mr Wright, given the consultation report states, “[Mr Wright] is wondering whether he should be investigated further. I agree a further MRI scan with a new x-ray would be beneficial”. Mr Wright’s view of his experience with Dr Al Muderis is the context in which the second opinion was sought. Mr Wright’s evidence as to his experience of Dr Al Muderis’ post-operative demeanour rings true, and I accept his evidence in respect of this. I note that other patients gave evidence that after surgery Dr Al Muderis would dismiss their concerns.
Ms Lesa Anne Slater
2177 Ms Slater is a sergeant in the RAAF and has been since 2001. On 19 January 2015 she had surgery on her right knee, performed by Dr Al Muderis.
2178 The applicant accepted that Ms Slater gave clear and direct answers, and her evidence could generally be accepted, except where it conflicts with contemporaneous documents.
2179 Ms Slater consulted with Dr Al Muderis on 18 November 2014. She was referred by Dr Aziz Iboyan, who noted she suffered from a long-standing history of pain and discomfort, with an MRI scan showing changes to her right knee. Around October 2014, Ms Slater dislocated her right knee (patella) while marching in a parade. At the consultation, Dr Al Muderis looked at the scans of Ms Slater’s knee that she brought with her. Ms Slater’s evidence was that Dr Al Muderis told her she needed surgery, but that he would not be sure of the extent of the damage until he went in. In cross-examination she accepted that Dr Al Muderis did not want to recommend surgery until he had done further tests (including a CT scan and x-ray). It was Ms Slater’s evidence that Dr Al Muderis did not elaborate on the kind of surgery he would be doing. Ms Slater explained she was told that “he had to go in” and she thought she needed another investigation surgery. She saw Dr Al Muderis again on 1 December 2014, where he looked at her recent CT scan and x-ray. Ms Slater accepted in cross-examination that Dr Al Muderis told her she needed a reconstruction, which required the creation of a ligament, and the tendon on her tibia being cut and realigned. After the consultation, Ms Slater sat down with a nurse who told her “about a knee surgery” and explained some of the risks and complications of the surgery. The surgery (being a right knee arthroscopy, followed by a mini open Medial Patellofemoral Ligament (MPFL) reconstruction with tibial tubercle osteotomy) was conducted on 19 January 2015.
2180 It is appropriate to address three specific topics.
2181 First, Ms Slater’s evidence was that she did not know what the surgery was, until after it was done. Despite being told about a surgery (as noted above), Ms Slater said Dr Al Muderis “never mentioned cutting [her] shin apart”. Her evidence was that she was not made aware that she was required to be on crutches. She said that nobody told her not to put weight on her leg. This came to a head in her first post-surgery consultation on 27 January 2015, when Ms Slater attended without crutches. Dr Al Muderis asked her where her crutches were, to which she replied to the effect of: “I don’t have crutches, I’ve been walking, I thought you’d be happy”. She gave evidence he replied to the effect of: “I broke your shin, get on crutches”. He told her she needed to be on crutches for six weeks. Until then, Ms Slater had been unaware of that, not having been told. Ms Slater maintained in cross-examination that the conversation with Dr Al Muderis about the crutches occurred. She gave evidence that she was concerned about what damage she might have done from walking around for a week without crutches. Dr Al Muderis in cross-examination said he could not recall the conversation about the crutches. He said that it is usually standard practice to be on crutches. I do not accept the applicant’s submission that Ms Slater’s evidence in relation to the crutches is implausible. Although Ms Slater was discharged from the hospital with crutches, I accept her evidence that she attended the consultation without them, and the conversation as she described with Dr Al Muderis ensured. If she had been instructed that she needed to use crutches for a particular time, there is no reason to suppose that she would not have done so. I also note that Ms Slater’s evidence, which I accept, was that in the hospital she went to the bathroom without the aid of crutches. Again, it is unlikely she would have done so, if she had been informed that she was required to use crutches.
2182 Second, an issue arose as to the extent Ms Slater was told of the risks and complications of the procedure. In cross-examination, Ms Slater accepted she received some explanation of the risks and complications by a nurse after the December consultation (as noted above), and by Dr Al Muderis in the anaesthetic bay before surgery. Regardless of what Ms Slater was told before the surgery, it is apparent from the post-surgery consultation, that she had not been told sufficient information to understand the nature of the procedure. That she had not been informed about the extent to which the surgery would impact her, which included the need to use crutches, reflects this. The document which Dr Al Muderis pointed to as providing Ms Slater with information in relation to post-operative care contains general statements relating to knee surgery, noting there is no reference to the use of crutches. As with other patients, Dr Al Muderis also pointed to Ms Slater’s signed consent form to establish he informed her of the risks. I have discussed elsewhere the limitation in that, given the generality of the form. Dr Ruff explained that Dr Al Muderis had a duty to inform Ms Slater of the complications associated with the surgery and arrangements she needed to make in the immediate post-operative period, perhaps for six weeks.
2183 Third, the respondents submitted that Ms Slater’s post-operative experience from her first surgery is recorded in a markedly different way in Dr Al Muderis’ records from that of Dr Paterson. They submitted that this pattern continues in the post-operative consultations following Ms Slater’s second surgery, as evidenced by a comparison between the consultation reports of Dr Al Muderis, Dr Paterson and other practitioners. I accept that submission (although I note there is only one practitioner apart from Dr Paterson, being Dr Salah Daradkeh, whose consultation report is in evidence). A proper consideration of the relevant reports bears that out. Dr Al Muderis’ reports tend to be generally positive, reflect that Ms Slater is progressing well and that he is satisfied with the results (although some note she experienced some stiffness and pain). The reports of Dr Paterson and Dr Daradkeh are relatively proximate to Dr Al Muderis’ reports and tell of a different position that is consistent with Ms Slater’s evidence of the nature and extent of the pain she was suffering.
2184 For example, on 23 July 2015, Dr Paterson recorded Ms Slater as still having significant pain and occasional swelling. On 11 August 2015, Dr Al Muderis recorded that Ms Slater was satisfied with results from her first surgery and only had “occasional pain however nothing significant”. Ms Slater accepted in cross-examination that she told Dr Al Muderis that at the consultation. On 10 September 2015, Dr Paterson recorded Ms Slater was making “slow and gradual progress” with there being a “slow decrease in her pain”, and ongoing pain medication (Gabapentin) was further prescribed.
2185 It is unnecessary to detail Ms Slater’s evidence any further (and I do not rely on it in relation to the topics not addressed).
2186 I accept that Ms Slater was not adequately advised of the risks of the surgery she underwent on 19 January 2015, including the need to be on crutches.
Ms Sharon Jones-Baldwin
2187 Ms Jones-Baldwin was diagnosed with leukaemia in or around April 2018. She received around six months of inpatient treatment and then four months of outpatient chemotherapy. On 23 July 2019, Ms Jones-Baldwin was referred to Dr Al Muderis by her GP for “severe pain to her left knee for a few [weeks] after a twisting injury getting off the bed”. She was 61 years old at the time. Following a consultation with Dr Al Muderis and Dr Stoita on 22 August 2019, the consultation report reflects that the plan was to review Ms Jones-Baldwin again with MRI results, as she had not fully recovered from her leukaemia to warrant surgical intervention. There is no suggestion anything occurred thereafter.
2188 On 8 February 2021, Ms Jones-Baldwin was again referred to Dr Al Muderis by her GP, this time for “persistent pain hip and knee after she picked up a heavy table”. She was 63 years old at this time. Her consultation with Dr Al Muderis was on about 9 February 2021. Her evidence was that she was in significant pain at that time. The referral letter records Ms Jones-Baldwin as having pain in her lower back, knee and the top of her right leg. In cross-examination, Ms Jones-Baldwin said that it was mostly in her lower back and that she did not recall the pain as coming from her hip.
2189 An issue arose in the hearing as to what occurred during that consultation, with Ms Jones-Baldwin giving evidence that neither of the two doctors who first saw her at the clinic, nor Dr Al Muderis, examined her. I note that the consultation report states that the examination Dr Al Muderis conducted involved him rolling her hip gently, but that any movement caused her pain. She was referred by Dr Al Muderis and admitted to Macquarie University Hospital for “pain management” that day. Various tests and scans including an x-ray, bone scan and SPECT-CT scan were conducted on 9 and 10 February 2021. Following a consultation on 11 February 2021 where Dr Al Muderis’ report described her as having “a severely collapsed femoral head on the left side”, he performed a left total hip replacement the following day on 12 February 2021 on “an emergency basis”. There is also a dispute as to what occurred in relation to Ms Jones-Baldwin’s care at Macquarie University Hospital and who instigated her transfer to another hospital. Suffice to say, Ms Jones-Baldwin was discharged on 15 February 2021 to Waratah Private Hospital for rehabilitation. Ms Jones-Baldwin’s evidence was that she did not see Dr Al Muderis after her transfer, by choice, because of her prior experience with Dr Al Muderis, as she described it. Her evidence was that she was then referred to Dr Stoita.
2190 The applicant submitted that Ms Jones-Baldwin was a witness of no credit, and no reliance can be placed on her evidence unless it is corroborated. He submitted that she reacted irrationally, in a hostile and obstinate manner when it was suggested to her that any aspect of her evidence-in-chief was not correct, and she refused to concede even the most basic and anodyne matters. During cross-examination, in addition to suggesting, inter alia, that Ms Jones-Baldwin was lying or that her evidence was false, the applicant accused Ms Jones-Baldwin of being a “lying fantasist”, a description repeated in closing submissions. That description is gratuitously disrespectful. I do not accept it.
2191 I do not propose to resolve the disputes as to all the events.
2192 There are three aspects that I do wish to address briefly.
2193 First, I observe that Ms Jones-Baldwin deposed that she had broken her left hip which is incorrect. X-rays taken on 9 February 2021 make no reference to a hip fracture, and Dr Ruff opined they did not show a fracture. Ms Jones-Baldwin said she was told that by doctors (other than Dr Al Muderis). The respondents submitted that she appeared to be provided incorrect information by Dr Al Muderis or his team. That appears correct. In Dr Al Muderis’ consultation report of 11 February 2021, he does refer, inter alia, to resolving the problem with the fracture by undergoing the hip replacement.
2194 Second, as mentioned briefly above, in his consultation report of 11 February 2021, Dr Al Muderis stated, “[Ms Jones-Baldwin] has a severely collapsed femoral head on the left side”. Dr Ruff disagreed with that conclusion. He described that there is a “huge disconnect between what [Dr Al Muderis] said was wrong with the femoral head and what was known to be wrong with the femoral head”. He explained that Dr Al Muderis’ statement is incorrect for two reasons. He explained that the pre-operative x-rays of her hip were “essentially normal”. That is, it did not show a collapsed femoral head. It appears from the x-ray conducted of Ms Jones-Baldwin’s hips and knees on 9 February 2021, that in relation to her hip joints, the report’s findings record that “[a]lignment is preserved”. As the respondents submitted, the radiologist’s report makes no reference to a hip fracture, referring only to “very early arthritic change”. On this point, Dr Ruff explained that the pathologist who examined the removed femoral head after the surgery, recorded that it was intact. The femoral head was sent to a histopathologist, who concluded that “[t]he shape of the femoral head appears relatively preserved”. When the images from the SPECT-CT were put to Dr Ruff in cross-examination, he disagreed with the applicant’s assertion, explaining that there was “no gross collapse” evident. Although Dr Ruff accepted the proposition that there was evidence of avascular necrosis in Ms Jones-Baldwin’s left hip in the bone scan, he explained that the femoral head still appeared spherical, that it maintained contours and cartilage and that there was no gross collapse. I accept Dr Ruff’s opinion.
2195 In his expert report, Dr Ruff described the notation by Dr Al Muderis in his consultation report (which is referred to above) that she had “a severely collapsed femoral head on the left”, as “exaggerated pathology against the background of the pre-operative x-ray and the findings of the pathologist who reported on the specimen sent for analysis”. Although Dr Ruff accepted that Ms Jones-Baldwin had areas of avascular necrosis which could have produced pain sufficient to justify a hip replacement, he opined in cross-examination, in effect, that Ms Jones-Baldwin may not have been adequately assessed prior to surgery. The applicant submitted that last opinion took him by surprise, and the matter is outside the pleaded case. This aspect was not pleaded, and that opinion did go further than expressed by Dr Ruff in his expert report (and the applicant was not on notice). In the circumstances, I do not propose to resolve the issue, and it is not matter I consider in determining the issues in this case study.
2196 Third, Ms Jones-Baldwin gave evidence that her meetings with Dr Al Muderis were brief, and she felt that she was being “treated with contempt” by him. Whatever the details of her interactions with him were, Dr Al Muderis had no further interactions with her after her discharge. Her evidence was that that was her choice. This does give rise to an inference that whatever happened in their interactions, she was unhappy with him at the time. On Dr Al Muderis’ evidence, there is no occasion for that to be so.
Mr Habibul Rahiman
2197 Mr Rahiman had a right total knee replacement with Dr Al Muderis on 22 March 2021. He was 63 years old at the time. There are some unsatisfactory aspects to his evidence. I note also that Dr Ruff was asked to provide an expert opinion based on Mr Rahiman undergoing a double knee replacement (although he observes a unilateral replacement occurred). In any event, Dr Ruff opined that there was a disconnect between what Mr Rahiman expected and what he experienced but there was no clear evidence that this was based on a breach of a duty of care by Dr Al Muderis. In the circumstances I do not propose to refer to his case study save for one aspect, which is not in dispute.
2198 The consultation report of 1 February 2021 records that Dr Al Muderis provided Mr Rahiman with the information pack from the Australian Orthopaedic Association regarding total knee replacement. As with other orthopaedic patients, this is the pamphlet the patient is provided with information about the surgery, rehabilitation, benefits, complications and the risks. As noted earlier, Dr Ruff’s opinion is that it is insufficient for the purposes of obtaining informed consent. I note that Mr Rahiman consented to the surgery on 1 February 2021, being the same day of his initial consultation with Dr Al Muderis. As I discussed earlier, it is difficult to see how Mr Rahiman would have had an adequate opportunity upon being provided the information pack to consider the information contained therein before making the decision to proceed with the surgery.
Mr Anthony Marlborough
2199 Mr Marlborough had a right total knee replacement and hip replacement with Dr Al Muderis on 15 September 2014 and 30 May 2016, respectively. He would have been 63 years old as at the date of his first surgery. He has a complex medical history. In cross-examination, Mr Marlborough took exception to questions which he disagreed with, such that he, in practical terms, was refusing to participate in the process and became a very agitated witness. He was combative. His evidence was unsatisfactory.
2200 The applicant submitted that the Court should put Mr Marlborough’s evidence to one side unless it is, inter alia, corroborated by a contemporaneous document. There are two aspects relating to his case study that I propose to address, both of which do not rely on his evidence.
2201 First, there is no evidence that Mr Marlborough was properly informed about the risks in relation to his knee replacement. None are referred to in the consultation reports dated 1 April 2014 and 15 July 2014, and Dr Al Muderis does not give evidence of having done so. The only evidence the applicant pointed to was a signed consent form dated 15 July 2014 for a bilateral total knee replacement which included an acknowledgement that Mr Marlborough was advised of various risks and the nature of the procedure. I note that the risks in the consent form are the pro forma general risks of surgery and not those specific to a knee replacement. Further, there is reference in Dr Al Muderis’ operation report that the patient was fully informed and aware of all risks and complications of the surgery. However, as Dr Ruff opined, this template document is retrospective and it does not, for instance, include for total knee replacements, the development of a fixed flexion deformity.
2202 I note also that in the second consultation report dated 15 July 2014, Dr Al Muderis states the following:
If he has exhausted all conservative measures I would be happy to offer him knee replacement and would replace the left knee first as this is the most painful for him. We could if he wishes, and if he is medically suitable, replace both knees at the same time however I will leave the decision to Anthony and his medical condition as to whether he is fit enough for bilateral knee replacement.
2203 Despite that position and before any medical assessments were conducted, there is a signed consent form in evidence dated 15 July 2014 for a “bilateral total knee replacement” surgery (noting he underwent a right total knee replacement on 15 September). Further, the consent form lists Mr Marlborough’s admission date for the procedure as 15 September 2014 and states that the material or specific risks to him are “[a]s per the AOA guidelines”. However, unlike the consultation reports for Mr Marlborough’s hip replacement, which I discuss immediately below, these consultation reports do not record that he was provided with the Australian Orthopaedic information pack. In any case, as I outline below, the provision of that document alone would not have been adequate for the purpose of informed consent.
2204 In relation to his hip surgery, it was eleven months after his knee replacement that Dr Al Muderis recorded that a hip replacement was necessary. That surgery did not occur for some time because of unrelated medical issues. In any event, for both the consultations concerning his hip on 11 August 2015 and 3 May 2016, the reports recorded that an information pack from the Australian Orthopaedic Association regarding hip replacements was provided. In cross-examination, Dr Al Muderis accepted he invited Mr Marlborough to read the pack and come to him with any questions. There is no other evidence that he was provided any other information as to the risks of the procedure by Dr Al Muderis. As noted elsewhere, Dr Ruff opined that an information pack is inadequate to fulfil the responsibility of ensuring there is informed consent. Further, I note the two signed consent forms for a right total hip replacement correspond with the dates of the consultations concerning Mr Marlborough’s hip. As discussed elsewhere, it is difficult to see how Mr Marlborough would have had an adequate opportunity upon being provided with the information pack to consider the information therein and ask questions before making a decision to consent to the surgery on the same day.
2205 Second, in relation to Mr Marlborough’s knee replacement, the first consultation report dated 1 April 2014 (and Dr Al Muderis’ affidavit) only refers to him having considered an x-ray organised by Mr Marlborough’s referring doctor and an x-ray completed on the day of the consultation. There is no record of a physical examination of, inter alia, his hip. The consultation report of 15 July 2014 also contains no suggestion that Dr Al Muderis physically examined Mr Marlborough’s hips. Dr Ruff opined that there was no recorded examination of the right knee prior to the total knee replacement. In cross-examination, Dr Al Muderis accepted that there was no reference to a physical examination in his consultation report and that he should have commented upon the effusion in the joint and recorded its range of motion, although his evidence was that he believed he conducted one.
2206 Dr Ruff opined that he could find no evidence of an examination in circumstances where such an examination is important, as it may be the cause of the knee pain. In cross-examination, Dr Ruff opined as follows:
So he’s a type 1 diabetic for 30 years. There’s no records that his pulses are taken. There’s no record they’ve examined behind the knee to see if he has got a popliteal aneurysm. All these things are fundamental. I can’t find evidence that he had his hip examined, and one of the great faults is to fail – fail to examine the hip when it’s known that probably five or 10 percent of people with hip arthritis present mainly with knee pain, so you’ve got to do an examination; it’s just so simple. You lift it up, internally rotate and abduct it. If it’s stiff or painful, you become concerned that the arthritis is coming from the hip. So this man presented with bilateral knee pain, worse on the left than the right; multiple comorbidities. I couldn’t find, Counsel – and I looked for evidence that he had had his pulses looked at, that he had had a neurological examination to exclude some form of sciatica causing his leg pain, when he had had it in the past, or that there was an examination of his hip … to fail to do those examinations, feel the pulses in this man – well, in any person, but in a – a type 1 diabetic for 30 years and someone that has got sciatica … He’s far from a well man. He needs a proper and a thorough physical examination.
2207 The only record relied on by Dr Al Muderis as evidence that any examination was conducted was an application to the Department of Veterans’ Affairs in support of funding for Mr Marlborough’s knee replacement, faxed 13 days after the consultation, containing mainly check boxes and plainly prepared for the purpose of receiving funding for surgery. It was no substitute for a consultation record.
2208 I note that only nine months after the right knee operation, Mr Marlborough was diagnosed with serious arthritis of his right hip.
2209 I note that whether a physical hip examination was undertaken is the same issue that arises in the case study of Ms Hutton. As in Ms Hutton’s case, there is no reference in the consultation reports for Mr Marlborough that a consultation was done. Again, the failure to record an examination means there is no documentary evidence supporting Dr Al Muderis saying he believed he conducted an examination of the hip. The implication from Dr Ruff’s evidence is that there should be a medical record of such an examination. I agree, given the purpose of medical records. Given the absence of a record where it would be expected that there be one, I am not persuaded a hip examination occurred.
PART 7 — SECTION 26: FURTHER CONSIDERATION – IMPUTATIONS
Section 1 — The defamatory stings
2210 Returning to the defamatory stings described above. It is to be recalled that it has not been established that the imputations in the Sneak Peek are carried, and therefore this defence is not required to be considered for that publication. That said, as explained above, the respondents can rely on the imputations not conveyed (being the Disputed Imputations conveyed in the sense contended for by the respondents) as contextual imputations to establish their defence. In practical terms, those imputations do not really add anything to the strength of the respondents’ case. Each of those imputations also convey one of the defamatory stings already identified and they are therefore already encompassed in my consideration below. As earlier discussed, there is considerable repetition in the pleaded imputations. I return to this below.
2211 Also as explained earlier, the respondents made submissions directed to the evidence they said established the stings. To that end, they also, in Aide Memoire 6 identified which patient case studies were said to relate to the each of the imputations. I pause to note that Aide Memorie 6 reflects that for some imputations, some of the witnesses identified as relied on to prove that imputation are not referred to in the respondents’ pleading on that imputation. Conversely, some witnesses are no longer relied on. I mention this as the applicant complained about the former during oral closing submissions. However, given the imputations overlap with the common stings conveyed (see Part 5, Section 2) and where the evidence of a patient case study identified in the pleadings as relating to one imputation is also plainly relevant to other like imputations conveying the same sting, there can be no prejudice. None has properly been identified.
2212 There are 22 patient case studies in relation to osseointegration patients spanning from 2013 to shortly before the Publications (with some patients still consulting Dr Al Muderis then). In addition, there are four principal case studies in relation to the orthopaedic patients, with the others being more limited (where I have considered discrete aspects of their experiences with Dr Al Muderis). The orthopaedic cases span from 2011 to 2021 (the four principal cases from 2011 to 2020). As previously explained, the evidence in the individual patient case studies is not to be considered in isolation. As will have been apparent from the consideration of each case study, there are similarities between what the patients said (which I have accepted), and what had occurred. As will also have been apparent is that, to a large degree, my factual findings are supported by documentary and/or other evidence.
2213 Further, evidence of patients’ experiences with Dr Al Muderis covering a span of years (as opposed to only “recent patients” being considered as the applicant submitted), is also relevant as it is informative as to Dr Al Muderis’ state of mind, knowledge and conduct on various topics. This includes whether, if Dr Al Muderis was aware of issues with his patients and practice, his practices changed overtime. This is in a context where, as explained above, the applicant relied heavily on what he says is his standard practice. It is also in a context where, as part of his practice (e.g. in consultation reports) and from his evidence in these proceedings, Dr Al Muderis relies on the number of surgeries he has conducted to support his evidence and expertise.
2214 In considering the stings below, I refer to factual findings I have already made. It is unnecessary to repeat all the findings, evidence, and details described above. This section is to be read in the context of the judgment as a whole and the fact finding already undertaken herein. Plainly this section is not exhaustive.
2215 Some of the imputations fall within multiple stings and will be addressed separately. Some imputations are in general terms while others, which may convey the same sting, refer to an identified patient. Annexure I identifies which conveyed imputations fall within each sting.
2216 The applicant submitted that even if the patients’ experiences in respect to risks and complications, or aftercare were established that could not establish the general imputations, because they are the personal experiences of a “relatively tiny” group of patients. That is in the context of the applicant’s submission as to the number of surgeries he has performed. I take this into account in considering those imputations (and the relevant stings). The applicant also repeatedly submitted that as an imputation is in the present tense, earlier patients of the applicant cannot establish the substantial truth of it. I have addressed this submission earlier: Part 5, Section 3. The flaws in that approach are discussed and as there explained, whether the substantial truth of any imputation has been established will be assessed by considering the evidence relevant to that imputation.
2217 It is important to recall the imputations conveyed by the Publications are to be understood and considered in that context. As discussed above, the Publications convey that for a cohort of patients, Dr Al Muderis similarly did or failed to do certain things (e.g. failed to explain or downplayed the risks and complications, failed to provide adequate aftercare). What is conveyed is that there is a cohort of patients negatively impacted by Dr Al Muderis’ services and that the conduct occurred with sufficient frequency such that the patients’ experiences are more than a coincidence. The patients are not, as the respondents described, outliers, or anomalies. That is in a context where the Publications convey that the picture portrayed by Dr Al Muderis about his services, is not the only one. It is also conveyed that there are many patients who have had positive experiences. In other words, the Publications convey there is another side to the story (see Generalisation, Part 5, Section 4). Terms the applicant uses in the pleaded general imputations (e.g. routinely and habitually, which I note are not used in the Publications) are to be understood in that light. Not all the general imputations use such language. That the evidence led by the respondents demonstrates a broader picture than that in the Publications, does not alter that.
2218 In that context, it will have been apparent that although, as the respondents describe, there is reference to a cohort of patients, the evidence is not so confined. For example, apart from evidence directed to the patient case studies, the respondents also relied on the evidence of Mr Grant, Ms Stewart and Mr Hernandez, and other general documentary evidence (e.g. brochures and Dr Al Muderis’ websites), which was of a broader compass. Noting also there is evidence from Dr Al Muderis himself, and documents from his practice (e.g. those in relation to the international patients and consultation reports) which support the respondents’ case in establishing the substantial truth of the stings.
2219 It is also helpful to recall that it is the sting of the defamatory imputation which the respondents must establish as substantially true. That does not require them to prove the truth of every detail of the words of the imputation, the defence is focused on meeting the sting or gravamen of the imputation: Roberts-Smith (Appeal) at [544]. One is not considering the imputation in a technical or meticulous sense: Part 5, Section 1
Sting 1 — Improper sales tactics
2220 Regarding the Articles, this sting captures Imputation [16.5]. Regarding the Grieve Video, this sting captures Imputation [28.5].
2221 The respondents put their case on this sting, as follows:
The sales tactics engaged in by Dr Al Muderis are many and varied, ranging from ensuring patients who were investigating osseointegration surgery spoke with those who had already had it, seemingly with good results, to engaging patients whose role it was actively to advocate for the surgery.
2222 The respondents identified evidence in relation to, inter alia, the following topics which are said to be examples of such tactics (many of which have been discussed at length elsewhere in this judgment): prepayment from overseas patients required before coming to Australia, prospective patients meeting other patients, the role of Mr Hernandez and the payment of commissions, the role of Mr Grant as a patient advocate, discount on fees, fundraising, socialising with patients, pressure by Dr Al Muderis to proceed with surgery and the promotion of services by other patients.
2223 This sting must be viewed in its proper context; it relates to a patient agreeing to undergo an expensive and highly invasive elective surgery, with life-long implications (including, on Dr Al Muderis’ evidence, a connection with him for life) which, even on Dr Al Muderis’ evidence, is in its infancy. As discussed in relation to sting 6 below, this is a business, with osseointegration as a surgery and Dr Al Muderis being marketed in a manner which promotes the surgery, and him, in a very positive light. Some of the marketing material presents a “rosy” picture and in some important respects, is misleading. The marketing strategically attracts patients.
2224 Turning to the conduct identified by the respondents.
2225 First, the circumstances of the United States practice are described elsewhere, and my findings are clear: see Part 6, Section 4. In particular, the impact of requiring prepayment from patients for the surgery before (even on Dr Al Muderis’ evidence) having been informed of the risks and complications of the surgery is relevant. The role of Mr Hernandez in promoting the surgery in the United States and the manner it was undertaken, including receiving commissions, is discussed elsewhere (see Mr Hernandez’s section in Part 5, Section 6). It is also to be recalled that his role was to be kept confidential, in that prospective patients were to be kept unaware of Mr Hernandez’s financial benefit.
2226 Second, Dr Al Muderis’ practice of using his existing patients to talk to prospective patients is problematic. He repeatedly said those patients spoke of “the good, the bad, and the ugly”. The consultation reports for osseointegration patients contain pro forma statements to the effect that the patient individually met with other patients who were at various post-operative stages and were able to share their experience and discuss “the pros and cons of such a procedure”. None of the patients who gave evidence about talking to others in the waiting room described that as their experience. For example, Ms Todd described the patients were praising him and all saying they were very happy with the procedure, it was the best thing they had ever done, the surgery all went well and that no one had a bad word to say about Dr Al Muderis. Her evidence was that it seemed strange to her that these patients were so openly discussing their experiences in a doctor’s waiting room. That is a fair observation. Ms McIntyre’s evidence of her experience was to the same effect, in that everyone in the waiting room said how wonderful Dr Al Muderis was. She was seated next to women with similar interests, education and age to her, in circumstances where both women spoke very positively. Mr Warland’s evidence was that the clinic manager did bring an above-knee amputee who was previously a below-knee amputee into the consultation to speak with him, but that was because of Mr Warland’s apparent relaxed attitude to the procedure (which he said the psychologist was concerned about). But Mr Warland’s evidence was that the patient told him the resultant amputation was his fault, for not following Dr Al Muderis’ instructions. It appears that despite the complication, the other amputee was a happy or positive patient. As referred to elsewhere, the purpose of involving the former below-knee amputee appears to have been to have Mr Warland appreciate that, if he proceeds with osseointegration, complications can occur in circumstances where patients fail to adhere to Dr Al Muderis’ advice. It shows a preparedness for Dr Al Muderis’ staff to have an existing patient speak to a prospective patient, for a purpose.
2227 When Mr Smith first met Dr Al Muderis and Ms Roberts in a hotel in Brisbane, another amputee was present. Mr Smith did not know why he was at the consultation, but the amputee and his wife had nothing but positive things to say. When Ms Ulrich first met Dr Al Muderis in the United States, sitting at the table was a patient who had had osseointegration. When Ms Todd first saw Dr Al Muderis at a conference in Brisbane, there was a patient speaking at the session. Similarly, Mr Mailler’s first introduction to the surgery was a talk by Dr Al Muderis where a former patient spoke (who I also note was the same patient who spoke to Mr Grant), and even though he had described some issues he experienced, the message presented to the audience was that having the surgery was worth it. Mr Mailler’s observation was that the patient “was a very strong advocate for osseointegration and for Dr Al Muderis”. In other words, it was a positive message. This illustrates that patients can be used to promote the surgery (and the surgeon) as worthwhile even if they had some issues (which can also be seen as downplaying the risks). In doing so, it can form part of a prospective patient’s consideration of whether they choose to undergo the (elective) surgery.
2228 Further, Dr Al Muderis utilised the services of patient advocates, for example, Mr Grant. His role was to promote osseointegration with Dr Al Muderis, a role which he was asked to do, because he was a success (with little complications). He promoted the surgery, with Dr Al Muderis as his surgeon, with the aim being to get people to have the surgery. He was asked to attend the clinic at certain times, and to speak to certain patients (and prospective patients) at Dr Al Muderis’ rooms, at the hospital, over the phone and at his gym. It is not surprising that the atmosphere in the clinic waiting room was a positive one. I note that Mr Grant himself, apparently had spoken to a patient before he decided to undertake the surgery, as recorded in the brochure “Osseointegration, The Australian Experience”, which details Mr Grant’s case, and its success. Mr Grant travelled with Dr Al Muderis when he presented to others domestically and internationally, where he participated in promoting the surgery.
2229 This is also in a context where Ms Stewart’s evidence was that she was instructed to ensure Mr Grant attended certain clinics, and she was to organise the clinic so that it looked busy.
2230 Third, some patients are asked to promote the surgery. For example, Ms Schaeffer was asked at an amputee conference in the United States, to wear a T-shirt advertising Osseointegration International while staffing a booth, and as Mr Bruha said, they were required to wear shorts so others could see their legs, which in itself was a form of marketing for the procedure. For all intents and purposes, this was a promotional booth for Dr Al Muderis and his surgery. Ms Ulrich was also asked to attend a conference in this capacity to model the implants. The use of Mr Grant, a patient, in his role as a patient advocate also illustrates this.
2231 Further, Dr Al Muderis had reached out to Ms Schaeffer requesting her to put a favourable comment about him on Facebook, in a context where Dr Al Muderis made the request because he was aware, at that time, that some patients had posted comments on Facebook regarding his failure to communicate with them: see Ms Schaeffer in Part 6, Section 4.
2232 Fourth, his practice of fee discounting and prepayment. It is trite to observe, as previously discussed, that if surgery is paid for in advance, it involves a significant commitment (occurring principally in this case with international patients). It may impact on the concerns prospective patients may raise or the likelihood of them changing their mind. As the respondents submitted, this type of sales tactic has the tendency to lock a patient into a procedure, making it less likely that they will back out, or feel they can back out, if they later have second thoughts. This is especially so for patients looking for a solution to their issues (noting patients were generally vulnerable at the time they consulted Dr Al Muderis: see Part 6, Section 1).
2233 Mr Ladouceur gave evidence that at his meeting with Dr Al Muderis in New York, he was offered a discounted price of US$50,000. It will also be recalled that Mr Wynne requested a discount for financial reasons: see Part 6 Section 4 above. Ms Roberts replied:
I discussed it with Munjed who is compassionate and does not want finances to delay surgery so he is willing to help by the following: (taking into consideration that the only fee that Munjed can control is his own surgical fees)
[having detailed the costs including for the implant, Ms Roberts continued]
- The reason being - because the implant company is not as compassionate and cannot lower the cost of the implant price.
2234 In this instance, the discount offered also promoted Dr Al Muderis as compassionate towards Mr Wynne, compared to the implant company which is not. The email is designed to promote to the patient that Dr Al Muderis cares about him. However, this is in 2018, where Dr Al Muderis used his own implant in the surgery. He owns the company that manufactures and supplies them. I note that in the Articles, Ms Asch-Martin is recorded as saying how grateful she was for Dr Al Muderis giving her a discount.
2235 Discounting incentives were not only offered to international patients. For example, Mr Smith gave evidence he was told at his first meeting with Dr Al Muderis that he needed to pay $10,000 to secure his place for surgery. When he contacted Dr Al Muderis’ rooms, he was told by Ms Roberts in writing that as Mr Smith was a veteran, Dr Al Muderis “would honour his discounted rate at $10,000” out of pocket, but that “[t]his needs to remain confidential please”. This was only part of the payment, with Mr Smith believing that outstanding costs were covered by his private health insurance. However, as discussed elsewhere, a patient being told they were getting some special treatment (as evidenced by the tenor of the communication and the need for confidentiality), particularly in a context where many of these patients gave evidence of their limited financial circumstances, alters the doctor-patient relationship. A patient may feel beholden to the doctor.
2236 As those examples also illustrate, these discounts were offered before (on the applicant’s case) the patient was assessed as suitable for the surgery, and before Dr Al Muderis had explained the risks and complications to them.
2237 Fifth, as already referred to, and explained in more detail below, fundraising was encouraged by Dr Al Muderis and his staff to enable patients to have the money to pay for this elective surgery. The clinic was actively involved in advising them to do so: see Fundraising in Part 6, Section 1 above. It will be recalled that in an email referred to earlier, Dr Al Muderis wrote in respect to a prospective patient, “[w]e may need to start a discussion with the patient to teach him how to do fund raising for his surgery”. This conduct related to both international and domestic patients (e.g. Ms Ulrich and Ms McIntyre). To suggest, as the applicant does, that there is obviously nothing unethical about a surgeon in private practice charging patients for surgery or for patients pursuing alternative means of funding surgery, is misconceived. The surgeon is entitled to be compensated for his or her exercise of skill and expertise in performing a surgery, not to mention covering expenses the surgeon will incur, such as paying staff. However, that is to miss the point. This is elective surgery, which Dr Al Muderis promotes. These are often vulnerable patients (physically, psychologically and financially). To suggest how these patients might obtain the money to pay him for the surgery, with the potential to put them in a financially vulnerable or even more financially vulnerable position to enable the surgery to occur, puts pressure on a patient (in many ways). In the case of the patients from the United States, on the applicant’s case, this is before the patient has been assessed as suitable.
2238 Sixth, if a patient did not sign up to the surgery, there would be an attempt to contact the patient again. Ms McIntrye provided a clear example, which is consistent with the evidence of Ms Stewart (her role being described above in Part 5, Section 6). Within four days of her consultation with Dr Al Muderis, where Ms McIntyre had communicated she was not prepared to consent to the surgery on the spot and she wanted to consult others (and knowing there was another surgeon involved), Ms Roberts attempted to contact her, first by phone and then by email a few days after that. It is to be inferred that this was to get that prospective patient to agree to the surgery.
2239 Seventh, Dr Al Muderis socialised with patients prior to surgery. For example, Ms Schaeffer gave evidence that she attended a dinner with other overseas patients following her arrival in Australia, but before she had a consultation with Dr Al Muderis. That is, Dr Al Muderis invited his patients to dinner. Dr Geffen gave evidence in that context, that he had:
… reservations about someone paying you large sums of money and then going out, and you organising the event and then proceeding to operate on them a few days later.
2240 Mr Grant also gave evidence that he was sometimes asked to help entertain someone at dinner as part of his patient advocate responsibilities. Dr Al Muderis took issue with Dr Geffen’s evidence and disagreed it was inappropriate for him to have dinner with a patient in Ms Schaeffer’s circumstances. However, again, such conduct prior to an operation creates a dynamic which alters the doctor-patient relationship.
2241 In a slightly different context, but nonetheless not dissimilar, the respondents also alleged that Mr Wynne attended such a dinner in New Orleans as evidence that inappropriate pressure is put on a prospective patient to undergo the surgery. In Mr Wynne’s case, he asked to go along with Mr Hernandez to the dinner. I accept that it was at his instigation and not an intentional act by Dr Al Muderis as a sales tactic. That said, pressure can be placed on a person by the circumstances nonetheless having that effect. In these circumstances, the person Mr Wynne contacted to ask about going out, was Mr Hernandez, being the person who was contracted to promote Dr Al Muderis and his surgery (for which he was paid a commission). Regardless, Mr Wynne did end up at dinner with Dr Al Muderis, in circumstances where if Mr Wynne decided to proceed with the surgery, Dr Al Muderis stood to gain a financial benefit. As is evident in an email Mr Wynne later sent to Ms Roberts, the dinner did have some influence on Mr Wynne’s decision to proceed with the surgery: “Honestly, what sold me on this was, the evening after meeting with Munjed, I went out to dinner with Munjed & a couple of his previous patients”. Dr Geffen further opined that socialising of this kind is “unusual and fraught with possible complications”. Dr Al Muderis disagreed, giving evidence that this is a standard practice for people who are participating in a conference, and that he did not see anything wrong with that.
2242 The possible complications of socialising, as illustrated above, can be readily accepted. It does not need an expert to opine on it.
2243 This raises a more fundamental issue. Dr Al Muderis portrays to prospective osseointegration patients that they will be family. He acts in a way that creates the impression with patients (and prospective patients) that he is a friend. Indeed, many patients gave evidence to this effect (e.g. Mr Urquhart and Ms Mattiske). Taking patients to dinner or on a cruise on the harbour (as was the case with Ms Mattiske) fosters this impression. It is not demonstrative of the role of a doctor who can give advice objectively to a patient. Rather, it imposes pressure on patients to be complaisant even if they have concerns or complaints. This may be because they believe, as their friend, Dr Al Muderis can be trusted, or because of a dependence on him for future help (especially as one of the few surgeons capable of helping given the unique nature of the surgery, which was particularly so for the international patients), they accept without complaint events that occur. This can lead, as I accept occurred in relation to some patients, to an effort on their part to be seen as friendly or positive towards him personally or on social media: see, for example, Ms Ulrich.
2244 Finally, as will be seen from the evidence of the conduct described, such tactics were employed in some circumstances before a patient had been assessed as suitable for the surgery. If they had been assessed, as in Ms McIntrye’s case, they generally received a consultation report which referred to the surgery being in Dr Al Muderis’ opinion, “necessary”. It will be recalled that Dr Doshi accepted in cross-examination, it would be wrong to tell a patient that it is necessary to have osseointegration surgery (Dr O’Carrigan also accepted the procedure is not necessary). That report to Ms McIntyre, as described above, contained errors. It promoted the need to have surgery in a timely manner (being an elective surgery), putting pressure on Ms McIntyre. She was also told, inappropriately, that if she did not proceed with the operation quickly, her bone density would decrease because she was not weight-bearing. Not surprisingly, Ms McIntrye felt pressured by her experience with Dr Al Muderis, and his clinic.
2245 Although in Ms McIntyre’s case she did not proceed with the surgery, conduct of this nature described operate as sales tactics, and impact on the issue of informed consent.
2246 Conduct of this nature (of which the above are examples) does put pressure on the prospective patient. That is so irrespective of whether that was the intent in relation to some, or all, of the practices. That said, it is plain most of the practices are designed to encourage the prospective patient to agree to have the surgery (or in the case of prepayment, as described below, to ensure Dr Al Muderis’ payment). This is a business.
2247 The applicant’s submission which referred to the evidence of various doctors who were present at consultations with Dr Al Muderis (Drs Doshi, O’Carrigan, Stoita, Alttahir, Haidary and Basten), other colleagues (Mr Laux and Ms Dean), and others who work in the clinic (Ms Moti and Ms Harris) to contend there were no sales pressure or tactics, is simplistic. The submission does not address or otherwise grapple with the conduct described above. The conduct described above is intentional in that the acts are deliberately undertaken. Once the underlying conduct is accepted (and much cannot realistically be disputed), the potential impact on prospective patients is obvious. Given the witnesses the applicant referred to (associated with the clinic), some of this conduct may not even have been known to them. Some is conduct outside the clinic. The circumstances in which these events occur may also not be known (an obvious example is Dr Doshi’s evidence that it would be unethical to require a patient to pay for surgery before they had been assessed as being suitable for it). Further, to suggest as the applicant did, that a patient can cancel at any time, or that prospective patients are told to speak to other patients as illustrations that there is no pressure, fails to consider the context in which that is occurring. For example, that a patient can cancel at any time, ignores that if they have prepaid or otherwise already committed to the surgery, they are less likely to do so or turn their mind to it. That said, such conduct is not referred to in the affidavits of the applicant’s witnesses. The conduct pleaded in the Amended Defence, is largely not addressed in these witnesses’ evidence on this topic. Rather, the approach by some was to make the general assertion that Dr Al Muderis has never pressured anyone to undergo surgery. That does not assist. It is the effect of this conduct on prospective patients (given their circumstances) which creates the pressure. It is not explicit. It could influence a patient when deciding whether to undergo the surgery with Dr Al Muderis including where they otherwise might have still had some reservations or might not have decided to proceed with the surgery as quickly. It is that underlying conduct which is generally not addressed (and which one would have been expected to be). Their generalised statements cannot carry much weight.
2248 I am satisfied that the conduct employed by Dr Al Muderis’ practice, as described above, given the circumstances, imposes inappropriate pressure on prospective patients to proceed with the osseointegration surgery, to be performed by him. As mentioned previously, the above conduct is not to be considered in isolation, but rather in the context in which it occurs, which is reflected in the discussion about other stings (e.g. in the context of Dr Al Muderis promoting his business, and where there are misleading statements in material available to patients, or downplaying of risks and complications, and poor patient selection). Also relevant is the consideration of sting 6 below which brings this conduct together with some of the conduct discussed in other stings.
2249 I am satisfied the respondents have established that the sting that improper sales tactics were employed by Dr Al Muderis’ practice, is substantially true.
2250 That is what is conveyed by Imputations [16.5], and [28.5] which are general imputations, and accordingly, I am satisfied that those imputations are substantially true.
Sting 2 — Misleading osseointegration patients (false promises, downplaying risks and complications)
2251 In the Broadcast, this sting captures Imputations [13.1] (which conveys more than 1 sting and is addressed below), [13.5] (Mr Urquhart), [13.9] (Mr Smith), [13.10] (Mr Smith), [13.16] (Ms Eang, Mr Pril), [13.25] (Mr Bruha) and [13.30]. In the Articles, it captures [16.6] (Mr Urquhart and Mr Smith), [16.21] (Mr Smith) and [16.26]. In the Grieve Video, it captures [28.1] (which conveys more than 1 sting and is addressed below).
2252 The assessment by a patient of any information provided to them about the surgery, including as to the risks and complications of a surgery, is in the context of the surgery to be conducted.
2253 The respondents submitted that in promoting himself and his surgical practices, Dr Al Muderis engages in seriously misleading conduct. They submitted:
Particularly in relation to osseointegration, he promises a better life after the surgery: pain free, low risk of infection, running, increased mobility, improved quality of life, limited discharge. He promises always to be available to his patients: their surgeon for life. He provides a mobile phone number and email address: an on-call doctor for any issues.
2254 Emphasising the vulnerability of his patients (and prospective patients), they submitted that:
They go to seek out solutions from the doctor with the glittering reputation and who has boundless confidence.
2255 I have already addressed above the respondents’ allegation that various brochures and websites associated with or relating to Dr Al Muderis contain misleading information, and that certain patients were misled on specific topics, or false promises given (see e.g. Brochures – misleading statements, Part 6, Section 1 above, and the case studies of Mr Bruha, Mr Smith and Mr Haskett).
2256 As referred to earlier, the applicant submitted that it is inherently very implausible that a surgeon in his position routinely tells patients nothing or almost nothing about material risks of major surgery, even more so “when one considers that he was accompanied during osseointegration consultations by other numerous medical professionals, including other orthopaedic surgeons”; see Standard practice in Part 6, Section 1 above. I am conscious of this submission in assessing the evidence. That said, there is a simplicity to the submission. It is pitched at a high level, in circumstances where the evidence in respect to some patients is focused on what they say they were not told. It does not address the allegation of Dr Al Muderis downplaying the risks and complications. The submission also relies on, in part, the assertion of other medical professionals being present at consultations, including orthopaedic surgeons, which does not recognise the evidence that that is not always the case (e.g. for the international patients and some of the interstate patients). It also considers the topic in isolation of other evidence as to Dr Al Muderis’ conduct (or the nature of his practice).
Downplaying risks and complications
2257 The applicant submitted that the very generalised way in which the respondents have (for the most part) put this allegation affects how the Court would go about considering whether it is justified. He submitted that in the limited instances where the respondents have identified specific risks of which the patient was allegedly not warned, the question is whether the patient was (or ought to have been) informed of those risks. In the cases where the respondents “baldly assert that the patient was told nothing or very little about risks”, the applicant submitted the Court need not descend to that level of detail. He submitted in that instance, an allegation in such general terms is refuted if the Court is satisfied that some discussion of risks and complications did occur. That last submission does not logically follow from a pleading of that nature. It is difficult to understand how a conclusion that some risks were discussed refutes the allegation that the discussion was inadequate (particularly if the conclusion is that there were certain risks not discussed). Moreover, the risks the patients are concerned about are not the general risks of undergoing a surgery (with which they no doubt were familiar with) but risks and complications from a surgery of a specific nature (i.e. specific to osseointegration or specific to another orthopaedic procedure).
2258 A common theme in the evidence from the patients was that they were not informed (or adequately informed) of the risks and complications associated with osseointegration surgery, or that those risks and complications were downplayed. For some, it is alleged specific risks were not referred to (see e.g. Ms Mattiske, Mr Urquhart and Mr Wynne). For others, they recall some risks, such as infection being discussed, but being told, in effect, it is not a problem as it could easily be addressed with antibiotics (i.e. although it was a risk, the impression created, was that it was not one of concern) (see e.g. Ms Todd, Mr Warland, Mr Smith and Mr Mortimer).
2259 It is beyond dispute that surgeons are required to obtain informed consent from their patients before performing surgery. That necessarily involves a patient being informed, in terms they can understand, of the proposed procedure and the available alternatives, the risks involved and potential complications. As already discussed, the patients’ vulnerability and the nature of this highly invasive procedure highlights the importance of and need for patients to not only be warned about the risks and complications, but in a manner that enables them to fully appreciate the potential consequences. These are people looking for a solution to issues they have. They may well have already decided that they want the surgery before attending the clinic. Leaving aside the trauma a patient may experience if there are complications from having the surgery, it is not as simple as being able to revert to a socket prosthesis. It may be, as in the cases of Mr Mortimer and Mr Haskett, that their limb is shorter which brings with it issues as to its functionality in the future.
2260 As explained elsewhere, red flags can be missed or discounted in a desire to attain what is perceived as beneficial (e.g. Ms McIntyre and Mr Wynne). There is no urgency or (contrary to some of Dr Al Muderis’ consultation reports in evidence) is it “necessary” to undergo this surgery. Osseointegration is an elective surgery. Patients need to be in a position and given time to consider their options and any risks and complications they are told it entails. Bearing in mind also that many of the patients have mental health issues (e.g. PTSD), and other medical issues, which are significant factors for providing adequate information about the procedure.
2261 This sting, like the others, is not to be considered in isolation. My conclusions in relation to other topics are relevant to the question of the assessment of the evidence. For example, in so far as the applicant relies on the evidence of his standard practice to suggest that risks were discussed, the issues with that are described above. This sting is also considered in the context of my findings that aspects of the brochures and websites used by his practice downplayed the risks and complications of osseointegration surgery. These are public-facing sources, that are a point of information for the patients (on the applicant’s case patients are directed to Dr Al Muderis’ website). Further, this sting is considered in a context where there was material used to promote the surgery (including the website); where existing patients were encouraged to speak to prospective patients, whether at conferences, consultations or otherwise (who, on the evidence, extolled the virtues of the surgery and the surgeon (see e.g. Mr Grant, Mr Hernandez, Ms Schaeffer, Mr Bruha, Ms Todd, Mr Warland and Mr Mailler)); where a patient advocate (Mr Grant) was asked to speak to interested patients on the basis that he was doing “really well”; and, where the terms of the consultation reports were at times inaccurate.
2262 As discussed above, the consultation reports (for those in evidence) typically refer to: the complication rate being “extremely low”; the procedure as “very standard”; the patient understanding the risk of infection, but is at a “relatively low risk”; that “it has been shown clearly that functional capacity of all our cases has increased dramatically with high statistical significance”; the cost effectiveness has been high with patients returning to the workforce after several years of unemployment; that he would expect to see an improvement in their mobility and quality of life; and that Dr Al Muderis considers the surgery “necessary”. A patient may assess the risks and complications differently, if they are led to believe the surgery is very standard and necessary. It will be recalled that the reports are sent to the patients.
2263 The reports generally portrayed a positive picture and reflected a promise of a better life after surgery: see Consultation reports, Part 6, Section 1. It can be inferred from the tenor of a patient’s consultation report that a positive picture of surgery is presented in the consultation to the patient. In doing so, the reports in evidence generally downplay the risks and accentuate the benefits. This is consistent with and supports the evidence of patients about what occurred, who said, in effect, that in those consultations, the risks and complications that were explained were downplayed. It is to be recalled this information is presented to a patient in a context where Dr Al Muderis promises to be available to them, providing his mobile telephone number to contact him and says they will be “family”.
2264 Therefore, in assessing the evidence of whether risks and circumstances were explained, or adequately so, it is to be assessed in a context where the positives of the surgery are heavily promoted by Dr Al Muderis. The public facing materials provided to patients painted a rosy picture and I have found them to have contained misleading statements and omissions about the surgery: see Brochures – misleading statements, Part 6, Section 1 (the material on the websites in evidence was accessible at the time of the Publications). It will also be recalled that this is also in a context where, as Ms Mattiske said, she was promised “I can make you walk again, Rowena”. That such promises were made is consistent with the evidence Dr Al Muderis gave in relation to Ms Çalan where in cross-examination he repeatedly stated that he promised her mobility and allowing her to walk (and “what I promised I delivered”). I note also that he spoke in such positive terms is consistent with his statements in the Foreign Correspondent program in relation to Ms Nasser (as shown in the Broadcast: “If we do osseointegration for her she will walk, for sure”). Any assessment of the risks and complications of the surgery the patient is told, is in this context. It also creates an expectation in the patient as to outcome of the surgery. Their experiences thereafter are in that light.
2265 It is to be borne in mind also, that in relation to some of the patients’ complaints, there is no evidence that a certain risk was ever mentioned to patients (e.g. maggots, or that the pain may be worse having had the surgery) (see e.g. Mr Urquhart, Ms Mattiske, Mr Warland and Ms Çalan). Those matters were not part of what the applicant said was his standard practice. Indeed, as discussed elsewhere, on the applicant’s case, Dr Al Muderis did not warn patients of the risk of maggot infestations (and did not think it necessary) until after the Broadcast. Further, the evidence in respect to odour, on the applicant’s case as to standard practice (which he submitted I should accept), was that patients were not always warned of that risk. I accept the evidence of those patients who said they were not warned of that (e.g. Mr Urquhart, Mr Mortimer and Mr Haskett). There is no suggestion in the evidence that patients were warned about the possibility of enduring stomas that “stink to high heaven” or have a “wretched smell” such that the patient may feel embarrassed in public (as described by Mr Urquhart and supported by Ms Haskett in respect of Mr Haskett), or “putrid” smell (as described by Mr Mortimer and Mr Haskett), which would adversely impact on their lives. I note also as discussed in considering the evidence of standard practice, Dr Al Muderis’ evidence that he tells patients about granulation or hypergranulation, is not supported by any of the other persons present at the consultations. Patients who suffered from ongoing issues with hypergranulation (e.g. Mr Urquhart and Mr Smith) gave evidence they were not warned about this. Mr Bruha and Ms Stewart gave evidence to a similar effect. I accept that they were not warned (or adequately warned) about this as an issue or its ongoing consequences. These risks are material matters which a patient would want to be told about, given the obvious impact of them on the quality of their lives.
2266 I also do not accept that a patient signing a consent form is indicative that relevant risks and consequences have been adequately explained. Further, it is no substitute for a specific discussion of the risks and complications by a patient’s surgeon.
2267 I accept that information about the risks and complications of the surgery were inadequately provided to prospective patients or otherwise downplayed (as described in considering the osseointegration patient case studies in relation to the surgery) in respect to Mr Haskett, Mr Mortimer, Mr Wynne, Ms Schaeffer, Mr Bruha, Ms Koolhoven, Ms Ulrich, Ms Çalan, Mr Smith, Ms Todd, Mr Urquhart, Ms Mattiske, Mr Warland, Ms McIntyre, Ms Eang and Mr Pril (it is unnecessary to repeat those conclusions): see patient case studies in Part 6.
2268 There are also particular issues that arise in relation to the international patients, as earlier explained: see Part 6, Section 4. The procedure in respect to those patients was such that the risks and complications were not explained to the patient by Dr Al Muderis until their consultation with him in Australia, which was typically the day or so before the surgery was scheduled to take place. That is, each had prepaid for their surgery and had a date for surgery without being informed (or adequately informed) of the risks and complications. I have discussed elsewhere the impact of this on the topic of informed consent. In respect to Ms Çalan, who does not speak English, Dr Al Muderis did not engage a translator to ensure that she understood the risks associated with the surgery (but relied on friends of hers to translate, noting also the consultation reports that were written in English contain no reference to risks). Mr Smith also prepaid before Dr Al Muderis had properly assessed him or discussed the risks and complications with him (noting that Ms Roberts had discussed some possible complications with him separately), in circumstances where he was told he needed to pay a deposit to secure his place.
2269 In respect to Mr Pril and Ms Eang, although there was discussion of some risks and complications, it was through a translator. This occurred shortly before the surgeries were to take place. As contrasted to the case of Ms Çalan in that a translator was engaged, it is plain from what occurred after the surgery that Mr Pril and Ms Eang did not understand from the discussion before surgery what was to occur, the nature of the surgery or the type of implant they were to receive. That they each were of the understanding they were getting the implant they had been shown – when that was not the case – reflects that (it is to be recalled, they were shown the Ottobock titanium limb in a video but received the ICRC plastic prosthesis which they had used before). Similarly, that Ms Eang wanted the implant removed very shortly after the surgery also reflects a lack of understanding of what the procedure would result in: see Part 6, Section 5.
2270 I note that in respect to the orthopaedic patients, typically they received information on the risks through the provision of the Australian Orthopaedic Association brochure (e.g. Ms Heffernan, Ms Hutton and Mr Rahiman). As discussed elsewhere, Dr Ruff’s evidence is that this is insufficient for the purposes of informed consent. In respect to the orthopaedic patients, some did not have a specific relevant risk explained (e.g. Mr Wright, Ms Brandon, Ms Hutton and Ms Slater). That said, the approach to risks in relation to the orthopaedic patients simply supports or confirms the approach evidenced to have been taken to risks in relation to the osseointegration patients (as discussed above).
2271 Returning to the respondents’ submission recited above. The inadequate provision (or downplaying) of risks in respect to the osseointegration patients is in the context of the positive presentation of the surgery. This is addressed in the section on brochures and misleading statements (see Part 6, Section 1). However, it is also evident from most of the reports in evidence from a patient’s first consultation with Dr Al Muderis, the features of which are discussed in Part 6, Section 1 above.
2272 I am satisfied that the respondents have established that this sting is substantially true. The experiences of the patients who gave evidence (in the context of the other evidence discussed) reflects they are not anomalies or outliers. Rather, they are part of a cohort of Dr Al Muderis’ patients who have had similar experiences. Their experiences are more than coincidence. This is in a context where, there is the broader evidence (e.g. brochures, consultations reports) which supports the patients’ evidence, and reflects an approach taken by Dr Al Muderis. The evidence establishes that in his practice, Dr Al Muderis has engaged in misleading conduct towards patients, including the downplaying of risks.
2273 General imputations, [13.30] and [16.26] convey this sting. Accordingly, I am satisfied that it has been established those imputations are substantially true.
2274 In relation to Mr Urquhart, Imputations [13.5] and [16.6] convey this sting. I have addressed Mr Urquhart in detail above (see his case study in Part 6, Section 7). This includes what he was informed about the surgery and the risks and complications of it (including risk of maggots), which are unnecessary to repeat here. That said, it is appropriate to recall the opinion expressed by Dr Al Muderis in his consultation report, that “the team is confident that Mark will be able to walk unaided with above knee amputation and osseointegration”. I am satisfied that these imputations have been established to be substantially true. I note that Mr Urquhart being in a worse condition since the surgery, can be readily accepted given what he has endured since that time as set out in his case study. That he may have had amputations (and been confined to a wheelchair) regardless of whether he had osseointegration, does not reflect otherwise. The applicant’s submission on these imputations fails to consider the impact the evidence shows the surgery has had (even if Mr Urquhart was able to use his legs for a period).
2275 In relation to Mr Smith, Imputations [13.9], [13.10], [16.6] and [16.21] convey this sting. I have addressed Mr Smith in detail above (see his case study in Part 6, Section 7) which includes what he was informed about the surgery and the risks and complications of it and the offer of the discounted rate of $10,000, which are unnecessary to repeat here. Suffice to recall that Mr Smith prepaid for his surgery having only had a consultation in the foyer of the hotel during which the risks and complications were not explained by Dr Al Muderis and no proper assessment of Mr Smith was undertaken. There is no report for that meeting nor is there any other pre-operative consultation report for Mr Smith. I am satisfied that these imputations have been established to be substantially true.
2276 In relation to Mr Bruha, Imputation [13.25] conveys this sting. I have addressed what Mr Bruha was informed about the surgery above (see his case study in Part 6, Section 7) which is unnecessary to repeat here. I am satisfied that the respondents have established that this imputation is substantially true.
2277 In relation to Ms Eang and Mr Pril, Imputation [13.16] conveys this sting. I have addressed what they were informed about the surgery above (see their case study in Part 6, Section 5) which is unnecessary to repeat here. I am satisfied that the respondents have established this imputation, in so far as it relates to patients in Cambodia, is substantially true. There is no evidence before me in relation to patients in Iraq.
Sting 3 — Poor patient selection
2278 In the Articles, this sting captures Imputations [16.17] and [16.25].
2279 The respondents submitted that there are examples in the evidence of negligence in the assessments by Dr Al Muderis of patient suitability for osseointegration surgery. It was submitted that the clear theme was that Dr Al Muderis was at times prepared to offer the surgery to patients: (a) who were entirely unsuited to it (Mr Ford and Patient X); (b) who had not exhausted alternative conventional treatments (such as different types of sockets e.g. Ms Todd); (c) who did not need the surgery as they were functioning well (Mr Mortimer); (d) for whom the surgery could never meet their desired goals (Ms Mattiske and Mr Haskett); and/or (e) for whom it was just too experimental (Mr Urquhart). The respondents relied on a broad cohort of patients to establish this sting.
2280 What is conveyed by this sting covers evidence where the patients were not suitable and patient’s where the assessment for evaluating their suitability by Dr Al Muderis was negligent (i.e. there had been an inadequate pre-operative assessment).
2281 The cases of Mr Ford and Patient X are obvious examples: see Part 6, Section 3. As explained when considering the evidence in each case study, the opinions expressed by Dr Al Muderis as to their suitability for surgery given the circumstances in which the patients were in (including their comorbidities and the concerns raised by others in the medical profession, including in some cases by professionals within Dr Al Muderis’ own team), fell below what would have been the standard expected. Indeed, Dr Al Muderis’ response to those concerns was generally one of dismissal (often in a belittling fashion). As explained elsewhere, the comorbidities of those patients raised red flags. They included conditions which, on the evidence (including material published by the applicant on osseointegration) would be considered exclusionary (e.g. Osseointegration Surgery A Guide for Patients). In respect to those cases, Dr Al Muderis was focused on the issue of mobility. It will be recalled that the first consultations with Dr Al Muderis in respect to each of these patients occurred in 2021. Suffice to recall that in Mr Ford’s case, the consultation report sent to his GP on Dr Al Muderis’ behalf referred to the osseointegration surgery as “necessary”, and Dr Al Muderis’ letter to the insurance company also strongly supported that position. This is in circumstances where Dr Tetsworth (who also supported the surgery), conceded in cross-examination that Mr Ford had a terrible prognosis generally, there was a material risk that he would not survive the surgery, he had been non-compliant with medical directions in the past, and that if he survived surgery, he would struggle with rehabilitation.
2282 In Mr Haskett’s case, he was offered osseointegration and TMR to make use of a myoelectric limb that could attach to his implant. He had surgery in circumstances where the custom implant that Dr Al Muderis used had no connector available to connect to any myoelectric arm, and where the implant was equipped to connect to a new generation myoelectric arm which had not yet been developed (and which was still not available at the time Dr Al Muderis gave evidence). These matters were unknown to Mr Haskett at the time he consented to surgery. The surgery could not meet his expectations: see his case study in Part 6, Section 6.
2283 Mr Mortimer had surgery in circumstances where he was functioning well with a socket. Contrary to what Dr Al Muderis recorded in his consultation report, his functional level was not declining, and Mr Mortimer did not tell him it was. Dr Al Muderis opined in the consultation report that surgery was “necessary”. This is in a context where Mr Mortimer was, if not the first, at least one of the earliest patients Dr Al Muderis had performed osseointegration on in relation to an arm: see his case study in Part 6, Section 6. As he was previously functioning well, Mr Mortimer was not a suitable candidate for the surgery.
2284 Ms Todd presented as having been highly functional and in general good health, able to perform all daily activities, including long distance walking, but was experiencing skin irritation and lower back pain from prolonged use of her prosthetic. She understood she had small bones (which it appeared Dr Al Muderis accepted given he told her she had to wait for a smaller implant to be made – although despite being made, he never used it for Ms Todd). A key outcome Ms Todd was seeking from the surgery was the ability for her to better assist her husband as his carer, as his Parkinson’s condition progressed. Given that, the risk of the surgery exacerbating her health would have a significant impact on her and her family. Consequently, the risk of losing mobility as a result of the surgery, would be a highly relevant consideration in deciding whether surgery was appropriate. There is no evidence this was appropriately addressed as part of the assessment of her suitability for the surgery. Rather, the risks were downplayed. Further, there is no evidence that alternative conservative options were proposed: see her case study in Part 6, Section 7.
2285 Mr Urquhart was a T7 incomplete paraplegic with little motor control over his legs who underwent simultaneous bilateral above-knee amputations and osseointegration surgery. Dr Paterson’s initial consultation report expressed the view that Mr Urquhart was unsuitable for the surgery for several reasons as outlined elsewhere. Those reasons included a distinct possibility that surgery would serve to make Mr Urquhart’s pain worse, cause him to become readdicted to opioids, and trigger and worsen his PTSD. His later report, properly read, expressed that he still had significant reservations. There is no evidence those reservations were addressed, or that the steps he said should take place were undertaken. This is in a context where, as the respondents described, the surgery could properly be described as experimental. The consultation report nonetheless described that Dr Al Muderis was confident he would be able to walk unaided with above-knee amputation and osseointegration: see his case study in Part 6, Section 7.
2286 For Ms Mattiske, the reports of Drs Basten and Paterson outlined that Ms Mattiske’s main goal from osseointegration was pain relief. That is so even though Ms Mattiske does not now recall that. They described the significant issues she was experiencing with pain. However, Dr Al Muderis’ consultation report was inaccurate as to the nature and extent of the pain. Dr Paterson suggested that because of her pain issues, they should review Ms Mattiske in three to six months after a period of using conservative treatment before addressing the potential role for osseointegration. Even though I have found that there was some discussion about pain, with Dr Al Muderis telling her he could not reduce it, that was somewhat undercut by him saying he “would try his best”. Ms Mattiske was not told it could make her pain worse, and there is no evidence that was considered, in circumstances where this was a particular concern for her. There is no evidence the concerns of Drs Paterson and Basten were addressed before the decision as to her suitability for surgery was made. No further conservative treatment was proposed before osseointegration was considered, despite there being no urgency. The surgery could not meet her goal of pain reduction. I note also in this context, as earlier explained, osseointegration incorporating a knee replacement (which was the surgery Ms Mattiske underwent) was described by Dr Stalley as a procedure not being well documented, within the “experimental range” and a “most unusual surgery”. None of that is reflected in the consultation report, but rather, described the surgery in the report as a “very standard procedure” and “necessary”: see Part 6, Section 7.
2287 In Mr Mailler’s case, he was assessed by Dr Al Muderis as the “perfect candidate for single stage” osseointegration surgery, without the input of a radiation oncologist or plastic surgeon, despite having undergone radiation therapy on his leg which resulted in massive scarring, damaged nerves, compromised circulation and a propensity for infection. This reflected an inadequacy in his assessment. In that context, he underwent the procedure in circumstances where, according to the applicant’s own evidence, radiotherapy on the affected limb is a contraindication to osseointegration: see his case study in Part 6, Section 7.
2288 Ms Eang and Mr Pril, who it is to be recalled were patients during Dr Al Muderis’ trip to Cambodia in 2015, were both able to walk using a socket device. There is no evidence of any assessment undertaken as to whether they were in a position (because of their personal circumstances, including financial position) to return to the hospital for any help or aftercare following their surgeries. This is also in a context where Dr Al Muderis described the nature of the surgery as in its infancy, where the risks and complications that can occur are significant, and the implications of aftercare would be particularly burdensome for patients who live in small Cambodian villages a great distance from medical support. In those circumstances, neither patient appeared to have been a suitable candidate: see Part 6, Section 5.
2289 As explained elsewhere (including in the discussion of the multidisciplinary approach), Dr Al Muderis’ approach to assessing whether an individual is suitable for osseointegration is considered only from an orthopaedic perspective: see Part 6, Section 1. His evidence in cross-examination, not considering or dismissing concerns or issues raised in consultation reports by members of his team who were not orthopaedic surgeons, makes this clear. As he said in evidence, there is a clear demarcation between each person’s roles, and persons who were not orthopaedic surgeons could not comment on suitability for surgery. Dr Al Muderis’ focus is on improving mobility (as he accepted in relation to Patient X). That approach has obvious shortcomings. A decision as to suitability may be impacted by other factors (for example, any mental health, or pain issues: see e.g. Mr Urquhart, Ms Mattiske, Mr Ford, and Patient X. Dr Al Muderis’ consultation reports in those cases do not reflect that there was any consideration of the matters raised by members of his team. It is no answer to say that consultation reports do not need to be comprehensive (or only a summary of pertinent points). These are matters of potential significance and impact on a prospective patient’s decision to proceed with the surgery and their overall health.
2290 As discussed elsewhere, the impact on some of the patients of having the surgery (which occurred in that context) (e.g. Mr Haskett, Mr Mortimer, Ms Todd, Mr Urquhart, and Ms Mattiske), have been dire.
2291 The applicant contended that the imputations relate to osseointegration surgery, and the evidence in relation to patients who had other types of surgery cannot be relied on in establishing justification. The respondents pointed to other orthopaedic patients in support of the sting arising from these imputations, submitting that the nature of the sting is broader than osseointegration: the gravamen is negligence in the selection of patients for surgery. On that basis, the respondents submitted that they are entitled to justify the imputations by reference to any kind of surgery in respect of which Dr Al Muderis was negligent in relation to patient selection.
2292 I am satisfied based on the evidence regarding osseointegration patients that this sting is established. Dr Al Muderis did not conduct himself with the level of care, skill and attention that an ordinary person in the position of his patients would have expected. I am satisfied that the patients are not outliers or anomalies. It is therefore unnecessary to determine whether the evidence concerning the orthopaedic patients can be considered in proof of the justification defence for this sting. Any factual findings reflecting an inadequacy of assessment, or lack of suitability would only reinforce the conclusion reached.
