FEDERAL COURT OF AUSTRALIA
Australian Competition and Consumer Commission v ACN 117 372 915 Pty Limited (in liq) (formerly Advanced Medical Institute Pty Limited)
[2015] FCA 368
IN THE FEDERAL COURT OF AUSTRALIA | |
DATE OF ORDER: | |
WHERE MADE: |
THE COURT DECLARES THAT:
1 Each of the first and second respondents (together, AMI) during the period 2008 to 2010, in connection with the supply and possible supply of medications (AMI medications) and medical services for the treatment of male sexual dysfunction (together, the AMI treatments), engaged in conduct that was unconscionable in contravention of s 51AB of the Trade Practices Act 1974 (Cth) (TPA) in the circumstances set out below:
(a) AMI promoted its business as the “Advanced Medical Institute” and advertised extensively across the media, including television, radio, newspapers and billboards, with such advertisements containing statements encouraging men suffering from male sexual dysfunction to “call the doctors at Advanced Medical Institute” and thereby represented to men seeking treatment for male sexual dysfunction (patients) that they would receive a proper and objective medical assessment of their condition by a qualified medical doctor and would only be prescribed medication if consistent with that assessment;
(b) on contacting AMI, patients were offered the opportunity to be medically assessed in either a telephone consultation or a consultation at one of AMI’s clinics, and:
(i) patients who chose a telephone consultation spoke initially with a salesperson who described themselves as a “Clinical Coordinator”, “Medical Coordinator” or “Administrative Assistant” (Clinical Coordinator), then spoke to an AMI doctor, and then spoke to the Clinical Coordinator again;
(ii) patients who chose an in-clinic consultation met initially with a nurse at the clinic, then spoke to an AMI doctor by telephone, and then met with a Clinical Coordinator;
(c) the AMI doctors:
(i) in consultations with each of the patients identified in Annexure B to the Further Amended Statement of Claim (Annexure B patients):
(A) did not offer or prescribe any medication other than the AMI medications, which the AMI doctors had not selected from the range of all medications available for prescription by Australian medical practitioners, and did not inform the patient that they prescribed only the AMI medications;
(B) conducted a consultation by telephone only and did not see or conduct any physical examination of the patient;
(C) recommended to the patient treatment plans, including plans of a length of 12 or 18 months; and
(D) did not seek to diagnose whether it would have been medically appropriate to refer the patient to a specialist or other medical practitioner for treatment or diagnosis; and
(ii) in consultations with 150 of the Annexure B patients, did not seek to diagnose any underlying cause for the presenting problem and only questioned the patient to ascertain whether the AMI medications were contraindicated;
(iii) in consultations with most of the Annexure B patients, did not inform the patient about the common side-effects of the medications prescribed adequately or at all;
(d) the Clinical Coordinators:
(i) were salespeople who were not medically trained and were paid by AMI on a commission, calculated by reference to the cost of the treatment plans sold to patients (the longer the contract period, the greater the commission) but described themselves as “Clinical Coordinators”, “Medical Coordinators” or “Administrative Assistants”;
(ii) in conversations with:
(A) each of the Annexure B patients, did not disclose to the patient that they were salespeople paid on a commission;
(B) most of the Annexure B patients, made statements to the patient concerning the efficacy of the AMI treatments;
(C) most of the Annexure B patients, made statements to the patient that he needed treatment or would suffer adverse medical and social consequences if he did not get treatment, including that his penis may shrink or he may become impotent; and
(D) most of the Annexure B patients, represented to the patient that he would be entitled to a refund of money paid if the AMI treatment purchased was ineffective, and did not disclose the conditions on which a refund would be offered under AMI’s “satisfaction guarantee”;
(e) AMI sold the AMI treatments to patients pursuant to contracts under which:
(i) patients were bound to pay for the AMI treatments for a set period of time, whether or not the patients wished to continue with the AMI treatments, with payment either made upfront or by way of instalments;
(ii) if the AMI treatments did not successfully treat the patient’s condition or the patient experienced adverse side effects, then pursuant to the terms of its “satisfaction guarantee” AMI refused to give the patient a refund or to cancel the contract unless the patient tried at least one option from each of the available delivery mechanisms for which the patient was not contraindicated (including injections into the base of the penis), after which AMI would deduct the cost of the medication supplied and a 15% administration fee from any refund given; and
(iii) patients who had telephone consultations were only provided with a copy of the terms of the “satisfaction guarantee” after they had already agreed to purchase the AMI treatments; and
(f) AMI knew that:
(i) male sexual dysfunction is perceived by patients as embarrassing or humiliating; and
(ii) patients would have trust in the AMI doctors and would expect that those doctors would act in the patients’ best interests consistent with a doctor and patient relationship.
2 The third respondent:
(a) aided and abetted, counselled or procured; and
(b) was directly or indirectly knowingly concerned in, and party to,
the contraventions by AMI of s 51AB of the TPA referred to in paragraph 1 of this order by reason that he:
(c) was a director of each of the first and second respondents;
(d) was the Chief Executive Officer of the first and second respondents;
(e) had overall responsibility for the management of AMI;
(f) made all critical decisions concerning the business practices of AMI; and
(g) oversaw the business practices of AMI.
3 The fourth respondent was knowingly concerned in, party to, and aided and abetted, counselled and procured the contraventions by AMI of s 51AB of the TPA, during the period 2008 to 2010, in the course of or in relation to his consultation with AMI patients, by:
(a) prescribing the AMI medications which he had not selected from the range of all medications available for prescription by Australian medical practitioners;
(b) not disclosing to patients that he was required by AMI to recommend only the AMI treatments and to prescribe only the AMI medications; and
(c) not seeing or conducting any physical examinations of all patients to whom he recommended the AMI treatments or prescribed the AMI medications.
4 Each of the sixth and seventh respondents (together, NRM) in 2011 and 2012, in connection with the supply and possible supply of medications (NRM medications) and medical services for the treatment of male sexual dysfunction (together, the NRM treatments), engaged in conduct that was unconscionable in contravention of s 21 of the Australian Consumer Law (ACL), in the following circumstances:
(a) NRM promoted its business as the “Advanced Medical Institute” and advertised across the media, including radio, newspapers and billboards, with such advertisements containing statements encouraging men suffering from male sexual dysfunction to “call the doctors at Advanced Medical Institute” and thereby represented to patients that they would receive a proper medical assessment of their condition by a qualified medical doctor and would only be prescribed medication if consistent with that assessment;
(b) on contacting NRM, patients were offered the opportunity to be medically assessed in either a telephone consultation or a consultation at one of NRM’s clinics, and:
(i) patients who chose a telephone consultation spoke initially with a salesperson who described themselves as an “Administrative Assistant”, then spoke to an NRM doctor, and then spoke to the Administrative Assistant again;
(ii) patients who chose an in-clinic consultation met initially with a nurse at the clinic, then spoke to an NRM doctor by telephone, and then met with an Administrative Assistant;
(c) the NRM doctors:
(i) in consultations with each of the patients identified in Annexure C to the Further Amended Statement of Claim (Annexure C patients):
(A) did not offer or prescribe any medication other than the NRM medications, which the NRM doctors had not selected from the range of all medications available for prescription by Australian medical practitioners, and did not inform the patient that they prescribed only the NRM medications;
(B) only conducted the consultation by telephone;
(C) recommended to the patient treatment plans, including plans of a length of 12 or 18 months;
(D) did not seek to diagnose any underlying cause for the presenting problem but only questioned the patient to ascertain whether the NRM medications were contraindicated; and
(E) did not adequately diagnose whether it would have been medically appropriate to refer the patient to a specialist or other medical practitioner for treatment or diagnosis; and
(ii) in consultations with 14 of the Annexure C patients, did not adequately inform the patient about the common side-effects of the medications prescribed;
(d) the Administrative Assistants:
(i) were salespeople who were not medically trained and were paid on commission by NRM, calculated by reference to the cost of the treatment plans sold to patients (the longer the contract period, the greater the commission), but described themselves as “Administrative Assistants” thereby representing that they were acting impartially in relation to the patients’ medical interests in selling the NRM treatments;
(ii) in conversations with:
(A) each of the Annexure C patients, did not disclose to the patient that they were in fact salespeople paid on a commission; and
(B) six of the Annexure C patients, made statements to the patient concerning the efficacy of the NRM treatments, the effect of which was to apply pressure to the patient to purchase the NRM treatments;
(e) NRM sold the NRM treatments to patients pursuant to contracts which bound patients to pay for treatment for a set period of time, including terms ranging from 12 to 18 months, whether or not the patients wished to continue with the treatment, with payment either made upfront or by way of instalments;
(f) The contracts which NRM entered into with patients between June 2011 and February 2012 contained a term (the refund term) which provided that, on giving notice of termination of their contract to NRM, patients were only entitled to receive a refund after NRM had deducted the following amounts:
(A) an “administrative fee” of 15 per cent of the entire initial cost of the contract, regardless of when the contract was cancelled;
(B) a pro-rated amount representing the “expired” period of the program prior to receipt of written notice (regardless of whether the patient used NRM’s services or medications during that period);
(C) a pro-rated amount representing the next 30 days of the program after receipt of written notice (regardless of whether the patient used NRM’s services or medications during that period); and
(D) the cost of any medication already provided to or prepared for the patient, at a price not specified in the contract but determined by NRM; and
the terms of the contract were played over the telephone to patients by the Administrative Assistants or provided to patients in NRM’s clinics; and
(g) NRM knew that:
(i) male sexual dysfunction is perceived by patients as embarrassing or humiliating; and
(ii) patients would have trust in the NRM doctors and would expect that those doctors would act in the patient’s best interests consistent with a doctor and patient relationship.
5 The third respondent:
(a) aided and abetted, counselled or procured; and
(b) was directly or indirectly knowingly concerned in, and party to,
the contraventions by NRM of s 21 of the ACL referred to in paragraph 3 of this order by reason that he:
(c) was a director of each of the sixth and seventh respondents;
(d) was the Chief Executive Officer of the sixth and seventh respondents;
(e) had overall responsibility for the management of the NRM business;
(f) made or approved all critical decisions concerning the business practices of NRM; and
(g) oversaw the business practices of NRM.
6 The refund term contained in the consumer contracts between NRM and its patients made during the NRM period, which provided that:
“Termination. Sexual dysfunction is a chronic condition and treatment can take some time. For this reason we stipulate that your contract with us for [sic] the period decided in the first consultation with the AMI doctor. You may cancel your treatment program with AMI at any time by giving AMI not less than 30 days notice. Cancelling your treatment program you will be entitled to a refund for the unexpired period of your treatment program less an administration fee of 15% and less the cost of any medication already provided to or prepared for you. No refund will be provided for the expired period of the treatment program or the 30 day notice period. All cancellation must be communicated to AMI in writing signed by you. Oral cancellation will not be accepted in any circumstances.”
was an unfair term within the meaning of sections 24 and 250 of the ACL because:
(a) the imposition of the administration fee was not reasonably necessary to protect NRM’s legitimate interests;
(b) the imposition of a charge for a pro-rated amount representing the expired portion of the treatment regardless of the quantity or effectiveness of the goods or services supplied by NRM to the patient during this period was not reasonably necessary to protect NRM’s legitimate interests;
(c) the imposition of a charge for a pro-rated amount for the additional thirty-day notice period regardless of whether the patient desired to continue receiving goods or services for this period and whether any goods or services provided by NRM were effective was not reasonably necessary to protect NRM’s legitimate interests;
(d) the imposition of a charge for an amount for the cost of any medication already provided by NRM when the method of calculation was not disclosed to the patient and regardless of the actual cost to NRM of providing the medication or whether the medication was effective was not reasonably necessary to protect NRM’s legitimate interests;
(e) the imposition of the fees referred to in sub-paragraphs (a) to (d) was not transparent when delivered in a pre-recorded telephone message; and
(f) the uncertainty and cost of terminating a contract would cause a financial and other detriment to a patient wishing to terminate,
and is void by operation of s 23 of the ACL.
THE COURT ORDERS THAT:
7 The fourth respondent be released from the undertaking given by him to the Court on 21 June 2012.
8 The fourth respondent be permanently restrained from being knowingly concerned in, party to, aiding and abetting, counselling or procuring the provision by a corporation of any medical treatment plan or medication for the treatment of male sexual dysfunction by contract which:
(a) provides for the supply or possible supply of any treatment or medication prior to the patient having been seen and physically examined by a qualified medical practitioner in relation to the medical condition for which the patient is seeking treatment;
(b) provides for the supply or possible supply for any treatment or medication which a qualified medical practitioner has not assessed as the most suitable or efficacious for the patient from the range of all appropriate medications available for prescription by Australian medical practitioners;
(c) provides for the supply or possible supply of any treatment or medication which he or another qualified medical practitioner has not discussed with the patient prior to entering into the contract;
(d) is for a period which exceeds the length of time which he or another qualified medical practitioner has determined the patient will necessarily require the treatment to entering into the contract;
(e) requires the patient to pay for treatment or medication for a period of more than two months; or
(f) provides for the supply of any treatment or medication, without prior consultation with a qualified medical practitioner who has provided information as to the efficacy, suitability, prior use and most common side effects of the treatment or medication.
9 Each of the sixth and seventh respondents be permanently restrained, whether by themselves, their servants or agents or otherwise, in trade or commerce, from:
(a) making an agreement with a patient for or in respect of the supply of medications or medical services for the treatment of male sexual dysfunction, unless the patient for whom the medications or medical services are intended has had a consultation with a duly qualified medical practitioner either in person or by video-link;
(b) making an agreement with a patient for the supply of medications or medical services for the treatment of male sexual dysfunction unless:
(i) before the agreement is made:
(A) the patient has been provided with a written statement by the sixth and seventh respondents by post, electronic mail, or in person:
a. setting out in plain English the terms of the agreement including a description of the medication or medical services to be provided, the total cost of the agreement, the proposed payment plan (if any), the period of treatment, and a statement that the patient has a right to terminate the agreement during the period of five business days commencing on the date on which the agreement is made (Cooling-Off Period);
b. stating that male sexual dysfunction may be a symptom of other medical conditions but NRM does not seek to diagnose those other medical conditions; and
c. stating that NRM does not provide general medical advice and that NRM’s doctors only consider whether the patient is suitable for NRM medications; and
(B) the sixth and seventh respondents receive from the patient a written acceptance of the terms of the agreement; and
(ii) the agreement contains terms which:
(A) give the patient a right to terminate the agreement, by notice in writing to the sixth and seventh respondents dispatched during the Cooling-Off Period; and
(B) provide that if the patient exercises the right to terminate the agreement during the Cooling-Off Period, the agreement is taken to be rescinded by mutual consent with all payments made refunded; and
(C) provide that the patient may at any time after the Cooling-Off Period terminate the agreement by giving 14 days’ notice, and that once this notice has been provided, the sixth and seventh respondents will cancel any direct debit arrangement referrable to the patient;
(c) making any statement or representation to any patient or prospective patient as to:
(i) the efficacy of NRM treatments;
(ii) the efficacy of any medications or medical services offered by parties other than the sixth and seventh respondents; or
(iii) the patient’s need for the NRM treatments and any adverse consequences that might result if the patient:
(A) does not acquire the NRM treatments, or
(B) does not receive NRM treatments for male sexual dysfunction.
except if that statement is made directly to a patient or potential patient by a duly qualified medical practitioner during a consultation either in person or by video-link;
(d) making an agreement with a patient for the supply of NRM treatments, unless during pre-contractual negotiations, the patient is offered an agreement with a term of no more than two months; and
(e) accepting in advance any payment or any other consideration from a patient in connection with the supply of NRM treatments for a future period of more than two months.
10 The third respondent be restrained, for a period of seven years from the date of this order (unless otherwise specified below), in trade or commerce, from:
(a) being in any way, directly or indirectly, knowingly concerned in, or a party to, or aiding and abetting, counselling or procuring conduct of the kind restrained in order 6 above; and
(b) from having a role in connection with training, supervising, counselling or terminating employees, agents or contractors of the sixth and seventh respondents and their related bodies corporate.
11 Pursuant to s 239 of the ACL, the sixth and seventh respondents refund the total amount of money paid by the Annexure C patients, except for patients NRM 7 and NRM 9, pursuant to their contract with NRM, less any refund already provided by NRM.
12 The sixth and seventh respondents cause to be published, at their own expense, within 21 days of the date of this order, a notice in the form contained in Annexure A to this order (website notice) on its website located at http://www.amiaustralia.com.au (AMI website) and, if the URL of such website is replaced, changed or redirected to another website, on the corresponding website, for a continuous period of 90 days and use its best endeavours to ensure that:
(a) the website notice shall be viewable by clicking a “click-through” icon located on the AMI website;
(b) the “click-through” icon referred to in (a) is located at the top of the homepage of the AMI website and any corresponding websites;
(c) the “click-through” icon shall appear as follows, with the words printed prominently in bold red text, in a font size no smaller than 14-point, on a white background:
Unconscionable Conduct by Advanced Medical Institute (AMI) –
Notice Ordered by Federal Court of Australia.
Click Here
13 The third, sixth, and seventh respondents pay the applicant’s costs of the proceeding, except for the applicant’s costs of and incidental to the proceeding against the fourth and fifth respondents.
14 The applicant and the sixth and seventh respondents have liberty to apply in writing by 6 May 2015 in relation to the issues referred to in [975], [988], [989], [993], and [1026] of these reasons for judgment.
Note: Entry of orders is dealt with in Rule 39.32 of the Federal Court Rules 2011.
ANNEXURE A
CORRECTIVE NOTICE ORDERED BY FEDERAL COURT OF AUSTRALIA
UNLAWFUL CONDUCT BY ADVANCED MEDICAL INSTITUTE
Following legal action by the Australian Competition and Consumer Commission, the Federal Court of Australia has ruled that NRM Corporation Pty Ltd and NRM Trading Pty Ltd, (together, NRM), engaged in unconscionable conduct in contravention of section 21 of the Australian Consumer Law in its dealings with men seeking treatment for male sexual dysfunction in 2011 and 2012.
NRM promoted its business as the “Advanced Medical Institute”. It represented that its patients would receive a proper medical assessment of their condition by a qualified medical doctor and would only be prescribed medication if consistent with that assessment. It knew that its patients were vulnerable by virtue of their condition, and that patients would expect NRM and its doctors to act in their best interests consistent with a doctor/patient relationship. In fact, a number of NRM’s patients:
• were not physically examined by NRM’s doctors;
• were only prescribed NRM’s treatments, which were not selected from all relevant and available treatments in Australia;
• were not informed that NRM’s doctors would only prescribe treatments from NRM’s limited range of treatments, or that other treatments were available;
• were not adequately informed of the side effects of NRM’s treatments;
• were not properly diagnosed with the underlying cause of their condition, but rather were only questioned as to whether NRM’s treatments were contraindicated;
• were not referred to specialists or advised to see their general practitioner;
• were misled by NRM’s salespeople, who described themselves as “Administrative Assistants” but in fact were paid on commission;
• were told that they would receive a refund under NRM’s refund policy if the NRM treatments were ineffective, when in fact any refund was subject to significant limitations and deductions that were not adequately disclosed to the patient when they entered into the contract; and
• were sold NRM treatments pursuant to contracts which bound the patients to pay for treatment for a set period of time, including terms ranging from 12 to 18 months, whether or not the patients wished to continue with the treatment.
The Court also found that NRM’s refund policy was an unfair term within the meaning of sections 24 and 250 of the ACL, because the imposition of fees and charges deducted from any refund to a patient was not transparent, was not necessary to protect NRM’s interests and would cause financial and other detriment to patients. The consequence of this declaration is that the refund policy is void.
The Court has also found that Jack Vaisman, Chief Executive Officer of NRM, was knowingly concerned in the unlawful conduct of NRM.
The Court has ordered declarations, injunctions and the refund of money to patients. A copy of the judgment, which details the Court’s findings and orders is located at [insert URL]
NRM purchased the AMI business from Advanced Medical Institute Pty Limited and AMI Australia Holdings Pty Ltd (together, AMI) in June 2011. The Court also declared that AMI had engaged in unconscionable conduct.
This notice has been placed because of an order of the Federal Court of Australia in a proceeding commenced by the Australian Competition and Consumer Commission.
VICTORIA DISTRICT REGISTRY | |
GENERAL DIVISION | VID 1113 of 2010 |
BETWEEN: | AUSTRALIAN COMPETITION AND CONSUMER COMMISSION Applicant |
AND: | ACN 117 372 915 PTY LIMITED ACN 117 372 915 (IN LIQUIDATION) First Respondent ACN 095 238 645 PTY LIMITED ACN 095 238 645 (IN LIQUIDATION) Second Respondent JACOV VAISMAN Third Respondent BRIAN LONERGAN Fourth Respondent JAMES VANDELEUR Fifth Respondent NRM CORPORATION PTY LTD ACN 151 468 601 Sixth Respondent NRM TRADING PTY LTD ACN 151 469 493 Seventh Respondent |
JUDGE: | NORTH J |
DATE: | 22 APRIL 2015 |
PLACE: | MELBOURNE |
REASONS FOR JUDGMENT
1 On 21 December 2010, the applicant, the Australian Competition and Consumer Commission (ACCC) commenced this proceeding against five respondents.
2 The first respondent was ACN 117 372 915 Pty Limited (ACN 117 372 915) (in liquidation) and was formerly known as Advanced Medical Institute Pty Limited. The second respondent was ACN 095 238 645 Pty Limited (ACN 095 238 645) (in liquidation) and was formerly known as AMI Australia Holdings Pty Ltd. Together they are referred to as AMI in these reasons for judgment. AMI conducted a business of providing treatment to men for erectile dysfunction (ED) and premature ejaculation (PE).
3 The third respondent was Dr Jacov Vaisman, who was the sole director and Chief Executive Officer of AMI. The fourth respondent was Dr Brian Lonergan, and the fifth respondent was Dr James Vandeleur. Both were doctors engaged by AMI to treat patients with ED and PE.
4 On 22 December 2010, both of the companies constituting AMI were placed into voluntary administration.
5 On 17 June 2011, the business of AMI was sold to NRM Corporation Pty Ltd and NRM Trading Pty Ltd.
6 On 19 July 2011, both of the companies constituting AMI were placed into voluntary liquidation.
7 On 21 July 2011, the ACCC discontinued the proceeding against Dr Vandeleur in accordance with a settlement reached with him.
8 On 17 August 2011, AMI filed a submitting appearance seeking to be heard only in respect of costs.
9 On 2 September 2011, the ACCC was granted leave to proceed against AMI under s 500(2) of the Corporations Act 2001 (Cth) and to join NRM Corporation Pty Ltd and NRM Trading Pty Ltd as the sixth and seventh respondents respectively. They are together referred to as NRM in these reasons for judgment.
10 On 21 June 2012, the ACCC and Dr Lonergan made an agreement including that Dr Lonergan would take no further part in the proceeding except as a witness, that there would be no order for costs between them, and that if the Court determined to make declarations against AMI, then there would be similar agreed orders and an injunction against Dr Lonergan.
11 As the only respondents who participated in the trial were NRM and Dr Vaisman, they are together referred to in these reasons for judgment as the respondents.
12 The ACCC alleged that in the period from 2008 to 2010, which is referred to as the AMI period, AMI engaged in unconscionable conduct in contravention of s 51AB of the Trade Practices Act 1974 (Cth) (TPA).
13 The ACCC alleged that NRM continued the business of AMI and engaged in unconscionable conduct after the purchase of the business on 17 June 2011 and during 2012. At those times unconscionable conduct was prohibited by s 21 of the Australian Consumer Law (ACL), contained in Sch 2 to the Competition and Consumer Act 2010 (Cth), in almost identical terms to s 51AB of the TPA.
14 The ACCC also alleged that a term of the contract between NRM and its patients concerning termination was unfair within the meaning of s 24 and s 250 of the ACL, and consequently void under s 23(1) of the ACL.
15 The ACCC alleged that Dr Vaisman made all the critical decisions in relation to the business and aided, abetted, counselled or procured, or was knowingly concerned in or party to, the contraventions by AMI and NRM.
1.2 The relief sought by the ACCC
16 The ACCC sought declarations against AMI, NRM, and Dr Vaisman that specified conduct was unconscionable, and that the term of the NRM contract regarding termination was unfair. The ACCC sought injunctions against NRM and Dr Vaisman restraining them from engaging in further such conduct. Against NRM, the ACCC also sought the publication of corrective advertising and the refund to certain patients of monies paid under contracts with NRM. The ACCC also sought an order for costs against NRM and Dr Vaisman.
17 Although AMI entered a submitting appearance, considerable time was taken by the ACCC in establishing the conduct of AMI between 2008 and 2010. That attention was necessary because the Court needed to be satisfied by evidence that AMI had engaged in unconscionable conduct if declarations were to be made against AMI, and further, because the conduct of AMI was relevant to the establishment of the case against NRM, in that both AMI and NRM were operated by the same people and NRM was said to have continued to use the same business model previously employed by AMI.
18 The proceeding was contested on almost every issue of fact and law. The hearing occupied 33 sitting days and the record of the hearing is contained in 2,828 pages of transcript. Thirty-two witnesses were called to give evidence including patients of AMI and NRM, doctors, medical and pharmacological experts, and employees and management of AMI and NRM. The documentary evidence was provided in both electronic and hard-copy form. In hard copy, the documentary evidence occupied about 40 large lever-arch folders. The case involved a highly detailed investigation of the business practices of AMI and NRM, and of the appropriate pharmacological and medical treatment of ED and PE. In view of the large amount of material before the Court, these reasons for judgment have, for ease of reference, included in the text of the judgment the source of much of the evidence.
1.4 The organisation of these reasons
19 These reasons for judgment first set out the legal principles to be applied. Then, in separate sections, the reasons for judgment address the factual allegations against AMI, NRM, and Dr Vaisman, and make relevant fact findings. Following the fact findings, the reasons for judgment examine whether the proved facts constitute unconscionable conduct and whether those facts establish that a term of the NRM contract regarding termination was an unfair contract term. The reasons for judgment then conclude with sections relating to a pleading point raised by the respondents, the form of relief, and costs.
2. APPLICABLE LEGAL PRINCIPLES
20 The ACCC contended that the conduct of AMI was unconscionable and thereby infringed the prohibition on such conduct contained in s 51AB of the TPA, which relevantly provided as follows:
51AB Unconscionable conduct
(1) A corporation shall not, in trade or commerce, in connection with the supply or possible supply of goods or services to a person, engage in conduct that is, in all the circumstances, unconscionable.
(2) Without in any way limiting the matters to which the court may have regard for the purpose of determining whether a corporation has contravened subsection (1) in connection with the supply or possible supply of goods or services to a person (in this subsection referred to as the consumer), the court may have regard to:
(a) the relative strengths of the bargaining positions of the corporation and the consumer;
(b) whether, as a result of conduct engaged in by the corporation, the consumer was required to comply with conditions that were not reasonably necessary for the protection of the legitimate interests of the corporation;
(c) whether the consumer was able to understand any documents relating to the supply or possible supply of the goods or services;
(d) whether any undue influence or pressure was exerted on, or any unfair tactics were used against, the consumer or a person acting on behalf of the consumer by the corporation or a person acting on behalf of the corporation in relation to the supply or possible supply of the goods or services; and
(e) the amount for which, and the circumstances under which, the consumer could have acquired identical or equivalent goods or services from a person other than the corporation.
(3) A corporation shall not be taken for the purposes of this section to engage in unconscionable conduct in connection with the supply or possible supply of goods or services to a person by reason only that the corporation institutes legal proceedings in relation to that supply or possible supply or refers a dispute or claim in relation to that supply or possible supply to arbitration.
(4) For the purpose of determining whether a corporation has contravened subsection (1) in connection with the supply or possible supply of goods or services to a person:
(a) the court shall not have regard to any circumstances that were not reasonably forseeable at the time of the alleged contravention; and
(b) the court may have regard to conduct engaged in, or circumstances existing, before the commencement of this section.
(5) A reference in this section to goods or services is a reference to goods or services of a kind ordinarily acquired for personal, domestic or household use or consumption.
…
21 Section 51AB of the TPA was replaced by s 21 of the ACL. The ACCC contended that the conduct of NRM was unconscionable and thereby infringed s 21 of the ACL. Section 21 applied to the conduct of NRM between 1 January 2011 and 1 January 2012. At that time, it provided as follows:
(1) A person must not, in trade or commerce, in connection with the supply or possible supply of goods or services to another person, engage in conduct that is, in all the circumstances, unconscionable.
(2) Without in any way limiting the matters to which the court may have regard for the purpose of determining whether a person (the supplier) has contravened subsection (1) in connection with the supply or possible supply of goods or services to another person (the consumer), the court may have regard to:
(a) the relative strengths of the bargaining positions of the supplier and the consumer; and
(b) whether, as a result of conduct engaged in by the person, the consumer was required to comply with conditions that were not reasonably necessary for the protection of the legitimate interests of the supplier; and
(c) whether the consumer was able to understand any documents relating to the supply or possible supply of the goods or services; and
(d) whether any undue influence or pressure was exerted on, or any unfair tactics were used against, the consumer or a person acting on behalf of the consumer by the supplier or a person acting on behalf of the supplier in relation to the supply or possible supply of the goods or services; and
(e) the amount for which, and the circumstances under which, the consumer could have acquired identical or equivalent goods or services from a person other than the supplier.
(3) A person is not to be taken for the purposes of this section to engage in unconscionable conduct in connection with the supply or possible supply of goods or services to a person by reason only that the person institutes legal proceedings in relation to that supply or possible supply or refers a dispute or claim in relation to that supply or possible supply to arbitration.
(4) For the purpose of determining whether a person has contravened subsection (1) in connection with the supply or possible supply of goods or services to another person:
(a) the court must not have regard to any circumstances that were not reasonably foreseeable at the time of the alleged contravention; and
(b) the court may have regard to conduct engaged in, or circumstances existing, before the commencement of this section.
(5) A reference in this section to goods or services is a reference to goods or services of a kind ordinarily acquired for personal, domestic or household use or consumption.
(6) A reference in this section to the supply or possible supply of goods does not include a reference to the supply or possible supply of goods for the purpose of re-supply or for the purpose of using them up or transforming them in trade or commerce.
(7) Section 4 applies for the purposes of this section in the same way as it applies for the purposes of Division 1 of Part 3‑1.
22 Section 21 of the ACL was amended, taking effect from 1 January 2012. It governed the conduct of NRM in 2012. This new section is relevantly in the following terms:
(1) A person must not, in trade or commerce, in connection with:
(a) the supply or possible supply of goods or services to a person (other than a listed public company); or
(b) the acquisition or possible acquisition of goods or services from a person (other than a listed public company);
engage in conduct that is, in all the circumstances, unconscionable.
…
(3) For the purpose of determining whether a person has contravened subsection (1):
(a) the court must not have regard to any circumstances that were not reasonably foreseeable at the time of the alleged contravention; and
(b) the court may have regard to conduct engaged in, or circumstances existing, before the commencement of this section.
(4) It is the intention of the Parliament that:
(a) this section is not limited by the unwritten law relating to unconscionable conduct; and
(b) this section is capable of applying to a system of conduct or pattern of behaviour, whether or not a particular individual is identified as having been disadvantaged by the conduct or behaviour; and
(c) in considering whether conduct to which a contract relates is unconscionable, a court’s consideration of the contract may include consideration of:
(i) the terms of the contract; and
(ii) the manner in which and the extent to which the contract is carried out;
and is not limited to consideration of the circumstances relating to formation of the contract.
23 Section 22 of the ACL, also taking effect from 1 January 2012, contains the considerations previously contained in s 51AB(2) of the TPA and s 21(2) of the ACL, but added some further considerations. It is relevantly in the following terms:
(1) Without limiting the matters to which the court may have regard for the purpose of determining whether a person (the supplier) has contravened section 21 in connection with the supply or possible supply of goods or services to a person (the customer), the court may have regard to:
(a) the relative strengths of the bargaining positions of the supplier and the customer; and
(b) whether, as a result of conduct engaged in by the supplier, the customer was required to comply with conditions that were not reasonably necessary for the protection of the legitimate interests of the supplier; and
(c) whether the customer was able to understand any documents relating to the supply or possible supply of the goods or services; and
(d) whether any undue influence or pressure was exerted on, or any unfair tactics were used against, the customer or a person acting on behalf of the customer by the supplier or a person acting on behalf of the supplier in relation to the supply or possible supply of the goods or services; and
(e) the amount for which, and the circumstances under which, the customer could have acquired identical or equivalent goods or services from a person other than the supplier; and
(f) the extent to which the supplier’s conduct towards the customer was consistent with the supplier’s conduct in similar transactions between the supplier and other like customers; and
(g) the requirements of any applicable industry code; and
(h) the requirements of any other industry code, if the customer acted on the reasonable belief that the supplier would comply with that code; and
(i) the extent to which the supplier unreasonably failed to disclose to the customer:
(i) any intended conduct of the supplier that might affect the interests of the customer; and
(ii) any risks to the customer arising from the supplier’s intended conduct (being risks that the supplier should have foreseen would not be apparent to the customer); and
(j) if there is a contract between the supplier and the customer for the supply of the goods or services:
(i) the extent to which the supplier was willing to negotiate the terms and conditions of the contract with the customer; and
(ii) the terms and conditions of the contract; and
(iii) the conduct of the supplier and the customer in complying with the terms and conditions of the contract; and
(iv) any conduct that the supplier or the customer engaged in, in connection with their commercial relationship, after they entered into the contract; and
(k) without limiting paragraph (j), whether the supplier has a contractual right to vary unilaterally a term or condition of a contract between the supplier and the customer for the supply of the goods or services; and
(l) the extent to which the supplier and the customer acted in good faith.
…
24 Section 51AB and s 21 in its two relevant forms prohibited unconscionable conduct, but the concept was not defined in the statute. However, other provisions shed light on what is meant by the concept.
25 For a start, it is clear that the assessment of unconscionable conduct involves a wide-ranging enquiry because the sections stipulate that the conduct be unconscionable in all the circumstances. Then, the provisions specify some matters which the Court may take into account in making the assessment. The specified matters are not exhaustive. They do not prevent the Court having regard to other matters if they are relevant.
26 Section 51AB(2), s 21(2) in the form applicable until 1 January 2012, and s 22(1) as applicable after 1 January 2012 all specify five matters to which the Court might have regard in determining whether the supplier engaged in unconscionable conduct. The considerations are:
1. the reality of bargaining strength of the parties;
2. whether the customers were required to comply with conditions that were not reasonably necessary to protect the supplier’s legitimate interests;
3. whether the customer was able to understand the documents relating to the transaction;
4. whether any undue influence or pressure was exerted on, or unfair tactics used against the customer; and
5. the price of or conditions for the provision of alternative or identical goods or services.
27 It was also established, before s 21 was amended, that the concept of unconscionable conduct in s 51AB was not limited by equitable doctrines concerning unconscionable conduct: Australian Competition and Consumer Commission v CJ Berbatis Holdings Pty Ltd (No 2) (2000) 96 FCR 491; [2000] FCA 2 at [24]; Australian Competition and Consumer Commission v Radio Rentals Ltd (2005) 146 FCR 292; [2005] FCA 1133 at [24]. That was put beyond argument by the 2012 amendment to s 21(4), which provided at the relevant time and currently provides that the section is not limited by the unwritten law relating to unconscionable conduct.
28 Section 21(4)(b) also makes clear that the concept of unconscionability is wide enough to apply to a system of conduct or pattern of behaviour, even if no individual is identified as having been disadvantaged. And in contract cases, by s 21(4)(c), the Court can examine the terms of the contract and the manner and extent to which it was carried out. The Court is not limited to a consideration of the circumstances relating to the formation of the contract.
29 Then, the amendment to s 22 added seven further considerations to which the Court may have regard when determining whether conduct is unconscionable (s 22(1)(f) – (l)). The width of the concept of unconscionability is further emphasised by these additional considerations which include, for instance, the requirements of an industry code, the extent to which the supplier was willing to negotiate the terms and conditions of the contract with the customer, whether the supplier has the right to vary unilaterally a term or condition of the contract, and the extent to which the supplier and the customer acted in good faith.
30 In order to explain how courts have understood the concept of unconscionable conduct, they have used alternative words and expressions which have tried to encapsulate the essence of the sections.
31 Most reviews commence with the judgment in Qantas Airways Limited v Cameron (1996) 66 FCR 246; [1996] FCA 1483 (Qantas) in which the Court relied on the dictionary definition of unconscionable conduct, that is to say, conduct which shows no regard for conscience, conduct which is irreconcilable with what is right or reasonable (at 262 per Davies J). In addition, Lindgren J, with whom Lehane J agreed at 298, said at 284 that victimisation, manipulation, exploitation, unfairness, unreasonableness, unscrupulous taking advantage and one person’s taking advantage of another’s special vulnerability or misadventure were all synonyms for unconscionable conduct, “all of them correctly imputing a pejorative moral judgment”. That approach was adopted by the Full Court of this Court in Hurley v McDonalds Australia Limited [1999] FCA 1728; [2000] ATPR 41-741 at [22] and was followed in a number judgments of single judges: Australian Competition and Consumer Commission v Simply No-Knead Franchising Pty Ltd (2000) 104 FCR 253; [2000] FCA 1365; Australian Competition & Consumer Commission v 4WD Systems Pty Ltd [2003] FCA 850; (2003) 200 ALR 491; and Australian Competition and Consumer Commission v Allphones Retail Pty Ltd (No. 2) [2009] FCA 17; (2009) 253 ALR 324.
32 The moral deficit involved in unconscionable conduct, mentioned in passing by Lindgren J in Qantas, was a vehicle used by Spigelman CJ in Attorney General (NSW) v World Best Holdings Limited (2005) 63 NSWLR 557; [2005] NSWCA 261 (World Best) as a means of imposing some limitation on the concept of unconscionable conduct as expressed in s 62B of the Retail Leases Act 1994 (NSW). His Honour said at [121]:
Unconscionability is a concept which requires a high level of moral obloquy. If it were to be applied as if it were equivalent to what was “fair” or “just”, it could transform commercial relationships in a manner which the Minister expressly stated was not the intention of the legislation. The principle of “unconscionability” would not be a doctrine of occasional application, when the circumstances are highly unethical, it would be transformed into the first and easiest port of call when any dispute about a retail lease arises.
33 In Tonto Home Loans Australia Pty Ltd v Tavares [2011] NSWCA 389; [2011] ASC 155 – 107 (Tonto), Allsop P, as he then was, said of the requirement of a high level of moral obloquy at [293]:
Whether that is too stringent and whether “significant” or “real” may be preferable need not be decided. What is required is some degree of moral tainting in the transaction of a kind that permits the opprobrium of unconscionability to characterise the conduct of the party.
34 In Australian Competition and Consumer Commission v Lux Distributors Pty Ltd [2013] FCAFC 90; [2013] ATPR 42-447 (Lux) at [41], the issue was revisited by the Full Court of this Court thus:
Notions of moral tainting have been said to be relevant, as often they no doubt are, as long as one recognises that it is conduct against conscience by reference to the norms of society that is in question.
35 The role of the element of moral taint was raised directly in Director of Consumer Affairs Victoria v Scully & Anor (No. 3) [2013] VSCA 292; (2013) 303 ALR 168 (Scully), in relation to the cognate provision of the Fair Trading Act 1999 (Vic). The Director of Consumer Affairs in Victoria argued on appeal that moral obloquy was not required to prove unconscionable conduct. The Director contended that the trial judge erred in rejecting this proposition. In dismissing the appeal, the Court of Appeal held at [58] that, “the trial judge understood statutory unconscionability as involving moral taint, and that absent such taint, conduct which might be thought otherwise to be unfair or unreasonable should not be held to be ‘unconscionable’.” The Court held that the trial judge applied the existing tests, which were not plainly wrong.
36 The Court of Appeal said at [48] that, “a distinctive quality of unconscionable conduct as against unreasonable or unfair conduct is that it is unethical.” It seems that this formulation was intended to parallel “some degree of moral tainting” referred to by Allsop P in Tonto. The Court of Appeal said at [18] that, “in every case in which there has been a holding of statutory unconscionability, there has been a finding that the conduct of the defendant showed a degree of moral taint: conduct which was unethical.”
37 At the same time the Court of Appeal cautioned against substituting the reference to the moral aspect of the unconscionable conduct for the words of the section. The Court referred to the judgment of Basten JA in Canon Australia Pty Ltd v Patton [2007] NSWCA 246; (2007) 244 ALR 759, in which his Honour said at [4]:
However, to treat the word “unconscionable” as having some larger meaning, derived from ordinary language, and then to seek to confine it by such concepts as high moral obloquy is to risk substituting for the statutory term language of no greater precision in an attempt to impose limits without which the Court may wander from well-trodden paths without clear criteria or guidance. That approach should not be adopted unless the statute clearly so requires.
38 This is the same point as made in Lux at [41], that the touchstone for the examination of evidence is the statutory concept of unconscionable conduct. And that means something against conscience or not done in good conscience: Lux at [41]; Australian Securities and Investments Commission v National Exchange Pty Ltd (2005) 148 FCR 132; [2005] FCAFC 226 (National Exchange) at [33].
39 Conduct which is unfair or unreasonable is not for those reasons alone unconscionable. By reference to what Spigelman CJ said in World Best to justify a requirement of a high moral obloquy, the Court of Appeal in Scully explained that such sections apply to conduct in trade and commerce and in that case, that factor had consequences for the interpretation of the relevant section. The Court of Appeal said at [46]:
That context is itself largely governed by existing legal principle. … The law of contract and that of property, and the principles that constitute them, are the very things which make trade and commerce possible. Without these legal principles, and the existence of institutions such as the courts that are constrained to apply them, the strong would prevail and the weak would go to the wall. It cannot have been the legislature’s intention to interfere with arm’s length commercial transactions by reference to loose notions of unreasonableness and unfairness. The contention favoured by the appellant that conduct may be found to be unconscionable within s 8(1) of the Act if it can be found to be irreconcilable with what was right and reasonable overlooks the force of the observation of Deane J in Muschinski v Dodds that judges in equity, whose jurisdiction was discretionary, had long since abandoned recourse to undefined notions of justice and what was fair.
[Footnotes omitted.]
40 In Lux, the Court identified the significance of community standards of conduct enacted in State consumer protection legislation in the evaluation of conduct for the purpose of the sections. The Court said at [23]:
The task of the Court is the evaluation of the facts by reference to a normative standard of conscience. That normative standard is permeated with accepted and acceptable community values. In some contexts, such values are contestable. Here, however, they can be seen to be honesty and fairness in the dealing with consumers. The content of those values is not solely governed by the legislature, but the legislature may illuminate, elaborate and develop those norms and values by the act of legislating, and thus standard setting. The existence of State legislation directed to elements of fairness is a fact to be taken into account. It assists the Court in appreciating some aspects of the publicly recognised content of fairness, without in any way constricting it. Values, norms and community expectations can develop and change over time. Customary morality develops “silently and unconsciously from one age to another”, shaping law and legal values: Cardozo, The Nature of the Judicial Process (Newhaven, Yale University Press, 1921) pp 104-105. These laws of the States and the operative provisions of the ACL reinforce the recognised societal values and expectations that consumers will be dealt with honestly, fairly and without deception or unfair pressure. These considerations are central to the evaluation of the facts by reference to the operative norm of required conscionable conduct.
41 After judgment was reserved in this case, the Full Court of this Court delivered judgment in Paciocco v Australia and New Zealand Banking Group Limited [2015] FCAFC 50 (ANZ). One claim made by the appellant was that certain fees charged by the ANZ Bank amounted to conduct which was unconscionable. This claim relied on provisions of the Australian Securities and Investment Commission Act 2001 (Cth) (ASIC Act) and the Fair Trading Act 1999 (Vic) which prohibited unconscionable conduct in similar terms to s 21 of the ACL. The terms of s 12CB of the ASIC Act, the central provision relied upon, were essentially the same as s 21 of the ACL, save that the section operated in the field of financial services.
42 The judgment of Allsop CJ, with whom Besanko and Middleton JJ agreed, added further to the learning concerning the proper approach to the construction of the statutory concept of unconscionability.
43 In a continuation of the debate about the relationship between the concepts of moral obloquy and unconscionability, there was a further warning concerning the substitution of synonyms for the words of the statute. At [262] the Chief Justice wrote:
That a degree of morality lies within the word “unconscionable” is clear. “Unconscionability” is a value-laden concept. “Obloquy” is “the condition of being spoken against; bad repute; reproach; disgrace; a cause of detraction or reproach,”; “obliquity” is “a deviation from moral rectitude, sound thinking or right practice; a delinquency; a fault or error.”: The Shorter Oxford English Dictionary on Historical Principles (3rd Ed, Oxford, 1969) Vol 2 p 1428. That unconscionability contains an element of deviation from rectitude or right practice or of delinquency can be readily accepted, as long as the phrase “moral obloquy” is not taken to import into unconscionability a necessary conception of dishonesty. The statutory language is “unconscionable”: that is, against conscience. A sense of moral obloquy or moral obliquity can be accommodated within the meaning or conception of unconscientious or unconscionable conduct. That said, an understanding of the meaning conveyed by the word “unconscionable” in the statute is not simply restated by substituting other words for those chosen by Parliament; danger easily lurks in the use of other words to capture the meaning of the statutory language.
44 And to similar effect, his Honour said at [305]:
The task is not limited to finding "moral obloquy"; such may only divert the normative inquiry from that required by the statute, to another, not tied to the words of the statute. The clearest example of the lack of need for dishonesty, at least in Equity in unconscionable conduct (in the unwritten law), is the lack of criticism of the bank manager in Amadio by Deane J: 151 CLR at 478. See also Johnson v Smith [2010] NSWCA 306 at [5] and Aboody v Ryan [2012] NSWCA 395 at [65]. Such is not to deny that, in many cases of unconscionable conduct in Equity, a degree of moral criticism may attend the evaluation that the relevant conduct was unconscionable.
45 Then, at [262] the judgment considered how the concept of unconscionability should be understood as follows:
The task involved is not the choice of synonyms; rather, it is to identify and apply the values and norms that Parliament must be taken to have considered relevant to the assessment of unconscionability: being the values and norms from the text and structure of the Act, and from the context of the provision. Parliament has given some guidance to its proper application (and to its meaning) by identifying in s 12CC [which is in relevantly the same terms as s 22 of the ACL] certain non-exhaustive factors that may be taken into account by a court in deciding whether conduct was unconscionable. Given the value-laden character of the word, it is necessary to ascertain and organise the relevant values and norms by reference to which the meaning of the word is to be ascertained, and by reference to which the application of the section is to be undertaken (the two tasks being distinct). It must, however, be emphasised at the outset that the values and norms that are relevant are those that Parliament has considered, or must be taken to have considered, as relevant. The following discussion should be understood as dealing with those matters, and not with any values or norms disembodied from, or unconnected with, the choice made by Parliament.
46 The judgment surveyed the values and the norms which have been recognised in the common law, equity, and in statutes. Reference was made to the comments on the difference in approach between equity and the common law by Lord Stowell in The Juliana [1822] EngR 235; (1822) 2 Dods 504 at 522; 165 ER 1560 at 1567, as cited by Dixon CJ, McTiernan and Kitto JJ in Jenyns v Public Curator (Qld) (1953) 90 CLR 113 at 119; [1953] HCA 2 at [3] as follows:
A court of law works its way to short issues, and confines its views to them. A court of equity takes a more comprehensive view, and looks to every connected circumstance that ought to influence its determination upon the real justice of the case.
47 Then, in a conclusion which applies equally to the consumer as to the business context, Allsop CJ said at [296]:
The working through of what a modern Australian commercial, business or trade conscience contains and requires, in both consumer and business contexts, will take its inspiration and formative direction from the nation's legal heritage in Equity and the common law, and from modern social and commercial legal values identified by Australian Parliaments and courts. The evaluation of conduct will be made by the judicial technique referred to in Jenyns. It does not involve personal intuitive assertion. It is an evaluation which must be reasoned and enunciated by reference to the values and norms recognised by the text, structure and context of the legislation, and made against an assessment of all connected circumstances. The evaluation includes a recognition of the deep and abiding requirement of honesty in behaviour; a rejection of trickery or sharp practice; fairness when dealing with consumers; the central importance of the faithful performance of bargains and promises freely made; the protection of those whose vulnerability as to the protection of their own interests places them in a position that calls for a just legal system to respond for their protection, especially from those who would victimise, predate or take advantage; a recognition that inequality of bargaining power can (but not always) be used in a way that is contrary to fair dealing or conscience; the importance of a reasonable degree of certainty in commercial transactions; the reversibility of enrichments unjustly received; the importance of behaviour in a business and consumer context that exhibits good faith and fair dealing; and the conduct of an equitable and certain judicial system that is not a harbour for idiosyncratic or personal moral judgment and exercise of power and discretion based thereon.
48 This collection of considerations taken from the review of the norms, values and principles applied in the common law, equity, and in statute is a helpful catalogue of the types of considerations which might illuminate the meaning of unconscionability. They reflect similar ideas to those expressed in the catalogue of synonyms referred to by Lindgren J in the early case of Qantas.
49 At [304] Allsop CJ referred to the margin allowable in the construction of the concept for differing views, and hence, differing outcomes in the assessment of what is or is not unconscionable conduct. His Honour said:
In any given case, the conclusion as to what is, or is not, against conscience may be contestable. That is inevitable given that the standard is based on a broad expression of values and norms. Thus, any agonised search for definition, for distilled epitomes or for shorthands of broad social norms and general principles will lead to disappointment, to a sense of futility, and to the likelihood of error. The evaluation is not a process of deductive reasoning predicated upon the presence or absence of fixed elements or fixed rules. It is an evaluation of business behaviour (conduct in trade or commerce) as to whether it warrants the characterisation of unconscionable, in the light of the values and norms recognised by the statute.
50 Two observations might be made about these issues addressed in ANZ.
51 The first relates to the purpose of statutory unconscionability provisions such as s 21 of the ACL. Whilst their construction is aided by reference to the values, principles, and norms applied in the development of the common law and equity, such provisions are designed to add to the protection already accorded by the law. They are not intended to codify existing law. Consequently, there is no case for restricting the scope of such provisions by reference to the existing law.
52 The second observation concerns the process by which the construction of such provisions occurs. Almost all of the judgment of Allsop CJ on this issue concerned what the process of construction does involve. Only at one point did he refer to what the process does not involve. On that matter his Honour said at [296]:
It does not involve personal intuitive assertion.
53 On the same subject Middleton J said:
402 On the issue of statutory unconscionability, a rationally based system of law needs to set out the limits of acceptable commercial behaviour in order that persons can order their commercial affairs in advance. Such a system cannot depend on the personal approach of a judge, based upon his or her view of commercial morality.
54 And continued:
405 Similarly, in the context of determining the content of statutory unconscionable conduct, as described by Allsop CJ, the task of a court is to make an evaluation of the facts and an ultimate determination by reference to a statutory standard of conduct, guided by the text and structure of the statute and its purpose. This task is a familiar one undertaken in the course of the judicial process.
406 This approach is not to be seen as any particular judge imposing his or her perception of desirable social goals as the basis for his or her ultimate determination. Nor does this process involve the court in determining policy. The legislature has enacted the law in pursuit of the community standard or expectation of commercial behaviour, which the court then applies in any given factual scenario.
55 These reflections were probably intended to say no more than that the process of construction and application cannot be the result of an individual judge’s idiosyncratic, capricious, or unreasoned preferences. So much would be uncontroversial, but leaves open the reason why the determination of what is, or is not, against conscience in particular fact situations may be contestable. It also leaves unexplained the process by which the values, norms, and principles of the common law and equity have developed and become accepted by judges. And it leaves unexplained how judges choose between competing values, norms, and principles where they conflict with each other. In the criminal law it is now orthodox that after taking account of the needs for punishment, deterrence, rehabilitation, and the totality principle, a sentencing judge must apply an instinctive or intuitive synthesis to arrive at the appropriate sentence: Markarian v The Queen (2005) 228 CLR 357; [2005] HCA 25 (Markarian). The following explanation by McHugh J in Markarian of the influences on the process of arriving at a sentence by instinctive synthesis has a similarity to the explanation given by Allsop CJ of the process by which unconscionability is determined:
84 … instinctive synthesis involves the exercise of a discretion controlled by judicial practice, appellate review, legislative indicators and public opinion. Statute, legal principle and community values all confine the scope in which instinct may operate.
Perhaps the unexplained reason for differences in the views of what constitutes unconscionable depends on a similar process.
56 The respondents appeared at times to suggest that the conduct of AMI or NRM was not unconscionable because the conduct had no disadvantageous consequences in that a particular patient did not enter into a contract at all, or if he did so, he had obtained a full refund of the cost of treatment.
57 In National Exchange the respondent at first instance argued that the conduct of National Exchange in sending out offers to purchase shares at well below value, in the expectation that some commercially naïve shareholders would sell as a result of ignorance was not unconscionable because the conduct was not directed to a particular person who had suffered any consequences. The trial judge upheld this argument. He said that it was not meaningful to speak of unconscionable conduct in the abstract. The Full Court disagreed, holding at [44] that the section:
[R]equires the Court to focus primarily on the unconscionable conduct of the offeror and to determine whether that conduct is contrary to the norm of conscientious behaviour.
[Emphasis in original.]
58 The view expressed in that judgment has statutory expression from 1 January 2012 in s 21(4)(b) of the ACL.
59 And in Lux, the Full Court held that the appellant had engaged in unconscionable conduct even though it had refunded the purchase price of the vacuum cleaners and replaced the old vacuum cleaners which had been taken from the customers. In other words, there was unconscionable conduct even though the disadvantageous consequences of it had been reversed.
60 In ANZ, Allsop CJ said at [299] that the assessment of unconscionability:
[M]ay involve behaviour that is best evaluated relationally in a transaction; they may involve conduct that can be evaluated against normative or ethical standards, apart from any particular transaction: see, for instance, National Exchange.
61 And his Honour explained at [309] that the particular case involved an assessment of:
… the transactions and contracts of Mr Paciocco and SDG, and … ANZ’s conduct generally relating to the group as a whole. Section 12CB(4)(b) emphasises that, even if there are factors militating against a conclusion that there was any unconscionable conduct by ANZ in its dealing with Mr Paciocco and SDG, that does not mean the “system of conduct or pattern of behaviour” of ANZ cannot exhibit unconscionable conduct.
62 The ACCC contended that a term of the contracts offered to patients by NRM relating to termination was an unfair term and was void within the meaning of s 23 of the ACL. That section provides and provided at all relevant times:
Unfair terms of consumer contracts
(1) A term of a consumer contract is void if:
(a) the term is unfair; and
(b) the contract is a standard form contract.
(2) The contract continues to bind the parties if it is capable of operating without the unfair term.
(3) A consumer contract is a contract for:
(a) a supply of goods or services; or
(b) a sale or grant of an interest in land;
to an individual whose acquisition of the goods, services or interest is wholly or predominantly for personal, domestic or household use or consumption.
63 Section 24 defines the meaning of unfair as follows:
Meaning of unfair
(1) A term of a consumer contract is unfair if:
(a) it would cause a significant imbalance in the parties' rights and obligations arising under the contract; and
(b) it is not reasonably necessary in order to protect the legitimate interests of the party who would be advantaged by the term; and
(c) it would cause detriment (whether financial or otherwise) to a party if it were to be applied or relied on.
(2) In determining whether a term of a consumer contract is unfair under subsection (1), a court may take into account such matters as it thinks relevant, but must take into account the following:
(a) the extent to which the term is transparent;
(b) the contract as a whole.
(3) A term is transparent if the term is:
(a) expressed in reasonably plain language; and
(b) legible; and
(c) presented clearly; and
(d) readily available to any party affected by the term.
(4) For the purposes of subsection (1)(b), a term of a consumer contract is presumed not to be reasonably necessary in order to protect the legitimate interests of the party who would be advantaged by the term, unless that party proves otherwise.
64 Section 25 provides examples of unfair terms and relevantly includes the following:
Examples of unfair terms
(1) Without limiting section 24, the following are examples of the kinds of terms of a consumer contract that may be unfair:
…
(c) a term that penalises, or has the effect of penalising, one party (but not another party) for a breach or termination of the contract;
65 Section 27 deals with standard form contracts as follows:
Standard form contracts
(1) If a party to a proceeding alleges that a contract is a standard form contract, it is presumed to be a standard form contract unless another party to the proceeding proves otherwise.
(2) In determining whether a contract is a standard form contract, a court may take into account such matters as it thinks relevant, but must take into account the following:
(a) whether one of the parties has all or most of the bargaining power relating to the transaction;
(b) whether the contract was prepared by one party before any discussion relating to the transaction occurred between the parties;
(c) whether another party was, in effect, required either to accept or reject the terms of the contract (other than the terms referred to in section 26(1)) in the form in which they were presented;
(d) whether another party was given an effective opportunity to negotiate the terms of the contract that were not the terms referred to in section 26(1);
(e) whether the terms of the contract (other than the terms referred to in section 26(1)) take into account the specific characteristics of another party or the particular transaction;
(f) any other matter prescribed by the regulations.
66 The ACCC claimed that, whilst AMI contravened s 51AB of the TPA, and NRM contravened s 21 of the ACL, Dr Vaisman aided, abetted, counselled or procured or was knowingly concerned in or party to the respective contraventions. As a result, the Court possessed power to grant injunctions against Dr Vaisman under s 80(1)(c) and (1)(e) of the TPA and s 232(1)(c) and (1)(e) of the ACL. The relevant provisions provide as follows:
80 Injunctions
(1) Subject to subsections (1A), (1AAA) and (1B), where, on the application of the Commission or any other person, the Court is satisfied that a person has engaged, or is proposing to engage, in conduct that constitutes or would constitute:
(a) a contravention of any of the following provisions:
(i) a provision of Part IV, IVA [in which s 51AB appears], IVB, V or VC;
…
(b) attempting to contravene such a provision; or
(c) aiding, abetting, counselling or procuring a person to contravene such a provision; or
(d) inducing, or attempting to induce, whether by threats, promises or otherwise, a person to contravene such a provision; or
(e) being in any way, directly or indirectly, knowingly concerned in, or party to, the contravention by a person of such a provision;
(f) conspiring with others to contravene such a provision;
the Court may grant an injunction in such terms as the Court determines to be appropriate.
232 Injunctions
(1) A court may grant an injunction, in such terms as the court considers appropriate, if the court is satisfied that a person has engaged, or is proposing to engage, in conduct that constitutes or would constitute:
(a) a contravention of a provision of Chapter 2 [in which s 21 and s 23 appear], 3 or 4; or
(b) attempting to contravene such a provision; or
(c) aiding, abetting, counselling or procuring a person to contravene such a provision; or
(d) inducing, or attempting to induce, whether by threats, promises or otherwise, a person to contravene such a provision; or
(e) being in any way, directly or indirectly, knowingly concerned in, or party to, the contravention by a person of such a provision; or
(f) conspiring with others to contravene such a provision.
67 The ACCC’s case was initially that the provisions relevant to the grant of injunctions against Dr Vaisman were s 75B and s 80 of the TPA, and s 232 of the ACL. In correspondence to the Court dated 2 March 2015, the solicitors for the ACCC clarified its position that the Court need only have regard to s 232 of the ACL. That is because of the effect of certain transitional provisions. The TPA continues to apply to proceedings commenced but not concluded before 1 January 2011. However, pursuant to item 7(2) of Schedule 7 of the Trade Practices Amendment (Australian Consumer Law) Act (No 2) 2010 (Cth), where the proceedings are proceedings for an injunction under s 80 of the TPA, the proceedings are taken to be proceedings for an injunction under s 232 of the ACL. Consequently, the Court need only have regard to s 232 in considering the claim for injunctions against Dr Vaisman and NRM.
68 In order to bring Dr Vaisman within s 232, the ACCC needed to show that Dr Vaisman knew of the essential elements which made up the contraventions: Yorke v Lucas (1985) 158 CLR 661 at 666–668 and 669–670; [1985] HCA 65 at [9]–[13] and [16]. In order to know the essential facts it is not necessary to know that those facts are capable of characterisation in the language of the statute: Rural Press Ltd v Australian Competition and Consumer Commission (2003) 216 CLR 53; [2003] HCA 75 at [48] per Gummow, Hayne and Heydon JJ. An example of these principles applied in a case of unconscionable conduct is Coggin v Telstar Finance Company (Q) Pty Ltd [2006] FCA 191; [2006] ATPR 42 – 107.
69 Section 140 of the Evidence Act 1995 (Cth) (the Evidence Act) provides:
(1) In a civil proceeding, the court must find the case of a party proved if it is satisfied that the case has been proved on the balance of probabilities.
(2) Without limiting the matters that the court may take into account in deciding whether it is so satisfied, it is to take into account:
(a) the nature of the cause of action or defence; and
(b) the nature of the subject-matter of the proceeding; and
(c) the gravity of the matters alleged.
70 When assessing the evidence in the present case, the Court is required to take into account that the cause of action arises in the context of provisions designed to protect consumers. At the same time, the relief sought would, if granted, have a major impact on the way the respondents conduct their business. Further, some of the allegations made against the respondents are close to allegations of fraud and certainly include allegations of dishonest conduct. In the terms of the oft-quoted passage from the judgment of Dixon J in Briginshaw v Briginshaw (1938) 60 CLR 336 at 361; [1938] HCA 34, the Court must feel an “actual persuasion” of the occurrence before it can find that the occurrence has been established. The finding of facts in this case must therefore be approached particularly bearing in mind the seriousness of the allegations made against the respondents.
3. THE SCOPE OF THE ACCC’S CASE
3.1 The Further Amended Statement of Claim
71 In order to understand the factual examination undertaken in these reasons for judgment, and to understand some of the criticisms made by the respondents of the structure of the ACCC’s case, it is necessary to set out the framework of the ACCC’s case. This is best done by a reference to parts of the ACCC’s further amended statement of claim dated 14 December 2011 (FASOC).
72 Paragraph 5 pleaded, inter alia, that AMI advertised its business extensively in newspapers, television, radio and other media under the name Advanced Medical Institute. The advertising emphasised that the treatment for ED and PE was by consultation with doctors.
73 Paragraph 6 pleaded that the consultations were by phone or by attendance at a clinic. When the consultations were by phone, patients spoke first to a clinical coordinator who obtained personal information, then to a doctor engaged by AMI, and finally patients spoke with the clinical coordinator again who organised payment by direct debit or credit card. When the consultations were in a clinic, patients first provided some personal information to a nurse, then spoke to a doctor by phone from the clinic, and finally spoke in person to a clinical coordinator who organised payment by direct debit or credit card.
74 Paragraph 7 pleaded that by publishing the advertisements referred to in [5] of the FASOC, by referring to itself as the Advanced Medical Institute, and by providing treatments only after a discussion with a doctor as referred to in [6], AMI represented that patients would receive a proper objective medical assessment, and treatment consistent with that assessment, by a qualified medical doctor.
75 Paragraph 8 pleaded that AMI sold or offered to sell treatments to consumers, including the patients listed in Annexure B to the FASOC (the Annexure B patients), on terms by which:
(a) the cost of the AMI treatments to the patient was calculated by reference to a fixed period of use, the effect of which was that the longer the treatment period the greater was the total amount paid by the patient;
(b) the patient was obliged to pay for the entire course of the AMI treatments purchased, regardless of how much or which of the AMI medications the patient actually used;
(c) when a prescribed AMI medication did not successfully treat a patient's condition AMI:
(i) refused to refund the cost incurred by the patient for the course of treatment unless the patient tried at least one option from each of the available delivery mechanisms for which the patient was not contraindicated by an AMI doctor, including intracavernous injections at the base of the penis, and
(ii) if each of the available delivery mechanisms was unsuccessful, AMI would only refund the agreed price less an amount charged by AMI for supplying the medication and an administration fee.
AMI described this term to its patients as a "satisfaction guarantee"; and
…
(d) the cost of the AMI treatments to the patient greatly exceeded the cost of treatment available during the period from general medical practitioners for the treatment of male sexual dysfunction.
76 Paragraph 10 pleaded that in the consultations with Annexure B patients, AMI doctors:
(a) did not offer, prescribe or discuss with the patient any treatment or medication other than that offered by AMI;
(b) did not advise the patient of the terms on which the AMI treatments they recommended and the AMI medications they prescribed would be provided by AMI as alleged in [8]
(c) recommended the AMI treatments, which included AMI medications which they had not discussed with the patient;
(c1) prescribed AMI Medications:
(i) which the doctors had not selected from the range of all medications available for prescription by Australian medical practitioners; and
(ii) in respect of which the doctors had not or had not adequately advised about side effects which included (in the case of intracavernous injections) the need to manage priapism if it occurred;
(d) did not seek to diagnose any underlying cause for the presenting problem;
(e) did not seek to diagnose whether it would have been medically appropriate to refer the patient to a specialist or other medical practitioner for treatment or diagnosis;
(f) were required by AMI to recommend only the AMI treatments and to prescribe only the AMI medications but did not disclose that fact to the patient; and
(g) did not see or conduct any physical examination of the patient;
77 Paragraph 11 pleaded that the conduct pleaded in [10] of the FASOC:
(a) was contrary to the requirements and standards applicable to the proper, objective and appropriate diagnosis and medical treatment of male sexual dysfunction; and
(b) involved the subordination of the patient's medical interests to the commercial interests of AMl.
78 Paragraph 13 pleaded that in consultations with the Annexure B patients clinical coordinators:
(a) followed scripts which were provided by AMI, including some or all of the scripts extracted in [20] of the FASOC;
(b) made statements to patients concerning:
(i) the adverse medical and social consequences that the patient would suffer if he did not purchase and use the AMI treatments;
(ii) the patient's need for the AMI treatments;
(iii) the efficacy of the AMI treatments,
the effect of which was to apply pressure to the patient to purchase the AMI treatments;
(c) represented to patients that they would be entitled to a refund of moneys paid for AMI treatments if the treatments were ineffective, without accurately or clearly disclosing the conditions on which the refund was offered, including the requirement that the patient use intracavernous injections at the base of the penis, as alleged in [8(c)]; and
(d) by describing themselves as "Clinical Co-Ordinators", "Medical Co-Ordinators" and "Doctors' Assistants" and by not telling the patient that they were in fact sales agents paid on commission, conveyed the impression that they were acting in the patients' medical interests in selling the AMI treatments.
79 Paragraph 15 pleaded that men to whom AMI offered to sell and sold the AMI treatments were, to AMI's knowledge, vulnerable to AMI's attempts to sell AMI treatments to them in that:
(a) the conditions from which they suffered were perceived as embarrassing or humiliating; and
(b) they reasonably reposed trust in AMI's doctors and expected that those doctors were acting in their best interests.
80 Then, [17] of the FASOC brought together the preceding allegations in a pleading of unconscionable conduct as follows:
By:
(a) AMI selling or offering to sell the AMI treatments on the terms described at each of sub-paragraphs 8(a)-(d), including to the patients identified at Annexure B;
(b) AMI's doctors doing or failing to do the things alleged at each of sub-paragraphs 10(a)-(g) in the course of consulting with the patients identified at Annexure B; and/or
(c) AMI's Clinical Co-ordinators doing or failing to do the things alleged at each of sub-paragraphs 13(a)-(d) in the course of sales consultations with the patients identified at Annexure B;
in circumstances in which:
(d) AMI promoted its business as described at sub-paragraph 5(c);
(e) AMI sold AMI treatments or offered them for sale through the process described in sub-paragraphs 6(a)-(d);
(f) AMI made the representations described in paragraph 7;
(g) the manner in which AMI's doctors conducted medical consultations was:
(i) contrary to the requirements and standards applicable to the proper, objective and appropriate diagnosis and medical treatment of male sexual dysfunction, and
(ii) involved the subordination of the patient's medical interests to the commercial interest of AMl,
as alleged at paragraph 11; and/or
(h) AMI knew that the men to whom it offered to sell and sold its treatments were vulnerable to its attempts to sell to them, as alleged at paragraph 15,
[AMI] has in trade or commerce in connection with the supply or possible supply of goods and services to consumers, engaged in conduct that is unconscionable within the meaning of, and in contravention of section 51AB of the Act.
81 Following a request from the respondents at an earlier stage of the proceedings, the ACCC added [17AA] to the FASOC to explain the way in which the conduct alleged was said to be unconscionable. Paragraph 17AA read as follows:
The conduct of AMI identified in paragraph 17 was unconscionable because, by this conduct:
(a) AMI knowingly exploited its superior bargaining position as a provider of medical expertise and treatment in relation to men who sought medical treatment from it, who were vulnerable to it, in order to extract sales from them;
(b) while holding itself out as a provider of medical expertise on which men who sought treatment for sexual dysfunction could rely, AMI:
(i) subordinated the medical interests of its patients to AMI's commercial interests; and
(ii) provided services in a manner which was contrary to the standards of proper, objective and appropriate medical treatment;
(c) AMI used unfair tactics and undue pressure in seeking to sell its treatments to men who sought medical treatment from it;
(d) in selling its treatments AMI required its patients to comply with terms that were not reasonably necessary to protect AMI's legitimate interests;
(e) AMI sold its treatments for amounts greatly in excess of the cost at which its patients could have acquired treatment for male sexual dysfunction, from general medical practitioners;
(f) AMI bound patients to contracts for supply of its treatments for periods far greater than its patients could, or normally would, have acquired medication and treatment from general medical practitioners for the treatment of male sexual dysfunction; and
(g) AMI did not provide clear and accurate information to its patients about the terms on which its treatments and services were supplied.
82 The case against NRM was pleaded in generally similar terms.
3.2 Is the ACCC’s case an individual-patients case or a business-system case?
83 In their final written submissions the respondents argued
80. The ACCC brought forward a case based on particular patients, not a business practice or tendency case. For that reason, the case must be determined in relation to each transaction. There can be no elision or inferences drawn or tendency reasoning. The respondents repeatedly asked that the ACCC make its case clear, and a tendency or business practice case was expressly disavowed. It is the particularized case that the respondents are meeting. Therefore, while it is possible for there to be a finding of unconscionable conduct where no particular consumers are identified, that is not the case brought and is not the relief sought by the ACCC. Instead, the ACCC seeks relief in relation to particular transactions with particular patients identified in Annexures B and C. Only those transactions are relevant.
84 This submission repeated an argument which was raised by the respondents on several occasions in directions hearings and in a strike-out application filed by the respondents on 12 October 2011 in the pre-trial management process. On each occasion the ACCC explained that its case was not limited in the way submitted by the respondents.
85 As early as 29 November 2011, in written submissions filed in opposition to the respondent’s strike-out application, the ACCC explained:
27. AMI’s conduct in dealing directly with consumers is described in paragraphs 10 and 13 of the claim and is, in summary, that:
AMI’s doctors consulted with the [then] 159 identified patients and in those consultations did or failed to do the things specifically described in subparagraphs 10(a)-(f);
AMI’s sales staff made statements to them the effect of which was to apply pressure to purchase AMI’s treatments; they did not accurately describe the terms of AMI’s refund policy to them; and they described themselves as “doctors’ assistants” or “clinical co-ordinators” rather than as sales agents paid on commission (paragraph 13).
28. Conduct engaged in by AMI to attract and manage patients seeking treatment, which was conduct directed to as a class of consumers generally, is also the subject of the claim. It comprises specifically:
(i) the fact that AMI advertised its business and promoted its expertise in the manner alleged in paragraphs 5(C) and 7 of the claim;
(ii) the fact that AMI structured the way in which it consulted with its patients, as alleged in paragraph 6 of the claim;
(iii) the fact that AMI sold or offered to sell its treatments (including to the [then] 159 identified patients) on the terms set out at paragraph 8 of the claim. The terms concern the cost of the treatment to the patient, the way the cost was calculated and the refund policy.
29 The claim does not, as the respondents contend, concern “each and every aspect of the way in which AMI conducted its business operations, in an unlimited way”. Rather, it concerns the specific aspects of the business alleged.
30 The claim identifies the reasons why the pleaded conduct is unconscionable (paragraphs 17 and 17AA of the proposed amended pleading). Given that unconscionability invokes notions of fairness and moral judgment, it is appropriate that the character of the conduct be described in the pleading. Plainly, the function of paragraph 17 is to do this, and not to allege separate and different conduct by AMI.
[Footnotes omitted.]
86 Then, in its Outline of Opening Submissions filed in Court on 18 March 2013, the ACCC again drew the distinction between evidence of the general business system operated by AMI and the evidence of the consultations with the Annexure B patients. For instance, the submissions stated:
3. Each aspect of the conduct is evidenced by particular patient transactions on which the ACCC relies, very often but not always, all in the same transaction.
4. It is not realistic or feasible for the ACCC to present a case dealing with every instance of conduct, every transaction or even a substantial proportion of those transactions in the given period (2 years for AMI, about 2 years for NRM). The case is brought in relation to a number of particular transactions about which the ACCC has evidence. The transactions are not put forward as representative of all transactions, but as being sufficiently numerous to deserve the intervention of the Court. That is to say, they are sufficiently numerous that they cannot be regarded as isolated failings by individuals who work for AMI, particularly given that they occurred within the business system established and operated by AMI, in a manner consistent with directions from AMI management.
5. Elements of the evidence, necessarily, are directed at the general way the AMI business was conducted. The advertising, by its nature, was of general application. The fact that prescription records show no prescriptions of non-AMI medications such as Viagra or Cialis supports the proposition that AMI doctors did not suggest or prescribe non-AMI medications…
[Footnotes omitted.]
87 The point was reiterated in the oral opening of the trial on 18 March 2013 when senior counsel for the ACCC said:
MR BURNSIDE: Well, your Honour, perhaps if I could start, and try and acquaint you with the geography of what has turned into a fairly sprawling case. The first broad proposition, your Honour, is the way AMI does business, and I think it’s important so as to forestall complaints about things that aren’t – or people that aren’t referred to in annexure B or annexure C is this: what we put forward, as is apparent from the pleadings, is that there are some allegations about the general way in which the AMI business is conducted, and then there are a particular instances of dealing with customers which build on the background of the general pattern, and they are to be the focus of any orders your Honour might ultimately make…
[TS 2]
88 The opening of the ACCC repeated that certain elements of the case were not specific to the Annexure B or Annexure C patients, but were alleged as part of the way AMI and NRM conducted their business, namely, the following elements:
advertising;
nature of a patient’s interaction with AMI and NRM;
role of salespeople and their commission payments;
contract terms and refund policy used during the AMI and NRM periods;
cost of treatment programs;
long-term contracts; and
vulnerability of patients.
This was the way in which the ACCC conducted its case.
89 Despite the exposition by the ACCC of the case it was propounding, the respondents continued to assert that the ACCC pleading did not articulate a case that the business system of AMI and NRM involved unconscionable conduct directed to a class of people. Thus, for instance, in their final written submissions the respondents contended:
128. In order to determine whether each transaction was ‘unconscionable’ an analysis is required of:
(a) The subjective state of the particular patient at the relevant time, including intelligence, age, ability to negotiate, relevant ‘vulnerability’, ability to afford the service, prior dealings with doctors in relation to the medical condition etc;
(b) Whether at the time of the transaction AMI intended to exploit the known weakness of the particular patient;
(c) All the ‘circumstances’ as pleaded by the ACCC.
[Footnotes omitted.]
90 By seeking to characterise the ACCC’s case as one only about individual cases, the respondents felt able to defend themselves by arguing that the ACCC had not established that particular patients had experienced unconscionable conduct. Thus, for instance, the respondents said in their final written submissions that the ACCC had not established that individual patients had a relevant vulnerability. At [141] the respondents contended:
It is only in those cases where a person has come forward and had the opportunity of giving evidence and that evidence being tested that the Court can make any conclusion about ‘vulnerability’. It cannot be done for a whole ‘class’.
91 This analysis also led the respondents to argue that evidence about how AMI operated generally was tendency evidence. That is to say, the respondents seem to have contended that such evidence was used by the ACCC to establish that because AMI operated in a particular way in the individual instances, it was the general tendency of AMI to act in this way. The respondents contended that such evidence was not admissible because the requirements of s 97 of the Evidence Act had not been complied with.
92 The evidence however is not tendency evidence subject to the Evidence Act. It is evidence of a system of operating which the ACCC sought to establish was itself unconscionable conduct. A similar situation was referred to Sackville J in Jacara Pty Ltd v Perpetual Trustees WA Ltd (2000) 106 FCR 51; [2000] FCA 1886 at [67] as follows:
If, for example, the evidence in a shopping centre misrepresentation case shows that the lessor’s agent gave instructions that particular representations should be communicated to prospective tenants, that evidence would [not be tendency evidence]. The evidence, if accepted, would go beyond proving that the agent had a propensity to make representations of the kind alleged. Rather, it would establish that the agent had set in place a system which, if implemented in the particular case, would have resulted in the representation being made to the applicant. The existence of the system, in the absence of evidence to the contrary, readily supports an in inference that it was implemented in the particular case. The evidence of the system makes it more likely that the fact in issue (the making of the representation to the applicant) occurred, independently of the agent’s propensity to act in a particular way.
93 The respondents’ continued attempt to define the ACCC’s case as a case based only on individual patient transactions was a strategy perhaps designed to allow the respondents to raise defences which were not available as answers to a business-system case. The strategy was based on a misconstruction of the ACCC’s case. That case was properly summarised in the ACCC’s written submissions in reply as follows:
8. As a matter of law a person may, by implementing a business model or strategy or by engaging in conduct directed towards a class of people, contravene s.51AB of the Trade Practices Act. Unconscionability under s.51AB is not confined to individual dealings in which one party exploits another who is found, subjectively, to be vulnerable or at special disadvantage (ACCC submissions, [459]-[467]).
9. As the ACCC’s submissions explain, the claim concerns several aspects of the respondents’ conduct, which is a product of the way that the respondents dealt with their patients. Two aspects of AMI’s dealings with its patients (conversations between salespeople and patients and consultations between doctors and patients) were individual to the particular patients, doctors and salespeople. Those aspects (and the other aspects of the conduct the subject of the claim) were expressions of AMI’s business strategy (ACCC submissions, [8-12]).
94 The ACCC explained the reasons for choosing to put before the Court 168 consultations. Having determined to prove, in part, that AMI and NRM had a system of operating which involved unconscionable conduct, the ACCC considered what would be necessary to persuade the Court to grant relief, including injunctions. It reasoned that the Court may need to be persuaded that the system of operating was not merely theoretical but was implemented.
95 In its written submission dated 10 July 2013 regarding the scope of its case, the ACCC sought to justify selecting the 168 cases as follows:
By saying “AMI/NRM had, and implemented a business model” we are not suggesting, nor do we need to say or prove, that AMI or NRM engaged in this conduct (implementation of a plan) all or most of the time. To conclude that AMI and NRM implemented a business model does not, of necessity, require or imply reliance on tendency (similar fact) evidence.
We do not mean, nor do we say, that “this is how AMI/NRM usually or typically acted”, or “these examples are typical of what you would find if you sampled any instance or time during the period”. We simply say, and mean, that AMI and NRM did certain things generically and certain things 170 times, and that those things, taken together (or separately or in more limited combination) reflected their intention – their ‘model’, and therefore their attitude towards consumers.
4. FACT FINDINGS IN RESPECT OF AMI
96 This section of the reasons for judgment addresses the following matters.
97 First, there is an explanation of the process by which patients were dealt with by AMI in the treatment of ED and PE.
98 Then, there is a description of how the recordings of the phone consultations with Annexure B patients were selected by the ACCC from a much larger number of recordings of consultations, and how the Annexure B recordings were utilised in evidence by the ACCC.
99 Then, there is a general consideration of the evidence of Dr Vaisman.
100 Finally, the reasons for judgment examine the conduct of AMI in six categories. The first is the advertising used by AMI to attract patients to use its services. The second is the techniques used by the salespeople to persuade patients to agree to treatment. The third is the practice by which AMI offered only a limited range of medications to patients. The fourth reviews the conduct of the doctors engaged by AMI. That discussion considers the standards applicable in the medical profession to the proper treatment of patients suffering from ED and PE, and examines whether the doctors engaged by AMI complied with those professional standards. The fifth considers the contracts terms on which treatments were provided to patients. The sixth examines the cost of the medications.
101 Although the primary focus of this section relates to AMI, there are some issues which are common to AMI and NRM. They are also dealt with in this section and, where necessary, reference is made to the relevance to NRM.
4.2 An overview of the AMI operation
102 AMI advertised its treatment for male sexual dysfunction extensively on radio, television, online, and on billboards. Patients who responded were able to consult by phone or at clinics. The majority of consultations were undertaken by phone. Thus, in the AMI period between 2008 and 2010, 111,954 patients dealt with AMI by phone and 49,566 patients attended clinics. In the financial year 2007 / 2008, AMI’s financial accounts reported that it received nearly $49 million from customers, in 2008 / 2009, it reported that it received nearly $55 million from customers, and in 2009 / 2010, it reported revenue of almost $40 million.
103 Where the interaction with AMI was by phone the patient first spoke to a salesperson, called a clinical coordinator by AMI, who then transferred the call to a doctor. If the doctor decided to prescribe medication the patient was transferred back to the salesperson who concluded the contractual and payment arrangements.
104 Where the interaction with AMI occurred at a clinic, the patient first met with a nurse. Then, the nurse contacted the doctor by phone and the patient consulted over the phone. Where the doctor decided to prescribe medication the patient dealt with a salesperson at the clinic to finalise the contractual and payment arrangements.
105 AMI advertising emphasised treatment by use of a nasal spray. This method of delivery of the medication was conceived by AMI. The medication was formulated by it and dispensed for it by a compounding pharmacy. Doctors engaged by AMI also prescribed troches, tablets, capsules, and gels made to AMI’s specifications. As a last resort, AMI doctors could prescribe intracavernosal injections which were self-administered by the patient into the base of the penis.
106 The treatment programs recommended to patients by AMI were generally for 12 to 18 months. The price increased with the length of the contracts. Thus, the cost of a 12 month contract was generally about $2,500, and the cost of an 18 month contract was generally about $3,500.
107 AMI had a refund policy in case the treatment did not work. That policy required the patient to try one option from each of the delivery systems of medication offered by AMI, including intracavernosal injections into the base of the penis for both ED and PE.
4.3 Recordings of the consultations
108 Before addressing the alleged conduct of AMI, it is necessary to refer to the evidence on which the ACCC relied to establish what occurred in the patient consultations.
109 On 17 February 2010, the ACCC executed a search warrant at the premises of AMI in Sydney and seized around 66 small cassette tapes. The tapes contained recordings of phone calls over the period from March 2006 to December 2009. Each tape contained 50,000 to 60,000 recordings, and related to a period noted on the tapes of between three to five weeks.
110 Gary Neil Franklin was a senior project officer employed by the ACCC. He was engaged in the investigation of AMI. He affirmed an affidavit on 14 October 2011 [ACCC 1.43], and also gave oral evidence. He estimated that the tapes contained over 3 million calls. It was therefore impractical for the ACCC to rely on all of the recordings, and it was necessary to reduce the number tendered in evidence to a manageable selection.
111 Mr Franklin and other employees of the ACCC listened to a large number of recordings and gained an understanding of their nature. In the end, the ACCC relied on 145 recordings.
112 Mr Franklin described how he went about selecting those recordings. He chose recordings in 2009 because they were the most recent. He then selected recordings on particular days by allowing for a spread of months and days within the week. In that way he ended up with recordings on about 80 days in 2009. He excluded calls which were outside the hours of 7 am to 7 pm because he ascertained that they generally originated from outside Australia and were consequently beyond the scope of the search warrant. As his aim was to capture calls which involved an initial patient contact and followed the salesperson / doctor / salesperson format. He excluded calls that were incomplete, any outgoing calls, and calls made by women. It became clear that initial calls were conducted on particular extension numbers so that the search was filtered by reference to those extension numbers. Mr Franklin also noticed that initial consultation calls usually took more than 12 minutes, so the duration was used as a further filter. Mr Franklin also tried to get a spread of doctors and a spread of salespeople in the selection. By this process Mr Franklin gathered 174 recordings. Of these, 145 recordings were ultimately used in the proceeding. Of the 145 recordings about 100 calls resulted in a sale and about 45 did not.
113 The ACCC tendered the 145 audio recordings and transcripts made from the recordings. It also produced an aide memoire (the aide memoire) which identified and extracted passages or identified omissions from each transcript and which it said supported the particular allegations made in the FASOC.
114 In addition to the 145 consultations evidenced by the recordings, eight AMI patients made witness statements relied on by the ACCC. It transpired that one of the audio recordings was of the consultation with one of the patients who made a statement. Thus, in total, the ACCC relied on consultations by AMI with 152 patients. The patients are listed in Annexure B to the FASOC and are together referred to as the Annexure B patients.
115 Each of the patients was given an identifying number in the proceeding. In order to protect the privacy of the patients whose consultations are in question, those identifying numbers rather than the names of the patients are used in these reasons for judgment. On 17 December 2012, the Court made an order which is still in effect and which prohibits the publication of the names of the Annexure B and C patients.
116 In the period 2008 to 2010, 111,954 patients dealt with AMI by phone. In that context 152 consultations is a small number. That circumstance caused counsel for the respondents to express concern that the Court may be asked to draw an inference that what occurred in the 152 consultations was representative of unconscionable dealing by AMI in the conduct of its business generally. This issue is addressed at [83] – [95] of these reasons for judgment in the section dealing with the scope of the ACCC’s case.
117 In final written submissions the respondents also said that the selection of recordings by Mr Franklin resulted in the omission of consultations that did not result in medications being prescribed. They said that this gave a picture of the prescribing practices of the doctors which did not reflect those instances where medications were not prescribed. The omission of these consultations, however, does not affect the claims in relation to the particular consultations which were in issue. And the omitted consultations would be relevant only if the ACCC was running a tendency case and alleging that the unconscionable conduct evident in the 152 instances demonstrated that such unconscionable conduct occurred in other consultations with AMI patients. This was not the case the ACCC was propounding.
118 Dr Vaisman is a central figure in this proceeding. He made 2 comprehensive witness statements and was cross-examined at length by senior counsel for the ACCC. His evidence addressed most of the major issues agitated in the proceeding. That evidence is dealt with when those particular issues are considered in these reasons for judgment. In view of his centrality to the operations of AMI and NRM and the scope of his evidence, it is timely to set out some background details concerning Dr Vaisman and some general observations about his evidence.
119 Dr Vaisman was born in 1945 in the Ukraine when it was part of the USSR. He qualified as a doctor of medicine in 1968 at the State University of Ukraine in Donetsk. He obtained a post-graduate qualification in obstetrics and gynaecology from that university in about 1974. In his examination in response to the ACCC’s notice to him under s 155 of the TPA, he said that this qualification was regarded by Australian authorities as equivalent to a PhD in Australia [ACCC 4.398]. He signed welcome letters to patients as Dr Jack Vaisman, PhD Medical Science. In 1975 he was appointed an Associate Professor of obstetrics and gynaecology at the same university. Later he was appointed head of the gynaecology department at the State University of Advanced Medical Training in Moldova. He applied for an exit visa in about 1974. He was regarded as a dissident and was imprisoned for 6 years as a result. He said that in 1989 he was among those allowed to leave the USSR following an intervention of Prime Minister Hawke with President Gorbachev.
120 In Australia, Dr Vaisman spent four years working and learning English. He wanted to undertake examinations at a university in Australia so that his medical qualifications would be recognised. However, financial pressures and the illnesses of his wife and daughter prevented this. In 1993 he opened his first male sexual dysfunction clinic and has operated the business since then.
121 Dr Vaisman’s personal circumstances have been challenging in major respects. He has an adult daughter who has advanced multiple sclerosis. She is confined to a wheelchair or to bed and depends on Dr Vaisman for daily attention. She requires regular intensive medical treatment. At one point in the course of the hearing Dr Vaisman was absent because he was required to take his daughter to hospital for such treatment. Although the proceeding was filed in Melbourne, much of the hearing took place in Sydney. That was the result of an application by Dr Vaisman, who lives in Sydney, supported by an affidavit sworn by his solicitor explaining that Dr Vaisman’s wife suffers from chronic depression and that he is her primary carer. She is often confined to bed as a result of her condition. Dr Vaisman must care for both his wife and daughter and his two grandchildren.
122 Dr Vaisman has himself had health issues. He has Type 2 Diabetes. Then, in January 2013 he was admitted to the Prince of Wales Hospital suffering from pneumonia. In evidence he said that since that time he has experienced memory problems. He said that there were some investigations under way to determine whether he might have suffered a small stroke. No evidence of the outcome of those investigations was provided to the Court.
123 There were times when Dr Vaisman’s evidence was confused and his memory was obviously faulty. It would not be surprising if these features could be explained by his health issues and also by the attention he needed to give to the medical conditions of his wife and daughter. However the difficulties with his evidence went deeper than those matters would explain. For instance, on major issues of medical science, which are examined later in these reasons for judgment, Dr Vaisman insisted that his views were supported by scientific publications produced by him. In fact, those publications simply did not support his views. Then, there were instances of internal inconsistences in his evidence and attempts to explain the inconsistences in a way which lacked credibility. Finally, there were occasions when Dr Vaisman tailored his evidence to suit his purposes in the litigation. This was especially apparent when he said that the prescribing practices of doctors were entirely the result of independent clinical decisions made by doctors, when in fact those practices were largely governed by the dictates of Dr Vaisman. Even allowing for the pressures on Dr Vaisman from the exigencies of his life, his evidence was largely unreliable and, on significant issues, untruthful. Whatever effect his health and other circumstances had on him, they did not dull his strong sense of self-interest.
4.5 The conduct alleged against AMI
4.5.1 Advertising medical treatment
124 AMI advertised its business in newspapers, in magazines, on television, on radio, online on its website, on YouTube, and on shopping dockets.
125 The advertising was extensive. In the 2008 and 2009 financial years, AMI spent $19.87 million and $29.9 million on advertising respectively. That expenditure amounted to about 35 per cent of its revenue.
126 Dilip Kumar Shrestha, the Chief Financial Officer of AMI, said in cross-examination that Dr Vaisman was responsible for the content of advertisements placed by AMI [TS 1935]. Dr Vaisman said that he made the decisions about whether the advertising which had been placed by AMI was effective to attract patients, [TS 1690] and that to increase the number of calls made to AMI he would increase the amount of advertising [TS 1625–1626]. This was supported, for instance, by advice from AMI’s advertising agent in November 2009 that advertising in the Sunday Telegraph produced an immediate increase in the number of calls to AMI [ACCC 4.393].
127 The advertising was effective in the case of the eight AMI patients who made statements relied on by the ACCC. In each case they said that they contacted AMI as a result of advertisements. Most heard about AMI through radio advertisements, but some also through television advertisements and billboards.
128 A typical example of the content of the many advertisements can been seen from the following newspaper advertisement placed in the New South Wales Suburban Press in January 2008:
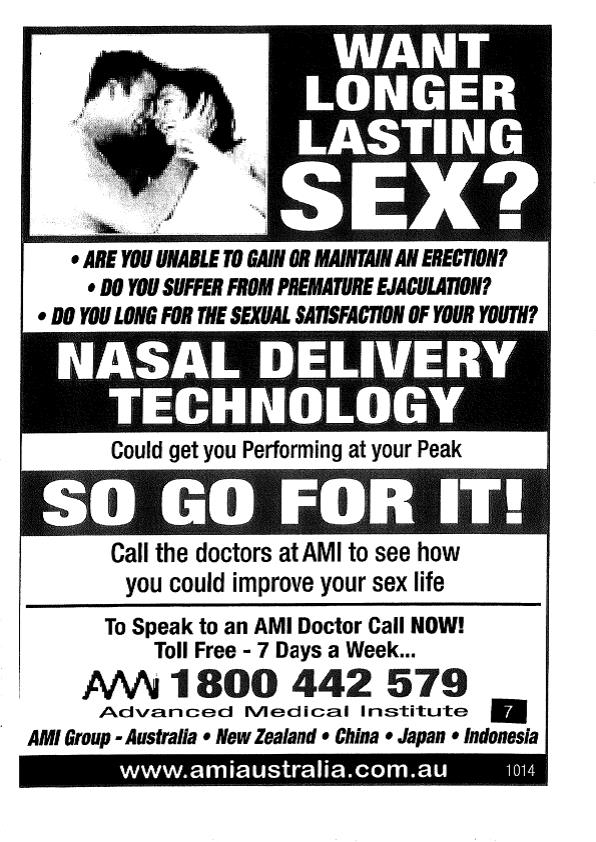
[Annexure A to the FASOC, p 7]
129 Another example is the newspaper advertisement placed in the Adelaide Advertiser in February 2009:

130 There were two predominant themes in AMI advertising. One was that the treatment was by a nasal spray delivery technology. The other was that the treatment was provided by doctors. The second advertisement emphasised the anxiety and lack of confidence associated with sexual dysfunction. The name Advanced Medical Institute conveyed the message that the treatment was based on scientific medical knowledge.
131 Evidence from the AMI patients showed that they responded to these themes. For instance, patient 40 said:
Prior to calling AMI it was my expectation from their ads that I would see one of their doctors about my problems.
[ACCC 1.7, [10]]
132 Patient 30 said:
In about late March 2008 I was driving a vehicle at work and listening to the radio when I heard an ad for a treatment for premature ejaculation. I recall I had heard the ad or similar ads many times before. The ad claimed that a business called AMI had a nasal spray treatment for premature ejaculation. I recall the ad included phrases to the effect of 'want longer lasting sex?' and 'up your nose and away it goes' and I recall that the ad claimed that all it took was a phone call. I understood this to mean that I would not have to attend at a medical clinic and meet with a doctor in person but rather that it could all be done over the phone.
[ACCC 1.3, [7]]
133 In respect of the 145 consultations with AMI patients evidenced by the recordings, it should be inferred that the patients generally contacted AMI as a result of advertising by AMI, and responded to the messages that treatment was by nasal spray, was by doctors committed to their welfare in accordance with accepted standards of medical practice, and had a scientific foundation.
4.5.2 The conduct of AMI salespeople
134 The ACCC alleged that features of the conduct of the salespeople, in relation to their contact with Annexure B patients, were unconscionable. It was alleged that the salespeople were:
put forward by AMI as a part of medical consultation during which they proffered medical views when they had no medical training;
trained by AMI to and did conceal from patients that they were paid on commission, so that the longer the contract term the more commission they earned;
trained by AMI and used high-pressure selling techniques designed to exploit the shame, embarrassment, guilt and inadequacy which AMI believed patients felt about suffering from ED or PE;
trained by AMI to and did persuade patients to enter into long-term treatment contracts when there was no proper medical basis for the length of the medical treatment offered; and
trained by AMI to and did tell patients that they would be entitled to a refund if they were not satisfied with the treatment without disclosing that, in order to obtain a refund, patients were required to try all of the treatment methods offered by AMI including intracavernosal injections into the base of the penis.
135 In each instance the ACCC said that the interests of patients were subordinated to the commercial interests of AMI.
4.5.2.2 Unqualified salespeople presenting as medically qualified
136 A patient who contacted AMI was channelled through a process which first required the patient to speak to a salesperson. In almost all of the 145 recorded consultations, the salespeople introduced themselves by name and then described their role as “clinical coordinators”. One salesperson, Hanspeter, sometimes described himself as a doctor’s assistant. This introduction was often followed by the explanation that their role was to assist the doctors or work with the doctors. The salesperson then usually asked about the problem which the patient was experiencing. In the course of the ensuing conversation, the salesperson often responded by offering a medical opinion. That process can be seen in the following exchanges with patients.
137 The exchange between patient 27 and salesperson Lori was as follows:
LORI: Okay, great. Now, [Patient], what is your main concern? I just need to gather some brief information, firstly.
PATIENT: Oh, it’s just lasting longer, because it’s like a premature thing. I’ve never – it’s just sort of all of a sudden – it’s been going on for probably, probably four or five months, right - - -
LORI: Mm.
PATIENT: - - - it was – but I had another – it happened to me one time before too, but then it, sort of, like, it went away. It didn’t go away for a long time, but then it come back again.
LORI: Okay, yeah, look, [Patient] that’s what happens. Premature ejaculation: it is a psychological impotence, and what happens, because it’s an enforcement of a bad habit it may be there on and off - - -
PATIENT: Yeah.
LORI: - - - but it’s going to get progressively worse unless you do something about it…
[Emphasis added.]
[ACCC 4.260, p 3]
138 The exchange with patient 32 was as follows:
BRIAN: All right. Now a lot of men are in the dark, so I just have to give you a few facts, okay?
PATIENT: Yeah.
BRIAN: Roughly 20 per cent of all men have premature ejaculation, which means after they penetrate they’re five or 10 minutes or under most times. Okay?
PATIENT: Yeah.
BRIAN: The other 80 per cent of men don’t have the problem. They can penetrate, thrust, go 20, 30 minutes, 40. No matter how good it feels, they can ejaculate when it suits them. All right?
PATIENT: Yeah.
BRIAN: That’s what you want. Have you had that control at all or not?
PATIENT: Not really.
BRIAN: Okay. We need to sort that out. Are you on any medicines at all?
PATIENT: No.
[ACCC 4.269, pp 2-3]
139 The exchange with patient 111 included the following:
IGOR: But you can still sometimes get a good, strong 100 per cent [erection]?
PATIENT: Oh, yeah. Yeah.
IGOR: That’s a very good sign. Okay. It is quite common, [Patient], for men who basically have been out of action for some time to develop erectile dysfunction, especially once you’re over 50.
PATIENT: Okay, yeah.
IGOR: It’s quite common, because your body starts to go into a decline, stuff going backwards, rather than forwards and your blood vessels - - -
PATIENT: So the theory of use it or lose it is quite correct?
IGOR: That's correct.
PATIENT: Okay.
IGOR: Basically your blood vessels start to atrophy or lose elasticity and start hardening up and the same, you know, like the rest of your body.
PATIENT: Yeah.
IGOR: That’s why we start getting wrinkles and all that and the same with the blood vessels in the penis.
PATIENT: Sure, yeah.
IGOR: It’s a natural aging process basically, but when you don’t use it, it starts happening a lot quicker - - -
PATIENT: Okay, yeah.
IGOR: - - - than what it normally would. So it is quite straightforward to get this problem treated, just a matter of exercising sort of thing over period of time - - -
PATIENT: Okay, yeah.
IGOR: - - - until you get to the point where - - -
PATIENT: Is it a confidence thing? Is it anything to do with confidence?
IGOR: Well, it’s a combination of things. It’s a combination of physical, as well as psychological.
PATIENT: Yeah, because that’s sort of the way I - you know, I feel awkward in
those situations now when you sort of - - -
IGOR: Of course.
PATIENT: Yeah.
IGOR: The more you worry about your performance, the more things go wrong.
PATIENT: Exactly, yeah.
IGOR: But the fact that most of the time you aren’t getting the - the automatic erections are around the same strength shows that there is some physical decline as well.
PATIENT: Okay.
IGOR: Which can make the problem even worse when you do have trouble.
PATIENT: Yeah. Yep.
IGOR: So, you know, when you’re sort of worrying about your performance, things go wrong and, when things go wrong, you worry about your performance.
PATIENT: Oh, that's right, yeah …..
IGOR: So it’s quite straightforward. Yeah, it is quite easy to treat this problem. It’s just a matter of sticking - you know, treating it over a period of time, getting yourself back to normal and then you should be right by yourself. Quite important though, after, you know, the treatment is completed, to keep yourself active regardless.
PATIENT: Yeah. Yeah, sure.
IGOR: You know, either with sex or at least masturbation because - - -
PATIENT: Yeah. Okay.
IGOR: - - - firstly, they say that - they’ve found that if you ejaculate regularly it cuts the chance of developing prostate cancer, about 50 per cent, so it’s quite important.
PATIENT: Oh, okay.
IGOR: Things like that.
PATIENT: Okay. I didn’t know that. I wasn’t aware of that.
IGOR: What I’ll do is basically - - -
PATIENT: That’s very important.
IGOR: It is very important because, well, all around it’s important.
PATIENT: It is.
IGOR: It gets your endorphins going and, you know, gets the blood flowing, gets everything working properly, gets the heart pumping, you know.
PATIENT: Yeah. Yeah. No, that's right. Oh, yeah, you just sort of lose the plot sometimes and, you know, as I say, I throw myself into work and, yeah, you know, just got completely out of the scene of meeting people and, yeah, that’s what happens.
IGOR: It is quite common, you know, and it is quite easy to treat, just a matter of time, just basically getting you to the point where you are getting consistently good, strong erections, so you’re over the psychological aspect and, with regular intercourse, basically your - the blood vessels become elastic again.
PATIENT: Okay, yeah. Yeah.
IGOR: So in fact, as you get older, you need to keep yourself more active than when you were younger, if you want everything to work well.
PATIENT: Oh, okay, yeah. Yeah.
[Emphasis added.]
[ACCC 4.340, pp 4-6]
140 Although the descriptions of their title and role used by the salespeople and the nature of their exchanges with the patients gave an impression that they had some medical knowledge to contribute to the consultation, in fact they were salespeople paid on commission with no medical training. Their remuneration did not depend on any exercise of medical expertise, but on the amount of, and method of payment for, the contract made between AMI and the patient.
4.5.2.3 Failure of salespeople to disclose their remuneration by commission
141 The salespeople were paid on a commission basis. They received higher commission for upfront payments by patients. They were generally paid seven per cent commission on daily totals of upfront payments of up to $10,000, 10 per cent for daily totals between $10,000 and $15,000, and 15 percent on daily totals of $15,000 or more. Where the patient paid by direct debit, the rate of commission was 6 per cent. If a contract was later cancelled and part of the price refunded to the patient, the commission previously paid to the salesperson was deducted from later earnings.
142 In none of the 145 recordings were the patients told that the clinical coordinators or doctors’ assistants were salespeople paid on commission. The respondents called Ms Maria Gabriel who was as salesperson for AMI. She confirmed that she did not tell patients that she was paid commission by AMI. She identified the document from AMI entitled “Instructions to Clinical Coordinators – Male Sexual Dysfunction” which included the following:
OBJECTION
A RELATED OBJECTION TO YOUR BEING PUSHY MAY BE AN ENQUIRY AS TO WHETHER YOU ARE ON A COMMISSION
If this question arises you should respond by advising the enquirer that as with most working Australians your income is based on results (without going into further details) but that your greatest reward is having a satisfied patient of AMI.
[ACCC 4.9, pp 8 -9]
4.5.2.4 High-Pressure sales techniques used by salespeople
143 In this section, these reasons for judgment first explain the source of the training provided to salespeople by AMI, and then how the sales techniques were designed to target the vulnerability of men who phoned AMI.
144 Then, the reasons for judgment examine the high-pressure sales techniques used by salespeople, namely, by emphasising the adverse consequences of the failure to agree to treatment, by making statements about the efficacy of the AMI medications and offering a cure for the conditions, by downplaying the side effects of the AMI medications, and by exaggerating the dangers of alternative medications not available through AMI.
4.5.2.4.2 The sales scripts and materials
145 The approach which salespeople should take in the consultations was set out in sales scripts and materials developed by Dr Vaisman, at times with input from external consultants. Mr Shrestha also met with Dr Vaisman in discussions about the development of the materials.
146 Numerous sales scripts were tendered and received in evidence, including those entitled, “Instructions to Clinical Co-ordinators – Male Sexual Dysfunction” (Instructions to Clinical Coordinators), “Comprehensive Treatment Program for Clinical Coordinator”, “Suggested Brainstorm in Patients Mind After Hearing Quotation on the Cost of the Treatment and How to Prevent Arising Objections” (Suggested Brainstorm), and “Four Pillars of AMI”. The document “Think Like a Patient” (Think Like a Patient) [ACCC 4.409.1 and ACCC 4.555] was the basis of a lecture given by Dr Vaisman to the salespeople in February 2008.
147 In final written submissions, the respondents contended that all but one of the sales scripts and materials were not particularised in the pleadings and could not be relied upon by the ACCC. However, this is to confuse the function of evidence and pleadings. In any case, most had been particularised. The pleadings were elaborate in the detail in which the critical representations were forecast to the respondents. For example, extracts from seven of the sales scripts and materials were set out verbatim in the FASOC. Then, in further and better particulars filed by the ACCC on 14 December 2011, the ACCC detailed over 40 sales scripts and materials on which it intended to rely. A copy of each had previously been provided to the respondents.
148 Mr Shrestha was in charge of the supervision and training of salespeople. When a new script was finalised he would disseminate it to the sales staff and conduct group training sessions and also regular one-on-one meetings to explain the use of the scripts. Dr Vaisman attended some of the training sessions.
149 Dr Vaisman also conducted sales conferences and lectures for the sales staff.
150 Dr Vaisman said in in cross-examination that some of the sales scripts and materials were not distributed to the salespeople. He also said that he had drafted the scripts from literature, that some of the statements were excerpts from that literature and not his own words, and that he agreed or had previously agreed with some of the statements but not others. However, it is not necessary to find whether each of the sales scripts was provided to the salespeople. On the balance of probabilities, some materials covering the sales ideas expressed by Dr Vaisman were provided to the salespeople, even if some of the particular materials relied upon by the ACCC were not. And Dr Vaisman acknowledged that he and Mr Shrestha had encouraged the salespeople to use the ideas found in the scripts as part of their sales routine. He also acknowledged that he had presented to the salespeople on the topics addressed in the materials.
151 Dr Vaisman and Mr Shrestha intended the salespeople to use the scripts and the training material in their interactions with patients. Dr Vaisman said that Mr Shrestha “hammered” the staff to stick to the scripts. That occurred in sales meetings held every month or six weeks. Dr Vaisman attended some of those meetings and told sales staff that if they did not stick to the scripts they could lose their jobs [TS 1638]. Dr Vaisman said that no salesperson actually lost their job for not sticking to the scripts, but that what he said was a way of putting pressure on them to do so [TS 1639].
152 That Dr Vaisman and Mr Shrestha were successful in training salespeople was evident in the recordings of the Annexure B consultations. The ideas, if not the words, which the salespeople were instructed to impart appear in virtually all cases.
153 The ACCC prepared attachment 6 to its final written submissions which tabulated the occurrence of certain phrases taken from specified training materials in the interactions between salespeople and patients as follows:
1. “untreated PE can lead to psychological impotence” was used in 34 consultations;
2. “untreated PE/ED can (lead to) shrinkage of the penis” was used in 11 consultations;
3. “use it or lose it” was used in four consultations;
4. “prevention of prostate cancer with frequent ejaculating” was used in seven consultations;
5. “men who have regular sex are 50% less likely to have a heart attack or stroke” was used in three consultations;
6. “… a significant number of our patients, who commit to a 12 month program, do not require ongoing treatment at the end of their program” was used in 35 consultations;
7. “our programs have been specifically designed to be undertaken over a standard 12 months period with the objective of having a patient complete the program, sexually rehabilitated, and without the need for ongoing program” was used in 61 consultations;
8. “benefit includes return of sexual confidence” was used in 25 consultations;
9. “a benefit includes to be able (most likely) in the end of the treatment program to perform (to control ejaculation in PE case) without medications” was used in 12 consultations;
10. “PE becomes a habit and that in order to break this habit the brain needs to be retrained” was used in 24 consultations;
11. “having treated some 500,000 patients with sexual dysfunction concerns over the last 16 years, you can be confident of AMI’s substantial experience and understanding of this complex area” was used in 46 consultations;
12. “we are receiving more than [x] inquiries per day/week from men Australia wide” was used in 29 consultations;
13. “you are not alone” was used in 27 consultations;
14. “most of our patients get excellent results from the start” was used in three consultations; and
15. “it costs 2 cups of coffee per day, can you afford 2 cups of coffee per day?” was used in three consultations.
154 In a corresponding schedule, the respondents sought to qualify the effect of that analysis, in particular, by adding information to show whether the patient in question proceeded to a purchase, sought a refund, or was given a refund.
155 These factors, however, do not detract from the force of the ACCC’s point, namely, that the training provided by AMI was translated into practice by the salespeople. The evidence established that the training given by Dr Vaisman and Mr Shrestha to salespeople in the techniques of selling were taken up and used by the salespeople.
4.5.2.4.3 Targeting vulnerability
156 In February 2008, Dr Vaisman conducted a sales conference which was attended by salespeople including seven salespeople who, between them, dealt with 120 of the Annexure B patients. Dr Vaisman set out his technique in Think Like a Patient, on which he based a lecture he gave to the salespeople. He explained the way he saw the state of a patient who rang AMI as follows:
He is frustrated, ashamed, dissatisfied, distressed and anxious about sex and decreased sexual self confidence. He is anxious with interruption of intimacy (which often results from his or her reaction to the short latency of sex. This anxiety subsequently affects the quality of both the sexual and nonsexual relationship.
[ACCC 4.555, p 3]
157 In an accompanying Power Point presentation “ABC of Sales – Think Like a Patient” (the Power Point presentation), the matter was emphasised where the state of a patient phoning AMI was described as:
Frustrated, ashamed, dissatisfied, distressed and anxious and decreased sexual self confidence.
[ACCC 4.403, p 3]
158 Dr Vaisman called this state, State A of the “ABC of Selling”. In cross-examination Dr Vaisman confirmed that the presentation reflected his own views and that their source was “taken from the books” [TS 1841]. A summary of the “ABC of Selling” was found on the wall of the office of Hanspeter, one of the salespeople. Under the heading “ABC” the following appeared:
A B C
A STAGE
WHERE ARE YOU NOW?
C RESULTS
WHERE YOU WANT TO BE?
B TREATMENT PROCESS
(AT LEAST 4 TREATMENT OPTIONS)
[ACCC 4.37]
159 Dr Vaisman admitted in cross-examination that he had written a number of times about the fact that men coming to AMI for treatment were likely to have low self-esteem and that that was his view. The following exchange occurred in cross-examination:
MR BURNSIDE: It’s something that you’ve written a number of times, isn’t it?
DR VAISMAN: Yes. I know that people may have low self esteem. So what.
MR BURNSIDE: Yes?
DR VAISMAN: Yes. They are talking to the doctor.
MR BURNSIDE: May have or likely to?
DR VAISMAN: Maybe. I don’t know. The – the literature says sometimes yes.
MR BURNSIDE: Yes. It’s your view, isn’t it, that they are likely to have low self esteem and likely to be anxious?
DR VAISMAN: Yes.
[TS 1755]
160 And Dr Vaisman said the following about the views expressed in the document Think Like a Patient:
MR BURNSIDE: “When a man rings us” – do you see that?
DR VAISMAN: Yes.
MR BURNSIDE: He is then so-called state A.
His current state (he has a problem with getting or maintaining an erection, or suffers from premature ejaculation. He is frustrated, ashamed, dissatisfied, distressed and anxious about sex and decreased self-confidence. He is anxious with interruption of intimacy).?
DR VAISMAN: Yes
MR BURNSIDE: Those were all views which you held when you sent that document, weren’t they?
DR VAISMAN: It’s all taken from the books. Yes, if you want my opinion. Yes.
MR BURNSIDE: Those were views you held?
DR VAISMAN: Yes.
MR BURNSIDE: About the nature of the people who rang with male sexual dysfunction?
DR VAISMAN: Yes.
[TS 1840 – 1841]
161 At other times he denied that this was his view and said that by ringing AMI men had overcome their shame or embarrassment as soon as they rang, or that the men who were ashamed and embarrassed did not ring AMI at all [TS 1831]. His scripts and materials for salespeople, in particular Think Like a Patient, established that his actual view was that patients were vulnerable. Where he sought to resile from that view, his evidence was contrived to advance his case in this proceeding, but did not reflect his view or the reality.
162 Some patients told the salesperson or the doctor that they experienced a lack of confidence. For example, patient 60 stated in his interaction with salesperson Csaba that, “[I] [d]efinitely don’t have much confidence at the moment.” [ACCC 4.312, p 4]
163 Ms Gabriel said that she would have read through the document Instructions to Clinical Coordinators. It included the following assessment of the mindset of patients:
PSYCHOLOGICAL OBJECTION – CHANGING THE MINDSET OF THE PATIENT WHO MAY WELL FEEL NOT WORTHY OF THE PROGRAMME.
Fundamental to your dealings with objections must be an understanding of the psychology of a man calling us in the first place with a PE or ED problem.
Given the nature of this condition such a man would be likely to have quite low self esteem.
His inability to perform sexually whether as a result of PE or ED, would over time, have had a profound emasculating impact on his male psyche or spirit.
In short he would feel less of a man and his low self worth as a consequence results in a lack of independence and decisiveness to make a decision that is rightfully his alone to make.
[ACCC 4.9, p 6]
164 The circumstances at a sales lecture given by Dr Vaisman on 7 January 2010 are particularly revealing. The purpose of the event was for Dr Vaisman to get the salespeople to change their approach. He regarded the practice which had developed as wasting selling time with issues which would be addressed by the doctors in any event, and that it was of concern that some salespeople were presenting to the patients as doctors Dr Vaisman said:
That’s why today – the role what we are going to do today is to come to the new level of the sales technique. I don’t want you sell the medication. Absolutely not. So, number one, stop taking details history. Okay. You can ask, “How long the problem?” and that’s it. “What kind of medications?” and all other things which doctor ask him – doctor – doctors tell me that very often when they start to ask the history of the patient, patient tell, “Listen, I just told all this thing to another doctor. What is going on?” Very unhappy. And when he says, “No. It wasn’t a doctor. It was a clinical coordinator,” people confuse. So, please – please – please, stop taking details history. Please – please stop about what kind of medications you are using. It doesn’t help you to – to sell – a different technique to sell.
[Emphasis added.]
[ACCC 4.415, pp 2-3]
165 In the January 2010 lecture Dr Vaisman circulated to the salespeople a document outlining the new approach. It was probably the Suggested Brainstorm script found by the ACCC in Dr Vaisman’s office [ACCC 4.27]. Dr Vaisman said he most likely worked from the document during the lecture [TS 1777]. The document included a series of questions which the salespeople were to ask as follows:
…
Do you experience?
(3) Sexual Dissatisfaction [ ] Yes [ ] No
(4) Anxiety [ ] Yes [ ] No
(5) Lack of Self-Confidence [ ] Yes [ ] No
(6) Diminished Quality of Life [ ] Yes [ ] No
(7) Relationship Tension [ ] Yes [ ] No
(8) Sexual Relationship Tension [ ] Yes [ ] No
(9) Some Sort of Guilt [ ] Yes [ ] No
[ACCC 4.27, p 1]
166 Following the introduction to the lecture, Dr Vaisman engaged in role plays which were designed to demonstrate to the salespeople how the questions should be asked in a way which encouraged patients to answer them. Dr Vaisman explained to the salespeople:
MR VAISMAN: And by the – and by the way, all these questions will be on computer which you really have to tick - - -
MR ..........: Okay.
MR VAISMAN: - - - and doctor really will see all these questions what you tick. It really – it will help him in social analysis of the mentality of the patients.
[ACCC 4.415.1, p 7]
167 Dr Vaisman explained the reason for asking patients about their psychological state as follows:
Why these questions I want? We know in seven minutes it won’t happen. Why I’m telling seven minutes, only for one reason. If you start to talk, “You have to use this medication with sex, without sex. Medication will be delivered to your door,” and all this, it’s not so important. He doesn’t want to hear this one.
…
It’s not what the question which will help him to make the decision to buy or not to buy. You have to talk only about psychological introduction to him such a way that he really have – will help make the decision to – to buy. With asking medication to the door and all these things, believe me, it won’t help him - - -
…
--- to make this decision.
…
But I want you change because it’s – believe me – it won’t help to sell. Be delivered to the – to the door and all other things.
[Emphasis added.]
[ACCC 4.415.1, pp 8-9]
168 An audio recording of this sales lecture is in evidence. What it reveals, which is not evident from the transcript of the lecture, is the force of delivery given by Dr Vaisman and the intense response which he drew from the salespeople.
169 Dr Andrew David Pattison, a general practitioner with a particular interest and experience in the area of sexual dysfunction was called as a witness for the ACCC. He shared the view of AMI and Dr Vaisman about the feelings of men suffering sexual dysfunction. In a report dated 15 November 2011 [ACCC 3.29] (Pattison Report 2), Dr Pattison stated “patients who present with sexual dysfunction problems such as ED and PE are frequently very embarrassed and lacking in self-esteem. They are often willing to try any treatment that might alleviate their problem.” [ACCC 3.29, p 303]
170 The evidence established that patients phoning AMI for treatment of ED or PE were likely to feel embarrassed and lack self-confidence as a result of their condition. The evidence also established that AMI was aware of this and tailored its sales techniques to take advantage of these feelings in order to make sales.
4.5.2.4.4 Emphasising adverse medical and social consequences of failing to treat
171 In many of the Annexure B patient’s interactions with salespeople, the salespeople emphasised adverse medical and social consequences which they said the patient would suffer without AMI’s treatments and medications. This technique followed the instructions and scripts given to salespeople by AMI.
172 For instance, the Power Point presentation found in the office of Hanspeter included the following:
SEX IS NOT JUST FOR ENJOYMENT OR FUN – IT’S A BIG HEALTH ISSUE – LET ME EXPLAIN TO YOU WHY:
E.D.
50% LESS CHANCE TO HAVE HEART ATTACK AND STROKE
LESS CHANCE TO DEVELOP PROSTATE CANCER
MEN WHO HAVE SEX AFTER 60 LIVE 10 YEARS LONGER
30% OF MEN WITH E.D. PARTNERS SUFFER FROM DEPRESSION
P.E.
POSSIBILITY OF BECOMING IMPOTENT AND SUFFER SHRINKAGE OF THE PENIS
[ACCC 4.37]
173 This reflected the Power Point of the “ABC of Sales – Think like a Patient” that stated:
What is the consequences fir [sic] staying at the point “A” (Penile shrinkage, heart attack, stroke, wife’s depression)
[ACCC 4.403, p 6]
174 A longer version of the “ABC of Sales” instructed the sales staff as follows:
Expand and repeat the benefits he will receive and the emotional relief you’ll provide.
…
2. To remove by 50% chance of developing heart attack or stroke.
3. If not increase than at least not to lose the size of the penis.
4. To remove the possibility to develop psychological impotence (PE patient).
[ACCC 4.51, p 3]
175 In the Instructions to Clinical Coordinators script, the same message was conveyed in the context of the salesperson seeking to overcome the patient’s objection that the patient needed to talk to his partner:
Never forget the serious potential flow on effects from untreated PE (possible psychological impotence, shrinkage of the penis – “use it or lose it” and continued low self esteem/diminished quality of life) OR for untreated ED (i.e. men who are not sexually active) (50% less change of a heart attack or stroke, your partner has less change of developing depression, as a result of your ED (30% of partners of men with ED develop depression), shrinkage of the penis – “use it or lose it” and continued low self esteem/diminished quality of life.)
[Emphasis in original.]
[ACCC 4.9, p 9]
176 The ACCC relied upon interactions between 137 Annexure B patients and salespeople to support the claim that salespeople told patients of adverse consequences which would follow if patients did not take the treatment.
177 A number of the interactions relied on amounted to no more than ordinary sales chatter which did not rise to a level to be relevant to a consideration of unconscionable conduct whether alone or in combination with other parts of the interaction. A typical example is a passage relied on by the ACCC in the interaction between patient 141 and salesperson Gary as follows:
GARY: … And are you in a relationship or single, what’s the story there?
PATIENT: I’m single.
GARY: Single, okay. So, yeah, quite important then to obviously last longer. Once you get them on the hook you want them to stay there, buddy.
PATIENT: Yes.
GARY: And have a lot more fun. That’s all right. Excellent.
[ACCC 3.306, pp 2–3]
178 An examination of the transcripts of the interactions with the 152 AMI patients disclosed that about 74 interactions exhibited circumstances in which the salesperson spoke of adverse medical consequences flowing from not taking the treatment which might be of sufficient seriousness to be relevant to a case of unconscionable conduct. These include patients 2, 3, 4, 6, 7, 10, 11, 17, 22, 23, 27, 28, 31, 32, 35, 38, 43, 44, 45, 47, 49, 52, 54, 57, 58, 59, 61, 62, 64, 69, 72, 74, 83, 88, 91, 94, 97, 98, 107, 108, 111, 113, 116, 121, 123, 124, 125, 127, 128, 131, 136, 140, 141, 145, 150, 154, 156.
179 The adverse medical consequences mentioned in many of these interactions included psychological impotence. A typical example was the interaction between the salesperson Hanspeter and patient 64 which included the following:
HANS: So it could be – see premature ejaculation is – first of all, you’re very young; we have patients up to 109 years, okay, and premature ejaculation is a condition. There’s a lot of people have the same problem, at least 20 to 30 per cent from all the male population, okay. That means you can’t control the ejaculation so you come very quickly, okay.
PATIENT: Yeah.
HANS: If that’s the case over years, if it’s not sorted out, it turns into impotence. That means you can’t get an erection any more.
PATIENT: Oh, okay.
HANS: But that does not happen straight away; that takes years. What will happen is - what you get first is the erections sometimes are not so strong any more. Yeah, so that’s what you’ve got, a bit of ED, okay.
PATIENT: Okay, yeah.
HANS: But the main problem, what you call this premature because if you can last longer, that means if you can pump away for 15, 20 minutes, the erection will be rock hard, because it’s like running a choke for so long; your muscles get really hard, yeah.
PATIENT: Yeah, sure.
HANS: So when we sort it out, most of the time the other problem will be gone anyway.
PATIENT: Oh, okay, yeah.
…
HANS: And we measure things like that. This generation - the last 10, 15 years has been much better because when you go in the gym, for instance, okay, and we look at these old guys in the sauna with their little willies, it’s not because they have a little willy, it’s just they didn’t fix a problem like that because that was always – they had this problem; it just hasn’t been treated before, okay. And when you don’t treat premature ejaculation – see, the penis is ..... The woman takes about 15 minutes to climax with penetration, okay. So if you penetrate her to make her climax, it takes about 10 to 15 minutes. That is normally how long you should control your ejaculation to, as a man, okay.
PATIENT: Yep.
HANS: If you don’t do that, then you short change yourself, obviously, with the woman, okay.
PATIENT: Yeah.
HANS: Now, this is like the – the penis is a muscle like every other. Now, if you don’t train it properly, it will start shrinking, because it doesn’t fill up with blood any more, and that’s why there’s little willies in the gym, because the arteries get hard; no blood gets in there, so the penis starts shrinking, yeah.
PATIENT: Yeah.
HANS: It’s exactly the same as blocked pipes. The reason why men don’t get so hard an erection any more as when they were younger is they haven’t treated premature ejaculation or it ends up with – what’s it called – psychologically impotence. When the arteries are hard, the blood can’t go into the penis. The penis is still the same size; it doesn’t fill up that much any more. And that way, it’s smaller, and that way, it doesn’t get hard any more, and it gets worse and worse, obviously, by the years, yeah. Does it all make sense?
PATIENT: Yeah.
[ACCC 4.317, pp 3–4, 13]
180 Each salesperson had an individual way of conveying that message. Thus, salesperson Brian told patient 59:
BRIAN: Long-term premature ejaculation does lead to impotence. A lot of young blokes don’t understand that but that’s what happens.
[ACCC 4.311, p 10]
181 And salesperson Vincent said to patient 145:
[Th]e – the longer you leave it the quicker it’s going to get, and if you keep leaving it, mate, it can lead to erection problems as well, besides the fact that, you know, you’re getting less and less sex, which means you’re getting less practice, so it’s going to start to compound itself and become a real problem, and certainly if you leave it, mate, you might end up having your penis stopping to work altogether. You don’t want that?
[ACCC 4.280, p 7]
182 Salesperson Lori told patient 94:
LORI: Yes. Look, that actually develops into an anxiety, you know, because you want to go the distance, but the more you think about it, the worse it actually gets.
PATIENT: Okay, that’s probably what it is then, because - - -
LORI: Yes. Look, it develops into what is called a “psychological impotence.”
PATIENT: Yes.
LORI: And you know, you put that anxiety on yourself, it – you know you’re not, perhaps, providing satisfaction for yourself, your partner. All these things play a part, and it’s a compounding effect. This problem, even though it may be there a short time, unless you treat it, premature ejaculation is something that isn’t just going to go away.
[ACCC 4.368, p 3]
183 There are examples of references to prostate cancer in the interactions between salespeople and patients, for instance, patients 31, 44, 57, 83, 111, 131. Salesperson Hanspeter said to patient 57:
HANS: The other thing is, the money is wise spent, that's for sure, because I don't know if you know, but if you have a good sex life, less likely to get a heart attack, less likely to get a stroke, and the most important thing is less likely to get prostate cancer which is in Australia the biggest killer in men.
PATIENT: Yeah. Yeah, that's for sure, yeah.
[ACCC 4.308, p 22]
184 There were also references by the salespeople to penis shrinkage. For example, salesperson Vincent said to patient 107:
VINCENT: Now when this problem is left untreated usually nothing changes or
there is chances of it getting worse and quicker over the years.
PATIENT: Okay.
VINCENT: Eventually when it’s left untreated altogether it can lead to erection
problems and shrinkage of the penis.
[ACCC 4.298, p 3]
185 There were references to heart attack or stroke, for instance, to patients 57, 83, 131. Salesperson Hanspeter told patient 83:
PATIENT: And it’s [the medication] not harmful to you?
HANS: No, no no. It’s good for you. Sex is good for you okay? The more sex you have, so - the better it will be for you in the long run to avoid prostate cancer, to avoid a stroke. To avoid a heart attack, you know?
PATIENT: Yeah.
HANS: It’s – when you only last a minute or two, that’s not long enough for all the blood to stay in the penis you see. The penis has to be like your legs or your hands, to be used all the time. And you using incorrectly, then obviously the arteries get hard. That also means that there’s more chance that there’s no blood pressure in there so that means you don’t get any erection anymore. So that’s why so many people with premature ejaculation, eventually it ends up in impotence. Yeah? So you losing your erection, yeah?
PATIENT: Okay, yep.
HANS: Makes sense, yeah?
PATIENT: Yep.
…
HANS: And you have full control of this, less likely to get prostate cancer, less likely to get a stroke. It’s a very small investment, it’s two cups of coffee a day.
PATIENT: Yep, and how much is it a month, sorry?
HANS: Sorry?
PATIENT: How much is it again, a month?
HANS: 198.
PATIENT: 198. Yep.
[ACCC 4.349, pp 9-10, 12]
186 In cross-examination Dr Vaisman conceded that treatment of ED does not reduce the risk of heart attack or stroke. The following exchange occurred:
MR BURNSIDE: And treating erectile dysfunction doesn’t alter the existence of cardiovascular disease, does it?
DR VAISMAN: Correct.
MR BURNSIDE: And so, whether or not a person has a heart attack as an associated condition is unrelated to whether or not they have the treatment?
DR VAISMAN: Correct.
MR BURNSIDE: Because the treatment is for erectile dysfunction?
DR VAISMAN: Correct.
MR BURNSIDE: Not for cardiovascular disease?
DR VAISMAN: Correct.
MR BURNSIDE: So that taking the treatment doesn’t reduce your chance of having a heart attack, does it?
DR VAISMAN: Correct.
MR BURNSIDE: And it doesn’t reduce your chance of having a stroke for the same reasons?
DR VAISMAN: Correct.
[TS 1753]
187 Patients were therefore given incorrect information when they were told by the salespeople that treatment would prevent stroke or heart attack. The salespeople were incorrectly trained when they were told by Dr Vaisman himself in the ABC of Sales and Instructions to Clinical Coordinators that they should tell patients that they would avoid heart attacks or strokes by taking the AMI medications.
188 Dr Vaisman was asked in cross-examination about his claim that failure to treat ED or PE would lead to shrinkage of the penis. The following exchange occurred in cross-examination:
MR BURNSIDE: And I suggest to you that there is no article which demonstrates that failing to take the treatment causes the penis to shrink.
…
DR VAISMAN: There is a scientific articles.
MR BURNSIDE: Yes?
DR VAISMAN: The three articles done by scientists and published in the International Journal of Impotence which says that people with – who suffer from impotence erectile dysfunction they have shorter penises, penises, yes. Absolutely prominent factor.
MR BURNSIDE: But the article doesn’t say that correcting erectile dysfunction causes the penis to grow longer and neither does it say that having, leaving it untreated causes the penis to shrink. They don’t say that, do they?
DR VAISMAN: I don’t understand. I don’t know. There is an article which says that people who stop to be sexually active is a signs of the penis shrinkage – shrinking. That’s what the scientific article says.
MR BURNSIDE: But again, it’s a matter of distinguishing between conditions that are associated and conditions that are causally connected, do you follow that?
DR VAISMAN: No.
MR BURNSIDE: Right. Do you know the difference between correlation and cause?
DR VAISMAN : Correlation, yes.
MR BURNSIDE: Yes?
DR VAISMAN: And cause, yes.
MR BURNSIDE: Right. So that if a person who is not sexually active is found on average to have a smaller penis, it does not mean that not being sexually active caused that?
DR VAISMAN: Absolutely. It says if person stopped to be sexually active, the size of the penis decrease. That’s exactly the conclusion of these articles.
[TS 1753 - 1754]
189 Then, the issue of penis shrinkage in patients with PE arose and the following exchange occurred:
MR BURNSIDE: But people who present with premature ejaculation are also told that they risk their penis shrinking if they don’t take the treatment, aren’t they?
DR VAISMAN: Absolutely wrong.
MR BURNSIDE: Pardon?
DR VAISMAN: Only for people with erectile dysfunction.
MR BURNSIDE: Okay. And you would agree that people who present with premature ejaculation should never be told that their penis will shrink if they don’t - - - ?
DR VAISMAN: Correct.
[TS 1757]
190 Dr Vaisman addressed the question of impotence as a consequence of failing to treat PE in the following exchange:
MR BURNSIDE: And they [men who suffer from PE] should never be told that they will become impotent if they don’t get the treatment?
DR VAISMAN: They – no, they can become impotent, that’s for sure.
MR BURNSIDE: They can become impotent from premature - - - ?
DR VAISMAN: Absolutely.
MR BURNSIDE: - - - ejaculation?
DR VAISMAN: Absolutely.
MR BURNSIDE: And have you got any article that suggests that?
DR VAISMAN: Yes, and I will explain why. It’s – coming the time when person – man understands he cannot satisfy the woman he try to avoid sex altogether and become psychological impotent.
MR BURNSIDE: So that’s psychological impotence, not actual impotence?
DR VAISMAN: What do you mean? It’s impotence, but psychological, he cannot get it up.
MR BURNSIDE: Yes. I want to suggest to you that the following annexure B patients who presented with PE were told of the risk of their penis shrinking. They’re Mr [B], Mr [B], Mr [C], Mr [C], Mr [L], Mr [M], Mr [O] and Mr [V]. So you would say that all of those people should not have been told of that risk, do you agree?
DR VAISMAN: You misunderstood.
MR BURNSIDE: Pardon?
DR VAISMAN: You misunderstood me. We explain to the patient untreated premature ejaculation can lead to psychological impotence, and as soon as he develops psychological impotence he can develop the shrinkage of the penis, correct.
MR BURNSIDE: So contrary to what you said a few minutes ago, it’s okay to tell them if they present with PE that their penis might shrink?
DR VAISMAN: Only in the context they will stop to be sexually active.
MR BURNSIDE: And you’re aware that the articles that talk about penis shrinkage say that even partial erections during sleep are sufficient to prevent any change in the size of the penis?
DR VAISMAN: No. Article says that the study of impotent men shows that the size of the penis decrease significantly.
MR BURNSIDE: I want to suggest to you that first of all that you do encourage the clinical coordinators to refer to the adverse effects of not using your treatments, do you agree with that?
DR VAISMAN: Yes, that’s their duty, to tell the consequences of not having treatment, continue to be impotent.
[TS 1757]
191 Dr Vaisman said that ED and PE robbed men of their confidence so that they avoided sexual intercourse. That process was described by Dr Vaisman as leading to “psychological impotence”. He claimed that psychological impotence had a physical consequence, namely, that there was shrinkage of the penis [TS 1757]. Dr Vaisman said that it was the responsibility of salespeople to tell patients of this consequence. He also agreed that he wanted the salespeople to use the suggestion of psychological impotence and shrinkage of the penis as part of their sales routine [TS 1750]. They did so.
192 The ACCC argued that the transcripts provided evidence that salespeople followed the training scripts produced by or for Dr Vaisman which made reference to psychological impotence and shrinkage of the penis as a consequence of ED and PE. The ACCC also argued that the information was medical information and should not have been imparted by salespeople. When the salespeople addressed medical issues, they gave an impression to patients that they had medical knowledge and that the advice was part of a professional medical program. In fact they were simply repeating information, of which they had no technical or expert understanding, designed to assist in the selling process.
193 When challenged about the correctness of the claim that ED and PE led to shrinkage of the penis, Dr Vaisman said there was an article about a study of impotent men that showed that “the size of the penis decreased significantly” [TS 1757]. In the course of final oral submissions, counsel for the respondents handed up a document to be read as part of the final written submissions which addressed scientific material relied on by the respondents generally (respondents’ additional reference to scientific evidence). In this document, the respondents referred to one article on this subject.
194 The article by Z. Awwad and others entitled, “Penile measurements in normal adult Jordanians and in patients with erectile dysfunction” (2005) 17 International Journal of Impotence Research 191, reported on a study which aimed to determine the penile size in an adult normal group of 271 and impotent group of 109 Jordanian men [R13.14, p 868]. The results of the study were aimed to assist patients in deciding whether to undertake penile lengthening procedures. The study of penile size was also thought to be possibly useful for the process of manufacturing condoms. In the normal group the mean flaccid length was 9.3 centimetres and in the impotent group the mean flaccid length was 7.7 centimetres. In the normal group the mean stretched length was 13.5 centimetres and the impotent group the mean stretched length was 11.6 centimetres.
195 The investigation undertaken by the study was to ascertain penile size. It was not designed to draw conclusions about the cause of any differences in size.
196 A number of speculative remarks were made about the cause of the difference in penile size between normal Jordanian men and Jordanian men suffering from erectile dysfunction. The respondents relied on part of a passage as follows:
The cause of impotence in our patients was mainly psychogenic, neurology, medication, and anxiety. Iacono et al reported the presence of structural disorders in the tunica albuginea of patients suffering from psychogenic, arteriogenic, and venogenic impotence with significant decrease in the elastic fibers in the tunica albuginea of impotent men compared to a control group. The decrease in length in impotent men in this study could be explained by the loss of elastic fibers, and the lack of intermittent stretching in the tunica albuginea, confirming the common saying (if you do not use it you lose it).
[Emphasis added.]
197 Immediately following that speculation was another potential reason for the difference in penile size, and that other reason was not related to continuing to engage in sexual intercourse. Rather it speculated that the cause could be related to the aging process as follows:
Organic impotence in aging men could be due to a venous leakage factor through veins that are situated normally on the distal third of the ventral penile surface. The impaired veno-occlusive function of the tunica albuginea is contributed to by the decrease in elastic fibers concentration found in impotent men.
198 This article, therefore, did not validate Dr Vaisman’s claim that by failing to treat ED or PE men will suffer shrinkage of the penis.
199 There were also instances of the salespeople emphasising that the patient would suffer adverse social consequences if he did not treat his ED or PE, such as that the patient’s partner may become depressed or that a patient would not satisfy his partner if he did not last longer. These exchanges played on the guilt and embarrassment of patients. For example, the following exchange occurred between salesperson Vincent and patient 28:
VINCENT: And you’ve had the problem almost the whole time you’ve been with this lady?
PATIENT: Yes. Yes.
VINCENT: Oh, no. I hope not many funny things go through her head. I mean, a lot of ladies who stay with men who have these sort of problems they get a bit depressed. They start to think maybe this guy doesn’t find me attractive anymore or, you know, or maybe he’s doing it with someone else, and things like that go through their head.
PATIENT: Yes.
VINCENT: Your wife, she’s not depressed?
PATIENT: She’s – it didn’t worry her for a while, but it’s starting to now, I think.
VINCENT: Yes.
PATIENT: Like she’s not all that interested in sex anyway.
VINCENT: Well, you know why that is, [Patient].
PATIENT: Yes.
VINCENT: Because of this problem. See men who have this problem – and they try to shy away from sex – the wife, after a while, maybe her libido goes down and they’re not going to want to have sex, mate.
PATIENT: Yes.
VINCENT: Because they don’t want to keep facing the disappointment every – imagine your wife – she tries to get it on with you, it doesn’t go hard and then, if it goes hard it goes soft again. It’s frustrating for them as well as you, [Patient].
…
VINCENT: The more – and your problem is the worse it gets, the more you think about it. The more you think about it, the worse it’s going to get, [Patient].
PATIENT: Yes.
VINCENT: And it doesn’t help the situation that your wife’s trying to avoid it. It’s going to really start to compound and, before you know it, mate, sex is going to stop. Is that what you want?
[ACCC 4.262, pp 5 – 7]
200 Salesperson Hanspeter said to patient 4:
HANS: Yeah. Have you got a girlfriend?
PATIENT: Yeah, I just started seeing a girl just not long ago.
HANS: That’s why you want to fix the problem?
PATIENT: Yeah, pretty much.
HANS: Smart move.
PATIENT: Yeah.
HANS: Smart move. It takes a woman about 10 to 15 minutes to penetrate, like plain, not like oral, just penetration, okay. It takes a woman about 10 to 15 minutes to climax, yeah.
PATIENT: After penetration?
HANS: No, just with penetration. Let’s say you just do intercourse with her, no oral sex, okay, no foreplay.
PATIENT: Yeah.
HANS: It will take her about 15 minutes to climax, so with one or two we are a bit shorter, aren’t we?
PATIENT: Yeah.
HANS: Yeah. So it’s good that you fix that problem, yeah?
PATIENT: Yeah, definitely.
HANS: Otherwise we don’t look very good and we don’t like that, do we? We want to look good.
PATIENT: No, it’s pretty embarrassing.
HANS: Yeah, and also you will never get the woman reacting. Like, you can never get out of her, like to really move, man, to how she really is because she can’t open up in that short time, you know. It’s just not possible, yeah?
[ACCC 4.231, pp 3 – 4]
201 And salesperson Csaba said to patient 100:
CSABA: Premature - you know, it's all about control.
PATIENT: Yes.
CSABA: Normal guys - they can control how long they last. They can just keep going on and on and on for 10, 15, 20 minutes or even longer. They decide when they ejaculate, yes.
PATIENT: Yes, yes.
CSABA: If it happens within few minutes, without you wanting to, it does happen prematurely, that's why it’s called premature ejaculation and so on.
PATIENT: Yes.
CSABA: Do you have a girl or are you married, [Patient]?
PATIENT: Yes, no, I'm married.
…
CSABA: Have you spoken to your missus about this at all?
PATIENT: Yes, yes look, it's a - yes, yes - yes, I have. It's - you know, we both sort of think that it would be good to do something about it, so here I am.
CSABA: Yes, no. It's much more fun for those guys who last, you know, 10-15 minutes or longer, as opposed to a few minutes only.
PATIENT: Yes.
CSABA: And that's how long it generally takes, you know, for a girl, for a woman, to get there and reach an orgasm, so important to keep her happy in the bedroom as well.
[ACCC 4.378, pp 3–4]
4.5.2.4.5 Statements about the efficacy of the AMI treatments
202 The training materials repeatedly instructed salespeople to tell patients that the treatment programs would cure their problems. Thus, in the Suggested Brainstorm script, salespeople were instructed to tell patients who asked why they needed a 12 to 18 month program that:
Our unpublished and international studies have confirmed that regular use of these medications during 12-18 months have a curative (rehabilitation) effect with the possibility by the end of this period to perform without medications.
[ACCC 4.27, p 2]
203 Most of the Annexure B patients were told by salespeople that the treatment would cure their problem or that the medication would be effective. Some examples include the following exchanges with patients.
204 Salesperson Hanspeter said to patient 57:
Yeah. We will, don't worry, you'll be fine. You'll be fine. Yeah. People up to 108/109 years, we treating. They have prostate cancer or their prostate cut out. That's worse than diabetic. They … anymore and we get them doing, so you'll be fine.
[ACCC 4.308, p 3]
205 Salesperson Kris told patient 135 who consulted for PE:
KRIS: Not a problem. All right, if – I mean, it’s not too late, [Patient]. If you started this medication last time you already fix your condition for good, permanently, but it’s never too late, isn’t it, right?
PATIENT: So this medication, does it actually – is it something that you need to then take for the rest of your life?
KRIS: No. That’s what I’m saying. If you started the medication last time, 2006, you already overcome your condition, [Patient].
PATIENT: Right.
KRIS: It’s like a retrain your body and brain, make sure you can come away from this medication after a certain period of time.
PATIENT: I see, yep.
KRIS: That’s why this is so popular, has been proven in the last 16 years, [Patient], but you could be one of them anyway. Well, it’s not too late. Okay. So let’s do it again, [Patient], okay?
…
And if you just keep, you know, practising over a period of time on a regular basis usually about 12, 18, 24 months later you don’t need it any more, [Patient].
[ACCC 4.323, pp 3 – 4]
206 And Salesperson Lori told patient 43:
LORI: We do find most of our patients start to notice some dramatic improvements in about two weeks. It’s a – it’s a medication that actually works better the more you use it.
PATIENT: Okay.
LORI: So week in week out you will find that you will last a little longer and longer each time.
PATIENT: Yep.
LORI: Because it delays ejaculation. So you’ll be able to penetrate, [Patient]. I have one of my colleagues here. He said to me, “You know, Lori, once you’ve gone in, no matter how good if feels, this medication helps you to hold back.”
PATIENT: Yeah. Right.
LORI: Even – you know – even when it does feel really good you’ll still be able to hold back. Okay.
PATIENT: Cool. Yeah.
LORI: Now, once you achieve these things, of course, your confidence is going to increase.
PATIENT: Yep.
LORI: Okay. So – which is all great ‘cause that will certainly – you know – make you go the distance…
…
LORI: You see, it’s quite simple. The short term goal – there’s a short term goal and there’s a long term goal. The short term goal is to bring you back to normal and the long term goal is to keep you there.
PATIENT: Yeah.
LORI: So that at the end of the treatment that’s it. You’re on your own and you won’t need to use medication anymore. Okay?
[ACCC 4.286, pp 12 – 13]
4.5.2.4.6 Downplaying side effects
207 Whilst the training materials instructed salespeople to tell patients that the medications had minimal side effects [see ACCC 4.403, p 9], in practice, information about side effects was conveyed to patients by the doctors. This is dealt with in [522] – [558] of these reasons for judgment.
4.5.2.4.7 Exaggerating dangers of alternative treatments
208 The training materials instructed salespeople to tell patients that other treatments for ED, namely, Viagra, Cialis, and Levitra, have common side effects of flushing, headache and indigestion, and may cause deafness or blindness without seeking to indicate how common or otherwise the severe side effects were [ACCC 4.551, p 3].
209 However, it was not usual in the Annexure B patient transcripts for the salespeople to mention Viagra, Cialis, and Levitra. On the few occasions where they did, the remarks denigrated these medications, although not in exaggerated terms. The only express example of this claim in the ACCC’s submissions was the consultation with ED patient 28, during which the following exchange occurred:
VINCENT: .... Have you tried anything for it at all?
PATIENT: I’ve tried Viagra and Cialis.
VINCENT: Yes. How did you go with those two?
PATIENT: They tend to work but they make me sick. They give me a headache and hot in the face.
VINCENT: Yes. They do, mate. They’ve got so many side-effects those medications and – I mean, in fact, we don’t use those two here in the Institute. And, [Patient], I don’t know whether you’re aware or not, mate – Viagra and Cialis – mate, they’re there to facilitate sex. But you’ve noticed – you’ve been using it but you still haven’t gotten over the problem. It’s designed so that you have to use it forever and ever.
PATIENT: Okay. Yes.
VINCENT: Whereas our treatment – what we do here is we actually work with our patients to help them to get rehabilitated so that we can get you to a stage where you can perform with or without the medication later down the track.
[ACCC 4.262, p 4]
4.5.2.5 Recommending long-term contracts
210 The ACCC alleged that salespeople and doctors were, in effect, required by AMI and NRM to recommend to patients that treatment was required for 12 to 18 months. It further alleged that there was no scientific basis for such a period of treatment. Consequently, the salespeople and the doctors, acting on behalf of AMI and NRM, acted unconscionably by recommending treatment periods of 12 to 18 months.
211 The discussion at [610] – [679] of these reasons for judgment concludes that there was no scientific basis for a treatment period of 12 to 18 months.
212 As to the role of the salespeople, the training materials repeatedly emphasised that they should tell patients that the treatment was required for 12 to 18 months. Thus, the Instructions to Clinical Coordinators stated:
Our programmes have been specifically designed to be undertaken over a standard 12 months period with the objective of having a patient complete the programme, sexually rehabilitated, and without the need for ongoing programme intervention.
[ACCC 4.9, p 2]
213 The ACCC claimed that in 62 cases of the Annexure B patients, it was the salesperson who suggested the treatment period to the patient, not the doctor.
214 The ACCC also claimed that the doctors were sometimes asked by salespeople to recommend a certain period of treatment, and that they did so. This occurred, for example, during the consultation with patient 28 salesperson when Vincent asked the following of Dr Vandeleur:
VINCENT: A very good patient, mate. I told him he’s probably going to need about four to 18 months to fix the problem.
DR VANDELEUR: Yes.
VINCENT: If you could just reiterate.
DR VANDELEUR: Yes.
VINCENT: Thank you, James.
DR VANDELEUR: Okay.
[ACCC 4.262, p 8]
215 Before Dr De Sayrah’s consultation with patient 38, salesperson Lori mentioned to her, “I just thought maybe if you – if you’re okay with 12 to 18 months.” [ACCC 4.277, p 6] And before Dr Berry’s consultation with patient 121, Vincent raised the subject of the length of treatment with her:
VINCENT: I told him he would probably be looking at 12 to 18 months - - -
DR BERRY: Yes.
VINCENT: - - - maybe 18 months, maybe more - - -
DR BERRY: Yes.
VINCENT: - - - because it's such a longstanding problem…
[ACCC 4.240, p 10]
In both of these cases Dr De Sayrah and Dr Berry prescribed treatment periods as indicated by the salespeople.
216 The recordings substantiated the claims of the ACCC that the salespeople often recommended a 12-to-18 month treatment period, and on other occasions, asked the doctors to do so.
4.5.2.6 Misleading patients about the refund term
217 It was regular and usual practice for salespeople to tell patients that there was a guarantee in place so that if they did not achieve the desired result they could obtain a refund. Patients were not told that they were required to try all methods of treatment offered by AMI, including self-administered intracavernosal injections in the base of the penis, to obtain a refund. This aspect is separately examined later in these reasons for judgment at [680] – [736] when dealing with the contractual terms of the treatments offered to patients.
4.5.3 Offering limited to AMI medications
218 The ACCC contended that AMI engaged in unconscionable conduct in relation to the Annexure B patients by limiting the choice of medications which doctors could prescribe to those medications which AMI formulated and had compounded for it. The ACCC further alleged that those medications were not the first-line treatments for ED and PE generally recognised by the medical profession, and that there was no proper evidence of the efficacy of those medications or of the alternative delivery routes used by AMI. Further, patients were not told that the doctors were limited in the choice of medications they could prescribe. The same allegations were made in relation to NRM in respect of the medications prescribed during the NRM period.
219 The respondents argued that the material they exhibited demonstrated that there was evidence of the efficacy of the AMI and NRM medications. They said that the efficacy of the drugs AMI and NRM used to treat ED and PE had been known for a long time. The respondents said that drug delivery systems are a means of improving patients’ adherence to medical therapy regimes. The respondents said their evidence showed that the alternative delivery routes used by AMI and NRM were effective. They relied on the evidence of Dr James Stephen Rowe and Dr Phillip Altman.
220 In this section, these reasons for judgment first address the evidence concerning the conventional medications used for the treatment of ED and PE. Then, the reasons for judgment explain that the medications available to AMI and NRM doctors to prescribe were not the conventional medications, but were limited in the main to apomorphine-based medications for the treatment of ED and to clomipramine-based medications for the treatment of PE. These reasons for judgment then examine the evidence concerning the efficacy of each of those medications. Finally, the reasons for judgment examine the standards applicable to prescribing those medications off-label, that is, for a use other than the use for which the medications were registered, and whether AMI and NRM’s practice conformed with those standards.
4.5.3.2 The conventional first-line treatment for ED and PE
221 The ACCC relied on Dr Pattison to give expert evidence on a number of matters, including the issues presently under consideration. Dr Pattison has been in general practice in East Ivanhoe in Melbourne since 1978. In 1998 and again in 2001, he published a book on men’s health. He has developed a large men’s health practice within his clinic. Between 1996 and 2004 Dr Pattison lectured undergraduate students at Melbourne, Monash, and Swinburne Universities on men’s health issues. He has also presented lectures to other general practitioners on the subject. He is regularly asked to address community groups on men’s health issues.
222 Dr Pattison wrote five reports which were tendered in evidence. His report dated 27 July 2011 [ACCC 3.28] (Pattison Report 1) answered specific questions about a number of issues raised in this proceeding, including the proper professional requirements for a medical practitioner treating ED and PE. That report also identified the medications accepted by the medical profession for the treatment of ED and PE and explained how they worked. Pattison Report 2 commented on the treatment of 14 Annexure B patients, including on the suitability of the medications which were prescribed for them. The third report dated 25 April 2012 (Pattison Report 3) commented on three NRM patients and on the suitability of the medications prescribed for them. The fourth report dated 3 March 2013 (Pattison Report 4) commented on the treatment by Dr Catherine Nora Berry, a doctor engaged by AMI and NRM, of six patients, including the suitability of the medications prescribed for them. Dr Berry responded to Dr Pattison’s comments in her second statement dated 18 July 2013 (Berry Statement 2). In his report dated 31 October 2013 (Pattison Report 5), Dr Pattison responded to Dr Berry’s explanations of her consultations.
223 Dr Pattison also gave oral evidence. His evidence inspired confidence. He presented as a doctor who is very knowledgeable in the area of male sexual dysfunction. His responses were direct, unhesitating, and obviously drawn from a considerable reservoir of experience and understanding. He articulated his responses clearly and rationally. Importantly, his approach was independent of the parties and disclosed no hint of partisanship. Dr Pattison’s approach in his reports and in his oral evidence demonstrated a doctor concerned with professional integrity, a focus on patient care, and a commitment to high professional standards. I have no hesitation in accepting his evidence, as outlined below.
224 Dr Pattison explained that the first-line treatment for ED is by using the oral phosphodiesterase 5 (PDE5) inhibitors such as Viagra, the main constituent of which is sildenafil, Levitra, the main constituent of which is vardenafil, and Cialis, the main constituent of which is tadalafil. Viagra and Levitra have a short half-life, that is to say, they remain effective for six to eight hours. They are therefore suited to men in stable relationships who are likely to know when sexual intercourse is likely to occur. Cialis has a half-life of 36 hours. Many men find this allows for greater spontaneity with their partner. It is particularly suitable for men in a new relationship when the timing of intercourse may be more uncertain. Dr Pattison stated that PDE5 inhibitors are well tolerated and very effective. Each has an excellent safety profile and a clinical success rate of 65 to 70 per cent. Some men experience facial flushing, nasal congestion, or headaches. Cialis can cause occasional muscular back pain. Less than two per cent of patients discontinue PDE5 inhibitors because of adverse side effects.
225 Dr Pattison explained that primary or lifelong PE is usually managed with selective serotonin re-uptake inhibitor medications (SSRIs), such as Aropax, the main constituent of which is paroxetine, 20 mg daily or Zoloft, the main constituent of which is sertraline, 50 mg daily. Most men with primary PE require ongoing therapy with SSRIs to give them satisfactory ejaculatory control. They usually require medication for six to twelve months before considering tapering off. SSRIs are generally well tolerated and side effects are usually mild. However, nausea, drowsiness, headaches, malaise or agitation may occur. The product information for paroxetine states that 13 per cent of patients using SSRIs for depression had to discontinue treatment due to adverse side effects. The treatment for secondary or acquired PE is more focused on counselling and behavioural techniques. However, if there is underlying ED, the use of PDE5 inhibitors would be helpful. At times, an SSRI might be warranted to reduce penile sensation.
226 The first-line medications for the treatment of ED and PE described by Dr Pattison follow Andrology Australia’s Clinical Summary Guide 8 “Premature Ejaculation and Other Ejaculatory Disorders – Diagnosis and Management” (Andrology Australia PE Guide) and Clinical Summary Guide 9 “Erectile Dysfunction – Diagnosis and Management” (Andrology Australia ED Guide). These guides, which were appended to the first affidavit of Dr Pattison dated 29 July 2011 and tendered in evidence by the ACCC, appear to date from May 2010. However, I infer from Dr Pattison’s evidence that they had not changed since the 2008 version relevant to this proceeding. Dr Pattison explained that Andrology Australia is the peak medical body in Australia formed to advise on men’s health issues. The guides are accepted by doctors generally as establishing best practice management for the conditions.
227 In his first report Dr Pattison also listed fourteen sources, including articles from medical journals dealing with the treatment of ED and PE, which he said supported his evidence as to the accepted first-line medications.
4.5.3.3 The limitation by AMI on medications available for doctors to prescribe
228 Despite the fact that it was accepted medical practice that the first-line medications for ED were PDE5 inhibitors and the first-line medication for PE were SSRIs, these medications were not usually offered to the Annexure B patients. Rather, doctors engaged by AMI mostly prescribed various nasal sprays compounded for AMI using apomorphine for treating ED, and using clomipramine for treating PE.
229 For practical purposes the choice of medications available to the AMI doctors to prescribe was limited. The prescriptions which they wrote were computer-generated. The system was governed by a drop-down menu which allowed only for the prescription of the medications compounded for AMI. The generally accepted first-line medications for ED, namely, sildenafil, vardenafil, and tadalafil in tablet form, were not available through the computer system. For some time vardenafil in troche form was available on the drop-down menu. Although doctors had prescribing pads available, Mr Shrestha said that, over time, as all the business processes became automated, the use of doctors’ prescribing pads became almost non-existent.
230 The choice of medication available to the doctors to prescribe was, in a practical sense, restricted. Both Dr Lonergan and Dr Vandeleur said that they preferred to prescribe vardenafil rather than apomorphine for the treatment of ED, and did so in the troche form which was the only form it was available through AMI. They both gave evidence that Dr Vaisman told them that he preferred them to prescribe apomorphine, because the vardenafil they were prescribing was “costing AMI a fortune” [ACCC 1.39, p 9; ACCC 1.37, p 11]. Dr Vaisman denied the conversation. However, it was independently corroborated in a recording when Dr De Sayrah, another doctor engaged by AMI, said in a conversation on 12 May 2009 with salesperson Lori, in relation to the possible prescription of vardenafil to a patient on the line, “I heard that Jack [Dr Vaisman] has called – two other doctors who were giving it regularly and asked them not to prescribe it as the first line treatment.” [ACCC 4.277, p 6]
231 I accept that there was pressure from the management of AMI for doctors to prescribe apomorphine rather than vardenafil troches as the first-line treatment for ED. Indeed, that is consistent with the case of the respondents that apomorphine is an effective and accepted medication for PE, and, according to Dr Vaisman, preferable to PDE5 inhibitors. It is also consistent with a recurrent theme of AMI’s advertising, namely, that it was using a new type of medication.
232 There was also pressure from the management of AMI for doctors to prescribe clomipramine as a first-line treatment for PE and this is discussed at [883] of these reasons for judgment.
233 The respondents argued that the limitation on the medications available from AMI and NRM was justified because medications prescribed by AMI and NRM doctors were effective and were made up of well-known and studied drugs that are or have been widely used throughout the world in the treatment of male sexual dysfunction. There are two questions implicit in the issue of the efficacy of AMI and NRM medications. The first is whether the drugs used in the AMI and NRM medications have been shown to be effective for the treatment of ED and PE. The second question is whether the alternative delivery routes used in AMI and NRM’s medications were effective. These issues will now be addressed.
4.5.3.4 The efficacy of apomorphine as a treatment for ED
234 Apomorphine as the main ingredient delivered by nasal spray was prescribed by AMI doctors for the treatment of ED for about 28 of the Annexure B patients. The nasal spray was prescribed for regular daily or every few days’ usage. It was not usually prescribed for on-demand usage [R13.12, p 194; ACCC 4.249, p 11].
235 At [33] of their written submissions, the respondents claimed that, “[a]pomorphine is as effective as PDE5 inhibitors for the treatment of ED.”
236 The evidence relied on by the respondents demonstrated that apomorphine taken sublingually (SL) was used to treat ED before PDE5 inhibitors were developed in the late 1990s. Thus, in an article by J. Buvat and F. Montorsi entitled, “Safety and tolerability of apomorphine SL in patients with erectile dysfunction” (2001) 88 BJU International 30, the authors stated “a sublingual formulation of apomorphine received regulatory approval in European Union member states as a first-line oral therapy for erectile dysfunction” [R 1.43, p 1].
237 However the scientific literature relied on by the respondents also showed that it is now recognised by the medical profession that PDE5 inhibitors are more effective than apomorphine SLs. In some scientific publications, apomorphine SLs were referred to as a second-line treatment, for instance, where patients are not able to tolerate PDE5 inhibitors. In others, apomorphine was not referred to at all.
238 Thus, for instance, in their written submissions the respondents relied on an article published in early 2010, in European Urology, the journal of the European Association of Urology (EAU). The article written by Konstantinos Hatzimouratidis and others entitled, “Guidelines of Male Sexual Dysfunction: Erectile Dysfunction and Premature Ejaculation” (2010) 57 European Urology 804 (Hatzimouratidis 2010) [R1.10] aimed to summarise and present an updated version of the 2009 guidelines of the EAU on ED and PE. The authors undertook a review of the recent literature of the epidemiology, diagnosis, and treatment of ED and PE. The EAU assigned levels of evidence and grades of recommendation to treatment. The abstract of the article summarised the treatment options for ED thus:
Treatment is based on phosphodiesterase type 5 inhibitors (PDE5-Is), including sildenafil, tadalafil, and vardenafil. PDE5-Is have efficacy and safety rates, even in difficult-to-treat populations such as patients with diabetes mellitus. Treatment options for patients who do not respond to PDE5-Is or for whom PDE5-Is are contraindicated include intracavernous injections, intraurethral alprostadil, vacuum constriction devices, or implantation of a penile prosthesis.
239 In what the article described as first-line therapy it described the operation and efficacy of PDE5 inhibitors as follows:
Sildenafil (Viagra), launched in 1998, was the first PDE5-I available. It is effective 30–60 min from administration. A heavy fatty meal may reduce or prolong absorption. It is administered in 25-, 50-, and 100-mg doses. The recommended starting dose is 50 mg, which is adapted according to patient response and side-effects. Efficacy may last for up to 12 h. In premarketing studies, after 24 wk of treatment in a dose-response study, improved erections were reported by 56%, 77%, and 84% of men taking 25, 50, and 100 mg of sildenafil, respectively, compared with 25% of men taking placebo. The efficacy of sildenafil in almost every subgroup of patients with ED has been well established in pre- and postmarketing studies.
Tadalafil (Cialis) was licensed for ED in 2003. It is effective from 30 min after administration, but its peak efficacy occurs after about 2 h. Efficacy is maintained for up to 36 h. Its efficacy is not affected by food. It is administered in 10- and 20-mg doses. The recommended starting dose is 10 mg, which is adapted according to patient response and side-effects. In premarketing dose-response studies, improved erections were reported after 12 wk of treatment by 67% and 81% of men taking 10 mg and 20 mg of tadalafil, respectively, compared with 35% of men taking placebo. The results were confirmed in postmarketing studies. Tadalafil also improved erections in difficult-to-treat subgroups.
Vardenafil (Levitra) was licensed for ED in 2003. It is effective 30 min from administration. A fatty meal (>57% in fat) reduces its effect. It is administered in 5-, 10-, and 20-mg doses. The recommended starting dose is 10 mg, which is adapted according to the response and side-effects. In vitro, it is 10-fold more potent than sildenafil; however, this does not necessarily mean greater clinical efficacy. In premarketing dose-response studies, improved erections after 12 wk of treatment were reported by 66%, 76%, and 80% of men taking 5 mg, 10 mg, and 20 mg of vardenafil, respectively, compared with 30% of men taking placebo. Efficacy was confirmed in postmarketing studies. Vardenafil also improved erections in difficult-to-treat subgroups.
240 Treatment using apomorphine was not discussed in the article, even as a possible second-line treatment. However, one line in table 4 in a list of treatment recommendations stated that, “apomorphine can be used in mild to moderate ED, psychogenic ED, or in patients with contraindications to PDE5-Is.” The recommendation was assessed at a 1b level of evidence and B grade of recommendation. In the same table, PDE5 inhibitors were recommended as first-line therapy and assessed at a 1a level of evidence and at an A grade of recommendation. There was also mention of apomorphine in the article at figure 2, a flow chart of the treatment path for ED. It pointed to apomorphine as a second-line treatment after PDE5 inhibitors.
241 The respondents also referred to an article by Dr Francesco Montorsi and others entitled, “Summary of the Recommendations on Sexual Dysfunction in Men” (2010) 7 Journal of Sexual Medicine 3572 (Montorsi 2010) [R 1.1]. The article set out a summary of the guidelines for the treatment of male sexual dysfunction formulated at an international consultation held in Paris in 2009, where 190 multidisciplinary experts from 33 countries were assembled into 25 consultation committees. Each committee undertook an extensive review of the available data and publications to develop evidence-based guidelines in each area. The summary stated that the treatment of ED has been revolutionised by PDE5 inhibitors, which represent a unique form of oral treatment for ED. There was no reference to the use of apomorphine for the treatment of ED.
242 An article published in the same journal by Ian Eardley and others entitled, “Pharmacotherapy for Erectile Dysfunction” (2010) 7 Journal of Sexual Medicine 524 [R 1.42] focused on the use of drugs for the treatment of ED. The article was a critical review of literature relating to the use of pharmacotheraputic agents undertaken by a committee of eight experts from five countries. The article reported that PDE5 inhibitors are “the initial form of pharmacotherapy for men with ED.” Three such drugs, sildenafil, tadalafil, and vardenafil are licensed for use around the world. They act locally by penetrating the smooth muscles of the penis allowing for an increased blood flow. There are multiple level one studies with consistent outcomes for each demonstrating the efficacy of the three drugs. The article also addressed apomorphine. It explained that apomorphine is a centrally acting drug, which has a grade A recommendation, and concluded that “[o]verall there is evidence that apomorphine is efficacious in the treatment of erectile dysfunction in the broad population at doses of 2 and 3 mg taken sublingually in an on demand fashion”. As to the comparative efficiency of sildenafil and apomorphine, the article concluded:
The authors consider that several trials comparing the efficacy and tolerability of apomorphine and sildenafil could be considered level 1 trials. All were all open-label studies, but were otherwise well designed trials, with adequate numbers of patients randomized. Overall there was clear evidence that sildenafil has greater efficacy in the treatment of men with ED than apomorphine.
[Emphasis added.]
243 The respondents’ expert Professor Jon Nicolas Currie expressed the opinion in his report dated 6 February 2013 (Currie Report 1) that “[a]ll medications used in the AMI program in their original formulations do have an evidence base in the treatment of male sexual dysfunction, including the use of apomorphine” [R 13.31, p 9]. He relied on an article by Amar Mohee and others, “The evaluation of apomorphine for the treatment of erectile dysfunction” (2012) 8(11) Expert Opinion on Drug Metabolism Toxicology 1447 (Mohee 2012), to support this view. The authors reviewed the evidence available for the use of apomorphine in the management of ED from both randomised placebo-controlled trials, and randomised non-placebo-controlled prospective trials. They found that apomorphine was an effective drug in the management of ED and was generally well tolerated over time. However, they said that that the trials showed that PDE5 inhibitors had better efficacy than apomorphine and that, “[a]pomorphine is a second-line treatment for ED at best.” They said:
Current evidence supporting the use of apomorphine as an ED drug is however limited due to the small number of RCTs [randomised controlled trials], and the small number of participants in each of these. The main barrier to apomorphine becoming a drug widely used in the treatment of ED is however its lack of efficacy compared with other drugs already marketed for the treatment of ED, namely PDE-5 inhibitors. Non-placebo controlled prospective studies show a higher success rate of successful sexual attempts for sildenafil compared with apomorphine with few side effects. The main asset of apomorphine is its high safety profile; its main side effects, namely headache, nausea and dizziness, are generally mild and self-limited.
Further research is, however, needed in this field as the absence of large head-to-head trials directly comparing the efficacy of apomorphine and other PDE5-Is limits the interpretation of these results. Current guidelines on the use of apomorphine in the treatment of ED limit its role to the management of mild to moderate ED in patients who fail treatment with the first-line PDE-5 inhibitors, or in those in whom PDE-5 inhibitors are contraindicated (European Association of Urology Guidelines).
[Emphasis added.]
244 In Pattison Report 2, Dr Pattison reviewed the treatment of five Annexure B patients who had been prescribed an apomorphine nasal spray as first-line treatment for ED. He said:
Apomorphine is a centrally-acting medication that increases the level of a chemical called dopamine in the body with the intention of indirectly enhancing erectile function. It was used several years ago as a sublingual tablet for ED but was not effective and was withdrawn from the market. Apomorphine has recently been used again in injection form for patients with severe Parkinson’s disease. The medication is not recommended in any of the accepted clinical guidelines for the management of ED.
[ACCC 3.29, p 304]
245 The reference to accepted guidelines is probably meant as a reference to the Andrology Australia ED Guide, which did not mention apomorphine as a treatment for ED. Further, where Dr Pattison stated that apomorphine was not effective, he should be taken to mean that apomorphine was not as effective as the first-line treatment using PDE5 inhibitors. So understood, Dr Pattison’s opinion accurately reflected the scientific literature relied on by the respondents in their submissions.
246 Dr Vaisman said in his first witness statement dated 13 September 2012:
38 I hold the view, based upon the scientific literature I have read that apomorphine is as effective as 5-PDE (of which Vardenafil is one) in treating erectile dysfunction. For patients with heart conditions who are receiving treatment using nitrates, the use of 5-PDE-based medication can be fatal. There is no such complication with the use of apomorphine in those conditions. I provided this medical literature to doctors as part of the education meetings. I discussed contraindications at education meetings and I provided up-to-date copies of pages from MIMS in relation to each of the medical formulations provided for the treatment of sexual dysfunction.
[R 13.1]
247 Further, in cross-examination, Dr Vaisman admitted that he believed apomorphine was as effective as PDE5 inhibitors, but that the substances acted in different ways [TS 1701].
248 Then, also in cross-examination, Dr Vaisman was asked if he had a preference for apomorphine over PDE5 inhibitors for the treatment of ED. He argued that it was a matter for the doctors not for him, but that there had been 500 deaths reported from the use of PDE5 inhibitors. Whilst Dr Vaisman was not initially prepared to accept that he preferred the use of apomorphine for the treatment of ED, he admitted, when asked by the Court, that he had told the AMI doctors that he preferred apomorphine to PDE5 inhibitors [TS 1703]. He said that he had provided information to the doctors that, “5PDE have the same action like apomorphine, but apomorphine is more safer.” [TS 1646] Despite his initial reluctance to concede that he preferred the use of apomorphine for the treatment of ED, that was the inevitable conclusion to be drawn from his evidence as a whole. Indeed, as discussed at [883] – [888], Dr Vaisman, in effect, insisted that doctors prescribe apomorphine as the first-line treatment for ED.
249 Dr Vaisman’s view about apomorphine as a treatment for ED was not only inconsistent with the specific scientific material relied on by the respondents in written submissions, but was also inconsistent with the scientific material on the subject exhibited to his first witness statement dated 13 September 2012.
250 Written materials which Dr Vaisman said he gave to the AMI doctors were contained in two exhibits to his first witness statement, exhibits JV-1 and JV-2. This material was not referred to by the respondents in closing submissions to support Dr Vaisman’s view about the efficacy and safety of apomorphine in treating ED. An examination of that material showed that it supported the opposite view, namely, that PDE5 inhibitors are the primary treatment for ED.
251 The material covered a wide variety of topics concerning male sexual dysfunction and came from diverse sources, mostly from scientific journals, but from some internet sources. The references to drug treatment for ED generally explained that PDE5 inhibitors are the first-line treatment. Thus, Luke Fazio and Gerald Brock wrote in their article entitled, “Erectile dysfunction: management update” (2004) 170(9) Canadian Medical Association Journal 1429 (Fazio and Brock 2004) that:
Dramatic advances in the management of erectile dysfunction have occurred over the past decade … Oral therapy with a PDE-5 inhibitor (sildenafil, vardenafil, or tadalafil) should be considered for first-line treatment of erectile dysfunction.
[R 13.3, p 97]
252 Although not referred to by the respondents, there were other references to apomorphine in that material. One was in an article published by Raymond Rosen and Sandra Leiblum entitled, “Treatment of Sexual Disorders in the 1990s – An Integrated Approach” (1995) 63(6) Journal of Consulting and Clinical Psychology 877). The authors wrote:
Dopaminergic and serotonergic drugs have similarly been evaluated as possible treatment agents for erectile disorder. For example, apomorphine is a short-acting dopamine agonist which has been shown to facilitate erectile responses in both control patients and patients with psychogenic or organic erectile dysfunction. Regrettably, significant side effects (e.g., nausea, drowsiness) have limited the clinical usefulness of this drug.
[References omitted.]
[R13.3, p 170]
This article predated the development of PDE5 inhibitors and hence had nothing to say about their comparative efficacy and safety.
253 Apomorphine was also discussed in an article included in the exhibits JV-1 and JV-2 by Geoffrey Hackett entitled, “What Do Patients Expect From Erectile Dysfunction Therapy?” (2002) 1(8) European Urology Supplements 4 (Hackett 2002) [R 13.2, p 35]. Hackett acknowledged that in circumstances where men wish to keep the fact of their ED from a new sexual partner:
[A] rapidly acting therapy, such as sublingual apomorphine, may be more appropriate than a drug such as sildenafil, as these men are more likely to complain about the need for premeditation associated with taking the therapy 1 hour before planned sexual intercourse.
254 Furthermore, in discussing the side effects of sildenafil (headache, dyspepsia and flushing), and the fact that some patients may wish to try alternatives, the author stated that:
[T]he centrally acting dopamine agonist apomorphine has a different mechanism of action and side-effect profile than those of PDE5 inhibitors. Nausea, headache and dizziness were among the predominant side effects seen in clinical trials with sublingual apomorphine.
255 However, in terms of the effectiveness of the two drugs, the author recognised that, “[a]mong patients with severe ED, a PDE5 inhibitor is more likely to be effective than sublingual apomorphine.”
256 In JV-2, Dr Vaisman exhibited an article by Dr Irwin Goldstein and Dr Robert Krane entitled “Diagnosis and Therapy of Erectile Dysfunction”. The article was undated and the copy in evidence did not disclose the publication in which it was published. The authors stated:
Attempts at neuropharmacologic therapy of erectile dysfunction have largely involved dopaminergic and serotoninergic agonists. The positive erectile effects of dopaminergic agonists was [sic] first noted in patients treated with L-dopa. In addition, subcutaneously administered apomorphine, a dopaminergic agonist, has been shown to enhance erectile responses in men. Laboratory investigations in rats and monkeys have corroborated this observation.
[References omitted.]
[R 13.3, p 148]
257 Another reference to apomorphine in exhibit JV-2 was in an article by Dr Stanley Brosman, “Erectile Dysfunction” (May 2004) published online at www.emedicine.com. Dr Brosman reported first that sildenafil is “the first oral agent to be well documented as an effective form of treatment for men experiencing ED” [R 13.3, p 188]. Dr Brosman then referred to apomorphine as not yet approved by the US Federal Drug Administration and that, “the administration of apomorphine by subcutaneous, oral and intranasal routes results in variable effects on erectile function [including] nausea and vomiting.”
4.5.3.5 The efficacy of clomipramine as a treatment for PE
258 Clomipramine as the main ingredient delivered by nasal spray was prescribed by AMI doctors for the treatment of PE for about 76 of the Annexure B patients. The clomipramine nasal spray was prescribed for use every day or every second day with or without sex. It was generally not prescribed for on-demand usage alone.
259 In Pattison Report 1, Dr Pattison said that the mainstay of treatment for primary PE was the SSRI Aropax (paroxetine) at 20 mg once daily or Zoloft (sertraline) at 50 mg once daily. He said that on-demand treatments for use just before intercourse had been investigated extensively overseas and were likely to become available in the near future.
260 In Pattison Report 2 Dr Pattison reviewed the treatment of 14 Annexure B patients. He noticed that clomipramine was prescribed as a first-line treatment for PE in seven instances. He expressed his view thus:
Clomipramine nasal spray was prescribed in transcripts 1, 2, 4, 5, 8, 9 and 12 as first line treatment for the management of PE. The use of this medication in a nasal spray formulation is not evidence-based. Although the medication might have some effect, I am unaware of any significant clinical trials to support its use. The drug is a tricyclic antidepressant and is sometimes still used orally in the treatment of narcolepsy, depression and obsessive compulsive disorder. Because it can be sedating and interfere with concentration it is usually advised to be taken at night and should be avoided when driving or operating machinery. It can also interact with a number of medications as well as alcohol and other drugs. For these reasons it is used very infrequently these days. Oral Clomipramine is mentioned in the Andrology Australia Guidelines as an alternative treatment for PE. However SSRI medications such as Aropax and Zoloft are better tolerated, safer and far more commonly used. Clomipramine capsules were prescribed for PE in transcript 14. Clomipramine nasal spray can cause quite significant nasal irritation. This was referred to in several of the transcripts. I have no personal experience in using Clomipramine nasal spray for PE and I know of no other doctor who prescribes it for this condition.
261 Dr Pattison noted in his oral evidence that clomipramine, in oral form, was recommended by Andrology Australia in the Andrology Australia PE Guide for patients with particularly resistant PE [TS 1055].
262 Patient 13 saw his GP after having taken clomipramine nasal spray prescribed for him by an AMI doctor and after developing unwanted side effects [ACCC 1.4]. His GP told him to stop using the nasal spray and that the medication was an old treatment which had been replaced by newer treatments. This is consistent with Dr Pattison’s view that clomipramine is not the first-line treatment for PE and is infrequently prescribed by doctors.
263 In closing submissions, the respondents said that Dr Vaisman had indicated his preference for clomipramine over SSRIs for the reason that withdrawal syndrome is associated with SSRIs and not clomipramine, and that using clomipramine on-demand caused less drowsiness than paroxetine [TS 2766]. The respondents sought to establish that clomipramine was an accepted and effective medication for the treatment of PE. They referred to guidelines published by professional bodies and to scientific articles relating to the treatment of PE. It is useful to consider this material in chronological order because such a consideration discloses a shift in medical consensus about the use of clomipramine for the treatment of PE.
264 In about 2004, the American Urological Association (AUA) published its “Guideline on the Pharmacological Management of Premature Ejaculation” (AUA Guideline 2004), which reviewed the scientific literature on the subject published between 1966 and October 2002 [R 13.3, p 1]. It claimed to be the first guideline to address the pharmacologic treatment of PE. The guideline recognised the SSRIs fluoxetine at 5 – 20 mg per day, paroxetine at 10, 20 or 40 mg per day, and sertraline at 20 – 200 mg per day, and the tricyclic antidepressant clomipramine at 25 – 50 mg per day, as options for the treatment of PE. The guideline indicated that there was some limited testing which suggested that on-demand dosing may be of some use, although the medications were designed for continuous usage, and that, “whether continuous or on-demand dosing is more effective in the management of PE is unclear.” [R 13.3, p 12]
265 In 2004 Marcel Waldinger and others published the article, “On-Demand Treatment of Premature Ejaculation with Clomipramine and Paroxetine: A Randomized, Double-Blind Fixed-Dose Study with Stopwatch Assessment” (2004) 46(4) European Urology 510 (Waldinger 2004) [R 13.6, p 2]. The authors reported that on-demand treatment with 25 mg of clomipramine led to clinically relevant ejaculation delay, whilst on-demand treatment with 20 mg of paroxetine led to no clinically relevant ejaculation delay. The study discussed by the authors involved 30 men with primary PE over a four-week drug treatment period. Both drugs had a high incidence of non-sexual side effects on the day of intercourse or the next day. On the day of intercourse, paroxetine led to significant sleepiness and yawning compared to clomipramine. On the day after intercourse, clomipramine induced significant nausea compared to paroxetine.
266 The respondents then referred to a further article by Marcel Waldinger entitled, “Premature Ejaculation, Definition and Drug Treatment” (2007) 67(4) Drugs 547 (Waldinger 2007) [R 1.11]. The respondents appeared particularly to rely on the conclusion that the daily use of clomipramine was effective for the treatment of PE. Whilst this is so, it is a selective reading of the conclusions.
267 The author described the medical history of the daily use of clomipramine thus:
3.3. 1 Clomipramine
In 1973, Eaton published the first report on the efficacy of clomipramine, the tricyclic antidepressant with the greatest effect on the serotonergic system, in the treatment of PE. Particularly in the 1970-80s, various studies demonstrated the efficacy of clomipramine in delaying ejaculation. However, its use was not very popular in those years, when it was still generally believed that genuine treatment of PE should consist of merely behavioural psychotherapy. Over the last decade, a number of studies have repeatedly confirmed that daily treatment with clomipramine at dosages ranging from 20 to 50 mg/day is efficacious in the treatment of PE.
268 Then the author explained that the first publication on the efficacy of daily treatment with paroxetine was in 1994. After this, various other studies confirmed paroxetine’s strong ejaculation delaying effects at doses of 20 – 40 mg per day, and that other SSRIs exerted clinically relevant ejaculation-delaying effects. He continued:
Currently, daily treatment with SSRIs or combined daily treatment with on-demand use has become the first-line treatment of PE.
269 The article, at table II, indicated that daily medication with an SSRI, such as paroxetine, was more effective for the treatment of PE than daily medication with clomipramine. Further, whilst nausea was a major adverse effect of clomipramine when taken daily, it was not a major adverse effect of SSRIs when taken daily, although fatigue, yawning and loose stools were [R 1.11, p 556]. These matters primarily explained why SSRIs were the first-line treatment for PE. And, as the article demonstrated, whilst clomipramine was more effective as an on-demand medication than SSRIs taken on-demand, clomipramine taken on-demand was not as effective as daily treatment with either SSRIs or clomipramine.
270 To the same effect was an article by Carlo Bettocchi and others entitled, “Ejaculatory disorders: pathophysiology and management” (2008) 5(2) Nature Clinical Practice 93 (Bettocchi 2008) [R1.2]. Again, the respondents highlighted the conclusion:
On-demand clomipramine use has yielded greater increases in IELT [Intravaginal Ejaculation Latency Time] than commonly used SSRIs.
271 But, the article also explained:
On-demand administration of SSRIs 4-6 h before sexual intercourse is reported to be efficacious and well tolerated, but it is associated with a smaller delay in IELT than seen with daily administration.
272 The article also explained that, compared with other medications, including clomipramine, “[a]bove all, daily use of paroxetine has been demonstrated to yield the strongest ejaculatory delay within 5 – 10 days.”
273 The respondents referred to the Andrology Australia PE Guide [R 13.3, p 20]. It seems that the version to which they referred was published in 2009. The guide recognised clomipramine taken daily or on-demand as an available oral treatment for PE. The guide noted that “SSRIs are now commonly prescribed for PE.” However, it did not include clomipramine in that remark. It also acknowledged that the guide was based on the EAU Guidelines published in 2001 and 2009.
274 The 2009 EAU Guidelines were updated in early 2010. The respondents again relied on Hatzimouratidis 2010, which presented the updated guidelines [R 1.10]. The 2010 EAU Guidelines did not recommend the use of clomipramine for the treatment of PE. Rather they stated that SSRIs were the first choice of treatment for PE. They said that daily treatment with paroxetine was superior to other SSRIs, and also superior to clomipramine. By the time of this article, dapoxetine had been approved in seven European countries for on-demand treatment of PE. The guidelines recommended the use of dapoxetine on-demand, without any reference to the use of clomipramine for on-demand use.
275 Finally, the respondents referred to another article by Stanley Althof and others, “International Society for Sexual Medicine’s Guidelines for the Diagnosis and Treatment of Premature Ejaculation” (2010) 7 Journal of Sexual Medicine 2947 (Althof 2010). The authors aimed to publish guidelines which were more comprehensive and dealt with essential new evidence not referred to in the existing guidelines. The International Society for Sexual Medicine identified three sets of clinical guidelines for the treatment of PE then in existence, namely, the AUA Guideline 2004, the European Association of Urology Guidelines on Male Sexual Dysfunction: Erectile Dysfunction and Premature Ejaculation, updated 2009, and the Practice Guidelines for the Pan Arab Society of Sexual Medicine (Disorders of Ejaculation). The International Society for Sexual Medicine’s guidelines were based on a review of the scientific literature. The respondents relied on table 3, which included clomipramine as one of the recommended daily or on-demand treatments. However, the article explained that paroxetine taken daily produced the greatest ejaculatory delay among the medications taken daily, and that the medications taken daily produced a much greater ejaculatory delay than the medications taken on-demand.
276 The evidence referred to by the respondents established that clomipramine used on-label as an antidepressant was found to have an ejaculatory delaying effect, both daily and on-demand. It was, however, only used in a limited way off-label to treat PE. When the ejaculation-delaying effects of SSRIs were discovered in the 1990s, they became the first-line of treatment for primary PE. Paroxetine had the greatest ejaculatory delaying effect if taken daily. Clomipramine taken on-demand produced the best ejaculatory delaying effect of the on-demand medications, but produced less ejaculatory delaying effect than a daily dosage of paroxetine.
277 Thus, whilst clomipramine had a limited role in the treatment of PE, it was displaced when the ejaculation-delaying effects of SSRIs were discovered. The value which the respondents sought to place on clomipramine as a treatment for PE was exaggerated. The opinion of Dr Pattison that SSRIs were the accepted first-line treatment for primary PE reflects that fact.
278 The final step in the assessment of the AMI and NRM medications, however, requires an examination of the role of the delivery systems of the medications. This is so because the evidence and materials just discussed relate to the oral dosages of clomipramine and apomorphine, that is to say, the medications taken in the form of tablets and also SLs in the case of apomorphine. That was not the way most of the AMI and NRM medications were delivered. Rather, clomipramine and apomorphine were mainly prescribed in the form of a nasal spray in the AMI period and in the form of oral strips in the NRM period. The next section of these reasons considers the experts’ opinions on whether the alternative delivery systems used by AMI and NRM affected the efficacy of the medications.
4.5.3.6 The efficacy of alternative drug delivery systems
279 Evidence on this issue was given for the respondents by two experts, Dr James Rowe, and Dr Phillip Altman.
280 Evidence on the issue was given for the ACCC by Professor Colin Pouton.
4.5.3.6.1 Dr Rowe’s first report
281 Dr Rowe is a pharmacist and formulation chemist. He graduated with a Bachelor of Pharmacy from the University of Sydney in 1966. For most of his career, he has been employed in both Australia and the UK by pharmaceutical companies in the development of drugs. Whilst in the UK he completed a PhD in pharmaceutics and taught at the School of Pharmacy at the University of London. For a brief period between 1983 and 1986, he operated a community pharmacy and for another brief period between 2004 and 2008, he operated a compounding pharmacy. Between 2003 and 2008 he has also lectured undergraduates at the Pharmacy School, University of Sydney on dosage form, design and evaluation. From 1990, he was a director of companies engaged in consulting on the development, formulation and stability testing in the pharmaceutical, veterinary and personal care industries. Since December 2011, Dr Rowe has undertaken independent consulting work.
282 From 2000, Dr Rowe performed consulting work of a technical nature for AMI. The work related to the formulation of products, stability work on formulations, and the feasibility of the introduction of new products. He was paid for these services. From July 2012 to December 2013 he earned about $30,000 from this work. He agreed in cross-examination that prior to that year, possibly in 2009, he could have earned over $100,000 in consulting fees from AMI in one year. In 2009, Dr Rowe co-authored an article with Dr Vaisman, Dr Altman, and Brooke Berry comparing the performance of vardenafil delivered by a 10 mg oral tablet with a solution of vardenafil delivered by a nebuliser devised by AMI entitled, “Comparison of Pharmacokinetics of Vardenafil Administered Using an Ultrasonic Nebulizer for Inhalation vs. a Single 10-mg Oral Tablet” (2009) Journal of Sex Medicine [R 13.3, p 31].
283 In his first report dated 25 October 2012, Dr Rowe expressed the view that nasal and oral-strip delivery of medications have advantages over oral delivery by tablet. He said:
These delivery systems usually enable the use of a smaller amount of the active drug to be administered for the equivalent therapeutic effect and usually a reduction in side effects.
[R 13.29, p 8]
284 And he explained further:
30. Nasal Spray dosage forms for systemic effect (which means that they are intended to be absorbed into the blood stream as distinct from acting locally) have the advantage over oral medications in that they are absorbed through the nasal mucosa and thus bypass the acidic conditions encountered in the stomach. The acidic conditions encountered in the stomach may cause many drugs to degrade if they are sensitive to acid. They also do not undergo the first pass effect [which is the result of metabolism of the drug in the liver resulting in a reduced amount of the drug reaching the intestine and hence available for absorption into the circulatory system] … and thus the bioavailability of a drug given by the nasal route can often result in a much higher concentration in the plasma than an equivalent amount given as an oral dosage form. This often enables a reduction in the dose of the drug to achieve an equivalent (or higher) therapeutic effect but resulting in fewer side effects to the patient.
31. Another significant advantage of the nasal route is a more favourable time course of drug action. For a drug given orally, to be effective, the dosage form must firstly disintegrate from the tablet or capsule into its primary particles. These particles must then dissolve to form a solution before any absorption process may occur. In the nasal spray technology employed by AMI the process of disintegration and dissolution has already taken place as the drug is administered as a nasal solution. The effect of this is a rapid onset of action (compared to an oral tablet or capsule) which time effect I understand is very desirable from a patient viewpoint in the area of assisting sexual dysfunction.
[R 13.29, p 9]
285 Dr Rowe said that there were the same advantages by the use of troches and oral strips. Oral strips were added to the delivery methods available in the NRM period. Of AMI and NRM’s medications, he said:
48. I am of the opinion that AMI’s drug dosage forms use novel delivery systems which entail extensive product development prior to deployment of these systems and which require development work on the selection of excipients [inactive substances added to the active ingredients to provide bulk or to add to the therapeutic effect of medication] which are suitable in terms of ensuring the dosage form is non-toxic, stable, and delivers the drug effectively to the right place at the right time. This gives a patient convenience of use, rapid onset of action, better bioavailability, and fewer side effects…
49. AMI has taken existing drugs which have been available in tablet and capsule form and formulated those drugs (and others) in such a way as to produce formulations which have a faster onset of action, lower incidence of side effects and a better absorption profile than conventional tablets and capsules.
[R 13.29, p 12]
4.5.3.6.2 Dr Altman’s first report
286 Dr Phillip Altman is a pharmacologist with expertise in designing and conducting clinical trials and in obtaining regulatory approval for new drugs in different dosage forms. He graduated with a Bachelor of Pharmacy (Honours) from the University of Sydney in 1970 and obtained a PhD from that University in 1981. Initially he was employed by several major pharmaceutical companies. In 1986 he started the first contract research organisation in Australia to provide a full consulting service to multinational pharmaceutical companies concerning clinical trials and regulatory requirements. In the course of his career he has conducted studies of absorption, metabolism, and excretion of drugs by several different routes of administration. In his work he has assisted companies to develop and test new formulations of drugs to improve their efficacy or safety.
287 Dr Altman has provided advice to Dr Vaisman over about ten years. The largest project concerned the investigation of the use of a nebuliser for the delivery of vardenafil. Dr Altman’s role was to coordinate the clinical trial. This trial is referred to in [282] of these reasons for judgment.
288 In his first report dated 26 November 2012 [R 13.28], in response to questions asked of him, Dr Altman explained that drugs may be administered by different routes, and gave various examples. He then explained the means of delivery adopted in the AMI and NRM medications, and explained why he thought the particular delivery systems may have been chosen. He said:
I notice that AMI lists a number of sublingual sprays, nasal sprays and oral strips as delivery mechanisms for various drugs. Whilst I have no specific knowledge of the pharmaceutical performance of these individual products, it does appear to me that the drugs chosen for delivery using sublingual sprays, nasal sprays and oral strips were probably chosen on the basis that either they may be delivered into the systemic blood circulation faster or more efficiently (because they suffer from first-past metabolism following oral administration) or both. Speed of absorption (and consequently pharmacological action) appears to be a theme for other products marketed by AMI including fast dissolving APQ [apomorphine, phentolamine, vardenafil] and Clom tablets. The speed of action of drugs is an important characteristic of a medication.
[R 13.28, p 20]
289 At the end of the report Dr Altman summarised his views thus:
52. The dose form, formulation and route of administration of a drug are important characteristics of a medication and each can affect the Therapeutic Quality of a medication (including the speed of onset of action, the duration of action, the reliability of action, the clinical effectiveness and the incidence, type or severity of any adverse effects associated with a medication). Drugs administered by different dosage forms are not necessarily therapeutically equivalent in terms of clinical efficacy or safety.
53. The administration of drugs via the buccal route (gum or troche) or via the nasal route using a spray are routes of administration which are known to avoid hepatic first pass metabolism of drugs significantly metabolised on first pass through the liver prior to entering the systemic blood circulatory system. The bioavailability of drugs can be improved by avoiding first-pass metabolism.
54. Improving the bioavailability of a drug delivered by a medication which has relatively low bioavailability is advantageous in that dosage forms with higher bioavailability generally have a more predictable pattern of absorption and, therefore, should produce more reliable clinical responses.
55. The administration of drugs in medications designed for buccal (gum or troche) or nasal administration can have a faster onset of action as compared to the same drug administered orally.
[R 13.28, pp 21 – 22]
4.5.3.6.3 Professor Pouton’s report
290 Professor Pouton is a professor of pharmaceutical biology at the Monash Institute of Pharmaceutical Sciences at Monash University. He graduated with a Bachelor of Pharmacy from the University of Bath in the UK in 1976. He completed a PhD in London in 1982 on the subject of certain drug delivery systems. He then held teaching positions at the University of Bath until 2001 when he was appointed to head the Department of Pharmaceutical Biology at Monash University. Professor Pouton has taught courses on pharmacy and pharmacology, including on drug formulation and delivery, and has supervised the research of many PhD students on this topic. He has served as a consultant to major international pharmaceutical companies and patent attorneys over the last ten years. He has conducted research and published widely in the field of drug discovery, delivery and development. His work integrates studies of the physical chemistry of drugs with their impact on biological systems. His research began in drug delivery and absorption, and has continued in that area.
291 Professor Pouton was asked by the solicitors for the ACCC to prepare a report commenting on particular parts of each of the first reports of Dr Rowe and Dr Altman. Professor Pouton’s report is dated 22 January 2013
292 In relation to the first report of Dr Rowe, Professor Pouton wrote on the critical issue of the therapeutic effect of alternative delivery systems as follows:
I do not agree with Dr Rowe's statement that nasal delivery systems and strip formulations (paragraphs 24-25) "usually enable the use of a smaller amount of the active drug to be administered for the equivalent therapeutic effect and usually a reduction in side effects." There is no reason to expect that a smaller dose will have an equivalent therapeutic effect. The drug may not be completely absorbed from the mouth or nasal cavity, and in practice much of the drug is often swallowed in both cases. Typically if the drug acts after absorption into the blood circulation one would need to deliver an equivalent dose to result in a similar therapeutic effect. It is true that avoidance of first-pass metabolism could in theory reduce the dose required, but the low mass of drug that can be absorbed from the mouth or nasal cavity means that these approaches are not usually practical. The doses required for most drugs would be too high. In circumstances where the effect is a local action in the mouth or nasal cavity, one might expect to reduce the overall dose, but this is not the case for drugs acting by way of the systemic blood circulation. In relation to side effects: again if the drug is intended to act systemically there is no reason to expect that side-effects will be reduced by buccal or nasal delivery. Indeed the argument that the drug might be absorbed rapidly implies a higher peak plasma concentration which is normally associated with more pronounced side-effects.
[Emphasis added.]
[ACCC 3.36, p 278]
293 Professor Pouton rejected some of the advantages claimed by Dr Rowe for alternative delivery systems via the oral route as follows:
Paragraph 30 [of Dr Rowe’s report] refers to acid degradation in the stomach and first-pass metabolism and suggests that the absence of these phenomena allow lower doses to be administered by the nasal route. Acid degradation is rarely a problem and is not a factor with the drugs used in AMI medications (as detailed above). In each case it is likely that the proportion of drug lost by first pass would be reduced after nasal administration but that the mass of drug that can be absorbed for most drugs from the nasal cavity is limited by surface area. As a result the bioavailability from nasal sprays rarely reaches 90-100% and much of the spray is likely to be swallowed in practice. The absolute bioavailability of the AMI drugs from nasal sprays cannot be adequately predicted. Even though the doses of the drugs used in AMI sprays are low, which works in favour of adequate absorption from the nasal cavity, without supporting human bioavailability data it is impossible to estimate how much drug will be absorbed in each case.
[ACCC 3.36, p 280]
294 Professor Pouton also questioned whether the alternative routes of delivery would lead to more rapid effect of the drug as follows:
The time course of action is discussed in paragraph 31. Dr Rowe suggests that there is specific advantage to be gained by using the nasal route, ie. “the effect of this is a rapid onset of action….”. The implication of this paragraph is that rapid onset can always be achieved. In fact onset of action will depend on many factors and is really only a possibility. It is conceivable that rapid initial rate of absorption could be achieved by nasal administration but whether this results in rapid onset depends on whether sufficient dose is absorbed and on the pharmacokinetics of each drug. Without access to clinical studies the statements in paragraph 31 of Dr Rowe’s report are simply speculative. The doses of clomipramine used in AMI formulations could well be sub-therapeutic.
[ACCC 3.36, p 280]
295 Then, Professor Pouton addressed the way troches and oral strips worked, and said:
Troches and oral strips are the subjects of paragraphs 33-34 and 35-39. These delivery systems are designed to release drug in the mouth so that absorption can take place through the mucosal surfaces in the oral cavity. This route has a low capacity and is only useful for absorption of small masses of drugs. Thus troches or oral strips would be expected to be unsuitable for normal doses of clomipramine or tramadol. Very small doses, perhaps below 5mg, could be absorbed. Otherwise the dose is likely to be absorbed in the intestine after the patient has swallowed the drug.
[ACCC 3.36, p 280]
296 Professor Pouton outlined the limitations of the delivery of medication through absorption in the mouth and nose:
The sub-lingual and buccal routes refer to routes of absorption within the mouth (relevant to oral sprays, oral strip formulations and troches). The surface area available in the mouth is very limited but can be used to achieve systemic absorption and rapid onset of action for highly potent lipophilic drugs. The limitations of sub-lingual and buccal routes relate to the low capacity for mass transfer that results directly from the limited surface area available. In contrast the effective surface area of the small intestine has been estimated to be equivalent to that of a tennis court, and this explains why most drugs are administered orally to take advantage of the large surface area of the small intestine. Given the limited surface area in the mouth, the most common applications of this route are to administer the traditional drugs used to treat angina attacks (glyceryl trinitrate (GTN) and isosorbide dintrate). Both of these drugs are very low molecular weight compounds, and they are used in low doses. GTN is usually used at a dose of 0.5 mg. The limited mass of drug that can be absorbed in the mouth normally precludes its use as a means of achieving rapid onset for the majority of drugs, and there is no reason to expect that the same therapeutic effect can be achieved with a lower dose. This depends on whether sufficient drug can be absorbed from the mouth and on the pharmacokinetics of the drug after absorption. The proportion of drug absorbed from the mouth is frequently less than 100% and the remainder of the dose is likely to be swallowed. Similar limitations apply to the nasal route, and as a result it is largely used to administer medication for relief of symptoms of colds direct to the nasal cavity, rather than as a means for systemic administration of drugs.
The perceived advantage of delivery to the mouth or nasal cavity gained by avoidance of the first pass effect may in fact be negligible. If the proportion of drug removed by first pass was limited, as it is for clomipramine, tramadol and paroxetine, the advantage would be limited even if the drug was fully absorbed after administration. Given that the fraction absorbed is likely to be less than unity, the advantage gained by avoidance of first-pass effect is likely to be negligible.
It is implied in the Rowe report that the case for use of delivery to the the [sic] mouth or nasal cavity includes a likely improvement in therapy by way of early onset and shorter direction of response. Absorption of small masses of lipophilic drugs may be more rapid from the nasal cavity than by the oral route, but whether this leads to rapid onset and short duration depends on the drugs specific pharmacokinetic properties. Rapid absorption does not necessarily lead to short duration of action. A drug with a long systemic half-life will not be rendered short acting by nasal administration. Once the dose is absorbed it will be subject to the same kinetics of elimination, thus nasal administration may not significantly affect the plasma profile if the drug has a long elimination half-life.
[Emphasis added.]
[ACCC 3.36, p 281]
297 Next, Professor Pouton responded to questions asked of him by the ACCC in relation to Dr Altman’s first report. As to Dr Altman’s central thesis, Professor Pouton said:
Paragraph 46 makes the case that the AMI sublingual spays, nasal sprays and oral strips seem to be used to achieve faster or more efficient availability of the drug to the blood circulation. Dr Altman states that he has no specific knowledge of the pharmaceutical performance of these individual products. Herein lies the key problem with the AMI products: there is no data available at this stage on their performance and with respect to specific drugs it is not clear whether sufficient drug can be absorbed by these low capacity routes (sub-lingual, nasal) to achieve a therapeutic effect.
[Emphasis added.]
[ACCC 3.36, p 283]
298 Professor Pouton commented on some further aspects of Dr Altman’s report as follows:
In paragraph 53 Dr Altman states that the buccal and nasal routes of drug administration can be used to avoid hepatic first-pass effects, resulting in improved bioavailability. The use of the word 'can' again is critical and as a result this statement is correct. However, in practice very few drugs can be effectively administered by these routes, due to the low surface area of the buccal and nasal mucosa.
…
In Paragraph 55 Dr Altman states that medications designed for buccal or nasal administration can have a faster onset of action. I agree with this statement but reiterate that this advantage cannot be realised for most drugs due to the limited masses of drug that can be absorbed from these sites.
[ACCC 3.36, p 284]
299 Professor Pouton concluded thus:
To a large extent the Altman report makes generally [sic] statements that are factually correct with regard to the possible advantages of buccal and nasal drug delivery. However, the statements lack practical perspective, in that clinically useful doses of most drugs could not be absorbed from these sites of administration. Furthermore there is no evidence presented in the report that the needs of patients suffering from erectile dysfunction or premature ejaculation cannot be met by existing proprietary products.
[ACCC 3.36, p 284]
300 Professor Pouton’s report elicited responses from Dr Rowe and Dr Altman.
4.5.3.6.4 Dr Rowe and Dr Altman’s second reports
301 In a second report dated 27 November 2013, Dr Rowe responded to Professor Pouton’s report. He disagreed with Professor Pouton’s view that without clinical data, it was not possible to determine if the alternative delivery forms could achieve therapeutic effect with lower dosages than those used in the oral administration of the drugs, or whether they would result in a reduction in side effects. Dr Rowe gave a number of reasons for this disagreement. One reason involved reference to the practice of off-label prescribing. This occurs when a medication is prescribed for a use other than the use for which it was approved by the Therapeutic Goods Administration. Clomipramine and apomorphine were used off-label in the AMI and NRM medications.
302 He said that compounding with off-label medications was common in relation to pain treatment and was well accepted. He gave examples of the use of off-label prescribing. He said that compounding was used, for instance, where no suitable dosage form was available, such as for medication of infants who could not swallow medication in tablet form, where the dosage required by a particular patient was not commercially available, where production of a medication had been discontinued but was still necessary for some patients, or where a doctor considered a novel combination of drugs useful for some patients. He said that a major factor in the use of off-label compounds was the cost of obtaining Therapeutic Goods Administration approval for new therapeutic uses.
303 He then said:
23. Compounding is based upon a physician's experience. I disagree that clinical trials are the only way in which it possible [sic] to prove efficacy. In the context of compounding, one would be very unlikely to find clinical trials undertaken for the same dosage and pharmaceutical presentation.
24. In my practice, and in my experience, a particular dosage is chosen by the physician in the light of that doctor's previous experience including what that person's peers may have experienced. Should the dose be either too low to be effective or so high as to produce side effects then the dosage is adjusted to suit the patient.
[R13.37, pp 4 – 5]
304 In a second report dated 28 November 2013, Dr Altman also responded to Professor Pouton’s report. Dr Altman rejected Professor Pouton’s view of the extent of the first-pass effect on clomipramine and vardenafil taken in tablet form, and relied on further material to demonstrate that there was a problem which could be addressed by an alternative delivery system. He again referred to the recently approved orodispersible [orally disintegrating] tablet of vardenafil marketed as Staxyn, which resulted in a higher systemic exposure than the 10 mg tablet of vardenafil, as an example of the advantage to be obtained from changing the delivery system. He said that, if Professor Pouton intended to argue that the advantage in this case was not significant, he disagreed.
305 Dr Altman agreed with Professor Pouton that the buccal route would be suitable for relatively few drugs, but said that it had a definite place as a legitimate route of pharmaceutical delivery. He referred to two scientific articles which examined the use of buccal delivery for a number of drugs.
306 Dr Altman then elaborated on his argument, articulated in his first report, that off-label prescribing is legitimate by referring to an article published by Dr Madlen Gazarian and others entitled, “Off-label use of medicines: consensus recommendations for evaluating appropriateness,” (2006) 185 (10) Medical Journal of Australia 105 (Gazarian 2006) [R 13.38, p 105]. The article, written by a working group of the NSW Therapeutic Advisory Group described the development of a guide for clinicians in evaluating the appropriateness of medicines for off-label use. Dr Altman quoted from the article that, “off-label prescribing is not illegal and may sometimes be clinically appropriate”. The article cited surveys in which “the extent of off-label prescribing is reported to be between 7.5 and 40 per cent in adults and may be up to 90 per cent in some hospitalised paediatric patients”.
307 Dr Altman said that Professor Pouton’s views could be summed up by saying that in order to reliably determine whether a drug is safe and efficacious, clinical trials of a high international standard would need to be conducted. However, he said that whilst this is the usual pathway, the cost of developing a drug in this way was extremely high. He emphasised his view that it has been a long-standing practice for doctors to prescribe medications which are not available commercially and which need to be compounded [R 13.38, p 11].
308 Dr Altman noted that the widespread use of off-label prescribing had prompted the NSW Therapeutic Advisory Group to develop recommendations to guide and improve off-label prescribing, and the US Federal Food and Drug Administration to consider guidelines for the appropriate off-label use of drugs.
309 Dr Altman then referred to circumstances in which off-label prescribing has a valuable role to play. In view of the difficulty of conducting research on children, registered medications which are specifically and commercially produced for them are often not available so doctors are forced to prescribe off-label. In other cases the market is not large enough to justify the commercial extension of the drug to other uses or age groups. Then there are cases where a patient has a serious illness, where there is no therapeutic alternative, and where the benefits outweigh the risks in the particular case. Individual circumstances then justify the use of off-label medications.
310 Dr Altman relied on the following view, expressed in an article by Dr Randall Stafford entitled, “Regulating Off-Label Drug Use – Rethinking the role of the FDA” (2008) 358(14) New England Journal of Medicine 1427, that:
Physicians' freedom to prescribe drugs off-label carries important advantages. It permits innovation in clinical practice, particularly when approved treatments have failed. It offers patients and physicians earlier access to potentially valuable medications and allows physicians to adopt new practices based on emerging evidence.
[R13.38, p 9]
311 This article however continued by stating that, “[a]t the same time, off-label use has potentially negative consequences. It undercuts expectations that drug safety and efficacy have been fully evaluated.”
4.5.3.6.5 Cross-examination of Dr Rowe and Dr Altman
312 In cross-examination Dr Rowe explained that when he compounded prescriptions for AMI the original dosages were modified when Dr Vaisman told him about feedback from patients, for instance, about side effects. The following exchange occurred during cross-examination:
MS NICHOLS: [Y]ou’re not aware of any clinical data to support any of AMIs compounded products, are you?
DR ROWE: I’m certainly aware of clinical data based on years of these products being available to patients.
MS NICHOLS: Well, that data is in the form of anecdotal reports to [sic] you have about what AMIs patient group – or how AMIs patient group is responding to the drugs, isn’t it?
DR ROWE: Yes, that’s correct.
[TS 2511]
313 Dr Rowe told the Court that he had been informed by Dr Vaisman that the repeat prescriptions were at about 67 to 70 per cent of patients [TS 2510]. There was no direct evidence from the respondents that this was the case, or the reason for it, and without further detail of the basis of the reports, this evidence does not assist. For example, other evidence seems to suggest that repeat deliveries of the AMI medications were made automatically, without any request from the patient. If this is what was meant by repeats, then it does not establish that patients necessarily wished to take more of the AMI medications.
314 Dr Rowe also provided further details about the collaboration with Dr Vaisman on the vardenafil nebuliser trial referred to at [282] of these reasons. He said the trial was a phase-one clinical trial intended as the first step in the possible registration of the medication delivered by nebuliser. The trial cost of $200,000 was paid for by AMI. It involved 12 subjects and was a double-blind, double cross-over (involving the same patients on both placebo and medication) study done according to good clinical practice.
315 In cross-examination, Dr Rowe explained his view about the therapeutic effect of an alternative delivery system in terms which were less emphatic than in his written reports. The following exchanges highlight the point:
DR ROWE: [T]hese [alternative] systems are generally designed to have a quicker onset of action, reduce side effects, avoid the first-pass effect, avoid gastric acid and so forth. They don’t work in every case. What I’m saying here is that it would be reasonable – given the fact that these are known and this is how they work it would [be] reasonable to use existing drugs in these delivery systems and see how they work from a compounding viewpoint.
…
MS NICHOLS: When you deal with compounding you’re necessarily relying upon, as you say, the physician’s experience and his or her relationship with the particular patient to form a view about efficacy in a particular case?
DR ROWE: In that instance that’s correct, yes.
[TS 2513]
316 Dr Rowe confirmed that it would not be possible to know how much of a dose of a drug reached systemic circulation in the body unless the patient’s blood plasma levels were tested [TS 2501]. He also confirmed that:
As far as I’m aware, and I certainly haven’t conducted it, that there are no plasma studies done on the amount of the drug which was delivered to the circulatory system via the – a nasal delivery system. The only thing I can say is that when, for example, we were developing clomipramine, based on clinical response of 5 patients, we were able to reduce the dose to about 20 per cent of what was given – what was given previously by the oral route. That was based on clinical response and not plasma levels.
[TS 2502]
317 Further, Dr Rowe said that because off-label prescribing depended on the doctor’s clinical judgment, it was important for the doctor to monitor the efficacy of the medication and its side effects. He was not, however, involved in any such process, as was revealed in the following exchange:
MS NICHOLS: And you’re not in a position to say what AMI doctors did or didn’t do in relation to questioning patients about side effects, or the efficacy of the drugs with which they were administered?
DR ROWE: I’m not in a position to comment on that, no.
[TS 2516]
318 In cross-examination, Dr Altman accepted that he was not aware of the formulations of the AMI or NRM medications or of their performance. He explained less emphatically than in his report the basis of his views as follows:
MS NICHOLS: Doctor, to be clear, leaving aside the nebuliser study concerning vardenafil, you can’t say one way or the other whether any of the compounds discussed in your report, or mentioned in your report, has any particular therapeutic effect, can you?
DR ALTMAN: I have no knowledge of the clinical performance. I’m not a clinician, and I’m not a prescriber, so I’ve never prescribed any of these formulations. I don’t know how patients react to them. All I can say is that, from the list, it appears as if AMI have used fundamental pharmacokinetic principles. They’ve chosen drugs often that have high first pass effect, and they’ve chosen to formulate these drugs in unique dosage forms, which have the potential to have a clinical effect.
MS NICHOLS: So it’s a potential, but it’s – to be clear – not to your knowledge, tested?
DR ALTMAN: I have no knowledge of the clinical data, or the patient response rates to these drugs. I have no knowledge of that at all.
[TS 2540]
319 Dr Altman reiterated his agreement with Professor Pouton that few drugs would reach therapeutic level, or have a faster onset than oral administration, by using the buccal route, because of the limited amount of drug which can be absorbed at that site [TS 2540 – 2541]. Dr Altman agreed with the following extract from an article annexed to his second report by Amir Shojaei entitled, “Buccal Mucosa As A Route For Systemic Drug Delivery: A Review” (1998) 1(1) Journal of Pharmacy and Pharmaceutical Sciences 15:
The nasal cavity as a site for systemic drug delivery has been investigated by many research groups and the route has already reached commercial status with several drugs including LHRH and calcitonin. However, the potential irritation and the irreversible damage to the ciliary action of the nasal cavity from chronic application of nasal dosage forms, as well as the large intra- and inter-subject variability in mucus secretion in the nasal mucosa, could significantly affect drug absorption from this site.
[R 13.38, p 79]
320 He also stated that he would assume that a doctor prescribing medication off-label would monitor the patient to see how the patient was going, and would change the dose depending on the clinical results seen in the patient reports [TS 2551].
321 The first reports of Dr Rowe and Dr Altman were written at a fairly high level of generality. At that level, it was possible for them to say that there was a theoretical pharmacological basis to support the efficacy of apomorphine and clomipramine delivered by the nasal route, the buccal route, or sublingually.
322 Both Dr Rowe and Dr Altman had previously had business relationships with AMI. Where it was possible to support the interests of the respondents in the course of their evidence, they were inclined to do so. It is not suggested that they compromised their professional integrity in the way they gave their evidence. For instance, Dr Altman made it clear in his first report that he had “no specific knowledge of the pharmaceutical performance of” the AMI and NRM nasal sprays or oral strips. In the end, the limitations on their evidence, which they accepted, rendered that evidence less useful than the evidence of Professor Pouton.
323 Professor Pouton was correct in his view that Dr Altman’s first report generally made statements which were factually correct, but related only to the possible effects of sublingual, buccal, or nasal delivery of the medications.
324 Professor Pouton’s report brought the issues down to a more particular level of discussion. Of central importance was his doubt that a sufficient quantity of the medications could be delivered by the nasal, sublingual, or buccal routes to have a therapeutic effect.
325 On this issue, Dr Altman, in his second report, agreed with Dr Pouton’s theoretical assessment. And again in cross-examination Dr Altman accepted this view. The following exchange demonstrates the point:
MS NICHOLS: In relation to the drugs that are delivered by the buccal route, Professor Pouton, whose report you’ve seen, states that medications designed for the buccal or oral administration – sorry, the buccal administration route can have a faster onset of action, but that advantage can’t be realised for most drugs due to the limited mass of drug that can be absorbed from that site. And that’s something you agree with in your report, isn’t it?
DR ALTMAN: I do, yes.
MS NICHOLS: And Professor Pouton says that, in fact, very few drugs would reach therapeutic levels using that delivery route, and that’s something with which you agree?
DR ALTMAN: Not many drugs, no.
MS NICHOLS: Yes. And you indicate that in your second report?
DR ALTMAN: Yes.
[TS 2540 – 2541]
326 Dr Rowe and Dr Altman had no clinical evidence of the efficacy of the AMI and NRM medications. In cross-examination, Dr Altman stated his opinion that:
[I]t appears to me that they’ve [AMI] gone through the literature, and they’ve picked a number of drugs that make sense to deliver via the routes that they’ve chosen. And that’s not to say that they would work by those routes, because I, as a pharmacologist, would say, well, I would like to prove that.”
[TS 2540]
When Dr Rowe altered the formulations of AMI medications for Dr Vaisman, he relied on the anecdotal evidence provided by Dr Vaisman to change the compounds. Dr Rowe said that there were no plasma studies done on the amount of medication delivered to the circulatory system by the nasal route. Excipients were added to the active ingredients of the AMI medications to provide bulk or to add to the therapeutic effect by facilitating absorption or solubility. This may have had an effect on the working of the active ingredient. Dr Altman had no knowledge of the excipients used by AMI and NRM in the medications.
327 In the end, Professor Pouton’s evidence that there is no scientific basis on which it can be concluded that the delivery of AMI and NRM medications through the nasal and buccal routes by nasal sprays, troches, or oral strips is effective should be accepted. A conclusion that the medications delivered in these ways were effective would be speculative.
4.5.3.7 Standards applicable to off-label prescribing
328 In this section, the standards applicable to off-label prescribing are examined. Then, these reasons for judgment consider whether AMI and NRM complied with these standards when doctors prescribed nasal spray, troches, and oral strips.
329 As discussed in the previous section, although Dr Rowe and Dr Altman had no knowledge of the clinical efficacy of AMI and NRM medications, they considered that the underlying pharmacology of the alternative delivery systems used in the AMI and NRM medications, and the assumptions that could be made about the medications because of this pharmacology, justified AMI and NRM prescribing those medications. The pharmacology suggested that the AMI and NRM delivery systems were chosen because they would have a therapeutic effect, would have the advantage of rapid onset of effect, and, because a lower dosage could be used, there would be an advantage of reduced side effects. Both doctors suggested that it was not necessary to have high-level clinical evidence for a doctor to be justified in prescribing a medication off-label.
330 Professor Pouton regarded the suggested advantages of the alternative delivery systems as less certain and expressed the view that AMI and NRM were not justified, in the state of existing knowledge, to prescribe the medications without some demonstrated evidence of efficacy and safety. This was so particularly he said, when the AMI and NRM medications were prescribed to patients off-label, to a large number of patients without consideration of their individual medical needs in an organised clinical way and without any real way of judging whether the medications were effective or not [TS 1210].
331 The respondents’ case was that off-label prescribing was widespread, accepted, legal, and justified when based on a doctor’s expertise and judgment. When AMI and NRM doctors prescribed registered medications delivered by novel delivery systems they were legally prescribing off-label, compounded products. The respondents criticised Professor Pouton’s standard that expensive clinical trials would need to be conducted in order to demonstrate efficacy [TS 2766 – 2767].
332 The respondents relied on the evidence of Dr Altman, who referred to Gazarian 2006, although he disagreed with the standards discussed in the article [R 13.38, p 105]. The article referred to a US survey of 150 million off-label prescriptions which found that 73 per cent of the prescriptions had little or no scientific support. The article then referred to a working group of a NSW government-funded body, the Therapeutic Advisory Group, which addressed the problems involved in off-label prescribing and made recommendations. The working group of ten included hospital-based doctors, pharmacists, and a representative from the Department of Health. The recommendations were implemented in 90 per cent of NSW public hospitals. The main recommendation was that off-label prescriptions should be limited to circumstances where there is high-quality evidence supporting the use of the drug. Whether there is high-quality evidence requires rigorous evaluation of the best available patient-based research, similar to that employed by the Therapeutic Goods Administration in evaluating a medication for registration. Where there is not high-quality evidence supporting the off-label use, the working group said that exceptional off-label use of a medication may be justified in individual circumstances, provided the following are satisfied:
• there is a serious underlying disease or condition; AND
• there is some evidence to support potential beneficial effect; AND
• potential benefits outweigh potential risks; AND
• standard therapy has been trialled or is inappropriate; AND
• written informed consent obtained.
333 The article explained the approach of the working group where there is extensive clinical experience to support off-label prescribing thus:
In some instances, high-quality research evidence supporting the use of a particular medicine (eg, older off-patent medicines) may not be available and may be unlikely ever to become available. However, there may be extensive experience supporting the efficacy and safety of such medicines. Although such data or “expert opinion” is considered to be of lower quality than high-quality research evidence, there are examples where it may be used to inform decisions about off-label use of a medicine. There are several authoritative medicines compendia that make recommendations for appropriate use supported either by research evidence and/or consensus opinion based on extensive experience with various medicines. These include the Australian medicines handbook, Therapeutic guidelines (Australia) and the British national formulary for children (UK). Other “authoritative” sources may include recommendations from professional societies, although the quality and validity of some of these can be quite variable. Less formal sources of support based on “experience” or “opinion” are less acceptable, and caution is recommended when considering this level of support for off-label use.
[R 13.38, p 107]
334 The working group recognised that some off-label prescribing may be justified by extensive experience or opinion, although a cautious approach needed to be taken.
335 In the present case, the respondents did not seek to justify the use of AMI and NRM medications on the basis of clinical experience. Rather, they relied on the opinions of Dr Rowe and Dr Altman who had no direct experience of the clinical effects of AMI or NRM medications. In the course of cross-examination Dr Vandeleur accepted that apomorphine and clomipramine nasal sprays were effective in some cases, but the source of this conclusion was not explored [TS 731]. His view cannot be regarded as the type of clinical evidence necessary to provide validation of the medication.
336 One is led to the inevitable conclusion that the respondents were not able to demonstrate from clinical experience that the medications did work. The respondents were in a position to demonstrate the efficacy of the medications if the medications were effective and safe, but they did not do so. Dr Vaisman referred in his evidence to his long experience with a very large number of patients of AMI and NRM. For instance, he said when pressed about a contrary view expressed in a published article about the need for a physical examination to treat ED or PE properly:
MR BURNSIDE: You disregard that or regard it as wrong, do you?
DR VAISMAN: I have big experience. I have big experience at any of this of others in the world.
MR BURNSIDE: I’m sorry, I can’t understand what you’re saying?
DR VAISMAN: I have bigger experience, my clinics have bigger experience in treating premature ejaculation, bigger than anybody in the world. I don’t publish.
[TS 1742]
337 There was evidence which is referred to in [528] – [529] and [533] – [534] of these reasons for judgment that AMI conducted surveys of its patients to ascertain the nature and frequency of side effects of the medications.
338 Further, AMI funded the trial of the delivery of vardenafil by nebuliser at a cost of $200,000.
339 There was also evidence of a survey done in 2008 by a salesperson, Wolfgang Rohr, which sought to establish why patients were dropping out of their treatment programs. The survey stated that it was based on a database presumably constituted from the records of AMI. The survey referred to reasons given by patients for giving up the treatment. It stated:
About 50% of dropouts claim they left because the treatment hadn’t worked.
[ACCC 4.383]
The survey also indicated that 50 per cent dropped out because the treatment was too costly for them. Although Dr Vaisman commissioned the survey, he sought to belittle its significance by saying that Mr Rohr was not a specialist in the area, and that he could have made up the figures. Dr Vaisman said that he paid no attention to the survey. Dr Vaisman’s evidence on this issue is improbable and should not be accepted. The survey demonstrated that AMI had data available which recorded what patients thought of the efficacy of the medications.
340 Further, in the response he provided to the ACCC following service on him of a notice under s 155 of the TPA to provide information, Mr Shrestha referred to a “patient feedback survey” conducted in 2003 to 2004 when AMI first introduced nasal-delivery medications into the market. He attached about 120 patient replies to his s 155 response [R13.12, p 127].
341 Mr Shrestha also referred to a clinical study conducted by AMI into the effectiveness of nasal spray from 1 May to 3 December 2003 from data relating to 12,558 patients. The survey and study were provided by Mr Shrestha in his first witness statement dated 7 September 2012 [R 13.14, p 1021], but no evidence was given about the substance of the testing. The material is not proof of the efficacy of the nasal spray, but it does demonstrate that the respondents were in a position to provide clinical material if they chose to do so.
342 Despite the capacity of the respondents to provide data demonstrating that the AMI and NRM medications did work, the respondents did not produce evidence of clinical experience that the medications were effective and safe.
343 Once it is accepted that there was no clinical evidence of the efficacy of the AMI and NRM medications, and that the theoretical claim for efficacy was speculative, there is no basis upon which to justify the prescribing of the AMI and NRM medications off-label. And, in accordance with Professor Pouton’s view, that is especially the case where AMI and NRM intended to prescribe the medications to a mass market without careful investigation of individual patients’ circumstances.
344 Although off-label prescribing is justified in some instances, such circumstances did not exist in the case of the apomorphine and clomipramine delivery forms used by AMI and NRM doctors because there was no evidence of the safety and efficacy over existing alternatives.
345 The following conclusions are based on the discussion in this section.
346 In practical terms, doctors engaged by AMI were required to prescribe apomorphine-based nasal spray for the treatment of ED, and clomipramine-based nasal spray for the treatment of PE.
347 About 28 of the Annexure B patients treated for ED were prescribed apomorphine-based nasal spray. About 76 of the Annexure B patients treated for PE were prescribed clomipramine-based nasal spray.
348 The accepted approach in the medical profession for the treatment of ED and PE, which was reflected in published treatment guidelines from authoritative bodies, was to use PDE5 inhibitors taken on-demand as the first-line treatment for ED, and SSRIs taken daily as the first-line treatment for primary PE.
349 Before the introduction of PDE5 inhibitors, apomorphine was used in the treatment of ED. Apomorphine was replaced as a first-line treatment because PDE5 inhibitors are more effective than apomorphine. When used in the past for the treatment of ED, apomorphine was taken on-demand and sublingually.
350 Clomipramine was used on-label as a treatment for depression. In the course of that use it was found to assist in the treatment of PE, and was used off-label for that purpose. However, when SSRIs were developed they replaced clomipramine as a first-line treatment for PE because, when paroxetine was taken daily, it proved more effective than clomipramine taken both daily or on-demand.
351 Whatever the effectiveness of apomorphine taken sublingually on-demand in the treatment of ED, or the effectiveness of clomipramine taken daily by tablet for the treatment of PE, there is no evidence that these medications administered by nasal spray or oral strip in much smaller doses is effective in the treatment of those conditions. Any potential effect of using the nasal, oral, or buccal routes for these medications is speculative.
352 The use of apomorphine and clomipramine in nasal sprays, troches, lozenges, and oral strips for ED and PE are off-label uses of those medications. Off-label use may be justified in certain circumstances. Those circumstances are recognised by the medical profession. The only potential circumstance relevant to the situation of AMI and NRM is where there is clinical evidence or a body of medical opinion recognising the efficacy and safety of the off-label use. A cautious approach is necessary in these circumstances. However, there is no body of clinical experience or medical opinion based on the scientific foundation which supports the off-label use of small doses of apomorphine or clomipramine in nasal spray or oral strips for the treatment of ED or PE respectively.
4.5.4 The conduct of the doctors
353 The ACCC alleged that the doctors engaged by AMI failed to treat patients in accordance with the professional requirements and standards applicable to the treatment of ED and PE. Much of this discussion is also relevant to the doctor consultations in the NRM period. That relevance is referred to in [783] – [836] of these reasons for judgment. Some elements of the doctor consultations in the NRM period are also dealt with in this section, because all of the NRM doctors conducting consultations with the Annexure C patients also consulted with Annexure B patients in the AMI period.
354 In particular the ACCC alleged that in consultations with Annexure B patients AMI doctors:
did not diagnose the underlying cause of the condition;
did not refer patients to a specialist or GP for the treatment of conditions disclosed in consultations;
did not, or did not adequately, explain the side effects of AMI medications to patients;
did not physically examine the patients, but consulted only by phone;
recommended long-term contracts without a proper medical basis for doing so; and
did not prescribe medications other than those formulated by and compounded for AMI, and did not disclose this fact to patients;
did not advise the patients of the terms on which the treatment programs were provided.
355 In each instance, the ACCC said that the conduct of the doctors failed to meet the standard of accepted medical practice, and preferred the commercial interests of AMI over the welfare of patients. The ACCC contended that these failures constituted unconscionable conduct.
356 Each of these alleged failures in the conduct of the doctors is addressed after first examining the source of the evidence concerning the conduct of the doctors, namely, the recordings of consultations, the statements of patients, the evidence of the doctors, and the expert medical evidence. Then, the reasons for judgment explain the general requirements accepted by the medical profession as reasonable for the professional treatment of ED and PE, before considering whether the doctors acted in accordance with those requirements.
357 In the respondent’s final written submissions they argued that the Court should not consider the conduct of the doctors as if it were a quasi-medical tribunal investigating the quality of medical services.
358 The task of the Court is to determine whether AMI and NRM engaged in unconscionable conduct arising, inter alia, from the way the doctors conducted consultations acting as consultants for AMI and NRM. That is a different question from questions which medical disciplinary tribunals are called upon to determine.
359 However, in the course of this very detailed consideration of the work of the AMI and NRM doctors it has become clear that the doctors did not meet professional medical standards. As the issues exposed in this case reveal there is a case for investigation by the medical regulatory body in view of the serious failings in the conduct of the AMI and NRM doctors it is appropriate that the Court bring these reasons for judgment to the attention of the appropriate regulatory agency.
4.5.4.2.1 Recordings and patients
360 In the AMI period phone calls with patients were recorded. Part of each of those phone calls recorded the consultation between the patient and the doctor. The ACCC selected 145 recordings of phone calls in the process described at [108] – [117] of these reasons for judgment. The audio recordings and transcripts of those 145 phone calls were tendered in evidence.
361 The ACCC also relied on witness statements or affidavits made by eight AMI patients. The phone call with one of those patients was also evidenced by one of the 145 recordings.
362 Thus, the ACCC relied on consultations by AMI doctors with the 152 Annexure B patients in total.
363 Four of those patients were cross-examined by counsel for the respondents.
364 In respect of the NRM period, the ACCC relied on written statements made by 16 patients of NRM. These patients are listed in Annexure C to the FASOC and hence are together referred to as the Annexure C patients. NRM did not record the phone calls with patients.
365 Seven of the NRM patients were cross-examined by counsel for the respondents.
366 There were 13 doctors involved in the consultations with Annexure B and C patients as follows:
Dr Balafas – 2 consultations;
Dr Berry – 32 consultations;
Dr Biswas – 1 consultation;
Dr Chan – 3 consultations;
Dr Condoleon – 2 consultations;
Dr Daood – 6 consultations;
Dr De Sayrah – 20 consultations;
Dr Durrani – 13 consultations;
Dr Goyer – 8 consultations;
Dr Lonergan – 51 consultations;
Dr Omar – 17 consultations;
Dr Quinney – 4 consultations;
Dr Vandeleur – 9 consultations.
367 Dr Lonergan and Dr Vandeleur affirmed affidavits and were called as witnesses for the ACCC. Dr Berry, Dr Paul George Condoleon and Dr Thomas Clement Goyer made statements and were called as witnesses for the respondents. The remaining eight doctors did not give evidence. Dr Gulpan Sarajsada, who was not involved in any of the consultations but is now engaged by NRM, made a witness statement which was filed on behalf of the respondents and was cross-examined. Her evidence was so general and unconnected to any of the consultations as to be of no particular relevance to this proceeding and is not referred to further in these reasons.
368 Counsel for the respondents asked that the names of the doctors involved in the consultations not be disclosed in these reasons for judgment. Counsel for the ACCC submitted that it was not necessary for the Court to name each of the doctors.
369 The Court must balance the value of open public scrutiny of professional conduct against the personal embarrassment and potential professional consequences to the doctors whose conduct has been criticised. There is a distinction to be drawn between the doctors who gave evidence, and who were thus given a full opportunity to explain their conduct, and the doctors who did not give evidence and thus did not explain their conduct.
370 In relation to the former category, there is no good reason to keep the names of the doctors confidential. Whilst their professional conduct has come under scrutiny, that scrutiny has occurred in a process that is public, and they have been able to defend their conduct in that public forum. Their points of view are recorded in these reasons for judgment. There is a greater value in public scrutiny of professional conduct, provided that the process is fair, than protection from personal embarrassment which may result from the public disclosure of the doctors’ conduct.
371 In relation to the latter category there is no explanation, except perhaps in the cases of Dr De Sayrah and Dr Durrani where it was said that sickness prevented them from attending Court, why the other doctors did not give evidence and whether they were invited to do so. It is unlikely that the doctors, including Dr Durrani and Dr De Sayrah, did not know of the proceeding and, hence, could have made any concern about publicity known to the Court. Whilst it would have been reassuring to know that each of these doctors had been invited to put their side of the story to the Court, their conduct is of sufficient public concern that their names should not be suppressed.
372 It is necessary to say something about each of the doctors who each gave evidence: Dr Berry, Dr Goyer, Dr Condoleon, Dr Lonergan, and Dr Vandeleur. The doctors were engaged by AMI and NRM pursuant to written agreements which designated them as consultants. The impression which they made in the witness box was one of the elements which has formed my views about what happened during, and the quality of, the consultations with patients by them.
373 Dr Berry qualified as a doctor at the University of Sydney in 1977 and has practised continuously since then. From mid-2006 until mid-2009, Dr Berry consulted for AMI full-time, five days per week. She did occasional other GP and hospital work in that period. At that time she worked from AMI’s premises. From mid-2009 until March 2012, Dr Berry consulted for AMI or NRM for two to three days per week. She worked from home where she now conducts a small homeopathic practice.
374 Dr Berry was involved in 32 of the 168 consultations in issue in the proceeding. From the recordings of her consultations, and from her oral evidence, it was plain that Dr Berry had care and concern for her patients. She also expressed a view that the work she did for AMI and NRM was worthwhile and professionally justified. That view is honestly held even though, as these reasons for judgment explain, it is misguided in most respects. Her talents deserved a better environment than the AMI or NRM operations and it is unfortunate that she did not appreciate that she was cooperating in a system which involved unprofessional practices. Dr Berry conceded that her conduct in a number of consultations was below the standard which she set for herself and which was generally accepted as appropriate in the medical profession. She recognised that her witness statements in some respects presented a picture of greater attention to the standards than was the fact. She also gave evidence that, since 2009 when the last recordings were made, she had changed some of the criticised deficiencies in her consultations in some cases as a result of the criticism, and in some cases as a result of her ever-developing knowledge of medicine. In part explanation for the examples of suboptimal conduct, Dr Berry maintained that the selection of consultations by the ACCC was not typical of her conduct at the time. However, the respondents did not provide any alternative selection from the many more recordings made at the time to support this claim.
375 Dr Berry was defensive in the witness box. In part that is explained by the uncomfortable experience of a longstanding professional whose conduct is under close critical evaluation in a public forum. But it is also explained by Dr Berry’s belief that her conduct could be explained, but that it was difficult to convey to non-medical people the multitude of factors which went into her consulting practices.
376 Dr Goyer qualified as a doctor at the University of Queensland in 2004. He had worked for AMI or NRM since 2008. In 2008 and 2009 he worked from the premises of AMI. Since 2010 he worked from his own premises four days a week. On the other day he worked in a clinic in the field of cosmetic, anti-aging, and wellness medicine. Unlike Dr Berry, Dr Goyer’s experience was relatively short and very narrow. Further, unlike Dr Berry, Dr Goyer displayed a limited degree of care or concern for his patients. For instance, in explaining his work for AMI he said in cross-examination:
[A]s a medical practitioner dealing in something which is not going to be a life threatening situation, no one dies of premature ejaculation. No one dies of erectile dysfunction. So this is a very different paradigm of medicine. What we’re dealing with here is lifestyle optimisation. Now, when it comes to lifestyle optimisation, we really have to adjust the way that we speak to people, as I do in cosmetic medicine. No one needs botox. No one dies of a wrinkle. So when I’m speaking about this medication to treat erectile dysfunction, we suggest medications. But we never tell people they will need it as I might if I were speaking to someone in emergency, who would have a heart attack, and I was telling them they would need a particular medication or they would die.
[TS 2320 - 2321]
377 He gave his evidence in an arrogant, obstructive, uncooperative and defensive way. When asked about his experience as a doctor, he was asked whether he practised as a GP outside of AMI. He replied “No. God, no. … Well, sorry, it’s a terrible job. I shouldn’t have said that, but no” [TS 2299]. He claimed to be “one of the most experienced clinicians, not just in Australia, but in the world, of speaking to people with these concerns” [TS 2360]. Yet his own colleagues at AMI, Dr Berry, Dr Condoleon, Dr Lonergan and Dr Vandeleur all had significantly more experience with AMI than he did. That is to say nothing of their much greater experience as doctors than Dr Goyer.
378 Early in his evidence Dr Goyer resisted giving a simple answer to junior counsel for the ACCC. I explained the Court process and how re-examination allowed for elaboration on some answers if necessary. Shortly afterwards he wound into a simple answer about the recordings of consultations an observation that the ACCC had “stolen” the recordings of the consultations from AMI. In fact, the recordings were obtained by the ACCC pursuant to a search warrant. The Court was adjourned so that counsel for the respondents could explain to Dr Goyer the need for decorum. On resumption, Dr Goyer appropriately apologised and explained, “I am not able to be comfortable … my legs are shaking under the table here. I am just trying to settle and I will promise to be more civil.” [TS 2311] A consideration of his oral evidence as a whole suggests that his discomfort in the witness box arose from a recognition that his practices were not readily defensible.
379 Dr Goyer understood that the job at AMI was not particularly demanding for a doctor because “no one dies of erectile dysfunction” and it was not as “terrible” as it would be to practice as a GP. The work was repetitious but paid him $1000 a day. Dr Goyer did not present as a doctor committed to patient care. He was involved in eight consultations in issue in this proceeding.
380 Dr Condoleon graduated as a doctor at the University of Sydney in 1987 and has practised continuously since 1988. He worked as a consultant for AMI full-time, five days per week from 1994 until 2000. At times between 2000 and 2008 he worked as a GP in a heart clinic in which Dr Vaisman had a commercial interest. From 2008 he has worked again as a consultant to AMI and NRM. In this period Dr Condoleon consulted by phone with patients who attended clinics, and with patients phoning in for reassessments of their treatment.
381 Dr Condoleon was responsive, straightforward, and business-like in giving his evidence. He held clear views which were generally expressed briefly and courteously with an assurance which came from of long experience. He provided treatment of ED and PE at AMI and NRM because he believed, on grounds he thought rational and valid, that there was a value to patients in the treatment provided.
382 Dr Condoleon was involved in two consultations in issue in this proceeding.
383 Dr Lonergan qualified as a doctor at the University of Sydney in 1974. From 1976 until 2002 he practised medicine for periods overseas as a GP and for 15 years in the casualty department at Johannesburg General Hospital. In 2002 Dr Lonergan returned to Australia to be near his daughter. Because he had let his Australian registration lapse, he did not qualify for Vocational Registration (VR) under a new system which had been introduced whilst he was away. As a result, his employment prospects were limited because the Medicare rebate for consultations with non-VR registered doctors was less than for VR-registered doctors. Dr Lonergan started working for AMI in 2002 and at that time consulted with patients face-to-face. From early 2003 he consulted almost exclusively by phone. He became dissatisfied with work for AMI, but continued because his non-VR status restricted his options and his flexible schedule allowed him to support his ex-wife, who had been diagnosed with breast cancer, and his daughter. His engagement with AMI was terminated by AMI on 14 December 2011.
384 Dr Lonergan was the fourth respondent in this proceeding. However, he settled the proceeding against him on 21 June 2012 and agreed to orders restraining him from engaging in the type of conduct which was alleged against him, and to declarations to the effect that such conduct was unconscionable. On the same day he affirmed his first affidavit in the proceeding. By this time Pattison Report 2 and McRae Report 2 had been filed. They contained detailed criticisms of five consultations conducted by Dr Lonergan. Further, the FASOC made allegations against Dr Lonergan in respect of 51 consultations. Dr Lonergan did not defend these consultations in detail in either of his two affidavits, the second of which was affirmed on 14 December 2012.
385 Counsel for the respondents cross-examined Dr Lonergan. Dr Lonergan said that he had prepared an explanation for each of the 51 consultations, but had concentrated on other matters which he thought were more important to the case. These were issues referred to in his affidavits about his disagreement with the conduct of the management of AMI. The Court invited counsel for the respondents to seek explanations from Dr Lonergan concerning each or some of the consultations. That invitation was not taken up. Instead, the respondents contended in final written submissions at [79]:
He [Dr Lonergan] did not give that evidence in chief. There is no onus on the respondent to elicit information from the ACCC’s witness to prove the ACCC’s case. The relevant Jones v Dunkel inference is that the evidence Dr Lonergan would have given would not have assisted the ACCC to prove unconscionability for these patients.
386 Senior counsel for the ACCC correctly submitted in final oral submissions that the principle in Jones v Dunkel (1959) 101 CLR 298 does not apply where, as in this case, a person is called as a witness. It applies where a person is not called as a witness.
387 Dr Vandeleur qualified as a doctor in 1996 and was registered with the NSW Medical Board in 1997. Since 2005 he has been a fellow of the Royal Australian College of General Practitioners. Before commencing to consult for AMI, Dr Vandeleur spent four years in Japan and then worked in hospitals and as a GP in Australia. In 2005 he worked for three days a week for AMI. Then, Dr Vandeleur worked for AMI for four days a week between September and December 2006. After that he worked full-time for AMI until 17 September 2009.
388 Dr Vandeleur resigned from AMI when he was served with a notice under s 155 of the TPA by the ACCC. When this proceeding was filed Dr Vandeleur was named as the fifth respondent. On 21 July 2011, the ACCC discontinued the proceeding against Dr Vandeleur in accordance with an agreement reached between them. The agreement provided that Dr Vandeleur would execute an enforceable undertaking under s 87B of the TPA and the ACL not to engage in the type of conduct alleged in this proceeding, and that he would affirm an affidavit in the proceeding prepared by the ACCC setting out the evidence he would give on behalf of the ACCC in terms acceptable to it.
389 Dr Vandeleur was involved in nine consultations in issue in this proceeding, one of which, the consultation with ED patient 28, was criticised in detail in McRae Report 2 and Pattison Report 2. His affidavits did not respond to this criticism but, like Dr Lonergan’s, focused on his disagreements with the management of AMI.
390 Dr Vandeleur gave evidence concerning the extent to which he was pressured or bound to prescribe the AMI medications, and to recommend to patients that treatment should be for 12 months or more. There were three sources of Dr Vandeleur’s evidence on these issues. First, his response to the s 155 notice, which was annexed to his first affidavit. Second, there was the evidence contained in his two affidavits affirmed on 27 October 2011 and 17 November 2012. And third, there was cross-examination of Dr Vandeleur by counsel for the respondents.
391 In relation to both issues Dr Vaisman contradicted the evidence of Dr Vandeleur and said that at all times these issues were matters for the independent clinical judgment of the doctors.
392 Several questions arose as to how Dr Vandeleur’s evidence should be viewed, and whether it should be preferred over the evidence of Dr Vaisman on these issues. The question of the recommended period of treatment provides a relevant vehicle to examine the question.
393 In his response to the s 155 notice served on him, Dr Vandeleur stated:
The management of AMI made it clear to me that they would prefer that I recommend at least 12 month treatment plans where possible; however, it remained open to me to recommend shorter programs or a short trial period, or no program or period, if I deemed it appropriate. I recommended 12 month treatment periods only where I felt that it was clinically appropriate; where I believed, based on my experience and clinical judgment that the patient would benefit from at least 12 months of treatment.
[ACCC 1.39, p 122]
394 In his first affidavit affirmed on 27 October 2011, Dr Vandeleur said:
41 AMI management made it clear to me that it was AMI's strong preference that I recommend that all patients should try the treatment for at least an initial period of at least 12 and preferably 18 months. That preference was communicated to me in several ways. During the course of doctors' meetings Jack Vaisman said that it was his preference for the doctors to recommend a 12 to 18 month treatment period. Separately, Dilip Shrestha told me that it was important that I mention "at least 12 months" during consultations with patients.
…
44 While it remained technically open to me to recommend shorter programs or no program or period at all, I concluded because of what had been communicated to me about management's preference, that I could not realistically work at AMI if I was not prepared to recommend at least 12 months to the patients I consulted.
…
47 I did not think that there was anything unsafe in the 12 month timeframe as such and accordingly reasoned at the time that I could make the recommendation. The only reason I recommended 12 months of medication was to comply with AMI's practices.
[ACCC 1.39, pp 11–12]
395 And in cross-examination, Dr Vandeleur said:
DR VANDELEUR: When it came to the 12 months, I had – the clinical coordinators were at me before Dilip, when I guess eventually it was – I really felt like I had to.
…
MR GREEN: Well, you only recommended 12 months, didn’t you, because that was what you thought was appropriate?
DR VANDELEUR: No, it was not the reason. I would never have mentioned 12 months if I hadn’t have been asked to mention 12 months.
[TS 740; TS 709]
396 There was a shift in Dr Vandeleur’s evidence from the position which he took in his response to the s 155 notice to the position that he took in cross-examination. The position in his response to the s 155 notice was closer to the evidence given by Dr Vaisman that the doctors had a free hand to decide the length of treatment and the medications to be prescribed.
397 However, when carefully examined, Dr Vandeleur’s evidence was in each instance consistent. The differences were a result of emphasising different aspects of the issue. Dr Vandeleur’s oral evidence of the practical pressure placed on him by Dr Vaisman and the management of AMI was persuasive. In some aspects it was supported by the evidence of other doctors. Whilst Dr Vaisman denied that, in practical terms, he directed the doctors to use apomorphine and clomipramine as first-line treatments for ED and PE respectively, and to recommend a 12-to-18 month treatment period, he did hold the view that those medications should be used as the first-line treatment and that they should be prescribed for 12-to-18 month periods. Dr Vaisman presented as a CEO who would enforce his views vigorously. When Dr Vandeleur provided his response to the s 155 notice, it was in his interest to emphasise to the ACCC that he had acted professionally and independently. Both his response to the s 155 notice and his affidavits were drafted by others. His oral evidence was his own authentic explanation. Furthermore, by the time he came to give evidence he had arrived at an agreement to settle the proceeding with the ACCC. It might reasonably be supposed that he then felt freer to emphasise the extent of control exercised by AMI over his prescribing conduct. I do not accept the suggestion made by the respondents that Dr Vandeleur’s oral evidence was inconsistent on these matters and that the earlier evidence was modified in his oral evidence as a result of the agreement reached between the ACCC and himself. Whilst the emphasis in the oral evidence was different, that evidence was credible and should be preferred over the contrary evidence of Dr Vaisman and Mr Shrestha on these issues.
398 In his response to the s 155 notice, Dr Vandeleur explained his process of conducting consultations with AMI patients. The explanation reflected proper professional standards in line with the requirements articulated by the expert medical evidence led by the ACCC. In his first affidavit Dr Vandeleur acknowledged that, on reflection, his consultations with Annexure B patients did not comply with those standards. Again, that acknowledgement, repeated in cross-examination, should be accepted as a truthful concession rather than a result of any agreement with the ACCC as a condition of resolving the proceeding with Dr Vandeleur.
399 Dr Pattison, Dr Roderick John McRae, and Dr Lester Walton were called as expert witnesses by the ACCC. Dr Pattison and Dr McRae each provided five written reports. Dr Walton provided one report.
400 Professor Currie was called as an expert witness by the respondents and provided two expert reports.
401 The expert evidence is best understood by following the development of that evidence in chronological order.
402 On 27 July 2011, Dr Pattison provided Pattison Report 1, which outlined the requirements for a proper medical consultation and for appropriate treatment of ED and PE. This has been referred to earlier in these reasons for judgment.
403 On 12 September 2011, Dr McRae provided his first report (McRae Report 1) [ACCC 3.31] which, inter alia, proffered his views on the standards, guidelines, or best-practice recommendations which govern medical practice.
404 On 15 November 2011 in Pattison Report 2, Dr Pattison considered the transcripts of 14 consultations and provided an opinion on the adequacy of each of them. Five of the consultations were by Dr Lonergan, and one each was by Dr Chan, Dr De Sayrah, Dr Vandeleur, Dr Daood, Dr Berry, Dr Goyer, Dr Quinney, Dr Durrani, and Dr Omar.
405 In his second report also dated 15 November 2011 (McRae Report 2) [ACCC 3.32], Dr McRae reviewed the transcripts of the 14 consultations also reviewed by Dr Pattison in Pattison Report 2.
406 On 25 April 2012 in Pattison Report 3 [ACCC 3.30], Dr Pattison, inter alia, reviewed four statements of NRM patients concerning one consultation each conducted by Dr Biswas, Dr Durrani, Dr Goyer, and Dr Omar.
407 In his third report dated 29 April 2012 (McRae Report 3) [ACCC 3.33], Dr McRae reviewed the statements of the consultations with three of the four NRM patients which were reviewed by Dr Pattison in Pattison Report 3, being those consultations by Dr Biswas, Dr Goyer, and Dr Omar.
408 In a report dated 26 April 2012 (Walton Report) [ACCC 3.35], Dr Walton addressed a number of issues including the appropriate steps that should be taken by a doctor in consulting with and prescribing medication to a patient.
409 In a statement dated 20 September 2012 (Berry Statement 1) [R 13.18], Dr Berry explained her consulting practices at AMI.
410 In Currie Report 1, Professor Currie expressed the view that Berry Statement 1 demonstrated that Dr Berry had generally complied with the requirements of good medical practice.
411 On 3 March 2013 in Pattison Report 4 [ACCC 3.44], Dr Pattison reviewed Berry Statement 1 and Currie Report 1, and provided his opinion on the audio and transcript records of six further consultations with patients by Dr Berry.
412 In his fourth report dated 19 March 2013 (McRae Report 4) [ACCC 3.45], Dr McRae reviewed Berry Statement 1 and Currie Report 1, and provided his opinion on the audio and transcript records of 27 consultations with patients by Dr Berry. Six of those consultations were the six consultations reviewed by Dr Pattison in Pattison Report 4.
413 In Berry Statement 2 dated 18 July 2013 [R 13.32], Dr Berry responded to Pattison Report 4 and McRae Report 4 and commented on the criticisms of each of the 27 consultations examined by Dr McRae in McRae Report 4.
414 On 31 October 2013 in Pattison Report 5 [ACCC 3.46], Dr Pattison responded to Berry Statement 2 both in respect of some general matters and to Dr Berry’s explanation of the six specific consultations which Dr Pattison had previously considered in Pattison Report 4.
415 In his fifth report dated 19 November 2013 (McRae Report 5) [ACCC 3. 47], Dr McRae responded to Berry Statement 2, including to Dr Berry’s explanations of the individual consultations previously criticised by Dr McRae in McRae Report 4.
416 In his second report dated 10 December 2013 (Currie Report 2) [R 13.39], Professor Currie responded to Pattison Reports 4 and 5, McRae Reports 4 and 5, and Berry Statement 2 in general terms. He did not deal with the individual consultations referred to by Dr Pattison and Dr McRae.
417 The qualifications of Dr Pattison have been set out earlier in these reasons for judgment at [221].
418 Dr McRae is a senior consultant anaesthetist and intensive care physician at Southern Health in Melbourne. He graduated as a doctor from Monash University in 1984. He has been the Chairman of the Council of the Federal Australian Medical Association (AMA) since 2009, and served in that position previously from 1999 until 2001. He is also a director of the Victorian Branch of the AMA. The objects of the AMA include:
[T]o advance good professional conduct and efficiency, to promote fair and honourable practice, to suppress, discourage or prevent malpractice or professional misconduct and to ensure the highest clinical, ethical and scientific standards in the delivery of health care to the community.
[ACCC 3.31, p 21]
419 Dr McRae has been a member of the AMA Ethics and Medico-legal Standing Committee since 1996. He was also a member of the writing group for the publication, “Good Medical Practice: A Code of Conduct for Doctors in Australia” (the Code). This Code was approved by the Medical Board of Australia under s 39 of the Schedule to the Health Practitioner Regulation National Law Act 2009 (Qld). The Schedule to the Queensland Act sets out the uniform national law regulating health practitioners (the National Law), which has been enacted in each State and Territory in substantially mirror terms. Section 39 of the National Law allows for National Boards, including the Medical Board of Australia, to develop and approve codes to provide guidance to registered health practitioners. The Code is also admissible in proceedings against such practitioners “as evidence of what constitutes appropriate professional conduct or practice for the health profession”: s 41 of the National Law. One aspect of the questions on which Dr McRae was asked to express views was the application of standards, guidelines, and best-practice recommendations relating to practice by medical practitioners to the conduct of AMI and NRM doctors. Dr McRae is also an admitted legal practitioner and part-time member of the Administrative Appeals Tribunal.
420 Dr McRae did not claim to be an expert in the treatment of ED and PE [TS 1349], but when challenged in cross-examination with the proposition that his long experience on ethics committees at hospitals at which he had worked was different to the expertise asked of him in this case he disagreed and said:
… I’ve regularly contemplated issues such as those that you’re describing [referring to the questions asked by the ACCC solicitors on which his views were sought]. And as a course [sic] of my studies and experience, I have above average knowledge in the area.
[TS 1341]
421 Dr McRae’s evidence supported his claim. Further, there was no challenge in the final submissions made by the respondents to his expertise in the areas on which he gave evidence. Needless to say, there were challenges by the respondents to the views he expressed.
422 Dr Walton is a forensic and general psychiatrist in private practice in Melbourne. He graduated in medicine in 1975 from the University of Otago in New Zealand. Since 1984 he has been a fellow of the Royal Australian and New Zealand College of Psychiatrists. In 1985 he completed a Diploma of Criminology at the University of Melbourne.
423 Professor Currie graduated as a doctor from the University of Melbourne in 1974. He practises as a specialist in neurology, behavioural neurology, addiction medicine, and psychiatry. He is a fellow of the Royal Australian College of Physicians and a fellow of the Australian Chapter of Addiction Medicine. He is the director of Addiction Medicine at St Vincent’s Hospital and a Professor of Medicine at the University of Melbourne. He has worked in the field of addiction medicine for 25 years. He is a member of the Australian National Council on Drugs, the principal advisory body to the Commonwealth Government on drug policy. Professor Currie is an active and expert clinician in the treatment of all aspects of addiction and drug abuse. He has particular expertise in off-label prescribing and the use of compounded alternative forms of medication. Because of the nature of the effects of drugs of addiction and the medication used to treat it, Professor Currie also has experience in the treatment of male and female sexual dysfunction. Professor Currie’s expertise was not challenged, save that the ACCC observed that he had never practised as a general practitioner.
424 A general observation should be made about the expert evidence of Dr Pattison and Dr McRae concerning the quality of the AMI and NRM doctors’ consultations on the one hand, and the evidence of Professor Currie on the other hand. The evidence of Dr Pattison and Dr McRae was based on reading the transcripts and listening to a significant number of recordings of consultations. Their witness statements provided a detailed critique of the consultations. Professor Currie approached the evidence at a higher level of generality. In that respect his evidence was of less assistance than that of Dr Pattison and Dr McRae.
425 More importantly, Professor Currie was not accurately briefed on some crucial matters. For instance, he wrongly believed that AMI and NRM doctors had available all medications used for the treatment of ED and PE and were not restricted in practice to prescribing medications developed by AMI and NRM containing apomorphine or clomipramine.
426 Professor Currie also accepted at face value some of the broad defences offered by Dr Berry concerning the quality of her consultations, and concluded that the consultations were generally acceptable. However, in cross-examination Dr Berry conceded that her witness statements were prepared before she had been given the recordings of the consultations and did not accurately reflect what actually occurred. Professor Currie had the transcripts of the consultations with Dr Berry, but seemed not to pick up the discrepancy between Dr Berry’s justification of the practices recorded in her witness statements and the events which occurred. Professor Currie extracted in Currie Report 1 passages from Berry Statement 1, for instance, concerning her practice of referring patients for treatment to their GP. Professor Currie approved of this aspect of the consultation. But Dr Berry resiled from her witness statement when asked in examination-in-chief whether it was correct in relation to referrals to GPs.
427 Although Professor Currie’s witness statement read as if he disagreed with Dr Pattison and Dr McRae on most issues, the final position was much less exactly defined. For example, whereas Professor Currie argued in his witness statement that physical examinations were not necessary for the diagnosis and treatment of ED and PE, in oral evidence his position was that although there were alternative methods of diagnosing and treating ED and PE, such as over the internet, he would not favour them himself. Rather, he saw them as possible rather than preferable alternatives. That said, the evidence of Dr Pattison and Dr McRae demonstrated a greater focus and deeper consideration of the issues which the Court needs to consider, and thus persuaded me to place greater weight on their opinions.
428 In final written submissions, the respondents submitted that the doctors engaged by AMI and NRM were experts in prescribing for the treatment of ED and PE, and suggested that their evidence on the subject should be preferred to the evidence of Dr Pattison who had only rare consultations with patients for ED and PE in his general practice.
429 Dr Pattison gave evidence that he saw about six to ten men each week on average for male sexual dysfunction. One of two of them would be new patients [TS 1007 and 2123]. He is well known for his interest in male sexual dysfunction and, consequently, other doctors often refer patients to him from areas outside the geographical area of his practice. The high quality of his evidence was referred to in [223] of these reasons for judgment.
430 The evidence of Dr Berry, Dr Condoleon, Dr Goyer, Dr Vandeleur, and Dr Lonergan did not compare favourably to the evidence of Dr Pattison. They each had a vested personal interest, to some extent, in the subject matter of the case. That made it unrealistic to expect them to engage with the issues in as objective and professional a way as Dr Pattison. They were to varying degrees required to defend their own conduct, whereas Dr Pattison was not. To a greater or lesser extent they were each defensive in the way they gave their evidence such that it did not have such an independent character which Dr Pattison’s evidence displayed. Coupled with his independence was Dr Pattison’s over 35 years of experience as a general practitioner, and his particular interest, reputation, and expertise in the area of male sexual dysfunction.
431 Counsel for the respondents did not differentiate among the AMI and NRM doctors whose expertise was said to eclipse Dr Pattison’s. However, the quality of their consultations and their evidence varied. For various reasons none of them created a favourable impression in the witness box. Dr Goyer created a particularly poor impression as mentioned earlier in these reasons. When faced with the views expressed in an article by Dr Waldinger, who is a recognised expert in the area, Dr Goyer said:
Well, put it this way, as I said initially, I would have spoken overall to over – over 10,000 people for these concerns. Now, at the age 35, that makes me one of the most experienced clinicians, not just in Australia, but in the world, of speaking to people with these concerns.
[TS 2360]
432 Dr Goyer graduated in 2004 and has worked for AMI and NRM since 2008. Compared with Dr Pattison, his experience of medicine is short and limited. His training came from Dr Vaisman, who, as will be seen, did not equip Dr Goyer with a proper education about ED and PE. Whilst Dr Berry, Dr Condoleon, Dr Lonergan, and Dr Vandeleur did not make claims to expertise as outlandish as Dr Goyer, Dr Pattison’s evidence generally provided a much firmer foundation of reliability than the evidence of those doctors.
433 Dr Pattison had 35 years’ experience as a GP and a particular interest and reputation in treating male sexual dysfunction. There is no basis for doubting his expertise.
4.5.4.3 The requirements for a reasonable standard of consultation for the treatment of ED and PE
434 The principles of good medical practice are set out in the Code. The Code was developed by the Australian Medical Council and the Medical Board of Australia. Since 2010, when the national scheme for the regulation of health professionals was implemented, the Medical Board of Australia has been responsible for the registration of medical practitioners and students and for the supervision of their professional conduct. The Code was a joint project of the Australian Medical Council and the former State and Territory medical boards. It brought together the standards which had been operating in each jurisdiction before the publication of the Code, and therefore reflects the standards applicable in the AMI period. The Code drew on similar documents formulated in the United States, the United Kingdom, Canada, and New Zealand. Dr McRae described the Code as:
[A] single nationally applicable guideline document representing the collective consideration from all Australian jurisdictions of the expected ethical conduct of registered medical practitioners by their then operating jurisdictional medical boards that had existed in the years prior to its publication.
[ACCC 3.31, p 23]
435 The Code was approved by the Medical Board of Australia in 2010 under s 39 of the National Law, with the consequence that it is admissible in disciplinary proceedings against doctors “as evidence of what constitutes appropriate professional conduct or practice for the health profession”: s 41 of the National Law. The Code outlines this aspect of its purpose thus:
To assist medical boards in their role of protecting the public, by setting and maintaining standards of medical practice. If your professional conduct varies significantly from this standard, you should be prepared to explain and justify your decisions and actions. Serious or repeated failure to meet these standards may have consequences for your medical registration.
[ACCC 3.31, p 62]
436 But the Code also outlined that it was to be used:
To support individual doctors in the challenging task of providing good medical care and fulfilling their professional roles, and to provide a framework to guide professional judgment.
[ACCC 3.31, p 62]
437 Whilst the Code addressed a wide variety of aspects of medical practice, the obligations most relevant to this proceeding were as follows:
1.4 Professional values and qualities of doctors
While individual doctors have their own personal beliefs and values, there are certain professional values on which all doctors are expected to base their practice.
Doctors have a duty to make the care of patients their first concern and to practise medicine safely and effectively. They must be ethical and trustworthy.
Patients trust their doctors because they believe that, in addition to being competent, their doctor will not take advantage of them and will display qualities such as integrity, truthfulness, dependability and compassion. Patients also rely on their doctors to protect their confidentiality.
Doctors have a responsibility to protect and promote the health of individuals and the community.
…
Good communication underpins every aspect of good medical practice.
Professionalism embodies all the qualities described here, and includes self-awareness and self-reflection. Doctors are expected to reflect regularly on whether they are practising effectively, on what is happening in their relationships with patients and colleagues, and on their own health and wellbeing. They have a duty to keep their skills and knowledge up to date, refine and develop their clinical judgment as they gain experience, and contribute to their profession.
2 Providing good care
2.1 Introduction
In clinical practice, the care of your patient is your primary concern. Providing good patient care includes:
2.1.1 Assessing the patient, taking into account the history, the patient’s views, and an appropriate physical examination. The history includes relevant psychological, social and cultural aspects.
2.1.2 Formulating and implementing a suitable management plan (including arranging investigations and providing treatment and advice).
2.1.3 Facilitating coordination and continuity of care.
2.1.4 Referring a patient to another practitioner when this is in the patient's best interests.
2.1.5 Recognising and respecting patients' rights to make their own decisions.
2.2 Good patient care
Maintaining a high level of medical competence and professional conduct is essential for good patient care. Good medical practice involves:
2.2.1 Recognising and working within the limits of your competence and scope of practice.
2.2.2 Ensuring that you have adequate knowledge and skills to provide safe clinical care.
2.2.3 Maintaining adequate records (see Section 8.4).
2.2.4 Considering the balance of benefit and harm in all clinical-management decisions.
2.2.5 Communicating effectively with patients (see Section 3.3).
2.2.6 Providing treatment options based on the best available information.
2.2.7 Taking steps to alleviate patient symptoms and distress, whether or not a cure is possible.
2.2.8 Supporting the patient's right to seek a second opinion.
2.2.9 Consulting and taking advice from colleagues, when appropriate.
2.2.10 Making responsible and effective use of the resources available to you (see Section 5.2).
2.2.11 Encouraging patients to take interest in, and responsibility for, the management of their health, and supporting them in this.
2.2.12 Ensuring that your personal views do not adversely affect the care of your patient.
3 Working with Patients
3.1 Introduction
Relationships based on openness, trust and good communication will enable you to work in partnership with your patients.
3.2 Doctor-patient partnership
A good doctor-patient partnership requires high standards of professional conduct. This involves:
3.2.1 Being courteous, respectful, compassionate and honest
3.2.2 Treating each patient as an individual.
3.2.3 Protecting patients' privacy and right to confidentiality, unless release of information is required by law or by public-interest considerations.
3.2.4 Encouraging and supporting patients and when relevant, their carer or family, in caring for themselves and managing their health.
3.2.5 Encouraging and supporting patients to be well informed about their health and to use this information wisely when they are making decisions.
3.2.6 Recognising that there is a power imbalance in the doctor-patient relationship, and not exploiting patients physically, emotionally, sexually or financially.
3.3 Effective communication
An important part of the doctor-patient relationship is effective communication. This involves:
3.3.1 Listening to patients, asking for and respecting their views about their health, and responding to their concerns and preferences.
3.3.2 Encouraging patients to tell you about their condition and how they are currently managing it, including any alternative or complementary therapies they are using.
3.3.3 Informing patients of the nature of, and need for, all aspects of their clinical management, including examination and investigations, and giving them adequate opportunity to question or refuse intervention and treatment.
3.3.4 Discussing with patients their condition and the available management options, including their potential benefit and harm.
3.3.5 Endeavouring to confirm that your patient understands what you have said.
3.3.6 Ensuring that patients are informed of the material risks associated with any part of the proposed management plan.
3.3.7 Responding to patients' questions and keeping them informed about their clinical progress.
…
[ACCC 3.31, pp 62 – 66]
438 It is immediately obvious that these principles are expressed in general terms. They are each capable of accommodating a spectrum of conduct. The Code applied to the AMI and NRM doctors involved in this proceeding, as acknowledged by Dr Berry in Berry Statement 1 [R 13.18, [64]]. The value to the Court of the expert opinions expressed in the evidence was to give a practical content to the general guidelines. As in many professions the boundaries of good conduct are identifiable by practitioners, even if difficult to articulate in the form of a set of concrete rules. The importance of the Code is underscored by the function provided to it by the National Law. At the same time, the foundational nature of the Code to the practice of medicine confers an obvious significance to it in the assessment of the conduct of the doctors in this case.
439 The way in which the general obligations of the Code translate into the proper way of treating ED and PE is demonstrated in the explanation of treatment provided by Dr Pattison in Pattison Report 1.
440 In common with medical treatment generally, Dr Pattison explained that there are five recognised steps in the treatment of ED and PE, namely, history, medical examination, diagnosis, treatment and follow-up.
441 ED and PE must be viewed separately because they raise different issues at each step. Dr Pattison defined each condition and then described what constituted reasonable professional conduct at each step.
442 ED, Dr Pattison said, can be defined as the inability to achieve an erection of sufficient rigidity for satisfactory sexual activity and intercourse.
443 Taking a history involves identifying the problems. For ED the doctor must make enquiries such as:
What has the patient or client actually noticed? Is the problem actually ED? Is it present all the time? Is he having difficulty achieving an erection or is it subsiding during intercourse? How long has the ED been present? Did the ED appear suddenly or has it gradually evolved? How severe is the condition? Does it make it impossible for him to have satisfactory sex? What impact is the ED having on him and his sexual partner(s)? Is he able to achieve a satisfactory erection with self-stimulation? Is he having early morning erections as previously? Are there any relationship issues that could be contributing to the ED? Are there any major stresses at work or at home? What is the state of his general health? Is he a smoker or does he drink alcohol to excess? Has he ever been treated for ED before? Has he ever had treatment for any prostate problems? Are there any co-existent health problems such as hypertension, diabetes or heart disease? What medications is he taking? What about other drugs eg over-the-counter medications from the chemist?
[ACCC 3.28, p 19]
444 Dr Pattison said that a proper medical examination is essential in assessing a patient with ED. He said:
A brief general examination should be undertaken with calculation of weight, waist circumference or other measure of obesity such as BMI (Body Mass Index). The arterial circulation and peripheral pulses should be checked. The genitalia (penis and testicles) should also be examined and a DRE (digital rectal examination) and prostate check might also be performed, particularly in men over 40 years.
[ACCC 3.28, p 20]
445 For ED, Dr Pattinson said that investigation should include a fasting blood sugar test to exclude diabetes, and a fasting cholesterol test to exclude underlying elevated cholesterol, a risk factor for arterial vascular disease. Other tests on the same blood sample might be done to test liver function, kidney function, thyroid function, a full blood examination, and a prostate specific antigen test for men over 40 – 50 to exclude prostate cancer.
446 As to treatment for ED, lifestyle changes to address risk factors such as being overweight, excessive consumption of alcohol, and stress can be discussed. Psychological counselling should also be considered. But it is unlikely that these measures alone would successfully treat ED without medication. First-line treatment with PDE5 inhibitors, Viagra, Levitra, and Cialis, have been discussed earlier in these reasons. Dr Pattison then addressed second-line treatment by vacuum devices and constriction rings, third-line treatment by self-administered intracavernosal injection with vasoactive agents, and fourth-line treatment by surgery. How each treatment works and the side effects should be discussed with the patient.
447 Finally, Dr Pattison said there should be a follow-up review to discuss the patient’s response to treatment. A review of about a month after prescribing a PDE5 inhibitor is fairly standard.
448 Dr Pattison defined PE as ejaculation that occurs within one minute or so of the penis being inserted into the vagina. The time from the penis being inserted into the vagina until ejaculation is called the intra-vaginal ejaculatory latency time or IELT. However, its significance depends on the degree of distress it causes to one or both partners. Dr Pattison referred to the American Urology Association, which now recommends that PE be diagnosed on the man’s reported reduced control of ejaculation, in association with patient and partner dissatisfaction and also the reduced IELT [ACCC 3.28, p 25].
449 The world range of average IELT times is three to seven minutes. Dr Pattison said:
[T]here are limitations in defining PE with a stopwatch approach. Some couples are quite content with ejaculation occurring after 1-2 minutes. Other couples might not be satisfied if ejaculation occurs after 4-5 minutes. In general terms however an IELT of less than 1 or 2 minutes can be quite distressing for one or both partners. The American Urology Association now recommends that PE be diagnosed on the man's reported reduced control of ejaculation in association with patient and partner dissatisfaction and also the reduced IELT. According to these criteria PE affects 25-30% of men, with about 5-10% men having the more severe form of PE.
PE can be diagnosed on a subjective basis in the grey areas between obvious PE and obvious normality. For instance a man who ejaculates after 30 seconds has PE and both he and his partner are likely to be distressed by the situation. A man who ejaculates within 2-3 minutes may or may not be concerned. However if the condition is distressing him and his partner it is worthy of treatment. On the other hand, if a man ejaculates after 10 minutes of penetrative sex he clearly does not have PE, regardless of whether he or his partner would prefer a longer time for ejaculation to occur.
PE can be classified as primary PE when the patient has had this problem all his life and secondary or acquired PE when the patient was previously able to control ejaculation. Men with primary PE tend to be younger and might present in their twenties. Secondary PE is commonly associated with ED and sometimes it can difficult to clarify whether the patient has PE, ED or both conditions together.
[Emphasis added.]
[ACCC 3.28, p 25]
450 There were differences between the definition of PE adopted by Dr Pattison and the definition adopted by AMI and NRM doctors. In Berry Statement 2, Dr Berry set out the definition of PE which she provided to patients. She said in relation to her consultation with Annexure B patient 27:
126. I believe that this is an effective way in which to efficiently and appropriately diagnose a patient:
“Defining premature ejaculation is coming before you want to and usually entailing you needing to withdraw, think of England, or change position in order to maintain the time of your performance”...
127. Rather than characterising PE solely by reference to a period of time, I consider that a more useful (and widely accepted) way in which to define PE is by reference to “ejaculation that occurs sooner than desired, either before or shortly after penetration, causing distress to either one or both partners.”
[Emphasis added.]
[R 13.32, p 26]
451 In Pattison Report 5, Dr Pattison commented on the definition of PE adopted by Dr Berry, which was also the definition adopted by the American Urological Association in the AUA Guideline 2004. Dr Pattison said:
9. At paragraph 126 Dr Berry says that she tells patients that "premature ejaculation is coming before you want to." There are risks in conveying this definition to patients. Some men have the notion that the normal time between penetration and ejaculation might be 10-15 minutes or longer, as popularized by the media and erotic movies. Considerable worldwide research has been done to get a clearer assessment of what is a normal time between vaginal penetration and ejaculation. As stated in my earlier reports, the range of intravaginal ejaculatory latency times (IELT) in various world studies is between 3-7 minutes, with a median time of about 5.4 minutes. Although there are limitations in defining PE with a stopwatch approach, in general terms an ejaculation time of less than 1 minute can be regarded as PE, less than 2 minutes is possible PE, and beyond that is probably normal. Some men may prefer not to ejaculate for 15 minutes but that would hardly constitute PE and it would not be appropriate to treat these patients with medication. If one relied solely on the patient self-report of "coming before you want to" many more patients would be treated with medications than would be appropriate. In paragraph 127 Dr Berry states that a more useful definition of PE is "ejaculation that occurs sooner than desired, either before or shortly after penetration, causing distress to either one or both partners." This is the position statement of the American Urological Society [the AUA Guideline 2004]. I would accept this definition as long as "ejaculation before or shortly after penetration" is understood to mean ejaculation that occurs prior to, or within 1 minute of penetration.
[Emphasis added.]
[ACCC 3.46, p 14]
452 In cross-examination, Dr Pattison explained that there are disagreements about the definition of PE in the medical community. And he explained his preference for the definition of PE involving a temporal aspect as follows:
MR GREEN But here there are two elements. There is the shortly after, which is a vague chronological or time judged element, but then there’s the additional causing distress to either, so it means that as a qualifying element, there has to be not only the time element but also some judgment by the parties about the affect [sic] on them?
DR PATTISON: Yes. Consideration needs to be given to that, although in the papers that we discussed yesterday, people weren’t even talking about medication in cases that went beyond three minutes, for instance. I mean, I’ve had people coming to see me and say that they’ve got premature ejaculation and then they will state that they ejaculate after minutes and I think we need to be very wary about accepting that premature ejaculation is ejaculation that occurs sooner than desired.
MR GREEN: But doctor, what I’m putting to you is that a body of experts has promulgated a definition. It may be in dispute with you. You certainly don’t agree with it?
DR PATTISON: No, I don’t agree with it.
MR GREEN: Yes. And doctor, the reason that there is a dispute in the literature is, is it not, that without a stop watch or some sort of formal measure of timing, it is hard to compare clinical studies and it’s hard to compare the efficacy of different kinds of medication?
DR PATTISON: No.
MR GREEN: Do you accept that?
DR PATTISON: No, I don’t believe that. No. I think that when you ask a patient, do you – give me an idea of the time that you might – most people would say, well, pretty quickly or sometimes I’m not even to manage penetration. Then a starting point is to say, well, is it – would it be a minute and people will say, much less than that. Well then you’ve cut to the chase already and you know where you are but if somebody says, well, it could be five, it could be 10 minutes, it could be longer, then to me the likelihood is that we’re not dealing with premature ejaculation and I take except [sic] to that. In fact, as I said, I was at the meeting where Waldinger disputed this and it went on for quite some time and now, this is the difficulty we have and we haven’t even got agreement on definitions. That’s the whole point. We don’t have agreement and that makes the discussion rather difficult.
HIS HONOUR: I think what Mr Green is trying to explore is the reason why you prefer, or why it is preferred in the trade, the stop watch definition as distinct from this one?
DR PATTISON: Well, I think it’s because you can at least put a figure on something. You can get some measure and even at that first consultation or the second consultation after we’ve had the discussion with a patient, we will get a better idea of what we’re talking about. Patient satisfaction; I find that – and partner satisfaction. I find that that’s fraught with difficulties because, as I said, it will increase depending upon which ..... you’re looking at; the incidence of premature ejaculation up to 40 per cent.
MR GREEN: But doesn’t that, doctor, reflect the premise of medicine that you’re endeavouring to assist a patient, if you’re able to assist a patient in attending to a condition which they feel they have?
DR PATTISON: Quite frankly, Mr Green, most of the time when I’m talking to patients - people will actually come and they may say, look, I’ve got premature ejaculation and we have a discussion and it turns out that it’s 10 minutes. Often times a person is just totally relieved when I say that’s pretty normal, so reassurance can sometimes be – and quite frequently, when patients come to see me, particularly, some distressed young man with PE, I may just reassure them and send them on their way without any consideration of medication at all, so it’s a very disputed area.
[TS 1120]
453 The difference in the views of Dr Pattison and Dr Berry is reflected in some of the assessments made by Dr Pattison that particular patients who reported an IELT of more than two minutes may not have PE. The existence of the differing views at the least required the AMI and NRM doctors to consider the significance of a patient’s IELT.
454 PE is likely to be seen in younger patients and to have a degree of associated anxiety either as contributing to the problem or as a result of the PE.
455 In taking the history of a PE patient questions such as the following should be asked:
What has the patient or client noticed? Is the problem actually PE or is it within the realms of normal? Is there any associated ED? Approximately how long after insertion of the penis does ejaculation occur? When was the PE first noticed? Did it appear suddenly or has it gradually evolved? Have there been any previous sexual relationships? Was the PE a problem in those relationships? Does the PE cause the patient or partner any distress? Are there any pressures within the relationship? Are there any fertility problems? What is the state of his general health? Are there any psychological issues such as anxiety or depression? Are there any religious or cultural beliefs contributing to the problem?
[ACCC 3.28, p 26]
456 Dr Pattison then explained that:
A brief general examination is required and then a genitourinary check with examination of the penis and testicles.
Usually there is no abnormality to find clinically.
A digital rectal examination and prostate check might also be performed, particularly in cases of secondary PE.
As part of this general assessment, a brief evaluation of the patient's mood and mental state can be made by simple observation and engaging him in conversation.
This is quite relevant if a prescription for medication is likely to be required.
[ACCC 3.28, p 26]
457 Dr Pattison said that for PE few investigations are required. Some basic investigation should be arranged for secondary PE, or if ED is also present.
458 The appropriate treatment will depend on whether the condition is primary or secondary PE. In the mid-20th century, secondary PE was regarded as a purely psychological problem. Dr Pattison was of the opinion that nowadays:
PE can be regarded as a physical or physiological problem but one where there is frequently a strong psychological component, either contributing to the condition or resulting from it.
[ACCC 3.28, p 25]
Thus, it is recognised that there is a significant physiological element of learned behaviour. As discussed earlier in these reasons, SSRIs are the first-line and mainstay of treatment for primary PE. Although the treatment of PE can simply involve counselling, most men with primary PE require ongoing treatment with an SSRI. Secondary PE can be helped with counselling and behavioural techniques, without the need for medication. As a result, Dr Pattison was of the view that doctors should not limit the treatments for PE to pharmaceutical treatments. Focusing on the same issue, but with an emphasis applicable from his own speciality, Dr Walton said in his statement that “a thorough psychological assessment is required because many of the sexual dysfunctions are psychological in origin and therefore command psychological treatment rather than medication” [ACCC 3.35, p 15].
459 Finally, a follow-up is an essential part of the treatment for PE.
4.5.4.4 Diagnosis of the underlying causes and referral of patients to specialists or other doctors for diagnosis or treatment
4.5.4.4.1 The standard of treatment required
460 The proper treatment of ED or PE in the manner described by Dr Pattison required the AMI and NRM doctors to take a patient’s history and investigate the cause of the presenting condition.
461 Dr McRae held the same view. He said there was:
[A] requirement and expectation for the medical practitioner to determine the root cause of any presenting symptom, rather than dealing with the symptom per se itself. This may require additional investigations for an organic cause of a symptom, or assessment for a psychological component of illness.
It is my opinion that it is difficult to contemplate a circumstance when it would be appropriate for a medical practitioner to conduct a medical consultation (whether telephone based or face-to-face, or the first consultation or a subsequent consultation) with a patient on the basis that the medical practitioner will not seek to diagnose and treat (or refer for diagnosis or treatment) any underlying cause for the presenting condition. Should this set of circumstances arise, it is my opinion that the medical practitioner ought to state this to the patient and ensure that the patient comprehended that that set of circumstances is the basis of the consultation.
[ACCC 3.31, p 43]
462 Relying on these views, the ACCC contended that the AMI and NRM doctors were bound by a professional standard to diagnose and treat the underlying causes of ED or PE for which they were consulted. The ACCC contended that even if this were not so, the doctors were bound to determine whether to refer patients to a specialist or to another doctor for those causes or other presenting conditions of which they became aware.
463 The need to diagnose the underlying cause of the condition is especially important in the treatment of ED because, as was accepted by all parties, ED is often associated with cardiovascular disease and diabetes.
464 Thus, Dr Vaisman gave evidence as follows:
MR BURNSIDE: Yes. And you’re aware that erectile dysfunction and cardiovascular disease and coronary artery disease, for that matter, are associated with erectile dysfunction?
DR VAISMAN: Correct.
MR BURNSIDE: And erectile dysfunction can be an early marker of those other conditions?
DR VAISMAN: Correct.
MR BURNSIDE: Which makes it important, doesn’t it, for people with ED to be diagnosed to see whether they might have cardiovascular disease?
DR VAISMAN: Correct.
[TS 1716]
465 Dr Vaisman’s evidence in this respect was consistent with numerous scientific articles on which he relied as relevant to various issues in the case. On the present issue the relevant articles span the period from 1988 until 2010. For instance, in Fazio and Brock 2004, the authors wrote:
The most important component of diagnosing erectile dysfunction is obtaining a complete medical and sexual history. … Concurrent medical illnesses and any medications the patient may be taking should be reviewed. Erectile dysfunction is often a component of generalized medical illness and may represent the initial presentation of cardiovascular disease or diabetes. The history may also reveal certain reversible or modifiable risk factors, such as tobacco use or inadequate diabetes control.
[R 13.3, p 92]
See also: Montorsi and others “Can Phosphodiesterase Type 5 Inhibitors Cure Erectile Dysfunction?” (2006) 29 European Urology 979 (Montorsi 2006) [R13.5, p 33]; and Montorsi 2010 [R 1.1, p 3575].
466 In 1998, Dr Ridwan Shabsigh and others wrote an article entitled, “Evaluation of erectile impotence” (1998) 32(2) Journal of Urology 83 [R 1.3, p 261], in which they estimated that 50 per cent of ED cases had an organic origin, namely, diabetes, vascular disease, radical surgery, trauma, endocrine disease, multiple sclerosis, alcoholism, medications or renal failure.
467 In Hackett 2002, the author wrote:
A number of studies have clearly demonstrated an association between ischemic heart disease (IHD) and ED, and the likelihood that a newly presenting ED patient has undiagnosed IHD has been estimated at 40%.
[R 13.2, p 39]
468 Professor Currie also gave evidence of the correlation between ED and cardiovascular disease, but said that much evidence of the strength of the connection had arisen since 2009 [R13.39, p 7].
469 Dr Condoleon also agreed that ED is associated with cardiovascular disease.
470 Viewed as a whole, this evidence should be taken to support the conclusion that prior to 2009, and throughout the AMI period, the correlation between ED and cardiovascular disease was well known and a doctor treating a patient for ED should investigate whether there is an underlying cardiovascular disease.
471 In relation to PE, Dr Pattison said that PE has a strong psychological component which either contributes to the condition or results from it. His opinion was that counselling could be used as a treatment for secondary PE, and, in combination with medication, for primary PE. Although Dr Pattison said that there were few co-morbidities in relation to PE, he suggested that there may be prostate problems involved when a patient presented with PE [TS 2162].
472 The respondents’ case was that notwithstanding the link between ED and PE and other conditions, the AMI and NRM doctors did not have any professional responsibility to treat the underlying causes of the ED or PE. They had a limited role, namely, to ensure that it was safe to treat ED or PE for that patient with the AMI and NRM medications. It was for the patient’s GP or other specialists to treat the underlying causes and any other associated conditions.
473 Dr Berry explained her position in cross-examination thus:
MR BURNSIDE: Yes. But let’s deal with the “often is associated with other conditions” which AMI doesn’t treat. You would agree that cardiovascular problems generally are a comorbid condition seen with erectile dysfunction in a number of instances?
DR BERRY: Yes.
MR BURNSIDE: And so if a person presents with, for example, erectile dysfunction, obesity and smoking, it’s a fair bet they might also have cardiovascular problems?
DR BERRY: Yes.
MR BURNSIDE: They might also be diabetic?
DR BERRY: Yes.
MR BURNSIDE: And you’re not going to be doing anything to help their cardiovascular problem?
DR BERRY: No.
MR BURNSIDE: No. Or their diabetes?
DR BERRY: No. But those patients are being – I would be recommending to see their doctor.
MR BURNSIDE: Yes. Okay. And it would be poor practice on your part not to recommend that they see their doctor?
DR BERRY: Yes.
[TS 2410]
474 And addressing a slightly different question in cross-examination she elaborated on her role in the following way:
MR BURNSIDE: … Has it ever occurred to you that any of the patients who you’ve consulted on the telephone might have other medical problems which you’re not detecting and not treating?
DR BERRY: My main purpose in my consultation is to make sure that I’m safely prescribing and supporting a patient for what they’ve been – for what they’re ringing me to see. I’m not doing a general medical consult. As long as their condition is appropriate to be treated medically, according to what I’m doing, I do not have a problem with that. I’m not treating them for their full medical profile. I’m not a general practitioner.
MR BURNSIDE: All right. And it’s not your purpose, then, to warn them that they may have other medical problems which you will not be dealing with?
DR BERRY: No.
[TS 2396]
475 Emphasising that she was not responsible for treating underlying causes or other presenting conditions, Dr Berry responded in cross-examination as follows:
MR BURNSIDE: And, of course, as a doctor, if you saw a patient and realised that they had a condition which – or might have a condition which you were not proposing to treat – you would tell them to have it looked at by their GP?
DR BERRY: Yes.
MR BURNSIDE: And that way the risk of that condition is reduced, if they do, in fact, get it looked at by their GP?
DR BERRY: Yes. That’s not actually the role that I’m playing. But, yes, that’s correct. That’s what GPs do.
[TS 2456]
476 Dr Condoleon explained his view in cross-examination as follows:
MR BURNSIDE: And if those two things [being overweight and having a florid complexion] together presenting with ED come to you then you would think it’s at least possible that they have an underlying cardiovascular condition?
DR CONDOLEON: Well, it’s up to their GP to determine whether they have cardiovascular disease. That’s not my ---
MR BURNSIDE: Yes?
DR CONDOLEON: It’s in the same way if a person went to see a dermatologist or a – you know, a – any other sort of doctor, they – it’s the GPs domain to look after the – the weight and the health of their patient and give advice about that.
[TS 2266 - 2267]
477 Later, Dr Condoleon elaborated in cross-examination thus:
MR BURNSIDE: If a patient came to you and he presented a seriously overweight, a heavy smoker, with a blood pressure of 220 over 150, would you think it desirable to suggest that he see a GP about other possible conditions?
DR CONDOLEON: Absolutely, yes. Absolutely, yes.
MR BURNSIDE: And would you agree that it would be bad medical practice to overlook the real likelihood of other conditions which you’re not going to treat?
DR CONDOLEON: Some patients come in, we pick up if they’ve got medical conditions
MR BURNSIDE: Can you listen to the question? Would you agree it would be bad medical practice not to pay attention to the other conditions which you are not going to treat?
DR CONDOLEON: Yes. Yes, definitely, we pay – or I pay attention to the other medical conditions
MR BURNSIDE: And it would be bad medical practice ---?
DR CONDOLEON: --- and often as a consequence
MR BURNSIDE: Would be bad medical practice ---?
DR CONDOLEON: --- I don’t prescribe the medication. Sorry?
MR BURNSIDE: It would be bad medical practice not to tell the person to see their GP about what you suspect might lie beneath the surface?
DR CONDOLEON: There are certainly patients that I don’t prescribe medication to, that I tell to go and see their GP, because there’s concerns in their history that I think need to be dealt with, yes.
MR BURNSIDE: Yes. And when you say “concerns in the history”, that includes concerns that come about from obesity or high blood pressure?
DR CONDOLEON: Obesity is very, very low in the scheme of things, and – and so is blood pressure. It’s more to do with other medications that they’re on, or whether they’re – there’s complications, or they’ve got an infection, or whether they’ve got – some people come in and then they report they’ve got, you know, pain or they’ve got bleeding or they’ve got some other medical condition that I think warrants attention before they would consider sexual treatment. But being overweight is not as – is not a major issue in any sense.
MR BURNSIDE: It may not mean that you can’t prescribe, but it may indicate an underlying condition which you’re not going to treat, do you agree – do you agree?
DR CONDOLEON: Well, that’s what – that would be for the – that would be for the GP – the person has obviously seen their GP at some time, and they’ve been identified as being overweight, and there’s, you know, it’s not something that’s not apparent to a GP, and it’s up to the GP whether they do something about it.
MR BURNSIDE: Yes. Now, you say the person has seen their GP, but you don’t know that unless you ask them, do you?
DR CONDOLEON: Yes, we generally, it’s part of the form, is the last – when they’ve seen a GP, or, you know, if they’re on prescriptions. If they’re on medications, then they’ve obviously seen their GP recently, because how do you get a prescription?
[TS 2282]
478 On the nature of his role, Dr Goyer responded in cross-examination in the following way:
MS NICHOLS: And is it correct that your role at AMI is not to diagnose any comorbid diseases or to treat?
DR GOYER: It’s not that we’re not to diagnose them so much, Ms Nichols. It’s more that we’re not there to treat their heart problems or high blood pressure.
MS NICHOLS: Well, it’s not your role at AMI as you conceive it to completely – to do any form of diagnosis that can’t be done over the telephone?
DR GOYER: No. That’s not quite correct. We ask – it’s a very specialised area of practice, Ms Nichols. I mean, if you go to see an orthopaedic surgeon, he’s not going to ask you about your worst childhood memory, you know. Medicine is specialised, and we ask questions which are salient specifically for sexual dysfunction. Now, given that information that we get there are a lot of people given the fact that they do have comorbidities who are not appropriate for treatment, and they are referred back to specialists and GPs.
MS NICHOLS: So you don’t treat them if they’re not appropriate to be treated?
DR GOYER: Correct.
MS NICHOLS: But it’s not your role at AMI, is it, to fully diagnose any comorbid diseases?
DR GOYER: Not to fully diagnose, but to refer back to specialists and GPs who will take care of that, yes.
[TS 2337]
479 Even though the AMI and NRM doctors who gave evidence did not regard it as their responsibility to diagnose or treat underlying causes or other presenting conditions, Dr Berry said that she referred patients to a GP in certain circumstances. In Berry Statement 1, she said:
28. When I conduct patient histories and assessments, if I become aware of a condition that is not within the remit of AMI, I advise patients to consult their general practitioner.
…
30. During the consultations I have provided to patients while at AMI, I have always asked patients how long it has been since they last saw their doctor for a general check-up. If a patient has not had a general check-up in the last 12 months then, depending upon their medical history, medical condition, and age, I may require that they see their doctor for a physical consultation before I prescribe any medication.
31. If a patient has not seen their doctor for a general check-up in the last 12 months and they have a history of alcohol abuse, smoking, obesity or mental illness, then I frequently require that they see their doctor for a physical consultation before I am prepared to prescribe any medication.
[ACCC 3.45, pp 13-14]
480 In her oral evidence she corrected [30] of her first statement by adding the words “intended to” after the word “always” in the first sentence. It is likely that the correction became necessary in view of the evidence of the recordings which Dr Berry had not heard when she made her first statement. The recordings demonstrated that it was not Dr Berry’s invariable practice to ask patients how long it had been since their last check-up.
481 In the end it was the respondent’s evidence from Professor Currie which established that it was, at least, necessary for the AMI and NRM doctors to advise patients if the doctors detected symptoms of underlying causes or presenting conditions. Professor Currie gave the following evidence in cross-examination:
MR BURNSIDE: … But if you’re not going to treat it and you recognise it may be there, the very least you should do is say, “There’s a risk, and you should see a doctor”?
DR CURRIE: Yes.
MR BURNSIDE: And it would be bad practice not to say that?
DR CURRIE: It would be – again, I don’t say that it would be bad practice. That’s your phrasing not my phrasing.
MR BURNSIDE: Because the patient otherwise may not be aware at all that they’ve got a condition that could be dangerous?
DR CURRIE: Yes. And that is – exactly – and that is something which, as I’ve said in my second report, is suboptimal, but the concept that it is bad practice is not what I’ve said.
[TS 2596]
482 Professor Currie’s reference to his second report concerns his assessment in Currie Report 2 after reviewing the recordings of 28 patient consultations that, “some of the patient case transcripts certainly illustrate several areas of Dr Berry’s clinical practice, as it was undertaken in 2009, that were less than optimal and could be (and may now have been) improved” [R13.39, p 7]. Professor Currie said that, “current practice now would warrant the association of erectile dysfunction and cardiovascular risk being discusses [sic] with patients and advice given as to further referral or investigation” [R13.39, p 7]. Professor Currie based the requirement for current practice on the scientific literature which has been published since 2009. However, in view of his explanation in cross-examination that the link between ED and cardiovascular disease was well known before 2009, and the common ground in all the other evidence that this was so, the responsibility to advise patients on the link and to refer them to their GP, which Professor Currie articulated, applied throughout the AMI and NRM periods.
483 The view expressed by Dr Vandeleur of the obligations of the consulting doctors is also revealing. He described his practice during the consultations for AMI in the response he provided to the ACCC following service on him of the notice under s 155 of the TPA as follows:
If I was unable to provide, over the telephone, the care required by the patient, I advised the patient to consult a treating doctor (a general practitioner or a specialist not associated with AMI or its treatments, depending upon the situation) for further assessment and management.
I might use the example of patients who presented with ED and who had a medical history and/or symptomatology suggestive of significant cardiovascular disease. In cases like this, I felt that a history taken via telephone consultation would not be sufficient to ascertain the patient's cardiovascular status and that it would, therefore, be unsafe to prescribe any form of treatment which might put undue strain on the heart. In cases like this I explained to the patient why it would be unsafe for me to prescribe treatment based on his medical history and advised him to consult his treating doctor, usually a cardiologist, for further assessment.
Another common example was patients presenting with PE who had a history of epilepsy or was currently taking antidepressants. In both these instances the use of seretonergic [sic] medications (which are the standard treatment for PE) would generally be contraindicated. In such a case I advised the patient to consult a treating doctor, usually a specialist such as a psychiatrist or neurologist, for further assessment and treatment.
[ACCC 1.39, p 106 – 107]
484 These practices reflect what Dr Vandeleur regarded as the proper approach to be taken.
485 The obligation of doctors laid down by the Code “to make the care of patients their first concern” and to refer a patient to another practitioner when this is in the patient’s interest confirm the views of Dr Pattison, Dr McRae, Dr Vaisman, Professor Currie and Dr Vandeleur that the doctors had a duty to diagnose underlying causes of ED and PE or refer a patient to a specialist or a GP for diagnosis or treatment of those and other presenting conditions. The evidence of Dr Berry, Dr Condoleon, and Dr Goyer, to the extent to which it denied such a duty, should not be accepted.
4.5.4.4.2 The failure to diagnose underlying causes of ED and PE
486 The next issue is to examine how the AMI doctors actually discharged this responsibility concerning underlying causes in the consultations with Annexure B patients. The comments made in this section apply equally to the consultations with Annexure C patients by the same doctors who were then engaged by NRM, although transcripts of those recordings were not available. Those consultations are specifically discussed at [783] – [836] of these reasons for judgment.
487 The task is formidable because of the volume of material which constitutes the record of the 168 consultations put forward in the proceeding. It is also formidable because of the variety of circumstances which are presented in the consultations, and the divergences in approach among the 13 doctors involved.
488 The task was made easier by the assistance provided by the experts and in particular, by the detailed critique of 44 consultations by Dr McRae, and of 24 of those consultations by Dr Pattison. The detailed critiques allowed Dr Berry, Dr Condoleon, and Dr Goyer to respond by explaining their approaches in detail, and by reference to actual consultations.
489 Whilst the existence of the recordings allowed an unusual opportunity to assess both the content and the nuances in expression and approach of the doctors in the consultations, there was valuable independent expert input from Dr McRae and Dr Pattison arising from their experience in the practice of conducting consultations with patients. Professor Currie’s reports did not descend into the detail of each consultation and did not directly respond to the detailed, consultation-specific criticisms made by Dr McRae and Dr Pattison. As a result there was no independent assessment provided to the Court of the quality of the 168 consultations from the point of view of the respondents.
490 Throughout the course of the management of the pre-trial phases of the proceeding, and during the trial, I asked the parties to limit the number of consultations under review to a manageable selection. Despite those efforts, the parties were not able to propose some reduced number of examples to make their points. The ACCC provided the aide memoire, which selected passages from the transcript of each consultation with AMI patients relevant to a specified deficiency in the consultation and upon which it relied to establish its case of unconscionability. By organising the records of the consultations in this way the ACCC sought to assist the Court by confining the exercise of reviewing the consultations to the material in the aide memoire. Whilst the aide memoire was a useful document, it had some limitations because the selection of what was relevant to the assessment of a deficiency in a consultation is a matter of judgment. In some important areas the judgment adopted in the aide memoire was open to contention. Thus, for instance, there were a number of cases in which the aide memoire correctly stated that the doctor did not refer a patient to a GP for treatment of an underlying cause. However, the aide memoire did not reveal that the patient had indicated in the course of the consultation that he had already seen a GP for that condition or for relevant tests.
491 The scope and pattern of history taking and the style by which it was taken in the 152 consultations with Annexure B patients varied to some degree between different doctors. On the other hand, there was a high degree of uniformity in the way each doctor went about history taking in all of the consultations in which that doctor was involved. That was particularly evident in respect of doctors involved in larger numbers of the selected consultations such as Dr Lonergan and Dr Berry who were respectively involved in 51 and 32 consultations of the 168 put forward in the proceeding. The same trends were not discernible in respect of doctors involved in only a few selected consultations, such as Dr Chan and Dr Balafas who were involved in three and two consultations respectively. Where the volume of consultations disclosed a pattern, particularly from the records of the AMI period, there was a greater assurance that the particular consultation was not just one bad example.
492 The overwhelming impression gained from an examination of the records of the doctor consultations during the AMI period was the brevity and limited nature of the history taking.
493 An extraordinary example is the consultation of patient 46 with Dr Daood. The patient sought treatment for PE. The only information provided by the salesperson to Dr Daood was the patient’s name, date of birth, and that the patient sought treatment for PE. The patient was 45 years old. Dr Daood did not enquire into the nature of the problem, but went directly to the patient’s medical history. That took about 45 seconds before Dr Daood prescribed an unnamed nasal spray. The transcript of the history taking reveals the following:
DR DAOOD: Yeah. Hi, how are you?
PATIENT: Good, thank you.
DR DAOOD: So, yeah, you have that problem for a while now, huh?
PATIENT: Yeah, yeah.
DR DAOOD: Okay. And have you tried any medication before or first time?
PATIENT: I tried before.
DR DAOOD: Mm.
PATIENT: Yeah, but not long time.
DR DAOOD: Mm.
PATIENT: But for a short time.
DR DAOOD: Short time. What's your health like? Do you have any health problems?
PATIENT: I don't have any health problem.
DR DAOOD: So you don't take any medication for any reason?
PATIENT: No, no.
DR DAOOD: No. And, okay, we give you some spray you put in the nose about
half an hour before, two / three times a week.
[ACCC 4.289, pp 5 - 6]
494 It is noteworthy that the patient volunteered that he had tried medication. The doctor did not follow up this lead to ask what medication and whether it was successful.
495 In straightforward PE cases, Dr Berry typically commenced the consultation by establishing the problem. She then ran through a series of questions taking a history of illnesses or conditions for about one minute before agreeing to prescribe an AMI medication immediately afterwards. This process is seen, for example, in consultations with patient 47 and patient 133. The consultation with patient 94 was another PE patient consultation by Dr Berry, but the history taking took slightly longer. Dr Chan took just over two minutes with patient 6 and Dr De Sayrah took about two minutes with patient 22.
496 In ED cases the history taking tended to take longer. Dr Vandeleur took two minutes to obtain the medical history of 45-year-old ED patient 28 before prescribing medication. Dr Berry spent about three minutes taking a medical history before prescribing medication for ED patient 138, but spent about four minutes taking a medical history before prescribing medication to patient 110, a 43-year-old complex ED and PE patient.
497 The method of questioning by doctors was revealing. Not only were the medical histories taken in a short time, but some of the doctors left it to the patient to volunteer their history by asking general, open-ended questions. Thus, Dr Daood asked patient 45, “Do you have any health problems?” Dr Chan enquired about illnesses and conditions by asking the question “are you physically fit?” The consultation with PE patient 6 is an example, and the consultation with ED patient 16 is a similar example. Whilst Dr Chan followed up with more focused questions, the open-ended question was criticised by Dr McRae as an inadequate method for history taking. That is presumably because it does not focus on issues relevant to the particular situation. It supports the argument that the consultation was just going through the motions.
498 Dr Vandeleur asked two open-ended questions of patient 28, “Do you have any medical conditions at all?” and “You don’t have any abnormalities of the penis, do you, like bending or scarring or Peyronie’s disease?” He then asked whether the patient was a smoker. The only other medical questions asked by Dr Vandeleur related to the prescription of the AMI medications, such as whether the patient had allergies or intolerances.
499 Other doctors asked questions about a number of specific conditions. Thus, Dr De Sayrah asked PE patient 22 about prostate, thyroid, eye conditions, asthma, diabetes, epilepsy, blood pressure, heart problems, liver or kidney problems and hepatitis. She asked these questions in short phrases allowing the patient to consider several illnesses and to respond to each group separately. However, some other doctors strung together half a dozen conditions with no connection to each other and asked a number of questions in a series. Thus, an example is when Dr Omar asked PE patient 116, “Do you have any problem with the cholesterol, blood pressure, heart, lung, liver, kidney?” On the other hand Dr Lonergan made enquiries about a large number of conditions and asked about one or two at a time, allowing the patient time to respond to each question. Then, he asked whether the patient could think of any he had missed. Examples of Dr Lonergan’s approach are seen in ED patients 21 and 85.
500 In more than a few cases, enquiries which would be relevant to establishing underlying diseases were omitted. For instance, height and weight are relevant to risk factors for diseases underlying or related to ED, yet these matters were not obtained by Dr De Sayrah in consultation with ED patient 15. And Dr Vandeleur did not establish the height and weight of 45-year-old ED patient 28. Similarly in the case of PE patient 63 in a consultation with Dr Berry.
501 Then there were instances where patients raised issues which pointed to an underlying cause, but which the doctor did not pursue. Rather, the doctor moved on to prescribe an AMI medication. One example is 36-year-old ED patient 113 who also had secondary PE. When asked by Dr Goyer what was his primary problem he replied, “it’s actually more of an anxiety thing”. In his second report Dr McRae said of the consultation that Dr Goyer:
[F]ails to pursue psychiatric history of symptoms or potential treatments. It is my opinion that it would be good medical practice to further explore the possibility of psychiatric illness and possibly seek appropriate psychological or psychiatric assistance prior to commencing a line of treatment that is known to effect brain function.
[ACCC 3.32, p 321.1]
502 Dr McRae expressed the same view in relation to the consultation for PE with patient 151 by Dr Quinney. When asked about the problem, the patient said, “sometimes it happens, sometimes it doesn’t…I’m not sure if it’s more of a psychological thing” [ACCC 4.261, p 6].
503 ED patient 6 told Dr Lonergan that he woke with erections, and that, “I don’t think it’s physical to a degree.” Dr Lonergan replied, “You see it doesn’t matter why, what it proves is that the physical mechanisms necessary to get an erection… are well intact. So once you know that you, basically, already ruled out any major physical issues.” The doctor did not go on to explore any possible psychological causes of the problem. Then, patient 128 consulted Dr Berry for ED. He was 35 years old with mild ED over the past two to three years. He smoked 20 to 25 cigarettes a day and had a binge drinking habit of drinking 10 or more Red Bull and vodkas on Friday and Saturday nights. Dr Berry prescribed him apomorphine nasal spray and a gel. Dr Pattison would not have prescribed any medication until he had discussed with the patient the effect his heavy cigarette smoking and binge drinking would have on his ED. [ACCC 3.44, p 309]
504 Patient 98 consulted Dr Berry for longstanding PE and more recently developed ED [ACCC 4.376]. He was 38 years old. Dr Berry took his medical history in about one minute and then prescribed medication for PE. In the course of that history taking Dr Berry asked whether the patient had blood pressure problems. He answered in the positive and later indicated the medication he was taking. Dr Berry did not respond to his answer, but kept on with the checklist of medical conditions. Dr McRae suggested that Dr Berry did not register the patient’s answer [ACCC 3.45, p 715]. Dr Pattison said:
This patient is a smoker and has hypertension. Both these conditions can be associated with ED. The possibility of other underlying health problems such as diabetes, vascular disease and coronary artery disease should also be kept in mind.
I feel that this patient requires a detailed history and physical examination. He should also have some basic investigations such as a serum cholesterol and glucose level. Lifestyle issues such as his smoking and alcohol intake need to be addressed. I would probably not prescribe any medication at all until his basic investigations have been completed.
[ACCC 3.44, p 311]
505 In Berry Statement 2, Dr Berry said that she assumed that the patient had been fully assessed by his doctor and would have regular check-ups for re-prescription of his medications, and that the medication for PE would not affect blood pressure [R 13.32, para 217].
506 Patient 63 consulted Dr Berry for PE. Dr Berry asked him five short questions about his medical history and then prescribed clomipramine nasal spray. The patient stopped using the nasal spray within a few weeks as a result of soreness and bleeding. The Patient History Record kept by AMI shows that the patient had nasal surgery in 2008 [ACCC 13]. Dr Berry did not ascertain this when obtaining the medical history. Dr Berry responded in cross-examination in the following terms:
MR BURNSIDE: Now, would you agree that a person who had had nasal surgery the year before probably shouldn’t be prescribed a nasal spray?
DR BERRY: Yes.
MR BURNSIDE: And discovering that they had had nasal surgery would be part of a proper history taking?
DR BERRY: Yes.
MR BURNSIDE: Are you aware that this was a patient who dealt with you?
DR BERRY: Yes, you’ve told me that. Yes. So that was remiss.
…
MR BURNSIDE: Do you regard that as a thorough and appropriate medical history?
DR BERRY: Well, obviously I missed his nasal problem there, but as far as the actual medication goes he probably would be fine with it in an oral form. I’m just sorry I didn’t ask about the nasal approach.
[TS 2441 – 2442]
507 Patient 110 consulted Dr Berry for ED and PE. He was 43 years old, weighed 129 kg, was 194 cm tall, was a long-term smoker of 20 to 30 cigarettes per day, and was pre-diabetic. Before prescribing apomorphine nasal spray for 18 months, Dr Berry informed the patient of the following:
There’s no reason why you can’t use our medication, [Patient], and I seriously think, despite your diabetes, there’s a good chance we can actually turn this around because your figures are really good, because you have got the long term premature there, aggravating, or certainly as a predisposing factor to erection difficulties and you’re 43. So you’re [sic] weight is obviously, you know, not something that’s helping. While you’re working with your diet and getting fit, that’s going to be helping everything as well, okay, and the cigarettes long term won’t be helping either, but there’s no reason why we can’t use this medication and actually turn this around at this point, [Patient].
…
As I say, the things you’ve got that may make it more difficult is your cigarettes, certainly the alcohol on the nights you drink more, your weight. You know, you are obviously a bit overweight there and the tendency to diabetes… If you work with your fitness, the chances of you getting back to, you know, pre - how you were with this medication are good… with the figures that you’ve given me here today.
[ACCC 4.319, pp 10 -11]
508 The patient did not inform Dr Berry that he was consulting a GP or that he was working on his diet and fitness. Dr McRae noted that Dr Berry was not concerned by the caller’s high body mass index [ACCC 3.45, p 709]. Dr Pattison said that the patient being at least 30 kg overweight, a heavy smoker, and pre-diabetic were all possible underlying causes of his ED. He said that the patient was a high-risk cardiovascular patient whose ED symptoms were likely to get worse, even with optimum treatment. The onset of ED in a patient such as this ought to alert a doctor to the possibility of coronary artery disease. Dr Pattison said that this should have been specifically enquired about and that a number of basic medical investigations ought to have been undertaken before medication was prescribed. He also noted that this was a good opportunity to discuss ongoing lifestyle advice, and that increasing the patient’s fitness should be an important part of his management of ED [ACCC 3.44, p 308].
509 In more than a few instances doctors ignored important factors in the medical history of the patient and prescribed medication regardless. A stark example is the not isolated instances where a patient with PE complained of ejaculating too soon when the IELT was well beyond the normal. The proper diagnosis in such a situation was, according to the ACCC’s experts, to advise that the patient did not suffer PE.
510 Patient 6 consulted Dr Chan for PE. In Pattison Report 2, Dr Pattison expressed the following view about that consultation:
This 30 year old patient presented with the concern that he had PE. In fact, he is probably completely normal. He stated that he usually ejaculates 5-10 minutes after penetration. From data the world over this is in the normal range.
It was quite clear from the history that he was under a great deal of stress comparing his sexual performance to other people who stated that they could last 30-60 minutes. This patient really needed a discussion about what was normal and what was not normal. Reassurance and encouragement might have been all that was required in this particular case.
[ACCC 3.29, p 305]
511 Dr McRae said “[i]t is my opinion that the majority of medical practitioners would deem such a person to not require any intervention, and should be just reassured that he is normal” [ACCC 3.32, p 314].
512 Patient NRM 2 consulted Dr Goyer for PE. He told Dr Goyer that he lasted “generally no more than five minutes”. In Pattison Report 3, Dr Pattison said that:
It is quite possible that this patient does not actually have PE at all. His estimated time to ejaculation was generally less than five minutes. By any accepted criteria for PE this is within the normal range. Interestingly, his girlfriend later reassured him that he was normal and needed no treatment.
[ACCC 3.30, p 82]
513 Finally, although it is accepted that there is often a psychological element in the origin of PE, particularly secondary PE, there is no case which I could find in the 152 Annexure B consultations where that issue was raised and pursued with a suggestion that a patient be treated with counselling or other psychological attention, whether alone or in conjunction with medication.
514 Dr Berry, Dr Condoleon, and Dr Goyer each explained how history taking involves making judgments about what factors should be explored in each case. So the lack of enquiry about a particular matter may be explained by answers given in respect of other matters. For instance, it was not necessary to ask the question whether a person was seeing a GP regularly if the answers to questions about specific conditions such as blood pressure disclosed that the patient was receiving regular treatment. There are examples of such cases in the consultations with patients 6, 15, 16, 85, and 138.
515 A clear picture emerged from an examination of the consultations with the Annexure B patients. The brevity of the consultations, the very short time between history taking and prescribing, the open-ended way of asking questions about medical history, the failure to pursue issues raised by patients relevant to the cause of ED or PE, the omission to obtain relevant details of medical history, and prescribing medication where it was questionable that the patient had PE are all features which appeared very often. Indeed, the brevity of history taking and speed with which medications were prescribed existed in most of the consultations in question.
516 From the evidence of the consultations themselves and the analyses of Dr Pattison and Dr McRae, and taking into account the evidence of Dr Berry, Dr Goyer, and Dr Condoleon, including the impressions they made in the witness box, it should be concluded that the doctor consultations with Annexure B patients were undertaken only for the purpose of determining whether to prescribe medication. Dr McRae came to the conclusion in McRae Report 4 after his review of the 27 consultations of Dr Berry as follows:
I have obtained an overwhelming impression that the arrangement is constructed to ensure a medication that requires a registered medical practitioner's prescription receives sufficient attention to permit the prescription to be written. Much of the process, such as the rapid reading of pre-prepared side-effect profiles leaves the impression of "going through the motions", particularly as it is my view that some of the clinical circumstances are dubious.
[ACCC 3.45, p 693]
517 He reached a similar conclusion in relation to the doctors’ consultations he assessed in McRae Report 2, stating:
My opinion is that the arrangement was to expeditiously overcome the regulatory requirement for prescription of medication by a registered medical practitioner and little else… It is my opinion that there is a standard format for the approach to the management of any caller irrespective of their past history. It involves the same hierarchy of medications provided there is no profound contraindication noted following specific direct questioning seeking their existence, and all recommended medications appear to be able to be provided by the organisation with which the several medical practitioners are associated.
[ACCC 3.32, p 310]
518 The evidence justifies this conclusion. The overriding purpose of the consultations was to prescribe a medication. The enquiries made by the AMI doctors were directed only to whether it was safe to do so.
519 I accept the contention of the ACCC that in 150 of the Annexure B patient consultations, the doctor did not seek to diagnose any underlying cause for the patient’s presenting problem.
4.5.4.4.3 The failure to refer patients to specialists or other doctors for diagnosis or treatment
520 The ACCC also contended that in no Annexure B cases did the doctor seek to determine whether it would be medically appropriate to refer the patient to a specialist or other medical practitioner for diagnosis or treatment of underlying causes or presenting conditions, and in none were they so referred. It may be accurate that no patient was referred to his GP or specialist in so many words. But there are a few examples in which it was unnecessary for the doctor to make the explicit referral because the patient had indicated in the course of the consultation that he had had a regular check-up with his GP.
521 This said, the sense of the ACCC’s contention is accurate for most of the consultations. There were many examples of ED patients presenting with risk factors such as obesity, excessive smoking, excessive drinking, or cardiovascular disease who were prescribed medication without reference by the doctors of the need to seek help from other doctors for important health issues. Further, there were PE patients suitable for psychological or behavioural treatment who were prescribed medication and were not directed to other doctors for that treatment.
4.5.4.5 The failure to warn of side effects
522 The ACCC alleged that the AMI and NRM doctors did not warn patients of the common side effects of the medications prescribed in consultations with 133 of the Annexure B patients and in consultations with 14 of the Annexure C patients. The ACCC alleged that this conduct alone, or in combination with other conduct, amounted to unconscionable conduct. The conduct of the NRM doctors is discussed at [783] – [836] of these reasons for judgment.
523 There was no dispute between the experts Dr Pattison, Dr McRae, and Dr Walton, who were called by the ACCC, and Professor Currie and the AMI and NRM doctors, Dr Berry, Dr Goyer, and Dr Condoleon, who were called by the respondents, that the doctors had a responsibility to warn patients of common side effects of the medications.
524 Dr McRae said that the obligation was reflected in provisions of the Code as follows:
‘Good Medical Practice: A Code of Conduct for Doctors in Australia’ refers to the doctor-patient partnership involving “Encouraging and supporting patients to be well informed about their health and to use this information wisely when they are making [their health] decisions.” It refers to “Informing patients of the nature of, and need for, all aspects of their clinical management, including examination and investigations, and giving them adequate opportunity to question or refuse intervention and treatment.” It states that part of effective communications includes “Discussing with patients their condition and the available management options, including their potential benefit and harm”. It states that part of effective communication includes “Ensuring that patients are informed of the material risks associated with any part of the proposed management plan.” It is my opinion that the expression “material risk” embraces the concept of ‘possible side effects’ and also adverse events, as well as the notion of not being informed of a potentially available treatment option from which the patient may derive benefit. ‘Good Medical Practice: A Code of Conduct for Doctors in Australia’, states that part of effective communication includes "Responding to patient's questions and keeping them informed about their clinical progress.
[ACCC 3.31, p 36]
525 He drew the following conclusions from the provisions of the Code:
Thus, in my opinion, it is not possible to point to a mandatory rule stating something like "You must / are required to discuss with a patient each of the medications that the medical practitioner prescribes for a patient", or "You must/ are required to inform a patient of the possible side effects of any prescribed medication". The entire notion of the doctor-patient relationship is underpinned by a trust relationship with the medical practitioner respecting the patient's autonomy, by providing sufficient information to permit the patient to make an informed choice and provide informed consent to a proposed course of treatment. This necessitates the communication that would cause the discussion about medications, their benefits, risks, side effects and adverse effects. Similarly, the patient respects the superior knowledge of the medical practitioner, and trusts that they will provide a full disclosure of the diagnosis and possible treatments, which may involve medications, clinical interventions or both.
[ACCC 3.31, pp 36 – 37]
526 Dr Walton observed that precisely what information is conveyed to an individual patient depends on the level of interest of the patient in relation to side effects [ACCC 3.35 p 16.7]. Professor Currie said the same thing in cross-examination [TS 2609]. Professor Currie explained a rationale for the provision of information about side effects which underscored the importance of the issue to patients. He said that a purpose of explaining major side effects was so that “patients may elect not to have a treatment. Which is their right.” [TS 2610]
527 The evidence of the side effects of the use of apomorphine came from AMI itself and from the Mohee 2012 article referred to by Professor Currie and annexed to Currie Report 1.
528 AMI conducted an internal clinical trial for the whole of the year 2008. The trial involved 20,530 patients treated with apomorphine together with phentolamine in nasal spray and lozenges. Phentolamine is a vasodilating agent which opens up blood vessels in the body to increase blood flow. The trial revealed the following local side effects:
[Nasal Spray] | |
Irritation | 33% |
Crustiness | 27% |
Burning | 9% |
Bleeding | 8% |
Congestion | 5% |
Pain | 1% |
[Lozenge] | |
Numbness of Mouth | 1% |
[ACCC 4.385, p1]
529 And the following systemic side effects:
Headache | 3% |
Ulceration | 2% |
Swollen mouth | 2% |
Dizziness | 0.34% |
Nausea | 1% |
Vomiting | 0% |
[ACCC 4.385, p 1]
530 Mohee 2012 reported on the results of three randomised placebo-controlled trials of the use of apomorphine SL in the treatment of ED. The trial by Dula and others involved 569 men, by Von Keitz and others 507 men, and another by Dula and others 296 men. The tolerability issues were reported as follows:
Tolerability issues | Dula et al. | Von Keitz et al. | Dula et al |
Nausea and vomiting (%) | 25 | 13.4 | 7.0 |
Hypotension (%) | - | 8.0 | 2.2 |
Yawning (%) | 10 | - | 8.1 |
Headache (%) | 16 | 7.6 | 2.2 |
Dizziness (%) | 10 | 3.6 | 6.5 |
[ACCC 3.44, p 572]
531 Dr Pattison reported that the most common side effect of apomorphine is nausea. It may be that the difference in results between the trials reported by Mohee and the AMI survey is explained by the fact that the AMI trial involved apomorphine delivered by nasal spray and the Mohee trials involved apomorphine delivered sublingually.
532 The evidence of the side effects of the use of clomipramine came from AMI itself and from Dr Walton.
533 In the internal clinical trial conducted by AMI for the year 2008, the side effects of clomipramine were also surveyed. The trial involved 14,935 men treated with clomipramine. The trial revealed the following local side effects:
[Nasal spray] | |
Irritation | 33% |
Burning | 22% |
Crustiness | 14% |
Bleeding | 10% |
Congestion | 4% |
[Lozenge] | |
Numbness of Mouth | 4% |
[ACCC 4.385, p 2.6]
534 And the following systemic side effects:
Headache | 4% |
Ulceration | 3% |
Swollen mouth | 3% |
Dizziness | 2% |
Nausea | 1% |
Vomiting | 0% |
[ACCC 4.385, p 2]
535 Dr Walton said that the common side effects of the use of clomipramine were lowered blood pressure with dizziness or even fainting, palpitations, blurring of visions, dry mouth, gastrointestinal distress, weight gain, headaches, lowered libido, and ED [ACCC 3.35, p 17]. Further, the rapid cessation of the use of clomipramine may cause rebound anxiety and depression and the risk of self-harm or suicide. Dr Walton reported that the usual dose of clomipramine for the treatment of depression was 50 – 150 mg. He also noted that the dosage in AMI oral strips was 10 mg. Dr Walton did not draw any distinction between the differences in dosages or delivery routes for the purpose of identifying side effects.
536 There were four reported cases of adverse effects from the use of clomipramine in the Annexure B patients. Patient 13 said that the nasal spray stung his nose greatly, gave a burning feeling, blocked his nose, and gave him a foul taste. He felt nauseous and dry-retched. He was affected for an entire day and felt like he had a head cold. Patient 30 felt dizzy, hot and nauseous. Patient 40 experienced an elevated heart rate. Patient 158 experienced severe headaches, dry mouth, numbing sensation in the mouth and gums, continuous vomiting, and difficulty in sleeping.
537 In six consultations with Annexure B patients, side effects were not mentioned at all by doctors, yet either apomorphine or clomipramine was prescribed. Three consultations were with Dr Vandeleur (patients 17, 28 and 41) and one each with Dr Lonergan (patient 42), and Dr Daood (patient 46) and Dr Goyer (patient 113).
538 The ACCC contended that bleeding, crustiness, and burning were side effects which should have been mentioned. In fact only one patient was told about bleeding (patient 96), two about crustiness (patients 81 and 96), and five about burning (patients 46, 66, 74, 76 and 88). The seven patients were treated by only three of the AMI doctors. Dr Durrani treated four, Dr De Sayrah two, and Dr Vandeleur one.
539 However, both Dr Berry and Dr Condoleon thought that a warning about irritation was enough to cover burning, crustiness, and bleeding. Dr Condoleon explained his reasons as follows:
MR BURNSIDE: Okay. Well, let’s get it very clear. Do you accept that, looking at apomorphine phentolamine, that irritation, crustiness, burning and bleeding are side effects which are sufficiently common that they should be mentioned in advance to a patient who is going to receive?
DR CONDOLEON: I think they are, because they are all – they are all under the one heading, which would be, “These medications inhaled in the nose can cause irritation in the lining of the nose, so please let us know if you get any issues with the lining of your nose.” That would cover all of those.
MR BURNSIDE: Right. And going over the page to clomipramine, do you also agree that irritation, burning, crustiness and bleeding are all side effects that should be mentioned in advance to people who are going to be prescribed the clomipramine nasal spray?
DR CONDOLEON: Yes, yes. Yes, in that broad terms that I’ve just mentioned then, that there can be irritation of the lining of the nose, and to be aware of that and to let us know that if that occurs, it wouldn’t be the right treatment for you.
[TS 2269]
540 And Dr Berry explained her approach as follows:
MR BURNSIDE: Would you agree that crustiness, burning, bleeding and dizziness are all potential side effects that should be advised to the patient in advance of them agreeing to take the medication?
DR BERRY: Yes, and that’s why I go into quite a lot of detail about how to use the nasal medication and if they have any signs of irritation, that they should let us know, or any uncomfortability [sic]. Do not persist with anything that causes any uncomfortability.
MR BURNSIDE: Yes. Would you agree that in many cases, the side effect that you mention is light-headedness?
DR BERRY: Yes.
MR BURNSIDE: But that you do not mention crustiness, burning or bleeding in most instances?
DR BERRY: Irritation in the nose, I would have thought varied mostly.
MR BURNSIDE: Yes. Would you agree that irritation is not quite the same as burning or bleeding?
DR BERRY: The burning and bleeding are if you persist using something that’s causing irritation. It starts with an irritation and I recommend to my patients not to persist if it’s irritating. It’s only if they keep using it that they start getting those sorts of symptoms.
[TS 2434]
541 In final oral submissions counsel for the respondents relied on suggested allowable differences in views among doctors to justify the practices of the AMI and NRM doctors. That submission might explain a failure to refer to bleeding, crustiness, or burning if doctors referred to irritation in cases where a nasal spray was prescribed. But this is not the picture which emerged from the recordings.
542 Nasal sprays were prescribed in about 100 Annexure B consultations.
543 The doctors typically warned against tiredness or drowsiness or light-headedness.
544 Thus, Dr Lonergan said to patient 62, for whom he prescribed clomipramine nasal spray:
DR LONERGAN: Now with the medicine, with the side effects, sometimes you get a little bit of tiredness or light headedness.
PATIENT: Yeah.
DR LONERGAN: So I wouldn’t take it, you know, in the middle of the day if you are doing something dangerous, driving long distance or doing dangerous sports or you know, using machinery. You know, things where obviously you don’t want to feel a bit tired. But it’s not common in the first place and if you take it early the night before it will slow things down through the night when you need it. Then it’s out of your system anyway, the next day. But just be aware of the possibility.
[ACCC 4.315, p 9]
545 Dr Lonergan used a similar formula often. Some random examples are patients 1, 19, 65, 69, 78, 80, 91, 92, 131, and 137. Sometimes in addition to tiredness, Dr Lonergan mentioned that the patient might experience “stuffiness”, in which case the medication might be changed to the tablet form. Some random examples are patients 4, 11, 71, 106, 107, 115, 129, 139 and 142. In a few instances he mentioned that patients might experience both stuffiness and irritation. Some random examples are patients 3, 21, 26, 85, 105. Dr Lonergan also referred many patients to the booklet which was sent to patients accompanying the AMI medications (the instruction booklet), stating that this contained a more complete list of the common side effects. He also informed most patients to contact AMI for a follow-up or if they experienced adverse side effects.
546 Dr Berry had a formula which referred only to light-headedness. An example from the consultation with patient 133 was as follows:
DR BERRY: Okay. Side effect wise: if anything, initially may cause a bit of light headedness. So we do recommend, at least for the first week or two, that you use it at night time rather than in the morning when you’re about to drive.
[ACCC 4.279, p 8]
547 Dr Berry also employed an alternative formula which referred to irritation. An example from the consultation with patient 145 was as follows:
DR BERRY: Side-effect-wise, if anything, when you start with it, it may cause a bit of light-headedness, so we do recommend at least from the – for the first week or so that you use it at night-time, rather than in the morning when you’re about to drive, and it should feel as bland in your nose as water. If you feel that it’s irritating, don’t keep using it. Ring in and we’ll change you either to the tablet form or to another medication depending which is most appropriate for you.
[ACCC 4.280, p 12]
548 In about 20 Annexure B consultations Dr De Sayrah mentioned light-headedness and drowsiness. She mentioned light-headedness and drowsiness without any other side effects in six consultations. She also mentioned “nasal irritation” in about ten consultations and mentioned nausea in about seven.
549 In about 15 Annexure B consultations Dr Omar mentioned drowsiness, dizziness, tiredness or light-headedness. In three consultations he also mentioned “irritation to the nose” (patients 33, 118 and 154). In all but four consultations he said that patients should contact AMI if they experienced unusual side effects.
550 Out of eight Annexure B consultations which were recorded and transcribed, Dr Durrani warned of tiredness and light-headedness, and of burning, stuffiness or irritation in the nose in six. In one consultation with patient 141, she did not refer to side effects at all.
551 In six of nine Annexure B consultations Dr Vandeleur mentioned “nasal irritation”. He also mentioned drowsiness or tiredness in three consultations. In three consultations he did not mention any side effects of the AMI medications.
552 In five of six Annexure B consultations Dr Daood referred to “problems in the nose” as a side effect. In two consultations he also referred to headaches and nausea. In the consultation with patient 46, he did not mention side effects at all. In none did he mention drowsiness, tiredness or dizziness.
553 This survey is sufficient to demonstrate that the doctors regarded it as important to stipulate that nasal irritation and drowsiness were side effects of apomorphine and clomipramine nasal spray which should have been referred to. All the doctors referred to some of the side effects in some consultations. However, none of the doctors discussed in this section of the reasons for judgment uniformly referred to both of these side effects in each consultation. That is to say, their own practices were inconsistent. There was also inconsistency in the practices among the doctors as a group. For instance, Dr Daood and Dr De Sayrah sometimes warned patients of nausea. Other doctors did not refer to nausea at all. Dr Berry explained her reason for not doing so, namely, that mentioning nausea was more likely to cause patients to develop the symptom.
554 The respondents also argued that rather than mention all the common side effects, it was sufficient for the doctors to say that if there were any particular side effects, the patients should call AMI. Dr Pattison’s view on this approach should be accepted. He said:
Asking the patient to report any side effect symptoms is not a satisfactory approach, especially if no specific follow-up appointment has been made for the patient and no particular doctor is taking responsibility for the patient's ongoing care.
[ACCC 3.46, p 10]
555 In any event, the practice of some doctors, such as Dr Lonergan, in inviting patients to call AMI in the event that they experienced unusual side effects, was not uniformly followed by all.
556 From listening to many of the recordings one observes a noticeable tendency among more than a few of the doctors to minimise the side effects of the medications. Some random examples are as follows. Dr Omar usually started his description of side effects by saying “this medication is generally safe to use” (patient 2). Dr Chan said, “the medication itself generally doesn’t cause too much problem” (patient 6). Dr De Sayrah said that the medication, “could make you light-headed and drowsy and dry-mouthed and nauseous and all these – every possible thing they put there, but no-one has ever experienced it” (patient 57). Dr Lonergan told patient 103, “they’re pretty safe too”, and he told patient 78 that side effects were “not common”. Dr Vandeleur told patient 114, “one in twenty get a lot of irritation in the nostrils”, whereas the 2008 AMI internal survey put the figure at more than six times that mentioned by Dr Vandeleur. Dr Goyer told patient 58, “now it is also a safe medication. It is relatively benign”.
557 Finally, there is a general pattern observable throughout the Annexure B patient consultations for the doctors to mention side effects at speed, without pause, in a flow of information with the result that attention is rather deflected away from the issue.
558 It follows from this discussion that the most reliable evidence of the side effects of the AMI nasal spray comes from the AMI survey. That required the doctors to warn of at least irritation, crustiness, burning, and bleeding. This was not done in most cases. And when side effects were mentioned the doctors presented the information in such a way as to downplay their significance. This approach made it less likely that patients would be deterred from entering a contract for treatment. In the many instances in which doctors failed to fully inform patients of significant side effects, they did not meet their professional duty to their patients.
559 The ACCC alleged that AMI and NRM engaged in unconscionable conduct by having the consultations conducted with doctors by phone and consequently without the doctors seeing or physically examining the patients.
560 The argument had two alternative limbs. The first limb was that it was not acceptable medical practice to treat ED or PE over the phone by prescribing medication without seeing or examining the patient. On this argument the content of the consultation was immaterial because the manner of treating was simply not appropriate in any circumstances.
561 The second limb was that even if there were some circumstances in which phone consultations could be justified, the consultations in question were not in that category because there were significant deficiencies in the way the doctors conducted the consultations. In other words, because of these other deficiencies, the consultations did not meet the standard required of phone consultations. This second limb relies on the establishment of the various other deficiencies in conduct otherwise addressed in these reasons for judgment. It does not depend on the consultation being by phone, but rather on whether the doctors undertook to diagnose and treat underlying causes, referred patients to GPs or specialists, provided sufficient information about side effects, or explained the financial arrangements attending the treatment, which are other matters examined in these reasons for judgment. Hence, in this section only the first limb of the argument needs to be addressed.
562 Dr McRae explained:
[T]hat the typical Australian medical consultation, particularly for a first medical consultation, is routinely undertaken face to face. This assists in the development of the doctor-patient relationship, as both parties may pick up visual clues about the other, just as for any interpersonal interaction in society. For the medical practitioner, many cues may be obtained from the patient's demeanour and behaviour which may influence their diagnosis. Examples are observations that the patient has a distended abdomen, a visible lump, are pale, obese, or appear to be in pain. Similarly, the patient may be able to assess the medical practitioner's body language or gauge the level of interest in the clinical problem with which the patient presents. It is uncommon for medical consultations to occur as a non face-to-face consultation, particularly related to a first consultation, and particularly when a clinical intervention is to be prescribed.
If there is no face-to-face consultation, the risk of missing any information that may have been cued by visual information occurs. Additionally, there is no opportunity to undertake a physical examination of the patient, including the measurement of vital signs and which may be as directed as clinically required. This presents a risk to the patient of an unnecessary or inappropriate clinical intervention, and exposes the medical practitioner to the risk of the consequences of undertaking or instigating an inappropriate or unnecessary clinical intervention. It is my opinion that the ramifications of this arrangement are likely to increase if there is never a face-to-face consultation, particularly if this circumstance is at the behest and instigation of the medical practitioner.
[ACCC 3.31, pp 30 – 31]
563 Dr Pattison expressed the view:
For every patient with either ED or PE, a face-to-face consultation with the doctor is an essential part of the management. Patients with ED often have associated co-morbid conditions such as high blood pressure, obesity, diabetes or vascular disease and these illnesses will not be diagnosed without a comprehensive medical check, including a detailed history and examination. The presence of ED can be a very important clue to detecting these other conditions.
Although patients with PE are often much younger and these co-morbid medical conditions are less likely to be present, a proper history and examination is still required.
[ACCC 3.28, p 28]
564 Dr Walton said:
Perhaps because it is considered axiomatic that the normal medical consultation consists of a face to face interview (often involving a direct physical examination of the patient) that there seems to be little direct reference to that in codes of conduct, position statements and the like guiding medical practitioners.
[ACCC 3.35, p 12]
565 Dr McRae also highlighted the particular difficulty of prescribing medications off-label by phone consultations:
When a medication is prescribed “off label”, an issue is, almost by definition, there is a paucity of readily available information about the “unapproved” use of the “approved” medication... [T]he prescribing medical practitioner must satisfy himself or herself that the medication and its mode of delivery are specifically indicated in the particular circumstances of that patient… It is my opinion that this is more difficult in a non face-to-face circumstance without the opportunity of a clinical examination or visual inspection, and when the conversation is rapid.
[ACCC 3.45, pp 720 – 721]
566 With the development of technology and the prospect of using new forms of communication in the practice of medicine, the State and Territory Medical Boards adopted a policy entitled, “Technology Based Patient Consultations”, effective from 1 July 2007. It provided for patient care as follows:
2.0 Standards of Patient Care
The JMBAC [Joint Medical Board of Australia Council] Good Medical Practice Guide (currently under review and development of national consultation) stipulates general principles under which patients can expect to be entitled to good standards of practice and care from their doctors. These principles apply to doctors who advise or treat patients in technology-based consultations.
Doctors who advise or treat patients in technology-based patient consultations shall:
(i) First confirm to their satisfaction the identity of the patient at each consultation. Doctors should be aware that it may be difficult to ensure unequivocal verification of the identity of the patient in these circumstances.
(ii) Include an adequate assessment of the patient's condition, based on the history and clinical signs and appropriate examination.
(iii) Keep colleagues well informed when sharing the care of patients.
(iv) Provide an explanation to the patient of the particular process involved in the technology-based patient consultation.
(v) Make their identity know[n] to the patient.
(vi) Ensure they communicate with the patient to establish the patient's current medical condition and history, and concurrent or recent use of medications, including non-prescription medications; identify the likely cause of the patient's condition; ensure that there is sufficient clinical justification for the proposed treatment; ensure that the proposed treatment is not contra-indicated. This particularly applies to technology-based consultations where the practitioner has no prior knowledge and understanding of the patient's condition(s) and medical history or access to their medical records.
(vii) Be ultimately responsible for the evaluation of information used in treatment, irrespective of its source. This applies to information gathered by a third party who may have taken a history from, or examined, the patient.
(viii) Be confident that a direct physical examination would not add important information to inform their treatment decisions or advice to the patient. This particularly applies to consultations where the practitioner has no prior knowledge or understanding of the patient's condition(s) and medical history or to access to their medical records.
(ix) Make a clear, accurate and legible record of the consultation.
(x) Make appropriate arrangements to follow the progress of the patient by monitoring the effectiveness and appropriateness of the recommended treatment and by informing the patient's general practitioner or other relevant practitioners.
In an emergency situation, it may not be possible to practice according to this policy. If an alternative is not available, a technology-based patient consultation should be as thorough as possible and ensure that more suitable arrangements are made for the continuing care and follow up of the patient.
[Emphasis added.]
[ACCC 3.31, pp 85 – 86]
567 In Currie Report 1, Professor Currie acknowledged that many clinical guidelines for the management of ED and PE include the need for direct or face-to-face clinical examination, but said that it was not a universal convention.
568 By way of example, Professor Currie referred to a pilot study undertaken by Leusink and Aarts in the Netherlands which was reported in an article entitled, “Treating Erectile Dysfunction through Electronic Consultation: A Pilot Study” (2006) 32 Journal of Sex and Marital Therapy 401. In particular Professor Currie referred to the following passage:
[S]ome 70% of Dutch users of the internet (approximately 6 million people) would prefer to be able to contact their family doctor or specialist through the internet. Erectile dysfunction affects 16% of Dutch males over 18 years of age; only 10.4% of those men suffering from ED receive treatment in part because many ED sufferers are too embarrassed to seek help. It is the consensus opinion of Dutch urologists, family doctors, and sexologists, that ED only requires physical examination on specific medical grounds. When a questionnaire indicates somatic complaints pointing to diabetes or angina for instance, the consultant may refer a patient to his family doctor. In other words it is not always necessary for a consultant to carry out a physical examination prior to issuing a prescription (emphasis mine), a point where Dutch practice differs from European and US practice….The Royal Netherlands Medical Association, the umbrella organization of physicians in the Netherlands that particularly occupies itself with medical-ethical affairs has made a case for not requiring a face to face meeting before an e-consultation”.
[R13.31, p 16]
569 The pilot study involved 219 men who used an e-consultation website to seek help for ED. Ninety-eight patients responded to a questionnaire which enquired whether their erections had improved as a result of the consultations. The study itself pointed to a number of limitations as follows:
First, it should be taken into account that there is no randomized control group. We therefore do not know whether the erection would have spontaneously improved with the passing of time or with the use of self-sought medication. Second, the self-selection of participants means that these conclusions only apply to this group of men who used the Internet to seek help. Third, we also encountered a degree of self-selection among the respondents. Within the consultation group, the respondents differed from the nonrespondents by the higher frequency with which they requested prescriptions. This raises the question of whether the measure of efficacy that we have found is not, in fact, a measure of the effectiveness [of] pharmaceutical treatment rather than of the website consultation. Even so, treatment whereby medication is prescribed can still be said to be effective, even though it has been supplied through e-consultation. The present study does not allow any statements regarding the effectiveness of the e-consultation compared with a personal, face-to-face consultation.
…
The ultimate goal of the website is for men to personally approach a general practitioner or a sexologist to deal with their erection problem.
[Emphasis added]
[R13.31, p 78]
570 Dr McRae pointed out that the e-consultation in question in the study was a 20-question questionnaire, with only the possibility of medication being prescribed. The e-service provided a letter to be forwarded to the patient’s family doctor. Unlike AMI’s practice, the medication was an approved use of PDE5 inhibitors. Dr McRae also highlighted the limited usefulness of the study. He said,
It is not correct to link use of e-consultation with improvement in erectile dysfunction. The improvement in erectile dysfunction is through use of the PDE5I. The medication could have been obtained from their family practitioner, who would have an appreciation of their full circumstances and be able to examine them or investigate them if deemed necessary.
…
They [the authors] state correctly that the paper has no bearing on anything to do with the effectiveness of e-consultation per se… If the goal of the website was to have “men personally approach a general practitioner or a sexologist to deal with their erection problem”, the authors concede it has failed. It appears to be little more than a convenient form of on-line shopping, with nobody able to account for the destination of any medications that are prescribed.
[ACCC 3.45, pp 732-733]
571 In Currie Report 2, Professor Currie referred to an article by Munger and others entitled “Safety of Prescribing PDE-5 Inhibitors via e-Medicine vs Traditional Medicine” (August 2008) 83 (8) Mayo Clinic Proceedings 890 [R 13.39, 213]. The article reported on a study comparing the safety of prescribing PDE-5 inhibitors for the treatment of erectile dysfunction over the internet with the safety of prescribing in face-to-face consultations with doctors. The records of 500 patients were selected from about 100,000 e-records of patients based in Utah who were prescribed PDE-5 inhibitors over the internet through the KwikMed website. The records of another 500 patients were selected from the records of patients who were prescribed PDE-5 inhibitors from a traditional primary-care, multidisciplinary practice in Salt Lake City. The study assessed the safety of the two prescribing systems by examining a number of factors including the comprehensiveness of the diagnosis process, the rate of contraindicated prescriptions, and the extent of patient education about the medications used. By reference to these features of the internet system used on the one hand, and the nature of traditional medical practices in Salt Lake City, the study concluded that the internet prescribing system was at least as safe as the face-to-face system, and in some instances, safer. However, the study was not a general endorsement of prescribing without face-to-face doctor consultations. The article recognised that:
Medical practice guidelines for erectile dysfunction recommend a medical interview regarding the sexual dysfunction of the patient. … A complete multisystem physical examination, including a genital examination, should be conducted to reveal cardiovascular disease and neurologic and urologic abnormalities
572 The e-medicine records showed that 80 per cent of patients had undergone a general medical examination within the last year and 97 per cent within two years. In effect, this internet prescribing system was regarded as safe in this respect because the patients had, and had been recorded as having had, a face-to-face consultation. Furthermore, the internet prescribing system was closely regulated as described in the following passage:
The State of Utah entered into a consent order with KwikMed, an Internet prescribing company, to permit e-prescribing of erectile dysfunction drugs under the Utah Practice Act, providing the welfare of the users remained paramount, that acceptable standards of care were consistently maintained, that properly supervised physicians and pharmacy personnel adhered to ethical conduct, and that monitors had constant access to Web site records while the users’ confidentiality was maintained. Further, patients are provided direct access to the State of Utah for concerns through the Web site.
573 The conclusion of the study relied on the availability of State regulation. That is demonstrated in the conclusion drawn in the study as follows:
Results of the current study suggest that, under a platform of regulatory oversight, the safety of e-medicine care can match or possibly exceed traditional medical care, providing an evidence-based framework to reexamine current guidelines.
574 In Currie Report 1, Professor Currie also referred to another case of internet prescribing of PDE5 inhibitors for the treatment of ED. He referred to the report of the conclusions of a study which was published online by Dr Miles Jones in an article entitled, “Internet-based Prescription of Sildenafil: A 2104 – Patient Series” (2001) 3(1) Journal of Medical Internet Research (Jones 2001). The study compared the in-clinic treatment of 36 ED patients with the internet prescribing of PDE5 inhibitors to 2,104 ED patients. Professor Currie relied on the conclusions drawn in the report that many men feel uncomfortable about discussing ED face-to-face with a doctor, that many patients seen in a clinic did not receive any examination or laboratory tests specific for ED, that there is little consensus as to what, if anything, beyond medical history, might be appropriate in the diagnostic work up of ED, and that the internet-based clinical history checklist provided more complete information than was obtained in the face-to-face consultations. The study covered the period from June 1998 to March 1999. As to the basis for the conclusion that no more than a medical history is necessary for the treatment of ED, Jones stated:
Although objective means exist for establishing the existence of erectile dysfunction and for distinguishing between organic and psychogenic causes, these tests are cumbersome and often omitted even from specialists’ most comprehensive recommendations. Indeed, there appears to be little in the way of consensus as to what, if anything, beyond the medical history might be appropriate in the diagnostic work-up of erectile dysfunction. Recommendations that the physical examination focus on signs of vascular and neurologic disease, together with palpation of the penis for Peyronie's disease and tests for atrophy are common. Except for detection of Peyronie's disease, which can usually be elicited by a thorough medical history, these observations are directed primarily toward determining a cause for the dysfunction.
[Footnotes omitted.]
[R13.31, p 94]
575 Thus, if the treatment of ED is meant to include ascertaining the cause of the problem, the article seems to accept that there is role for physical examination. Furthermore, Professor Currie’s own evidence was that knowledge of the strength of the link between ED and cardiovascular disease has emerged in more recent times. The view expressed in 2001 about the value of a physical examination in ED cases to address the linkage with cardiovascular disease or diabetes might be outdated now.
576 The respondents tendered the 2012 First Quarter Report of the National Health Call Centre Network [R 9]. Part of the work of the Network is to provide an afterhours GP phone helpline. A GP consulting by phone assesses the situation and advises the caller on self-care, to attend a doctor the next day, or to attend an emergency department. As an example of the use of technology in medicine, the National Health Call Centre Network is rather remote from the circumstances of the treatment regime operated by AMI and NRM. Another example of the use of technology in medical practice, but also quite remote from the AMI and NRM situation, is the accepted use of technology in providing medical treatment to remote areas in emergency situations.
577 In the respondents’ additional reference to scientific evidence, the respondents relied on six scientific articles to support the view that a face-to-face consultation was not necessary for the diagnosis of PE. The articles were said to establish that the diagnosis of PE was on self-report and sexual history alone.
578 However, these articles were selectively quoted and, when read in full, the articles recognised that a physical examination was a part of the diagnosis of PE. It is also important to observe that the articles took for granted that there would be a face-to-face consultation. They were not concerned to address the unusual method of consultation by phone used by AMI and NRM.
579 In order to demonstrate the true scope of the articles, those parts of the articles relied on by the respondents are reproduced below in italics, and then, the passages which complete the picture are reproduced in a standard font.
580 The respondents relied on the following passage in the Andrology Australia PE Guide:
Clinical notes: PE is a self reported diagnosis and can be based on sexual history alone.
GP's are typically the first point of contact for men with a disorder of ejaculation. The GP's role in management of PE includes diagnosis, treatment and referral. Offer brief counselling and education as part of routine management.
[21] Specialist referral. For general assessment refer to a specialist (CP, endocrinologist or urologist) who has an interest in sexual medicine.
[R 13.3, p 20]
581 The respondents did not refer to what is contained in the Guide immediately after the first extracted passage where it set out the steps in diagnosis and included the following:
Physical Examination
- General examination
- Genito-urinary: penile and testicular-rectal examination (if PE occurs with painful ejaculation)
- Neurological assessment of genital area and lower limb.
582 Then the respondents relied on the following passages from Montorsi 2010:
The 2009 International Consultation on Sexual Dysfunctions was convened in Paris in 2009. It identified the following fundamental concepts as the basis for the management of sexual dysfunctions in men and women:
…
• Sexual dysfunctions are essentially self-reported conditions. Therefore, diagnostic tests or procedures should not be recommended without controlled clinical data or research-based evidence supporting their use.
[R1.1, p 3573]
The medical and sexual history is essential and frequently the most revealing aspect of the assessment process.
[R1.1, p 3575]
583 The sentence immediately following the first extract stated:
The International Consultation of Sexual Medicine (ICSM-5 (Figure 1) is a stepwise diagnostic and treatment algorithm for sexual dysfunction in men and women.
Figure 1 set out the diagnostic steps which were described as mandatory on the one hand and highly recommended on the other. In the latter category were "focused physical exam" and "lab tests". This was repeated in the text of the article on the same page where it was stated:
Physical examination and laboratory tests are strongly recommended but not always
necessary.
584 This statement was part of a summary of the conclusions in the article. The article was divided into two parts, the first dealing with ED and the second dealing with PE. The respondents’ reference to page 3575 related to ED. It is not complete, but in any event did not relate to the point the respondents seek to make which concerns PE. Where the article dealt with the evaluation of PE it commenced with the following:
Men with PE should be evaluated with a detailed medical and sexual history; a physical examination; and appropriate investigations to establish the true presenting complaint, identify obvious biologic causes such as medication or recent pelvic surgery, and uncover sufficient detail to establish the optimal treatment plan. [Emphasis added.]
585 The respondents relied on the following passage from Bettocchi 2008:
Owing to the absence of validated tools for diagnosing PE, the American Urological Association guidelines recommend that the diagnosis of PE be based solely upon information gathered from taking a sexual history, such as questions concerning the frequency and duration of PE, the proportion of sexual attempts with PE, the patient's relationships with specific partners, the frequency and nature of sexual activity, and the effects of PE on sexual activity and quality of life.
[R1.2, p 97]
586 However, that passage was immediately followed by a paragraph which assumed that a physical examination would be undertaken. That passage stated:
Genital and rectal physical examinations are necessary to establish the absence of penile shaft abnormalities (i.e. short frenulum) or prostatic inflammation; the latter requires the performance of transrectal ultrasonography and a Meares-Stamey test. Laboratory tests are required only when there is suspicion of illicit drug use or excessive alcohol consumption.
[R1.2, p 97]
587 Again it should be emphasised that the article was not focused on the controversy concerning whether there should be a physical examination for the diagnosis of PE.
588 Next, the respondents relied on the following passage in Hatzimouratidis 2010:
Diagnosis of PE is based on the patient's medical and sexual history.
[R1.10, p 810]
589 In the next paragraph under the same heading of diagnostic workup, the following appeared:
Physical examination includes a brief examination of the vascular, endocrine, and neurologic systems to identify underlying medical conditions associated with PE or other sexual dysfunctions, such as chronic illness, endocrinopathy, autonomic neuropathy, Peyronie's disease, urethritis, or prostatitis. Laboratory or physiologic testing should be directed by specific findings from history or physical examination and is not routinely recommended.
[R1.10, p 810]
590 The respondents referred to the following passage from the AUA Guideline 2004:
III. Evaluation of the Patient With Premature Ejaculation
Premature ejaculation is a self-reported diagnosis. A sexual history in which the patient uses language that explicitly communicates the circumstances of the condition is the .fundamental basis of assessment with time to ejaculation as the most important feature. The opinion of a partner can provide a significant contribution to clinician understanding a complete description is essential in distinguishing PE from ED, i.e., the inability to attain or maintain an erection, because these conditions frequently coexist…
Recommendation 1:
The diagnosis of PE is based on sexual history alone. A detailed sexual history should be obtained from all patients with ejaculatory complaints.
[R13.3, p 1]
591 Immediately following that extract this statement appeared:
When obtaining the patient's history, several important sexual and psychological characteristics should be assessed: frequency and duration of PE, relationship to specific partners, occurrence with all or some attempts, degree of stimulus resulting in PE, nature and frequency of sexual activity (foreplay, masturbation, intercourse, use of visual clues, etc.), impact of PE on sexual activity, types and quality of personal relationships and quality of life, aggravating or alleviating factors, and relationship to drug use or abuse. Laboratory or physiological testing is not required unless the history and a physical examination reveal indications beyond uncomplicated PE.
[Emphasis added.]
[R13.3, p 9]
592 Finally, the respondents relied on the following extract from Waldinger 2007:
Lifelong, acquired, natural variable PE and premature-like ejaculatory dysfunction are recognisable by taking a brief medical and sexual history with special attention to the duration of the ejaculation time and the course since the first sexual encounter. In daily clinical practice, diagnosis of the four PE syndromes is not difficult and evaluation with questionnaires or the use of a stopwatch is not required.
[R1.11, p 552]
593 This extract, taken alone, is misleading as to the author’s view about the proper process for diagnosis for PE. In relation to acquired PE, which seemed to be the more common form of PE seen at AMI and NRM, the article stated:
Acquired PE has a different pattern. The complaint differs in relation to the underlying somatic or psychological problem, and is characterised by the following symptoms:
• early ejaculation occurs at some point in a man's life;
• the man has usually had normal ejaculation experiences before the start of complaints;
• there is either a sudden or gradual onset.
• the dysfunction may be secondary to urological dysfunction (e.g. erectile dysfunction or prostatitis), thyroid dysfunction, or psychological or relationship problems;
In contrast to lifelong PE, the acquired form of PE can be cured by treatment of the underlying cause. A physical, blood and/or urine examination is always necessary.
[Emphasis added.] [Footnotes omitted.]
[R1.11, p 5]
594 Finally, in Althof 2010, which was exhibited to Dr Vaisman’s first witness statement dated 13 September 2012 as part of the material he provided to the AMI and NRM doctors, the authors stated the following:
For lifelong PE, a physical examination is highly advisable but not mandatory and should be conducted in most, if not all, patients. Some patients find it reassuring for the physician to examine them.
For acquired PE, a targeted physical examination is mandatory to assess for associated/causal diseases such as ED, thyroid dysfunction, and prostatitis.
[R 13.3, pp 60 – 61]
595 It is clear on the evidence before the Court that the conventional way of treating ED and PE is by a face-to-face consultation, especially where the patient is unknown to the doctor, the consultation is for the first time, and a medication is prescribed.
596 The opinion of experienced clinicians, Dr McRae, Dr Pattison, and Dr Walton should be accepted. Professor Currie, whilst drawing attention to alternative internet prescribing, did not embrace that practice as his own view. When addressing the Jones 2001 study, the following exchange occurred in cross-examination:
MR BURNSIDE: Okay. And your view that doctors prescribing this way are not denied any information relevant to their task is ---?
DR CURRIE: That’s not my view.
MR BURNSIDE: Your point is they’re not denied any information routinely obtained in a direct patient contact setting?
DR CURRIE: That’s the – that’s not my view. That’s the view of the article. That’s the statement from the article. That’s not my view.
MR BURNSIDE: Okay. In your view, are the doctors denied information routinely obtained in a direct patient contact setting if it takes place via the internet?
DR CURRIE: The whole point of putting this in is to show that this is possible to do, that it occurs and that comprehensive information is obtained particularly because this and the Munger article you referred to before demonstrate that in the face-to-face setting, very frequently are the history taking and/or the examination is suboptimal. So therefore, in the real world, what is being said here is that this form can get information. Now, the not denying any information routinely obtained is what the people suggesting that this can be done. It’s not necessarily what I do, nor is it the best way of doing things but it is a way that exists.
[TS 2598]
597 The present practice accepted in the medical profession of requiring a face-to-face consultation to diagnose and treat ED and PE has a rational basis as explained in the expert evidence. In particular, the comorbidity of ED with cardiovascular disease and diabetes, the diagnosis of which require physical examination and investigative tests, makes a strong case for face-to-face consultation. In relation to secondary PE, there is a need for physical investigation and testing. There is also the ability in face-to-face consultations for doctors to pick up on visual clues which would not be available to them over the phone and which may be important if the cause of PE is psychological. Some patients may also prefer to try counselling or other psychological treatment before medication, which treatment cannot satisfactorily be undertaken over the phone.
598 It was generally accepted by the medical experts that a significant number of men do not seek treatment for ED or PE as a result of embarrassment in raising the matter with their GP. The respondents relied on this to argue that it is not unconscionable to provide patients with treatment over the phone when, if that method was not used, the patients would not obtain any treatment whatsoever. However, that is a medical education issue which should be addressed by the medical profession. It is not a reason to offer substandard medical treatment.
599 Whilst the conventional position requires in-person or face-to-face consultations, it must be acknowledged that this is a time of change. The respondent’s evidence indicates that the medical profession is accommodating some of its practices to technological change. Furthermore, the Court cannot close its eyes to the practice of internet prescribing for PDE5 inhibitors for the treatment of ED. A judge addressing the present issue in five years’ time may well be faced with developments and more sophisticated means of doctor-patient interaction which may lead to a different conclusion. But in the present state of affairs and in the circumstances of AMI and NRM, I find that proper medical practice required doctors diagnosing and treating new patients for ED or PE by prescribing medication to conduct the initial consultation if not in person, then at least face-to-face, but not by phone. Subject to the requirements set out in the “Technology Based Patient Consultations” policy, such a consultation might be conducted by video-link.
4.5.4.7 Recommending long-term contracts without medical basis
600 The evidence referred to at [613] – [615], [624] – [627], and [881] – [882] of these reasons for judgment demonstrates that AMI doctors were, in effect, directed by Dr Vaisman and Mr Shrestha to recommend treatment for 12 to 18 months. In practical terms, doctors would not be employed by AMI if they did not recommend long term contracts. Such contracts suited the commercial interests of AMI and later, NRM but were not necessarily in the interests of the patients.
4.5.4.8 Prescribing only AMI medications
601 The ACCC alleged that AMI doctors only offered AMI medications to the Annexure B patients and did not discuss other medication options other than to denigrate them.
602 The discussion at [218] – [352] of these reasons for judgment concludes that there is no proper scientific basis which establishes that the apomorphine and clomipramine-based medications offered by AMI and NRM were effective. At the same time, conventional first-line medications used for the treatment of ED and PE have been shown by clinical trials to be effective.
603 Further, the discussion at [883] – [888] of these reasons for judgment concludes that Dr Vaisman, in effect, directed doctors to prescribe the AMI medications.
604 The ACCC alleged that, in these circumstances, it was unconscionable for AMI to offer only its own medications. The ACCC also alleged that doctors failed to act in accordance with professional standards by restricting themselves to prescribing only the AMI medications, which, the ACCC said, was unconscionable conduct of the doctors undertaken on behalf of AMI. That was not in the best interests of patients and did not treat the health of patients as a matter of primary concern as required by the Code.
605 Further, in re-examination Dr Pattison explained the obligation of doctors prescribing off-label as follows:
MR BURNSIDE: In your opinion, what duty do you have to the patient if you’re prescribing off-label?
DR PATTISON: Well, when we’re prescribing off-label we have to be – there are certain extra obligations to the doctor and part of that I think really is to explain to the patient, “Well, we’re going to use this medication.” I would explain – I try to do it as frequently as I could, but I would say that this medication has been demonstrated to be effective and so I feel as though we should talk about that in the consultation. I am mindful that when you’re prescribing off-label, there are extra obligations for the doctor and that’s to make sure that there’s no other treatment, particularly one that has been TGA or FDA approved that, you know is superior to the treatment that you’re offering. So my obligation to the patient is to make sure that I’m offering the patient the best and the safest treatment and if it’s not TGA or FDA approved, then I would need some further discussion.
[TS 1213]
606 The evidence established that the AMI doctors failed to comply with the professional standards required of them by restricting themselves to prescribing only the AMI medications. Further, the doctors failed in their obligation to tell patients that they were prescribing the medications off-label and that there were alternative medications, approved by regulatory authorities, which were superior.
4.5.4.9 The failure to advise of the terms on which treatment would be provided
607 The ACCC alleged that the AMI and NRM doctors failed in their responsibility to advise patients of the terms on which the treatment would be provided including the cost of the treatment and the refund provisions.
608 The evidence established that the doctors did not explain these matters to patients. In relation to the refund provisions, AMI and NRM did not make doctors aware of their terms. This is discussed at [707] to [709] of these reasons for judgment. The evidence also established that most of the doctors were not aware of the cost of the treatment programs.
609 The responsibility for explaining the contractual terms was with the salespeople. Whilst this may have been undesirable, the evidence did not establish that, as a matter of accepted medical professional obligation, it was always necessary for doctors themselves to advise patients of the cost of treatment. In some practices administrative staff fulfil that function. The evidence did not establish to the requisite standard that the doctors failed in their professional duties by not explaining the cost of treatments or the refund provisions to patients. And, in any event, no relief was sought in reliance on this allegation.
610 AMI recommended to almost all of the Annexure B patients that they sign contracts for treatment periods between 12 and 18 months.
611 The ACCC alleged that, by recommending and signing up patients to these treatment periods, AMI engaged in unconscionable conduct because there was no proper scientific basis for treatment for those periods. Rather, the ACCC alleged, lengthy treatment periods served the commercial interests of AMI because the longer the treatment period the higher the cost to the patient.
612 A spreadsheet handed up as part of the in the respondents’ closing submissions showed that about 106 Annexure B patients signed contracts, and about 77 patients signed contracts for treatment for periods of 12 months or longer. Of these 77 patients, 16 were ED patients, 56 were PE patients, and 5 were ED and PE patients. About 13 ED patients were treated with apomorphine, and about 53 PE patients were treated with clomipramine.
613 These figures show that most contracts were for periods of 12 months or more. Dr Vaisman’s evidence demonstrated that this was the objective of AMI. He explained why AMI aimed to have patients sign up for 12 months or more as follows:
MR BURNSIDE: And your objective, one of your objectives, was to get patients to sign up for contracts for treatment for between 12 and 18 months?
DR VAISMAN: Correct.
MR BURNSIDE: And you encouraged the clinical coordinators to urge people to sign up for 12 to 18 months?
DR VAISMAN: Correct.
MR BURNSIDE: And yet it’s your position, isn’t it, that the lengths of the contract is a matter for the doctor to decide?
DR VAISMAN: Absolutely.
MR BURNSIDE: Yes. But, of course, you told the doctors that you thought people should be signed up for 12 to 18 months?
DR VAISMAN: That means the literature tells them the treatment should be at least 12 to 18 months.
HIS HONOUR: Sorry, who said?
DR VAISMAN: Literature.
HIS HONOUR: The literature?
DR VAISMAN: Yes.
MR BURNSIDE: We will go to the literature a bit later. But you drummed into the doctors that they should recommend 12 to 18 months?
DR VAISMAN: Not me, the literature which I supplied to them tells us the treatment should be between 12 to 18 months.
MR BURNSIDE: Now, did you tell the doctors in plain terms that they should try to recommend 12 to 18 months?
DR VAISMAN: I give them the literature, which confirms that the treatment should be between 12 to 18 months.
MR BURNSIDE: Did you ever discuss with any of the doctors that they should try to prescribe for 12 to 18 months?
DR VAISMAN: Of course, after I gave the literature we discuss.
MR BURNSIDE: Yes. And your clear message to them was, “Try and prescribe 12 to 18 months.”?
DR VAISMAN: Is the best interests of the patient, yes.
[TS 1630 – 1631]
614 Dr Vaisman gave doctors scientific literature which he said established that 12 to 18 months of treatment was needed for ED and PE. Because that literature verified the need for treatment for that period, Dr Vaisman said that he knew that doctors would recommend those periods to patients. He discussed the issue with doctors in regular meetings. Dr Vaisman also had meetings with salespeople. They were aware of the suggested treatment period of 12 to 18 months. Dr Vaisman was confident that the doctors would recommend such periods, and so salespeople could say that the doctor had recommended 12 to 18 months in their interactions with patients after the doctor consultation. Dr Vaisman said that the salespeople should check with the doctors what period they had recommended. Dr Vaisman explained this position when he was asked about a sales script [ACCC 4.558] which he authored and which was likely in use as at September 2007:
MR BURNSIDE: And it [the script] then says:
In your case doctor has recommended 12 to 18 months.
How did you know that the doctor would have recommended 12 to 18 months when you wrote this script?
DR VAISMAN: Because I gave the literature to the doctors which says the treatment should be between 12 and 18 months.
MR BURNSIDE: And you were confident, were you, that the doctors would do as you wanted them to do?
DR VAISMAN: Absolutely, because the literature says.
MR BURNSIDE: Yes. And you were confident that they would understand the literature the way you understood it?
DR VAISMAN: It’s very simple. If literature tells it, treatment should be at least 12 to 18 months.
MR BURNSIDE: Okay. And you were so confident that you would have the clinical coordinators say that regardless whether the doctor had specified 12 to 18 months?
DR VAISMAN: Because I am confident doctor will tell how long should be the treatment, yes.
MR BURNSIDE: Well, then, let’s just examine that for minute. Are you saying to his Honour that when you prepared this script, you believed that the doctors would always prescribe 12 to 18 months for the nasal spray, and therefore the clinical coordinators could say what they did whether or not they had heard what the doctor said?
DR VAISMAN: Because it’s clinical data which confirms that 12 to 18 months has a curative effect. Why would the doctor need to be told what is a curative effect?
MR BURNSIDE: Okay. So it doesn’t matter whether the clinical coordinator hears the doctor. They can say the doctor has recommended 12 to 18 months. Is that it? ---
DR VAISMAN: Because we’ve discussed ---
MR BURNSIDE: Is that right?
DR VAISMAN: We’ve discussed with the doctor – doctors – all doctors, the length of the treatment.
MR BURNSIDE: Right. The length of the treatment which they would always prescribe?
DR VAISMAN: Not – not because of me. It’s because of the studies.
MR BURNSIDE: But what if a doctor decided in some case that they weren’t going to recommend 12 to 18 months?
DR VAISMAN: Correct.
MR BURNSIDE: What if they didn’t? Still the clinical coordinator would say it?
DR VAISMAN: In majority of cases, I would say 95 per cent, doctors ..... and because it’s not ..... from the patient for, “How long should I take this treatment?”
MR BURNSIDE: Yes. Now, I will go back to the page 2669?
DR VAISMAN: 2669.
MR BURNSIDE: And about halfway through that text:
As you have just heard from Dr Blank, we have a medical solution to your problem. A treatment program will require your commitment for at least 12 months.
Now, was that supposed to be the clinical coordinator’s advice, or what the doctor had said?
DR VAISMAN: As I say, it’s well-accepted practice of all doctors to recommend 12 to 18 months, because it’s agreed .....
MR BURNSIDE: Please answer my question. Was that written there as medical advice to be given by the clinical coordinator, or on the assumption that the doctor would say at least 12 months?
DR VAISMAN: The clinical coordinator never gives medical advice. Only doctor.
MR BURNSIDE: Okay. So were the doctors expected to say 12 months, or 12 to 18 months?
DR VAISMAN: 12 to 18 months. Some of the doctors say 12, some of them say 12 to 18 months, some of the doctors even tell do it two years.
MR BURNSIDE: And how is the clinical coordinator meant to react, if they don’t know what the doctor has said as to the length of treatment?
DR VAISMAN: My instruction to clarify, “Doctor, for how long patients would take the treatment?”
MR BURNSIDE: Right. Okay. So the clinical coordinator should check with the doctor what the doctor has prescribed and what period he has recommended?
DR VAISMAN: Correct.
[TS 1633 – 1634]
615 The literature on which Dr Vaisman relied to support the need for a 12-to-18 month treatment period for ED and PE was produced as exhibit JV-4 to his first witness statement dated 13 September 2012 [R13.5]. The nature of JV-4 was explained in Dr Vaisman’s statement thus:
At the doctor’s education meetings I have regularly referred to the available medical and scientific literature which indicated that the chronic use of medications for PE and ED has a curative effect. This literature indicated to me that the appropriate period of treatment to most likely obtain such a curative effect was more than six months, and more probably in the range of 12 to 18 months. This period was not a “management preference”, as Dr Vandaleur indicates; rather, it was recommended duration based upon clinical evidence which I discussed at the doctors’ meetings. I now exhibit to this my witness statement as JV-4 a bundle of documents comprising medical and scientific literature which I had gathered in my office relating to the topic of chronic use of medications to treat sexual dysfunction conditions.
[Emphasis added.]
[R13.1, [42]]
616 The question arises whether the material on which the respondents relied supported treatment for a period of 12 to 18 months for ED and PE.
617 The articles in JV-4 made no reference to the treatment of PE at all. Dr Vaisman was forced to acknowledge this in cross-examination:
MR BURNSIDE: You remember all the articles in JV-4 that we went to, they were all referring to erectile dysfunction?
DR VAISMAN: Correct.
MR BURNSIDE: Yes, and the chronic use, as you say, of PDE5s?
DR VAISMAN: Correct.
MR BURNSIDE: You told his Honour this morning that you provide those articles to the doctors to demonstrate the utility of chronic use of apomorphine for the treatment of premature ejaculation?
DR VAISMAN: No, erectile dysfunction.
MR BURNSIDE: No, I took you to it very carefully in paragraph 42 of your statement?
DR VAISMAN: Apomorphine only for erectile dysfunction.
MR BURNSIDE: Okay. But you provide those articles to the doctors to show them the way to deal with both erectile dysfunction and premature ejaculation?
DR VAISMAN: Yes, and I particularly – I stressed this is the most safest way to treat the patients.
MR BURNSIDE: What is there in the articles in JV-4 that tells you anything at all about the treatment of premature ejaculation?
DR VAISMAN: Premature ejaculation?
MR BURNSIDE: Yes?
DR VAISMAN: Premature ejaculation absolutely different ---
MR BURNSIDE: Yes?
DR VAISMAN: --- ball game, nothing to do with erectile dysfunction. Different group of medication.
MR BURNSIDE: Yes. But at paragraph 42 of your statement you exhibit JV-4:
A bundle of documents comprising medical and scientific literature which I had gathered in my office relating to the topic of chronic use of medications to treat sexual dysfunction conditions.
Conditions, plural. And I asked you specifically this morning whether that referred to the chronic use of medication for PE and ED, as you say in paragraph 42?
DR VAISMAN: Correct.
MR BURNSIDE: Do you follow all that?
DR VAISMAN: Yes.
MR BURNSIDE: What is there in JV-4 that says anything at all about the treatment of PE?
DR VAISMAN: A lot of articles which says its treatment – the effect of the treatment very often started in a couple of months altogether.
MR BURNSIDE: Dr Vaisman, I will ask you to attend to the question carefully. What is there in JV-4 that has anything to do with PE?
DR VAISMAN: I don’t remember, I have to have a look what is in JV-4.
MR BURNSIDE: Yes. You looked at them over lunchtime and I want to suggest to you that none of them refer to PE at all?
DR VAISMAN: So, nobody ask me about PE.
MR BURNSIDE: You put those forward as medical and scientific literature relating to the topic of the chronic use of medications to treat PE and ED?
DR VAISMAN: Correct.
MR BURNSIDE: Yes?
DR VAISMAN: But that’s what I was asked. I have 10 times more literature about treatment of PE literature.
MR BURNSIDE: And they’re the documents you provide to the doctors?
DR VAISMAN: Correct.
MR BURNSIDE: Which tell them nothing about the treatment of PE?
DR VAISMAN: No, that’s history, that’s nothing – that was prepared three years ago, two years ago. A lot of things change for two years, for three years.
MR BURNSIDE: Well, wait as many years as you like, those articles still don’t refer to PE, do they?
DR VAISMAN: No. These articles represent ED.
MR BURNSIDE: And none of the articles in JV-4 say anything at all about the chronic use of medication for PE?
DR VAISMAN: Correct, because nobody ask me.
MR BURNSIDE: Well, then why did you say in paragraph 42 that you that this was:
A bundle of documents comprising medical and scientific literature […] relating to the topic of chronic use of medications to treat sexual dysfunction conditions
– plural, which you agreed referred to ED and PE?
DR VAISMAN: I’m sure I gave to my lawyers, I don’t know why it’s not here. But for PE even more material which proves the treatment should be at least between 12 to 18 months, even more.
MR BURNSIDE: Are you able to refer to any article which supports what you’ve just said?
DR VAISMAN: Because nobody ask me.
[TS 1746 –1748]
618 In its final written submissions, the ACCC made the direct allegation that the literature produced in exhibit JV-4 did not address the treatment of PE at all. The ACCC’s submissions contained an analysis of and commentary on all the articles in JV-4 in attachment 4. The ACCC also contended that the articles did not support the 12-to-18 month treatment period. The respondents’ final written submissions did not make any direct response to these allegations.
619 However, in the course of final oral submissions, counsel for the respondents handed up the respondents’ additional reference to scientific evidence. The document asserted that the ACCC had overlooked the scientific material produced by Dr Vaisman in other exhibits to his statement, including exhibit JV-1. This exhibit was described in Dr Vaisman’s first statement as containing material which he considered reflected good medical practice and the state of medical knowledge on the topic of sexual dysfunction.
620 The respondents then relied on the AUA Guideline 2004, which stated in relation to the duration of therapy for PE:
Therapy for PE most likely will be needed on a continuing basis. There is no clear consensus as to whether SRIs will effect an eventual cure of PE, allowing for discontinuation of the medication, or whether SRIs will be required for life. The Panel members’ experience is that PE usually returns upon discontinuing therapy.
[R13.3, p 12]
621 This Guideline does not support the practice of AMI in recommending 12-to-18 month treatment period for the treatment of PE.
622 Apart from the suggestion by Dr Vaisman that the scientific literature supported a 12-to-18 month period for the treatment of PE, there was no evidence supporting that practice.
623 Dr Pattison gave evidence that PE may be treated using behavioural techniques, counselling, and SSRIs. But this treatment was on a quite different model than that employed by AMI. Dr Pattison said that primary PE or serious secondary PE would usually require treatment by SSRIs to give patients satisfactory ejaculatory control. A patient would usually experience an improvement within a few weeks. Dr Pattison would review progress about a month after commencing treatment and thereafter at three months, and then possibly at six monthly intervals, to monitor the medication. He said that medication would usually be required for 6 to 12 months at least before considering tapering off [ACCC 3.28, p 27]. Dr Pattison’s comments do not provide support for the AMI contract length as they were made in relation to a different and accepted treatment method.
624 In their final written submissions, the respondents argued that the period of approximately 12 months was justified and appropriate for the treatment of “sexual dysfunction”. The only evidence referred to was evidence given during the cross-examination of Dr Vandeleur. He was asked about some answers which he had given to the ACCC in response to the s 155 notice served on him. In the answers, he said that he quite often recommended a starting period of 12 months where he thought it was clinically appropriate, and that with medication some patients could learn to delay ejaculation, for which, in his experience, 12 months was a reasonable timeframe [TS 732 – 733].
625 However, Dr Vandeleur also responded to the s 155 notice by saying that Dr Vaisman made it clear to him that Dr Vaisman’s preference was for him to recommend that patients try a treatment for an initial period of 12 months, and that he felt a general pressure to comply.
626 Dr Vandeleur explained the position in relation to PE more fully elsewhere in cross-examination as follows:
MR GREEN: And when you were doing that [informing the clinical coordinator of the treatment and the period of treatment] were expressing [sic] what you considered on, based upon your medical training and judgment, to be the appropriate time period, weren’t you?
DR VANDELEUR: No, not really. Initially, I didn’t set a timeframe when I was – I preferred not to have a timeframe but eventually, I felt that I probably should mention as I was told at least 12 months. So then I usually mentioned 12 months in the recommendation to the patient.
MR GREEN: Well, you only recommended 12 months, didn’t you, because that was what you thought was appropriate?
DR VANDELEUR: No, it was not the reason. I would never have mentioned 12 months if I hadn’t have been asked to mention 12 months.
MR GREEN: Well, you know, don’t you, that from the medical literature you’ve read, that premature ejaculation requires a period of time in order for a patient to potentially avoid the need for further medication?
DR VANDELEUR: But I didn’t read 12 months anywhere.
…
MR GREEN: Well, you go into great detail, don’t you, in your 155 statement about the considerations that you employed in determining a period to recommend for treatment, don’t you?
DR VANDELEUR: Yes. Look, I think that what the general gist of that was that I was within the framework. It seemed that I had to recommend 12 months and I made sure that it was still safe in doing so. But
MR GREEN: Well, you didn’t – sorry, doctor
DR VANDELEUR: So if I did prescribe a medication or recommend medication for 12 months, although I thought that that’s not ideal practice, I would prefer not to have to mention a 12 month period. But I never prescribed the medication in an unsafe way.
MR GREEN: Well, Dr Vaisman never told you how long to recommend. He simply told you that you needed to recommend a treatment period, didn’t he?
DR VANDELEUR: That wasn’t so much Dr Vaisman. I think it was more so the pressure from the salespeople via Dilip [Shrestha]. Really, I mean, I was told more than once to please recommend 12 months.
MR GREEN: So it’s correct to say that Dr Vaisman didn’t once tell you how long in which to prescribe. He didn’t direct you?
DR VANDELEUR: It may not have – it may have been Dilip but definitely from management, I was told not just once, but probably a couple of times, to please mention 12 months.
[TS 708 – 709, 710]
627 Dr Vandeleur’s position in relation to long-term contracts generally was accurately stated in his first affidavit sworn on 27 October 2011 as follows:
44 While it remained technically open to me to recommend shorter programs or no program or period at all, I concluded because of what had been communicated to me about management's preference, that I could not realistically work at AMI if I was not prepared to recommend at least 12 months to the patients I consulted.
…
46 I hated mentioning the 12 month period because it was an arbitrary period that I was expected to recommend to suit AMI's interests. In ordinary practice (meaning outside of AMI) I would not prescribe medication for 12 months and just send the patient away. …
47 I did not think that there was anything unsafe in the 12 month timeframe as such and accordingly reasoned at the time that I could make the recommendation. The only reason I recommended 12 months of medication was to comply with AMI's practices.
[ACCC 1.39]
628 Thus, Dr Vandeleur’s evidence provides no support for the AMI practice of recommending a 12-to-18 month treatment period for PE as scientifically based.
629 In relation to the treatment period for ED, Dr Vaisman again relied on the scientific material in JV-4 and on the respondents’ additional reference to scientific evidence, which included the references to material contained in exhibit JV-1. That material related to a wider range of topics than JV-4, which was specifically directed to the duration of treatment issue.
630 The respondents’ additional reference to scientific evidence then extracted from JV-1 seven articles relevant to the issue of the duration of treatment for ED and PE and set out the passages from those articles on which the respondents relied. As it happens five of the seven articles were already contained in JV-4.
631 Furthermore, there was an additional article, not referred to by the respondents but contained in JV-4 which, unlike the others, at least had a marginal relevance to the circumstances of AMI in that it referred to a study concerning the use of apomorphine in the treatment of ED.
632 The following analysis of those seven articles demonstrates that they do not support the 12-to-18 month treatment period recommended by AMI to ED patients. The italicised portions of the passages extracted below are the passages relied on by the respondents in their additional reference to scientific evidence.
633 An article published by Arthur Burnett entitled, “Vasoactive Pharmacotherapy to Cure Erectile Dysfunction: Fact or Fiction?” (2005) 65 Urology 224 (Burnett 2005), the author examined whether, as PDE5 inhibitors had become established as first-line therapy for ED in the on-demand use model, vasoactive pharmacotherapy might have a curative effect for ED [R13.5, p 13].
634 Burnett surveyed the clinical evidence relating to the use of pharmacological agents in restoring cavernosal tissue health after radical prostatectomy. He first referred to a study by Montorsi as follows:
An innovative study by Montorsi and colleagues involved early postoperative intracavernous injections of alprostadil in men with normal preoperative erectile function undergoing nerve-sparing radical prostatectomy. The investigators reported an increased recovery rate of spontaneous erections at 6 months postoperatively in 8 (67%) of 12 patients receiving alprostadil injections for 12 weeks compared with 3 (20%) of 15 patients monitored without treatment. Despite concerns of low patient enrollment, a lack of long-term follow-up, and possible biased accounts by patients who knew their treatment category, the study results yet suggested the intriguing possibility of vasoactive pharmacotherapy to improve or restore penile health under conditions threatening erectile function.
[Footnotes omitted.]
[R13.5, p 14]
635 Burnett then referred to a report by Padma-Nathan on which the respondents relied. Burnett stated:
A subsequent brief report further supported the possibility of improved spontaneous erection recovery in men using intracavernous alprostadil after radical prostatectomy. The principal observation was that an improved erection recovery rate occurred among men using the therapy within 300 days after surgery compared with after that time (73% versus 35%). A recognized major shortcoming of this evaluation was the absence of a control group.
[Footnotes omitted.]
[R13.5, p 14]
636 The passage relied on by the respondents is no basis for justifying the 12-to-18 month treatment period for several reasons. The study was not concerned with the treatment period other than to report the result as at the 300 day mark. It did not concern itself whether the recovery occurred earlier within that period. It related to recovery after radical prostatectomy which seems to be concerned with the recovery from nerve damage occurring in surgery. Further, it concerned medication by injected alprostadil, not the medication used generally by AMI or NRM for the treatment of ED in the cases in issue. And finally, the passage relied on by the respondents omits the shortcomings referred to in the sentence immediately following the sentence relied on by the respondents. It should also be noted that the Montorsi study reported similar recovery rates at six months post-operatively. Taken together, if anything relevant at all is to be drawn from these passages, it is that 26 weeks of treatment may be justified. But given the limitations referred to, this is not a conclusion which sufficiently relates to the circumstances of the practices of AMI.
637 Burnett then referred to two studies which assessed the use of PDE5 inhibitors for a curative effect on ED. The first was a study by Hellstrom of which Burnett said:
[I]t was demonstrated that the PDE-5 inhibitor vardenafil used on demand for 26 weeks in a randomized, double blind trial was associated with a greater likelihood of restoring normal erection compared with placebo, with function restored to a level between 79% and 89% among patients with mild erectile dysfunction and 39% of patients with severe erectile dysfunction. Although the study further exemplified the benefit of PDE-5 inhibitors to treat erectile dysfunction, it also revealed the potential of such treatment to achieve normalization of erectile function as an outcome exceeding less robust criteria such as erection improvement and successful penetration attempts. However, it is noteworthy that the results of such reports testify to the response to ongoing therapy without clearly demonstrating the resumption and persistence of natural function subsequently separate from treatment.
[Footnotes omitted.]
[R13.5, p 15]
638 The second study was by Sommer. Burnett wrote of this study:
A provocative study examining the long-term effects of daily use of sildenafil for erectile dysfunction was recently reported. The study was a prospective, randomized trial in which three groups of men with erectile dysfunction for more than 6 months were assigned to receive 50 mg sildenafil nightly, 50 to 100 mg sildenafil on demand, or no medical therapy (groups 1 to 3 respectively) for 1 year. After an additional 1-month "wash-out" phase of no treatment, 58.8% of group 1 and 9.7% of group 2 demonstrated a "normal" score of at least 26 on the erectile function domain of the International Index of Erectile Function questionnaire that was maintained after a 6-month "washout" phase in virtually all patients (19 of 20) of group 1 whose erectile function had normalized at 1 month. Penile ultrasound studies done at the 1-year interval evaluating cavernosal peak systolic velocity confirmed a statistically significant average improvement in group 1, with a slight improvement in group 2 and a decline in group 3. … The study did promote PDE-5 inhibitors as having potential curative benefit for erectile dysfunction. However, because of the limited information about the patient population and the likelihood that erectile function among the participants was not significantly impaired at baseline, such definitive conclusions from this preliminary report should be made cautiously.
[Footnotes omitted.]
[R13.5, p 15]
639 Again, these studies do not justify the 12-to-18 month treatment period offered by AMI. They did not involve the medications used by AMI. They had limitations in the process used for testing. In the first study the treatment period was 26 weeks.
640 Burnett then turned attention from clinical evidence to experimental evidence:
Direct experimental evidence showing that vasoactive pharmacotherapy sustains the health of erectile tissue has remained limited.
[R13.5, p 16]
641 And finally Burnett postulated, in a passage relied on by the respondents:
It may be contended that conventional pharmacotherapeutic agents used for erectile dysfunction offer long-term beneficial effects on erectile tissue based on their known pharmacologic properties.
[R13.5, p 16]
642 This was a speculative exercise which Burnett then applied to the medications alprostatil and PDE5 inhibitors. In respect of PDE5 medications, Burnett hypothesised that they may exert healthful effects on cavernosal tissue by the regulatory actions of their “biochemical products, cyclic adenosine monophosphate and cyclic guanosine monophosphate.”
643 Dr Vaisman said that apomorphine did not act in that way. The following exchange occurred in cross-examination:
MR BURNSIDE: Have you any article which supports the idea that apomorphine operates so as to stimulate smooth muscle cell replacement via a cycle [sic] guanosine monophosphate mechanism?
DR VAISMAN: Absolutely different mechanism affection.
MR BURNSIDE: Yes?
DR VAISMAN: Apomorphine acting centrally so the brain, not the same – this mechanism only local.
MR BURNSIDE: Right?
DR VAISMAN: For the blood vessels. Apomorphine working for the brain.
MR BURNSIDE: So the fact that they operate quite differently makes it difficult to say that because chronic use – whatever that may mean – of PDE5 inhibitors may be indicated that therefore chronic use of apomorphine will be similarly indicated?
DR VAISMAN: Correct.
[TS 1733]
644 Burnett advocated a rigorous clinical trial process to establish a treatment regime. In particular, he noted the limits of using patients who had undergone radical prostatectomy for this purpose because:
[E]ventual recovery of spontaneous function may occur as assorted physical and psychosocial impediments to be sexually functional heal or are overcome.
[R 13.5, p 17]
645 Burnett concluded:
This review conveys the opportunities and challenges associated with advancing the "curative intent" of vasoactive pharmacotherapy for erectile dysfunction. Current observations have revealed the excitement of this mode of therapy, particularly for men after radical prostatectomy, although the extent of evidence-based support for it remains limited. In this light, continued basic scientific and clinical investigations of this subject are encouraged.
[R13.5, p 18]
646 Wayne Hellstrom and Muammer Kendirci published an article entitled, “Type 5 Phosphodiesterase Inhibitors: Curing Erectile Dysfunction” (2006) 49 Journal of the European Association of Urology 942 (Hellstrom 2006) in which they considered whether chronic administration of PDE5 inhibitors had a curative effect on ED [R13.5, p 29].
647 In a passage relied on by the respondents the authors explained the subject matter of the article thus:
Vasoactive pharmacotherapy (ie, type 5 phosphodiesterase [PDE5] inhibitors) traditionally uses an “on demand,” acute method of administration. However, recent data propose “chronic” long-term administration of these agents as a “curative purpose” in the management of ED. There have been clinical and basic research findings supportive of this application of PDE5 inhibitors in “curing” ED.
[Footnotes omitted.]
[R13.5, p 29]
648 In passing, it might be noted that reference to this passage is duplicated in the respondents’ additional reference to scientific evidence (at [2] and [6]), and on both occasions it is wrongly attributed to different articles. Paragraph 2 attributes the passage to an article by Brock and others, and [6] of that submission attributes it to an article by Guilaino and others.
649 The authors of Hellstrom 2006 first examined the clinical evidence for the chronic use of PDE5 inhibitors to treat ED. They referred to a further study by Sommer. The respondents again relied on this reference in their additional reference to scientific evidence.
650 The authors also referred to a study by Caretta and said:
Caretta et al. investigated the effect of continuous, regular administration of tadalafil on erectile function in elderly men with ED. Sixty subjects, aged 60–70 yr, with a history of ED for 6–12 mo received 20 mg tadalafil on alternate days for 3 mo. Men younger than 40 yr old with psychogenic ED served as controls. At baseline and 1 mo after the end of treatment, all patients were evaluated with nocturnal penile tumescence and rigidity (NPTR) monitoring and penile Doppler ultrasound evaluation of the carotid artery intima-media thickness (IMT). They reported that in elderly men with increased or normal carotid IMT, chronic treatment with tadalafil improved endothelial function and concomitantly induced spontaneous resumption of erectile function.
[Footnotes omitted.]
[R13.5, pp 29 – 30]
651 The authors then examined the clinical evidence of the treatment of radical prostatectomy patients by chronic use of PDE5 inhibitors. They said:
Although, evidence from studies on penile rehabilitation after RP support the concept of chronic administration of vasoactive agents to recover spontaneous erectile function, the rationale and mechanism for their use in penile rehabilitation programs after RP have not been fully elucidated nor have they been replicated in large multicentre placebo-controlled trials.
[R13.5, p 30]
652 The authors then referred to the Montorsi study also referred to in Burnett 2005. Additionally, they referred to another study by Padma-Nathan and others as follows:
A recent prospective study reported a significant benefit of either 50 mg or 100 mg of sildenafil administration each night for 7 mo, compared to placebo, in men after undergoing bilateral nerve-sparing RP. In this study, the patients receiving sildenafil for 36 wk documented a 27% return of spontaneous, normal erectile activity compared to 4% in the placebo group. This study remains in abstract form and still has not been published.
[Footnotes omitted.]
[R13.5, p 30]
653 The respondents relied on a passage at the end of this discussion which stated:
In a recent prospective study, Mulhall et al. evaluated the use of an erectogenic pharmacotherapy regimen following RP as to whether it improved recovery of spontaneous erectile function. Chronic use of oral and intracavernous vasoactive agents in this study resulted in improvements in a number of outcomes …
[Footnotes omitted.]
[R13.5, p 30]
654 No details were provided concerning the Mulhall study. The reference is therefore of no value.
655 Hellstrom and Kendirci then referred to animal studies which supported the concept of chronic use of PDE5 inhibitors to improve endothelial dysfunction.
656 And, in relation to the biologic effects of chronic administration of PDE5 inhibitors on human erectile tissue, the authors stated in a passage relied on by the respondents:
Given the importance of the NO/cyclic guanosine monophosphate pathway in cavernosal smooth muscle function, chronic administration of vasoactive agents (including PDE5 inhibitors) may offer long-term beneficial effects on erectile tissue. Vardenafil has recently been shown to increase circulating progenitor cells in humans. These cells are recognised to play a role in the process of neovascularisation and the continuous repair of the endothelium.
[Footnotes omitted.]
[R13.5, p 31]
657 Then the authors concluded:
A number of animal model experiments, where induced ED has shown benefit from longterm PDE5 inhibitor administration, is the most plausible evidence that we have on supporting this concept. However, in short, more is certainly still needed at the basic research level to further elucidate these biologic concepts.
[R13.5, p 31]
658 And, in relation to clinical practices, the authors concluded:
On the clinical front, although many clinicians have instituted chronic PDE5 inhibitor therapy as the standard of care in their prostate cancer treatment and diabetic patients, with the hopes of improving erectile function, the reality is that there is a paucity of published studies available on which to base their claims. For the most part, studies are of short duration, are in abstract form, are single centre, have few subjects, and often confuse preference with documented physiologic benefit. Many are not placebo-controlled and, as most investigators in sexual medicine are aware, the placebo effect has a strong psychogenic benefit.
… evidence to support the reversal of ED by chronic administration of a PDE5 inhibitor is still not convincing to many.
[R13.5, p 31]
659 For the same reasons as expressed in [633] – [642] of these reasons for judgment in relation to Burnett 2005, this article does not justify a treatment period for AMI medication for ED of 12 to 18 months. The article added the study by Caretta which demonstrated improvement in erectile function after three months.
660 Dr Antonio Aversa and others published an article entitled, “Relationship between chronic tadalafil administration and improvement of endothelial function in men with erectile dysfunction: a pilot study” (2007) 19 International Journal of Impotence Research 200 (Aversa 2007), which reported on the therapeutic effect of tadalafil taken on-demand compared to the therapeutic effect if taken on a regular scheduled basis. This was a randomised cross-over study in which 20 men took 20 mg of tadalafil in two treatment periods. In one period they took tadalafil on-demand and in the other they took it on alternative days (AD). Each period was four weeks. The result was reported in the passage relied on by the respondents thus:
The present study provides evidence, not previously reported, of an expected outcome that tadalafil on an AD dosing improves endothelial dysfunction and that these effects are also evident in other vascular districts, that is, carotid arteries, even after discontinuation of therapy.
[R13.5, p 5]
661 The article concluded thus:
We are aware of the caveats of this study, lacking a placebo arm which might have demonstrated effectiveness in improving endothelial responsiveness in patients with vascular impairment. … This is a confirmatory study, which suggests that larger controlled multicenter studies involving representative populations for longer duration periods and follow-up after withdrawal should be encouraged.
[Footnotes omitted.]
[R 13.5, p 7]
662 Again this article does not assist the respondents’ argument. The medication was not the medication used by AMI to treat the majority of the Annexure B and C patients. The treatment time was four weeks not 12 to 18 months. The study was limited to 20 men and the study itself recognised inherent limitations.
663 The respondents also relied on an article by Edward D. Kim entitled, “Local Therapies to Heal the Penis: Fact or Fiction?” (July/August 2009) 30(4) Journal of Andrology 384. The article reviewed the scientific evidence concerning penile rehabilitation therapy using PDE5 inhibitors and alprostadil. The author observed that most studies had involved treatment following radical prostatectomy. On the then current state of the clinical studies, Kim said:
Although an increasing number of studies are providing a signal that therapies for penile rehabilitation facilitate the return of spontaneous erections after RP, these publications have relatively small numbers of patients and have not yet been replicated. Reproducible largescale, long-term, randomized double-blind placebo controlled studies are necessary.
[R13.5, p 104]
664 In addition to the studies which have already been outlined in the previous articles, Kim reported studies undertaken in 2007 and 2008. Bannowsky and others conducted a post radical prostatectomy trial involving 23 men who took 25 mg of sildenafil nightly for 52 weeks and 18 men who received a placebo. There was a significant improvement in the recovery of penile function for the men taking nightly sildenafil over those receiving a placebo. By contrast, Montorsi and others conducted a trial involving 628 men following radical prostatectomy. It was a randomised, double-blind, double-dummy, multi-centre, parallel group study. The men were randomised to placebo, nightly vardenafil, or on-demand vardenafil for nine months. No statistically significant differences were observed in relation to the strength of erection or sexual success rates. On-demand dosing was efficacious but nightly vardenafil for the purpose of penile rehabilitation was not efficacious.
665 Kim concluded:
This well-designed study provides a cautionary note for the present enthusiasm of oral PDE-V inhibitors for penile rehabilitation therapy.
[R 13.5, p 105]
666 Overall, Kim concluded:
At the present time, the study of penile rehabilitation is in active evolution. The body of literature suggests a beneficial role of local therapies for the restoration of erections after injury. However, although most published reports point towards improved outcomes with active treatment, nearly all studies have significant limitations. As a result, point-counterpoint debates have become common regarding this subject (Mulhall and Morgentaler, 2007).
The basic arguments supporting the role of local therapies for penile rehabilitation therapy are that 1) a mechanism for the protection of endothelial function and smooth muscle function is present, 2) animal models of chronic dosing of PDE-V inhibitors clearly demonstrate improvement in erectile response, and 3) human data with intracavernous, intraurethral, and oral PDEV therapies point to improvement of erectile function. The counterpoint argument notes that the present human studies have significant limitations that do not permit any type of definitive conclusions regarding the benefit of therapy. However, all agree that reproducible, randomized, controlled trials whose results can be replicated are necessary to clearly define the role of penile rehabilitation therapy.
[R13.5, p 106]
667 It is against the context of this article that one must view the two sentences relied on by the respondents. Those sentences are italicised in the following passage:
I offer penile rehabilitation therapy to those patients who are motivated to pursue a 9–12-treatment course. I explain that although the basic science is compelling and the clinical studies are suggestive, I consider this field still investigational. Although use of oral PDE-V inhibitors on a regular basis after RP is popular and commonplace, the body of evidence is still limited. I offer these men a PDE-V inhibitor with every-other-day dosing starting 2–4 weeks postoperatively. I encourage them to split the highest-dose tablet for cost savings.
These men are instructed that the best return of erectile function may take 18–24 months postoperatively. They are instructed to try the highest dose of their PDE-V inhibitor before sexual activity for use on demand. I remind them that results may not be evident for over 1 year. They are cautioned that if ED, however mild, is present preoperatively, I am not optimistic about the return of erectile function.
[R13.5, p 107]
668 And the author concluded:
Significant advances over the last decade have led to an increased understanding of the possibilities for local therapies for healing of the penis. The most studied model has been penile rehabilitation after RP. Compelling rat models demonstrate a beneficial effect of PDE-V inhibition after cavernous nerve injury. Clinical studies in men have been suggestive, but not yet conclusive, regarding the benefit of local therapies in restoring the return of spontaneous erections. Although the practice of frequent administration of PDE-V inhibitors has become a standard for urologists, a reproducible, randomized, placebo-controlled trial is necessary for more definitive conclusions.
[R13.5, p 107]
669 To the extent that this article brings the history of the development of the treatment up to date from the earlier articles, it similarly fails to support the respondents’ claim that a 12-to-18 month treatment period for ED is validated. Again, the medications used in the recent studies were not those generally used by AMI, most studies were concerned with the restoration of function after damage caused by surgery in radical prostatectomy, which is a different circumstance than ED otherwise caused, and the limitations of the studies are indicated in respect of each study. But critically, none of these studies were directed to the question of the appropriate duration of treatment for ED.
670 Then, the respondents relied on an article published by Dr Patrick Teloken and others entitled, “Post-Radical Prostatectomy Pharmacological Penile Rehabilitation: Practice Patterns Among the International Society for Sexual Medicine Practitioners” (2009) 6 Journal of Sexual Medicine 2032, in which the authors reported on a survey of practices of members of the International Society for Sexual Medicine Practitioners in pharmacological penile rehabilitation following radical prostatectomy. Three hundred and one physicians out of a membership of 3,000 answered an on-line questionnaire. Ninety-five per cent of those who responded used PDE5 inhibitors as part of the primary strategy for penile rehabilitation. As to the duration of treatment for rehabilitation:
With regard to the duration preferred for rehabilitation approximately 40% used rehabilitation for less than 12 months, and almost 30% used rehabilitation for 13-18 months, and a similar proportion opted for durations longer than 18 months.
[R13.2, p 9]
671 Again, this article does not bear on the validity of the 12-to-18 month treatment period recommended and offered by AMI. These rehabilitation practices used different medications and were directed to repairing nerve injury following prostate surgery.
672 The respondents quoted from an article by Dr Benny Verheyden and others entitled, “Effects of 12-Month Tadalafil Therapy for Erectile Dysfunction on Couple Relationships: Results from the DETECT Study” (2009) 6 Journal of Sexual Medicine 3458 as follows:
The Determinants of Continued Use of Tadalafil (DETECT) is a prospective observational study designed to evaluate, over 12 months, predefined treatment outcomes associated with tadalafil therapy in men with ED in a natural, clinical practice setting. The effectiveness of, and satisfaction with, tadalafil treatment continuation has previously been reported. We report here the views of the patient with ED on his partner's awareness and support of treatment, and his perception of problems in his relationship before and after 12 months of treatment with tadalafil, as well as those factors identified as being associated with relationship changes.
…
A total of 1,900 patients with ED were included.
…
Approximately 17% of men with ED initiating tadalafil treatment in this study perceived that they had relationship problems with their partner. Improvement of ED with tadalafil therapy was associated with a significant reduction in perceived relationship problems. Conversely, treatment with tadalafil was infrequently associated with newly perceived relationship problems and newly perceived sexual problems in the partner.
[Footnotes omitted.]
[R13.5, p 42, 49]
673 It is not clear why the respondents referred to this article because it does not state any conclusions about the length of treatment necessary for ED.
674 Finally, the article which was not referred to by the respondents, but was the only one which, in passing, dealt with the use of apomorphine for the treatment of ED, was Hackett 2002 referred to earlier at [253] and [467] of these reasons. When discussing the risks of myocardial infarction associated with taking sildenafil for men with ischemic heart disease Hackett said:
Many patients will select sublingual apomorphine or ICIT [intracavernosal injection therapy] because of concerns about MI [myocardial infraction] with sildenafil. However, a number of men with severe IHD [ischemic heart disease] may be disappointed in the outcomes of therapy with sublingual apomorphine. In a recent randomized, doubleblind, placebo-controlled crossover study of 296 men with ED of various severities and etiologies, 42% of attempts resulted in erections firm enough for sexual intercourse among men with CAD [coronary artery disease] who were treated with sublingual apomorphine 3 mg for 4 weeks compared to 28% with placebo; this difference was not statistically significant, although the number of CAD patients was small (n = 14).
[Footnotes omitted.]
[R 13.5, p 25; R 13.2, p 39]
675 This study does not justify the practice of AMI. To the extent that the results support the use of apomorphine, the improvement occurred after treatment for four weeks.
676 Then, the respondents argued that patients did not uniformly enter into contracts for 12 months or more. There were examples of three or six-month contracts. However, those examples are few in number. In those cases, salespeople often tried to sign up patients for 12 months or more, but offered a reduced term in response to the patient insisting that they could not afford the greater expense of a longer contract.
677 Dr Pattison gave evidence about the duration of treatment for ED and PE using conventional treatments. He stated in Pattison Report 1 that “… ED is rarely cured. It is better to regard ED as a lifelong condition that can be successfully managed with oral medications in about 65 – 70% of cases … Most men with significant ED have a continuing need for medication” [ACCC 3.28, p 24].
678 For primary PE, Dr Pattison stated that most men require ongoing treatment [ACCC 3.28, p 27]. For secondary PE, if medication is required the Andrology Australia PE Guide suggests a trial of three to six months [ACCC 3.28, p 59].
679 From this discussion, it follows that the 12-to-18 month treatment period recommended and offered by AMI to patients for both ED and PE is not supported by the scientific evidence before the Court.
680 The ACCC alleged that AMI engaged in unconscionable conduct in the terms on which it agreed to refund to patients part of the cost of treatment where the treatment was unsuccessful (AMI refund term), by the way in which the term was represented to patients, and by the way in which it was applied and enforced.
681 In particular, the ACCC alleged that AMI did not disclose to patients that, in order to obtain a refund, they would need to try at least one option from each treatment method offered, including self-administered intracavernosal injections in the base of the penis for both ED and PE. Further, patients were not told that AMI would deduct from the refund sum amounts for administration costs and for the cost of any medication provided.
682 The AMI refund term was as follows:
Satisfaction and Privacy Policy
Introduction
Congratulations on choosing AMI’s treatment program. Our Doctors and staff will work with you to optimize the most appropriate treatment program to enable you and your partner to dramatically improve your lifestyle by re-establishing an active sex life and recapturing the sexual intimacy experienced by you and your partner in your relationship.
With AMI’s assistance you can experience the real Healing Power of Sex.
Guarantee
AMI offers programs designed to assist you in overcoming your current problem with your first treatment. Another goal of your program it to offer lasting results. It is however our experience that some patients do not always respond successfully at first.
AMI will at all times endeavour to obtain the best solution for your problem where you understand all appropriate therapies prescribed by the doctor.
There is a range of treatment options and delivery methods which can include:
• Nasal Spray
• Troches (Lozenges)
• Intra Urethral Gel
• Self Injection Therapy
A doctor from AMI will diagnose and prescribe the most appropriate form of treatment available to assist you.
AMl experience shows that between 60% and 70% of patients obtain immediate results and are well satisfied following their first course of treatment.
If required AMI doctors will work with you to achieve a successful outcome by adjusting your prescribed medication, varying your medication options or by trying an alternative delivery method.
Satisfaction
The following terms are agreed by both parties;
1. You agree to try at least one option from each of the treatment methods as prescribed by your AMI doctor before a refund case can be considered.
2. If you are still unable to overcome your current problem using all AMI treatment methods as prescribed by the AMI doctor and an AMI doctor decides that the treatment has not been successful and that further treatment options and methods under the program are inappropriate or unavailable to you, then AMI will refund the cost of the treatment incurred by you, less a 15% administration fee and less the cost of the medication supplied to you.
3. You must notify AMI immediately if you are experiencing any problems with your medication and if these are of a medical nature, you agree to see a medical doctor for appraisal.
4. You must notify AMI of any drugs you are taking or any change to your medication routine.
5. For all enquiries please call the Customer Service Department on 1300 857 009 which will facilitate the process.
6. Where a refund is either in dispute or needs further clarification it will be passed onto a case manager in the Refund Department who will review the case and discuss the various options available. The Case Manager will pass on his recommendations to the Refund Manager for final determination.
Cancelation of Direct Debit Request (DDR)
Before a DDR can be considered for cancellation you agree to:
1. Try at least one option from each of the treatment methods as prescribed by your AMI doctor.
2. Cancellation will only be approved if an AMI doctor finds you are medically unsuitable for AMI medications.
[Emphasis added.]
[ACCC 1.41, pp 40 – 41]
683 These terms were contained in the last three pages of the 20-page instruction booklet. The instruction booklet was sent to a patient by mail with the AMI medications after the phone call in which he had agreed to undertake AMI’s treatment. The first 17 pages of the instruction booklet dealt with the treatment options for ED and PE. They explained how to use the different medications and covered such subjects as dosage and timing of administration. The instruction booklet also referred to the side effects of the medications and the manner in which they had to be stored.
684 Save for the reference to the AMI refund term, the instruction booklet did not appear to be a contractual document. It did not, for instance, contain the cost of the particular treatment for the patient in question, the duration of the treatment or the payment obligations of the patient.
685 Usually some reference was made either by the doctor or the salesperson to the instruction booklet in the course of a phone call with a patient. However, in no case was reference to the instruction booklet made to alert a patient to the AMI refund term. Rather, the instruction booklet was usually mentioned in relation to instructions for the use of the medication or perhaps in relation to the side effects of the medication.
686 The responsibility for explaining the AMI refund term to patients lay with the salespeople. Mr Shrestha said that there had been problems before 2008 because salespeople did not always explain the term [TS 2233–2234]. As a result, AMI issued a direction to the salespeople. When they were taking the credit card payment authorisation from the patient, the salespeople were directed to say to the patient:
If you do not receive the desired result with the first recommended treatment followed by other available options if needed, AMI’s refund policy will be applicable to you.
Do you agree?
[ACCC 17]
687 The direction did not adequately draw attention to the compulsion on the patient to try all the treatment options in order to obtain a refund, and made no mention of any deductions in the calculation of the refund amount. The brevity of the reference suggests that it was devised in such a way as to be lost in the general flow of the conversations.
688 A consideration of a random selection of the Annexure B consultations illustrates that even this cursory reference to the refund term was regularly omitted.
689 I selected seventeen consultations at random, but with the aim of having a spread of salespeople represented. The selected consultations involved 11 different salespeople, namely, Vincent, Kris, Brian, Hanspeter, Gary, Lori, Csaba, Igor, Jacob, George, and Zac.
690 In nine cases (patient 28, patient 42, patient 50, patient 62, patient 86, patient 95, patient 100, patient 111, and patient 140) the words of the direction were used, or the general sense was captured. Thus, patient 95 was told:
GARY: So that's pretty much the way it works. Um, look, if the medication stopped working or none of our medications work, we stop the program.
PATIENT: Okay.
GARY: Yeah. So, you know, you're not locked into something that doesn't work, of course.
…
GARY: And, of course, the following warranty applies. As I said to you before, if you don’t get the desired results with the first medication, we can swap and change that for no additional charge for you, and if none of the medications work then, of course, AMI’s refund policy will work and we’ll stop the program for you there.
[ACCC 4.371, p 16, 19]
691 And patient 140 was told:
JACOB: Okay. It will also come with a written satisfaction policy. It’s just the safety net for every single patient and entitles everybody to a refund in the unlikely event that we couldn’t get you a result with any of the medications or if they didn’t agree with you.
[ACCC 4.355, p 21]
692 In four cases (patient 34, patient 52, patient 73, and patient 156) the direction was not followed, but the AMI refund term was mentioned without any further explanation and often with the remark deflecting the patient’s consideration away from the issue. Thus, patient 34 was told:
KRIS: You can put that on the credit card, so you can pay for 12 months or 18 months, 24 months, whatever there is, and everything all under control. We will even give you a refund policy just in case to back you up, but it won’t happen to you.
[ACCC 4.272, p 16]
693 And patient 156 was told:
VINCENT: Now, what we do for you, [Patient], over the 12 to 18 months we give you an unlimited supply of it. You get round the clock medical support. There’s a satisfaction policy in place that backs it up for you as well. And really, mate, I can have you started within about a week…
[ACCC 4.232, p 11]
694 Then, in four cases (patient 60, patient 88, patient 124, and patient 131) nothing was said about the AMI refund term.
695 Apart from the question in issue in this case, namely, whether these circumstances on their own or together with others constituted unconscionable conduct, there is a real question whether the AMI refund term became part of the contract between the parties at all. However, that matter need not be explored further.
696 On the analysis of the ACCC, which the respondents did not challenge, 48 of the 152 Annexure B patients were contraindicated for intracavernosal injections by doctors during the consultations with patients. That meant that 104 patients, including PE patients, if they entered into contracts with AMI after the consultation with doctors, would be required to try self-administered injections into the base of the penis if the other treatments did not work.
697 Dr Vaisman said that 40 per cent of ED patients would need to try injections because other methods of treatment would be ineffective for them [TS 1705 – 1706]. Dr Goyer said that the idea of a needle in the penis was to most men “the worst possible thing imaginable” [TS 2329]. He also said in an exchange with the Court:
HIS HONOUR: Yes, I’m just trying to draw on your – not your – this is not directed to your practice because you’ve said you didn’t know about the contracts, but making these assumptions, what do you, with your medical training and your experience in AMI, but more particularly your knowledge of medical good conduct … what you think doctors should do in that situation about the prospect that there might be a legal obligation to undergo up to the point of injections?
DR GOYER: Yes. It’s a very a good question and having that knowledge on board, you know, I would think it would be appropriate to give information about other medications. If it is under contract, that would be needed. I think so. I mean, it kind of – it jumps across a barrier between medicine and finance, doesn’t it? A little bit because it’s the – you know, refunds is a financial thing, not a medical thing so that’s kind of a bit in both courts, but I would agree, your Honour. Yes.
[Emphasis added.]
[TS 2329 – 2331]
698 Mr Shrestha also said that it was important that patients be told of the possibility of injections before committing to the treatment [TS 1986]. Mr Shrestha said that it was the doctors’ role to tell patients of the possibility of injections.
699 A review of the Annexure B consultations shows that no patient was told directly that he would have to self-administer an injection in the base of his penis in order to qualify for a refund.
700 And on the ACCC’s analysis, which the respondents did not challenge, in 52 of the 104 cases of patients not contraindicated for injections, no reference was made in the consultations with doctors or in the interactions with salespeople to injections as a method of treatment.
701 In the remaining 52 cases, the doctors referred to injections as a mode of treatment, but not in connection with the topic of AMI’s refund term. The ACCC submitted that these references were general and made in a way which generally deflected from the possibility of the patient needing to use them. There were certainly examples of that type of reference. Thus, Dr De Sayrah told patient 64:
So what we do is we treat the premature ejaculation first. Now, to treat the premature ejaculation, we have medications of varying types. We have the nasal spray and the capsules, are the same medication. We also have the injections. You don’t have to bother about the injections at this stage, okay. Now, what the nasal spray does is – we prefer the nasal spray because it acts quickly. It gets absorbed from the lining of the nose, and within 20 to 30 minutes, it becomes effective, and once it becomes effective, it stays in your system for about approximately six to eight hours.
[ACCC 4.317, p 10]]
702 A similar example can be seen with patient 83 [ACCC 4.349, p 8].
703 In other instances, the reference was cursory. Thus, Dr De Sayrah told PE patient 36:
So what we use, we use medication in the form of a nasal spray or tablet. We also have injections – that’s a last resort – when things don’t work out. For some people we resort to that. But you don’t have to even … think about it. We start with the nasal spray.
[ACCC 4.275, p 7–8]
704 Dr Vandeleur adopted a similar approach with patient 28 [ACCC 4.262, p 10].
705 On the other hand, Dr Lonergan usually explained the treatment quite fully. He told patient 11:
DR LONERGAN: If that bothers the patients at all, we immediately replace it for them with a tablet form. It’s the same drug. It works exactly the same. It works just as well. It’s just a little bit slower to kick in. That’s the only difference.
PATIENT 11: No problem.
DR LONERGAN: So we’ve really got it there to suit the patients. If we need something a bit stronger – sometimes in some people you do for a while – we change it to the next thing we use, then we use a similar sort of thing to what diabetics use. We use a tiny insulin syringe in a diabetic pen and you just put the tip of the pen down the base of the penis at your body, press a button and it does it for you. They’re tiny. You can’t feel it or see it. That can also give quite good results. But usually in a healthy man like yourself we start with the nasal spray because, as I said, it’s just so quick and easy to use it.
[ACCC 4.242, p 8]
706 Other examples of virtually the same explanation by Dr Lonergan can be seen in consultations with patients 71, 92, 105, 129 and 130.
707 Dr Vaisman said that the doctors knew the terms of the contracts between patients and AMI. It was up to them to determine as a matter of clinical judgment whether to tell the patient about injections. He explained in cross-examination:
MR BURNSIDE: Dr Vaisman, do you agree that yesterday you said that about 40 per cent of ED patients ultimately need injections?
DR VAISMAN: Correct.
MR BURNSIDE: And you would agree that every patient who presents with ED should be warned of the possibility that they will need injections?
DR VAISMAN: Yes. It’s up to the doctors. I cannot tell them what to do, what not to do.
MR BURNSIDE: Well, you would agree that it’s medically appropriate that they be told of that possibility?
DR VAISMAN: It’s up to the doctor. If doctor decided not to tell because to frighten the patient, maybe, he doesn’t tell, I cannot tell him what to tell, what not to tell.
MR BURNSIDE: Were the doctors told that the patients would be signed up to a contract which required them to accept each level of treatment - - - ?
DR VAISMAN: Of course.
MR BURNSIDE: - - - if necessary?
DR VAISMAN: Of course.
MR BURNSIDE: The doctors knew that, did they?
DR VAISMAN: Yes.
MR BURNSIDE: And knowing that, you would agree that it was necessary for them to warn people that they would have to have injections if the other stages of treatment didn’t work?
DR VAISMAN: Maybe they didn’t want to threaten them. Some of the doctors mention this, as far as I know, some of them not. I cannot tell them what to do, what not to do. It’s their duty.
MR BURNSIDE: Well, as a medical practitioner yourself, you would agree that it would be medically appropriate to warn patients that their condition may require injections and their contract would require injections if other treatments didn’t work?
DR VAISMAN: Yes and no. Yes and no because a lot of patients as soon as you mention them about the injection they refuse from any treatment. They stay impotent for the rest of their life only because of the fear of the injection.
MR BURNSIDE: And that’s - - - ?
DR VAISMAN: It’s not in the best interest of the patient.
MR BURNSIDE: That’s a pretty wide-spread fear, is it?
DR VAISMAN: I think so.
MR BURNSIDE: Yes. When you looked through the transcripts that you did look through, did you notice that in a number of ED cases there was no reference to injections?
DR VAISMAN: Yes.
MR BURNSIDE: And you saw that that was a bad thing?
DR VAISMAN: As I repeat, it’s up to the doctor. I cannot tell to the doctor what to do, what not to do, but as far as I know some of the doctors regularly mention the possibility of the injections.
HIS HONOUR: But Dr Vaisman, what you can do is not employ particular doctors?
DR VAISMAN: It’s not correct. The country is short so much of the doctors that I always employ the first who apply. I never have a choice from two. The country is so short of the doctors, and I pay to the doctors a lot of this money, up to $2000 per day to do this job. And I cannot find the doctors.
HIS HONOUR: But if the doctors are doing things which you know are not proper in terms of disclosing, for instance, the consequences of the treatment, then you had the option to let them go?
DR VAISMAN: If I let them go I will lose a lot of money. Nobody else will do the job.
[TS 1811 – 1812]
708 The evidence of Dr Berry and Dr Goyer was that they did not know of the terms of the contract between the patients and AMI [TS 2400 and 2327]. Dr Berry said she did not know that the contract required the patients to try injections [TS 2401]. Dr Vandeleur learned of the requirement for patients to try injections when a complaint was made against him to the Medical Board of South Australia. He explained in his first affidavit affirmed on 27 October 2011 that:
48 One of the treatment options offered by AMI was intracavernous injections that were administered at the base of the penis (ICls). As I mention below, in September 2007 I received a complaint from the Medical Board of South Australia regarding my consultation with an AMI patient. As a result of being provided with documents and information concerning the complaint I learned that patients who wished to discontinue an AMI treatment program were expected to try all AMI treatments (including ICls) before being offered a refund for the program. I understood from the complaint that if one treatment did not work, the patient would contact AMI and be directed to a designated team of nurses and that there would be a requirement to use ICls unless an AMI doctor had expressly contraindicated ICls for that particular patient.
49 I did not consider it appropriate to prescribe ICls for the treatment of PE. I thought that it was an unnecessary risk to prescribe ICls to any patient with no erection problem because it might induce a priapism (an erection that does not subside) which is a medical emergency and can result in permanent damage to the patient's penis. The use of ICls also requires careful instruction which, in my opinion, should be given in person. There are circumstances in which the use of ICls is appropriate, for example patients with minimal erectile function and who are not responding to 5PDE inhibitors.
[ACCC 1.399]
709 Dr Condoleon was the only doctor who gave evidence that he had knowledge of the AMI refund term. The following exchange occurred in cross-examination:
MR BURNSIDE: Were you aware that up until the time, up until late-2010, early-2011, the patient was contractually obliged to try each of the other medications before they were allowed to cancel their contract?
DR CONDOLEON: Unless any of those were contraindicated, I did have that impression, yes.
MR BURNSIDE: Yes. You were aware of that?
DR CONDOLEON: Yes.
[TS 2272]
710 Dr Vandeleur told how Dr Vaisman and Mr Shrestha encouraged doctors not to mention injections. He said in his first affidavit:
54 During doctors' meetings Jack Vaisman said that his preference was that doctors not recommend injections to patients at the outset and instead recommend medication such as nasal spray, to avoiding deterring patients from taking up treatment.
55 On one occasion on a date I cannot recall, Dilip Shrestha spoke to me personally about mentioning injections during consultations with patients. Dilip Shrestha said that I did not have to talk to every patient about injections and that I should try to talk more positively about the treatments.
56 On another occasion on a date I cannot recall, either Jack or Dilip told me and some other doctors that they did not like using the word "needles" as it invoked fear in some patients. He said words to the effect of "do not use the word needle, use words like small prick instead". I do not believe that I ever used the word "needle" in any case.
57 Separately, on one or two occasions either Jack or Dilip told me not to overemphasise side effects.
[ACCC 1.39]
711 Dr Vaisman and Mr Shrestha denied these suggestions [R 13.1, [50]-[52]; R 13.11, [151]].
712 It was clear from the genuine surprise expressed by Dr Berry and Dr Goyer in the course of giving oral evidence that they were not aware of the contractual requirement that patients try injections. Their evidence should be preferred over the evidence of Dr Vaisman on the subject.
713 The ignorance of the doctors resulted in a gap in the AMI model of the provision of critical information to the patient about the AMI refund term. The doctors informed patients about the medications, but did not discuss the contract and thus, the AMI refund term. The salespeople were required to explain the AMI refund term, but were prohibited from discussing medications and thus did not descend into the detail of the particular medications required to be taken under the term, including injections. This resulted in the practical situation where no one at AMI took responsibility for informing patients that they would be required to try all medications, including injections, before qualifying for a refund.
714 Bruce Kyle gave evidence for the ACCC about the way the AMI refund term was administered. He swore affidavits on 8 August 2012 and 14 December 2012, and was cross-examined.
715 Mr Kyle was employed by AMI in April 2007 as a customer service representative. In that role he spoke with patients who rang in with difficulties in their treatment programs. If a patient had not tried all medications, Mr Kyle referred him to a registered nurse to switch the medication. He said that under the AMI refund term, a patient was required to try each of the types of medication listed in the instruction booklet sent to them before they were entitled to a refund. The list always included injections. Mr Kyle said that the AMI refund term was strictly enforced. That view was based on instructions he received from the manager of the customer service department, from observing other customer services representatives, and from his own work in the department.
716 From 2008 until October 2010 Mr Kyle worked as a refunds case officer. In this role he received the details of refund claims from the customer service representatives. He then contacted the patients and attempted to convince them to stay on the AMI program. If they did not want to stay on the program, he determined whether the claim fell within the AMI refund term. Even if it did so, Mr Kyle still tried to persuade the patient to remain on the program. His number one priority was “always to try to and convince the patient to stay on the program if I could.” [ACCC 1.41, [13]] In this role he answered to the refunds manager. Mr Alex Nizhnikov was the last refunds manager before Mr Kyle himself was appointed to that role in 2010. Mr Kyle resigned from his position as refunds manager in May 2012. Mr Kyle said:
33. … Applying the AMI Policy was very black or white - patients had either complied with the terms or they had not.
[ACCC 1.41]
717 Mr Kyle described the strictness with which the AMI refund term was administered thus:
34. On numerous occasions, patients informed me that they had suffered adverse side effects from the medications prescribed by AMI or that the medication was not effective, and were unwilling to try additional types of medication. Some claimed that AMI was treating them like a "guinea pig". At least two patients sent me photographs, claiming that they showed adverse reactions which the patient had suffered from medications prescribed by AMI. On one I saw a photograph sent by a patient who told me that he had a bad reaction to the troches prescribed by AMI, and had a severely swollen tongue and couldn't eat. In each of these circumstances, regardless of the claims, the patient was not entitled to a refund unless they had either tried each type of medication offered by AMI or had been contraindicated from all remaining types of medication by an AMI doctor. There was no allowance for such patients to verify their claims and be granted a refund because of adverse reactions.
[ACCC 1.41]
718 Mr Kyle did, however, explain that there was a 48-hour cooling-off period applied to refund applications. Thus, if a patient wished to cancel a contract and phoned within 48 hours expressing a change of mind, they were entitled to cancel the contract. However, patients were not told about the existence of this policy and if they rang within that time they were instead encouraged to remain on the program by AMI customer service representatives [ACCC 3.41, [41], [43]].
719 Mr Kyle explained that he used a price list provided by the manager to calculate that part of the refund amount which related to the cost of medication. Nasal sprays were charged at $200 for 4 mls and $250 for 8 mls, and capsules and troches at $200 for 30, $250 for 60 and $300 for 90. Dr Vaisman denied that the price list was used and that the process by which Mr Kyle calculated refunds were approved by AMI [R 13.10, [14]]. But Mr Kyle’s evidence should be accepted as he administered the system and it is improbable that he would have done so without approval.
720 Mr Kyle also said that, after deducting amounts for the medications provided and 15 per cent of the contract price for administration costs, there would sometimes be no money left over to provide the patient for the refund. Where patients had not paid for the treatment program in full and the amount still owed was greater than the total potential refund, patients would be required to pay the difference in order to terminate their contract [ACCC 3.41, [49]].
721 When Mr Kyle was appointed refunds manager there were four refunds case officers who reported to him. He said that the practices he described were standard practices of AMI which he saw other customer service representatives, refunds case officers and refunds managers utilise.
722 Mr Kyle’s evidence that the AMI refund term was strictly enforced was supported by the evidence of the seven Annexure B patients who filed witness statements. In each case, these patients described their experience of the refund system.
723 Patients 13, 30, 40, 49 and 158 suffered unpleasant side effects from the nasal spray, but were refused refunds.
724 Patient 13 was a manager in a furniture business. In February 2009 he agreed to treatment for PE for twelve months at $2,500. He paid $800 initially and committed to a direct debit payment of $217 per month. He explained what happened when he first took the nasal spray:
The nasal spray stung my nose greatly, it was a burning feeling and it blocked my nose within a minute and a foul taste went back down the back of my throat. I felt nauseous and dry retched. The nasal spray affected me for the entire day, my nose was blocked it was like a bad head cold.
[ACCC 1.4, [27]]
725 He rang AMI and told the nurse what had happened. He was told to try a penile spray and if that did not work to try an injection. He said that he wanted a refund and was told “You are in a legally binding contract” [ACCC 1.4, [29]]. He then cancelled his credit card so no further payments could be made. Patient 13 did not receive a refund. He was not cross-examined.
726 Patient 30, who was a farmhand, paid $2,500 in March 2008 for a 12-month treatment program for treatment for PE [ACCC 1.3]. He used the clomipramine spray prescribed by Dr Lonergan within the first week of receiving it. The next morning he awoke with a dull headache and later felt dizzy, hot, and nauseous. He felt disoriented and unbalanced so he went home from work and stayed in bed all day. The next day he could not go to work. He took four to five days before he returned to normal. He said in his statement, “I have never felt like that before and I never want to feel like that again” [ACCC 1.3, [33]]. He rang AMI on two occasions. When he rang the second time Dr Lonergan said that he should try two other nasal medications, but Dr Lonergan told him that he could not guarantee that the medications would not make him sick. The patient did not try any other medication. He made a number of calls to AMI seeking a refund and was told, “you tried the first medication and refused any further medication. You will not get your money back” [ACCC 1.3, [45]]. Patient 30 was cross-examined but not challenged on the matters just referred to. He did not receive a refund.
727 Patient 158, who was a company compliance officer, agreed in December 2010 to pay $4,500 for a two-year program for treatment for PE. He paid $400 immediately and authorised a direct debit of $97.62 per fortnight. He took the first tablet shortly afterwards and began to feel progressively unwell. He experienced severe headaches, dry mouth, a numbing sensation in the mouth and gums, continuous vomiting and difficulty sleeping. He did not connect the symptoms with the medication. About two weeks later he took another tablet and experienced the same side effects but worse. He was sick for about three days the second time [ACCC 1.6, [33]]. In early January 2011, he wrote to AMI requesting that no further payments be debited and requesting a refund. In the letter he explained:
I was instructed to take the medication before bed as it may cause a “slight headache”. After a nauseous ridden, sleep deprived night I spent the following day in nauseous sweats, headaches and vomiting. The loss of mental clarity and the ability to perform my duties was a direct result of your “prescribed” medication.
[ACCC 1.6, p 10]
728 AMI did not respond to his letter, which he sent twice, so the patient cancelled his credit card. That provoked AMI to send a letter requesting payment. The patient responded with several further emails explaining the position. Mr Kyle then contacted the patient and said that he had failed to report the side effects to AMI immediately as required by the contract. In April 2011, the debt collection department wrote to the patient but he did not respond. He had no further contact with AMI and did not receive a refund. He was not cross-examined.
729 In June 2008 patient 40, who was a plumber, agreed to pay $4,595 for treatment. He paid $600 immediately and authorised a direct debit of $99.88 per fortnight. He took the prescribed tablets on four occasions. On the first occasion the medication did not work. On the three other occasions he took the medication they caused his heart to race. He phoned AMI after the third occasion and was told to continue taking the tablets. After the next occasion he rang AMI and asked to cancel the contract. He was told, “Well you’ve got a contact, we’ll keep deducting the money” [ACCC 1.7, [44]]. AMI deducted ten payments between August and December 2008. In January 2009 the patient cancelled the direct debit authority. AMI made a number of calls and sent a letter of demand threatening that failure to pay could affect his future credit rating. The demands ceased after the patient made a complaint to Consumer Affairs Victoria. But he received no refund. Patient 40 was cross-examined, but not challenged on the matters referred to in this paragraph.
730 Patient 49 also experienced side effects [ACCC 1.11]. In July 2009 he agreed to pay $594 as the first payment of a total contact sum of $3,564. He also agreed to pay monthly instalments of $198 by direct debit. He tried the nasal spray within a few days of receiving it. He felt his blood pressure build up and a migraine begin. He also developed heartburn and sniffles. He tried to cancel the contract because the medication did not agree with him. He cancelled his credit card in May 2010 to stop the direct debits. Prior to that date he had allowed the payments to be deducted out of fear that he would otherwise damage his credit rating. Patient 49 was not cross-examined.
731 Patient 90 tried to cancel his contract with AMI because the medication did not work [ACCC 1.9]. He was a truck driver. He paid $500 in August 2008 as a first payment for a treatment costing $4,595 for treatment of PE. He found that the nasal spray did not work. He rang AMI and was told that he had signed a contract and would be in breach of his contract if he did not try other medications. As a result of this conversation, patient 90 cancelled his bank account so that further payments could not be taken out. He was then approached by AMI which insisted that he had signed a contract. He responded that the medication did not work and he had been told by the salesperson that he could cancel. In a number of phone calls from AMI he was told that if he did not pay his credit rating would suffer. AMI continued to press for payment until mid-2009. He did not receive a refund and AMI then no longer pursued payment. In cross-examination he acknowledged that his statement recorded that he was told that he could cancel at any time but that he was also told that to do so he just needed to have a consultation with some of the AMI staff and be deemed unsuitable for any ongoing treatment program. Patient 90 described the situation in his own words in cross-examination:
PATIENT: And I said, well, I’m not really happy with it and they said “too bad, you signed the contract.” So they were just – it was like there was an intimidation that you’ve signed a legal document and therefore you’re bound to it. And that’s what really turned me off it. It was the – if we look at paragraph – the one where the guy was saying – when I said to him, “I really don’t want to continue using any of AMIs products,” the man said – he just kept repeating and he almost started screaming to me, “That’s too bad. You’ve signed the contract and it’s too bad, you’ve signed the contract.” And that’s when I realised that I was involved in something that wasn’t, you know – it wasn’t a wholesome sort of a – or a professional institution.
HIS HONOUR: When the terms of the contract were first explained to you and they said, well you can cancel but you’ve got to try other medications, you went out of that first consultation knowing that there were other possible ways of achieving what you wanted, did you?
PATIENT: That didn’t even enter into my mind.
[TS 105]
732 Patient 32 agreed in mid-December 2009 to an 18-month treatment program for a cost of $3,200 [ACCC 1.5]. He paid $500 up front and agreed to a monthly direct debit of $172.22. The salesperson gave him the impression he could cancel at any time. At the end of December the patient decided that the cost of the program was not reasonable. He rang AMI and was told he could not cancel unless he tried all the AMI treatments and they did not work for him. He rang again to cancel the contract and said that he could not afford the costs. AMI persuaded him not to cancel because he had already paid for a lot of the treatment [17]. Instead, AMI agreed to reduce the amount of the direct debit. On the third occasion when the patient tried to cancel he was told that it was his bad luck. Patient 32 never took the medication. Payments were deducted until late September 2010 although no further medication was delivered to him. The patient closed his bank account and continued to receive demands for payment from AMI. In February 2010 the patient agreed to settle with AMI. He paid $2,000 for the treatment in all and only ever received one delivery of medication. In cross-examination the patient described his experience thus:
I spoke to the accounts department on many different occasions trying to cancel, and they refused every time. The person, Brett, who I actually spoke to was very rude, at times saying, “Bad luck”, and, “That’s it.” That this is the end of the conversation and that was it. So I’ve rung back other times trying to cancel on three different occasions, and the only way I could get through was to cancel my credit card and get AMI to call me. That was the only way I could deal with them.
[TS 118]
733 Apart from Dr Vaisman and Mr Shrestha denying some details of the evidence on this issue [R 13.10; R 13.17], the respondents offered no defence to the central allegation, being the terms and the strict application of the AMI refund term. Mr Shrestha annexed spreadsheets to his second statement made on 19 November 2012 with some analysis of patient refunds, but no mention of this material was made in submissions and the nature and purpose of it was not clear.
734 Counsel for the respondents initially indicated that Mr Nizhnikov was on the list of witnesses to be called, but he was ultimately not called. It can be presumed that his evidence of the implementation of the refund policy would not have assisted AMI.
735 It follows from the foregoing analysis of the evidence that patients who consulted by phone did not receive notice of the AMI refund term until after they had agreed to the treatment. The salespeople either did not explain the term at all, or did not do so in a way which alerted the patient to the requirement that they try all options before qualifying for a refund. One treatment option was self-administered injections in the base of the penis. No Annexure B patient was told that he would need to try such injections to obtain a refund. Where injections were mentioned by doctors in other contexts, the reference was often made in a way that indicated that the patient would not be required to use injections.
736 Further, patients were not told during the phone call that there would be deductions made from the refund of a 15 per cent administration fee, the cost of medication supplied, and the cost of the expired portion of the treatment.
737 The ACCC alleged that the cost of treatment charged by AMI and NRM was unconscionable because treatment and medication for ED and PE by conventional methods which were proven to be effective could be obtained for substantially less cost.
738 AMI and NRM patients were committed to long-term contracts which cost around $200 per month. That cost covered both medication and any necessary access to medical services provided by AMI and NRM.
739 Mr Mark Deacon, a retail pharmacist, gave expert evidence for the ACCC in a report dated 12 October 2011 on the pricing of pharmaceuticals normally used in the treatment of ED and PE. As submitted by the ACCC, the monthly cost for Aropax (paroxetine) or Zoloft (sertraline), the first-line medications used for PE, was about $30. In addition, the patient would need to pay for at least one consultation with his GP. In relation to the treatment for ED, the cost of four tablets of Viagra (sildenafil) varied between about $60 and $86, and the cost of four tablets of Cialis (tadalafil) varied between $72 and $94. Again, the patient would incur the cost of at least one consultation with his GP. Those medications were taken on-demand, so the cost of treatment depended on the sexual activity of the patient.
740 Using these comparisons, the evidence at least established that the cost of medication and treatment for PE by AMI and NRM was much greater than the cost of medication and treatment for PE by conventional methods. The position is less clear with ED because the use of conventional medication on-demand depended on the sexual activity of the patient.
741 The most significant point is that AMI and NRM were charging patients for medications delivered in a way for which there was no scientific or clinical evidence of efficacy. The comparison between the AMI medication and conventional medication is therefore a false comparison. In any event, whilst the ACCC made submissions that AMI and NRM were not justified in charging patients so much for treatment, no specific relief was sought consequent upon this submission.
5. FACT FINDINGS IN RESPECT OF NRM
742 The NRM period commenced when NRM purchased the business from AMI by the agreement with the administrators on 17 June 2011. The last consultation of an Annexure C patient with an NRM doctor about which evidence was given occurred on 16 February 2012. But the claims made against NRM which fall within the ACCC’s business-system case include the whole of 2012.
5.2 Acquisition of the business by NRM
743 On 22 December 2010, AMI was placed into voluntary administration. There is no doubt that by this time it was in a dire financial situation. The administrators stated in their 10 May 2011 Report to Creditors (the Report to Creditors) that there was a deficiency of $65.6 million [R 13.12, p 66]. Assets amounted to $243,462.93 and, whilst some of the liabilities were interrelated company dealings, there was $7.7 million owing to trade creditors and $9.3 million owing to secured creditors [R 13.12, p 88].
744 Dr Vaisman said that a failed expansion into the United Kingdom was a major cause of AMI’s financial problems [TS 1854, 1856]. From 2008, when the UK expansion started, until early 2010, when AMI decided to cease that operation, AMI had spent over $6 million developing and supporting the expansion.
745 AMI was not able to pay its media placement agent, PHD Networks Pty Ltd, for advertising placed between October 2009 and January 2010. Consequently, in May 2010 the agency served a statutory demand on AMI [R 16].
746 Then, in September 2010, the Westpac Bank (Westpac) demanded repayment of a secured loan [R13.12, p 80]. AMI did not have the funds to repay the loan, and Mr Shrestha’s evidence was that Dr Vaisman obtained funding from various people in order to repay about $2.2 million to Westpac [TS 2243]. The evidence does not disclose when the repayment to Westpac was made. However, on 6 December 2010, Westpac assigned to Life Science Group Pty Ltd (Life Science) fixed and floating charges which had secured the loan. At this time Dr Vaisman was the sole director of Life Science.
747 Further, on 2 December 2010, Brereton J handed down judgment in the case of AMI Australia Holdings Pty Ltd & Anor v Fairfax Media Publications Pty Ltd & Ors [2010] NSWSC 1395. The administrators later reported that the judgment included a costs order against AMI amounting to approximately $500,000, and that this liability impacted on the company’s ability to continue to trade.
748 The ACCC commenced this proceeding on 21 December 2010. Life Science sought the appointment of administrators on 22 December 2010 [R 13.12, p 70].
749 The ACCC implied that the administrators were appointed in response to the filing of this proceeding against AMI. Dr Vaisman told the Court that the timing of the appointment of administrators and the filing of this proceeding was coincidental [TS 1856]. He said that the administrators were appointed in response to the statutory demand served by PHD Networks Pty Ltd. That evidence was in error because the statutory demand was served on AMI in May 2010, not December 2010 as stated by Dr Vaisman. However, there were still compelling financial reasons for the appointment of administrators. Furthermore, according to the Report to Creditors, AMI was served with the proceeding on 23 December 2010, that is to say, after the administrators were appointed.
750 Then, the ACCC said that the assignment of the Westpac charges gave Dr Vaisman the ability to appoint administrators to AMI. It suggested that the taking of the assignments, which made Life Science the only secured creditor, and the appointment of administrators were actions by Dr Vaisman designed to allow for the transfer of the AMI business to a company controlled by him, and for the business to continue as before, free of the obligations of AMI to its creditors. Perhaps this argument was meant to assist the ACCC’s underlying contention that, in practice, the conduct of NRM was just a continuation of the conduct of AMI. However, that argument was better supported by evidence of the conduct itself than by evidence of the motivation for taking the assignments and for seeking the appointment of administrators.
751 The evidence that these steps were motivated to leave the business in Dr Vaisman’s hands is not compelling. As set out above, there were financial reasons for the appointment of the administrators. Further, Dr Vaisman, as sole director of both companies constituting AMI, did not need the assignments to obtain the power to appoint administrators. In the financial circumstances of AMI, the companies were able to appoint administrators under s 436A of the Corporations Act 2001 (Cth), which provides that a company many appoint an administrator if the board thinks it is or will become insolvent.
752 Dr Vaisman effectively controlled the majority of creditors, because the largest creditor of Advanced Medical Institute Pty Ltd, the first respondent, was AMI Holdings Pty Ltd, the second respondent, which was owed about $29 million. The largest creditor of AMI Holdings Pty Ltd, was Advanced Medical Institute Inc, the parent company of Life Science Group Pty Ltd. Advanced Medical Institute Inc was owed about $14.5 million. The Quarterly Report for the quarter ending 31 December 2008 for Advanced Medical Institute Inc filed with the US Securities and Exchange Commission was in evidence [ACCC 4.466]. Although signed by Dr Vaisman as Chief Executive Officer, it does not show the shareholding in this company. The ACCC’s submissions proceeded on the basis that Dr Vaisman controlled this company. The respondents did not contest that proposition. It should therefore be accepted as a joint position. Although control of the majority of the creditors gave Dr Vaisman a significant say in the course of the administration, control of the majority of creditors did not protect AMI from the danger of a winding-up application by other creditors on the grounds of insolvency, and it did not protect Dr Vaisman and other officers of the companies from prosecutions, including for insolvent trading.
753 In the end, the motivation for the appointment of administrators seems to be of little moment for the purposes of the proceeding.
754 The administrators advertised the business in the Australian Financial Review and the Australian newspapers. They received 22 expressions of interest but only two genuine offers. The offer from NRM was higher and was the only viable offer. It provided for a purchase price of $4.7 million. The administrators favoured the sale particularly because, as they reported, “[t]his offer allowed for not only the continued employment of the employees of the companies, but also involved the assumption by the new owners of approximately $1.8 million in entitlements owing to these employees” [ACCC 4.431, p 7].
755 On 10 June 2011, the administrators applied for and obtained directions from the Supreme Court of New South Wales that they would be justified in selling the business to a related party, without seeking creditor approval.
756 By an agreement dated 17 June 2011, NRM Corporation Pty Ltd, the sixth respondent, and NRM Trading Pty Ltd, the seventh respondent, purchased the business of AMI for $4.3 million [ACCC 4.NRM71, p 9]. The unsecured creditors did not receive any return.
757 Dr Vaisman was the sole shareholder in NRM Family Pty Ltd, which was the ultimate holding company of both the sixth and seventh respondents [ACCC 4.459, 4.460, 4.462]. Hence Dr Vaisman had control of the business operated by NRM and previously operated by AMI. NRM Trading Pty Ltd purchased all existing customer contracts held by AMI. NRM Corporation Pty Ltd bought the stock, plant, equipment, interest in leases, third party contracts, and the business telephone numbers of AMI [ACCC 4.NRM71, pp 4, 11].
758 The administrators stated their opinion in a further Report to Creditors dated 8 July 2011 that AMI should be wound up because the companies were clearly insolvent [ACCC 4.431, p 11]. On 19 July 2011, AMI was placed into voluntary liquidation.
5.3 Continuation of the AMI business system
759 The way in which patients interacted with NRM was a continuation of the business system operated by AMI. Patients who consulted with NRM by phone dealt first with a salesperson. That person was designated by NRM as an “administrative assistant” rather than a “clinical coordinator”, the way in which AMI had described the role. Then, the patient was put through to a doctor and, when the consultation with the doctor was completed, the patient was returned to the administrative assistant who would organise payment.
760 Where the patient attended a clinic, he was first seen by a nurse who took down some of the patient’s details or had the patient complete a form with personal details and medical history. Then the patient consulted with a doctor over the phone, and finally, met with a salesperson who advised about cost and organised payment.
761 In 2012, 31,158 patients consulted by phone, and 4,291 patients attended a clinic [R 13.34].
762 The core personnel of NRM were the same as the core personnel of AMI. Dr Vaisman was the Chief Executive Officer, Mr Shrestha was the Chief Financial Officer, and Mr Khan was the Chief Operating Officer. According to Mr Kyle, who was employed by NRM until April 2012, from a practical perspective, nothing of significance changed after the purchase of the business by NRM and the business appeared to operate as it had previously, controlled by Dr Vaisman and Mr Shrestha [ACCC 1.41,[ 69]].
763 All of the doctors who consulted with the Annexure C patients, Dr Goyer, Dr Durrani, Dr Omar, Dr Condoleon, and Dr Berry, were also engaged during the AMI period.
764 Seventeen salespeople from the AMI period continued to be employed in the NRM period. In addition, about five new salespeople were employed.
5.5 The conduct alleged against NRM
5.5.1 Advertising medical treatment
765 NRM continued AMI’s practice of advertising and Dr Vaisman accepted that the advertising placed by NRM was extensive. The website used by NRM was the same website as AMI had operated. NRM marketed itself by the name Advanced Medical Institute as had AMI, and NRM used the same phone numbers as had been used by AMI. As with AMI, NRM created the impression by its advertising that it was providing medical treatment in accordance with accepted professional medical standards through consultation with doctors who would diagnose and treat ED and PE. The focus in the advertising on the provision of medical treatment remained unchanged. Many of the NRM patients heard advertisements for NRM on the radio. A few said that they had learned of AMI through billboards or television advertisements, and several accessed NRM through its website.
5.5.2 The conduct of NRM salespeople
766 Ms Gabriel was the only administrative assistant who gave evidence. She was called by the respondents. She worked for AMI and then NRM. She was always paid commission, but she did not have a practice of telling patients this [TS 2493].
767 Dr Vaisman said that the NRM salespeople were all on wages and, “very very little commission. Like one per cent, two per cent… [a]nd good wages, up to $100,000” [TS 1863] .
768 Mr Shrestha said that NRM was transitioning to the payment of wages to salespeople. He said, “many are already getting wages – no commissions, so that a few of them still are either wages or commission” [TS 1984].
769 When asked by the Court why NRM was moving away from payment by commission, Mr Shrestha said, “we just want to improve what things are not liked by the regulatory departments” [TS 1984 line 25].
770 Ms Gabriel said that she was paid solely on commission by NRM. She was paid 10 per cent on upfront sales and 6 per cent on direct debit sales. From June 2011 to January 2012 Ms Gabriel earned on average about $15,000 per fortnight in commission [ACCC 15]. Although Ms Gabriel had been asked by Dr Vaisman whether she was interested in converting to payment by wages, this had not occurred and she was still considering it at the time she gave evidence in December 2013. The remuneration records tendered by the ACCC indicated that, at least until the end of 2011, all but one of the NRM administrative assistants were paid on a commission basis.
771 The ACCC alleged, and it was established, that in their interactions with the Annexure C patients, NRM salespeople continued their practice during the AMI period of telling the patients that the medications prescribed by NRM doctors were effective, and, by that technique put pressure on patients to enter into treatment programs.
772 One example was patient NRM 8. At the time of the consultation, he was a 22-year-old apprentice. He attended a clinic for treatment of PE. After he consulted with Dr Goyer by phone, Ms Gabriel discussed the question of cost with him. The patient related the conversation in his witness statement thus:
17 The woman and I then had a conversation in words to the following effect:
She said: "The program is going to cost you around $3,000 for 1 year. It's about $50 per week. We'll get you to pay a deposit of $500 today."
18 I said: "That's too expensive. I am only an apprentice."
She said: "Do you think your problem is just going to go away? How long did you smoke pot for?"
I said: "Six months or so."
She said: "Well, with your pot smoking, you are going to have to be with us for a while. You need the medication to adjust the serotonin levels in your brain. You really need us. This treatment really works. And, what about your girlfriend? These problems don't just go away. What else are you going to do? You don't have any other option."
I said: “Yeah, but I can’t afford it.”
She said: "It's only $50 a week."
I said: "I can't afford it."
She said: "Well how about we do this? You can pay a $300 deposit today and we won't start taking money out of your account for a month. If you can just give me your bank card?"
[Emphasis added.]
[ACCC 1.19]
773 The patient stated:
21 The woman spoke to me in a loud and intimidating way. I felt under pressure to agree to sign up for the program. I felt tired because I had waited for a long time and I had a lot going through my mind at the time.
[ACCC 1.19]
774 The patient was cross-examined and challenged on this conversation, but confirmed that the administrative assistant spoke to him in a confronting and stern manner [TS 70 – 71]. Ms Gabriel was called by the respondents but gave no evidence on the conversation. The evidence of the patient should be accepted. It demonstrated how the salesperson promoted the efficacy of the treatment in order to pressure the patient into entering a treatment program.
775 Another example was patient NRM 10. He was a 31-year-old driver and student at the time of the consultation. He consulted NRM over the phone for treatment of PE. His statement recorded:
17. The man then began to tell me about the cost of the program. The man told me that the program would cost between $3,000 and $4,000 for a 12 month period. I was surprised by how expensive the program was. The man and I exchanged words to the following effect:
I said: "There is no way that I could afford that much, I have a young child and I am studying, I can't afford to spend this much money."
He said: "Don't you want to keep your wife happy?"
I said: "Yeah"
18. The man then became pretty pushy. I felt a fair amount of pressure from him to sign up to AMI. He kept insisting that I pay the full amount for the program upfront, after I already told him that I couldn't afford it. He said words to the effect of, "It's only $3,000, it's about your happiness". This went on for a couple of minutes and he started to wear me out.
[ACCC 1.20]
776 In cross-examination the patient was asked about the pressure applied to him and the following exchange occurred:
MR GREEN: There was no suggestion to you, [Patient], that you had to take the medication, was there?
PATIENT: Well, no, they said that it would help improve my sex life, but they didn’t tell me I had to take it, no.
MR GREEN: No. And there was no pressure applied to you that you needed to enter into an agreement with [NRM] at all about the medication that you had spoken to the doctor about?
PATIENT: Well, once I got off the phone from the – I got transferred back to the sales person, they put a lot of pressure on you to buy the product, yes.
MR GREEN: Well, when you say “a lot of pressure,” can you remember what words were used?
PATIENT: Well, when I said I couldn’t afford it, because they wanted to take the whole amount – the 12 month period out straightaway, I said I couldn’t afford that. They put a lot of pressure on me to, then they tried to put it down to monthly repayments and stuff like that, but I felt like I couldn’t say no.
MR GREEN: Well, [Patient], you invited the sales consultant to come to a different arrangement, to try to accommodate your financial circumstance. You would agree with that, would you not?
PATIENT: Yes.
MR GREEN: And so that the way in which the sales consultant endeavoured to – the clinical coordinator endeavoured – or sales consultant, I should say, endeavoured to assist you, was to find a way which made it affordable – the treatment affordable for you. Do you agree with that?
PATIENT: To a certain aspect, yes.
MR GREEN: I’m correct in reading your affidavit his Honour should draw the conclusion that you didn’t formally ask AMI for a refund, did you?
PATIENT: No.
MR GREEN: And I just want to clear up a few other things about your statement. When you gave evidence before – I will come back to your statement later – when you gave evidence before you felt pushed to enter into an arrangement, there was nothing specifically said to you that compelled you to enter into the arrangement, was there?
PATIENT: No. But I felt at no point that I could simply say no. Every time I said I couldn’t afford it, they kept pushing me in another way.
MR GREEN: You agree with me you could hang the telephone, don’t you?
PATIENT: But I’m not that type of person.
[TS 272]
777 The patient returned to the pushiness of the salesperson several more times. His evidence on the issue was compelling. The respondents did not call the salesperson to give evidence. The evidence of patient NRM 10 on this issue should be accepted.
778 Another example was patient NRM 5 who was told by Ms Gabriel when the cost of treatment was discussed that he would “get the results you are after” [ACCC 1.17, [30]]. The patient was not required for cross-examination and neither Ms Gabriel nor the respondents challenged this account.
779 Similar accounts were given by patients NRM 14 and 16, neither of whom were required for cross-examination. The respondents did not call the salesperson in either case. The evidence of the patients should be accepted on this issue.
780 And, finally, patient NRM 13 was a 33-year-old accountant who attended a clinic seeking treatment for PE. He described in his witness statement the conversation with the salesperson when the discussion turned to the cost of treatment thus:
24 The woman and I had a conversation to the following effect:
She said: "How did you go with Nurse Margaret?"
I said: "Fine thanks."
She said: "Good. Nurse Margaret is very experienced. Are you in a relationship?"
I said: "Yes, I have a girlfriend."
She said: "Is your girlfriend happy?"
I said: "Yes, I think so."
She said: "I'm sure she could be happier. What do you do for a living?"
I said: "I'm an accountant."
She said: "So do you want to go ahead with the treatment program?"
I said: "Well how much does it cost?"
She said: "Well, we send you a supply every 3 months for 12 months. It's $1,100 for a three month supply."
25 I thought that the price was very expensive as it would amount to over $4,000 for the year. I said to the woman words to the effect of "That's very expensive. I will need to think about it and talk it over with my girlfriend."
26 The woman was polite and sympathetic at the beginning of the conversation but after I told her that I was going to think about it, the tone of her voice and her body language became more rude and dismissive.
[ACCC 1.23]
781 The patient was cross-examined but not challenged on this aspect. The respondents did not call the salesperson to give evidence. The patient’s evidence on this issue should be accepted.
5.5.3 Offering limited to NRM medications
782 The ACCC made the same allegations concerning the limitation on the medications offered by NRM as it made against AMI. Those allegations have been discussed extensively at [218] – [352] of these reasons for judgment. The discussion applies equally to the allegations against NRM. The only relevant change made by NRM to the medications used by AMI was that it added oral strips to the delivery methods available. This alternative delivery system was also considered at [285], [295] – [296], and [327] of these reasons for judgment.
5.5.4 The conduct of the doctors
783 Dr Lonergan, who consulted for NRM until 14 December 2011, said that from his perspective as a doctor, the same people controlled the business after the purchase by NRM and the policies the doctors were required to follow did not change in any substantive way [ACCC 1.37 [24]].
784 As with the doctors’ consultations in the AMI period, the ACCC alleged that the doctors’ consultations with the Annexure C patients in the NRM period involved unconscionable conduct. The ACCC alleged that, in the consultations with the Annexure C patients, NRM continued the practice of doctors consulting without physically examining the patients, of recommending treatment for 12 to 18 months, of only offering medications compounded for NRM and not disclosing this fact to patients, of not explaining to patients the terms on which the treatments were provided, of not seeking to diagnose the underlying causes of the ED or PE, and of not referring patients to GPs or specialists for treatment of underlying causes and presenting conditions. The ACCC also alleged that in consultations with 14 of the Annexure C patients the doctors in the NRM period, as in the AMI period, failed to advise patients adequately, or at all, of the side effects of the medications.
785 There was no doubt about what occurred in the consultations in the AMI period because the recordings provided a direct contemporary record. The position was different in respect of the Annexure C patients, because the evidence of what occurred in the consultations in the NRM period was contestable.
786 The ACCC relied on the statements or affidavits (together which are referred to as the statements) made by each of the 16 Annexure C patients concerning their experience with NRM. That included their contact with salespeople as well as with the doctors. Ten of the consultations were conducted entirely by phone, and in six consultations the patient attended a clinic where the consultation with the doctor was by phone. Some of the witness statements were particularly focused on the patients’ attempts to obtain refunds of the cost of the programs.
787 The account of the consultations with the NRM doctors contained in the statements of the Annexure C patients was short, usually occupying a few paragraphs over about half a page. In many cases it was clear from other sources that the account was incomplete.
788 These accounts of the doctors’ consultations were adequate as part of a narrative of the general experience of the patient in his contact with NRM. However, the accounts were usually too truncated to be useful in establishing the detail of what occurred in the consultation with the doctors. On the other hand, there are some accounts in which the patient provided a particular recollection of an important issue, such as a discussion about side effects.
789 In addition to the evidence in the statements made by Annexure C patients, seven of the 16 patients were cross-examined. Only in a few cases did the cross-examination, or limited further examination-in-chief, deal with the subject of the doctors’ consultations. As will be seen that oral evidence was of assistance in providing a foundation for an assessment of the adequacy of the NRM doctors’ consultations.
790 The ACCC relied on the expert opinion of Dr Pattison expressed in Pattison Report 3 concerning the consultations with patients NRM 2, 5, 12 and 13. The ACCC also relied on the expert opinion of Dr McRae expressed in McRae Report 3 concerning the consultations with patients NRM 2, 5, and 13. Dr McRae was not specifically cross-examined on the particular consultations with Annexure C patients. Dr Pattison gave some evidence in cross-examination in relation to patients NRM 12 and 13, which is referred to below.
791 The respondents relied on the evidence of some of the doctors engaged by NRM and on the records kept by NRM.
792 Dr Goyer consulted with six Annexure C patients, namely, patients NRM 1, NRM 2, NRM 7, NRM 8, NRM 15 and NRM 16. Dr Berry consulted with two Annexure C patients, namely, patient NRM 11 and patient NRM 14. Dr Condoleon consulted with one Annexure C patient, namely, patient NRM 6. Each of these doctors gave general evidence of their consulting practices in witness statements filed before trial. In Berry Statement 1, Dr Berry dealt specifically with the witness statement made by patient NRM 14. Each of these doctors was cross-examined.
793 Three doctors who consulted with Annexure C patients did not give evidence, namely, Dr Durrani who consulted with four NRM patients, namely, patient NRM 3, NRM 9, NRM 10 and NRM 12, Dr Omar who consulted with two NRM patients, namely, patient NRM 4, and NRM 5, and Dr Biswas who consulted with one NRM patient, namely, patient NRM 13.
794 The respondents relied on the records kept by NRM which included reference to the doctors’ consultations. The Patient History and Patient Assessment Forms for the Annexure C patients were contained in exhibit DKS-1 to the statement of Mr Shrestha. As well as recording personal details and medical history obtained at the consultation, the Patient Assessment Form contained a place for doctors’ comments. It also had a tick box checklist of a large number of medical conditions which was meant to be completed with confirmation from the patient. The Patient History Form included a brief reference to the outcome of the consultation, but also recorded all the interactions with or concerning the patient including, for instance, delivery dates of medications, and details of reassessments when medications had to be readjusted or replaced.
795 There was a contest between the parties over whether these records were reliable. The ACCC produced attachment 5 to the final written submissions, listing examples from the AMI period where the records of the doctors’ comments failed to accurately record events which were recorded in the Annexure B patients’ recordings. It said that similar deficiencies in the NRM patient records made them unreliable. The respondents replied with a schedule explaining each of the alleged inaccuracies.
796 The Patient Assessment Forms and the Patient History Forms were potentially significant in respect of the Annexure C patients on two issues, namely, the completeness of the patients’ recollection of the history taking in the consultation, and whether the doctor referred to side effects. In the end, the records turned out to be useful in respect of the first matter, but not in respect of the second.
797 As to the first matter, namely, the completeness of the account of the history taking in the consultation, the example of patient NRM 3 is illustrative. The account of the consultation with the doctor in his witness statement comprised five lines [ACCC 1.15, [9]]. The patient said he spoke to the doctor for no more than five minutes. Cross-examination disclosed that he had told the doctor that he was a weight lifter and that he suffered asthma. These matters were recorded in the Patient Assessment Form [R13.12, p 336]. That form also showed that he had told the doctor that he did not smoke and that he drank alcohol on weekends. None of these matters were referred to in the witness statement. The Patient Assessment Form recorded responses to over 20 questions concerning medical conditions, whereas the witness statement recorded the doctor asking only about blood pressure and heart conditions.
798 At the same time it must be accepted that the Patient Assessment Forms were not infallible. For instance, the Patient Assessment Form for patient NRM 2 was incomplete in that all the history sections were blank [R 13.12, p 286]. The only part filled in was in the doctor’s comments section at the end of the form, and the section relating to medication contraindication.
799 As to the record in the Patient Assessment and Patient History Forms concerning reference by doctors to side effects, the primary problem is that the record of what was allegedly said was too indefinite to be meaningful. Often there was a record in the doctor’s comments to “SE”. This apparently was intended to mean that side effects were discussed. But such an entry gave no detail of the content of the discussion. The issue in the proceeding was not simply whether side effects were mentioned, but also whether the discussion was sufficiently comprehensive. In some Annexure B cases where specific side effects were recorded in the forms as having been mentioned, the recordings demonstrated that they had not been mentioned. For example, the Patient History Form for AMI patient 36 indicated that Dr De Sayrah had warned him of the side effect of dry eyes, but in fact she did not. It seems likely that doctors had standard phrases to be entered into the doctor’s comment section of the Patient Assessment Form, and that sometimes these phrases were inserted as a matter of routine whether they reflected what occurred in the consultation or not. For instance, for a number of Annexure B patient consultations, the Patient Assessment Form recorded that the doctor told the patient to inform his GP of the medications prescribed by AMI. The recordings demonstrated that the doctor did not so inform the patient. The respondents conceded that the forms did not reflect the consultation in that regard on many occasions. There is no reason to suggest that the deficiencies in relation to the Annexure B patients did not apply to the Patient Assessment and Patient History forms in relation to the Annexure C patients.
800 The evidence of the doctors’ consultations in the NRM period can usefully be considered in four categories. It is not intended to describe all aspects of all of the doctors’ consultations with Annexure C patients, but rather to focus on particular aspects which are relevant to an assessment of the quality of the consultations by reference to the criticisms raised by the ACCC.
801 The first category is where the patient was not cross-examined on his witness statement and where the doctor gave no evidence.
802 Patient NRM 4 was a 22-year-old man who rang NRM for treatment for PE. He was treated by Dr Omar. The patient said that Dr Omar spoke extremely fast and mumbled in a very soft voice. The patient said he could not understand what the doctor said. Dr Omar asked the patient a series of questions about his medical history but did not wait for an answer before asking the next question. The patient did not remember Dr Omar telling him about side effects [ACCC 1.15, p 2]. Although the Patient Assessment Form contained an entry “S/eff..disc”, it is probable that side effects were not mentioned.
803 Patient NRM 5 was a 37-year-old electrician. He attended a clinic. The nurse took his blood pressure and the patient filled in a medical history form. Before the consultation with the doctor the nurse said to the patient that he would take oral strips for 12 to 18 months. As to the consultation with Dr Omar, the patient stated:
18 Doctor Omar introduced himself and asked me similar questions to those on the form I had filled out. This took approximately 2 minutes.
19 Doctor Omar did not ask me about my problem or discuss with me whether or not I was suffering from premature ejaculation.
20 After Doctor Omar had finished asking me questions he said words to the effect of: “You are a healthy person and can take the treatment. I recommend a 12 month program for you. You should take one strip every day for 12 months. When you get the medication, you will get information about techniques you can use. If you follow the instructions for the medication and the techniques, you will get the results that you are after. You should be able to see results after two weeks of using the medication.”
21 Our conversation then continued in words to the following effect:
I said: "Will there be any side effects to the medication?"
He said: "Because you are healthy there shouldn't be any major side effects."
I said: "How does the medication work?"
He said: "It works with serotonin in the brain."
22 My consultation with Doctor Omar lasted for less than 5 minutes.
[ACCC 1.17]
804 Both Dr Pattison and Dr McRae said that Dr Omar did not enquire as to the presenting illness and that the history taking in this case was inadequate and too rapid [ACCC 3.30, p 96; ACCC 3.33, pp 97–99]. Dr McRae expressed the view that the consultation suggested that there was a predetermined decision to treat with oral strips.
805 Dr Omar was not called to give evidence. The account of the patient that Dr Omar said that there would be no major side effects should be accepted.
806 The second category of consultations is where the patient was cross-examined and the doctor did not give evidence, namely, consultations with patients NRM 3, NRM 10, NRM 12 and NRM 13.
807 Patient NRM 3 consulted by phone and spoke to Dr Durrani for treatment of PE [ACCC 1.15]. He was a 46-year-old civil supervisor. He was cross-examined about the record of the consultation on his Patient Assessment Form. He denied that the doctor discussed side effects or that he should speak to his GP about the medication. In the absence of evidence from Dr Durrani, the evidence of the patient should be accepted.
808 Patient NRM 10 was a 32-year-old driver and student. He also consulted Dr Durrani by phone for treatment of PE. In his witness statement he said that the doctor only mentioned oral strips and no other medications [ACCC 1.20, p 2]. He said that the doctor did not say what the medication was. Nor did the doctor say anything about talking to the patient’s GP about the medication. These were all items recorded in the Patient History Form and the Patient Assessment Form as having occurred [R 13.12, pp 328-329]. The patient was not cross-examined on the inconsistency. In the absence of evidence from Dr Durrani the evidence of the patient should be accepted. Further, the Patient History Form seems to adopt a recurring formula used by Dr Durrani in the doctor’s comments. In this case the comment seemed to adopt two different formulae resulting in a repetition of some subjects, such as the arrangements for follow-up of the patient. The entry is unreliable and cannot be accepted as evidence, for instance, that side effects were discussed. In an exchange with the Court the patient said that the doctor “seemed a bit rushed” and that he did not feel that he had the opportunity to ask questions [TS 271].
809 Patient NRM 12 was a 51-year-old truck driver. He initiated a phone consultation for ED and possibly PE. Dr Durrani prescribed oral strips containing apomorphine. The patient said that the doctor did not discuss the type of medication or the strength of it. The doctor did not mention the length of treatment or possible side effects [ACCC 1.22, p 3]. The Patient History Form recorded a doctor’s comment “SE…explained” [R 13.12, p 308]. The patient was not challenged in cross-examination to the effect that his evidence on this subject was wrong. In the absence of evidence from Dr Durrani, the evidence of the patient should be accepted.
810 Dr Pattison criticised the consultation on the grounds that a full history was not taken [ACCC 3.30, p 83]. However, the Patient Assessment Form indicated that more questions were asked than the patient recorded in his witness statement. Dr Pattison did not have access to the Patient Assessment Form. As the form involved simply ticking boxes in a list, it may well be a better guide to the extent of the history taking than the witness statement. Dr Pattison, however, also criticised the consultation because side effects of the treatment were not discussed.
811 The patient was later prescribed injections when the oral strips proved ineffective. In cross-examination Dr Pattison reiterated the comments he had made in Pattison Report 3 that it was unsatisfactory to prescribe injections over the phone because:
[I]f you’re going to give somebody medication to inject into their penis, you would need a very thorough counselling and discussion about how that’s done.
[TS 1200]
812 Patient NRM 13 was a 33-year-old accountant. He went to a clinic and consulted with Dr Biswas by phone. He said in his witness statement that he filled in a form and that the nurse took some medical history. The doctor asked a few general questions including “Are you healthy”, “Have you any health problems?”, and, “Are you prone to depression or stress?” The doctor told him there were two treatments available, either by oral strip or by nasal spray. The patient asked whether there were any side effects and Dr Biswas said no. The doctor did not say what was in the strips. He did not say they contained an antidepressant [ACCC 1.23, pp 2–3]. The Patient Assessment Form stated that the patient had been told of specific side effects, that clomipramine was an anti-depressant, that he should discuss the medication with his GP before taking it, and that he was advised about monitoring with blood tests [R 13.12, p 270]. In examination-in-chief the patient denied being told these things. In cross-examination the patient confirmed that he was told by the doctor that there were no side effects [TS 933]. He said that the entire consultation, including with the nurse, took 10 to 15 minutes. In the absence of evidence from Dr Biswas the evidence of the patient should be accepted.
813 Dr Pattison and Dr McRae criticised this consultation for failing to take a detailed history, failing to identify the medication in the oral strips, and failing to advise correctly about side effects [ACCC 1.30, p 95; ACCC 1.33, pp 94–94]. In cross-examination Dr Pattison accepted that his views were formed from reading the patient’s witness statement. Again without evidence from Dr Biswas, Dr Pattison and Dr McRae’s opinions that the consultation fell below acceptable professional standards should be accepted.
814 The third category of consultations is where the patient was not cross-examined but the doctor was cross-examined about what occurred in consultations with patients. In this category are five NRM patients, namely, patients NRM 6, NRM 11, NRM 14, NRM 15, and NRM 16.
815 Patient NRM 6 was a 20-year-old apprentice. He attended a clinic for PE. He explained what happened at the consultation with Dr Condoleon in his witness statement thus:
15. … The doctor told me what the oral strip did and what I should expect from taking it. He didn't ask me too many questions and we were only on the phone for a couple of minutes.
16. The doctor asked me some questions about my health. I don't remember all the questions he asked me but I remember that I answered "no" to many of the questions because I am pretty healthy. I didn't always understand what the questions meant. The doctor spoke pretty fast.
17. I didn't ask the doctor any questions. From what the doctor told me, I thought that I would be getting the oral strips …
[ACCC 1.18]
816 Dr Condoleon did not refer to this consultation in his witness statement and was not cross-examined about it specifically. He gave evidence of his general practice which included discussing common side effects. The Patient Assessment Form for this consultation recorded that side effects were discussed [R13.12, p 331]. In the absence of reference by the patient to any default in this regard, Dr Condoleon’s evidence on the issue should be accepted. He did not contest, and it should be accepted, that Dr Condoleon spoke “pretty fast”.
817 Patient NRM 11 was a 52-year-old forklift driver. He consulted Dr Berry by phone for PE. He said in his witness statement:
15 The doctor did not mention any side effects to me. I know this because I was listening out for side effects because I am a fork lift driver and cannot take medication that would effect [sic] my concentration or make me drowsy when I do my job.
[ACCC 1.21]
818 The Patient History Form stated that side effects were discussed [R 13.12, p 317]. The patient was not required for cross-examination and Dr Berry did not specifically deal with this consultation in her statements or her oral evidence. In the circumstances where the patient’s evidence was that he was not told of the side effects of the oral strips, that evidence should be accepted.
819 Patient NRM 14 was another patient of Dr Berry. He was a 39-year-old OHS Manager. He sought treatment for PE. In relation to side effects, he said that Dr Berry told him that he might experience numbness in the mouth and funny after taste which soft drink would counteract [ACCC 1.24, p 3]. In Berry Statement 1, Dr Berry directly responded to the witness statement of this patient [R 13.18, p 13]. She said that she recalled that she discussed common side effects with him. However, Dr Berry agreed in cross-examination that she could not remember the particular patient or contradict his recollection of the particular circumstances of the consultation [TS 2457]. The Patient Assessment Form indicated that side effects were discussed [R 13.12, p 293]. That is consistent with the reference to numbness in the mouth, but leaves open the issue whether the explanation was sufficient.
820 Patient NRM 15 was a 43-year-old electronic technician. He attended a clinic and consulted Dr Goyer by phone for PE. He said in his witness statement that the consultation took about three minutes. He said that he had been on antidepressant medication. Dr Goyer told him not to take the oral strips if he went back on to the antidepressant medication, but did not investigate whether the PE and depression might have been linked [ACCC 1.25, p 3]. Dr Goyer did not respond to this statement directly in his witness statement. This evidence of the patient was not contradicted and should be accepted. The Patient History Form recorded that side effects were discussed, but no detail was given sufficient to conclude that the explanation was adequate.
821 Patient NRM 16 was 28-year-old public servant. He consulted Dr Goyer by phone for treatment for PE. The patient did not mention any discussion about side effects in his witness statement. The Patient Assessment Form was blank save for the doctor’s comment which included “side effects explained” [R13.12, p 347]. Dr Goyer did not refer to this patient directly in his witness statement. In the absence of any reference to side effects in the patient’s witness statement, the Patient Assessment Form should be accepted as evidence that side effects were explained. However, as mentioned earlier, there is little value in this evidence without further evidence of the content of the discussion.
822 The final category of consultation is where both the patient and the doctor were cross-examined. In this category are three consultations, namely, with patients NRM 1, NRM 2, and NRM 8 each of whom consulted with Dr Goyer for PE.
823 Patient NRM 1 was a 35-year-old carpenter. He attended a clinic. He filled in a form with questions about his medical history. When he was put through to Dr Goyer on the phone, the patient asked about side effects. In his witness statement the patient stated that Dr Goyer said that the dosage was really low and the patient should not see any major side effects [ACCC 1.12, p 3]. This is consistent with the Patient Assessment Form entry which stated, “Side effects explained” [R13.12, p 312]. The patient did not recall the doctor asking any questions about his health. The patient said that the conversation with the doctor lasted less than two minutes. He was not cross-examined on these issues. Dr Goyer’s witness statement did not refer to this consultation directly in his statement, and thus did not take issue with the patient’s evidence on this aspect. Nor was Dr Goyer cross-examined on the specific consultation. That evidence of the patient should be accepted.
824 Patient NRM 2 was a 21-year-old accountant. He consulted over the phone. In his witness statement he outlined the short history taken by Dr Goyer [ACCC 1.13, pp 2–3]. He told Dr Goyer that he generally ejaculated in no more than five minutes. The patient said that the conversation with Dr Goyer took around two minutes. There is no reference in the patient’s statement to Dr Goyer explaining side effects to him.
825 Dr Pattison and Dr McRae expressed the view that the consultation fell below acceptable professional standards. Dr Pattison said that it was necessary to determine exactly what the problem was. The patient may not have had PE at all. He may simply have needed reassurance about what was normal [ACCC 3.30, p 82]. Dr McRae said that is was not clear how Dr Goyer arrived at his decision to prescribe and that there was a sense of undue haste about the consultation [ACCC 3.33, p 101].
826 Consistent with the limited history taking alleged is the fact that the Patient Assessment Form was blank, save for nine lines of doctor’s comments recorded in standard phrases, the note that the patient was calling for problems with PE, and the notes regarding contraindications [R13.12, pp 286 – 287]. The doctor’s comments stated, “Side affects [sic] discussed”.
827 Nonetheless, in his witness statement Dr Goyer directly disagreed with the allegation that the consultation took about two minutes [R13.20, [64]]. He said that there was a timer on the telephone he used and that he had observed that initial patient consultations usually took about seven to eight minutes.
828 In cross-examination, patient NRM 2 disagreed insistently that the consultation took seven to ten minutes [TS 227–228]. In cross-examination Dr Goyer said that his disagreement with the suggestion that the consultation lasted about two minutes was based on his general impression about what he did with patients [TS 2365]. The evidence of the patient should be accepted. His recollection was particular to his experience and is more likely to be correct than Dr Goyer’s extrapolation from his general practice.
829 The patient also said in cross-examination that Dr Goyer did not discuss side effects with him, but a salesperson did [TS 236]. Again, this evidence should be preferred over the formula contained in the doctor’s comments in the Patient Assessment Form. Not only is the patient’s recollection more likely to be reliable, but the form in an otherwise blank state raised questions as to whether it was an accurate record of real events.
830 Patient NRM 8 was 22-year-old apprentice. He consulted Dr Goyer whilst attending a clinic for treatment. He described the consultation in his witness statement as follows:
13 The man on the phone introduced himself as a doctor. The doctor explained that he was going to prescribe me with the tongue strips. The doctor mentioned that the tongue strips had a mild dose of medication, the name of which I cannot remember. He said that I would need to take a tongue strip every night for a week before I went to bed and then every second day after that. The doctor told me that if I had any side effects from the medication, I should call AMI. The doctor did not tell me how long I would need to take the medication for. The doctor did not ask me anything about my medical history and we did not discuss premature ejaculation. The doctor and I spoke for around two minutes.
[ACCC 1.19]
831 In cross-examination the patient confirmed that the conversation with Dr Goyer was very brief [TS 71]. The Patient Assessment Form stated, “Side effects explained” [R13.12, p 323]. Read consistently with the patient’s witness statement, this comment may mean no more than the patient was told to ring AMI if there were any side effects. In any event, Dr Goyer did not refer directly to this consultation in his witness statement. Consequently, the patient’s evidence in this regard should be accepted. Although the Patient Assessment Form stated that alternative treatments and follow-up in a couple of weeks were spoken about, the patient denied this in evidence-in-chief [TS 69]. His evidence should be preferred over the Patient Assessment Form.
832 In Berry Statement 2, Dr Berry stated that since the Annexure B recordings she had changed some of her consulting practices in view of the ACCC allegations, even though she did not accept that the allegations were justified [R13.32, p 5]. The changes referred to were mostly unspecified. The evidence of the two Annexure C consultations with Dr Berry did not exhibit any particular changes from her past consulting practices during the AMI period. Dr Goyer and Dr Condoleon did not say that their consulting practices had changed in the NRM period.
833 The evidence of and relating to the Annexure C consultations demonstrated that, as alleged by the ACCC, doctors did not conduct physical examinations of, or face-to-face consultations with, patients, prescribed only NRM medications and did not disclose this to the patients, did not advise the patients as to the terms on which the treatment was provided, did not diagnose or treat underlying causes of the patients’ conditions, and did not refer the patients to GPs or specialists for those causes or other presenting conditions. The evidence also established that in 14 of the Annexure C patient consultations, doctors did not advise or adequately advise about side effects of the NRM medications.
834 Save in respect of the doctors not advising patients as to the terms on which the treatment was provided, each of the matters referred to in the previous paragraph were instances in which the NRM doctors failed to meet the accepted professional standards of medical practice.
835 Further, there are examples in the 16 Annexure C patient consultations of doctors failing to take adequate medical histories and of determining to prescribe oral strips rapidly, without proper medical foundations for the prescription.
836 The evidence of the NRM consultations as a whole supports an inference that the role of the doctor was, as Dr McRae suggested, to provide the capacity to supply a prescription in a system operated to produce that result. The overriding impression provided by the evidence of the Annexure C consultations was that they were conducted as a necessary part of a commercial exercise designed to serve the financial interests of NRM without a real consideration for the welfare of the patients.
837 The respondents did not suggest that the recommendation to patients that they should enter into treatment programs for 12 to 18 months changed from the AMI to the NRM period.
838 Seven NRM patients, namely patients NRM 2, NRM 4, NRM 6, NRM 8, NRM 10, NRM 14 and NRM 16 entered 12-month treatment programs, and four NRM patients, namely patients NRM 3, NRM 5, NRM 11 and NRM 15, entered into 18-month treatment programs. All of these patients sought treatment for PE.
839 The ACCC alleged that the lengthy fixed-terms served the commercial interests of NRM, but were not medically justified. As discussed at [610] – [679] of these reasons, there was no medical justification for long-term treatment periods with the medications used by AMI and NRM.
840 A significant change in the practice of the AMI business from the AMI period to the NRM period was the contractual term relating to termination and refunds.
841 The administrators of AMI utilised a new refund term (first NRM refund term) [ACCC 4.447; ACCC 1.41, pp 49 – 50]. NRM continued to use that term from the date it purchased the business in June 2011 until, certainly December 2011, but on the evidence relating to one Annexure C patient, potentially February 2012.
842 The first NRM refund term was as follows:
Sexual dysfunction is a chronic condition and treatment can take some time. For this reason, we stipulate that your contract with us [is] for the period decided in the first consultation with the AMI doctor.
You may cancel your treatment program with AMI at any time by giving AMI not less than 30 days notice. Cancelling your treatment program you will be entitled to a refund for the unexpired period of your treatment program less an administration fee of 15% and less the cost of any medication already provided to or prepared for you. No refund will be provided for the expired period of the treatment program or the 30 day notice period. All cancellation must be communicated to AMI in writing signed by you. Oral cancellation will not be accepted in any circumstances.
[ACCC 1.41, p 50]
843 Mr Kyle said that the 48-hour cooling-off period used by AMI was not used in the period of administration or by NRM. Mr Kyle was the refunds manager of NRM from the date of the purchase.
844 The ACCC alleged that the lack of a cooling-off period amounted to unconscionable conduct. Six NRM patients tried to cancel their contracts within a day of making the agreement with NRM, but their requests were refused.
845 Patient NRM 1 felt pressured into signing the contract when he attended a clinic for treatment for PE. He told the salesperson that he thought he could not afford the cost. He was uncomfortable when he left the clinic and worried about paying the $950 for a four-month program. That evening, he spoke to his girlfriend. They agreed that he did not need the medication and that $950 was too much to spend on it. The next day he requested a cancellation and refund for those reasons. The contract was not cancelled and the patient did not receive a refund.
846 Patient NRM 2 paid $2,100 for a 12-month treatment program in February 2012. He borrowed the money from his father. That night he spoke to his girlfriend who said that he had nothing to worry about. He had told Dr Goyer that he ejaculated in no more than five minutes. Dr Pattison expressed the view that the patient probably did not have PE. The patient rang NRM several times to cancel the contract the next day. He then wrote a letter requesting to cancel. In the letter he wrote that a family emergency had just arisen and he needed the money for that purpose. It took until 15 June 2012 for him to receive a partial refund of $1,662.50.
847 Patient NRM 5 paid a deposit of $500 for a $4,500, 18-month treatment program. The day after making the agreement he tried unsuccessfully to cancel the contract and obtain a refund of the deposit. He told NRM that after discussion with his wife he felt that he could not afford the cost of the program.
848 Patient NRM 8 signed a contract at a clinic for a 12-month treatment program at a cost of $3,000. He paid a deposit of $300. As he left the clinic he panicked as he realised that he could not afford the cost. He was a first-year apprentice. The next day he rang NRM to cancel the contract. He said that he could not afford it and felt he was pushed into signing. He was refused a refund unless he paid 25 per cent of the outstanding contract price. He asked his mother to pay NRM to protect his credit rating.
849 Patient NRM 13 paid $1,100 in September 2011 for a three-month treatment program. His evidence was that he was told by the salesperson that, “If you change your mind within 48 hours, you won’t be charged. There is no obligation at all.” [ACCC 1.23, p 4] On the same day, he spoke with his girlfriend who said he had no reason to worry. After many calls it took until December 2011 for the cost to be refunded.
850 Patient NRM 16 agreed to 12 months of treatment at $50 per week. He paid a deposit of $70. That evening he came to the view that he could not afford the cost and his girlfriend told him that she did not think he had a problem. The next day he called and then wrote to NRM seeking to cancel the contract and explain that he could not afford the cost. He was told that he would have to pay a $560 cancellation fee which had been approved by the ACCC. In the end, no further payments were deducted by NRM and he did not pay the $560 cancellation fee.
851 In addition to the absence of a cooling-off period, the ACCC criticised the first NRM refund term for several reasons.
852 First, the patient was charged for the expired portion of the contract even where the medication was ineffective, and whether or not the patient had received any medication in that period. Further, the expired portion included the 30-day notice period.
853 Then, the 15 per cent administration fee was calculated on the entire program cost. The basis for the calculation was not disclosed to patients. It could not relate to NRM’s reasonable costs because it was applied to that part of the program cost covering the unexpired portion of the program. It also applied to the expired portion of the contract, for which the patient had paid and/or had been charged already pursuant to the refund policy.
854 And finally, the patient was required to pay for the cost of medication provided or prepared, but was not told how that cost was calculated. The cost of medication would be expected to have been included as part of the cost of the expired portion of the contract, for which the patient was charged, or included in the administration fee.
855 Mr Kyle explained that when patients attempted to cancel their contracts, even if they were entitled to do so under the terms of the contract, he and other refund staff always tried to persuade them to continue with the program. Patient NRM 11 is an example. He rang to cancel the contract after about two weeks because it gave him a rash on his face and an upset stomach. He was told to try a lower dosage. He said, “I don’t really want a lower dosage, I just want to cancel”. Then he was told, “Look, just try this lower dosage. See what happens.” [ACCC 1.21, [24]]
856 Then, the ACCC established that the first NRM refund term was not brought to the attention of patients in a way which practically informed them of its contents before they agreed to treatment.
857 Patients who consulted entirely by phone were played a recording of the contract terms. Although lengthy, it is useful to set out those terms as follows:
AMI'S TERMS AND CONDITIONS
By reason of this contract, the following obligations arise:
1. AMl's obligations to you
a. Before you entered this contract, one of AMI's registered doctors, undertook with you a confidential medical consultation, made a diagnosis of sexual dysfunction and advised you whether one or more of our treatment options would be appropriate for you to be prescribed.
b. Pursuant to this contract and subject to the provisions below, we will during the period of contract:
i. Arrange for our associated pharmacist to supply you with the treatment which is prescribed by the AMI doctor for as long as it continues to be prescribed for you;
ii. Arrange delivery of any medication and devices which are part of your treatment at an address which you notify to us;
iii. Provide such follow-up care and treatment as may be prescribed by AMI doctors, including monitoring of results through information provided by you, adjusting prescribed medication, varying your medication options or trying an alternative method of delivering medication;
iv. Provide you with nursing advice and guidance as to the use of the medication that we have prescribed, including helpline.
c. WE DO NOT
i. Give general medical advice. For advice and treatment of all other issues than sexual dysfunction, you must attend your GP;
ii. Prescribe or supply treatments available otherwise than through AMI. If the AMI doctor considers that another type of treatment is in your best interests, he will not recommend entry into a treatment contract with AMI.
iii. Under any circumstances prescribe or supply medication which, in the opinion of an AMI doctor, is or might be contra-indicated in your case;
iv. Guarantee the success of the prescribed treatment. Although AMI doctors will work with you in the event that the treatment does not produce immediate results, you should understand that, as with any medical treatment, it is possible that even after prolonged use and therapeutic adjustments it will not achieve your hopes and expectations;
v. Guarantee that the medication will not cause side effects. As with all prescription medication there is a possibility of side effects, which are usually quite mild and will usually decrease with repeated use of the medication. You will receive with the medication a booklet explaining the use of the medication and its known side effects. You should read this booklet carefully and ensure that you understand its meaning.
d. We will treat the information that you supply to us [as] confidential in accordance with our privacy policy attached. However, we encourage you strongly to disclose the treatment that we provide to your GP, or to permit us to make this disclosure on your behalf.
2. Your obligations to AMI
a. The success and safety of treatment is dependent partly on the accuracy and completeness of the information you supply. It is a fundamental term of this contract that you disclose candidly to AMI, and keep us informed at all times of, any material change to your state of health, the diagnosis of any disease and any medication or other drugs that you are taking. If you do not do so, we reserve our right to treat this contract as discharged forthwith;
b. You agree further to notify AMI immediately if you are experiencing any side effects other than those explained in the booklet supplied with the medication or if the side effects do not abate with regular use or if the side effects are such that the booklet advices [sic] you to contact AMI.
c. You undertake not to use the items supplied to you except for your own personal use. In particular, you will not administer or supply them to anyone else, whether or not for reward. If you do so, we reserve our right to treat this contract as discharged forthwith;
3. Termination
Sexual dysfunction is a chronic condition and treatment can take some time. For this reason, we stipulate that your contract with us [is] for the period decided in the first consultation with the AMI doctor.
You may cancel your treatment program with AMI at any time by giving AMI not less than 30 days notice. Cancelling your treatment program you will be entitled to a refund for the unexpired period of your treatment program less an administration fee of 15% and less the cost of any medication already provided to or prepared for you. No refund will be provided for the expired period of the treatment program or the 30 day notice period. All cancellation must be communicated to AMI in writing signed by you. Oral cancellation will not be accepted in any circumstances.
[ACCC 1.41, pp 49–50]
858 In the recording played to the patient, these entire terms were read out. Two versions of the recording used by NRM were played in Court. In the first recording, the terms were read out so fast and softly as to be practically inaudible. In the second recording, again, all the terms were read out. The diction was clear. However, the tone was monotonous and the pace fast. These factors, taken with the length of the presentation, made it unlikely that the patient would retain attention to notice the last paragraph setting out the first NRM refund term. Patient NRM 10 said that the recording was “really fast” and that “it was hard to concentrate and listen to what was being said.” He thought it was just a formality [ACCC 1.20, [23]]. Furthermore, the recording was played after he had made the agreement and given his bank details to pay for the cost of the treatment. In another instance, the reaction of patient NRM 11 was not surprising. He stated:
12 After taking my credit card details, the man played me a recording of the terms and conditions of the contract. The recording played for a long time, it felt like several minutes. I could barely hear it because it was played at a low volume and because I was at work, there was a bit of noise around me. I switched off after a while and was not listening to it closely, but just waiting for it to finish.
[ACCC 1.21]
859 It may also be that the recording was not always played. Patient NRM 14 had no recollection of being played any recorded message over the phone [ACCC 1.24, [15]]. Further, although unclear whether he was played the recorded message, patient NRM 12 gave evidence that he was not provided with a written form of the terms and conditions until three shipments into the treatment program [ACCC 1.22, [40]; TS 113–114]. Furthermore, the terms and conditions provided were incorrect because the AMI refund term, and not the first NRM refund term, was set out in the document eventually provided to the patient [ACCC 1.22, exhibit BR-4].
860 Where patients attended a clinic they were given the terms in writing in the form set out at [857] of these reasons for judgment, and were asked to sign the document. None of the Annexure C patients who attended a clinic were told by the salesperson about the first NRM refund term. Further, the witness statements of Annexure C patients who attended clinics show, for instance, that some were asked to sign whilst the salesperson was talking to them (patient NRM 5) [ACCC 1.17, [32]], or that some did not have time to read the terms as they were rushed by the salesperson (patient NRM 8) [ACCC 1.19, [19]].
861 And, finally, the ACCC established that there were situations in which the first NRM refund term operated harshly outside the circumstances where a patient simply changed his mind. Patients who experienced unpleasant side effects or who found that the treatment did not work were denied full refunds.
862 Patient NRM 15 entered into a contract for an 18-month treatment program in July 2011. In September 2011 he suffered a back injury and was required to take constant pain medication. He formed the view that the oral strips were not helping with his PE. For these reasons, he sent a letter requesting cancellation of his contract for this reason. Despite the letter NRM, did not stop the direct debit of instalments from his account. The patient cancelled his debit card in order to stop further payments being deducted [ACCC 1.25].
863 Patient NRM 11 took oral strips over two weeks and developed a rash with bumps on his face, and experienced an upset stomach and diarrhoea. He requested cancellation of his contract, but NRM deducted payment for a further shipment of medication. He ended up paying $400 for a treatment which gave him unpleasant side effects and for a second shipment of medication that he did not use [ACCC 1.21].
864 Patient NRM 14 was told that the oral strips would produce results in two to three weeks. After using the strips for about a month, the patient experienced no improvement in his condition. He was sent a second shipment of medication without being asked whether the first shipment was working. A few weeks later he sent a letter requesting to cancel his contract, but NRM continued to take direct debit payments for three weeks. He ended up paying $797.35 for about seven weeks of treatment, which did not work.
865 In his first witness statement dated 7 September 2012, Mr Shrestha stated that from December 2011, NRM changed its standard terms and conditions [ACCC 4.449; R 13.11, [74]]. Paragraphs 1 and 2 remained unchanged from the version set out in the first NRM refund term, but paragraph 3 relating to termination provided:
Sexual dysfunction is a chronic condition and treatment can take some time. For this reason, and also to cover some of our underlying cost of providing the services AMI offered to you, the AMI contract [is] based upon the recommended treatment period mentioned in your consultation with the AMI doctor, In any event, You may cancel your treatment program with AMI after an initial 60 days, at any time without reason by giving AMI not less than 14 days prior written notice. Upon cancelling your treatment program you will be entitled to a refund for the unexpired period of your treatment program.
(second NRM refund term)
[R 13.11, p 203]
866 Thus, the notice period was reduced from 30 days to 14 days, but could not be exercised until 60 days after the commencement of the contract. Further, no deduction from the refund was made for the cost of medication or for any administration fee. Again, a recording of the contract terms was played to patients. The recording which was tendered in evidence was spoken at a similar pace as the better audio version which contained the first NRM refund term, and was shorter by the omission of clause 2 of the terms. The terminology used mostly followed the written version set out at [857] of these reasons for judgment.
867 One possibly important omission from the second NRM refund term as read in the recording were the words “without reason” which appear in the written version. Nor did the recording specify that the notice of cancellation ought to be in writing [ACCC 4.450].
868 Mr Shrestha stated that the change to the first NRM refund term was made in consultation with Dr Vaisman after considering the claims made by the ACCC in this proceeding [R 13.11, [74]].
869 There is no complaint by the ACCC in this proceeding about the second NRM refund term.
6. FACT FINDINGS IN RESPECT OF DR VAISMAN
870 The ACCC alleged that Dr Vaisman was largely responsible for the advertising and selling methods, and hence the unconscionable conduct involved in those aspects, of the business of AMI and NRM. It said that Dr Vaisman knew of and endorsed the terms of the AMI and NRM contracts and the conduct of the doctors which was unconscionable. The ACCC also alleged that Dr Vaisman knew that men who rang AMI were frustrated, ashamed, dissatisfied, distressed, anxious, and were lacking in self-confidence, and were thus vulnerable.
871 Dr Vaisman was the founder of the business. He was the Chief Executive Officer and Managing Director of AMI and NRM. He was also the sole director of NRM at all relevant times.
872 Dr Vaisman agreed that he made the critical decisions of the organisation [TS 1621]. In a document setting out his personal history Dr Vaisman is described as:
[R]esponsible for the overall management and strategic direction of AMI's Australian impotency business.
[ACCC 4.404].
873 As was explained in [126] of these reasons for judgment, Dr Vaisman was responsible for the content of the advertising and for monitoring its effectiveness.
874 As was explained in [145] – [155] of these reasons for judgment, the selling techniques used by the salespeople were designed by Dr Vaisman. They were disseminated to the salespeople in scripts and materials made or approved by him, and in training sessions addressed by him. Although Mr Shrestha was responsible for ongoing regular training of the sales staff, Dr Vaisman participated in that process. Dr Vaisman put pressure on the salespeople to comply with the instructions which he gave. The result of Dr Vaisman’s work was that his techniques were used by the salespeople and he was thus directly responsible for the conduct in which they engaged. The sales techniques taught by Dr Vaisman were designed to manipulate patients by engendering fear of social and medical consequences of not taking the treatment, and by preying on the anxieties common among men seeking treatment for sexual dysfunction.
875 The business model which Dr Vaisman adopted involved offering to patients treatment for 12 to 18 months. He attempted to explain the length of this period on a medical basis. However, as demonstrated at [610] – [679] of these reasons for judgment, such long-term treatment with AMI and NRM’s medications was not medically justified on the evidence presented to the Court. He knew that the longer the contract the greater the return to AMI. His objective was to have patients agree to treatments for 12 to 18 months. Thus, he instructed sales staff through training scripts and materials, and in training seminars and regular meetings, to tell patients that the treatment was for 12 to 18 months.
876 Dr Vaisman knew how the contracts operated, and in particular, how the refund terms were implemented. For instance, in relation to the AMI refund term, he was asked in cross-examination about patients who were frightened of the prospect of self-administered intracavernosal injections in the base of the penis. He said that the effectiveness of other medications for ED would become clear within about two weeks. He said that even if a patient refused treatment by injections when these other medications had failed within a short period of time, AMI would still keep the money paid for the full period of treatment. Asked why AMI should retain the money in those circumstances, he replied:
Because contract says clear that if none of the treatment options with injection is not working, then only he can get the refund.
[TS 1823]
877 In view of Dr Vaisman’s role in the companies and his direct participation in the everyday management of the operation, he was familiar with issues which arose concerning claims for refunds. For example, he signed all the refund cheques [R 13.1, [46]]. And Mr Kyle said in his witness statement that Dr Vaisman told the refund staff at meetings that the AMI refund term should be strictly applied [ACCC 1.41, [54]].
878 Other aspects of Mr Kyle’s evidence about Dr Vaisman’s knowledge of the application of the refund terms were denied by Dr Vaisman and Mr Shrestha. However, Mr Kyle was cross-examined on the issues and he proved to be a reliable and straightforward witness. His account should be preferred. He said that Dr Vaisman was present at some weekly sales-staff meetings when refund issues were discussed. For example, the refund staff members were invited to sales-staff meetings to discuss complaints by patients that they had not been provided with an understanding of the refund term. Dr Vaisman instructed the refund staff to try to convince patients to stay on the program even if they were entitled to a refund. Dr Vaisman conducted role plays in which he told the patient that they should stay on the program because the medications prevent strokes and heart attacks. As set out at [186] of these reasons for judgment, Dr Vaisman himself admitted that this was not true.
879 Dr Vaisman said that he held the view that physical examination by a doctor was not necessary for the treatment of ED or PE [TS 1738]. He also said he held the view that the first treatment for ED should be apomorphine delivered by nasal spray and later, by oral strip, and the first treatment for PE should be clomipramine delivered by nasal spray and later, by oral strip. He said he regarded the side effects of these medications as minimal. He said that he held the view that treatment with apomorphine was as effective as and was preferable to treatment with PDE5 inhibitors, and treatment with clomipramine was preferable to treatment with SSRIs [R 13.1, [38]–[39]]. However, he said that the decision of which medication to prescribe was left to the doctors alone. Dr Vaisman said he held the view that treatment for ED and PE should be over a 12-to-18 month period [R 13.1, [42]; TS 1710, 1714]. All of these views were unconventional and departed from the mainstream of medical understanding and practice for the treatment of ED and PE. Yet they all found a place in the consultations with Annexure B and C patients conducted by doctors engaged by AMI and NRM.
880 There is no coincidence in that phenomenon. Dr Vaisman trained most of the doctors when they were initially engaged by AMI or NRM (see for example, R13.18, [73]; R 13.20, [15]). He held regular meetings on about a monthly basis at which treatments and medications were discussed. He distributed to doctors scientific materials which he said supported his views [R 13.1, [34]]. When Dr Vaisman gave his evidence he defended his views with vigour and force. He conveyed the impression that he would brook no opposition to the approach he took because he regarded that approach as unarguably correct. That argument lent support to the claims of Dr Lonergan and Dr Vandeleur that Dr Vaisman enforced his views directly on the doctors.
881 Dr Vandeleur said that Dr Vaisman told doctors at doctors’ meetings that he preferred them to recommend treatment for 12 to 18 months [ACCC 1.39, [41]]. Dr Vandeleur said that he could not realistically work at AMI if he did not recommend 12-to-18 month treatment periods [ACCC 1.39, [44]]. The only reason he did so was to comply with AMI’s practices. Dr Vandeleur was cross-examined on the subject and repeated that there was pressure to mention 12-month treatments periods. This was conveyed by Dr Vaisman to everybody [TS 741, 771]. Dr Vandeleur’s evidence on this matter was convincing. He had left AMI. He did not appear to bear any animus against Dr Vaisman and gave his evidence in a matter-of-fact way.
882 Dr Lonergan said that Dr Vaisman told doctors at doctors’ meetings “I can’t pay your wages if you don’t sell them 12 to 18 months. I can’t survive on small sales.” [ACCC 1.37, [37]]. Dr Lonergan said that Dr Vaisman told doctors at the regular meetings that if they did not recommend 12 to 18 months’ treatment, “I don’t need you here”. Dr Lonergan exhibited a degree of antipathy towards Dr Vaisman. Unlike Dr Vandeleur, Dr Lonergan’s engagement was terminated by Dr Vaisman. However, he presented as a meticulous, if not pedantic man who was committed to accuracy in the evidence which he gave. His evidence on this matter should be preferred to the evidence of Dr Vaisman and Mr Shrestha.
883 Dr Lonergan and Dr Vandeleur also said that Dr Vaisman enforced the practice of prescribing apomorphine and clomipramine. Dr Lonergan said that Dr Vaisman demanded that he prescribe apomorphine rather than vardenafil because vardenafil, “costs me too much money” [ACCC 1.37, [43]]. He recalled Dr Vaisman saying words to him to the effect:
I forced all of the other doctors to prescribe clomipramine.
[ACCC 1.37]
884 Dr Vandeleur preferred to prescribe vardenafil for the treatment of ED and thought it was more effective than apomorphine. Dr Vaisman told him that it was more expensive and he preferred Dr Vandeleur to prescribe apomorphine because it was “costing AMI a fortune” [ACCC 1.39 [33]]. Dr Vandeleur said that had he not been working for AMI he would likely not have prescribed apomorphine [ACCC 1.39, [36]].
885 Dr Vaisman denied the conversations alleged by Dr Lonergan and Dr Vandeleur. In cross-examination Dr Vaisman repeated many times that the choice of medications was up to the doctor. That it was their choice. That they were independent. He said that he gave them literature which supported his views, but that they had to make their own clinical judgment. A substantial difficulty with this argument is that, as previously discussed in these reasons for judgment, the literature given to the doctors by Dr Vaisman did not support the use of apomorphine and clomipramine as first-line treatment.
886 Dr Lonergan said that Dr Vaisman provided written directions to doctors from time to time [ACCC 1.37, [81]]. One example was provided to him by Dr Vaisman’s personal assistant in 2010. It referred to the use of apomorphine and clomipramine as first-line treatment as follows:
ED
Treatment start with APD nasal spray (Apomorphine, Phentolamine and Domperidon instead of Metoclopramide which theoretically can cause carditive dyskinesia.) If nasal spray causes side effects like burning sensation or bleeding than [sic] APM trochey can be used. In trochey we left metoclopramide because the taste of Domperidone is very bitter.
Of course you can use pure Apomorphine (A) or Apomorphine and Phentolamine (AP) in nasal spray or trochey forms. Please, keep in mind that some time it takes up to 3 weeks of regular use of Apomorphine containing formulations to start to work and that should be explained to the patient. If after regular use of Apomorphine formulations for 3-4 weeks patient complain that the treatment is not effective we recommend him Selfinjection Therapy. The best explanation of the rational [sic] behind it that the blockage of the arteries in the penis is more than it was anticipated and that is why for a short period of time his blood vessels in the penis required burst from inside for short period of time. As soon patient after trial realize that injections are not painfull [sic] (particularly with the use of our autoinjectors) we don’t need to convince him more. I always give analogy with pneumonia – always treatment start with oral antibiotics and if they are not effective we have to use injectable antibiotics. The acceptance of injectables is such explanations is very high, particularly when we never stop APD (AP or A) spray or trochey because Apomorphine stimulate production of Dopamine and Dopamine is a “good feeling” hormone presence of which gives patient a feeling of naturalness of an erection. Always in case of ED injectables started from 2 units of INJECT ED and patient increase every time himself 2 units till he is reaching desirable result of duration and rigidity of an erection. Maximum dosage can be up to 100 units or very rare up to 200 units (2 syringes from both sides of penis). But in such cases (when it’s required more than 90 units sex should be recommended once a fortnight with proper palpation of the penis and if any nodules or scars are detected not to use this side till this nodule (scar) is dissolved. If nodules or scars appeared from both sides – injections must stopped. When patient using up to 80 units he can have sex 2 – 3 times per week no more.
If patient ask doctor for injectables which are not required refrigeration than you can use INJECT NF. If patient had a history of prolong erection of priapism from INJECT ED or INJECT NF then only INJECT PGE1 is used. The same INJECT PGE1 can be used for treatment of PE if clomipramine, paroxetine or tramadol are not effective.
If patient categorically refuses from injections then intraurethral gel (Alprostadil) can be prescribed and if patient is refusing even from that then PQ nasal spray or trochey recommended.
PE
Treatment always started from Clomipramine nasal spray or tablets or capsules (20 or 40 mg). If Clomipramine causing nausea than [sic] CD (Clomipramine and Domperidone) nasal spray or tablets can be prescribed.
If Clomipramine is contraindicated new Paroxetine trochey 20 mg can be prescribed, if the taste of trochey is unpleasant patient can swallow trochey. In case of Clomipramine and Paroxetine at least 1 week require of daily use (nasal spray or trochey) and then as “required” use.
IF Clomipramine or Paroxetine are contraindicated then Tramadol nasal spray or trochey can be prescribed. If none of the antidepressants are can be used (contraindicated, ineffective or side effects) than [sic] local anaesthetic sprays (on the glans of the penis) can be prescribed. If none of above mentioned treatment options can be used than [sic] INJECT PGE1 should be used.
It is very important to treat one problem at the time. Never combine treatment of PE and ED. If patient is younger than 40 years and complanes [sic] on both PE and ED problems treat him on as PE patient. If he is older than 40 years old then treat only as ED irrespective of PE problem. In 3-4 month of treatmen[t] of 1 problem if he is still complaines [sic] on [other] (ED or PE) than [sic] you can added treatment option.
Exclusion only when even 100 units of injectables are not effective that PQ trochey can be added.
Jack
[Emphasis added.]
[ACCC 1.37, p 76]
887 The document concluded with the typed word “Jack”. Dr Vaisman said that he wrote it, but that it was not distributed because all documents distributed by him were signed by him [TS 1697]. The probabilities are that the document was provided to the doctors by Dr Vaisman. There was no other reason Dr Lonergan would have it. The document reflects Dr Vaisman’s preference for the use of apomorphine and clomipramine, and supports the conclusion that Dr Vaisman, in practice, sought to govern the prescribing practices of doctors.
888 In view of these matters, and of the definite views expressed and the forceful character exhibited by Dr Vaisman, his denial that he enforced his views on the doctors was not credible. I find that Dr Vaisman, in effect, required the AMI and NRM doctors to recommend to patients that they take treatment for 12 to 18 months, and that the doctors prescribe apomorphine and clomipramine. In truth, the doctors had no practical or realistic choice to depart from the preferences expressed by Dr Vaisman if they wanted to remain employed.
7. WAS THE CONDUCT OF AMI, NRM, AND DR VAISMAN UNCONSCIONABLE?
889 The question addressed in this section is whether the facts found in Sections 4 and 5 of these reasons for judgment constitute unconscionable conduct in view of the principles applicable as set out in Section 2 of these reasons for judgment, and whether the facts show that Dr Vaisman was liable as an accessory.
890 Each of the instances of unconscionable conduct alleged against AMI and NRM by the ACCC are now considered.
891 Dr Vaisman knew that men who suffered from ED or PE generally felt anxious about their condition. He believed that they felt frustrated, ashamed, dissatisfied, distressed, and that they suffered from low self-esteem. Dr Vaisman targeted these characteristics as a method of pressuring patients to agree to treatment programs. Salespeople were trained by him to take advantage of these feelings as a means to sell treatment programs.
892 Selling techniques used in commercial transactions are generally aimed to take advantage of the characteristics of potential customers. The young man encouraged by a used-car salesman to buy a “chick magnet” is an example. What made the targeting of consumers by AMI and NRM unconscionable was that the selling techniques utilised the feelings generated by a medical condition for which the patient was seeking assistance. There is particular opprobrium attached to such targeting because it is directed to a personal condition which generates strong emotional responses in sufferers. Those responses are prone to cloud the decision-making capacity of the patient. The selling techniques of AMI and NRM were directed to compromise the patient’s consideration of his self-interest in favour of the commercial interest of AMI and NRM. It is immoral to seek to harness the fears and anxieties of men suffering from ED or PE for the purpose of selling medical treatments. To target the patient’s vulnerability in this way is to use an unfair tactic and that is a possible marker of unconscionable conduct referred to in s 51AB(2)(d) of the TPA, s 21(2)(d) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(d) of the ACL in operation after 1 January 2012.
7.2.2 High-pressure sales techniques
893 AMI and NRM salespeople were trained to use high-pressure sales techniques to sell the treatment programs. They were instructed in methods which were likely to frighten men into agreeing to the treatments offered by AMI and NRM.
894 The salespeople were trained to tell men that if they did not agree to treatment, they would suffer adverse medical consequences, including shrinkage of the penis and psychological impotence. There was no scientific basis established before the Court for these claims. The salespeople were instructed to say that the treatment for ED would reduce the chance of heart attack or stroke. They were also instructed to inform patients that their partners may suffer from depression if they did not take the treatments. The threat of dire medical and social consequences placed pressure on men to accept the treatments.
895 The salespeople also told men that the medications would be effective not just to treat, but to cure their problems. This offered a further inducement to agree to treatment. And the men were reassured that if the treatment did not work they would be entitled to a refund.
896 This technique of selling was prone to rob men of independent judgement of the need for, and value of, the treatment, and induce them to enter into agreements which they would not otherwise have accepted if the pressure had not been applied.
897 The technique of frightening men by telling them of the dire adverse consequences of not agreeing to treatment and assuring them that the treatment was effective was part of the business system of AMI and NRM. It was formulated by management and imparted in an organised fashion through scripts and training sessions.
898 The 145 Annexure B recordings and the statements of the seven other Annexure B patients, together with the oral evidence of some of them, demonstrated that the training was implemented by the salespeople. In the case of the Annexure C patients, the evidence showed that six patients were told by salespeople that the treatment would be effective for them. Patients gave evidence that they felt pressured by salespeople.
899 Training salespeople to trap vulnerable men into agreeing to treatment programs by the use of high-pressure selling was dishonest conduct. It resulted in undue pressure on the consumer, which is a marker of possible unconscionable conduct referred to in s 51AB(2)(d) of the TPA, s 21(2)(d) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(d) of the ACL in operation after 1 January 2012. These selling techniques also relied on the advertisement to patients that AMI and NRM were providers of medical treatment. That placed them in a superior bargaining position in relation to men who sought medical treatment. Exploiting a superior bargaining position is a marker of possible unconscionable conduct referred to in s 51AB(2)(a) of the TPA, s 21(2)(a) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(a) of the ACL in operation after 1 January 2012.
900 The respondents submitted that the conduct of AMI and NRM could not be unconscionable because the patients rang AMI and NRM of their own free will, and, in the course of the call, were able to hang up the phone and terminate the contact. The respondents called in aid the circumstances in Lux, in which salespeople visited customers’ homes, gained entry by deception, and thereby placed customers in a position where they could not easily terminate the interaction.
901 The argument seeks to elevate the facts of Lux to a principle applicable to the establishment of unconscionability in other cases. The facts of the present case are very different. But the circumstance that the interaction in this case was over the phone rather than in the victims’ homes says nothing meaningful about whether the alleged conduct was unconscionable. Rather than knocking on the door of a patient’s home, AMI and NRM lured patients to contact them by phone by advertising that they provided medical treatment by new and convenient medication. For men worried about their condition, this was a potent method of AMI and NRM procuring the patients to phone.
902 The argument of the respondents assumed that patients had a real choice to hang up the phone and terminate the interaction. But the facts demonstrated otherwise. The sales techniques used by AMI and NRM were designed to manipulate the fears and insecurities of the patients so that they would agree to the treatment and not hang up the phone. This was particularly clear in the cases in which patients agreed to treatment and then changed their mind as soon as they hung up the phone. As long as the pressure was being applied by the salespeople, the patients were captive. Only when that direct pressure was released did some try to cancel their agreements. The sales techniques used by AMI and NRM had the purpose and effect of preventing the patients from hanging up the phone, and pressuring them into taking the treatment. Thus, any negotiation by the patient about the price of the treatment was more likely to signify a degree of desperation on his behalf, than to signify an ordinary process of commercial bargaining.
7.2.3 Remuneration of salespeople by commission
903 The salespeople were told by AMI and NRM in scripts and training materials not to disclose to patients that they were paid by commission. Payment by commission meant that the salespeople had an interest in selling higher priced programs. Had they disclosed that they were paid on commission, patients may have been alerted to the interest of the salespeople in selling higher priced programs. It may also have alerted patients to the fact that they were not consulting a traditional medical practice.
904 In many other commercial circumstances salespeople are remunerated by commission and do not disclose the fact to consumers. However, in the circumstances of AMI and NRM, the failure to disclose the basis of remuneration was part of a pattern of conduct which kept relevant details from patients in a bid to obtain their agreement to treatment programs, and aided the selling process. It was an integral part of the business system because it was part of the training provided to salespeople. The operation of the system was seen in all 168 individual transactions because in no case did the salespeople disclose that they were paid on commission.
905 The failure to disclose the basis of the remuneration of salespeople was dishonest and exploitative, it was sharp practice and deceptive, particularly in the circumstances when men believed they were consulting a medical practice which characteristically make patient welfare a primary concern. It was an unfair tactic, which is a possible marker of unconscionable conduct referred to in s 51AB(2)(d) of the TPA, s 21(2)(d) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(d) of the ACL in operation after 1 January 2012.
906 The AMI refund term required patients to try all treatment options, including self-administered injections into the base of the penis, before being entitled to a refund or cancellation of direct debits. Salespeople were directed to tell patients that a refund policy was available to them if the desired result was not achieved with the first recommended treatment followed by other available options if needed. This explanation concealed the full extent of the pre-conditions to obtaining a refund. In particular, it did not draw attention to the requirement for the patient to try self-injection in the base of the penis before being entitled to a refund.
907 The practice of AMI was to send out a copy of this term with the first delivery of medication, that is to say, after the patient had agreed to the treatment program. Even then, the refund term was at the end of the instruction booklet, which was not otherwise a contractual document.
908 It was unduly harsh of AMI to impose on parties a requirement to try all treatment options before becoming entitled to a refund.
909 It was particularly severe to impose this term when the idea of injecting into the base of the penis was a very disagreeable prospect to most men. Further, the requirement applied equally to PE patients even though intracavernosal injection was generally not a medication used to treat PE, except in very rare cases.
910 And, the term could operate unfairly in certain circumstances.
911 A major drawcard of the program offered by AMI was the convenient form of delivery by nasal spray. Where a patient agreed to the nasal spray treatment and that proved ineffective, it was reasonable that he be permitted to cancel the contract. The AMI refund term did not allow this to happen.
912 The term also operated where a patient agreed to the treatment program, but on reflection changed his mind within a short time after the call to AMI. Having regard to the anxiety associated with ED and PE, and the high cost of the programs, there was a need for a cooling-off period to allow patients to consider their need for the treatment and their capacity to pay for it. AMI recognised this need by allowing the patients to cancel within 48 hours if they had a change of mind. But AMI did not tell patients that it had such a policy. Hence, patients were not aware that they could cancel the treatment program if they had a change of mind shortly after the call.
913 The AMI refund term also operated when a patient experienced severe side effects and, for that reason, did not wish to continue treatment. He was committed to continue paying for the treatment when it was reasonable for him to refuse further medications.
914 The refund term also allowed AMI to deduct the cost of medications supplied from the refund amount, but patients were not told how the cost of medications was calculated. Further, the 15 per cent administration fee was calculated on the entire contract cost even though there was no administration cost involved for AMI after the contract was terminated. Neither basis for calculation of the cost of termination was disclosed to the patient.
915 The refund term applied in all Annexure B cases in which men entered into contracts with AMI. The directive to salespeople which instructed them to tell patients of the term, but which did not disclose the full effect of it, applied in all cases. This was part of the way AMI operated. The evidence of the 152 Annexure B patients demonstrated that the system applied at the level of the individual transactions. The requirement to try all forms of treatment was not clearly and expressly disclosed in any case. The requirement to try self-administration injection in the base of the penis as a pre-condition for obtaining a refund was not disclosed in any of the individual cases. There were examples of individual cases in which patients were refused refunds by strict application of the refund term, even where they had changed their mind almost immediately after the call because they had been pressured into accepting treatment but then realised that they could not afford it or did not need it, where they had suffered unpleasant side effects, or where the initial medication which had attracted them to the treatment was not effective.
916 The failure of the salespeople to disclose the requirement that patients were required to try all forms of treatment including self-administered injections into the base of the penis was a serious concealment of an important element of the transaction. It prevented patients from exercising their informed consent to treatment. Such concealment is a marker of unconscionable conduct. It is more prejudicial to the consumer than where the consumer is provided with a document but cannot understand it. And yet that situation is a possible marker of unconscionable conduct which is referred to in s 51AB(2)(c) of the TPA and s 21(2)(c) of the ACL operating between 1 January 2011 and 1 January 2012. In the circumstances of the Annexure B patients, the concealment of the full requirements of the refund term was an unfair tactic. The patient was reassured by the reference to a refund and to a satisfaction guarantee that he was not taking a risk by signing up because, if the treatment did not work, he would get a refund. By AMI not disclosing the limitations of the refund policy it aided the selling process to its commercial advantage.
917 The refund term itself bound the patient to AMI when AMI had no legitimate interest in continuing the treatment program. It was not legitimate for AMI to force patients to continue to pay for treatment when they had a reason for changing their mind, when they had suffered unpleasant side effects, or when the initial medication had not worked. Patients who had to continue paying for their treatment programs in such circumstances, or suffer the penalty of paying the costs of termination, were exploited by AMI. Their medical interests were subordinated to the commercial interests of AMI. That was unconscionable conduct.
7.2.5 Enforcement of the AMI refund term
918 Mr Kyle gave evidence that, as a matter of policy, the AMI refund term was strictly enforced. The individual examples in the witness statements of the Annexure B patients attest to that fact. That meant that the unconscionable nature of the term, and the way it was imposed, were not mitigated in the way it was applied. The policy of strict enforcement of the term as part of the business system operated by AMI and NRM was also unconscionable conduct.
919 An essential element of the business system operated by AMI and NRM was that PE patients would be treated with clomipramine nasal spray or oral strips, and ED patients would be treated with apomorphine nasal spray or oral strips. AMI and NRM, in effect, required doctors to prescribe those medications as the first-line treatment for those conditions.
920 However, there was no proper scientific evidence that these forms of medications worked. Patients were not told that the medications were being used off-label and had not been proved to be effective. Nor were patients told that there were other medications generally used by doctors as first-line treatments which had been tested and had been shown to be effective. It was not in the interests of AMI and NRM to disclose these facts because patients probably would have been dissuaded from agreeing to the treatment programs if they had been told. On the other hand, it was in the best interests of the patients to be told these facts because it would have allowed them to make an informed decision about their medical options.
921 The Code recognises that there is a power imbalance in the doctor / patient relationship. Patients place trust in the integrity of doctors and rely on them to act openly, honestly, and in patients’ best interests. The use of the AMI and NRM medications without disclosing their limitations or the alternatives available was exploitation by AMI and NRM of their trusted position as providers of medical treatment to patients. The abuse of that relationship was unconscionable because it took advantage of the superior bargaining position of trusted medical advisors. The abuse of a superior bargaining position is relevant to a consideration of unconscionable conduct and is referred to in s 51AB(2)(a) of the TPA, s 21(2)(a) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(a) of the ACL in operation after 1 January 2012.
922 Concealing the full story about the limitations of the AMI and NRM medications was also an unfair tactic which aided AMI and NRM in pressuring men to agree to expensive treatments. The use of unfair tactics is a marker of possible unconscionable conduct which is referred to in s 51AB(2)(d) of the TPA, s 21(2)(d) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(d) of the ACL in operation after 1 January 2012.
923 AMI and NRM, in practical terms, required doctors to recommend treatment programs of 12 to 18 months. This was an essential part of the business system. They required salespeople to check with doctors as to the length of the program recommended by the doctors, but as the system was well known to the salespeople, they often recommended the length of treatment to patients without input from the doctor.
924 The reason AMI and NRM required doctors to recommend long-term treatment programs was that such contracts produced more revenue for AMI and NRM than short-term programs. Dr Vaisman told the doctors that the business could not survive on short-term programs. And AMI and NRM saw it as in their commercial interests to sell long-term programs.
925 There was no proper scientific evidence to support long-term treatment programs with AMI and NRM medications. The result was that patients were committed to a period of treatment which had no proper medical justification, but which entailed considerable cost to the patient. For AMI and NRM to require doctors to recommend long-term treatment programs without a proper medical reason for so doing was to exploit the patients for the commercial benefit of AMI and NRM. That conduct was unconscionable because AMI and NRM had no legitimate interest in having patients agree to long-term contracts. They were not providing a treatment for a period which had a verified medical reason. That was not legitimate business. The inclusion in such circumstances of terms which are not reasonably necessary to protect the legitimate interests of a supplier is akin to the possible marker of unconscionable conduct referred to in s 51AB(2)(b) of the TPA, s 21(2)(b) of the ACL operating between 1 January 2011 and 1 January 2012, and s 22(1)(b) of the ACL in operation after 1 January 2012.
926 As part of their business system, AMI and NRM marketed themselves as a medical institute. They offered diagnosis and treatment by doctors. As a result, the patients were led to believe and were entitled to trust that their conditions would be diagnosed and treated in accordance with accepted professional standards of medical practice. Doctors have a primary responsibility to safeguard the health and welfare of patients. The way in which AMI and NRM operated prevented their doctors from fulfilling this responsibility. Patients were not told of the unusual and limited role to be performed by the doctors
927 The doctors did not act in accordance with accepted professional standards of medical practice. In part that was a result of the fact that AMI and NRM governed the way doctors were expected to treat patients. In conducting the consultations the doctors acted on behalf of AMI and NRM, and AMI and NRM were responsible for the deficiencies in their conduct.
928 The AMI and NRM business model required doctors to consult by phone. The accepted professional standard for treatment of ED or PE, in the circumstances of patients of AMI and NRM, required a face-to-face consultation.
929 Doctors were, in practice, limited by AMI and NRM to prescribing clomipramine nasal spray or oral strips as the first-line treatment for PE, and to prescribing apomorphine nasal spray and oral strips as the first-line treatment for ED. In the majority of the Annexure B and C patient consultations, doctors prescribed those medications. The accepted professional standard for doctors required them to be free to make independent prescribing decisions from the range of medications available in Australia.
930 In each of the Annexure B and C patient consultations, where doctors recommended the length of treatment plans, they usually recommended treatment for 12 to 18 months. The doctors were, in effect, directed to recommend treatment programs of 12 to 18 months although there was no proper scientific basis for that length of treatment with the AMI and NRM medications. That denied them professional independence.
931 The way the AMI and NRM doctors consulted was seen in the evidence of the individual Annexure B and Annexure C patients. All of the 168 consultations with doctors were undertaken by phone. The Annexure B and Annexure C patients were offered treatment programs of 12 to 18 months. The doctors only prescribed medications available from AMI and NRM. In 150 of the consultations with Annexure B patients, and in all of the consultations with Annexure C patients, the doctors did not seek to diagnose the underlying cause of the presenting problem. None were referred to GPs or specialists. In most of the consultations with the Annexure B patients the doctors did not advise the patients adequately or at all of the common side effects of the medications.
932 The Code provided a normative standard for professional medical practice accepted by the community. It required doctors to make the welfare of the patient their primary concern. By not consulting face-to-face, by limiting the medications they would prescribe, by recommending long-term treatment programs, by failing to diagnose the cause of the condition, by failing to refer patients to a GP or specialist for underlying causes or presenting conditions, and by failing to advise or advise adequately about common side effects, the doctors failed to meet the standard of practice established by the Code. Instead, doctors were a cog in a commercial machine. In practice, and when taking into account the way in which the consultations were conducted, it was clear that the role of the doctors engaged by AMI and NRM was simply to produce a prescription for the AMI and NRM medications. They did this by conducting phone consultations for the purpose only of determining whether there was any reason why the AMI or NRM medications should not be prescribed. This was a limited and unusual function which did not conform to the conventional model of medical practice.
933 In Lux it was said at [23]:
The task of the Court is the evaluation of the facts by reference to a normative standard of conscience. That normative standard is permeated with accepted and acceptable community values.
The Code reflects accepted community values in relation to the proper relationship between doctor and patient. It was unconscionable for the doctors to treat patients in ways which did not meet the standards set by the Code, and it was unconscionable for AMI and NRM to require them to do so.
934 The doctors’ conduct had a commercial benefit for AMI and NRM. Phone consultations meant that AMI and NRM did not have to provide clinic facilities for the consultations. Limiting the medications which could only be obtained through AMI and NRM meant that they were free from competition by others offering treatment using those medications. Doctors could treat more patients if they were not required to provide a more comprehensive medical consultation and diagnose underlying causes such as cardiovascular disease or diabetes in the case of ED patients, or psychological issues in the case of PE patients, for example. And limiting discussion about side effects assisted in the selling process. In these ways the conduct of the doctors elevated the commercial interests of AMI and NRM above the medical interests of the patients. That also made the conduct unconscionable.
935 The doctors were in a position of influence by reason of the relationship with the patient. The Code recognises that there is a power imbalance in the doctor / patient relationship. Particularly in relation to the doctors limiting medications to the AMI and NRM medications and recommending long-term programs, AMI and NRM were in a strong bargaining position because patients trusted the integrity of the doctors and expected that they would act in the patients’ best interests. AMI and NRM took advantage of that superior bargaining position by having the doctors prescribe only AMI and NRM medications and having them recommend long-term treatment programs. That was unconscionable conduct by AMI and NRM.
7.2.9 The first NRM refund term
936 The first NRM refund term was a considerable improvement on the AMI refund term. But there were still penalties imposed on a patient for terminating the contract where it was reasonable for a patient to stop the treatment. For instance, where the medication was ineffective or caused adverse side effects, there was no good reason why the patient should be bound to the contract. Nonetheless, the patient was still required to pay for treatment in the 30-day-notice period. He was also required to pay an administration fee calculated on the total cost of the program. If an 18-month contract was cancelled in the first month, the administration fee was calculated on the whole 18-month period even though only one month had been utilised.
937 The patient was also obliged to pay for the cost of medications used or prepared for him. This applied even where the patient was not able to use the medication because of adverse side effects, where it had proved ineffective, or where he had not requested a further shipment of medication. The basis on which the cost of the medications was charged was not disclosed to the patient. The penalty imposed on the patient for terminating the contract placed a restriction on cancellation where the circumstances justified the patient bringing the treatment to an end. And the first NRM refund term did not limit the cost to the patient to the expense incurred by NRM in cancelling the contract.
938 Additionally, the term was provided to the patient by way of a recorded message in such a manner that it is probable that most patients would not have had an opportunity to understand its substance. Both factors made the first NRM refund term, and reliance on it, unconscionable.
939 The ACCC demonstrated that AMI and NRM designed a system of conducting business which included some general elements. The nature of the advertising, the process by which patients interacted with AMI and NRM, the role of salespeople and their remuneration by commission, the contract terms and relevant refund policies, and the length and cost of treatment programs, were all matters which AMI and NRM implemented systemically and marked the way they conducted business. These systemic features could be seen in the individual cases which the ACCC proved.
940 In addition, the 168 individual cases demonstrated some features which occurred in most of those cases, such as the offering of medications being limited to the AMI and NRM medications, the failure of doctors to diagnose an underlying cause or refer patients to GPs or specialists for those causes or presenting conditions, and the use of high-pressure selling techniques by salespeople. The individual cases also involved some features which were specific to those cases, such as the refusal of refunds in particular cases.
941 The conduct which has been found to have been unconscionable existed in most of the 168 individual instances. Certainly, the most serious unconscionable conduct existed in most cases. That is not to say that all of the unconscionable conduct existed in all 168 cases. However, all the conduct found to have been unconscionable was sufficiently widespread to justify the relief sought, as discussed later in these reasons for judgment.
942 Although the point has been made elsewhere in these reasons for judgment, it is useful to repeat at this point that the ACCC did not set out to show that the patients in each of the 168 cases suffered some disadvantage. Proof of unconscionable conduct depended on what AMI and NRM did, whether or not it had an effect on the individual patient. For instance, some of the Annexure B patients did not enter into agreements at all. That did not mean that, for example, in using high-pressure selling techniques in attempting to procure contracts, AMI and NRM did not engage in unconscionable conduct. The circumstances that no contract was concluded may bear on whether the Court would grant relief, but it does not prevent a finding that AMI and NRM engaged in unconscionable conduct. So much is clear from National Exchange and, now, s 21(4)(b) of the ACL.
7.2.11 Liability of Dr Vaisman
943 For reasons which have been explained in the course of these reasons for judgment, Dr Vaisman was the architect of the business model used by AMI and NRM. He designed the central features of the model, and either implemented each element or supervised such implementation. He controlled the advertising placed by AMI and NRM. He trained the salespeople and the doctors. He gave the instructions to the salespeople and the doctors to engage in the conduct which has been found to be unconscionable. He stipulated the period of treatment to be offered, and he determined what medications were to be available to the doctors to prescribe. He wrote the refund cheques. His evidence demonstrated that he had a very close familiarity of the way in which the contracts operated.
944 There could be no clearer case of a person who aided, abetted, counselled, or procured AMI and NRM to contravene s 51AB of the TPA and s 21 of the ACL, or who was directly or indirectly knowingly concerned in or party to the contraventions.
8. WAS THE FIRST NRM REFUND TERM AN UNFAIR CONTRACT TERM?
945 A term of a consumer contract is void if two characteristics are established, namely, that the term is unfair and the contract is a standard form contract (s 23(1) of the ACL).
946 It is presumed that the NRM contract is a standard form contract unless NRM proves otherwise (s 27(1)). In determining whether a contract is a standard form contact, the Court is required to take into account the factors referred to in s 27(2) of the ACL. The onus was on NRM to show that those circumstances did not exist. The circumstances were whether NRM had all or most of the bargaining power relating to the transaction, whether the contract was prepared by NRM before any discussion relating to the transaction occurred with a patient, whether the patients were in effect required to accept or reject the terms of the contract, other than the term concerning the cost of treatment, in the form in which they were presented, whether the patient was given an effective opportunity to negotiate the terms of the contract other than the term concerning the cost of treatment, and whether the terms of the contract took into account the particular characteristics of the patient or of the particular transaction.
947 NRM failed to show that these circumstances did not exist. In fact, the evidence positively established that NRM had a dominant bargaining position obtained by using high-pressure selling techniques. The pressure applied to the patients denied them the power to resist entering into the agreement. This was manifested in the NRM patients who said they felt pressured and in the case of some who tried to cancel their contracts immediately following the phone call. Patients did not have the chance to negotiate the terms of the contract apart from price. The terms were set by the parameters of the business model of NRM. The terms were set out in the instruction booklet sent to patients, often after they had entered into the contract, and were in the same form irrespective of the individual circumstances of the patient.
948 The next question is whether the refund term was unfair within the meaning of s 24(1) of the ACL. The section requires the Court to examine three factors.
949 One factor is whether the term was reasonably necessary in order to protect the legitimate interests of NRM (s 24(1)(b)). It is presumed that the term was not reasonably necessary to protect the legitimate interests of NRM unless NRM proved otherwise (s 24(4)). NRM did not so prove.
950 Then, the term is unfair if it would cause a significant imbalance in the parties’ rights and obligations arising under the contract (s 24(1)(a)), and would cause detriment, whether financial or otherwise, to the patient if it were to be applied or relied upon (s 24(1)(c)). These two factors may be considered together and in the light of one of the examples of an unfair term provided by s 25(1)(c). That section provides that a term which has the effect of penalising one party and not the other for terminating the contract may be unfair. As to the nature of a significant imbalance in rights, in Director General of Fair Trading v First National Bank plc [2002] 1 AC 481 at 494; [2001] UKHL 52, Lord Bingham said at [17] of a regulation in similar terms:
The requirement of significant imbalance is met if a term is so weighted in favour of the supplier as to tilt the parties’ rights and obligations under the contract significantly in his favour. This may be by the granting to the supplier of a beneficial option or discretion or power, or by the imposing on the consumer of a disadvantageous burden or risk or duty.
951 The NRM refund term required the patient to pay a 15 per cent administration fee, a pro-rata fee for the expired portion of the treatment, a pro-rata fee for the 30-day notice period, and the cost of medication supplied or prepared for the patient. The term operated whether the reason for the termination was a change of mind very soon after the phone consultation, a severe adverse side effect, or where the medication proved ineffective. The term thus caused detriment to the patient, if relied upon, within the meaning of s 24(1)(c). It also caused a significant imbalance in the parties’ rights and obligations because it had the effect of binding patients to continue treatment in disadvantageous circumstances, or alternatively suffer a financial penalty.
952 In determining whether a term of consumer contract is unfair, the Court must take into account the extent to which the term is transparent and also take into account the contract as a whole (s 24(2)). A term is transparent if it is expressed in reasonably plain language, is legible, is presented clearly, and is readily available to any party affected by the term (s 24(3)).
953 The NRM refund term lacked transparency to a significant extent. The basis on which the administration fee was calculated was not disclosed to the patient at all. The method of calculation of the cost of the medication was not disclosed to the patient at all. At the time that the agreement was made, the patient was told about the NRM refund term in a recorded message which suffered from the deficiencies outlined at [858] of these reasons for judgment. The patient was not provided with a written copy of the refund term until after the contract was entered into, save in the case of patients who attended clinics.
954 When regard is had to the contract as a whole, the unfairness of the term becomes incontrovertible. The contract provided for the supply of medications which were not regarded by the medical profession as the usual forms of treatment and there was no cogent evidence that they were effective to treat ED or PE. In those circumstances it was unfair to hold the patient to the agreement on penalty of payment of fees, the method of calculation of which was unknown, imposed in order to cancel the treatment.
955 For completeness, reference should be made to an argument raised by the respondents in relation to the ACCC’s pleading. The point had been raised several times in pre-trial case management hearings. It again appeared in the final written submissions.
956 The submission was stated thus:
100. The principal vice of the FASOC is that it employs a cumulative manner of pleading broad definitions, many conclusions (by repeated recourse to the phrase “in the circumstances”) without any supporting factual allegation and pays little or no regard to the requirements of the statutory provisions, which it is alleged that the corporate respondents have contravened. In turn, this affects the position of Dr Vaisman who is alleged to be accessorily liable in the most general of terms. In a short hand way the pleading is open-ended and reductionist: when analysed, the central question, whether AMI or NRM has acted unconscionably or whether NRM has employed an unfair term in a contract, is merely asserted as against the background of all the operational facets involved in the AMI business and the NRM business (leaving it to the Court to determine if any of those might be relevant).
957 The central criticism was directed to [17] of the FASOC which is set out at [80] of these reasons for judgment, but which is repeated below for convenience.
By:
(a) AMI selling or offering to sell the AMI treatments on the terms described at each of sub-paragraphs 8(a)-(d) [which alleged long term contracts, the AMI refund term, and the cost of medications], including to the patients identified at Annexure B;
(b) AMI's doctors doing or failing to do the things alleged at each of sub-paragraphs 10(a)-(g) [which alleged, inter alia, that the doctors only offered AMI medications, did not seek to diagnose underlying causes, and did not conduct physical examinations etc] in the course of consulting with the patients identified at Annexure B; and/or
(c) AMI's Clinical Co-ordinators doing or failing to do the things alleged at each of sub-paragraphs 13(a)-(d) [which alleged, inter alia, that clinical coordinators followed scripts, made statements about adverse medical and social consequences, the patient’s need for treatment, and the efficacy of AMI treatments, and failed to disclose that they were salespeople paid on commission] in the course of sales consultations with the patients identified at Annexure B;
in circumstances in which:
(d) AMI promoted its business as described at sub-paragraph 5(c) [which described the advertising of the AMI business];
(e) AMI sold AMI treatments or offered them for sale through the process described in sub-paragraphs 6(a)-(d) [which described the process whereby patients first spoke with a clinical coordinator, then a doctor, and then again spoke with the clinical coordinator];
(f) AMI made the representations described in paragraph 7 [which alleged that AMI represented that it would provide proper objective medical treatment to patients];
(g) the manner in which AMI's doctors conducted medical consultations was:
(i) contrary to the requirements and standards applicable to the proper, objective and appropriate diagnosis and medical treatment of male sexual dysfunction, and
(ii) involved the subordination of the patient's medical interests to the commercial interest of AMl,
as alleged at paragraph 11 [which made that same allegation]; and/or
(h) AMI knew that the men to whom it offered to sell and sold its treatments were vulnerable to its attempts to sell to them, as alleged at paragraph 15 [which alleged that patients were vulnerable],
each of the First Respondent and the Second Respondent has in trade or commerce in connection with the supply or possible supply of goods and services to consumers, engaged in conduct that is unconscionable within the meaning of, and in contravention of section 51AB of the Act.
958 Then in [102] of the final written submissions, the respondents argued:
The cumulative and alternative pleadings in 17(a) – (c) coupled with further cumulative and alternative pleadings in 17(d) – (h) make this pleading unfair and impossible to answer.
959 The submissions then examined the allegations made in each paragraph of the FASOC and contended that many of the allegations were vague, embarrassing, or ambiguous. Most of the criticisms amounted to claims for the evidence on which the ACCC intended to rely.
960 The ACCC responded to an early complaint about the pleadings by providing a 77-page document containing further and better particulars (the further and better particulars) which was, in many instances, a preview of the evidence to be relied upon by the ACCC. No reference to the effect of this document was made in the respondents’ final written submissions concerning the pleadings. An example illustrates the significance.
961 The respondents’ submissions complained that [11] of the FASOC, which is set out at [77] of these reasons, made serious allegations against doctors. The submissions continued, “the paragraph pleads a number of conclusions without pleading any of the “requirements and standards” which are said to have been contravened”. In [32] of the further and better particulars, the ACCC referred to and set out relevant extracts from the Code and the AMA’s position statements and code of ethics which were ultimately relied on at trial. The further and better particulars also stated that the matter would be proved by expert evidence. Written statements of Dr Pattison, Dr McRae, and Dr Walton were filed before trial and dealt in part with the subject.
962 Even if there was a basis for criticism of the pleading, which there was not, the ACCC explained the nature of its case on a number of occasions. This matter is discussed in detail in these reasons in Section 3, which is concerned with the scope of the ACCC’s case. Indeed, now that the case of the ACCC has been laid out at trial, it is clear that the detailed plan of its case was conceived by the time the proceeding was filed. The plan of the case was communicated in the pleadings and at case management hearings in the very way the case was conducted at trial.
963 The point of the present submission is not clear. It is too late in the day for any application that the pleading be struck out. Indeed, such an application was made on similar grounds in October 2011 and was then rejected. There is no basis for any argument that the respondents were not made aware from the beginning of the way in which the ACCC intended to put its case.
964 The respondents also submitted that the pleaded case, read literally, meant that all elements of the pleaded conduct and circumstances had to exist in respect of each Annexure B and C patient. If one element was not proved in an individual instance, the case of unconscionable conduct in respect of that patient failed on the pleadings. Thus, for instance, if a patient was adequately told about the side effects of a medication, then even if all the other elements of unconscionable conduct were present, the case would fail in respect of that patient.
965 However, the ACCC explained early in the proceeding that the elements pleaded in [17] were to be read distributively. That is an obvious reading. There is no doubt that the respondents were made aware of the way in which the case of the ACCC was to be put. The respondents’ argument is without foundation.
10. RELIEF AGAINST AMI, NRM AND DR VAISMAN
966 In reliance on the power of the Court in s 21 of the Federal Court of Australia Act 1976 (Cth) to make binding declarations of right, the ACCC sought declarations that AMI contravened s 51AB of the TPA and that Dr Vaisman aided, abetted, counselled or procured and was directly or indirectly knowingly concerned in and party to that contravention. It also sought declarations that NRM contravened s 21 of the ACL and that Dr Vaisman aided, abetted, counselled or procured and was directly or indirectly knowingly concerned in and party to that contravention.
967 The form of the declarations sought were as follows:
1 Each of the First and Second Respondents (together, AMI) during the period 2008 to 2010, in connection with the supply and possible supply of medications (AMI medications) and medical services for the treatment of male sexual dysfunction (together, the AMI treatments), engaged in conduct that was unconscionable in contravention of section 51AB of the Trade Practices Act 1974 (Cth) (Act) in the circumstances set out below:
(a) AMI promoted its business as the “Advanced Medical Institute” and advertised extensively across the media, including television, radio, newspapers and billboards, with such advertisements containing statements encouraging men suffering from male sexual dysfunction to ‘call the doctors at Advanced Medical Institute’ and thereby represented to men seeking treatment for male sexual dysfunction (patients) that they would receive a proper and objective medical assessment of their condition by a qualified medical doctor and would only be prescribed medication if consistent with that assessment;
(b) on contacting AMI, patients were offered the opportunity to be medically assessed in either a telephone consultation or a consultation at one of AMI’s clinics, and:
(i) patients who chose a telephone consultation spoke initially with a sales person who described themselves as a ‘Clinical Co-ordinator’, ‘Medical Co-ordinator’ or ‘Administrative assistant’ (Clinical Co-ordinator), then spoke to an AMI doctor, and then spoke to the Clinical Co-ordinator again;
(ii) patients who chose an in-clinic consultation met initially with a nurse at the clinic, then spoke to an AMI doctor by telephone, and then met with a Clinical Co-ordinator;
(c) the AMI doctors:
(i) in consultations with each of the patients identified in Annexure B to the Further Amended Statement of Claim (Annexure B Patients):
(A) did not offer or prescribe any medication other than the AMI medications, which the AMI doctors had not selected from the range of all medications available for prescription by Australian medical practitioners, and did not inform the patient that they prescribed only the AMI medications;
(B) conducted a consultation by telephone only and did not see or conduct any physical examination of the patient;
(C) recommended to the patient treatment plans, including plans of a length of 12 or 18 months; and
(D) did not seek to diagnose whether it would have been medically appropriate to refer the patient to a specialist or other medical practitioner for treatment or diagnosis; and
(ii) in consultations with 150 of the Annexure B Patients, did not seek to diagnose any underlying cause for the presenting problem and only questioned the patient to ascertain whether the AMI medications were contraindicated;
(iii) in consultations with 133 of the Annexure B patients, did not inform the patient about the common side-effects of the medications prescribed adequately or at all;
(d) the Clinical Co-ordinators:
(i) were salespeople who were not medically trained and were paid by AMI on a commission, calculated by reference to the cost of the treatment plans sold to patients (the longer the contract period, the greater the commission) but described themselves as ‘Clinical Co-ordinators’, ‘Medical Coordinators’ or ‘Administrative Assistants’;
(ii) in conversations with:
(A) each of the Annexure B patients, did not disclose to the patient that they were salespeople paid on a commission;
(B) 137 of the Annexure B patients, made statements to the patient concerning the efficacy of the AMI treatments;
(C) 151 of the Annexure B patients, made statements to the patient that he needed treatment or would suffer adverse medical and social consequences if he did not get treatment, including that his penis may shrink or he may become impotent; and
(D) 116 of the Annexure B patients, represented to the patient that he would be entitled to a refund of money paid if the AMI treatment purchased was ineffective, and did not disclose the conditions on which a refund would be offered under AMI’s ‘satisfaction guarantee’;
(e) AMI sold the AMI treatments to patients pursuant to contracts under
which:
(i) patients were bound to pay for the AMI treatments for a set period of time, whether or not the patients wished to continue with the AMI treatments, with payment either made upfront or by way of instalments;
(ii) if the AMI treatments did not successfully treat the patient’s condition or the patient experienced adverse side effects, then pursuant to the terms of its ‘satisfaction guarantee’ AMI refused to give the patient a refund or to cancel the contract unless the patient tried at least one option from each of the available delivery mechanisms for which the patient was not contraindicated (including injections to the base of the penis), after which AMI would deduct the cost of the medication supplied and a 15% administration fee from any refund given; and
(iii) patients who had telephone consultations were only provided with a copy of the terms of the ‘satisfaction guarantee’ after they had already agreed to purchase the AMI treatments; and
(f) AMI knew that:
(i) male sexual dysfunction is perceived by patients as embarrassing or humiliating; and
(ii) patients would have trust in the AMI doctors and would expect that those doctors would act in the patients’ best interests consistent with a doctor and patient relationship.
2 The Third Respondent (Vaisman):
(a) aided and abetted, counselled or procured; and
(b) was directly or indirectly knowingly concerned in, and party to,
the contraventions by AMI of section 51AB of the Act referred to in paragraph 1 of this Order by reason that he:
(c) was a director of each of the First and Second Respondents;
(d) was the Chief Executive Officer of the First and Second Respondents;
(e) had overall responsibility for the management of AMI;
(f) made all critical decisions concerning the business practices of AMI;
and
(g) oversaw the business practices of AMI.
3 Each of the Sixth and Seventh Respondents (together, NRM) in 2011 and 2012, in connection with the supply and possible supply of medications (NRM medications) and medical services for the treatment of male sexual dysfunction (together, the NRM treatments), engaged in conduct that was unconscionable in contravention of section 21 of the Australian Consumer Law (ACL), in the following circumstances:
(a) NRM promoted its business as the “Advanced Medical Institute” and advertised across the media, including radio, newspapers and billboards, with such advertisements containing statements encouraging men suffering from male sexual dysfunction to ‘call the doctors at Advanced Medical Institute’ and thereby represented to patients that they would receive a proper medical assessment of their condition by a qualified medical doctor and would only be prescribed medication if consistent with that assessment;
(b) on contacting NRM, patients were offered the opportunity to be medically assessed in either a telephone consultation or a consultation at one of NRM’s clinics, and:
(i) patients who chose a telephone consultation spoke initially with a sales person who described themselves as an ‘Administrative Assistant’, then spoke to an NRM doctor, and then spoke to the Administrative Assistant again;
(ii) patients who chose an in-clinic consultation met initially with a nurse at the clinic, then spoke to an NRM doctor by telephone, and then met with an Administrative Assistant;
(c) the NRM doctors:
(i) in consultations with each of the patients identified in Annexure C to the Further Amended Statement of Claim (Annexure C Patients):
(A) did not offer or prescribe any medication other than the NRM medications, which the [NRM] doctors had not selected from the range of all medications available for prescription by Australian medical practitioners, and did not inform the patient that they prescribed only the NRM medications;
(B) only conducted the consultation by telephone;
(C) recommended to the patient treatment plans, including plans of a length of 12 or 18 months;
(D) did not seek to diagnose any underlying cause for the presenting problem but only questioned the patient to ascertain whether the NRM medications were contraindicated; and
(E) did not adequately diagnose whether it would have been medically appropriate to refer the patient to a specialist or other medical practitioner for treatment or diagnosis; and
(ii) in consultations with 14 of the Annexure C Patients, did not adequately inform the patient about the common side-effects of the medications prescribed;
(d) the Administrative Assistants:
(i) were salespeople who were not medically trained and were paid on commission by NRM, calculated by reference to the cost of the treatment plans sold to patients (the longer the contract period, the greater the commission), but described themselves as ‘Administrative Assistants’ thereby representing that they were acting impartially in relation to the patients’ medical interests in selling the NRM treatments;
(ii) in conversations with:
(A) each of the Annexure C Patients, did not disclose to the patient that they were in fact salespeople paid on a commission; and
(B) 8 of the Annexure C Patients, made statements to the patient concerning the efficacy of the NRM treatments, the effect of which was to apply pressure to the patient to purchase the NRM treatments;
(e) NRM sold the NRM treatments to patients pursuant to contracts which bound patients to pay for treatment for a set period of time, including terms ranging from 12 to 24 months, whether or not the patients wished to continue with the treatment, with payment either made upfront or by way of instalments;
(f) The contracts which NRM entered into with patients between June 2011 and February 2012 contained a term (the Term) which provided that, on giving notice of termination of their contract to NRM, patients were only entitled to receive a refund after NRM had deducted the following amounts:
(A) an “administrative fee” of 15% of the entire initial cost of the contract, regardless of when the contract was cancelled;
(B) a pro-rated amount representing the “expired” period of the program prior to receipt of written notice (regardless of whether the patient uses NRM’s services or medications during that period);
(C) a pro-rated amount representing the next 30 days of the program after receipt of written notice (regardless of whether the patient used NRM’s services or medications during that period); and
(D) the cost of any medication already provided to or prepared for the patient, at a price not specified in the contract but determined by NRM; and
the terms of the contract were played over the telephone to patients
by the Administrative Assistants or provided to patients in NRM’s clinics; and
(g) NRM knew that:
(i) male sexual dysfunction is perceived by patients as embarrassing or humiliating; and
(ii) patients would have trust in the NRM doctors and would expect that those doctors would act in the patient’s best interests consistent with a doctor and patient relationship.
4 Vaisman:
(a) aided and abetted, counselled or procured; and
(b) was directly or indirectly knowingly concerned in, and party to,
the contraventions by NRM of section 21 of the ACL referred to in paragraph 3 of this Order by reason that he:
(c) was a director of each of the Sixth and Seventh Respondents;
(d) was the Chief Executive Officer of the Sixth and Seventh Respondents;
(e) had overall responsibility for the management of the NRM business;
(f) made or approved all critical decisions concerning the business practices of NRM; and
(g) oversaw the business practices of NRM.
968 A declaration will not be made unless there is a proper contradictor. AMI are in liquidation and the liquidators did not oppose the making of the declarations against AMI. The requirement that there be a proper contradictor does not, however, mean that the making of the declaration must be opposed. Parties may have opposing views about certain conduct and one party may agree to or not oppose a declaration being made. That does not mean that the Court lacks jurisdictional power to make the declaration. The proceeding will have resolved a pre-existing controversy: Australian Competition and Consumer Commission v MSY Technology Pty Ltd (2012) 201 FCR 378; [2012] FCAFC 56 at [17], citing French J (as he then was) in IMF (Australia) Ltd v Sons of Gwalia Ltd (administrator appointed) [2004] FCA 1390; (2004) 211 ALR 231 at [47]. It follows that the fact that AMI are in liquidation and that the liquidators do not oppose the making of the declarations are no impediments to the making of declarations against AMI.
969 The declarations in paragraphs 1 and 3 identify the elements of the conduct which made it unconscionable. The declarations reflect the findings of fact made in these reasons for judgment. In so doing the declarations serve a useful purpose. They indicate to NRM and Dr Vaisman the limits within which they may conduct the business. They also signal to others in the business community some of the boundaries which the legislative provisions establish in relation to acceptable selling techniques and contractual terms. The declarations also define some of the professional obligations required of doctors under the statute. The declarations thereby clarify the operation of the law. They also vindicate the regulatory function of the ACCC. Each of these outcomes also flows from the reasoning reflected in these reasons for judgment. It may be wondered why it is necessary to duplicate that effect by the making of declarations where they have no additional operative effect. However, the making of declarations in these circumstances has become an accepted practice. They have the practical virtue of encapsulating the outcome of the reasoning in a short form. Separation from the reasons of judgment perhaps gives them some apparent special authority.
970 Similarly, the declarations sought in respect of the conduct of Dr Vaisman reflect his involvement in the contraventions of s 51AB of the TPA and s 21 of the ACL as found in these reasons for judgment.
971 The reference to specific numbers of patients who were the subject of particular conduct in paragraphs 1(c)(ii) and (iii) and 1(d)(ii)(B), (C) and (D) of the proposed declaration is unnecessary.
972 To replace the specific numbers with a reference to “most” in each case reflects the facts. A declaration in those terms meets the purposes of making the declaration. It avoids the large task of creating precise criteria of the conduct in question and an analysis of each of the 168 cases in detail to establish whether the criteria have been met. Although the respondents did not contest the numbers proposed by the ACCC, some of those numbers are contestable without a precise definition of the conduct addressed.
973 Paragraph 3(d)(ii)(B) of the proposed declaration refers to eight Annexure C patients to whom statements were made about the efficacy of treatments. The evidence indicates that there were only six Annexure C patients in this position. The declaration should reflect the evidence by replacing the reference to eight patients with a reference to six patients.
974 Paragraph 3(e) of the proposed declaration states that NRM sold treatments to patients including for terms ranging from 12 to 24 months. The evidence before the Court did not establish that NRM sold treatments to patients for up to 24 months. The longest treatment program sold to an Annexure C patient was for 18 months. The declaration should reflect this evidence by replacing the reference to 24 months with a reference to 18 months.
975 Should any of the parties wish to argue against the alterations to the proposed declarations referred to in the previous two paragraphs, the party should apply to vary the terms of the declarations within 14 days and the matter will be listed for hearing on that issue.
976 The ACCC also sought a declaration that the first NRM refund term was an unfair term.
977 The proposed declaration was as follows:
5 The term contained in the consumer contracts between NRM and its patients made during the NRM period which provided that:
“Termination. Sexual dysfunction is a chronic condition and treatment can take some time. For this reason we stipulate that your contract with us for the period decided in the first consultation with the AMI doctor. You may cancel your treatment program with AMI at any time by giving AMI not less than 30 days notice. Cancelling your treatment program you will be entitled to a refund for the unexpired period of your treatment program less an administration fee of 15% and less the cost of any medication already provided to or prepared for you. No refund will be provided for the expired period of the treatment program or the 30 day notice period. All cancellation must be communicated to AMI in writing signed by you. Oral cancellation will not be accepted in any circumstances.”
was an unfair term within the meaning of sections 24 and 250 of the ACL because:
(a) the imposition of the administration fee was not reasonably necessary to protect NRM’s legitimate interests;
(b) the imposition of a charge for a pro-rated amount representing the expired portion of the treatment regardless of the quantity or effectiveness of the goods or services supplied by NRM to the patient during this period was not reasonably necessary to protect NRM’s legitimate interests;
(c) the imposition of a charge for a pro-rated amount for the additional thirty day notice period regardless of whether the patient desired to continue receiving goods or services for this period and whether any goods or services provided by NRM were effective was not reasonably necessary to protect NRM’s legitimate interests;
(d) the imposition of a charge for an amount for the cost of any medication already provided by NRM when the method of calculation was not disclosed to the patient and regardless of the actual cost to NRM of providing the medication or whether the medication was effective was not reasonably necessary to protect NRM’s legitimate interests;
(e) the imposition of the fees referred to in sub-paragraphs (a) to (d) was not transparent when delivered in a pre-recorded telephone message; and
(f) the uncertainty and cost of terminating a contract would cause a financial and other detriment to a patient wishing to terminate,
and is void by operation of section 24 of the ACL.
978 Section 250(1) of the ACL gives the Court power to declare that a term of a standard form contract is an unfair term.
979 NRM contended that a declaration should not be made because the termination provision is no longer used. However, the rationale for the making of a declaration, as stated in [968] – [969] of these reasons for judgment remain, and it is appropriate to make such a declaration.
980 There are further reasons which particularly justify the making of a declaration in respect of the unfair term. An unfair term will be void pursuant to s 23(1) of the ACL, and a declaration to that effect signals the legal consequence which flows from the finding of unfairness. In this way the declaration has an operative effect. Additionally, the making of a declaration is a prerequisite for the making of orders pursuant to s 239(1)(a)(ii) of the ACL for redress to third party consumers who have or may have suffered loss or damage from the unfair term.
981 The approach taken in the ACCC’s proposed order is to regard the whole of the first NRM refund term as unfair. The consequence is that the term is void and the patient has no express contractual right to terminate. An alternative approach would be to view each of the unfair elements as a term in itself. Then, each impost would be void but the right to terminate would remain. The conditions on which the termination could be exercised might be regulated by an order under s 239. In the end, nothing turns on this distinction in approach because the ACCC has proposed orders under s 239, albeit of a different nature than would be called for under the alternative approach.
982 The ACCC did not seek any injunctive relief against AMI. The companies are in liquidation and are not carrying on business.
983 The ACCC sought the following injunction against NRM:
6 Each of the Sixth and Seventh Respondents be permanently restrained whether by themselves, their servants or agents or otherwise, in trade or commerce, from:
(a) making an agreement with a patient for or in respect of the supply of medications or medical services for the treatment of male sexual dysfunction, unless the patient for whom the medications or medical services are intended has had a consultation with a duly qualified medical practitioner either in person or by video-link;
(b) making an agreement with a patient for the supply of medications or medical services for the treatment of male sexual dysfunction unless:
(i) before the agreement is made:
(A) the patient has been provided with a written statement by the Sixth and Seventh Respondents by post, electronic mail or in person:
a. setting out in plain English the terms of the agreement including a description of the medication or medical services to be provided, the total cost of the agreement, the proposed payment plan (if any), the period of treatment, and a statement that the patient has a right to terminate the agreement during the period of 5 business days commencing on the date on which the agreement is made (Cooling-Off Period);
b. stating that male sexual dysfunction may be a symptom of other medical conditions but AMI does not seek to diagnose those other medical conditions; and
c. stating that AMI does not provide general medical advice and that AMI’s doctors only consider whether the patient is suitable for AMI medications; and
(B) the Sixth and Seventh Respondents receive from the patient a written acceptance of the terms of the agreement; and
(ii) the agreement contains terms which:
(A) give the patient a right to terminate the agreement, by notice in writing to the Sixth and Seventh Respondents despatched during the Cooling-Off Period; and
(B) provide that if the patient exercises the right to terminate the agreement during the Cooling-Off Period, the agreement is taken to be rescinded by mutual consent with all payments made refunded; and
(C) provide that the patient may at any time after the Cooling-Off Period terminate the agreement by giving 14 days’ notice, and that once this notice has been provided, the Sixth and Seventh Respondents will cancel any direct debit arrangement referrable to the patient;
(c) making any statement or representation to any patient or prospective patient as to:
(i) the efficacy of NRM treatments;
(ii) the efficacy of any medications or medical services offered by parties other than the Sixth and Seventh Respondents; or
(iii) the patient’s need for the NRM treatments and any adverse consequences that might result if the patient:
(A) does not acquire the NRM treatments, or
(B) does not receive NRM treatments for male sexual dysfunction.
except if that statement is made directly to a patient or potential patient by a duly qualified medical practitioner during a consultation either in person or by video link;
(d) making an agreement with a patient for the supply of NRM treatments, unless during pre-contractual negotiations, the patient is offered an agreement with a term of no more than two months; and
(e) accepting in advance any payment or any other consideration from a patient in connection with the supply of NRM treatments for a future period of more than two months.
984 The power of the Court to grant injunctions where it finds a contravention of s 21 of the ACL is provided by s 232 as follows:
(1) A court may grant an injunction, in such terms as the court considers appropriate, if the court is satisfied that a person has engaged, or is proposing to engage, in conduct that constitutes or would constitute:
(a) a contravention of a provision of Chapter 2 [in which s 21 and s 23 are found], 3 or 4; or
(b) attempting to contravene such a provision; or
(c) aiding, abetting, counselling or procuring a person to contravene such a provision; or
(d) inducing, or attempting to induce, whether by threats, promises or otherwise, a person to contravene such a provision; or
(e) being in any way, directly or indirectly, knowingly concerned in, or party to, the contravention by a person of such a provision; or
(f) conspiring with others to contravene such a provision.
(2) The court may grant the injunction on application by the regulator or any other person.
(3) Subsection (1) applies in relation to conduct constituted by applying or relying on, or purporting to apply or rely on, a term of a consumer contract that has been declared under section 250 to be an unfair term as if the conduct were a contravention of a provision of Chapter 2.
(4) The power of the court to grant an injunction under subsection (1) restraining a person from engaging in conduct may be exercised:
(a) whether or not it appears to the court that the person intends to engage again, or to continue to engage, in conduct of a kind referred to in that subsection; and
(b) whether or not the person has previously engaged in conduct of that kind; and
(c) whether or not there is an imminent danger of substantial damage to any other person if the person engages in conduct of that kind.
(5) Without limiting subsection (1), the court may grant an injunction under that subsection restraining a person from carrying on a business or supplying goods or services (whether or not as part of, or incidental to, the carrying on of another business):
(a) for a specified period; or
(b) except on specified terms and conditions.
(6) Without limiting subsection (1), the court may grant an injunction under that subsection requiring a person to do any of the following:
(a) refund money;
(b) transfer property;
(c) honour a promise;
(d) destroy or dispose of goods.
(7) The power of the court to grant an injunction under subsection (1) requiring a person to do an act or thing may be exercised:
(a) whether or not it appears to the court that the person intends to refuse or fail again, or to continue to refuse or fail, to do that act or thing; and
(b) whether or not the person has previously refused or failed to do that act or thing; and
(c) whether or not there is an imminent danger of substantial damage to any other person if the person refuses or fails to do that act or thing.
985 The general scheme of the proposed injunction is designed to respond to the elements of the business model of NRM which involved unconscionable conduct and the use of unfair contract terms, and to ensure that such conduct is not repeated in the future. Injunctions of that nature fall within the statutory power: BMW Australia Limited v Australian Competition and Consumer Commission [2004] FCAFC 167; (2004) 207 ALR 452 at [36]. Whether the terms of the injunction are appropriate and whether the power should be exercised calls for an exercise of discretion by the Court.
986 One consideration in the exercise of discretion is whether the terms of the injunction provide a reasonable protection to patients in view of the way NRM has conducted business in the past.
987 The requirement of the face-to-face or video-link consultation provides a basic protection against substandard medical treatment, even though it cannot guarantee that doctors will act professionally in those consultations. The cooling-off period, the 14-day termination provision, and the requirement that NRM offer patients a contract with a maximum term of two months, and not accept payment in advance for a period of more than two months, give patients reasonable opportunities to withdraw from the treatment if they wish to do so.
988 The proposed injunction does not provide for immediate termination where the medication causes serious side effects. It may not be appropriate for patients in that situation to have a commitment to give 14 days’ notice where the cooling-off period has already expired. Similarly, it may not be appropriate for a 14-day notice period to apply where medication has proved ineffective. If it is regarded as appropriate to include a term to this effect, an application in writing should be made within 14 days to vary the injunction in that regard.
989 Proposed paragraph 6(b)(ii)(C) provides for the cancellation of direct debit payments where a patient gives 14 days’ notice of termination. It makes no provision for refund where the patient pays up front for the two-month contract. Again, if any of the parties regard it as appropriate to include such a term, that party should make an application in writing within 14 days to vary the injunction in that regard.
990 The proposed injunction requires NRM to disclose certain information to patients prior to any contract being concluded. The NRM business model rested on manipulating patients by playing on their vulnerability. This was done by emphasising the dangers of their condition, playing on the patients’ fears of sexual inadequacy, exaggerating the chances that the treatments would be effective, and dismissing the effectiveness of alternative treatments. These matters are addressed in [6(c)] of the proposed injunction.
991 But NRM also failed to disclose that apomorphine and clomipramine were not first-line treatments for ED and PE respectively and were being used off-label. In its interactions with patients, NRM also minimised the side effects of the medication. It may be that these matters should be disclosed as part of the procedure designated in [6(b)(i)] of the proposed injunction.
992 It may also be appropriate in this case to require a report to the ACCC by an independent auditor after, say six months, as to compliance by NRM in accordance with the injunction.
993 If it is regarded as appropriate to include provisions in accordance with the remarks made in the last two paragraphs, an application in writing should be made within 14 days to vary the injunction in those ways. The invitation to consider whether the injunction should be varied does not mean that any application made in response will necessarily be granted. Rather, the Court would hear argument and determine the issues following a consideration of the submissions made by the parties.
994 The exercise of discretion should also take into account the impact of the injunctions on NRM. Although negative in form, the injunctions are in substance mandatory injunctions. Caution should be exercised in making orders of that type.
995 The injunctions impose significant changes for the operation of the NRM business. Despite this, NRM did not make any submissions of substance contesting the terms of the injunctions against it. The failure to make such submissions has particular significance because the Court directly raised with Mr Shrestha the potential impact on NRM of injunctions requiring face-to-face consultations. He explained that in 2001 AMI operated 38 clinics, but gradually reduced the number because the number of patients attending clinics declined [TS 2026]. Mr Shrestha said that NRM would not be able to trade if it had to provide face-to-face consultations. This bald assertion was not persuasive. NRM did not seek to make a case that such an order or an order for consultation via video-link would cause undue hardship on it. The evidence demonstrated that a significant proportion of patients in the NRM period attended clinics. Those clinics did not provide doctor consultations on-site but only by phone. NRM did not establish that providing doctors on-site or by video-link would place an unreasonable burden on it.
996 Paragraphs 6(b)(i)(A)(b) and (c) of the proposed injunction require a written statement to be provided to prospective patients stating that, inter alia, AMI does not seek to diagnose underlying causes of the condition. These references should be to NRM, given that the injunctions are to be made against the sixth and seventh respondents. The final form of orders will reflect this.
997 The ACCC sought an injunction against Dr Vaisman in the following terms:
7 Vaisman be restrained, for a period of seven years from the date of this Order (unless otherwise specified below), in trade or commerce, from:
(a) being in any way, directly or indirectly, knowingly concerned in, or a party to, or aiding and abetting, counselling or procuring conduct of the kind restrained in paragraph 6 above; and
(b) from having a role in connection with training, supervising, counselling or terminating employees, agents or contractors of the Sixth and Seventh Respondents and their related bodies corporate.
998 The final written submissions of the respondents concerning Dr Vaisman argued against this injunction as follows:
230. The injunction in paragraph 7(a) is for the period of 7 years. Dr Vaisman is not well and is in his late sixties. He graduated in medicine in 1969 and has been involved in medicine for approximately 45 years. His role in the operational aspects of the business now is minimal. To prevent him from having any role in the business is inequitable and excessively punitive.
231. Dr Vaisman has clearly been passionate about assisting men seek treatment for sexual dysfunction. It is highly likely that his company has assisted in removing the stigma from this condition. There is no evidence that he ever wanted to cause any harm to any patient.
232. No order ought to be made in relation to Dr Vaisman
999 Mr Shrestha gave evidence in July 2013 about the role Dr Vaisman performed for NRM at that time. He responded to a question from the Court as follows:
HIS HONOUR: Just on that point, can you describe generally to me the role that [Dr Vaisman] plays and how it interlocks with the management team now in NRM?
MR SHRESTHA: Dr Vaisman, he mainly focuses on the medical side of the business, research and development, dealing with the doctors, training with the doctors. The rest of the operation, besides marketing, I am the person who makes all the decisions. The system, the CMS system is designed by me and the programmers has helped me to code it into the – put it into frame. With the financial side, I’m the person who makes all the decisions. And also a signatory of the council, I don’t take any approvals of Dr Vaisman of doing any fund transfers or paying any suppliers, creditors, putting orders. So day-to-day operations, I am the person who is in charge, unless there is a medical concern and that’s where I seek assistance from Dr Vaisman.
…
… he has been very sick recently and he has had very – issues with his health and also the – he is kept busy with his other family commitments and sickness at home. So all the business aspect of the NRM, I’m – I’m the one who’s dealing with the most.
…
And it’s actually increasing on a daily basis. So now in a nutshell, I’m the person who makes almost all the decisions.
[TS 1963 – 1964]
1000 And Dr Vaisman gave evidence thus:
HIS HONOUR: Dr Vaisman, how old are you now?
DR VAISMAN: 68.
HIS HONOUR: 68. And what do you see as your personal plan for involvement in the business in the next five years? What do you hope to do in that time?
DR VAISMAN: Definitely my health, not like it was even five years ago. Particularly my memory is suffering after this pneumonia – what I had half a year, particularly. And it became very difficult for me to run this business, and I’m considering to step down and to be the consultant for the business.
HIS HONOUR: And when would you plan to do that?
DR VAISMAN: This year [2013].
[TS 1855]
1001 The ACCC observed that the terms of the draft injunction do not intend to exclude Dr Vaisman from assisting NRM in a research capacity.
1002 In all of these circumstances, the terms of the proposed injunction do not impose undue hardship on Dr Vaisman. They may only crystallise his own intention to retreat from active involvement in the business.
1003 In any event, the injunction is most important for the protection of the public. Dr Vaisman was the architect of the business model and he operated AMI and NRM in accordance with that model. He devised a selling technique which manipulated the fears of patients suffering from ED and PE. He developed medication and delivery systems which had no proven efficacy and sold them as if they did. In practice, he controlled the prescribing practices of doctors which were contrary to accepted medical practice. He utilised contracts which locked patients into unjustified treatment periods. And he oversaw a refund system which operated in a way that deterred patients from claiming their money back when the circumstances justified their claims. Dr Vaisman was the central player in each of the elements of unconscionable conduct which have been found by the Court. He carries prime responsibility for the operation.
1004 The attempt made in [231] of the respondents’ final written submissions to paint Dr Vaisman as a public benefactor is not supported by the facts. The evidence established that Dr Vaisman used his scientific knowledge together with a certain entrepreneurial skill to design a system which would enable NRM to exploit patients so that it could profit at their expense. Dr Vaisman had an interest in the scientific aspects of treatment, but essentially for the value they had to produce profit for himself through AMI and NRM.
1005 Dr Vaisman’s attitude in the witness box demonstrated that unless he was restrained by orders of the Court, he would continue the business model he had designed. He stuck doggedly to beliefs about the treatments offered which were not supported by the literature on which he himself relied. He did not acknowledge any disadvantage caused to patients in the operation of the system despite many instances of patients who were placed under financial and emotional stress by the contracts into which they had entered. Dr Vaisman demonstrated no insight into the criticisms which gave rise to the proceeding. There is no realistic chance that he would change his views, and hence his actions, without the intervention of the Court.
1006 That Dr Vaisman will not be deterred from pursing his commercial interests without restraint imposed by the Court is illustrated by his involvement in cases in this Court in 1996, 2002, and 2004, in which relief including injunctions was granted, although in 2002 by consent, in respect of advertisements and representations about the treatments for sexual dysfunction offered by companies operated by Dr Vaisman.
1007 The duration of the orders effectively excludes Dr Vaisman from the conduct of the business of NRM for the rest of his working life. That is necessary to protect the public from his actions. Were he a younger man, a longer period of exclusion would have been justified given the seriousness of the conduct which has been found against him.
10.3 Refund to Annexure C patients
1008 The ACCC sought an order as follows:
10. Pursuant to section 239 of the ACL, the Sixth and Seventh Respondents must refund the total amount of money paid by the Annexure C patients, except for Patients 7 and 9, pursuant to their contract with NRM less any refund already provided by NRM.
1009 The order relies on the powers provided by s 239(1) – (4) of the ACL as follows:
(1) If:
(a) a person:
(i) engaged in conduct (the contravening conduct) in contravention of a provision of Chapter 2 [in which s 21 and s 23 appear], Part 3‑1, Division 2, 3 or 4 of Part 3‑2 or Chapter 4; or
(ii) is a party to a consumer contract who is advantaged by a term (the declared term) of the contract in relation to which a court has made a declaration under section 250; and
(b) the contravening conduct or declared term caused, or is likely to cause, a class of persons to suffer loss or damage; and
(c) the class includes persons who are non‑party consumers in relation to the contravening conduct or declared term;
a court may, on the application of the regulator, make such order or orders (other than an award of damages) as the court thinks appropriate against a person referred to in subsection (2) of this section.
(2) An order under subsection (1) may be made against:
(a) if subsection (1)(a)(i) applies—the person who engaged in the contravening conduct, or a person involved in that conduct; or
(b) if subsection (1)(a)(ii) applies—a party to the contract who is advantaged by the declared term.
(3) The order must be an order that the court considers will:
(a) redress, in whole or in part, the loss or damage suffered by the non‑party consumers in relation to the contravening conduct or declared term; or
(b) prevent or reduce the loss or damage suffered, or likely to be suffered, by the non-party consumers in relation to the contravening conduct or declared term.
(4) An application under subsection (1) may be made at any time within 6 years after the day on which:
(a) if subsection (1)(a)(i) applies—the cause of action that relates to the contravening conduct accrued; or
(b) if subsection (1)(a)(ii) applies—the declaration is made.
1010 The Court may make an order pursuant to s 243(d) that a person referred to in s 239(1)(a) refund money to a non-party consumer. The Court may have regard to the conduct of the person and the non-party consumer since the contravention occurred (s 240(1)).
1011 Each of the Annexure C patients sought refunds in circumstances in which, but for the unconscionable conduct and / or the unfair term, they either would not have entered into the agreement or they should have received their money back. On that basis there should be an order that NRM refund the amounts paid. The Court may take into account the refunds made by NRM since the contraventions in calculating the balance of the refunds payable to the relevant Annexure C patients. The amount of the refunds already paid to those patients should be taken into account. No refunds are sought in relation to NRM patients 7 and 9 who were officers of the ACCC.
1012 The respondents argued that no order should be made under s 239(1) because no loss or damage had been particularised. The circumstances of each of the NRM patients are set out in their witness statements and, in some cases, further evidence emerged in cross-examination. Those circumstances demonstrated that the patients suffered loss or damage by entering into the contracts with NRM. The damage suffered requires that the agreements be undone by the Court. By the Court requiring the refund of monies paid, the patients are put into the financial position as if they had not had been subjected to the contravening conduct. The damage suffered was entering into the contract with NRM and no further particularisation is necessary. It may be that only a more limited order would be justified under s 239(1)(a)(ii), because the loss and damage caused by the unfair term may be different from the loss and damage resulting from the unconscionable conduct more generally. The loss and damage suffered as a result of the unfair term was the inability to cancel the contract without incurring a financial penalty. An order which allows the patient to cancel the contract without incurring a penalty provides the redress referred to in s 239(3) of the ACL. In this case, that form of order is not required because the form of order sought by the ACCC, which should be granted, addresses the loss and damage resulting from the unconscionable conduct more broadly.
1013 The ACCC sought an order that NRM publish a corrective notice. The form of the proposed order and notice are as follows:
The Sixth and Seventh Respondents cause to be published, at their own expense, within 21 days of the date of this Order, a notice in the form contained in Annexure A to this Order (website notice) on its website located at http://www.amiaustralia.com.au (AMI website) and, if the URL of such website is replaced, changed or redirected to another website, on the corresponding website, for a continuous period of 90 days and use its best endeavours to ensure that:
(a) the website notice shall be viewable by clicking a ‘click-through’ icon located on the AMI website;
(b) the ‘click-through’ icon referred to in the previous sub-paragraph is located at the top of the homepage of the AMI website and any corresponding websites;
(c) the ‘click-through’ icon shall appear as follows, with the words printed prominently in bold red text, in a font size no smaller than 14-point, on a white background:
Unconscionable Conduct by Advanced Medical Institute (AMI) –
Notice Ordered by Federal Court of Australia.
Click Here
UNLAWFUL CONDUCT BY ADVANCED MEDICAL INSTITUTE
Following legal action by the Australian Competition and Consumer Commission, the Federal Court of Australia has ruled that NRM Corporation Pty Ltd and NRM Trading Pty Ltd, (together, NRM), engaged in unconscionable conduct in contravention of section 21 of the Australian Consumer Law in its dealings with men seeking treatment for male sexual dysfunction in 2011 and 2012.
NRM promoted its business as the “Advanced Medical Institute”. It represented that its patients would receive a proper medical assessment of their condition by a qualified medical doctor and would only be prescribed medication if consistent with that assessment. It knew that its patients were vulnerable by virtue of their condition, and that patients would expect NRM and its doctors to act in their best interests consistent with a doctor/patient relationship. In fact, a number of NRM’s patients:
• were not physically examined by NRM’s doctors;
• were only prescribed NRM’s treatments, which were not selected from all relevant and available treatments in Australia;
• were not informed that NRM’s doctors would only prescribe treatments from NRM’s limited range of treatments, or that other treatments were available;
• were not adequately informed of the side effects of NRM’s treatments;
• were not properly diagnosed with the underlying cause of their condition, but rather were only questioned as to whether NRM’s treatments were contraindicated;
• were not referred to specialists or advised to see their general practitioner;
• were misled by NRM’s salespeople, who described themselves as
“Administrative Assistants” but in fact were paid on commission;
• were told by the salespeople that they would suffer adverse medical and social consequences if they did not purchase and use the NRM treatments;
• were told that they would receive a refund under NRM’s refund policy if the NRM treatments were ineffective, when in fact any refund was subject to significant limitations and deductions that were not adequately disclosed to the patient when they entered into the contract; and
• were sold NRM treatments pursuant to contracts which bound the patients to pay for treatment for a set period of time, including terms ranging from 12 to 24 months, whether or not the patients wished to continue with the treatment.
The Court also found that NRM’s refund policy was an unfair term within the meaning of sections 24 and 250 of the ACL, because the imposition of fees and charges deducted from any refund to a patient was not transparent, was not necessary to protect NRM’s interests and would cause financial and other detriment to patients. The consequence of this declaration is that the refund policy is void.
The Court has also found that Jack Vaisman, Chief Executive Officer of NRM, was knowingly concerned in the unlawful conduct of NRM.
The Court has ordered declarations, injunctions and the refund of money to patients. A copy of the judgment, which details the Court’s findings and orders is located at [insert URL]
NRM purchased the AMI business from Advanced Medical Institute Pty Limited and AMI Australia Holdings Pty Ltd (together, AMI) in June 2011. The Court also declared that AMI had engaged in unconscionable conduct.
This notice has been placed because of an order of the Federal Court of Australia in a proceeding commenced by the Australian Competition and Consumer Commission.
[Emphasis added.]
1014 The power to make such orders is found relevantly in s 246(1) and (2)(c) and (d) of the ACL as follows:
(1) A court may, on application of the regulator, make one or more of the orders mentioned in subsection (2) in relation to a person who has engaged in conduct that:
(a) contravenes a provision of Chapter 2, 3 or 4; or
(b) constitutes an involvement in a contravention of such a provision.
(2) The court may make the following orders in relation to the person who has engaged in the conduct:
…
(c) an order requiring the person to disclose, in the way and to the persons specified in the order, such information as is so specified, being information that the person has possession of or access to;
(d) an order requiring the person to publish, at the person’s expense and in the way specified in the order, an advertisement in the terms specified in, or determined in accordance with, the order.
1015 The purpose of such an order is to advise visitors to the website of the outcome of the proceeding and thereby aid in the enforcement of the orders of the Court and prevent repetition of NRM’s contravening conduct: Australian Competition and Consumer Commission v Real Estate Institute of Western Australia Incorporated (1999) 95 FCR 114; [1999] FCA 1387 at [49].
1016 The terms of the proposed notice are appropriate for these purposes, save for two issues which are discussed below. The respondents did not mount any argument against the Court making an order in this form.
1017 First, in the first highlighted passage in the proposed corrective notice it is stated that a number of NRM’s patients “were told by the salespeople that they would suffer adverse medical and social consequences if they did not purchase and use the NRM treatments”. However, the ACCC did not allege this in its pleading. Such a finding was not made in these reasons for judgment nor is it recorded in the declarations arising from them. A statement in those terms should not be included.
1018 Second, for the reasons explained in [974], the second highlighted passage in the proposed corrective notice should refer to contracts of 18 months rather than 24 months.
11. RELIEF AGAINST DR LONERGAN
1019 In June 2012, Dr Lonergan and the ACCC settled the proceeding between them. By that agreement Dr Lonergan was to take no further part in the proceeding except as a witness, there were to be no costs ordered between them, and Dr Lonergan agreed to the making of a declaration and injunction against him. The orders to which he agreed were similar to the orders sought against AMI. As the proceeding against AMI was continuing, it was not appropriate to make orders by consent without determining the case against AMI. Consequently, Dr Lonergan and the ACCC agreed that if the relevant orders were made against AMI after the trial, then the agreed orders would also be made against Dr Lonergan. In the meantime, Dr Lonergan gave an undertaking in effect not to engage in the conduct alleged against him.
1020 The evidence in the proceeding against AMI demonstrated that the agreed declaration and injunction against Dr Lonergan were justified. The form of the agreed orders was updated by the ACCC and Dr Lonergan and orders will be made in accordance with the minute dated 18 May 2014. Dr Lonergan will also be discharged from the undertaking given to the Court in the form of the document dated 21 June 2012.
1021 In view of the outcome of this proceeding and the principle that costs should follow the event, the Court will order that the third, sixth, and seventh respondents pay the ACCC’s costs of the proceeding, except for the ACCC’s costs of and incidental to the proceeding against the fourth and fifth respondents.
1022 However, in the course of the trial there were various discussions about potential costs issues. They were not addressed in final submissions. From one of those discussions it may have been assumed that the detailed consideration of costs should await the outcome of the determination of issues of liability.
1023 The discussions in the course of the hearing related to the way in which the ACCC had structured its case. By relying on the 168 particular instances of unconscionable conduct as part of its case, the ACCC created the need for a large amount of evidence. At various times I raised the question whether it was necessary to multiply the instances of conduct rather than selecting several examples as representative. I suggested that declarations and injunctions in respect of several instances would serve the purpose of vindicating the ACCC’s claim of unconscionable conduct as effectively as relief based on the multitude of instances. In response, the ACCC explained that it was concerned that if too few cases were selected the claim for relief might be jeopardised because the respondents might argue that the selected consultations could be explained as aberrant and out of the ordinary, and consequently not deserving of declaratory or injunctive relief.
1024 On many occasions I pressed the parties to make an agreed selection of representative cases to render the proceeding more manageable. The parties reported that efforts had been made but had not yielded results. In an attempt to limit the scope of the Court’s enquiry, the ACCC made detailed final written submissions on 17 Annexure B patients and all of the Annexure C patients, but maintained its position that all the consultations were in issue.
1025 From what occurred in Court it appears that this situation may have arisen from the respondents’ failure to agree to a selection of representative patients. The respondents insisted that the case involved separate instances of conduct and that each transaction had to be examined. They criticised the way in which the group of Annexure B patients had been selected. Dr Berry said in her first statement that the consultations in which she was involved were atypical. The respondents were committed to contesting every consultation and sought to demonstrate that, taking account of all of the circumstances, the conduct in respect of each patient was not unconscionable. In this exercise the respondents failed. The way in which the parameters of the case were set thus may have resulted from a choice made by the respondents.
1026 Although there is probably no scope for further discussion, the parties should be given leave to apply within 14 days to vary the costs order if they have arguments about costs which they wish to put to the Court.
I certify that the preceding one thousand and twenty six (1026) numbered paragraphs are a true copy of the Reasons for Judgment herein of the Honourable Justice North. |
Associate: