Neurim Pharmaceuticals (1991) Ltd v Generic Partners Pty Ltd (No 5) [2024] FCA 360
ORDERS
DATE OF ORDER: |
THE COURT ORDERS THAT:
1. By 4.00pm 26 April 2024 the parties provide proposed short minutes of order to the Associate to Nicholas J in accordance with his Honour’s reasons published today.
2. By 4.00pm 26 April 2024 the parties provide to the Associate to Nicholas J written notice of the scope of any disagreement between them in relation those parts of the short minutes of order referred to in order 1 that are not agreed.
3. The proceeding stand over to 9.30am on 2 May 2024 for the making of further orders.
Note: Entry of orders is dealt with in Rule 39.32 of the Federal Court Rules 2011.
REASONS FOR JUDGMENT
[1] | |
[9] | |
[9] | |
[12] | |
[13] | |
[14] | |
[30] | |
[31] | |
[37] | |
[40] | |
[41] | |
[42] | |
[50] | |
[68] | |
[69] | |
[70] | |
[70] | |
[76] | |
[118] | |
[147] | |
[147] | |
[158] | |
[166] | |
[195] | |
[207] | |
[222] | |
[225] | |
[227] | |
[259] | |
[290] | |
[298] | |
[304] | |
[310] | |
[313] | |
[384] | |
[464] | |
[469] | |
[474] |
NICHOLAS J:
1 This is a proceeding brought by the applicant (“Neurim”) against the first respondent (“Generic Partners”) and the second respondent (“Apotex”) for infringement of claims 1-7 of Australian Patent 2002326114 (“the Patent”) entitled “Method for treating primary insomnia”. The Patent was based on a PCT application filed on 12 August 2002 (“the PCT application”) and claims priority from a patent application filed in Israel on 14 August 2001 (“priority date”). The Patent was granted on 5 July 2007 and expired on 12 August 2022.
2 Neurim applied to amend claims 1, 2, 4, 5, 6, 8 and 9 and related consistory statements so as to bring those statements into alignment with the proposed amended claims. The amendments were allowed by this Court on 19 February 2019 see: Neurim Pharmaceuticals (1991) Ltd v Generic Partners Pty Ltd (No 2) (2019) 139 IPR 424.
3 The patent has nine claims, including, independent claims 1 and 8, each of which is a Swiss-style claim, and independent claims 4 and 9, each of which is for a method of treatment. Claims 1-9 (as amended) are in these terms:
1. Use of melatonin in the manufacture of a medicament for treating a patient suffering from primary insomnia characterized by non-restorative sleep and improving the restorative quality of sleep in said patient, wherein said medicament comprises also at least one pharmaceutically acceptable diluent, preservative, antioxidant, solubilizer, emulsifier, adjuvant or carrier, said medicament is a prolonged release formulation in unit dosage form and said melatonin is present in said medicament in an effective amount within the range of 0.025 to 10 mg.
2. Use according to claim 1, wherein the medicament comprises at least one of the following features:
(i) it is adapted for oral, rectal, parenteral, transbuccal, intrapulmonary (e.g. by inhalation) or transdermal administration;
(ii) it is in a depot form which will release the melatonin slowly in the body, over a preselected time period.
3. Use according to claim 2, wherein said prolonged release formulation includes an acrylic resin.
4. Method for treating a patient suffering from primary insomnia characterized by non-restorative sleep and improving the restorative quality of sleep in said patient, which comprises administering an effective amount within the range of 0.025 to 10 mg of melatonin to said patient, wherein said melatonin is administered in the form of a medicament, said medicament is a prolonged release formulation in unit dosage form, and said melatonin is the only therapeutically active agent administered according to said method.
5. Method according to claim 4, wherein the medicament comprises also at least one pharmaceutically acceptable diluent, preservative, antioxidant, solubilizer, emulsifier, adjuvant or carrier.
6. Method according to claim 5, wherein the medicament comprises at least one of the following features:
(i) it is adapted for oral, rectal, parenteral, transbuccal, intrapulmonary (e.g. inhalation) or transdermal administration;
(ii) it is in a depot form which will release said at least one compound slowly in the body, over a preselected time period.
7. Method according to claim 6, wherein said prolonged release formulation includes an acrylic resin.
8. Use of melatonin in the manufacture of a medicament for treating a patient suffering from primary insomnia characterized by non-restorative sleep and improving the restorative quality of sleep in said patient, substantially as herein described with reference to any one of the examples but excluding comparative examples.
9. Method for treating a patient suffering from primary insomnia characterized by non-restorative sleep and improving the restorative quality of sleep in said patient, substantially as herein described with reference to any one of the examples but excluding comparative examples.
4 Neurim’s commercial embodiment of the medicament described in (inter alia) claim 1 is registered on the Australian Register of Therapeutic Goods (“ARTG”) under the product name “CIRCADIN melatonin 2 mg prolonged release tablet blister pack” (“Circadin”). It is registered in respect of “Monotherapy for the short term treatment of primary insomnia characterized by poor quality of sleep in patients who are aged 55 or over”.
5 On or around 3 April 2017, Generic Partners registered products containing 2 mg of the pharmaceutical compound melatonin in prolonged release form on the ARTG (“Generic Partners Products”). The Generic Partners Products, including “MELOTIN MR melatonin 2 mg modified release tablet blister pack” (“Melotin”), were registered for the same indication as Neurim’s product, Circadin.
6 On or around 17 July 2018, Generic Partners transferred sponsorship of some of the Generic Partners Products to Apotex (“Apotex Products”). Generic Partners remains the sponsor of Melotin, which it has supplied to Apotex from 12 March 2020. Apotex admits that from 22 April 2020, it has undertaken, and continues to undertake, marketing activities in respect of Melotin as the Australian distributor of the product. Apotex further admits that from around 28 April 2020, it has supplied Melotin with instructions for its indicated use, and authorises medical practitioners to prescribe Melotin for its indicated use.
7 The respondents have filed cross-claims seeking declarations of invalidity and orders for revocation of the Patent. The validity issues are to be determined by reference to the provisions of the Patents Act 1990 (Cth) (“the Act”) in the form it took prior to its amendment by the Intellectual Property Laws Amendment (Raising the Bar) Act 2012 (Cth) and, as explained later in these reasons, in the form s 7 of the Act took as at 12 August 2002. The grounds of invalidity relied on include that the invention as claimed lacks novelty and does not involve an inventive step. The respondents also contend that the complete specification does not fully describe the invention as required by s 40(2)(a) of the Act and that the claims are not fairly based or clear as required by s 40(3) of the Act.
8 The parties agreed on a statement of issues to which I have had regard, though I have chosen not to frame my reasons for judgment around it.
9 The field of the invention is described in the Patent as follows at page 1, lines 4-9:
The present invention relates to a method for treating primary insomnia (as defined by DSM-IV or nonorganic insomnia as defined by ICD-10) when characterized by non-restorative sleep, to the use of melatonin or certain other compounds in the manufacture of a medicament for this purpose, and to a medicament comprising a combination of compounds, for use in improving both the quality and quantity of sleep, in primary insomnia.
10 “DSM-IV” refers to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders which was first published in 1994 by the American Psychiatric Association. It is a diagnostic system used to diagnose patients suffering from mental disorders. A revised edition, DSM-IV-TR, was published in 2000 and was current at the priority date. However, the diagnostic criteria for primary insomnia are identical in DSM-IV and DSM-IV-TR and minor differences in the description of the primary insomnia between those versions of texts would not result in any change in how a person skilled in the art would understand the Patent.
11 “ICD-10” refers to the tenth edition of the International Statistical Classification of Diseases and Related Health Problems which was published in 1992, and which was current at the priority date. It is a diagnostic system published by the World Health Organization (“WHO”).
12 The background to the invention is set out as follows at page 1, line 15 to page 3, line 24:
Sleep disorders, which are complex, are widespread, especially in Western industrial countries, in which it is estimated that about one third of the adult population reports at least occasional difficulties with sleeping, while at least half of the sleep-disordered population have had sleep complaints for years. In US 5,776,969 (James), which discloses a method of treating various sleep disorders, by therapy with a specified combination of chemical compounds, there is discussed and defined inter alia, primary insomnia, which may or may not be characterized by non-restorative sleep.
The definition of primary insomnia in the fourth revision of the [DSM-IV] (American Psychiatric Association, 1994) states: “The predominant complaint is difficulty initiating or maintaining sleep, or non-restorative sleep, for at least one month. The sleep disturbance (or associated daytime fatigue) causes clinically significant distress or impairment in social, occupational or other important areas of functioning.” Furthermore, according to the definition, non-restorative sleep alone is sufficient to establish the diagnosis of primary insomnia, providing it results in impaired daytime functioning.
The tenth revision of the International Classification of Diseases (ICD-10) (World Health Organisation, 1991) describes nonorganic insomnia as “a condition of unsatisfactory quantity and/or quality of sleep.” It goes on to state that “there are people who suffer immensely from the poor quality of their sleep, while sleep in quantity is judged subjectively and/or objectively as within the normal limits.”
The diagnostic guidelines from ICD-10 state that the essential clinical features for a definitive diagnosis of primary insomnia are as follows: a) the complaint is either of difficulty falling asleep or maintaining sleep, or of poor quality sleep; b) the sleep disturbance has occurred at least three times per week for at least one month; c) there is preoccupation with the sleeplessness and excessive concern over its consequences at night and during the day; d) the unsatisfactory quantity and/or quality of sleep either causes marked distress or interferes with social and occupational functioning. Thus, there is repeated emphasis in ICD-10 on the equal importance of quality of sleep and quantity of sleep in the diagnosis of insomnia. The invention thus relates to primary insomnia (DSM-IV) or nonorganic insomnia (ICD-10).
Because, in normal humans, the natural hormone melatonin has an increased nocturnal concentration in the blood (according to a particular profile, see e.g. US 5,498,423 (Zisapel)), compared with its daytime concentration, and because also a lack of nocturnal melatonin appears to correlate with the existence of sleep disorders, especially although not exclusively in the elderly, the possibility of administering exogenous melatonin to ameliorate sleep disorders has been investigated and is the subject of many scientific papers.
Thus, for example, in James, S.P., et al. (Neuropsychopharmacology 1990, 3:19-23), melatonin (1 and 5 mg) and placebo were given at 10:45 pm for one night each to 10 polysomnographically pre-screened insomniacs with a mean age of 33.4 years. These patients (who may not necessarily have had non-restorative sleep related insomnia) had quantitative sleep deficits that were demonstrable by PSG. Administration of melatonin did not alter sleep latency, sleep efficiency, total sleep time, or wake after sleep onset. The patients reported improved sleep quality, though they were not more rested in the morning and believed that their total sleep time had been shorter when on melatonin.
In Ellis, C.M., et al. (J. Sleep Res., 1996, 5: 61-65), where melatonin (5 mg) was given at 8:00 pm for 1 week to patients with psychophysiological insomnia, there was no reported change in sleep quantity or quality; 8 patients out of 15 were unable to distinguish the period of active melatonin treatment.
In Hughes, R.J., et al. (Sleep 1998, 21: 52-68), immediate release and controlled release formulations of melatonin (0.5 and 5 mg) were given 30 min before sleep and additionally, an immediate release preparation of 0.5 mg melatonin was given halfway through the night to polysomnographically prescreened elderly patients with sleep maintenance insomnia. They found that both melatonin preparations reduced sleep latency but did not alter wake time after sleep onset (an important variable in sleep maintenance insomnia) or total sleep time. No melatonin-induced changes in reported sleep quality or daytime measure of mood and alertness were found.
MacFarlane J.G., et al. (Biol Psychiatry 1991, 30(4): 371-6) have reported that melatonin (75 mg per os), administered at 10 PM daily to 13 insomniac patients for 14 consecutive days gave a significant increase in the subjective assessment of total sleep time and daytime alertness, whereas 7/13 patients reported no significant effect on subjective feelings of well-being.
Thus, there appears to be little or no evidence from published articles, that administration of exogenous melatonin (or other melatonergic agents, melatonin agonists or melatonin antagonists), in the dosages contemplated by the present invention, would be likely to improve the restorative quality of sleep in subjects affected by primary insomnia characterized by non-restorative sleep.
However, in contrast with the results of the above published papers, the present inventors have surprisingly found that melatonin (and other melatonergic agents, melatonin agonists or melatonin antagonists) in fact improves the restorative quality of sleep in subjects suffering from primary insomnia. Suitable melatonin agonists and antagonists for use in the present invention include (but are not restricted to) such compounds described in US Patents Nos. US 5,151,446; US 5,318,994; US 5,385,944; US 5,403,851; and International Patent Specification No. WO 97/00069.
13 The Summary of the Invention includes two consistory statements (at p 4 line 23-p 4a line 5 in the marked-up copy of the Patent), the first of which uses the same language of claim 1, and the second of which uses the same language as claim 4:
In a first aspect, the present invention provides use of melatonin in the manufacture of a medicament for treating a patient suffering from primary insomnia characterized by non-restorative sleep and improving the restorative quality of sleep in said patient, wherein said medicament comprises also at least one pharmaceutically acceptable diluent, preservative, antioxidant, solubilizer, emulsifier, adjuvant or carrier, said medicament is a prolonged release formulation in unit dosage form, and said melatonin is present in said medicament in an effective amount within the range of 0.025 to 10 mg.
In a second aspect, the present invention provides method for treating a patient suffering from primary insomnia characterized by non-restorative sleep and improving the restorative quality of sleep in said patient, which comprises administering an effective amount within the range of 0.025 to 10 mg of melatonin to said patient, wherein said melatonin is administered in the form of a medicament, said medicament is a prolonged release formulation in unit dosage form, and said melatonin is the only therapeutically active agent administered according to said method.
14 The Patent states that the invention will be illustrated by examples (“Examples”). Five Examples are provided.
15 Example 1 involved a randomised double-blind trial of 40 elderly primary insomnia patients treated with either a 2 mg prolonged-release melatonin formulation, or placebo. Melatonin (or placebo) was administered every evening for three weeks.
16 On the last two days of treatment, full-night polysomnographic recordings were used to measure quantitative aspects of sleep, and on each morning following sleep recording in the laboratory, a battery of psychomotor tests was administered to assess daytime vigilance. In addition, sleep diaries were used daily to record patient assessments of their perceived quality of sleep for the previous night.
17 In the results section, it is reported that sleep induction (as measured by sleep onset latency, duration of wake prior to sleep onset and percentage of time spent asleep prior to sleep onset) significantly improved with melatonin compared with placebo. Sleep maintenance variables (number of awakenings, duration of wake after sleep onset, sleep efficiency, total sleep time) did not improve.
18 The study conclusions were:
These results show beneficial effects of melatonin on sleep initiation, similar to effects of hypnotic drugs. The hypnotic effects of melatonin were in line with reports in the literature showing that melatonin promotes sleep in humans without altering normal sleep architecture. In contrast to this apparently hypnotic effect, psychomotor skills were significantly higher in the melatonin compared to placebo-treated group: significant treatment effects for the Critical Flicker fusion test and total reaction time under melatonin vs. placebo were observed at the end of treatment.
These results thus show for the first time the association of hypnotic effect (shortening of sleep latency) by melatonin with enhanced daytime vigilance in primary insomnia patients suggesting that the restorative value of sleep has increased in these patients. With hypnotic drugs shortening of sleep latency and improved quality of sleep is associated with impaired psychomotor skills in the morning or at best no significant deterioration. No hypnotic drug has ever been shown to increase daytime vigilance. Surprisingly, in their diaries, patients did not evaluate the ease of getting to sleep as being better with melatonin compared to placebo. In fact, the patients judged their quality of sleep to be improved with melatonin but not placebo treatment. The restorative value of sleep may thus be associated with a perceived improvement in quality of sleep.
(Emphasis added)
19 It is apparent that this trial was assessing both quantitative aspects of the patients’ sleep (such as sleep latency) and daytime vigilance, and the quality of sleep based on the patients’ subjective reports. The patients’ subjective reports indicated that the quality of sleep of the patients given melatonin improved, compared to the control arm. It is apparent that the phrase “restorative value of sleep” (which is not used in the claims) is referring to the objective measurements of patients’ sleep latency and daytime vigilance rather than the patients’ subjective assessment of their sleep quality. The final sentence in the passage quoted above is pointing to an association between improvements in the restorative value of sleep and improvements in perceived quality of sleep (i.e., a subjective measurement).
20 Example 2 involved another randomised, double-blind trial in which 170 elderly patients suffering from primary insomnia were treated with either melatonin or placebo, to study the effects of a prolonged release melatonin formulation on subjectively assessed sleep quality and daytime vigilance. The subjects were treated for two weeks with a placebo to establish baseline characteristics, and then for three weeks with prolonged release melatonin (2 mg per night) or placebo. On the last three days of the baseline and treatment periods, patients were asked in the morning to indicate:
(a) the quality of their sleep (when compared to their usual, non-medicated sleep) by marking on a visual analogue scale with the end points “more restless than usual” and “more restful than usual”; and
(b) their feeling in the morning by responding to the question “how do you feel now?” using a visual analogue scale with the end points “tired” and “alert”.
21 It was found that both quality of sleep and daytime alertness improved significantly with melatonin, compared to the placebo, showing a link between improved restful sleep and less fatigue in the morning. It was concluded that the results showed that melatonin enhanced the restorative value of sleep in the primary insomnia patients.
22 Example 3 was also a randomised, double-blind trial of 131 insomnia patients aged between 20 and 80 years whose sleep quality and feeling at daytime was subjectively assessed. The subjects were treated for one week with a placebo to establish baseline characteristics, and then for three weeks with prolonged release melatonin (2 mg per night) or placebo. On the last three days of the baseline and treatment periods, patients were asked to assess the quality of their sleep the previous night and their feeling at daytime as described in Example 2.
23 In the results section, it is reported that: “[i]n the 55 years and older patients, there was an improvement of quality of sleep and daytime alertness… Surprisingly, it was found that in patients <55 years of age there was a significant worsening of the quality of sleep and daytime alertness compared to placebo.”
24 The results are set out in Table 2. Row 4 of Table 2 records that there was a mean improvement (-1.6mm) in perceived quality of sleep after treatment with melatonin (relative to perceived quality of sleep prior to melatonin treatment) in patients under the age of 55, but that the mean improvement was much greater with placebo (-13.7 mm) in this treatment group.
25 The conclusion drawn was that the results of the trial clearly indicate that melatonin was effective in primary insomnia related to non-restorative sleep, but could be detrimental to insomnia related to other causes (e.g., a sleep deficit due to an inability to initiate sleep). The Patent states:
The elderly are more likely to have maintenance and non-restorative sleep problems … Younger people typically have sleep onset problems and their main problem may be due to sleep deficit not non-restorative sleep. These results (Table 2) clearly indicate that melatonin was effective in primary insomnia related to non-restorative sleep, but can be detrimental to insomnia related to other aetiologies (e.g. sleep deficit due to inability to initiate sleep).
(Citation omitted)
26 The suggestion is that the mean improvement in perceived quality of sleep was less significant in the younger patients because few of them would be expected to suffer from non-restorative sleep (as opposed to, for example, primary insomnia characterised by difficulty initiating sleep). Thus, the Patent seeks to attribute the difference between the mean response in the two age groups to the elderly being more likely to have complaints of sleep maintenance and non-restorative sleep, whereas younger people are more likely to have a complaint of difficulty initiating sleep.
27 Example 4 was a randomised, double-blind, cross-over study which assessed psychomotor skills and driving performance in 16 healthy elderly volunteers given a tablet of placebo in the evening to establish baseline, and then a tablet or melatonin, zolpidem or placebo in a random order in the evening with one week with no treatment between treatments. A battery of psychomotor tasks, driving performance and wake EEG during a driving test were studied in the subjects at pre-selected intervals after administration of the tablet.
28 Example 4 involved healthy volunteers, not primary insomnia patients, and did not subjectively assess the quality of sleep of those healthy volunteers. The results found that there were several acute impairments seen with zolpidem compared to the placebo, while no cognitive effect of melatonin (adverse or otherwise) was identified. It was concluded that improvement in quality of sleep reported by patients (as is the case with zolpidem) does not necessarily indicate enhanced restorative sleep, since it is not associated with improved daytime vigilance. Further, the example was found to demonstrate that melatonin did not improve vigilance in non-insomnia patients.
29 Example 5 describes the method by which the formulation used in Examples 1-4 was prepared.
30 I have previously set out claims 1-9 of the Patent. The Swiss-style claims (claims 1-3), the method of treatment claims (claims 4-7) and the omnibus claims (claims 8-9) are concerned with the treatment of “a patient suffering from primary insomnia characterised by non-restorative sleep and improving the restorative quality of sleep in said patient”. A proper understanding of each of the claims requires consideration of the meaning of the following terms as used in the claims:
primary insomnia;
non-restorative sleep;
primary insomnia characterised by non-restorative sleep;
restorative quality of sleep; and
improving the restorative quality of sleep.
31 DSM-IV is incorporated in the Patent by reference.
32 Section 307.42 of DSM-IV is entitled “Primary Insomnia”. It is a nosology that was widely used by psychiatrists practicing in Australia at the priority date.
33 DSM-IV relevantly states at pages 553-557:
Primary Sleep Disorders
Dyssomnias
Dyssomnias are primary disorders of initiating or maintaining sleep or of excessive sleepiness and are characterized by a disturbance in the amount, quality, or timing of sleep. This section includes Primary Insomnia, Primary Hypersomnia, Narcolepsy, Breathing-Related Sleep Disorder, Circadian Rhythm Sleep Disorder, and Dyssomnia Not Otherwise Specified.
307.42 Primary Insomnia
Diagnostic Features
The essential feature of Primary Insomnia is a complaint of difficulty initiating or maintaining sleep or of nonrestorative sleep that lasts for at least 1 month (Criterion A) and causes clinically significant distress or impairment in social, occupational, or other important areas of functioning (Criterion B). The disturbance in sleep does not occur exclusively during the course of another sleep disorder (Criterion C) or mental disorder (Criterion D) and is not due to the direct physiological effects of a substance or a general medical condition (Criterion E).
Individuals with Primary Insomnia most often report a combination of difficulty falling asleep and intermittent wakefulness during sleep. Less commonly, these individuals may complain only of nonrestorative sleep, that is, feeling that their sleep was restless, light, or of poor quality. Primary Insomnia is often associated with increased physiological or psychological arousal at nighttime in combination with negative conditioning for sleep. A marked preoccupation with and distress due to the inability to sleep may contribute to the development of a vicious cycle: the more the individual strives to sleep, the more frustrated and distressed the individual becomes and the less he or she is able to sleep. Lying in a bed in which the individual has frequently spent sleepless nights may cause frustration and conditioned arousal. Conversely, the individual may fall asleep more easily when not trying to do so (e.g., while watching television, reading, or riding in a car). Some individuals with increased arousal and negative conditioning report that they sleep better away from their own bedrooms and their usual routines. Chronic insomnia may lead to decreased feelings of well-being during the day (e.g., deterioration of mood and motivation; decreased attention, energy, and concentration; and an increase in fatigue and malaise). Although individuals often have the subjective complaint of daytime fatigue, polysomnographic studies usually do not demonstrate an increase in physiological signs of sleepiness.
Associated Features and Disorders
Associated descriptive features and mental disorders. Many individuals with Primary Insomnia have a history of “light” or easily disturbed sleep prior to the development of more persistent sleep problems. Other associated factors may include anxious overconcern with general health and increased sensitivity to the daytime effects of mild sleep loss. Symptoms of anxiety or depression that do not meet criteria for a specific mental disorder may be present. Interpersonal, social, and occupational problems may develop as a result of overconcern with sleep, increased daytime irritability, and poor concentration. Problems with inattention and concentration may also lead to accidents. Individuals with Primary Insomnia may have a history of mental disorders, particularly Mood Disorders and Anxiety Disorders. Conversely, the chronic sleep disturbance that characterizes Primary Insomnia constitutes a risk factor for (or perhaps an early symptom of) subsequent Mood Disorders and Anxiety Disorders. Individuals with Primary Insomnia sometimes use medications inappropriately: hypnotics or alcohol to help with nighttime sleep, anxiolytics to combat tension or anxiety, and caffeine or other stimulants to combat excessive fatigue. In some cases, this type of substance use may progress to Substance Abuse or Substance Dependence.
Associated laboratory findings. Polysomnography may demonstrate poor sleep continuity (e.g., increased sleep latency, increased intermittent wakefulness, and decreased sleep efficiency), increased stage 1 sleep, decreased stages 3 and 4 sleep, increased muscle tension, or increased amounts of EEG alpha activity during sleep. These features must be interpreted within the context of age-appropriate norms. Some individuals may report better sleep in the laboratory than at home, suggesting a conditioned basis for sleep complaints. Other psychophysiological tests may also show high arousal (e.g., increased muscle tension or excessive physiological reactivity to stress). Individuals with Primary Insomnia may also have elevated scores on self-report psychological or personality inventories (e.g., on profiles indicating chronic, mild depression and anxiety; an "internalizing" style of conflict resolution; and a somatic focus).
Associated physical examination findings and general medical conditions. Individuals with Primary Insomnia may appear fatigued or haggard, but show no other characteristic abnormalities on physical examination. There may be an increased incidence of stress-related psychophysiological problems (e.g., tension headache, increased muscle tension, gastric distress).
Specific Age and Gender Features
Survey data consistently demonstrate that complaints of insomnia are more prevalent with increasing age and among women. Young adults more often complain of difficulty falling asleep, whereas midlife and elderly adults are more likely to have difficulty with maintaining sleep and early morning awakening. Paradoxically, despite the greater prevalence of insomnia complaints among elderly women, polysomnographic studies generally indicate better preservation of sleep continuity and slow-wave sleep in elderly females than in elderly males. The reason for this discrepancy between self-report and laboratory data is not known.
Prevalence
The true prevalence rate of Primary Insomnia in the general population is unknown.
Population surveys indicate a 1-year prevalence of insomnia complaints of 30%-40% in adults (although the percentage of those whose sleep disturbance would meet criteria for Primary Insomnia has not been studied). In clinics specializing in sleep disorders, approximately 15%-25% of individuals with chronic insomnia are diagnosed with Primary Insomnia.
Course
The factors that precipitate Primary Insomnia may differ from those that perpetuate it. Most cases have a fairly sudden onset at a time of psychological, social, or medical stress. Primary Insomnia often persists long after the original causative factors resolve, due to the development of heightened arousal and negative conditioning. For example, a person with a painful injury who spends a great deal of time in bed and has difficulty sleeping may then develop negative associations for sleep. Negative associations, increased arousal, and conditioned awakenings may then persist beyond the convalescent period, leading to Primary Insomnia. A similar scenario may develop in association with insomnia that occurs in the context of an acute psychological stress or a mental disorder. For instance, insomnia that occurs during an episode of Major Depressive Disorder can become a focus of attention with consequent negative conditioning, and insomnia may persist long after resolution of the depressive episode. In some cases, Primary Insomnia may develop gradually without a clear stressor.
Primary Insomnia typically begins in young adulthood or middle age and is rare in childhood or adolescence. In exceptional cases, the insomnia can be documented back to childhood. The course of Primary Insomnia is variable. It may be limited to a period of several months, particularly if precipitated by a psychosocial or medical stressor that later resolves. The more typical course consists of an initial phase of progressive worsening over weeks to months, followed by a chronic phase of stable sleep difficulty that may last for many years. Some individuals experience an episodic course, with periods of better or worse sleep occurring in response to life events such as vacations or stress.
Familial Pattern
The predisposition toward light and disrupted sleep has a familial association. Formal genetic and/or family studies have not been conducted.
Differential Diagnosis
“Normal” sleep duration varies considerably in the general population. Some individuals who require little sleep (“short sleepers”) may be concerned about their sleep duration. Short sleepers are distinguished from those with Primary Insomnia by their lack of difficulty falling asleep and by the absence of characteristic symptoms of Primary Insomnia (e.g., intermittent wakefulness, fatigue, concentration problems, or irritability).
Daytime sleepiness, which is a characteristic feature of Primary Hypersomnia, can also occur in Primary Insomnia, but is not as severe in Primary Insomnia. When daytime sleepiness is judged to be due to insomnia, an additional diagnosis of Primary Hypersomnia is not given.
Jet Lag and Shift Work Types of Circadian Rhythm Sleep Disorder are distinguished from Primary Insomnia by the history of recent transmeridian travel or shift work. Individuals with the Delayed Sleep Phase Type of Circadian Rhythm Sleep Disorder report sleep-onset insomnia only when they try to sleep at socially normal times, but they do not report difficulty falling asleep or staying asleep when they sleep at their preferred times.
Narcolepsy may cause insomnia complaints, particularly in older adults. However, Narcolepsy rarely involves a major complaint of insomnia and is distinguished from Primary Insomnia by symptoms of prominent daytime sleepiness, cataplexy, sleep paralysis, and sleep-related hallucinations.
A Breathing-Related Sleep Disorder, particularly central sleep apnea, may involve a complaint of chronic insomnia and daytime impairment. A careful history may reveal periodic pauses in breathing during sleep or crescendo-decrescendo breathing (Cheyne-Stokes respiration). A history of central nervous system injury or disease may further suggest a Breathing-Related Sleep Disorder. Polysomnography can confirm the presence of apneic events. Most individuals with Breathing-Related Sleep Disorder have obstructive apnea that can be distinguished from Primary Insomnia by a history of loud snoring, breathing pauses during sleep, and excessive daytime sleepiness.
Parasomnias are characterized by a complaint of unusual behavior or events during sleep that sometimes may lead to intermittent awakenings. However, it is these behavioral events that dominate the clinical picture in a Parasomnia rather than the insomnia.
Primary Insomnia must be distinguished from mental disorders that include insomnia as an essential or associated feature (e.g., Major Depressive Disorder, Generalized Anxiety Disorder, Schizophrenia). The diagnosis of Primary Insomnia is not given if insomnia occurs exclusively during the course of another mental disorder. A thorough investigation for the presence of other mental disorders is essential before considering the diagnosis of Primary Insomnia. A diagnosis of Primary Insomnia can be made in the presence of another current or past mental disorder if the mental disorder is judged to not account for the insomnia or if the insomnia and the mental disorder have an independent course. In contrast, when insomnia occurs as a manifestation of, and exclusively during the course of, another mental disorder (e.g., a Mood, Anxiety, Somatoform, or Psychotic Disorder), the diagnosis of Insomnia Related to Another Mental Disorder may be more appropriate. This diagnosis should only be considered when the insomnia is the predominant complaint and is sufficiently severe to warrant independent clinical attention; otherwise, no separate diagnosis is necessary.
Primary insomnia must be distinguished from Sleep Disorder Due to a General Medical Condition, Insomnia Type. The diagnosis should be Sleep Disorder Due to a General Medical Condition when the insomnia is judged to be the direct physiological consequence of a specific general medical condition (e.g., pheochromocytoma, hyperthyroidism) (see p. 597). This determination is based on history, laboratory findings, or physical examination. Substance-Induced Sleep Disorder, Insomnia Type, is distinguished from Primary Insomnia by the fact that a substance (i.e., a drug of abuse, a medication, or exposure to a toxin) is judged to be etiologically related to the insomnia (see p. 601). For example, insomnia occurring only in the context of heavy coffee consumption would be diagnosed as Caffeine-Induced Sleep Disorder, Insomnia Type, With Onset During Intoxication.
Relationship to International
Classification of Sleep Disorders
Primary Insomnia subsumes a number of insomnia diagnoses in the International Classification of Sleep Disorders (ICSD), including Psychophysiological Insomnia, Sleep State Misperception, Idiopathic Insomnia, and some cases of Inadequate Sleep Hygiene. Psychophysiological Insomnia most closely resembles Primary Insomnia, particularly in terms of arousal and conditioning factors. Sleep State Misperception is a condition characterized by complaints of insomnia with a marked discrepancy between subjective and objective estimates of sleep. Idiopathic Insomnia includes those cases with onset in childhood and a lifelong course, presumably due to an abnormality in the neurological control of the sleep-wake system. Inadequate Sleep Hygiene refers to insomnia resulting from behavioral [sic] practices that increase arousal or disrupt sleep organization (e.g., working late into the night, taking excessive daytime naps, or keeping irregular sleep hours).
• Diagnostic criteria for 307.42 Primary Insomnia
|
34 Appendix C of DSM-IV is entitled “Glossary of Technical Terms” and includes the following definition of “insomnia”:
A subjective complaint of difficulty falling or staying asleep or poor sleep quality. Types of insomnia include
initial insomnia Difficulty in falling asleep.
middle insomnia Awakening in the middle of the night followed by eventually falling back to sleep, but with difficulty.
terminal insomnia Awakening before one’s usual waking time and being unable to return to sleep.
35 Appendix H of DSM-IV is entitled “DSM-IV Classification With ICD-10 Codes”. The introduction states:
As of the publication of this manual (in early 1994), the official coding system in use in the United States is the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). At some point within the next several years, the U.S. Department of Health and Human Services will require for reporting purposes in the United States the use of codes from the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). To facilitate this transition process, the preparation of DSM-IV has been closely coordinated with the preparation of Chapter V, “Mental and Behavioural Disorders,” of ICD-10 (developed by the World Health Organization). Consultations between the American Psychiatric Association and the World Health Organization have resulted in DSM-IV codes and terms that are fully compatible with the codes and terms in the tabular index of ICD-10. Presented below is the DSM-IV Classification with the ICD-10 codes.
36 “Primary Insomnia” is listed in the appendix with a reference to ICD-10 code F51.0 and a cross-reference to page 553 of DSM-IV which is extracted above.
37 ICD-10 is incorporated in the Patent by reference.
38 Section F51 of ICD-10 is entitled “Nonorganic Sleep Disorders” and relevantly states:
This group of disorders includes:
(a) dyssomnias: primarily psychogenic conditions in which the predominant disturbance is in the amount, quality, or timing of sleep due to emotional causes, i.e. insomnia, hypersomnia, and disorder of sleep — wake schedule; and
(b) parasomnias: abnormal episodic events occurring during sleep; in childhood these are related mainly to the child’s development, while in adulthood they are predominantly psychogenic, i.e. sleepwalking, sleep terrors, and nightmares.
This section includes only those sleep disorders in which emotional causes are considered to be a primary factor. Sleep disorders of organic origin such as Kleine — Levin syndrome are coded in Chapter VI of ICD-10. Nonpsychogenic disorders including narcolepsy and cataplexy and disorders of the sleep — wake schedule are also listed in Chapter VI, as are sleep apnoea and episodic movement disorders which include nocturnal myoclonus. Finally, enuresis is listed with other emotional and behavioural disorders with onset specific to childhood and adolescence, while primary nocturnal enuresis, which is considered to be due to a maturational delay of bladder control during sleep, is listed in Chapter XVIII of ICD-10 among the symptoms involving the urinary system.
In many cases, a disturbance of sleep is one of the symptoms of another disorder, either mental or physical. Even when a specific sleep disorder appears to be clinically independent, a number of associated psychiatric and/or physical factors may contribute to its occurrence. Whether a sleep disorder in a given individual is an independent condition or simply one of the features of another disorder (classified elsewhere in Chapter V or in other chapters of ICD-10) should be determined on the basis of its clinical presentation and course, as well as of therapeutic considerations and priorities at the time of the consultation. In any event, whenever the disturbance of sleep is among the predominant complaints, a sleep disorder should be diagnosed. Generally, however, it is preferable to list the diagnosis of the specific sleep disorder along with as many other pertinent diagnoses as are necessary to describe adequately the psychopathology and/or pathophysiology involved in a given case.
…
F51.0 Nonorganic insomnia
Insomnia is a condition of unsatisfactory quantity and/or quality of sleep, which persists for a considerable period of time. The actual degree of deviation from what is generally considered as a normal amount of sleep should not be the primary consideration in the diagnosis of insomnia, because some individuals (the so-called short sleepers) obtain a minimal amount of sleep and yet do not consider themselves as insomniacs. Conversely, there are people who suffer immensely from the poor quality of their sleep, while sleep quantity is judged subjectively and/or objectively as within normal limits.
Among insomniacs, difficulty falling asleep is the most prevalent complaint, followed by difficulty staying asleep and early final wakening. Usually, however, patients report a combination of these complaints. Typically, insomnia develops at a time of increased lifestress and tends to be more prevalent among women, older individuals and psychologically disturbed and socioeconomically disadvantaged people. When insomnia is repeatedly experienced, it can lead to an increased fear of sleeplessness and a preoccupation with its consequences. This creates a vicious circle which tends to perpetuate the individual’s problem.
Individuals with insomnia describe themselves as feeling tense, anxious, worried, or depressed at bedtime, and as though their thoughts are racing. They frequently ruminate over getting enough sleep, personal problems, health status, and even death. Often they attempt to cope with their tension by taking medication or alcohol. In the morning, they frequently report feeling physically and mentally tired; during the day, they characteristically feel depressed, worried, tense, irritable, and preoccupied with themselves.
Children are often said to have difficulty sleeping when in reality the problem is a difficulty in the management of bedtime routines (rather than of sleep per se); bedtime difficulties should not be coded here, but in Chapter XXI of ICD-10 (Z62.0, inadequate parental supervision and control).
Diagnostic guidelines
The following are essential clinical features for a definite diagnosis:
(a) the complaint is either of difficulty falling asleep or maintaining sleep, or of poor quality of sleep;
(b) the sleep disturbance has occurred at least three times per week for at least 1 month;
(c) there is preoccupation with the sleeplessness and excessive concern over its consequences at night and during the day;
(d) the unsatisfactory quantity and/or quality of sleep either causes marked distress or interferes with ordinary activities in daily living.
Whenever unsatisfactory quantity and/or quality of sleep is the patient’s only complaint, the disorder should be coded here. The presence of other psychiatric symptoms such as depression, anxiety or obsessions does not invalidate the diagnosis of insomnia, provided that insomnia is the primary complaint or the chronicity and severity of insomnia cause the patient to perceive it as the primary disorder. Other coexisting disorders should be coded if they are sufficiently marked and persistent to justify treatment in their own right. It should be noted that most chronic insomniacs are usually preoccupied with their sleep disturbance and deny the existence of any emotional problems. Thus, careful clinical assessment is necessary before ruling out a psychological basis for the complaint.
Insomnia is a common symptom of other mental disorders, such as affective, neurotic, organic, and eating disorders, substance use, and schizophrenia, and of other sleep disorders such as nightmares. Insomnia may also be associated with physical disorders in which there is pain and discomfort or with taking certain medications. If insomnia occurs only as one of the multiple symptoms of a mental disorder or a physical condition, i.e. does not dominate the clinical picture, the diagnosis should be limited to that of the underlying mental or physical disorder. Moreover, the diagnosis of another sleep disorder, such as nightmare, disorder of the sleep wake schedule, sleep apnoea and nocturnal myoclonus, should be made only when these disorders lead to a reduction in the quantity or quality of sleep. However, in all of the above instances, if insomnia is one of the major complaints and is perceived as a condition in itself, the present code should be added after that of the principal diagnosis.
The present code does not apply to so-called “transient insomnia”. Transient disturbances of sleep are a normal part of everyday life. Thus, a few nights of sleeplessness related to a psychosocial stressor would not be coded here, but could be considered as part of an acute stress reaction (F43.0) or adjustment disorder (F43.2) if accompanied by other clinically significant features.
(Some citations omitted)
39 ICD-10 also includes a diagnostic criteria for “F51 Nonorganic sleep disorders” and relevantly states:
F51 Nonorganic sleep disorders
Note: A more comprehensive classification of sleep disorders is available (International classification of sleep disorders) but it should be noted that this is organized differently from ICD-10.
For some research purposes, where particularly homogeneous groups of sleep disorders are required, four or more events occurring within a 1-year period may be considered as a criterion for use of categories F51.3, F51.4, and F51.5.
F51.0 Nonorganic insomnia
A. The individual complains of difficulty falling asleep, difficulty maintaining sleep, or non-refreshing sleep.
B. The sleep disturbance occurs at least three times a week for at least 1 month.
C. The sleep disturbance results in marked personal distress or interference with personal functioning in daily living.
D. There is no known causative organic factor, such as a neurological or other medical condition, psychoactive substance use disorder, or a medication.
(Footnote omitted)
40 The International Classification of Sleep Disorders (“ICSD”) is discussed in DSM-IV at pages 556-557 (in the extract set out above) but is not itself incorporated in the Patent by reference.
41 There were eight principal witnesses, all of whom made affidavits. All except for Associate Professor Rawlin and Mr Anthony Jennings gave oral evidence and were cross-examined.
42 Dr Behi made two affidavits dated 21 August 2019 and 4 February 2020. He is a psychiatrist specialising in child, youth and family psychiatry who has 18 years of experience in the field of psychiatry. He holds a Bachelor of Medicine and Bachelor of Surgery and a Postgraduate Diploma in Psychological Medicine from the University of Wales College of Medicine. He is a Member of the Royal College of Psychiatry in the United Kingdom and a Fellow of the Royal Australian and New Zealand College of Psychiatrists (“RANZCP”).
43 Over the course of his career, he has diagnosed and treated numerous patients with non-respiratory sleep complaints including insomnia in patients of all ages. He is familiar with a range of medications that are available in Australia for the treatment of sleep complaints (both as a sole and primary complaint, or accompanying other disorders), and has many years of experience in prescribing for patients in Australia medications and treatment regimes for non-respiratory sleep complaints such as insomnia.
44 Dr Krapivensky made two affidavits dated 22 August 2019 and 31 January 2020. She is a psychiatrist who has 30 years of research and clinical experience in mental health, including non-respiratory sleep disorders such as insomnia. She holds a Bachelor of Medicine and Surgery and a PhD in Psychological Medicine in psychoendocrinology from Monash University. She has held various roles in clinical psychiatry at Alfred Hospital, Montclair Hospital, Southern Health group of hospitals, Cedar Court Private Hospital, St Vincent’s Hospital and Melbourne MediBrain Centre and MediSleep.
45 She is the founder of the Melbourne MediBrain Centre, which is a private hospital providing specialised assessment and treatment programmes addressing non-respiratory sleep disorders, including insomnia in psychiatric patients. She is also the Medical Director of MediSleep, the sleep unit she established at the Melbourne MediBrain Centre. Throughout her career, she has diagnosed and treated a significant proportion of her patients for non-respiratory sleep disorders including insomnia, and this has been the focus of her practice since 2009. She is very familiar with the range of medications that have been available in Australia for the treatment of non-respiratory sleep disorders, including insomnia, and has prescribed these medications for the treatment of such disorders throughout her career.
46 Professor Roth made two affidavits dated 5 December 2019 (“Roth 1”) and 30 January 2020 (“Roth 2”). He is a professor of sleep medicine and has approximately 50 years of clinical and research experience in sleep medicine, a speciality or subspecialty devoted to the diagnosis and therapy of sleep disturbances and disorders. He holds a Masters and a Doctorate in Psychology from the University of Cincinnati, Ohio and a Bachelor of Arts degree in Psychology from the City University of New York, Hunter College.
47 Professor Roth is the founder and Director of the Henry Ford Sleep Disorders Centre, a Professor of Internal Medicine and Psychiatry at the Wayne State University, a Clinical Professor in the Department of Psychiatry at the University of Michigan School of Medicine, and a Consulting Professor and Advisor for the Division of Public Mental Health and Public Sciences for Stanford Medicine. He estimated that 65-80% of his work in sleep medicine involved the diagnosis and management of insomnia with the main focus of his research being related to the different phenotypes of insomnia, the pathophysiology of insomnia, and the different approaches to the pharmacological management of insomnia.
48 Professor Roth has held various clinical and research roles at Howard University, the University of Cincinnati, the Sleep Research Laboratory at Veterans Administration Hospital in Cincinnati, Xavier University, the Sleep Disorders Center at Cincinnati General Hospital, and the University of Michigan School of Medicine. He has also served as President of the American Academy of Sleep Medicine, the Sleep Research Society and the National Sleep Foundation. He has authored approximately 270 articles and approximately 130 book chapters relating to insomnia, its diagnosis and its treatment and is the former Editor-in-Chief of the primary journal in the field of sleep, Sleep. He is the former Chairman of the WHO’s worldwide project on sleep and health.
49 As his qualifications are in psychology, Professor Roth does not have prescribing rights, but in his clinical practice and teaching roles he supervises fellows (in psychiatry and other disciplines) who do have prescribing rights.
50 Professor Wheatley made four affidavits dated 23 August 2019 (“Wheatley 1”), 21 November 2019 (“Wheatley 2”), 29 January 2020 (“Wheatley 3”) and 12 March 2020 (“Wheatley 4”). Wheatley 4 was prepared and affirmed approximately four weeks after the Joint Expert Reports which I refer to below. He is a Professor of Respiratory and Sleep Medicine at the University of Sydney and at Westmead Hospital in Sydney. He holds a Bachelor of Medicine with First Class Honours from the University of Sydney and a PhD in respiratory physiology, and has been admitted to the Fellowship of the Royal Australasian College of Physicians (“FRACP”).
51 Professor Wheatley currently holds several positions at Westmead Hospital including Director of the Department of Respiratory Medicine where he is responsible for the delivery of respiratory and sleep medicine services. He also is a Senior Staff Specialist Physician in the Department of Respiratory Medicine, as part of which he is appointed as a senior clinician in respiratory and sleep disorders to manage patients requiring admission to hospital with complex respiratory and sleep disorders, as well as managing outpatients with complex medical problems requiring specialist medical consultation. He is also responsible for running an outpatient clinic twice a week for patients with sleep disorders. He is the Founder and Director of the Sleep Laboratory at Westmead Hospital where he is responsible for overall management of the laboratory services with the assistance of the Sleep Services Manager, and the provision, scoring and interpretation of all sleep tests undertaken by the laboratory, as well as supervision of all teaching and research functions of the laboratory. He is also the Founder and Director of the Respiratory Failure and Sleep Disorders Service at Westmead Hospital, which undertakes clinical management of all patients with respiratory sleep disorders including obstructive sleep apnoea, central sleep apnoea and nocturnal respiratory failure.
52 Professor Wheatley is also a Director in the Department of Respiratory and Sleep Medicine at the Western Sydney Local Health District (formerly Sydney West Area Health Service), where he is the senior clinical leader for all respiratory and sleep clinical services for the local area health service comprising Westmead, Blacktown, Mount Druitt and Auburn Hospitals. The service manages patients with both acute and chronic respiratory and sleep disorders.
53 Professor Wheatley has also simultaneously held clinical academic positions in the Faculty of Medicine at the University of Sydney including as a Clinical Senior Lecturer, Clinical Associate Professor and Clinical Professor. He has taught both undergraduate and postgraduate medical students in the fields of respiratory medicine and sleep medicine. He was also involved in the development of the post-graduate FRACP training program in sleep medicine and the FRACP curriculum in Australia for sleep medicine training of respiratory physicians in the mid-1990s.
54 Professor Wheatley has also conducted research programs in both sleep and respiratory disorders and has been involved as the principal investigator of a number of research clinical trials at Westmead Hospital including in the fields of chronic insomnia and primary insomnia. Several of the clinical trials involved the assessment of new pharmaceutical agents in the treatment of chronic and primary insomnia. He has also researched and authored around 100 peer reviewed journal articles and book chapters on respiratory and sleep medicine and he has held a number of research grants for research in the field of respiratory and sleep medicine.
55 Professor Glozier made three affidavits dated 22 November 2019 (“Glozier 1”), 31 January 2020 (“Glozier 2”) and 13 March 2020 (“Glozier 3”). Glozier 3 was prepared and sworn approximately four weeks after the Joint Expert Reports. He is a Professor of Psychological Medicine at the Brain and Mind Centre and Clinical School at the University of Sydney, and is a Senior Staff Specialist in Psychiatry for the Sydney Local Health District. He has more than 20 years’ experience in psychiatry. He holds a Bachelor of Medicine and a Bachelor of Arts majoring in physiology from Oxford University, and a Bachelor of Medicine and a Bachelor of Surgery from London University, and is a member of the Royal College of Psychiatrists in the United Kingdom. He also holds a Masters in Health Policy from the London School of Economics and was awarded a PhD from London University. He is currently a Fellow of the RANZCP.
56 Professor Glozier is also a part-time Senior Staff Specialist Psychiatrist with the Sydney South West Area Health Service where he established Australia’s first sleep treatment program for public psychiatric inpatients. Since 2009 he has held academic positions at the University of Sydney as an Associate Professor and Professor and has been extensively involved in teaching medical students all aspects of psychiatry. He has also taught the Masters course on sleep medicine which is aimed at specialists and advanced trainees with a high level of prior knowledge of sleep disorders. He also has experience in conducting psychiatric clinical trials of novel medicines and behavioural and digital treatments predominantly in patients with depression, sleep and cognitive disorders. He was, or is currently, the chief investigator of three trials relating to insomnia and has undertaken significant and extensive research into insomnia and sleep disorders.
57 Professor Glozier is a member of the editorial boards for the Australian and New Zealand Journal of Psychiatry and Sleep Health and reviews academic papers for several journals including Lancet Psychiatry, Sleep, Medical Journal of Australia, British Journal of Psychiatry and Sleep Research. He has delivered insomnia and sleep health focused plenary lectures, symposia, and has been a panel member at numerous conferences including at World Sleep, American Professional Sleep Society, World Association of Psychiatry, European Sleep Research Society and Australasian Sleep Association.
58 For a period of five years, Professor Glozier ran twice-yearly courses in psychiatric diagnostic classification methods for European psychiatrists in the UK, and overseas psychiatrists in Singapore, Ethiopia, Ukraine and Sri Lanka. He was a member of a Specialist Advisory Group for the review undertaken by the Australian National Prescribing Service on insomnia treatments resulting in published insomnia treatment guidelines.
59 Before the priority date Professor Glozier worked as a Senior House Officer and Specialist Psychiatry Registrar for the Bethlem and Maudsley National Health Service (“NHS”) Trust and as a Specialist Psychiatry Registrar in Australia for the Central Sydney Area Health Service. He was also a UK Project Manager for the Classification and Assessment Division of the WHO, where he worked with Australian psychiatrists and directors of the Australian Health Classification Centres at the Institute of Health and Welfare. From 1999 to 2003, he completed a clinical training fellowship and gained a qualification in Advanced Psychiatry Training in Consultation Liaison Psychiatry. After the priority date, he also worked as a Consultant Liaison and Occupational Psychiatrist with the Kings College Hospital and London Ambulance Service NHS Trusts in London.
Associate Professor Morton Rawlin
60 Associate Professor Rawlin made two affidavits dated 22 November 2019 and 15 October 2020. He is a General Practitioner at the Macedon Medical Centre, an Associate Professor of General Practice at the University of Sydney, and the Medical Director of the Royal Flying Doctor Service (Victoria). He has more than 30 years’ experience in general medical practice. He holds a Bachelor of Medicine and a Master’s Degree of Medical Science (Clinical Epidemiology) from the University of Newcastle. He is a Fellow of the Royal Australian College of General Practitioners, the Australian College of Rural and Remote Medicine, the Mental Health Association and Advanced Rural General Practice RACGP.
61 Before the priority date he worked as a Medical Registrar doing specialist physician training at Blacktown Hospital and Hornsby Hospital and held the role of Acting Director of the Emergency Department at Mt Druitt Hospital. His career in general practice commenced in 1988 when he founded a rural general practice. Between 1998 and 2001 he was involved in a successful trial of Standards for General Practice, and he worked as a Senior Lecturer in Rural General Practice at the University of Melbourne and was a Member of the Assessment Committee of the Faculty of Medicine. Between 2000 and 2001, he worked as the Director of Medical Services at Dianella Community Health and achieved full Australian General Practice Accreditation Limited accreditation of the practice. He then began his current role as a General Practitioner at Macedon Medical Centre in 2000.
62 Between 2000 and 2001 he was also State Education Manager of Victoria for General Practice Education Australia where he managed the education of all general practitioner registrars for Victoria, and between March 2002 and April 2003 he was National Education Manager, Fellowship also for General Practice Education Australia, where he managed the education of all general practice registrars across Australia. He was also involved in the RACGP training program as both an educator and an assessor over many years and played an active role in the RACGP in various leadership capacities including as a Board Member, Vice Chair, Vice President and Chair. He has also undertaken research in the following areas: accreditation in general practice; integration in teaching medicine; promotion of rural practice in undergraduate education; standards and training of general practitioner teachers; and dermatology and mental health in general practice.
63 Mr Anthony Jennings made one affidavit dated 28 August 2019. Mr Jennings is a principal partner at an independent research firm, Intellectual Technology Services Pty Ltd, which specialises in conducting searches of commercial patent and scientific literature databases. He was retained by the respondents’ solicitors to conduct both literature and patent searches relevant to the respondents’ inventive step case.
64 Mr Manuel made one affidavit dated 15 October 2020. He is a registered pharmacist and a 50% shareholder and Director of Elements Health Care Pty Ltd, trading as Amcal+ Tuart Hill, Western Australia. He is also a 50% equity partner of Amcal+ Express Max Burswood, an Amcal pharmacy in Burswood, Western Australia. He holds a Bachelor of Pharmacy from the Western Australian Institute of Technology, now known as Curtin University. In 1985 he became a registered pharmacist and a member of the Pharmaceutical Society of Australia. He has been practicing as a proprietor pharmacist since 1989 and since 1999 has been a partner in Amcal+ Express Max Burswood.
65 In his role as a pharmacist, he has a special interest in opiate dependency treatments, aged care medication management services, compounding and healthcare innovation and technology. He has provided pharmacy advice and dispensing services to the many and varied populations within the community for a wide range of conditions, including insomnia, for over 25 years. He estimated that during this period he has personally dispensed over 1 million medicine prescriptions.
66 He is a member of the Opioid Pharmacotherapy Recruitment and Advisory Committee and a committee member of the Western Australian branch of the Pharmacy Guild of Australia (the national peak body that represents community pharmacy proprietors and provides member services).
67 Mr Manuel’s evidence was principally directed to the decision of the Secretary of the Department of Health to “down schedule” melatonin dosages of 2 mg or less from Schedule 4 to Schedule 3 with effect from 1 June 2021 and his understanding of the therapeutic indication for Circadin. He described the words “characterised by poor quality sleep” as a “blunt instrument” and “broad term” encompassing a wide range of difficulties with sleep. Ultimately, Mr Manuel’s evidence received very little attention in the parties’ submissions. I do not regard his evidence as of any real assistance in resolving the issues to be determined in this proceeding. To be clear, that is not in any sense a reflection on the quality of Mr Manuel’s evidence (none of which was challenged) or his extensive qualifications and experience as a pharmacist.
General Comment on Expert Evidence
68 As to the witnesses’ evidence more generally, I have approached the written evidence of the witnesses, but particularly that of Dr Krapivensky, Dr Behi and Professor Roth, with caution. Regrettably, parts of Dr Krapivensky’s, Dr Behi’s and Professor Roth’s written evidence were overstated, needlessly tendentious and argumentative and, in that respect, not what the Court expects to see from witnesses presenting themselves as independent experts. Parts of their written evidence commenting on the evidence of Professor Wheatley were also quite disrespectful and dismissive in tone. That said, all three witnesses were the subject of detailed and probing questioning in the oral evidence which I generally found more helpful than their written evidence even though it was at times (particularly in the case of Dr Behi) verbose and non-responsive. Professor Wheatley and Professor Glozier were both impressive witnesses who, in my opinion, did their best to assist the Court.
69 There were two expert conclaves held prior to the hearing and two concurrent sessions of expert evidence at the hearing. The first expert conclave included Dr Behi, Dr Krapivensky, Professor Roth, Professor Glozier and Professor Wheatley who together prepared a Joint Expert Report dated 12 February 2020 (“JER 1”). The second expert conclave included Professor Roth, Professor Glozier and Professor Wheatley who together prepared a Joint Expert Report dated 13 February 2020 (“JER 2”). Associate Professor Rawlin and Mr Manuel did not participate in the joint expert conclaves or contribute to the Joint Expert Reports.
THE NOTIONAL SKILLED ADDRESSEE
70 The notional skilled addressee is a legal construct and a tool of analysis framed by reference to the available evidence. This will include the patent specification and, typically, evidence of persons with knowledge and experience in the field of the invention.
71 The notional skilled addressee is a person who is likely to have a practical interest in the subject matter of the invention: Catnic Components Ltd v Hill & Smith Ltd [1982] RPC 183 at 242 per Lord Diplock. A person may have a practical interest in an invention at a number of levels. He or she may have an interest in using the products or methods of the invention, making the products of the invention, or making products used to carry out the methods of the invention either alone or in collaboration with others having such an interest: Apotex Pty Ltd v Warner-Lambert Company LLC (No 2) (2016) 122 IPR 17 at [27]. Broadly speaking, the skilled addressee will be a person who also has knowledge and experience in the field of the invention and who will bring to the reading of the relevant document the background knowledge and experience available to those working in that field.
72 It is through the eyes of the notional skilled addressee that the Patent must be construed. As French CJ observed in AstraZeneca AB v Apotex Pty Ltd (2015) 257 CLR 356 (“AstraZeneca HCA”) at [23]:
… The notional person is not an avatar for expert witnesses whose testimony is accepted by the court. It is a pale shadow of a real person – a tool of analysis which guides the court in determining, by reference to expert and other evidence, whether an invention as claimed does not involve an inventive step.
73 Neurim submitted that it was not sufficient that a person with a practical interest in the subject matter of the invention be a person skilled in the relevant art unless they also had practical knowledge and experience in the field of the invention. On this view, the notional skilled addressee is someone not only with a practical interest in the subject matter of the invention but also the relevant background knowledge and experience shared by those working in the field of the invention.
74 I accept Neurim’s submission which is consistent with authority. As Middleton J observed in Ranbaxy Laboratories Ltd v AstraZeneca AB (2013) 101 IPR 11 at [93] (“Ranbaxy Laboratories”), “[t]he first step in identifying the membership of the skilled team is to identify the field of knowledge to which the invention relates”. This is not a case in which either party suggested that the notional skilled addressee would consist of a notional team. However, I accept that it is necessary to identify the field of knowledge to which the invention relates and then identify the notional skilled addressee by reference to that body of knowledge. That approach is consistent with the High Court’s observation in Kimberly-Clark Australia Pty Ltd v Arico Trading International Pty Ltd (2001) 207 CLR 1 (“Kimberly Clark”) at [24] (per Gleeson CJ, McHugh, Gummow, Hayne and Callinan JJ) that in construing the complete specification, the Court is to place itself “in the position of some person acquainted with the surrounding circumstances as to the state of [the] art and manufacture at the time”. In Meat & Livestock Australia Ltd v Cargill, Inc (2018) 129 IPR 278 Beach J observed at [219]:
… A patent specification is addressed to those having a practical interest in the subject matter of the invention; such persons are those with practical knowledge and experience of the kind of work in which the invention is intended to be used.
(Emphasis added)
75 It is common ground between the parties that Dr Behi, Dr Krapivensky, and Professor Glozier are skilled addressees with a practical interest in and knowledge of the field of primary insomnia and the diagnosis and treatment of that condition. There is a significant debate between the parties as to whether Professor Wheatley and Professor Roth are properly regarded as skilled addressees. I will return to this question shortly, and merely note at this stage that Neurim contends that the notional skilled addressee is a clinician with expertise in primary insomnia and the diagnostic guidelines used in the diagnosis of primary insomnia, including, as at the priority date, DSM-IV and ICD-10. Neurim contends that Professor Wheatley is not representative of the notional skilled addressee because the focus of his clinical and research work is on the diagnosis and treatment of insomnia due to respiratory sleep disorders in patients that do not have primary insomnia. The respondents contended that Professor Roth is a psychologist who is not a prescriber of pharmacological treatments who is not representative of the notional skilled addressee. They also said that he was “over-qualified”.
76 The experts who participated in JER 1 were asked to express their views as to the identity of the person skilled in the art at the priority date. The experts agreed that the person skilled in the field of primary insomnia and likely to have a practical interest in the subject matter of the Patent would have knowledge and experience in taking a history of sleep disturbances and identifying causes and associations of such disturbances in the course of making a diagnosis of primary insomnia. They also agreed the person would have experience, knowledge or a research interest in the psychopharmacology of sleep and its disorders, and an ability to understand the diagnosis of primary insomnia specifically in relation to DSM-IV. Relevantly, the experts agreed that primary insomnia in the patent is a reference to that term as it appears in DSM-IV.
77 The experts did not agree, however, on the role of other classification systems, and specifically the extent to which ICSD was translatable to the diagnosis of primary insomnia in the context of the Patent. The main area of disagreement consequently was whether a person familiar with ICSD but not DSM-IV would be a person skilled in the art. Dr Behi stated that where a person did not recognise or understand the concept of non-restorative sleep in the context of DSM-IV, such a person could not be skilled in the art because the Patent specifically requires an understanding of that term to make a diagnosis. Dr Krapivensky and Professor Roth were of largely the same view, and each pointed out that while different nosologies were “translatable”, that translation would require familiarity with DSM-IV in the first place. Dr Krapivensky also considered that such a translation would be highly subjective.
78 Professor Glozier held the view that a person who understood the relevant diagnoses in ICSD that are subsumed by a diagnosis of primary insomnia in DSM-IV would be a person skilled in the art, and pointed to the fact that DSM-IV specifically refers to ICSD and enables the translation between the two nosologies. Professor Wheatley held the same view, and asserted that a sleep physician who embodied the characteristics agreed upon by the group would be able to fully understand the diagnosis of primary insomnia in DSM-IV and would be a person skilled in the art.
Criticism of Professor Wheatley
79 Professor Wheatley was heavily criticised in Neurim’s submissions in relation to various corrections and qualifications he made to views expressed by him in JER 1. It will be necessary to refer to some of the differences between those views and the contents of his supplementary affidavit where relevant. Insofar as the identity of the person skilled in the art is concerned, Professor Wheatley did not purport to correct or qualify any of the information contained in response to Q1 of JER 1. However, in his affidavit evidence, he did make a number of statements which Neurim submitted showed that Professor Wheatley was “plainly not appropriately qualified to give evidence as the notional skilled addressee”. There were three statements in Professor Wheatley’s affidavit evidence that Neurim focused on in support of that submission:
(a) while Professor Wheatley was aware of DSM-IV and ICD-10, he did not refer to them in his clinical practice for the diagnosis and management of sleep disorders;
(b) non-restorative sleep is not a technical term Professor Wheatley was familiar with or a concept he used in diagnosing patients; and
(c) Professor Wheatley did not know what non-restorative sleep was from either the Patent or his own background knowledge.
80 Neurim submitted that a clinician who does not use DSM-IV or ICD-10, and who does not understand terms that are used in those nosologies, cannot give admissible evidence about a patent that defines the invention by reference to those terms and, in those circumstances, Professor Wheatley’s evidence should be “wholly disregarded”. Neurim submitted that, alternatively, if his evidence was to be admitted, it should be given no weight. It was also submitted that the circumstances in which his supplementary affidavit came to be filed demonstrated that he did not have the necessary expertise and that he was “out of his depth in the task he was asked to perform”.
81 I previously referred to Professor Wheatley’s qualifications and experience but there are certain matters that, in the present context, require emphasis. According to Professor Wheatley, all respiratory physicians in Australia have basic training in sleep medicine. To become a sleep physician, respiratory physicians undertake a further one year post-graduate qualification in sleep medicine. On completion of this further qualification, the physician will be referred to as a respiratory and sleep physician. Professor Wheatley said that while it was possible to undertake specialist medical training only in sleep medicine, and not first become qualified as a respiratory physician, he was not aware of any sleep physician within Australia, at the priority date, or at the time of giving his evidence, who was not also a respiratory physician. Professor Wheatley was involved in the development of a post-graduate FRACP curriculum for sleep medicine training of respiratory physicians in the mid-1990s. The FRACP curriculum spans respiratory and non-respiratory sleep disorders and includes training in diagnosis and management of insomnia including primary insomnia. On that basis, Professor Wheatley considered that respiratory physicians with specialist training in sleep will have an interest in the subject matter of the Patent.
82 While Professor Wheatley specialises in the clinical management of patients with respiratory sleep disorders including obstructive sleep apnoea, central sleep apnoea and nocturnal respiratory failure, he also treats insomnia patients including those suffering from primary insomnia, which he defined as insomnia that is not caused by any known underlying medical condition or drug use.
83 The nosology with which Professor Wheatley was most familiar is ICSD which is, as I have already noted, referred to in DSM-IV. Professor Wheatley explained that his training and practice in sleep medicine was based around ICSD as well as the text on sleep medicine co-edited by Professor Roth, Principles and Practice of Sleep Medicine, 3rd Edition, published in 2000 (“Sleep Medicine”). In its opening submissions, Neurim submitted that Sleep Medicine was a text widely used in Australia which reflected the common general knowledge. Professor Roth’s evidence (relied on by Neurim) was that Sleep Medicine is and was at the priority date, the leading textbook in the field and he would expect any clinician working in sleep medicine to be familiar with it. Dr Behi was not familiar with Sleep Medicine. Dr Krapivensky’s evidence did not disclose whether she was familiar with Sleep Medicine but there is no reason to think that she was.
84 Whether or not Sleep Medicine was common general knowledge at the priority date can be put to the one side for the moment. What is important for present purposes is that the leading textbook on sleep medicine in Australia at the priority date included a chapter on the subject of primary insomnia (Chapter 55) which it approached from the perspective of the various subgroups recognised in ICSD that empirically make up most of what DSM-IV called primary insomnia.
85 Sleep Medicine also includes a chapter titled “Evaluation and Management of Insomnia: An Overview” (Chapter 53), which the authors (Frank J Zorick and James K Walsh) commence with a discussion of the definition of insomnia. They state:
The [ICSD] defines insomnia as “difficulty in initiating and/or maintaining sleep.” Many variations on this definition have been proposed or used in research, and a consensus definition of insomnia has not been reached. A recent working group of the National Center for Sleep Disorders Research stated, “Insomnia is an experience of inadequate or poor quality sleep characterized by one or more of the following: difficulty falling asleep, difficulty maintaining sleep, waking up too early in the morning, nonrefreshing sleep.” Insomnia also involves daytime consequences, such as “tiredness, lack of energy, difficulty concentrating, irritability.”
(Footnotes omitted)
86 Under the heading “Causes of Insomnia” the authors state:
The most important concept is that insomnia is a complaint and a symptom and is never the diagnosis. Except for idiopathic (or primary) insomnia and sleep state misperception, this sleep symptom will always be found secondary to a medical, psychiatric, circadian, sleep, behavioral, or environmental disorder. Table 53-2 lists the major differential diagnostic categories of insomnia. The clinician must have a working familiarity with the major causes of insomnia. The primary goal of this section is to acquaint the reader with this conceptual framework so that treatment is rational and planned according to a reasoned diagnosis after a comprehensive evaluation. In addition, the clinician must develop a continuing relationship with the patient. Sometimes, with further interaction and an ongoing evaluation of the patient—in particular, the patient's response to treatment efforts—the diagnostic formulation may change. It is imperative to understand that two or more diagnoses may be relevant and require treatment in the insomnia patient.
(Footnotes omitted)
87 Table 53-2 is a list of various disorders discussed in other sections of the textbook including psychiatric disorders, medical disorders, neurological disorders, circadian rhythm disorders, and primary sleep disorders including what the authors describe as “idiopathic” (or primary) insomnia. The authors continue:
To summarize, during the assessment of the insomnia patient, the clinician identifies a working medical diagnosis according to the criteria in the [ICSD] and the cognitive/behavioral framework within which the sleep problem developed. It is important to determine the presence of diagnoses, such as restless legs syndrome, sleep apnea, major depression, or movement disorders, that will require specific medical treatment. Likewise, chronic insomnia requires a behavioral analysis to address the precipitating and perpetuating factors. The psychiatric diagnosis is identified according to the criteria of the DSM-IV after a psychiatric history and mental status examination are conducted. Each evaluative system improves the accuracy of the assessment, and a specific diagnosis (or diagnoses) improves the effectiveness of the treatment plan.
(Footnotes omitted)
88 The opening paragraphs of Chapter 55 point to the existence of a controversy as to which of DSM-IV and ICSD “makes better empirical sense”. The author (Peter J Hauri) observed:
Insomnia may be the basic, root problem in some patients rather than a symptom of some other disease. Specifically, some types of insomnias are not caused by problems such as anxiety, depression, pain, allergy, or restless legs syndrome. For these types of free-standing insomnia, the word primary is used in the [DSM-IV]. This does not imply that such patients are totally free of any medical or psychiatric disorders. It simply means that as far as can be determined, these other disorders are probably not involved in the cause of the insomnia.
The [ICSD] does not recognize a category of primary insomnia, but discusses three free-standing insomnia subgroups: psychophysiological insomnia, sleep state misperception, and idiopathic insomnia. These three ICSD subgroups empirically make up most of what DSM-IV calls primary insomnia. There is controversy about which classification makes better empirical sense.
(Footnotes omitted)
89 The author also observed:
It will be a matter of clinical judgment and further research to determine whether we are dealing with three separate and distinct subcategories of insomnia, as ICSD implies, or with three general dimensions along which all patients with primary insomnia vary, as DSM-IV maintains. However, the remainder of this chapter is organized according to the ICSD point of view.
(Footnotes omitted)
90 In my view, it is highly significant that the chapter on primary insomnia in what the parties accept was the leading sleep medicine textbook is written around the classification of sleep disorders used by Professor Wheatley.
91 Professor Wheatley gave evidence that as at August 2001, the field of insomnia was in a state of flux with respect to the three nosologies (i.e., DSM-IV, ICD-10 and ICSD) and that there was no requirement to use any one nosology over the other for the diagnosis of insomnia and primary insomnia. I accept that evidence. The inference I draw from Professor Wheatley’s evidence is that sleep physicians in Australia were in August 2001 unlikely to be using DSM-IV for the purpose of diagnosing and treating insomnia because they were likely to have come from a background in respiratory medicine (as had Professor Wheatley) rather than psychiatry. Similarly, psychiatrists diagnosing and treating insomnia in Australia in August 2001 were more likely to use DSM-IV than ICSD. That does not mean that in diagnosing and treating insomnia psychiatrists and sleep physicians were practicing in separate fields. In relation to the diagnosis and treatment of insomnia, including primary insomnia, they were working in the field of sleep medicine. Both were qualified to diagnose and treat primary insomnia.
92 Professor Glozier gave evidence that most clinicians who practice in the area of sleep (including psychiatrists, psychologists and sleep physicians) are familiar with and use ICSD. He said that ICSD, published by the American Academy of Sleep Medicine, is designed to be used and referenced by those with different clinical backgrounds who practice in the area of sleep. I accept that evidence. I note that an article co-authored by Professor Roth in 1994 in the journal Sleep entitled “Clinical Diagnoses in 216 Insomnia Patients Using the International Classification of Sleep Disorders (ICSD), DSM-IV and ICD-10 Categories” states that “[m]any sleep disorders clinicians have begun to use the [ICSD] since its introduction in 1991”.
93 Professor Glozier rejected the suggestion that psychiatrists as part of their training, were lectured on the topic of non-restorative sleep. In fact, his evidence was that the vast majority of his colleagues had no idea how to diagnose primary insomnia and that he was currently involved in the preparation of training materials for the RANZCP which, as I understood his evidence, would seek to fill that gap in their training. However, Professor Glozier agreed with Dr Krapivensky and Dr Behi that the training of psychiatrists placed considerable emphasis on patient communication, the eliciting of patient history, and the identification of matters through that process which are clinically significant. Their evidence indicates that these skills are of particular importance in the practice of psychiatry.
94 It was put to Professor Wheatley in cross-examination, and he agreed, that he was not trained in the diagnosis of primary insomnia characterised by non-restorative sleep as at August 2001. In fairness to Professor Wheatley, I doubt very much whether either Dr Krapivensky or Dr Behi had been trained in the diagnosis of that condition at the priority date. First, as Professor Glozier observed (and with whom Professor Roth agreed) the relevant diagnosis is primary insomnia. Non-restorative sleep is only a symptom of that condition as defined by DSM-IV. Secondly, and more importantly, Professor Glozier gave oral evidence that in his psychiatric training, only one full, or a half lecture, would have been dedicated to sleep broadly with primary insomnia as a “smaller component” of that. When Dr Krapivensky was asked whether she agreed with that statement, she could not recall the amount of training that she had in relation to insomnia or primary insomnia, and her response was not indicative of any definitive recollection of specific training dealing with primary insomnia characterised by non-restorative sleep. In any event, I find that Professor Wheatley was trained and experienced in the diagnosis and treatment of primary insomnia at the priority date. The fact that this training was not based on DSM-IV but focused on Sleep Medicine and the ICSD is not inconsistent with that finding.
95 It was also suggested by Neurim that Professor Wheatley’s clinical work is primarily concerned with objective criteria, and that, by implication, he did not have the experience required to take a detailed patient history of the kind that was necessary to make a diagnosis of primary insomnia. In my view, this was answered quite convincingly by Professor Wheatley who said:
PROF WHEATLEY: So I – I wouldn’t agree with you on that. I think training in internal medicine also involves taking of a detailed history to – in the first instance, to assess the symptoms that the patient is presenting. Those symptoms, as Professor Glozier has stated, have to be determined whether they’re significant enough or relevant enough to continue on the path to formulating a diagnosis, but history-taking is a large and important component of – of internal medicine in general and in both respiratory and sleep medicine specifically. That’s always followed up by physical examination of – of relevant systems to assist in finding further evidence for a diagnosis or against differential diagnoses and in most cases would be followed up with relevant investigations that may, again, assist in formulating that diagnosis. So that’s general clinical practice for physicians.
MR SHAVIN: In the nature of that clinical practice, the way in which you extract the history will vary with the area in which you’re investigating a condition with a patient, won’t it? So that if you’re investigating a patient that may have an issue with internal medicine – may differ from a patient that has got a psychiatric condition.
PROF WHEATLEY: Well, in my own field, if I’m investigating a patient with asthma, that will have a series of questions that you follow. If I’m investigating a patient with a parasomnia, that would have a different path and set of questions that you would follow, and that’s where training comes from. I don’t investigate people with psychiatric disorders, so I’m not trained to make those diagnoses. I’m trained enough to elicit symptoms that would allow me to be concerned that that is a diagnosis, at which point, it would be more appropriate to refer a patient on for specialist diagnosis with a psychiatrist.
96 I accept Dr Behi’s evidence that psychiatrists are trained intensively in the skill of ascertaining and interpreting subjective experience which travels beyond what is imparted in general medical training. However, it does not follow that the person skilled in the art must be a psychiatrist. Further, neither Dr Behi or Dr Krapivensky have any particular expertise in sleep medicine beyond that of most other psychiatrists who routinely make use of DSM-IV in the diagnosis of psychiatric disorders. In contrast to this, Professor Wheatley has specialist experience in sleep medicine.
97 In 2013, after the priority date, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (“DSM-5”) was published. The section on sleep-wake disorders in DSM-5 includes diagnostic criteria for Insomnia Disorder and distinguishes between mental health and general medical clinicians who are not experts in sleep medicine, and the sleep specialist community. DSM-5 states at p 362:
DSM-IV represented an effort to simplify sleep-wake disorders classification and thus aggregated diagnoses under broader, less differentiated labels. At the other pole, the [ICSD] 2nd Edition (ICSD-2) elaborated numerous diagnostic subtypes. DSM-IV was prepared for use by mental health and general medical clinicians who are not experts in sleep medicine. ICSD-2 reflected the science and opinions of the sleep specialist community and was prepared for use by specialists.
98 That statement tends to confirm the strong impression conveyed by the evidence more generally that a clinician’s expertise in sleep medicine, in 2013 and at the priority date, did not depend on their familiarity with DSM-IV.
99 Professor Wheatley gave evidence that prior to August 2001, and still today, he approaches the diagnosis of insomnia by conducting a patient medical history, including the patient’s sleep history, to ascertain what he can as to the patient’s sleep routine, sleep complaint, and possible causes of insomnia. He described his approach as consistent with the teachings in Sleep Medicine, which in Chapter 53 (“Evaluation and Management of Insomnia”) states:
The first and most important aspect of the evaluation is the clinical interview and sleep history (Table 53-1). From this initial encounter with the patient, the clinician develops the differential diagnosis and treatment plan. The nature and development of the sleep problem must be elicited. Attention must be paid to daytime symptoms as well as to the complaints about sleep.
100 Professor Roth’s evidence was clear that the hour to hour and a half that Dr Behi and Dr Krapivensky indicated they would typically set aside to take a patient’s history is not required to determine whether a patient suffering from primary insomnia had experienced non-restorative sleep. According to Professor Roth, while taking a psychiatric history and a sleep history can take an hour and a half, determining whether the patient is experiencing non-restorative sleep can be done relatively easily including through the use of a questionnaire.
101 The implication of Dr Krapivensky’s and Dr Behi’s evidence was that determining whether a patient was experiencing non-restorative sleep required the skills and experience of a psychiatrist rather than those of a respiratory and sleep physician such as Professor Wheatley. I do not think that is correct, even though the Patent approaches a diagnosis of primary insomnia through the lens of the particular nosologies (DSM-IV and ICD-10) quoted in the body of the specification and also incorporated by reference.
102 The question raised by Neurim’s submission is whether a clinician trained in the field of sleep medicine, including in the diagnosis and treatment of primary insomnia, who is not familiar with either of those two psychiatric nosologies, but who is trained in a different nosology (i.e. ICSD) should not be considered a skilled addressee. As previously mentioned, this is ultimately a question for the Court rather than any expert witness.
103 In her first affidavit Dr Krapivensky stated that she considered the Patent was aimed at psychiatrists and sleep physicians with clinical experience in diagnosing and treating non-respiratory sleep disorders. In her oral evidence, she agreed with the proposition that sleep physicians in Australia are able to and do diagnose and treat non-respiratory sleep disorders. She also accepted that a clinic which she had established in Melbourne employed a prominent sleep physician (Dr Schachter) who had many years of experience as a sleep and respiratory physician with expertise in the diagnosis and treatment of all sleep disorders.
104 The field of sleep medicine in Australia therefore includes clinicians with quite different backgrounds, including those with training and experience in sleep medicine (such as Professor Wheatley and Dr Schachter) and those with training and experience in psychiatry (such as Dr Behi, Dr Krapivensky and Professor Glozier).
105 Neurim sought to confine the field of the invention to the treatment of primary insomnia (as defined by DSM-IV or nonorganic insomnia defined by ICD-10) when characterised by non-restorative sleep (a term not used in ICD-10). While that language is used to describe the field of the invention in the first paragraph of the Patent, I think that is more in the nature of a description of the invention rather than the relevant field. The relevant field is in my opinion the diagnosis and treatment of sleeping disorders, which will include primary insomnia. The field should not be defined by the specific symptoms of the specific condition to be treated as defined by a particular nosology, nor should it be defined by the particular agent (i.e. “melatonin or certain other compounds”) used in the course of such treatment.
106 Professor Roth contended in his affidavit evidence that the Patent is not directed to clinicians who have not studied or practiced extensively in the area of primary insomnia. I do not accept that proposition. Professor Glozier’s evidence, which I accept, was that in Australia psychiatrists rarely saw patients with insomnia that was not comorbid with a psychiatric disorder. There was no evidence given by either Dr Behi or Dr Krapivensky that would lead me to conclude that either of them had studied or practiced extensively in the area of primary insomnia at the priority date, or that they had any greater training or experience in the diagnosis or treatment of patients suffering from primary insomnia than Professor Wheatley.
107 There were parts of Dr Behi’s and Dr Krapivensky’s evidence which suggested that they were regularly treating patients who they diagnosed with primary insomnia. Given Dr Behi’s background, that is unlikely to have been correct as at the priority date even if it was correct at the time he gave his evidence. To the extent that Dr Krapivensky’s evidence suggested that she was regularly diagnosing and treating patients for primary insomnia at the priority date, I did not find her evidence persuasive and, in any event, I would not regard it as representative of psychiatrists in general. On this point, I prefer the evidence of Professor Glozier which leads me to conclude that at the priority date there were relatively few (if any) psychiatrists in Australia who were likely to have in Professor Roth’s words, “studied or practiced extensively in the area of primary insomnia”.
108 There are three further points to make concerning Neurim’s challenge to Professor Wheatley’s qualifications.
109 First, as to Professor Wheatley’s lack of familiarity with DSM-IV and ICD-10, in my opinion the Patent does not expressly or impliedly assume that the reader will be familiar with the content of those nosologies. Although they are both quoted from and incorporated by reference, there is nothing in the Patent which would suggest that sleep physicians would not be able to understand and perform the invention. The fact that they may need to read and interpret relevant parts of DSM-IV and ICD-10 to understand the invention does not preclude them being skilled addressees. In my opinion, the Patent is agnostic as to the particular background (i.e. psychiatrist or sleep physician) of the skilled addressee. I do not accept Professor Roth’s evidence (as stated in JER 1) that “a person skilled in the art must fully understand [DSM-IV]”. According to Sleep Medicine, the three free-standing ICSD insomnia subgroups empirically make up most of what DSM-IV calls primary insomnia. I find that a physician with training and experience in sleep disorders who used ICSD to diagnose sleep disorders would be able to use DSM-IV as required by the Patent, even if they had difficulty with some of the concepts and terminology used in that nosology, and even though they used ICSD rather than DSM-IV in clinical practice.
110 Secondly, in my opinion, Professor Wheatley’s lack of familiarity with DSM-IV and ICD-10 and the concept of “non-restorative sleep” does not mean that he cannot be a skilled addressee. Professor Wheatley was cross-examined in relation to evidence given by him in Wheatley 4 regarding his answers to questions in the JERs as follows:
MR SHAVIN: … Now, do you accept from what you’ve learned in the course of preparing for this proceeding that non-restorative sleep is a diagnosis that is identified in the DSM-IV?
PROF WHEATLEY: So as of today and in preparing for this proceedings, yes, non-restorative sleep is a concept that comes from the DSM-IV.
MR SHAVIN: Yes. And does it follow then that as at August 2001 you did not have as part of your professional background which was extensive in many areas an ability to understand the diagnosis of primary insomnia specifically in relation to the DSM-IV?
PROF WHEATLEY: As at August 2001 I did not have an understanding of the non-restorative sleep and primary insomnia as in the DSM-IV, but based on my training as a sleep physician if I had been referred to that document I would have had an ability to understand the concepts that are expressed in that.
111 I accept that evidence. DSM-IV defines a complaint of non-restorative sleep as a “feeling that … sleep was restless, light, or of poor quality”. Beyond that, DSM-IV gives no meaningful guidance as to the meaning of the term “non-restorative sleep”. The difficulty which Professor Wheatley has with the concept of “non-restorative sleep” is not based on any lack of understanding of what those words convey, but with the difficulties involved in disentangling non-restorative sleep as an independent complaint, distinct from sleep complaints attributable to difficulty initiating and maintaining sleep. I will return to the evidence on this topic when considering the respondents’ complaints about the language of the claim.
112 Moreover, the concept of the notional skilled addressee is a legal fiction and a tool of analysis. There will be some fields of scientific knowledge where those with a practical interest in the subject matter of the invention may come from a variety of different backgrounds. One way in which patent law has accommodated this possibility is to recognise that the skilled addressee may be a team. However, another approach involves recognising that the notional person skilled in the relevant art has expertise and experience drawn from different backgrounds, even though in the real world, those working in the field may have been differently trained and, therefore, possess different background knowledge. The point is taken up in Terrell on the Law of Patents (19th ed, Sweet & Maxwell, 2020) at para 8-34 where the learned authors acknowledge that:
There may be more than one relevant art or skill and therefore more than one person skilled in the art. In such cases, if the invention is obvious to a person skilled in the art of any one of those skills, then the invention is obvious, for it would otherwise impede a class of person who found it obvious.
113 The authorities cited by the authors include Inhale Therapeutic Systems Inc. v Quadrant Healthcare Plc [2002] RPC 21 in which the invention involved improvements in the stabilisation of proteins and other biologically active materials by incorporating them in glass. The claims of the patent expressly excluded the use of freeze drying methods to perform the invention, but included the use of spray drying. The patentee submitted that, since freeze drying was by far the more widely used technique in the field of application of the invention, the person skilled in the art would have only a slight acquaintance with spray drying techniques, and because the task of considering a solution to stability problems would be the responsibility of one individual, the person skilled in the art would be an expert in the field of freeze drying methods and no other. In rejecting this submission Laddie J said at [42]:
…In some cases a patent claim may cover a wide field so that some parts of it will be obvious to the notional skilled person in one field and other parts will be obvious to the notional skilled person in another. This is not unfair to the patentee, as Mr Waugh suggests, but simply a reflection of the fact that the scope of protection sought is wide. I accept, of course, that in some cases there will be invention in marrying together concepts from two unrelated arts, but that is not what Mr Carr is arguing for here. He says that the notional skilled worker in the art, whether he comes from the freeze-drying field or the spray-drying field, would find it obvious to work within the wide limits of the claim. When considering what would be obvious to the notional uninventive but skilled spray-dryer one must have in mind what would be common general knowledge in that field. Likewise when one is considering what is obvious to the notional uninventive but skilled freeze-dryer…
His Lordship’s analysis was approved in Schlumberger Holdings Ltd v Electromagnetic Geoservices AS [2010] RPC 33 at [53] per Jacob LJ (with whom Sullivan and Waller LJJ agreed).