2293 In the Articles, Imputations [16.17] and [16.25] convey this sting and are general imputations. I am satisfied that the respondents have established these imputations are substantially true. In respect to [16.17], see also Mr Urquhart’s case study in Part 6, Section 7, and Multidisciplinary approach in Part 6, Section 1.
Sting 4 — Negligent post-operative care
2294 This sting concerns negligence in post-operative care. It encompasses concepts involving ignoring complications, abandoning patients and callous disregard. Regarding the Broadcast, this sting captures Imputations [13.1] (which conveys more than 1 sting and is addressed below), [13.3] (Smith), [13.7] (Urquhart), [13.8] (Urquhart), [13.11] (Smith), [13.12] (Smith), [13.15] (Ms Eang, Mr Pril), [13.21], [13.22] (Bruha) and [13.23] (Bruha). Regarding the Articles, this sting captures Imputations [16.1] (in relation to the Age Article), [16.2], [16.3], [16.7] (Urquhart), [16.11] (Urquhart), [16.12] (Urquhart), [16.14] (Todd), [16.22] (Koolhoven) and [16.24] (Ulrich). In the Grieve Video, this sting captures Imputations [28.1] (which conveys more than 1 sting and is addressed below), [28.2] (Urquhart), [28.3] (Smith), [28.4] and [28.7].
2295 This sting, as with the others, must be viewed in its context. That includes, amongst other things, the vulnerability of many of the patients. As discussed elsewhere, patients often had other medical issues including, mental health and existing pain, which Dr Al Muderis was aware of (e.g. Mr Urquhart, Mr Smith, Ms Mattiske, Mr Warland and Patient X). These are issues that must be properly considered in treating patients. On the evidence, it is not just a question of a patient’s mobility post-surgery but other issues or complications that may arise. It is also to be considered in the context of patients’ expectations, which are impacted by what Dr Al Muderis told them, including what they were told, or not told, as to the risks and complications of the surgery, amongst other things.
2296 There are some general observations to be made.
2297 First, osseointegration was described by Dr Al Muderis in cross-examination as a technology in its infancy. It will be recalled this is a description used by Dr Al Muderis in his answer to questions about his conduct in relation Mr Warland (described in Mr Warland’s case study in Part 6, Section 7 above). His answer bears repeating:
[Osseointegration is] a technology in its infancy. It confuses a lot of clinicians when they see it … even when GPs see a piece of metal sticking out of the leg with serious [serous] discharge coming out, they would – the first thing come to their mind is that, “Is this infected or not?” And that’s a natural occurrence and that’s what – what we face with osseointegration technology, as osseointegration surgeons, and it will take decades to educate the population of clinicians about what is infected, what’s not infected. So my clinical diagnosis about this, as the person that has done the largest number of osseointegration surgeries in the world – that this was not infected, and his symptoms were clearly neuropathic symptoms.
2298 As explained earlier, the technology being in its infancy only serves to highlight the importance of Dr Al Muderis responding to requests for help and ensuring his osseointegration patients received adequate aftercare.
2299 This is particularly acute for international patients. Sending patients home to locations without organising a local contact for them who has the relevant experience, is fraught. As discussed elsewhere, the evidence shows this was the experience of international patients from the United States, and Ms Çalan from Turkey: see Part 6, Section 4. It is why those patients who made requests for help needed a prompt and constructive response. This is also in a context where in the United States, the technology was not FDA approved at the time, and in Turkey, Dr Al Muderis was not aware of any surgeons familiar with his technology.
2300 Second, in respect to osseointegration, Dr Al Muderis promises himself to patients as being the point of contact for any issues or concerns. His evidence is that he provides patients with his direct mobile phone number and email address inviting them to contact him at any time (whether in Australia or overseas). The applicant advanced the proposition that as he provides his direct contact details to patients, he is providing a service to them over and above what is reasonable. In that context, the applicant put to patient witnesses in cross-examination that they could not complain about their aftercare (e.g. Mr Urquhart and Ms Schaeffer). The applicant suggested to them that no other doctor had done that for them. That submission entirely misses the point.
2301 In promoting his surgery, Dr Al Muderis also tells prospective patients they will be “family”, or other words with that import. That they can and will rely on him thereafter. As Ms Schaeffer said, Dr Al Muderis told her that “[he] will always be there as [they are] going to be family now”. The applicant accepted this is the type of statement he makes. Ms Ulrich was told they would have “a connection for life”. He is to be their first port of call. This was re-emphasised when his previous representatives in the United States (Dr Rosenblatt and Mr Hernandez) ceased working for him in 2018. At that time, Ms Roberts sent emails to international patients reminding them that she “strongly encourage[s] all clinical enquires to be forwarded directly to Munjed or [her]self”. Even when Mr Bruha then raised in response that “Australia is a reach when things go wrong”, Ms Roberts confirmed that she “will be [his] first line of contact along with Munjed anytime [he] needs [them]”: see Part 6, Section 4.
2302 Accordingly, it is evident the applicant created an expectation in his patients that they could contact him directly if they had any issues, and he would respond (irrespective of time). The evidence in relation to his quality of aftercare in relation to osseointegration patients is against that background. Not surprisingly, patients acted accordingly by contacting him. They can hardly be criticised for doing so. It is no answer for Dr Al Muderis to point to occasions when he responded to a patient, when on other occasions he did not. The applicant’s approach reinforced the patients’ vulnerability and dependency on him. It is a dynamic he positively cultivated.
2303 Yet in cross-examination, one explanation proffered by Dr Al Muderis for not responding to messages requesting help, is that he triages them and only responded when he considered it was appropriate for him to do so. As one example, it will be recalled Ms Çalan emailed him and Ms Roberts (from Turkey, on 29 August 2018) describing that “[t]he doctors here say that they do not have enough resources or experience to help me …”. And later that day she wrote: “Very very pain please help me”. Dr Al Muderis disagreed that was a cry for help “because she knows I’m not the pain specialist”. There is no evidence of any response to Ms Çalan. That was a callous approach to patient care, given the expectation he created in providing his telephone number, in a context where Dr Al Muderis had not made any arrangements for a doctor in Turkey (or anywhere else) to take over her care after she returned home: see Part 6, Section 4. As explained above, there is no evidence that he told his patients he may not respond, if contacted.
2304 Third, when patients contacted Dr Al Muderis, the evidence reflects that they received responses ranging from a prompt response from him (or Ms Roberts) through to no response at all (or not until he was chased up). On the evidence, in many instances, Ms Roberts, who is not a doctor, would fend off inquiries from patients following up requests for help and chasing up responses from Dr Al Muderis, when he was not responding. Those inquiries commonly related to concerns about pain and infections (e.g. Mr Urquhart, Mr Haskett, Mr Wynne, Mr Warland, and Ms Çalan). Some patients appeared to be responded to more often than others. For some, the speed and responses themselves varied. That said, it does not follow that, simply because Dr Al Muderis points to some of his responses to certain patients, he has not been negligent in his aftercare. It can be readily accepted that there were occasions that aftercare was promptly attended to. However, that does not overcome other occasions that aftercare was not promptly attended to. Nor does it follow that just because there was a response, it was responsive to the issue raised, or of the quality required. A patient could still justifiably feel aggrieved by the outcome.
2305 As patient numbers grew and Dr Al Muderis became busier and travelled more, it is difficult to understand how it could have been considered that this a responsible approach to aftercare. There is no evidence of the system changing. In that context, it is no answer to say there was a system of scheduled follow-ups with patients post-surgery. For the overseas patients, any follow-ups were limited and disappeared once they returned overseas (which was when issues of concern generally arose): see Part 6, Section 4. Nor is it an answer to say that patients could contact the clinic (noting the evidence of the difficulties patients had in getting a response, e.g. Mr Haskett, Mr Smith and Mr Warland).
2306 Dr Al Muderis was informed of complaints about his aftercare as some of his patients told him directly, and in very blunt terms (e.g. Mr Mortimer at [1413], Ms Çalan at [1202], [1215], [1216] and [1217], Mr Urquhart at [1552], [1563], [1575] and [1576], Ms Todd at [1811], Ms Schaeffer at [1098] and Mr Cahill and Mr Merlo on behalf of Mr Haskett at [1464] and [1468]). These complaints depicted circumstances of not being listened to, and feelings of being ignored and abandoned (e.g. Ms Todd, Ms Çalan and Mr Urquhart). Mr Hernandez also raised with Dr Al Muderis the concerns of patients about his lack of patient follow-up in 2018, at [426]. In August 2019, when Dr Al Muderis was aware there was criticism on Facebook by patients that he had not been communicating with them, he reached out to Ms Schaeffer denying it and asked her to post on Facebook a positive comment that he had responded to her. The complaints made by the patients were relevantly contemporaneous to their experiences that were the subject of the complaints. There is limited evidence anything was done by Dr Al Muderis to adequately addressed these concerns. Rather, in cross-examination he generally denied the veracity of the contents of those complaints (e.g. in relation to the complaints of Ms Çalan, Mr Urquhart and Ms Todd).
2307 Fourth, in that context, Dr Al Muderis gave inconsistent evidence in cross-examination to questions about his apparent failure to respond to requests for his help by patients. For example, during cross-examination about Mr Warland’s case (to which the quote at [1864] above is part of), Dr Al Muderis explained the apparent failure to respond as follows:
… there is no correspondence from the GP, and if there was a correspondence from a GP raising serious concern about infection, … that would be responded to, and a swab sample does not mean that there is an infection.
2308 He said that “if he had clinical features of an infection, he could have gone to emergency, gone to his GP, and the GP would have contacted us” describing that as the “normal path of communication”. That does not sit with his statements that patients can and should contact him, nor does it obviate the need for him to respond to them. He is the patient’s surgeon. There is also no evidence that patients are informed that is what they are to do. On the other hand, in relation to Ms Çalan’s pleas about her level of pain and whether it was normal, Dr Al Muderis said when questioned about there being no response, that he is “not qualified to – respond to pain” as he is not a pain specialist and “I don’t comment on pain unless it’s related to an injury that occurs or a complication of osseointegration surgery”. That does not excuse there being no response to the messages. He also gave evidence he triages messages from patients and then decides whether to respond. There is no evidence that patients are told that he will triage their message and only respond if he considers it necessary to do so. Again, that response does not sit with the patients’ expectation of a response, as created by him. On some occasions he said a response would have been provided, but there is no evidence in support of that, and often the message chain itself reflected otherwise.
2309 Being busy is the charitable explanation for the failure to provide aftercare, but as evident from the various explanations proffered in cross-examination to attempt to explain the failures (as illustrated in the paragraphs above) some of those reasons reflect a more deliberate decision by him to not respond (and implemented inconsistently without the knowledge of the patients who otherwise had the expectation of a response expect a response as promised by him).
2310 Fifth, the applicant submitted that there are numerous surgeons in Australia and around the world who have familiarity with osseointegration and are able to assist patients. On this basis, he submitted that the notion that patients are abandoned or left without any support when they cannot directly access Dr Al Muderis “is a fiction”. In Australia, the applicant referred to Dr Tetsworth, Dr Savvoulidis (Adelaide) and Dr Carey-Smith (Perth). He also submitted that there are “new clinics in Sydney which have engaged in one or two surgeries” referring to Dr Huang and Dr Wines. He pointed to, at an international level, Dr Rozbruch (New York), Dr Rosenblatt (California), Dr van Waes (Netherlands), Dr Stoneback (Colorado), and Dr Hillock (Nevada).
2311 The submission is rather disingenuous. Throughout the trial, the evidence demonstrated that the applicant had actively disparaged Dr Wines and Dr Huang as not being qualified, and in closing submissions raised Dr Huang as possibly to blame for the position Mr Urquhart is now in. For example, when Mr Urquhart requested his file from the LRC (after stating he was no longer a patient of Dr Al Muderis), Ms Roberts’ response, based on a discussion she had with the applicant, mentioned the qualifications of Dr Huang in a manner intending to dissuade him from seeing Dr Huang. In relation to Dr Savvoulidis, the evidence of Ms McIntyre is that the applicant implied he was a superior surgeon and said words to the effect of: “I am the most experienced surgeon at performing this surgery in Australia and we have the most experienced team”. It can be inferred this was said to entice her to use his services for surgery. When Ms McIntyre then told him she had seen Dr Savvoulidis, he said words to the effect of: “I believe he’s not very experienced”. I also note that the applicant did not refer to any of the doctors at The Alfred in his submission of alternate surgeons. Dr Al Muderis was critical of the doctors from The Alfred, including those who expressed opinions about Mr Mortimer. Further, a common theme in the evidence (and submissions) is that when other doctors, who gave evidence about a patient’s care, said anything adverse about Dr Al Muderis’ opinion or conduct, they were criticised. Doctors who treated or consulted with patients (or provided a medical report on them) when patients sought a second opinion were also criticised by the applicant if he perceived their report reflected adversely on him (even though the report identified his patient had medical issues).
2312 In relation to the overseas patients, the list of overseas doctors mentioned above seems to refer to those who some patients eventually saw. Even leaving aside the issue of access to these doctors, the applicant’s submission is that, amongst other things, patients could have chosen to travel to a different country, or a different state in the United States, at their expense (when they may not have the financial resources) to get help (when Dr Al Muderis was not responding to their concerns). However, if they did travel, it did not mean the doctors would have sufficient knowledge of osseointegration or Dr Al Muderis’ proprietary implants to help them. For example, Ms Çalan was dismissed by doctors in Istanbul for treatment of her open wounds because they were not experienced in osseointegration and did not want to risk intervening in the healing process: see Part 6, Section 4.
2313 Further, the applicant’s list points to five international doctors who may be qualified enough to assist overseas patients with aftercare issues. This became less once Dr Rosenblatt stopped working with Dr Al Muderis in 2018, and was followed by Ms Roberts strongly encouraging all clinical inquires to be directed to her or Dr Al Muderis (noting in the letter to Mr Bruha’s insurer dated 18 May 2017, Dr Al Muderis reported that as at that time “64 patients from the United States have chosen to undergo Osseointegration procedures”). Even when Dr Al Muderis referred Ms Koolhoven to Dr Rozbruch (in New York), she had difficulty getting an appointment even with Dr Al Muderis’ assistance (and on one occasion her appointment was cancelled). That is not to suggest that the list provided in Dr Al Muderis’ submission is necessarily exhaustive, but it illustrates that the patients (especially the international patients) relied on him and when he did not respond, they were left to their own devices and had to attempt to locate help elsewhere.
2314 Significantly, the applicant’s submission is inconsistent with his message to patients – that they will need him, he is the best, and he will be there for them. As referenced in Dr Al Muderis’ letter to Mr Bruha’s insurer, they “pride [them]selves in the close follow-up [they] establish with each and every one of [their] patients”: see Mr Bruha’s case study, Part 6, Section 4. And, as the applicant used his own patented implant, the image created was that he was necessary to address any issues that arose. Indeed, the attempts by Dr Stoneback (and Ms Koolhoven) to obtain information about what her dual cone is made of to assist her treatment, given it is proprietary, have not been answered: see Ms Koolhoven’s case study in Part 6, Section 4.
2315 Sixth, the submission, that the applicant scheduled follow-up appointments with patients, is relevant but is to be considered in the context above. In so far as the applicant relies on a standard practice for review of patients after surgery (e.g. follow-up consultations in place at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months), I note that this did not apply to the international patients in this case. Further, having a standard practice that patients are reviewed at certain stages after surgery does not address the patients’ concerns of the nature of the reviews (e.g. the brevity, not being listened to etc.), or their ability to obtain care when issues arose outside those times.
2316 A common theme in the evidence is that these appointments were short and from the evidence of Mr Urquhart and Mr Warland, frustratingly so: see Part 6, Section 7. They described travelling to appointments (sometimes interstate) to wait around all day to be seen briefly and be told everything was fine (e.g. in Mr Urquhart’s letter terminating his relationship with Dr Al Muderis he says, “I fly down to sydney to see you along with a myriad of other people I wait patiently then I get 5 or 10 minutes in the room with you and leave very disappointed with you, then fly home. One ten minute appointment with you takes two days out of my life”: see Part 6, Section 7. Mr Wright described his observation that Dr Al Muderis’ demeanour changed post-operation, describing that he was “dismissive” of him and “abrupt” or “wanting to rush [him] through”: Part 6, Section 8.
2317 The evidence as to the timing of appointments in relation to Dr Al Muderis’ clinics is discussed above in considering the evidence of Ms Stewart. As referred to there, two emails are in evidence with lists of attendees for clinics to be held on 7 July 2016 and 14 March 2017. As discussed, the lists refer to new patient and review patient appointment times and evidence the double booking of appointments. The number of new patients listed for each clinic day was seven and twelve, respectively. Dr Al Muderis accepted in cross-examination that he would typically see about 30, sometimes more, patients in a day at the clinic. Although it was put to him this could include four or more new patients, the applicant said it would typically be zero to four. Ms Roberts accepted that in 2018 there would usually be about 30 patients at a clinic day. She also said the number of new osseointegration patients would vary, noting that in 2017, it would include anywhere between one to six new patients, with the balance being follow-ups. The number of listed patients did not include any emergencies, where Ms Roberts said they “never decline[d] a patient”. She described that the follow-ups would “often just happen in a side room … concurrently”, explaining it depends on the patient. Although she did not think the follow-ups were as short as 5 to 10 minutes, she accepted a new patient might usually have an hour appointment. Dr Doshi gave evidence that a clinic day typically had 30 to 40 patients, with four to eight being new osseointegration patients and the remaining were follow-ups (although not necessarily osseointegration). Dr O’Carrigan suggested these days usually had three to four new osseointegration patients. That reflects, regardless of whether it is based on the email schedules in evidence or above estimations by witnesses, that the math does not add up, unless the consultations were as brief as some patients described, particularly post-surgery. The email schedules do not contain fixed appointment times for review patients, which is also consistent with patients’ description of waiting around all day at the clinic, and then, as Mr Urquhart said, being in the room with Dr Al Muderis for only five to ten minutes. Regardless of the precise time estimations, the evidence shows that review consultations, in particular, could be very brief.
2318 It is the applicant’s choice to take on the number of patients he does, at the rate he does. Regardless of whether being busy affected his ability to provide appropriate care (he said it did not), the evidence establishes that in some circumstances, care was not provided with the level of care, skill and attention that an ordinary person in the position of his patients would have expected.
2319 Seventh, as Dr Anstee said, a surgeon has a responsibility to their patients after surgery. He explained that complications happen and when they happen “it is the job of the surgeon to manage it”. Such responsibility is, for some of his patients, in the context of osseointegration being in its infancy.
2320 The applicant takes issue with the respondents’ case as to the extent of the responsibility of a surgeon. He submitted that he accepts he has ongoing care obligations to his patients beyond the immediate post-operative period but contended that “is not an admission on his part of the absurd characterisation the respondents wish to place on the surgeon/patient relationship”. He submitted the ordinary person would consider the “post operative” period to be the time during which the patient recovers from the immediate after-effects of surgery, and it is “not, as the respondents would have it, forever – until the patient dies”. In saying that, the applicant further submitted that he:
… is not responsible for every mishap that occurs in a patient’s life, merely by the fact that it occurs after the osseointegration operation. He cannot be expected to chase patients down to ascertain their care needs for years after surgery. Rather, as adults, patients have the onus of seeking him out if they need medical attention or advice. The ordinary reader or viewer would not have some other, strained understanding, of what post operative care means.
2321 There are flaws with that submission. It flies in the face of what he tells patients, being that they are family, he would always be there for them, and they will have a “connection for life”. It ignores the nature of the surgery, and his own evidence that it is in its infancy, with other doctors therefore not understanding it. What the ordinary person would consider the “post operative” period must be viewed in the context of the environment created by Dr Al Muderis. He again sets up a strawman, that on the respondents’ approach, he is responsible for any mishap in a patient’s life. That is not the respondents’ case, nor the evidence of the respondents’ witness, Dr Anstee, who spoke of the responsibility of a surgeon (noting the applicant’s submission takes Dr Anstee’s comment out of context). The evidence in relation to the aftercare complaints relates to the patients’ osseointegration surgery, not any mishap in their life. The ordinary reasonable person would not interpret aftercare as presented in the Publications in the manner contended for by the applicant.
2322 Eighth, it is not as simple as the applicant submitted, that Dr Al Muderis took care of the patients, or that the patients received care from him.
2323 The applicant in his written closing submissions listed each patient with a statement of the care they received from Dr Al Muderis, which for some included how long he cared for them. To take just four examples: (1) Mr Mortimer, “received ongoing care for 2 years”; (2) Ms Çalan, “[r]eceived direct care for 3 months and then ongoing care will (sic) overseas throughout 2018 until she stopped communicating”; (3) Mr Haskett, “[r]eceived care until COVID in March 2020 and was then cared for by Dr Carey-Smith”; and (4) Ms Todd, “[r]eceived care for 1.5 years after surgery until she transferred to Professor Tetsworth – a matter that she elected to do for convenience”.
2324 That reasoning is simplistic. A consideration of the evidence in respect to those patients (see patient case studies in Part 6) amply reflects that. Leaving aside whether the timeframe of those patients’ dealings with Dr Al Muderis is correct (e.g. Ms Todd), each of those patients have either complained to him and/or obtained a second opinion. Mr Haskett was never provided with an appropriate connector to attach a myoelectric arm, with the implant now having been removed. His requests for help were not responded to. Mr Mortimer had ongoing issues, with his implant being removed because he had osteomyelitis. His ongoing problems were not addressed. Ms Todd has had infection issues since the outset, being on ongoing antibiotics thereafter (with significant bone loss of her left femur associated with the infection by October 2015), the infection being such that the implant may be removed. She eventually stopped seeing Dr Al Muderis because she did not want him operating on her. Ms Çalan’s issues and complaints are clearly documented in these reasons. She was sent back to Turkey with no arrangements in place for her aftercare. To suggest that Dr Al Muderis “cared” for these patients during the period he identified (as set out above) such that substantial truth has not been established, fails to recognise the concept of adequate care.
2325 The applicant’s submission that he took care of his patients says nothing about the quality or adequacy of the care. It says nothing as to whether Dr Al Muderis responded to them (which is apparent at times he did not) or appropriately addressed the issues they raised. As described elsewhere, there is a difference between responding and being responsive to a patient’s issue. As readily apparent from the case studies above, prior to the Publications, some patients sought second opinions in circumstances in which it can be inferred they were unhappy with the applicant’s care (e.g. Ms Todd, Ms Mooney, Mr Smith, Ms Heffernan, Mr Mortimer, and Mr Urquhart), and some messaged or wrote letters to him expressing that (e.g. Mr Mortimer, Ms Todd, Ms Mattiske and someone on behalf of Mr Haskett). Moreover, the applicant’s submission does not grapple with the evidence that Dr Al Muderis failed to conduct proper investigations to diagnose conditions his patients were suffering from, which he should have been alerted to occurring (e.g. Ms Mooney, Mrs Gollan, Ms Young and Mr Mailler).
2326 Ninth, the position of the orthopaedic patients is different to that of the osseointegration patients in relation to their (expectation of) access to Dr Al Muderis. Nonetheless, some of the orthopaedic witness’ complaints are the same (e.g. including shortness of appointments, dismissiveness, failure to be listened to and absence of response to requests for help (e.g. Ms Rochford)).
2327 That said, the applicant made the same submission about care (referred to immediately above), in relation to orthopaedic patients. For example, he submitted that he provided care to Mrs Gollan and substantial care to Ms Mooney, even if it was proved that errors were made. In respect to Ms Heffernan and Ms Young, he submitted that they received care until they chose to change doctors. The submission is artificial for the reasons already referred to. These cases have similarities. In relation to each (as explained in the patient case studies in Part 6 above), the evidence establishes that Dr Al Muderis failed to carry out the appropriate investigations (given the circumstances faced in each of those cases). Of the two of those patients who gave evidence, Ms Mooney and Ms Heffernan, their evidence was they raised their concerns with Dr Al Muderis, and he was dismissive. In relation to Ms Mooney’s case, Dr Al Muderis had also dismissed the views of another doctor, Dr Watson, who had provisionally diagnosed ongoing osteomyelitis of the tibia (noting Ms Mooney was ultimately diagnosed with established osteomyelitis). Further, when Ms Mooney and Mrs Gollan raised their concerns with Dr Al Muderis that they were struggling and in pain, they were both, in effect, told to do more rehabilitation (in Mrs Gollan’s case, that she needed to walk). Second opinions were also sought by Ms Mooney, Ms Heffernan and Ms Young because of the concerns about their conditions. Complaints were made by Ms Mooney, Mrs Gollan, and Ms Heffernan proximate to the events (with two bringing legal proceedings).
2328 Those cases bear a similarity to (for example) the evidence in Mr Mailler’s case which also establishes that Dr Al Muderis should have been alert to infection (given his circumstances), and given his condition should have conducted the appropriate tests to determine if infection was present, which he did not do in a timely manner. Similarly, Mr Mortimer’s case, which included, amongst other things, that he asked Dr Al Muderis why he could not lift his arm in certain ways, which called for particular attention to be directed to determining the cause. This was in a circumstance where a scan had been taken which, I accept, showed that the implant breached Mr Mortimer’s humeral head.
2329 Having made those observations, I turn to the patients.
2330 As reflected in the findings with respect to the patients, I am satisfied that there was a failure in their aftercare, at least on occasions, in relation to some patients: for example, Mr Mortimer, Mr Haskett, Mr Urquhart, Mr Smith, Ms Todd, Mr Warland, Ms Çalan, Ms Koolhoven, Mr Bruha, Mr Wynne, Ms Ulrich and Ms Schaeffer, Mr Mailler, Ms Eang, Mr Pril, Ms Rochford, Ms Mooney, Mrs Gollan, Ms Young and Ms Heffernan: see Part 6. The details in respect to each patient’s case, and the circumstances in which the conduct occurred is discussed in the case studies, and it is not necessary to repeat. It may be accepted that the seriousness of the failures in aftercare does vary between the patients, as evident from the case studies. That said, there are similarities between them.
2331 For the international patients, the failure of aftercare is not confined to instances where the care was inadequate, but also where that failure existed at a more general level. For the American patients who gave evidence (whose surgeries spanned from 2015 to 2018), there is no evidence any attempt was made by Dr Al Muderis to liaise with doctors in the United States prior to the patients returning home, to ensure they could be properly looked after on their return (in a context where Dr Al Muderis did not have a licence to practice medicine in the United States). Rather, the patients were provided with their medical records to give to their doctor in the United States. And, as explained when considering those patients, the system in place was that they were expected to call Dr Al Muderis or Ms Roberts if they had any issues. As referred to above, an email seemingly directed to all the American patients, was sent by Ms Roberts, in August 2018, encouraging them to do that. In relation to Ms Çalan, no arrangements were made when she was returning to Turkey: see Part 6, Section 4. As explained above, although the surgery occurred in different circumstances, issues also arose as to the adequacy of the aftercare for Ms Eang and Mr Pril: see Part 6, Section 5.
2332 For some of the patients, despite the repeated problems that arose, no solution was provided (see e.g. Mr Urquhart who had issues with protruding bone, smell, hypergranulation and maggots and Mr Smith who had issues with hypergranulation). Further, for some, their symptoms were not properly investigated or diagnosed (and hence remained untreated for some time) (see e.g. Mr Mailler, Ms Mooney, Ms Heffernan, Mrs Gollan and Ms Young). That is to be considered in the circumstances of the case, which includes the conduct of the surgery (e.g. Ms Mooney and Mrs Gollan).
2333 The evidence reflects some patients felt frustrated, ignored or abandoned (e.g. Mr Urquhart, Mr Smith, Mr Warland and Ms Çalan). Those feelings can arise if their request for help from Dr Al Muderis goes unanswered. A patient can also reasonably have those feelings from not being listened to, being told not to worry and that everything is fine or normal (when it was not), and when issues that were repeatedly raised are not properly addressed (e.g. Mr Urquhart). It includes also, for example, repeatedly telling the patient the same thing (e.g. when Mr Smith was responded to, he was repeatedly told to use silver nitrate to resolve his hypergranulation), where the solution provided was not an answer.
2334 The experiences of the patients who gave evidence (in the context of the other evidence discussed) reflects they are not anomalies or outliers. As explained above, they are part of a cohort of Dr Al Muderis’ patients who have had similar experiences with him.
2335 I am satisfied that the respondents have established that this sting is substantially true. In relation to the patients referred to above (and as set out in more detail in the patient case studies in Part 6) on at least some occasions after surgery, Dr Al Muderis failed to conduct himself in relation to patient aftercare with the level of care, skill and attention that an ordinary person in the position of his patients would have expected. This also includes the failures at a general level (e.g. his approach to the international and Cambodian patients). It has been established that he acted with neglect.
2336 There are several imputations that are in general terms within this sting: Imputations [13.21], [16.1] (limited to the Age Article), [16.2], [16.3], [28.4], [28.7]. I note the only one of those imputations which refers to osseointegration is [16.2], the others being in general terms. I note also that in respect to [13.21], [16.1] and [16.2], the respondents’ Aide Memoire 6 which addresses which patients are relied on, records that Ms Mooney and Mrs Gollan are no longer relied on. That does not impact my decision. They are relied on for other general imputations. The orthopaedic patients I have referred to are relevant to proof of the general imputations. They relate to his practice as an orthopaedic surgeon, of which osseointegration is a part. Accordingly, I am satisfied that it has been established that these general imputations are substantially true.
2337 I note three further matters in relation to the general imputations. First, in relation to Imputation [13.21], the applicant submitted that arranging for other qualified specialists to care for patients interstate or overseas is not “palming them off”. He submitted that the patients are welcome to return to Sydney to see Dr Al Muderis whenever they choose, but that is not convenient to the patient. Although it may be accepted that arrangements can be made for others to care for patients, or to provide aspects of their care, the surgeon ought to be satisfied that they have the expertise to do so. That is particularly so when the surgery is in its infancy and concerns a proprietary implant. That is not what occurred in relation to these complaints. The international patients were “palmed off” to others, with there being no evidence that any arrangements were in place for the patient to receive adequate post-operative care. Second, as to Imputations [16.3] and [28.4], the applicant submitted that the allegation that the failure of aftercare left some patients reliant on heavy pain medication or mutilated is not established. The sting of the imputations is the lack of aftercare. That said, the evidence does establish that patients were left worse off, including in pain or ultimately being required to have their implant removed (e.g. Mr Urquhart, Ms Todd, Mr Bruha, Mr Mortimer and Mr Haskett). Mr Urquhart is wheelchair bound. That is not answered by the submission that he is the same as he was before the surgery, where Mr Urquhart is plainly in a worse medical situation than before undergoing osseointegration surgery (with the submission failing to grapple with what he has endured). Similarly, it is no answer to submit, as the applicant did, that the situation Mr Urquhart finds himself is in is because he went to another doctor. I note also Ms Todd uses a wheelchair in certain circumstances. Third, as to Imputation [16.1] which is only carried in respect to the Age Article, the word “rot” appears. As addressed earlier, that term is not used in the body of the Age Article (only the headline). In the context of the article, I accept the respondents’ submission that the term would have been understood by the ordinary reasonable reader to mean being left injured, unwell or languishing due to their parlous medical condition. As explained earlier, it would not be understood as the applicant suggested, to mean patients are “literally ‘rotting’ because of infections”. The imputation in the manner explained is satisfied on the evidence I have found established.
2338 Having established the sting has been conveyed I turn to the specific imputations. The identified patients are Mr Smith, Mr Urquhart, Ms Todd, Mr Bruha, Ms Koolhoven, Ms Ulrich, and patients in Cambodia and Iraq. My conclusion in respect to the aftercare of each of those patients (as reflected in their case studies), is relied on (together with other evidence) for the conclusion the sting is substantially true.
2339 It follows, in my view, that the imputations which identify specific patients which convey negligent aftercare, are generally also established. The evidence of those individual patients is also relied on by the respondents in relation to satisfaction of the general imputations. As such, although the evidence of the identified patient is relied on in proof of the specific imputation relevant to that patient, it is not necessary to consider the evidence in a vacuum.
2340 Nonetheless, I address those specific imputations.
2341 The few imputations under this sting that relate to Mr Smith are similar, relating to the same topic, being Dr Al Muderis’ care in relation to Mr Smith’s hypergranulation: see [13.3], [13.11] and [28.3]. Imputation [13.12] is in more general terms. For the reasons already given (including in the patient’s case study), I am satisfied that the respondents have established the imputations in relation to Mr Smith are substantially true.
2342 The imputations under this sting that relate to Mr Urquhart’s care in relation to his maggots, smell, exposure of his bone, and failing to identify and treat an infection which led to osteomyelitis include: [13.8], [16.7], [16.12] and [28.2]. Although some are phrased differently, all these imputations carry the sting that Dr Al Muderis was negligent in his aftercare. That is what is conveyed. For the reasons already given (including in the patient’s case study), I am satisfied that the respondents have established that the imputations in relation to Mr Urquhart are substantially true. I note that the applicant submitted that in relation to the Imputation [13.28] there is no evidence that Dr Al Muderis ignored Mr Urquhart in relation to the maggots. The evidence is discussed above in his case study, and I do not propose to repeat the earlier analysis, as it must be considered in context. That said, as explained earlier, although Dr Al Muderis did respond to Mr Urquhart’s complaint about the maggots in April 2018, no information was provided to Mr Urquhart about how to get rid of the maggots for a week. This must also be viewed with the context of the later videos sent, and Mr Urquhart’s ongoing issues. I am satisfied the sting in the imputation is established. Although [16.11] also conveys failure in aftercare, it is of a different nature than the other imputations. Given the evidence, I am not satisfied that this imputation has been established to be substantially true. Similarly, although Imputation [13.7] coveys a failure in aftercare, the imputation includes that Dr Al Muderis made fun of Mr Urquhart in that respect. That relates to the Febreze incident. That is not established.
2343 I have already referred above to the Cambodian patients. One imputation falls within this sting: [13.15]. For the reasons already given (including in the case study for the Cambodian patients) the respondents have established this imputation. The sting of the imputation is lack of aftercare, that Dr Al Muderis went overseas and conducted surgery and abandoned his patients. It has been established that is substantially true, in respect to the osseointegration patients in respect to his trip to Cambodia, two of whom gave evidence. As mentioned above, the respondents did not lead any evidence on this defence in relation to patients in Iraq.
2344 In relation to this sting, Imputations [13.22] and [13.23] relate to Mr Bruha. The sting conveyed in relation to [13.22] is negligence in his aftercare, which for the reasons already given (including in his case study), I am satisfied that imputation is substantially true. Imputation [13.23] is in a different category, being that Dr Al Muderis “ripped off his patient Chris Bruha by placing a defective implant in him that snapped and charging him for a replacement part”. That imputation does not really relate to aftercare, and the evidence is that although Mr Bruha was initially charged for the part, he complained, and that was withdrawn. In those circumstances, while correct in part, I am not satisfied that Imputation [13.23] has been established as substantially true.
2345 Imputation [16.14] within this sting relates to Ms Todd and conveys the sting of negligence in aftercare. For the reasons given above (including in her case study), the respondents have established this imputation is substantially true.
2346 Imputation [16.22] within this sting which relates to Ms Koolhoven, is phrased differently. It relates to Dr Al Muderis using a defective product, which broke, causing an infection and costing Ms Koolhoven $65,000 to rectify it. As reflected in her case study, the evidence establishes that the dual cone did break from which there has been long term consequences. Ms Koolhoven had infection issues. Although the figure of $65,000 is not referred to in the evidence, what was plain from Ms Koolhoven’s evidence was that to address the issue (e.g. to see Dr Rozbruch), was at her own “costly expense”. The events described in the case study as to what Ms Koolhoven endured thereafter, as there explained, is negligent aftercare (which is the essence of the imputation – that Ms Koolhoven received negligent aftercare). In those circumstances, I am satisfied that the respondents have established the sting is substantially true.
2347 Imputation [16.24] which relates to Ms Ulrich, is also phrased differently, being that “Dr Al Muderis callously dismissed [her] life-threatening blood clots caused by surgery he performed as a mere mistake that was not his fault”. As plain from Ms Ulrich’s case study, I accept that the incident she described in her final consultation with Dr Al Muderis post-surgery occurred. The extent of the evidence is limited: see Part 6, Section 4. I accept the blood clots left untreated can be fatal. I am satisfied that it has been established that the sting of the imputation is substantially true.
Sting 5 — Illegal surgery in the United States
2348 Imputation [13.27] alleged by the applicant is that Dr Al Muderis performed surgery in the United States where he was unlicensed to do so.
2349 The respondents rely on a video depicting Dr Al Muderis replacing a patient’s dual cone on the bed of a hotel room in the United States and submitted that the Court should find that this constituted providing medical services, specifically a surgical procedure.
2350 In addition to the video, in their Amended Defence the respondents relied on Ms Schaeffer who gave evidence of two occasions after she had returned to the United States where she saw Dr Al Muderis who fixed issues with her prothesis, including an internal broken screw. That is said to be evidence to the same effect as that shown in the video. In their closing submissions, the respondents also relied on the evidence of Mr Bruha, Mr Wynne, Mr Ladouceur and Ms Ulrich as to their dealings with Dr Al Muderis in the United States and the advice they were given.
2351 In that context, the respondents sought to tender, pursuant to s 174 of the Evidence Act, legislation from the relevant states in the United States in which these events occurred to establish the truth of the imputation that the applicant illegally performed surgery. The applicant objected to the evidence. The question of admissibility was the subject of written submissions in closing, with the ruling to be addressed in these reasons.
2352 Before addressing the issue of the legislation’s admissibility, it is appropriate to first refer in more detail to the evidence the respondents rely on to establish the truth of this imputation.
Respondents’ evidence
2353 I now turn to address each group of evidence, the first being the video.
2354 As the respondents submitted, it was accepted by Dr Al Muderis that this video involved a patient in the United States and the procedure took place in a hotel room, being a non-sterile environment. In cross-examination, Dr Al Muderis denied providing professional medical services to that patient in her hotel room and gave evidence that he was undertaking a “prosthetic replacement”.
2355 Dr Anstee, having viewed the video before giving his expert report, expressed the following opinion in cross-examination:
I would have called it a surgical procedure. It’s – it’s certainly a procedure. It’s being done by a surgeon, and it is – “invading” is too strong a word. It is entering the amputation stump. Now, look, I understand that this is just a question of definition, but do I consider it to be an operation? I think so, yes.
2356 Having been shown the video again in re-examination, Dr Anstee described the video as follows:
There’s a penetrating wound, and an indeterminate depth through which this device goes to lock into the fixture. And I don’t know how deep that hole is, but it’s not skin-lined. It’s internal. It’s inside the stump.
2357 He described it on several occasions as “an open wound” and observed that “we’re seeing a penetration through the internal tissues of the amputation stump. I would suggest that’s a surgical procedure”. He opined that the depth in which the device was inserted into the patient’s leg, although difficult to tell, might be 20 mm, or more. He said the replacement part:
[came] out of a [sterilised] peel pack, but then it’s handled [by Dr Al Muderis] with un-gloved, unsterilized – as far as I can see, unwashed – hands, and goes in through that open wound.
2358 There were differing views amongst the experts. Dr Leung said although it is best performed in a clinical environment, it was not a strictly sterile procedure. He agreed that what he saw in the video was a change of the external components of the implant. Dr Ruff, although agreeing with the applicant’s proposition in cross-examination that it was not a surgical procedure, emphasised that when working adjacent to a stoma (as in the video), best practice is to wear gloves. He noted this was the case whether the health practitioner dealing with the stoma was a surgeon, prosthetist or nurse. Dr Tetsworth gave evidence that the dual cone exchange is “routine maintenance” that can be carried out by a prosthetist in an unsterile setting. He said it was not a surgical procedure, because it did not involve an incision of any sort or manipulation or excision of any human tissue. Dr Stoita said it was not a surgical procedure because: it did not alter the size, shape or alignment of the limb; no incisions were made; no tissue suturing was required; and no surgical instruments were used. The applicant emphasised that dual cones in the OPL system which Dr Al Muderis uses, can be changed by non-medical personnel outside a surgical environment because they are external components (as opposed to the OPRA system). This was relied on to challenge Dr Anstee’s evidence. The applicant submitted that as this procedure, by design, can be carried out by the patients themselves or by a non-medically qualified prosthetist, it cannot sensibly be described as a medical procedure, let alone a surgical procedure.
2359 Stepping back, it is to be recalled that it is uncontested that the procedure in the video took place in a hotel room in the United States. This is consistent with the evidence of Ms Schaeffer that on two occasions, she made an appointment to see Dr Al Muderis when he was in the United States: first when the inner screw of her implant broke and second to adjust her prosthesis. She gave evidence that on both of those occasions, Dr Al Muderis performed the procedures in a hotel room. As she described for the first occasion, the hotel organised by Dr Al Muderis appeared to have been set up as a room for treating patients during a convention.
2360 It is appropriate to recall that the respondents referred to the event shown on the video as a “surgical procedure” and led evidence in support of that proposition (although in cross-examination the respondents put to Dr Al Muderis that he was “providing professional medical services”). A surgical procedure would necessarily be described as a medical procedure, but a medical procedure is not necessarily a surgical procedure. The terms, at times, appeared to be used interchangeably, along with the term “procedure” by itself.
2361 Moreover, simply because a procedure can be performed by a prosthetist, does not mean it is not a medical procedure. Although the applicant also relied on the proposition that a patient could do the procedure themselves, it was apparent from Ms Schaeffer’s evidence that she considered she could not, herself, do what was necessary. In any event, the evidence begs the question of why the patients waited to see Dr Al Muderis to have him do this procedure if a prosthetist could do it (noting also that he gave evidence on other occasions that he was “not a prosthetist” as an explanation for not responding to requests from patients for help). If the patients had the kit and tools to do it themselves, why was it necessary for them to wait to have him do the procedure? Or why did Dr Al Muderis not direct them to somebody local who could assist more quickly? If Dr Al Muderis did not need to do this procedure, that the patient waited for him to be in the United States to have him do it, reflects on the nature of his relationship (with the patients being dependent on him) and a lack of local suitably qualified persons to assist.
2362 Dr Anstee’s opinion that the video is of a surgical procedure is a reasonable one. However, on the evidence, I am not persuaded that the procedure undertaken in the video is surgical, given opinions vary on that, as Dr Anstee recognised. That said, the video shows a procedure being performed by the patient’s surgeon. It may be described as a medical procedure. It occurred on the bed of a hotel room. As Ms Schaeffer described regarding her experience, the hotel room was set up to treat his patients, of which she was one. She described “it wasn’t a major – it wasn’t surgery, but he did work on me in a hotel room”. Ms Schaeffer attended what, in effect, was a medical appointment to be treated by her doctor. Turning back to the video, although the replacement part in the video was sealed in a sterile manner, once the package was opened, Dr Al Muderis handled the part where there were no steps that appear to have been taken to ensure it remained sterile. As Dr Al Muderis conceded, he did not wear gloves, and no handwashing observed. Dr Ruff explained this succinctly:
… although it is not intraosseous the procedure was clearly internal to the body … basic principles dictate it be performed in as sterile a manner as possible. This was clearly not the case.
2363 If what occurred in the video is characterised as a medical procedure as opposed to a surgery, an issue arises as to whether a doctor needs to have a medical licence in the United States (or elsewhere), if they undertake to do it, in the manner done in this case. The respondents’ submission did not address this nuance. That is, although they submitted in closing that Dr Al Muderis has routinely provided medical services without a license (e.g. by giving advice in the United States), they submitted that in at least one case he performed a “surgical procedure” (being what is depicted on the video). The respondents did not address the significance of the video if it was not found to be a surgical procedure.
2364 There are two further observations to make about the video.
2365 First, the respondents submitted that the video shows that Dr Al Muderis touched the patient’s stump during this procedure, which Dr Al Muderis denied. The respondents made this submission primarily directed at the applicant’s credit. That is, he denied the obvious in the face of the video because he claimed he had never touched a patient’s stump in the United States. In the video, he appears to touch her stump. Regardless, it reflects the ease with which that could happen, which highlights the appropriateness of the procedure being performed in as sterile a manner as possible.
2366 Second, the applicant submitted that the context of Imputation [13.27] as it appeared in the Broadcast involved:
… an alarming allegation that Dr Al Muderis “treated a patient in a Kentucky hotel room using a Dremel, a drill you can buy at a hardware store” after “at least six hours of Munjed … taking turns on the Dremel, we finally cut it out”. Mr Steinfort then asks Dr Al Muderis whether he used a Dremel “on a patient” in a Kentucky hotel room.
2367 He submitted the plain meaning imputed to the viewer is that “the Dremel was used for 6 hours on a patient’s body (flesh and/or bone) to cut something out of the person”. That submission cannot be accepted, as at that point in the Broadcast, Mr Steinfort’s questions are accompanied by a photograph showing the Dremel being used on an external piece of hardware (not on a patient’s body).
2368 Turning to the evidence regarding the patients attending the conferences in the United States. The circumstances of their dealings with Dr Al Muderis are described earlier in these reasons and are unnecessary to repeat here. Dr Al Muderis accepted that he could not practice medicine in the United States, and said he did not do so. In his affidavit he said:
During these conferences, I have spoken to people who were osseointegration patients or were considering the surgery. During these conversations, I answered questions about the surgery and the devices and provided general information and education. I did not give medical advice about particular people’s medical situation or their personal suitability for the surgery. I did not take notes, collect records, or charge any fees for these discussions.
2369 As evident from my findings in relation the American patients, I do not accept Dr Al Muderis’ evidence. The respondents submitted that his evidence was wilfully false. I agree. His evidence was given where he was conscious of the consequences of not having a medical licence to practice in the United States. The evidence of these meetings, which I have found to be consultations, was not only from the patients themselves (see patient case studies in Part 6, Section 4 above), but documentary evidence tendered (e.g. the emails of Ms Roberts dated 9 May 2018 and 6 June 2018, and the letter sent on Mr Bruha’s behalf to his insurance company dated 18 May 2017, which refers to Dr Al Muderis’ consultation with Mr Bruha and the offer for him to come to Australia to undergo surgery). What occurred would have been understood by an ordinary reasonable person as the applicant providing medical services, and medical advice. From a lay perspective it had the ostensible appearance of practicing medicine.
Legislation
2370 As referred to above, the respondents relied on s 174 to tender various aspects of United States legislation (being: Medical Practice Act of 1987, 225 Ill Comp Stat 60/3, 60/3.5, 60/50, 60/59 (2017); NY Education Law §§ 6512, 6520-6521 (2018); NY Public Health Law (2018); La Rev Stat Ann § 37:1271 (2018); Ky Rev Stat Ann § 311.560 (2017); Fla Stat § 456.065). The extracts appear to be printouts of legislation from a LexisNexis site, and most refer to, on their face, as being archived versions relating to the time of the event (i.e. when Dr Al Muderis had dealings with these patients in the United States). They submitted that the lawfulness of Dr Al Muderis’ conduct in the United States is responsive to his pleaded imputations, and was the subject of a significant body of evidence of which Dr Al Muderis was fully on notice of well prior to trial.
2371 The applicant objected primarily on the basis of there being a failure to particularise in the pleadings, illegality and the foreign law relied on (where there was no application to further amend the defence). The applicant also submitted that the prejudice caused by the admission of the evidence outweighs its probative value. He submitted that notwithstanding the extremely late stage at which the United States legislation was sought to be tendered, it was done in a manner which gives little assistance to the Court (or the applicant) in construing it. The applicant identified four bases for that submission. First, the Court is left to assume or derive from the legislation tendered that the provisions were in force at the relevant time, for although the respondents contended that is so, that is not evident. Second, reliance on the United States legislation would involve consideration of how the terms contained therein (e.g. “the practice of medicine”, or “practice in any profession”) may have been interpreted under the laws of the relevant States (for example, Illinois and New York). Third, the provisions are evidently only part of larger statutory provisions, not before the Court. Fourth, the form of the respondents’ tender provides no basis to know if there are other applicable statutes in the relevant jurisdictions, or other common law principles, which might apply to the circumstances of this case.
2372 The respondents addressed the applicant’s objection in their written submission in reply. They took issue with the contention they were required to plead the foreign law and submitted that the applicant was on notice from the outset that the lawfulness of Dr Al Muderis’ conduct in the United States was responsive to Imputation [13.27], in respect of which the respondents pleaded the truth defence. The respondents deny there is any relevant prejudice. They submitted that it appears common between the parties that little would ultimately turn on the legislation’s content. First, there is no serious question that Dr Al Muderis could not legally perform surgical procedures in the United States. Second, Dr Al Muderis had also accepted when he gave evidence, more broadly, that his understanding was that it is illegal for him to provide medical services in the United States. They submitted that concession was unexceptional and the fact that Dr Al Muderis was correct in his understanding (as the respondents submitted the legislation establishes), is unsurprising. To this point, Dr Al Muderis’ case is that he did not practice in the United States, where he denied giving “medical advice about particular people’s medical situation or their personal suitability for the surgery”. The respondents submitted that no “expert evidence” that might have been called about the foreign legislation is identified by the applicant, nor any example given of how cross-examination of Dr Al Muderis might have been approached in a different way. They pointed out that the applicant had been given additional time to respond to the tender.
2373 I am not troubled by the failure to plead the legislation, although it is unclear why that information could not have been identified and provided to the applicant before near the close of evidence.
2374 Section 174(1) of the Evidence Act provides, relevantly:
174 Evidence of foreign law
Evidence of a statute, proclamation, treaty or act of state of a foreign country may be adduced in a proceeding by producing:
(a) a book or pamphlet [or other publication] that purports to have been printed by the government or official printer of the country or by authority of the government or administration of the country; or
(b) a book or other publication … that appears to the court to be a reliable source of information; or
(c) a book or pamphlet that is or would be used in the courts of the country to inform the courts about [the relevant law]; or
(d) a copy of the statute, proclamation, treaty or act of state that is proved to be an examined copy.
2375 Where evidence is adduced which meets one of the above conditions in s 174, “a court is entitled to ascertain the content of the foreign law by reference to the material before it, in [the] absence of expert evidence”: Deputy Commissioner of Taxation v Shi [2021] HCA 235; (2021) 273 CLR 235 at [31].
2376 Section 174 permits the tender of foreign legislation provided a condition is satisfied, subject to any exclusionary ruling (e.g. s 135). The respondents did not directly address the applicant’s submissions about the limited content provided and potential issues with interpreting the legislation and its use (referred to above). I also note there appears to be no definition of the concepts of practicing medicine or providing medical services in the legislation relied upon by the respondents in closing, apart from the New York legislation.
2377 Further, the respondents’ contention that “it appears common between the parties that little would ultimately turn on the legislation’s content”, does not appear to be supported by their submission, which rather focused on the fact that Dr Al Muderis had accepted that he could not practice medicine without a licence and gave evidence he did not do so. That submission presupposes that, if the relevant factual findings are made, what Dr Al Muderis did in the United States was practice medicine contrary to the legislation. The submission as described above, appears to be premised on a surgical procedure occurring, a factual matter not established. Where it refers to medical services more broadly, it relies on Dr Al Muderis’ denials (and factual findings about the clinics etc) to, in effect, submit that the legislation is of no moment. Although he denied conducting clinics and what occurred with respect to the patients at the clinics, I have not accepted that evidence. I am satisfied that Dr Al Muderis denied the conduct on the basis that he had no medical licence. However, that does not address the issue of whether the imputation has been established to be substantially true.
2378 Imputation [13.27] is directed to Dr Al Muderis illegally performing surgery with the sting framed by the respondents as the performance of an illegal procedure (although the respondents’ submission described it as a surgical procedure). As the applicant submitted, unlike some of the other imputations where the respondents in pleading contended “surgery” would have been understood in the broader sense (see Disputed Imputations in Part 2, Section 3), the respondents did not do so for this imputation. Rather, the respondents admitted the imputation was carried on the applicant’s contended meaning of surgery (in the narrow sense). That is, the imputation on the pleading which the respondents sought to establish as substantially true (which explains the pleading of the video, Ms Schaeffer procedures). That is also consistent with what the Broadcast conveys (although broader aspects are also conveyed). Although performing a surgical procedure would self-evidently be regarded as practicing medicine for which a licence is required, I have not found that to be established.
2379 Dr Al Muderis may have provided other medical services and/or practiced medicine, but those concepts do not naturally fall within the meaning of surgery, as pleaded. As described earlier, what Dr Al Muderis did in the clinics in the United States would be understood by the lay person to be the provision of medical services. That he provided advice in his capacity as a doctor, to prospective patients, about their suitability for the surgery he performs, is not what is pleaded by the respondents in their defence to this imputation. Nor is it how the respondents advanced their case (with the broader evidence not being identified as being relied on in relation to this sting until closing submissions).
2380 Consequently, it is unnecessary to reach a conclusion on the admissibility of the legislation. It would not alter my conclusion on this imputation that it is directed to whether Dr Al Muderis illegally performed a surgical procedure in the United States. That said, I note the limited nature of the material sought to be relied on (as mentioned above).
2381 For those reasons, and conscious of the Briginshaw standard, I am not persuaded that the respondents have established Imputation [13.27] is substantially true.
2382 As already explained above, the evidence of the patients who saw Dr Al Muderis in the United States, and other evidence in relation to the conduct of his practice in relation to the United States, is nonetheless relevant to several other imputations. It is also relevant to other aspects of the evidence, for example Dr Al Muderis’ standard practice. That is so, whether the conduct is established to be illegal or not.
2383 For the reasons earlier described, regardless of whether aspects of the conduct involved practicing without a licence, I am satisfied that the conduct of this practice in respect to the United States patients (and what that involved as described in the international patient case studies and observations in Part 6, Section 4 above) is properly described as unethical (see discussion below in sting 9).
Sting 6 — Prioritising money, fame, reputation and numbers
2384 Regarding the Broadcast, this sting captures Imputations [13.4], [13.13], [13.14], [13.17], [13.18], [13.19] and [13.26]. Regarding the Articles, this sting captures Imputation [16.16].
2385 To establish this sting, it is not necessary that the applicant intended to prioritise money, fame, reputation and numbers over patients, just that he in fact did. Dr Al Muderis denying he did so (e.g. in the Broadcast) therefore, can only go so far. Priorities may change over time. That said, the evidence which I accept reflects that the business model he has set up was a deliberate one, designed to attract persons to undergo osseointegration with him. This was applied in a context where he was aware patients were vulnerable. To state the obvious, osseointegration is an elective surgery, and how many operations Dr Al Muderis schedules, or how many orthopaedic patients he chooses to accept, is in his hands. As is how many extra activities he chooses to undertake (e.g. speeches, conferences etc).
2386 The following is to be read in conjunction with the evidence and earlier factfinding, including the discussion of the other stings. It is not necessary to repeat the detail referred to earlier.
2387 It is appropriate to start with the respondents’ submission that Dr Al Muderis’ image was carefully curated. On the evidence, that description is apt. As the respondents submitted, when patients first enter his orbit, they encounter an enormously successful orthopaedic surgeon who specialises in groundbreaking osseointegration surgery. He has a high profile in the media, in which he is (excepting the Publications in this case) portrayed positively. He has an active online presence, is well published (having published two books about his life and numerous academic articles), is a prolific author and presents seminars arounds the world. He is represented by Saxton Speakers, for speaking engagements at high profile events and gatherings. He also hires PR agents. It can be inferred that Dr Al Muderis has actively been involved in creating a public profile such that he has a “celebrity” status (a description of him by one of his witnesses).
2388 He is the face of osseointegration such that when Ms McIntyre googled “osseointegration” in Australia, he came up as the first entry. He is the face of the clinic, with his picture and profile being at the forefront of the websites and marketing brochures promoting the surgery. As discussed elsewhere, that marketing presents a rosy picture of the surgery performed by Dr Al Muderis and promotes positive images of individuals who had undergone osseointegration surgery (some of which contain misleading statements as discussed above in sting 2 and Part 6, Section 1). It similarly promotes positive images of himself, and his success.
2389 He is protective of that image. He has a history of suing in defamation (and related claims) (e.g. Mr Hernandez, see Part 5, Section 6). Further, Facebook sites, such as the “Osseointegration Peer Support Group”, had negative stories removed, as experienced by Ms McIntyre (whose evidence I accept). As seen in screenshots in evidence of the Facebook page for this group, next to the title, on the cover page is a photograph of Dr Al Muderis in scrubs (as he appears in marketing material). Regardless of who removed the negative posts, Dr Al Muderis was associated with the site and referred prospective patients to it.
2390 In that context, there is also evidence that on at least one occasion, Dr Al Muderis sought to counter negative comments on social media, with positive ones. Dr Al Muderis’ request to Ms Schaeffer in August 2019 – that she post a positive message about him on Facebook – reflects that he was aware at that time that patients had complained on social media about his lack of communication (see [1100]):
Dr Al Muderis: Can you please mention on Facebook that I got back to you. Some people are trying to make me look bad and they posted on Facebook that I am not communicating with my patients which is not true. It is not [sic] disheartening to see some people using innocent components like your [sic] to damage my relationship with the osseointegration family.
I would really appreciate it Lisa.
Ms Schaeffer: No problem:)
2391 His response was to deny the accuracy of the complaints and to use a patient to post a positive message. His public image mattered.
2392 As discussed earlier, this is a business. Numbers are important to him. To Mr Steinfort he said (part of which was included in the Broadcast):
You should have come to my clinic. We’re choked with patients. We can’t even, we can’t even do our day-to-day work. And in a sensible way, we try to provide safe practice and I don’t have enough hours in the day to function.
2393 In his affidavit, he refers to himself as “one of the busiest orthopaedic surgeons, if not the busiest, in Sydney”. As apparent from his evidence, he equates being busy with being successful. He equates patient numbers with being successful. (see e.g. Ms Stewart’s evidence as to having a busy waiting room at [484]-[486]).
2394 In evidence, he attempted to bolster his opinions by relying on the number of surgeries he has performed. Dr Al Muderis volunteered that his opinion is as “the person that has done the largest number of osseointegration surgeries in the world”. He has promoted himself to patients as “the most experienced surgeon at performing this surgery in Australia and we have the most experienced team”, when a patient is considering using another surgeon (e.g. Ms McIntyre). The pro forma paragraphs in a patient’s first consultation report typically also refer to the number of surgeries performed (with this figure continuously updated) and the functional success of all of them in promoting surgery with him (although Dr Al Muderis accepted in cross-examination the statement is inaccurate).
2395 In the context of his business, it is also important to recognise the proprietary nature of the implants used in the surgery. From 2014, the implants Dr Al Muderis used were proprietary. That, and any replacement parts, would come from his business, generating a financial benefit by essentially charging for the parts and the procedure. There is no suggestion that it is legally impermissible for Dr Al Muderis to own the implant used by him in his surgery, provided he discloses his financial interest in the product to his patients. There were financial disclosure forms amongst the forms that patients were given to sign. The patients from the United States would not have known about such interests until the forms were signed, which generally occurred a day or so before the surgery (that was already paid for). Further, as discussed elsewhere, Mr Hernandez’s arrangement with Dr Al Muderis meant he was contractually obliged not to disclose the financial interest of Dr Al Muderis or his company when he spoke to prospective patients and promoted the surgery.
2396 There is an obvious impact of owning and promoting the use of one’s own equipment for surgeries performed. When asked to describe the duties of a surgeon when prescribing a medical device in which they have a financial interest, Dr Ruff opined the following:
The duty of care of a surgeon to his patient with respect to conflict of interest is best not to have a conflict of interest. Most surgeons don’t and acknowledge that a conflict of interest declared is not necessarily a conflict of interest resolved. Disclosure that is opaque and incomplete is not only inadequate, it can serve to result in the opposite of its intended purpose. It may invert what is in essence a financial incentive to use a prosthesis to an insinuation of expertise. In the extreme circumstance where the medical devices in which the surgeon has a financial interest are only available to themselves this makes the patient unreasonably beholden to that surgeon and could interfere with their interaction with the surgeon because of their fear of not having an alternative should problems arise.
2397 An interest of this nature means that the doctor receives an additional financial benefit for each surgery performed that uses medical equipment he has a financial interest in, such that it may impinge on a doctor’s obligation to discuss alternative options with a patient (or on the advice as to the appropriateness of the surgery). It has the capacity to compromise the integrity of the patient’s decision whether to proceed with the surgery. As referred to elsewhere, Mr Grant gave evidence of his perception of the conflict of interest that arises, explaining that the surgeon “could potentially not do what’s best for the patient, [but] do best what’s for their bottom dollar”. Although that is only his opinion, the logic behind it is obvious. As Ms McIntyre described, Dr Al Muderis told her that the implant that would be used was designed by him and was the best available (noting also this is in the context of also telling her he was “the most experienced surgeon at performing this surgery in Australia”): see Part 6, Section 2. He is promoting his own equipment to his own advantage.
2398 In this context, it will be recalled that when a discount was provided to Mr Wynne, Ms Roberts not only informed him of that fact but also described Dr Al Muderis as being compassionate, unlike the company that made the implants (the company being Dr Al Muderis’ company).
2399 The evidence reflects that some of the implants’ components need to be replaced or changed over time. Dr Al Muderis criticised anyone who used parts that were not manufactured by him (e.g. Mr Smith, relating to a connector). I note Mr Grant’s evidence was that prosthetists and patients were told by Dr Al Muderis not to use Mr Grant’s parts (which is supported by documentary evidence). Mr Grant understood from correspondence sent to him from Osseointegration International that that instruction was put on the basis that patients using the parts he was selling voided their warranty: see Mr Grant’s section in Part 5, Section 6. I note also, both Dr Stoneback’s and Ms Koolhoven’s repeated requests for information about what the dual cone is made of, have not been responded to: see Ms Koolhoven’s case study in Part 6, Section 4.
2400 Pausing here. The applicant’s submissions on the imputations conveying this sting were very limited. In effect, they denied the imputations were proven to be substantially true. I note the applicant did submit that this imputation was not put to him, either in a general sense or in relation to a specific patient. However, he was on notice of the respondents’ position that the imputations are said to be true, and the applicant had the opportunity to address it in evidence if he chose. In any event, as described above, the sting conveyed is Dr Al Muderis prioritising his interests over his patients. That said, despite the applicant’s limited submission, it is nonetheless also appropriate to refer to a number of factors raised by the applicant during the hearing, which at least implies that because Dr Al Muderis undertakes humanitarian work, offers financial concessions on fees, is very busy, does not need to promote his services, and provides his mobile telephone number to his patients giving them unlimited access to him, it necessarily follows that this sting is not established. To put it another way, features such as those are said (at least implicitly) to mean he puts his patients first. However, there is a simplicity to that reasoning. Although these matters are plainly relevant, it is important to look at that evidence in its proper context, together with other evidence of what Dr Al Muderis did. The applicant also submitted that although he may care about his reputation that is not proof he cares more about it than caring for his patients. So much can readily be accepted. Again, that highlights the importance of considering the evidence of what has been established to have occurred, and what can be drawn from that.
2401 Against that background, it is appropriate to now turn to the respondents’ submission that the evidence was of a practice being operated as a numbers game, driven by the number of patients and the money they generated, at the expense of patient care. The overwhelming impression from the patient evidence was of a surgeon who was too busy and had too little time to provide appropriate pre-surgical and post-surgical care and attention.
2402 Patients are vulnerable. Yet the misleading statements in the brochures and other marketing material, the statements touting the number of successful procedures Dr Al Muderis had completed, the promotion of the surgery by recruited patient advocates (whom prospective patients would trust or at least relate to), the rosy picture painted which generally included the downplaying of the risks and complications reflected in the consultation reports of patient witnesses, and the opinions expressed in the reports that the surgery is necessary – all of these could only have been designed to secure patient consent to the surgery, thereby increasing Dr Al Muderis’ patient numbers.
2403 In considering the respondents’ submission, I now turn to consider aspects of Dr Al Muderis’ practice relevant to this sting.
Promotion
2404 In the above context, and despite telling Mr Steinfort that:
I do not need to promote [the osseointegration technology]. I’m not in the business of promoting it. I am here to provide a service for the patients.
Dr Al Muderis has promoted his surgery and services. This is done to attract patients, with the obvious consequence of increasing his patient numbers.
2405 Dr Al Muderis’ evidence that he does not need to promote his services contains a fallacy. It is based on the premise that because he is busy, he does not want or need more patients. However, that fails to grapple with the evidence of what he did. It was put to Ms Stewart in cross-examination that Dr Al Muderis’ rooms were busy because he a was successful surgeon, not because of any sales promotion. Given the evidence of what he did (as discussed below), it can be inferred that Dr Al Muderis denied promoting his services, because he sought to maintain the perception that his busyness was a result of primarily his success. That does not mean that he is not a successful surgeon, but rather that there is evidence that establishes that he has promoted osseointegration surgery, and himself as a surgeon. It is possible to be a successful surgeon and also partake in promoting their services.
2406 The evidence establishes that he has promoted the benefits of his surgery, his implant system, his use of a multidisciplinary team in assessing the patients, himself as a surgeon, and the aftercare provided. As explained above, his website and the brochures are marketing tools, which are published in circumstances where aspects of the brochures and websites are misleading such as to paint an unduly positive image of the surgery. Even if promotion may not in and of itself be harmful, it becomes problematic when it is misleading. Mr Hernandez and Mr Grant were, amongst others, presented as positive patient stories in these brochures (e.g. “Osseointegration: The Australian Experience” referred to in Brochures – misleading statements, Part 6, Section 1 above), while patients with issues or complications were not featured. Further in relation to the first consultation reports for patients in evidence, they generally painted a positive picture of the surgery, by downplaying the risks (see Consultation reports, Part 6, Section 1 above and sting 2). Despite it being elective surgery, Dr Al Muderis also generally referred to osseointegration as “necessary” for the patients (e.g. Ms Koolhoven, Mr Warland, Ms Ulrich, Ms Schaeffer, Ms Mattiske, Mr Mailler, Mr Wynne, Ms McIntyre, Mr Mortimer, Mr Ford (which was written on his behalf)). The evidence establishes, as discussed in relation to sting 1, that Dr Al Muderis engaged in improper sales tactics.
US practice
2407 The evidence of Dr Al Muderis’ United States practice provides a stark example of prioritising his desires over those of his patients. His practice of obtaining patients from the United States was a lucrative one. As of 2019, he was making a profit of US$75,000 for every patient from the United States who underwent the osseointegration procedure. This aspect of his practice and the apparent business imperative is described elsewhere and is unnecessary to repeat here. As apparent from the discussion of his practice in the United States elsewhere in this judgment, the evidence reflects that Dr Al Muderis wanted to get as many people to attend his clinics as possible. The patients who saw him in the United States were given advice to the effect they were suitable for the surgery, without any proper examination (noting he sometimes reviewed x-rays that patients brought with them). His standard practice required prepayment for surgery. Patients who travelled to Australia for the surgery were required to pay in full before arriving in Australia (a policy implemented for financial reasons, to avoid bad debts on Dr Al Muderis’ evidence), at which time Dr Al Muderis had not had a consultation with them nor warned them of the risks and complications of the surgery. On his evidence that occurred at the consultation that happened in Australia, which was, for some, the day before the scheduled surgery (the date of which had been confirmed before they travelled to Australia). The circumstances in which the overseas patients returned to their home country, and the obvious aftercare issues are referred to above: see international patient case studies and observations, Part 6, Section 4 and sting 4. This applies equally to the position of Ms Çalan from Turkey.
2408 His practice in the United States, as I have described in Part 6, Section 4, sting 5 and sting 9, is unethical. Dr Al Muderis’ preparedness to adopt and maintain the practice he did in relation to the international patients who gave evidence, reflects an attitude that prioritises money and numbers over his patients.
Fundraising
2409 Related to the above, is the evidence that discussions were sometimes had as to how patients would pay for the surgery with advice given to prospective patients as to how to fundraise (as discussed in Fundraising, Part 6, Section 1, and sting 1 above). To state the obvious, a person resorts to fundraising to pay for their surgery because they could not otherwise afford to do it. As discussed above, there is an email from Dr Al Muderis in evidence, where he writes: “[the patient] is suitable for osseointegration … We may need to start a discussion with the patient to teach him how to do fund raising for his surgery”. This, and other methods presented to patients to assist in paying for the surgery (i.e. discounts offered to patients), reflects on the financial vulnerability of patients and the imposition this surgery can have on them (where they may also be vulnerable physically and psychologically).
Changing practice
2410 Dr Al Muderis’ practice changed over time in relation to his assessment of patients, as initially fewer patients were assessed as suitable. Mr Grant gave evidence that the selection criteria broadened, with the pool of prospective patients he saw at the clinic having changed (including smokers, diabetics, elderly patients and severely overweight patients, which was not previously the case). Accepting that Mr Grant stopped working at the clinic in 2017, that evidence nonetheless is consistent with the evidence of others (including Dr Al Muderis himself, Dr Doshi, Dr O’Carrigan, and Dr Tetsworth), and reflected in some of the patient case studies (e.g. Mr Ford and Patient X).
2411 His assessment of a patient’s suitability for surgery is considered in sting 3 above (which is to be considered in the context of other stings including sting 2, misleading information and downplaying of the risks and complications). The effect is cumulative and can lead to a patient agreeing to surgery on an inadequate assessment for suitability, or when the surgery is not suitable for them, or without being properly informed of the risks and consequences.
2412 One only needs to consider Mr Haskett who only learnt after surgery there was no myoelectric arm available for him to use (and Dr Al Muderis’ evidence is the technology still does not exist). Mr Haskett was not informed of this before he had the surgery. Rather, he was told by Dr Al Muderis he would have far greater functionality from undergoing osseointegration, and that he was “one of only three surgeons in the world who has done an osseointegration to the humerus and the only one in Australia”. Despite Dr Al Muderis’ knowledge of there being no suitable prosthesis available (and no suitable connector to attach any myoelectric arm), he still recommended Mr Haskett have the surgery: see Part 6, Section 6. Referring to only one example, is not to diminish the significance of the other patient cases discussed in this judgment.
2413 Additionally, Mr Grant gave evidence that while working with the Dr Al Muderis, he also observed the workplace atmosphere and culture change for the worse over time as Dr Al Muderis became more famous and wealthier (see Mr Grant’s section in Part 5, Section 6 above). It is to be recalled that the applicant in closing accepted that Mr Grant was a witness of credit.
Aftercare
2414 As discussed above (see sting 4), when considering aftercare, a common theme in the patients’ evidence was that consultations were very short, in particular, after surgery had been performed. The evidence described above is consistent with that of the patients as to the brevity of their appointments (at least at times). Patients were double (and in one instance in evidence, triple) booked, and as some patients scheduled for a post-operative review described, they often waited around in the clinic for hours (e.g. Mr Urquhart). That is not to suggest that a short consultation per se, is necessarily inadequate. A consultation should be of the time appropriate to address the relevant issues. These patients had major surgery. The patients’ complaints were that the short consultations meant they were not given appropriate attention and were not listened to.
2415 In this context, there were also complaints regarding failures by Dr Al Muderis (or Ms Roberts on his behalf, or his clinic) to respond to messages for help (including failures to respond in a timely manner), patients feeling that they were not being listened to, their concerns being dismissed, and the impression that Dr Al Muderis was rushed in his interactions with them: see discussion in sting 4 above.
2416 Some patients raised these complaints with him, in writing, prior to the Publications, and in explicit terms: see, for example, Ms Todd, Ms Çalan, Mr Mortimer, Mr Urquhart and Ms Schaeffer (see patient case studies in Part 6, Sections 4, 6 and 7 above).
2417 This is also evident in an email exchange Mr Hernandez wrote to Dr Al Muderis in 2018 (before any legal proceedings were instituted against him, and well before the Publications):
I don’t think you have any idea of how many people are unhappy with the level of service coming out of Sydney; other than the nursing staff and physio team.
2418 Dr Al Muderis took issue with the accuracy of those complaints but, as evident from the patient case studies, I accept the evidence of each of those patients. When Dr Al Muderis’ relationship with Mr Hernandez and Dr Rosenblatt ceased in 2018, the email sent by Ms Roberts directed the United States patients to directly contact Dr Al Muderis and herself with any issues (apart from mechanical issues, wherein another contact was provided). It is difficult to understand how that could be seen as providing an adequate system of aftercare for patients living overseas in different time zones. Dr Al Muderis was aware he was not always available, yet the system he created involved a dependency on him. This is particularly so given the complaints raised by patients as to the lack of responsiveness and communication by Dr Al Muderis. It is one thing for him to have provided his telephone number if he only has a handful of patients, it is another to do so where he has hundreds of osseointegration patients (of note, in a 2018 consultation report this number was said to be over 500, and that was around the time when Ms Roberts’ email referred to above was sent: see e.g. Mr Wynne’s report).
2419 Dr Al Muderis was plainly on notice that the complaints about his aftercare were an ongoing issue. So much is clear from his response in August 2019, requesting Ms Schaeffer to post a positive message about him on social media, as described above.
2420 It will be recalled that Mr Mortimer’s evidence was that some weeks after he had his implant removed in November 2017, Dr Al Muderis called him asking him to take steps to have another osseointegration surgery, saying: “If you have the operation, I will treat you like you are my only patient”. I accept that evidence. It can readily be inferred that Dr Al Muderis was aware that Mr Mortimer was unhappy with his treatment as a patient of his and sought to entice Mr Mortimer to undergo a further operation with that promise: see [1366] above. I note Mr Haskett’s experiences, being the only other witness who had undergone osseointegration to the humerus (after Mr Mortimer), are in that context: see Part 6, Section 6.
2421 Also as explained earlier, after Dr Al Muderis became aware that Ms Mattiske had sought a second opinion, he attempted to contact her. An ensuing text exchange between them included a complaint to him about aspects of his conduct, with Dr Al Muderis’ response accepting that “being busy can get in the way” – although claiming when he gave evidence that being busy did not affect his ability to care for his patients. However, as demonstrated from the patient case studies, that was not the experience of many of the patients who gave evidence in the hearing.
2422 Being busy has with it many consequences, as discussed elsewhere. After all, how busy Dr Al Muderis is (i.e. how many patients he chooses to take on), is entirely within his remit and control. So too, the number of other commitments he undertakes. There is no evidence of his system changing despite being aware of patients’ complaints. Further, for the international patients, the practice in relation to their aftercare was such, as illustrated above, that there was no proper system in place, or steps taken to ensure on their return to the United States or Turkey, that they can properly be cared for. This reinforces the approach taken by Dr Al Muderis, which prioritises his position over that of his patients.
Conclusion
2423 It is not to be taken from my above consideration of this sting that making money, and attaining fame per se is an issue. Of course, many professionals are paid well for the work they undertake, and they are recognised publicly for it. As evident from the discussion above, that is not the issue in this sting, it is the prioritisation of Dr Al Muderis’ success (as represented by fame, money, reputation and numbers) over his patients.
2424 His practice has brought him fame and money, with the numbers of surgeries being used to promote his success. Those matters are all important to him. I am persuaded that Dr Al Muderis sees these as signs of success. The evidence establishes that from his perspective he equates the number of surgeries he has performed with success. That he has conducted more surgeries than any other person, means for him, he is the most experienced osseointegration surgeon, and hence necessarily he is the best (and therefore knows best). Indeed, that appeared to be the premise on which the hearing was conducted (and his evidence was given). As discussed, the nature of the conduct described above, engaged in by Dr Al Muderis (or others) as part of his practice could only have been designed to secure a patient’s consent to surgery, thereby increasing his patient numbers (noting also the financial reward that follows). Again, Dr Al Muderis chooses to take the cases he does, and the number of patients he does, and at the rate at which he does. Taking on so many patients with the systems he has in place for patients’ post-operative care (or booking patients for surgery in circumstances where there is no urgency) is a matter of choice. This is in the context of the other activities he chooses to undertake. Those circumstances jeopardise the care he can adequately provide.
2425 Considering the conduct that is undertaken by Dr Al Muderis in his practice, as described above (and expanded upon elsewhere in these reasons), I am satisfied that he does prioritise fame, numbers and money over his patients.
2426 I am persuaded that the respondents have established that this sting is substantially true.
2427 Imputations [13.4], [13.13], [13.14], [13.17], [13.18], [13.19] and [13.26] for the Broadcast, and [16.16] for the Articles are general imputations that convey this sting, and are established.
Sting 7 — Mistreating staff
2428 This sting relates to Imputation [16.18] in the Articles.
2429 I have addressed above Ms Stewart’s evidence that she was poorly treated, bullied and belittled by Dr Al Muderis, and she observed him do that to others (including Ms Bosley) (see Part 5, Section 6). It is unnecessary to repeat that evidence. Suffice to say, that it is supported by email evidence, and the evidence of Mr Grant, Mr Hernandez, and Ms Schaeffer regarding Dr Al Muderis’ treatment towards his staff. The evidence earlier discussed provides examples of conduct, which I accept occurred, including staff being required to write consultation reports, and sign scripts. Being required to do such tasks when not qualified to do so was entirely inappropriate.
2430 Mr Grant described he had witnessed Dr Al Muderis generally bullying staff, especially female staff (providing detail with respect to Ms Bosley), from when Mr Grant first became involved with him: see Mr Grant’s section in Part 5, Section 6. Mr Hernandez and Ms Schaeffer gave evidence which supported those observations. Although the evidence focused on Ms Stewart and Ms Bosley (which I accept), the allegation was broader. However, given the generality of the broader evidence (e.g. in relation to surgical fellows), I am not prepared to make those findings. Although the respondents submitted that the Court was privy to multiple examples of the applicant denigrating other doctors as referred to in the evidence, in my view, that does not overcome the generality of the evidence in relation to the Dr Al Muderis’ workplace (outside the evidence relating to Ms Stewart and Ms Bosley).
2431 The applicant submitted that the evidence is overwhelmingly one way against the respondents on this imputation, and the evidence was imprecise. His evidence on his treatment of staff was from several witnesses he called to give evidence, who said they had not observed any bullying (including of Ms Stewart or Ms Bosley), and that the work environment was collegiate. The respondents’ evidence is discussed earlier on in this judgement (see Mr Grant’s and Ms Stewart’s sections in Part 5, Section 6), and is unnecessary to repeat. It is therefore plainly not all one way. Further, the applicant submitted that the passage in the Articles is in the present tense, referring to the quote, “Shona and other staff speaking anonymously to protect their positions say …”. However, the applicant takes the sentence out of context, as it continues “Dr Al Muderis was a demanding boss …” (emphasis added).
2432 As explained above, I accept the evidence of Ms Stewart, Mr Grant, Mr Hernandez, and Ms Schaeffer on this topic.
2433 I am persuaded that the respondents have established this sting is substantially true. This has been established as true in respect to the treatment of Ms Stewart and Ms Bosley. Imputation [16.18] conveys this sting and is established. That said, even if this sting is not established it would not affect the outcome of my findings in relation to the contextual truth defence: see Part 7, Section 2.
Sting 8 — Lied to the journalists
2434 This sting relates to three imputations. In the Broadcast, this sting relates to Imputation [13.28], that Dr Al Muderis lied to 60 Minutes about encouraging staff to teach patients how to fundraise for surgeries, and Imputation [13.29], that Dr Al Muderis lied about paying people to recruit patients for him. Imputation [16.19], that Dr Al Muderis lied about paying commissions to Mr Hernandez, relates to the Articles. This sting is established to be substantially true.
2435 Each of the topics the subject of the imputations has already been addressed above.
2436 Both Imputations [13.29] and [16.19] relate to Dr Al Muderis paying people to recruit patients for him, which concerns the role of Mr Hernandez. This topic is primarily addressed in Mr Hernandez’s section in Part 5, Section 6. I am satisfied that the respondents have established that these imputations are substantially true.
2437 Imputation [13.28] alleges that Dr Al Muderis lied to 60 Minutes about encouraging staff to teach patients how to fundraise for surgeries. This is addressed in the Fundraising section in Part 6, Section 1 above. I am satisfied that the respondents have established that the sting from the Imputation that Dr Al Muderis lied to the journalists about fundraising is substantially true.
Sting 9 — Unethical conduct
2438 In the Articles, this is conveyed by Imputation [16.10]. In the Grieve Video, it relates to Imputations [28.8] and [28.9]. In respect to the Grieve Video, the applicant submitted that the allegations in respect to his practice in the United States is not relevant because it was not pleaded in the Amended Defence nor referred to in the video itself. I note that in the Amended Defence, the respondents rely on almost all of their particulars in respect to these imputations (including those about Dr Al Muderis’ practice in the United States). Just because those matters are not referred to in the Grieve Video, does not mean that the evidence of Dr Al Muderis’ United States practice cannot be relied on as proof of the imputation said to be conveyed. I note that in Imputation [16.10], the term “malpractices” is used. In my view, in the context of the Publications, that phrase would have been understood as negligent, in the manner I have previously described above: see Negligence, Part 2, Section 4.
2439 It will be recalled that I have accepted that the meaning of unethical in the context of the Publications, is conduct that fell short of the standards of honesty, integrity, candour, morality or propriety that ordinary persons in the position of Dr Al Muderis’ patients would have expected: see Unethical, Part 2, Section 4. That is how an ordinary reasonable viewer/reader would understand the concept. In proof of these imputations, the respondents rely on the evidence of all patients/witnesses who are part of their case.
2440 As the respondents described, Dr Al Muderis is a “very complex personality”. This is illustrated by him, on the one hand, doing enormous good but there is another side. The Publications relate to that other side involving his conduct in relation to a cohort of patients, with more patients of his giving evidence in the hearing. As explained above, I am satisfied that the patients on whom the findings are based are not outliers or anomalies. The conduct that I have accepted has been established occurred with sufficient frequency, such that the patients’ experiences are more than a coincidence.
2441 I am satisfied that conduct (which I have found established) which involves improper sales tactics, misleading and downplaying the risks and complications of surgery, a failure to provide adequate aftercare, and a prioritisation of money, fame and reputation over his patients, is conduct which would be understood as unethical. As a starting point, given the evidence underpinning my conclusions that the respondents have established stings 1, 2, 4 and 6, in my view, it necessarily follows that this sting is established. As explained elsewhere, this is a business for Dr Al Muderis, and his practice has features which, as evidence discussed earlier establishes, were designed to attract patients to him and his surgery. The evidence in relation to the United States practice as discussed above (including in sting 5), is of conduct that falls within the meaning of unethical. Although I have not found that sting to be established, it does not follow that the conduct cannot be unethical. The basis of my conclusion on that sting related to the basis on which the case was advanced by the respondents, and evidence directed to that. I have made more general findings about the international patients throughout this judgment as they are plainly relevant, inter alia, to the consideration of other stings. The features of the experiences of those patients and the impact of them are described in Part 6, Section 4.
2442 It is in the context of those stings, that poor patient selection in sting 3 is to be considered. For example, one only needs to consider Mr Haskett’s case, where the surgery was undertaken without Mr Haskett being informed by Dr Al Muderis that there was no prothesis available to be attached to his implant. Mr Haskett did not know this until after his surgery in 2018, and in the two years following his surgery (before his implant was removed in 2020 because of infection), he never received a myoelectric arm (or suitable connector for his arm), with the technology not yet developed: see Mr Haskett’s case study in Part 6, Section 6. As illustrated by Mr Haskett’s case, Dr Al Muderis’ conduct in relation to the inadequate assessments referred to above in sting 3 can be properly described as unethical.
2443 That some of the patient witnesses are ultimately happy that they have osseointegration does not alter the nature of their experiences, or the conduct by Dr Al Muderis (and that of his practice) which has been found to be established (including that which has been described as unethical). That other patients of Dr Al Muderis are happy patients also does not detract from the experiences of patient witnesses who might not be, or the conduct found to be established.
2444 The potential consequences for patients from the conduct characterised as unethical being undertaken, are self-evident and illustrated by what I have found to be established in relation to the patient case studies.
2445 Again, to take one example, Ms Todd described, if she had been warned she “would lose my quality of life I would not have gone ahead with the procedure. I had coped in my daily life and had lived with my existing stump for 63 years”. Dr Al Muderis described her surgery as successful because “she managed to walk” and so “from the functional point of view, which is what this surgery is designed to provide, that was successful”. The life altering consequences she experienced (as set out in her case study, see Part 6, Section 7) hardly reflects that.
2446 I am satisfied that the respondents have established this sting is substantially true. The imputations which convey this sting, being Imputations [16.10], [28.8] and [28.9] are in general terms. I am satisfied that the respondents have established that those imputations are substantially true.
Remaining imputations
2447 As flagged at the outset of this Part, there are several imputations which convey multiple stings.
2448 For example, Imputation [13.1] conveys both misleading patients (sting 2), and the failure to take adequate care of his patients (sting 4). Noting it is a general imputation and given my conclusions in respect to stings 2 and 4, I am satisfied that this imputation is substantially true.
2449 Imputation [28.1] conveys both misleading patients by downplaying the risks (sting 2) and inadequate aftercare (sting 4). Noting it is a general imputation and given my conclusions on stings 2 and 4, I am satisfied this imputation is substantially true.
2450 The other stings referred to that convey multiple imputations are already dealt with elsewhere.
2451 Before leaving this topic, it is appropriate to return the Disputed Imputations. As referred to earlier, those imputations not conveyed in the narrow sense contended for by the applicant (Disputed Imputations – see imputations highlighted in yellow in Annexure I) are (on the broader basis) also relied on by the respondents as contextual imputations. That is, in so far as they are established to be substantially true. That said, they add little given the overlap in the imputations. The evidence that underlies establishing the truth of those imputations is also relied on in proving the truth of other imputations which are conveyed. They fall within one of the defamatory stings already considered above and the analysis therein. The Disputed Imputations would generally fall within sting 4, (Imputations [10.1]-[10.6], [13.2], [13.6], [13.20], [16.8], [16.13], [16.15], [16.20], [16.27], [16.29] and [16.30]), or sting 3 (Imputation [16.4]) or both (Imputation [16.23]). Only two of these contextual imputations are in general terms. Accordingly, given my findings as to the substantial truth of the stings (and of the general and specific imputations addressed therein), generally these contextual imputations (whether they are general imputations or identify a specific patient) are also established to be substantially true.
2452 There are two Disputed Imputations that are appropriate to address in more detail. Imputation [16.15] which relates to Ms Todd includes the allegation she had “no choice but to amputate her leg or she will die”. There is no evidence to establish that. I note Ms Todd’s evidence related to advice she received as to the removal of the implant. Imputation [16.23] relates to Ms Ulrich and falls within both stings 3 and 4. This imputation alleges that Ms Ulrich almost died. When discussing the need for Ms Ulrich to receive post-operative Clexane, she was described by Dr Flecknoe-Brown as a high-risk patient having high risk surgery. The evidence establishes that she was in a dangerous situation. Ms Ulrich experienced blood clots after her surgery, exposing her to the attendant risks. The condition left untreated may be fatal. In that context, the description in the imputation could not be inapt. It is understandable that a patient may describe their experience in that manner. In any event, this imputation adds nothing to the as the evidence as to what occurred to Ms Ulrich pre-and post-surgery, which is otherwise relevant to establishing other imputations. In any event, I am satisfied the remaining Disputed Imputations have been established to be substantially true.
Section 2 — Contextual truth
2453 There are 4 imputations to which there is no truth defence pleaded by the respondents, being: Imputations [13.24], [16.9], [16.28] and [28.6]. However, as discussed earlier, Imputation [13.24] was not carried. In addition, there are a small number of other imputations conveyed that have not been established to be substantially true (which are addressed below).
2454 In determining whether contextual truth has been established, it is necessary when undertaking the assessment of whether as a result of the substantial truth of the contextual imputations, the defamatory imputations do not further harm the reputation of an applicant, the Court considers the facts, matters and circumstances relied upon to support the substantial truth of the contextual imputations rather than the terms of the imputations themselves. It is the combined effect of all the contextual imputations which is considered: Palmer v McGowen [2021] FCA 430 at [30]; Schiff v Nine Network News Pty Ltd (No 2) [2022] FCA 1120 at [18]. It is a weighing exercise.
2455 The applicant submitted in respect to the assessment of further harm, that there are different sectors of Dr Al Muderis’ reputation, as opposed to a single reputation. Those sectors were identified as Dr Al Muderis’ competence as a medical practitioner, and his honesty and conduct in business, including his treatment of staff. He submitted that even if the imputations relating to his dishonesty or business practices were true, his reputation would still be harmed by the many other imputations concerning his professional competence (to the extent they are not proved to be substantially true) as a surgeon because they are in a different sector of his reputation. He identified Imputations [13.27] [13.28], [13.29], [16.18], [16.19], [28.5], as relating to his business practices.
2456 The respondents take issue with the approach, which is premised on the applicant’s submission that the law recognises that people do not have a single reputation. The respondents submitted that is incorrect, and there is High Court authority that a person has a single reputation, not separate reputations for different aspects of their life, citing Radio 2UE Sydney Pty Ltd v Chesterton [2009] HCA 16; (2009) 238 CLR 460 at [35]-[36], [44]-[46]. They submitted that authorities relied on by the applicant concerned the question of mitigation of damages. I accept that was generally so, with the limited exception being O’Brien v Australian Broadcasting Corporation [2017] NSWCA 338; (2017) 97 NSWLR 1 at [225] (O’Brien). I note in Roberts-Smith, Besanko J at [2605] refers to that passage from O’Brien, a case the applicant in those proceedings had referred to him. There the respondents challenged the approach on a factual basis. His Honour concluded at [2606]:
Once the conduct is clearly and fully described (and that is the appropriate basis upon which to proceed), then there is sufficient similarity in the conduct to preclude an approach based on different sectors of reputation.
2457 He went on to conclude at [2607]:
There is another approach which leads to the same result. The imputations which I found to be substantially true because of the conduct I have identified are so serious that the applicant has no reputation capable of being further harmed. I consider that this is an appropriate case to take such an approach.
2458 The appeal from Besanko J’s judgment in Roberts-Smith was dismissed. The appeal did not address this aspect, as it was based on a challenge to the factual findings of some of the contextual truth imputations.
2459 The respondents, referring to Roberts-Smith, submitted that all of the imputations of which Dr Al Muderis complains concern, in one way or another, his conduct as a surgeon. The imputations concern his conduct before, during or after surgery, the way he treats his staff in a professional context, or the way he advertises and promotes or seeks to defend his conduct as a surgeon. They submitted that:
[t]here is, in Besanko J’s language, a sufficient similarity in the alleged conduct to preclude an approach based on different sectors of reputation. The position might have been different if, for example, the publications had strayed beyond Dr Al Muderis’ conduct as a surgeon and attacked (say) his personal morality in his private life. But that is not this case.
2460 Factually, I agree that the imputations of which Dr Al Muderis complains concern in one way or another his conduct as a surgeon.
2461 The applicant’s distinction is artificial, given the imputations said to relate to the business sector, as a general proposition, ignore the nature of the allegations and evidence relied on to establish the truth of those imputations (as illustrated by a consideration of the stings above). The same applies to his honesty. As a general proposition the applicant’s submission does not grapple with the facts, matters and circumstances relied upon by the respondents to support the substantial truth of the contextual imputations (regardless of what sector of his reputation the applicant suggests they fall in).
2462 As an example, the applicant identifies as part of his business sector reputation, Imputations [13.28], [13.29] and [16.19] (all in sting 8) which relate to lying to the media. The lies that have been established relate to two aspects of Dr Al Muderis’ practice, and the compelling inference is that they were said in the 60 Minutes interview to deny topics which Dr Al Muderis perceived reflected adversely on him (and his practice as a surgeon). This conduct also reflects the importance to him of his public profile. This is highlighted by his denial of encouraging the use of fundraising, which went further when he gratuitously added his moral disagreement to the use of fundraising (by saying he is “philosophically oppositional to anyone raising money …”). The other lie being in relation to paying people to recruit patients for him, relates to his United States practice. As is evident from the earlier discussion above in relation to that practice, the circumstances of his involvement with those patients, involve issues of his conduct as a medical practitioner. Further, in respect to Imputation [16.18], which relates to him mistreating his staff and is also relied on by the applicant as a business sector imputation, the evidence relied on by the respondents relates to his practice (e.g. requiring Ms Stewart to write consultation reports and forge prescriptions). That relates to his conduct as a medical practitioner.
2463 That said, although it is the cumulative effect of the imputations that are considered in the contextual truth defence, the weighing process in assessing whether no further harm is caused by the defamatory imputations involves a consideration of those imputations themselves (and what they convey). As discussed, in that exercise the Court considers the facts, matters and circumstances relied upon to support the substantial truth of the contextual imputations. The nature of the defamatory imputations is plainly relevant. Not all imputations are equal.
2464 The respondents submitted that in conducting the weighing exercise of the imputations (in the manner discussed above), if general imputations are established in a publication, given the proof relies on the experience of a large group of patients (and other evidence), it would follow no further harm would be caused by imputations relating to specific patients. The respondents said Dr Al Muderis’ reputation would be swamped by the evidence in proving the substantial truth of those general imputations. Although that must necessarily depend on an assessment of the imputations, as a general proposition, I agree with the reasoning. Having considered the imputations and given the general imputations that I have found to be established, and in the context of the Publications, that reasoning is applicable in this case.
2465 In that context it is timely to observe that the facts, matters and circumstances relied upon to support the substantial truth of the contextual imputations can only be appreciated by considering all of the relevant factual findings, the breadth and seriousness of which cannot be properly reflected in the discussion of the stings and imputations in Part 7. Further, as apparent from the discussion in Part 7, examples are provided to illustrate a conclusion (e.g. Mr Haskett in relation to some stings), where other examples are evident from my findings in the patient case studies or elsewhere in this section.
2466 Given the nature of the contextual imputations which have been established to be substantially true, in my view no further harm is done to Dr Al Muderis’ reputation by the defamatory imputations. Stings 1, 2, 3, 4, 6, and 9 (and imputations encompassed within them which I have found to be established) are, given the underlying evidence, self-evidently very serious. Stings 7 and 8 (and the imputations which convey those stings) are in that context and are also established.
2467 There is an artificiality in considering this process by each individual publication because they are each related factually and temporally. The contextual truth imputations established to be substantially true apply to the Publications. The harm done to Dr Al Muderis’ reputation relates to the Publications. The overlap between the imputations and evidence is evident from the discussion above in relation to the stings.
2468 Of the nine stings conveyed, the respondents have established eight are substantially true. In respect to the sting not established (illegal surgeries in the United States), it is only conveyed in the Broadcast as Imputation [13.27]. As discussed above, the evidence did not establish Dr Al Muderis performed surgery (in the narrow sense) in the United States. However, the broader conduct of Dr Al Muderis in relation to the United States patients, has been established to have occurred and is properly described as unethical.
2469 I turn to address the individual Publications.
The Broadcast
2470 The remaining defamatory imputations are [13.7] (made fun of Mr Urquhart’s concerns), [13.23] (Mr Bruha’s defective part, and being charged for a replacement), Imputations [13.15] and [13.16] (in respect to Iraq, as I am satisfied that these are established in relation to Cambodia) and Imputation [13.27] (illegal surgery in the United States).
2471 In relation to Imputation [13.27] (illegal surgery in the United States), as explained in addressing sting 5, the respondents pleaded that imputation in relation to what occurred in the hotel room in the United States as a surgical procedure. A consideration of the Broadcast shows that what was said about the United States related to Dr Al Muderis performing consultations in hotel rooms and holding medical clinics, and the evidence of his practice in the United States is relevant to and used in proof of other stings. Dr Al Muderis accepted that he does not have a medical licence. Even if Imputation [13.27] is not established to be substantially true (for reasons noted in sting 5 above), his conduct in respect to the United States patients was unethical: see sting 9. I note that the applicant characterised this imputation as relating to his business reputation.
2472 The stings conveyed by the Broadcast (and the imputations carrying those stings) that were otherwise established to be substantially true are misleading patients (and downplaying risks and complications), negligence in aftercare, prioritising money, fame, reputation and numbers over patients and having lied to the journalists. The contextual imputations found to be established include general imputations on significant topics. As discussed above, proof of those imputations by their nature, was based on a broader range of evidence and patient case studies, than in relation to imputations specific to a patient. In the context of the findings made and having regard to the facts, matters and circumstances relied upon to support the findings of the contextual imputations I have found to be established, I am satisfied no further harm is caused by the defamatory imputations.
The Articles
2473 The remaining imputations are [16.9] (the Febreze comment to Mr Urquhart), [16.11] (refused to see Mr Urquhart) and [16.28] (performing multiple unnecessary surgeries on a patient). I note that the other imputations in respect to Mr Urquhart and his aftercare are established to be substantially true.
2474 The stings conveyed in the Articles (and the imputations carrying those stings) established to be substantially true are improper sales tactics, misleading patients (and downplaying risks and complications), poor patient selection, negligence in aftercare, prioritising money, fame, reputation and numbers over patients, mistreating staff, having lied to the journalists and unethical conduct. Again, those established include general imputations.
2475 Given the seriousness of stings 1, 2, 3, 4, 6, 8 and 9, in the context of the findings made and having regard to the facts, matters and circumstances relied upon to support those findings of the contextual imputations, I am satisfied that no further harm is caused by the defamatory imputations.
The Grieve Video
2476 It is Imputation [28.6] (threatens to sue) that is defamatory.
2477 The stings conveyed in the Grieve Video (and the imputations carrying those stings) established to be substantially true are improper sales tactics, misleading patients (and downplaying risks and complications), negligence in aftercare, prioritising money, fame, reputation and numbers over patients and unethical conduct.
2478 Given the seriousness of stings 1, 2, 4, 6, and 9, in the context of the findings made and having regard to the facts, matters and circumstances relied upon to support those findings of the contextual imputations, I am satisfied that no further harm is caused by the defamatory imputations.
PART 8 — SECTION 26: CONCLUSION
2479 I am satisfied that the respondents have established the s 26 defence in respect to each of the Publications for which it has been established. In respect to each publication, the respondents have established that having regard to the facts, matters and circumstances relied upon to support the substantial truth of the contextual imputations, the defamatory imputations do not further harm the reputation of the applicant.
PART 9 — SECTION 29A
2480 The respondents each plead s 29A as a defence. It is a complete defence to a defamatory matter: s 29A(1). See also Russell v Australian Broadcasting Corporation (No 3) [2023] FCA 1223 (Russell) at [316].
2481 It is helpful to commence with consideration of the relevant legal principles, as the discussion thereafter is to be viewed in that light.
Section 1 — Legal principles
2482 Section 29A provides:
29A Defence of publication of matter concerning issue of public interest
(1) It is a defence to the publication of defamatory matter if the defendant proves that—
(a) the matter concerns an issue of public interest, and
(b) the defendant reasonably believed that the publication of the matter was in the public interest.
(2) In determining whether the defence is established, a court must take into account all of the circumstances of the case.
(3) Without limiting subsection (2), the court may take into account the following factors to the extent the court considers them applicable in the circumstances—
(a) the seriousness of any defamatory imputation carried by the matter published,
(b) the extent to which the matter published distinguishes between suspicions, allegations and proven facts,
(c) the extent to which the matter published relates to the performance of the public functions or activities of the person,
(d) whether it was in the public interest in the circumstances for the matter to be published expeditiously,
(e) the sources of the information in the matter published, including the integrity of the sources,
(f) if a source of the information in the matter published is a person whose identity is being kept confidential, whether there is good reason for the person’s identity to be kept confidential (including, for example, to comply with an applicable professional code or standard),
(g) whether the matter published contained the substance of the person’s side of the story and, if not, whether a reasonable attempt was made by the defendant to obtain and publish a response from the person,
(h) any other steps taken to verify the information in the matter published,
(i) the importance of freedom of expression in the discussion of issues of public interest.
(4) Subsection (3) does not—
(a) require each factor referred to in the subsection to be taken into account, or
(b) limit the matters that the court may take into account.
…
2483 The defence has three elements: see Murdoch v Private Media Pty Ltd [2022] FCA 1275 at [64]-[67]; Russell at [265]; Deeming v Pesutto (No 3) [2024] FCA 1430 at [630]-[635] (Deeming).
2484 First, that the matter concerns an issue of public interest. Section 29A(1)(a) focuses attention on the relevance of the publication to “an issue of public interest”, which is objectively determined: see Russell at [318]-[319].
2485 Second, that the respondent believed the publication of the matter was in the public interest. Section 29A(1)(b) is concerned with the respondent’s actual state of mind at the time of publication: Russell at [321]. This element of the defence is not made good by showing that a notional reasonable person in the respondent’s position could have believed that publication was in the public interest: Russell at [322]. The respondent must prove this element by adducing evidence that the publisher turned their actual or attributed mind to the issue and did hold the relevant belief: Russell at [322]. Ex post rationalisations are not enough: Russell at [322].
2486 Third, that the respondent’s belief that the publication of the matter was in the public interest was reasonable. It has been said that in most cases this will be the “heart of the enquiry”: Russell at [324]; Deeming at [634]. In determining whether the defence is established, a court must take into account “all of the circumstances of the case”: s 29A(2). See also: Murdoch at [68]; Russell at [265], [324]; Deeming at [635]. As Wigney J said in Murdoch at [67]:
The question, essentially, is whether a reasonable person standing in the defendant’s “shoes” – that is, in particular, possessing the information that the defendant possessed at the time – would have held that belief.
2487 An important aspect is an honest and reasonable belief in the truth of what is published; but this is not to be confused with an assessment of the actual truth or falsity of the allegations concerned: Russell at [339]. The standard of reasonableness should not be conflated with factual accuracy. Public interest journalism does not pretend to be a form of fact-finding that is functionally equivalent to the judicial process, and it is not the case that its public utility depends on such an equivalence: Russell at [339]. The knowing publication of misinformation has never found protection in Australia (except on occasions of absolute privilege): Russell at [340].
2488 Section 29A(3) of the Defamation Act sets out a non-exhaustive list of factors that the Court may take into account to the extent that the Court considers them applicable in the circumstances. The factors listed should not be treated as a checklist, as the provision does not require each to be taken into account, nor does it limit the matters a court may take into account: s 29A(4) of the Defamation Act.
Issues as to interpretation
2489 Two issues as to the interpretation of s 29A arise in these proceedings.
2490 First, the respondents submitted that the applicant’s submissions tended to erroneously conflate the requirements of s 29A with those applicable to s 30 (the defence of qualified privilege) and involved a selective reading of Russell. The applicant did submit that: several factors in s 29A(3) are comparable to those relevant to whether a publisher’s conduct was reasonable for the purposes of the defence in s 30 of the Defamation Act; the list in s 29A(3) was copied substantially from s 30(3) (as it was prior to the 2020 amendments); in Russell at [335] Lee J accepted that “it is clear on the face of s 29A and the explanatory materials that the defence is intended to continue and extend the previous law in this area”, which, according to the applicant, is another way of saying that s 29A is evolutionary rather than revolutionary in its operation; and his Honour at [330] noted Parliament’s intention to “mirror” s 4 of the Defamation Act 2013 (UK) (UK Act).
2491 However, as the respondents submitted, Lee J was at pains to point out that s 29A was not to be approached as a mere extension of s 30 and its predecessors, and differs from s 4 of the UK Act and the common law Reynolds defence: Russell at [270]-[271], citing Reynolds v Times Newspapers Ltd [2001] 2 AC 127 (Reynolds) at [336]. In response to a suggestion that s 29A had not brought about a substantive change to the law, his Honour at [336] observed that:
[T]his submission ignores Parliament’s recognition that pre-existing defences have not lived up to the objectively discernible expectations of the jurists, law reform bodies and legislatures who conceived of them. Reform ensures a court is to have regard to all the relevant circumstances in making allowances for editorial judgments as to publications of certain character. The submission is also apt to mislead because it does not recognise that where ss 22 and 30 were concerned with the objective reasonableness of the respondent’s conduct, s 29A is concerned with the reasonableness of the respondent’s belief the publication of the matter was in the public interest.
(emphasis in original)
2492 Moreover, Murdoch at [60]-[62] reflects that s 29A was not to be burdened by the baggage that plagued s 30 of the Act. The Explanatory Note for the Defamation Amendment Bill 2020 (NSW), in introducing s 29A, explains that “section 30 has been largely unsuccessful in liberalising the approach taken by the courts to publications concerning issues that may be of public interest”.
2493 A consequence of the applicant’s approach has led to a tendency to focus submissions on impugning the reasonableness of the respondents’ conduct rather than, as applicable to s 29A, the reasonableness of the respondents’ belief that publication of each matter was in the public interest. As Lee J explained in Russell at [337]:
Of course, conduct may evidence subjective belief. Indeed, almost all of the factors in s 29A(3) are focussed upon the publisher’s conduct (leaving to one side ss 29A(3)(d) and 29A(3)(i)). But this shift is nonetheless notable; the renewed focus eschews speculation about what a reasonable person would have done and instead requires the Court to trace a respondent’s reasoning as it happened and conduct an objective assessment from that position.
(citations omitted)
2494 As the respondents submitted in these proceedings:
The “reasonableness” enquiry is not directed to the respondents’ conduct … but, rather, to the reasonableness of their belief. … Conduct that might be considered unreasonable (for example, procuring a whistleblower to disclose information in breach of the law) will not necessarily affect the reasonableness of a defendant’s belief that a publication is in the public interest (if, eg, the information so procured provides a reasonable basis for such a belief).
(emphasis in original)
2495 Second, as the respondents contended, the applicant repeatedly submitted that, because a particular fact in the Publications, or an imputation conveyed by the Publications, was allegedly false, it was not in the public interest to publish those matters (i.e. the Publications). That approach is reflected in the applicant’s Reply to the Amended Defence. At one stage, he asserted that “s 29A requires the defamatory matter to be engaged by each element of the defence, not just the matter”. At another, he challenged the respondents’ reasonable belief “that the allegations about Dr Al Muderis were in the public interest”.
2496 The applicant’s approach was rejected in Russell at [314]-[316]. Section 8 of the Defamation Act reflects a clear distinction between the matter and the defamatory imputations conveyed by the matter. The same is true of s 29A. In Murdoch, although Wigney J did not decide the issue, his Honour expressed a strong inclination to the view that the reference to “defamatory matter” and “matter” in s 29A is a reference to the article, report or program which conveyed the defamatory imputation or imputations, not a reference to the alleged defamatory imputation or imputations, or the defamatory sting, found to have been conveyed: at [70]-[72]. In Russell, Lee J agreed: at [316]. O’Callaghan J adopted this approach in Deeming: at [638].
2497 Applying the well-established principles of statutory construction, the starting point for ascertaining the meaning of a provision is its text, having regard to its context and purpose: SZTAL v Minister for Immigration and Border Protection [2017] HCA 34; (2017) 262 CLR 362 at [14], citing Project Blue Sky v Australian Broadcasting Authority [1998] HCA 28; (1998) 194 CLR 355 at [69]-[71]. I agree that s 29A is directed towards the matter, and not to the imputations. As the respondents submitted, the applicant’s approach falls into the trap of approaching s 29A from the perspective of the defamatory imputations rather than the “matter” as a whole. That said, the nature, character and seriousness of any defamatory imputations carried by the “matter” may be relevant to assessing whether s 29A’s elements have been established: s 29A(3)(a).
Approach to s 29A
2498 As noted above, the applicant’s submissions were generally impaired by his interpretation of s 29A. The concluding paragraph of his written submissions on s 29A contended that:
Section 29A is designed to protect responsible investigative journalism. It provides a defence when the journalists do everything right, but still get it wrong. This is a far cry from the conduct of the respondents in relation to each of the Publications.
2499 This appears to be the premise on which much of the applicant’s submissions proceeded. His submissions tended to focus on aspects of each matter and the respondents’ conduct in isolation, apparently to demonstrate that the respondents fell short of “do[ing] everything right”. The applicant’s approach (“do everything right, but still get it wrong”) appears to follow the approach for s 29A’s antecedents: see e.g. the discussion in Lehrmann at [905]-[907].
2500 As the respondents submitted in reply (some of which bears repeating):
… Dr Al Muderis’ failure to recognise the full force of the legal change brought about by s 29A has led to a tendency on his part to do precisely what Lee J warned against in Russell: to impugn the reasonableness of the respondents’ conduct (for example, the alleged failures to maintain audio recordings, report on positive patient experiences and give Dr Al Muderis sufficient notice of the topics for discussion at his interview with Mr Steinfort), rather than grapple with the reasonableness of the respondents’ belief that the Publications were in the public interest.
… A consistent feature of Dr Al Muderis’ closing submissions is the repeated assertion that because a particular fact in the Publications, or imputation conveyed by the Publications, was allegedly false (eg the matters in the Articles concerning the “Febreze” incident and the corresponding imputation; or the question of whether or not Mr Urquhart was “abandoned”), it was not in the public interest to publish those matters. That approach is not consistent with legal principle. It falls into the trap of approaching s 29A from the perspective of the defamatory imputations rather than the “matter” as a whole.
(emphasis in original) (citations omitted)
2501 The imposition on s 29A of a requirement that the journalists “do everything right” is also not supported by its text, given its purpose, and considered in context. That is to ask the wrong question. As explained above, s 29A is directed to proof of reasonable belief by taking into account all of the circumstances of the case. Although several considerations which may refer to conduct are listed in s 29A(3), they are factors a court “may” take into account “to the extent the court considers them applicable”. The terms of s 29A admit that flaws in a matter (or in one’s conduct, in so far as it informs an element of the defence) will not necessarily preclude the application of the defence. Whether the defence is established will necessarily depend on the particular facts of the case: s 29A(2). There is no express bar to the defence, such as disentitling conduct: cf s 30(4).
2502 As stated in the Explanatory Note for the Defamation Amendment Bill 2020 (NSW):
One of the objects of the [Defamation Act 2005 (NSW)] was to ensure that the law of defamation does not place unreasonable limits on freedom of expression and, in particular, on the publication and discussion of matters of public interest and importance. The new defence is aimed at promoting that object.
(emphasis added)
2503 As explained above, this reflects the context in which the defence was enacted. Lee J provided further background on this point in Russell at [336]: see [2491] above.
2504 There is no warrant to impose an additional criterion or standard that a journalist “do everything right” to establish the s 29A defence.
2505 I also note that s 29A is not limited to “protect[ing] investigative journalism”, as its application is not confined to journalists or to investigative reporting: see e.g. Deeming at [625]. As the respondents submitted:
Section 29A is not, in terms, a defence of “responsible journalism”. Its availability is not limited to journalists. It has a potentially broad reach and is capable of adapting to the circumstances of a particular case. In its plain meaning, it affords a defence to any publisher who publishes any type of defamatory matter that concerns an issue of public interest, so long as the publisher reasonably believed that the publication was in the public interest. Those criteria should not be construed merely as a synonym for, or conflated with, “responsible journalism”, although it is not disputed that in applying the criteria the court naturally would derive assistance where relevant from earlier decisions on s 4 of the UK Act and Reynolds before it.
Section 2 — Overview of Part 9
2506 In dispute is whether the respondents reasonably believed that the Publications were in the public interest. That is, whether the respondents subjectively believed the publication of the matters was in the public interest, and whether those beliefs were objectively reasonable. The applicant admitted that the Publications are concerned with an issue or issues of public interest (although the description of that public interest is in issue).
2507 It is appropriate to outline the structure of this part of the reasons given the range of issues falling for consideration, and to make several observations.
2508 Section 3 identifies the parties responsible for each publication and addresses corporate state of mind. Section 4 addresses the credit of Ms Grieve, Mr Steinfort and Ms Clancy, and related submissions. Section 5 provides a brief summary of the parties’ submissions as to whether the respondents reasonably believed that the Publications were in the public interest. Section 6 addresses the applicant’s submission that the respondents failed to prove what information they had at the time of the Publications, such that they cannot rely on s 29A. His submissions on this topic, at times, were also directed to the substantive elements of the defence. Section 7 summarises the respondents’ investigation into Dr Al Muderis’ practice. Section 8 summarises the material before the respondents as a result of that investigation. Section 9 addresses several issues relating to the respondents’ interview with Dr Al Muderis. Section 10 notes that the Publications were presented as a joint investigation and raises some implications. Section 11 emphasises several issues relevant to subjective belief. Section 12 emphasises several issues relevant to the objective reasonableness of that belief.
2509 Section 13 records reasons in relation to the balance of the applicant’s principal submissions. It is appropriate to address those submissions together. Inter alia, they have little, if any, delineation between the subjective and objective elements of the defence. His submissions in respect to the objective element largely take the form that, if his submission that the journalists’ subjective belief is not accepted, the belief was not reasonable in any event. The limited exceptions (which included his submission in reply that the objective truth or falsity of the matter is not relevant to the reasonableness of the respondents’ belief), do not meaningfully address the respondents’ submissions. As a consequence of his focus, his submissions generally failed to grapple with the detail of the material before the respondents or engage in an assessment from an objective viewpoint. Moreover, as already referred to, his submissions were very much directed at the journalists’ conduct (rather than belief), as reflected in the concluding paragraph to his written submissions (recited above at [2498]), which focuses entirely on their conduct. Section 14 addresses the conclusions reached. Section 15 considers the issue of ongoing belief.
2510 Although consideration of the defence’s subjective element and objective element are foregrounded in Sections 11 and 12, respectively, consideration of each element is not confined to any one section of these reasons. Nor does any one section seek to exclude consideration of either element. That approach in recording the reasons is warranted due to the nature of these proceedings and the submissions. My consideration of this defence, and its subjective and objective elements take into account the evidence relevant to this defence, the parties’ submissions in the context of each other’s, and all the circumstances of the case.
Section 3 — The parties responsible for the defamatory matters
2511 It is convenient to revisit which respondents are sued in relation to each Publication, as the belief to be assessed for the purposes of s 29A will vary accordingly.
Publication(s) | Respondent(s) sued |
Sneak Peek | Nine Network |
Broadcast | Nine Network Ms Grieve Mr Steinfort Ms Clancy |
SMH Article SMH Online Article
| Fairfax Ms Grieve Mr Steinfort Ms Clancy |
Age Article Age Online Article | The Age Company Ms Grieve Mr Steinfort Ms Clancy |
Grieve Video | The Age Company Ms Grieve |
2512 All six respondents nevertheless pleaded s 29A in relation to each publication.
2513 Where a respondent is sued in defamation in relation to a matter, they will avoid liability for that matter if they establish the defence contained in s 29A as it relates to that matter. Where a respondent is sued for multiple matters, they must establish the defence for each matter for which they are sued to avoid liability altogether pursuant to s 29A; a respondent may succeed in establishing the defence for some matters, but not others. In these proceedings, the respondents will avoid liability altogether pursuant to s 29A, if each respondent establishes that they reasonably believed that the publication of each matter for which they are sued was in the public interest: Defamation Act s 29A(1)(b). See also Russell at [342]; Deeming at [649], [677].
2514 In that context it is now appropriate to address the state of mind of the corporate respondents.
Corporate state of mind
2515 The applicant contended that there is no evidence as to the state of mind of the persons responsible for the corporate respondents’ decision to publish the Publications, and as such, the s 29A defence should be dismissed in relation to the corporate respondents. The submission is based on the premise that the person “ultimately responsible for the decision to publish the matters” must give evidence. Indeed, he submitted that absent evidence from the ultimate decision maker, the Court does not have the evidence necessary to find that the corporate respondents had the requisite actual state of mind for the purposes of s 29A(1)(b). The applicant submitted that Mr Michael Bachelard, the editor of the investigations team, was the ultimate decision maker for The Age Company and Fairfax, and Ms Thomson for Nine Network.
2516 The applicant submitted that although the actions and state of mind of a journalist are attributable to the corporate defendant and may inform its state of mind, the journalist is unlikely to be the ultimate decision maker. It was submitted that if evidence is not adduced from the ultimate decision maker who is responsible for the ultimate decision to publish, there would be a significant gap in the evidence and it would be difficult for the corporate defendant to satisfy the Court that it had the requisite corporate state of mind, citing Duma v Fairfax Media Publications Pty Ltd (No 3) [2023] FCA 47 at [307]-[308] (Duma) in support. He further submitted that:
In the case of corporate defendants, the enquiry will necessarily focus on the state of mind and actions of the employees or agents who were responsible for the company’s decision to publish the publication …
2517 In support he cited Herron at [157]-[160]. However, the recited submission does not reflect the principle as stated in Herron, and earlier authorities.
2518 In Russell, Lee J stated at [349] that:
In determining the state of mind of the ABC, a statutory corporation constituted under the Australian Broadcasting Corporation Act 1983 (Cth), the focus must be on its servants or agents responsible for the matter being published: Austin v Mirror Newspapers Ltd [1986] AC 299 (at 316 per Lord Griffiths); John Fairfax Publications Pty Ltd v Zunter [2006] NSWCA 227 (at [12] per Handley JA, with whom Spigelman CJ and McColl JA agreed); Waterhouse v Broadcasting Station 2GB Pty Ltd (1985) 1 NSWLR 58 (at 72 per Hunt J).
2519 As will be apparent, the authorities do not refer to the person responsible for the company’s decision to publish. The difference may appear subtle, but it is important. The applicant’s recitation places the emphasis on the ultimate decision maker.
2520 A similar submission was rejected in Russell. There it was submitted the evidence was that Mr Lyons, the ABC’s Executive Editor and Head of Investigative Journalism, was the “ultimate decision maker” and, as he was not called to give evidence, it should be inferred his evidence would not have assisted the ABC. Lee J declined to draw any inference where, on the evidence before the Court, it was plain Mr Lyons had a very limited role, which might be described as procedural rather than substantive. Rather, his Honour identified the persons he said on the evidence were “substantially responsible” for the publication, which included the journalists, and the investigations editor: Russell at [350]-[351]. His Honour did not approach the application of s 29A to corporate respondents by confining its application to the “ultimate decision maker”.
2521 Further, the passage from Duma that the applicant relies on does not assist. As the respondents submitted, that case was not about the attribution of state of mind to a corporation, but rather involved an evidentiary gap in relation to proof of the reasonableness of the publishers’ conduct for the purpose of s 30.
2522 Whether the evidence led satisfies proof of the state of mind of a corporate defendant must necessarily depend on the circumstances of the case. Here, that includes the Publications which were a result of a joint investigation between the respondent companies, conducted over some considerable time. That also includes the topic of the Publications.
Fairfax; The Age Company
2523 I accept the respondents’ submission that for the purpose of assessing Fairfax and The Age Company’s corporate states of mind, the evidence establishes that Ms Grieve was the person who was substantively responsible for the publication of the Articles and the Grieve Video, that hers was the relevant directing mind or will for the purposes of the publication of the Articles and the Grieve Video, and that she was so closely and relevantly connected with the publication of the Articles and the Grieve Video so as to have her state of mind treated as the state of mind of the corporations.
2524 The evidence establishes that Ms Grieve drafted the Articles in a Google Doc and made changes to them over time, before later placing the draft into The Age Company’s internal news production system. The draft was then edited over 12 days by Ms Grieve and a number of editors. Changes of substance were the product of decisions taken by Ms Grieve in consultation with Mr Bachelard.
2525 The evidence also establishes that Ms Grieve conceived the idea for the Grieve Video, scripted it, provided a voiceover, appeared in it, and oversaw its edit.
Nine Network
2526 I also accept that the evidence establishes that Mr Steinfort was the person who was substantively responsible for the publication of the Broadcast and the Sneak Peek, that his was the relevant directing mind or will for the purposes of the publication of the Broadcast and the Sneak Peek, and that he was so closely and relevantly connected with the publication of the Broadcast and the Sneak Peek so as to have his state of mind treated as the state of mind of Nine Network.
2527 As the respondents submitted, the evidence establishes that Mr Steinfort was the person who decided what would be in the Broadcast. He scripted virtually the entirety of the Broadcast, anchored the Broadcast and provided his voiceovers. He made editorial decisions as to matters to exclude from the Broadcast, in conjunction with Ms Thomson. He then participated in a lengthy screening process, during which a team of people reviewed and fact-checked the story.
2528 As the respondents submitted, Ms Clancy’s evidence was that she was as responsible as everyone else in her team for the quality of the Broadcast. That team included editorial supervisors, but the responsibility for the Broadcast on a “day-to-day production level” was shared between Ms Clancy and Mr Steinfort. Ms Clancy said: Ms Thomson and Mr Taylor performed both administrative and editorial functions; that Ms Thomson had the ability to offer editorial views; but that Mr Steinfort was the “ultimate decision-maker” (although Ms Thomson could theoretically overrule him).
Section 4 — The journalists
2529 Ms Grieve, Mr Steinfort and Ms Clancy gave evidence for the purposes of establishing the s 29A defence.
2530 Ms Grieve initiated the respondents’ investigation of Dr Al Muderis’ practice and was the driving force behind it. That said, the applicant criticised all three journalists for engaging in a malicious campaign to destroy him, a campaign which extended to the evidence they gave in these proceedings. The criticism, in other words, was that the journalists’ evidence as to their intents and beliefs should not be accepted. In opening, the applicant submitted:
[W]hat your Honour will see … is evidence of a malignant, dishonest and malicious campaign by at least one journalist, Charlotte Grieve, and followed through by others who worked with her, Mr Steinfort and Ms Clancy. What we have seen is startling communications between the journalists, and in particular Ms Grieve, and sources for these stories that can only be described as single-minded in their pursuit to destroy [Dr Al Muderis].
2531 In closing, the crux of the applicant’s challenge to each journalist’s evidence was that each gave dishonest evidence as to their beliefs that publication of the matters was in the public interest.
2532 As is clear from the reasons below, I do not accept that submission. As the respondents submitted:
In the course of some 15 weeks of evidence … nothing was exposed that could be remotely described as a malignant, dishonest or malicious campaign against Dr Al Muderis.
2533 It is to be recalled that each of the journalists’ background and experience is described earlier in Part 1, Section 2 of these reasons.
Ms Grieve
2534 Justice Bromwich considered Ms Grieve as a witness during the hearing in relation to s 126K of the Evidence Act: Al Muderis v Nine Network Australia Pty Limited [2023] FCA 1623 (Al Muderis (No 1)). He accepted her evidence. I must make my own findings.
2535 Ms Grieve was cross-examined for five days. In my view, she gave evidence honestly and carefully. She was responsive to questions, making proper and sensible concessions where appropriate, in a context where she was protecting the identity of her confidential sources (as she was entitled to do). Contrary to his submission, Ms Grieve’s answers when she was questioned about identities of confidential sources the applicant had purported to discern, is not a failure to make proper concessions. That the applicant does not agree with her responses does not detract from that, and is in that context, of no moment. The cross-examination was, at times, very aggressive. Despite this, Ms Grieve maintained her composure and gave considered answers. The respondents’ submission that Ms Grieve “presented as credible, insightful and reasonable” accords with my assessment of her evidence. Although Ms Grieve has experience in investigative journalism and in June 2022, at the time of this investigation, had been appointed as a secondee in The Age’s Investigation Team, it is apt to describe her as being relatively new to investigative journalism.
2536 I accept Ms Grieve’s evidence. That she was relatively new to her role explains some of her actions and evidence which the applicant criticised. Considered in context, those matters do not diminish her credibility or reliability as a witness. I do not accept that Ms Grieve gave evidence dishonestly.
2537 The applicant submitted that Ms Grieve was dishonest in the preparation of her examination-in-chief, alleging that much of her affidavit evidence about why she found sources credible or not credible was disingenuous and incapable of belief. He submitted that several aspects of her conduct in preparing the Publications were deliberately dishonest and that her conduct in the investigation and preparation of the Publications “was beneath contempt”. He submitted that she deliberately destroyed evidence, knowingly published false material, did not believe what she was publishing was in the public interest, and in any event, her belief was not reasonable. The applicant put to Ms Grieve that she was “hell-bent on maligning” him and that she “wanted to utterly destroy him”. He submitted that the intent to malign him extended to Ms Grieve’s answers in cross-examination, with the proposition put to her that she was willing to do so “at every opportunity in the witness box”.
2538 The applicant has no onus to establish a motive for Ms Grieve (or the other respondents) in publishing the matters. That said, what is clear, is that his case is that Ms Grieve deliberately set out to malign him. Yet he advanced no motive for Ms Grieve or the respondents to malign him. There is no obvious motive for them to do so. Bearing in mind this is in the context where they were alert from the outset the applicant had a reputation for being highly litigious. They expected he was likely to bring legal proceedings. Mr Steinfort’s evidence was there had been multiple discussions with Ms Grieve to this effect, and that there was an anticipation he would be litigious. That tells strongly against the applicant’s assertions.
2539 I do not accept the applicant’s submissions. It does not accord with my assessment of Ms Grieve as a witness, having regard to her evidence, the evidence of the investigation and the Publications themselves.
2540 The applicant made many submissions directed to supporting the assertion that Ms Grieve deliberately and knowingly published false material. However, they appeared to generally fall within the following categories: (1) the articulation of unpublished allegations in relation to Dr Al Muderis in her affidavit; (2) ignoring positive or exculpatory statements; (3) misleading sources and otherwise failing to test the veracity of their claims; (4) criticism of her use of confidential sources; (5) the failure to inform Mr Steinfort and Ms Clancy of certain material; (6) the deletion of material ; and, (7) the publication of false statements.
2541 I have considered those submissions in reaching my conclusion about Ms Grieve. I address them in detail below, as they appear largely also to be directed towards Mr Steinfort and Ms Clancy and must be considered in their proper context.
2542 Nevertheless, there are two submissions which are directed to Ms Grieve’s evidence which are appropriate to refer to briefly at this stage.
2543 First, the destruction of documents. It was not in dispute that Ms Grieve destroyed material relating to her communications with several sources. The applicant submitted, inter alia, that the Court should make “a terrible finding” about her credit as a result. I address these submissions below: see Destruction of documents in Section 6. In sum, although her conduct was plainly imprudent, I do not consider it to undermine her credit as a witness or the respondents’ reliance on s 29A.
2544 Second, in so far as the applicant criticised Ms Grieve in her approach to answering questions about her confidential sources (particularly about their identities), I do not accept it undermines her credit as a witness or the respondents’ reliance on s 29A. Ms Grieve was entitled to protect her sources’ confidentiality: Al Muderis (No 1). That Dr Al Muderis claimed to have deciphered the identity of several of Ms Grieve’s confidential sources does not alter that. As Bromwich J observed in Al Muderis (No 1) at [56]:
There is a world of difference between the source being identified by other means, and a journalist being compelled to reveal it, including by way of any confirmation of a suspicion or belief to that effect.
2545 It is plain from the redactions to the documents that were intended to protect the identities of sources that Ms Grieve tried to redact as little as possible, to provide as much information as possible to the applicant. I elaborate on the use of confidential sources below: see Section 6.
Mr Steinfort
2546 The respondents submitted that Mr Steinfort was a very impressive witness. They submitted he presented as a responsible and insightful journalist who made reasonable concessions when warranted. He displayed a keen understanding of some of the nuances in the information uncovered by the respondents’ investigation and brought a high degree of common sense and emotional intelligence to his interviews and his evidence.
2547 I agree with that description. He gave evidence in a careful and considered manner, demonstrating an understanding of the material, and the nuances involved. He clearly explained his actions, including his approach to the interviews he conducted for the Broadcast. I accept his evidence.
2548 The applicant submitted, inter alia, that Mr Steinfort relied on the material given to him by Ms Grieve, without taking any real steps of his own to verify that material or conduct independent investigations. He submitted Mr Steinfort’s own contributions were inadequate or unreasonable, because: (1) his interviews (except for Dr Al Muderis’) merely provided the sources with a soapbox, instead of challenging their stories or interrogating them; (2) source interviews were edited in misleading ways; (3) he did not put all the allegations to Dr Al Muderis which were ultimately published, nor broadcast all his denials to allegations that were published; (4) he unjustifiably put to Dr Al Muderis an allegation of sexual harassment, which he knew to be false (I note this was not a matter referred to in the Publications); (5) he denied Dr Al Muderis the opportunity of giving further answers to questions; and, (6) he failed to interview any staff or doctors with current or recent experience working with Dr Al Muderis at the time of publication. The applicant identified aspects of Mr Steinfort’s evidence that ought not be accepted, including his belief that the Publications were in the public interest. I have considered the applicant’s submissions in relation to Mr Steinfort in assessing his evidence.
2549 I note at this stage, that the applicant’s submissions concerning Mr Steinfort contained several assertions not borne out by the evidence. It is sufficient to refer to several examples identified by the respondents. Contrary to the applicant’s submissions, Mr Steinfort did not accept that:
(1) he had very little experience in relation to medical stories. His evidence was: “I’ve covered medical stories in the past, but probably not to this step” and that he had covered “numerous medical stories”;
(2) the Articles misrepresented the benefits of osseointegration surgery (subject to one minor exception), with the passage the applicant cited for this submission being from Ms Clancy’s evidence, which I return to below. The exception, as explained below, appears in a different passage of Mr Steinfort’s evidence; and
(3) the Articles misrepresented osseointegration surgery. In the passage of evidence relied on by the applicant, Mr Steinfort responded that he “couldn’t disagree more” to the proposition put in cross-examination that the Publications “wholly misrepresented osseointegration surgery to the public to [his] knowledge”.
2550 Those misrepresentations by the applicant are significant. The erroneous propositions were part of the foundation for submissions as to why his evidence, including as to his belief, ought not be accepted.
2551 I address below the applicant’s criticism of Mr Steinfort’s interview with Dr Al Muderis and that he did not take any real steps to verify the information Ms Grieve gave him.
Ms Clancy
2552 Ms Clancy was cross-examined for considerably less time than Ms Grieve, or even Mr Steinfort. This may simply reflect the smaller role that she had in the preparation of the Publications.
2553 I accept her evidence. It was credible and reliable. She was careful and considered in her answers and made concessions where appropriate.
2554 As with Mr Steinfort, the applicant’s submissions in relation to Ms Clancy contain some propositions not supported by the evidence. As referred to above, the passage cited by the applicant in relation to the evidence as to the benefits of osseointegration relates to Ms Clancy, and not Mr Steinfort. That said, the passage is still inaccurate. Ms Clancy did not accept that the Articles misrepresented the benefits of osseointegration, but rather, when that proposition was put to her, she disagreed with it. She accepted that there was not “a whole lot of information about the benefits” of osseointegration in the Articles, before explaining: “the public interest in this story was … the problems with it, not the benefits. The benefits had been widely reported”. Contrary to the applicant’s submission, Ms Clancy’s evidence was not that she had “very little experience” with medical stories. Again, her evidence was to the contrary.
Section 5 — Summary of submissions
2555 The respondents submitted that they reasonably believed that the publication of each of the Publications was in the public interest. They submitted that Ms Grieve, Mr Steinfort and Ms Clancy gave detailed evidence about the investigation they conducted prior to the Publications, the preparation of the Publications, and the views and opinions they formed and held and continue to hold. They submitted that each journalist explained in cogent terms their reasons for considering that the Publications were in the public interest.
2556 The respondents submitted that the investigation was lengthy and detailed and that it revealed a very different side to Dr Al Muderis from the one he had cultivated publicly. They submitted the journalists uncovered, among other things:
(1) a significant number of patients who had experienced adverse outcomes as a result of their treatment by Dr Al Muderis;
(2) patients who were either too afraid to complain about Dr Al Muderis’ treatment due to fear of being sued for defamation, or who could not afford to bring legal action, or whose complaints to regulators had fallen on deaf ears;
(3) patients who had gone into surgery with Dr Al Muderis with unrealistic expectations, partly because of the positive media hype around Dr Al Muderis, partly because of the sales tactics and business practices utilised by Dr Al Muderis, and partly due to Dr Al Muderis not adequately informing them of the risks;
(4) medical professionals who believed Dr Al Muderis deviated from acceptable medical standards and expressed strong criticism about his practice; and
(5) serious issues with Dr Al Muderis’ conduct, including in relation to patient selection, advising in relation to risks, the provision of post-operative care and business and sales practices.
2557 The respondents submitted that the information Ms Grieve obtained from confidential sources, to the extent it was relied upon in the Publications, was corroborated by and consistent with information received from sources who were willing to go on the record. They submitted the information Ms Grieve obtained from the many patients was also corroborated by or consistent with information and opinions she received from a large number of expert medical practitioners (and has since been corroborated by various medical professionals and independent experts who the respondents called at the trial). They submitted the substance of the allegations was put to Dr Al Muderis during a detailed, fair and lengthy interview lasting almost two hours.
2558 They submitted in summary that:
These were stories that deserved to be told. The totality of the circumstances supports a conclusion that the respondents reasonably believed that the Publications were in the public interest. The respondents exercised editorial judgement and care in deciding what parts of the story to tell. Various serious and potentially career-ending defamatory allegations made against Dr Al Muderis were not included. The exercise of such judgement is wholly inconsistent with Dr Al Muderis’ assertion that the respondents were motivated by an unwavering desire to denigrate and inflict damage on him, or that they were part of a conspiracy to destroy him by concocting complaints.
2559 The applicant submitted that the defence is not established in relation to any of the Publications. In short, he submitted Ms Grieve’s conduct in the investigation and preparation of the Publications was “beneath contempt”, that she did not believe that what she was publishing was in the public interest, and, in any event, her belief was certainly not reasonable. Against that background, he submitted that the defence fails in relation to Ms Clancy given, amongst other reasons, her reliance on Ms Grieve and her materials. He submitted the defence fails in relation to Mr Steinfort for substantially similar reasons to Ms Clancy, but also because of his own contributions to the Publications.
2560 The applicant’s particular submissions varied. In addition to the above, they included criticisms relating to: the respondents’ use of, misuse of, and failure to use certain sources and materials; the respondents’ approach to interviewing sources (both on- and off-camera), including Dr Al Muderis; Ms Grieve misleading Mr Steinfort and Ms Clancy; and, the way in which the material was presented in the Publications.
2561 Although I address the applicant’s submissions in detail below, it is appropriate to address one submission at this stage – that the respondents had failed to prove the information they had before them at the time of the Publications – which he submitted is a precondition to establishing the defence.
Section 6 — Failures of proof
2562 The applicant submitted that proof of s 29A’s subjective and objective elements can only be tested upon disclosure of all the information the respondents held prior to publication, the steps they took to verify that information, and what they knew about the reliability of their sources. He submitted the Court must be satisfied that proper disclosure of such information has occurred. He also submitted that the respondents must fail on both aspects of s 29A because they had failed to prove, in any satisfactory way, what information each of them had at the time of the Publications. He alleged they failed to prove:
(1) the material available to them at the time of publication because they did not adduce evidence from a range of known sources;
(2) the material Ms Grieve made available to Mr Steinfort and Ms Clancy at the time of publication;
(3) the material available to them at the time of publication because Ms Grieve destroyed documents; and
(4) it was reasonable for the respondents to rely on the information confidential sources provided because the applicant could not fairly test evidence relating to those sources.
2563 I do not accept that the respondents’ reliance on s 29A is undermined for the reasons the applicant contends.
Evidence from known sources
2564 The applicant submitted that the s 29A defence must fail in relation to all respondents as they had failed to prove the information that they had from a range of known sources. He submitted many of those sources were called as witnesses in the truth case, providing a list of examples. He submitted the respondents did not adduce any evidence from these witnesses to support Ms Grieve’s evidence about what they allegedly told her. He submitted that, beyond the evidence these witnesses did give, the Court would infer from the respondents’ failure to adduce evidence, that these witnesses’ evidence about their conversations with Ms Grieve would not have supported her evidence. In support, the applicant cited Ferrcom. The submission was put at a very high level of generality.
2565 The submission is artificial. Most of these sources gave evidence as part of the respondents’ case to the same effect as what is reported in the Publications, and in those circumstances, there is no proper basis to draw any such inference, let alone in respect to each witness. Moreover, as already discussed above, there is no obligation on a party to produce corroborating evidence. In the circumstances of this case, I am not prepared to draw any adverse inference. Contrary to the applicant’s contention, I do not consider the respondents’ failure to adduce evidence in the way he described to be a basis for not accepting Ms Grieve’s evidence. Nor do I consider it impinges on the respondents’ ability to rely on the s 29A defence.
Material before Mr Steinfort and Ms Clancy
2566 The applicant highlighted that Ms Grieve made documents available to Mr Steinfort and Ms Clancy by uploading them to a Google Drive, and Mr Steinfort and Ms Clancy also reviewed briefing notes she prepared before interviewing sources. He submitted that the difficulty with this evidence is that it is apparent that the Google Drive and the briefing notes both continued to be added to, updated and amended from time to time after publication. He submitted the Google Drive tendered to the Court plainly includes documents which Ms Grieve did not obtain until after publication, such as documents relating to Mrs Gollan and Ms Mooney. He submitted the presentation of the evidence in this form means that there is no satisfactory proof of the material which was actually available to Mr Steinfort and Ms Clancy at the time of publication.
2567 I do not accept the applicant’s submissions. It is not in dispute that Ms Grieve gave Mr Steinfort and Ms Clancy access to a Google Drive containing many documents. The respondents conceded some of the documents in the Google Drive (as produced) were added post-publication, such as documents concerning Mrs Gollan, Ms Mooney and Ms Çalan. The evidence is that the three sources contacted and provided documents to Ms Grieve after publication. It is self-evident that, in this case, documents added to the Google Drive post-publication which Ms Grieve received post-publication do not affect the respondents’ reliance on s 29A (putting considerations of ongoing belief to one side). The applicant’s submission is to be considered in that context.
2568 The import of the applicant’s submission is that because there is some uncertainty as to the scope of the Google Drive pre-publication, the respondents’ evidence of the Google Drive’s contents at publication is wholly unreliable. I do not accept that submission. In submitting that the Google Drive had been altered since publication such that it is not clear what was actually available to Mr Steinfort and Ms Clancy at the time of publication, the applicant relies solely on the additional documents from Mrs Gollan and Ms Mooney, and evidence from Ms Clancy that the Google Drive and the briefing notes both continued to be added to, updated and amended from time to time after publication. He points to no other evidence, let alone any evidence that would affect the respondents’ reliance on s 29A. It is reasonably clear that the preponderance of the Google Drive’s contents, as produced, were those Ms Grieve provided to Mr Steinfort and Ms Clancy prior to publication. As the respondents submitted, excluding documents which were plainly added post-publication, there were approximately 660 pages of documents in the Google Drive covering matters relevant to Mr Hernandez, Mr Smith, Ms Todd, Mr Bruha, Ms Asch-Martin, GoFundMe campaigns, Mr Ford, Mr Urquhart and Ms Stewart (amongst other things).
Destruction of documents
2569 As mentioned earlier, it was not in dispute that Ms Grieve destroyed material relating to her communications with several sources. The applicant submitted that, as a result, the respondents failed to prove s 29A’s subjective and objective elements. It is apparent the submissions also sought to demonstrate that, in the alternative, Ms Grieve’s destruction of documents would tell against subjective and objective belief. I do not accept the applicant’s submissions on either alternative.
2570 The applicant submitted that a person who destroys documents faces the strongest possible inference against them. He relied on Allen v Tobias at 375 quoting The Ophelia [1916] 2 AC 206 at 229 (The Ophelia):
If any one by a deliberate act destroys a document which, according to what its contents may have been, would have told strongly either for him or against him, the strongest possible presumption arises that if it had been produced it would have told against him; and even if the document is destroyed by his own act, but under circumstances in which the intention to destroy evidence may fairly be considered rebutted, still he has to suffer. He is in the position that he is without the corroboration which might have been expected in his case.
2571 He urged the Court to draw an adverse inference that the material would not assist Ms Grieve. He submitted that, as a result, there is a failure to prove the totality of the material which was available to the respondents at the time of publication. In that context, he also submitted that the Court should make “a terrible finding” about Ms Grieve’s credit.
2572 As explained below, in the circumstances, I am not prepared to make any adverse finding against the respondents. I do not accept the applicant’s submissions on this point, including with respect to Ms Grieve’s credit.
2573 As is evident from the passage relied on, the principle articulated in The Ophelia requires the applicant to show that the respondents deliberately destroyed documents with “the intention to destroy evidence”. It is not enough to show that a respondent merely destroyed documents deliberately. Moreover, whether such an adverse inference will be drawn, and the strength of that inference, necessarily depends upon the circumstances of the case: Katsilis v Broken Hill Pty Co Ltd (1977) 18 ALR 181 at 197-198; Bridges v Pelly [2001] NSWCA 31 at [52]. Suffice to say, I do not accept that Ms Grieve destroyed documents with the intention to destroy evidence.
2574 The destroyed materials the applicant refers to fall into two categories. Their destruction was prior to publication, these proceedings, and any concerns notice being issued.
2575 First, Facebook messages Ms Grieve exchanged with Mr Hernandez and with Mr Grant, between approximately July 2022 and on or shortly after the 60 Minutes interview with Dr Al Muderis on 6 September 2022. Ms Grieve explained that she deleted her Facebook Messenger conversations with each after Dr Al Muderis told her on the sidelines of the interview that he thought they were responsible for the stories. She deposed that “[i]t was a knee jerk reaction … to protect Mr Hernandez and Mr Grant”. She said that in hindsight she wished she had not done so because she had nothing to hide. She said that she had forgotten about doing this until questions from her solicitors jogged her memory and the information was disclosed promptly.
2576 The respondents submitted that it was imprudent of Ms Grieve to have deleted the messages, but she did not do so dishonestly, and her credit is not adversely affected by having done so. They submitted that Ms Grieve was otherwise entirely forthcoming about her communications with Mr Hernandez and Mr Grant, about the fact that Mr Hernandez and Mr Grant each put her in touch with other sources, and that Mr Hernandez had a vested interest and animus towards Dr Al Muderis.
2577 The respondents submitted in reply that the applicant’s written submissions point to no document or evidence from which it could be inferred that the deletion of these documents, or the deletion of some of Ms Grieve’s audio recordings of conversations with sources, was “nefarious or had the effect of hiding relevant information from Dr Al Muderis or the Court”. Regardless of whatever may be contended to be the effect, the applicant has not suggested any reasonable basis, apart from the messages being deleted by Ms Grieve, as to why the deletion of these messages should be viewed as sinister. As the respondents submitted, it was apparent from Ms Grieve’s evidence that Mr Hernandez and Ms Grant put her in touch with other sources.
2578 During cross-examination, Mr Grant confirmed he too had deleted messages he had exchanged with Ms Grieve from 8 June 2022 until publication. He explained he deleted the messages:
… because I just didn’t think it was relevant. Obviously I didn’t know it was going to get to this. … you could have got them from her, so I have nothing to hide. … I would delete a lot of my text messages, if they’re not someone that I don’t really know – I will just delete them straight away after I send a text.
2579 When asked if Ms Grieve had spoken with him about deleting his messages with her, Mr Grant said he did not recall. When asked if Ms Grieve had told him about deleting her side of the conversation of the Facebook messages on or about 6 September 2022, Mr Grant replied: “No, we didn’t really speak about that. No, not that I recall”.
2580 Contrary to the applicant’s submission, although Ms Grieve was aware that Dr Al Muderis was litigious, it does not necessarily follow that she deliberately destroyed evidence in anticipation of legal proceedings. In the circumstances of this case, I do not accept the applicant’s submission. The applicant now accepts that Mr Grant is a credible witness, and he chose not to require Mr Hernandez for cross-examination. In the circumstances, I am not prepared to draw an adverse inference against the respondents, including that Ms Grieve deleted those messages because they contained information that would tell against them. I do not consider that a likely or plausible explanation. I accept her evidence that it was a knee-jerk reaction prior to the Publications to protect Mr Grant and Mr Hernandez. Her evidence was that she did this on or after the 60 Minutes interview, on or about 6 September 2022. She said she deleted it because Dr Al Muderis informed her on the sidelines of the interview that he thought Mr Hernandez and Mr Grant were responsible for the stories. That is, her motivation was the protection of their involvement, not that the contents of the documents would tell against her. Ms Grieve has been forthcoming in her evidence about her communications with Mr Grant and Mr Hernandez. Further, Ms Grieve has otherwise produced many documents in these proceedings, including documents that could be viewed as positive for the applicant.
2581 The applicant also relied on these deletions in support of the general assertion of Ms Grieve’s dishonesty. He submitted that Ms Grieve lied to Dr Al Muderis and Ms Reddin (his PR advisor) about the involvement of Mr Grant and Mr Hernandez in her investigation, and that the destruction of their messages was to cover up that lie. As explained above, I accept Ms Grieve’s evidence of the reason for her deletion of those messages. The applicant submitted that a person whose immediate response is to destroy evidence is not a person who one can rely on and questioned Ms Grieve’s explanation for the timing of her disclosure. I accept Ms Grieve’s explanation as to the circumstances of the disclosure, that she had thought she had disclosed everything until conversations with her solicitors jogged her memory.
2582 Second, the deletion of some of Ms Grieve’s audio recordings of conversations with sources. The respondents submitted that there was evidence that Ms Grieve recorded conversations with Confidential Source 2, Dr Rosenblatt, Dr Robert Turcotte (a Canadian surgeon who performs osseointegration) and likely Dr Jeffrey Cain (a patient of Dr Al Muderis from the United States). The respondents submitted that the recordings with Dr Rosenblatt and Mr Turcotte were produced by them in the discovery process. It has not been suggested that is incorrect.
2583 Ms Grieve conceded that she had deleted the recordings of her conversations with Confidential Source 2 and likely Dr Cain (Ms Grieve does not remember recording Dr Cain, but she accepted it was possible). Those two conversations were the subject of Ms Grieve’s notes which were produced and are in evidence.
2584 The respondents submitted that these conversations being the subject of Ms Grieve’s notes in evidence is inconsistent with a desire to conceal the substance of the conversations. They submitted the suggestion that Ms Grieve deleted recordings to conceal information that was exculpatory of Dr Al Muderis should not be accepted. I agree that Ms Grieve’s conduct, particularly the retention of those notes, is inconsistent with any sinister motive. I note that Dr Cain contacted Ms Grieve because of a request from one of Dr Al Muderis’ staff, and in respect to him, the applicant does not suggest that Ms Grieve’s notes are not an accurate representation of what she was told during their conversation.
2585 I am not persuaded in the circumstances that the recordings in those limited cases were deleted because they contained information adverse to the respondents’ case, or that it was done for any adverse reason. In that context, I do not accept it constitutes a failure of proof.
2586 Moreover, given my findings in respect to the deleted material, I do not accept that Ms Grieve’s conduct affects the respondents’ subjective belief or its objective reasonableness for the purposes of s 29A.
2587 Given the above, and the evidence of the investigation, I do not accept, as the applicant contended, that the Court should speculate from Ms Grieve’s deletions as to what else has been destroyed.
Use of confidential sources
2588 The respondents relied on confidential sources in their investigation.
2589 As with the destruction of documents, although the applicant’s submissions on this point were directed to his inability to fairly test evidence relating to the respondents’ confidential sources (such that the respondents failed to prove that it was reasonable to rely on the information they were provided), he also sought to criticise the respondents’ reliance on confidential sources. That is, he appeared to submit that, in the alternative, the respondents’ use of confidential sources tells against establishing subjective or objective belief. However, the use of confidential sources by itself does not necessarily tell against the defence being established, although, depending on the circumstances, it may well impact on a respondent’s ability to do so.
2590 The applicant submitted that investigative journalists should usually use confidential sources sparingly. He submitted that people who do not have to publicly put their name to the allegations can avoid scrutiny through anonymity. He submitted that while there are some exceptions, sources who insist on confidentiality are generally less credible because they are unwilling to stand by their allegations publicly, and a journalist should therefore approach them with caution. He referred to Nine’s Editorial Code of Conduct and clause 3 of the Media, Entertainment & Arts Alliance Journalist Code of Ethics.
2591 He submitted that Ms Grieve did not accord confidentiality sparingly but rather used an extraordinarily high number of confidential sources. On his account:
In addition to the 23 confidential sources listed in her affidavit, at the time of publication Dr Elton Edwards, Professor Ian Harris, Professor Michael Leung, David Lee-Gow, Geoff Todd, Helen Kennedy, Mitch Grant, Shane Mortimer and Matthew Ames were also confidential sources.
2592 He submitted that because of the refusal of his series of applications which were directed towards obtaining material to enable him to test that evidence (see Al Muderis (No 1); Al Muderis v Nine Network Australia Pty Limited (No 2) [2024] FCA 136 (Al Muderis (No 2)), the applicant has been denied procedural fairness in testing Ms Grieve’s evidence about her communications with these sources. He submitted that the confidential sources were not merely background information, and that Ms Grieve relied on them directly in the Publications. He criticised Ms Grieve for taking objection even to “anodyne” questions about sources. The applicant submitted that as the evidence cannot be fairly tested it is not safe for the Court to conclude that it is reliable. He further submitted that the Court has no means of knowing whom the confidential sources were or making any kind of informed assessment of whether they were reliable or whether it was reasonable for the respondents to rely on them, citing Duma at [237], [277]-[295], [417]-[420].
2593 The applicant’s submissions must be considered in context.
2594 Ms Grieve did consult a high number of confidential sources. Yet, as Mr Steinfort correctly pointed out, this needs to be viewed in the context of the “extremely large” number of sources in total, including an unusually large number of people who spoke on the record. That is a logical consideration, as sheer numbers, absent context, are misleading.
2595 Mr Steinfort did not accept the proposition put to him in cross-examination that, irrespective of the reasons for seeking confidentiality, a person who is not to be held to account publicly by having their name disclosed is more likely to lie, given they would not have to face the consequences of that dishonesty. However, he properly accepted that a journalist must be more careful with confidential sources than others. He explained that a desire for confidentiality is not necessarily driven by a nefarious motive, and there are many reasons why a person may seek anonymity, including that they may be under threat. Indeed, several of Ms Grieve’s sources told her they held concerns in speaking with her for fear of being sued by Dr Al Muderis.
2596 It is appropriate to recall that s 29A(3)(f) stipulates that a court may take into account that:
… if a source of the information in the matter published is a person whose identity is being kept confidential, whether there is good reason for the person’s identity to be kept confidential (including, for example, to comply with an applicable professional code or standard).
2597 The applicant did seek to have the identities of some, but not all, of the confidential sources revealed. The application before Bromwich J in Al Muderis (No 1), was confined to 13 sources identified as health professionals, with the claims of confidentiality in relation to the lay sources never being challenged (there being 23 confidential sources at that time). The respondents identified that 21 remain confidential sources with two agreeing to be identified. Of the lay sources for whom no application was made, two fall within the description of “colleagues, former colleagues or otherwise had first-hand experience of Dr Al Muderis”.
2598 Justice Bromwich was satisfied that 12 of the 13 sources held fears of disclosure which constituted an adverse effect on them for the purposes of s 126K(2)(a): at [185]-[212] (although the respondents could not identify any specific adverse consequences CS-16 would suffer, the applicant failed to discharge the onus of establishing that the public interest in disclosure of CS-16’s identity outweighed the public interest in non-disclosure: at [212], [266]). His Honour accepted the confidential sources feared various adverse effects, including being sued by Dr Al Muderis, being bullied by Dr Al Muderis, reputational damage, and damage to their practice: at [185]-[211].
2599 Justice Bromwich was not satisfied to order disclosure of the confidential sources’ identities. His Honour explained that the applicant did not establish that any public interest in the disclosure of their identities outweighed the combination of the likely adverse effect of that disclosure on a given source (except CS-16), and the public interest in the ability of the news media to access sources of facts, and in the communication of facts and opinion by the news media to the public: at [307]. His Honour did not accept the applicant’s submissions in relation to his asserted centrality of the confidential sources to the Publications or to the defences directed to the pleaded imputations: at [273], [280]. His Honour explained at [280] that the “confidential sources are far from central to the defences relied upon by the respondents”.
2600 The subsequent application, Al Muderis (No 2), related to the applicant issuing subpoenas to seven persons for the purpose of establishing their identities as confidential sources. As I there explained, the subpoenas were an abuse of process as they attempted to circumvent Bromwich J’s ruling. His Honour’s orders were not the subject of appeal. I note there was a natural hiatus after that hearing (between the first and second tranches of evidence), so to do so would not have fragmented the judicial process. I note also that the applicant flagged before me that he may seek to reagitate his s 126K application if circumstances changed. That never occurred.
2601 The respondents submitted that it was plain from the cross-examination of Ms Grieve that there was nothing in Ms Grieve’s description of her sources that had caused Dr Al Muderis to labour under any misunderstanding or misapprehension as to the positions held by any of the sources. They submitted that, in every case, Ms Grieve identified each source either by reference to their occupation or their status as a former patient or colleague of Dr Al Muderis. Ms Grieve properly conceded CS-7 ought not to have appeared in her affidavit under the heading “Medical practitioners”. The applicant contended he knew the identity of that person, in any event. That said, as the respondents pointed out, contrary to the applicant’s submission, her affidavit did not claim that the person was a “surgeon” and there was nothing in the evidence to suggest that her intention was to mislead Dr Al Muderis or the Court.
2602 The applicant’s submission about his inability to test the reliability of Ms Grieve’s confidential sources is also to be considered in the context of him claiming he knows many of their identities, that the identities of some were never sought, and that on the evidence, the respondents corroborated the confidential sources’ allegations. I note in this context, that although the applicant alleged that Mr Laux is a confidential source, he was called as a witness for the applicant, yet he led no evidence on that topic from him: see [341]-[346].
2603 The issue regarding the use of confidential sources is relevant to both the subjective and objective limbs of s 29A.
2604 I accept the respondents’ submission that the evidence establishes that the information provided by Ms Grieve’s confidential sources used in the Publications was corroborated in one way or another by on-the-record sources: see Sections 7 and 8 below. As the respondents submitted, “no central allegation, in any of these publications, relied entirely upon something which had been provided by a confidential source”. It is plain Ms Grieve’s preference was to have sources speak on the record. Ms Grieve’s evidence was that she would deploy the promise of not disclosing the identity of many sources, at least initially, to overcome fears, concerns or a general reluctance to speak. As explained below, Ms Grieve was conscious of the need for supporting evidence, such that information obtained about several topics was not published because the respondents considered there was insufficient evidentiary support.
Section 7 — The respondents’ investigation
2605 The context of the investigation is important, and bears repeating. The nature and extent of the investigation provides evidence relevant to subjective beliefs and the reasonableness thereof for the purposes of s 29A.
Genesis of the investigation
2606 The genesis of the investigation is Ms Grieve’s father, Mr Grieve. It will be recalled that he is a left below-knee amputee and was a witness in these proceedings: see Part 6, Section 2.
2607 In June 2018, Mr Grieve attended a function at the Australian Club, where Dr Al Muderis gave a speech. He approached Dr Al Muderis afterwards, and the two briefly discussed osseointegration. Mr Grieve attended a consultation with Dr Al Muderis to discuss the procedure further on 25 October 2018.
2608 Ms Grieve deposed:
Shortly after the consultation with Dr Al Muderis, my father informed me at that consultation, he was told by Dr Al Muderis that if he does not have osseointegration surgery, his condition would deteriorate and he would be in a wheelchair within a matter of years. My father said to me that he felt Dr Al Muderis seemed quite nonchalant about the risks of the surgery. Following this, my father sought second opinions. He was told by his prosthetist and others that he did not need the osseointegration surgery, that it was not an appropriate procedure to have done at his age, and that the risks outweighed the benefits. My father did not go through with the surgery.
… It was a casual conversation that stuck in my mind. It has always been something that stayed in the back of my mind and something I thought I might look at in the future.
2609 She said the conversation occurred in a context where she “had a very positive impression of Dr Al Muderis – to me he was an inspiring figure and a great refugee success story”, having first become aware of him in or around 2016.
2610 In mid-2022, Ms Grieve joined The Age’s investigations team. In late May, as part of her transition to the team, she prepared a list of possible investigation subjects. One of those subjects was: “Munjed Al Muderis patients with complications (Sydney prosthetists, former patients, experts)”. Before joining the team, she met Mr Bachelard, the editor of the investigations team, to discuss the list. He indicated that he was interested in her investigating Dr Al Muderis’ osseointegration surgery. She then spoke with her father again in more detail about his consultation with Dr Al Muderis and procured contacts from him, including Mr Laux.
2611 I note that, separately, at some time in 2018 or 2019, Ms Clancy was working as a producer for A Current Affair when she received an anonymous tip-off that Dr Al Muderis was mistreating his staff and may have been involved in improper billing practices. She communicated with several people, including Mr Hernandez, Mr Bob Lye and Mr Grant. She said that although she thought there was potentially a story, not enough people were willing to go on the record.
2612 The applicant put to Ms Grieve that because of the position of Mr Grieve, she had a conflict of interest in investigating Dr Al Muderis. I address this issue below. Suffice to say, I do not consider that the position of Mr Grieve undermines Ms Grieve’s credit, or the respondents’ subjective or objective belief.
The investigation itself
2613 The respondents in closing described the investigation that followed. It was, on any account, a major investigation:
Between late May and 30 June 2022, Ms Grieve conducted an exhaustive investigation into Dr Al Muderis. She watched Dr Al Muderis’ previous appearances on 60 Minutes, Foreign Correspondent and Ahn’s Brush with Fame, reviewed a number of legal judgments involving him, reviewed documents relating to his litigation against Fred Hernandez, conducted ASIC and title searches relevant to Dr Al Muderis and his business, read his books, reviewed documents received from Mr Hernandez regarding the recall of dual cones, and spoke to approximately 50 sources, which included 25 surgeons, doctors, nurses, academics or prosthetists and 20 of Dr Al Muderis’ former patients.
Ms Grieve formed the view that the story was significant and she mentioned to Mr Bachelard that it might be conducive to a collaboration with 60 Minutes. A meeting was arranged on 22 June 2022. Ms Grieve prepared a briefing document for the purposes of that meeting. The briefing document recorded Ms Grieve’s thoughts on what the Broadcast might involve. She had in mind at the time that it would include interviews with at least three of Dr Al Muderis’ patients and at least one expert surgeon. She identified the themes that the Broadcast should explore: whether, behind the scenes, there was a different story to Dr Al Muderis’ glittering reputation; the dichotomy between those patients for whom Dr Al Muderis is a “messiah”, and others whose lives were destroyed; allegations involving inappropriate patient selection, inadequate disclosure of risks, abandoning patients, silencing complaints, a toxic workplace culture, cut-throat business tactics, patients being made to feel like numbers and patients forced to crowd-fund or mortgage their homes to pay for surgery, while Dr Al Muderis enjoys luxury cars, boats and expensive property. The document also identified a number of allegations that the Publications ultimately did not pursue: sexual harassment and “fudging of figures”. 60 Minutes was interested. Mr Steinfort and Ms Clancy were assigned to the investigation and agreed to start conducting on-camera interviews with sources.
Between 30 June 2022 and the date of the Publications (18-19 September 2022): (a) Ms Grieve spoke to a further 26 sources, including 8 surgeons, doctors, nurses, academics or prosthetists and 10 of Dr Al Muderis’ former patients (including former patients in Iraq and Cambodia); (b) the respondents conducted recorded interviews with Mr Urquhart, Mr Smith, Mr Bruha, Mr Hernandez, Cindy Asch-Martin, Shona Stewart, Dr Anstee, Dr Chris Rudge, Dr Tetsworth, Dr Al Muderis and Ms Grieve; (c) Ms Grieve read various academic papers, including papers authored by Dr Al Muderis; (d) Mr Steinfort and Ms Grieve read hundreds of pages of scientific papers provided to them by Dr Al Muderis; (e) Ms Grieve sought information or comment from the Australian Health Practitioners Regulation Agency (AHPRA), the Australian Medical Association, the NSW Ministry of Health, the Medical Council of NSW, the Royal Australian College of Surgeons, the New York State Health Department, the New York State Education Department, the Office of Professional Medical Conduct in New York, the Arizona State Ombudsman, the New York State Medicine Board, and the Arizona Medical Board; and (f) Ms Grieve made enquiries of the NSW Coroners Court.
…
By the conclusion of their investigation, the respondents had spoken to approximately 76 sources (23 of whom were confidential – 21 remain confidential), and reviewed thousands of pages of emails, business records and scientific papers.
2614 I generally accept that description of the investigation.
Section 8 — The material before the respondents
2615 The respondents provided an aide memoire in closing submissions summarising the information they obtained during their investigation (Aide Memoire 2), arranged by reference to the ten defamatory stings (as articulated by the respondents: see Part 5, Section 2). They submitted that while the aide memoire “is not intended to be exhaustive”:
It demonstrates the sheer breadth of the respondents’ investigation, the wealth of corroborative information they received from confidential and on-the-record sources and, ultimately, the reasonable basis the respondents had for their view that the Publications were in the public interest.
2616 Having read and considered the material before the respondents (together with the parties’ submissions), I accept that this aide memoire accurately depicts the evidence of the information garnered from the investigation, except for some minor items – primarily aspects of Ms Grieve’s second affidavit which were not read in these proceedings (being relevant to the s 126K hearing as they relate, inter alia, to fears of sources, or complaints made). I note also some entries where the paragraph references to Ms Grieve’s affidavit are incorrect, although the entry itself is supported by the different references referred to or elsewhere in her affidavits.
2617 Given its volume, it is impractical and unnecessary to describe all the material that was before the respondents at the time of the Publications. The aide memoire is plainly not exhaustive. Although a useful guide or summary, it cannot reflect the extent or breadth of the material. Nonetheless, it does illustrate the respondents’ submission referred to above, that the confidential sources used in the Publications were corroborated in one way or another by on-the-record sources. The applicant made no submissions addressing the aide memoire despite having had the opportunity to do so.
2618 In addition to the aide memoire, in their written submissions the respondents provided a summary of material before them at the time of the Publications, also arranged by reference to the ten stings. I accept that summary is generally accurate. Again, the applicant made no submission directed to these passages. It is convenient to recite as it summarises the number of sources on each topic (the contents of footnotes in the submissions identifying the sources referred to are noted in square brackets at the relevant juncture):
Patient selection. There were 39 separate sources of information about Dr Al Muderis’ approach to patient selection. These included 21 doctors or prosthetists; 11 people who were colleagues, former colleagues or otherwise had first-hand experience of Dr Al Muderis (Confidential Source (CS) 5, Dr Rosenblatt, Dr Kumar, Shona Stewart, Dr Al Maawi, Dr Aschoff, CS 15, CS 19, Dr Stoita, Mr Hernandez and Mr Grant), and a number of former patients. The information provided was almost uniformly consistent: Dr Al Muderis’ approach to patient selection had slackened over time, to the point where he now regularly agreed to perform osseointegration on patients who were not suitable candidates.
Ms Grieve read the decision in Ford v Narrabri Shire Council [2022] NSWPIC 119. Contrary to propositions that were put to her in cross-examination, the judgment was critical of Dr Al Muderis personally: see [184]–[186], [192]–[194]. The gist of the criticism was that Dr Al Muderis had been pre-occupied with giving Mr Ford a chance to walk and had not given sufficient consideration to his comorbidities, rehabilitation prospects and the risks of surgery. Those criticisms were consistent with views expressed to Ms Grieve about Mr Ford’s case by a number of sources [CS 1 (orthopaedic surgeon), CS 2 (plastic surgeon), CS 16 (surgeon)]. Sources also provided consistent information regarding Dr Al Muderis over-prescribing osseointegration [CS 1 (orthopaedic surgeon), CS 2 (plastic surgeon), Professor Harris (orthopaedic surgeon), Dr Anstee (plastic surgeon), Dr Leung, CS 6 (foot and ankle surgeon), Dr Ellis (orthopaedic surgeon), CS 11 (orthopaedic surgeon), CS 12 (prosthetist), Dr Horst-Heinrich Aschoff (orthopaedic surgeon), Mr Frances (prosthetist), CS 15 (prosthetist), CS 19 (researcher)], targeting the vulnerable veteran community [CS 1 (orthopaedic surgeon), CS 3 (paediatric orthopaedic surgeon), CS 4 (orthopaedic surgeon), CS 6 (foot and ankle surgeon), CS 7, Dr Ellis (orthopaedic surgeon), CS 19 (researcher)], operating on smokers [Dr Rosenblatt (orthopaedic surgeon), Ms Stewart, CS 12 (prosthetist), Dr Al Maawi (resident-Doctor), CS 13 (prosthetist), CS 15 (prosthetist), CS 16 (surgeon)] and children [CS 1 (orthopaedic surgeon), CS 3 (paediatric orthopaedic surgeon), CS 16 (surgeon)], and his decisions to operate on Mr Urquhart [CS 1 (orthopaedic surgeon), CS 2 (plastic surgeon), Dr Anstee (plastic surgeon), CS 5, Dr Leung (plastic surgeon), Ms Stewart], Mrs Todd [CS 1 (orthopaedic surgeon), CS 7], and an anorexic patient [CS 1 (orthopaedic surgeon), CS 6 (foot and ankle surgeon), CS 11 (orthopaedic surgeon)].
Disclosure of risks. There were 20 separate sources of information about Dr Al Muderis’ approach to disclosure of risks. These included 7 doctors or prosthetists; 3 people who were colleagues, former colleagues or otherwise had first-hand experience of Dr Al Muderis (Shona Stewart, CS 19 and Mr Hernandez), and 10 former patients (including Mr Hernandez). The information provided was consistent: Dr Al Muderis habitually failed to disclose or downplayed the risks and complications of osseointegration surgery, including the risk of persistent infection, hypergranulation and pain. Some sources alleged that Dr Al Muderis had gone so far as to manipulate research and reporting of complications – allegations which the respondents did not publish.
False promises / misleading patients. The respondents received information from 19 sources on this topic. They included 5 doctors or prosthetists; 3 people who were colleagues, former colleagues or otherwise had first-hand experience of Dr Al Muderis (Shona Stewart, Mr Grant and CS 5) and 11 former or prospective patients (including Mr Grant). The consistent image presented was that Dr Al Muderis engendered false expectations in his patients, particularly in relation to post-surgical outcomes such as reduced pain, incidence of infection and hypergranulation, and the efficacy of TMR.
Improper sales tactics. The respondents received information from 16 sources on this topic. They included 6 doctors or prosthetists; 3 people who were colleagues, former colleagues or otherwise had first-hand experience of Dr Al Muderis (Shona Stewart, Mr Grant and Mr Hernandez) and 8 former or prospective patients (including Mr Grant and Mr Hernandez). Recurring themes in the information provided included patients being encouraged to fundraise, patients having to re-mortgage their homes or drain their superannuation to pay for surgery, patients being pressured in Dr Al Muderis’ waiting room by other patients who extolled the virtues of osseointegration surgery, offering patients payment plans, and paying commissions to Mr Hernandez to refer patients.
Prioritising money / reputation / fame / numbers. The respondents received information from 38 sources on this topic. They included 15 doctors or prosthetists; 6 people who were colleagues, former colleagues or otherwise had first-hand experience of Dr Al Muderis (Shona Stewart, Dr Rosenblatt, CS 15, CS 19, Mr Grant and Mr Hernandez) and 16 former patients or prospective patients (including Mr Grant and Mr Hernandez). The information provided was multi-faceted. A large number noted that Dr Al Muderis was litigious and voiced their concerns about being sued by him. This information, coupled with the information the respondents had from court judgments where Dr Al Muderis had sued former patients or business associated (including Mr Hernandez and Gerardo Mazzella), contributed to a picture of Dr Al Muderis as a person who prioritises the management and cultivation of his reputation, including by the curation of his public image on Facebook [e.g. CS 6 (foot and ankle surgeon), CS 12 (prosthetist), CS 18 (anonymous patient 2), Mr Urquhart, Mr Hernandez, Mr Grant]; who is motivated financially (including by reason of profiting from both the performance of surgery and ownership of the implants) [e.g. Dr Anstee (plastic surgeon), CS 4 (orthopaedic surgeon), CS 6 (foot and ankle surgeon), CS 7, Dr Rosenblatt, Ms Stewart, CS 19, Mr Urquhart, Mr Smith, Mr Hernandez]; and who treats patients as numbers [Dr Leung (plastic surgeon), Ms Stewart, CS 17 (anonymous patient 1), Mr Urquhart, Ms Mattiske].
Negligence in the operating theatre. The respondents received information from 17 sources on this topic, including 8 medical practitioners. The information provided ranged from allegations that Dr Al Muderis performs surgery for which he is unqualified (TMR, children, hands and shoulders), to specific examples of negligent surgery: Mr Urquhart, Mrs Mooney, Mrs Todd and Mr Mortimer.
Abandoning patients. The respondents received information from 21 sources to the effect that Dr Al Muderis had abandoned some of his patients. They included 13 former patients who expressed feelings of abandonment.
Negligent post-operative care. The respondents received information from 26 sources on this topic, including 8 medical practitioners or prosthetists. The concerns raised were almost uniform: a habitual failure on the part of Dr Al Muderis to provide, manage and oversee adequate rehabilitation and post-surgical care, including management of complications such as maggots, infections, hypergranulation, odour, and faulty dual cones.
Performance of surgery in USA. The respondents received information from Dr Rosenblatt, Mr Hernandez and Ms Schaeffer to the effect that Dr Al Muderis provided medical services in the US, despite not being licensed to do so.
Poor treatment of staff. The respondents received information from 10 sources on this topic, including 6 colleagues, former colleagues or persons with first-hand experience of Dr Al Muderis (Shona Stewart, CS 5, Dr Kumar, CS 19, Mr Grant and Mr Hernandez).
(emphasis in original)
Section 9 — The interview with Dr Al Muderis
2619 As part of the investigation, Mr Steinfort interviewed Dr Al Muderis for nearly two hours on 6 September 2022. Parts of the interview were included in the Publications (primarily in the Broadcast, the Articles, and to a lesser extent, the Grieve Video). Ms Grieve, Ms Clancy and Dr Al Muderis’ PR advisor, Ms Reddin, were present.
2620 The applicant criticised Mr Steinfort’s conduct in relation to the interview. He submitted that: when Ms Grieve was drafting an email to invite him for an interview Mr Steinfort intervened so that the email gave him less warning of the nature of what he would be asked during the interview; when Mr Steinfort did interview him, he did not put to him all of the allegations about him which were ultimately published, or broadcast all of the denials he gave; during the interview, Mr Steinfort unjustifiably put an allegation of sexual harassment to him, even though he knew that this allegation was false; and, Mr Steinfort denied him the opportunity of giving further answers to questions.
2621 Mr Steinfort’s evidence was that after the interview had finished, Dr Al Muderis wanted to stay around and have a friendly chat with the team, which Mr Steinfort found surprising given the serious nature of the allegations put to him. Mr Steinfort believed, given the conversation that ensued, that Dr Al Muderis wanted to tell them things he did not want to say on the record. He deposed that, during this time, Dr Al Muderis disparaged several of his own patients as aggrieved and mentally ill, singling out Mr Urquhart as an example, and said words to the effect that Mr Hernandez was “a piece of work and not to be trusted”. Mr Steinfort, Ms Grieve and Ms Clancy each gave evidence that, during this time, Dr Al Muderis explained he had expected everything that Mr Steinfort had asked. After about 15 minutes, the post-interview conversation ended amicably.
2622 There are several issues to be addressed relating to the interview.
2623 First, although not every allegation was put to Dr Al Muderis, I accept the respondents’ submission that the substance of the allegations in relation to each of the defamatory stings that were the subject of the Publications was fairly put to him, and the substance of his responses was included in the Publications. So much is evident from a consideration of the interview and the Publications. This is also reflected in a non-exhaustive list of the allegations put to Dr Al Muderis, and the responses included in the Publications set out in Aide Memoire 3 to their closing submissions. I note that Dr Al Muderis declined to answer questions about specific patients, which, as a matter of fact, impeded the respondents from putting allegations to him.
2624 The applicant submitted that, when Mr Steinfort interviewed Dr Al Muderis, it was inadequate or unreasonable for him to not put to Dr Al Muderis “all” of the allegations about him which were ultimately published, or to broadcast “all” of the denials that Dr Al Muderis gave to allegations that were published. That submission does not sit with Parliament’s manifest intention with respect to s 29A, having regard to its text, context, and purpose. Section 29A(3)(g) provides:
… the court may take into account … whether the matter published contained the substance of the person’s side of the story and, if not, whether a reasonable attempt was made by the defendant to obtain and publish a response from the person.
(emphasis added)
2625 Moreover, the object of the Defamation Act which the public interest defence is aimed at promoting, per s 3(b) is:
[T]o ensure that the law of defamation does not place unreasonable limits on freedom of expression and, in particular, on the publication and discussion of matters of public interest and importance.
2626 And see the Explanatory Note, recited at [2502] above.
2627 As to whether the respondents made a reasonable attempt to obtain and publish a response from Dr Al Muderis, Mr Steinfort’s cross-examination was as follows:
Ms Chrysanthou: I’m going to put to you that in the course of that interview, you did not put to him all of the allegations that were ultimately broadcast.
Mr Steinfort: We endeavoured to.
Ms Chrysanthou: And you certainly did not put to him all of the allegations that found themselves in the articles that ended up with your byline on them?
Mr Steinfort: I don’t think so.
Ms Chrysanthou: You agree with that, or you disagree?
Mr Steinfort: That we didn’t put them all to him?
Ms Chrysanthou: Yes?
Mr Steinfort: I mean, to be perfectly honest, I don’t recall every allegation that was in the articles. But I would probably believe that to be true.
Ms Chrysanthou: And had you known that your name was going to go on the articles, in your experience as a journalist, you would have wanted to have put everything to him in those articles prior to publication, wouldn’t you?
Mr Steinfort: Where possible.
Ms Chrysanthou: And to be fair, as fair as possible?
Mr Steinfort: We did – we went above and beyond to be fair.
Ms Chrysanthou: Yes. But if you had understood
Mr Steinfort: If we did not want to be fair, we would not have offered an interview.
2628 Mr Steinfort explained that he gave Dr Al Muderis every opportunity to respond, and he could have sent through any follow-up statement (as Mr Steinfort had been emailing Ms Reddin prior to the interview). Ms Grieve gave evidence to the same effect.
2629 Second, Dr Al Muderis was aware prior to the interview that it was not going to be a “puff piece” but was to address both positive and negative aspects of osseointegration. So much is apparent from his response after the interview, where Mr Steinfort deposed Dr Al Muderis said words to the effect of: “There was nothing you asked that I was not expecting.” Moreover, Dr Al Muderis’ evidence was that Mr Laux warned him in early June 2022 that the story stood to be negative, and that he hired Ms Reddin in that context.
2630 Although Dr Al Muderis now claims he was surprised by the questions asked during the interview, I accept the evidence of Mr Steinfort, Ms Clancy and Ms Grieve. It is consistent with the fact he had prepared for the interview. He had hired Ms Reddin as, on his evidence, he had not faced these “kind of circumstances before”. Ms Grieve’s evidence was that while with them Dr Al Muderis postulated theories as to who was behind the story. It is apparent that Dr Al Muderis was conscious of optics, parking his car some distance away from the location of the interview so it could not be photographed or recorded. Indeed, it was put to Mr Steinfort in cross-examination that Dr Al Muderis knew what to expect because patients and staff members who had spoken to Ms Grieve had told him what they had been asked. Dr Al Muderis had spoken to Ms Asch-Martin before she was interviewed. I note that although the applicant filed an affidavit from Ms Reddin, he did not call her to give evidence.
2631 Mr Steinfort, Ms Clancy and Ms Grieve each denied the proposition that they intended to mislead Dr Al Muderis as to what the interview was about.
2632 That Dr Al Muderis was not told specific questions or topics in advance, or patient names, is not to mislead as to the nature of the interview. As Mr Steinfort explained, there was an obvious risk that advance notice of questions would afford Dr Al Muderis and his PR team an opportunity to prepare pre-scripted answers. This is in a context where the respondents were concerned that if they provided him patient names, he would contact them. As explained by Mr Steinfort:
This is a man who has a history of calling up people that have spoken negatively about him, and we had people that were, as you’ve said, with their own mental health issues, emotionally drained. We didn’t need them having more pressure applied to them by Dr Al Muderis calling out of the blue to say, “I hear you’ve done an interview. Hey, what’s all this about?”
2633 Ms Grieve gave evidence to similar effect:
We were a bit worried about naming specific patients ahead of the interview because … I was concerned that he might – or they felt he might … intimidate them … I knew he was calling around sources, trying to get them to change their story or whatnot.
2634 On the evidence, I accept the respondents’ submission that that was a legitimate concern. This is in a context where the investigation revealed some of the sources would only speak on a promise of confidentiality because of fears they held, and others who did speak on the record expressed concerns that there may be retaliation. As published in the Broadcast, Dr Al Muderis did telephone Ms Stewart asking, “what’s going on?” (when he was aware she had spoken to a journalist). In any event, Dr Al Muderis’ response after the interview – where he explained he had expected everything Mr Steinfort had asked – makes it clear that he was not misled.
2635 Third, Dr Al Muderis requested, through Ms Reddin, a second interview. The request was put on the basis that Dr Al Muderis was “happy to arrange another time to meet to discuss not only osseointegration (where the first interview was pitched), but complications, maggots, nerve pain; everything to do with the treatment”. Mr Steinfort explained the reasons for refusing the request:
… there would have to be the most extraordinary extenuating circumstances to consider that … the simple fact is that you would come back with scripted answers to all of the questions. … you wouldn’t cross-examine me and then two days later say, “Come back. Let’s do it all again. We will discount the first ones and now you know what’s coming. Here’s – you can have another go at it.” … He had ample time, endless time, limitless, to answer on the day all of these issues. The idea that he would then get to come back four days later and have thought up a perfectly worded answer to everything … it’s just fanciful to suggest that’s how it would work.
2636 That explanation is an understandable one. When subsequently challenged, he explained that he regarded Dr Al Muderis “as a man of great intellect and as such there were no questions on that day that he did not have the capacity to answer”. Mr Steinfort gave evidence that he had assistance from Ms Reddin, who would interject during the interview and attempt to reframe questions. It can be inferred, including from Dr Al Muderis’ evidence, that he had prepared in advance. Indeed, it would be startling if he had not in the circumstances.
2637 Fourth, it was put to Mr Steinfort and Ms Grieve in cross-examination that the method of providing patients’ consent to Dr Al Muderis for him to discuss their cases by way of pre-recorded videos was a stunt designed to ambush Dr Al Muderis. The applicant submitted that it demonstrates that the respondents had no interest in giving him a fair opportunity to respond, they instead wanted to make the Broadcast more sensational. Mr Steinfort accepted he could have made further inquiries as to what was legally necessary to provide consent. However, it does not follow that consent provided in this way was not a genuine attempt to do so, and to enable Dr Al Muderis to be given the opportunity to address the allegations. Mr Steinfort explained:
… in a rushed time frame, I made a decision based on what would be the most easily digestible version for Dr Al Muderis, that these patients gave consent … I had thought … that if I showed a signed piece of paper, the response would be, “That could have been signed by anyone.” Whereas I thought a video was a much clearer demonstration for [Dr Al Muderis] that these people gave permission for him to discuss their cases.
2638 That is a logical explanation, and a reasonable one. Indeed, when Dr Al Muderis said he could not discuss patients without written consent, Ms Grieve immediately sought written consent from Mr Urquhart. Again, this demonstrates a desire to put the allegations to Dr Al Muderis.
2639 I note, as the respondents pointed out, despite Dr Al Muderis’ concerns of patient confidentiality during the interview, he did speak of some patients in a disparaging way after the interview. For example, Mr Steinfort deposed Dr Al Muderis “said that Mark Urquhart had a mental illness and had other issues he was dealing with”. That Dr Al Muderis was willing, at that stage, to discuss Mr Urquhart’s medical issues is inconsistent with his assertions during the interview of having to maintain patient confidentiality.
2640 Mr Steinfort rejected the suggestion that he had no intention of giving Dr Al Muderis a proper opportunity to respond to the allegations, including because of the time between the interview and intended publication. He rejected the contention that the content of the Broadcast was already set in stone. As explained above, Dr Al Muderis could have sent through any follow-up statement. Mr Steinfort explained that:
… we were very interested in hearing what Dr Al Muderis had to say … when he could disprove one of the allegations or a number of the allegations, we took that on board and removed it from the broadcasts.
2641 Having interviewed Dr Al Muderis, he was considered to have been an evasive and unimpressive interviewee. I agree that the respondents were entitled to form that opinion, and there remained a public interest in publishing many of the allegations against him following the interview. Moreover, Dr Al Muderis’ evasiveness was reflective of Mr Steinfort’s belief that the Publications were in the public interest, in that “he has gone out of his way to try and keep [the horrible cases] out of the limelight for so long”.
2642 I am satisfied that a genuine, honest and reasonable attempt was made to put the defamatory allegations to Dr Al Muderis, and that the substance of his responses was included in the Broadcast and Articles. I also accept the respondents’ submission that there is nothing connected with their conducting of the interview that would permit a finding that that they did not honestly and reasonably believe the Publications were in the public interest.
Section 10 — The Publications as a joint investigation
2643 The Publications were presented as a joint investigation. Mr Steinfort, in introducing the Broadcast, describes it as a “joint 60 Minutes, The Age and Sydney Morning Herald investigation”. Later in the program he says, “The Age and Sydney Morning Herald’s Charlotte Grieve has been working with us on this joint investigation”. The Articles provide a similar description, both on the front page, and in the subsequent text. The Age Article provides, for example, “Now a joint investigation by The Age, The Sydney Morning Herald and 60 [M]inutes has uncovered a darker side of Al Muderis’ lucrative practice”. The Articles ultimately invite readers to “Watch Charlotte Grieve, Tom Steinfort and Natalie Clancy’s 60 Minutes report on 9Now”, with the Online Articles hyperlinking the Broadcast.
2644 The parties’ submissions do not address how, if at all, the fact of the Publications being presented as a joint investigation impacts the s 29A assessment.
2645 That said, the assessment cannot be approached on the assumption that a viewer or reader of any one of the Publications will consume more than one matter. To the contrary, it is necessary to consider each matter individually, albeit in all the circumstances. That said, it does not follow that the assessment is necessarily in isolation. For example, the applicant’s submission that a journalist dishonestly published a statement in a particular publication, may be informed by what was published on that topic in the other Publications. That is, it is unlikely a journalist would have acted in the way alleged where, noting this is a joint investigation, that topic is also addressed in another publication in an unchallenged manner, given the Publications invite attention to each other.
2646 The principal Publications are the Broadcast and the Articles. They utilise vastly different mediums. The Grieve Video is a short video embedded in the Online Articles. The Sneak Peek is an online video advertisement, and the content would be considered by the viewer in that context. That is, not expecting or understanding that it was in any way complete. It is fair to describe that very little attention during the trial or closing submissions was directed to the Sneak Peak or the Grieve Video publications.
2647 I note that given s 29A is a defence, the assessment of a matter does not fall for consideration unless the matter is established as defamatory. That is done by establishing the alleged imputations are conveyed, which as explained above, I was not so satisfied in relation to the Sneak Peek. I return to this topic below.
2648 Before leaving this topic, it is appropriate to address the applicant’s submission about the byline to the Articles. Mr Steinfort and Ms Clancy did not know they were to have a byline until the publication of the Articles. The applicant asserted that The Age Company and Fairfax have published (and continue to publish) the Articles containing a serious misrepresentation about authorship. He was not aware of this until Mr Steinfort gave evidence about it during cross-examination in the trial. The applicant submitted that:
These were front page stories and Ms Grieve was a junior journalist. Misrepresenting to readers that Tom Steinfort was also an author gave credence to the allegations because of his standing and reputation as a journalist on 60 Minutes. No witness has been called to explain that lie. No documents have been tendered in which it is discussed or explained. That misrepresentation, which continues to this day, deprives the Age Company and Fairfax of the s 29A defences. It is not in the public interest to mislead readers about authorship of a front page article, claiming to be a “special investigation” and an “exclusive”.
(citations omitted)
2649 Mr Steinfort rejected the proposition that his name was included in the byline because he was a more recognisable, reputable and experienced journalist than Ms Grieve. The obvious basis of attribution is that the Publications were the result of a joint investigation. As the respondents submitted:
The Articles were, in part, a product of the various interviews conducted by Mr Steinfort. Those interviews were partly a product of Ms Clancy’s work as a producer and she contributed directly to some of the interviews by asking or suggesting questions that were pursued. Quotes from some of the interviews (in particular, the interview with Dr Al Muderis) feature prominently in the Articles. It was, in these circumstances, appropriate (and neither sinister nor dishonest) for Mr Steinfort and Ms Clancy’s names to appear in the by-lines. The submission that “no witness has been called to explain that lie” is also wrong. Mr Steinfort squarely explained that he was given a by-line because quotes from his interviews were used in the Articles.
2650 I do not accept the submission that the byline was a dishonest attempt by The Age Company and Fairfax to mislead its readers. The Articles plainly incorporate work done by Mr Steinfort and Ms Clancy during the joint investigation.
Section 11 — Some issues relevant to subjective belief
2651 The emphasis of my consideration in this section is on subjective belief. However, as will be apparent, the consideration at times extends to the reasonableness thereof. Moreover, my consideration as to subjective belief is not confined to this section.
2652 Each of Ms Grieve, Mr Steinfort and Ms Clancy gave evidence that they believed the publication of the matters was in the public interest. Noting that I have found the journalists to be witnesses of credit, I accept their evidence and their description or characterisation of that public interest. In reaching that conclusion, I have considered the applicant’s submissions described in more detail below: see Section 13. I am satisfied that the respondents have established the subjective element of s 29A in respect to each relevant Publication.
Journalists’ descriptions of the public interest
2653 The journalists’ descriptions of the public interest centred around a belief that the information then available to the public of Dr Al Muderis’ practice was critically incomplete. The positive media coverage his practice had enjoyed needed correcting; the investigation revealed, as the Articles described, “a darker side” of his practice. A number of Dr Al Muderis’ patients had negative experiences with significant similarities. It was something the public, especially prospective patients, needed to be informed of given the nature of his practice and osseointegration surgery.
2654 I note that the journalists at times referred to their belief that each Publication was in the public interest using the present tense. It was nevertheless plain they were doing so to give evidence that such beliefs existed from at least the time of publication (i.e. that they were not formed post-publication). It was equally plain that evidence of those beliefs, though given in the past tense, was not intended to suggest that those beliefs had ceased.
2655 Ms Grieve deposed:
I believe that a lot of Dr Al Muderis’s patients go into his surgery with unrealistic expectations. That is partly because of positive media hype around Dr Al Muderis and the surgery he performs. It is partly because they are vulnerable people and susceptible to pressure tactics. It is also partly because Dr Al Muderis doesn’t explain or emphasise the risks to them properly. I believe it was important those matters were addressed.
I believe patients should be making decisions with both sides of the story, not just the good news story Dr Al Muderis and others have told.
2656 In cross-examination she said:
… these questions … around, well, if the majority are happy, does that negate the experiences of the few that are not, and is that unfair to focus on people who, you know, have had really bad outcomes when, as Dr Al Muderis says, the majority are happy. But we ultimately formed the view that, because the outcomes for the patients where it had gone wrong were so significant, and appeared to have systemic similarities in terms of the failures of Dr Al Muderis along the way, that those were worthwhile exploring, even if they were a minority …
2657 Mr Steinfort explained:
There were numerous points throughout the story where we pointed to the great work that he’s done. I don’t deny that he has done some amazing things in his lifetime, and changed many lives for the better. The point that we were making is the one that no one, up until that period of time had made, and that is that there are significant complications, lifechanging effects. And this is what’s in the public interest here, that just needs to be really focused on, is the fact that, yes, no one denies he has done amazing things, but there are horrible cases. And this is what he has gone out of his way to try and keep out of the limelight for so long. And these are uncomfortable truths, I don’t deny that. But there are numerous people, be they patients or medical colleagues, who say that this man operates beyond what is ethically and morally acceptable and what is responsible as a surgeon.
…
I would say that the story that had been told up until this point was not the full story. And we were here to show that there is another side to this story. And a side to the story that people absolutely need to know, especially those people who already have health challenges, making big decisions on how their life might pan out, and whether they would undergo this surgery. … I would say that there had been an exceptionally disproportionate level of coverage of the negative outcomes of his work as opposed to the positive.
2658 Ms Clancy’s evidence was to a similar effect: “… the public interest in this story was … the problems with it, not the benefits. The benefits had been widely reported.” She deposed:
I believe that the publication of the broadcast would help to inform future patients by putting more information on the public record, particularly information about the risks of osseointegration surgery.
2659 The journalists offered further explanations for why they believed the Publications were (and remain) in the public interest. This evidence is not to be considered in isolation and is against the backdrop of their evidence above. Some of these explanations, as set out below, can properly be described as consequences, in the public interest, that might flow from the Publications.
2660 First, the Publications sought to improve outcomes for Dr Al Muderis’ patients and others. Ms Grieve deposed:
I was aware that former patients of Dr Al Muderis were not receiving adequate care after surgery. I believed the story might draw awareness to that and result in them receiving better care. This might happen either by spurring Dr Al Muderis to take better care, by prompting regulators to take action, or by encouraging other doctors to assist. Further, many patients believe Dr Al Muderis is the only doctor qualified to conduct this surgery. The story alerted patients that there were alternative options and reminded patients of the importance of getting second opinions.
2661 Mr Steinfort deposed:
I believed there was a chance that the airing of these negative stories in the Publications would make Dr Al Muderis be a better doctor and provide better services to his patients. On this, I emphasise that I bear Dr Al Muderis no ill will. I hope that he continues to be able to perform surgeries. But I want to make sure that Dr Al Muderis does this with the utmost care for his patients.
I hope that reporting on these issues will make Dr Al Muderis reconsider the way he looks after vulnerable people who come to him for help and how he runs his practice.
2662 Ms Clancy deposed:
I believed that the Publications might cause Dr Al Muderis to provide better care to his patients in future and thereby result in better patient outcomes. I also thought other doctors might also learn from the story and provide better care to their patients.
2663 Second, Ms Grieve deposed:
I felt that the patients harmed by their interactions with Dr Al Muderis had no recourse. Complaints to regulators fell on deaf ears. Legal cases were too expensive and legal fees outweighed any damages so there was no point in bringing them. Yet these people were facing life altering consequences. I felt the media was in many ways the last forum that these serious concerns could be aired. I was aware that patients were nervous about defamation because Dr Al Muderis had successfully sued at least one patient in the past. I had been told Dr Al Muderis had also made legal threats to one former patient in New Zealand. This was a common issue that arose with former patients. Most were fearful of being sued.
2664 Mr Steinfort explained that the Broadcast:
… was about saying … there is a significant cohort [of patients] that feel like [Dr Al Muderis] has failed them, and these people deserve a voice. They feel silenced, they feel voiceless, and they need to be heard.
2665 Third, the Publications sought to address the dangers of mixing fame and business with medicine and surgery. Ms Grieve deposed:
Dr Al Muderis had the cult of celebrity and patients were being drawn into that. It is important to explore how that affects health outcomes. …
The story looked at the effects of aggressive business tactics and marketing tactics in medicine, and whether that led to good health outcomes.
I also wanted to explore how conflicts of interest are managed in the medical industry. Dr Al Muderis owns the patent for the osseointegration implant, so makes a profit each time he prescribes the treatment. Patients are informed of this in writing – but were they encouraged to explore other implant systems not owned by Dr Al Muderis? How are these conflicts managed?
2666 Mr Steinfort deposed:
It seemed to me many people perceived Dr Al Muderis to be motivated by “a numbers game” in that he tried to do as many procedures as possible. It seemed that as a result, after the procedures he would cut corners. Some patients I spoke to speculated Dr Al Muderis was driven by money and by fame but they all felt the level of care post procedure was not up to scratch. …
I was also concerned with the issues surrounding promotion of medical work and extremely serious surgeries. I was also concerned with Dr Al Muderis’s use of PR teams and the use of financial incentives for former patients to promote Dr Al Muderis’s work.
2667 Fourth, the Publications also sought to raise and discuss informed consent and the balance of power between surgeons and patients. Ms Grieve deposed:
The story also raised questions about informed consent and the duty doctors have. There is an enormous power imbalance between the surgeon and the patient, especially when the operation is complex and has life altering consequences. At what point does a patient provide informed consent, and at what point is the surgeon making a value judgment for the patient? I believe surgeons have a duty not just to inform patients but to warn them of serious risks.
2668 Fifth, the Publications sought improvement for Australia’s medical regulators, which the respondents perceived as deficient. Ms Grieve deposed:
I also wanted to look at the competence of medical regulators. I was concerned that when legal cases were brought and settled out of court that was the end of the matter – regulators didn’t continue to investigate as they should. I was concerned that when the regulator did take action against Dr Al Muderis following a complaint (by forcing him to undergo further education), that was kept secret and there was no public record of the matter.
2669 Mr Steinfort deposed:
I believed and still believe that regulators are not doing enough for people who have concerns or complaints about people in the medical profession. I believed and still believe that patients do not have enough recourse when doctors do not provide them sufficient treatment and care. The conduct of Dr Al Muderis raised and raises questions of whether, if some sort of regulatory authority had intervened or taken action against him, some patients may not have suffered in the way that they have.
2670 Ms Clancy gave evidence to a similar effect.
One-sided media coverage
2671 As apparent from the passages recited above, the respondents’ evidence reflects that they believed that the public interest in the Publications was in a context where the benefits of osseointegration surgery had been publicised, and Dr Al Muderis had enjoyed overwhelmingly positive media coverage. As Mr Steinfort explained:
… all the stories that I saw, really pointed to this halo effect of a man who was performing miracles. And there seemed to be little to no … insight into what happens when it goes wrong.
2672 There had at that time been, what the respondents described as, one-sided media coverage of Dr Al Muderis. The evidence reflects that up until that time, there had been positive media coverage.
2673 It is convenient to address the applicant’s submissions on this point.
2674 The applicant appeared to take issue with the respondents’ description as the 60 Minutes segment “The Surgeon and the Soldier”, discussed one of Dr Al Muderis’ patients having committed suicide after the surgery. However, that program was filmed before his patient died, with his parents wishing for it still to be published. In that context, Dr Al Muderis provided a further interview. The end of the segment also referred to “Munjed’s miracle surgery [having] eased [the patient’s] physical pain”. That publication did not portray Dr Al Muderis other than in a positive light.
2675 Further, the applicant cast the meaning of the previous positive media coverage very differently. The applicant submitted, for example, that as Mr Steinfort had reviewed earlier publications about Dr Al Muderis (e.g. the Inside Story episode lauding Dr Al Muderis’ visit to Cambodia), he must have been aware of material which contradicted what was published in the Publications. That is, the applicant submitted the previous publications, far from providing a context for a belief in the public interest in this story, demonstrated the falsity of the Publications.
2676 This submission presumes the earlier publications accurately and exhaustively portrayed Dr Al Muderis’ practice. It proceeds on the basis that these earlier publications cannot be challenged. To take the Cambodia trip as an example, the episode says nothing about the difficulties the Cambodian patients experienced after their contact with Dr Al Muderis, where the evidence in these proceedings reflects a lack of understanding by them of the procedure. Nor does the episode say anything about the applicant’s practice in relation to other patients (domestically and internationally).
2677 Mr Steinfort gave evidence of his experience as to how positive media publications can come to be produced. In cross-examination he referred to previous “PR campaigns” conducted by Dr Al Muderis which resulted in the publication of positive stories. He was subsequently challenged:
Ms Chrysanthou: Now, when you talk about PR campaigns, you’re talking about, aren’t you, repeatedly, positive media articles about [Dr Al Muderis]?
Mr Steinfort: Yes.
Ms Chrysanthou: Positive media articles done by serious journalists, to your knowledge?
Mr Steinfort: Yes.
Ms Chrysanthou: And it’s not a PR campaign, is it, if a serious journalist has decided to take up an issue about a person and write about it, don’t you agree?
Mr Steinfort: I disagree. They can be framed by PR representatives, who do everything in their power to put forward all the positive elements and make zero effort to put forward the negative elements.
Ms Chrysanthou: And in circumstances where independent and competent journalists wrote stories, including people from your employer, about Dr Al Muderis, that does not amount, does it, on any understanding of the word, to your knowledge, as a PR campaign?
Mr Steinfort: In the media industry, I think there are times, it’s safe to say, that people will be pitched a story that would be described as a heartwarming or a positive story, and in such an instance, I think there’s less effort made to make sure that there isn’t a darker side to it. Often … people are searching for good news, and I think often people will be pitched a good story and think, “That’s nice. That will make people feel nice and share a positive message in the community”, and as such, perhaps, don’t quite do the depth of research for this, because they see it as … a human interest story and a positive story, and they want to focus on the positives … when you’re only being pitched positives, sometimes, people don’t think to examine the negatives.
2678 Mr Steinfort explained his basis for believing PR agents were assisting Dr Al Muderis, was his knowledge of and experience in the industry, having worked in the industry for decades. As he said, in preparing the Broadcast, his team dealt with Dr Al Muderis through his PR agent, Ms Reddin, who had told him she had worked for Dr Al Muderis for some time prior. Dr Al Muderis’ evidence was Ms Reddin was a PR agent who he had engaged to assist him from time to time “in the past” and for the Broadcast. Mr Steinfort knew that Dr Al Muderis had had multiple PR representatives.
2679 Given the information that Mr Steinfort had, and his experience, his view that there was a PR campaign to promote positive stories about Dr Al Muderis was not unreasonable: see e.g. Russell at [363].
2680 Before leaving this topic, it is appropriate to refer to one other program, the ABC Foreign Correspondent program in 2017 titled “Machine Man”. As explained above, the applicant submitted that the content of these previous publications contradicted the information the respondents had obtained during their investigation.
2681 A clip from that program formed part of the Broadcast. It showed Ms Nasser, a patient from Iraq. As apparent from that clip, Dr Al Muderis told Foreign Correspondent that: “If we do osseointegration for her she will walk, for sure. She has a very high chance that she will be a very high-performing amputee”.
2682 The Broadcast then shows Mr Steinfort saying:
Despite those assurances from Dr Al Muderis, five years after he and the cameras left, this is Amane Nasser now. Her osseointegration a failure. She’s since had the surgery reversed.
2683 I note in the Foreign Correspondent episode, Dr Al Muderis is also heard saying “I can make her walk” while standing in front of Ms Nasser, seemingly talking to her and the rest of his medical team and showing her a video on his phone of a person walking with osseointegration implants. This statement, as with the passage shown in the Broadcast, was said by Dr Al Muderis in a confident manner, as if there was no question that the surgery would be successful.
2684 Ms Grieve described Ms Nasser’s case as:
… a very stark example of when, what is on the public record is a very rosy picture and a very certain assurance. And when you contrast that to the reality, just merely by looking at Instagram, it’s a very different story.
2685 Ms Grieve’s evidence was that she understood, from publicly available information and Instagram messages with Ms Nasser, that she was able to walk with aids for a short period but has since had complications and her implants removed, where she is now confined to a wheelchair. That fact is not challenged.
2686 This case is a stark illustration of what Ms Grieve described (regardless of whether Ms Nasser walked with crutches for a limited time). The footage from the Foreign Correspondent segment also reflects the information available to the respondents, including from the applicant himself, about what was promised to patients. Dr Al Muderis assured Ms Nasser, that he “can make her walk”. To the journalists and camera operators while being filmed in the hospital in Iraq, he further assured them that Ms Nasser would walk, and that there was “a high chance that she would be high performing”. It is difficult to understand how such assurances can be made, given the nature of the surgery. They present a very rosy picture to the patient. The Foreign Correspondent segment does not contradict the information the respondents obtained during their investigation. Rather, it highlights the importance of the issue, given the information the respondents received from several patients. Where that information included downplaying risks, with the surgery presented in an overly positive light, this segment illustrates how Dr Al Muderis communicates with prospective patients.
Mr Steinfort’s and Ms Clancy’s reliance on Ms Grieve
2687 The applicant submitted that Mr Steinfort’s and Ms Clancy’s reliance on Ms Grieve’s work, and their failure to verify it, meant that their s 29A defences must fail. It was put to them that it was not reasonable for them to have relied on her work. The submission implied that to establish the defence, Mr Steinfort and Ms Clancy must have checked all the facts themselves. That, in a joint collaborative investigation such as this one, is unnecessary and unrealistic. The Publications were the product of a collaborative process across different mediums, with each of the three journalists having distinct roles and responsibilities. The practical import of the applicant’s approach would require Mr Steinfort and Ms Clancy to, in effect, redo the investigation. That submission is unsustainable: see Russell at [387].
2688 Plainly, Mr Steinfort and Ms Clancy had direct knowledge of the matters in the Broadcast. They also gave evidence that they satisfied themselves of, amongst other things, Ms Grieve’s thoroughness and diligence in the investigation in relying on the materials she provided. I accept their evidence. Mr Steinfort explained:
I’ve never seen such diligent briefing background research as I have with Charlotte. She was thorough, meticulous and I’ve worked with many producers over the years. I’ve never received as many briefing documents, background information, sources, attributions. Charlotte was exceptional in the way that she went about it.
2689 He rejected suggestions in cross-examination that Ms Grieve was inexperienced or lacked objectivity. He said he had “ultimate confidence in” their work together “because of things that she has done that I have worked on with her. She has been diligent, accurate, fair and concise”. He trusted her to provide him with the material he needed. I note that Mr Steinfort’s evidence was that he conducted his own research. For example: he conducted online research to educate himself about Dr Al Muderis and other subjects he intended to interview, including patients; he read documents in the Google Drive provided by Ms Grieve; he reviewed much of the scientific papers Ms Reddin provided on the eve of the interview; he read some of Dr Al Muderis’ promotional material; he watched some of Dr Al Muderis’ previous television appearances; he conducted all the recorded interviews and scripted most of the Broadcast; and, he participated in a lengthy screening and editing process.
2690 In cross-examination, Ms Clancy denied the suggestion that she did not have sufficient knowledge about Ms Grieve to trust her journalism: “I trusted Charlotte’s journalism, and I also knew that the types of allegations they were making were consistent with other patients who we had spoken with”. She rejected the suggestion that Ms Grieve was not objective. Her evidence was that Ms Grieve acted consistently with that of a responsible journalist.
2691 Contrary to the applicant’s submissions, I do not accept that Mr Steinfort’s and Ms Clancy’s reliance on Ms Grieve undermines their beliefs as to whether the Publications were in the public interest, or the reasonableness of those beliefs. Nor do I accept the applicant’s submission that Mr Steinfort knowingly failed his own standards by not checking Ms Grieve’s assertions, such that he did not reasonably believe the Broadcast, or the Articles, were in the public interest. The applicant submitted that Mr Steinfort agreed that:
He needed to go over all of the information and see for himself if it was the truth. In particular, he needed to see for himself what the patients’ stories were and if he believed that they were genuine.
2692 The applicant cited a paragraph of Mr Steinfort’s evidence in support. As is plain from that paragraph, the applicant does not accurately represent Mr Steinfort’s evidence:
Before [the joint investigation], I didn’t know Charlotte at all and had not had any experience working with her. For this reason I was cautious and thought I needed to go over all the information and see for myself if it was the truth, but the more I spoke to people and interrogated people … I formed the view that it did all seem to stack up.
(emphasis added)
2693 Mr Steinfort and Ms Clancy played a smaller role in the development of the Articles relative to the Broadcast. It is apparent neither journalist participated in drafting the Articles (although they were shared with them before publication), and they did not know they would be attributed in the bylines before publication. They were not aware of all the information that featured in the Articles. Both Mr Steinfort and Ms Clancy explained that they were nevertheless satisfied that the Articles were in the public interest and emphatically rejected the suggestion that they were not able to form that view.
2694 I do not accept that Mr Steinfort’s and Ms Clancy’s belief that the publication of the Articles was in the public interest, including their beliefs as to the accuracy of its contents, are affected by their reliance on Ms Grieve. Each clearly described the reasons why that was so. They explained (and I accept) there was considerable overlap between the material in the Broadcast and the Articles, and their confidence in Ms Grieve was justified given their collaboration in respect to the Broadcast. For those reasons and given that the allegations peculiar to the Articles were consistent with those in the Broadcast, I do not accept that their reliance on Ms Grieve affects the reasonableness of their beliefs.
2695 As the respondents submitted, citing Russell at [387], the reasonableness of each respondent’s belief must be assessed in the context of their respective degree of participation in each of the Publications and the extent of their knowledge of the reliability of sources.
2696 On the evidence in this case, the fact that Mr Steinfort and Ms Clancy did not verify each of the facts in the Publications themselves, does not undermine the evidence of their belief that there was a public interest in the Publications, or the reasonableness of that belief. I accept their evidence.
The Sneak Peek
2697 The applicant submitted that the Sneak Peek was an advertisement, sensational, and not a piece of investigative journalism. He submitted that no truthful journalist would believe that it was in the public interest and that, to the extent that the respondents gave that evidence, it was disingenuous.
2698 Mr Steinfort and Ms Clancy explained that, although the Sneak Peek was an advertisement, they believed it was in the public interest because it pointed viewers to a fuller piece (being the Broadcast) that was in the public interest. Mr Steinfort likened it to a headline in a newspaper. The respondents submitted that the Court should find that the respondents reasonably believed there was an ancillary or attendant public interest in the publication of the Sneak Peek. I accept that was their subjective belief.
Section 12 — Some issues relevant to objective belief
2699 Although the focus of the applicant’s submissions on the public interest defence was on the subjective element, the principal issue, in my view, is whether it has been established that the subjective beliefs are objectively reasonable. In my view the following factors weigh in favour of the objective belief being established in respect to the Publications. That said, these factors address issues which have been considered in respect to my findings on both aspects of s 29A (i.e. subjective and objective belief). Further, my consideration as to objective belief is not confined to this section. I have considered the applicant’s submissions described in more detail below: see Section 13. As earlier explained, very little submissions were directed by the parties to the Sneak Peek and the Grieve Video, with the Broadcast and the Articles being the primary focus.
2700 First, the objective public interest in the subject of the Publications is pronounced. As the respondents submitted, the allegations concerned matters of public safety in connection with Dr Al Muderis’ performance of osseointegration surgery, a complex, niche, invasive and inherently risky form of surgery which leaves patients with a lifelong, open wound (a stoma). Osseointegration is an elective surgery. It services patients who are likely to be vulnerable. This is also in a context where, as the respondents contended (and I accept), the media coverage on Dr Al Muderis (and osseointegration surgery) to date had presented a one-sided picture, which emphasises or heightens the objective public interest in this topic. That accords with the material they had.
2701 The allegations also implicate the public’s perception of Australia’s healthcare system and its surgeons. As Dr Anstee explained in his interview with Mr Steinfort: “The place that I enjoy in society is because I and most other practitioners look after patients as well as they can. That goodwill [will] dry up if we don’t.” He elaborated, when giving evidence:
Nothing ever goes perfectly all the time, and I think that we, as surgeons, should appraise the public of that. We don’t ever want my profession or your profession to be regarded … as a conspiracy against the public, and the way to avoid that is to have the public fully informed.
2702 That said, when addressing a submission directed to the degree of public interest in a matter, Lee J observed in Russell at [347]:
… there is not some sliding scale which means the greater the public interest in the matter, the greater the margin for error in what is published. To embrace this notion would distort and oversimplify the requirement to make a value judgment about whether the impugned publication was in the public interest by reference to all relevant circumstances. The extent of public interest is relevant to making such allowances for editorial judgment as is appropriate but does not overwhelm the evaluative assessment.
2703 Second, the extent and breadth of the investigation and sources. By the time of the Publications, the respondents had spoken to an array of sources and reviewed thousands of pages of documents: see [2613], [2618]. The sources spoken to included medical professionals affiliated and unaffiliated with Dr Al Muderis (such as surgeons, doctors, nurses, and prosthetists), his current and former patients, his colleagues and employees, academics, and Dr Al Muderis himself. The respondents obtained or attempted to obtain information from medical regulatory bodies here and abroad. The detail of the investigation and extent of it is recited above.
2704 Third, the journalists’ approach bespeaks a desire to attempt to verify information. They relied on the complaints of multiple sources which, for all intents and purposes, are corroborated expressly or by implication (as illustrated by Aide Memoire 2). The respondents sought to obtain corroborative documentary evidence where possible. That approach is reflected in Ms Grieve’s email to Ms Todd after a call: “As discussed, please send through as many photos and other documents related to your experience here or via text. I’m trying to build up as much evidence as possible.” It lends support to the credibility of the information obtained.
2705 Fourth, the evidence reflects that during the investigation and in making the decisions as to publication, the respondents were conscious of the need to assess the credibility and reliability of the witnesses and information they received. It reflects a responsible approach to investigative journalism. They were conscious that honest witnesses may be unreliable (by considering matters such as mental health). They tested witnesses who were prima facie unreliable or lacked credibility. They were cognisant that sources may have had improper motives, and to the extent it was apparent that they did, the respondents sought to test them (see e.g. [2870]-[2876]) or sought material to corroborate the information provided (see e.g. [2860], [2866]). As the respondents submitted:
[Ms Grieve’s] nuanced consideration of the motivations and reliability of her sources was evident time and again during [her] evidence and speaks to the reasonableness of her belief that the Publications were in the public interest. Mr Steinfort gave similarly nuanced evidence about Ms Stewart’s motivations.
2706 That approach extended to confidential sources. As explained above, it is plain Ms Grieve’s preference was to have sources speak on the record. Nevertheless, the respondents were cognisant of the challenges of relying on confidential sources, taking care to corroborate their claims. The evidence reflects that Ms Grieve would ask off-the-record sources if she could be connected to others who may be able to verify their claims, including where she was unable to procure corroborative documents. As is reflected in her text to one confidential source: “Can you connect me with others who might be able to verify? It’s hard to publish anonymous claims without documents”. She would push confidential sources for means of verification where they were unwilling.
2707 As described below, many allegations that arose from the information gathered during the investigation were not published, either because the respondents did not consider they had sufficient evidence to support them, or considered they were not in the public interest. This reflects a level of assessment of the information obtained, and a discrimination between what was sufficient or appropriate to publish and what, in the circumstances, was not: (see further Unpublished allegations in Section 13 below).
2708 As with the applicant’s submissions in respect to the truth defence, his submissions on the public interest defence approaches questions of credibility and reliability in a simplistic manner. It is based, among other things, on considering the patients and other sources in isolation, and on the reasoning that if a patient is unreliable about something in one respect, they are necessarily unreliable generally. It is also premised on the fact that if the patient was mobile for any time, their surgery was a success (such that no complaint can reasonably be made, or entertained), including if shown on earlier media publications purportedly then contradicting the material obtained by the respondents (such that the witnesses are not credible or reliable). His submissions also failed to grapple with the breadth and nature of the information obtained. There was a raft of sources with information being obtained from a diverse set of cohorts, and many sources within each of those cohorts.
2709 Fifth, much of the information relied upon could reasonably be considered as credible per se, including documentary evidence (see e.g. Mr Hernandez’s contract at [2860]) and case law.
2710 Ms Grieve’s reliance on Ford is illustrative. Contrary to the propositions put to Ms Grieve in cross-examination, that judgment was critical of Dr Al Muderis personally. The criticism is consistent with the view expressed by some of Ms Grieve’s sources about Mr Ford’s case, and generally with views expressed to her about Dr Al Muderis’ patient selection. As the respondents submitted, the gist of the criticism was that Dr Al Muderis had been pre-occupied with giving Mr Ford a chance to walk again and had not given sufficient consideration to his rehabilitation prospects and the risks of the surgery: Ford at [184]-[186], [192]-[194]. The decision in Ford details, inter alia, the medical condition of Mr Ford and the various reports from relevant experts. The criticism is to be read in that context.
2711 Sixth, although Dr Al Muderis is not a public official, the allegations concern public activities, in the sense of surgery being performed on members of the public, particularly on vulnerable members of the public: see s 29A(3)(c).
2712 Seventh, as explained elsewhere, I am satisfied that a genuine, honest and reasonable attempt was made to put the defamatory allegations to Dr Al Muderis, and that the substance of his responses was reasonably included in the Broadcast and the Articles: see 29A(3)(g).
2713 Eighth, the Publications distinguished between suspicions, allegations and proven facts: s 29A(3)(b). For example, the introduction to the Broadcast and the Articles state that former patients of Dr Al Muderis accused him of failing to provide adequate care. What follows can generally be described as the reporting of a series of allegations and opinions of former patients, colleagues and other medical practitioners, and responses given by Dr Al Muderis. The Articles have a break-out section which makes it clear that they are quotes from patients; a description “in their own words”. The Broadcast and the Articles both use language which make the distinction clear (e.g. “accused of”, “claims”, “allege”, “allegation”, “have raised questions”, “some say”, or variations thereof).
Section 13 — The applicant’s submissions
2714 As described earlier, the applicant made submissions which were, in large part, directed to challenging the journalist’s credibility, alleging that the evidence as to their subjective beliefs cannot be accepted. The submissions are also relevant to the assessment of whether the respondents have established the objective element of s 29A. I have considered all the submissions. This section addresses the principal submissions. Although they are considered by topic, it is to be recalled they are not to be, and have not been, considered in isolation.
2715 Further to my comments on the applicant’s submissions, as a general observation, the applicant’s submissions: consider aspects of the evidence in isolation, ignoring the breadth of the investigation and supporting information; proceed on his interpretation of the material, one that is not necessary to accept; and, fail to grapple with the basis of the respondents’ subjective belief that the Publications are in the public interest. The submissions, at times, mischaracterise the evidence. There is overlap in some of the submissions. It is also unexplained how some of the applicant’s submissions (which are directed to Ms Grieve, Mr Steinfort and Ms Clancy’s conduct), if accepted, affect the assessment of the objectiveness of the belief.
2716 The applicant’s submissions include what is described as a source chronology for s 29A, which I have considered. The applicant explained that the purpose of the chronology was to support his submission “that, overwhelmingly, Ms Grieve had a particular outcome in mind when it came to what she was going to publish, and that she ignored relevant material”.
2717 It is appropriate to make two observations about the chronology. First, it contains factual inaccuracies. For example, the description that Ms Grieve read legal cases of which “none … criticised Dr Al Muderis” is incorrect because, as explained elsewhere, Ford is critical of his approach. The applicant also misdescribes some of the sources (e.g. he records that Mr Warland was “overwhelmingly positive about Dr Al Muderis”; his descriptions relating to Mr Grant and Mr Hernandez largely omit their negative statements about Dr Al Muderis). Second, the chronology (although not comprehensive) underscores the breadth of sources Ms Grieve spoke to, and the lengths she went to in conducting the investigation, including in seeking supporting material.
2718 It is to be recalled that, in determining whether the public interest defence is established, the material before the journalists at the time of publication is to be assessed.
Ms Grieve’s alleged conflict of interest
2719 The applicant put to Ms Grieve that she had a conflict of interest in investigating Dr Al Muderis given her father had consulted him and claimed, inter alia, he pressured him into undergoing the procedure. I do not accept that Ms Grieve was conflicted. I do not accept Mr Grieve’s connection to the investigation affects the respondents’ reliance on s 29A, or Ms Grieve’s credit as a witness.
2720 Ms Grieve’s evidence was that her father’s story was the starting point, but that was its only significance. The applicant never articulated any coherent logical connection to explain how Mr Grieve’s position would lead Ms Grieve to act other than honestly and reasonably in her investigation and reporting. To put it another way, the applicant did not make good his contention that Mr Grieve’s position led Ms Grieve to deliberately and dishonestly publish false information to denigrate Dr Al Muderis.
2721 Ms Grieve accepted that she did not inform Mr Steinfort or Ms Clancy that she became aware of complaints about Dr Al Muderis through her father. She explained she did not consider there was a conflict, did not think disclosing her father’s identity was relevant, and did not want to involve her family. She said she thought at that time that the only person it was necessary to disclose it to was Mr Bachelard, her editor. Ms Grieve raised with him whether there would be a perception of a conflict because of her father’s consultation. He told her that in the circumstances, that there would be no perceived conflict. The joint investigation with Mr Steinfort and Ms Clancy began after her conversation with Mr Bachelard, such that her non-disclosure was in that context.
2722 In cross-examination, Ms Clancy considered that although Ms Grieve should have told her about her father, she expressed the view it did not affect Ms Grieve’s objectivity in the investigation and story. Mr Steinfort was not asked about this topic.
2723 In the circumstances, I do not accept that Ms Grieve’s failure to disclose the matter to the other journalists affects her credibility or the respondents’ reliance on s 29A.
Unpublished allegations
2724 It will be recalled that the applicant put to Ms Grieve that she was “hell-bent on maligning” him and that she “wanted to utterly destroy him” and submitted that the journalists engaged in a “malignant, dishonest and malicious campaign” to destroy him.
2725 As referred to above, Ms Grieve recorded in her affidavit a long list of allegations she learned of during the investigation which were not included in the Publications, either because they were not considered to be in the public interest in the context of the present reporting, or because there was not enough information to verify the matter.
2726 It was put to Ms Grieve in cross-examination that the list of allegations was included in her affidavit for the purpose of maligning and damaging the applicant. The applicant put that:
… the inclusion of this paragraph [in which the allegations were listed] was in order, under absolute privilege in the Federal Court, to set out a list of untested, unverified allegations, not in the public interest [about the applicant, which Ms Grieve] knew could be reported by media companies … even though those allegations are untested or otherwise not in the public interest …
2727 The Reply to the Amended Defence pleads that “instead of reasonably believing that the allegations about Dr Al Muderis were in the public interest, the Respondents were actuated by the improper purpose or purposes of harming Dr Al Muderis”.
2728 The relevance of the evidence is self-evident. The respondents summarised their position as follows:
Neither Ms Grieve nor Mr Steinfort could be blamed for compiling such a list and seeking to explain salient parts of their editorial decision-making process in circumstances where Dr Al Muderis asserts in this proceeding that the Publications were motivated by a desire to denigrate and inflict damage on him … and that the respondents were part of a conspiracy to destroy Dr Al Muderis by concocting complaints … The exercise by Ms Grieve, Mr Steinfort and their colleagues of an editorial judgment not to publish various serious and potentially career-ending defamatory allegations about Dr Al Muderis on the basis that those allegations were either not sustainable or not in the public interest (including, in some cases, judgements exercised on the basis of information provided by Dr Al Muderis himself) is wholly inconsistent with Dr Al Muderis’ case concerning the respondents’ motives and so was plainly relevant evidence to include in Ms Grieve’s and Mr Steinfort’s affidavits.
2729 The respondents provided four examples to illustrate their points, and then proceeded:
Each of these allegations was serious, emotive and potentially career ending for Dr Al Muderis. The fact that the respondents decided not to publish them (notwithstanding the allegations came from multiple sources) confirms that they were not hell-bent on destroying Dr Al Muderis nor on publishing scandalous or salacious allegations about him without a proper basis. Their exercise of editorial judgment to omit these allegations speaks to the responsibility of their journalism and the honesty and reasonableness of their belief that what they did publish was in the public interest.
(emphasis in original)
2730 It is unnecessary to detail the examples relied on, or the broader list of allegations. That said, having considered the list, I accept the respondents’ submission.
2731 When Ms Grieve was asked in cross-examination why the allegations were included in her affidavit, she replied:
Because we were trying to make the point that what we did publish was a well-thought-through, very considered approach to crystallising what is and what isn’t in the public interest and what evidence we do have to support things versus what we don’t. … if we were intentionally trying to malign [Dr Al Muderis] … this information was in our domain, but we did not publish it because we considered the main public interest of this story was about patient selection and aftercare.
2732 I accept that evidence. Curiously, despite the cross-examination of Ms Grieve on this topic, Mr Steinfort and Ms Clancy, whose affidavits contained similar lists of allegations, were not cross-examined on this point.
2733 The respondents’ conduct in preparing the Publications in that manner bespeaks a considered, professional and responsible approach. The submission that there was some nefarious motive in explaining this in the manner Ms Grieve and Mr Steinfort did in their affidavits is entirely without foundation. I do not accept the applicant’s submission that the inclusion of unpublished allegations in the respondents’ affidavits adversely affects their credit or their reliance on s 29A. It was plainly relevant.
2734 To a similar effect, Ms Grieve gave evidence of allegations in the Articles being toned down or removed during the drafting process when she or Mr Bachelard decided the allegations were too strong or lacked sufficient support. Again, that approach is a responsible one and, I accept, was not one done with the intention of dishonestly damaging the applicant.
Publication of positive patient experiences
2735 This is a matter heavily relied on by the applicant. It underpinned much of his submissions and cross-examination of the journalists. He submitted that sources who contacted Ms Grieve to provide positive information about Dr Al Muderis were not included in the Publications, and that such information from sources who were included was not referred to. The submission, in large part, founded the applicant’s assertions as to the respondents’ motives. The submission proceeds on the premise that the journalists were required to include in the Publications all the positive statements that sources had said about him. I do not accept the respondents’ reliance on s 29A is undermined for the reasons the applicant contended.
2736 The applicant provided examples of sources with positive information about Dr Al Muderis and submitted that there is no credible explanation for why these sources were not included in the Publications, and why the Publications advanced allegations which were directly contradicted by the information they provided. He submitted that the failure to use these sources is indicative of the seriously unbalanced nature of the Publications and Ms Grieve’s total lack of interest in contradicting the negative allegations which other sources made about Dr Al Muderis. This was said to reflect an intention to only inflict damage on Dr Al Muderis.
2737 Leaving aside for the moment the accuracy of the applicant’s submission as to the content of these sources’ information, the submission erroneously proceeds on the premise that other patients speaking positively of Dr Al Muderis disproves the evidence of patients who had negative experiences. It also proceeds on the basis that there are no positive statements about him in the Publications (which as discussed below is incorrect). Moreover, on the evidence as discussed further below, there is a reasonable explanation for the editorial choices made. Once it is accepted that the editorial choices made were reasonable, the complaints that the Publications were misleading because positive information was not included cannot be accepted.
2738 In that context, as the respondents submitted, there was an editorial decision to focus on negative patient experiences that had not previously received public attention. They submitted:
The public interest in investigative journalism resides in exposing to the public matters, which the targets of it would rather was never exposed. It has to be done fairly, but it doesn’t have to be done in some sort of encyclopaedic manner.
2739 On the evidence of Ms Grieve, Mr Steinfort and Ms Clancy, that was the central public interest in the Publications: see e.g. [2653]-[2658]. The applicant’s submission also fails to grapple with what was said to be the public interest in the Publications. The interest was in what happens when things go wrong with the surgery.
2740 Given the public interest in this story, that editorial decision, in those circumstances, was not unreasonable, and does not evince a malicious motive by the respondents. Justice Lee observed in Russell that s 29A’s enactment: “ensures a court is to have regard to all the relevant circumstances in making allowances for editorial judgments as to publications of certain character”: at [336]; and “[t]he extent of public interest is relevant to making such allowances for editorial judgment as is appropriate”: at [347]. See also at [306].
2741 However, it does not follow from the respondents’ editorial decision that positive stories were ignored. The Publications did refer to the positive experiences of patients. They made clear that most of his patients were happy. To take several examples. At the outset of the Broadcast, Dr Al Muderis is referred to several times as a “hero”, “[a] hero doctor devoted to helping people walk again”, and “[a] hero to many performing cutting edge surgery on amputees, helping them walk again”: see Annexure B. Dr Al Muderis is quoted in the Broadcast as saying:
The vast majority of patients have very good outcome. We can talk about thousand of patient that are very happy and we can talk about the handful of patients that had complications and things went wrong …
2742 In the Broadcast, Mr Steinfort also refers to the fact that many people contacted them, “wanting to speak glowingly” about Dr Al Muderis. Mr Steinfort concludes in the Broadcast, “Dr Munjed Al Muderis’ critics readily accept the doctor does have plenty of happy patients”.
2743 Dr Al Muderis is quoted in the Articles and in the Grieve Video: “The facts are that the vast majority of patients are extremely happy”. The Articles also report that Dr Al Muderis “apologised to patients who felt abandoned but said these were a disgruntled minority”. The subheadings to the Articles (in particular, the online versions) expressly acknowledged that there are many happy patients (e.g. “many are profoundly grateful”). The Broadcast and the Articles also referred to the journalists being sent a large number of emails from patients detailing the benefits of osseointegration and praising Dr Al Muderis’ care.
2744 Ms Asch-Martin, an American patient of Dr Al Muderis, was interviewed. She had approached the respondents at the instigation of Ms Nikki Grace-Strader who works for Dr Al Muderis. I return to Ms Asch-Martin below at [2758]. I note that she is shown in the Broadcast being physically active, having had osseointegration surgery.
2745 A portion of the footage taken at Dr Al Muderis’ rooms, which was played in the Broadcast, presented positive views being expressed. It included a patient present who spoke about how wonderful Dr Al Muderis was. This was said to undermine the information they had obtained from other sources. It was suggested by the applicant in that context, the respondents’ decision to not show more of the footage, and for them not to accept at face value what they saw that day at his rooms is evidence that their beliefs were unreasonable. I do not agree. As Mr Steinfort explained:
… the way that people behave when television cameras are present is often the polar opposite of reality. People change their behaviour when there is a television camera, plus their PR manager there. They know that they are on their best behaviour and they are there to promote a positive image.
2746 The applicant submitted that showing the video was undermined by an implication conveyed in the Broadcast that it was a “put on” while the cameras were there. The implication is said to arise by Mr Steinfort subsequently raising the question of how osseointegration surgery has gone wrong for so many people. Again, on the material the respondents had, his question was not unreasonable.
2747 In that context, the respondents’ decision to not include in the Publications the interview with Dr Tetsworth is not evidence of unreasonable belief. As Mr Steinfort explained, “this is a man on the payroll. … he is fairly compromised in the way that he’s going to analyse the work being done by his colleague next to him”. I note that the respondents had Ford before them (see [2710] and including the criticism of Dr Tetsworth contained therein), and information that it was he who suggested Mr Urquhart use Febreze.
2748 It is not necessary to address all the examples of positive sources referred to by the applicant. Suffice to say that I have considered the applicant’s list of what he described as examples of Ms Grieve’s positive sources. He submitted the Publications advanced allegations which were contradicted by those sources. Having reviewed the material in relation to the persons identified, I do not accept that submission. The applicant’s submission is indicative of his failure to grapple with a key aspect of the public interest in the Publications. That is, that there is a darker side to his practice – not that his practice is mostly or invariably flawed.
2749 I note also that the applicant’s submission – that some sources were either wholly or overwhelmingly positive about Dr Al Muderis when they spoke to Ms Grieve – is often contradicted by Ms Grieve’s notes. It suffices to refer to two examples relied on by the respondents to illustrate.
2750 First, the applicant’s summary of Ms Stewart’s statements to Ms Grieve, which reflects a wholly positive picture of Dr Al Muderis. However, Ms Grieve’s notes of her first conversation recorded, inter alia, that Ms Stewart said that: she found her job ethically compromising; Dr Al Muderis was “ruthless”; patients’ expectations were “higher than the reality”; patients were vulnerable and this played to Dr Al Muderis’ advantage; patients were taking money out of their superannuation and remortgaging their homes to pay for the surgery; sometimes surgery was rushed; and, Dr Al Muderis was abusive towards staff and would humiliate them in public.
2751 Second, the applicant’s summary of what Dr Anstee told Ms Grieve is highly selective. Ms Grieve’s notes of her first conversation with Dr Anstee record that his criticism of Dr Al Muderis was not limited to soft tissue management: there were problems with an osseointegration surgeon owning the implants they use; appropriate treatment of maggots required going to an operating theatre, removing the maggots, debriding the wound to take out all the dead tissue, and, if necessary, considering complex reconstructive surgery; and, he did not understand how one could run an osseointegration unit without a plastic surgeon. Moreover, the applicant’s submission that Dr Anstee’s evidence was that he told the journalists he did not have a view about patient care generally, reads his response in a selective way, and out of its context. I note also that Ms Grieve’s evidence was that in a conversation with Dr Anstee after she had sent him Mr Urquhart’s medical records, he expressed the view that it was entirely inappropriate for Dr Al Muderis to have operated on Mr Urquhart and that his management of Mr Urquhart’s stoma was messy and substandard.
2752 Other examples include the applicant’s summaries of Ms Grieve’s conversations with Mr Grant and Mr Hernandez, which omit references to the many negative statements they made about Dr Al Muderis.
2753 These examples reflect that the applicant at times made broad submissions not supported by the evidence.
2754 The evidence properly considered does not establish that Ms Grieve only sought to speak to people she believed to hold adverse views against Dr Al Muderis; ignored those who had positive views of osseointegration and Dr Al Muderis; or that she ignored positive or exculpatory information that she received. As is reflected in her email correspondence with Ms Asch-Martin, the evidence is to the contrary:
Ms Asch-Martin: … I have heard that you are stating very incorrect/slandering things about Prof. Munjed Al Muderis. I am one of his Osseointegration patients from 2019; I would be very Happy to share my personal experience with you. … You are attacking a brilliant man who has made the amputee world a better place …
Ms Grieve: … Thank you for this information. I would like to know more about your case. But first may I ask why you think I am attacking Dr Al Muderis? Or what “incorrect/slandering things” you believe I am stating? …
2755 In that event, I do not consider that the respondents’ editorial decisions undermine their reliance on s 29A.
2756 In so far as the applicant submitted that in the break-out section in the Articles titled “In their own words”, Ms Grieve sought only to publish negative experiences of the patients referred to, I note that a separate article (titled “In their own words: how some patients feel let down by Munjed Al Muderis”) was published online by the Sydney Morning Herald and The Age on 18 September 2022 which is an expanded version of the break-out section. It provides further detail of those patients’ experiences, describing, inter alia, that Mr Smith was able to walk after his surgery, Mr Bruha was able to live an active life, that Mr Warland had a history of neuromas prior to surgery and that, after surgery, Mr Warland could feel the wind on his skin and feel the ground underneath him. I also note that Ms Grieve separately published an article about Dr Al Muderis’ Iraqi patients (titled “Lifelong wounds: How Munjed Al Muderis operates in developing countries”, published on 19 September 2022 in both the Sydney Morning Herald and The Age), which covered patients who had both positive and negative experiences with osseointegration surgery. Neither publication is sued on. These additional publications are inconsistent with the assertion that only negative details of the patients’ experiences were used by the journalists. I note that in relation to the “In their own words” section, apart from Mr Warland, Ms Grieve said that to the best of her recollection, had what was published read to the patient, and none demurred from the publication (I note an issue arose as to whether Ms Koolhoven agreed to her photograph being used).
2757 Aligned with this was the applicant’s submission that Ms Grieve sought to only find negative information about Dr Al Muderis. In part, the applicant relies on the story pitch to the editor of investigations, Mr Bachelard. It will be recalled that Ms Grieve provided a list of possible topics for investigations to him, one being “Munjed Al Muderis patients with complications (Sydney prosthetists, former patients, experts)”. Mr Bachelard indicated that he was interested in her investigating Dr Al Muderis’ osseointegration surgery. That Ms Grieve had information suggesting the topic was worth investigating does not connote a closed mind. An investigation is conducted to determine if there is any basis to publish a story. One can assume that the genesis of any investigation is some information considered appropriate to investigate further. Not every investigation leads to a story.
Ms Asch-Martin
2758 As explained above, Ms Asch-Martin, an obviously happy patient, featured in the Articles, the Broadcast and the Grieve Video. As reported in the Articles (I note that the final line is included in the SMH Online Article and the Age Online Article):
Washington patient Cindy Asch-Martin said: “I won’t have a bad word said about Al Muderis.
I know a few people who had osseointegration done by him and for some reason, there was bad blood between them and they started talking very negatively about him. I was sickened by that.
Munjed ... continues to perfect it. And he’s doing an amazing job.”
2759 And in the Broadcast:
Mr Steinfort: Cindy Asch-Martin is one of Dr Al Muderis’ loyal followers … who emailed us wanting to speak glowingly about the surgeon after his office issued a callout for support. … [she] underwent osseointegration surgery with Dr Al Muderis in 2019 … Her prosthetic may be working well these days, but even Cindy admits she did suffer major complications and was sent back to America afterwards with a dangerous infection.
Ms Asch-Martin: The infection started almost immediately. The whole plane ride home the smell from the infection was making me nauseated, I couldn’t imagine how the person beside me must have felt. I went to the washroom numerous times to stick my limb under the tap to try to rinse things off.
Mr Steinfort: In the end Cindy claims natural remedies helped solve the issues and now she’s delighted to say she’s not only walking again, but pushing her body to the limit. And for that she believes she owes everything to Dr Al Muderis for taking a chance when other surgeons wouldn’t.
Ms Asch-Martin: He is a wonderful man who is helping as many people as he can. He is a true humanitarian.
Mr Steinfort: What’s Dr Al Muderis done for your life?
Ms Asch-Martin: He enabled me to walk again.
2760 And, as referred to above, in the Grieve Video:
Ms Grieve: … There’s no denying the work Al Muderis has done has helped people and there are patients who regard him as their God. Cindy Asch-Martin is one patient who won’t hear a bad word about him.
Ms Asch-Martin: He is a wonderful man who is helping as many people as he can no matter what their situation is. He is a true humanitarian. He’s my hero. I can only speak for myself. He’s – I believe he’s brilliant.
2761 The applicant does not challenge the accuracy of the content of the reporting of her interview. Consideration of her in the edited interview, as with her earlier conversation with Ms Grieve, reflects she informed the respondents of events which were plainly complications, and the need for further surgeries.
2762 I observe that some of the information Ms Asch-Martin provided the respondents about her experience, is consistent with information provided to the respondents by Mr Bruha, another source who appeared in the Broadcast, as to his experience (which was critical of Dr Al Muderis). That is, they each provided information that they were sent home to the United States after surgery with Dr Al Muderis, with an infection.
2763 The applicant submitted that in relation to the Broadcast, Ms Asch-Martin (and others) who support him were “presented as irrational people who are part of some sort of cult, that they support him, irrespective of his obvious flaws. … [Ms Asch-Martin] was presented as some sort of lunatic”. This was refuted by Ms Grieve and Ms Clancy.
2764 Viewers and readers may consider that Ms Asch-Martin, given her unwavering support for Dr Al Muderis, blindly accepts Dr Al Muderis despite complications she and others experienced. That was a product of her story, which the respondents presented in her words. It is difficult to understand in those circumstances the applicant’s submission as to how that is unfair. Her story was that, ultimately, Dr Al Muderis “enabled me to walk again”. It is to be borne in mind that Dr Al Muderis’ team told Ms Asch-Martin to approach the respondents. Her contact with them was by design. She was there to support Dr Al Muderis. On the case presented by the applicant, Ms Asch-Martin is a success story.
2765 That said, the material before the respondents reflected that many considered Dr Al Muderis a hero or a “God”, and some patients who were spoken to would not tolerate any criticism of him regardless of any complications they or others had experienced. Ms Grieve had material which reflected that persons critical of Dr Al Muderis would endure criticism from his supporters, and that negative messages were deleted from the osseointegration Facebook support group (to which Dr Al Muderis directed potential patients). It was in a context where several sources would only speak if given an assurance of anonymity, for fear of the consequences for having made any critical comment.
2766 I do not accept that the presentation of Ms Asch-Martin’s story undermines the respondents’ belief (or reasonableness thereof).
Downplaying the benefits of osseointegration
2767 The applicant submitted the Articles significantly downplayed the benefits of osseointegration. He submitted that an article that misrepresents a medical procedure to the public is not in the public interest, and it is not reasonable for any journalist to believe it to be so. He submitted that the s 29A defences must fail in relation to the Articles because of this.
2768 Although the applicant did not explain how he believed the Articles downplayed the procedure’s benefits in his submissions, so much is apparent from his cross-examination of the journalists. He focused on the Articles’ descriptions that: “At best, [osseointegration] restores people’s ability to walk without the blisters and discomfort of a normal ‘socket’ prosthetic”; and “When successful, the procedure gives amputees a new life by removing the blisters that come with traditional sockets”. It was put to Ms Clancy that the procedure’s benefits were not limited to allowing an amputee to mobilise without the problems associated with sockets; they extended to allowing people to walk who could not use sockets at all and gave people a feeling that was closer to having their real leg back when compared to sockets.
2769 I note the material before the journalists included a brochure from Dr Al Muderis stating, “The major advantage of [Dr Al Muderis’ method of osseointegration] is the absence of a socket. This ensures the prosthesis always fits comfortably…” (emphasis added).
2770 In cross-examination Mr Steinfort accepted there was a misrepresentation in the Articles by the reference to “at best”:
Ms Chrysanthou: Now, you see in [the Articles] there’s a description there of osseointegration surgery, and this final sentence says:
At best, [osseointegration] restores people’s ability to walk without the blisters and discomfort of a normal socket prosthetic.
Mr Steinfort: Yes.
Ms Chrysanthou: You knew, didn’t you, at the time of publication that that was a wholly misleading statement about the benefits of osseointegration surgery?
Mr Steinfort: No.
Ms Chrysanthou: To suggest:
At best, [osseointegration] restores people’s ability to walk without the blisters and discomfort of a normal socket.
Mr Steinfort: Yes. That’s probably not the best case scenario.
Ms Chrysanthou: Yes. You knew that the benefits, even just from talking to Brennan Smith, for example, were far greater than that; isn’t that right?
Mr Steinfort: Yes. Agree.
2771 This evidence must be seen in context. To the proposition put in cross-examination that the Publications “wholly misrepresented osseointegration surgery to the public to [his] knowledge”, Mr Steinfort responded that he “couldn’t disagree more”. Ms Grieve and Ms Clancy expressed the same view. I note Ms Grieve disputed that the “at best” passage was wholly misleading as to the benefits of osseointegration.
2772 In all the circumstances, I do not accept the inclusion of that passage in the Articles undermines the respondents’ reliance on s 29A. The public interest defence does not require factual accuracy: see e.g. Russell at [339], or that a respondent “do everything right”: see Approach to s 29A in Section 1 above. A respondent must prove they reasonably believed that the publication of the matter was in the public interest: s 29A(1)(b). Evidently, Mr Steinfort did not consider the passage to be misleading prior to publication (and I do not consider his concession to affect his post-publication belief). Although he accepted that he knew the procedure’s benefits were greater than what the passage alleges, it does not follow that he considered it such that he knowingly published misleading material. I do not accept the evidence undermines Mr Steinfort’s honest and reasonable belief in the truth of what was published: see Russell at [339], or the reasonableness of his (or the respondents’) belief.
2773 Each of the Articles read as a whole, as well as the passage read in context, plainly conveys that the primary benefit of osseointegration is to help amputees walk, including those who could not do so with a socket. I accept the respondents’ submission that it could not sensibly be contended that ordinary readers of the Print Articles (the SMH Article and the Age Article) would have been left in any doubt that osseointegration is a potentially life-changing surgery that helps amputees who cannot walk, to walk again. The Online Articles (being the SMH Online Article and the Age Online Article) give additional information to that effect. Among other reasons, the Print Articles’ lead is:
The refugee-turned-surgeon has found fame by helping amputees walk. Some rue the day they submitted to his knife. Charlotte Grieve, Tom Steinfort and Natalie Clancy report.
(emphasis added)
2774 Although, in a vacuum, the passage may be considered misleading, I do not accept that the Articles downplayed or misrepresented the benefits of osseointegration (or that the respondents intended so much).
Obtaining further material
2775 The applicant made submissions highlighting further steps he said the respondents should have taken in the investigation to verify what was being said to them.
2776 It is apparent the submissions erroneously presume that if further information was obtained it would show that the information they had was incorrect. For instance, the applicant submitted most sources did not provide medical or other records to substantiate the allegations they made to Ms Grieve, but she proceeded to publish those allegations anyway, without attempting to obtain objective contemporaneous evidence to test their claims. He later submitted that, post-publication, the respondents had access to thousands of medical records that contradict many of the specific allegations in the Publications about a number of patients. I address these submissions below.
2777 The submissions are also premised on the proposition that an investigation must be exhaustive. I do not accept that s 29A, in the circumstances of this case, requires the material before the respondents to be exhaustive (in that it must be totally or completely comprehensive). The terms of s 29A do not support such a reading and the object the defence is aimed at promoting militates against it. That is:
[T]o ensure that the law of defamation does not place unreasonable limits on freedom of expression and, in particular, on the publication and discussion of matters of public interest and importance.
Defamation Act, s 3(b). And see above at [2502].
2778 To ask whether the material is exhaustive is to ask the wrong question. So too is asking whether the journalist could have done more, or what more could have been included in the Publications. The issue is, on the material the respondents had obtained, whether their subjective belief that the Publications were in the public interest was objectively reasonable. That said, any steps taken to verify the information in the matter published may be a relevant consideration in making that assessment: Defamation Act s 29A(3)(h). As explained elsewhere, the respondents went to considerable lengths to verify the material during their investigation. A consideration of the material reflects this. Further, and accepting that more can always be done, given the nature of this investigation, that the applicant submitted that further investigation was necessary only serves to reflect its extent and breadth.
2779 There was a general assertion that most sources did not provide medical files or other records to the journalists before publication to support their allegations, but Ms Grieve published the allegations anyway. It was said she should have sought those files.
2780 As explained above, the submission as advanced presupposed the correctness of the assertion contained therein. It proceeds on the premise that the files contradicted what the patients said, or would, if obtained. As apparent from my consideration of the patients in relation to the truth defence, the general premise of the applicant’s submission cannot blankly be accepted. The medical records cannot be said to contradict the import of the patients’ allegations: see [2940].
2781 Even if the submission is that the medical records will test sources’ allegations, and might contain disconfirming information, it is general in nature and presupposes that medical files are always necessary (without discrimination). It fails to grapple with the circumstances of this case. Given the breadth of the investigation, I do not accept that Ms Grieve should have expected further investigations to disprove, in any meaningful way, the material she had before her.
2782 As the respondents submitted, journalists never have available to them the information which is available after a hard-fought piece of adversarial litigation, such as this one. They lack coercive powers and rely on information they can gather from public sources or whistleblowers. In Russell, Lee J observed at [339]:
Public interest journalism does not pretend to be a form of fact-finding that is functionally equivalent to the judicial process; and it is certainly not the case that its public utility depends upon such an equivalence.
2783 Ms Grieve did not require possession of the medical records for her or the respondents’ belief to be reasonable. She also corroborated sources by other means. Moreover, even if a patient may be a poor historian, it does not necessarily follow the import of their evidence is unreliable. This is not a publication that relied on one patient or one doctor, but multiple patients and doctors informing Ms Grieve of the same or similar types of complaints. The nature and extent of the investigation is relevant to determining the reasonableness of any further inquiries. As explained above, source information was not considered in isolation.
2784 For example, Dr Anstee expressed the opinions he did in the Publications having relied on Ms Grieve and the material she provided, which included the medical files of Mr Urquhart, Mr Smith and Ms Todd (I note Ms Todd was a patient he consulted with at The Alfred). Dr Anstee’s preparedness to speak in the Publications is in that context, as were the opinions he expressed. So much is apparent from the Publications (e.g. in the Age Article, “Retired Alfred hospital plastic surgeon John Anstee reviewed patient files and said some outcomes were unacceptable, including the presence of maggots in a wound”, and see Dr Anstee section below).
2785 The applicant provided Ms Todd as an example to demonstrate this submission. The Articles allege that “new doctors [unaffiliated with Dr Al Muderis] say the only option [for Ms Todd] is to amputate what is left of her leg, or she will die.” The applicant submitted that the respondents published that serious allegation without any medical record, and not having spoken to any doctor who confirmed it. The applicant went further, and submitted this is a:
… shocking allegation … [which] only came from Carol Todd. So Ms Grieve saw fit to publish that allegation, based only on the say-so of a non-medically qualified patient. No checks, no verification. It is an utter and disgraceful failure of a person calling herself a journalist, let alone an investigative journalist. It is part of imputing how awful my client is, leaving this old lady in this pain, and leaving her to require her whole leg to come off.
2786 Ms Grieve accepted she did not see any medical record that drew that conclusion. She rejected the suggestion that it was wholly incompetent of her to make the allegation in that circumstance.
2787 Ms Grieve’s notes of an August 2022 call with Ms Todd reflect that she was attending hospital during this period. The notes record:
Now [I] think [I’m] going to [l]ose my leg, it’s a bit of a shock to go that far backwards. They’re definitely thinking about it. They want me to think about it. … Other options? None. They had a meeting down in [Melbourne] – [I] told them [I] was back in hospital, s[h]owed them the photos. Tried to speak to the other colleagues, no one knows what [to do]. Only that [I] get my leg off. There’s no other options.
2788 Ms Todd texted Ms Grieve on 10 August 2022: “I am still thinking the only way I can move forward is [to] have the operation. At least I would [be off] all the antibiotics [and] live [a] happy long life”. She texted again on 20 August 2022:
… since I have been in [hospital,] I found out from X-ray that most of bone on one side of my stump has gone. They are worried that if I don’t get this rod out that it could go right my body n infection will kill me. I don’t want you mention Dr [Tetsworth] in Brisbane) his name in written story. I have to see him soon to work out operation on my stump. …
2789 The applicant’s submission is simplistic. Ms Todd made the 20 August 2022 representation to Ms Grieve in a context where she says she was attending hospital and receiving advice. The description, “They are worried that if I don’t get this rod out that it could go right my body n infection will kill me”, was made contemporaneously. Moreover, any submission about the need for further investigation in relation to Ms Todd must be considered against the background of what steps had been undertaken and information obtained. Ms Grieve did not take Ms Todd’s statement in isolation. Its credibility was bolstered in a context where multiple medical professionals told Ms Grieve that Ms Todd was in an emergency situation and her life was at risk, where Ms Grieve recognised the dangers of osteomyelitis. Ms Grieve understood that Ms Todd had chronic osteomyelitis at the time. Pre-publication, she also understood that Mr Mortimer was told by Dr Al Muderis that if he had osteomyelitis, his implant would have to come out (and that both of those things ultimately occurred). Ms Grieve also gave evidence that Dr Anstee told her, “the big thing that worries the surgeons is … osteomyelitis”.
2790 I do not consider, in the circumstances, the failure to obtain any further records undermines the journalists’ credibility, or the sincerity of their belief that it is in the public interest to publish the matters. Nor, given all the circumstances of this case, the reasonableness of that belief. Each example also illustrates that the applicant’s submission is dependent on their interpretation of the material sought, which is not one that a journalist, acting reasonably, was required to accept. Nor do I accept the applicant’s submission that Ms Grieve gave unresponsive answers on this issue.
Knowing publication of false material
2791 The applicant submitted that the respondents knowingly published false material, which he described as “the death knell” for their reliance on s 29A. He pointed to examples, both relating to Mr Urquhart.
2792 First, the Articles report:
… the procedure left [Mr Urquhart] with a chronic infection and the worst pain he had ever experienced – like there was “a welder blowing on my legs”.
Al Muderis, Urquhart says, did not seem interested. “This is normal, you’ll be right,” he recalls the surgeon saying. In one of their final meetings, Urquhart says he was told to spray his legs with “Febreeze” – an air freshener sold in supermarkets – to deal with the smell, which had grown so bad he says he “could taste it”.
(emphasis added)
2793 Ms Grieve deposed that she knew, prior to publication, that Dr Tetsworth (not Dr Al Muderis) had advised Mr Urquhart to spray his legs with Febreze, and did not consider that Dr Al Muderis was responsible for the comments. Against that background, the applicant submitted that Ms Grieve “imputed in the Articles that Dr Al Muderis made the Febreze statement to Mr Urquhart, knowing that this was false”.
2794 Ms Grieve denied intending to impute so much. The text of the Articles (as emphasised, above) does not strictly attribute the comment to Dr Al Muderis; the comment is attributable to a third party. Ms Grieve did not accept she imputed the statement, knowing it to be false. She explained:
The decision was made, at the time, not to attribute … that particular comment; we tried to keep it vague as to, you know, it was said in a meeting. In hindsight, I think we should have attributed it to … a colleague. But, in any event, I think that the effect was the same. He … was told that, and that was a significant turning point for Mark in terms of his dealings with Dr Al Muderis, and he felt that that was … a symptom of … the culture of the team. … I accept we should have had attribution in there, but that was a deliberate decision at the time.
2795 The meaning of her answer is not entirely clear. Nonetheless I am not persuaded that Ms Grieve knowingly published such a claim, or that she acted dishonestly; the highest the evidence rises is that the drafting of this section of the Articles could have been improved. I am fortified in that conclusion by the way the respondents conveyed the Febreze incident in the Broadcast. They plainly do not seek to impute that Dr Al Muderis advised Mr Urquhart to spray his legs with Febreze:
Mr Steinfort: Mark travelled to Sydney to see Dr Al Muderis and his team, but instead of them taking his concerns seriously the patient became the butt of jokes.
Mr Urquhart: This other doctor who was a Professor pipes up and says “why don’t you spray Febreze on it”. And I don’t know if you know what Febreze is, but it’s a carpet deodoriser. And I looked at Munjed and then all the little other soon to be doctors were laughing.
(emphasis added)
2796 Bearing in mind that Ms Grieve is credited with being a producer of the Broadcast (with Ms Clancy). In that context, and knowing the content of the Broadcast, makes the applicant’s submission that she was dishonest in the Articles improbable. That the respondents now accept that the Articles impute that Dr Al Muderis suggested Mr Urquhart use Febreze is of no moment. The concession was made with respect to what imputations are carried to the ordinary reasonable reader; it is not to be understood as an admission of what the journalists knowingly or intentionally imputed at publication.
2797 The applicant also submitted that, given the respondents conceded the Articles conveyed that Dr Al Muderis suggested Mr Urquhart used Febreze, Mr Steinfort knowingly published the false claim in his capacity as an author of the Articles. He submitted that Mr Steinfort otherwise knew that the comment was made by another surgeon, given the Broadcast correctly attributed the comment as such. As is plain from the reasons above, I do not accept the submission.
2798 Second, the Articles report Mr Urquhart “claims to have been ignored when he found maggots in his leg after his bone was left exposed for years”. The Broadcast includes the exchange:
Mr Steinfort: The breaking point for the veteran was this. When he discovered maggots breeding in his leg.
…
Mr Urquhart: I actually didn’t know what to do. … I don’t know how to fix this. And I sent the video to Munjed straight away and I never got a response from him.
2799 Mr Urquhart had told Ms Grieve he tried to get Dr Al Muderis and his team to help him on a number of occasions about the maggots, but they were either slow to respond or did not respond to some of his queries.
2800 Prior to publication, Ms Grieve had photos of a text message exchange between Mr Urquhart and Ms Roberts from December 2020. In the exchange, Mr Urquhart sent two videos to Ms Roberts of maggots in his stoma, complained about “[flies] getting at [the stoma]” and having to “[clean] maggots out of me”, and asked if she can show Dr Al Muderis. The second video appears to be the video used in the Broadcast, referred to above. Ms Roberts replied, “[w]ill show him for sure and will get back to you”. Ms Grieve accepted in cross-examination that she knew Ms Roberts had sent that reply to Mr Urquhart the same day.
2801 The applicant contended that because Ms Grieve was aware Dr Al Muderis (through Ms Roberts) had responded to that video the same day, the respondents knowingly published a false claim.
2802 It was put to Ms Grieve that she knew Mr Urquhart’s claim he had been ignored was false in light of that material. Ms Grieve explained that, although she was aware of Ms Roberts’ response to the video:
When I saw that document, I asked Mark Urquhart about it. I tested his version of events, and he explained that … there were multiple episodes of maggots. … he stood by the claim that they weren’t responded to immediately, they weren’t responded to in time in a timely manner for what should have been considered an emergency situation.
2803 Ms Grieve explained Mr Urquhart’s allegation was consistent with those made by many other patients who felt their problems were being dismissed. I accept Ms Grieve’s evidence. As the respondents submitted, her answer was that the totality of the information she received from Mr Urquhart supported his claim.
2804 Mr Steinfort’s explanation on this point in cross-examination, which I also accept, is illustrative:
The allegation made was consistent with the overall feelings of Mark Urquhart and there were other instances when he had got in touch, and you know, let’s keep in mind there’s maggots in his leg, like, let’s not underplay how awful that is, that he had got in touch with Dr Al Muderis’ clinic and there had been delays in getting back to him. I think it was Anzac Day another year when it had taken the better part of a week for someone to respond to him about concerns with the maggots in his leg. And this was part of an overarching sentiment from Mr Urquhart that he had had numerous complications, several infestations of maggots, and that he, (1), did not feel like he was receiving the urgent attention that it needed; and (2), he was not getting a resolution and this left him extremely upset. And so, to the overall tenor of what he was getting at there – whilst that specific message was replied to with speed – in terms of the overall sentiment of what we’re trying to get across from Mark Urquhart, I think it still stands accurate.
2805 Mr Steinfort’s understanding that Mr Urquhart had been left untreated for a week is correct. Mr Steinfort was aware prior to publication that:
… there were numerous instances of maggots infesting [Mr Urquhart’s] leg, which he was highly upset about, and that there were instances where the response had not been what he had wanted as a traumatised patient.
2806 The applicant also submitted that it was “wholly … untrue” that Dr Al Muderis told Mr Urquhart not to worry about maggots. The Articles describe, “when Urquhart’s wound was infested by maggots, he was told there was nothing to worry about”. I do not accept the applicant’s submission.
2807 Ms Grieve, during cross-examination, could not recall whether she had any document to corroborate Mr Urquhart’s claim prior to publication. Nevertheless, the material before her (which Mr Steinfort and Ms Clancy also possessed) included an email from Ms Roberts to Mr Urquhart:
In my experience I have witnessed people develop maggots in the wound and as much as it sounds awful and I have never had it personally, it terrifies people however the treatment is reasonably straight forward. I used to see maggot treatment as a method of treatment when I worked in intensive care.
2808 Self-evidently, the import of that email is that Mr Urquhart was told he need not worry. I note Dr Al Muderis, in his interview with Mr Steinfort, said maggots are “often harmless … We tell [patients] not to panic about it”.
2809 Finally, I note that in closing oral submissions, the applicant submitted that it was “wholly dishonest of Ms Grieve to say that Mr Urquhart was ignored, when she had all of his messages with Dr Al Muderis”, and in circumstances where Mr Urquhart had revision procedures to try and address the issues he complained about. He also submitted that it “was wholly dishonest by the respondents and, given the prominence of Mr Urquhart in the [P]ublications, is a reason on its own, why [s] 29A cannot succeed”, because it had been proved each of the journalists knew the claim to be false. This submission is premised on the basis that the claim was false, and on the material before the respondents, that was not so. The submission is broad and fails to engage with all the material before the respondents.
2810 Before turning to the next topic of submissions, I also note that the applicant criticised Ms Grieve in cross-examination, contending that the use of a photograph of Mr Smith in the Grieve Video was false and misleading. This photograph, which is very briefly shown, is of a person, perhaps having had surgery (although there is a reference during the cross-examination to it being Mr Smith in a coma, that is not referred to in the Grieve Video and is not a necessary inference). There is no identification of it being Mr Smith. The questions put to Ms Grieve asserted the use of the photograph was designed to create the impression that that state was the consequence of Dr Al Muderis, as opposed to relating to an earlier operation by another doctor. Ms Grieve denied the allegation. The applicant did not refer to this topic in closing submissions or advance it as a basis for a finding against Ms Grieve.
2811 Ms Grieve’s evidence describing the process in drafting the Grieve Video is indicative of how the photograph of Mr Smith came to be used in the video. Ms Grieve wrote the script. She worked with video editor, Mr Cormac Lally, to put together the Grieve Video. Mr Lally filmed Ms Grieve voicing the script. During this process, Mr Lally also took images of documents from patients and other sources. He also had a draft version of the Broadcast. Mr Lally then put together a draft of the Grieve Video. He made the editorial decisions regarding what footage to use and how it was cut together. After the first cut of the Grieve Video was finished, Ms Grieve reviewed it and said she might have made some minor tweaks. The Grieve Video was based on the script Ms Grieve had prepared, and the footage was from the Broadcast or filming they had done. According to her evidence, there were no surprises in it given what the video was based off of (I note as explained below, the photograph of Mr Smith is shown in the Broadcast).
2812 The criticism in the cross-examination appears to be the use of the photograph in the context of Ms Grieve’s narrative in the video, implying that Dr Al Muderis was responsible for the state of Mr Smith in the photograph. But the photograph is of a person who appears to have had surgery (in a hospital bed with tubes/equipment). The evidence establishes that the use of the photograph, and the timing thereof was not Ms Grieve’s decision or doing. I am not satisfied that she had any intent to mislead, as was put to her in cross-examination. There is no allegation in relation to such a photograph (or a person being in that condition) in the Online Articles in which the Grieve Video is embedded. The photograph is used in the Broadcast where it is apparent that it is Mr Smith, and that it is from an earlier operation (and of which no criticism is made). It is therefore unlikely that a journalist (or news organisation) in a joint investigation would intentionally use the photograph to mislead in a related publication. The use of the photograph was careless (and should have been picked up on Ms Grieve’s review). However, I do not consider that it undermines her subjective belief in that publication. Nor, given all the circumstances, the objective reasonableness of her belief in that publication. As I mentioned above, the applicant did not advance any submission to that effect, or on this topic at all, in his closing submissions.
Ms Grieve misleading Mr Steinfort and Ms Clancy
2813 The applicant submitted that Ms Grieve misled Mr Steinfort and Ms Clancy by withholding certain material. He submitted Ms Grieve did not provide to Mr Steinfort nor Ms Clancy: Mr Urquhart’s 24 November 2019 email to Dr Al Muderis; Mr Urquhart’s December 2020 text messages with Ms Roberts; consultation records which showed the risks and complications Mr Urquhart had been warned about; Mr Urquhart’s Facebook messages with Dr Al Muderis; Mr Urquhart’s email to Gabrielle Upton in September 2020; texts on 2 December 2020 where Mr Urquhart explained the plan to remove the implants and replace them with the OPRA system; and, emails with Dr Phil Huang which showed that Mr Urquhart made a choice to remove his implants and not have new ones re-inserted. It was said these documents contradicted many of Mr Urquhart’s claims (including allegations ultimately published in relation to him). This matter (withholding of certain material) was not generally put to Ms Grieve in cross-examination. I observe that the last submission about the documents contradicting Mr Urquhart depends on the applicant’s interpretation of the material.
2814 The applicant’s submissions on this topic at times included allegations of dishonesty on Ms Grieve’s part, including that she lied or at least misled Mr Steinfort and Ms Clancy about the key information she had. For instance, the most prominent aspect of this submission is that she deliberately did not give Mr Steinfort and Ms Clancy the full November 2019 email, calling it a serious act of dishonesty. That email is the highpoint of his submission. I do not accept Ms Grieve deliberately withheld information from Mr Steinfort or Ms Clancy, or that she acted dishonestly.
2815 In particular, the applicant relied on Mr Steinfort and Ms Clancy not having been informed that Dr Al Muderis had responded to Mr Urquhart’s maggot video, and on a “cut-off” copy of Mr Urquhart’s lengthy email chain with Dr Al Muderis following the Febreze incident.
2816 However, the applicant did not put to Ms Grieve in cross-examination that she misled Mr Steinfort or Ms Clancy. I accept it is a matter which may well have a reasonable explanation. In those circumstances, I do not consider it appropriate to draw any adverse inference. In any event, there is no evidence that Mr Steinfort or Ms Clancy were misled in any material respect.
2817 I note that in relation to the email chain Mr Urquhart sent Dr Al Muderis, as I explain elsewhere, I do not accept that it contradicts the import of what was published. Moreover, it is evident from Mr Steinfort’s cross-examination recited below, he did not consider himself to have been misled. As to the text exchanges, the highest the evidence rose was that neither Mr Steinfort nor Ms Clancy were aware that Dr Al Muderis’ clinic had responded to the maggot video. As the respondents submitted, Mr Steinfort and Ms Clancy’s post-publication discovery of the response to the maggot video did not shake their evidence that, on the whole, Mr Urquhart’s story was one of a patient having been steadily abandoned over a period of time. Again, so much is apparent from Mr Steinfort’s evidence on this point, recited above.
2818 I have referred elsewhere to the evidence of Mr Steinfort and Ms Clancy about relying on Ms Grieve. In this context, Mr Steinfort did not consider he was materially misled by Ms Grieve. It was put to Mr Steinfort that he did not know if Ms Grieve was being selective about what she gave him. He responded:
No. I think she discovered a pretty consistent and compelling narrative from a lot of people that there was - and that is one thing that’s worth pointing out. If this was one complainant in isolation, I suspect we probably - and this may be what happened with Natalie Clancy previously when she found out about it. When you hear these things on their own, you think, “Okay. Maybe there’s something here, maybe there’s not.” When you hear two people, you say, “Okay. Well, maybe there’s something here.” When you have dozens upon dozens of people who have the same take and the same experiences and the same analysis of the same situation, then you start to think, “All right. This isn’t just one person making something up.” There was a clear and consistent theme from numerous people that we spoke to about the conduct of Dr Al Muderis.
2819 In cross-examination Mr Steinfort took issue with the accusation that Ms Grieve concealed information from him, rather he characterised the matters put to him as omissions. It plainly did not affect his opinion of the public interest in the story or of Ms Grieve. In cross-examination, Mr Steinfort stated that he had “ultimate confidence in [her] because of things that she has done that I have worked on with her. She has been diligent, accurate, fair and concise”.
2820 Another example of the applicant’s submission on this topic is Ms Grieve’s failure to inform Mr Steinfort or Ms Clancy about her father, which is addressed above.
Approach to sources
2821 The applicant submitted that Ms Grieve misled the sources as to the true nature of the investigation to get them to talk to her. It was put to her that she sought to “trick” sources into speaking to her by misleading them about what the investigation was going to be about. The evidence, properly considered, does not establish that Ms Grieve relevantly misled sources about the nature of her investigation.
2822 Ms Grieve explained that when she initially approached a source, she would make “broad inquiries” because she “didn’t want to colour anyone’s view”. I agree that Ms Grieve’s approach is conducive to procuring uncoloured information. She was also conscious that Dr Al Muderis was litigious. That approach is not apt to mislead a source. She explained that, despite her approach:
… a conversation about osseointegration quickly turns into [a conversation about] Dr Al Muderis, because he’s the person … who has performed the most [osseointegration] surgeries in the world.
2823 In any event, it is entirely unclear how this approach is said to have affected the credibility or reliability of information the sources gave to Ms Grieve. It was not suggested in cross-examination that the information given by any of the patient sources who gave evidence was incorrect or false because of Ms Grieve’s approach (nor was any basis provided for why it would be). It is also unclear how it otherwise affects the honesty or reasonableness of Ms Grieve’s belief that the Publications were in the public interest. Suffice to say, I do not accept that Ms Grieve’s approach to sources undermines her, or the respondents’ reliance on the public interest defence.
2824 Nor do I accept the applicant’s submission that Ms Grieve influenced sources by telling them negative things about Dr Al Muderis. The implication in this submission is that Ms Grieve influenced the source to say something other than the truth. The evidence does not support that contention.
Reliance on particular sources
2825 It is unnecessary to address each of the applicant’s complaints about the sources relied on by the respondents in the Publications. Suffice to say I have considered the submissions and the material before the respondents at the time of publication, as well as their responses to the applicant’s assertions. I do not accept that they, taken together, undermine the respondents’ evidence of their subjective belief or the reasonableness thereof. I address what appears, from the conduct of the trial, to be said by the applicant to be the most egregious patients, being Mr Urquhart, Mr Smith, and Ms Todd. I also refer to the respondents’ reliance on Mr Hernandez and Ms Stewart.
2826 As a general observation, many of the applicant’s submissions on this topic are based on his interpretation of information before the respondents, an interpretation that need not be accepted. That accords generally with the applicant’s approach in relation to this defence. The applicant’s submissions contain repeated assertions that something is implausible, improbable, or unreliable, based on an interpretation of events or material, which are not required to be considered in that manner. That is, in relation to whether information can be relied on, the submission presumes the correctness of the propositions contained therein. I note, as I have previously, this submission also suffers from the applicant considering each source in isolation.
2827 Further, as previously explained, and elaborated on below, the evidence reflects that each of the journalists considered matters that went to issues of credibility and reliability of the source, before using them in the Publications.
Mr Urquhart
2828 The applicant referred to positive comments Mr Urquhart had made about Dr Al Muderis, including those in his November 2019 email to Dr Al Muderis, to challenge the respondents’ reliance on his complaints. He submitted that these comments contradict what was published. Although I have addressed above the applicant’s general submissions relating to patients’ positive comments, the character of Mr Urquhart’s comments (and the respondents’ understanding of them) are illustrative.
2829 Ms Grieve gave evidence that:
I think quite often what we see with Dr Al Muderis’ patients is that in writing while they’re under his care, they feel as though they don’t have any other options. And so they feel like they have to stay on his good side, pay him compliments, keep the relationship good, like it’s on them to do that. And I saw Mark’s correspondence as being reflective of that position. And it was only until he saw new doctors who observed his care and he realised … that his feelings … were legitimate, that he had been abandoned.
…
Mark said – and his story matched the story of many other patients that I spoke to – that, when he raised these concerns with Dr Al Muderis, he was dismissed, and he was told, “No, don’t worry, that’s normal. The smell is normal. It will heal. We will fix the exposed bone.” He was made to feel as though his problems were being dismissed, and this was not just Mark saying it. It was many other patients, and so, it was consistent with the information that I had from Mark, from the documents and from many other patients that they felt ignored.
2830 Mr Steinfort gave similar evidence. He said he knew from Ms Grieve’s material that Mr Urquhart had “for a very long time [been] hugely glowing about Dr Al Muderis”. He was pressed on that response:
Ms Chrysanthou: And what was your understanding of when his attitude changed in relation to that?
Mr Steinfort: Well, I think there came a point in time where he continued to suffer complications, infections, maggots in the wound where there was a sense in his mind that this was not a solution. In fact, it was creating significantly more problems to his life than – to the point that it was doing great damage to his mental health as well as his physical health. And … he was jack of it.
…
Ms Chrysanthou: Would it have been relevant for you to know if it were the case that Mr Urquhart wished to continue his relationship with Dr Al Muderis as a doctor after the Febreze incident?
Mr Steinfort: Of course. He was deeply hurt, but in his mind, I think at that point, he needed Dr Al Muderis. Like, what was he supposed to do at that point? … when you said “the point that Mark Urquhart turned”, I don’t think he woke up one morning and clicked his fingers and said, “I used to love him yesterday and today I hate him”. … these kind of things are a gradual dawning.
Ms Chrysanthou: But it would have been relevant to you, wouldn’t it, to know if right up until the point where Mr Urquhart saw a different surgeon, he in fact was communicating about and towards my client in a wholly positive way?
Mr Steinfort: Of course. You’re not going to go and tell your surgeon that you hate him and he’s a so-and-so if you depend on this person to manage your health. You’re trying to keep them sweet.
Ms Chrysanthou: Well, that’s an assumption that you’ve made?
Mr Steinfort: I think it’s pretty reasonable that you would think that, of course, he’s going to try. This is a guy who is, like, at the end of his tether and desperate for solutions and looking at maggots in his leg and repeated infections. He needed help. … when you say this is the assumption I’ve made, this is what he conveyed to me in the extended period that we spent together, that he needed Dr Al Muderis to solve the problems. … okay you [Dr Al Muderis] might have created problems, but hopefully you can solve them too. And I think over time eventually it dawned on him that once he sought expert advice elsewhere, that he realised there were other options and he didn’t need Dr Al Muderis any more.
2831 As reflected in the cross-examination of Ms Grieve, the applicant’s submissions as to the respondents’ reliance on Mr Urquhart proceeded on the basis that doing so was ill-founded due to Mr Urquhart’s mental health issues. It was put to Ms Grieve that she “considered [Mr Urquhart] as someone who was unstable, because of his PTSD”. Each journalist gave evidence of their assessment of Mr Urquhart, and why they considered him to be a credible witness.
2832 For example, although Ms Clancy accepted Mr Urquhart was inconsistent at times, and that he had a history of PTSD, she did not consider that he was an unreliable source. She said:
I thought Mark was a reliable source. Mark seemed deeply affected by his experiences with Dr Al Muderis. He also had suffered past trauma as an ex-serviceman and in his youth, so I approached him with caution prior to the interview.
However, after observing Mark in the interview, speaking to him throughout the day, and reviewing his documents, I formed the view that he was a credible witness. I thought he came across as honest and truthful in the interview.
2833 Ms Clancy said that she had further comfort of that belief, as Ms Grieve told her she had spoken to one of Mr Urquhart’s treating doctors who verified the allegations being made. Mr Steinfort accepted that Mr Urquhart was inconsistent at times.
2834 Mental health and related issues do not necessarily render a person unreliable. It would depend on the circumstances. As Ms Grieve explained, “I wouldn’t say that having PTSD automatically undermines someone’s credibility”. The respondents accounted for Mr Urquhart’s mental health in assessing his credibility and reliability, but did not accept that it undermined his evidence. I accept their evidence. Mr Urquhart’s information was not considered in isolation, contrary to the approach taken by the applicant.
2835 I accept that the respondents reasonably believed in all the circumstances that there was a public interest in publishing Mr Urquhart’s central allegation that he felt he was, over an extended period of time, abandoned by Dr Al Muderis, including in relation to recurrent maggot infestations.
2836 The applicant also criticised the respondents in relation to the following passage of Mr Urquhart’s interview, which was not included in the Publications:
Mr Steinfort: There might be people who would say you knew about the risks of this surgery, went ahead with it anyway, and it hasn’t worked out … as planned. What … would you say to them?
Mr Urquhart: I would say, yes, I did know the risks, and yes, actually, [the surgery] did work out. But I wasn’t listened to, and now it hasn’t worked out, and that’s life.
2837 The applicant submitted that, despite this exchange:
… to then publish article after article, broadcast, sneak peek, allegations that Mr Urquhart was not fully informed of risks and complications, in the face of that interview, was wholly dishonest by Mr Steinfort and the other people who are respondents.
2838 Elsewhere in the interview, Mr Urquhart said that the risks and complications are not spelt out clearly enough to prospective patients.
2839 Ms Grieve was also criticised because she removed from a draft of the Articles a reference to Mr Urquhart having been warned about risks. Her evidence was that she did not consider Mr Urquhart had been informed about the “full range of risks”, including maggots (and it is plain from the information before the respondents that he had not been warned about maggots). The Articles reported that Mr Urquhart claimed he was “not properly warned of the risks” (emphasis added). I do not accept the applicant’s submission. It proceeds, as it does in relation to the truth defence, on the basis that if a witness said they were told the risks, they were adequately or fully informed of the risks. Given the information Mr Urquhart provided, the view that he had not been properly warned about the risks was a reasonable one despite his representation that he “did know the risks”.
Mr Smith
2840 The applicant submitted that Mr Smith’s history of mental health issues affected his reliability. The journalists denied in cross-examination that it was irrational for Mr Smith to cut off his own skin.
2841 Mr Steinfort explained his position in cross-examination:
Ms Chrysanthou: Did you form the view that it was likely that Mr Smith had mental health issues in order to [cut off his own flesh with a kitchen knife]?
Mr Steinfort: No. … when you say “likely”, I don’t think that is a cause and effect there. I think this was a man at the end of his tether having not received what he thought was appropriate care for issues that he was dealing with.
…
Ms Chrysanthou: So you understood that had he not cut himself with a kitchen knife and instead gone and seen a surgeon, he wouldn’t have had to have cut himself with a kitchen knife?
Mr Steinfort: I believe he was, as I say, at the end of his tether. He had gone down this path so many times of having to drive significant distances to get treatment, and this was causing serious issues for his life. The point that he was at home and thought, “I can’t keep doing this. Stuff it, I will just do it myself”, spoke to just how mentally crippling the recovery from a procedure like this can be.
…
Ms Chrysanthou: But wasn’t the real question for you, knowing the chronology, why Mr Smith did not see another doctor before he cut himself with a kitchen knife?
Mr Steinfort: It’s hard to imagine what it’s like to be feeling so let down [by one’s surgeon].
Ms Chrysanthou: And did you ask him why he didn’t see another surgeon before he took to himself with a kitchen knife?
Mr Steinfort: I think at that point, he was still believing that, because these people had operated on him, that they were his only hope, his only help, and his only way out of this. So he had to keep dealing with them. It’s similar to Mark Urquhart … once someone does the operation, you kind of need them to help you through the recovery. And he trusted them to that point, until that he didn’t trust them any more.
2842 Ms Grieve explained, when similarly pressed:
Ms Chrysanthou: … you understood, did you, that it was some sort of act of desperation that he took a knife to himself
Ms Grieve: So he had been following Dr Al Muderis’ instructions for a very long time, going to the GP, getting the silver nitrate. He said that that was creating an immense impact on his work life, taking up a lot of time. The pain was so severe that he wasn’t sleeping at night. He was, sort of, you know, sleep deprived, and I think in that point, he took the knife to his skin. … that was an extreme reaction.
Ms Chrysanthou: Right, and it was an unhinged reaction you thought, didn’t you?
Ms Grieve: It was the reaction of someone in significant distress and desperation.
…
Ms Chrysanthou: You understood, didn’t you, that it was not a normal reaction of a person who had the option to seek medical advice, to treat the problems they were having, to take a kitchen knife to themselves?
Ms Grieve: It was someone who felt as though they had been abandoned …
2843 This was in a context where Ms Grieve said she understood that:
… at no point did Dr Al Muderis explain to [Mr Smith] that he could be dealing with hypergranulation that could cause such extreme pain for so many years after the operation, and that maybe silver nitrate won’t work. Maybe you will have to have this constant care. … he didn’t know that. So when that situation was unfolding, he became incredibly distressed, his PTSD was being triggered and he felt like he had been abandoned, because on his telling, Dr Al Muderis said, “Just go to the GP, just do the silver nitrate.” He felt like he didn’t have any solution to this.
2844 Ms Clancy gave substantially similar evidence.
2845 The respondents submitted that these “were reasonable and emotionally intelligent explanations of Mr Smith’s plight”. I agree.
2846 I do not accept the applicant’s submission that the fact that the respondents knew that Mr Smith had not seen Dr Al Muderis for the two years leading up to the Publications should have affected his description of the experiences he had. That was the position Mr Smith was in at the time of publication.
2847 Ms Grieve deposed that, during their first conversation, Mr Smith informed her that:
In about 2018, Mr Smith met Dr Al Muderis in a hotel lobby at a conference related to amputee issues in Australia. During the initial conversation with Dr Al Muderis in the hotel lobby, Dr Al Muderis informed Mr Smith on the spot that he could successfully make him walk again by performing osseointegration surgery. He informed Mr Smith that he should transfer $10,000 into his personal bank account which will secure his spot in the osseointegration program.
2848 The applicant asserted that Ms Grieve’s evidence is false because Mr Smith had never told her that the $10,000 was a deposit; rather, he told her it was the total price of the surgery. In cross-examination, Ms Grieve conceded that statement was not consistent with her notes of her first conversation with Mr Smith. However, she explained that her evidence-in-chief was likely informed by her subsequent conversations with him, in which he did tell her that the $10,000 was a deposit. As the respondents submitted, Ms Grieve was correct because when Mr Smith was interviewed by Mr Steinfort in Ms Grieve’s presence, he said (in the raw footage, but was not included in the published Broadcast):
[The procedure is] quite expensive. And when I met [Dr Al Muderis], I had to transfer [$10,000] into his account before I could even go in the hospital, and then it was put through as a knee surgery with … my private health, as I didn’t have a DVA at that time.
…
I don’t know anyone else who’s had to pay a deposit for … an operation like that.
2849 In a similar vein, the applicant’s submission that Ms Grieve’s affidavit at [305(i)-(l)] is not supported by her notes is incorrect. That material is referred to in Ms Grieve’s supplementary affidavit, with the notes having been produced.
2850 Further, the assertion that Mr Steinfort selectively edited Mr Smith’s answer in the Broadcast in relation to Dr Al Muderis’ motives, cannot be sustained when Mr Smith’s answer is properly read. It is plain from that that what appears in the edited answer is Mr Smith’s opinion.
2851 Although not advanced in closing submissions, I note that during the cross-examination of Mr Steinfort, the applicant accused him of being misleading in relation to what was included in the Broadcast, specifically Mr Smith’s responses concerning whether he had been warned about the risks. Mr Steinfort denied that the editing of what was published resulted in what he knew to be misleading. He explained that the tone used by Mr Smith in his interview when describing what risks were explained to him was dismissive. Although he conceded that it probably would have been helpful to use more of Mr Smith’s responses in what was ultimately published, for “time reasons” not everything could be included, but:
… the nuts and bolts of what [Mr Smith] was saying is that he felt he was shown pamphlets and glossy promotions to say, “This will be the outcome” and he wasn’t told about the issues to the extent that he ended up experiencing of repeated and horrible bouts of hypergranulation.
2852 As the respondents submitted, the substance of Mr Smith’s complaint against Dr Al Muderis was not a failure to disclose the generic risks of the surgery, but rather the marketing of the surgery in glossy brochures as a “successful procedure”, the absence of any information in the public domain about negative impacts, and Dr Al Muderis’ failure to disclose to Mr Smith the risk of “repeated and horrible bouts of hypergranulation”. That does reflect the substance of his complaint. As with all the patients, the concern was not being told about the specific risks that can arise with this type of surgery, not the general risks of having surgery.
2853 That that was the import of Mr Smith’s complaint is apparent from the Articles, where he is recorded in his own words in the break-out section as saying that he has “pain around the rod where skin tries to grow back” (hypergranulation), including the effect on him of burning it off with silver nitrate twice a week, and that he “was never told about the constant oozing, the blood, the pain. It was not what [he] was marketed, not what [he] was sold”.
2854 Finally, the applicant also submitted that at the end of the interview, Mr Smith said that he wanted to put Dr Al Muderis “into a fucking car boot and do something with it”. He submitted any person who would say such an appalling thing, in an apparently serious way, was clearly to be treated with extreme caution, and could not be regarded as reliable or trustworthy. Mr Steinfort accepted that he thought that was a concerning thing to hear from a source. I do not accept that statement per se leads to the conclusion that they should have regarded Mr Smith as unreliable and untrustworthy. The journalist assessed him as a source, as with the other witnesses. His information was not considered in isolation.
Ms Todd
2855 I have already addressed the applicant’s submission about Ms Grieve’s failure to obtain evidence to confirm whether Ms Todd had been told that the remainder of her leg would need to be amputated, or she would die.
2856 The applicant also submitted that Ms Grieve knew that Ms Todd, after being treated for an infection in 2014, had successfully mobilised thereafter for years and that Ms Grieve was given an article published in 2021 about Ms Todd’s physical activity and active life. He submitted she ignored those key matters in preparing the Articles.
2857 A failure to refer to material does not mean it has been ignored. More importantly here, the content of the article and its context need to be borne in mind. The article, properly read, does not suggest that she has successfully mobilised since 2014. The article is plainly an upbeat one, where Ms Todd speaks of having a positive approach. It focuses on her activities at a time well before her osseointegration surgery. It does refer to her swimming, but states that she “can no longer swim because a botched operation in 2014 left her leg vulnerable to infection”. That is a reference to her osseointegration operation at a time well before the Publications. She said she “now walk[s] to keep fit”, which is the extent of the physical activity described.
2858 But this article is also not to be considered in isolation. In cross-examination, Ms Grieve did not accept the proposition that she understood that at least up until January 2021 Ms Todd was highly active. Ms Grieve explained that she understood that there were periods where she was highly active, but she had “described having constant problems, constant hospitalisations, constant infections”. This is consistent with the material before the respondents. There is no basis to suggest the 2021 article was ignored. That said, the submission also reflects the applicant’s general approach to this case; if the patient was mobile (for any period), their surgery was deemed a success, and the patient cannot have a legitimate complaint, or Dr Al Muderis cannot be criticised. That simplistic approach is addressed elsewhere.
Mr Hernandez
2859 The applicant submitted that the Publications presented Mr Hernandez as credible when, in reality, the documents relied on by the respondents demonstrate the contrary and otherwise cast doubt on his relationship with Dr Al Muderis.
2860 In particular, the applicant submitted that documents Mr Hernandez provided to Ms Grieve failed to demonstrate any commercial connection between him and Dr Al Muderis. During cross-examination, it was put to Ms Grieve that she knew paragraphs [49]-[51] of the SMH Article (see Annexure C) were false because she was in possession of documents that demonstrated that: (a) Mr Whelan paid for Mr Hernandez’s surgery; and (b) Mr Hernandez was never engaged or paid commissions or fees by Dr Al Muderis but rather, was engaged by Mr Whelan or his company, whose arrangements with Mr Hernandez were not connected with Dr Al Muderis. As the respondents submitted, neither proposition was supported by the documents which Ms Grieve had in her possession. To the contrary, as discussed elsewhere, the documents in Ms Grieve’s possession supported the published statements. The recitals to the draft contract between Osseointegration International and Mr Hernandez referred to earlier, stated that the “Contractor agrees to provide services to the Practice and the Surgeon” in return for payment, in circumstances where “the Contractor” was defined as Mr Hernandez and “the Surgeon” as Dr Al Muderis.
2861 The applicant submitted that, in any event, the documents as a whole make clear that Mr Hernandez was paid to sell the implants (rather than the surgery). Ms Grieve and Mr Steinfort rejected the suggestion that there was a distinction to be drawn between Mr Hernandez’s promotion of Dr Al Muderis’ implants and the promotion of his surgery. Ms Grieve’s evidence was that she considered the surgery and implants went “hand in hand”. Mr Steinfort’s evidence was to the same effect. When asked whether he understood from the documents he had read that the commission was received for the surgery, or for the sale of the implant, he replied: “It’s one and the same. You can’t have the surgery and what, they’re going to not implant anything?” As he explained, “what was relevant to us was that Fred Hernandez was being financially incentivised to send patients to Australia to undergo surgery with Dr Munjed Al Muderis”. As explained elsewhere, I agree with those descriptions of the evidence. That Mr Steinfort and Ms Grieve held those views is entirely reasonable.
2862 The applicant’s submission on this topic highlights that it is based on his interpretation of the information, an interpretation that need not be accepted.
Ms Stewart
2863 The applicant’s submission that Ms Grieve deleted Facebook messages with Ms Stewart is unfounded. As the respondents submitted, they were provided to the applicant and tendered in these proceedings.
2864 I have already addressed that the applicant’s description that Ms Stewart was overwhelmingly positive, is inaccurate.
2865 The applicant submitted that none of the allegations Ms Stewart made were verified. That submission is not supported in light of the material before the respondents. I will address two examples.
2866 First, the Articles report Ms Stewart’s allegation that her job included directing patients who refused osseointegration surgery to other patients who had positive outcomes. Ms Grieve denied that Ms Stewart’s allegation was not corroborated, highlighting broadly corroborative emails. The respondents referred to three emails in their submissions as examples:
(1) on 12 August 2015, Ms Bosley emailed a prospective patient. She suggested that he speak to Mr Hernandez and join the osseointegration Facebook group (I note that this patient had not refused surgery. I note also that Dr Al Muderis is copied into the email chain and responds after a couple of days following up about what is happening with the patient;
(2) on 31 July 2015, Mr Hernandez and Ms Stewart discussed a prospective patient, who Mr Hernandez said is interested, but they “cannot push on this one”, so he told Ms Stewart he arranged to have Paul (a below-knee osseointegration patient) “to see about getting him to the next step”; and
(3) on 3 February 2016, Ms Bosley emailed Ms Stewart and others about inviting a reluctant patient (who cancelled his initial consultation because he was concerned about the cost) to a clinic to talk to other patients. I note in that email exchange, Ms Livingstone said that she spoke to him when he cancelled, and “despite [her] efforts to convince him to rebook” he was not convinced to do so.
2867 Second, the allegation that Dr Al Muderis overruled colleagues was corroborated, despite the applicant suggesting the contrary in his cross-examination of Ms Grieve. A consideration of the material before them reflects that.
2868 The applicant also submitted that friendly text messages between Ms Stewart and Dr Al Muderis, that occurred between the date that she stopped working at his clinic to 10 June 2022, contradicted her claims about her attitude and relationship with Dr Al Muderis. Ms Grieve disagreed with that suggestion during cross-examination, explaining that Ms Stewart appeared to be processing her feelings about Dr Al Muderis and had sought to maintain a good relationship with him, as part of a process of putting her poor experience of working with him behind her.
2869 The respondents submitted Ms Grieve’s answers displayed a high degree of insight. I agree that the material before the respondents reflects that the applicant has constructed a false dichotomy. Ms Grieve’s assessment of Ms Stewart’s position is not unreasonable. Mr Steinfort advanced a similar view: “[y]ou can get along with someone, but disapprove of their business practices.” He explained:
I’m aware and was aware that [Ms Stewart and Dr Al Muderis] had got along famously … for a very long time, and that it was only in more recent times that she had started to reflect fully upon her time working for Dr Al Muderis and begin to have regrets about the way that she worked for his business.
Testing Broadcast interview subjects
2870 The applicant criticised Mr Steinfort in cross-examination and in his submissions for failing to challenge or test the people he interviewed in the Broadcast (other than Dr Al Muderis), despite being aware there were problems with the reliability of sources. Mr Steinfort did not accept the criticism. He accepted that his job as an interviewer was to test sources and ask questions to expose any credit issues. Nevertheless, he explained that while:
some people needed to be pressed harder than others… sometimes, people that you interview can go into their shell, and that is pretty useless, if you’re trying to get information out of them. So sometimes, you need to take a softer approach.
2871 It was in that context that Mr Steinfort accepted that some of the interviews were not combative. He rejected the suggestions that: he did not interrogate the persons he interviewed; he did not test their claims; he did not employ journalistic rigour in assessing their credibility; or the tone and content of the interviews were more akin to a “mid-morning chat show”. Mr Steinfort explained that testing sources’ credibility went beyond the interview process: “there are numerous instances of things that were alleged by people in their interviews that we went on to disprove ourselves and remove from broadcast”.
2872 The respondents submitted that Mr Steinfort’s responses to these criticisms demonstrated the wealth of his experience and insight. They pressed the Court to find that his approach was particularly intelligent in the circumstances of this case, where many of the people who Mr Steinfort interviewed were traumatised. They also submitted that the applicant’s suggestion that Mr Steinfort adopted a tone more suitable to a mid-morning chat show was overly simplistic and ignored the personal and emotional dynamics that Mr Steinfort had to navigate.
2873 The applicant’s submission, as with many others, is directed to Mr Steinfort’s conduct, not to his belief. That said, I agree with the respondents that the position is not as simple as the applicant suggested. I accept one’s approach to interviewing requires nuance and will vary in the circumstances. Several interviewees in the Broadcast were vulnerable patients who felt that Dr Al Muderis had exacerbated their hardship. It does not follow that, for Mr Steinfort to conduct the interviews in the way he did, that the information provided was not tested or assessed.
2874 The respondents provided examples of Mr Steinfort testing his interview subjects. They submitted that in relation to Mr Hernandez, Mr Steinfort: repeatedly tested his motivations for initially spruiking Dr Al Muderis’ surgery; tested his motives for speaking out against Dr Al Muderis; put to him that he was in the wrong in relation to Dr Al Muderis’ lawsuit against him; and put to him that he had transferred assets to avoid enforcement of a judgment. The respondents also pointed to the fact that when Ms Stewart suggested that Dr Al Muderis turns away only 5% of prospective patients, Mr Steinfort repeatedly challenged her by suggesting that perhaps Dr Al Muderis was trying to help as many people as possible.
2875 As the respondents submitted:
As [Mr Steinfort] said, these were not combative interviews with the patients, and why would they be? One’s not required to cross-examine everybody in the way in which counsel at the bar table does in a serious adversarial litigation, but insofar as there were participants in the broadcast with axes to grind – and the obvious ones were Mr Hernandez and Ms Stewart – a high degree of care was taken in relation to the use of what they had to say.
2876 I do not accept that the approach taken undermines Mr Steinfort’s evidence, or the respondents’ reliance on s 29A.
Ms Amane Nasser
2877 The applicant is critical of the portrayal of Ms Nasser’s case, asserting that Ms Nasser complained post-publication. He submitted Ms Nasser did not consent to her medical details or image being included in the Publications, and that she complained on 21 October 2022 about this and was ignored. Ms Nasser is addressed above.
2878 Ms Grieve gave evidence that Ms Nasser declined to be interviewed on camera, but did not refuse consent for Ms Grieve to discuss her medical issues in the Publications. Ms Nasser declined to attend the scheduled interview with Ms Grieve, with the preceding communications reflecting that Ms Nasser needed to first talk to her producer. Ms Grieve’s evidence was that the information used in the program was from publicly available sources, being Ms Nasser’s public Instagram account and the information from the discussion of her case in Foreign Correspondent. Despite the applicant’s criticism of Ms Grieve, Ms Nasser is only referred to in a very limited way, and only in the Broadcast. Describing what occurred in relation to Ms Nasser does not adversely impinge on the assessment of the Publication being in the public interest.
Dr Anstee
2879 The applicant submitted that Dr Anstee was misled. I simply note that Dr Anstee’s evidence was consistent with the opinions he expressed in the interview with Mr Steinfort. He expressly stated that he still holds those opinions. So much was apparent from his evidence. Considering the material as a whole, I also do not accept the applicant’s submission that the respondents’ published statements of Dr Anstee were knowingly false and misleading.
AHPRA
2880 The applicant submitted that AHPRA complained to Ms Grieve and Mr Steinfort on the day of the Broadcast about the inaccuracy of the claims made in the Broadcast about AHPRA, but that complaint was ignored.
2881 However, ignoring a complaint is not objectively unreasonable simply because one was made. As the respondents submitted, Ms Grieve sought a comment from AHPRA about a range of issues, as is apparent in her correspondence:
A range of allegations have been made about [Dr Al Muderis’] practice, including high pressure sales tactics and the use of testimonials to attract new patients.
We understand much of this activity exists in a regulatory grey zone so it would be great to include an expert opinion from the regulator.
2882 AHPRA’s response is to be considered in that context:
… we are unable to comment on complaints about the conduct, health or performance of NSW medical practitioners as these are not dealt with by Ahpra or the Medical Board of Australia. Any enquiries should be directed to the NSW Health Care Complaints Commission or the Medical Council of NSW.
… we declined the interview as we cannot comment on NSW surgeons. That is for the HCCC or NSW Medical Council.
2883 The response was confined, leaving unaddressed other issues Ms Grieve had raised. I do not accept that Ms Grieve’s refusal to accept AHPRA’s answer was dishonest. Nor do I accept, given AHPRA’s role and the issues raised with them, that the journalists were required to accept that AHPRA could not relevantly comment.
2884 The respondents submitted that AHPRA was able to comment if it saw fit to do so in its capacity as the peak health regulator in Australia and could have furthered the public interest by explaining the confused nature of the regulatory system for the medical profession and its role in that system. It was not unreasonable for the respondents to have held that view.
2885 I do not accept that Ms Grieve misled viewers of the Broadcast about her interactions with AHPRA or misled viewers about AHPRA’s role.
Dr Qutaiba Al Maawi
2886 The applicant complains that Ms Grieve ignored the information provided to her by Dr Al Maawi in respect to the training and set up for patients in Iraq, and that she misrepresented what he said, in an article not sued upon, also published on 19 September 2022. Dr Al Maawi gave evidence that he complained to Ms Grieve after reading the article. In evidence is the correspondence between Ms Grieve and Dr Al Maawi in relation to the complaint and some changes that Ms Grieve made to the article (to which he still complained). Also in evidence is the notes Ms Grieve had of her conversation with Dr Al Maawi. I note that Dr Al Maawi’s evidence in cross-examination attempting to explain the basis of his complaints to Ms Grieve reflected that some appeared to be based on very subtle distinctions. He did not seem to want his name associated with aspects of what, on Ms Grieve’s evidence, he told her. In any event, it does not follow that because a complaint was made, that it necessarily has substance. The applicant put to Ms Grieve in cross-examination that in publishing what she did in the Broadcast about the Iraqi patients feeling neglected, it was misleading. Ms Grieve disagreed with that, referring to material before the respondents at the time of publication. I accept her evidence.
Sensationalism and language in the Publications
2887 Returning to the Publications.
2888 The applicant submitted that the Sneak Peek and the Grieve Video are sensational. Before addressing them, it is appropriate to refer to the principal Publications: the Broadcast and the Articles. In respect to the Broadcast, that submission is only made in respect to the video of patients’ consent (addressed above at [2637]). I note there was also a suggestion in cross-examination, that “the real reason” the maggot video was played repeatedly was for shock value.
2889 The respondents properly accepted the video was shocking. Mr Steinfort explained:
… for people that are considering this kind of procedure … there had been numerous stories on how wonderfully this pans out for patients. It was immensely in the public interest for anyone who would consider this operation in future to be fully armed with the reality of how this could actually pan out. And how, as Dr Al Muderis said himself, it’s not uncommon for people to get maggots after this. Doesn’t put that in the brochure.
2890 However, he “completely disagree[d]” that the real reason why it was shown repeatedly was for shock value. He explained it was shown repeatedly because when the Broadcast:
… come[s] back to talking [to] Dr Al [Muderis] about it, it’s 30 minutes later in the broadcast. There is every chance that someone was watching [another channel] at that point in time, and has flicked over and has no idea what we’re talking about. … you can’t have assumed knowledge for people that they have seen what has been referred to earlier.
2891 The applicant did not make any submission in closing that the Articles were sensationalised. Nevertheless, I propose to address two related topics which were the subject of the applicant’s cross-examination.
2892 First, the applicant cross-examined Ms Grieve on the use of the word “botched” in the headline of the SMH Article and the word “mutilated” in its first paragraph. In relation to “botched”, Ms Grieve said that she considered that to mean “to have not done something to a reasonable standard of care”, rather than negligent in the legal sense. She accepted that “mutilated” meant “to leave someone grossly deformed”, and beyond the normal scarring of surgery. Her evidence was that a planned surgical amputation is a mutilation if it is not necessary or well-advised. Mr Steinfort described “mutilated” as “damaged” and being “worse off than when [the person] began”. Both journalists gave Mr Urquhart as an example. The Articles employ the word “mutilate” as context to descriptions of Mr Urquhart’s circumstances, including the condition of his legs at the time he saw his new doctor.
2893 The respondents in closing described “mutilated” and “botched” as “colourful words”. They submitted “botched” simply means “got wrong”. They submitted “mutilated” would have been understood by ordinary reasonable readers, in the context of the Publications, to mean that “the patient has been left off worse than before, whether by physical injury, scarring, disfigurement or other debilitation”, (in cross-examination Ms Grieve and Mr Steinfort gave as an example, Mr Urquhart). The words used are colourful, but I accept that is how they would have been interpreted. Their use would not have been misleading. That said, I accept that language used in a publication can impact on the issues raised in the s 29A defence. This does, however, highlight the importance of language, and the care that does need to be taken. The issue is not whether other words might have been used, but the effect of the words used on the issues to be decided.
2894 Second, the applicant criticised the phrase “wheelchair-bound” in relation to Mr Urquhart and Ms Todd during cross-examination. Ms Grieve’s evidence was that Mr Urquhart was wheelchair-bound, without legs, despite having walked following his surgery. The Articles make plain he walked for a while after the surgery. In the Articles, the phrase in relation to Mr Urquhart is particularised: “Now, Urquhart is wheelchair-bound once again”. That tells against the suggestion that the phrase is misleading. The criticism in relation to Ms Todd is that she is pictured in a wheelchair. Ms Grieve’s evidence was that she understood that at that time, Ms Todd was regularly using a wheelchair, and that Ms Todd had told her she was wheelchair-bound.
2895 The subject matter of the investigation is inherently sensational. As explained above, there are explanations given for why those matters appeared as they did. They do not distort the information that was before the respondents. This must be considered in the context of each matter, considered as a whole.
2896 Turning to the Sneak Peek and the Grieve Video. As mentioned earlier, it is fair to describe that very little attention during the trial or closing submissions was directed to these publications.
2897 The applicant submitted that the Sneak Peek was an advertisement, it was sensational, dramatic with music, and published for the purposes of promoting the Broadcast. He submitted that it was not a piece of investigative journalism, and no truthful journalist would believe that it was in the public interest. That is the extent of the submission. As recognised above, it is plainly an advertisement. So much is clear from the applicant’s written submissions.
2898 I do not consider that the imputations in relation to this publication have been conveyed, and therefore consideration of this defence is unnecessary.
2899 That said, I propose to address the submission. It is plainly an advertisement, and not, of itself a piece of investigative journalism. Those features by themselves do not necessarily preclude the application of s 29A. Advertisements are a “matter” under the Defamation Act s 4, and the public interest defence is not limited to journalism. On a more practical level, if advertisements were viewed otherwise, programs involving investigative journalism could never advertise and enjoy s 29A protection. Its viewers would understand it was an advertisement and view its content as such. It plainly does not contain the whole story, or purport to. It is designed to have viewers watch the Broadcast, which the respondents subjectively believe is in the public interest. Mr Steinfort and Ms Clancy each gave evidence that it is in the public interest because it is pointing people towards the fuller piece, which is in the public interest. The assessment of its content is against that background, including the respondents’ submission that they reasonably believed there was an ancillary or attendant public interest in its publication.
2900 In relation to the Grieve Video, the applicant submitted that it is sensational and exaggerated with baseless claims. He highlighted Ms Grieve’s concluding comment in the matter: “I’ve spoken to more than a dozen high profile surgeons in major Australian hospitals. They describe [Dr Al Muderis’] practice as unethical at best, dangerous at worst”, which he contended is highly misleading. Again, that is the extent of the submission.
2901 In oral submissions, the applicant submitted that:
Ms Grieve says in the [Grieve Video] that over a dozen doctors told her my client was unethical at best, dangerous at worst. … if she’s not telling the truth about that, she cannot win the [s 29A] defence for that publication, and the onus is on my learned friends to prove that she’s telling the truth about that, to prove in the material that over a dozen doctors said that to her.
2902 It was put to Ms Grieve in cross-examination that the number of surgeons, patients and business associates referred to in the SMH Article as having held concerns about Dr Al Muderis’ patient selection and aftercare was “utterly inaccurate”. A similar proposition was posed in relation to the reference to surgeons in the Grieve Video. While under cross-examination, Ms Grieve produced a list to verify her tally. It was tendered. Having received that list, the applicant did not make any closing submissions about it.
2903 Having considered the list and the material before the respondents, in relation to the Grieve Video, there is material from over a dozen surgeons which contains statements with the import to support the passage complained of. A review of the respondents’ Aide Memoire 2 confirms that list to be broadly accurate.
Conclusions as to the applicant’s submissions
2904 As already explained, I am satisfied that Ms Grieve, Mr Steinfort and Ms Clancy each held the subjective belief that the Publications were in the public interest. In making that finding, I have considered, inter alia, the applicant’s submissions. I do not consider that the applicant’s submissions, considered together, undermine the evidence of Ms Grieve, Mr Steinfort and Ms Clancy as to their subjective belief that the Publications were in the public interest. Nor, as evident from my conclusions throughout Section 13 and Section 14, do they undermine the objective reasonableness of the respondents’ belief. The applicant’s approach considers matters in isolation and fails to grapple with the extent and breath of the information obtained by them in the investigation, and the basis of the public interest. Contrary to the applicant’s contention, his submissions do not evidence that the respondents were engaged in a “malignant, dishonest and malicious campaign” against him.
Section 14 — Conclusions
2905 As stated above, I accept that each of the journalists held the requisite subjective belief in the Broadcast, Articles, Grieve Video (and Sneak Peek).
2906 It is important to recall that this defence focuses on whether the respondents have established that they reasonably believed the publication of the matters was in the public interest. The focus is on the belief. As previously explained, flaws in a matter will not necessarily preclude the application of the defence. It is appropriate to recall that a publication does not need to be free from error to be capable of being in the public interest in accordance with s 29A.
2907 The question of whether, in relation to a matter, a journalist’s belief that its publication is in the public interest is a reasonable one, involves an assessment of that belief in the context of all the information garnered from the investigation that the journalist had. Although the content of the matter is plainly relevant, its assessment is in that broader context. The nature of the publications and the medium on which they are published are also relevant (e.g. an advertisement has a different purpose and would be understood by a viewer in a different manner compared to a broadcast or article). The nature of the mediums also necessarily impacts on the amount of content, its formatting and presentation (and the manner it is received). There are constraints of time, for a televised broadcast, and space, for newspaper publications.
2908 The assessment of the reasonableness of the belief is in the context of the nature of the public interest, the subject of the belief.
2909 Put simply, the question is: having regard to all the information available to the respondents, have the respondents established that the belief they held (which I am satisfied is subjectively held) that the publication of the matters was objectively reasonable.
2910 I have considered the applicant’s submissions in the context of the information available to the respondents in my assessment of the objective reasonableness of their beliefs.
2911 A consideration of the information before the respondents necessarily includes, amongst other things, its nature, content and quality, the sources (including the fact there are confidential sources), and whether there is support for the accuracy of the information.
2912 The public interest existed, as described by the journalists, in the context of the positive media coverage about Dr Al Muderis up until that time. The investigation they had undertaken was extensive, with some 76 sources being spoken to (being a diverse cohort) and thousands of pages of emails, business records and scientific papers. It was also in the context of the publicly available information (e.g. Ford). A consideration of the material gathered by the respondents reflects common themes. There was a cohort of patients who had negative experiences with Dr Al Muderis with significant similarities. Given the positive portrayal, and the nature of osseointegration surgery, the journalists describe the public interest being the public, especially prospective patients, being informed of the other experiences. As I have discussed above, this is an elective surgery, which is highly invasive and brings with it potential risks and complications that can be ongoing and adversely affect a patient’s quality of life.
2913 I have highlighted above several factors which tell in favour of the journalists’ beliefs being objectively reasonable: see [2699]-[2713]. It is unnecessary to recite those considerations here. Suffice to say, they include the respondents’ approach to the investigation and the Publications. In the circumstances, those factors directed to that weigh heavily in favour of the reasonableness of their beliefs.
2914 Having regard to the information available to the journalists at the time of the Publications (and considering the submissions advanced), I am satisfied that the respondents have established that their beliefs that it was in the public interest to publish the matters, were objectively reasonable.
2915 It follows, that I am satisfied that the defence is established in relation to each relevant respondent for the Broadcast, the Articles and the Grieve Video. As mentioned earlier, as I do not consider the imputations in relation to the Sneak Peek have been conveyed, as such, the defence is not necessary to consider for this publication. If it were necessary to decide, I accept in the circumstances (and based on my discussion above) that the respondents’ belief that the Sneak Peek is in the public interest is a reasonable one on the material before them.
Section 15 — Ongoing belief
2916 A further dispute between the parties was, if the defence were to be established, whether the circumstances which have transpired since the first publication of the Publications means that the respondents no longer reasonably believe that the Publications, to the extent they remain available to be viewed, read or downloaded from the internet, are in the public interest. The applicant pleaded that if the respondents held a reasonable belief that the matters were in the public interest at the time of the Publications, they no longer do so by reason of a subsequent change in circumstances. I note the journalist each gave evidence that they still hold the belief.
2917 Given the public interest defence is established it is appropriate to address the parties’ submissions on this point. For the reasons below, I do not accept that the defence has been lost in respect to any of the Publications (for which it has been established).
2918 Although factually this issue did not arise for consideration in Russell, Lee J observed at [341]:
English authorities have recognised that, even if the respondent reasonably believed that publication was in the public interest at the time of initial publication, the defence may be lost if circumstances change, such that the [respondent] no longer holds the belief or the belief is no longer reasonable: Flood v Times Newspapers Ltd [2010] EWCA Civ 804; [2011] 1 WLR 153 (at 177 [78] per Lord Neuberger MR); Lachaux QB (at [159] per Nicklin J); Banks v Cadwalladr QBD (at 5270 [135] per Steyn J).
2919 Apart from Russell, there has been no meaningful consideration of this issue in Australia.
2920 Although the general proposition as articulated by Lee J can be accepted, it is necessarily confined to the ongoing publication of matters and so can only really apply to those fitting that category (e.g. online publications).
2921 Little attention was paid in submissions to describing what, in practical terms, is necessary to qualify as a change of circumstances. The respondents submitted the position can arise:
… where a publisher publishes an allegation of fact, reasonably believing that fact to be true, and then [after publication] is presented with incontrovertible evidence that the central fact underlying the publication is false, but then declines to take the matter down.
2922 The applicant’s submissions centred around a complaint that, post-publication, the respondents have had access to information contradicting “many of the specific allegations in the Publications”.
2923 In Banks v Cadwalladr [2022] EWHC 1417 (QB); [2022] 1 WLR 5236 (Banks), referred to in Russell, Steyn J explained that a change of circumstances necessarily focuses on a consideration of whether there has been a “significant change of circumstances”: at [134]-[135], [400]-[415]. Logically, that must be so given the terms of s 29A; any change would need to be such that, considering all the circumstances, it leads to a respondent ceasing to hold a belief that publication of the matter was in the public interest, or to such a belief ceasing to be reasonable. I note that although this proceeding went on appeal, this aspect of the judgment was not affected: Banks v Cadwalladr [2023] EWCA Civ 219; [2023] 3 WLR 167 (Banks (Court of Appeal).
2924 Two UK cases offer instructive examples of changes of circumstances leading to a loss of the public interest defence.
2925 In Flood v Times Newspapers Ltd [2010] EWCA Civ 804; [2011] 1 WLR 153 (Flood), a June 2006 online publication reported that Mr Flood, a police sergeant, was under investigation for making unauthorised disclosures in exchange for money. The report had attracted the common law Reynolds defence (the antecedent to the statutory public interest defence: UK Act s 4). In early September 2007, the publisher was informed that the internal investigation, and an accompanying report, failed to find any evidence that Mr Flood had engaged in the alleged conduct. The Court concluded that the defendant had ceased to attract the Reynolds defence after that time. Lord Neuberger opined that “once the report’s conclusions were available, any responsible journalist would appreciate that those allegations required speedy withdrawal or modification”: at [78].
2926 In Banks, the situation was similar, although by this time the statutory public interest defence had been enacted (and the Reynolds defence abolished): UK Act s 4. The Court concluded that the public interest defence had been established in one of the original publications, an April 2019 TED Talk (the other publication, a Tweet, was found not to be defamatory because it was not demonstrated that it caused or was likely to cause serious harm: UK Act s 1). A video of the TED Talk was published on TED’s website shortly after it was given. The trial judge determined that the single meaning of the TED Talk was that:
… on more than one occasion Mr. Banks told untruths about a secret relationship he had with the Russian Government in relation to acceptance of foreign funding of electoral campaigns in breach of the law on such funding.
See Banks v Cadwalladr [2019] EWHC 3451 (QB) at [45].
2927 The National Crime Agency (NCA) and the Electoral Commission had responsibility for determining whether Mr Banks had breached the law. In September 2019, the NCA published a statement to the effect that it had found no evidence Mr Banks had committed any criminal offences. Steyn J opined at [406]:
The NCA’s investigation and decision demanded appropriate respect. But that is not the same as saying that it was beyond reasonable questioning, or criticism. On the face of it, when the NCA’s statement was made, there appeared to be a difference of view as to the law between the NCA and the Electoral Commission. … The Electoral Commission appeared to have regarded [Mr Banks’ conduct] as impermissible … In these circumstances, I do not consider the NCA’s statement alone was such a significant change as to render the defendant’s continuing belief that publication of the TED Talk (without amendment or qualification) was in the public interest unreasonable.
2928 The Electoral Commission and Mr Banks (and others) released a joint statement on 29 April 2020 accepting the NCA’s conclusions. Justice Steyn at [407]-[408] found that constituted a significant change of circumstances:
Once the Joint Statement was made, in my view, it was no longer reasonable to believe that it was in the public interest to assert that there were grounds to investigate whether the source of Mr Banks’s donations was foreign funding, accepted in breach of the law on the funding of electoral campaigns, at least, without any qualification referring to the NCA’s statement and the Joint Statement. …
Accordingly, I consider that the public interest defence fell away on 29 April 2020.
2929 The changes in these cases were the result of institutional investigations and conclusions into the events which were the subject of the publications. Both investigations brought the allegations inhering in each publication’s sting into considerable doubt. It can be readily understood how matters of that nature may result in a conclusion that a belief in the public interest is no longer reasonably held. These cases are vastly removed from the circumstances of this case.
2930 The Banks proceedings also discuss a requirement that, if the public interest defence is lost, serious harm must be demonstrated again. The respondents in this case submitted that if the defence is lost, an applicant must demonstrate serious harm to their reputation on and from the date the defence was lost, by reason of publications occurring after that date, for the cause of action to be complete, citing Banks (Court of Appeal) at [41]-[51]. The applicant accepted that there are “some observations about this in … Banks v Cadwalladr”, but submitted they do not “apply to the structure of the” Defamation Act. Given my conclusions below, it is unnecessary to resolve this issue. However, if the defence is lost, what damage is done by the continued publication will necessarily depend on the time for which the publication continues. This requires some precision with the plea of a change of circumstances. Each of the cases referred to above nominated dates of specified events that were said to be a change of circumstance. That degree of specificity was not articulated in this case.
2931 The applicant’s pleadings nominated several changes of circumstance which were said to alter the respondents’ reasonable belief (if established), namely, the provision of:
(1) the information in the concerns notice;
(2) the information in the SOC;
(3) medical records in response to subpoenas;
(4) the applicant’s discovery; and
(5) the affidavits served by the applicant.
2932 As pleaded, these are to be regarded as alternative events (i.e. occasions that may have caused the defence to be lost).
2933 The applicant’s written submission in chief on the factual matters concerned with this topic of continuous publication is scant (five paragraphs). The applicant made a general assertion that the medical records contradict many of the specific allegations, but despite that, the Publications remained online. He then asserted:
[The respondents] without a doubt know about the maggot text messages, the false imputation about Febreze, that Ms Todd still has her implant in and is not dead, that Brennan Smith last happily saw Dr Al Muderis for a free operation in COVID in 2020 and has never been ignored or turned away since, that Blythe Warland lost his house, business and partner over a year before his osseointegration surgery, that Michelle Koolhoven is not Ms Oritz, does not want her picture in the newspaper and did not break her leg 6 years after surgery.
2934 He also submitted that it must be clear to the respondents that the Articles mislead the public about the benefits of osseointegration.
2935 The applicant concluded:
By reason of those examples alone [the respondents] cannot still honestly hold the view that the Publications are each in the public interest. If they do – that view is plainly not reasonable. If the defence somehow succeeds for any of the Publications, it has plainly now been lost.
2936 The respondents submitted:
There has been no change in circumstances since the Publications were first published which would support a finding that the respondents’ belief is no longer reasonably held. At most, the evidence at trial has revealed errors in relation to isolated and peripheral facts that do not contradict or undermine the substance or sting of the Publications, or detract from the overwhelming public interest in the Publications.
2937 Given the nature of the applicant’s submission, it is important to recall that the defence is directed to public interest in the matter, not to imputations.
2938 Apart from the alternative pleadings in amorphous terms, the applicant does not identify when the public interest defence was said to have been lost (noting that in relation to at least three of those categories in the pleading, all the material would not necessarily have been provided at the same time). The list of alternatives is so general as to be of no assistance. Apart from the concerns notice, these documents were provided in accordance with Court orders in relation to the preparation of these proceedings. The respondents filed a defence and their evidence in support. This was a contested hearing, and these were contested facts. The difference between this and the types of change of circumstances in Flood and Banks is self-evident.
2939 Turning to the matters that the applicant referred to in their very brief submissions on this topic. These purported errors are matters of detail that do not alter the substance of the defamatory sting conveyed by the Publications.
2940 First, in relation to the medical files said to contradict specific allegations in the Publications about a number of patients, it is no more than a bald general assertion. There is no articulation by the applicant as to what record, when, and in respect of which patients. That approach is inadequate. In any event, as is clear from my consideration of the truth defence, the medical records do not contradict the import of what was being said by the patients (as reflected in my factual findings in relation to contextual truth in Parts 5 to 7). That the patient may be unreliable about details does not necessarily alter that conclusion. The medical files also cannot be viewed in isolation. No particular aspects of the medical records and what they are said to contradict are identified. Given my findings in respect to the patient case studies, I do not accept the applicant’s submission.
2941 Second, in relation to the maggot text message (i.e. Mr Urquhart receiving a response from Ms Roberts to the maggot video he texted), the import of what was said, as explained above, remains. Therefore, although I accept that the allegation in the Broadcast could have provided additional detail, that cannot be said to amount to a change of circumstances sufficient for the defence to be lost. It did not alter the reasonableness of the belief held by the respondents at the time of publication.
2942 Third, in relation to the Febreze statement, Ms Grieve conceded the language was unfortunate. As discussed above at [2794], she did not expressly attribute it to Dr Al Muderis, where the complaint is based on implication. She gave evidence that if she had her time again, she would make clear that it was a colleague. That said, as Ms Grieve explained, the sting of the imputation that Mr Urquhart felt abandoned, and that the incident was a turning point for him, remained. The comment was in a team context, and I note elsewhere that Dr Tetsworth, the colleague who made the comment in the consultation, gave evidence that there was nothing wrong with recommending Febreze and he has done so on other occasions.
2943 Fourth, as explained above, I do not accept the interpretation of the evidence advanced by the applicant in relation to Mr Smith.
2944 Fifth, although the information Ms Grieve had at the time was that Mr Warland lost his house, business and partner over a year before his osseointegration surgery, Mr Warland accepted in evidence he was wrong about the timing.
2945 Ms Grieve’s evidence was that, after Mr Warland gave evidence in these proceedings, he had confirmed with her he had muddled the timeline. Although it may be accepted this is a change of circumstance, I do not accept that, in all the circumstances, it is of a kind leading to a loss of the s 29A defence.
2946 Ms Grieve gave evidence that she had a discussion with her editor as to whether she should remove the statement concerning Mr Warland but, ultimately, she came to the view that this was a small detail that did not bear on the public interest in the story. The respondents submitted that was “an understandable position to adopt in the context of fiercely contested and unresolved litigation”. I agree. The defence is directed to a respondent’s belief that the publication of the matter was in the public interest, not its defamatory imputations, viewed in isolation.
2947 Sixth, I do not accept that the language in the Articles in respect to Ms Koolhoven, “six years after surgery, [her] leg broke”, would have been understood as her leg breaking as opposed to her implant or componentry breaking. The statement was immediately followed by the word “and was replaced”. As the respondents submitted, this could only have been understood by ordinary readers as a reference to the statement, a mere five sentences later, that her “Type B implant” broke. As Ms Grieve reasonably stated, “for [amputees] it’s their leg” and ordinary readers would have understood this in the context of an article about amputees.
2948 I note the Articles’ use of Ms Koolhoven’s previous surname, and its misspelling, but these could hardly be suggested to affect the respondents’ reasonable belief that the Publications were in the public interest, yet it is relied on by the applicant.
2949 Seventh, as previously explained, I do not accept that the Publications mislead as to the benefits of osseointegration, given the nature of the Publications.
2950 Eighth, I do not accept the submission in relation to Ms Todd’s implant, for the reasons expressed above.
2951 These, it can be assumed, are the high points of the applicant’s case on this aspect. As the trial has shown, none of the events or assertions recorded in those documents necessarily or obviously disproved the allegations in the Publications. They were challenged by the respondents.
2952 I accept that each of the journalists maintained a reasonable belief that the Publications are in the public interest, including the evidence they gave to that effect. Ms Grieve and Mr Steinfort explained that was so despite the minor errors, and that those errors did not impact on the import of the Publications, or the overarching public interest.
2953 That view is manifestly correct, and an understandable position to adopt in the context of fiercely contested and unresolved litigation.
2954 The respondents submitted that the Court should find that, notwithstanding that the Publications contain a small number of factual errors, exposed as a result of the resources and energy that has been devoted to the conduct of this trial, those errors are matters of detail that do not alter the substance of the defamatory sting conveyed by the Publications, and that the respondents continue to reasonably believe that the Publications as a whole remain in the public interest. They submitted it is a testament to the thoroughness of the research underlying the Publications that, after a 16-week trial, and the vast amounts of information that is available to the Court but were not available to the respondents at the time of publication, the factual errors exposed are so trivial, and do not undermine the themes of or public interest in the Publications.
2955 I agree as to their description as to what was exposed in the trial. In my view, the matters the applicant relies on do not undermine the respondents’ reasonable belief.
PART 10 — CONCLUSIONS WITH RESPECT TO THE PROCEEDINGS
2956 As explained earlier, given my conclusions in respect to the s 26 and s 29A defences, it is unnecessary to consider the defence in s 30 of honest opinion.
2957 Given the defences have been successful, the question of damages does not arise. Any consideration would be hypothetical, and I do not consider that would be appropriate in this case.
2958 The proceedings are dismissed. In the ordinary course, costs would follow the event.
I certify that the preceding nil (2958) numbered paragraphs are a true copy of the Reasons for Judgment of the Honourable Justice Abraham. |
Associate:
Dated: 8 August 2025
ANNEXURES
Annexure A — Sneak Peek transcript
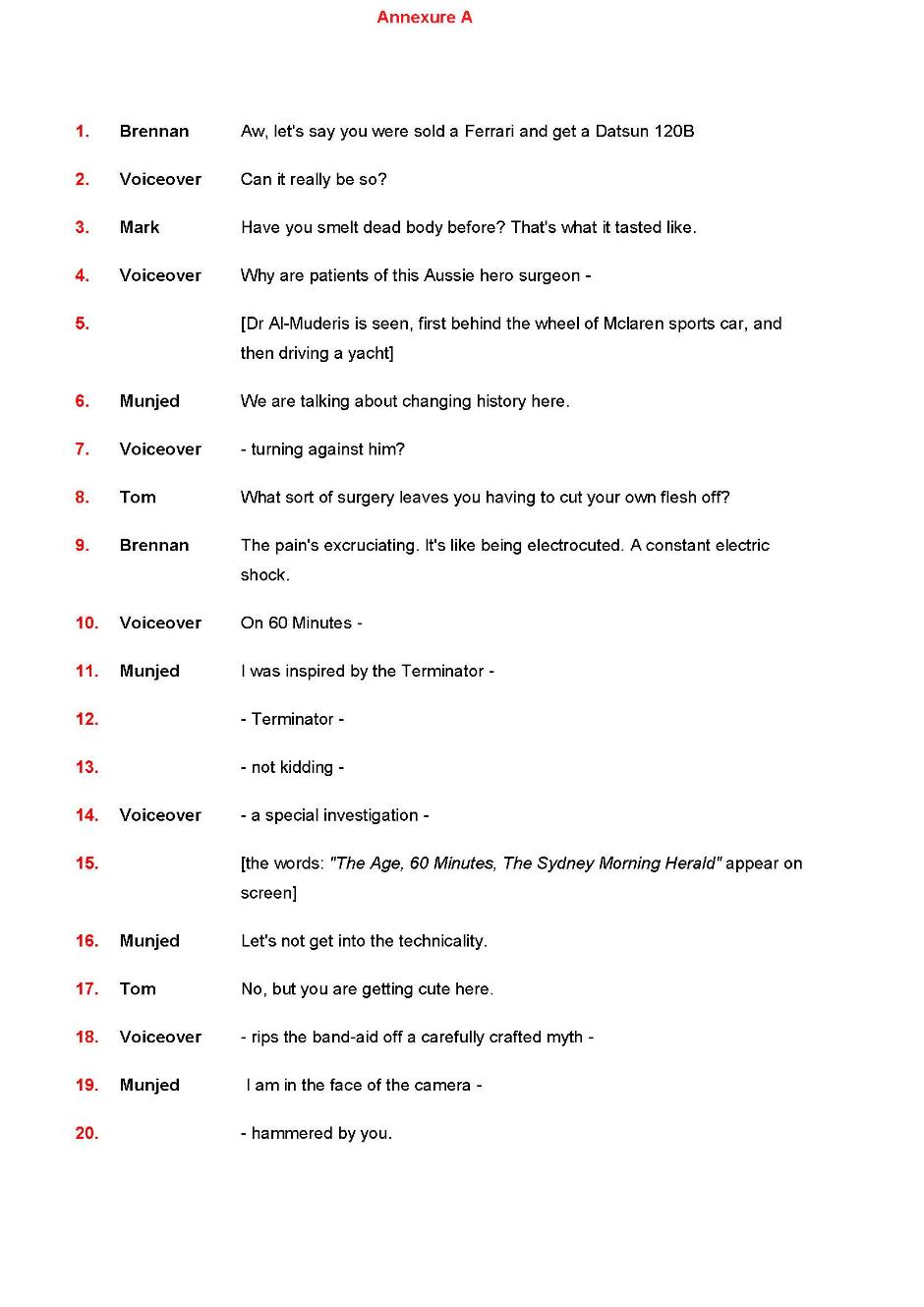
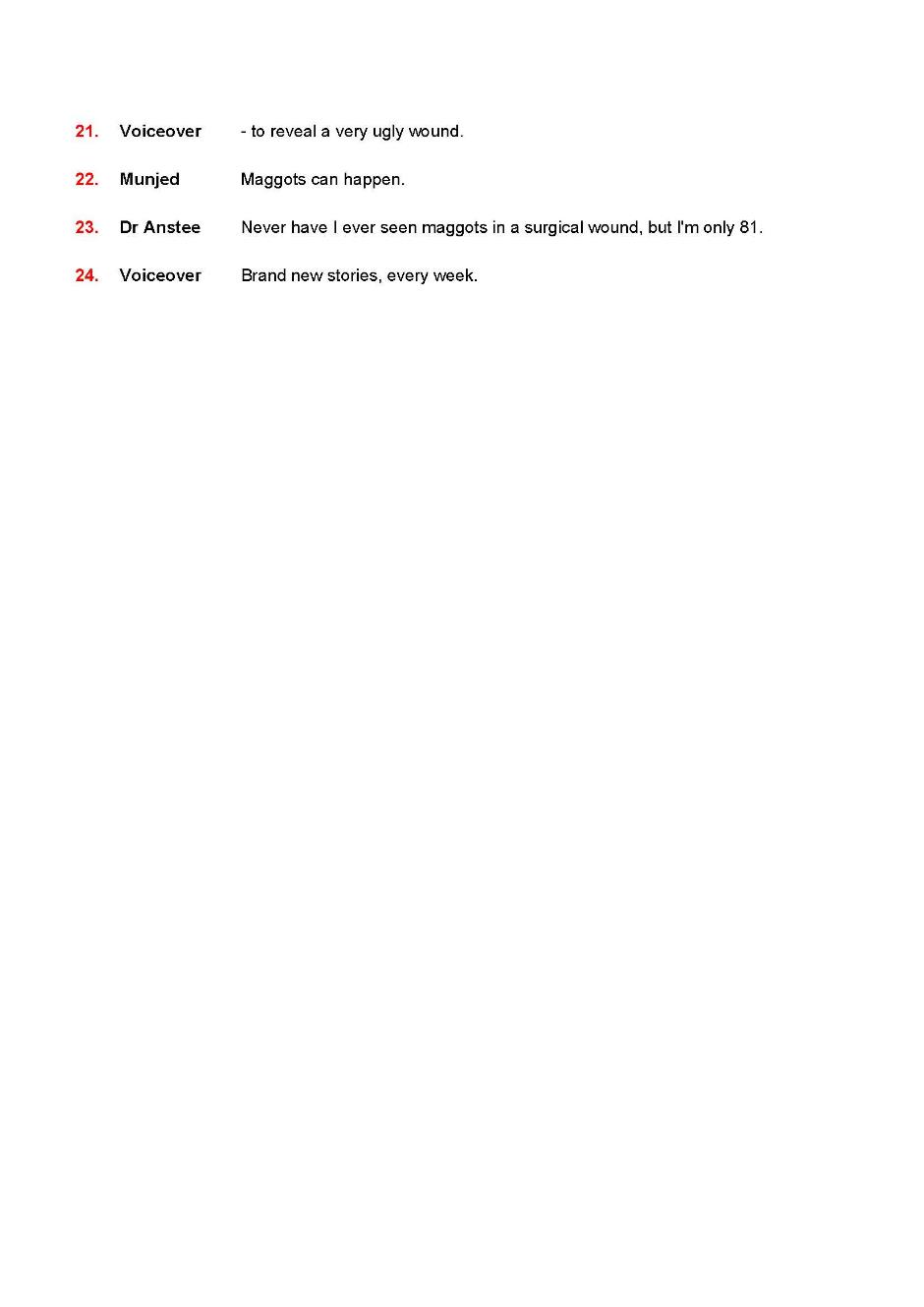
Annexure B — Broadcast transcript
Annexure C — SMH Article
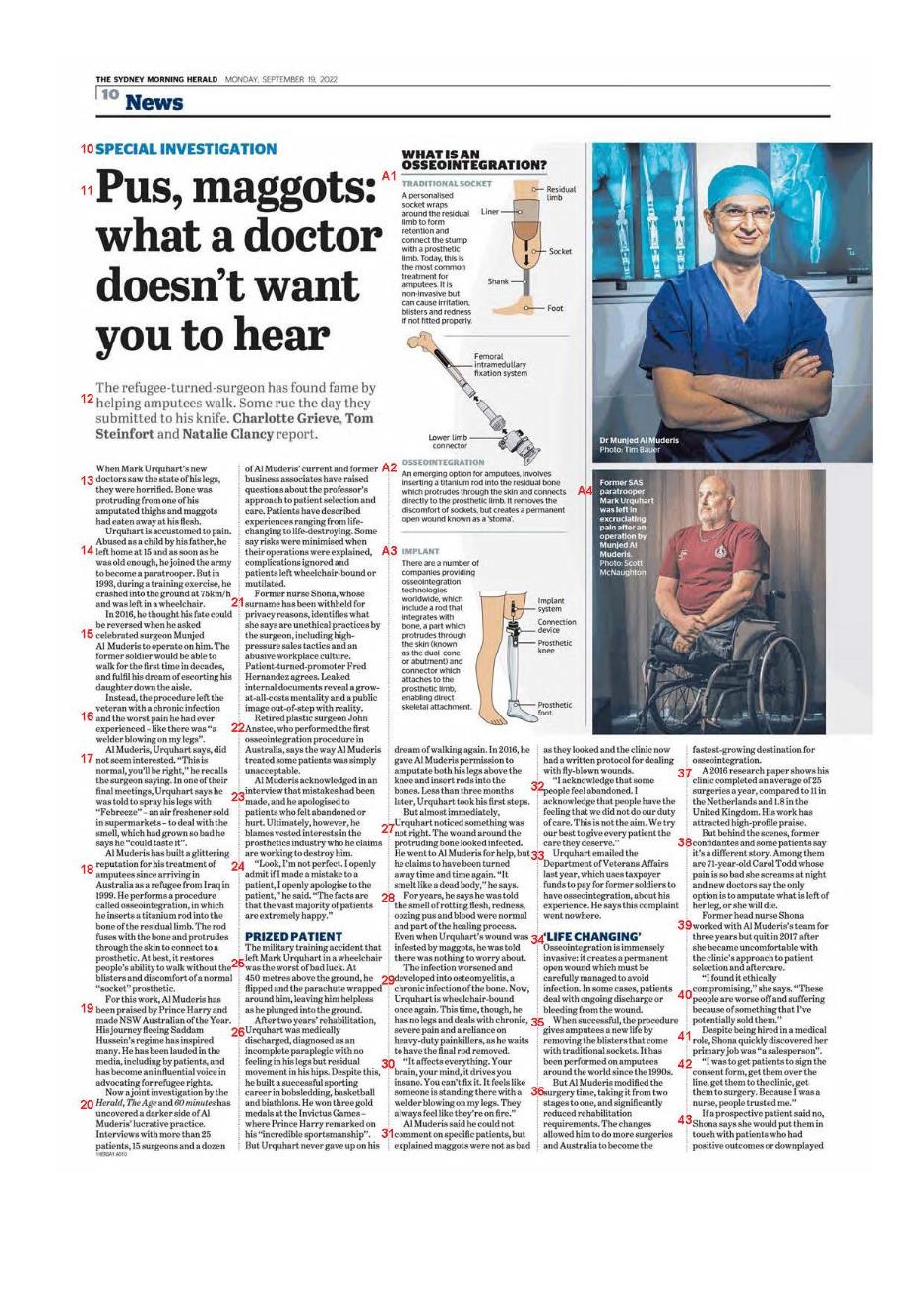
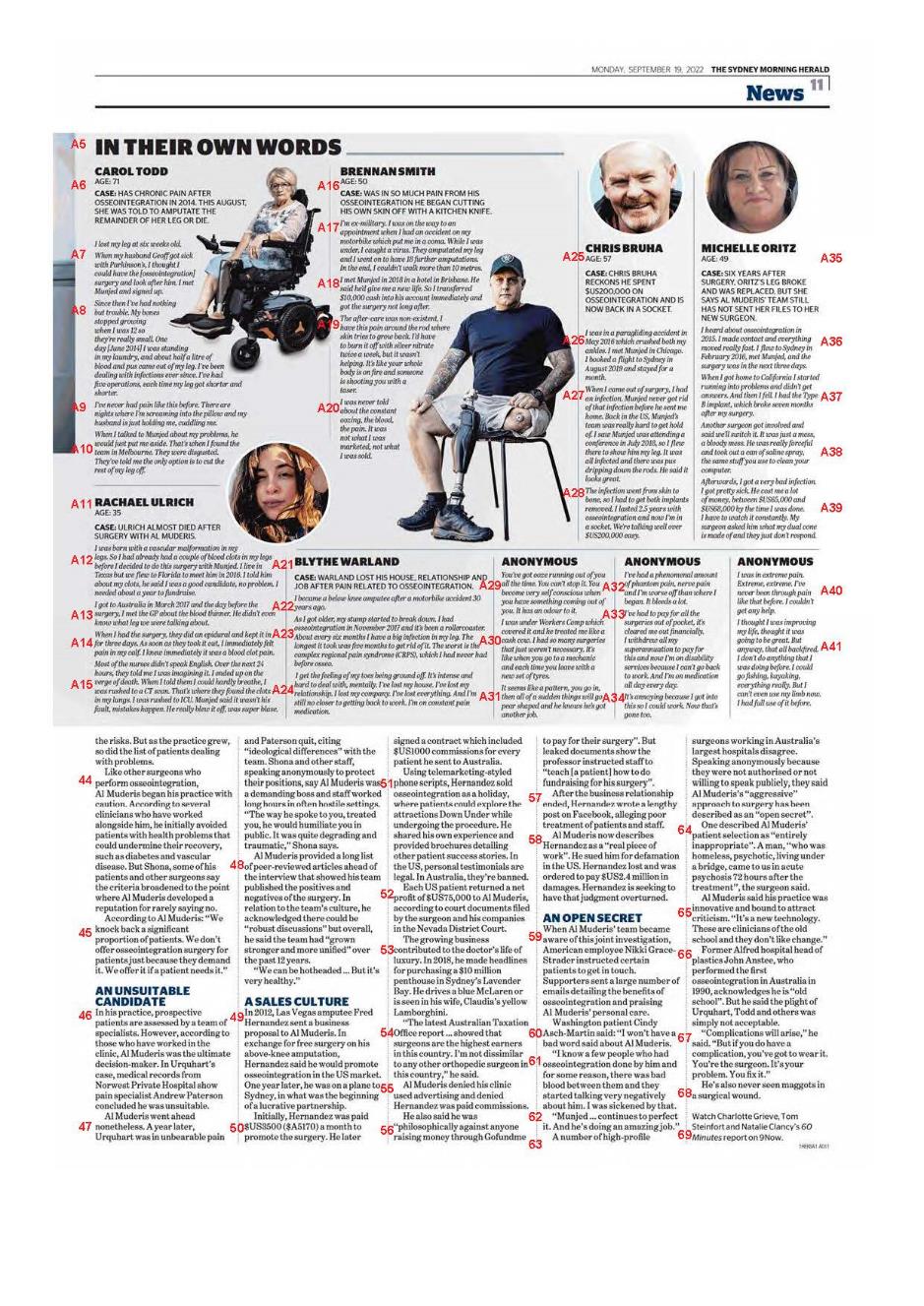
Annexure D — SMH Online Article
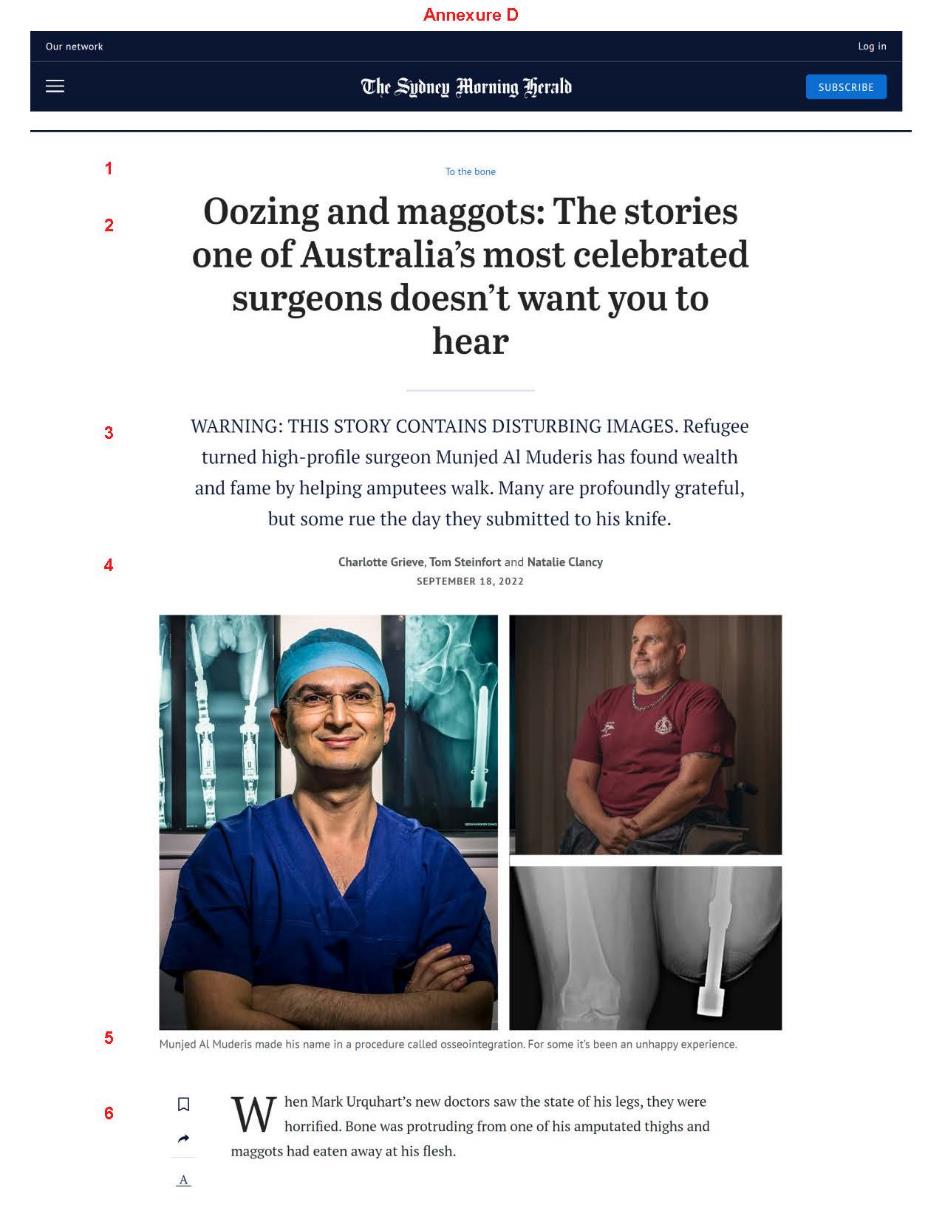
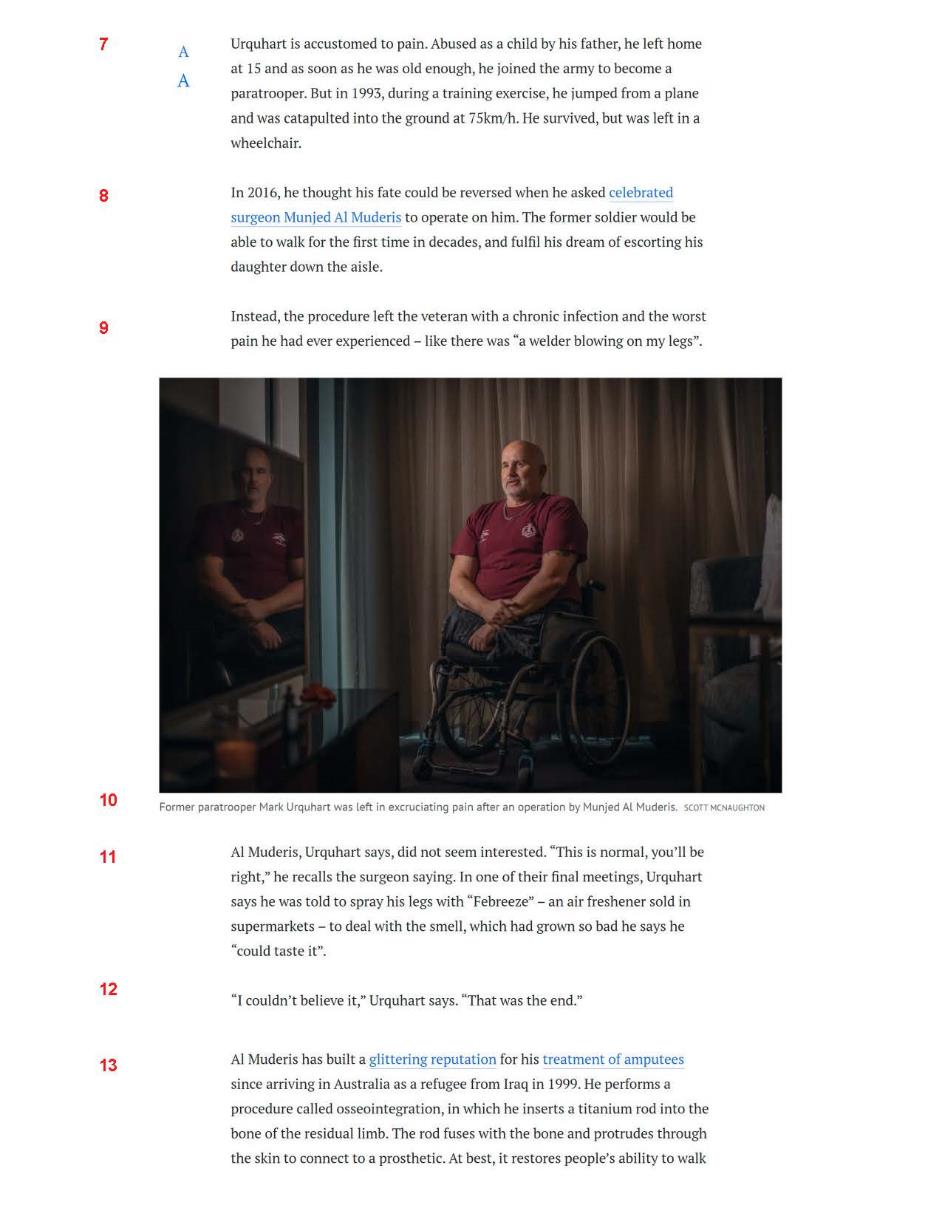
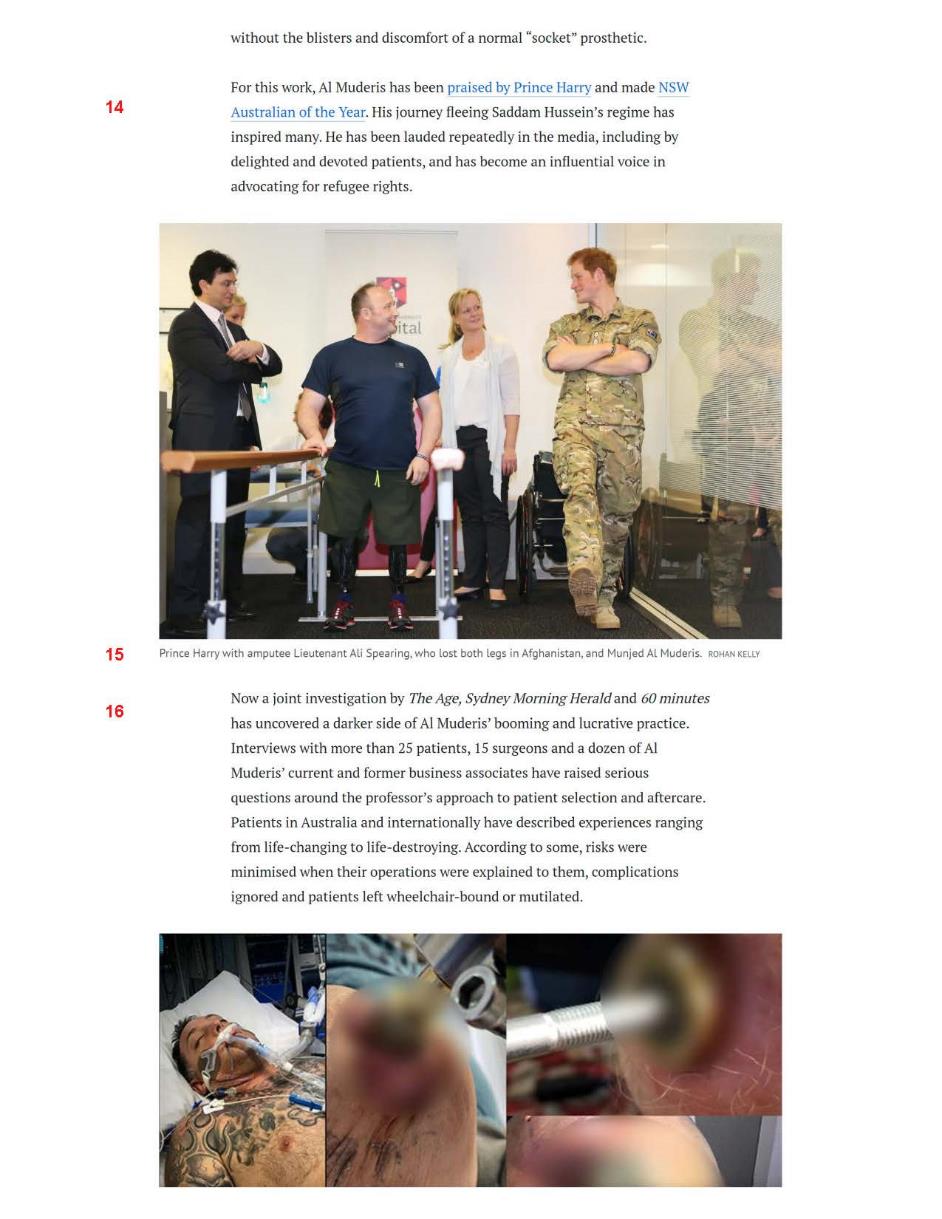
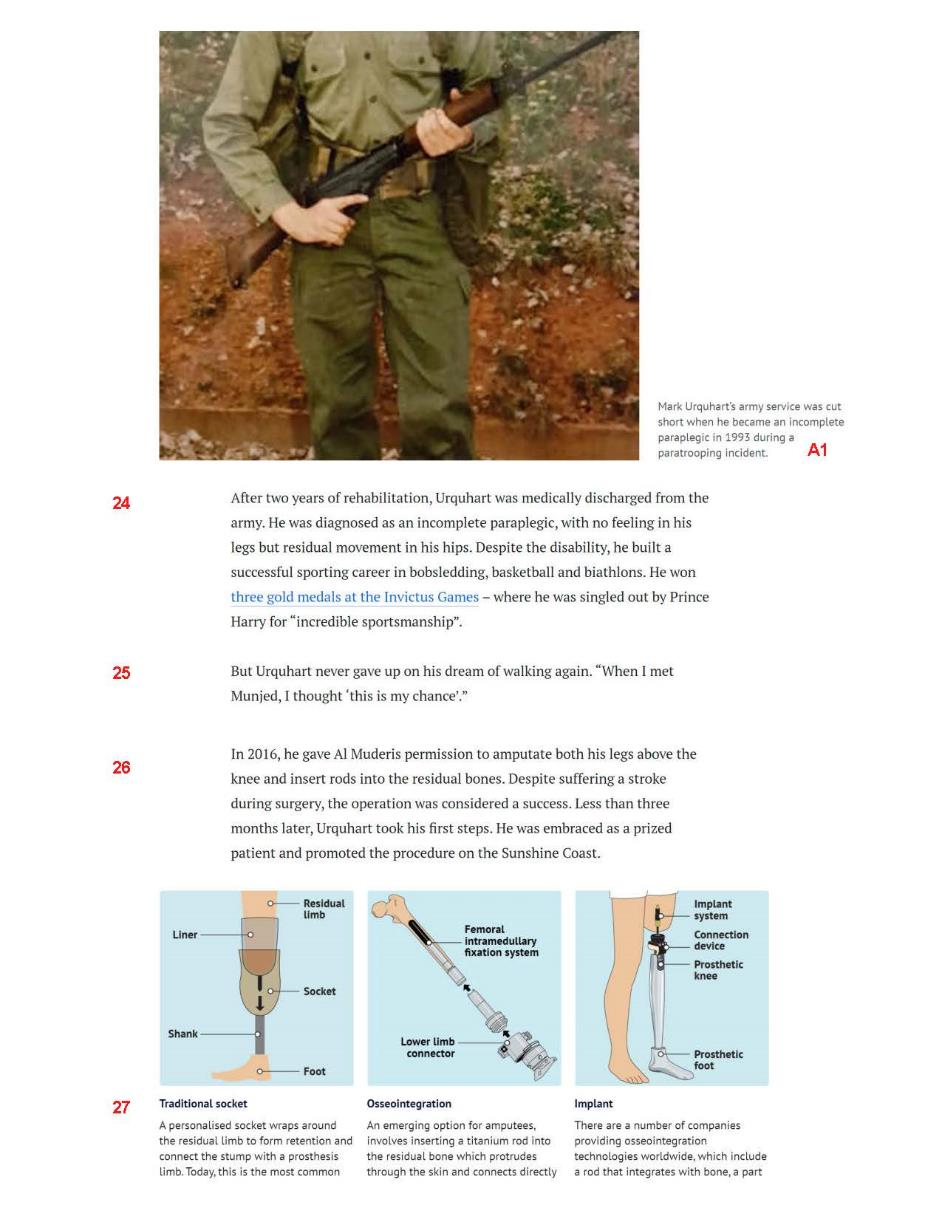
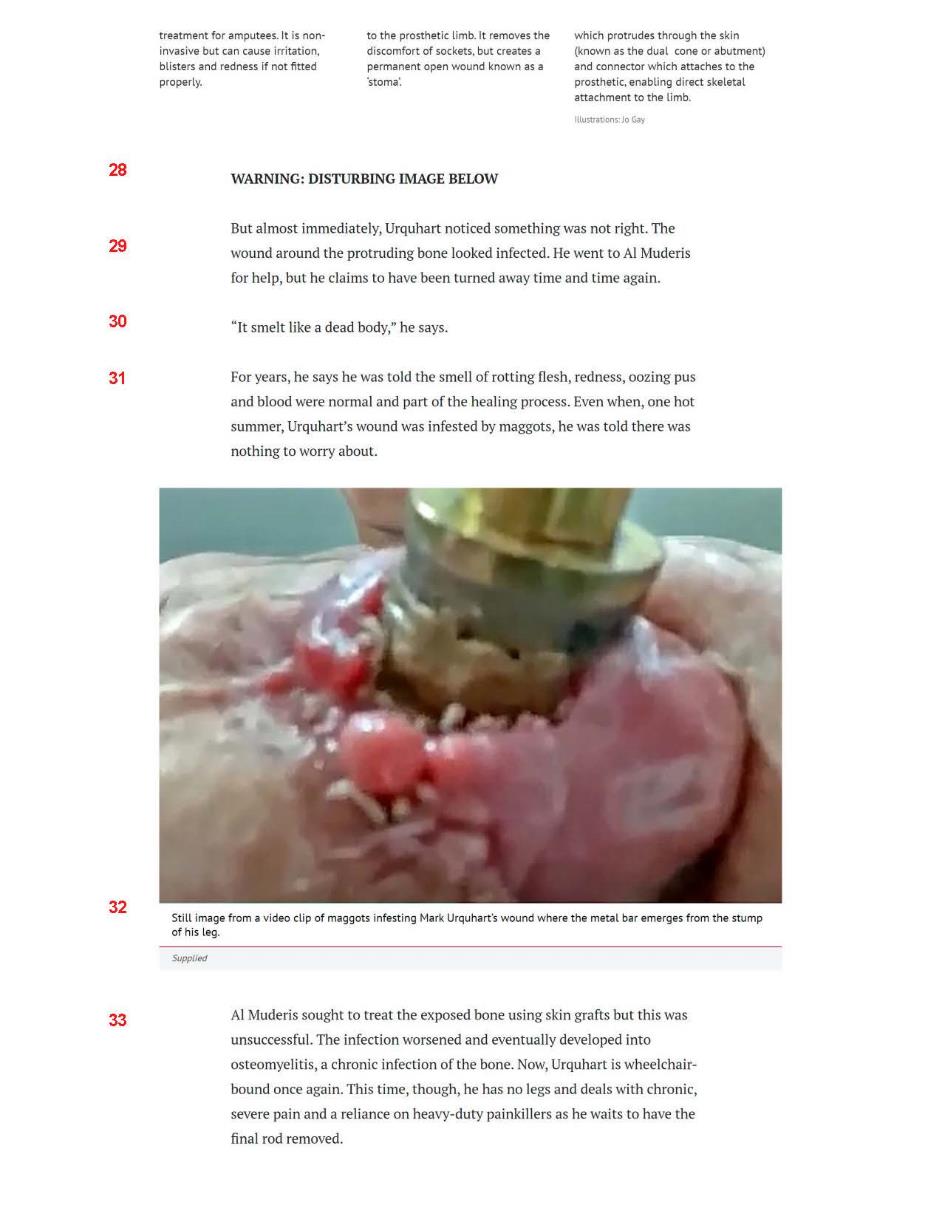
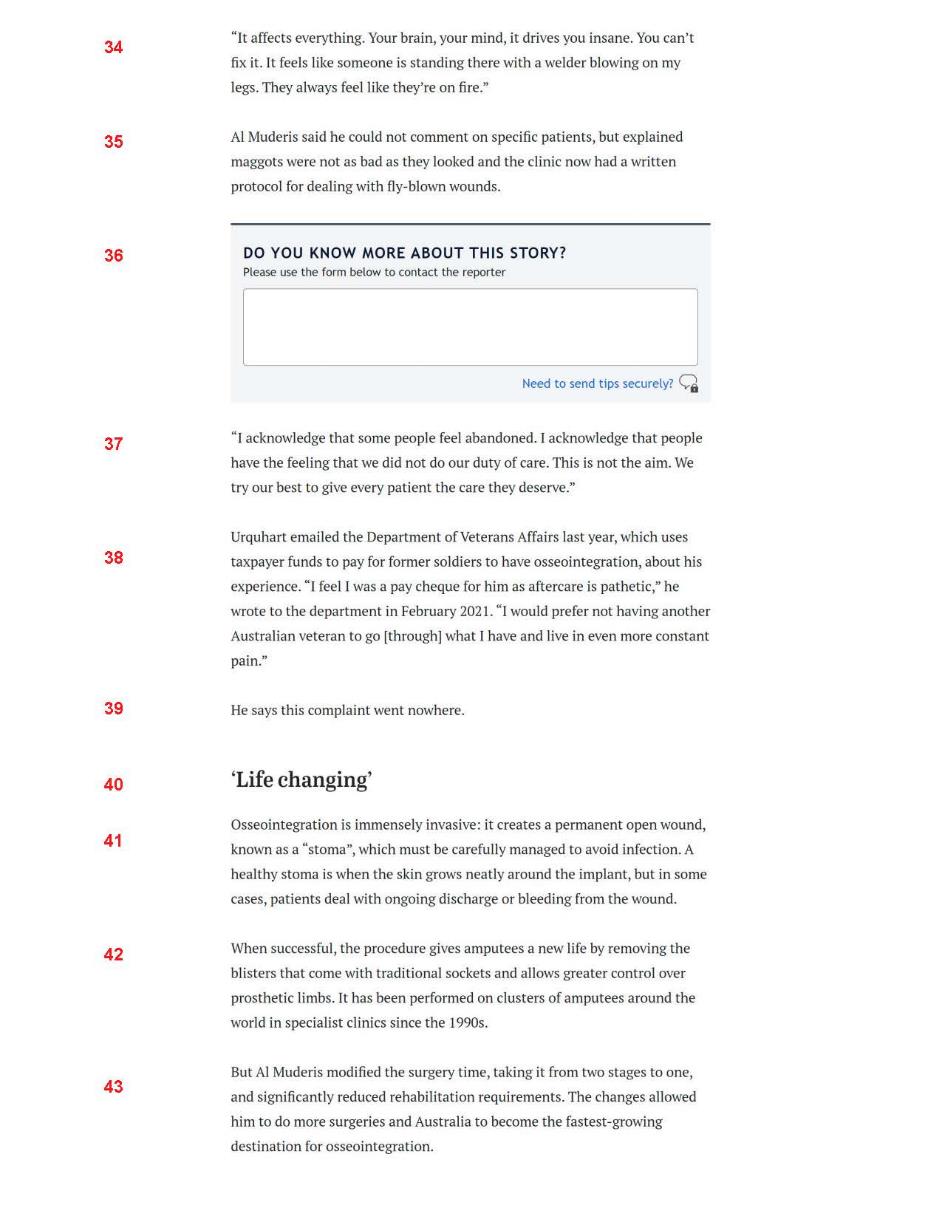
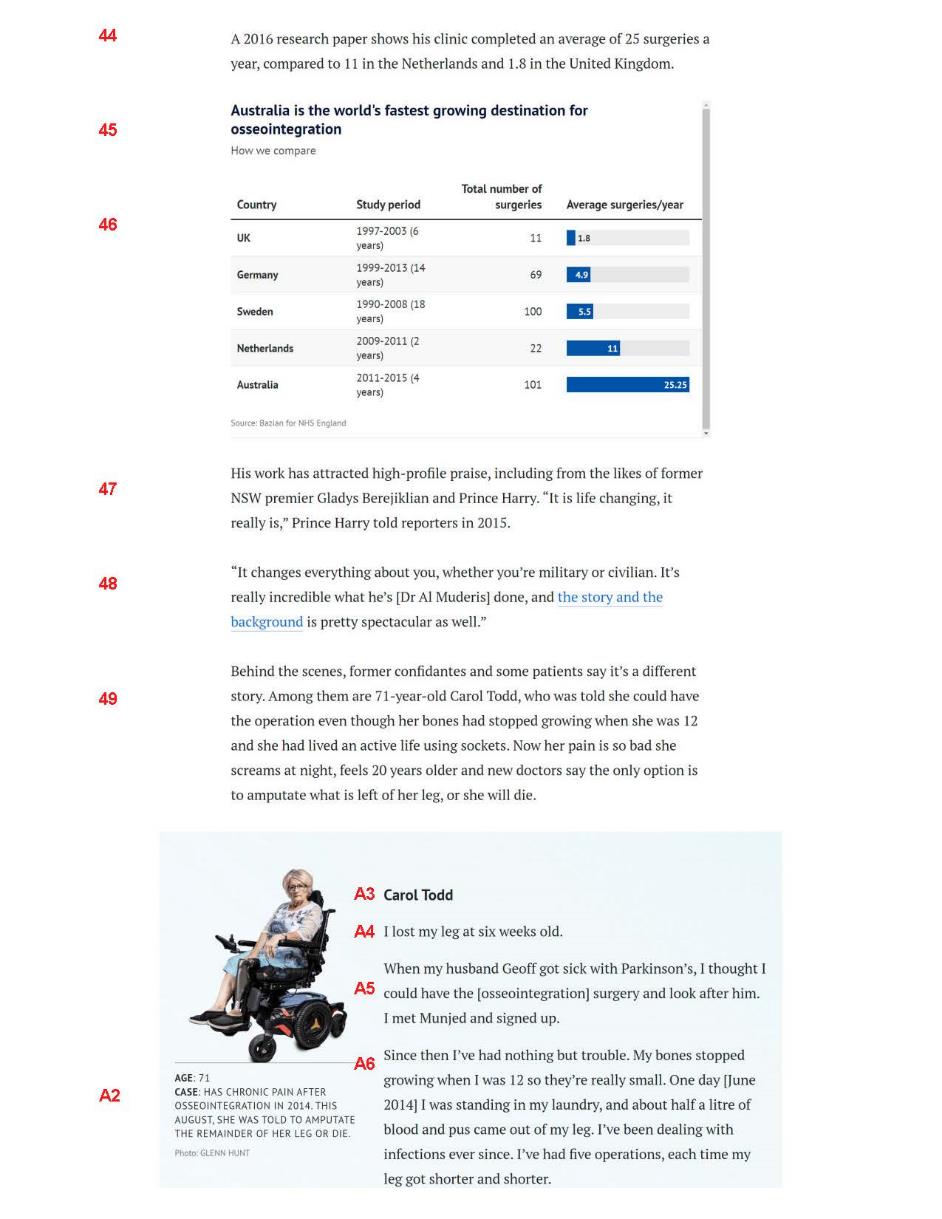
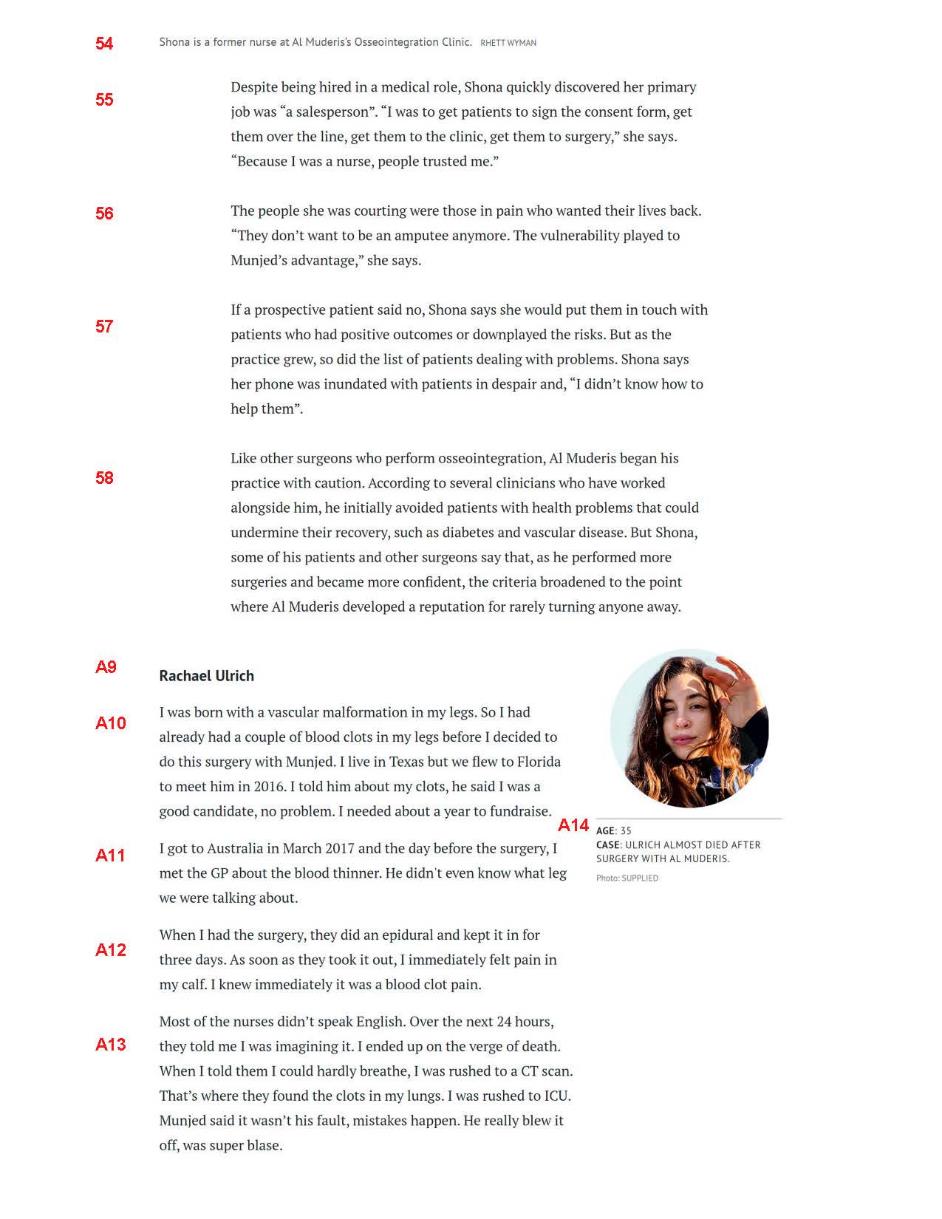
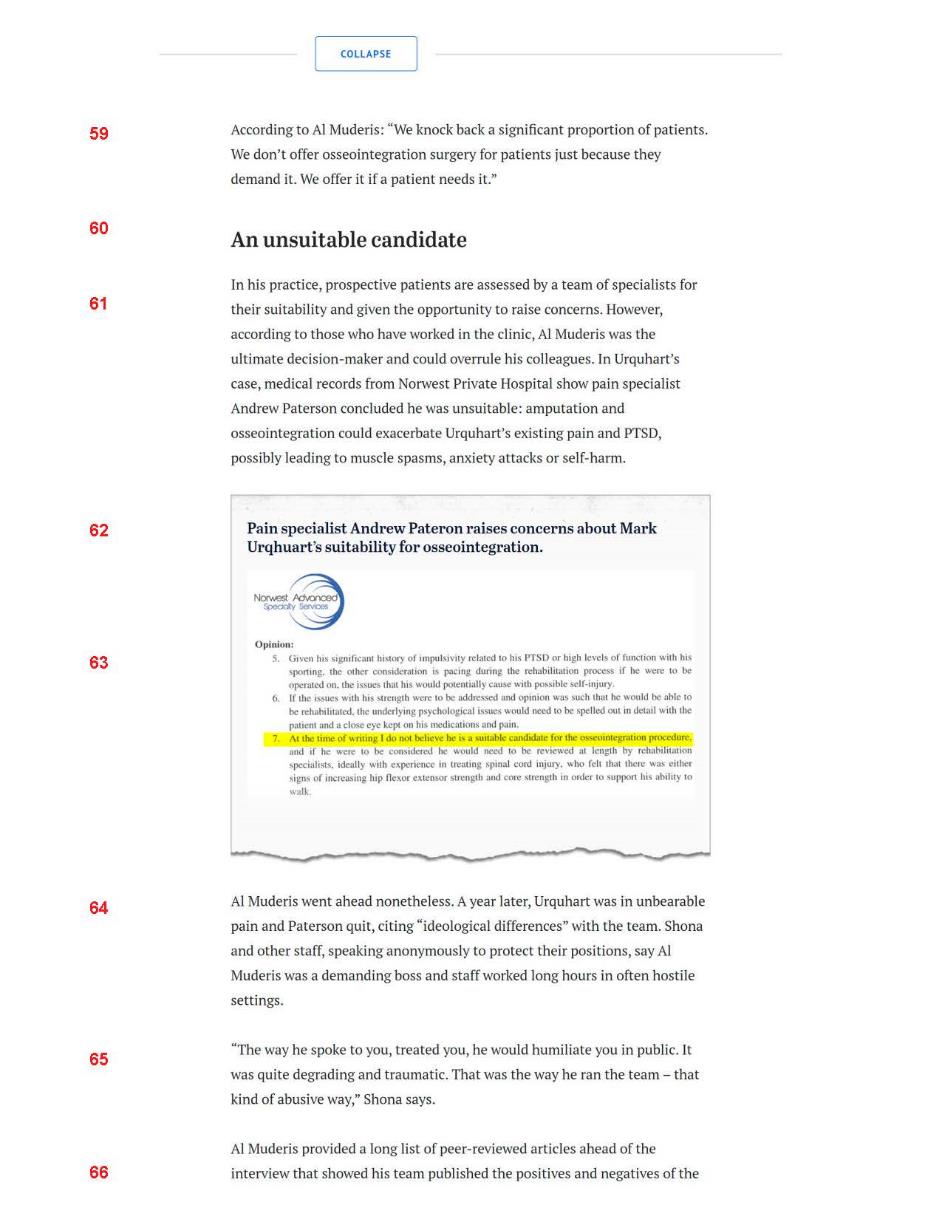
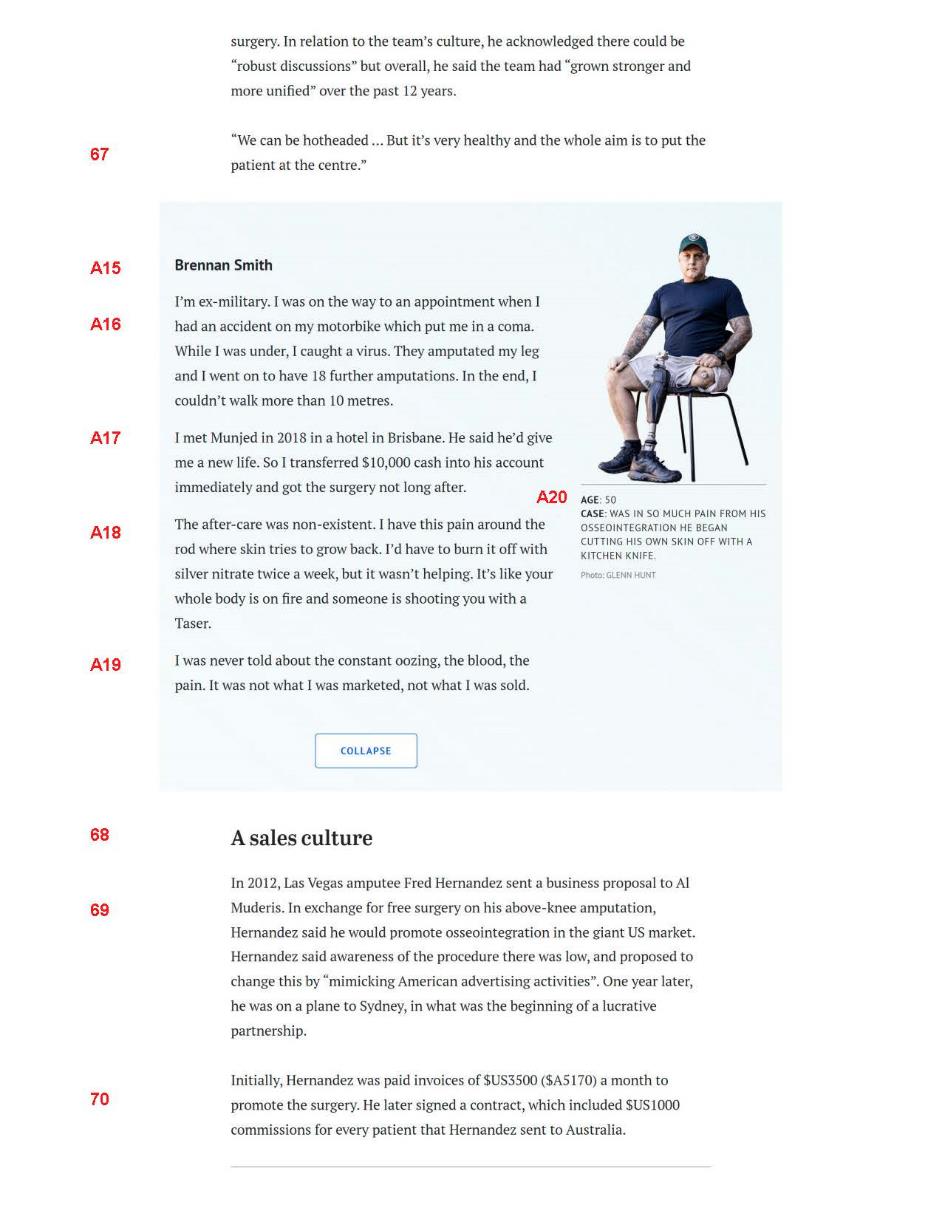
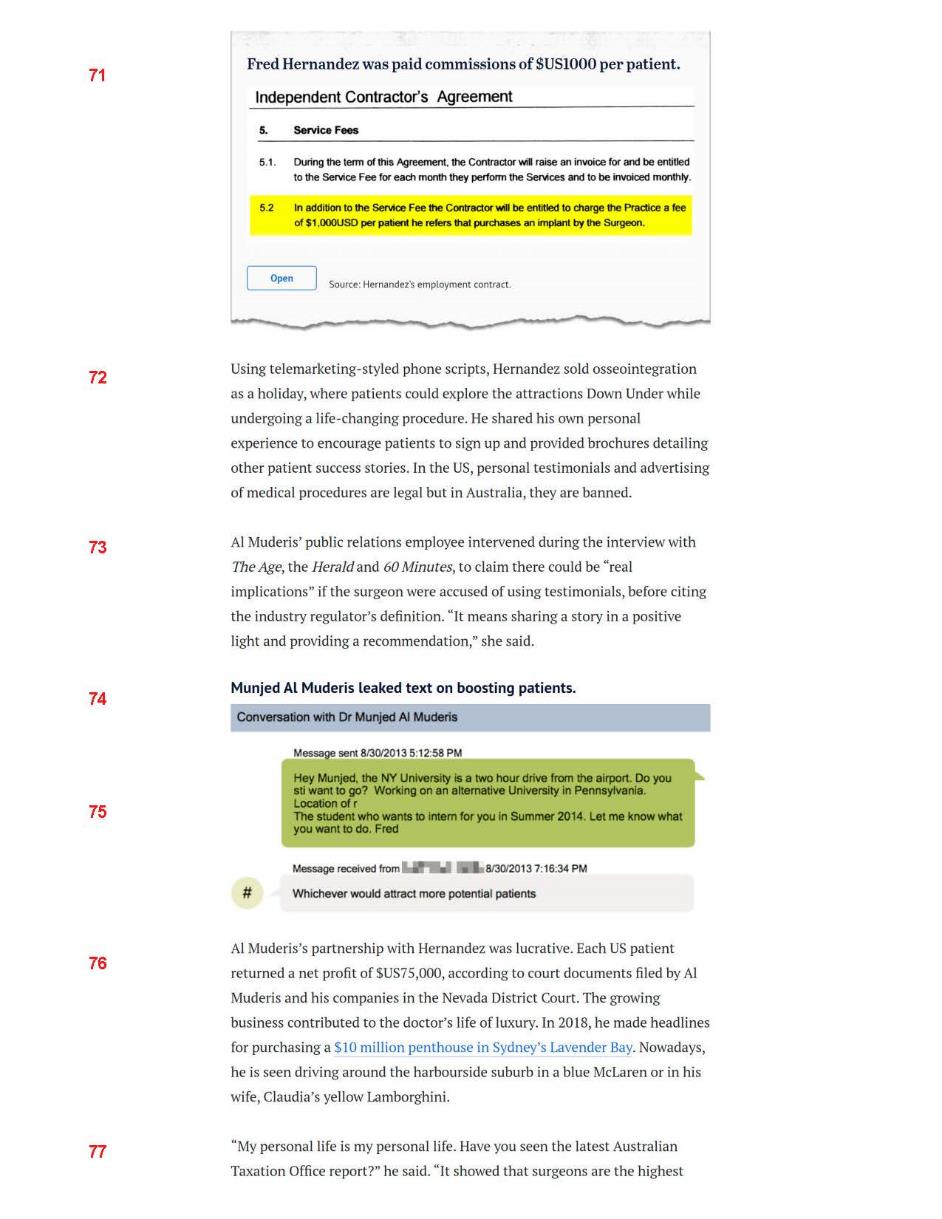
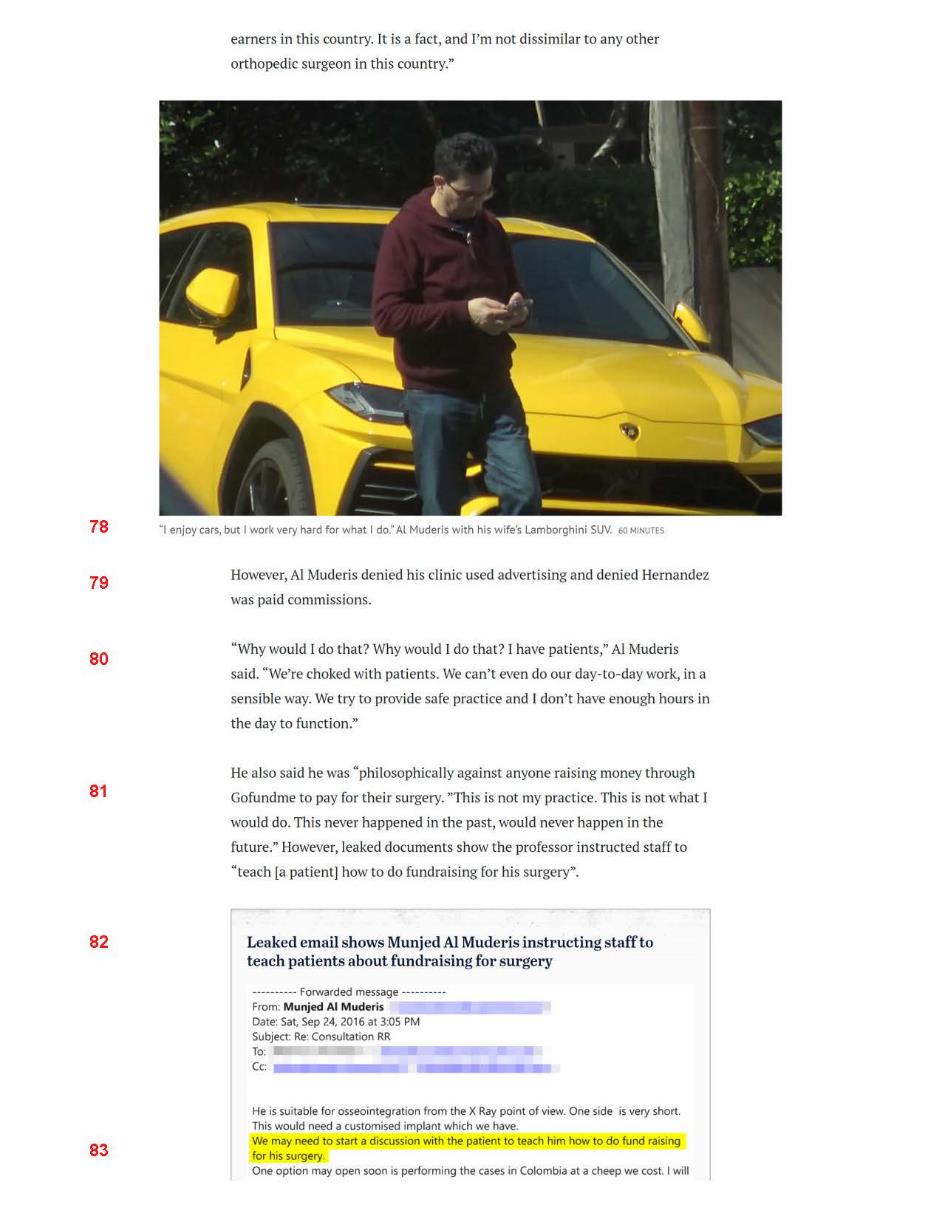
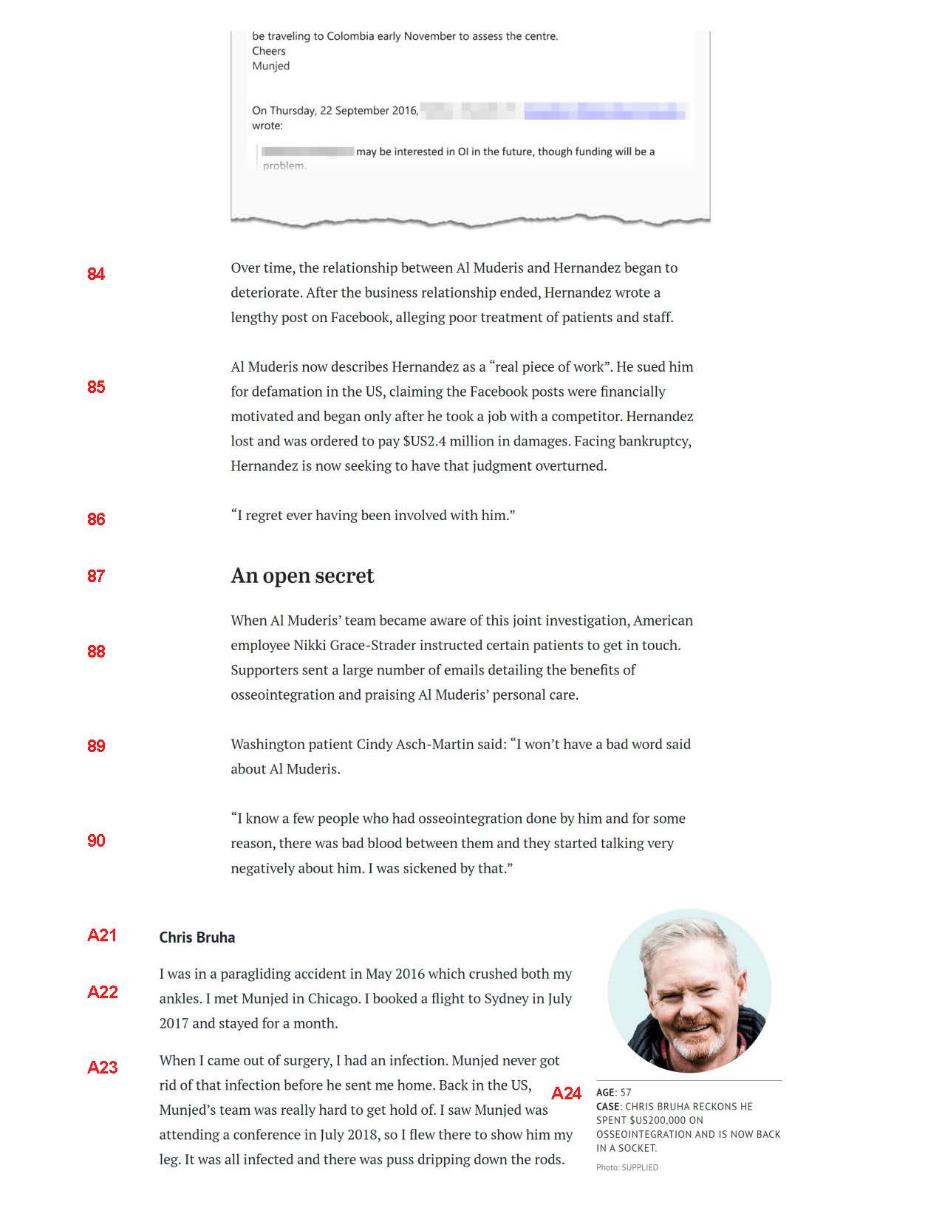
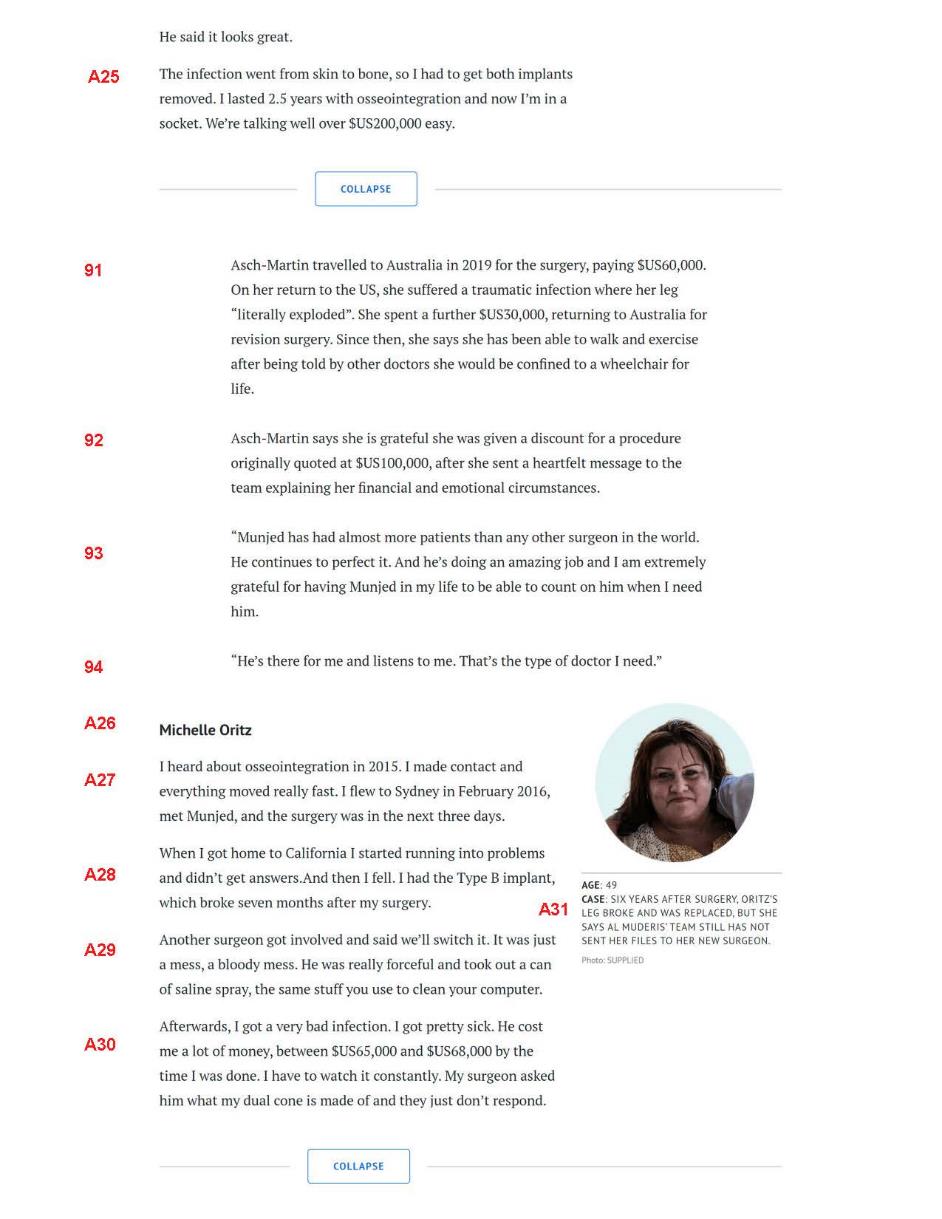
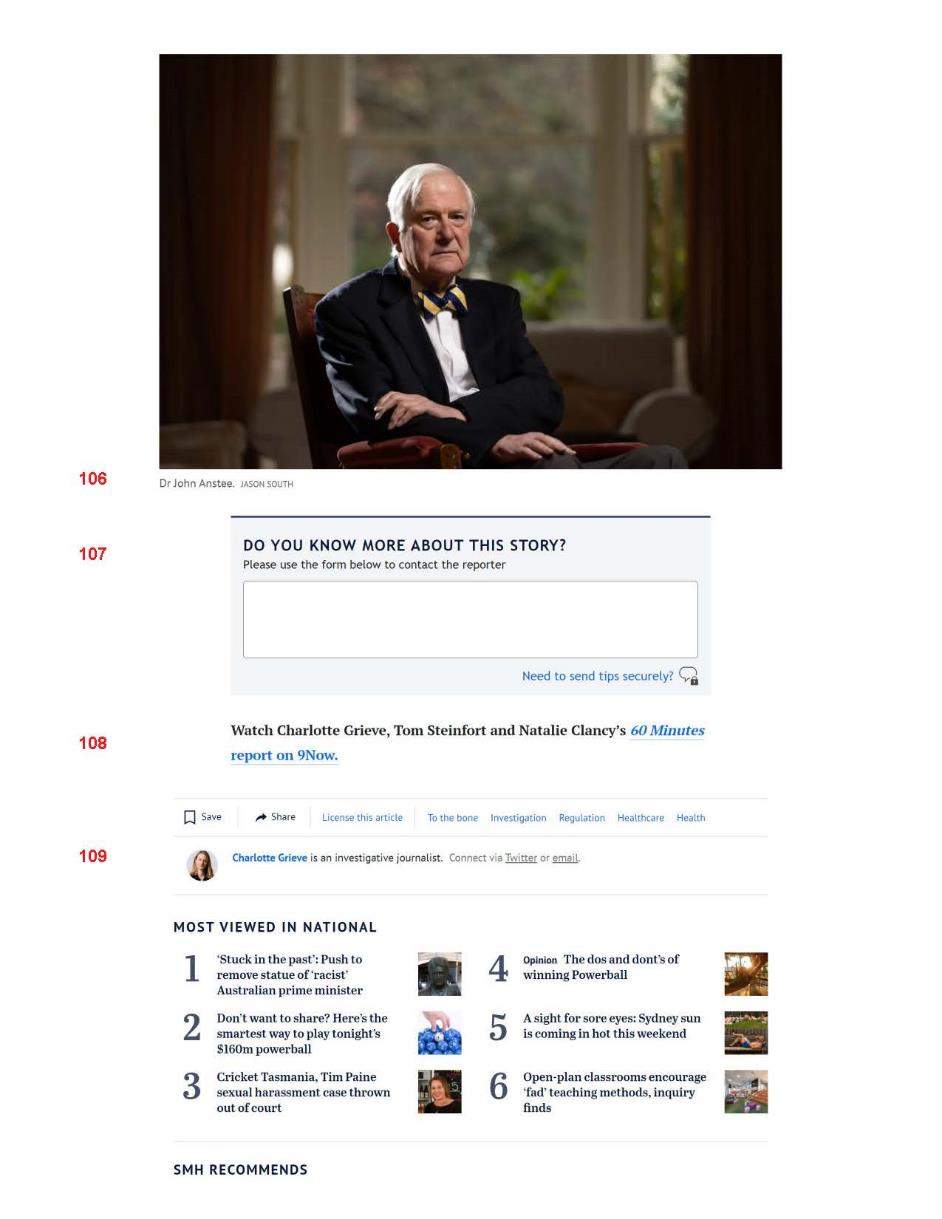
Annexure E — Age Article


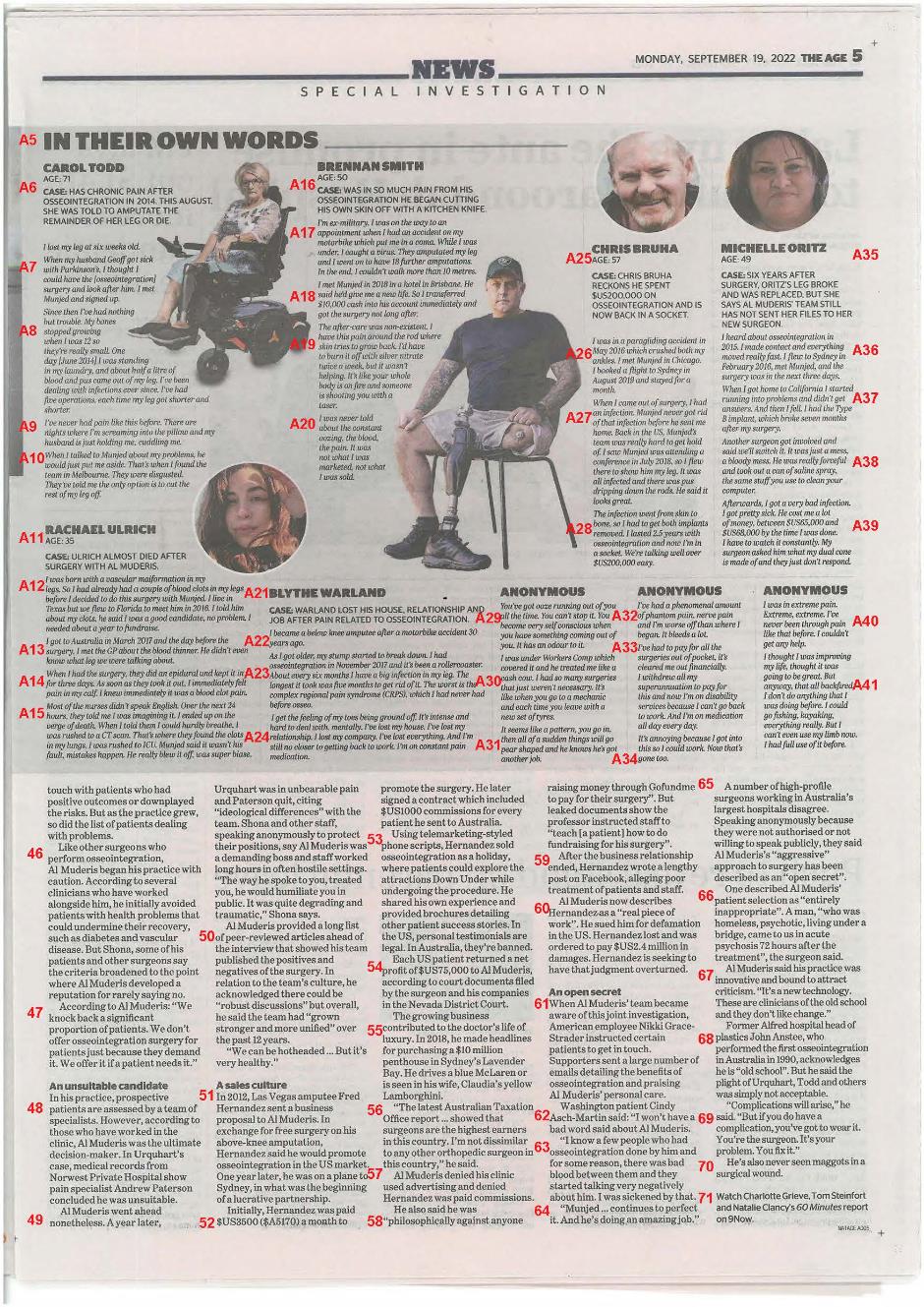
Annexure F — Age Online Article

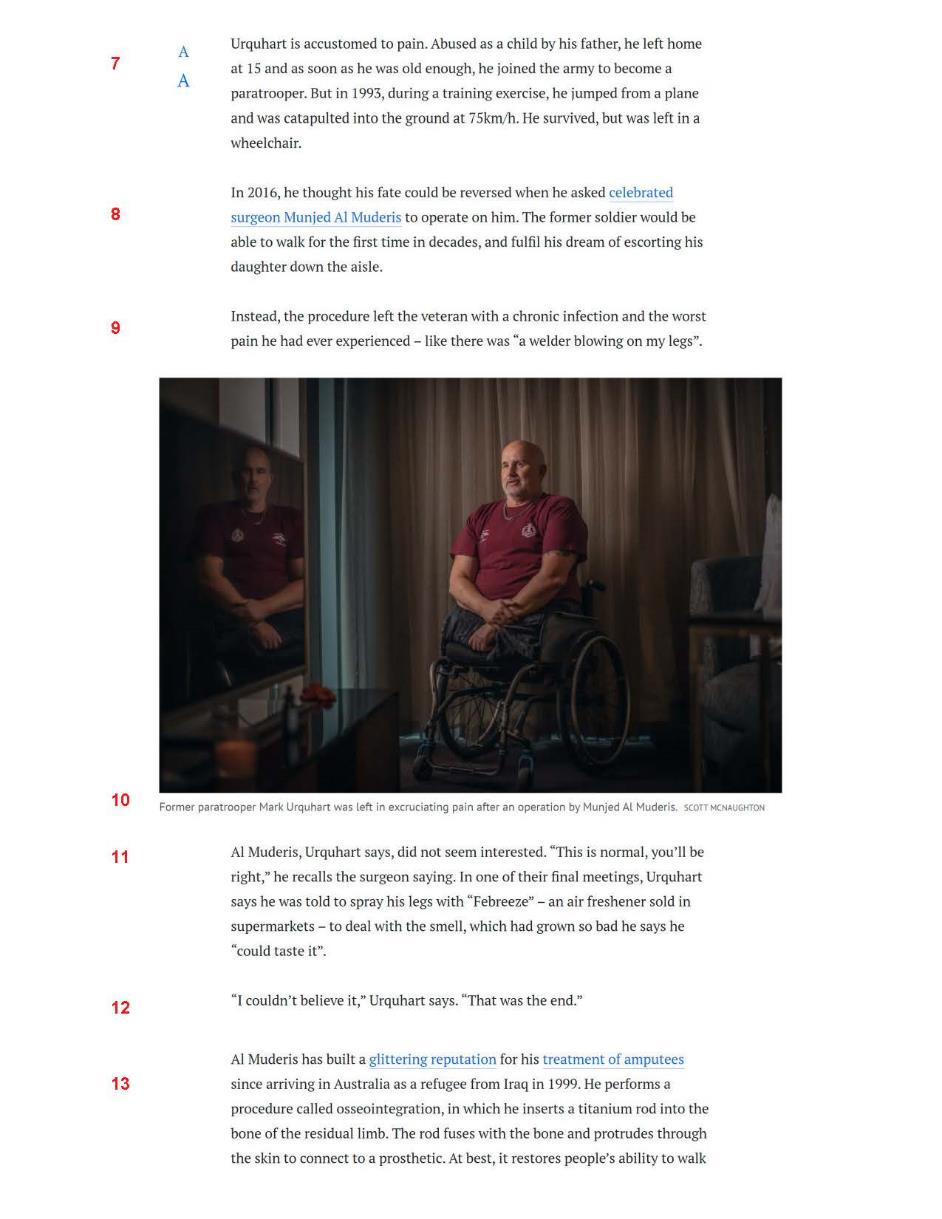
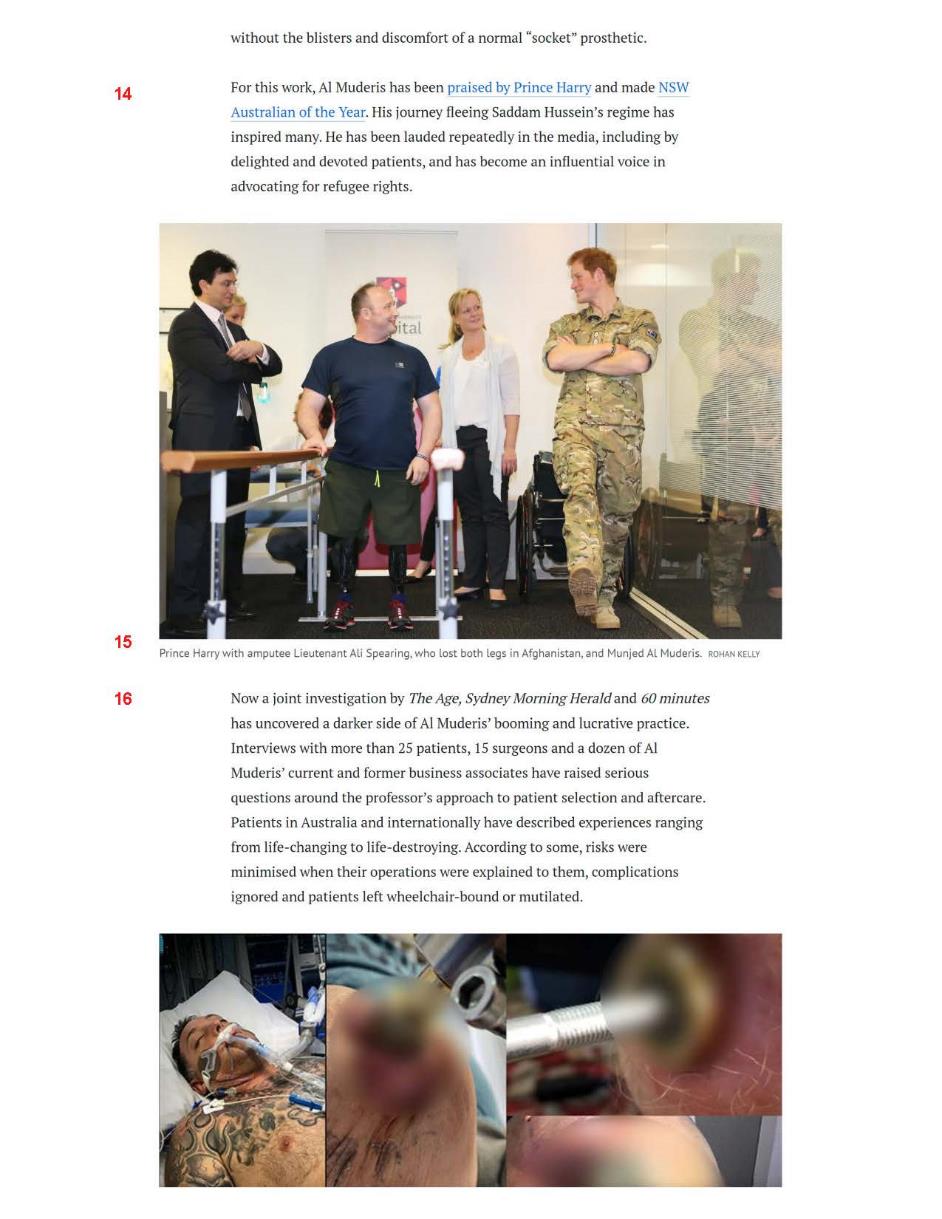
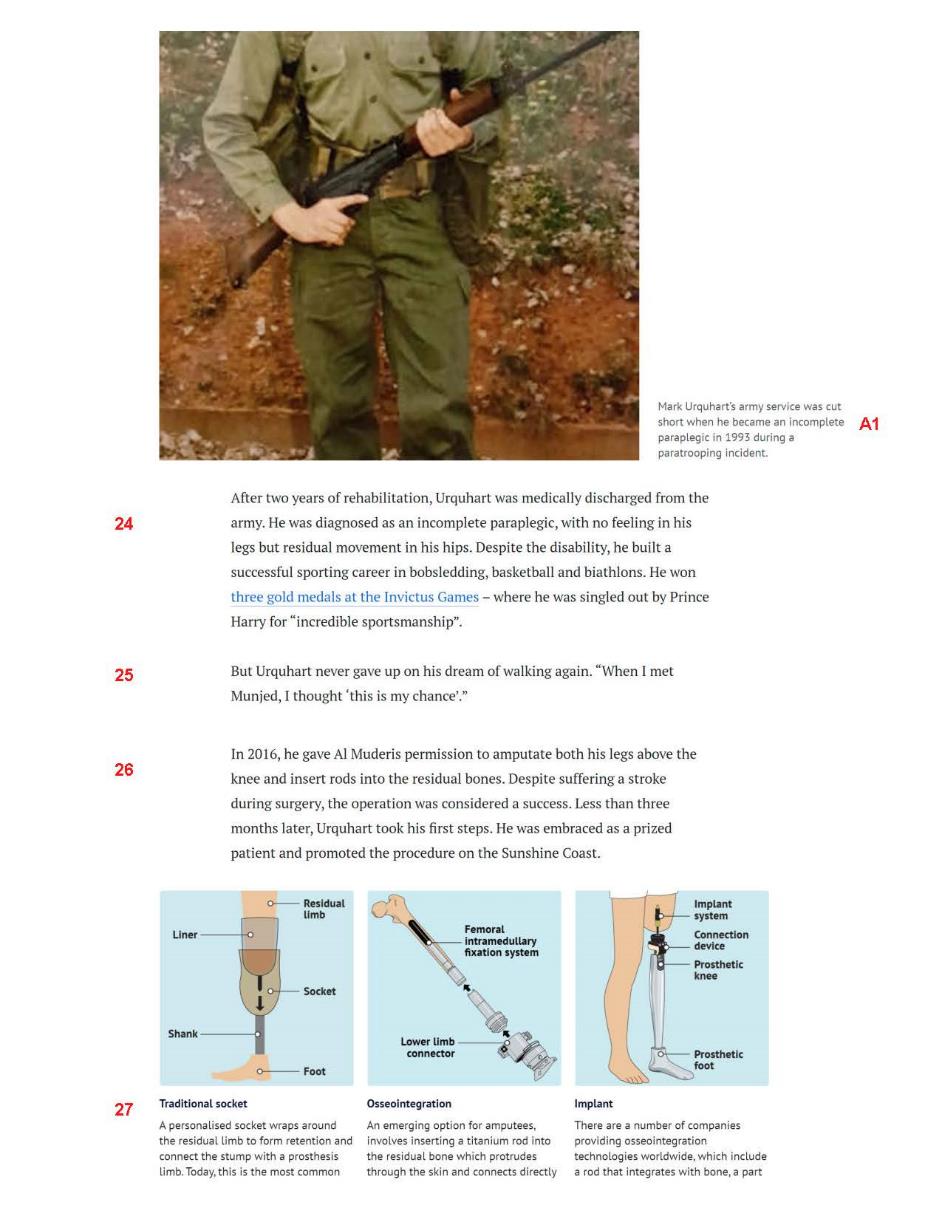
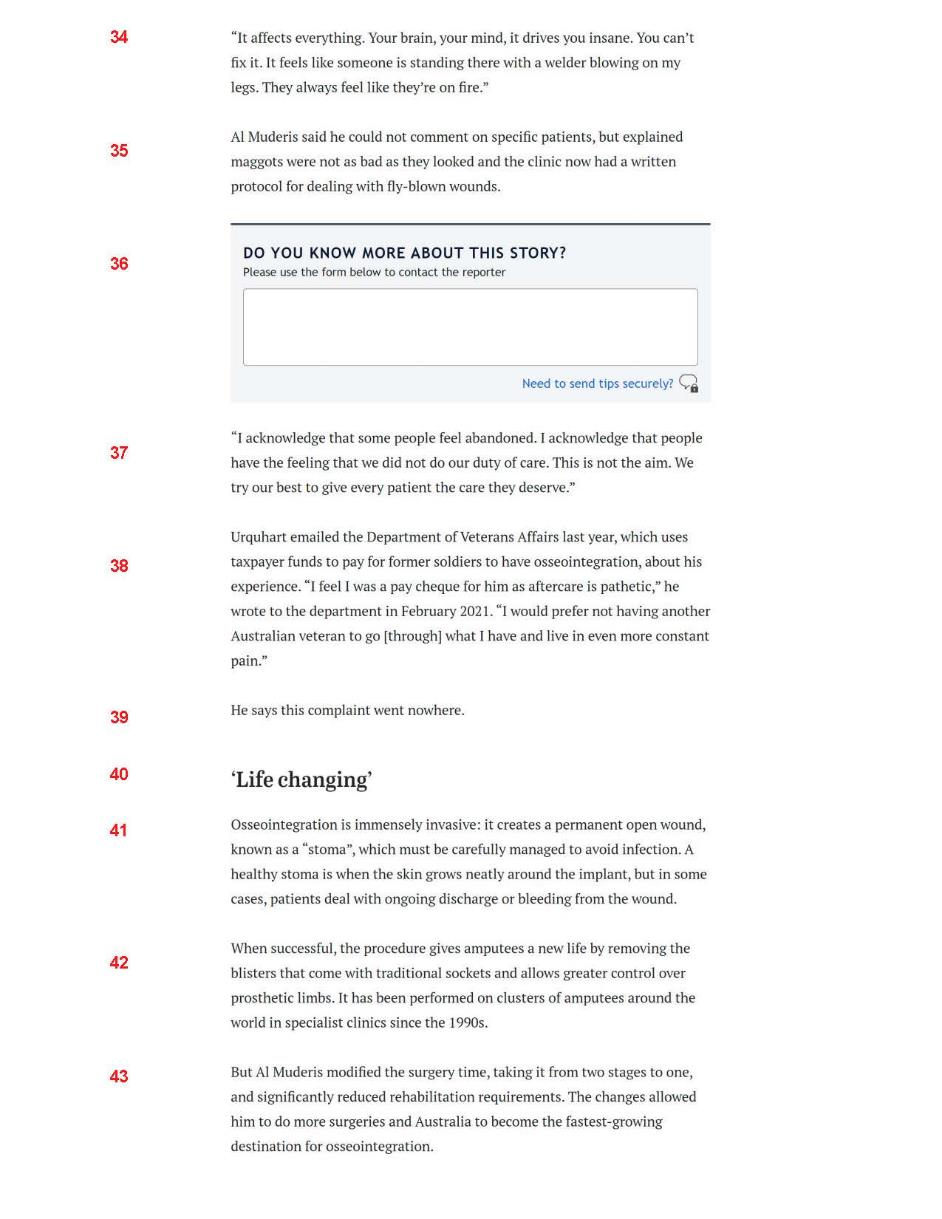
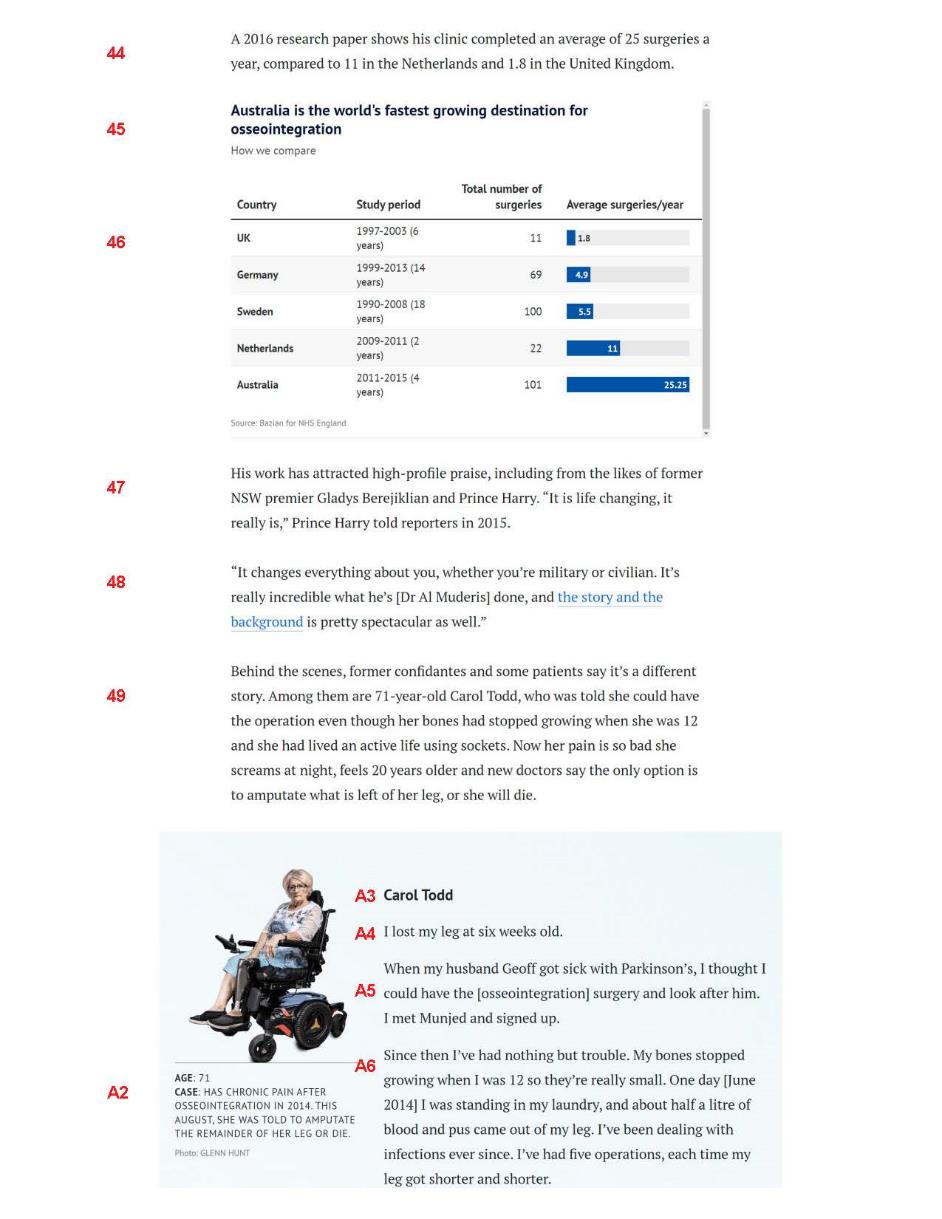
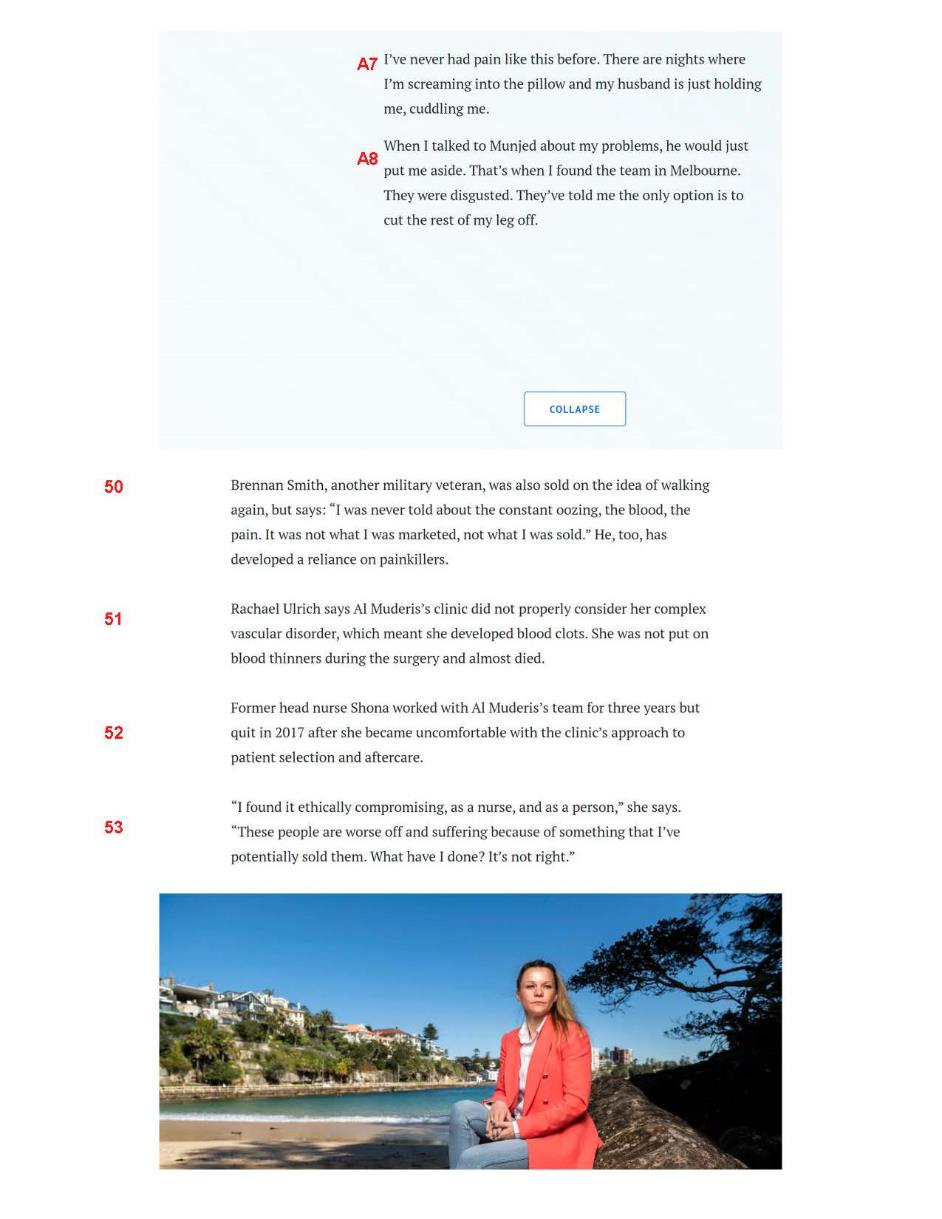
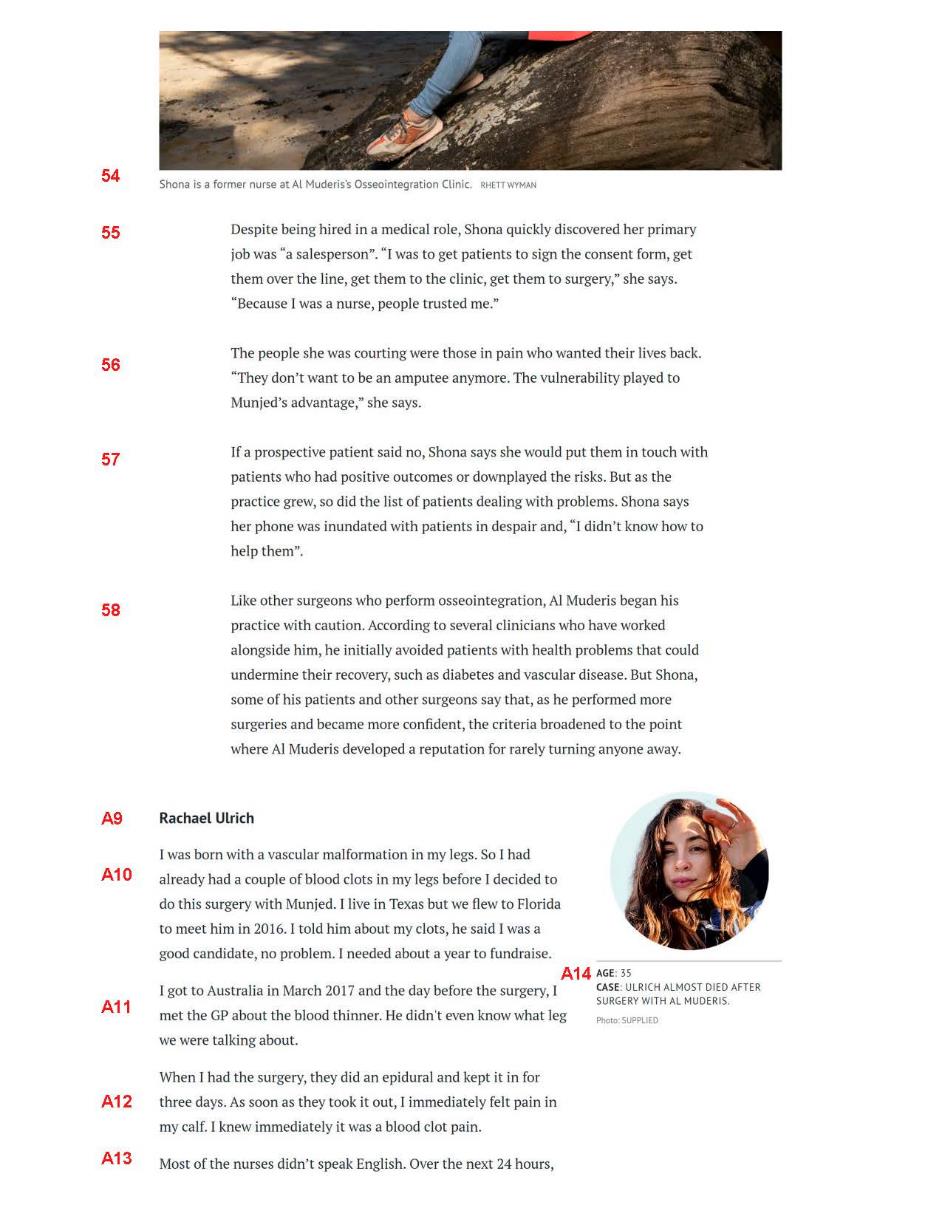
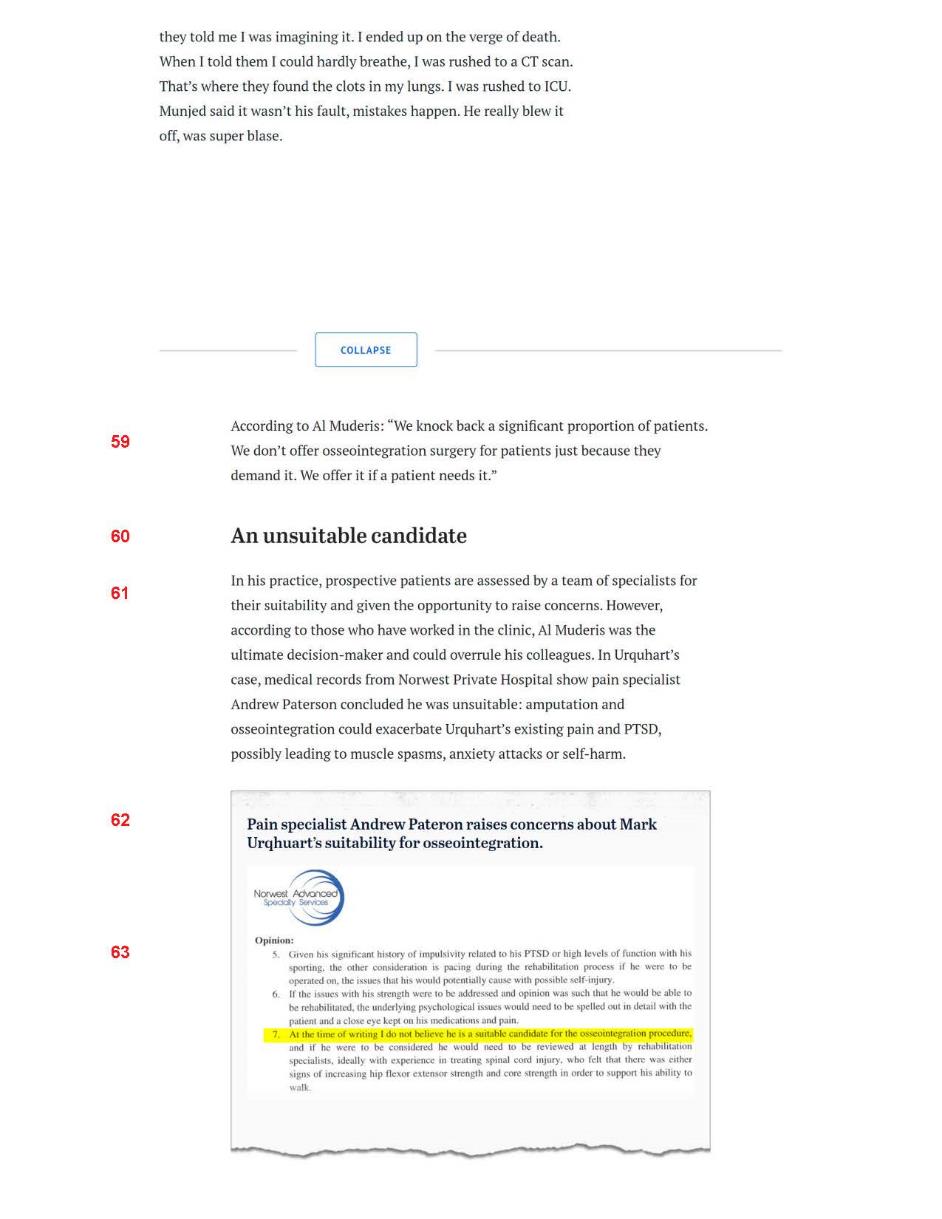
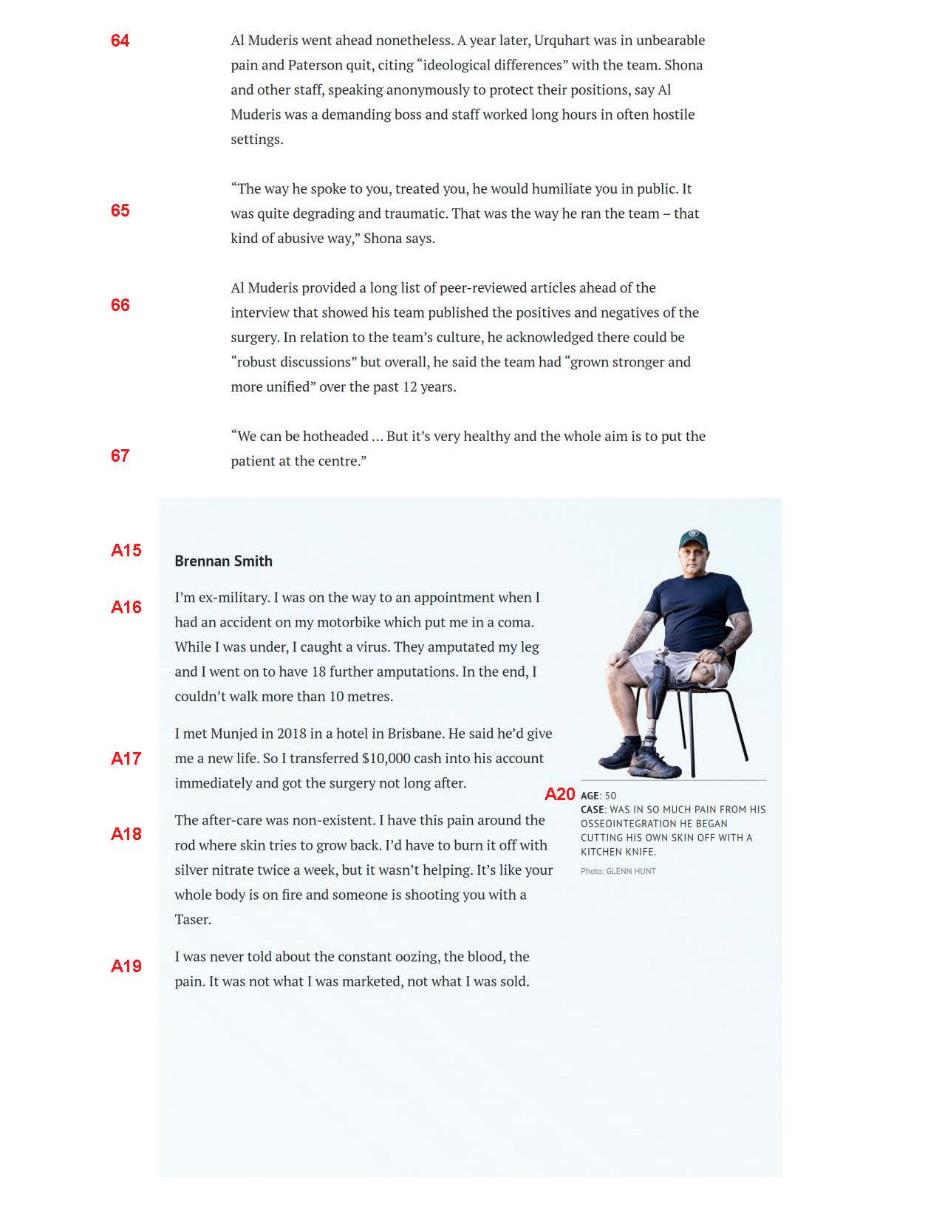
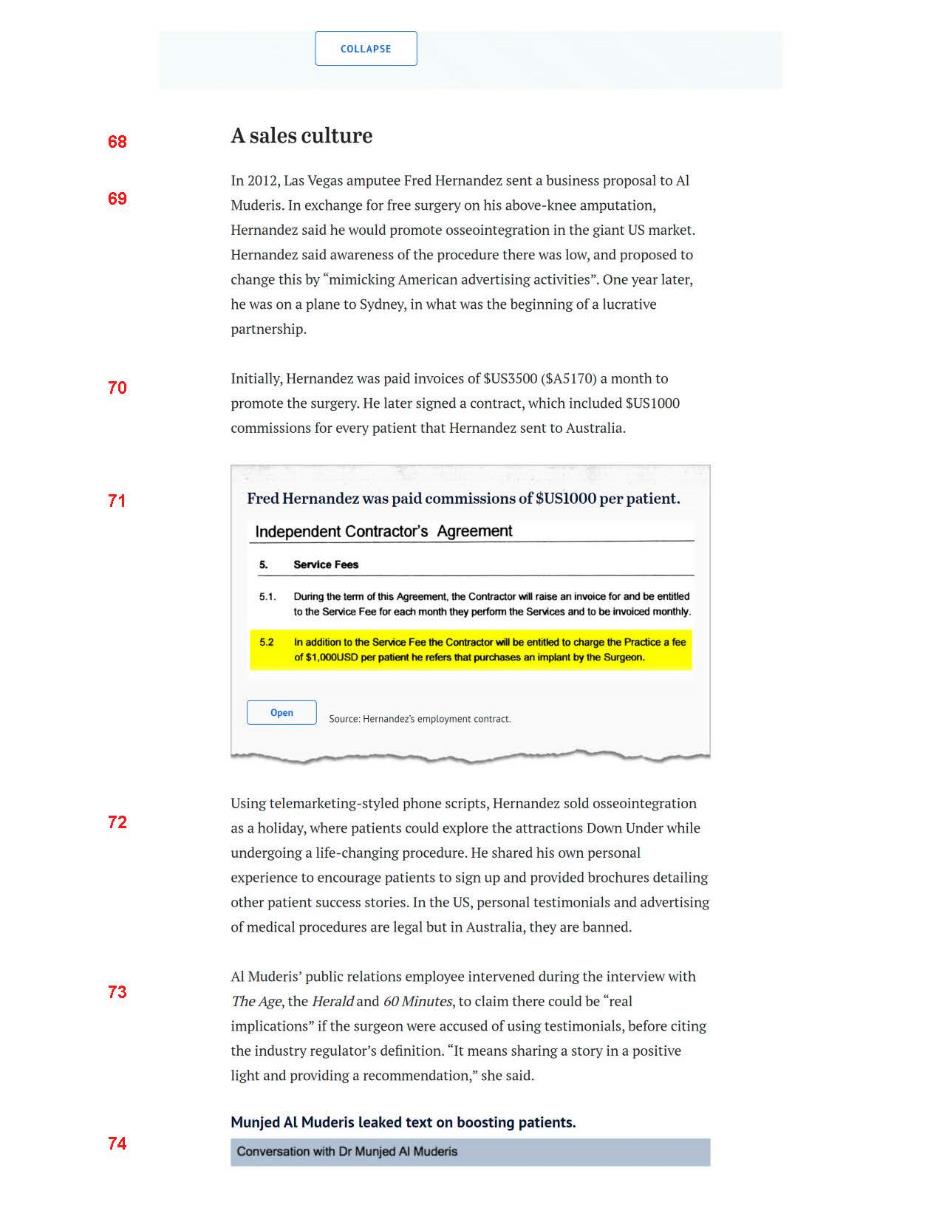
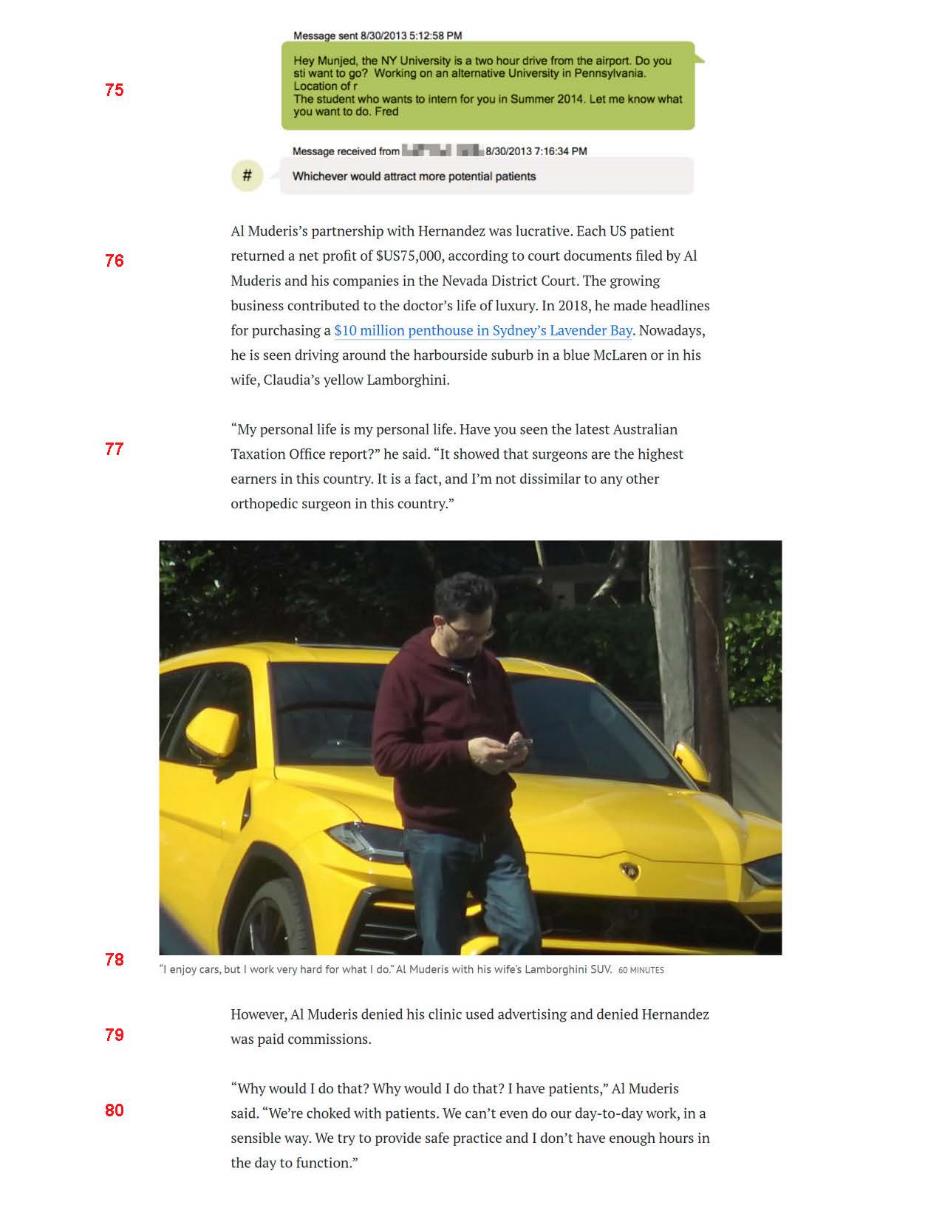
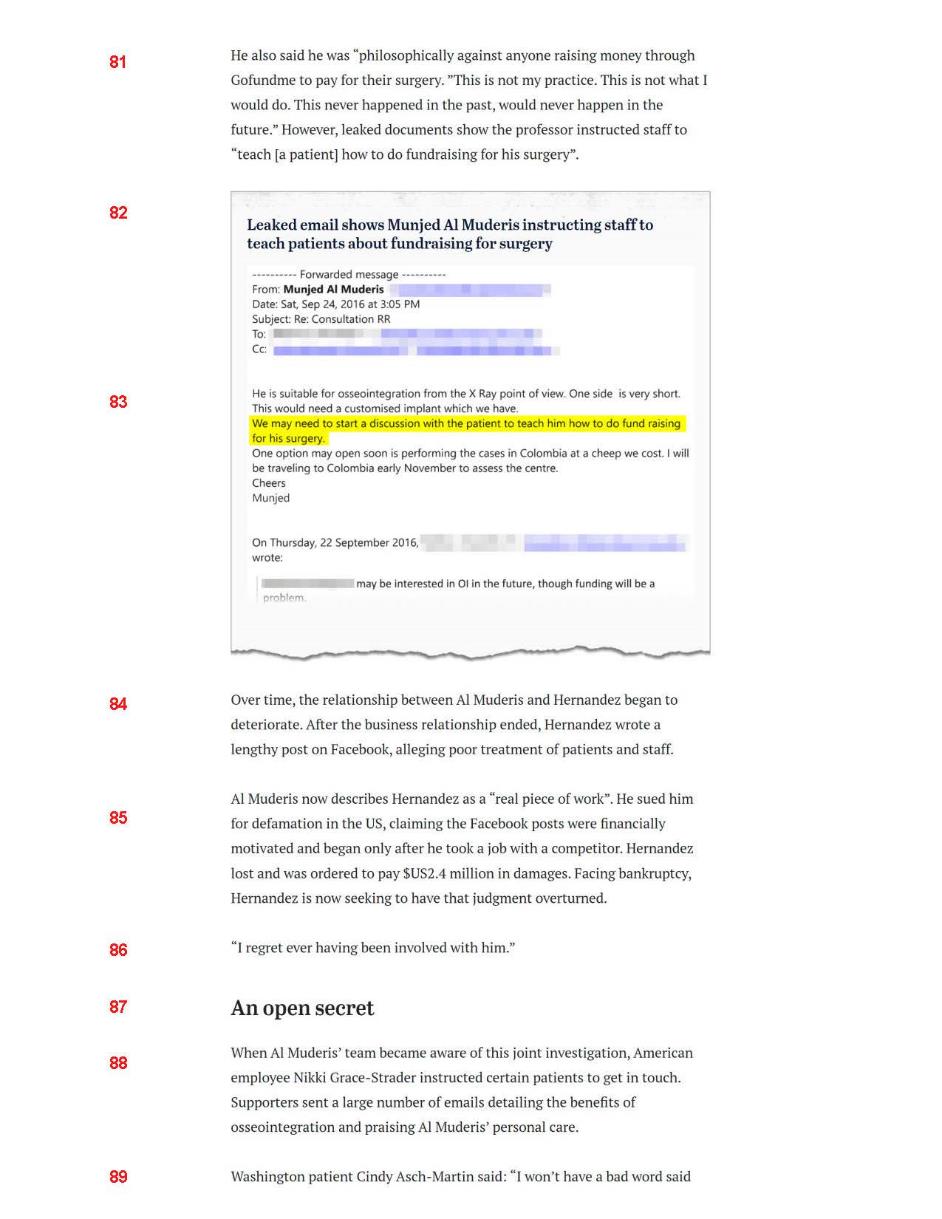
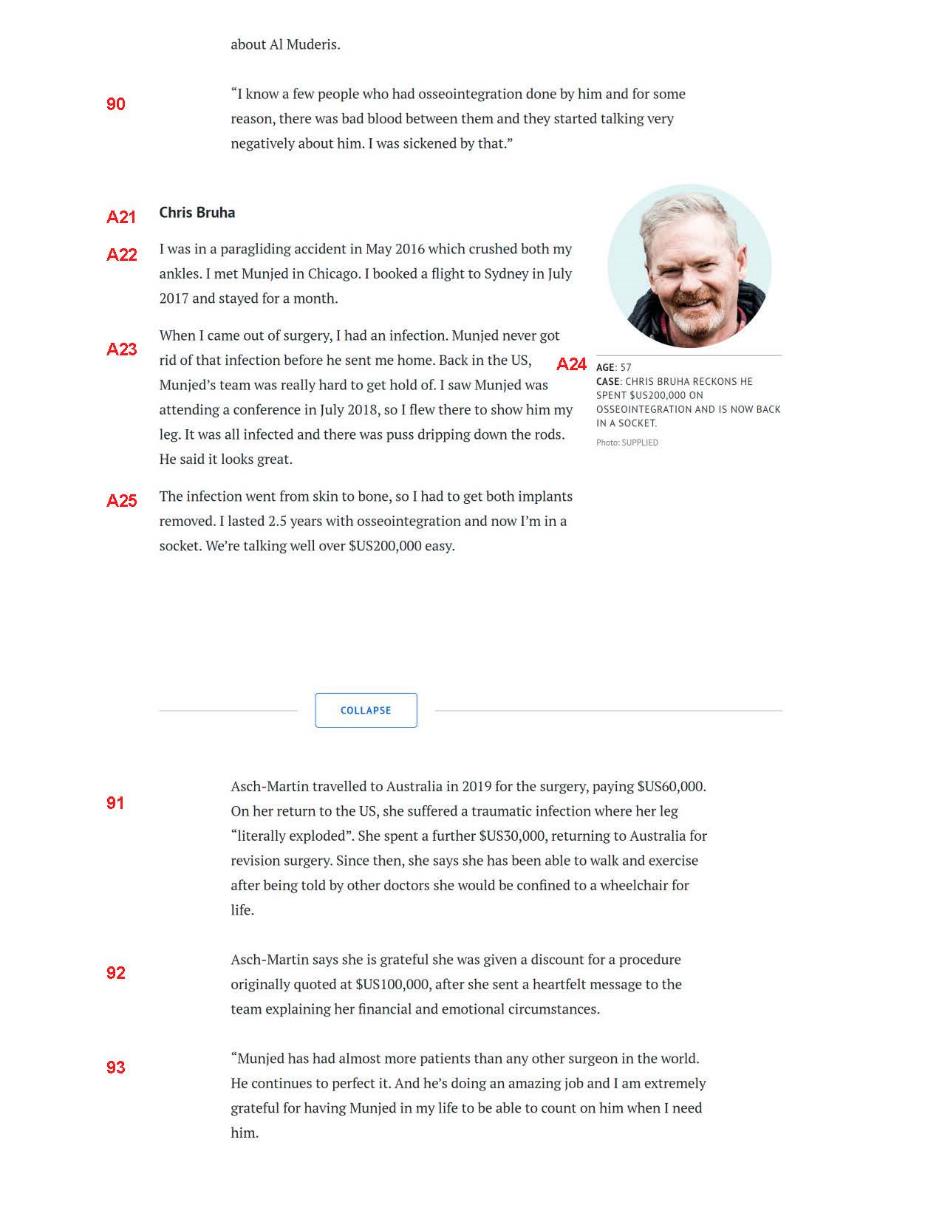
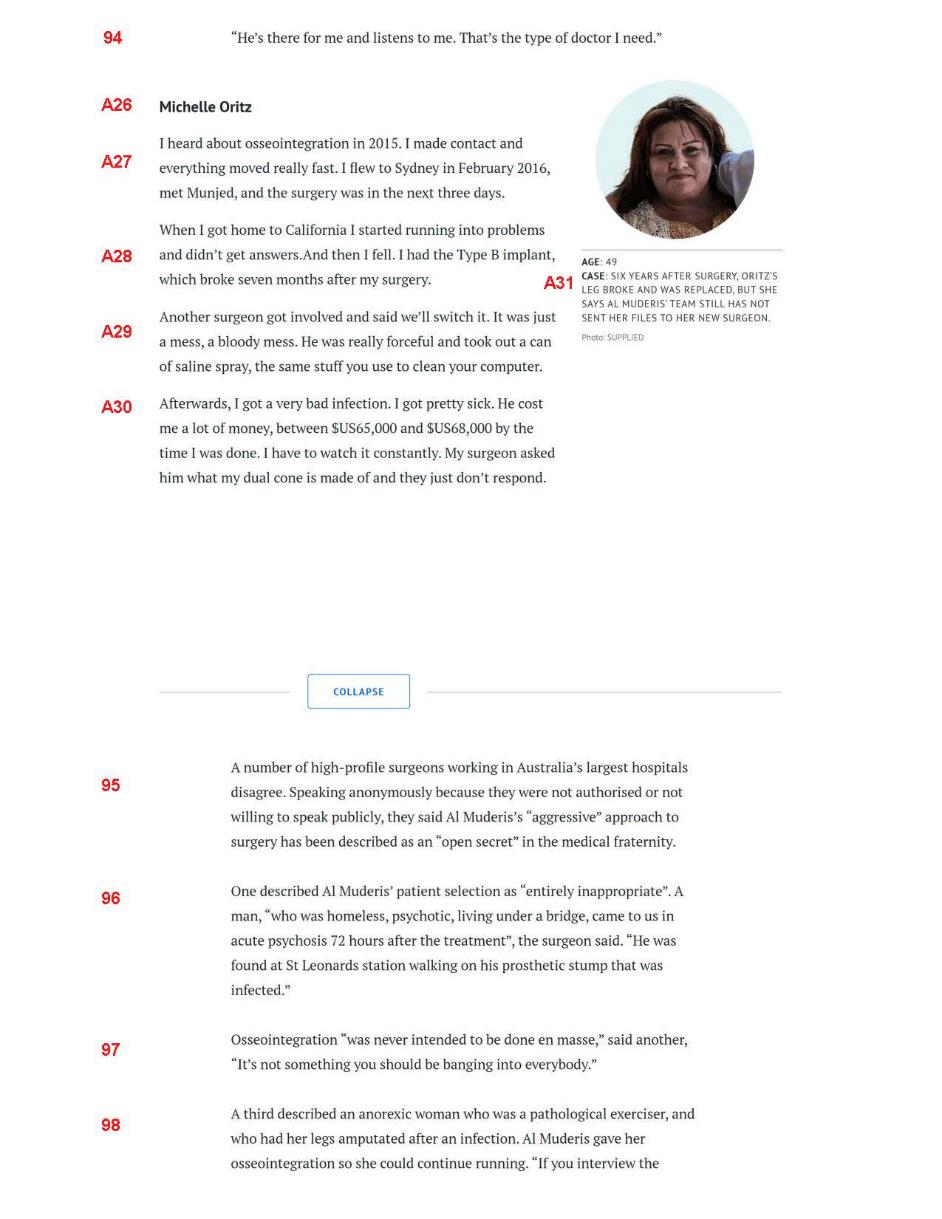
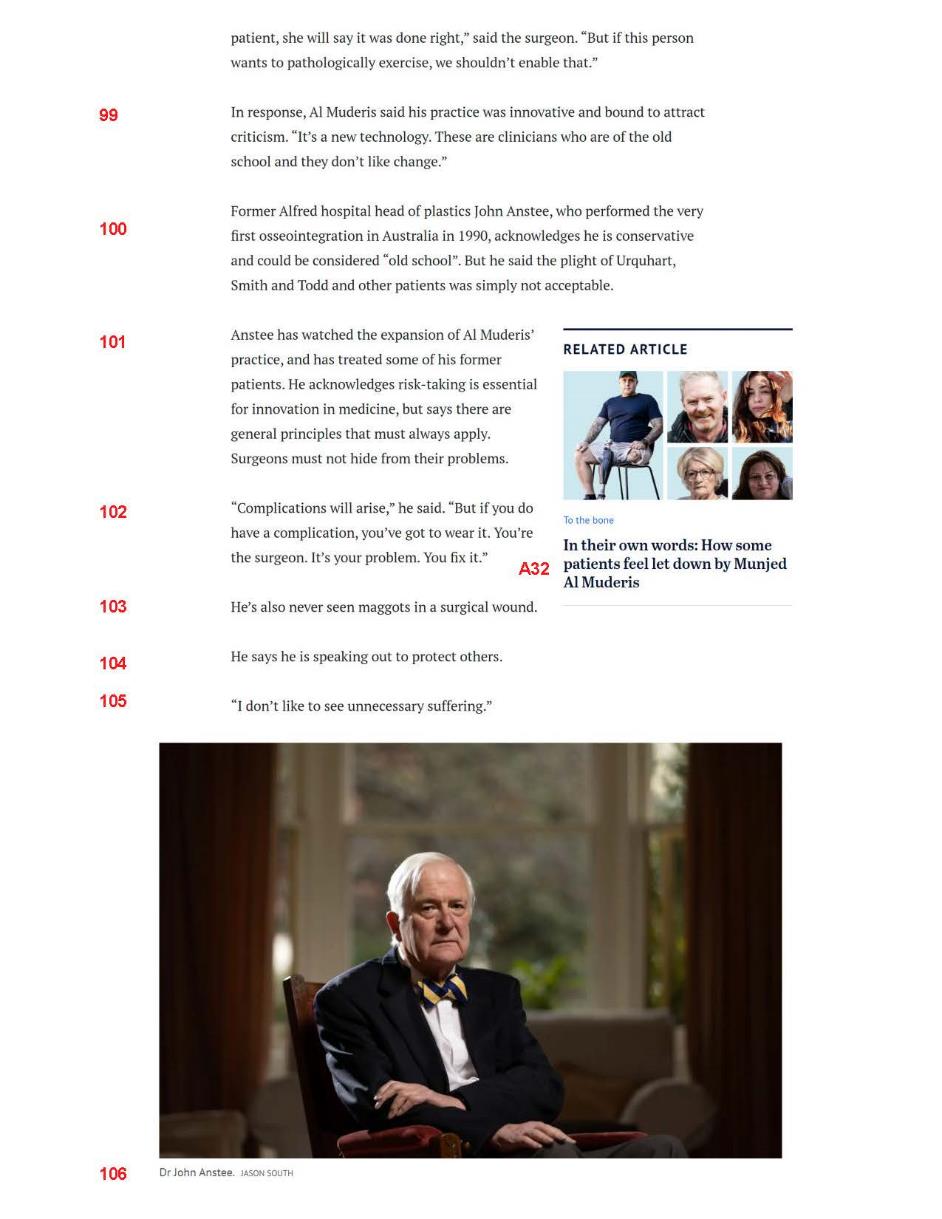
Annexure G — Grieve Video transcript
Annexure H — Pleaded Imputations
The Sneak Peak |
10.1. Al Muderis has negligently operated on his patients causing them to turn against him; 10.2. Al Muderis has deliberately misled his patients about his surgical abilities, advertising first class service but delivering sub-standard care; 10.3. Al Muderis has negligently conducted surgery on a patient causing him to cut off his own flesh; 10.4. Al Muderis has negligently conducted surgery on a patient causing him ongoing excruciating pain; 10.5. Al Muderis has negligently conducted surgery on his patients resulting in maggots in their surgical wounds; and 10.6. Al Muderis’s negligence in performing surgery that resulted in maggots in a surgical wound was unprecedented. |
The Broadcast |
13.1. Al Muderis falsely portrays himself as a devoted doctor when in fact he does not take adequate care of his patients; 13.2. Al Muderis negligently performed surgery on Mark leaving him with out of control infections and maggots infesting his open wound; 13.3. Al Muderis abandoned his patient Brennan Smith after surgery causing him to take to his own leg with a kitchen knife; 13.4. Al Muderis prioritises money over his patients’ care; 13.5. Al Muderis made false promises to his patient Mark about the prospective success of his surgery when in fact the surgery caused Mark’s condition to worsen; 13.6. Al Muderis negligently performed surgery on Mark causing horrible complications namely excruciating pain and disturbing infections that gave off a repulsive odour; 13.7. Al Muderis made fun of his patient Mark’s concerns about an infected wound after surgery instead of taking them seriously; 13.8. Al Muderis callously ignored a video from his patient Mark which showed maggots breeding in his leg after surgery; 13.9. Al Muderis made false promises to Brennan Smith about the prospective success of his surgery and failed to properly warn him about possible complications; 13.10. Al Muderis falsely led his patient Brennan Smith to believe that the surgery he was going to have was always successful when the reality was it was a disaster; 13.11. Al Muderis ignored his patient Brennan’s hypergranulation causing him to cut the growth off himself with a kitchen knife; 13.12. Al Muderis breached his duty of care as a doctor to his patient Brennan in relation to his post-operative care; 13.13. Al Muderis cares more about his reputation, status, profits and the media than properly caring for his patients; 13.14. Al Muderis runs his surgical practice as a numbers game, focussing on getting large numbers of patients to have the surgeries and then neglecting their care afterwards; 13.15. Al Muderis abandons patients in Iraq and Cambodia after surgery leaving them to deal with traumas and infections; 13.16. Al Muderis makes false promises to patients in Iraq and Cambodia that he fails to deliver on; 13.17. Al Muderis preyed on patients who were vulnerable both physically and mentally in order to exploit them for his own financial gain; 13.18. Al Muderis exploited vulnerable patients by performing surgeries on them that they could not afford; 13.19. Al Muderis’s conduct of his business as a numbers game, exploiting vulnerable patients, was appalling and beneath contempt; 13.20. Al Muderis’s negligence in performing osseointegration surgery, that resulted in maggots in a surgical wound, was unprecedented; 13.21. Al Muderis behaved inexcusably towards his patients by palming them off to others to care for after surgery; 13.22. Al Muderis was negligent in his care for his patient Chris Bruha by his refusal to care for his patient’s post-surgical open infected wound; 13.23. Al Muderis ripped off his patient Chris Bruha by placing a defective implant in him that snapped and charging him for a replacement part; 13.24. Al Muderis improperly profits from his patients by charging them twice for the parts and procedure; 13.25. Al Muderis misled his patient Chris Bruha about the success of his prospective surgery; 13.26. Al Muderis cares more about fame and large patient numbers than patient care; 13.27. Al Muderis has illegally performed surgery in the United States where he is not licenced to practice; 13.28. Al Muderis lied to 60 Minutes about encouraging staff to teach patients how to fundraise for surgeries; 13.29. Al Muderis lied about paying people to recruit patients for him; and 13.30. Al Muderis misleads prospective patients by only discussing positive outcomes with them and trying to silence any negative outcomes whilst downplaying any risks of the surgeries. |
The SMH Article |
16.1. Al Muderis is a callous surgeon who routinely left patients in pain to rot after their surgeries; 16.2. Al Muderis routinely negligently failed to provide after surgery care to his patients who undergo osseointegration surgery; 16.3. Al Muderis was so negligent in his failure to provide after surgery care that some patients were left mutilated, wheelchair bound or reliant on heavy pain medication; 16.4. Al Muderis negligently performs osseointegration surgery on patients who are not suited to having that procedure; 16.5. Al Muderis uses improper sales tactics on his patients to pressure them to agree to osseointegration surgery when it is not appropriate for them; 16.6. Al Muderis negligently failed to warn his patients Mark Urquhart and Brennan Smith of the risks associated with osseointegration surgery; 16.7. Al Muderis negligently ignored his patient Urquhart who reported finding maggots in his leg as a result of his bone being exposed for years after surgery conducted by Al Muderis; 16.8. Al Muderis’s negligent performance of osseointegration surgery on Mark Urquhart caused him chronic infection and extreme agonising pain; 16.9. Al Muderis callously dismissed Mark Urquhart’s concerns about his pain and the smell of his wound, suggesting he use Febreze, a supermarket air freshener, to deal with it; 16.10. Al Muderis’s glittering reputation and praise for his work as a surgeon is undeserved because his malpractices and unethical conduct as a doctor have left many patients devastated and mutilated; 16.11. Al Muderis repeatedly refused to see his patient Mark Urquhart after surgery when he complained about the smell of his wound; 16.12. Al Muderis negligently failed to identify and treat an infection developed by Mark Urquhart post-surgery that developed into osteomyelitis, a chronic infection to the bone, causing him to become wheelchair bound and with chronic severe pain; 16.13. Al Muderis’s performance of osseointegration surgery on Carol Todd was so negligent that it caused her chronic pain for years, about half a litre of blood and pus to come out of her leg, multiple ongoing infections, and the need for five further operations; 16.14. Al Muderis callously ignored his patient Carol Todd’s chronic pain, blood and pus coming out of her leg, multiple ongoing infections, and the need for five further operations when she complained to him about it; 16.15. Al Muderis’s negligent performance of osseointegration surgery on Carol Todd has left her in extreme pain and with no choice but to amputate her leg or she will die; 16.16. Al Muderis prioritised growing his practice over patient care, operating on patients who were not suitable for the surgery, talking up positive outcomes and downplaying risks to get patients to agree to surgery; 16.17. Al Muderis overrode the protocol of a specialist assessment team deciding suitability of patients to have surgery, by going ahead irrespective of the team’s decision; 16.18. Al Muderis overworked his staff, humiliated them in public, and degraded and traumatised them; 16.19. Al Muderis lied about paying commissions to Fred Hernandez; 16.20. Al Muderis’s performance of osseointegration surgery on Brennan Smith was so negligent that his pain was so bad that he began cutting his own skin off; 16.21. Al Muderis failed to inform his patient Brennan Smith of the side effects and adverse consequences of osseointegration surgery before he agreed to have it and falsely promised the surgery would give him a new life in order to convince Mr Smith to pay him $10,000; 16.22. Al Muderis used a defective product on his patient Michelle Oritz which broke, caused a bad infection and cost her over $65,000 to rectify; 16.23. Al Muderis performed osseointegration surgery so negligently on Rachael Ulrich she almost died; 16.24. Al Muderis callously dismissed Rachael Ulrich’s life threatening blood clots caused by surgery he performed as a mere mistake that was not his fault; 16.25. Al Muderis is negligent in his selection of patients for osseointegration surgery, causing life changing and life destroying consequences to patients; 16.26. Al Muderis is a negligent surgeon in that he has habitually failed to explain risks and complications to patients before performing osseointegration surgery on them; 16.27. Al Muderis’s negligent performance of osseointegration surgery on Blythe Warland caused him to suffer major infections about every six months which take months to subside, and complex regional pain syndrome resulting in his losing his house, his relationship and his company; 16.28. Al Muderis performed multiple unnecessary surgeries on a patient because he had workers compensation insurance to pay for them but then dumped the patient when things went wrong; 16.29. Al Muderis’s negligent performance of osseointegration surgery on a patient made him/her worse off causing phantom pain, nerve pain and bleeding such that he/she could not return to work; and 16.30. Al Muderis’s negligent performance of osseointegration surgery on a patient made him/her worse off causing extreme pain, such that he/she could no longer use a limb that was fully functional before the surgery. |
The Grieve Video |
28.1. Al Muderis, who operates on patients around the world, habitually downplays the risks of osseointegration surgery and ignores the complications; 28.2. Al Muderis has ignored patients with maggots in their wounds; 28.3. Al Muderis has ignored patients forcing them to use a kitchen knife to cut off their own flesh; 28.4. Al Muderis has negligently left patients mutilated, addicted to pain medication and antidepressants; 28.5. Al Muderis employs high pressure sales tactics to the detriment of his patients in order to grow his business at all costs; 28.6. Al Muderis ignores his patients and then threatens to sue them when they have complained to the medical regulator; 28.7. Al Muderis’s treatment of his patients is unacceptable in his failure to treat post-surgery complications; 28.8. Al Muderis’s practice of osseointegration surgery is unethical and dangerous; 28.9. Al Muderis has falsely misrepresented a rosy image of his surgical practice to the public when in fact it is unethical and dangerous. |
Annexure I — Imputations Table
Please note the imputations in the table highlighted in yellow are the Disputed Imputations: see Part 2, Section 2. These imputations are relied on as contextual imputations discussed at Remaining imputations, Part 7, Section 1.
The sting numbers reflect the stings identified in Part 5, Section 2, and considered in Part 7, Section 1.
The N/A denotes those imputations that the respondents did not plead the truth defence.
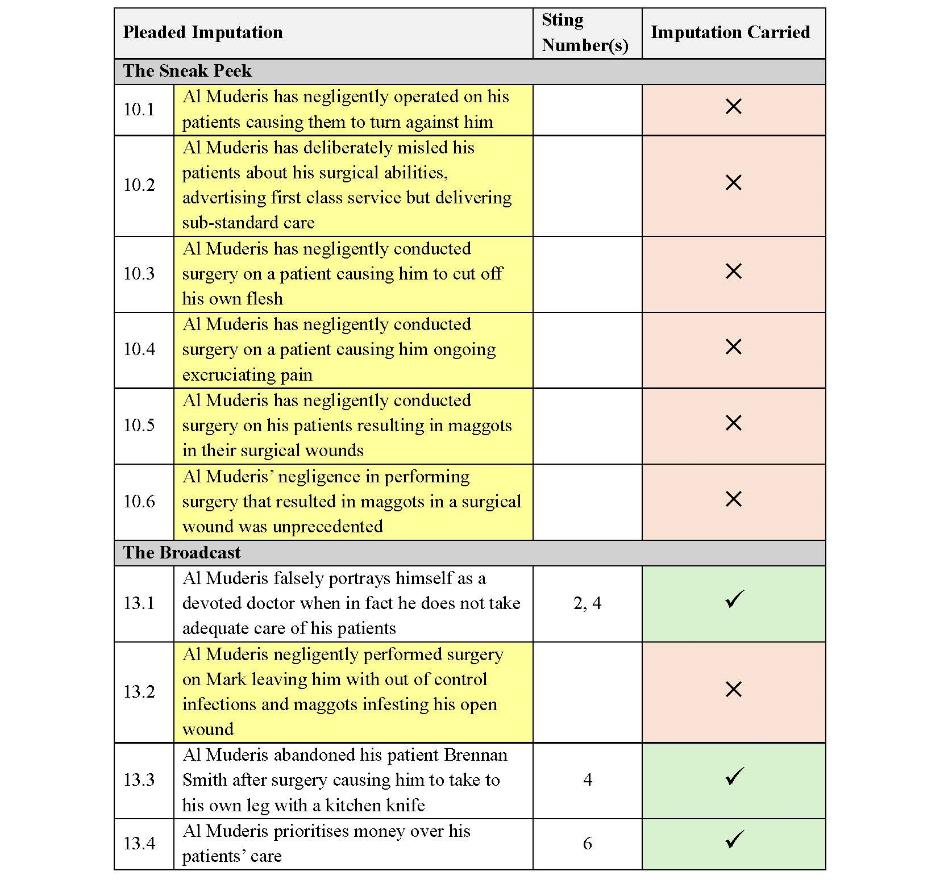
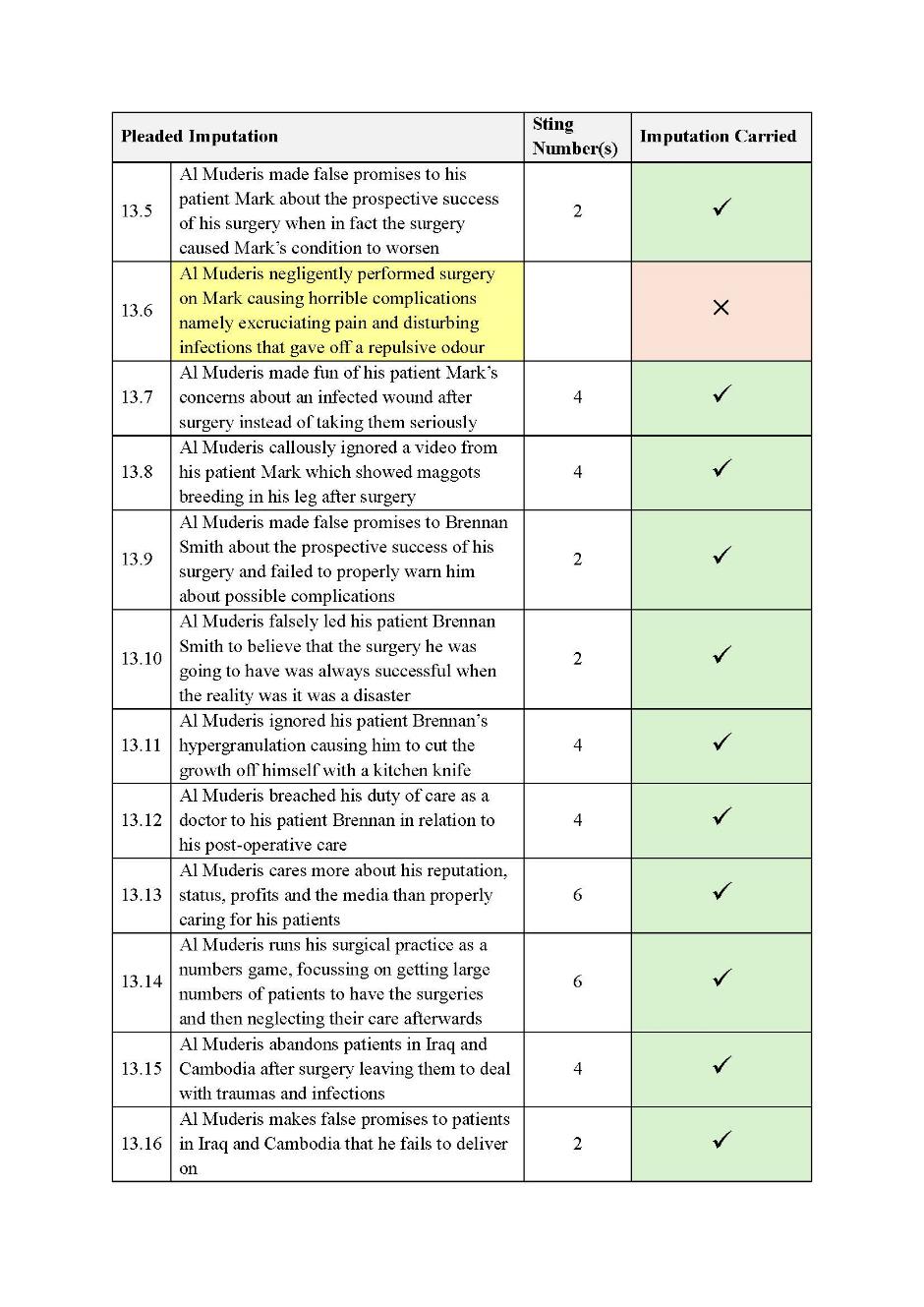
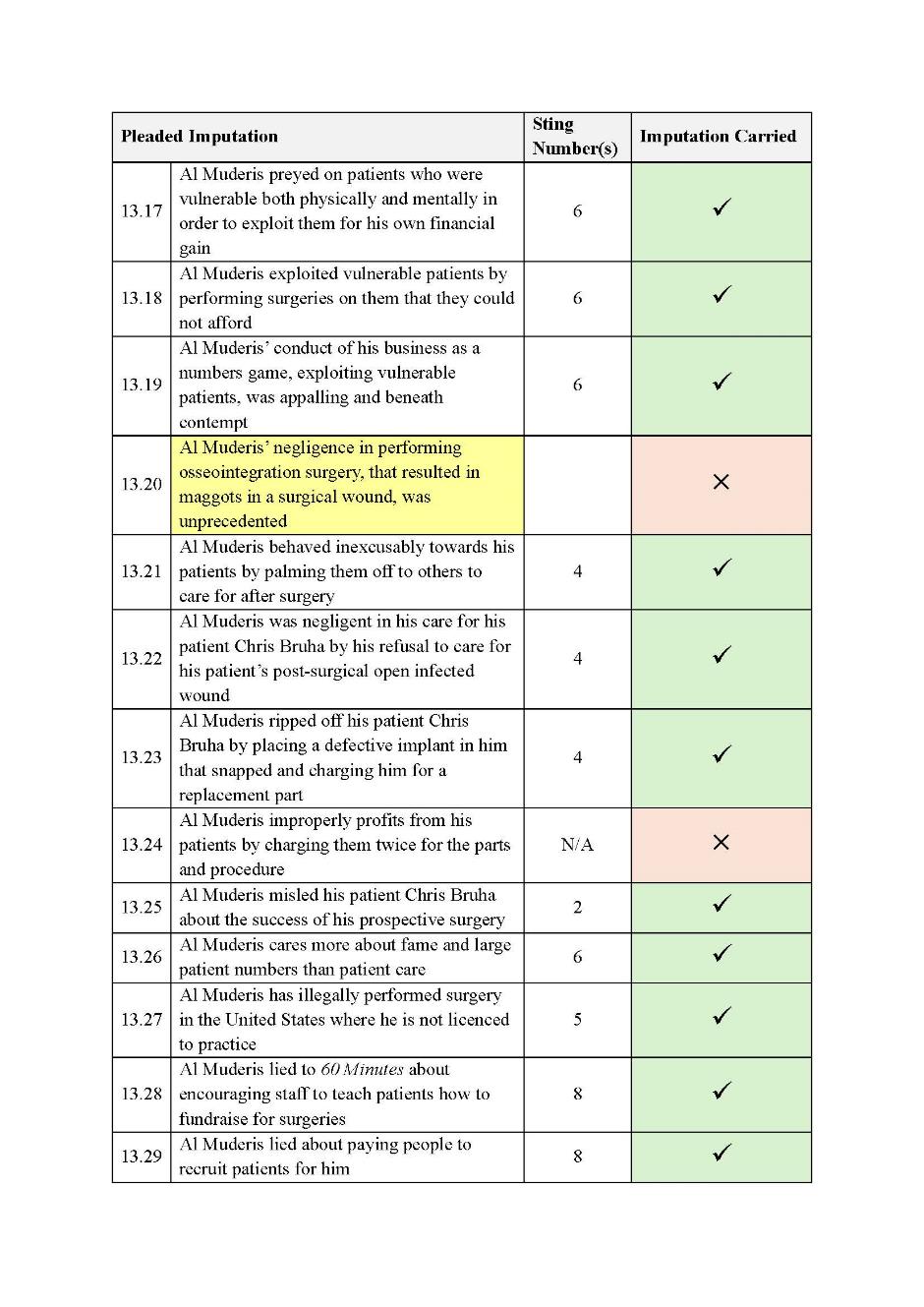
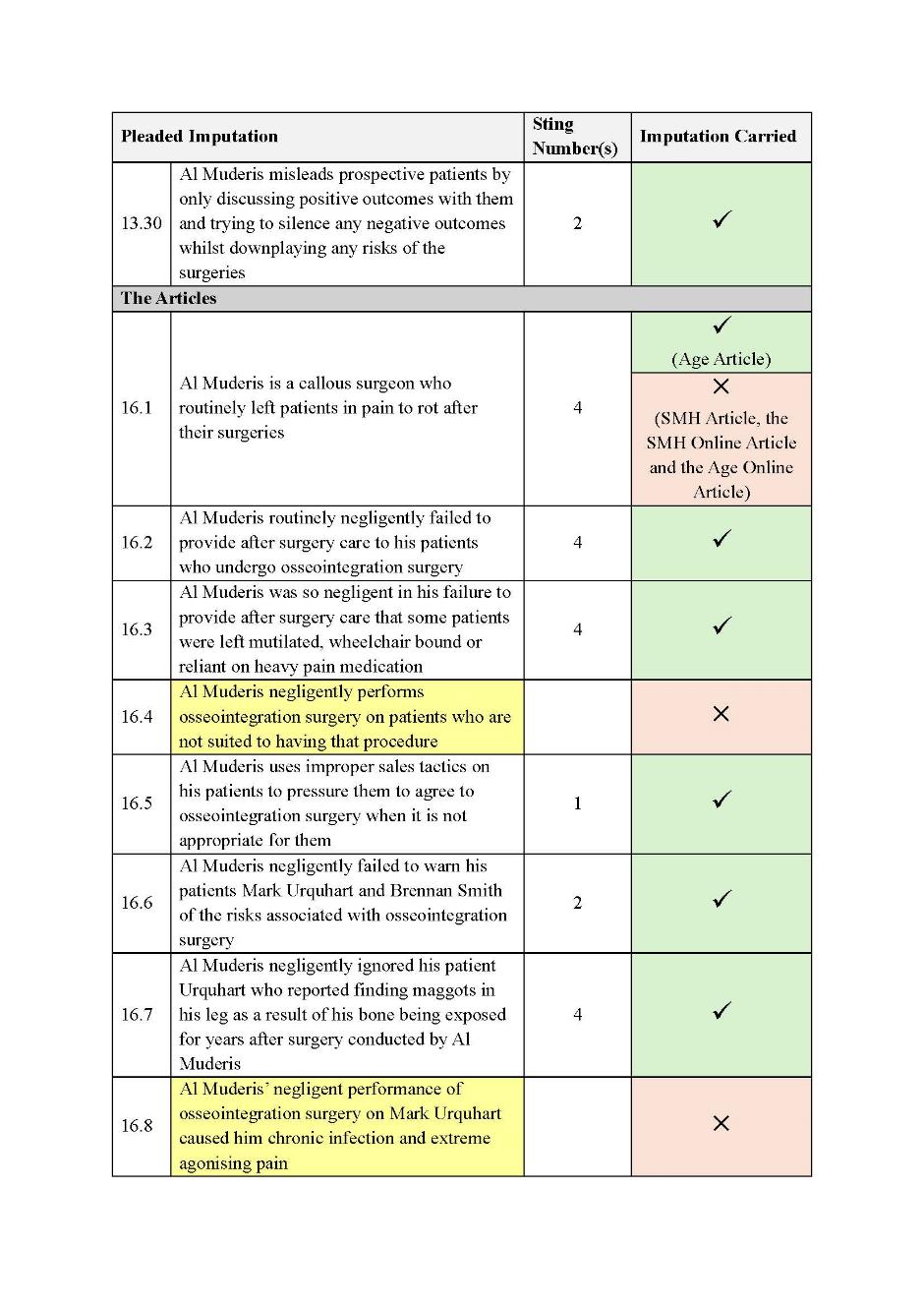
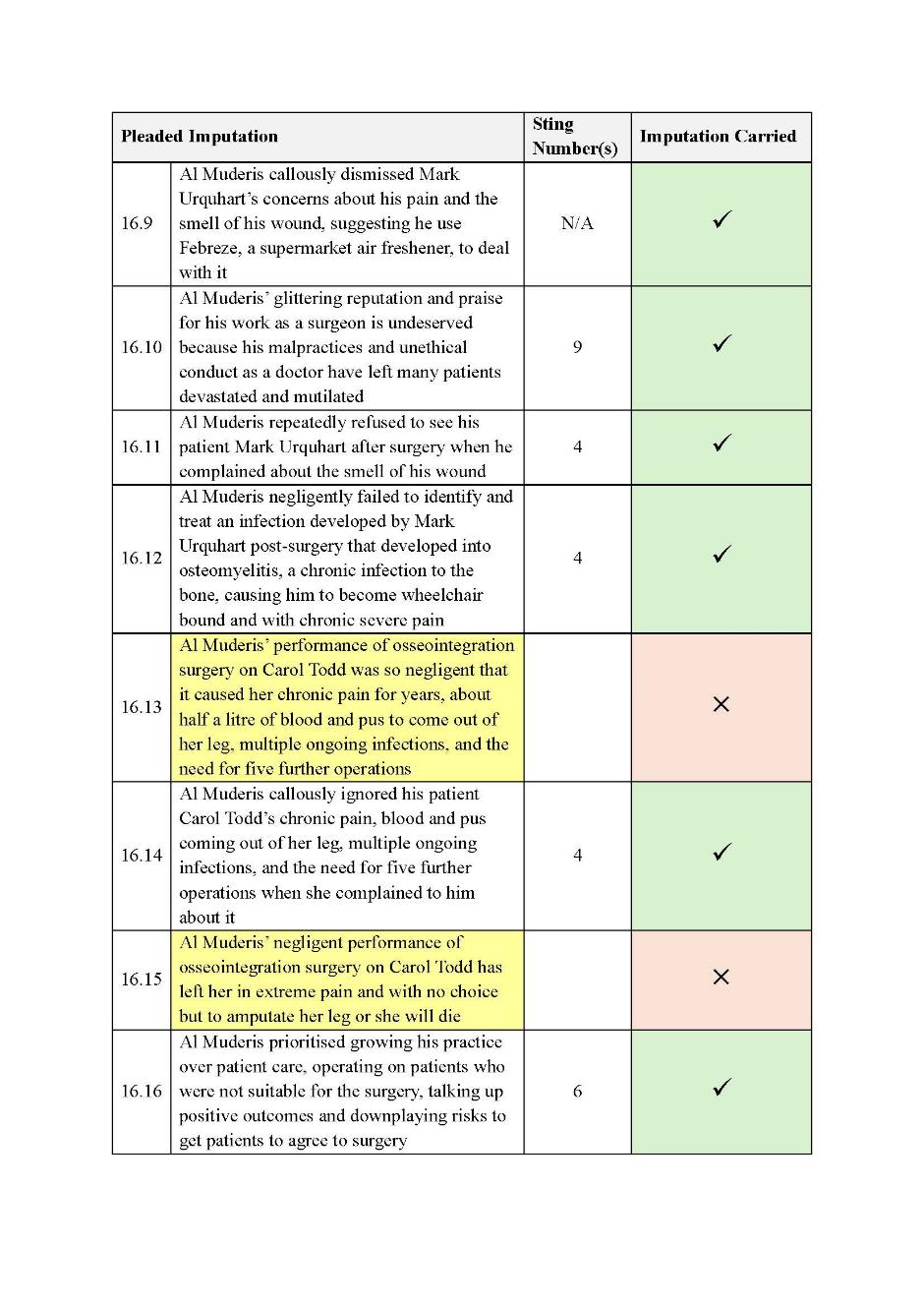
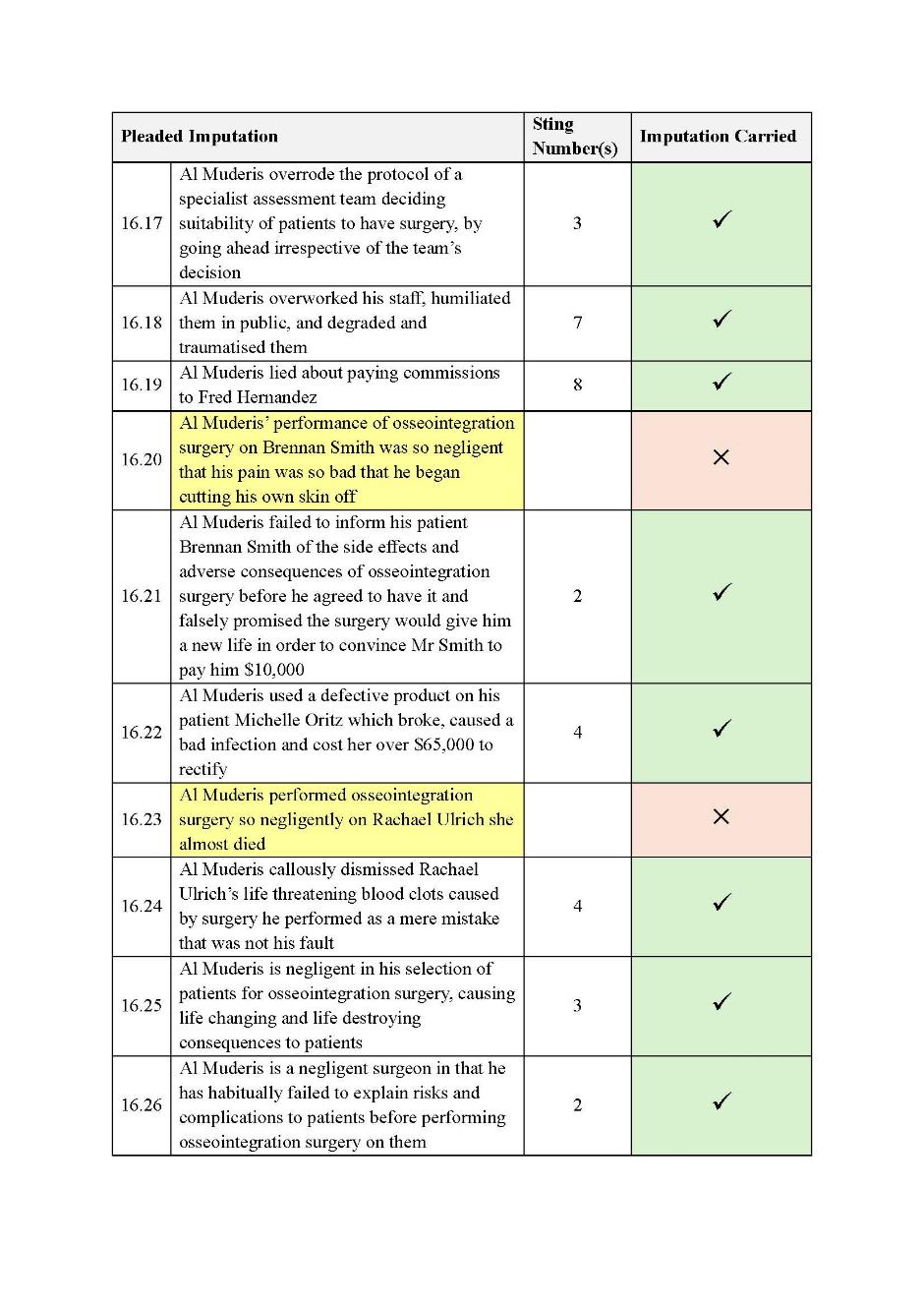
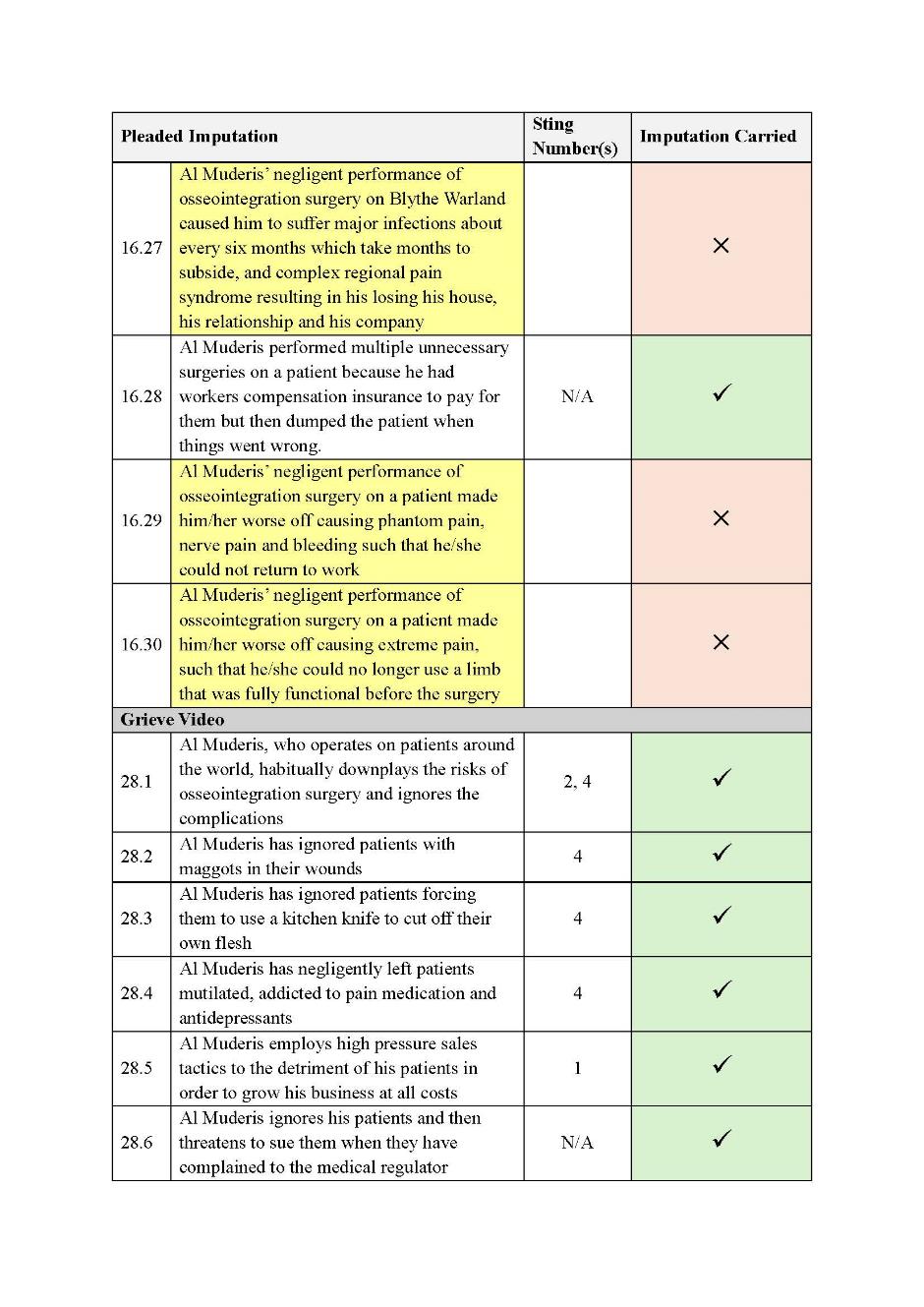
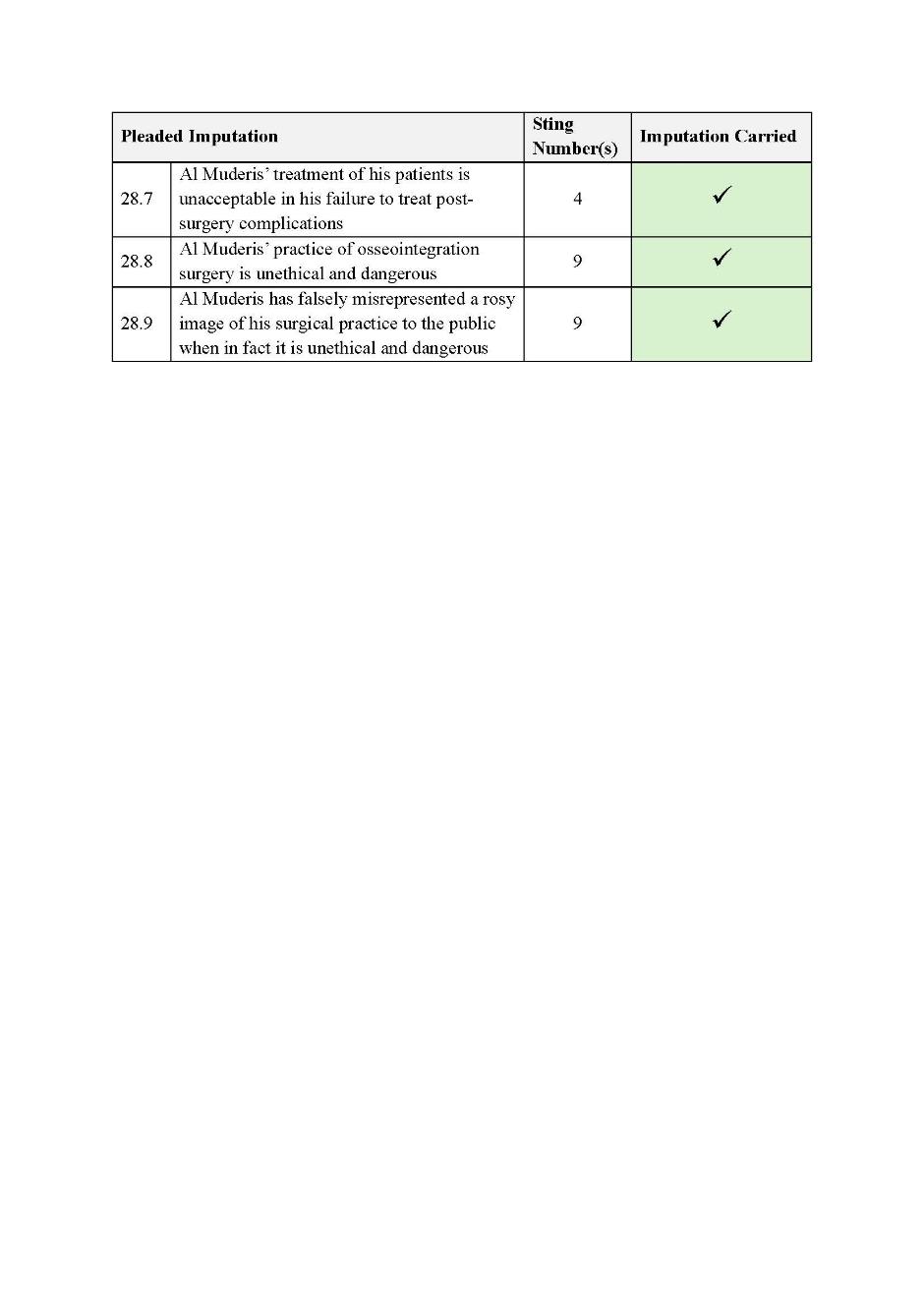
SCHEDULE OF PARTIES
NSD 917 of 2022 | |
Respondents | |
Fourth Respondent: | CHARLOTTE GRIEVE |
Fifth Respondent: | TOM STEINFORT |
Sixth Respondent: | NATALIE CLANCY |