114 In the present case, the claims do not cover what I would regard as a wide field. However, they do cover a field in which clinicians from different backgrounds work. Each has a practical interest in the subject matter of the invention even though not all of them use a nosology that is incorporated by reference into the Patent or approach the diagnosis and treatment of insomnia in precisely the same way that a psychiatrist would. In determining which clinicians would have had a practical interest in the subject matter of the Patent and practical knowledge and experience in the area in which the invention was intended to be used, it is necessary to focus not on the particular nosology which was used by them (DSM-IV, ICD-10 or ICSD), but on the area in which they trained and worked. On this basis the skilled addressee might be either a sleep physician or a psychiatrist.
115 Neurim submitted that, to the extent Professor Wheatley had practiced as a sleep physician and not a sleep respiratory physician, he was a person “uniquely lacking knowledge in the DSM-IV and the ICD-10”. As I understood this submission, there are sleep physicians who are familiar with DSM-IV or ICD-10 who may be considered skilled addressees, but Professor Wheatley is not one of them. In so far as Neurim is taken as suggesting that Professor Wheatley’s lack of familiarity with either DSM-IV or ICD-10 was atypical of sleep physicians more generally, I do not accept that submission. The evidence indicates that sleep physicians are trained in ICSD rather than DSM-IV or ICD-10. In any event, for reasons I have explained, since DSM-IV and ICD-10 are incorporated into the Patent by reference, it is not essential that the skilled addressee be familiar with either of those nosologies. Professor Wheatley was trained as at the priority date in ICSD and the Sleep Medicine text book. I reject Neurim’s submission that Professor Wheatley is not qualified by his training and experience to give admissible evidence in relation to the Patent whether on the basis that he is not a skilled addressee or that he lacks training and experience in either DSM-IV or ICD-10.
116 Professor Roth, who Neurim says is a skilled addressee, is a psychologist with expertise in sleep medicine. He is not a psychiatrist or a sleep physician. The respondents submitted that Professor Roth could not be a person skilled in the art because he was not licensed to prescribe medications either in Australia or elsewhere (a fact not disputed by Professor Roth). However, I do not think that precludes the Court from recognising that Professor Roth is a person with both a practical interest in the subject matter of the Patent and extensive knowledge and experience in the field of sleep medicine. Professor Glozier gave evidence that in Australia, sleep difficulties such as insomnia were primarily managed by general practitioners but that, by August 2001, there were a number of specialist sleep physicians (which he described as a sub-specialty of respiratory medicine), some psychologists and a few psychiatrists treating patients with sleep difficulties.
117 Moreover, as I have mentioned, the respondents’ principal witness, Professor Wheatley, was trained in sleep medicine using Professor Roth’s text, Sleep Medicine, and was himself overseeing the training of other sleep physicians in Australia using the same text. It is clear that Professor Roth is regarded as one of the world’s leading researchers in the field. In fact, in their closing submissions, the respondents referred to him as “a uniquely eminent researcher in sleep medicine with a vast knowledge of the literature”. But they also submitted that he was “overqualified” on the basis that his knowledge and experience in sleep medicine would exceed that of clinicians diagnosing and treating sleep disorders in Australia at the priority date. That may well be the case, and if so, may have implications for the weight to be given to some of his evidence. However, I consider Professor Roth is a skilled addressee and is able to give admissible evidence as to the state of the relevant art and the common general knowledge at the priority date. What weight is given to his evidence is another matter.
118 The common general knowledge is a general body of knowledge attributed to the hypothetical non-inventive skilled person or team. In Minnesota Mining and Manufacturing Company v Beiersdorf (Australia) Limited (1980) 144 CLR 253 (“3M”), Aickin J (Barwick CJ, Stephen, Mason and Wilson JJ agreeing) at 292 referred to common general knowledge as “the background knowledge and experience which is available to all in the trade in considering the making of new products, or the making of improvements in old, and it must be treated as being used by an individual as a general body of knowledge”. It is “knowledge actually known or used by skilled addressees generally, or accepted by “the bulk of those who are engaged in the particular art””: Ranbaxy Laboratories, Middleton J at [215] citing British Acoustic Films Ltd v Nettlefold Productions (1936) 53 RPC 221 at 250 (“British Acoustic Films”).
119 Knowledge is not common general knowledge unless it is sufficiently widely known or used to become generally accepted and assimilated into the minds of people skilled in the relevant art: see Gilead Sciences Pty Ltd v Idenix Pharmaceuticals LLC (2016) 117 IPR 252 at [210]-[214] (“Gilead”) where Jagot J referred to some of the leading authorities including, Aktiebolaget Hässle v Alphapharm Pty Ltd (2002) 212 CLR 411 at [31] (“Alphapharm”). It will include publications to which the skilled addressee would refer as a matter of course: ICI Chemicals & Polymers Ltd v Lubrizol Corporation Inc (1999) 45 IPR 577 at [112] per Emmett J. However, information does not become common general knowledge merely because it might appear in a journal even if it is widely read by persons in the art: Ranbaxy Laboratories at [217] per Middleton J citing (inter alia) Eli Lilly & Co Ltd v Apotex Pty Ltd (2013) 100 IPR 451 at [468]; Wake Forest University Health Sciences v Smith & Nephew Pty Ltd (No 2) (2011) 92 IPR 496 at [96], General Tire & Rubber Co v Firestone Tyre & Rubber Co Ltd [1972] RPC 457 (“General Tire”) at 482-3, British Acoustic Films at 250.
120 Difficulties arise in relation to the determination of the common general knowledge in this case due to the way each side has conducted its case. In its written submissions, Neurim contended that Sleep Medicine was the leading textbook in the field and reflected the common general knowledge. Further, as I have previously pointed out, it relied on evidence from Professor Roth that he would expect any clinician working in the field of sleep medicine to be familiar with this book. The respondents agreed that Sleep Medicine was common general knowledge. Despite this, there was no evidence to indicate that any of the psychiatrists who gave evidence were familiar with Sleep Medicine at the priority date. That suggests that either the psychiatrists were not persons skilled in the relevant art or that Sleep Medicine was not common general knowledge. The only witness familiar with Professor Roth’s book (aside from himself) as at the priority date was Professor Wheatley. As already pointed out, the chapter in Sleep Medicine on primary insomnia analyses the topic by reference to ICSD.
121 It is questionable whether the evidence supports a finding that Sleep Medicine was common general knowledge at the priority date if, as the parties all agreed, the three psychiatrists who gave evidence are skilled addressees. That said, the case was conducted by both parties on the basis that Sleep Medicine was common general knowledge at the priority date, and I propose to decide the case on that footing. The common general knowledge includes the information appearing in the following chapters:
Chapter 31: “Melatonin in the Regulation of Sleep and Circadian Rhythms”;
Chapter 32: “Hypnotics: Basic Mechanisms and Pharmacology”;
Chapter 33: “Hypnotics: Efficacy and Adverse Effects”;
Chapter 45: “Use of Clinical Tools and Tests in Sleep Medicine”;
Chapter 53: “Evaluation and Management of Insomnia: An Overview”; and
Chapter 55: “Primary Insomnia”.
122 Neurim submitted that at the priority date the notional skilled addressee would also have a working understanding of DSM-IV and ICD-10. It also noted in its submissions that the experts agreed that “[t]he clinical diagnostic process in Australia was broadly comparable to the rest of the world and utilised predominantly the [DSM-IV] and ICSD rather than ICD-10, though all three were translatable to one another in terms of diagnostic criteria”. That submission references an agreement referred to in JER 2 between Professors Roth, Glozier and Wheatley.
123 Professor Roth, Professor Wheatley, and the three psychiatrists were aware of the existence of DSM-IV and ICD-10 before the priority date. Professor Roth, Dr Krapivensky and Dr Behi each used DSM-IV in their clinical practice. Professor Glozier indicated that while he was aware of DSM-IV and ICD-10 (as well as ICSD), he did not and does not diagnose patients with strict adherence to classification systems, unless asked to for legal purposes. Professor Wheatley knew of but did not use DSM-IV. He explained that he did not use any of the classification systems as day to day diagnostic tools, but, as I have set out above, he was familiar with ICSD which he used in training and practice. Although it is clear from the evidence DSM-IV was widely used by psychiatrists who would routinely refer to it in the course of their clinical practice, it was not used by Professor Wheatley and was, I find, unlikely to have been used by sleep physicians whose training and experience was more likely to have focused on the ICSD and Sleep Medicine.
124 Professor Glozier and Dr Behi used ICD-10 in their clinical practice to varying degrees, but neither Dr Krapivensky nor Professor Wheatley did so.
125 I find that the common general knowledge included a knowledge of the existence of DSM-IV, ICD-10 and ICSD and, as is apparent from a reading of Sleep Medicine, some understanding of the manner in which these nosologies classified different types of insomnia as well as some of the terminology used in them when doing so.
126 Chapter 45 of Sleep Medicine includes a section entitled “Evaluation of Insomnia” which refers to “the complaint of inadequate, insufficient or nonrestorative sleep”. Similarly, Chapter 53 refers to the ICSD definition of insomnia as “difficulty in initiating and/or maintaining sleep” but notes that a consensus definition of insomnia has not been reached. It also makes reference to a paper prepared by a working group of the National Center for Sleep Disorders Research and includes the following quotation from that paper:
Insomnia is an experience of inadequate or poor quality sleep characterized by one or more of the following: difficulty falling asleep, difficulty maintaining sleep, waking up too early in the morning, nonrefreshing sleep.
127 Chapter 55 entitled “Primary Insomnia” (which I have previously discussed) refers to the use of the word “primary” in the DSM-IV when describing insomnia that is not caused by another medical or psychiatric condition. However, as I have set out above, the author also notes that the ICSD does not recognise a category of insomnia called primary insomnia, but instead discloses three subgroups of “free-standing insomnia” that empirically make up most of what DSM-IV calls primary insomnia.
128 It follows that the person skilled in the art would have some knowledge of each of the three nosologies (DSM-IV, ICD-10 and ICSD) derived from their knowledge of Sleep Medicine together with a detailed familiarity with any nosology that they used in the course of their clinical work. For psychiatrists working in Australia this would most likely be DSM-IV, while sleep physicians would be more likely to use the ICSD. That said, the question whether DSM-IV or ICD-10 was common general knowledge is, in my opinion, of little significance to the construction issues arising in the case because relevant parts of those nosologies are referred to in the Patent and each is, in any event, incorporated by reference. Accordingly, the notional skilled addressee’s knowledge and understanding of the invention described in the Patent and, in particular, at least some of the terminology used, is assisted by the disclosure of each of those documents, regardless of whether they were common general knowledge at the priority date.
129 There was a measure of agreement between the experts who participated in JER 2 (Professors Roth, Glozier and Wheatley) in relation to common general knowledge directed to the diagnosis of primary insomnia in clinical practice in Australia at the priority date, and the potential use of melatonin. They agreed:
as at August 2001, primary insomnia was diagnosed in clinical practice in Australia by taking a thorough clinical history including a detailed sleep history, arranging any appropriate clinical examination and organising any necessary diagnostic tests to exclude alternative diagnoses. They also agreed, as set out above and referred to by Neurim in its submissions, that the clinical diagnostic process in Australia was broadly comparable to the rest of the world and utilised predominantly DSM-IV and ICSD rather than ICD-10, though all three were translatable to one another in terms of diagnostic criteria;
there is no objective clinical test that can diagnose insomnia in its broadest sense or “primary insomnia characterised by non-restorative sleep” in its specific sense. No routine clinical testing was conducted to diagnose primary insomnia and specific diagnostic tests were only utilised to exclude other clinical diagnoses where appropriate; and
as at August 2001, the extent of knowledge in Australia regarding the potential use of melatonin was as a chronobiotic for treatment of circadian rhythm disorders. There was preliminary research into the use of melatonin as a potential hypnotic agent. There was no clinical use of melatonin in Australia by medical practitioners, but members of the public used to obtain it overseas, predominantly for jetlag, and there was widespread knowledge of that use in the sleep community.
Professor Roth also noted that the minimal preliminary research into the use of melatonin as a in the treatment of insomnia had focussed on its effect on initiating sleep.
130 Professor Wheatley noted that as a sleep physician in Australia in 2001, he utilised the ICSD nosology to diagnose insomnia, which did not contain a category of “primary insomnia characterised by non-restorative sleep” and he did not make this diagnosis in patients. Later in Wheatley 4, Professor Wheatley said that the closest diagnosis available to him, referring to the ICSD and based on the description of the condition by the other experts (relying on subjective reports of the patient), was psychophysiological insomnia. Read in context, I do not understand Professor Wheatley to have accepted in JER 2 that “non-restorative sleep or primary insomnia characterised by non-restorative sleep” were terms used by sleep physicians in Australia in 2001 in diagnosing patients suffering from primary insomnia.
131 Professor Wheatley noted in JER 2 that in DSM-IV, nonrestorative sleep is defined in terms of a patient who feels “that their sleep [is] restless, light or of poor quality”.
132 Professor Wheatley said that restless, light or poor quality sleep are not unique to non-restorative sleep and may also be used by patients to describe “difficulty maintaining sleep”, which is another key symptom of primary insomnia in DSM-IV. In Wheatley 4, he also noted that had a patient approached him with a dominant complaint of not feeling rested after sleep, he would have suspected that the patient had a sleep disorder, sleep state misperception or illness, and he would have conducted further testing accordingly.
133 Neurim contended the following two documents were, or at least reflected, the common general knowledge at the priority date:
the article published in the Journal of Sleep Research (2000) Vol 9, 397-398 entitled “In what circumstances is melatonin a useful sleep therapy? Consensus statement, WFSRS Focus Group, Dresden, November 1999” (referred to in Neurim’s submissions and in these reasons as “the Consensus Statement”);
the article published in the International Journal of Clinical Practice, January/February 2001, Vol 55, No 1 356-366 entitled “Consensus for the Pharmacological Management of Insomnia in the New Millennium” (referred to in Neurim’s submissions and these reason as “the Consensus Paper”).
134 Neurim submitted that the Consensus Statement was coordinated by Professor Arendt (who it said was the world’s leading researcher in melatonin) based on the results of a focus group assembled to define conditions in which there was good evidence for the usefulness of melatonin.
135 According to the Consensus Statement:
Many claims have been made for the efficacy of melatonin as a sleep therapy (and indeed as a treatment for numerous other conditions). Induction of sleepiness by melatonin taken during the day has been known for many years. This focus group was assembled in order to define as far as possible the conditions in which there is good evidence for the usefulness of melatonin, those where evidence is lacking and the dose range for specific objectives. An important objective was to assess any known risks of long-term or short-term treatment.
136 The Consensus Statement includes a number of statements relied upon by Neurim as common general knowledge including, most importantly, that “[t]here appears to be no point in addressing sleep disorders of unknown origin with melatonin treatment”.
137 Professor Roth gave evidence that the eleven named individuals who endorsed the Consensus Statement included “probably the five most notable people in the universe on melatonin”. He described them in Roth 1 as leading researchers and clinicians in sleep medicine, particularly insomnia, circadian rhythm disorders, and the use of melatonin at the relevant time. Those who endorsed the Consensus Statement included Drew Dawson. In Roth 1, Professor Roth also noted that the Drew Dawson was “an Australian researcher”, although he did not identify his field of research or expertise specifically. Professor Wheatley knew of Drew Dawson (now Professor Dawson) before 2001. He described Professor Dawson as a sleep psychologist who was part of a research group based in South Australia, and the focus of his research in the field of sleep as being circadian rhythms and shiftwork.
138 There is no evidence that any witness apart from Professor Roth read the Journal of Sleep Research or that any of them was familiar with the Consensus Statement either before or around the priority date. Professor Wheatley considered the Consensus Statement was “broadly consistent” with Chapter 31 of Sleep Medicine.
139 As to the Consensus Paper, it includes a summary which states as follows:
Insomnia, a common symptom throughout the world, is characterised by difficulty initiating or maintaining sleep or non-restorative sleep and is associated with significant morbidity. A comprehensive medical and sleep history and physical examination are necessary before treating patients with insomnia; the presence of co-morbidities, including medical and psychiatric disorders, or the possible use of substances that may contribute to sleeplessness should be thoroughly investigated. Non-pharmacological approaches include correction of sleep hygiene as well as behavioural treatments. Pharmacotherapy includes benzodiazepine-receptor agonists, which are the drugs of choice for this disorder. They can be subdivided into classic benzodiazepines and non-benzodiazepines. Although many agents in these classes have been prescribed, potential shortcomings include residual sedation, rebound insomnia, and psychomotor and memory impairment. Novel pharmacological strategies that address limitations of the traditional treatment approach, combined with proven modes of behavioural therapy, offer the most successful results in the management of insomnia. These advances provide the opportunity to establish these current recommendations for the optimal management of insomnia. This report from the XXII Collegium Internationale Neuro-Psychopharmacologicum Consensus Workshop outlines recommendations to serve as the foundation for developing a therapeutic plan for each patient. (Int J Clin Pract 2001; 55(1): 42-52)
140 The Consensus Paper includes a paragraph dealing with primary insomnia which it describes as an “intrinsic sleep disorder”. The paper refers to the DSM-IV and explains that primary insomnia is defined therein as a sleep disorder that:
• is characterised by difficulty initiating or maintaining sleep or non-restorative sleep for at least one month
• produces clinically significant distress or impairment in social, occupational, or other important areas of function
• does not occur exclusively during the course of another sleep disorder
• does not occur exclusively in the course of another mental disorder
• is not due to the direct physiological effects of a substance or a general medical condition.
Thus, symptoms should occur in the absence of other primary sleep disorders, circadian rhythm disorders, general medical conditions and psychiatric disorders.
(Footnote omitted)
141 The Consensus Paper purports to record the outcome of a workshop held in Brussels in July 2000 aimed at developing recommendations for the treatment of insomnia, the XXII Collegium Internationale Neuro-Psychopharmacologicum Consensus Workshop. It includes a brief discussion of melatonin which notes that while it “may be useful in treating abnormalities of the circadian rhythm, it is premature to propose a primary role for this hormone in the treatment of insomnia”.
142 There was no evidence to indicate that any of the expert witnesses, apart from Professor Roth, were familiar with the Consensus Paper or read the International Journal of Clinical Practice in which it appeared at the priority date. Professor Wheatley gave oral evidence that he was not familiar with the journal, he would not read or review it regularly, and it would be rare for him to see an article from the journal in his practice. Beyond the three named authors, there is no evidence of who endorsed the content of the article, to whom it was circulated, or by whom it was reviewed.
143 Professor Glozier, although familiar with the Internationale Neuro-Psychopharmacologicum, gave oral evidence that he did not know the journal and had never attended a consensus conference of that organisation specifically.
144 In the circumstances, I am not persuaded that the Consensus Paper was common general knowledge at the priority date. However, Neurim submitted that the Consensus Statement and the Consensus Paper reflected the common general knowledge at the date of their publication.
145 So far as the Consensus Paper is concerned, I accept that it would have been generally accepted among persons skilled in the art at the time that it would be premature to propose a primary role for the use of melatonin in the treatment of insomnia, including primary insomnia. Put another way, I would accept that the bulk of persons working in the field of sleep medicine would have accepted that there was at the priority date insufficient evidence to show that melatonin was an effective treatment for insomnia.
146 Further, to the extent that the Consensus Statement is to be understood as suggesting that there was at that time insufficient evidence to support the use of melatonin as a treatment for primary insomnia then I would also accept that the bulk of those working in the field at that time would have been of the same mind. These findings are in my opinion consistent with what appears in Chapter 31 of Sleep Medicine which hypothesises in its conclusion that melatonin could be useful for the treatment of insomnia, but that this had yet to be established through properly controlled clinical trials. The experts who participated in JER 2 all knew of the existence of preliminary research into the use of melatonin as a potential hypnotic agent.
147 There was no dispute between the parties as to the principles governing the construction of a complete specification and its claims. The relevant principals were conveniently summarised by the Full Court in Jupiters Ltd v Neurizon Pty Ltd (2005) 222 ALR 155 (Hill, Finn and Gyles JJ) as follows at [67]:
…
(i) the proper construction of a specification is a matter of law: Décor Corporation Pty Ltd v Dart Industries Inc (1988) 13 IPR 385 at 400;
(ii) a patent specification should be given a purposive, not a purely literal, construction: Flexible Steel Lacing Co v Beltreco Ltd (2000) 49 IPR 331; [2000] FCA 890 at [81] (Flexible Steel Lacing); and it is not to be read in the abstract but is to be construed in the light of the common general knowledge and the art before the priority date: Kimberley-Clark Australia Pty Ltd v Arico Trading International Pty Ltd (2001) 207 CLR 1; 177 ALR 460; 50 IPR 513; [2001] HCA 8 at [24];
(iii) the words used in a specification are to be given the meaning which the normal person skilled in the art would attach to them, having regard to his or her own general knowledge and to what is disclosed in the body of the specification: Décor Corporation Pty Ltd at 391;
(iv) while the claims are to be construed in the context of the specification as a whole, it is not legitimate to narrow or expand the boundaries of monopoly as fixed by the words of a claim by adding to those words glosses drawn from other parts of the specification, although terms in the claim which are unclear may be defined by reference to the body of the specification: Kimberley-Clark v Arico at [15]; Welch Perrin & Co Pty Ltd v Worrel (1961) 106 CLR 588 at 610; Interlego AG v Toltoys Pty Ltd (1973) 130 CLR 461 at 478; the body of a specification cannot be used to change a clear claim for one subject matter into a claim for another and different subject matter: Electric & Musical Industries Ltd v Lissen Ltd [1938] 4 All ER 221 at 224–5; (1938) 56 RPC 23 at 39;
(v) experts can give evidence on the meaning which those skilled in the art would give to technical or scientific terms and phrases and on unusual or special meanings to be given by skilled addressees to words which might otherwise bear their ordinary meaning: Sartas No 1 Pty Ltd v Koukourou & Partners Pty Ltd (1994) 30 IPR 479 at 485–6 (Sartas No 1 Pty Ltd); the court is to place itself in the position of some person acquainted with the surrounding circumstances as to the state of the art and manufacture at the time (Kimberley-Clark v Arico at [24]); and
(vi) it is for the court, not for any witness however expert, to construe the specification; Sartas No 1 Pty Ltd at 485–6.
148 The notion of purposive construction, as explained by the Full Court in GlaxoSmithKline Consumer Healthcare Investments (Ireland) (No 2) Ltd v Generic Partners Pty Ltd (2018) 264 FCR 474 requires that the specification be read as a whole and in light of the common general knowledge, and that a practical and common sense approach be taken to its construction. The Full Court said at [106]:
More recent cases have continued to emphasise the need to read a patent specification as a whole and in light of the common general knowledge. They also confirm that a patent specification should be read in a practical and common sense way and given a “purposive” construction. This approach to construction requires the court to read the specification through the eyes of the skilled addressee with practical knowledge and experience in the field of work in which the invention was intended to be used and a proper understanding of the purpose of the invention.
149 The Full Court referred with approval to what Lord Hoffmann said in the well-known passage in Kirin-Amgen Inc v Hoechst Marion Roussel Ltd [2005] RPC 169. His Lordship said at [34]:
“Purposive construction” does not mean that one is extending or going beyond the definition of the technical matter for which the patentee seeks protection in the claims. The question is always what the person skilled in the art would have understood the patentee to be using the language of the claim to mean. And for this purpose, the language he has chosen is usually of critical importance. The conventions of word meaning and syntax enable us to express our meanings with great accuracy and subtlety and the skilled man will ordinarily assume that the patentee has chosen his language accordingly. As a number of judges have pointed out, the specification is a unilateral document in words of the patentee’s own choosing. Furthermore, the words will usually have been chosen upon skilled advice. The specification is not a document inter rusticos for which broad allowances must be made. On the other hand, it must be recognised that the patentee is trying to describe something which, at any rate in his opinion, is new; which has not existed before and of which there may be no generally accepted definition. There will be occasions upon which it will be obvious to the skilled man that the patentee must in some respect have departed from conventional use of language or included in his description of the invention some element which he did not mean to be essential. But one would not expect that to happen very often.
150 The claims of the Patent are all Swiss-style claims or claims to a method of treatment using a pharmaceutical compound that was known and used in the treatment of sleep disorders at the priority date. Claims of this type are often referred to as “second medical use claims”.
151 The discussion of the prior art in the Patent makes clear that melatonin had previously been used to treat patients suffering from insomnia. In JER 2, the experts agreed that at the priority date, the extent of knowledge in Australia regarding the potential use of melatonin was that it was used in research trials as a chronobiotic for treatment of circadian rhythm disorders. There was also knowledge of preliminary research use of melatonin as a potential hypnotic agent. Professor Wheatley gave evidence (which I accept) that melatonin was a readily available and popular “over the counter” (“OTC”) medicine for insomnia in the United States well before August 2001 and throughout the 1990s. Professor Roth acknowledged in his affidavit evidence that melatonin was, at the priority date, useful in treating circadian rhythm disorders. In my opinion, the claims of the Patent are properly characterised as “second medical use claims”.
152 In Apotex Pty Limited v Sanofi-Aventis Australia Pty Limited (2013) 253 CLR 284 (“Leflunomide HCA”), Crennan and Kiefel JJ construed the relevant claim (for a method of preventing or treating psoriasis by administering leflunomide) as being limited to the use of the method for a specific purpose. Their Honours said at [289]:
Claim 1 is recognisably a claim limited to the specific purpose of preventing and treating psoriasis. Given the prior art, any novelty and inventive step reposes in, and is confined to, that hitherto unknown therapeutic use of leflunomide. The compound (with prior therapeutic uses) was disclosed in Patent 341. The monopoly granted in respect of claim 1 is limited to the purpose (hitherto undiscovered) for which the (known) compound can be used.
153 Justice Hayne adopted (at [172]) a similar analysis to that adopted by Keane CJ in the Full Court. Keane CJ said at Apotex Pty Ltd v Sanofi-Aventis Australia Pty Ltd (No 2) (2012) 204 FCR 494 (“Leflunomide FFC”) at [37]:
…The claim is for a method of treatment of a human ailment. That method necessarily presupposes a deliberate exercise of diagnosis and prescription by a medical practitioner. The treatment or prevention of psoriasis by the use of the claimed method presupposes a diagnosis of psoriasis and the consequent prescription of the application of leflunomide. That this is so is hardly controversial: as is apparent from all the potential constructions of the patent advanced by the parties, the claim in the patent involves the application of leflunomide by a medical practitioner.
154 With regard to Swiss-style claims, the Full Court in Mylan Health Pty Ltd v Sun Pharma ANZ Pty Ltd (2020) 279 FCR 354 (Middleton, Jagot, Yates, Beach and Moshinsky JJ) (“Mylan ”) also emphasised the importance of the therapeutic purpose for which the relevant medicament is to be manufactured. Swiss-style claims are “purpose-limited claims in the sense that the medicament resulting from the method or process is characterised by the therapeutic purpose for which it is manufactured, as specified in the claim”: Mylan at [196]. The Full Court said at [197]:
The specification of a therapeutic purpose imposes an important limitation on the scope of the claim. In theory, it is this limitation which supports the novelty, and hence the patentability, of the invention. Without this limitation, the claim would be invalid because its scope would be broadened to include old subject matter (bearing in mind that Swiss type claims are directed to methods or processes whose products are for second or later therapeutic uses). It is appropriate, therefore, to consider this purpose as one that confines the use of the method or process to the achievement of one end and one end only — a medicament for the specified therapeutic purpose; not a medicament for any other therapeutic purpose. Put another way, a Swiss type claim does not claim the invention in terms of a medicament that is useful for, or can be used for, the specified therapeutic purpose and other therapeutic purposes. In order to support its patentability, and preserve its validity, the invention, as claimed through a Swiss type claim, is necessarily more limited in scope.
155 Accordingly, in construing both Swiss-style claims and method of treatment claims for a second medical use, it is necessary to have close regard to the purpose of the relevant treatment as specified in the claim as the specificity with which the purpose is defined may have significant implications for both validity and infringement.
156 The respondents contend that the claims of the Patent are invalid on the ground that they lack clarity, and therefore do not comply with s 40(3) of the Act. In Novozymes A/S v Danisco A/S (2013) 99 IPR 417 Jessup J (which whom Greenwood and Yates JJ agreed) said at [93]:
[93] The problem of locating the dividing line which separates a claim which is bad for want of clarity from a claim which, though troublesome in its construction, is sufficiently clear to be valid, is scarcely less difficult than the problem of construction itself. In the present case, both sides have been able to draw upon general statements in the cases which provide some support for the opposite positions which they take. For my own part, I would find it sufficient for present purposes to refer to Welch Perrin & Co Pty Ltd v Worrel (1961) 106 CLR 588, in which the High Court said (at 610):
If it is impossible to ascertain what the invention is from a fair reading of the specification as a whole, that, of course, is an end of the matter. But this objection is not established by reading the specification in the abstract. It must be construed in the light of the common knowledge in the art before the priority date. The general principles governing the construction of specifications are well known, and no lengthy reference to them is necessary. It is, however, fitting that we remind ourselves of the criterion to be applied when it is said that a specification is ambiguous. For, as the Chief Justice pointed out in Martin v Scribal (1954) 92 CLR 17 at 59, referring to Lord Parker’s remarks in National Colour Kinematograph Co Ltd v Bioschemes Ltd (1915) 32 RPC 256, we are not construing a written instrument operating inter partes, but a public instrument which must, if it is to be valid, define a monopoly in such a way that it is not reasonably capable of being misunderstood. Nevertheless, it is to be remembered that any purely verbal or grammatical question that can be resolved according to ordinary rules for the construction of written documents, does not, once it has been resolved, leave uncertain the ambit of the monopoly claimed (see Kauzal v Lee (1936) 58 CLR 670 at 685).
157 I also refer to Aickin J’s well-known statement in 3M where his Honour observed at 274: “Lack of precise definition in claims is not fatal to their validity so long as they provide a workable standard suitable to the intended use …”.
Primary insomnia in the DSM-IV
158 It is clear that the term primary insomnia, as used in the claims, refers to the condition defined in DSM-IV. That view of the claims is confirmed by the reference to “non-restorative sleep” (or “NRS”) which features in both the DSM-IV definition of primary insomnia and the claims. The claim language both in its reference to primary insomnia and non-restorative sleep is drawing on the diagnostic criterion for primary insomnia in DSM-IV.
159 Each of the experts, in JER 1, also agreed that the patent defines primary insomnia according to the DSM-IV criteria. Neurim referred to this agreement in its written submissions, and the respondents also submitted that Patent “clearly intends” that primary insomnia in the claims refers to primary insomnia as defined in DSM-IV.
160 As to how the term “primary insomnia” is understood within the DSM-IV, I have previously referred to what DSM-IV refers to as the diagnostic features of primary insomnia of which there are five (Criteria A, B, C, D and E). The relevant extract from DSM-IV is set out above.
Equivalence to nonorganic insomnia according to the ICD-10
161 ICD-10 does not refer to primary insomnia but instead uses the term “nonorganic insomnia” to refer to “a condition of unsatisfactory quantity and/or quality of sleep which persists for a considerable period of time” (F51.0). Each of the experts in JER 1, except for Professor Glozier, agreed that primary insomnia as in the DSM-IV was equivalent to nonorganic insomnia according to the ICD-10 as at the priority date. Professor Glozier noted that although primary insomnia and nonorganic insomnia are “very similar”, they are not exactly the same.
162 The diagnostic guidelines included in ICD-10 identify what are referred to as four essential clinical features of nonorganic insomnia. The first requires that “the complaint is either of difficulty falling asleep or maintaining sleep, or a poor quality of sleep” (Criterion A). The second requires that the sleep disturbance must occur at least three times a week for at least one month (Criterion B). The third requires that it is accompanied by a “preoccupation with the sleeplessness and excessive concern over its consequences at night and during the day” (Criterion C). The fourth requires that “the unsatisfactory quantity and/or quality of sleep either causes marked distress or interferes with ordinary activities in daily living” (Criterion D). Drs Behi and Krapivensky also equated “non-restorative sleep” in DSM-IV to “poor quality sleep” in ICD-10, as at the priority date.
163 In my view, Professor Glozier is correct that the diagnosis of primary insomnia in the DSM-IV, and nonorganic insomnia in the ICD-10, are not precisely the same. Some of the diagnostic criteria in ICD-10 (e.g., that the sleep disturbance occur at least three times per week) are not replicated in the DSM-IV diagnostic criteria for primary insomnia. I nevertheless accept that the diagnosis of primary insomnia under DSM-IV and nonorganic insomnia under ICD-10 are very similar.
164 Professor Wheatley was heavily criticised in Neurim’s submissions for resiling from his answers in JER 1 in Wheatley 4 (made after JER 1), including in relation to the meaning of non-restorative sleep in DSM-IV and poor quality sleep in ICD-10. He was cross-examined on the issue at some length.
165 I accept Professor Wheatley’s evidence that he misunderstood the JER process, and mistakenly deferred to the opinion of the other experts who he considered were more familiar than him with DSM-IV and ICD-10 diagnostic criteria, and sought to assimilate his answers with theirs. With respect to key issues of construction, the experts were asked how, as at August 2001, persons skilled in the art would understand the expressions “primary insomnia” and “non-restorative sleep”. Professor Wheatley had recorded in affidavit evidence filed before the expert conference that he was not familiar with the term “non-restorative sleep” at the priority date and that he was not familiar with the diagnostic criteria for primary insomnia in DSM-IV. Not only did Neurim accept that evidence, but it was also central to Neurim’s submissions that Professor Wheatley was not a person skilled in the art.
166 There are two issues that arise in relation to the use of the term non-restorative sleep in the claims. The first concerns the meaning to be given to that term, while the second concerns what the respondents submitted was the lack of clarity of the phrase “primary insomnia characterised by non-restorative sleep”.
167 The respondents did not dispute that the Patent intends to use non-restorative sleep in the sense that the term is used in DSM-IV, which in turn defines non-restorative sleep as meaning a complaint of restless, light or poor quality sleep. However, evidence relied on by the respondents suggests that the term non-restorative sleep at the priority date was a controversial topic, and the definition of the term as used in DSM-IV lacked clarity at both the conceptional and practical level. In short, the respondents contended that the claim did not provide a workable standard suitable for use in the diagnosis of insomnia.
168 In my opinion the term “non-restorative sleep” as used in the claim refers to a subjective complaint of restless, light or poor quality sleep that is non-refreshing. It is a complaint about the quality of a patient’s sleep. It is to be distinguished from complaints in relation to sleep onset, sleep maintenance or sleep duration, all of which relate to the quantity rather than the quality of the patient’s sleep.
169 The respondents submitted that at the priority date a person skilled in the art could readily differentiate between a patient suffering from primary insomnia and other insomniacs, but could not differentiate patients “suffering from primary insomnia characterized by NRS” from other primary insomnia sufferers with the necessary degree of certainty, consistency and predictability.
170 Professor Wheatley gave evidence concerning the difficulty in differentiating light, restless or poor quality sleep from difficulties in initiating or maintaining sleep. He agreed that the terminology of “non-restorative sleep” was unfamiliar to him in 2001. He went on to say that, based on what he now knows, while patients do not complain of suffering from “non-restorative sleep”, the diagnosis is based on a conclusion drawn from the patient’s subjective complaints, rather than objective tests. He gave the following oral evidence:
And you’ve [alluded] to my expertise in sleep apnoea and that’s clearly an area where there are more objective tests that you can do to make a diagnosis. Insomnia, as a clinical disorder, remains one of the ones where there are no – there’s no gold standard of objective tests with which you can make a diagnosis of insomnia. There are certainly diagnostic tests that can assist you, but the clinical diagnosis is still one of a subjective symptom report from the patient for those disorders. That always leaves a perception element around it and a communication between the patient and the physician in arriving at the diagnosis.
171 Professor Wheatley gave evidence that patients who suffer from difficulty initiating sleep do complain of unrefreshing sleep. He went on to say that “whether those two things are combined or separate, I don’t think there is any evidence that tells us that”. His oral evidence reflects an acceptance that DSM-IV describes the condition of primary insomnia by reference to (inter alia) the symptom of non-restorative sleep, but also his doubts as to whether non-restorative sleep is a recognisable symptom that can exist, or be detected and recognised in practice, independently of other symptoms of sleep disturbance. That is to say, I understood Professor Wheatley to be in some doubt whether a patient could experience non-restorative sleep (which he equated with unrefreshing sleep) unless the patient had also experienced difficulty in initiating or maintaining sleep, and that it was those symptoms, or a combination of them, which gave rise to the patient’s subjective complaint that their sleep was non-refreshing.
172 Professor Wheatley said in his oral evidence:
One of the articles that Professor Roth tendered in evidence about non-restorative sleep I think sometimes illustrates the difficulty of separating these symptoms both for clinicians and patients. As to whether they’re completely separate or how much they overlap, and I don’t profess to be an expert at saying whether the symptom is separate, but I would certainly elicit symptoms of unrefreshing sleep and I would agree with Dr Behi that occasionally there is no difficulty initiating or maintaining sleep as per the patient report, but that there may be a complaint of unrefreshing sleep.
173 I regard that evidence as significant, because it reflects an acknowledgement that there are some patients who complain of unrefreshing sleep that is not associated with any complaint of difficulty initiating or maintaining sleep. For those patients, their insomnia will be associated not with a deficiency in the quantity of sleep, but in the poor quality of that sleep, whether it be called non-restorative sleep, unrefreshing sleep or poor quality of sleep.
174 Professor Glozier also referred in his evidence to the problem of identifying non-restorative sleep as distinct from poor quality sleep attributable to difficulties in initiating or maintaining sleep. He referred to differences between clinicians in making their assessments and the presence of “a degree of unreliability” in such assessments. He also referred to the “Drake paper”, co-authored by Professor Roth and published in 2014 in the Journal of Clinical Sleep Medicine entitled “Development and Evaluation of a Measure to Assess Restorative Sleep” which he said “produced a very nice example of a method of actually assessing non-restorative sleep”. Professor Glozier said this in relation to the clinician’s assessment of non-restorative sleep:
… I think the closest that DSM-IV comes to a definition of non-restorative sleep is the phrase:
Non-restorative sleep, that is feeling their sleep was restless, light or of poor quality.
So there are three things that they say that non-restorative sleep is. I differ in – I don’t think it says such as. It says very clearly in black and white “that is”, which for me is as close as one can get to a definition of it. But it doesn’t make it in such distinct terms. I think the comment of restlessness would then need to be explored as to whether that is a difficulty in maintaining sleep or of non-restorative sleep. Interestingly here, poor sleep quality or poor quality here is a subset of non-restorative sleep. I think I differ slightly from my colleagues in that we define symptoms and people come with a symptom, and I think the symptom is – I would agree with these papers that the symptom itself has – or a symptom or the symptom complex or what forms it, isn’t necessarily very reliably assessed, and I think it wasn’t until 2014 when the Drake paper produced a very nice example of a method of actually assessing non-restorative sleep, and I think Professor Roth was one of the authors on that paper.
…
So I think, as we’ve described here, there are numerous ways of describing it. There are numerous ways the patients describe it and when clinicians put their lens on it and deciding whether it is or is not, and I think the, again, that Drake paper … contained quite a lot of qualitative work looking at how different clinicians actually do address this and show that there is some consistency but not complete consistency and reliability is the technical term that we use for whether two clinicians or two assessors describe exactly the same thing in exactly the same way. Now, as Dr Kaprivensky has said quite correctly, psychiatric symptoms and subjective symptoms, full stop, are never 100 per cent reliably identified. I don’t think there’s a single one that is – has ever been shown in any of the ICD or DSM field trials so 100 per cent reliability just does not occur so there’s always some unreliability. Whether NRS is substantially more or less unreliable [than] other symptoms, I don’t know.
175 Professor Glozier was referring here to problems in relation to the reliability of psychiatric symptoms more generally. The last statement in that passage of Professor Glozier’s evidence is significant because it tends to suggest that the problem of making a reliable diagnosis of non-restorative sleep may be no more difficult than making a diagnosis of other psychiatric symptoms based on a patient’s subjective complaint. The evidence of Dr Krapivensky and Dr Behi indicates that the difficulties involved in making the relevant diagnosis are not beyond the skill of a clinician familiar with the diagnostic criteria specified in DSM-IV who is able to elicit the information needed to make the assessment in the course of taking a patient history. As Dr Krapivensky explained when asked by counsel for the respondents to explain her understanding of the definition of non-restorative sleep as used in the Patent:
My understanding very clearly is that it is a subjective patient complaint and I agree with Dr Behi’s comments that patients do not walk in usually saying, “I have nonrestorative sleep”. It’s a complaint that we elicit in the course of taking a history, and it’s a subjective – it’s a range of words that patients use and that we sometimes elicit that conveys to me that the patient when they first wake up in the morning feel not refreshed, for – or not – they feel like they haven’t slept well. They still feel listless and they feel that they’re just not right. And the question that I would ask is how do you feel when you first wake up in the morning? And that is what – and the patient answers that question as best they can, and we put that together to mean or not to mean nonrestorative sleep.
176 It is apparent from the evidence that making a diagnosis of non-restorative sleep will be more difficult in some cases than others. If a patient reports not experiencing any difficulty initiating or maintaining sleep, yet still complains that their sleep is of poor quality or is unrefreshing, then a complaint of non-restorative sleep might be readily identified. But the diagnosis would be more difficult in a case where the complaint involves a mixture of symptoms where, for example, the patient had difficulty initiating or maintaining sleep and poor quality sleep. Professor Roth acknowledged in answer to questions from the Court that it is very difficult to disentangle non-restorative sleep from other symptoms of primary insomnia which he said tend to occur together. He said the symptoms could be disentangled by a therapeutic approach which, as I understood his evidence, would involve using a pharmacological intervention that might affect sleep latency or maintenance, but not non-restorative sleep. Presumably this would enable the clinician to determine whether the patient’s complaint of feeling unrefreshed after sleep was no more than a consequence of not getting enough sleep, or a consequence of non-restorative sleep.
177 Dr Krapivensky said in her oral evidence that she did not think that it was difficult to distinguish between problems of non-restorative sleep and sleep maintenance. In fact, she said that they are “two distinct things that are quite easy to distinguish”, and that she did not think there was any difficulty in distinguishing them clinically. I think Dr Krapivensky’s evidence considerably understates the difficulty facing a clinician in making the assessment in those cases where it may be difficult to disentangle the patient’s complaint of difficulty initiating or maintaining sleep from a complaint of poor quality sleep. I prefer Professor Glozier’s evidence to that of Dr Krapivensky on this point. I accept that there may be cases in which it is not possible to make a reliable diagnosis. On the other hand, I accept that there will be cases where a reliable diagnosis can be made because the patient complains of poor quality sleep, but not of any other sleep disturbance. The diagnosis may be much less reliable in cases where the patient reports difficulty initiating or maintaining sleep and poor quality sleep.
178 The respondents relied on another paper co-authored by Professor Roth and published in 2001 at around the time of the priority date in the Journal of Psychosomatic Research entitled “What are the contributing factors for insomnia in the general population?”. The paper refers to a number of difficulties in the “[d]ecision-making process of insomnia diagnosis”, observing that the first criterion in the DSM-IV definition of insomnia (“the predominant complaint is difficulty initiating or maintaining sleep, or nonrestorative sleep, for at least 1 month”) was “pretty large and difficult to apply in [an] epidemiological study”. The first issue the authors refer to in this context is the word “predominant”, specifically in relation to the phrase “predominant complaint”. I note that this word, and its use in the DSM-IV, was not said by any witness to be a source of any difficulty, and the respondents do not contend that its use in the DSM-IV definition of primary insomnia is in any respect problematic. Although the authors propose new definitions and decision trees of insomnia and sleep deprivation (Table 4) these continue to distinguish between difficulty initiating sleep (“DIS”), difficulty maintaining sleep (“DMS”) and non-restorative sleep (“NRS”).
179 The particular definition of NRS proposed by the Professor Roth and his co-author in the 2001 paper was as follows:
Nonrestorative sleep
(A) The report of feeling the sleep is nonrestorative nearly every night (at least three nights per week) AND a normal sleep duration according to the age and gender of the subject
(B) At least one of the two following:
(1) Feeling rather to completely unrested upon awakening
(2) Light to important difficulties getting started in the morning nearly everyday
180 What is most significant about this definition is that it confines diagnosis of NRS to situations in which the subject experiences normal sleep duration which would preclude a diagnosis of NRS if the patients experienced DIS or DMS which reduced their sleep duration to less than would be considered normal.
181 In another article by Stone et al published in Sleep Medicine Reviews in 2008 (post priority date) entitled “Nonrestorative Sleep” the authors reviewed the history of NRS, which they describe as “a subjective experience of unrefreshing sleep”, and the different ways in which NRS has been defined across various studies as well as in diagnostic and classification manuals (ICD-10, ICSD and DSM-IV). They concluded (inter alia) that NRS is “poorly understood and variably defined”, and they could find “no empirical justification for the inclusion of NRS as a primary symptom of insomnia in diagnostic nosologies”. Referring to Professor Roth’s 2001 paper, the authors state:
The epidemiological study conducted by Ohayon and Roth supported guidelines for operationalizing insomnia symptoms, including NRS, in order to increase their specificity. They determined that when assessing NRS as a symptom of insomnia, more than one question (e.g., "Do you feel refreshed upon awakening?") is needed. Assessing sleep duration appears particularly helpful in making an NRS diagnosis. Of the 8.9% with an NRS complaint (of the 24,600 individuals surveyed), 7.2% had a normal sleep duration whereas only 1.7% did not. Therefore, Ohayon and Roth concluded that to be classified as having NRS, individuals should not only have a complaint of NRS at least 3 times a week but should also have reported a normal sleep duration. Ohayon and Roth advise that without a normal sleep duration, the complaint alone does not justify NRS.
(Footnotes omitted)
182 The respondents also relied on a paper co-authored by Professor Roth and published in 2010 (also post priority date) in Sleep entitled “Nonrestorative Sleep as a Distinct Component of Insomnia”. The paper includes the following introduction:
INSOMNIA IS CHARACTERIZED BY NIGHTTIME SLEEP PROBLEMS, WHICH MAY MANIFEST AS THE COMPLAINT OF DIFFICULTY INITIATING SLEEP (DIS), difficulty maintaining sleep (DMS), or nonrestorative sleep (NRS), or a combination of these complaints, and daytime symptoms. An insomnia diagnosis is confirmed if the sleep complaints or associated daytime problems cause significant distress or functional impairment for at least 1 month. Thus, one critical feature to consider in making the diagnosis of insomnia, over and above the amount of time spent asleep, is the patient’s experience of being insufficiently rested or refreshed to be able to carry out normal social and occupational functions. This is reflected in the recognition of NRS as a core component of insomnia according to DSM-IV diagnostic criteria. However, in practice DIS and DMS remain the most readily recognized sleep complaints in insomnia, and the main targets of treatments for insomnia. NRS, by comparison, remains poorly characterized.
Few studies investigating the prevalence and burden of insomnia have focused on NRS. However, two large surveys have shown that it is a prevalent complaint, occurring in 11% to 25% of the insomnia population. Estimation of the prevalence of NRS is hampered by imprecise or inconsistent definitions used to identify patients with NRS, as well as a lack of validation of patient reports of NRS with objective measures. A recent review of literature on NRS by Stone et al. highlighted the variation in constructs addressed by different insomnia studies that have attempted to quantify NRS. The authors concluded that there is a lack of empirical data to substantiate a clear conceptualization of NRS, pointing to a need for further research in this area. Furthermore, many reports of NRS arise in the context of other conditions such as fibromyalgia syndrome and chronic fatigue syndrome, leading some clinicians to question whether NRS occurs in the absence of other sleep or health problems. Nonetheless, DSM-IV diagnostic criteria recognize that NRS can occur in the context of primary insomnia (insomnia that does not occur exclusively during the course of another sleep or mental disorder, nor due to effects of a substance or medical condition) and that NRS can in some cases be the sole sleep complaint in primary insomnia. Where attempts have been made to clarify the concept of NRS, proposed criteria include daytime complaints of difficulty getting started in the morning and/or feeling rather or completely unrested upon awakening nearly every day, despite a normal sleep duration for the individual’s age and gender. However, no study to date has provided polysomnographic confirmation that NRS does occur in the absence of other primary sleep disorders, sleep deprivation, or other insomnia symptoms.
Patients with NRS could be an important segment of the insomnia population—survey data gathered to date indicate that that [sic] individuals with NRS experience significant daytime impairment, including irritable mood, physical and mental fatigue, and role impairment. Patients also commonly report that increased effort is required to perform work and daily activities. The apparent burden associated with NRS suggests that, to be fully effective, the management of insomnia should take account of this component. Currently only the German Society of Sleep Research and Medicine sets out guidelines for the diagnosis and management of NRS. There is a need for research to improve our understanding of NRS and guide management of the condition.
(Footnotes omitted)
183 The paper goes on to report the results of a study designed to define the population in which NRS occurs. The study sought to compare patterns of daytime symptoms, and their persistence, between cohorts experiencing NRS, grouped by the presence or absence of DIS or DMS. The paper states that it identified a “pure NRS” population and provided empirical data on NRS that had until then been lacking. The paper provides support for the view that NRS is a symptom of insomnia that may exist independently of DIS or DMS. In particular, it showed that daytime symptoms (i.e., sleepiness and fatigue) of individuals enrolled in the study with NRS in the absence of DIS and DMS were as severe as those experienced by individuals whose NRS was combined with DIS or DMS.
184 There are a number of additional points to make in relation to Professor Roth’s 2010 paper.
185 First, the authors acknowledge that DIS and DMS are the most readily recognisable sleep complaints in insomnia and that, in comparison, NRS is poorly characterised. However, the authors also observe that two large surveys showed that NRS is a prevalent complaint of insomnia. I do not understand the authors to say that a clinician cannot diagnose NRS, but rather that NRS is more difficult to diagnose compared to DIS or DMS.
186 Secondly, the paper indicates that imprecise or inconsistent definitions of NRS and a lack of validation of patient reports using objective measures has made it difficult for clinicians to estimate the prevalence of NRS, and that the many reports of NRS arising in the context of other conditions such as fibromyalgia syndrome and chronic fatigue syndrome led some clinicians to question whether NRS occurs in the absence of other sleep or health problems. The authors note that their study was the first to make use of polysomnographic data for the purpose of confirming that NRS may occur in the absence of other primary sleep disorders, sleep deprivation or other insomnia symptoms. The authors’ use of polysomnographic testing confirmed that NRS may occur in circumstances where the patient is not experiencing either DIS or DMS.
187 A commentary on Professor Roth’s 2010 paper, also published in Sleep, referred to the debate concerning NRS and whether or not it should be retained as a diagnostic feature of insomnia. The author commented at pp 417-418:
The work by Roth and colleagues suggests that if one searched for subjects with NRS-only and daytime impairments without other symptoms of insomnia like prolonged sleep latency or disturbed sleep maintenance, one might be able to identify subjects suffering from this specific insomnia subtype. The study cannot say anything about the prevalence of this condition in the general population, because it was specifically designed to detect only subjects with NRS. Further epidemiological work will be necessary to learn more about the prevalence and incidence of NRS-only.
(Footnote omitted)
188 The respondents submitted that Professor Roth’s 2010 paper, written some nine years after the priority date, showed that even by that time:
… NRS was still a theory in search of a meaningful definition notwithstanding that DSM-IV had included it as part of a group of symptoms any of which was sufficient to satisfy Criterion A of a primary insomnia diagnosis.
189 In support of their submission, the respondents also relied on the Drake paper, to which Professor Glozier referred in his oral evidence quoted above, which reports on work done with focus groups and expert panels with a view to developing a restorative sleep questionnaire (“RSQ”). The authors conclude that the results of their study provide support for the reliability and validity of the RSQ as a measure of non-restorative sleep in subjects with and without self-reported or polysomnographic confirmed sleep initiation and maintenance difficulties.
190 The Drake paper notes that the expert panels that were convened confirm the importance of non-restorative sleep as a frequently encountered problem either with or without other sleep complaints. The paper defines non-restorative sleep as “feeling sleep was restless, light, of poor quality, or awakening feeling unrestored or unrefreshed”. That definition, insofar as it refers to “awakening feeling unrestored or unrefreshed”, appears to be drawing from DSM-5 (published in 2013) which refers to non-restorative sleep as “a complaint of poor sleep quality that does not leave the individual rested upon awakening despite adequate duration”.
191 Referring to Professor Roth’s 2010 paper, the Drake paper states at p 734:
A recent study showed that complaints of NRS can exist even in individuals with polysomnographically determined normal sleep onset, duration, and continuity. The restorative quality of sleep is an important component of insomnia as a significant portion of insomnia patients present exclusively with this complaint, reporting normal sleep initiation and maintenance. Data from the National Comorbidity Study show the prevalence of individuals in an insomnia population with exclusive complaints of NRS is estimated at 7%. Importantly, in the largest study to date, people with NRS were found to report daytime consequences significantly more often than those with difficulty initiating or maintaining sleep.
(Footnotes omitted)
192 The authors also note at p 735:
Both expert panels agreed that existing scales with the ability to assess NRS may not be optimal for clinicians interested in making therapeutic decisions or measuring treatment outcomes. The need for measures of NRS based on qualitative as well as quantitative research, including content validity consistent with patient experiences, was emphasized. In addition, panelists indicated that the information reported from the focus groups was meaningful and relevant for the development of instruments assessing NRS. Clinicians described NRS in a fashion similar to patient focus groups. Consensus was obtained around the point that NRS represents a unique symptom that has been difficult to define precisely or measure and separate from nocturnal sleep symptoms and possible comorbid conditions (i.e., arthritis).
193 Returning to the respondents’ submission, I do not accept that NRS was at the priority date, or at any time thereafter, a mere theory or “a theory in search of a meaningful definition”. The scientific literature relied on by the respondents in support of their submission shows that while NRS may have been difficult to define and measure, it was experienced by a not insignificant proportion of patients who did not experience DIS or DMS. The literature also shows that daytime symptoms for patients experiencing NRS on its own may be just as severe for patients suffering from NRS combined with DIS or DMS.
194 I am not persuaded that the meaning of non-restorative sleep, as that term is used in the claims, is insufficiently precise or clear to render the claims invalid for lack of clarity. The concept is sufficiently well defined to enable a person skilled in the art to determine whether a patient complaint is one of non-restorative sleep in an appropriate case. The fact that the diagnosis might be difficult to make in some cases due to the presence of other symptoms of sleep disturbance, or that there was continued investigation into how such a diagnosis may be made and the definitive characterisation of non-restorative sleep, does not mean that the term is insufficiently precise or clear to form the basis of a claim for a method of treatment.
Characterised by Non-Restorative Sleep
195 There was a significant debate between the parties and the expert witnesses as to the meaning of the words “characterised by” in the context of the phrase “primary insomnia characterised by non-restorative sleep”.
196 Neurim submitted that the ordinary meaning of “characterised by” should be adopted and that this required that the complaint of non-restorative sleep be a significant symptom but not the dominant symptom of the patient’s primary insomnia.
197 On Neurim’s construction of the relevant words, a patient’s primary insomnia would be characterised by non-restorative sleep if non-restorative sleep is present in the patient “as a significant or subjective complaint”, but it is not required to be the dominant symptom of their condition.
198 The respondents’ principal submission was that the phrase “characterised by non-restorative sleep” lacks clarity. They submitted that in circumstances where neither the Patent nor DSM-IV provides any assistance in defining the words “characterised by” the Court should conclude that the proper construction of these words remains a matter of doubt. They also submitted, in the alternative, that the words “characterised by” should be understood as referring to the sole or dominant characteristic of the patient’s sleep complaints.
199 Dr Behi, Dr Krapivensky and Professor Roth did not accept that the words “characterised by” required that non-restorative sleep be the dominant element of the patient’s complaint. Dr Behi maintained that any patient who subjectively complained of non-restorative sleep (and who otherwise met the diagnostic criteria for primary insomnia) would be a person whose primary insomnia was characterised by non-restorative sleep. He also said that it was common place in medicine for the term “characterised by” to refer to a condition that was significant though not necessarily dominant.
200 Dr Behi was asked about a patient with primary insomnia that complained of difficulty initiating sleep, difficulty maintaining sleep and non-restorative sleep. He was asked to assume that those difficulties were all contributing to their primary insomnia broadly equally and whether he would in those circumstances say that the patient’s primary insomnia was characterised by non-restorative sleep. Dr Behi said:
Yes, I would. But I would not go on to say to the exclusion of the other two symptoms. I would say it’s characterised by non-restorative sleep and sleep initiation and early waking, if that’s you meant, I’m guessing. For example, it does what they discern – it would be characterised by whichever of the three symptoms they described in that case. But it might be two of the three, and it might be more of one than the other that they’re reporting is bothering them or that has become clear. In some patients, when their sleep initiation or maintenance improves, they continue to complain about the non-restorative sleep in disproportion of the improvement in the sleeping issues maintenance. Then I would redescribe it as, you know, it’s not only characterised by the three symptoms still without the improvement into not. So it’s a – I would use the terms “characterised by non-restorative sleep” if they had non-restorative sleep but it’s not – and I think I’m not including the word exclusively non-restorative sleep or characterised solely by non-restorative sleep.
201 It is apparent that Dr Behi would consider a diagnosis of primary insomnia characterised by non-restorative sleep if the patient complained that they did not have restorative sleep, even though the cause of the patient’s distress or impairment (Criterion B in the DSM-IV diagnostic criteria for primary insomnia) was primarily due to difficulty initiating or maintaining sleep.
202 Dr Krapivensky’s evidence was to much the same effect as Dr Behi. In JER 1 she indicated that the symptom of non-restorative sleep “should be present and relevant” but that “dominance within the clinical picture is not relevant”.
203 The psychiatrists emphasised that patients do not typically report that they have experienced “non-restorative sleep”. They emphasised the need for the clinician to ask appropriate questions to determine that the patient was experiencing non-restorative sleep. It does not follow that, because a patient says that they are experiencing poor quality sleep, the patient is suffering non-restorative sleep. A patient who complains of having experienced poor quality sleep may use that language to describe what is properly characterised as difficulty in initiating or maintaining sleep. I accept the presence of non-restorative sleep is to be ascertained by the clinician based on their analysis of the patient’s history and the patient’s subjective complaints. What I understand Dr Behi to say is that if the clinician concludes based on the patient’s subjective complaint that non-restorative sleep is a symptom of the patient’s primary insomnia, then the patient’s condition will be “characterised by non-restorative sleep” even though difficulty initiating or maintaining sleep may be the more dominant of the three symptoms.
204 In JER 1 Professor Wheatley stated that when a medical disorder is “characterised by” a particular symptom, then it will be the primary or dominant symptom by which the disorder is recognised or defined. He said this was a conclusion relating to the use of language, not to sleep research or literature. In his oral evidence, Professor Wheatley accepted that the word “characterised” does not have a special meaning to people in the medical field of “dominant”. He also accepted that it would be common in the medical field to find references in the literature to something being “characterised” by one or more things. Professor Glozier agreed that there was no technical definition of the word “characterised”.
205 It follows that the word “characterised” as used in the claim is to be given its ordinary meaning as it would be understood by the skilled person in the context of the Patent as a whole. DSM-IV defines primary insomnia by reference to “[t]he predominant complaint [of] difficulty initiating or maintaining sleep, or non-restorative sleep”. However, this does not require that only one of these symptoms be present. A person may be diagnosed with primary insomnia even though their complaint of poor sleep quality covers all three symptoms.
206 In my opinion the words “characterised by” when used in the claim are to be understood as meaning that non-restorative sleep is a diagnosed characteristic (or symptom) of the patient’s primary insomnia. The language of the claim does not expressly or impliedly require it to be the sole or dominant symptom. The respondents’ interpretation involves reading into the claims a limitation that cannot be supported by the words used in the claim or elsewhere in the complete specification. On the other hand, the claim must be read in a practical and commonsense way. I would therefore accept that non-restorative sleep must be a clinically meaningful element in the diagnosis of primary insomnia.
Improving the Restorative Quality of Sleep
207 In JER 1 the experts state:
We agree that as at August 2001 in Australia, those skilled in the art would understand the term “improving the restorative quality of sleep” to be a subjective patient report to the effect that conveys a feeling that sleep is more restorative.
208 In his supplementary affidavit, Professor Wheatley resiled from this agreement on the basis that “restorative quality of sleep” is not a term he was familiar with as at the priority date. However, his supplementary affidavit did not proffer any alternative view as to the meaning of those words as used in the context of the Patent.
209 The respondents contended that the phrase “improving the restorative quality of sleep” as used in the claims lacks clarity.
210 There were two aspects to the respondents’ argument that the phrase “improving the restorative quality of sleep” lacks clarity. First, the respondents submitted that if an improvement in the restorative quality of sleep was understood to mean simply an improvement in the NRS symptom, then it was unclear whether that improvement had to be independent of any improvement in DIS or DMS. Second, the respondents submitted that the words “restorative quality of sleep” are used in the Patent to indicate something distinct from a subjective perception of sleep quality, and that what the Patent refers to as improvements in the “restorative value of sleep” are assessed by reference to objective measurements of daytime vigilance. In developing this submission the respondents focussed on the various examples in the Patent.
211 Professor Wheatley’s written evidence includes a detailed critique of Examples 1-4 in the Patent noting that they are said to be illustrative of the invention. Many of Professor Wheatley’s criticisms are concerned with the lack of detail provided in respect of each of the trials including, for example, the lack of definition of quantitative and qualitative parameters, lack of information concerning trial design and statistical analysis, and the use of a single scale to measure different variables. Professor Wheatley was also of the view that there was no information provided in relation to Examples 1, 2 or 3 which would indicate whether the primary insomnia patients studied experienced non-restorative sleep.
212 With regard to Example 1, while Professor Wheatley noted in his affidavit that he did not understand the intended meaning of “restorative value of sleep”, he said that the study did not include any data to establish the reason for the enhanced daytime vigilance observed in primary insomnia patients. He said that he did not consider that it was possible, in August 2001, to draw any firm conclusions as to the efficacy of melatonin on the “restorative value” of sleep in the absence of a defined measure of “restorative sleep” and data establishing the statistical significance of the results for that measure as compared to placebo.
213 As to Example 2, Professor Wheatley noted that the qualitative measurements used to assess the quality of sleep were open to different interpretations by patients and could be associated with both quantitative and qualitative aspects of sleep. While Professor Wheatley agreed that melatonin was shown to significantly improve the subjective assessment of the restfulness of sleep and the subjective assessment of daytime fatigue, he said that the data did not establish a link between these two parameters. He therefore considered that the stated conclusion with respect to Example 2 was more of a hypothesis than a matter established by the data.
214 In relation to Example 3, Professor Wheatley observed that there was no reason given for the patients to be divided into two age groups (i.e., those aged 55 and over and those aged under 55). He noted that for the patients aged less than 55, there was a very large difference in the placebo response to the change in perceived quality of sleep and the change in perceived day time alertness. He also noted that the size of the placebo effect on the perceived quality of sleep in the patients aged less than 55 approximated to the size of the melatonin effect on the perceived quality of sleep in the patients aged 55 and over. With respect to the conclusion that “[t]hese results (Table 2) clearly indicate that melatonin was effective in primary insomnia related to non-restorative sleep, but can be detrimental to insomnia related to other aetiologies (e.g. sleep deficit due to inability to initiate sleep)” he considered that this conclusion was pure speculation and unsupported by Example 3. He suggested that it was also possible, for example, that the treatment improved sleep quantity and that this caused the reported subjective improvement in sleep quality and day time alertness.
215 Dr Behi did not consider that Example 3 demonstrated what the effect of melatonin on patients under the age of 55 years was. He considered that the trial failed to demonstrate anything meaningful in that regard. Dr Krapivensky was of the same opinion. She observed that there was no information provided about overall patient numbers, patient numbers in either group, or how many of them had primary insomnia characterised by non-restorative sleep. The latter observation is obviously correct, and is consistent with the evidence of Professors Wheatley and Glozier that none of the examples provide any indication of how many patients in each trial were suffering from primary insomnia characterised by non-restorative sleep.
216 Both Dr Krapivensky and Professor Roth suggested that there was an unusually high or exaggerated placebo response. Professor Roth regarded Example 3 as a “failed trial” and stated further clinical trials were needed to gain an understanding as to the effects of melatonin on patients under the age of 55 years. Professor Wheatley agreed with Professor Roth that Example 3 was a failed trial for patients under the age of 55 years. He considered that the data raised a hypothesis that melatonin is less effective in patients under 55 years of age and may in fact be detrimental, but that further trials would be required to investigate that question. Similarly, Professor Glozier considered that Example 3 raised the possibility that melatonin may have been harmful to patients in the younger group, but that further study would be required before drawing any firm conclusion in that regard.
217 With regard to Example 4, it is apparent that the study has nothing at all to say about improvements in the quality of sleep of any of the trial participants. There is nothing in the description of the methods or the results to suggest that the trial participants’ quality of sleep was assessed. Professor Roth and Dr Behi considered this study was directed to establishing the safety profile of the invention. Professor Glozier was of the opinion that Example 4 was “pretty much irrelevant” to the construction of the Patent and revealed nothing about the function of melatonin in the treatment of people with insomnia.
218 In their submissions the respondents placed considerable emphasis on the statement in the Example 4 conclusion that “improvement in quality of sleep reported by patients … does not necessarily indicate enhanced restorative sleep, since it is not associated with improved daytime vigilance”. This statement was said by the respondents to amount to an express rejection of the proposition that an improvement in perceived quality of sleep necessarily indicates enhanced restorative sleep, unless it is associated with improved daytime vigilance.
219 The Patent includes an express statement concerning the lack of evidence that melatonin “would be likely to improve the restorative quality of sleep in subjects affected by primary insomnia characterized by non-restorative sleep”. It then states that the inventors have found that melatonin “improves the restorative quality of sleep in subjects suffering from primary insomnia”. Taking these statements together, it is apparent that the inventors found that in individuals suffering from primary insomnia characterised by non-restorative sleep, melatonin could improve the restorative quality of their sleep. There is a question that will require further consideration as to the scope of that finding and whether it relates only to elderly patients (aged 55 or over) or whether it also applies to younger patients suffering from primary insomnia. I will return to this topic when considering the respondents’ lack of fair basis case.
220 Non-restorative sleep is a symptom of primary insomnia under Criterion A in DSM-IV. It is clear that the Patent is representing that, in accordance with the inventor’s finding, non-restorative sleep experienced by an individual suffering from primary insomnia may be relieved by the administration of melatonin. In this context, the phrase “restorative quality of sleep” as used in the claims is to be understood as referring to a subjective report of the patient that their sleep is restorative in the sense that it is refreshing. It is assessed on the basis of subjective reports of the patient rather than objective measures such as those used to assess sleep onset, sleep maintenance and sleep duration. The phrase “improving the restorative quality of sleep” as used in the claims is to be understood as referring to a subjective report of the patient that the restorative quality of their sleep has improved.
221 The stated conclusion in Example 4 is puzzling, but I do not think it provides a sound basis for rejecting the interpretation of the phrase “improving the restorative quality of sleep” adopted by the experts in JER 1 which in my opinion reflects the preferable construction of that phrase as used in the claims.
222 The respondents admit that each of the Generic Partners Products:
(a) comprises tablets containing 2 mg of melatonin;
(b) is in unit dosage form;
(c) is indicated as monotherapy for the short term treatment of primary insomnia characterised by poor quality of sleep in patients who are aged 55 years or over;
(d) is adapted for oral administration;
(e) is a prolonged release formulation; and
(f) contains at least one pharmaceutically acceptable diluent, preservative, antioxidant, solubilizer, emulsifier, adjuvant or carrier, and includes an acrylic resin.
223 Neurim alleges that each of the respondents is liable for infringement of the method of treatment claims 4 to 7 under ss 117(2)(b) and 117(2)(c) of the Act and the Swiss-style claims 1 to 3 under s 13(1) of the Act. Further, or alternatively, Neurim also alleges that each of the respondents have infringed the same claims by authorisation and common design.
224 For reasons previously explained, the claims of the Patent are all purpose limited by the requirement that the medicament or method be manufactured or used for the purpose of treating a patient suffering from primary insomnia characterised by non-restorative sleep. In the case of the method of treatment claims, there could only be a direct infringement where the patient has been diagnosed with primary insomnia characterised by non-restorative sleep and the method is used for treatment of that condition and improving the restorative quality of the patient’s sleep. Those claims are not infringed by a medical practitioner who prescribes melatonin as a treatment for some more generalised complaint in which the patient’s subjective complaint was of lack of sleep as opposed to unrefreshing quality of sleep. It follows that a medical practitioner who prescribes melatonin for the purpose of helping a patient get to sleep or stay asleep, does not use the invention of the claims. Whether or not melatonin has been prescribed or recommended on the basis of a diagnosis of primary insomnia characterised by non-restorative sleep must be determined as a matter of substance (i.e., the relevant diagnosis need not be made or articulated in those exact terms).
225 Section 117 of the Act provides:
117 Infringement by supply of products
(1) If the use of a product by a person would infringe a patent, the supply of that product by one person to another is an infringement of the patent by the supplier unless the supplier is the patentee or licensee of the patent.
(2) A reference in subsection (1) to the use of a product by a person is a reference to:
(a) if the product is capable of only one reasonable use, having regard to its nature or design—that use; or
(b) if the product is not a staple commercial product—any use of the product, if the supplier had reason to believe that the person would put it to that use; or
(c) in any case—the use of the product in accordance with any instructions for the use of the product, or any inducement to use the product, given to the person by the supplier or contained in an advertisement published by or with the authority of the supplier.
226 The issues that arise under s 117 are as follows:
(a) whether Melotin is a staple commercial product (s 117(2)(b));
(b) if the answer to the question above is “no”, whether the respondents have reason to believe that Melotin will be prescribed or recommended by medical practitioners for use by patients as a treatment for primary insomnia characterised by non-restorative sleep to improve the restorative quality of their sleep (s 117(2)(b));
(c) whether the respondents have provided any instructions or inducement to use Melotin as a treatment for primary insomnia characterised by non-restorative sleep to improve the restorative quality of sleep (s 117(2)(c)).
227 Neurim submitted that Melotin (which is for present purposes equivalent to Circadin) is not a staple commercial product.
228 The active ingredient in Melotin is melatonin and the name of the medicine as specified in the relevant product information is melatonin. Melotin also includes various excipients used for the purpose of producing a stable modified release tablet. There may be a question as to whether the relevant product in this case is melatonin and not the particular form in which it is produced (i.e., Melotin). However, I consider Neurim is correct in submitting that the question whether Melotin is a stable commercial product does not depend in this case on which approach is adopted.
229 Section 117 was considered by the High Court in Northern Territory of Australia v Collins (2008) 235 CLR 619 (“Collins”). Both Hayne J and Crennan J each gave detailed reasons concerning the scope and operation of s 117 and the “staple commercial products” exception to s 117(2)(b). Hayne J said at [41]-[43]:
[41] I agree with Crennan J that a staple commercial product is one that is supplied commercially for various uses. While I agree with her Honour that this does not mandate an inquiry into whether there is “an established wholesale or retail market”, I greatly doubt that a product could be described as a “staple commercial product” if there were not some market for its sale for various uses. The doubt lies in the fact that the product must be a commercial product and that, to be a “staple commercial product”, it must be an article of commerce that not only can be used in a variety of ways but also is traded for use in various ways …
[42] The phrase “staple commercial product” must be read as a whole and it must take its meaning from the context in which it sits. In particular, it is to be recalled that s 117 creates a liability in a supplier of a product where the act of supply would otherwise not infringe a patentee’s rights. Section 117 imposes liability on the supplier if use of the product supplied by the person to whom it is supplied would infringe.
[43] In this setting “staple commercial product” should not be given a narrow meaning. To do so would expand the classes of supply which are reached by s 117, thus expanding the rights of the patentee where, by hypothesis, the act of supply is not otherwise an infringement of the patentee’s monopoly. Further, the meaning given to “staple commercial product” must recognise that the central focus of s 117 falls upon the use of a product. The construction of the section must be approached with these two matters at the forefront of consideration.
(Footnotes omitted)
230 His Honour referred to the drafting history of s 117, and the 1984 report of the Industrial Property Advisory Committee (“the IPAC report”). His Honour said at [48]-[50]:
[48] To read “staple commercial product” as identifying a product that is supplied commercially for various uses does not reflect the notion of principal or chief importance sometimes conveyed by the adjective “staple”. But as Crennan J concludes, “staple”, used adjectivally in the compound expression “staple commercial product”, should not be read as directing attention to the economic significance of the product concerned. Rather, it should be read as inviting attention to the variety of uses to which the product both can be, and is in fact, put. It is that variety of uses which, when the product is supplied commercially, makes the product a staple commercial product.
[49] As the reasons of Crennan J show, this construction of the provision is not inconsistent with the desire, expressed in the government’s published response to the [IPAC report], to harmonise Australian patent law with the laws of Australia’s major trading partners. But, as those reasons also show, the laws of the United States of America and the United Kingdom relating to indirect infringement are each expressed in terms that differ in important respects from s 117. There is, therefore, only limited assistance to be gained from considering the expressed desire for harmony with major trading partners.
[50] It may be thought that to read “staple commercial product” as identifying a product that is supplied commercially for various uses leaves little effective work to be done by s 117(2)(b). In particular it can be observed that cases of “only one reasonable use” are dealt with in s 117(2)(a), and yet many cases in which a product has various uses will not fall within s 117(2)(b). The resolution of this apparent tension between the two provisions lies in the recognition that s 117(2)(a) is concerned with a product capable of only one reasonable use, whereas “staple commercial product” takes its operation from what is seen to occur in the market-place. The two paragraphs pose radically different questions. The question posed in s 117(2)(a) is: For what can the product be used? By contrast, the question posed in s 117(2)(b) is: To what uses is the product in fact put? If it is in fact supplied commercially for various uses, it is a staple commercial product and the supplier of such a product is not to be held liable as an infringer because the person to whom the product is supplied uses it in a way that infringes, even if the supplier has reason to believe that it may be used in that way. Reading the provision on this basis would bring within the reach of s 117(2)(b) the supply, for example, of a product previously traded for only one use where the supplier has reason to believe that it will be used for a new and infringing use. It would leave beyond the reach of s 117 the supply of a product that has previously been traded for various uses unless the supply falls within s 117(2)(c) – where the supplier instructs or induces a particular use which infringes, or advertises the product for that use.
(Footnote omitted)
231 Justice Crennan considered the meaning of the expression “staple commercial product” at [138]-[145]. Her Honour said at [142]-[145]:
[142] The precise scope of the expression “staple commercial product” is not clear. One ordinary adjectival use of “staple”, applied to raw materials, conveys the meaning that the material is capable of being used as a constituent element in a number of other products. That focuses on the inherent qualities of the product. Another equally well-known ordinary adjectival use of “staple” conveys the meaning that a product has a foremost place among products, for example, in a particular location. That focuses on the distribution of a product rather than upon its inherent capacity to be a constituent in a number of other products and overlaps with the idea that the product be a “commercial” product.
[143] It has been suggested by at least one writer in respect of European rights that a “staple commercial product” has two main qualities: first, it must be “[a] basic product commonly used for various purposes”, and secondly, it must be “[g]enerally available on the market”.
[144] Raw materials such as wool or timber undoubtedly have the first quality. As to the second quality, it is necessary to recognise that s 117(2)(b) operates to limit liability for contributory infringement. Policy arguments in favour of imposing liability for contributory infringement are much weaker with a product that has significant non-infringing uses. The legislative intention evinced in the statutory language, and apparent also from the relevant secondary materials, is to except from liability, the supply of products with significant non-infringing uses, or as it has been put in relation to the American provisions, products with “lawful as well as unlawful uses”. A preference for such a construction has also been essayed in respect of s 60(3) of the Patents Act 1977 (UK) by a writer who states “the intention is to stop material particularly adapted to the use of an invention being made available to a putative infringer, but that material which has and, importantly, had, a general purpose of more than de minimis utility, falls within the [UK] exception.”
[145] The phrase “staple commercial product” means a product supplied commercially for various uses. This does not mandate an inquiry into whether there is “an established wholesale or retail market” or into whether the product is “generally available” even though evidence of such matters may well be sufficient to show that a product is a “staple commercial product”. The relevant inquiry is into whether the supply of the product is commercial and whether the product has various uses …
(Footnotes omitted)
Justice Heydon agreed with Crennan J’s reasons with respect to the operation of s 117(2)(b) of the Act.
232 Collins was applied by the Full Court in AstraZeneca AB v Apotex Pty Ltd (2014) 226 FCR 324 (“AstraZeneca FFC”). In that case the Full Court was not satisfied that rosuvastatin was a staple commercial product. The Full Court said at [429]-[431]:
[429] In argument before us, the generic parties placed considerable reliance on the judgment of Crennan J in Collins at [145]. Her Honour said that the phrase “staple commercial product” means “a product supplied commercially for various uses”. Hayne J (at [41]) and Heydon J (at [57]) agreed. However, Crennan J’s statement must be read in its proper context including the factual setting in which it came to be made. Collins involved the supply of a species of timber which Crennan J acknowledged at [143]-[144] constituted “[a] basic product commonly used for various purposes”.
[430] Whether a product meets that description is a question of fact. Considerations relevant to the question whether a product is a staple commercial product include how widely the product is used and for what range of purposes. In a passage in Thorley S, Miller R, Burkill G, Birss C and Campbell D, Terrell on the Law of Patents (16th ed, Thomson Sweet & Maxwell, 2006) at [8-37] referred to in a footnote to Crennan J’s judgment at [144] the learned authors, referring to the use of the expression “staple commercial product” in s 60(3) of the Patents Act 1977 (UK), state:
The use of the word “staple” is presumably a reference to raw materials or other basic products commonly available and with a multitude of possible applications, and the purpose of the subsection is to protect the supplier of such products even if he has knowledge that they are to be put to an infringing purpose. The scope of the words is far from clear and the dividing line between protecting the supplier of raw materials on the one hand and giving a fair monopoly to the patentee must be a question of fact in each case.
The authors of the IPAC report referred (at paragraph 14.2) to the undesirability of preventing a person from selling “a staple commodity with a wide variety of possible uses” suggesting that they also considered that a staple commodity was one that had a wide range of uses.
[431] We are not satisfied that rosuvastatin is a staple commercial product. The fact that it may be used for both infringing and non-infringing purposes is not conclusive. There are many products capable of being used for both infringing and non-infringing purposes that cannot be characterised as either raw materials or basic products commonly used for a variety of purposes. The uses to which rosuvastatin may be put appear to us to be limited to the prevention or treatment of cardiovascular disease and its associated risk factors (eg, high cholesterol). This is apparent from the evidence of Dr Wilson, a cardiologist called by AstraZeneca, who said that he does not prescribe rosuvastatin (or any other statin) for any indication other than cardiovascular disease or its associated risk factors. It is true that Dr Hay, a general practitioner called by AstraZeneca, gave evidence that he also prescribes rosuvastatin for the treatment of conditions such as cerebrovascular disease, chronic renal disease and diabetes. However, as we read his evidence, rosuvastatin is prescribed by Dr Hay in order to prevent or treat cardiovascular disease in situations where there is increased risk of it occurring due to the existence of these conditions.
233 The respondents submitted that the statutory words “staple commercial product” refer to a product that is supplied commercially for a substantial non-infringing use or uses. They submitted that the statutory words should not be given a narrow meaning because, as Hayne J observed in Collins at [43], they are used within a provision that confers liability upon a supplier of a product where the act of supply could not otherwise constitute an infringement. They submitted that it is the variety of uses for which that product can be, and in fact is supplied commercially, that will determine whether the product is a staple commercial product.
234 The respondents also submitted that Crennan J in Collins should be understood as rejecting a construction of “staple” as being confined to raw materials, favouring instead a “significant non-infringing uses” analysis at [142]-[145], and that Hayne J’s analysis was essentially to the same effect. They submitted that the Full Court’s reasoning in AstraZeneca FFC at [431] was inconsistent with Crennan J’s and Hayne J’s analysis and that the Full Court’s conclusion that “the uses to which rosuvastatin may be put … appear to be limited to the prevention or treatment of cardiovascular disease and its associated risk factors” considered the question of multiple uses at too high a level of abstraction. The respondents said that it is necessary to focus on the extent to which the product in issue is used for non-infringing purposes.
Analysis
235 All the experts agreed, in JER 1, that they either would or did prescribe Circadin in clinical practice for the TGA approved indication, as a monotherapy for the short-term treatment of primary insomnia characterised by poor quality of sleep, in patients aged 55 or over. Both Dr Behi and Dr Krapivensky gave evidence that they prescribe Circadin to patients who they diagnose as suffering from primary insomnia characterised by non-restorative sleep. However, Professor Glozier’s evidence establishes that psychiatrists also prescribe Circadin for its hypnotic effect in order to assist patients getting to sleep. However, Professor Glozier does not prescribe Circadin as a hypnotic, and almost only prescribes Circadin for use in the treatment of circadian rhythm disorders. Dr Krapivensky also indicated that she might have, at times, prescribed Circadin for circadian rhythm disorders, but that it was less effective than melatonin compounded at higher doses. Dr Behi also prescribes Circadin to treat children suffering from insomnia associated with neurodevelopmental disorders, and Professor Glozier was aware of the practice of prescribing Circadin to young people with neurodevelopmental disorders such as autism. Professor Glozier also stated (in JER 1) that he was aware Circadin was prescribed for people with any kind of insomnia, whether primary or not, and as a cheaper way of obtaining melatonin compared to obtaining it through a compounding pharmacy.
236 With regard to evidence given by Dr Behi and Dr Krapivensky to the effect that they regularly prescribe Circadin to treat primary insomnia characterised by non-restorative sleep, I have approached that evidence with some caution. While I accept that each of them does prescribe Circadin for that indication, I am not persuaded that they would make a diagnosis of primary insomnia characterised by non-restorative sleep as often as their evidence suggested.
237 Most insomnia is associated with a related medical condition (e.g. sleep apnoea) or psychiatric disorder (e.g. depression). Many insomnia diagnoses made by psychiatrists will be associated with a related psychiatric disorder. DSM-5 states that individuals with insomnia disorder frequently have a comorbid mental disorder, including, in particular, bipolar, depressive and anxiety disorders. According to DSM-5, difficulty maintaining sleep is the most common single symptom of insomnia with difficulty initiating sleep the next most common, and that a combination of those symptoms represents the most common presentation overall. However, DSM-5 also states that non-restorative sleep is a common sleep complaint that usually occurs in association with difficulty initiating or maintaining sleep or, less frequently, in isolation.
238 DSM-5 no longer provides for a diagnosis of primary insomnia and instead includes diagnostic criteria for what is referred to as insomnia disorder, which can, broadly speaking, include insomnia not adequately explained by comorbid medical conditions or mental disorders. DSM-5 notes if a complaint of non-restorative sleep occurs in isolation (i.e., in the absence of difficulty initiating or maintaining sleep) then a diagnosis of “other specified insomnia disorder” or “unspecified insomnia disorder” is made, assuming all other diagnostic criteria for insomnia disorder are met. In this respect, non-restorative sleep is the defining feature of a diagnosis of “other specified insomnia disorder” or “unspecified insomnia disorder” under DSM-5.
239 Professor Glozier said in Glozier 1:
[I]t remains the case that psychiatrists will rarely see a patient with insomnia that is not co-morbid with a psychiatric disorder. I am aware of this through discussions with psychiatrist colleagues, where issues of sleep are typically discussed in the context of psychiatric issues, and also through my participation in the running of workshops and seminars that are attended by GPs, psychiatrists, psychologists, physicians in other specialities and pharmacists. These workshops and seminars relate to subjects that include insomnia, sleep health, mood health, cognition and the correlation between these matters. Also, I am aware generally that the major sleep centres or clinics in Australia do not typically have a psychiatrist on staff. Rather, the clinics are staffed by specialist sleep physicians and sleep psychologists. Further, I know through my current involvement in writing the post-graduate professional training course for psychiatry for the Royal Australian and New Zealand College of Psychiatrists that insomnia is not a unit of specialist training in psychiatry in Australia. As a psychiatrist with a particular interest in sleep, it is uncommon even for me to be referred patients with insomnia that is not associated with a psychiatric disorder.
240 Professor Glozier understands non-restorative sleep, in the sense the term is used in DSM-IV, to mean sleep which is “restless, light or of poor quality” or, more generally, as a subjective patient complaint of not feeling restored or refreshed by sleep. He has seen patients who experience non-restorative sleep but who do not report any difficulty initiating or maintaining sleep. However, he says that this condition is usually attributable to a related condition such as sleep apnoea or restless legs, which would exclude a diagnosis of primary insomnia under the DSM-IV. Professor Glozier has rarely seen a patient suffering from primary insomnia and an isolated complaint of non-restorative sleep. Moreover, he does not agree with Dr Behi and Dr Krapivensky that non-restorative sleep and poor quality sleep are equivalent conditions. In his opinion, patients who experience difficulty initiating or maintaining sleep suffer from poor quality sleep, and almost certainly will not feel satisfied with or refreshed by their sleep. In his opinion, non-restorative sleep may be an indicator of poor quality sleep, but they are not the same thing. He considers that sleep quality is a much broader concept than non-restorative sleep and reflects how satisfied a patient is with one or more aspects of their sleep.
241 I consider that a diagnosis of primary insomnia under DSM-IV is not one that would be made by psychiatrists very often, and I consider a diagnosis of primary insomnia under DSM-IV that singles out non-restorative sleep (as opposed to difficulty initiating or maintaining sleep) to be relatively uncommon. Similarly, I would consider a diagnosis by psychiatrists of “other specified insomnia disorder” or “unspecified insomnia disorder” under DSM-5 to be one that is even less common, given that such a diagnosis requires a complaint of non-restorative sleep in the absence of difficulty initiating or maintaining sleep. In arriving at this conclusion, I have given considerable weight to the evidence of Professor Glozier that it is uncommon for him, even as a psychiatrist with a particular interest in the treatment of sleep disorders, to be referred patients with insomnia not associated with a psychiatric disorder.
242 Professor Wheatley prescribes melatonin to patients with primary insomnia, particularly those who complain primarily of difficulty with falling asleep, because of its hypnotic qualities. He does not understand the term poor quality of sleep in the approved indication and the PI to mean non-restorative sleep. The PI for Melotin would not be understood by Professor Wheatley or, I infer, other sleep physicians who do not have a background in psychiatry, as directing that they use Melotin as a treatment for primary insomnia characterised by non-restorative sleep. While they may make a diagnosis of primary insomnia (in the sense that term is understood by Professor Wheatley) that would be a relatively infrequent occurrence.
243 So far as general practitioners are concerned, Professor Glozier’s evidence included some analysis of the extent to which various clinicians (general practitioners, sleep physicians and psychiatrists) treat patients with insomnia. His evidence (which I accept) was that general practitioners are the predominant group treating patients with insomnia. There is no evidence to suggest that general practitioners would understand the PI or the approved indication to direct that they prescribe Melotin for the treatment of primary insomnia characterised by non-restorative sleep. Associate Professor Rawlin does not use the term “primary insomnia” in the course of diagnosing or prescribing treatments for sleep difficulties. He understands the concept of “primary” as signifying the absence of an identifiable cause, and I infer that he would therefore understand primary insomnia to mean insomnia for which there was no identifiable cause. However, he does not understand the term “sleep quality” to have a technical or scientific definition. He views it as “a broad and subjective concept”. With regard to the approved indication, he understands the phrase “characterised by poor quality sleep” to be a very broad indication that can encompass many aspects of sleeping difficulties reported by patients. There is nothing in Associate Professor Rawlin’s evidence that suggests he would associate the term poor quality sleep with non-restorative sleep or that he would prescribe Circadin (or Melotin) for the treatment of primary insomnia characterised by non-restorative sleep.
244 Neurim submitted that evidence Associate Professor Rawlin gave of his clinical practices with regard to the diagnosis or treatment of sleep difficulties, or his understanding of the approved indication, were representative of his own prescribing practices, and his evidence did not support the view that such practices were representative of general practitioners more broadly. I do not accept that submission. Associate Professor Rawlin is a general practitioner of more than 30 years’ experience. His experience both as a general practitioner and as a researcher in relation to various aspects of general practice are described in his affidavit in considerable detail. There is nothing in his evidence to suggest that Associate Professor Rawlin’s understanding of the approved indication, including the meaning he attributes to the terms “primary insomnia” and “poor quality sleep” would not be representative of that of other general practitioners who are consulted by patients suffering from sleep difficulties and who prescribe melatonin to help those patients initiate or maintain sleep or to normalise their sleep patterns. Neurim did not cross-examine Associate Professor Rawlin or call any other general practitioner to give evidence either in chief or in reply. Associate Professor Rawlin’s evidence also suggests (and I find) that general practitioners frequently prescribe Circadin to promote sleepiness and sleep initiation, and to assist patients with specific issues related to sleep patterns such as shift workers or travellers suffering jet-lag. These are all uses outside the scope of the method of treatment claims.
245 The question is not whether the product has non-infringing uses, but whether it is a staple commercial product. This involves asking whether it is a product supplied commercially for various uses. There are various matters relevant to the question whether a use is infringing or non-infringing including matters of claim construction and validity, which will often have no bearing on the question whether a product is a staple commercial product. Contrary to the respondents’ submissions, I do not accept that the Full Court’s characterisation in AstraZeneca FFC of the uses to which rosuvastatin could be put was overly broad or otherwise inappropriate nor do I consider the reasoning in that case was in any respect inconsistent with what Crennan J or Hayne J said in Collins.
246 Collins was concerned with a species of timber commonly used for a wide variety of purposes (including in the production of mulch, potting mix and firewood, and as a constituent element in poles, fence posts, flooring and other things). By contrast, melatonin’s principal, if not sole, use is as a therapeutic treatment for sleep disorders of various kinds. The range of purposes for which the product is used is in this respect quite narrow. The present case is very different from both Collins and Hood v Down Under Enterprises International Pty Ltd (2022) 166 IPR 436, in which the relevant product (an essential oil) was used for a variety of therapeutic and non-therapeutic purposes including as an ingredient in a range of personal care products. The facts of this case more closely resemble Otsuka Pharmaceutical Co., Ltd v Generic Health Pty Ltd (No 4) (2015) 113 IPR 191 (“Otsuka”) in which Yates J found that an antipsychotic (aripiprazole) used for both infringing and non-infringing purposes was not a staple commercial product. In my opinion, melatonin is not a staple commercial product.
247 It is useful at this point to refer to a number of additional propositions relating to the interpretation and application of s 117(2)(b):
The onus is on the patentee to show that use of the product supplied would be infringing use. The language “reason to believe” implies that there will be a reasonable basis for such a belief. Whether or not that is so will depend upon the objective facts and circumstances disclosed by the evidence. Actual knowledge is not required. See generally Collins v Northern Territory (2007) 161 FCR 549 (“Collins FFC”) at [64]-[66] per French J, Generic Health v Otsuka (2013) 296 ALR 50 (Emmett, Greenwood and Bennett JJ) (“Otsuka FFC (No 1)”) at [35] per Emmett J, [103] and [106] per Bennett J, [221]-[230] per Greenwood J, and Otsuka at [192]-[197] per Yates J.
It is not necessary for the patentee to identify any particular person or persons who the supplier has reason to believe will use the product in an infringing manner: AstraZeneca FFC at [433]. In that case it was found that the respondents (suppliers of generic pharmaceuticals) had reason to believe that some consumers would engage in “tablet splitting” of the respondents’ product (in the 20 mg dose) and thereby infringe the relevant method of treatment claims of the “low dose” patent: AstraZeneca FFC at [439].
It has been held that s 117(2)(b) may apply in circumstances where the respondent has reason to believe that a not insignificant number of clinicians will use a product to perform a method of treatment that is within the scope of a method of treatment claim: Otsuka per Yates J at [246]. Aspects of his Honour’s analysis of the relevant law and its application to the facts of the case were the subject of a notice of contention raised by the respondents in that case but it was not necessary for the Full Court to consider those matters: Otsuka Pharmaceutical Co Ltd v Generic Health Pty Ltd (No 2) (2016) 120 IPR 431 (“Otsuka FFC (No 2)”) at [112] per Besanko and Nicholas JJ.
Section 117(2)(b) requires that the respondent have reasonable grounds to believe, at the time of supply, that the product will be put to an infringing use. It is not sufficient for the patentee to show that the products supplied by the respondent may be used in an infringing manner or that the respondent has reason to believe that the product may be used in an infringing manner: See Otsuka FFC (No 1) at [33] - [35] per Emmett J. For the patentee to succeed under s 117(2)(b) in this case, it must show that a not insubstantial number of persons to whom the product is supplied will use it as a method of treatment within one or more of the relevant claims.
The fact that the product supplied by the respondent may be used in a non-infringing manner does not prevent s 117(2)(b) applying, even if that manner of use is the most common form of use for the product and even though the infringing use is relatively uncommon. The extent to which the product is capable of non-infringing use, and the extent to which it is in fact used for non-infringing purposes, may be relevant to the remedies that may be granted by the Court for an infringement based on s 117(2)(b): Otsuka at [247] per Yates J. As the Full Court observed in relation to injunctive relief in AstraZeneca FFC at [444]:
It may be undesirable to impose a blanket restraint upon a supplier who has reason to believe that only some consumers, perhaps a very small minority, may put the product that is or may be supplied to them to an infringing use. This is because the effect of such an injunction may be to deny a supplier access to a market, and consumers’ access to a product, in circumstances where the supplier could have no reason to believe that the majority of consumers would put the product to an infringing use. It seems to us that, all other things being equal, the more difficult it is for the patentee to establish that there is a likelihood of widespread infringing use, the more difficult it should be for the patentee to obtain injunctive relief in the broad terms restraining any supply of the relevant product. In the present case, even if AstraZeneca established that the generic parties had reason to believe that some consumers would engage in infringing use, the likely scale of that activity, were it to occur, was not shown to be such as would justify the grant of the wide injunction that AstraZeneca sought. Given our conclusion in relation to the validity of claims of the 051 or low dose patent, it is not necessary for us to consider what other injunctive relief, if any, might have been appropriate in lieu of that sought by AstraZeneca.
Similar reasoning may apply in relation to other remedies (i.e., damages or account of profits) if a respondent had reason to believe that only a small proportion of the total quantity of products supplied would be put to an infringing use.
248 Neurim relied on evidence from Dr Behi and Dr Krapivensky that they prescribe melatonin to treat primary insomnia characterised by non-restorative sleep and, in doing so, improve the restorative quality of sleep in those patients. Neurim submitted that since this evidence was not challenged in cross-examination, nor disputed by the respondents’ experts, it should be accepted. It followed, according to Neurim, that the respondents have reason to believe that the Generic Partners Products will be put to an infringing use, at least by clinicians such as Dr Krapivensky and Dr Behi.
249 Neurim submitted that the respondents’ evidence, taken at its highest, is that some practitioners do not equate the term “quality of sleep” with “non-restorative sleep”. It submitted that this does not diminish the significance of the evidence of Dr Behi and Dr Krapivensky that they do in fact prescribe Circadin for primary insomnia characterised by non-restorative sleep. Neurim submitted that even if the Court finds that the respondents have reason to believe that a relatively small proportion of their product will in fact be used to treat primary insomnia characterised by non-restorative sleep, that is still sufficient for the whole of the supply to be infringing pursuant to s 117(2)(b).
250 The respondents submitted that Neurim must establish that, objectively, they had reason to believe that the Generic Partners Products would be used in a way that would infringe claim 1. The respondents submitted that nothing in the authorities suggests that it is sufficient for the purposes of s 117(2)(b) to demonstrate that one or more prescribers might use the product for the claimed method, because that would give the words “reason to believe” in s 117(2)(b) no work to do. I accept the respondents’ submissions in relation to those matters. The question is whether, objectively speaking, the respondents had reason to believe that their products would be put to an infringing use.
251 The respondents submitted that the objective evidence provided no reason to believe that Melotin would be put to an infringing use. They also submitted (at least implicitly) that Dr Behi’s or Dr Krapivensky’s prescribing practices are idiosyncratic and not shown to be representative of other psychiatrists who diagnose and treat patients suffering from primary insomnia.
Analysis
252 It should be inferred that a generic supplier of prescription medicines in Australia seeking to obtain ARTG approval for a generic prescription medicine on the basis of an existing ARTG approval of an originator’s product would be familiar with the indication for which the product is to be prescribed, and any Australian Public Assessment Record (“AusPar”) relating to the approved product. The AusPar is a publicly available document that provides information about the TGA’s evaluation of the prescription medicine and the considerations that led to approval. The AusPar for Circadin was published in December 2009.
253 Although melatonin was used to treat a variety of sleep related disorders, Circadin was approved for use in Australia by the TGA in accordance with the approved indication only. The TGA approval obtained for Melotin was for precisely the same indication as Circadin.
254 Primary insomnia was, at the time Neurim’s TGA approval was granted, a medical condition identified in both DSM-IV and ICD-10, both nosologies which I have discussed in detail above. The former included diagnostic criteria for primary insomnia that expressly distinguished between complaints of difficulty initiating or maintaining sleep and complaints of non-restorative sleep (defined to mean restless, light, or poor quality sleep). As I have found above, the diagnosis of primary insomnia under DSM-IV broadly corresponded with the diagnosis of nonorganic insomnia under ICD-10, which also expressly distinguishes between quantity and quality of sleep. According to ICD-10, the complaint associated with nonorganic insomnia is either of difficulty falling asleep or maintaining sleep, or of poor quality sleep. In this context, the term poor quality sleep is broadly synonymous with the term non-restorative sleep.
255 A reasonable person seeking approval for a prescription medication to be used in the treatment of primary insomnia characterised by poor quality sleep would be aware that it was likely that the medication would be prescribed by psychiatrists as a method of treating primary insomnia characterised by non-restorative sleep, diagnosed in accordance with DSM-IV. The AusPar for Circadin makes reference to DSM-IV in several places when describing selection criteria (“insomnia according to DSM-IV criteria”) for clinical studies relied on by the sponsor. Referring to the efficacy studies relied on, the AusPar states at p 43:
It is appropriate to restrict the indication to “poor quality of sleep” as there is no evidence that total sleep duration or time to onset of sleep is improved to a clinically significant extent by Circadin. Differences in quality of sleep could be detected by subjects with primary insomnia under controlled conditions so it is considered that degree of efficacy has been demonstrated. No safety concerns were apparent from short term use of Circadin.
The distinction drawn between quality of sleep and quantity of sleep (i.e., sleep duration and time to onset of sleep) is consistent with the distinction drawn in DSM-IV between complaints of non-restorative sleep and difficulty initiating or maintaining sleep.
256 Although DSM-5 does not use the term primary insomnia, the diagnosis of insomnia disorder under DSM-5 is made when a patient’s sleeping difficulties (i.e., initiating or maintaining sleep or early morning awakening with inability to return to sleep) are not explained by another sleep wake disorder, a mental disorder, or substance use. A complaint of non-restorative sleep may occur either with or without other sleep complaints, but when it occurs in isolation, the diagnosis under DSM-5 will be of “other specified insomnia disorder” or “unspecified insomnia disorder”. It follows that DSM-5 still provides for a diagnosis of a sleep disorder which would include primary insomnia in which the patient complains of poor quality sleep in the sense of non-restorative or unrefreshing sleep.
257 With regard to the evidence of Dr Behi or Dr Krapivensky, I am not persuaded that their prescribing practices are idiosyncratic or unlikely to be representative of other psychiatrists who diagnose and treat patients suffering from primary insomnia even though, as I have previously observed, their evidence may overstate the frequency with which they make that diagnosis. I am satisfied that their approach to the diagnosis and treatment of primary insomnia is likely to be representative of a significant number of other psychiatrists.
258 I am satisfied on the evidence that a reasonable person engaged in the supply of generic prescription medicines in Australia of a prescription medicine approved by the TGA for use in the treatment of primary insomnia characterised by poor quality sleep would have reason to believe that the medication would be prescribed by a not insignificant number of psychiatrists as a treatment for primary insomnia where the patient complained of non-restorative (or unrefreshing) sleep. In those circumstances, I am satisfied that Neurim’s infringement case based on s 117(2)(b) succeeds.
259 Neurim submitted that “primary insomnia characterized by poor quality of sleep” means the same as, or at the very least, is wholly encompassed by, the patented indication “primary insomnia characterized by non-restorative sleep” and that, consequently, all supply of the Generic Partners Products for the approved indication infringes the Patent pursuant to s 117(2)(c). For the purpose of considering this submission it is necessary to refer to the product information supplied with Melotin.
260 The product information document (“PI”) for Melotin is in terms that are relevantly the same as the PI for Circadin. For the purpose of determining infringement issues, it is necessary to have regard to the PI for Melotin which constitutes the relevant instruction or inducement for the purposes of s 117(2)(c). The question is whether the PI for Melotin amounts to an instruction or inducement to use Melotin as a treatment for primary insomnia characterised by non-restorative sleep. The PI for Melotin does not contain any statement to the effect that Melotin is not indicated for that condition: cf. Leflunomide HCA at [303].
261 The PI sets out the approved indication for Melotin, namely “[m]onotherapy for the short term treatment of primary insomnia characterized by poor quality of sleep in patients who are aged 55 or over”.
262 The PI describes the pharmacological actions of melatonin, including its mechanism of action and rationale for use, as follows:
Melatonin is a naturally occurring hormone produced by the pineal gland and is structurally related to serotonin. Physiologically, melatonin secretion increases soon after the onset of darkness, peaks at 2-4 am and diminishes during the second half of the night. Melatonin is associated with the control of circadian rhythms and entrainment to the light-dark cycle. It is also associated with a hypnotic effect and increased propensity for sleep.
Mechanism of action
The activity of melatonin at the MT1 MT2 receptors is believed to contribute to its sleep-promoting properties via their distinct actions on the circadian clock. The MT1 receptors are thought to inhibit neuronal firing, while the MT2 receptors have been implicated in the phase-shifting response.
Rationale for use
Because of the role of melatonin in sleep and circadian rhythm regulation, and the age related decrease in endogenous melatonin production, melatonin may effectively improve sleep quality particularly in patients who are over 55 with primary insomnia.
263 There are several points to make in relation to the discussion of pharmacological actions in the PI. First, there is reference made to the “control of circadian rhythms and entrainment of the light-dark cycle”. This is followed by the statement indicating that the activity of melatonin at the MT1 and MT2 receptors is believed to contribute to its sleep-promoting properties by actions on the circadian clock. This is clearly referencing the sleep-promoting attributes of melatonin through phase-shifting. Secondly, there is also a reference to melatonin’s association with “a hypnotic effect and increased propensity for sleep”. This statement is also referring to the sleep-promoting quality of melatonin. None of these statements directly suggest that melatonin has any effect on non-restorative sleep or that it is useful in the treatment of non-restorative sleep. Thirdly, the discussion concerning the rationale for use of melatonin also references its role in sleep and circadian rhythm regulation, in patients suffering from an age-related decrease in endogenous melatonin production. In that context, it is asserted that “melatonin may effectively improve sleep quality particularly in patients who are over 55 with primary insomnia”.
264 The PI does not include any definition of primary insomnia or cross-reference to any nosology that provides any definition of the condition. Nor does the PI provide any other information that might lead the reader (whether they be a sleep physician, a psychiatrist, a psychologist, a general practitioner or a patient) to infer that the reference to “quality of sleep” in the PI is synonymous with “non-restorative sleep”. In particular, the PI does not refer to “non-restorative sleep”, “restorative quality of sleep”, DSM-IV or any other nosology that uses those terms, or ICD-10.
265 The PI includes a section on pharmacokinetics and a summary of a number of clinical trials, which includes the following discussion:
Three Phase 3 studies and a sleep laboratory study were considered pivotal. These studies enrolled patients with primary insomnia who were aged at least 55 years. Patients suffering from severe neurological, psychiatric or neurosurgical diseases or taking CNS medications including benzodiazepines or other hypnotic agents were excluded.
266 The exclusion criteria applied appears to be aimed at ensuring that patients enrolled in the studies were suffering from primary insomnia in the sense that their insomnia was not caused by other conditions or drug use. There is no indication provided that patients were screened for the purpose of determining whether they experienced non-restorative sleep or that those whose primary insomnia was not characterised by non-restorative sleep were excluded from the study. In his affidavit evidence, Dr Behi asserted that he would expect many of the patients would have complained of non-restorative sleep both in insolation and in addition to a complaint of difficulty initiating and/or maintaining sleep. However, there is nothing that appears in the description of the studies which supports his supposition. There is nothing said about the trial designs which indicate that they were designed to measure the effect of melatonin on primary insomnia characterised by non-restorative sleep. It follows that there is nothing said in the PI regarding trial design that would indicate to a clinician reading the PI that the studies were aimed at assessing the effects of melatonin on primary insomnia characterised by non-restorative sleep.
267 The primary assessment tool used in the three clinical studies was the Leeds Sleep Evaluation Questionnaire (“LSEQ”). The PI states:
The primary assessment tool was the Leeds Sleep Evaluation Questionnaire (LSEQ), comprising 10 self-rated 100 mm-line analogue questions concerning aspects of sleep and early morning behaviour. The LSEQ measures ease of getting to sleep (GTS), quality of sleep (QOS), ease of waking from sleep (AFS) and behaviour following wakefulness (BFW). The primary outcome variable in the pivotal clinical trials was QOS, or a combination on QOS and BFW, where a patient had to show a clinically relevant improvement on both QOS and BFW. Time to onset of sleep and duration of sleep were measured objectively only in a polysomnography study. Efficacy of melatonin modified release tablets in combination with other hypnotic agents has not been assessed.
268 The passage extracted above is the extent of the information about the LSEQ provided. Professor Roth gave evidence that he was familiar with the LSEQ as an internationally recognised tool for assessing a change in a patient’s subjective perceptions about the efficacy of treatment. He said that LSEQ is used to measure treatment effects, primarily in clinical trials, rather than as a diagnostic tool. In particular, it is not used to diagnose a patient having primary insomnia characterised by non-restorative sleep. I will say more concerning LSEQ and Professor Roth’s evidence concerning this tool later in these reasons. The immediate significance of that evidence is that even a clinician who was familiar with LSEQ would not understand it to have been used for the purpose of determining whether patients enrolled in the trial were suffering from primary insomnia characterised by non-restorative sleep.
269 Another point to note is that melatonin is described in the PI as “associated with a hypnotic effect and increased propensity for sleep”. Professor Roth gave evidence that the scientific literature does not support the use of melatonin for the induction or maintenance of sleep in primary insomnia patients. He agreed with Professor Glozier that there was no strong evidence to support the use of melatonin as a hypnotic. On the other hand, Professor Wheatley gave evidence (which I accept) that he prescribes melatonin for treatment of primary insomnia, particularly for those patients who complain primarily about difficulty falling asleep, because of its hypnotic qualities. It is unnecessary to resolve this difference of opinion, although I would note that Professor Wheatley’s view would most likely be shared by many other medical practitioners. Although Professor Glozier gave evidence that he does not prescribe melatonin as a hypnotic based on his review of the clinical literature, he also gave evidence that many of his peers prescribe melatonin as a hypnotic for insomnia patients of all ages, primarily for the purpose of assisting patients to get to sleep.
270 Chapter 31 in Sleep Medicine (“Melatonin in the Regulation of Sleep and Circadian Rhythms”) refers to a number of studies in which daytime ingestion of melatonin improved sleep induction and sleep latency. The authors state that “[m]elatonin is a natural hormone that partially fits the definition of a hypnotic because it induces sleepiness and facilitates and can maintain sleep”. Based on Professor Wheatley’s and Professor Glozier’s evidence, I am satisfied that melatonin is widely prescribed by sleep physicians and psychiatrists for what they consider to be its hypnotic effect and to assist patients in getting to sleep. In any event, the PI itself suggests that melatonin is a hypnotic and the clinical studies referred to in the PI include reports of improvements in sleep latency of those taking melatonin. A clinician reading the PI would be likely to understand from the document that melatonin has sleep promoting qualities and therefore may reasonably be described as a mild hypnotic or (at least) an agent that has hypnotic qualities.
Polysomnographic study and clinical studies reported in the PI
271 The polysomnographic study reported in the PI assessed a number of objective elements of patients’ sleep including time to onset of sleep (i.e., sleep latency) which was reported to be significantly less for the treatment group than for the placebo group:
In a polysomnographic (PSG) study (N=40; 20 melatonin modified release tablets, 20 placebo) with a run-in of 2 weeks (single-blind with placebo treatment), followed by a treatment period of 3 weeks (double-blind, placebo-controlled, parallel group design) and a 3-week withdrawal period, time to onset of sleep was shortened significantly by 9 minutes compared to placebo. A statistically significant difference favouring melatonin modified release tablets was seen for total duration of time awake prior to sleep onset (approx change from 10 to 11 minutes for melatonin modified release tablets and from 21 to 20 minutes for placebo). There were no modifications of sleep architecture and no effect on REM sleep duration by melatonin modified release tablets. Modifications in diurnal functioning did not occur with melatonin modified release tablet 2 mg. [M]elatonin modified release tablets did not prolong the duration of sleep significantly compared to placebo.
It is apparent from this passage that the polysomnographic study referred to in the PI showed a statistically significant difference in sleep latency in favour of the treatment group when compared with the placebo group. On its face, that result would provide support for the use of melatonin in patients experiencing difficulty falling asleep. The results obtained in the clinical studies referred to in the PI also provide some support, at least on their face, for the use of melatonin in such patients.
272 Three clinical studies are briefly discussed in the PI. The first of the clinical studies is described as an outpatient study with a primary efficacy endpoint of QOS. The PI states:
In an outpatient study (Neurim VII: N=170; 82 melatonin modified release tablets, 88 placebo) with two week run in baseline period with placebo, a randomised, double blind, placebo controlled, parallel group treatment period of 3 weeks and two week withdrawal period with placebo, the primary efficacy endpoint was Quality of Sleep (QOS). The rate of patients who showed a clinically significant improvement in both quality of sleep and morning alertness was 47% in the melatonin modified release tablets group as compared to 27% in the placebo group. There was a mean difference of approximately 6 mm in quality of sleep and approximately 9 mm in morning alertness, both favouring melatonin modified release tablets compared to placebo. Sleep variables gradually returned to baseline with no rebound, no increase in adverse events and no increase in withdrawal symptoms.
273 In the second clinical study, a significant improvement in quality of sleep and morning alertness was reported for the treatment group compared to the placebo group. However, the PI also reports that time to onset of sleep was significantly improved in the treatment group compared to placebo. There is also a report of improved number of awakenings (i.e. fewer sleep interruptions) in the treatment group compared to placebo. The PI states:
In a second outpatient study (N=334; 169 melatonin modified release tablets, 165 placebo) with two week run in baseline period with placebo and a randomised, double blind, placebo controlled, parallel group treatment period of 3 weeks, the rate of patients who showed a clinically significant improvement in both quality of sleep and morning alertness was 26% in the melatonin modified release tablets group as compared to 15% in the placebo group. Melatonin modified release tablets shortened patients’ reported time to onset of sleep by 24.3 minutes vs 12.9 minutes with placebo. In addition, patients’ self-reported quality of sleep, number of awakenings and morning alertness significantly improved with melatonin modified release tablets compared to placebo. Quality of life was improved significantly with melatonin modified release tablet 2 mg compared to placebo.
274 The third clinical study measured the difference between the treatment and placebo groups in sleep latency (assessed using sleep diaries). What appears to be a statistically significant difference between the treatment and control groups was reported. The PI states:
A third study involved more than 600 patients over 55, over 400 of whom were on melatonin modified release tablets treatment for up to 6 months. Patients given melatonin modified release tablets demonstrated a difference from placebo in mean change from baseline in subjective sleep latency, assessed using a sleep diary, of -7.8 minutes after 3 weeks (p=0.014). Small differences in sleep latency were generally maintained over 13 weeks of placebo- controlled treatment.
The percentage of patients showing both remission of insomnia (PSQI of <6) and a clinically relevant improvement of 10% in quality of life scores (WHO-5 index) increased from 16.7% (cf. 10.6% placebo, p=0.044) at week 3 to 25.8% at week 13 (cf. 15.7% placebo, p=0.006).
…
275 Neurim submitted that the quality of sleep (QOS) component of the LSEQ is a tool known to measure efficacy for non-restorative sleep in primary insomnia patients. Neurim also submitted that it would be apparent to a person familiar with, or who looked up the LESQ, that the QOS component is a measure of poor sleep quality, in the sense that the patient complains that their sleep is non-restorative or non-refreshing. This was said to support the submission that the reference to poor quality sleep in the PI would be understood by the readers as referring to non-restorative sleep. There are several points to make about that submission.
276 Professor Roth’s evidence made clear that LSEQ is not a diagnostic tool. It is not used to determine if a patient is suffering from primary insomnia characterised by non-restorative sleep. In so far as Neurim is to be understood as suggesting that quality of sleep (QOS) referred to in LSEQ is synonymous with non-restorative sleep, then I would reject the submission on the basis that LSEQ does not purport to measure quality of sleep in that specific sense. The relevant questions in LSEQ, numbered 4 and 5, are as follows:
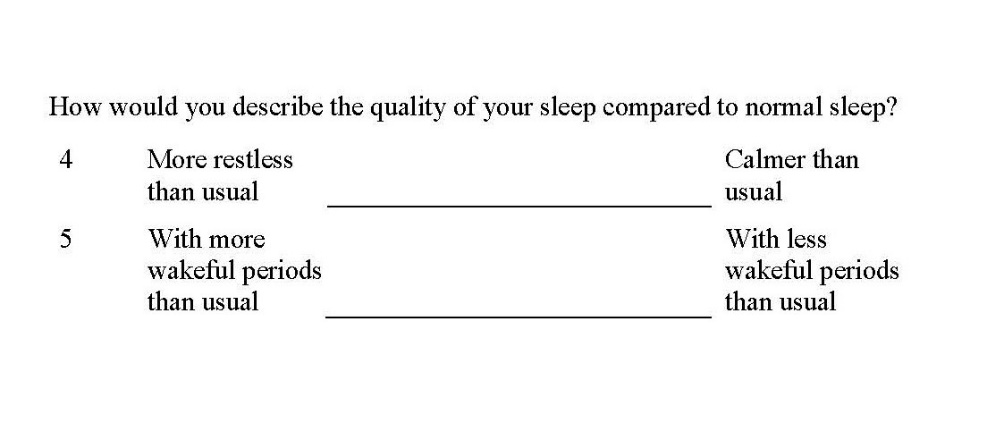
277 The question is not directed to ascertaining how restorative or refreshing the patient’s sleep is in the limited sense that Neurim says those terms should be understood. The question concerning QOS relates solely to “restlessness” and “wakeful periods”. The other questions in LSEQ are directed to GTS (Q1-3), AFS (Q6-7) and BFW (Q8-10).
278 Professor Glozier gave evidence that he understands QOS in the LSEQ to measure sleep quality related to the patient’s perception of how restless or calm their sleep is and whether it has more or less wakeful periods than usual. Referring to the PI for Circadin in Glozier 1 Professor Glozier said:
Based on the clinical studies described in the PI, I therefore expect that in using Circadin in accordance with the indication, that the particular components of sleep quality that were reported in the clinical trials would be improved compared to if I had used a placebo, and only in people aged over 55, and that this will improve the patients' overall sleep quality. In other words, that a patient's sleep quality will likely improve because it takes less time for the patient to get to sleep (i.e. improved sleep initiation), the patient will experience sleep they perceive to be calmer or less restless, the patient will have less time spent awake (i.e. improved sleep maintenance) and will feel more alert the next day.
279 Professor Roth contended that in patients suffering from primary insomnia, the QOS parameter measures whether there has been “an improvement in the patient’s quality of sleep (i.e. non-restorative sleep)”. I am not persuaded this is correct. I prefer Professor Glozier’s evidence on this point. It seems to me that the QOS parameter encompasses a number of aspects of sleep quality (i.e. periods of wakefulness; degrees of restlessness/calmness) that cannot be equated with the concept of non-restorative sleep. With regard to restlessness, the term is not defined in LSEQ, and can be understood as referring to either restlessness while awake or restlessness while asleep. LSEQ does not appear to be directed to distinguishing non-restorative sleep from other types of poor quality sleep (in the general sense of that term) or eliciting from the patient a complaint of non-restorative sleep. In my opinion, QOS is directed to quality of sleep in the broader sense, which takes into account restlessness and wakeful periods that occur following sleep initiation. It follows that I do not regard the fact that QOS was assessed using LSEQ as providing support for Neurim’s submission that “poor quality of sleep” as that term is used in the PI and the approved indication should be understood as referring to non-restorative sleep.
280 Neurim submitted that since the term “poor quality sleep” in the approved indication is used in the context of primary insomnia, many clinicians would understand this to refer to a specific diagnostic entity that gives meaning to the term “poor quality of sleep” as a diagnostic term equivalent to “non-restorative sleep”. In support of that submission, Neurim relied on evidence from Dr Behi and Dr Krapivensky. Dr Behi’s evidence was that since primary insomnia is a diagnostic entity derived from DSM-IV, he would understand the indication by reference to the insomnia complaints described in criterion A of the DSM-IV (which include non-restorative sleep). He reasoned that because non-restorative sleep is equivalent to a complaint of poor quality sleep in Appendix C to the DSM-IV, and the diagnosis of nonorganic insomnia in the ICD-10, he therefore understood the PI to be referring to non-restorative sleep each time it used the term poor quality of sleep. Dr Krapivensky said that it was clear to her that the the indication “primary insomnia characterized by poor quality of sleep” means primary insomnia according to the DSM-IV diagnostic criteria, characterised by non-restorative sleep. She maintained that in the DSM-IV diagnostic context, poor quality sleep and non-restorative sleep were equivalent. She reasoned (in evidence admitted as submission) that if the approved indication was intended to refer to poor quality sleep in some broader sense (i.e., including difficulty initiating or maintaining sleep) then other language would have been used.
281 I have previously referred to statements and information disclosed in the PI that suggest the terms sleep quality and poor quality sleep are to be understood as referring to the effects of various sleep variables, including sleep duration and sleep latency. The PI does not refer to DSM-IV and I am not persuaded that sleep physicians or general practitioners who are consulted by patients suffering from sleep difficulties would interpret the PI or the approved indication by reference to either DSM-IV or ICD-10, or that they would interpret the approved indication as referring to primary insomnia characterised by non-restorative sleep. In my opinion, neither sleep physicians nor general practitioners would be likely to understand the approved indication to mean primary insomnia characterised by non-restorative sleep.
282 So far as the evidence of Dr Behi and Dr Krapivensky is concerned, I accept that they interpret the approved indication by reference to DSM-IV and that they equate primary insomnia characterised by poor quality sleep with a diagnosis under DSM-IV of primary insomnia, characterised by non-restorative sleep. Their evidence on this topic was criticised by the respondents (at least implicitly) as not likely to be representative of other psychiatrists. It was also submitted that their affidavit evidence on this topic was elicited after they were first shown the Patent, which refers to the definitions of primary insomnia in DSM-IV and nonorganic insomnia in ICD-10. The submission was, in effect, that their evidence as to the interpretation of the approved indication was influenced by their prior exposure to the Patent and the views they formed as to its meaning, without sufficient regard to the PI.
283 I have considered the respondents’ criticism of Dr Behi’s and Dr Krapivensky’s evidence and the possibility that their views have been shaped as a result of each having been shown the Patent prior to giving evidence about the meaning of the approved indication. I am not persuaded that their views as to the meaning of the approved indication would be any different were they not aware of the Patent. I consider that their views reflect their understanding of DSM-IV. It is the only nosology referred to in their evidence that provides for a diagnosis of primary insomnia. That fact is central to their thinking and is what directs their thought processes to DSM-IV and the distinction drawn between complaints of difficulty initiating or maintaining sleep or poor quality sleep (in the sense of non-restorative sleep). I would regard Dr Behi and Dr Krapivensky as representative of a cohort of psychiatrists familiar with DSM-IV who would from time to time make a diagnosis of primary insomnia as defined by that nosology. This cohort of psychiatrists would equate the reference to primary insomnia in the approved indication as a reference to primary insomnia as defined by DSM-IV, and the reference to poor quality sleep in the approved indication as a reference to non-restorative sleep.
284 Professor Glozier is in my view representative of another cohort of psychiatrists who would have a different understanding of the approved indication and who would not necessarily equate poor quality sleep with non-restorative sleep. There was no evidence that Professor Glozier had ever prescribed melatonin as a treatment for primary insomnia characterised by poor quality sleep. He explicitly stated, in Glozier 1, that he did not prescribe melatonin as a treatment for patients with an isolated complaint of non-restorative sleep. To the extent that evidence left open any possibility that he prescribed melatonin for primary insomnia of any other kind (including characterised by poor quality sleep), he explained later in Glozier 1 that he almost only prescribes Circadin for use in patients with circadian rhythm disorder of all ages. In JER 1, he is recorded as agreeing that he does or would prescribe Circadin for the approved indication. However, it is apparent from his evidence that he has never done so. To the extent his answer in JER 1 indicated that he would do so, it is not at all apparent whether in giving that answer, he was equating “poor quality sleep” with “non-restorative sleep”. His answer in JER 1 is in my opinion of little assistance in determining whether he or any other clinician would be likely to prescribe melatonin for the patented (as opposed to the approved) indication. I make the same observation in relation to Professor Wheatley’s answer to the same question in JER 1.
285 Neurim placed considerable reliance on the oral evidence given by Professor Glozier who was said to have agreed with the proposition that “the patented indication is wider than and wholly encompasses the approved indication”. That is to say, Neurim contended that non-restorative sleep is a broader concept than poor quality sleep and that the latter is a subset of the former.
286 I will say more about Professor Glozier’s evidence shortly, but it is significant that this interpretation of the approved indication to the effect that it was broader than the patented indication, does not find any support in the evidence of Dr Behi or Dr Krapivensky. Relying on the evidence of Professor Glozier, Neurim submitted that “all uses for the TGA approved indication would amount to infringing use”.
287 It is desirable that I reproduce in full relevant parts of Professor Glozier’s oral evidence on this topic. Professor Glozier was referred by Mr Shavin QC (Senior Counsel for Neurim) to the approved indication as set out in the PI. The questioning continued as follows:
MR SHAVIN: And you see there:
Monotherapy for the short-term treatment up to three weeks of primary insomnia, characterised by poor quality of sleep, in patients who are aged 55 and over.
PROF GLOZIER: Yes.
MR SHAVIN: And so what we have there, you would understand – you would understand that, wouldn’t you, as a therapy for improving the restorative quality of sleep in a patient suffering from primary insomnia characterised by non-restorative sleep.
PROF GLOZIER: No. I have explained quite clearly why I don’t see non-restorative sleep or sleep quality as being completely synonymous.
…
MR SHAVIN: Do you recall a discussion earlier today where we discussed the appearance of the words “quality of sleep” in the DSM-IV in the context of primary insomnia and non-restorative sleep?
PROF GLOZIER: I do.
…
PROF GLOZIER: … this is where [I] state that, poor quality of sleep is one of the examples of non-restorative sleep and therefore not synonymous with.
MR SHAVIN: No. But encompassed by.
[objection taken but withdrawn]
MR SHAVIN: Professor Glozier, I – I believe that the question was to the effect that poor quality of sleep is encompassed in the DSM by non-restorative sleep.
PROF GLOZIER: That is my understanding. Therefore I do not think you can make the equation that you made earlier on that the two are the same thing.
MR SHAVIN: Right. Let me explore - - -
HIS HONOUR: In – you mean by that, in this – as expressed in this indication?
PROF GLOZIER: Correct.
MR SHAVIN: Would you accept that, when you have in this indication, primary insomnia characterised by poor quality of sleep, the poor quality of sleep is something encompassed within the symptom non-restorative sleep?
PROF GLOZIER: I think that is a reasonable statement. Yes.
MR SHAVIN: Yes. Thank you.
HIS HONOUR: Well, can I – I just want to make sure I understand that. You – do you say, poor quality of sleep is a subset of restorative sleep or is it the other way around? I – I’m not following.
PROF GLOZIER: It’s a – I – my reading of DSM-IV, and I know others differ, is that - - -
HIS HONOUR: No. I’m – sorry, I’m asking about the indication. …
PROF GLOZIER: So – so the indication is that this would be a subset. Yes. In this particular case.
HIS HONOUR: Non-restorative sleep.
PROF GLOZIER: That would be my – the – my problem is – is that primary insomnia is a – is – is the hybrid nature of this, means I don’t know whether to draw quality of sleep, as used in DSM-IV where I read it as a subset of non-restorative sleep or as in ICD-10 where it forms, very clearly, the third of the three diagnostic criteria. That’s – and - - -
HIS HONOUR: Mr Shavin, just so – I’m sorry – just so I – I can follow this, are you putting to the witness that in relation to this indication, non-restorative sleep is a subset of poor quality of sleep? Or were you putting the – the converse?
MR SHAVIN: The converse, your Honour.
…
PROF GLOZIER: And I – and I – and I would agree that my interpretation would be the converse.
…
MR SHAVIN: I think that Professor Glozier and I understand each other but I want to make sure that the transcript is clear. If I put it in this way: a monotherapy for the short-term treatment of primary insomnia, characterised by poor quality of sleep, in patients who are aged 55 years or over, would be a subset of a monotherapy for the short-term treatment of primary insomnia, characterised by non-restorative sleep in patients who are aged 55 years or over.
PROF GLOZIER: That’s a proposition I can agree with, Mr Shavin.
288 I was at first perplexed that Professor Glozier was so willing to accept that “quality of sleep” is a narrower concept than “non-restorative sleep”. However, on reflection, it is apparent that having been referred back to a previous discussion concerning the term “quality of sleep” in DSM-IV in the context of primary insomnia and non-restorative sleep, Professor Glozier was basing his answers on the definition of “nonrestorative sleep” in DSM-IV which refers to patient complaints of “feeling that their sleep was restless, light, or of poor quality”. Given that meaning, Professor Glozier’s concession makes perfect sense if the approved indication is to be read in accordance with that definition. However, this merely takes one back to the question whether the approved indication would be interpreted in accordance with the definition of non-restorative sleep in DSM-IV on which Professor Glozier’s concession was based. As I have explained, Dr Behi’s and Dr Krapivensky’s evidence was that they understood the term “poor quality sleep” in the approved indication to be synonymous with the term non-restorative sleep as used in DSM-IV. On the other hand, sleep physicians and general practitioners would give the term “poor quality sleep” a much broader interpretation that encompasses difficulties initiating or maintaining sleep.
289 Ultimately, whether the PI or the approved indication amounts to an instruction or an inducement for the purposes of s 117(2)(c) is a question for the court. The evidence of expert witnesses may be of assistance, but is not necessarily determinative. In circumstances where neither the PI nor the approved indication makes any reference to DSM-IV or “non-restorative sleep” and where the various studies summarised in the PI investigated various aspects of sleep quality, I am not persuaded that the PI or the approved indication can be said to provide any instruction or inducement to use Melotin as a treatment for primary insomnia characterised by non-restorative sleep.
290 Each of the Swiss-style claims is for the use of melatonin in the manufacture of a medicament for treating a patient suffering from primary insomnia characterised by non-restorative sleep.
291 In Mylan the Full Court observed at [222] that “infringement of a Swiss type claim is concerned with what the allegedly infringing manufacturer has done, not what it intended to do.” The Court went on to observe that the most important consideration in determining whether a Swiss-style claim is infringed are the physical characteristics of the product including its packaging, dosage and product information. The Court said at [223]-[225]:
[223] Plainly, one badge of therapeutic purpose (to adopt Lord Sumption’s expression) is the physical characteristics of the medicament as it emerges as a product of the manufacturing process, including its formulation and dosage, packaging and labelling, and its patient information. This is a most important consideration. But it does not represent the only evidence that could rationally affect, directly or indirectly, the determination of the question of medicament’s therapeutic purpose. Although we do not read the Swiss type claims as adding the manufacturer’s intention as an essential feature of the invention, we do not reject the relevance of direct evidence of the manufacturer’s actual intention in making the medicament, where that evidence is available. This is not to say that such evidence would be determinative. If such evidence is available, it would form part of the circumstances of the case to be taken into account with all the other circumstances. Such evidence was not available in the present case.
[224] Further, we would not reject consideration of the reasonably foreseeable use or uses to which the medicament would be put after manufacture. Such consideration would also form part of the circumstances of the case. However, we agree with the primary judge that, where a medicament would be used extensively for purposes that fall outside the monopoly of a Swiss type claim, the fact that it is reasonably foreseeable, or indeed likely, that a substantial portion of the manufactured medicament would also be used for the claimed therapeutic purpose will not be determinative of infringement: it might be reasonably foreseeable that a product might be put to a particular use, but it does not necessarily follow that the product, as manufactured, is for that use. Thus, we reject Mylan’s submission that the primary judge acted inconsistently by rejecting the case on infringement of the Swiss type claims whilst nevertheless finding infringement under s 117(1) of the Act with reference to s 117(2)(b) in respect of the method of treatment claims. Different considerations inform the question of infringement arising under s 117(1). Ground 4 of the notice of appeal fails.
[225] We also agree with the primary judge that mere suitability of a medicament for a claimed purpose cannot be determinative of the question of infringement of a Swiss type claim. We have already touched on this consideration when discussing the limited scope of these claims. The fact that the patent has been granted on the basis of a second or later therapeutic use necessarily means that there are multiple uses to which, potentially, the medicament can be put. Thus, evidence of suitability for use is ambiguous and cannot alone answer the question whether the medicament, as manufactured, is one for the specified therapeutic purpose.
292 In the present case there are various uses for Melotin that are outside the scope of the Swiss-style claims. The fact that Melotin is bioequivalent to Circadin and therefore suitable for use as a treatment for primary insomnia characterised by non-restorative sleep is not determinative of the infringement question. Of greater significance to the resolution of the infringement question are the PI and approved indication.
293 The approved indication is not the same as the patented indication. For reasons previously explained, the meaning of “quality of sleep” in the approved indication is broader than the meaning of “non-restorative sleep” in the claims. Contrary to Neurim’s submissions, those terms are not synonymous, nor is the former “wholly encompassed by” the latter. For reasons also previously explained, neither the PI nor the approved indication provides any instruction or inducement to use Melotin to treat primary insomnia characterised by non-restorative sleep. The fact that Melotin and Circadin have the same approved indication is therefore at best equivocal.
294 Neurim relied on the AusPar for Circadin to which I have previously referred. I do not regard that document to be of any assistance in interpreting either the PI or the approved indication. In my opinion, it does not establish that the approved indication is limited to primary insomnia characterised by non-restorative sleep. It is apparent from the AusPar that the decision to restrict the indication to “poor quality of sleep” was based on the answers to the “Quality of Sleep” questions (Q4 and Q5) in the LSEQ which, as I have previously explained, are not directed to ascertaining how refreshing the patient’s sleep was. For that reason, the AusPar does not assist me in deciding whether Melotin is a medicament for the treatment of patients suffering from primary insomnia characterised by non-restorative sleep.
295 The PI includes statements that melatonin is associated with the “control of circadian rhythms” and “a hypnotic effect and increased propensity for sleep”. It suggests that Melotin is a product that may be suitable for use in treating a variety of sleep related disorders including primary insomnia with symptoms that include difficulty initiating or maintaining sleep.
296 I accept that it is reasonably foreseeable that Melotin will be used by some clinicians for the therapeutic purpose specified in the Swiss-style claims. It is apparent from Dr Behi’s and Dr Krapivensky’s evidence that they have prescribed Circadin for that purpose. However, it is also reasonably foreseeable, and in my opinion highly likely, that Melotin will mostly be used for other therapeutic purposes related to its postulated hypnotic effect and the regulation of circadian rhythms.
297 Looking at the evidence, I am not persuaded that Melotin is a medicament manufactured for the therapeutic purpose specified in Swiss-style claims.
298 Neurim alleges that the respondents have authorised, procured, induced or joined in a common design with persons treating primary insomnia characterised by poor quality sleep to use the Generic Partners Products for that purpose and thereby infringed the method treatment claims. In its closing submissions this aspect of Neurim’s case was primarily put on the basis of authorisation of patent infringement under s 13(1) of the Act.
299 Apotex has admitted that from around 28 April 2020 it authorised medical practitioners to prescribe the Generic Partners Products for the approved indication but denies that it thereby infringed the Patent. The question with respect to authorisation as agreed by the parties was whether authorisation of medical practitioners to prescribe the Generic Partners Products for use in accordance with the approved indication would also amount to authorisation to use the products to treat a patient in accordance with any of the method of treatment claims. If the answer to that question is “yes”, the respondents accept that Generic Partners’ supply to Apotex of the Apotex products amounted to authorising, procuring, inducing or joining in a common design with persons treating primary insomnia characterised by poor quality sleep to use the Apotex products in accordance with each of the method of treatment claims.
300 The meaning of the word “authorise” in s 13 of the Act is taken to have the meaning as in the Copyright Act 1968 (Cth). To authorise infringement is to sanction, approve or countenance the infringement. Authorisation is not limited to granting the legal right to exploit an invention: Roadshow Films Pty Ltd v iiNet Ltd (2012) 248 CLR 42 at [49]-[51] and [124]-[125]. Further, as Beach J observed in Streetworx Pty Ltd v Artcraft Urban Group Pty Ltd (2014) 110 IPR 82 at [394]:
For “authorise”, no intention to infringe or knowledge that the relevant acts would or would be likely to infringe is necessary. More particularly, knowledge of the patentee’s intellectual property rights does not need to be shown. All that may be required is knowledge of the acts that constitute infringement rather than their legal characterisation as infringing acts.
It is not necessary that the authoriser have formal authority to make such an authorisation. It is, however, necessary that the authoriser has the power to prevent the infringing conduct.
301 The essential facts relevant to authorisation may be summarised as follows:
The approved indication for the respondents’ product constitutes an instruction to medical practitioners to use such product in accordance with the approved indication.
While the words “quality of sleep” in the approved indication are not synonymous with restorative sleep or quality of restorative sleep, they encompass those concepts. The restorative quality of a patient’s sleep is one factor that determines the overall quality of the patient’s sleep.
As previously found, a reasonable person in the respondents’ position would have reason to believe that the Generic Partners’ Products would be prescribed by a not insignificant number of psychiatrists as a treatment for primary insomnia where the patient complained of non-restorative (or unrefreshing sleep).
It would be open to the respondents to either not supply their products at all or, at least, to limit the approved indication to exclude the patented indication or to include a statement in the PI that the products should not be used for the patented indication. Whether or not the TGA would give an approval subject to such an exclusion is a question that was not explored in evidence.
302 In their submissions the respondents contended that Neurim’s authorisation claim could only succeed if the case based on s 117(2)(c) succeeded because “[w]ithout an instruction or inducement to use the product for the claimed purpose, there is no basis on which to conclude that such use was sanctioned, authorised [or] countenanced.” I do not accept that submission.
303 Even though I found that the requirements of s 117(2)(c) were not met, it does not follow that the respondents have not authorised infringement of the method of treatment claims. In my opinion, they have authorised the use of their products by medical practitioners who the respondents have reason to believe will use the respondents’ products as a treatment for primary insomnia characterised by non-restorative sleep and to improve the restorative quality of sleep in patients aged 55 and over. In this regard, I refer to the findings made in relation to s 117(2)(b) of the Act. I do not consider that any authorisation by the respondents would extend to any “off-label” use including in patients aged under 55 because I am not persuaded that the respondents have authorised use of their product for therapeutic purposes outside the scope of the approved indication.
304 The grounds of invalidity relied on by the respondents include that the invention as claimed in claims 1-9 lacks novelty and does not involve an inventive step. The respondents also contend that the complete specification does not fully describe the invention as required by s 40(2)(a) of the Act and that claims 1-9 are not fairly based or clear as required by s 40(3) of the Act.
305 Neurim’s submissions assumed that the provisions of the Act relevant to novelty and inventive step were those in force at 14 August 2001 (i.e. the priority date): see, for example, Neurim’s Closing Submissions para 357, footnote 598 and para 425. However, while the priority date is 14 August 2001, the Patent was not applied for until 12 August 2002: see the particulars to para 5 of Neurim’s Amended Statement of Claim.
Patents Amendment Act 2001 (Cth)
306 Schedule 1 of Part 1 of the Patents Amendment Act 2001 (Cth) (“the 2001 Amendment Act”) commenced on 1 April 2002. By virtue of Item 13 in Schedule 1 of Part 1 of the 2001 Amendment Act the amendments apply to (inter alia) patents for which the complete application was made on or after that date: see also Colin Bodkin, Patent Law in Australia (Thomson Reuters, 3rd edition, 2019) (“Bodkin”) at [16610].
307 The copy of the Patent in evidence nominates 12 August 2002 as the international filing date of the application filed by Neurim under the Patent Cooperation Treaty (“PCT”). Pursuant to s 88(1) of the Act as it stood at 12 August 2002, a PCT application was to be treated as a complete application under the Act for a standard patent. Pursuant to s 88(4) of the Act, the filing date of a PCT application was to be taken to be its international filing date.
308 Section 7(1)-(3) of the Act at the date of the making of the complete application provided as follows:
7 Novelty and inventive step
Novelty
(1) For the purposes of this Act, an invention is to be taken to be novel when compared with the prior art base unless it is not novel in the light of any one of the following kinds of information, each of which must be considered separately:
(a) prior art information (other than that mentioned in paragraph (c)) made publicly available in a single document or through doing a single act;
(b) prior art information (other than that mentioned in paragraph (c)) made publicly available in 2 or more related documents, or through doing 2 or more related acts, if the relationship between the documents or acts is such that a person skilled in the relevant art would treat them as a single source of that information;
(c) prior art information contained in a single specification of the kind mentioned in subparagraph (b)(ii) of the definition of prior art base in Schedule 1.
Inventive step
(2) For the purposes of this Act, an invention is to be taken to involve an inventive step when compared with the prior art base unless the invention would have been obvious to a person skilled in the relevant art in the light of the common general knowledge as it existed in the patent area before the priority date of the relevant claim, whether that knowledge is considered separately or together with the information mentioned in subsection (3).
(3) The information for the purposes of subsection (2) is:
(a) any single piece of prior art information; or
(b) a combination of any 2 or more pieces of prior art information;
being information that the skilled person mentioned in subsection (2) could, before the priority date of the relevant claim, be reasonably expected to have ascertained, understood, regarded as relevant and, in the case of information mentioned in paragraph (b), combined as mentioned in that paragraph.
309 An important change to s 7(3) made by the 2001 Amendment Act concerns the circumstances in which two or more prior art documents may be combined. Before amendment, two or more related documents could only be combined if the relationship between the documents was such that a person skilled in the relevant art would treat them as a single source of information. The different language introduced by the 2001 Amendment Act relaxed that requirement.
310 For reasons previously stated I am not persuaded that any of the claims is invalid for lack of clarity. The term “non-restorative sleep” is to be interpreted in accordance with DSM-IV and in the context in which it is used. The phrase “improving the restorative quality of sleep” is also to be read in that context and is to be understood as referring to a subjective report of the patient that the restorative (or refreshing) quality of their sleep has improved. The term “primary insomnia characterized by non-restorative sleep” is to be understood as describing a condition, primary insomnia, which manifests with a complaint of non-restorative sleep that is a clinically meaningful element of that condition but not necessarily the sole or dominant complaint. So understood, the claims do not lack clarity.
311 The respondents also contended that the claims of the Patent were invalid because the complete specification did not, as required by s 40(2)(a) of the Act as it then stood, “describe the invention fully”. They submitted that a specification describes the invention fully if “it makes the nature of the invention plain to persons having reasonably competent knowledge of the subject and also makes it plain, to persons having reasonable skill, how to perform the invention”: Patent Gesellschaft AG v Saudi Livestock Transport and Trading Company (1997) 37 IPR 523 at 530. The invention for the purpose of s 40(2) is the embodiment which is described, and around which the claims are drawn: Kimberly Clark at [21].
312 The respondents submitted that each of the claims was invalid for lack of full description for the same reasons they relied on in support of their contention that the claims lacked clarity. In this context, the respondents submitted that reference to “characterized by non-restorative sleep” creates what they referred to as “inherently unascertainable boundaries”. I do not accept that submission. Nor do I accept that the invention of the claims (i.e. a method of treating primary insomnia characterised by non-restorative sleep to improve the restorative quality of sleep by administration of a prolonged release formulation of melatonin as specified in the claims) is not fully described. In my opinion the complete specification read as a whole (including the claims) makes the nature of the invention and how to perform it clear to a person skilled in the art. I am therefore not persuaded that the complete specification does not describe the invention fully as required by s 40(2)(a).
313 Section 18(1)(b)(i) of the Act provides that an invention is a patentable invention, for the purposes of a standard patent, if the invention, so far as claimed in any claim, when compared with the prior art base as it existed before the priority date, is novel. Section 7(1) of the Act provides that an invention is taken to be novel when compared with the prior art base unless it is not novel in light of relevant prior art information (as set out in the Act).
314 The respondents relied on the following prior art:
(1) the offering for sale and use of “Melatonex”, a 3 mg melatonin time-release tablet, in the United States before 14 August 2001 (“sale and use of Melatonex”);
(2) a webpage: web.archive.org/web/20010801150259/http://www.sunsource.com/melatonex/melatonex.html, published before 14 August 2001 (“Melatonex Webpage”);
(3) an academic journal article: Haimov et al, “Melatonin Replacement Therapy of Elderly Insomniacs” (1995) 18(7) Sleep 598-603 (“Haimov 1995”); and
(4) a patent: EP 0724878 entitled “Use of melatonin for treating patients suffering from drug dependencies”, published on 13 October 1999 / AU 695366 entitled “Use of melatonin for treating patients suffering from drug addiction”, published on 21 August 1996 (“878 Patent”).
315 The first question to be answered is whether any of the above pieces of prior art information anticipate the claims for the use of melatonin for treating a patient suffering from primary insomnia characterised by non-restorative sleep and improving the restorative quality of sleep in such a patient. If the answer to this question is yes, then it is necessary to consider whether the relevant prior art also discloses the following additional features of the claims:
(1) Claims 1 and 5: the medicament comprises also at least one pharmaceutically acceptable diluent, preservative, antioxidant, solubilizer, emulsifier, adjuvant or carrier;
(2) Claims 2 and 6: the medicament will release the melatonin slowly in the body over a preselected time period;
(3) Claims 3 and 7: the medicament is a prolonged release formulation that includes an acrylic resin;
(4) Claim 4: melatonin is the only therapeutically active agent administered; and
(5) Claims 8 and 9: use of melatonin substantially as described in any one of the Examples in the Patent,
(together the “additional integers”).
316 The test for whether a patent claim lacks novelty by reason of a prior publication (or is “anticipated” by a prior publication) has been described as follows in General Tire at 485 to 486:
When the prior inventor’s publication and the patentee’s claim have respectively been construed by the Court in the light of all properly admissible evidence … the question whether the patentee’s claim is new … falls to be decided as a question of fact. If the prior inventor’s publication contains a clear description of, or clear instructions to do or make, something that would infringe the patentee’s claim if carried out after the grant of the patentee’s patent, the patentee’s claim will have been shown to lack the necessary novelty, that is to say, it will have been anticipated. The prior inventor, however, and the patentee may have approached the same device from different starting points and may for this reason, or it may be for other reasons, have so described their devices that it cannot be immediately discerned from a reading of the language which they have respectively used that they have discovered in truth the same device; but if carrying out the directions contained in the prior inventor’s publication will inevitably result in something being made or done which, if the patentee’s patent were valid, would constitute an infringement of the patentee’s claim, this circumstance demonstrates that the patentee’s claim has in fact been anticipated.
If, on the other hand, the prior publication contains a direction which is capable of being carried out in a manner which would infringe the patentee’s claim, but would be at least as likely to be carried out in a way which would not do so, the patentee’s claim will not have been anticipated, although it may fail on the ground of obviousness. To anticipate the patentee’s claim the prior publication must contain clear and unmistakable directions to do what the patentee claims to have invented … A signpost, however clear, upon the road to the patentee’s invention will not suffice. The prior inventor must be clearly shown to have planted his flag at the precise destination before the patentee.
317 In Bristol-Myers Squibb Company v F H Faulding & Co Limited (2000) 97 FCR 524 (“Bristol-Myers”), Black CJ and Lehane J reviewed the relevant authorities on novelty and concluded at [67]:
What all those authorities contemplate, in our view, is that a prior publication, if it is to destroy novelty, must give a direction or make a recommendation or suggestion which will result, if the skilled reader follows it, in the claimed invention. A direction, recommendation or suggestion may often, of course, be implicit in what is described and commonly the only question may be whether the publication describes with sufficient clarity the claimed invention or, in the case of a combination, each integer of it…
318 A prior art document must expressly or implicitly disclose each of the essential integers: AstraZeneca FFC at [350]-[352] per Besanko, Foster, Nicholas and Yates JJ.
319 The “inevitable result” test with respect to anticipation is best described as follows at [12910] of Bodkin:
Where what is claimed is a new use of a known thing, the fact that prior use of that thing would have inevitably led to the newly-claimed result may lead to the result that the new claim is anticipated even if the prior art did not make knowledge of the new result available to the public.
320 In AstraZeneca FFC the Full Court referred to the limitations of the “inevitable result” test for novelty in circumstances where the invention is for a new method of medical treatment using a known compound at [296]:
… it is important to note the cautionary observations of Bennett and Yates JJ in [Leflunomide FFC] … at [165] that there is a question whether the unyielding logic of the “inevitable result” cases can be applied uncritically in every case of alleged anticipation, particularly where the invention in suit is claimed as a new method of medical treatment involving the administration of a known compound for a hitherto unknown and unexpected, but nevertheless useful, therapeutic use.
321 It was submitted by Neurim that in order for an anticipation by inevitable result to be made out, it must be established that the prior art document contains directions that, if followed, must inevitably “as a matter of hard fact” produce something falling within the claims. Further, Neurim submitted that if the prior publication contains directions which would at least be likely to be carried out in a manner that would not infringe the claims, then those claims will not have been anticipated.
322 Accordingly, Neurim argued that in order for the prior art documents to inevitably result in the claimed invention, the prior art documents must contain directions to use a prolonged release formulation of melatonin to treat a patient suffering from primary insomnia characterised by non-restorative sleep and improve the restorative quality of sleep in such a patient. Neurim submitted that it was not sufficient for the prior art documents to contain directions to use a prolonged release formulation of melatonin to treat a condition that is not primary insomnia. Neurim submitted that the Patent is directed to a particular type of insomnia (primary insomnia characterised by non-restorative sleep) and that the evidence establishes that there is no basis to conclude that any of the patients in the studies reported in the prior art had any form of primary insomnia, let alone primary insomnia characterised by non-restorative sleep specifically.
323 The respondents argued that there is a distinction drawn between, on the one hand, “true new cases” of a new use of a known product and, on the other, “mere more information about old uses”. They relied on, inter alia, the judgment of Beach J in Otsuka FFC (No 2) at [176] where his Honour observed:
… novelty is not conferred merely by:
(a) providing more information about an old use;
(b) explaining the scientific theory for the mechanism which underlines a use already described in the prior art; or
(c) claiming a narrower use of an old product, where that narrower use fits within the broader use for the old product already described in the prior art.
324 In Otsuka FFC (No 2), Beach J found at [177] that the patent in suit suffered from “a variant form of parameteritis” as it had merely taken a subset of the use and method disclosed in an earlier patent and had justified the narrowing based on a scientific theory that, as at the priority date, was not robust. In making this finding, Beach J relied on observations in Actavis UK Ltd v Janssen Pharmaceuticals NV [2008] FSR 35 at [99] and [100] per Floyd J and Bristol-Myers Squibb Co v Baker Norton Pharmaceuticals Inc [1999] RPC 253 at [59] per Jacob J. The other members of the Full Court in Otsuka FFC (No 2) did not consider the issue of parameteritis.
325 The respondents accepted that none of the prior art expressly disclosed a diagnosis of “primary insomnia characterized by non-restorative”, or “improvement in the restorative quality of sleep” in those terms. In closing oral submissions, Mr Murray SC (Senior Counsel for the respondents) submitted that if the approach of Beach J in Otsuka FFC (No 2) was accepted, then this lack of express disclosure would not be an issue. In support of this proposition, the respondents submitted that the use of melatonin as a method of treatment of primary insomnia characterised by non-restorative sleep to improve the restorative quality of sleep in the Patent, merely claims a narrower use of an old product, which fits within the broader use for that product already described in the prior art: Otsuka FFC (No 2) at [176]. This is because, on the respondents' case, the information made available by each of the disclosures relied upon is that prolonged release melatonin within the claimed dose range can treat insomnia and improve the restfulness of sleep and/or sleep quality. At the priority date, a disclosure of a treatment for insomnia would be understood as disclosure of a treatment for insomnia, whether primary or secondary, and however characterised, and directed generally at the symptoms of insomnia, namely, a subjective complaint about sleep and its daytime consequences.
326 In this regard, the respondents submitted that:
(1) The persons taking Melatonex in the US would be understood necessarily to include primary insomniacs.
(2) Haimov 1995 would specifically be understood as a study of primary insomniacs.
(3) EP878 expressly discloses treatment of “conditions susceptible to alleviation by administration of a benzodiazepene”, and expressly discloses insomnia. This would be understood as a disclosure necessarily including primary insomniacs.
327 The respondents further submitted that the prior art citations each disclose a treatment for insomnia, including primary insomnia, which would be understood as an express disclosure of a treatment for primary insomnia, however characterised. They argued that the Patent’s overlaying of the additional parameter “characterised by NRS” as a diagnostic qualification invoking DSM-IV, and “improvement in the restorative quality of sleep” as a necessary intended treatment effect, merely constitutes an attempt to re-patent the prior art and therefore, on the approach taken by Beach J in Otsuka FFC (No 2), cannot confer novelty.
328 In addressing the respondents’ contention that the Patent amounted merely to parameterisation of the prior art, Neurim relied on the observations of Laddie J in Raychem Corp’s Patents [1998] RPC 31 at p 37, where his Lordship defined the concept of parameteritis as:
… the practice of seeking to repatent the prior art by limiting claims by reference to a series of parameters which were not mentioned in the prior art. Sometimes it includes reference to parameters measured on test equipment which did not exist at the time of the prior art. The attraction of this to a patentee is that it may be impossible to prove now that the prior art inevitably exhibited the parameters and therefore it is impossible for an opponent to prove anticipation. Even if that is what has happened here, it does not alter the task of the court. It must decide whether the opponent has proved anticipation or some other statutory ground of invalidity. Parametritis may make the court’s task more difficult, but at the end of the day the test of invalidity must be the same, whatever the form of the claims.
329 Neurim also relied on the approach of Bennett J in Williams Advanced Materials, Inc v Target Technology Company LLC (2004) 63 IPR 645, where her Honour, in determining whether claim features amounted to parameteritis, considered whether there is any advantage or any difference to the prior art teaching arising out of the claimed additional features. Her Honour also held in Austal Ships Pty Ltd v Stena Rederi Aktiebolag (2005) 66 IPR 420 at [108] that where the parameters have been carefully chosen, are part of the invention, and are related to a claimed advantage as part of the combination of the design, parameteritis will not arise.
330 Relying on these authorities, Neurim submitted that each of the relevant features of the claims asserted by the respondents to amount to mere parameterisation do, in fact, have a technical effect and are not arbitrary integers included merely to facilitate the patenting of the prior art. In support of that submission, Neurim asserted that at the priority date, melatonin was known as a chronobiotic that could be used to improve insomnia secondary to a circadian rhythm disorder through regulation of the sleep-wake cycle, which is the mechanism which underlies the use described in the prior art. Neurim submitted that it was a new and surprising result that melatonin could, additionally, be used to improve the restorative quality of sleep in a specific group of insomnia patients that had not previously been addressed in the prior art. Neurim therefore asserted that the claims are directed to an entirely new therapeutic use which was not taught by the prior art, namely the use of prolonged release melatonin to treat primary insomnia characterised by non-restorative sleep.
331 I do not accept the respondents’ characterisation of the claims of the Patent as mere parameterisation whereby the features of “primary insomnia characterized by non-restorative sleep” and “improvement in the restorative quality of sleep” support a claim to a narrower use of an old product, where that narrower use fits within the broader use for the old product already described in the prior art. I accept Neurim’s submission that the features identified in the claim have a technical effect, are part of the invention, and are directly related to a claimed advantage of the invention. I find that the claims are directed to a new therapeutic use, namely, the treatment of primary insomnia characterised by non-restorative sleep, and it was not an inevitable result of the prior use of melatonin that it had been or would be used as such a treatment.
332 As an alternative to their argument that the claims of the patent are merely parameterisation of the prior art, the respondents advanced a different novelty argument which assumed, contrary to my previous finding, that a diagnosis of primary insomnia characterised by non-restorative sleep was not required by the claims, contrary to the approach of Keane CJ in Leflunomide FFC at [37]).
333 The respondents said that, if it was found that infringement arises despite an absence of a deliberate diagnosis by a clinician of primary insomnia according to DSM-IV criteria, characterised by non-restorative sleep as defined in the DSM-IV, then the fact that prior art documents lack the same specific integers should not preclude a finding of anticipation.
334 Although I have not taken an approach which is inconsistent with that of Keane CJ referred to above, and despite this have found that infringement still arises under s 117(2)(b), I have dealt with the respondents’ alternative novelty argument by reference to the relevant prior art against the possibility that my previous finding is not correct.
Sale and use of Melatonex and Melatonex Webpage
335 The Melatonex Webpage was made available through a Wayback Machine search result and is dated 1 August 2001. The relevant aspects of the product description are as follows:
Sleep better to feel better
MELATONEX is a dietary supplement containing melatonin, a substance produced by our own bodies that regulates the body’s natural sleep/wake cycle. After we reach maturity, melatonin production declines with age which can make restful sleep more difficult to achieve. Melatonin production can also diminish through our use of substances like alcohol, tobacco, caffeine, aspirin and many common medications. MELATONEX supplementation can help to restore the melatonin we need for a restful, natural sleep.*
Unique time-release delivery
MELATONEX uses a unique time-release delivery system that releases melatonin the way the body does, gradually while you sleep.
…
* These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
336 The respondents did not rely on any evidence of the actual supply of Melatonex to any persons for any purpose and justified this course by submitting that there were copious references to its availability and sale in the United States in the literature at the priority date and that there was no dispute between the parties as to the fact of its availability. The respondents did not go as far as to say that Melatonex as a particular brand was common general knowledge, but rather submitted that it was common general knowledge that melatonin generally, as a dietary supplement, was available over the counter in the United States.
337 The respondents’ submitted that the Melatonex Webpage recommends use of Melatonex to restore melatonin to levels needed for a restful, natural sleep and that this amounts to a disclosure that taking Melatonex will result in more restful sleep. According to the respondents, this disclosure amounted to disclosure of use for insomnia, which necessarily includes use for primary insomnia and primary insomnia characterised by non-restorative sleep. The respondents submitted that the Court can, and should, infer that one or more consumers of Melatonex had primary insomnia, would complain about the restorative quality of their sleep (if asked about it), and took the Melatonex tablet in the expectation that it would improve the restorative quality of their sleep.
338 Neurim submitted that the extent of the evidence on this issue is the cross-examination of Professor Roth on the use of melatonin generally in the United States (where it was available over the counter as a health food supplement) before the priority date. Professor Roth conceded that as a matter of probability, it was likely that at least some people using melatonin had primary insomnia, and that, as a matter of probability, it was also likely that at least some of those people had primary insomnia characterised by non-restorative sleep. However, when asked whether, at the priority date, he would have expected the use of melatonin to have improved the restorative quality of sleep in these people, his answer, based on data published in 2001 was “no”.
339 Neurim also submitted that the test for anticipation by prior use is no less stringent than the test for anticipation in a published document. It was submitted that the prior use has to be an enabling disclosure such as to enable a person skilled in the art to put the claimed invention into practice. Neurim submitted that “uninformative use” will not amount to an anticipation, relying on Damorgold Pty Ltd v JAI Products Pty Ltd (2015) 229 FCR 68 at [46]-[55] per Bennett J, [74]-[90] per Yates J. I accept that submission.
340 In opening submissions, Mr Murray SC referred to the disclaimer appearing on the Melatonex Webpage stating that it is not intended to “diagnose, treat, cure or prevent any disease”. Mr Murray SC submitted that:
…that box arises from the regulatory requirements of the US system. Where it’s a dietary supplement rather than a medication, then there are limits as to how the product can be promoted….Despite the language in the box where it is being suggested, as it plainly is in that first paragraph, that melatonin supplementation can help to restore the melatonin we need for a restful, natural sleep, the plain suggestion is take this to have a more restful sleep, and so here is an example of the product being available before the priority date, apparently on the face of this advertisement for the claimed use.
The explanation given by Mr Murray SC does not assist the respondents case and merely reinforces Neurim’s argument that dietary supplements are not medications and therefore are not intended for the treatment of any disease or disorder.
341 Neurim submitted that the Melatonex Webpage is a non-scientific document that includes no reference to any type of insomnia whatsoever (including primary insomnia or nonorganic insomnia) or any reference to non-restorative sleep. In Roth 1, Professor Roth gave the following evidence in relation to the Melatonex Webpage:
318. … I have no idea what is meant by “restful sleep” in this context, other than the fact that it cannot refer to the sleep of a person with insomnia, including primary insomnia and primary insomnia characterized by non-restorative sleep, or any other disorder or disease. As discussed above, the product is not approved for the treatment of any disease or disorder, and is not referring to any diagnosis or diagnostic criteria.
319. There is nothing on the Melatonex Webpage, or in the use of this product on the market at the Priority Date, that would teach me that Melatonex could be used as treatment for a patient diagnosed with Primary Insomnia characterized by non-restorative sleep, or a patient diagnosed with any form of Primary Insomnia. As discussed above, the Melatonex product had not, and is still not, approved as a therapeutic drug with any medical indication. It has thus not been approved as safe and efficacious for the treatment of any sleep disorder, nor for the complex condition of Primary Insomnia and, in particular, not for Primary Insomnia characterized by non-restorative sleep.
342 I am not persuaded that the Melatonex Webpage conveyed or disclosed any clear direction, recommendation or suggestion to use Melatonex to treat a patient diagnosed with primary insomnia characterised by non-restorative sleep, or a patient diagnosed with any form of primary insomnia. Furthermore, I am also not persuaded that the Court should infer that any individual used Melatonex to treat primary insomnia before the priority date. In this regard, the respondents did not lead any evidence of any actual use of Melatonex by patients diagnosed with insomnia. Accordingly, I am not persuaded that the sale or use of Melatonex or any disclosure appearing on the Melatonex Website before the priority date is novelty defeating.
343 Haimov 1995 was published in the journal Sleep in 1995 and reports on a study which “investigated the effect of melatonin treatment on melatonin-deficient insomnia in the elderly” and which hypothesised that “elderly insomniacs could benefit from melatonin replacement therapy”.
344 The study was a randomised and double-blinded study which involved three patient groups. The first group comprised eight patients who were independently living insomniacs. The second group comprised 18 patients who had lived in a nursing home for at least six months. The third group comprised 25 patients who lived independently in the community and did not have sleep disorders. The third group was studied in order to validate the subjective complaints about insomnia and this group was not included in the treatment part of the study.
345 The patients in the study were considered to have insomnia if they reported all of the following:
(1) they had been sleeping poorly at least three nights per week;
(2) their insomnia lasted for a minimum of six months;
(3) their insomnia was clearly affecting their daytime functioning; and
(4) their insomnia was not caused by chronic pain or any known medical disease or by either alcohol or drugs.
346 The subjects were personally interviewed by an experienced physician to rule out significant sleep apnoea syndromes which could be related to physiologically based insomnia or any medical illnesses that might interfere with sleep.
347 The study included an initial seven-day period of no treatment, followed by three seven-day experimental periods where subjects were given 2 mg sustained-release melatonin, 2 mg fast-release melatonin, or a placebo, two hours before bed time. Between each experimental period, there was a “washout” period of at least two weeks to exclude the possibility of carryover effects. Following the three experimental periods, there was a two-month experimental period where 17 of the 26 insomnia subjects were given 1 mg sustained-release melatonin daily two hours before bed time. The sleep-wake patterns of nine of the insomniacs living within a nursing home were monitored for a further 3 months after melatonin treatment was withdrawn.
348 During each of the experimental periods, a subject’s sleep was continuously monitored using actigraphy. For the two-month treatment period, a subject’s sleep was monitored using actigraphy during the last week of the treatment period. Subject movements recorded by actigraph were translated into an electrical signal, which was analysed to determine the following sleep parameters using an automated algorithm: sleep duration, sleep efficiency, sleep latency and mean activity level during sleep.
349 The following extracts from Haimov 1995 are relevant to both novelty and obviousness:
…melatonin has an estimated half-life between 35 and 50 minutes and is rapidly eliminated, while in the human study of the plasma pharmacokinetics of melatonin it was shown that slow-release preparation (2 mg) is able to extend high plasma melatonin for 5-7 hours. Thus, we used a sustained-release melatonin in order to restore melatonin levels in the elderly throughout the night. We report here on the effects of fast- and sustained-release melatonin administered nightly on sleep in the elderly insomniacs.
…
All subjects were in good clinical condition, and none met any criteria for dementia or depression according to the Mini-Mental State Examination (MMSE) or the Hamilton rating scale. Subjects were personally interviewed by an experienced physician to rule out significant sleep apnea syndromes which could be related to physiologically based insomnia, or any medical illness that might interfere with sleep. None of the subjects used any medication that could affect sleep or the noradrenergic system for at least 1 month prior to the study.
Because in the International Classification of Sleep Disorders (ICSD) there is no diagnosis of insomnia in the elderly, we accepted volunteers if they reported sleeping poorly on at least 3 nights per week and if their insomnia had lasted for a minimum of 6 months. Volunteers also had to report that their insomnia clearly affected their daytime functioning, that it was not caused by chronic pain or any known medical disease and that the volunteer did not use either alcohol or drugs that might affect sleep. Volunteers were then sent a number of questionnaires, including a one-week sleep log, a mini-sleep questionnaire (MSQ) and the Technion Sleep Questionnaire.
…
The study comprised one 7-day, running-in, no-treatment period, followed by three 7 -day experimental periods, during which subjects were administered tablets 2 hours before desired bedtime. The tablets were either 2 mg melatonin administered as sustained-release (S-1w) or fast-release (F-1w) or an identical looking placebo (PL).
…
a subject’s sleep was continuously monitored for 1 week by miniature actigraphs worn on the wrist which enabled monitoring of sleep under natural circumstances, with minimal distortions.
…
The actigraph measures wrist activity utilizing a piezoelectric element, and translates wrist movements into an electrical signal which is digitized and memorized. Recordings were analyzed by an automatic algorithm as previously described to determine sleep duration (total number of minutes defined as sleep), sleep efficiency index (% of sleep duration out of total bedtime), sleep latency (time to fall asleep from bedtime) and mean activity level (the mean sum of actigraphic movements recorded during sleep divided by sleep duration). Activity level during sleep can be viewed as an index of the restfulness of the sleep period.
…
In order to validate the subjective sleep quality, we compared the sleep maintenance (sleep efficiency and activity level during sleep) of those who complained of sleep disorders with that of those who did not, during the 1-week, running-in, no-treatment period, by actigraphic measurements.
…
Therefore, to assess the efficacy of melatonin on sleep quality, the effects of melatonin treatment were studied during the first 6 hours after sleep onset. Repeated measures ANOVA showed that sleep duration was not influenced by melatonin treatment within each group (F = 0.19, df = 3,63, p > 0.91).
…
In the present study, we investigated the effect of melatonin treatment on melatonin-deficient insomnia in the elderly. To our knowledge, this is the first report examining the therapeutic effect of melatonin on the elderly population.
…
Our results suggest that melatonin replacement therapy, using a low dosage (1 or 2 mg) of melatonin, has specific effects on sleep initiation and maintenance in these patients. A 1-week treatment of 2 mg sustained-release melatonin was effective on sleep maintenance (i.e. sleep efficiency and activity level) of elderly insomniacs, while sleep initiation was improved after a 1-week, fast-release melatonin treatment.
…
[T]he benefit of the sustained-release tablets comes from the release of melatonin in small dosages during the entire night. The fact that sleep initiation was improved upon long-term treatment with sustained-release melatonin suggests stabilization of the sleep-wake cycle in melatonin-deficient elderly insomniacs.
…
This study suggests two important principles of melatonin replacement therapy of melatonin-deficient elderly insomniacs. i) melatonin appears to have a beneficial effect when administered in the form of sustained-release tablets and ii) to ensure efficacy, long-term treatment is recommended.
…
From the results of the present study, it seems likely that melatonin replacement therapy may beneficial in the initiation and maintenance of sleep in this population.
(Emphasis added. Citations omitted)
350 The respondents argued that Haimov 1995 would be understood by the skilled addressee as disclosure of a method of using prolonged release melatonin to treat primary insomnia (however characterised) and improve the patient’s sleep quality.
351 I accept that Haimov 1995 clearly discloses the use of prolonged release 2 mg melatonin as a treatment which it refers to as “sustained-released melatonin”. However, the purpose of the use of the treatment as disclosed in Haimov is less clear.
Primary insomnia
352 The respondents said that the inclusion criteria of the study (including by exclusion of comorbidities, i.e., dementia and depression, ruling out of significant sleep apnoea syndromes and absence of other medical illness that could affect sleep), are consistent with the subjects having primary insomnia and therefore the disclosure of the paper should be understood as being a study in primary insomniacs. The respondents relied on the evidence of Professor Wheatley in Wheatley 1 where he stated that the inclusion criteria used in Haimov 1995 are consistent with the subjects in the study having been identified as suffering from primary insomnia. They also relied on Professor Wheatley’s statement in JER 2 that it is likely that a majority of the subjects described in Haimov 1995 had primary insomnia based on the clinical description given and the context of the study.
353 In JER 2, Professor Roth disagreed with Professor Wheatley. Professor Roth contended that potentially none of the patients in the study populations had primary insomnia and that nowhere are they described as having been diagnosed with any type of primary insomnia or nonorganic insomnia. He noted that Haimov 1995 does not include the terms “primary insomnia”, “nonorganic insomnia” or “non-restorative sleep” nor does it include any reference to DSM-IV or ICD-10. He also noted that there is a reference to ICSD, but only to note that ICSD does not include a diagnosis of “insomnia in the elderly”. He stated that this suggested to him that neither DSM-IV nor ICD-10 were used in identifying the study populations and that, while ICSD was considered, ultimately no diagnostic criteria from any of those nosologies were utilised.
354 In JER 2, Professors Roth, Wheatley and Glozier all agreed they could not determine what proportion of the participants (if any) in Haimov 1995 may have met the diagnostic criteria for primary insomnia. They acknowledged that this was in part complicated by the fact that the authors did not use the term “primary insomnia” as an inclusion criterion. In addition, no specific inclusion and exclusion criteria was listed in Haimov 1995 to allow the experts to determine whether the participants did or did not meet the criteria for a diagnosis if primary insomnia. Professors Wheatley and Glozier also accepted in cross-examination that neither primary insomnia nor non-restorative sleep are discussed in Haimov 1995 and the participants were not selected on the basis of specifically meeting those criteria.
355 Neurim argued that the subjects in Haimov 1995 were elderly patients who could have a large burden of health problems that can cause secondary insomnia. Whilst patients were excluded from the study groups if they had certain health conditions, this was not a systematic exclusion of patients with health conditions that would cause them to be outside the DSM-IV or ICD-10 criteria for primary insomnia characterised by non-restorative sleep, including some conditions which are common in elderly patients, such as anxiety and mild sleep apnoea.
356 Additionally, Neurim relied on the evidence of Professor Roth that in his opinion, the majority of the patients in Haimov 1995 had a circadian rhythm disorder rather than primary insomnia disorder. This was based on the references in Haimov 1995 to the patients being “melatonin deficient”, references to the cohort in Haimov 1995 overlapping with previous research conducted in elderly cohorts with delayed onset and peak times of excretion of a melatonin metabolite, and that the melatonin treatment results indicated “stabilization of the sleep-wake cycle in melatonin-deficient insomniacs”,
357 Professor Glozier in Glozier 2 stated that he disagreed with Professor Roth’s conclusions in Roth 1 that at least the majority of the patients discussed in Haimov 1995 had a circadian rhythm disorder for various reasons, including that he understood the ruling out of medical illness that might interfere with sleep in the patients in Haimov 1995 would have included circadian rhythm disorders. During cross-examination, Professor Roth subsequently conceded that he could not say if the patients had a circadian rhythm disorder as the patients sleep history was not reported in Haimov 1995. Accordingly, the respondents submitted that the evidence of Professor Roth should not be accepted as it was an overstatement in light of this concession. On this topic I found Professor Glozier more persuasive than Professor Roth.
358 At this point it is important to revisit the exclusion criteria in Haimov 1995 which stated that all patients were in good clinical condition, did meet the criteria for dementia or depression, were personally interviewed by an experienced physician to rule out significant sleep apnoea, and did not suffer from an illness or take any medication (for at least one month prior to the study) that might interfere with sleep. On the basis of this exclusion criteria, I am persuaded that the skilled addressee would understand from Haimov 1995 that a proportion of the subjects described by the authors as insomniacs, were suffering most likely from primary insomnia. I therefore accept the respondents’ argument that Haimov 1995 discloses the use of prolonged release melatonin for treatment of primary insomnia generally.
Non-restorative sleep and improving the patient’s restorative quality of sleep
359 The respondents argued that the patients’ report of “sleeping poorly” in Haimov 1995 can be understood as a complaint of non-restorative sleep. The respondents also relied on the proposition that the authors of Haimov 1995 were using actigraphy as an index of subjective restfulness, and the study’s conclusion that restfulness improved with the administration of 2 mg melatonin. The respondents submitted that this should be understood as disclosing an improvement in the patient’s restorative quality of sleep. Accordingly, the respondents argued that this amounts to a disclosure of the use of prolonged released melatonin to treat primary insomnia characterised by non-restorative sleep to improve the restorative quality of sleep. In support of this submission, the respondents relied on the evidence of Professor Glozier in Glozier 2 where he stated:
…The patients in Haimov 1995 were accepted if they reported ‘...sleeping poorly on at least 3 nights per week and if their insomnia had lasted for a minimum of 6 months’. I would consider these patients to be complaining about the quality of their sleep, which encompasses non-restorative sleep. I therefore disagree with Professor Roth’s view at paragraph 213 of the Roth Affidavit that ‘sleep quality’ is used in Haimov 1995 to refer only to the quantity of the patient’s sleep.
(Emphasis added)
360 Professor Roth’s evidence at para 212-214 of Roth 1 was as follows:
212. Separately, in the “Results” section, Haimov 1995 discusses the validation of the insomnia complaints made by insomnia patients when they were first enrolled into the study, stating that: “In order to validate the subjective sleep quality, we compared the maintenance (sleep efficiency and activity level during sleep) of those who complained of sleep disorders with that of those who did not”. Later in the “Results” section, Haimov 1995 says: “to assess the efficacy of melatonin on sleep quality, the effects of melatonin treatment were studied during the first 6 hours after sleep onset”.
213. It is clear that those references to “sleep quality” are not intended to, and do not, refer to “poor quality of sleep”, as that term is used in relation to the diagnosis of nonorganic insomnia in the ICD-10. Poor quality of sleep in that diagnostic context in the ICD-10 is a subjective complaint, and distinct from a complaint of difficulty falling asleep or staying asleep. It has the same meaning as non-restorative sleep in the diagnosis of Primary Insomnia in the DSM-IV and cannot be measured objectively. Here, Haimov 1995 is discussing measuring objective parameters using actigraphy. It is clear that “sleep quality” is used in Haimov 1995 in a general sense to refer to the quantity of the patient’s sleep. Haimov 1995 does not include any indication that any of the patients in the study populations subjectively assessed the restorative quality of their sleep prior to the start of the study or at the conclusion of any of the treatment periods.
214. In conclusion, I consider that Haimov 1995 would not have disclosed anything to me as at the Priority Date about a possible treatment for Primary Insomnia characterized by non-restorative sleep for the following reasons, which I have discussed more fully above:
…
(c) Haimov 1995 does not include any reports of the subjective assessment of the restorative quality of the sleep of the insomnia patients in the study populations either prior to the studies or at the end of any of the treatment periods. The DSM-IV is unequivocal that the restorative quality of an insomnia patient’s sleep can only be measured by a patient’s subjective assessment;
(d) all of the sleep parameters measured in Haimov 1995 relate to sleep quantity, not quality, and were measured objectively by actigraphy;
(e) the limited positive conclusions expressed in Haimov 1995 regarding the use of melatonin on the objectively measured quantitative aspects of sleep, which would not have disclosed anything to me as at the Priority Date about a possible treatment for Primary Insomnia characterized by non-restorative sleep, are of questionable validity and reliability for the numerous reasons that I have identified.
(Emphasis added)
361 In JER 2, Professors Roth, Glozier and Wheatley disagreed on whether objective assays of sleep (in these cases various measures derived from actigraphy) can indicate efficacy in improving non-restorative sleep. All experts agreed that actigraphy was not a validated means of measuring non-restorative sleep. Professor Roth stated and confirmed in his course of cross-examination that he knew of no research justification or clinical validation of any actigraphic endpoint to measure non-restorative sleep. He explained that, at that time, no actigraphic measure had been shown to indicate that it was a measure of patients’ reports of non-restorative sleep, and also pointed to research which had attempted, and failed, to identify objective measures of non-restorative sleep. Professor Glozier disagreed with Professor Roth’s statement that an improvement in an objective assay of sleep could not indicate an improvement in the subjective self-report of non-restorative sleep. Professor Wheatley also disagreed with Professor Roth and believed that it was possible to have objective measures of sleep that are useful for assessing the symptoms related to non-restorative sleep and sleep quality.
362 During the cross-examination of Professor Roth, Mr Murray SC relied on two publications in support of the respondents’ submission that a skilled reader would have understood that actigraphy can demonstrate improvements in non-restorative sleep.
363 The first publication was a book chapter entitled “Assessment and Differential Diagnosis” authored by Professor Colin Epsie, in the book “Treatment of Late-Life Insomnia” edited by Lichstein and Morin and published in 2000 (“Epsie Chapter”). Mr Murray SC relied on the following extract from the Epsie Chapter:
Actigraphy may also provide an index of sleep quality; it has been shown that movement during sleep is strongly related to sleep diary ratings of sleep quality (Horne, Pankhurst, Reyner, Hume, & Diamond, 1994).
364 The second publication (which is not evidence) was the academic paper by Horne et al cited by Epsie for the above proposition published in 1994 (“the Horne Paper”). According to Professor Roth, the study in the Horne Paper had two important features that distinguished it from Haimov 1995. First, the Horne Paper was a study of people who lived near an airport, and it used actigraphy to measure movements across the night and led “to some questionnaire about sleep quality in people who sleep by airports”. Secondly, the study did not involve insomniac patients and was conducted on healthy volunteers. Professor Roth stated that he did not know what the term “sleep quality” was referring to within the Horne Paper, but seemed to suggest that because of the differences between the Horne Paper and Haimov 1995, the term as used in each source had a different meaning.
365 During the cross-examination of Professor Roth, Mr Murray SC asked whether he agreed that a skilled reader, as at August 2001, reading Haimov 1995, would accept at face value the proposition that movement measured by actigraphy can be viewed as an index of the subjective perception of the restfulness of sleep. Professor Roth emphatically disagreed with that proposition and stated that there was no basis for it.
366 Mr Murray SC also asked Professor Roth whether, if a reader of Haimov 1995 made the assumption that “the activity level during sleep, as measured by actigraphy, is an index of the restfulness of the sleep period”, then the observation of a statistically significant improvement in the actigraphy data in the melatonin treatment group would tell the reader that those subjects had been suffering from non-restorative sleep. Professor Roth agreed with that proposition, on the basis of the assumption he was asked to make by Mr Murray SC. He added, however, that he would have some level of concern about the measure because the actigraphy data was only recorded for the first six hours of sleep, and most sleep disturbances, especially in the elderly, tend to occur in the last two hours of sleep.
367 The respondents did not submit that the Espie Chapter or the Horne Paper were common general knowledge at the priority date. There was no evidence to suggest that any witness apart from Professor Roth was familiar with these publications. I accept the evidence of Professor Roth that the skilled addressee would not, at the priority date, have thought that movement measured by actigraphy can be viewed as an index of the subjective perception of the restfulness of sleep. I see no basis for the assumption postulated by Mr Murray SC, that in the Haimov 1995, the activity level during sleep (as measured by actigraphy) is an index of the subjective perception of restfulness of the sleep period.
368 The respondents also submitted that Professor Roth’s evidence on this topic should be rejected, as it does not reflect the common general knowledge of the skilled addressee at the priority date and rather is informed by his own vast knowledge of non-common general knowledge literature, and his belief that objective measures have not been shown to correlate with subjective perception. However, to say that it was later found to be the case that objective measures do not correlate with subjective perception, does not establish that the converse was true at the priority date or that the skilled addressee would have understood there to be any such correlation. I accept Professor Roth’s evidence that the skilled addressee would not approach Haimov 1995 with the understanding that activity levels as measured by actigraphy provided a basis from which to draw inferences as to the restorative quality of patients’ sleep.
369 I find that Haimov 1995 does not provide any clear direction, recommendation or suggestion to use prolonged release melatonin to treat primary insomnia characterised by non-restorative sleep and to improve the patient’s restorative quality of sleep. Haimov 1995 is not novelty defeating.
370 The 878 Patent is an EU patent in the name of Neurim and was published on 13 October 1999. The invention is described in paragraph 1 of the 878 Patent as relating to:
melatonin for use in the manufacture of a medicament for treating, or for preventing, symptoms of dependence on, tolerance of, or addiction to benzodiazepine drugs, for treating multidrug addicts and to a pharmaceutical formulation, for use in such treatments.
(Emphasis added)
371 Other parts of the 878 Patent relevant to novelty and inventive step are extracted below:
…
[0002] Dependence on benzodiazepines often develops in insomniacs who use them for the induction of sleep and in multi-drug addicts who in the process of withdrawal from narcotics, become addicted to benzodiazepines to ease anxiety and convulsions.
…
[0004] It has surprisingly been found in connection with the present invention that administration of melatonin concurrently with benzodiazepine drugs can potentially (1) wean a patient away from dependence on, addiction to, or tolerance of such drugs, and (2) in the case of a patient who has been diagnosed as requiring a benzodiazepine drug (where such undesired symptoms have not yet occurred), prevent the occurrence of such symptoms.
…
DESCRIPTION OF THE INVENTION
[0008] The present invention thus provides use of melatonin in the manufacture of a medicament for treating addiction to benzodiazepines in a multidrug addict, or a patient who has symptoms of having become dependent on, tolerant of, or addicted to a benzodiazepine drug, or for treating a patient who has been clinically diagnosed as having a condition susceptible to alleviation by administration of a benzodiazepine drug, while simultaneously preventing the occurrence in the patient of symptoms of dependence on, tolerance of, or addiction to said benzodiazepine drug, wherein said medicament contains at least an amount of melatonin effective for any of said treatments, said amount being adapted for a daily rate of administration within the range of 0.01-100 mg, provided that such use excludes use in the manufacture of a medicament containing 10-100 mg melatonin for treating a patient who has been clinically diagnosed as having a condition susceptible to alleviation by administration of a benzodiazepine drug, while simultaneously preventing the occurrence in the patient of symptoms of dependence on, tolerance of, or addiction to said benzodiazepine drug.
[0009] The said medicament may be a pharmaceutical formulation adapted for oral, rectal, parenteral or transdermal administration and which comprises at least one diluent, carrier or adjuvant, and may be additionally characterized by at least one of the following features: (i) it is in unit dosage form, each unit dosage comprising an amount of melatonin which lies within the range of 0.0025-100 mg; (ii) it is in the form of a controlled release formulation, wherein the melatonin is preferably released at a predetermined controlled rate; (iii) it comprises also at least one melatonin receptor modifier and/or melatonin profile modifier. The medicament may comprise also, and the pharmaceutical formulation according to the invention comprises, at least one benzodiazepine drug, such as at least one of Alprazolam, Chlordiazepoxide, Clorazepate, Diazepam, Flunitrazepam, Flurazepam, Halazepam, Lorazepam, Oxazepam, Prazepam, Temazepam and Triazolam. The formulation which comprises at least one benzodiazepine drug may also be characterized further by one or more of the features (i), (ii) and (iii) as described above.
…
[0015] In applying the invention for preventive purposes, i.e. in treating a patient who has been clinically diagnosed as having a condition susceptible to alleviation by administration of a benzodiazepine drug, while simultaneously preventing the occurrence in the patient of symptoms of dependence on, tolerance of, or addiction to said benzodiazepine drug, a benzodiazepine drug is administered in an amount effective to alleviate said condition, while concurrently administering to the patient an amount of melatonin which is effective to prevent at least one of such symptoms. The various embodiments described above as applicable to treating a patient having the stated symptom(s) are also correspondingly applicable to preventive purposes, except insofar as they will not be applicable for reasons which are self-evident to a person of the art, e.g. in this instance treatment with a benzodiazepine drug is a desideratum, so that evidently the amount of benzodiazepine administered, while possibly being reduced in any particular case as determined by a physician, will not be reduced to zero.
[0016] However, it will be within the scope of the preventive application of the invention, not only to administer, concurrently with melatonin, the benzodiazepine drug(s) at the conventional daily dosage rate to achieve a particular purpose, but in the alternative to similarly administer such drug(s) at a daily rate which is less than that which is conventionally administered to a patient in order to alleviate said condition.
…
EXAMPLE 3
[0037] This example illustrates the effects of long term administration of melatonin in the treatment of insomnia in patients dependent on a benzodiazepine drug.
[0038] Two volunteers, Y.L, an 80 year old male, and E.L., a 73 year old female, had each suffered for a number of years from insomnia and/or frequent awakenings during the night accompanied by difficulty in resuming sleep afterwards. Both were found to have low melatonin secretion, by determination of the amount of the metabolite 6-sulphatoxymelatonin, in the urine. Both patients had been taking 1 -2 mg of flunitrazepam orally prior to retiring each evening.
[0039] Each patient was weaned off the flunitrazepam by gradually reducing the dose and simultaneously administering melatonin orally (2 mg melatonin daily in controlled release form) over a two-month period. Since the end of that period, each patient has continued taking melatonin in the same form and at the same dosage rate over approximately two years.
[0040] Each patient has subjectively reported good sleep inducement and a substantial improvement in sleep quality. Specifically, patient E.L. noted an improvement in sleep quality at the beginning of the weaning period and Y.L noted a similar effect about two weeks into the weaning period. Each patient reported reduced fatigue during the daytime within several days after the beginning of the weaning period, and also indicated that the melatonin has caused neither residual tiredness in the morning, nor any hangover feeling. No side effects were reported by either patient.
(Emphasis added)
372 In their written closing submissions, the respondents argued that three scenarios are identified in para 8 of the 878 Patent. The first is treating addiction in a multi-drug addict. The second is treating a person who has symptoms of having become dependent, tolerant, or addicted to benzodiazepines. The third is use in a preventative sense to prevent a patient from becoming dependent, tolerant, or addicted to benzodiazepines by administering melatonin to a patient who has been clinically diagnosed as having a condition susceptible to alleviation by administration of a benzodiazepine drug (“i.e. preventative use”).
373 The respondents submitted that insomnia, including primary insomnia, is a condition susceptible to alleviation by administration of a benzodiazepine drug. The respondents submitted that this interpretation arose in light of the common general knowledge, given that benzodiazepine receptor agonist drugs were known to be a drug of choice for the treatment of insomnia including primary insomnia. Accordingly, they submitted that the 878 Patent, insofar as it teaches “preventative use” of melatonin in insomniacs, contains an express disclosure of the method of the Patent, in that it is the patients’ insomnia that is being treated by the use of melatonin.
Primary insomnia
374 The term “primary insomnia” does not appear in the 878 Patent. Neurim relied on the agreement of Professors Roth, Glozier and Wheatley in JER 2 that they could not determine what proportion of the participants (if any) in the 878 Patent may have met the diagnostic criteria for primary insomnia. Neurim submitted that this alone is sufficient to dispose of the lack of novelty case based on the 878 Patent.
375 As I have noted above in relation to para 8 of the 878 Patent, the respondents submitted that the 878 Patent discloses the use of melatonin in patients with primary insomnia because primary insomnia is “a condition susceptible to alleviation by administration of a benzodiazepine drug.” In support of this submission, the respondents relied on the evidence of Professor Wheatley in Wheatley 1 where he explained that given the context of para 4 and the examples of the 878 Patent, he “would understand the patient group described to be insomnia patients including, but not limited to, patients with primary insomnia.”
376 The respondents also relied on the evidence of Professor Roth during cross-examination, where he agreed that the statement in para 2 “dependence on benzodiazepines often develops in insomniacs” would include primary insomniacs because benzodiazepines were a treatment of choice for insomnia, including primary insomnia. Professor Roth also agreed during cross-examination that insomnia would be an example of “a condition susceptible to alleviation by administration of a benzodiazepine”. However, he observed that such a “condition” would also include Generalized Anxiety Disorder, seizures, depression, and REM behaviour disorder, as all of these conditions are treatable with benzodiazepines. On balance, I am not persuaded that there is a disclosure of the treatment of patients suffering from primary insomnia in the 878 Patent.
Use of prolonged release melatonin to treat primary insomnia
377 It is not in dispute that the melatonin disclosed in the 878 Patent was a prolonged release formulation. It is described in dependent claim 5 as a “controlled release formulation, wherein the melatonin is released at a predetermined controlled rate.”
378 As stated above, the respondents submitted that the preventative use disclosed in paras 1 and 8 of the 878 Patent, is the use of melatonin to treat a patient who has a condition susceptible to alleviation by administration of a benzodiazepine, such as primary insomnia, who is not dependent, tolerant, or addicted to benzodiazepines. According to the respondents’ submission, the 878 Patent discloses the use of melatonin in place of benzodiazepines to treat the relevant condition (i.e. insomnia, including primary insomnia) and to prevent the occurrence of symptoms of dependence, tolerance, or addiction to benzodiazepines. On this interpretation of the 878 Patent, the patient, who has not developed a tolerance, dependence or addiction to benzodiazepines, uses melatonin to treat the condition and avoid the development of such a dependence, tolerance or addiction.
379 The respondents accepted in their written closing submissions that there is no specific example in the 878 Patent that is directed to the preventative use of melatonin. They submitted that this does not negative the existence of such a disclosure.
380 The respondents relied on Example 3 to support the proposition that the 878 Patent discloses melatonin as a monotherapy to treat insomnia, including primary insomnia. Example 3 states that it “illustrates the effects of long term administration of melatonin in the treatment of insomnia in patients dependent on a benzodiazepine drug”. In Example 3, two patients who each suffered for a number of years from insomnia and/or frequent awakenings during the night, accompanied by difficulty in resuming sleep afterwards, who had been taking a benzodiazepine before retiring each evening, were simultaneously administered benzodiazepines with melatonin for two months during a “weaning off period”. Following that period, the 878 Patent states that the patients had continued to take melatonin in the same form and same dosage for approximately two years.
381 Example 3 specifically focuses on the patient’s sleep quality improvement during the two-month weaning off period only and does not describe the patient outcomes during and after the two-year treatment with melatonin alone. The experts were not asked to give their opinion about what could be deduced from the use of melatonin alone (i.e. as monotherapy) during and after this two-year period. Accordingly, I am not persuaded that Example 3 provides any direction, recommendation or suggestion to use melatonin to treat primary insomnia, or primary insomnia characterised by non-restorative sleep to improve the quality of restorative sleep in such a patient.
382 During cross-examination, Professor Roth agreed that he understood the third category identified in paragraph 8 of the 878 Patent to be a preventative use of melatonin to prevent a patient becoming dependent, tolerant, or addicted to benzodiazepines. He further explained that his understanding of the “preventative use” of melatonin was that melatonin was given simultaneously with benzodiazepines. He stated that when he read the 878 Patent as a whole (noting that none of the examples included the preventative use relied on by the respondents), he recognised the possibility that the 878 Patent disclosed the use of melatonin alone (i.e. instead of benzodiazepines) to treat a condition (that could be treated with benzodiazepines) and in doing so prevented the development of symptoms of dependence, tolerance or addiction to benzodiazepines. However, he drew particular attention to paragraphs 15 and 16 which state:
[0015] In applying the invention for preventive purposes, i.e. in treating a patient who has been clinically diagnosed as having a condition susceptible to alleviation by administration of a benzodiazepine drug, while simultaneously preventing the occurrence in the patient of symptoms of dependence on, tolerance of, or addiction to said benzodiazepine drug, a benzodiazepine drug is administered in an amount effective to alleviate said condition, while concurrently administering to the patient an amount of melatonin which is effective to prevent at least one of such symptoms. The various embodiments described above as applicable to treating a patient having the stated symptom(s) are also correspondingly applicable to preventive purposes, except insofar as they will not be applicable for reasons which are self-evident to a person of the art, e.g. in this instance treatment with a benzodiazepine drug is a desideratum, so that evidently the amount of benzodiazepine administered, while possibly being reduced in any particular case as determined by a physician, will not be reduced to zero.
[0016] However, it will be within the scope of the preventive application of the invention, not only to administer, concurrently with melatonin, the benzodiazepine drug(s) at the conventional daily dosage rate to achieve a particular purpose, but in the alternative to similarly administer such drug(s) at a daily rate which is less than that which is conventionally administered to a patient in order to alleviate said condition.
(Emphasis added)
383 I consider that paragraphs 15 and 16 make clear that Professor Roth’s understanding of the preventative use, described in the 878 Patent, is correct. Accordingly, I accept that the 878 Patent discloses the use of benzodiazepines co-administered with melatonin in patients that are not yet dependent, tolerant or addicted to benzodiazepines. When co-administered with melatonin, the benzodiazepine treats the condition (i.e. insomnia, General Anxiety Disorder, depression), whilst the melatonin prevents or reduces symptoms of dependence, tolerance, or addiction to the benzodiazepine. I am not persuaded that there is any clear direction, recommendation or suggestion conveyed by the 878 Patent to use melatonin to treat insomnia, or primary insomnia or primary insomnia characterised by non-restorative sleep. In the result, the novelty challenge based on the 878 Patent fails.
384 An invention is a patentable invention if the invention, when compared with the prior art base, involves an inventive step: see s 18(1)(b)(ii) of the Act. Section 7(2) of the Act uses the word “obvious” in the course of describing what must be established before an invention can be held not to involve an inventive step. Something may be “obvious” in light of the common general knowledge, or the common general knowledge coupled with relevant s 7(3) information.
385 An invention may be obvious in light of the common general knowledge if the person skilled in the art faced with the same problem as the inventor would have taken, as a matter of routine, whatever steps might have led from the prior art to the invention, whether they be the steps of the inventor or not. If the person skilled in the art would be directly led as a matter of course to take such steps in the expectation that doing so might well produce a useful or better alternative to the prior art then the invention will be obvious: Wellcome Foundation Limited v VR Laboratories (Aust.) Proprietary Limited (1981) 148 CLR 262 (“Wellcome”) at 286 per Aickin J, Alphapharm at [50]-[53]. In Alphapharm at [53] the plurality approved what is commonly referred to as the reformulated or modified Cripps question as providing an acceptable approach to obviousness.
386 A claimed invention is not obvious merely because the person skilled in the art would consider that it was “worthwhile to try”. However, there will be some cases in which the person skilled in the art will be directly led, as a matter of course, to try a number of different alternatives in the expectation that each may well produce a useful alternative. Merely because one pathway to an invention is shown to be obvious, does not mean that another such pathway might not also be obvious. Two or more pathways may be obvious, even though some of them might be more obvious than others.
387 Further:
The question is not whether the claimed invention is obvious to the Court, but whether it would be obvious to the person skilled in the art who is taken to be equipped with the relevant common general knowledge as it stood at the priority date together with any relevant s 7(3) information but who lacks any capacity for inventiveness.
A “scintilla of invention” can sustain a valid patent, but there must be “some difficulty overcome, some barrier crossed” or something “beyond the skill of the calling”: Lockwood Security Products Pty Ltd v Doric Products Pty Ltd (No 2) (2007) 235 CLR 173 (“Lockwood (No 2)”) at [52]; RD Werner & Co Inc v Bailey Aluminium Products Pty Ltd (1989) 25 FCR 565 at 574; Allsop Inc v Bintang Ltd (1989) 15 IPR 686 at 701.
The court must be wary of the misuse of hindsight or ex post facto analysis in deciding whether a claimed invention lacks any inventive step: see Aicken J in 3M at 293-294 and Wellcome at 286, and the plurality in Alphapharm at [21].
388 When postulating the modified Cripps question solely in the context of s 7(2) of the Act (i.e., in the absence of any relevant s 7(3) information) the prior art referred to must be confined to prior art information that forms part of the common general knowledge in the field at the relevant date. To the extent it is shown that there is any additional information of the kind referred to in s 7(3) then the person (or team) skilled in the art will also be taken to be in possession of that information.
389 The respondents’ obviousness case relies on the common general knowledge and the following documents (“7(3) documents”):
(1) Haimov 1995;
(2) Garfinkel et al, “Improvement of sleep quality in elderly people by controlled-release melatonin”, The Lancet, 346:541-544 (1995) (“Garfinkel 1995”);
(3) Zisapel, “Development of a Melatonin-Based Formulation for the Treatment of Insomnia in the Elderly”, Drug Development Research, 50:226-234 (2000) (“Zisapel 2000”); and
(4) Garfinkel et al, “Facilitation of Benzodiazepine Discontinuation by Melatonin”, Arch Intern Med, 159:2456-2460 (1999) (“Garfinkel 1999”).
Garfinkel 1999 is relied on by the respondents as a 7(3) document but only in combination with other 7(3) documents.
390 The respondents did not advance any obviousness case based on the common general knowledge alone. However, they said that the invention as claimed was obvious at the priority date in light of the common general knowledge together with Haimov 1995, Garfinkel 1995 and Zisapel 2000 each considered separately. In addition, the respondents also relied on the following combinations of 7(3) documents:
(1) Haimov 1995 and Zisapel 2000;
(2) Haimov 1995, Garfinkel 1995, and Zisapel 2000; and
(3) Haimov 1995, Garfinkel 1995, Garfinkel 1999 and Zisapel 2000.
391 The first question to be answered is whether a person skilled in the art would be reasonably expected to have ascertained, understood and regarded each of the 7(3) documents as relevant to treating a patient with primary insomnia characterised by non-restorative sleep and improving the restorative quality of sleep in such patient. If the answer to this question is yes, it must then be determined whether the person skilled in the art could reasonably have been expected to combine the documents in the combinations proposed by the respondents. The next question is whether the invention as claimed is obvious in the light of the common general knowledge together with any of the 7(3) documents considered separately or in any permissible combination of those documents.
Reasonably expected to have ascertained, understood and regarded the prior art documents as relevant
392 The operation of s 7(3) was summarised by Kiefel J (with whom Gageler and Keane JJ agreed) in AstraZeneca HCA at [68]-[70]:
[68] Before a document containing prior art information can be used along with the common general knowledge for the purposes of the s 7(2) inquiry, it is necessary that it meet the requirements of s 7(3). In [Lockwood (No 2)] it was explained that prior art information which is publicly available in a single document is “ascertained” if it is discovered or found out, and “understood” means that, having discovered the information, the skilled person would have comprehended it or appreciated its meaning or import. The Court also explained that the phrase “relevant to work in the relevant art” is directed to publicly available information, not part of the common general knowledge, which the skilled person could be expected to have regarded as relevant to solving a particular problem, or meeting a long-felt want or need, as the patentee claims to have done.
[69] [Lockwood (No 2)] also explains [at [127]] that, in answering the question of obviousness, the information referred to in s 7(3), like that part of the prior art base which is the common general knowledge, is considered for a particular purpose. That purpose is to look forward from the prior art base to see what the skilled person is likely to have done when faced with a problem similar to that which the patentee claims to have solved with the claimed invention. It is this aspect of the s 7(2) inquiry which assumes particular importance on these appeals.
[70] In addressing s 7(2), it is to be borne in mind that the skilled person is an artificial construct, intended as an aid to the courts in addressing the hypothetical question of whether a person, with the same knowledge in the field and aware of the problem to which the patent was directed, would be led directly to the claimed invention. The statute’s creation of the skilled person construct for this purpose is not to be taken as an invitation to deal with the question posed by s 7(2) entirely in the abstract. Whilst the question remains one for the courts to determine, the courts do so by reference to the available evidence including that of persons who might be representative of the skilled person.
(Footnotes omitted)
393 Her Honour’s reference to “a problem similar to that which the patentee claims to have solved” reflects what was said by the plurality in Lockwood (No 2) at [127]. However, I note that the plurality in Lockwood (No 2) at [153] and Aickin J in Wellcome at 286 referred to “the same problem” rather than “a similar problem”. In light of those authorities, it is appropriate to ask whether the documents containing the prior art information would be perceived by the person skilled in the art as relevant to the same or a similar problem to that addressed by the Patent.
394 The meaning of the component parts of “reasonably expected to have ascertained, understood and regarded as relevant” was also considered by Beach J in Sequenom, Inc v Ariosa Diagnostics, Inc. (2019) 143 IPR 24 (“Sequenom”). His Honour observed at [556]-[570]:
[556] As at the priority date, in order for information in addition to common general knowledge to be able to be taken into account in assessing inventive step, it was a requirement pursuant to s 7(3) (in its then terms) that a person skilled in the art could, before the priority date, be reasonably expected to have ascertained, understood, and regarded as relevant that information.
[557] The word “ascertained” means “discovered or found out”. The fact that a document has been published does not mean that a person skilled in the art could be reasonably expected to have ascertained that information. The relevant question is whether the document was published in such a manner or form that it could reasonably have been expected to be found by a person skilled in the art.
[558] In assessing whether a person skilled in the art could be reasonably expected to have ascertained the information, it is important to consider the characteristics of the person skilled in the art, the nature of the problem, and the information typically used by the persons skilled in the art. Section 7(3) does not assume an ascertainability by any and all skilled persons, of whatever description, of all publicly available prior art documents anywhere in the world.
…
[564] Further, the requirement of “reasonableness” is applied to each of the “ascertained”, “understood” and “regarded as relevant” limbs of the s 7(3) test.
[565] In Aspirating IP Ltd v Vision Systems Ltd (2010) 88 IPR 52; [2010] FCA 1061, it was explained at [457] to [458] that whether something could be reasonably expected requires a prediction and that in the context of s 7(3) the question is whether, having regard to the evidence, it may be reasonably predicted that the hypothetical non-inventive skilled worker faced with the relevant problem before the priority date would have ascertained, understood and regarded as relevant the particular s 7(3) information in question.
…
[570] So a mere “possibility” of an alleged s 7(3) document being ascertained or treated as relevant is not sufficient for the purposes of s 7(3). And the relevant question is to be posed in terms of “would find” rather than “could find”.
395 The respondents’ relied on the evidence of Professor Wheatley concerning a hypothetical research exercise he undertook with the assistance of a researcher, Mr Jennings, to prove that the skilled addressee could reasonably be expected to have ascertained each of the 7(3) documents.
396 The respondents’ solicitors, Herbert Smith Freehills (“HSF”), asked Professor Wheatley to describe what treatments he would prescribe for an insomnia patient who:
(1) has no underlying condition that causes the insomnia; and
(2) complains of day time fatigue and/or not feeling rested after sleep.
(“the Task”).
397 Professor Wheatley completed the Task prior to being shown the Patent and considering the claims. I will reiterate here that Professor Wheatley’s evidence was that, at the priority date, he knew of but did not use DSM-IV and that the term “non-restorative sleep” was unfamiliar to him. Furthermore, during cross-examination, Professor Wheatley accepted that at the priority date, he was not familiar with primary insomnia characterised by non-restorative sleep within the meaning of the DSM-IV.
398 In Wheatley 1, Professor Wheatley first gave evidence of the available and existing treatments he would have prescribed at the priority date for an insomnia patient of the kind described in the Task. He identified the approaches he already used at the date, including sleep hygiene therapy, behavioural therapy and prescribing temazepam, zolpidem and zopiclone.
399 HSF then asked Professor Wheatley if there were any additional treatments that he would want to prescribe if they were available to him. He responded that he would (and did) refer some patients to sleep clinics for cognitive behavioural therapy (“CBT”), and he would also consider prescribing melatonin which he did not do at the time because it was not available in Australia. He said that he would have prescribed melatonin because:
(1) at the priority date, even though the safety profile of melatonin was not well-established through clinical trials, melatonin was readily available over the counter and popular in the United States;
(2) melatonin is short-lived, being rapidly metabolised following its absorption over the course of a few hours;
(3) there was a significant amount of research conducted on the effect of melatonin on circadian rhythms including the safety and side effect profile of melatonin doses;
(4) melatonin had been shown to be a mild hypnotic at doses of between 1 to 3 mg;
(5) melatonin likely had a wide safety margin based on extensive use in the United States including at doses which exceeded 10 mg; and
(6) no significant adverse effects were known to be associated with melatonin despite the wide use and he therefore did not have any significant concerns about the safety of melatonin use in the short-term.
Professor Wheatley said he would have had been more interested in an oral tablet dosage form rather than liquid formulation.
400 Professor Wheatley acknowledged that there was uncertainty surrounding the dose or dose range that would be safe or efficacious for treatment of insomnia at the priority date. He gave evidence that he would have consulted the textbook Sleep Medicine to find information about a dose or dose range of melatonin that may be useful for the treatment of an insomnia patient described in the Task. He identified Chapter 31 as being relevant to his task. He explained at paras 130-131 of Wheatley 1:
130. …In general terms, I considered that Chapter 31 provided a very useful and contemporary summary of studies that examined the effect of melatonin on sleep regulation (and also circadian rhythms) at around the time of publication of the text, including its effect as a hypnotic to induce and / or maintain sleep across a range of physiological and pharmacological doses (0.3 — 80 mg) in both healthy subjects and in people with chronic insomnia. A ‘physiological’ dose of melatonin is a dose of a size up to 1 mg that produces similar peak levels of melatonin in the blood to that produced in normal circadian cycles. A ‘pharmacological’ dose of melatonin is a dose of a size intended to exert a therapeutic effect, as opposed to replacement of normal endogenous melatonin levels. Consistent with my understanding of textbooks generally (discussed at paragraph 122 above), the authors took a cautious approach to their recommendations and conclusions, noting the lack of carefully controlled clinical trials regarding the efficacy and safety of melatonin, including for the treatment of sleep disorders. The caution expressed by the authors of this text does temper my approach to the Task, by which I mean that I would need to review any clinical trial research reports with an awareness that there is not a large body of clinical research that supports the efficacy and safety of melatonin for the treatment of insomnia. Although, as stated in paragraph 112 above, the need for further clinical research to establish the long-term safety and appropriate dose for melatonin in insomnia is something that I was aware of at the time. In general terms, I found Chapter 31 to support the view that melatonin may be a useful treatment for primary insomnia and for the patients described in the Task.
131. Chapter 31 contained references to several published papers on the use of melatonin. If I had read Chapter 31 as at August 2001 with the Task in mind, then I would have obtained copies of the following footnoted articles that I consider, based on the context in which the footnotes appear in Chapter 31 and the title of the articles, likely to be of relevance to the Task:
…
(g) Footnote 38: Garfinkel D, Laudon M, Nof D, et al. ‘Improvement of sleep quality in elderly people by controlled-release melatonin.’ Lancet (1995) 346: 541 — 544 (Garfinkel 1995); and
(h) Footnote 39: Haimov I, Lavie P. ‘Potential of melatonin replacement therapy in older patients with sleep disorders.’ Drugs Aging (1995) 7: 75 — 78 (Haimov).
401 The article referred to in Footnote 38 is Garfinkel 1995. The article by Haimov and Lavie referred to in Footnote 39 (“Haimov”) is not the same article as Haimov 1995 which is referred to above and relied on by the respondents in support of their novelty and inventive step case. However, Haimov 1995 is referenced at footnote 35 of Haimov. Professor Wheatley explained the relevance and usefulness of Haimov and Haimov 1995 in para 133 of Wheatley 1 as follows:
Haimov is a review article related to the potential use of melatonin as replacement therapy in elderly patients with sleep disorders that includes a summary of recent clinical trials with melatonin. Haimov includes reference to a study ‘recently’ conducted by the authors using 2 mg sustained release (SR) and conventional release melatonin where sleep-wake patterns of subjects were monitored objectively using actigraphs. This study is footnote 35 in Haimov and is to an article in Sleep titled ‘Melatonin replacement therapy of elderly insomniacs’. The article is stated to be ‘in press’. I would have obtained a full text copy of the article in Sleep to review because I consider that it would likely contain information that would assist me with the Task.
402 In Wheatley 1, Professor Wheatley contended that textbooks including Sleep Medicine tend to take a cautious approach to recommendations, as they are targeted at reflecting established practice rather than newer or evolving approaches, and do not necessarily capture the most recent research. Therefore, in addition to consulting Sleep Medicine, he said that he would also seek to obtain information about melatonin to assist with the Task by conducting a literature search. His objective in requesting a literature search was to identify the dose or dose range of melatonin that would be safe and efficacious for the treatment of an insomnia patient.
403 A crucial feature of Professor Wheatley’s approach to the Task was his decision to try melatonin as a treatment for patients suffering from insomnia not caused by any underlying condition (i.e. what might generally be termed primary insomnia) who complain of day time fatigue and/or not feeling rested after sleep. It is notable, as well, that the complaints described by the Task are complaints which may be made by patients whose insomnia is solely attributable to difficulties initiating or maintaining sleep leading to inadequate sleep duration, but might also be made by patients who do not experience inadequate sleep duration, but complain of day time fatigue and/or not feeling rested after sleep in the sense of non-refreshing sleep. The Task as presented to Professor Wheatley does not distinguish between non-restorative sleep, and other symptoms of insomnia, which may or may not occur in isolation.
404 In Wheatley 1, Professor Wheatley explained his process at the priority date of conducting or requesting a literature search as follows:
123. Prior to August 2001, I had experience with both conducting literature searches myself and requesting literature searches to be conducted on my behalf, and reviewing the result of those searches. Most commonly, I requested a researcher from our research unit to conduct the searches on my behalf. We had, and continue to have, a dedicated research unit in the Department of Respiratory and Sleep Medicine at Westmead Hospital to assist clinicians with research. The research staff were (and are) familiar with the use of databases for conducting these searches, and I relied upon their expertise to identify appropriate databases to search and to formulate appropriate search terms and techniques to ensure that the searches produced optimal results. By optimal results I mean that the number of titles/abstracts generated by the search would be in the order of around 50, and that those titles or abstracts would be relevant to the research task. In my experience, around 50 documents is a manageable number of documents to review in abstract form and make an informed decision regarding the need and benefit of a full text review of any of the documents.
124. Prior to August 2001, when requesting literature searches, I typically provided the researcher assisting me with background information about the search task including a description of the nature of the information I was seeking and some potential search terms to consider. I then asked the researcher to use their expertise to formulate and conduct an appropriate search to address the task I had given them. I would expect that if the researcher encountered any difficulties or if the search was not returning any useful results, the researcher would come back to me for some further input on the search. I would also expect the researcher to narrow the search until about 50 abstracts/titles were identified. I would then review this relatively short list of results to identify the articles that I would want to review in full.
405 Professor Wheatley devised the following task and instructions that he would have given to a researcher prior to August 2001 for the purpose of carrying out the literature search:
TASK
I would like to find information about:
(a) the use of melatonin for an insomnia patient who:
(i) has no underlying condition that causes the insomnia, such as respiratory sleep disorders or periodic limb movement disorder; and
(ii) complains of day time fatigue and/or not feeling rested after sleep.
(Insomnia Patient); and
(b) the dose or dose range of melatonin that would be safe and efficacious for the treatment of an Insomnia Patient.
Instructions
• Please include all available types of information that you consider to be relevant. Please use your expertise to determine the appropriate databases to search.
• Please search for documents published in English;
• Search terms to consider are ‘melatonin’, ‘insomnia’, ‘hypnotic’, and ‘dose’. However please use your expertise in formulating appropriate search terms and techniques to address the task and to generate about 50 titles or abstracts for my review.
406 HSF retained a patent and literature searcher, Mr Anthony Jennings, to conduct both literature and patent searches and he presented Professor Wheatley with two sets of search results. Whilst Professor Wheatley did not request patent searches, HSF explained to him that this course was the typical practice of Mr Jennings in response to Professor Wheatley’s instructions.
407 Professor Wheatley reviewed the literature and patent results to identify any records that he considered potentially relevant to the Task and which he would like to review in full. Based on his review, he was comfortable that the searches had identified a sufficient number of literature articles that would likely assist him in the Task, being 45 literature records. He did not identify any patents that were of interest to him as potentially relevant to the Task.
408 From the 45 literature records, Professor Wheatley considered 14 literature records were of interest to him because the titles and abstracts indicated that these publications all involved a consideration of the efficacy and/or safety of one or more doses of melatonin in adults to improve sleep. He reviewed (in full) the 14 literature records while considering the following parameters in order to assess their relevance to the Task: (a) the dose of melatonin studied (he was particularly interested in papers reporting on the use of pharmacological doses), (b) any side effects of melatonin treatment and (c) efficacy of melatonin in the treatment of insomnia. Following this review, he identified 12 literature records relevant to the Task including Zisapel 2000, Garfinkel 1999 and Garfinkel 1995. He also observed that Zisapel 2000, as well as two other literature records identified in the search, included a reference to Haimov 1995 and that based on these references, and the fact that the article was published in the journal Sleep (which he read regularly), he would have obtained a full copy of Haimov 1995 to see if it was relevant to the Task.
Neurim’s criticism of the Task
409 It is useful at this point to refer to a number of criticisms made by Neurim in relation to Professor Wheatley’s evidence concerning obviousness. First, Neurim submitted that Professor Wheatley was not a person skilled in the art and therefore could not give admissible evidence on the topic. That argument has already been considered and rejected. Next it was submitted that the Task was “fundamentally flawed” because it was not directed to a patient suffering from primary insomnia characterised by non-restorative sleep. In particular, Neurim submitted that “the Patent defines primary insomnia characterized by non-restorative sleep according to the DSM-IV criteria, and a patient that had “daytime fatigue” or “not feeling rested after sleep” (but not both), does not meet those criteria” (emphasis in original). Neurim also submitted that in addressing the Task, Professor Wheatley “was inappropriately led towards melatonin” by HSF. As a consequence of what Neurim characterised as “inappropriate leading”, Professor Wheatley is said by Neurim to have had recourse to various publications which he would not otherwise have ascertained or considered relevant.
410 Further, Neurim was highly critical of the follow-up question asked by HSF after Professor Wheatley first identified a range of available treatments for insomnia patients, which asked whether there were any additional treatments that he would want to prescribe if they were available. Neurim submitted that, in addressing the Task, Professor Wheatley was “steered away” from the use of a range of different treatments that he might otherwise have considered worth trying as a treatment for the patient described in the Task.
411 There were also a number of criticisms made by Neurim of the search processes undertaken by Mr Jennings. Neurim criticised the fact that Mr Jennings searched for patents and patent applications, notwithstanding that Professor Wheatley did not ask him to do so. In circumstances where none of the s 7(3) documents identified by Professor Wheatley or relied on by the respondents include any such documents, that criticism goes nowhere. Considerable emphasis was placed on the fact that Mr Jennings chose not to include the search term “hypnotic”, and did not explain why, even though this term was specified by Professor Wheatley. Neurim submitted that the use of that search term may have returned results relating to various hypnotic drugs which Professor Wheatley identified as being suitable to the pharmaceutical management of insomnia, and those which he identified as specifically suitable for treating primary insomnia. I do not think there is any substance to that criticism. Professor Wheatley’s instructions make clear that he was interested in obtaining information about melatonin, not any hypnotic, so Mr Jennings’ decision to exclude that term is understandable. As Neurim’s submission implicitly acknowledges, use of the search term “hypnotic” may well have produced many search results that had nothing to do with melatonin. What is in my opinion more important, is the fact that Professor Wheatley identified melatonin as a potential treatment before providing any instructions to Mr Jennings. In this regard, the instructions provided by Professor Wheatley to Mr Jennings were directed to the use of melatonin as a treatment for primary insomnia and the suitable dose or dose range.
Analysis
412 Chapter 31 of Sleep Medicine suggests that melatonin can induce and maintain sleep due to its mild hypnotic effect. However, the authors make the point that few attempts had been made to determine the effects of melatonin as a hypnotic in persons with insomnia. Rather, the Chapter indicates that a number of studies to that time had examined the effects of melatonin in the treatment and alleviation of perceived effects of jetlag and to elicit changes in endogenous circadian rhythms. Even there, the authors refer to a study that concluded the effect of melatonin was not sufficient to warrant its use as a phase shifting agent for alleviation of the effects of jetlag. The authors state in their conclusions that “the combined circadian and hypnotic effects of melatonin would make it an attractive candidate for the treatment of sleep disorders related to inappropriate circadian timing”. They refer to the need for carefully controlled clinical trials that focus on the possible beneficial effects of melatonin on specific sleep disorders. They also warn against the chronic use of melatonin for any sleep disorder because “neither the therapeutic nor the potential toxic effects of long-term use of this hormone, which has profound effects on the reproductive system of other mammals, are known”.
413 Professor Roth stated in his affidavit evidence that, at the priority date, melatonin was known as an effective chronobiotic but not thought to be useful in the treatment of insomnia. That evidence, originally admitted provisionally, is now admitted by me as evidence of his opinion. It is broadly consistent with what appears in Chapter 31 of Sleep Medicine which highlighted the potential for melatonin to be used in the treatment of sleep disorders related to inappropriate circadian timing. However, there is nothing in Chapter 31 of Sleep Medicine (or any other chapter in evidence) which directly suggests that melatonin may be useful in treating patients whose primary insomnia is characterised by non-restorative or unrefreshing sleep.
414 The various considerations that led Professor Wheatley to say that he would have prescribed melatonin (if it was available) primarily related to what he regarded as melatonin’s wide safety margin. With regard to its potential as an efficacious treatment, he referred to melatonin’s effect on circadian rhythms and its mild hypnotic effect. The first of those effects was known at the priority date as was the possibility that melatonin may also act as a mild hypnotic.
415 However, Professor Wheatley’s evidence does not explain why he would be led to try melatonin as a treatment for a patient complaining of non-restorative or unrefreshing sleep. In this regard, Professor Wheatley acknowledged (as previously discussed) that there are some patients suffering from primary insomnia who complain of unrefreshing sleep that is not associated with any complaint of difficulty initiating or maintaining sleep. His evidence does not explain why he would have viewed melatonin as a promising treatment for such patients, or patients who experience the symptom of non-restorative or unrefreshing sleep alongside difficulties initiating or maintaining sleep. To some extent this is due to the terms in which the Task was formulated.
416 Professor Wheatley was not asked to advise on a potential treatment for primary insomnia where the patient’s complaint was of unrefreshing sleep either independent of any difficulty initiating or maintaining sleep, or in tandem with those symptoms. The respondents submitted that it would not have been appropriate to frame the Task in those terms because, as I understood the submission, this would have involved leading Professor Wheatley to the invention. I do not accept that submission. Identifying in the Task the problem addressed in the Patent would not amount to leading unless the inventor’s perception of the problem was said to involve an inventive step. It was also submitted that it would not have been appropriate to use, in describing the Task, terminology which Professor Wheatley did not use in practice. However, that submission still does not answer the criticism made, which is that the language in the Task misdescribes the problem addressed by the Patent.
417 The way in which the Task was formulated (i.e., “complains of daytime fatigue and/or not feeling rested after sleep”) was broad enough to include potential treatments for primary insomnia that were solely directed to improving sleep initiation or maintenance rather than quality of sleep in the sense of the restorative quality of a sleep. This meant that the scope of the question prompted Professor Wheatley to consider new treatments which assisted in sleep initiation and maintenance regardless of whether such treatments might also contribute to any improvement in a patient’s non-restorative (or unrefreshing) sleep. In circumstances where the claimed invention is directed specifically to the treatment of primary insomnia characterised by non-restorative sleep, I do not consider that the Task given to Professor Wheatley is directed to the same or a similar problem to that addressed by the Patent.
418 While I considered Professor Wheatley to be an impressive witness, there are a number of other matters which to my mind diminish the persuasiveness of his evidence in relation to obviousness. While it is true that he had not been shown the Patent prior to addressing the Task, there is no doubt that by the time he completed the Task he had been aware for some years that melatonin was approved for use in Australia as a treatment for patients suffering from primary insomnia. Melatonin had not been approved at the priority date for the approved indication or any other indication. This is a common problem in cases where the invention becomes well-known to persons skilled in the art after the priority date. In that respect, to the extent that Professor Wheatley’s evidence is affected by hindsight, it is difficult to see how that problem could have been avoided. But the fact that the problem of hindsight could not be avoided does not mean that it can be ignored and, in this particular case, it diminishes considerably the weight which I give to Professor Wheatley’s evidence as to what he would have done if asked to address the Task at the priority date.
Was Professor Wheatley steered towards melatonin as a starting point?
419 As I have explained above, apart from the formulation of the Task, Neurim was highly critical of a “follow up” question HSF asked Professor Wheatley (i.e., were there any additional treatments that he would have wanted to prescribe if they were available).
420 The drugs known to Professor Wheatley in August 2001 that had a hypnotic effect included various benzodiazepines (including temazepam, triazolam, flunitrazepam and nitrazepam), zolpidem (stilnox), zopiclone, various antianxiety agents, various tricyclic anti-depressants, anti-histamines and various herbal products. He was aware that benzodiazepines, zolpidem, zopiclone, antianxiety agents, and tricyclic anti-depressants had been prescribed for the management of insomnia patients by general practitioners and by respiratory and sleep physicians prior to August 2001. He was also aware that anti-histamines and herbal products (both over-the-counter medications) were taken by patients suffering from primary insomnia.
421 As at August 2001, Professor Wheatley had prescribed temazepam, zolpidem and zopiclone for the treatment of primary insomnia. He knew that there was some use by general practitioners of tricyclic anti-depressants for their hypnotic qualities in the treatment of insomnia though he did not suggest that tricyclic anti-depressants or antianxiety agents had been prescribed for the treatment of primary insomnia. I infer that those drugs were primarily prescribed for the treatment of other disorders (e.g. depression and anxiety) and that, to the extent they were used to treat insomnia, it was most likely in the context of a comorbidity.
422 In cross-examination Professor Wheatley was referred to that part of Wheatley 1 in which he states (para 121) that he would have considered prescribing melatonin if it had been available in Australia as at August 2001. Having been referred to that part of his affidavit, Mr Shavin QC, asked Mr Wheatley “of all the possible treatments for insomnia, professor, what caused you to jump to melatonin?” Professor Wheatley gave this evidence in response to that and related questions:
PROF WHEATLEY: As I understand of [sic] this point of the task, I have been asked what treatments I would prescribe, and we went through the routine ones in the paragraph before that I would normally have employed. It moved to a discussion about CBT which I was not qualified to perform but was certainly well aware was a very valuable adjunct to the treatment. And it was available in a very limited fashion in Australia at that time. So I would have potentially wanted to trial that. And I guess the context of this question was were there any additional treatments I would want to prescribe if they were available to me. The context that I understood that was being put to me was, are there other medications or therapies that you, potentially, could consider? And I’m not – I don’t profess to understand why I would have been wanting to do that at the time, having not necessarily gone through the existing treatments, but that was the question I was asked.
And really, the only medication that I was aware of that potentially might be being used in insomnia management would be melatonin. I had no other drug knowledge of development of new drugs in insomnia that I could pursue. And an awareness that melatonin, albeit, not in a licensed form that was being used in the US to a large degree. And that’s – a lot of discussions both at meetings and with colleagues around the availability of that medication in the US but not – it was not available in Australia. I don’t think it was even available as a – as a herbal supplement at that time it was more controlled in this country.
MR SHAVIN: Can I take you back to paragraph 101 … did you turn your mind to whether you would want to explore whether there were other drugs within the class of benzodiazepines that you would want to undertake research into?
PROF WHEATLEY: No, I think I had assumed that benzodiazepines were covered in standard response to managing a patient with insomnia.
MR SHAVIN: Did you understand the question to which you’ve referred at paragraph 121, to be specifically pointing you to something that was not in the list at paragraph 101?
PROF WHEATLEY: The – yes, that would be my reading of that question at the moment, yes. And ..... - - -
MR SHAVIN: So that you understood yourself to having been directed away from considering whether there was prospective research that could be undertaken in relation to any of the drugs in paragraph 101 or any analogues of them?
PROF WHEATLEY: It’s – yes. I – I think my attention is being pushed away from the existing list of medications that I was aware of and towards something else if it was available. So it’s looking at new drugs.
(Emphasis added)
423 It would be logical for a clinician such as Professor Wheatley who was presented with the Task to explore the range of treatments that were available in Australia as at August 2001 for the purpose of determining whether they might alleviate the patient’s primary insomnia. This would include a range of different drugs with hypnotic effect that were available, including tricyclic anti-depressants and antianxiety agents. I note that the chapter on primary insomnia in Sleep Medicine (Chapter 55) states that some patients suffering from idiopathic insomnia (which, according to the same chapter, is a free-standing form of insomnia which is subsumed by primary insomnia under DSM-IV) had responded to tricyclic anti-depressants. However, the manner in which Professor Wheatley was asked to address the Task effectively excluded consideration of tricyclic anti-depressants and any other drugs that were approved for use in Australia when addressing the Task. He was instead directed to what he referred to as “new drugs” which I took to mean drugs that had not at that time been approved for use in Australia. Melatonin was the only new drug that he was aware of that he thought might be useful in insomnia management.
424 In the circumstances, I am not persuaded that a sleep physician such as Professor Wheatley would have, as at the priority date, been led directly to try melatonin as a treatment for primary insomnia characterised by non-restorative sleep in the expectation it may well provide an effective treatment. In saying this I recognise that the respondents do not contend that the invention of the claims was obvious at the priority date in light of the common general knowledge considered alone. Nevertheless, the starting point for Professor Wheatley’s search for a new treatment was melatonin and it is necessary to consider whether a person skilled in the art would have, at the priority date, adopted his starting point. I am not persuaded that a person skilled in the art would have done so.
425 Each of s 7(3) publications relied on by the respondents is specifically concerned with the use of melatonin as a treatment for insomnia. It is apparent that the research task given by Professor Wheatley to Mr Jennings was specifically targeted at the use of melatonin as a treatment for primary insomnia. It follows that the search results obtained by Mr Jennings, which includes most of the s 7(3) documents on which the respondents relied, were ascertained as a result of Professor Wheatley’s decision to propose melatonin as a treatment for the condition described in the Task. It also follows that the search and selection process followed by Professor Wheatley was fundamentally shaped by his decision to adopt melatonin as his starting point. The following analysis of the s 7(3) documents relied on by the respondents reflects the fact that Professor Wheatley was searching specifically for publications relevant to the use of melatonin as a treatment for primary insomnia.
Haimov 1995
426 Haimov 1995 was identified by Professor Wheatley as a result of consulting Chapter 31 of Sleep Medicine. Haimov 1995 is referred to in the footnotes of another paper, Haimov, which was referred to in the footnotes of Chapter 31 of Sleep Medicine. Haimov 1995 was also referred to in the footnotes of two other papers (one of which was Zisapel 2000) identified by Mr Jennings.
427 The respondents’ argued that Haimov 1995 would have been reasonably ascertained because it was published in the leading journal Sleep (which Professor Wheatley read at the priority date), has “melatonin” and “insomniacs” in the title, has “melatonin” in the keywords, and was one of the 13 articles ultimately selected by Professor Wheatley as relevant to the Task.
428 Assuming for present purposes that the person skilled in the art would have regarded melatonin as a promising candidate for use in the treatment of primary insomnia characterised by non-restorative sleep, then I do not think there is any doubt that Haimov 1995 would have been ascertained. It was published in what Professor Wheatley and Professor Roth agreed to be a leading journal in the field of sleep medicine. The title refers to melatonin and the abstract refers to the use of melatonin in the treatment of melatonin-deficient elderly insomniacs. The abstract also describes the dosages used in the course of the trial and refers to improvement in patients’ sleep maintenance and initiation. I am satisfied based on the subject matter of Haimov 1995 and the journal in which it appeared that it would have been ascertained by the person skilled in the art looking for information relating to the use melatonin in the treatment of primary insomnia.
429 The next question is whether the person skilled in the art would have understood Haimov 1995 in the sense of comprehending or appreciating the information it disclosed, and also regarded it as relevant to the problem addressed by the invention. I have previously discussed Haimov 1995 in the context of novelty. Among other things, I accepted Professor Roth’s evidence that the skilled addressee would not approach Haimov 1995 with an understanding that activity levels as measured by actigraphy provide a basis from which to draw inferences about the restorative quality of a patient’s sleep.
430 Professor Wheatley in Wheatley 1 said that he understood Haimov 1995 to provide convincing objective data that melatonin both in fast release and slow release formulations shortens sleep latency. He said that the data was consistent with his understanding that melatonin has a hypnotic effect which would reduce sleep latency. He understood reduced sleep latency and improvements to other objective parameters reported in Haimov 1995 would correlate with patients feeling more rested after sleep and less fatigued during the day because they would have less disrupted sleep. He said:
In summary, I consider that Haimov 1995 provides convincing objective data that [sustained release] melatonin causes a decrease in sleep latency, an increase in sleep efficiency and a decrease in the mean level of activity during sleep. These improvements indicate less disrupted, more continuous sleep.
I accept that evidence. However, I do not accept that the person skilled the art would have understood Haimov 1995 as suggesting that reduced levels of activity during sleep was indicative of improvements in the restorative sleep of patients. The abstract to Haimov 1995 and the discussion of the results makes clear that the therapy investigated by the authors led to improvements in sleep initiation and maintenance.
431 Professor Glozier gave evidence that Haimov 1995 suggests melatonin as a possible treatment for primary insomnia where a patient experiences non-restorative sleep. I am not persuaded that it does so. That said, I accept that the person skilled in the art would regard Haimov 1995 as relevant in that it provides potentially useful information concerning the safety of melatonin at dosages of 1 mg and 2 mg for sustained release and fast release formulations used in the study.
432 There is in my opinion no information disclosed in Haimov 1995 which would, if considered together with the common general knowledge as it stood at the priority date, directly lead a person skilled in the art to try melatonin as a treatment for primary insomnia characterised by non-restorative sleep. While Haimov 1995 provides useful information as to the safety of melatonin in a 1 mg or 2 mg dosage and indicates that it can reduce sleep latency (i.e. time to fall asleep) and improve sleep efficiency (i.e. ratio of time spent asleep to the time spent in bed), it does not suggest that the restorative quality of the patients’ sleep may be improved by administration of melatonin.
433 Garfinkel 1995 was identified by Professor Wheatley in the footnotes of Chapter 31 of Sleep Medicine. Garfinkel 1995 was also identified in the literature search conducted by Mr Jennings.
434 Garfinkel 1995 includes a summary which states that the authors investigated the effects of a 2 mg controlled release (“CR”) formulation of melatonin on sleep quality in 12 elderly subjects who were receiving various medications for chronic illnesses and who complained of insomnia. The subjects were suffering from a variety of medical conditions including heart disease, Parkinson’s disease and diabetes. All subjects also had documented melatonin deficiency.
435 The subjects’ “[s]leep quality was objectively monitored by wrist actigraphy”. The sleep variables measured were sleep efficiency, sleep latency, total sleep time (i.e. time spent asleep after sleep onset) and WASO (i.e. accumulated time awake after sleep onset). Garfinkel 1995 states:
Melatonin deficiency may have an important role in the high frequency of insomnia among elderly people. Controlled-release melatonin replacement therapy effectively improves sleep quality in this population.
…
This study shows that despite the presence of chronic diseases and the use of drugs, controlled-release melatonin has an overall beneficial effect on sleep quality in melatonin-deficient elderly people. The therapeutic effects of melatonin on circadian-based sleep disorders in blind people, travellers with jet-lag, and patients with delayed-sleep-phase syndrome are well established. In people with chronic insomnia and in healthy adults with artificially induced insomnia, however, melatonin in doses of 1-75 mg given for up to a week failed to show consistent hypnotic effects, though there was some improvement of sleep.
Before treatment the sleep variables in our 12 subjects were similar to those previously reported for insomniac elderly people. These findings objectively confirmed our subjects' complaints of poor sleep quality. After 3 weeks’ treatment with controlled-release melatonin, values for both sleep efficiency and WASO were similar to actigraphic and polysomnographic values reported for healthy elderly people without insomnia …
(Footnotes omitted)
436 In Wheatley 1 Professor Wheatley said that he considered the results described in Garfinkel 1995, “specifically the demonstrated effects in decreasing WASO (and increasing sleep efficiency as a result) and tendency to reduce sleep latency, indicate that treatment of insomnia patients with 2 mg CR melatonin was quite effective in reducing disruption to sleep, and improving sleep continuity”. He also said:
If I had read Garfinkel 1995 in connection with the Task prior to August 2001, I would have wanted to use 2 mg CR melatonin for treatment of the insomnia patient described in the Task. If the cause of the insomnia patient's day time fatigue and/or not feeling rested after sleep are the result of a disrupted pattern of sleep or of fragmented sleep, based on Garfinkel 1995 my expectation would have been that 2 mg CR melatonin would likely assist to improve sleep continuity and thereby reduce day time fatigue and/or a feeling of not being rested after sleep (i.e. I expect that this use of melatonin would help alleviate the patient's symptoms). I would also have had the expectation that 2 mg CR melatonin would be a safe treatment for the insomnia patient given my knowledge regarding melatonin safety noted above at paragraph 112 and also given that 2 mg CR melatonin was well tolerated by the elderly subjects who complained of insomnia in Garfinkel 1995.
437 The respondents’ submitted that Garfinkel 1995 would have been ascertained by the person skilled in the art because it was published in a leading journal, The Lancet, and has “sleep”, “sleep quality” and “melatonin” in the title, and was one of the 13 articles ultimately selected by Professor Wheatley. They also relied on the fact that Garfinkel 1995 was cited in a number of other publications that Professor Wheatley considered as part of his review, including Zisapel 2000.
438 In Wheatley 1, Professor Wheatley indicated that he did not regard Garfinkel 1995 as relevant after requesting and reviewing it at that time. Shortly before the trial, Professor Wheatley sought to amend Wheatley 1 to indicate that he had in fact identified both Garfinkel 1995 and another paper by MacFarlane et al as papers of interest at that time. When questioned about this amendment during cross-examination, Professor Wheatley stated that he had an “independent memory” of being interested in Garfinkel 1995, but not MacFarlane. Neurim suggested, as I understood its submission, that the change in Professor Wheatley’s evidence was indicative of Professor Wheatley having been led to Garfinkel 1995 by HSF.
439 I have no doubt that a person skilled in the art would have ascertained and understood Garfinkel 1995. I do not accept that Professor Wheatley was led to it. The title of the article and the well-known journal in which it appears are proof enough that the article was reasonably ascertainable to a person skilled in the art looking for information relating to the use of melatonin in the treatment of primary insomnia. As to the relevance of Garfinkel 1995 to the problem addressed by the invention, the respondents submitted that it was not only relevant, but that:
The invention is obvious in the light of Garfinkel 1995. Taking Garfinkel 1995 as a starting point, there is “no barrier crossed” to arrive at the invention in the context of the Task. Further and alternatively, it would lead a skilled reader to try PR [prolonged release] melatonin within the claimed dose range to treat primary insomnia (however characterized) with an expectation that it would (or may well) improve the quality of the patient’s sleep (however measured).
440 Much of what I have said in relation to Haimov 1995 applies to Garfinkel 1995. It does not suggest melatonin would make a suitable treatment for primary insomnia characterised by non-restorative sleep. Improvements in quality of sleep investigated in Garfinkel 1995 were assessed using objective measures of time spent asleep or awake either before or after sleep onset. In addition, the subjects in Garfinkel 1995 were suffering from a variety of chronic diseases. While some of these conditions may not cause insomnia, it is clear that some (e.g. Parkinson’s disease) would contribute to a patient’s sleep disturbance. Moreover, all of the subjects were suffering from a melatonin deficiency. The focus of the discussion in the article is on the use of melatonin to treat “melatonin-deficiency-related insomnia”, i.e. as a “replacement” therapy.
441 I find that a person skilled in the art would have considered Garfinkel 1995 as relevant in that it provides potentially useful information concerning the safety of a 2 mg controlled release formulation of melatonin. I am not persuaded that a person skilled in the art would have considered Garfinkel 1995 as relevant to the treatment of primary insomnia characterised by non-restorative sleep. There is in my opinion no information disclosed in Garfinkel 1995 which would, if considered together with the common general knowledge as it stood at the priority date, directly lead a person skilled in the art to try melatonin as a treatment for primary insomnia characterised by non-restorative sleep.
442 Zisapel 2000 is a review article which discusses the potential use of prolonged release melatonin in the treatment of insomnia particularly in elderly patients. The article was published in the journal Drug Development Research which is not one that Professor Wheatley read or that Professor Roth read routinely at the priority date. Zisapel 2000 was only identified through Mr Jennings’ literature search. However, while the evidence suggests that the journal was a “low impact” publication, there is nothing in the evidence which would lead me to conclude that it was obscure or that a clinician seeking information in relation to the use melatonin for the treatment of primary insomnia would be unlikely to access it.
443 It is useful to refer to the abstract to Zisapel 2000:
Melatonin, a hormone produced by the pineal gland at night, influences circadian rhythms, most notably the sleep–wake cycle. Much scientific evidence indicates that melatonin has sleep-enhancing properties. Sleep after melatonin administration is more similar to that recorded during normally occurring sleep than after administration of currently available hypnotic agents. Impairment in melatonin production may contribute to the well-known increased incidence of insomnia in the aged. In addition, some medications may impair sleep by inhibiting or distorting the melatonin rhythm. Insomnia associated with diminished nocturnal melatonin secretion may benefit from melatonin replacement therapy. Melatonin is rapidly eliminated from the body. Hence, to maintain effective serum concentrations of melatonin throughout the night, a prolonged-release (PR) formulation of melatonin (Circadin™) has been developed which provides a melatonin profile that simulates the normal nocturnal increase in melatonin concentrations. The sleep-inducing effects of PR-melatonin, at a dosage strength of 2 mg, have been demonstrated in exploratory studies in elderly insomnia patients and patients with depression or schizophrenia and sleep complaints. In the USA melatonin is available without any medical indication as a nutritional supplement. Animal toxicological studies and clinical experience has not revealed any consistent pattern of adverse events or laboratory test value alterations associated with the administration of the PR-melatonin. Clinical trials in a large population of elderly insomniacs have been set up to provide the regulatory bodies with the required evidence on the safety and efficacy of PR-melatonin.
444 There are a couple of points to note in relation to Zisapel 2000. The article is concerned with insomnia generally and not primary insomnia specifically. In the introduction insomnia is defined by the author as “the subjective complaint of insufficient or inadequate sleep [that] is characterized by difficulty in initiating and/or maintaining sleep (increased nocturnal awakenings and sleep fragmentation)”. This definition of insomnia makes no reference to non-restorative or unrefreshing sleep. The discussion of melatonin therapy that follows is solely concerned with the effects of melatonin on sleep initiation and maintenance. The author refers to the influence of melatonin on the sleep-wake cycle and its sleep-enhancing properties. The author also observes that “there is a medical need for a safe and efficacious alternative treatment for chronic insomnia, particularly for older patients”. Referring to the need for such treatment, the article concludes that the safety of Neurim’s prolonged release formulation of melatonin has been established especially in older persons who, in addition to poor sleep quality, have other health problems which require drug treatment.
445 I find that a person skilled in the art would have considered Zisapel 2000 as providing information relevant to the safety of a 2 mg prolonged release dose of melatonin. However, as with Haimov 1995, I am not persuaded that a person skilled in the art would have considered Zisapel 2000 as relevant to a treatment for primary insomnia characterised by non-restorative sleep.
446 This article, entitled “Facilitation of Benzodiazepine Discontinuation by Melatonin”, was published in November 1999 in the Archives of Internal Medicine. The authors include Dr Garfinkel and Dr Zisapel. As previously mentioned, Garfinkel 1999 is not relied on by the respondents except in combination with other s 7(3) documents.
447 The study reported in Garfinkel 1999 included 34 subjects receiving benzodiazepine therapy as long term treatment for insomnia. They were randomised to either the treatment arm or the placebo arm; those in the treatment arm received 2 mg of melatonin in a controlled release formulation (“CRM”).
448 There were two periods of study. In period 1, patients received the CRM or placebo for six weeks. They were encouraged to reduce their benzodiazepine dosage in weeks two, three and four and to discontinue it completely during weeks five and six. In period 2, CRM was administered for another six weeks to 30 subjects (after four dropped out). Those who had not discontinued benzodiazepine therapy in period 1 were over the next six weeks again encouraged to reduce and then stop.
449 Benzodiazepine consumption and subjective sleep quality scores were reported daily by all subjects using a simple questionnaire every morning. Sleep quality scores were reported using a numerical rating (1-10). Subjects were allowed to continue melatonin therapy after the end of period 2 and reassessed six months later.
450 Various results were reported including for the six month follow up which showed that of the 24 patients who discontinued benzodiazepine therapy and received melatonin therapy, 19 maintained good sleep quality. The conclusion drawn by the authors was that controlled release melatonin may effectively facilitate discontinuation of benzodiazepine therapy while maintaining good sleep quality. The authors also reported that overall safety and tolerability were good and that no subjects withdrew from the study due to adverse effects.
451 In Wheatley 1, Professor Wheatley said:
210. If I had read Garfinkel 1999 in connection with the Task prior to August 2001, I would have considered it supportive of my knowledge that melatonin has a hypnotic effect and therefore could be useful in the treatment of insomnia; further, that a dose of 2 mg CR melatonin would be likely to have this effect. Although the results in Garfinkel 1999 do not provide data on the sleep quality experienced by patients taking melatonin in the absence of benzodiazepine use, the results support the conclusion that CR melatonin at a dose of 2 mg assists insomnia patients with the discontinuation of long-term benzodiazepine therapy with no deterioration of subjectively assessed sleep quality. I would therefore want to try 2 mg CR melatonin for treatment of the insomnia patient described in the Task with the expectation that use of a 2 mg dose of CR melatonin would improve the quality of their sleep by having some degree of hypnotic effect. This hypnotic effect may lead to an improvement in sleep efficiency and a reduction in the time taken to fall asleep. This would like likely [sic] result in the patient feeling more rested and less fatigued.
211. Given the absence of any reported safety issues in Garfinkel 1999, and my knowledge that much higher doses were available OTC in the United States and had not caused any serious adverse events that I was aware of, I would have considered using a dose up to 4 mg if necessary. I would have first observed the effect of 2 mg in the individual patient before increasing the dose up to 4 mg if necessary.
452 It is apparent from the passage of evidence extracted above that, despite considering Garfinkel 1999 to be supportive of his view that melatonin had a hypnotic effect and therefore could be used in the treatment of insomnia, Professor Wheatley did not understand Garfinkel 1999 to suggest that melatonin may improve the restorative quality of patients’ sleep.
Combination of s 7(3) documents
453 Each of the combinations relied on by the respondents includes Zisapel. The respondents submitted:
280. Professor Roth’s evidence in the concurrent session makes it clear that a skilled reader interested in the use of melatonin reading Zisapel 2000 and wishing to understand what was being discussed in Haimov 1995, Garfinkel 1995, or any other paper in the document, would go and read that document. Garfinkel 1995, Haimov 1995, Garfinkel 1999 and Zisapel all appear to be from the same research group, and this group was engaged in continuous pursuit of a research program relating to use of melatonin in insomnia.
281. As Professor Glozier observed in JER2, Zisapel 2000 describes what seems to be a drug development program by reference to the findings of the previous studies. The continuity of the research program told him it was having success.
(Citations omitted)
454 Professor Wheatley asserted in his affidavit that if he had read each of Garfinkel 1995, Haimov 1995, Garfinkel 1999 and Zisapel 2000 in connection with the Task prior to August 2001, then he would have combined the information in them. He would do so, as I understood his evidence, because each of those documents contains information that would be useful to him in identifying a dose or dosage range of melatonin suitable to the Task and because they appear to be from the same research group. He said in Wheatley 1:
If I had read Garfinkel 1995, Haimov 1995, Garfinkel 1999 and Zisapel [2000], I would have considered that together these papers provided strong support for the use of a dose of 2 mg PR melatonin in the treatment of the insomnia patient noted in the Task. I would therefore have started treatment with a 2 mg dose of PR melatonin in the expectation that such a dose would be likely to improve the symptoms of the insomnia patient described in the Task. Given the absence of any reported safety issues I would have considered using a dose up to 4 mg if necessary. If the treatment at a 2 mg dose successfully treated a patient's insomnia, that is their symptoms of day time fatigue and/or not feeling rested after sleep had resolved, I would consider the possibility of titrating the dose of PR melatonin down to a 1 mg PR dose of melatonin.
455 There is detailed reference made to Haimov 1995, Garfinkel 1995 and Garfinkel 1999 in Zisapel 2000. Haimov 1995 and Garfinkel 1995 are discussed under the heading “Efficacy of PR-Melatonin in Insomnia” while Garfinkel 1999 is discussed under the heading “PR-Melatonin use with Benzodiazepines”. All are said to have involved the study of Neurim’s 2 mg prolonged release melatonin on insomniacs, and all are relied on to support the following conclusion to Zisapel 2000:
In response to the clinical need for a safe and efficacious alternative treatment for insomnia, Neurim Pharmaceuticals began preclinical toxicology and clinical program with the PM formulation of melatonin. This program systematically and rigorously addressed the toxicology, safety, and efficacy issues of melatonin therapy for insomnia. The studies were designed to provide regulatory authorities with sufficient information to demonstrate the efficacy of the product at the recommended doses, timing, and duration of melatonin use. In addition, the safety of the product has been established, especially in older persons who, in addition to poor sleep quality, quite often have additional health problems which require drug treatment.
456 It would be readily apparent to the persons skilled in the art that they could obtain more detailed information concerning the clinical program referred to in Zisapel 2000 by consulting Haimov 1995, Garfinkel 1995 and Garfinkel 1999. I accept that a person skilled in the art who had ascertained Zisapel 2000, Haimov 1995, Garfinkel 1995 and Garfinkel 1999 and was interested in obtaining more information concerning the safety and efficacy of melatonin as a potential treatment for insomnia could reasonably be expected to combine the information in these four documents on the basis that they all concern trials of a 2 mg prolonged release melatonin formulation conducted by the same research group which are said to have established that the formulation was safe for use in patients requiring treatment.
457 I also accept that those documents would when taken together provide strong support for the view that a 2 mg prolonged release melatonin formulation would be safe to use as a treatment for insomnia at least in the short term. However, even when read in combination, Zisapel 2000, Haimov 1995, Garfinkel 1995 and Garfinkel 1999 do not suggest that melatonin may improve the restorative quality of a patient’s sleep. As previously explained, the focus of Haimov 1995 and Garfinkel 1995 is on the use of melatonin to initiate or maintain sleep while the focus of Garfinkel 1999 is on the use of melatonin to facilitate the discontinuation of benzodiazepine therapy in patients with insomnia. None of those publications when read together with Zisapel 2000 would suggest to the person skilled in the art that melatonin may be useful in treating primary insomnia characterised by non-restorative sleep.
458 What was known about the mechanism of action of melatonin at the priority date suggested that due to either its effect on circadian rhythms and the sleep-wake cycle, or its potential hypnotic effect, melatonin may assist a patient suffering from insomnia to initiate or maintain sleep. Assuming that the person skilled in the art would have considered melatonin as worth trying as a treatment for primary insomnia in the case of patients who experienced difficulty initiating or maintaining sleep, and also assuming that they would have done so in the expectation that it may well provide a useful treatment for such patients (both of which assumptions I consider justified on the evidence), I do not think the person skilled in the art would have reason to think that the treatment would (or may well) improve the restorative quality of a patient’s sleep. While the common general knowledge and the individual or combined s 7(3) documents considered together suggest that melatonin may assist patients who experience difficulty initiating or maintaining sleep, they do not offer any support or encouragement for the view that the restorative quality of the patient’s sleep may be improved.
459 In the result, I do not consider that any of the s 7(3) documents considered alone or in any of the combinations relied on by the respondents together with the common general knowledge as it stood at the priority date would have directly led the hypothetical non-inventive person skilled in the art to try melatonin in the expectation that it may well provide a useful treatment for primary insomnia characterised by non-restorative sleep. I am not persuaded that the invention of the claims does not involve an inventive step.
460 Neurim referred extensively in its submissions to the paper by Hughes et al published in Sleep in 1998 (“Hughes 1998”) which is cited in a footnote to Chapter 31 of Sleep Medicine. Hughes 1998 includes a discussion of Garfinkel 1995 and Haimov 1995. Ultimately, it was submitted by Neurim that in light of Hughes 1998 and the authors’ criticisms of those studies, the skilled addressee would not have been motivated to pursue melatonin as a treatment for insomnia generally, including primary insomnia characterised by non-restorative sleep.
461 I do not think Hughes 1998 can be relied on for that purpose in circumstances where it is not shown to be common general knowledge. The relevant enquiry contemplated by s 7(2) of the Act as it stood at the relevant time is whether a piece of prior art information, or pieces of prior art information which the skilled addressee could be reasonably expected to have combined, ascertained pursuant to s 7(3), would render the invention obvious to the skilled addressee in light of the common general knowledge: see AstraZeneca HCA at [113] per Gageler and Keane JJ. Such an enquiry does not make allowance for the use of Hughes 1998.
462 Hughes 1998 was also relied on by Neurim as providing support for Professor Roth’s evidence as to the common general knowledge and the statement in the Consensus Statement relied on by Neurim, that “[t]here appears to be no point in addressing sleep disorders of unknown origin with melatonin treatment”. However, there is nothing in Hughes 1998 which would lead me to modify or qualify my previous findings as to the common general knowledge.
463 For completeness I should add that if I am mistaken about the application of the changes made to s 7(3) by the 2001 Amendment Act, then I would agree with Neurim that none of the combinations of documents relied on by the respondents could be justified given the terms of s 7(3) as it stood before its amendment. In my opinion, there is no evidence which could support a finding that the person skilled in the art could reasonably be expected to have treated any one or more of the s 7(3) documents as “a single source of information”: cf. Bristol-Myers Squibb Company v Apotex Pty Ltd (No 5) (2013) 104 IPR 23 at [281], Orion Corporation v Actavis Pty Ltd [2015] FCA 909 at [227]. In this case the s 7(3) documents appeared in different journals over a period of some five years. The fact that the earlier publications are all discussed in Zisapel 2000 and that they appear to be the work of the same research group is insufficient to meet the more stringent test.
464 The respondents alleged that each of the claims is invalid for lack of fair basis. The test to be applied for the purpose of determining whether a claim is fairly based on the matter described in the specification as required by s 40(3) of the Act (as it stood at the relevant time) requires that the specification contain “a real and reasonably clear disclosure” of what is claimed: Lockwood Security Products Pty Limited v Doric Products Pty Limited (2004) 217 CLR 274 (“Lockwood (No 1)”) at [68]-[69]. In support of their submission that the claims were invalid for lack of fair basis, the respondents placed particular reliance on the High Court’s analysis in Lockwood (No 1) of the decision in Atlantis Corporation Pty Ltd v Schindler (1997) 39 IPR 29. The High Court said at [87]:
Finally, it is necessary to consider the trial judge’s citation of Atlantis Corporation Pty Ltd v Schindler for the proposition that to couch a claim “in the same terms as the description of the invention in the specification” did not of itself, by that mere “coincidence of language”, establish fair basing. That proposition is correct, but it is not fatal to the Patentee’s position in this case. A “coincidence of language” between a claim and part of the body of a specification does not establish fair basing if that part of the language of the specification does not reflect the description of the invention in the light of the specification as a whole. In the Atlantis Case, the specification, read as a whole, described an apparatus limited to a particular use as a sub-soil drainage system. The claims, however, were “pure apparatus” claims without that limitation on use. The Full Court of the Federal Court of Australia refused to construe them narrowly so as to conform with the description in the specification. A statement in the specification of a description of the invention in similar language to the first claim was not treated as the description of the invention. While the Full Court did not engage in close textual analysis, it did distinctly hold that the statement in the specification:
“should not be allowed to disguise the fact that the invention disclosed in the body of the specification is truly ‘a sub-soil drainage method based on a particular apparatus’ or ‘a particular apparatus in its application to sub-soil drainage’. The claims, however, are ‘pure apparatus claims’. They are not subject to any limitation as to use. They travel beyond, and are not fairly based on, the matter described in the specification.”
In short, the case is distinguishable. Here, the Patentee does not rely on mere “coincidence of language”: it contends that the language used, unlike that employed in the Atlantis Case, does describe the invention.
(Footnotes omitted)
465 The High Court also said at [99]:
... the correct position is that a claim based on what has been cast in the form of a consistory clause is not fairly based if other parts of the matter in the specification show that the invention is narrower than that consistory clause. The inquiry is into what the body of the specification read as a whole discloses as the invention [Welch Perrin & Co Pty Ltd v Worrel (1961) 106 CLR 588 at 612–613]. An assertion by the inventor in a consistory clause of that of which the invention consists does not compel the conclusion by the court that the claims are fairly based nor is the assertion determinative of the identity of the invention. The consistory clause is to be considered by the court with the rest of the specification.
466 The respondents’ lack of fair basis case was based on what was said by the respondents to be the different effects of the invention as claimed in patients below the age of 55 from those in patients above the age of 55, in circumstances where the claims are not qualified by reference to the age of the patients to be treated. As developed by Mr Murray SC in his oral submissions, the respondents’ point is that “[a]s a matter of disclosure, this [P]atent is telling you it is directed towards over 55s” and what is disclosed is an invention for treatment of that cohort.
467 I do not accept the respondents’ submission. The basis for the submission rests solely on the observation that in Example 3 of the Patent, the increase in perceived quality of sleep and daytime alertness in those aged less than 55 given melatonin was less than the increase reported for those given the placebo. However, there are a number of explicit disclosures in the Patent, which make it clear that the invention is not limited to the treatment of patients aged 55 or over. In particular, the section of the Patent entitled “Field of the Invention” describes the invention as relating to the treatment of primary insomnia as defined in the DSM-IV, or nonorganic insomnia as defined by ICD-10, when characterised by non-restorative sleep. There is no suggestion that only patients of certain ages suffer from primary insomnia, or that only certain patients would benefit from the method of treatment of the invention depending on their age. There are also the two consistory clauses using language commensurate with that of the claims. Similarly, the sections of the Patent entitled “Detailed Description of the Invention” contains a description of various preferred embodiments. There is nothing contained in that section of the Patent to suggest that only patients suffering from primary insomnia aged 55 and over would benefit from the invention. The consistory clauses are consistent with the other disclosures in the Patent and, when read with those other disclosures, provide fair basis for the claims.
468 In my opinion there is a real and reasonably clear disclosure in the body of the specification of the invention as claimed that is not limited to a method of treatment for use in patients aged 55 or over.
469 There were objections taken by the parties to evidence which was admitted provisionally. The most important evidence in this category was the affidavit evidence of Professor Wheatley and Professor Roth. For reasons previously explained, I consider that Professor Wheatley is a person skilled in the art, qualified to give admissible evidence as to the state of the art at the priority date. Similarly, for reasons previously explained, I am of the view that Professor Roth is also a person skilled in the art. Evidence given by them that was received provisionally has been admitted, subject to specific rulings referred to below.
470 Neurim raised numerous objections to documents first published after the priority date which it contended were not relevant to construction of the Patent. The first of these objections relates to the second sentence of para 103 in Wheatley 3. I agree with Neurim that the Circadin AusPAR document is not relevant to the proper construction of the Patent and the prior art. I reject that part of para 103 in Wheatley 3.
471 Various other objections of this kind were raised by Neurim in relation to Glozier 2. My rulings in relation to these objections are set out in Annexure A to these reasons.
472 There were also many objections taken by the respondents to particular parts of Professor Roth’s affidavits. His affidavits were prolix and often argumentative and speculative. With regard to those parts of Roth 1 which were admitted provisionally, I reject those parts of paras 111, 119 (but only the last sentence), 402, 575, 578, 591, 602, 613 and 617. As to those parts of Roth 2 that were admitted provisionally, I reject those parts of paras 32, 37-39, 44, 46-50, 56-57, 62, 115, 183, 188, 193 and 257. The other parts of the paragraphs that were objected to and admitted provisionally which I have not rejected are in my opinion admissible as evidence of Professor Roth’s opinion.
473 Of course, the fact that Professor Roth’s opinions are admitted into evidence says nothing about the weight which is to be given to them. In that regard, much of what Professor Roth has said in his affidavit evidence that was the subject of objection concerns the “Person Skilled in the Art”. In circumstances where I have held that Professor Wheatley and other sleep medicine physicians with a similar background and experience in the diagnosis and treatment of insomnia (including primary insomnia) are skilled addressees, it will be apparent that I have given little weight to Professor Roth’s evidence concerning the identity of the person skilled in the art and his assertion that they must be familiar with DSM-IV.
474 I find that claims 4-7 of the Patent were infringed by the respondents by the supply of Melotin (s 117(2)(b)) and by authorisation of medical practitioners prescribing it as a treatment for primary insomnia characterised by non-restorative sleep in patients aged 55 and over (s 13). I also find that each of the respondents is jointly liable for infringement of those claims on the basis that they were at all relevant times acting in concert and pursuant to a common design to supply Melotin in Australia. I am not persuaded that any claim of the Patent is invalid.
475 It is not necessary to express any view as to whether it would have been appropriate to grant an injunction (and, if so, in what terms) had the Patent not expired. However, given my findings about the extent to which the respondents’ products are likely to be used for non-infringing purposes and the relative infrequency with which melatonin is prescribed by medical practitioners as a treatment for primary insomnia characterised by non-restorative sleep, it seems to me that this was not a case in which it would have been appropriate to grant an injunction in general terms restraining the respondents from supplying their products. In this regard, the reasoning of the Full Court in AstraZeneca FFC at [444] would be directly applicable.
476 So far as other relief is concerned, Neurim is entitled to declaratory relief in appropriate terms and an inquiry in relation to pecuniary relief in respect of all infringing sales of Melotin and any other Generic Partners Products or Apotex Products supplied by the respondents during the term of the Patent. While Neurim has asserted an entitlement to both an award of compensatory and additional damages, my understanding is that it has not yet made an election between damages and an account of profits.
477 The parties will be given an opportunity to submit agreed minutes of order including declaratory relief in appropriate terms, an order dismissing the cross-claim, and procedural orders relating to the determination of Neurim’s claim to pecuniary relief.
478 Given that Neurim has established that the Patent was valid and infringed by each of the respondents, costs should in my opinion follow the event. The respondents should pay Neurim’s costs of the proceeding including the cross-claim but excluding the costs previously awarded to the respondents, and the costs reserved on 11 December 2020. Who should pay the costs reserved on 11 December 2020 can be determined at the same time as Neurim’s claim for pecuniary relief is determined.
I certify that the preceding four hundred and seventy-eight (478) numbered paragraphs are a true copy of the Reasons for Judgment of the Honourable Justice Nicholas. |
Associate: